Care and support statutory guidance
Updated 22 July 2025
Using the Care Act guidance
This publication is currently under review
The Health and Care Act 2022 revoked Schedule 3 and amended Section 74 of the Care Act 2014 on 1 July 2022. This means that certain parts of this guidance are out of date and in the process of being updated to reflect the relevant statutory changes.
How to search the guidance
On your keyboard, press Ctrl + F on a PC or Command + F on a Mac
This will open a search box in the top right hand corner of the page. Type the word you are looking for in the search bar and press enter. The word will then be highlighted in yellow where every it appears in the guidance. Click on the enter key to move to the next word found.
How to print a copy of the guidance
On your keyboard, press Ctrl + P on a PC or Command + P on a Mac
You have an option to print the entire Care Act guidance (approximately 375 pages) or select a page range.
General responsibilities and universal services
This section includes chapters on:
1. Promoting wellbeing 2. Preventing, reducing or delaying needs 3. Information and advice 4. Market shaping and commissioning of adult care and support 5. Managing provider failure and other service interruptions
1. Promoting wellbeing
This chapter provides guidance on section 1 of the Care Act 2014 and covers:
- definition of wellbeing
- promoting wellbeing
- wellbeing throughout the Care Act
1.1 The core purpose of adult care and support is to help people to achieve the outcomes that matter to them in their life. Throughout this guidance document, the different chapters set out how a local authority should go about performing its care and support responsibilities. Underpinning all of these individual ‘care and support functions’ (that is, any process, activity or broader responsibility that the local authority performs) is the need to ensure that doing so focuses on the needs and goals of the person concerned.
1.2 Local authorities must promote wellbeing when carrying out any of their care and support functions in respect of a person. This may sometimes be referred to as ‘the wellbeing principle’ because it is a guiding principle that puts wellbeing at the heart of care and support.
1.3 The wellbeing principle applies in all cases where a local authority is carrying out a care and support function, or making a decision, in relation to a person. For this reason it is referred to throughout this guidance. It applies equally to adults with care and support needs and their carers [footnote 1].
1.4 In some specific circumstances, it also applies to children, their carers and to young carers when they are subject to transition assessments (see chapter 16 on transition to adult care and support).
Definition of wellbeing
1.5 ‘Wellbeing’ is a broad concept, and it is described as relating to the following areas in particular:
- personal dignity (including treatment of the individual with respect)
- physical and mental health and emotional wellbeing
- protection from abuse and neglect
- control by the individual over day-to-day life (including over care and support provided and the way it is provided)
- participation in work, education, training or recreation
- social and economic wellbeing
- domestic, family and personal
- suitability of living accommodation
- the individual’s contribution to society
1.6 The individual aspects of wellbeing or outcomes above are those which are set out in the Care Act, and are most relevant to people with care and support needs and carers. There is no hierarchy, and all should be considered of equal importance when considering ‘wellbeing’ in the round.
Promoting wellbeing
1.7 Promoting wellbeing involves actively seeking improvements in the aspects of wellbeing set out above when carrying out a care and support function in relation to an individual at any stage of the process from the provision of information and advice to reviewing a care and support plan. Wellbeing covers an intentionally broad range of the aspects of a person’s life and will encompass a wide variety of specific considerations depending on the individual.
1.8 A local authority can promote a person’s wellbeing in many ways. How this happens will depend on the circumstances, including the person’s needs, goals and wishes, and how these impact on their wellbeing. There is no set approach – a local authority should consider each case on its own merits, consider what the person wants to achieve, and how the action which the local authority is taking may affect the wellbeing of the individual.
1.9 The Act therefore signifies a shift from existing duties on local authorities to provide particular services, to the concept of ‘meeting needs’ (set out in sections 8 and 18 to 20 of the Act). This is the core legal entitlement for adults to care and support, establishing one clear and consistent set of duties and power for all people who need care and support.
1.10 The concept of meeting needs recognises that everyone’s needs are different and personal to them. Local authorities must consider how to meet each person’s specific needs rather than simply considering what service they will fit into. The concept of meeting needs also recognises that modern care and support can be provided in any number of ways, with new models emerging all the time, rather than the previous legislation which focuses primarily on traditional models of residential and domiciliary care.
1.11 Whenever a local authority carries out any care and support functions relating to an individual, it must act to promote wellbeing – and it should consider all of the aspects above in looking at how to meet a person’s needs and support them to achieve their desired outcomes. However, in individual cases, it is likely that some aspects of wellbeing will be more relevant to the person than others. For example, for some people the ability to engage in work or education will be a more important outcome than for others, and in these cases ‘promoting their wellbeing’ effectively may mean taking particular consideration of this aspect. Local authorities should adopt a flexible approach that allows for a focus on which aspects of wellbeing matter most to the individual concerned.
1.12 The principle of promoting wellbeing should be embedded through the local authority care and support system, but how the local authority promotes wellbeing in practice will depend on the particular function being performed. During the assessment process, for instance, the local authority should explicitly consider the most relevant aspects of wellbeing to the individual concerned, and assess how their needs impact on them. Taking this approach will allow for the assessment to identify how care and support, or other services or resources in the local community, could help the person to achieve their outcomes. During care and support planning, when agreeing how needs are to be met, promoting the person’s wellbeing may mean making decisions about particular types or locations of care (for instance, to be closer to family). To give another example, the concept of wellbeing is very important when responding to someone who self-neglects, where it will be crucial to work alongside the person, understanding how their past experiences influence current behaviour. The duty to promote wellbeing applies equally to those who, for a variety of reasons, may be difficult to engage.
1.13 The wellbeing principle applies equally to those who do not have eligible needs but come into contact with the system in some other way (for example, via an assessment that does not lead to ongoing care and support) as it does to those who go on to receive care and support, and have an ongoing relationship with the local authority. It should inform the delivery of universal services which are provided to all people in the local population, as well as being considered when meeting eligible needs. Although the wellbeing principle applies specifically when the local authority performs an activity or task, or makes a decision, in relation to a person, the principle should also be considered by the local authority when it undertakes broader, strategic functions, such as planning, which are not in relation to one individual. As such, wellbeing should be seen as the common theme around which care and support is built at local and national level.
1.14 In addition to the general principle of promoting wellbeing, there are a number of other key principles and standards which local authorities must have regard to when carrying out the same activities or functions:
-
a) The importance of beginning with the assumption that the individual is best-placed to judge the individual’s wellbeing. Building on the principles of the Mental Capacity Act, the local authority should assume that the person themselves knows best their own outcomes, goals and wellbeing. Local authorities should not make assumptions as to what matters most to the person.
-
b) The individual’s views, wishes, feelings and beliefs. Considering the person’s views and wishes is critical to a person-centred system. Local authorities should not ignore or downplay the importance of a person’s own opinions in relation to their life and their care. Where particular views, feelings or beliefs (including religious beliefs) impact on the choices that a person may wish to make about their care, these should be taken into account. This is especially important where a person has expressed views in the past, but no longer has capacity to make decisions themselves.
-
c) The importance of preventing or delaying the development of needs for care and support and the importance of reducing needs that already exist. At every interaction with a person, a local authority should consider whether or how the person’s needs could be reduced or other needs could be delayed from arising. Effective interventions at the right time can stop needs from escalating, and help people maintain their independence for longer (see chapter 2 on prevention).
-
d) The need to ensure that decisions are made having regard to all the individual’s circumstances (and are not based only on their age or appearance, any condition they have, or any aspect of their behaviour which might lead others to make unjustified assumptions about their wellbeing). Local authorities should not make judgments based on preconceptions about the person’s circumstances, but should in every case work to understand their individual needs and goals.
-
e) The importance of the individual participating as fully as possible. In decisions about them and being provided with the information and support necessary to enable the individual to participate. Care and support should be personal, and local authorities should not make decisions from which the person is excluded.
-
f) The importance of achieving a balance between the individual’s wellbeing and that of any friends or relatives who are involved in caring for the individual. People should be considered in the context of their families and support networks, not just as isolated individuals with needs. Local authorities should take into account the impact of an individual’s need on those who support them, and take steps to help others access information or support.
-
g) The need to protect people from abuse and neglect. In any activity which a local authority undertakes, it should consider how to ensure that the person is and remains protected from abuse or neglect. This is not confined only to safeguarding issues, but should be a general principle applied in every case including with those who self-neglect.
-
h) The need to ensure that any restriction on the individual’s rights or freedom of action that is involved in the exercise of the function is kept to the minimum necessary. For achieving the purpose for which the function is being exercised. Where the local authority has to take actions which restrict rights or freedoms, they should ensure that the course followed is the least restrictive necessary. Concerns about self-neglect do not override this principle.
1.15 All of the matters listed above must be considered in relation to every individual, when a local authority carries out a function as described in this guidance. Considering these matters should lead to an approach that looks at a person’s life holistically, considering their needs in the context of their skills, ambitions, and priorities – as well as the other people in their life and how they can support the person in meeting the outcomes they want to achieve. The focus should be on supporting people to live as independently as possible for as long as possible.
1.16 As with promoting wellbeing, the factors above will vary in their relevance and application to individuals. For some people, spiritual or religious beliefs will be of great significance, and should be taken into particular account. Local authorities should consider how to apply these further principles on a case-by-case basis. This reflects the fact that every person is different and the matters of most importance to them will accordingly vary widely.
1.17 Neither these principles, nor the requirement to promote wellbeing, require the local authority to undertake any particular action. The steps a local authority should take will depend entirely on the circumstances. The principles as a whole are not intended to specify the activities which should take place. Instead, their purpose is to set common expectations for how local authorities should approach and engage with people.
Independent living
1.18 Although not mentioned specifically in the way that wellbeing is defined, the concept of ‘independent living’ is a core part of the wellbeing principle. Section 1 of the Care Act includes matters such as individual’s control of their day-to-day life, suitability of living accommodation, contribution to society - and crucially, requires local authorities to consider each person’s views, wishes, feelings and beliefs.
1.19 The wellbeing principle is intended to cover the key components of independent living, as expressed in the UN Convention on the Rights of People with Disabilities (in particular, Article 19 of the Convention). Supporting people to live as independently as possible, for as long as possible, is a guiding principle of the Care Act. The language used in the Act is intended to be clearer, and focus on the outcomes that truly matter to people, rather than using the relatively abstract term ‘independent living’.
Wellbeing throughout the Care Act
1.20 Wellbeing cannot be achieved simply through crisis management; it must include a focus on delaying and preventing care and support needs, and supporting people to live as independently as possible for as long as possible. (See chapter 2 for more detail on approaches to prevention).
1.21 Promoting wellbeing does not mean simply looking at a need that corresponds to a particular service. At the heart of the reformed system will be an assessment and planning process that is a genuine conversation about people’s needs for care and support and how meeting these can help them achieve the outcomes most important to them. Where someone is unable to fully participate in these conversations and has no one to help them, local authorities will arrange for an independent advocate. Chapters 6 (Assessment and eligibility), 10 (Care and support planning), and 7 (Independent advocacy) discuss this in more detail.
1.22 In order to ensure these conversations look at people holistically, local authorities and their partners must focus on joining up around an individual, making the person the starting point for planning, rather than what services are provided by what particular agency. Chapter 15 (integration and cooperation) sets this out in more detail.
1.23 In particular, the Care Act is designed to work in partnership with the Children and Families Act 2014, which applies to 0 to 2.5 year old children and young people with SEN and Disabilities. In combination, the 2 Acts enable areas to prepare children and young people for adulthood from the earliest possible stage, including their transition to adult services. This is considered in more detail at chapter 16.
1.24 Promoting wellbeing is not always about local authorities meeting needs directly. It will be just as important for them to put in place a system where people have the information they need to take control of their care and support and choose the options that are right for them. People will have an opportunity to request their local authority support in the form of a direct payment that they can then use to buy their own care and support using this information. Chapters 3 (Information and advice) and 12 (Direct payments) explain this in more detail.
1.25 Control also means the ability to move from one area to another or from children’s services to the adult system without fear of suddenly losing care and support. The Care Act ensures that people will be able to move to a different area without suddenly losing their care and support and provides clarity about who will be responsible for care and support in different situations. It also includes measures to help young people move to the adult care and support system, ensuring that no one finds themselves suddenly without care on turning 18. Chapters 20 (Continuity of care), 19 (Ordinary residence) and 16 (Transition to adult care and support) set this out in more detail.
1.26 It is not possible to promote wellbeing without establishing a basic foundation where people are safe and their care and support is on a secure footing. The Care Act puts in place a new framework for adult safeguarding and includes measures to guard against provider failure to ensure this is managed without disruption to services. Chapters 14 (Safeguarding), and 5 (Managing provider failure) set this out in more detail.
The role of the Principal Social Worker in care and support
1.27 The purpose of this section of the guidance is to further clarify arrangements to have in place a designated principal social worker in adult care and support. Local authorities should make arrangements to have a qualified and registered social work professional practice lead in place to:
- lead and oversee excellent social work practice
- support and develop arrangements for excellent practice
- lead the development of excellent social workers
- support effective social work supervision and decision making
- oversee quality assurance and improvement of social work practice
- advise the director of adult social services (DASS) and/or wider council in complex or controversial cases and on developing case or other law relating to social work practice
- function at the strategic level of the Professional Capabilities Framework
The local authority role in supporting principal social workers
1.28 All local authorities should ensure principal social workers are given the credibility, authority and capacity to provide effective leadership and challenge, both at managerial and practitioner level and are given sufficient time to carry out their role. The principal social worker should also be visible across the organisation, from elected members and senior management, through to frontline social workers, people who use services and carers. Local authorities should therefore ensure that the role is located where it can have the most impact and profile.
1.29 Whatever arrangements are agreed locally, the principal social worker should maintain close contact with the DASS and frontline practitioners and engage in some direct practice. This can take several different forms, including direct casework, co-working, undertaking practice development sessions, mentoring.
1.30 The integration of health and care and support will increasingly require social workers to lead, both in their teams and across professional boundaries, particularly in the context of safeguarding, mental health and mental capacity. Organisational models of social work have traditionally focused on managerial, as opposed to professional leadership - through their direct link to practice, principal social workers can ‘bridge the gap’ between professional and managerial responsibility, to influence the delivery and development of social work practice.
Principal social workers and safeguarding
1.31 Chapter 14 of this statutory guidance endorses the: ‘Making Safeguarding Personal’ approach. This represents a fundamental shift in social work practice in relation to safeguarding, with a focus on the person not the process. As the professional lead for social work, principal social workers should have a broad knowledge base on safeguarding and Making Safeguarding Personal and be confident in its application in their own and others’ work. Local authorities should, therefore, ensure that principal social workers lead on ensuring the quality and consistency of social work practice in fulfilling its safeguarding responsibilities. In particular they should have extensive knowledge of the legal and social work response options to specific cases and in general.
2. Preventing, reducing or delaying needs
This chapter provides guidance on section 2 of the Care Act 2014.
This chapter covers:
- defining prevention
- primary prevention/promoting wellbeing
- secondary prevention/early intervention
- tertiary prevention/formal intervention, intermediate care and reablement
- the focus of prevention
- developing local approaches to prevention
- working with others to focus on prevention
- identifying those who may benefit from prevention
- enabling access to preventative support
- charging for preventative services
2.1 It is critical to the vision in the Care Act that the care and support system works to actively promote wellbeing and independence, and does not just wait to respond when people reach a crisis point. To meet the challenges of the future, it will be vital that the care and support system intervenes early to support individuals, helps people retain or regain their skills and confidence, and prevents need or delays deterioration wherever possible.
2.2 There are many ways in which a local authority can achieve the aims of promoting wellbeing and independence and reducing dependency. This guidance sets out how local authorities should go about fulfilling their responsibilities, both individually and in partnership with other local organisations, communities, and people themselves.
2.3 The local authority’s responsibilities for prevention apply to all adults, including:
- people who do not have any current needs for care and support
- adults with needs for care and support, whether their needs are eligible and/or met by the local authority or not (see chapter 6)
- carers, including those who may be about to take on a caring role or who do not currently have any needs for support, and those with needs for support which may not be being met by the local authority or other organisation
2.4 The term ‘prevention’ or ‘preventative’ measures can cover many different types of support, services, facilities or other resources. There is no single definition for what constitutes preventative activity and this can range from wide-scale whole-population measures aimed at promoting health, to more targeted, individual interventions aimed at improving skills or functioning for one person or a particular group or lessening the impact of caring on a carer’s health and wellbeing. In considering how to give effect to their responsibilities, local authorities should consider the range of options available, and how those different approaches could support the needs of their local communities.
2.5 ‘Prevention’ is often broken down into 3 general approaches – primary, secondary and tertiary prevention – which are described in more detail below. The use of such terms is aimed to illustrate what type of services, facilities and resources could be considered, arranged and provided as part of a prevention service, as well as to whom and when such services could be provided or arranged. However, services can cut across any or all of these 3 general approaches and as such the examples provided under each approach are not to be seen as limited to that particular approach. Prevention should be seen as an ongoing consideration and not a single activity or intervention.
Prevent: primary prevention/promoting wellbeing
2.6 These are aimed at individuals who have no current particular health or care and support needs. These are services, facilities or resources provided or arranged that may help an individual avoid developing needs for care and support, or help a carer avoid developing support needs by maintaining independence and good health and promoting wellbeing. They are generally universal (for example, available to all) services, which may include, but are not limited to interventions and advice that:
- provide universal access to good quality information
- support safer neighbourhoods
- promote healthy and active lifestyles (for example. exercise classes)
- reduce loneliness or isolation (for example: befriending schemes or community activities such as the case study below)
- encourage early discussions in families or groups about potential changes in the future (for example: conversations about potential care arrangements or suitable accommodation should a family member become ill or disabled)
Case Study: LinkAge programme
The LinkAge programme aims to promote and enhance the lives of older people (55+ years old) through a range of activities, from walking groups to coffee mornings, through a number of older people-led ‘hubs’ across the city. The main aim is to bring those people that feel socially isolated and lonely into their local communities. In an evaluation of a new hub there was significant improvement on a friendship scale with scores moving from people feeling isolated or with a low level of social support at the beginning of the hub to very or highly socially connected at follow up.
Eileen (85) said:
I look forward to Fridays each week and enjoy the social aspect of the club too.
Lyn said:
if it wasn’t for LinkAge I don’t quite know what would have happened. It’s made life bearable, well more than bearable, it’s made it life.
Reduce: secondary prevention/early intervention
2.7 These are more targeted interventions aimed at individuals who have an increased risk of developing needs, where the provision of services, resources or facilities may help slow down or reduce any further deterioration or prevent other needs from developing. Some early support can help stop a person’s life tipping into crisis, for example helping someone with a learning disability with moderate needs manage their money, or a few hours support to help a family carer who is caring for their son or daughter with a learning disability and behaviour that challenges at home.
2.8 Early intervention could also include a fall prevention clinic, adaptions to housing to improve accessibility or provide greater assistance, handyman services, short term provision of wheelchairs or telecare services. In order to identify those individuals most likely to benefit from such targeted services, local authorities may undertake screening or case-finding, for instance to identify individuals at risk of developing specific health conditions or experiencing certain events (such as strokes, or falls), or those that have needs for care and support which are not currently met by the local authority. Targeted interventions should also include approaches to identifying carers, including those who are taking on new caring responsibilities. Carers can also benefit from support to help them develop the knowledge and skills to care effectively and look after their own health and wellbeing.
Delay: tertiary prevention/formal intervention
2.9 These are interventions aimed at minimising the effect of disability or deterioration for people with established or complex health conditions, (including progressive conditions, such as dementia), supporting people to regain skills and manage or reduce need where possible. Tertiary prevention could include, for example the rehabilitation of people who are severely sight impaired (see also chapter 22 sight registers). Local authorities must provide or arrange services, resources or facilities that maximise independence for those already with such needs, for example, interventions such as the provision of formal care such as meeting a person’s needs in their own home; rehabilitation/reablement services, for example, community equipment services and adaptations; and the use of joint case-management for people with complex needs.
2.10 Tertiary prevention services could also include helping improve the lives of carers by enabling them to continue to have a life of their own alongside caring, for example through respite care, peer support groups like dementia cafés, or emotional support or stress management classes which can provide essential opportunities to share learning and coping tips with others. This can help develop mechanisms to cope with stress associated with caring and help carers develop an awareness of their own physical and mental health needs.
2.11 Prevention is not a one off activity. For example, a change in the circumstances of an adult and/or carer may result in a change to the type of prevention activity that would be of benefit to them (see para 2.32). Prevention can sometimes be seen as something that happens primarily at the time of (or very soon after) a diagnosis or assessment or when there has been a subsequent change in the person’s condition. Prevention services are, however, something that should always be considered. For example, at the end of life in relation to carers, prevention services could include the provision of pre-bereavement support.
Intermediate care and reablement
2.12 There is a tendency for the terms ‘reablement’, ‘rehabilitation’ and ‘intermediate care’ to be used interchangeably. The National Audit of Intermediate Care categorises 4 types of intermediate care:
- crisis response – services providing short-term care (up to 48 hours)
- home-based intermediate care – services provided to people in their own homes by a team with different specialities but mainly health professionals such as nurses and therapists
- bed-based intermediate care – services delivered away from home, for example, in a community hospital
- reablement – services to help people live independently which are provided in the person’s own home by a team of mainly care and support professionals
2.13 The term ‘rehabilitation’ is sometimes used to describe a particular type of service designed to help a person regain or re-learn some capabilities where these capabilities have been lost due to illness or disease. Rehabilitation services can include provisions that help people attain independence and remain or return to their home and participate in their community, for example independent living skills and mobility training for people with visual impairment.
2.14 ‘Intermediate care’ services are provided to people, usually older people, after they have left hospital or when they are at risk of being sent to hospital. Intermediate care is a programme of care provided for a limited period of time to assist a person to maintain or regain the ability to live independently – as such they provide a link between places such as hospitals and people’s homes, and between different areas of the health and care and support system – community services, hospitals, GPs and care and support.
2.15 To prevent needs emerging across health and care, integrated services should draw on a mixture of qualified health, care and support staff, working collaboratively to deliver prevention. This could involve, for instance, reaching beyond traditional health or care interventions to help people develop or regain the skills of independent living and active involvement in their local community.
Carers and prevention
2.16 Carers play a significant role in preventing the needs for care and support for the people they care for, which is why it is important that local authorities consider preventing carers from developing needs for care and support themselves. There may be specific interventions for carers that prevent, reduce or delay the need for carers’ support. These interventions may differ from those for people without caring responsibilities. Examples of services, facilities or resources that could contribute to preventing, delaying or reducing the needs of carers may include but is not limited to those which help carers to:
- care effectively and safely – both for themselves and the person they are supporting, for example, timely interventions or advice on moving and handling safely or avoiding falls in the home, or training for carers to feel confident performing basic care tasks
- look after their own physical and mental health and wellbeing, including developing coping mechanisms
- make use of IT and other technology
- make choices about their own lives, for example managing their caring role and paid employment
- find support and services available in their area
- access the advice, information and support they need including information and advice on welfare benefits and other financial information and about entitlement to carers’ assessments (see chapter 6)
2.17 As with the people they care for, the duty to prevent carers from developing needs for support is distinct from the duty to meet their eligible needs (see chapter 6). While a person’s eligible needs may be met through universal preventative services, this will be an individual response following a needs or carers assessment. Local authorities cannot fulfil their universal prevention duty in relation to carers simply by meeting eligible needs, and nor would universal preventative services always be an appropriate way of for meeting carers’ eligible needs.
The focus of prevention
Promoting wellbeing
2.18 Local authorities must have regard to promoting wellbeing and the principles set out in chapter 1. Local authorities should look at an individual’s life holistically. This will mean considering any care and support needs in the context of the person’s skills, ambitions and priorities. This should include consideration of the role a person’s family or friends can play in helping the person to meet their goals. This is not creating or adding to their caring role but including them in an approach supporting the person to live as independently as possible for as long as possible. In regard to carers, the local authority should consider how they can be supported to look after their own health and wellbeing and to have a life of their own alongside their caring responsibilities.
2.19 As highlighted in the case study, where people live alone a person may not always have the support from family or friends because they may not live close by. For this group of people prevention needs to be considered through other means, such as the provision of community services and activities that would help support people to maintain an independent life.
Case Study
An older man lives alone with some support from his daughter who works full-time. He needs occasional personal care to remain living independently with dignity, and it is likely that these needs will increase. He has lost contact with family and friends following his wife’s death and rarely goes out without support from his daughter who is restricted to taking him out at weekends because of work commitments.
An assessment would consider all of his needs, including those currently being met by his daughter, along with the outcomes he wishes to achieve. A separate carer’s assessment offered to his daughter (or a combined assessment if both father and daughter agreed) would establish the daughter’s willingness and ability to care and continue to care and how best to promote her own wellbeing, for example by having regard to the outcomes she wishes to achieve. This joint assessment would look at issues such as the possible impact on the daughter of supporting her father while in full-time employment as well as the father’s isolation, ability to connect with others or be an active citizen.
Community groups, voluntary organisations, and buddying services could support the father to reduce the social isolation that he may be feeling and maximise opportunities to look after his own health and wellbeing and participate in local community activities. This, in turn could lessen the impact of caring on his daughter and enable her to continue to support her father effectively alongside paid employment. Such support can be identified/suggested alongside other, perhaps more formal services to meet personal care needs, and can be an effective way of promoting wellbeing. In this example, the aspects of wellbeing relating to social wellbeing and family relationships might be promoted.
Developing resilience and promoting individual strength
2.20 In developing and delivering preventative approaches to care and support, local authorities should ensure that individuals are not seen as passive recipients of support services, but are able to design care and support based around achievement of their goals. Local authorities should actively promote participation in providing interventions that are co-produced with individuals, families, friends, carers and the community. ‘Co-production’ is when an individual influences the support and services received, or when groups of people get together to influence the way that services are designed, commissioned and delivered. Such interventions can contribute to developing individual resilience and help promote self-reliance and independence, as well as ensuring that services reflect what the people who use them want.
Case Study
Derby City Council used co-production to develop clear and easy to use customer information to support their new customer journey for self-directed support. New information that has been produced includes an assessment form, support planning tools for people using services, customer leaflets and a staff handbook. A small project team held discussions and workshops to identify information that needed improving to be clearer and suggestions for improvement, for example, a new assessment form. Staff working in adult social care assessment teams had training on how to make best use of the new suite of information.
The inclusive approach taken to re-designing the information took longer than an internally managed process, but has resulted in better information, informed people using services and bringing their own perspective and experience. The co-production approach led to the development of key principles which can be used in other areas of communication. The approach is being continued.
2.21 Through the assessment process, an individual will have direct contact with a local authority. A good starting point for a discussion that helps develop resilience and promotes independence would be to ask: ‘what does a good life look like for you and your family and how can we work together to achieve it?’ Giving people choice and control over the support they may need and access to the right information enables people to stay as well as possible, maintain independence and caring roles for longer.
2.22 Social workers, occupational therapists, other professionals, service providers and commissioners who are effective at preventing, reducing, or delaying needs for care and support are likely to have a holistic picture of the individuals and families receiving support. This will include consideration of a person’s strengths and their informal support networks as well as their needs and the risks they face. This approach recognises the value in the resources of voluntary and community groups and the other resources of the local area.
Developing a local approach to preventative support
2.23 A local authority must provide or arrange for services, facilities or resources which would prevent, delay or reduce individuals’ needs for care and support, or the needs for support of carers. Local authorities should develop a clear, local approach to prevention which sets out how they plan to fulfill this responsibility, taking into account the different types and focus of preventative support as described above. Developing a local approach to preventative support is a responsibility wider than adult care and support alone, and should include the involvement, by way of example, of those responsible for public health, leisure, transport, and housing services which are relevant to the provision of care and support.
2.24 Whilst local authorities may choose to provide some types of preventative support themselves, others may be more effectively provided in partnership with other local partners (for example, rehabilitation or falls clinics provided jointly with the local NHS), and further types may be best provided by other organisations (for example, specialist housing providers or some carers’ services). A local authority’s commissioning strategy for prevention should consider the different commissioning routes available, and the benefits presented by each. This could include connecting to other key areas of local preventative activity outside care, including housing, planning and public health.
2.25 In developing a local approach to prevention, the local authority must take steps to identify and understand both the current and future demand for preventative support, and the supply in terms of services, facilities and other resources available.
2.26 Local authorities must consider the importance of identifying the services, facilities and resources that are already available in their area, which could support people to prevent, reduce or delay needs, and which could form part of the overall local approach to preventative activity. Understanding the breadth of available local resources will help the local authority to consider what gaps may remain, and what further steps it should itself take to promote the market or to put in place its own services.
2.27 Where the local authority does not provide such types of preventative support itself, it should have mechanisms in place for identifying existing and new services, maintaining contact with providers over time, and helping people to access them. Local approaches to prevention should be built on the resources of the local community, including local support networks and facilities provided by other partners and voluntary organisations.
2.28 Local authorities must promote diversity and quality in provision of care and support services, and ensure that a person has a variety of providers to choose from (see chapter 4). Considering the services, facilities and resources which contribute towards preventing or delaying the development of needs for care and support is a core element of fulfilling this responsibility. A local authority should engage local providers of care and support in all aspects of delivery and encourage providers to innovate and respond flexibly to develop interventions that contribute to preventing needs for care and support.
2.29 Local authorities should consider the number of people in its area with existing needs for care and support, as well as those at risk of developing needs in the future, and what can be done to prevent, delay or reduce those needs now and in the future. In doing so, a local authority should draw on existing analyses such as the Joint Strategic Needs Assessment, and work with other local partners such as the NHS and voluntary sector to develop a broader, shared understanding of current and future needs, and support integrated approaches to prevention.
2.30 In particular, local authorities must consider how to identify ‘unmet need’ - for example, those people with needs which are not currently being met, whether by the local authority or anyone else. Understanding unmet need will be crucial to developing a longer-term approach to prevention that reflects the true needs of the local population. This assessment should also be shared with local partners, such as through the health and wellbeing board, to contribute to wider intelligence for local strategies. Preventative services, facilities or resources are often most effective when brought about through partnerships between different parts of the local authority and between other agencies and the community such as those people who are likely to use and benefit from these services.
2.31 Local authorities should consider how they can work with different partners to identify unmet needs for different groups and coordinate shared approaches to preventing or reducing such needs, for example working with the NHS to identify carers, and working with independent providers including housing providers and the voluntary sector, who can provide local insight into changing or emerging needs beyond eligibility for publically-funded care.
Case Study: Midland Heart’s reablement service
At 82, Beryl was diagnosed with stomach cancer and admitted to hospital. As a result of a major operation, she now has a permanent colostomy bag. After only a month Beryl was successfully discharged from hospital to her own home with a reablement package from Leicester City Council and support from the housing association, Midland Heart, to help her regain her independence.
If Beryl had not received this support, she would have been discharged to a more costly care home. The reablement service ensured that Beryl’s home was suitably adapted for her return, which allowed a speedy discharge and avoided the need for institutional care. The support service has assisted her attendance at medical appointments with her GP and monitored the impact of her medication.
Working with other partners to focus on prevention
2.32 Developing and delivering local approaches to prevention, the local authority should consider how to align or integrate its approach with that of other local partners. Preventing needs will often be most effective when action is undertaken at a local level, with different organisations working together to understand how the actions of each may impact on the other.
2.33 Within the local authority, prevention of care and support needs is closely aligned to other local authority responsibilities in relation to public health, children’s services, and housing, for example. Across the local landscape, the role of other bodies including the local NHS (for example: GPs, dentists, pharmacists, ophthalmologists), welfare and benefits advisers (for example at Jobcentre Plus), the police, fire service, prisons in respect of those persons detained or released with care and support needs, service providers and others will also be important in developing a comprehensive approach.
2.34 Local authorities must ensure the integration of care and support provision, including prevention with health and health-related services, which include housing (see chapter 15). This responsibility includes in particular a focus on integrating with partners to prevent, reduce or delay needs for care and support.
2.35 A local authority must cooperate with each of its relevant partners and the partners must cooperate with the local authority (see chapter 15 on cooperation and details of specific relevant partners), for example, in relation to the provision of preventative services and the identification of carers, a local authority must cooperate with NHS bodies.
2.36 A local authority must also set up arrangements between its relevant partners and individual departments in relation to its care and support functions, which includes prevention. Relevant partners and individual departments include, but are not limited to, housing departments where, for example, housing services or officers may be well placed to identify people with dementia and their carers, and provide housing related support and/or in partnership with others, home from hospital services or ‘step up step down’ provision.
Identifying those who may benefit from preventative support
2.37 Local authorities should put in place arrangements to identify and target those individuals who may benefit from particular types of preventative support. Helping people to access such types of support when they need it is likely to have a significant impact on their longer-term health and wellbeing, as well as potentially reducing or delaying the need for ongoing care and support from the local authority.
2.38 In developing such approaches, local authorities should consider the different opportunities for coming into contact with those people who may benefit from preventative support, including where the first contact may be with another professional outside the local authority, for example, GPs, pharmacists or welfare and benefit advisers. There are a number of interactions and access points that could bring a person into contact with the local authority or a partner organisation and act as a trigger point for the local authority to consider whether the provision of a preventative service, or some other step is appropriate. These might include, for example:
- initial contact through a customer services centre, whether by the person concerned or someone acting on their behalf
- contact with a GP, community nurses, housing officers or other professionals which leads to a referral to the local authority
- an assessment of needs or a carer’s assessment (see chapter 6 on assessment), which identifies that the person would benefit from a preventative service or other type of support available locally
2.39 Many people with low level care and support needs will approach the voluntary sector for advice in the first instance. Local authorities and the voluntary sector should work together on how it can share this information to gain a fuller picture of local need as possible. Authorities should bring data from these different sources together to stratify who in the community may need care and support in the future and what types of needs they are likely to have, and use this information to target their preventative services effectively.
2.40 Prevention should be a consistent focus for local authorities in undertaking their care and support functions. However, there may be key points in a person’s life or in the care and support process where a preventative intervention may be particularly appropriate or of benefit to the person. Approaches to identifying those people who may benefit from preventative support should consider how to locate people in such circumstances, for example:
- bereavement
- hospital admission and/or discharge
- people who have been recently admitted to or released from prison
- application for benefits such as Attendance Allowance, or Carer’s Allowance
- contact with/use of local support groups
- contact with/use of private care and support
- changes in housing
2.41 A local authority must establish and maintain a service for providing people with information and advice relating to care and support (see chapter 3). In addition to any more targeted approaches to communicating with individuals who may benefit from preventative support, this service should include information and advice about preventative services, facilities or resources, so that anyone can find out about the types of support available locally that may meet their individual needs and circumstances, and how to access them.
Helping people access preventative support
2.42 A variety of different kinds of service, facilities or resources can be preventative and can help individuals live well and maintain their independence or caring roles for longer.
2.43 Local authorities should be innovative and develop an approach to prevention that meets the needs of their local population. A preventative approach requires a broad range of interventions, as one size will not fit all.
2.44 Where a local authority has put in place mechanisms for identifying people who may benefit from a type of preventative support, it should take steps to ensure that the person concerned understands the need for the particular measure, and is provided with further information and advice as necessary.
2.45 Contact with a person who is identified as being able to benefit from preventative support may lead to the local authority becoming aware that the person appears to have needs for either or both care and support and support in a role as a carer. This appearance of need may trigger the requirement to carry out a needs assessment (in the case of an adult with needs for care and support), or a carer’s assessment (see paragraphs 2.48 to 2.54 below). However, where a local authority is not required to carry out such an assessment under the Care Act, it should nonetheless take steps to establish whether the person identified will benefit from the type of preventative support proposed.
2.46 Where a person is provided with any type of service, or support to access any facility or resource as a preventative measure, the local authority should also provide the person with information in relation to the services offered or measure undertaken. The local authority is not required to provide a care and support plan or a support plan where it only takes steps under section 2 of the Care Act; however, it should consider which aspects of a plan should be provided in these circumstances, and should provide such information as is necessary to enable the person to understand:
- what needs the person has or may develop, and why the intervention or other action is proposed in their regard
- what the expected outcome for the action proposed is, and any relevant timescale in which those outcomes are expected
- what is proposed to take place at the end of the measure (for instance, whether an assessment of need or a carer’s assessment will be carried out at that point)
2.47 The person concerned must agree to the provision of any service or other step proposed by the local authority. Where the person refuses, but continues to appear to have needs for care and support (or for support, in the case of a carer), then the local authority must proceed to offer the individual an assessment.
Assessment of adults’ and carers’ needs
2.48 In assessing whether an adult has any care and support needs or a carer has any needs for support, the local authority must consider whether the person concerned would benefit from the preventative services, facilities or resources provided by the local authority or which might otherwise be available in the community. This is regardless of whether, in fact, the adult or carer is assessed as having any care and support needs or support needs. As part of the assessment process, the local authority considers the capacity of the person to manage their needs or achieve the outcomes which matter to them, and allows for access to preventative support before a decision is made on whether the person has eligible needs (see chapter 6 on assessment).
2.49 As part of this process, the local authority should also take into account the person’s own capabilities, and the potential for improving their skills, as well as the role of any support from family, friends or others that could help them to achieve what they wish for from day-to-day life. This should not assume that others are willing or able to take up caring roles. Where it appears to the local authority that a carer may have needs for support (whether currently or in the future), a carer’s assessment must always be offered.
2.50 Children should not undertake inappropriate or excessive caring roles that may have an impact on their development. A young carer becomes vulnerable when their caring role risks impacting upon their emotional or physical wellbeing and their prospects in education and life. A local authority may become aware that a child is carrying out a caring role through an assessment or informed through family members or a school. A local authority should consider how supporting the adult with needs for care and support can prevent the young carer from under taking excessive or inappropriate care and support responsibilities. Where a young carer is identified, the local authority must undertake a young carer’s assessment under part 3 of the Children Act 1989.
2.51 Considering the support from family, friends or others is important in taking a holistic approach to see the person in the context of their support networks and understanding how their needs may be prevented, reduced or delayed by others within the community, rather than by more formal services (also see chapter 6, paras. 6.65 to 6.71, about the whole family approach to assessment).
2.52 If a person is provided with care and support or support as a carer by the local authority, the authority must provide them with information and advice about what can be done to prevent, delay, or reduce their needs as part of their care and support plan or support plan. This should also include consideration of the person’s strengths and the support from other members of the family, friends or the community (see chapter 10 on care and support planning).
2.53 Regardless of whether or not a person is ultimately assessed as having either any needs at all or any needs which are to be met by the local authority, the authority must in any case provide information and advice in an accessible form, about what can be done to prevent, delay, or reduce development of their needs. This is to ensure that all people are provided with targeted, personalised information and advice that can support them to take steps to prevent or reduce their needs, connect more effectively with their local community, and delay the onset of greater needs to maximise their independence and quality of life. Where a person has some needs that are eligible, and also has some other needs that are not deemed to be eligible, the local authority must provide information and advice on services facilities or resources that would contribute to preventing, reducing or delaying the needs which are not eligible, and this should be aligned and be consistent with the care and support plan for the person with care needs, or support plan for the carer.
2.54 It is important that people receive information in a timely manner about the services or interventions that can help or contribute to preventing an escalation in needs for care and support. Supporting people’s access to the right information at the right time is a key element of a local authority’s responsibilities for prevention.
Charging for preventative support
2.55 Preventative services, like other forms of care and support, are not always provided free, and charging for some services is vital to ensure affordability. The Care and Support (Preventing Needs for Care and Support) Regulations 2014 continue to allow local authorities to make a charge for the provision of certain preventative services, facilities or resources. The regulations also provide that some other specified services must be provided free of charge.
2.56 Prevention services facilities or resources may not involve local authorities directly providing or commissioning a service. Some effective forms of prevention result from partnerships with other public services, voluntary and community organisations and other providers. In developing these partnerships local authorities should consider what obstacles there may be which might prevent people on low incomes from benefitting from the activities and take reasonable steps to avoid this.
2.57 Where a local authority chooses to charge for a particular service, it should consider how to balance the affordability and viability of the activity with the likely impact that charging may have on uptake. In some cases, charging may be necessary in order to make a preventative service viable or keep a service running.
2.58 When charging for any type of preventative support, local authorities should take reasonable steps to ensure that any charge is affordable for the person concerned. This does not need to follow the method of the financial assessment used for mainstream charging purposes; and the use of such a process is likely to be disproportionate.
2.59 However, local authorities should consider adopting a more proportionate or ‘light-touch’ approach which ensures that charges are only paid by those who can afford to do so. In any event, a local authority must not charge more than it costs to provide or arrange for the service, facility or resource.
2.60 The regulations require that intermediate care and reablement must be provided free of charge for up to 6 weeks, as must aids and minor adaptations (for example: adaptations up to the value of £1,000) (see also 8.14).
2.61 Where local authorities provide intermediate care or reablement to those who require it, this must be provided free of charge for a period of up to 6 weeks. This is for all adults, irrespective of whether they have eligible needs for ongoing care and support. Although such types of support will usually be provided as a preventative measure under section 2 of the Act, they may also be provided as part of a package of care and support to meet eligible needs. In these cases, regulations also provide that intermediate care or reablement cannot be charged for in the first 6 weeks, to ensure consistency.
2.62 Whilst they are both time-limited interventions, neither intermediate care nor reablement should have a strict time limit, since the period of time for which the support is provided should depend on the needs and outcomes of the individual. In some cases, for instance a period of rehabilitation for a visually impaired person (a specific form of reablement) [footnote 2], may be expected to last longer than 6 weeks. Whilst the local authority does have the power to charge for this where it is provided beyond 6 weeks, local authorities should consider continuing to provide it free of charge beyond 6 weeks in view of the clear preventative benefits to the individual and, in many cases, the reduced risk of hospital admissions.
2.63 Local authorities should consider the potential impact and consequences of ending the provision of preventative services. Poorly considered exit strategies can negate the positive outcomes of preventative services, facilities or resources, and ongoing low-level care and support can have significant impact on preventing, reducing and delaying need.
Case Study
Mr A is a 91 year old man who lives alone with his dog in his house. He is usually independent, is a passionate cook and enjoys socialising. He drives a car. Whilst out walking his dog he suffered a stroke, he fell, causing a fractured neck of femur. He was admitted to hospital and underwent surgery for a hip replacement which meant he had to follow hip precautions for 6 weeks.
The stroke had left him with slight left-sided weakness and problems with concentration, sequencing and attention. He was transferred to a community hospital for rehabilitation where the physiotherapists (PTs) and occupational therapists (OTs) worked on mobility, transfers, personal care following hip precautions, stair climbing and kitchen tasks. Cognitive screens were completed and the OTs targeted their input on helping improve concentration, sequencing and attention.
Mr A was discharged, independently mobile using a frame, independent transferring using equipment and stair climbing with supervision. He was discharged home with 4 calls per day from BEST plus (Bradford Enablement Support Team). Joint sessions between the PTs and OTs and BEST plus were completed to work on the following:
- practising walking safely indoors using 2 walking sticks
- increase hip strength through exercises
- to be safe and independent washing and dressing
- to be safe and independent preparing hot drinks and simple snacks and transport safely using trolley
The above goals were achieved and new goals were set in consultation with Mr A:
- to be safe and independent walking outdoors using 2 sticks
- to be safe and independent bathing using bath lift
- to be safe and independent preparing hot meals from scratch
- to be safe and independent completing shopping using Access bus
- to be safe and independent walking dog short distances using 4 wheeled walker.
After 6 weeks of continued BEST plus input in Mr A’s home, he was able to achieve all of his goals and all Social Services input was withdrawn. Aspects of Mr A’s wellbeing have been promoted including physical wellbeing, social wellbeing, and control over day-to-day life.
3. Information and advice
This chapter provides guidance on section 4 of the Care Act 2014 and covers:
- the duty placed on local authorities to establish and maintain information and advice services relating to care and support for all people in its area
- the broad audience for the information and advice service
- the local authority role with respect to financial information and advice
- the accessibility and proportionality of information and advice
- the development of plans/strategies to meet local needs
3.1 Information and advice is fundamental to enabling people, carers and families to take control of, and make well-informed choices about, their care and support and how they fund it. Not only does information and advice help to promote people’s wellbeing by increasing their ability to exercise choice and control, it is also a vital component of preventing or delaying people’s need for care and support.
3.2 Local authorities must: ‘establish and maintain a service for providing people in its area with information and advice relating to care and support for adults and support for carers’.
3.3 The local authority has an active and critical role in the provision of information and advice and must take an active role. To fulfil its duty under section 4 of the Act, a local authority is likely to need to go further than providing information and advice directly (though direct provision will be important) by working to ensure the coherence, sufficiency, availability and accessibility of information and advice relating to care and support across the local authority area. Importantly, this duty to establish and maintain an information and advice service relates to the whole population of the local authority area, not just those with care and support needs or in some other way already known to the system.
3.4 It is important to be clear that the duty to establish and maintain an information and advice service is distinct from the duty to meet eligible needs (see chapter 6): this is true for both people with care and support needs and their carers. While a person’s eligible needs may be met by the provision of information and advice this will be an individual response following a needs or carers assessment. Local authorities cannot fulfil their universal information and advice duty simply by meeting eligible needs, and nor would information and advice always be an appropriate way of meeting eligible needs.
3.5 The local authority must ensure that information and advice services established cover more than just basic information about care and support and cover the wide range of care and support related areas set out in para. 3.22. The service should also address, prevention of care and support needs, finances, health, housing, employment, what to do in cases of abuse or neglect of an adult and other areas where required. In fulfilling this duty, local authorities should consider the people they are communicating with on a case by case basis, and seek to actively encourage them towards the types of information and/or advice that may be particularly relevant to them.
3.6 Local authorities must also have regard to identifying people that contact them who may benefit from financial information and advice independent of the local authority and actively facilitate those people to access to it (see paragraph 3.50). Separately to the duty to establish and maintain an information and advice service, local authorities must provide independent advocacy to facilitate the person’s involvement in the care and support assessment, planning and review processes where an individual would experience substantial difficulty in understanding, retaining or using information given, or in communicating their views, wishes or feelings and where there is nobody else appropriate (see chapter 7).
3.7 The availability and provision of information and advice, whether more general information about the way the system operates in the local authority area or more personalised information on a person’s specific needs, are essential building blocks to all of the reforms and many of the specific duties the Act introduces. This chapter of guidance should therefore be read in conjunction with guidance throughout this document, including:
- promoting individual wellbeing (chapter 1)
- prevention of needs for care and support (chapter 2)
- integration of care and support with health and housing related services (chapter 15)
- promoting diverse and high quality services (chapter 4)
- assessment and eligibility (chapter 6)
- personal budgets, personal care and support planning and direct payments (chapters 10 to 13)
- deferred payment agreements (chapter 9)
- continuity of care (chapter 20)
- safeguarding (chapter 14)
- transition to adult care and support (chapter 16)
- independent advocacy (chapter 7)
Terminology
3.8 In this section of guidance, the term ‘information’ means the communication of knowledge and facts regarding care and support. ‘Advice’ means helping a person to identify choices and/or providing an opinion or recommendation regarding a course of action in relation to care and support.
3.9 This section of guidance also uses the term ‘advocacy’ to mean supporting a person to understand information, express their needs and wishes, secure their rights, represent their interests and obtain the care and support they need.
3.10 This guidance talks about ‘financial information and advice’ which includes a broad spectrum of services whose purpose is to help people plan, prepare and pay for their care costs. In places it talks of ‘independent’ financial information or advice which in this document means services independent of the local authority. This guidance also refers to ‘regulated’ financial advice which means advice from an organisation regulated by the Financial Conduct Authority (FCA) which can extend to individual recommendations about specific financial products. Local authorities should ensure that people are able to access all of these types of financial information and advice which help people plan and pay for their care.
The duty to establish and maintain a service
3.11 Local authorities must establish and maintain a service for providing people in their areas with information and advice relating to care and support for adults and support for carers. In doing so local authorities should take account of the services currently in place and actions already taken and plans with partner organisations resulting from Joint Strategic Needs Assessments and Joint Health and Wellbeing Strategies. The information and advice service must cover the needs of all its population, not just those who are in receipt of local authority funded care or support. For example, people may often require information and advice before they need to access care or support services, to consider what actions they may take now to prevent or delay any need for care, or how they might plan to meet the cost of future care needs.
3.12 People need information and advice across many areas to support them to make informed choices about their care and support (see para. 3.23).
3.13 In establishing and maintaining an information and advice service, local authorities should ensure that they engage widely with people with care and support needs, carers, the wider public and local providers of information and advice and other types of care and support, to identify what is available and exactly what is needed locally, and how and where information and advice should best be provided.
3.14 It is important to recognise that while local authorities must establish and maintain a service, the duty does not require they provide all elements of this service. Rather, under this duty local authorities are expected to understand, co-ordinate and make effective use of other high quality statutory, voluntary and/or private sector information and advice resources available to people within their areas. This may also include provision of a service or parts of a service in conjunction with one or more local authorities, health services, children’s services, [footnote 3] or reuse of information from other local or national sources. When a local need for additional information and advice services is identified, local authorities should recognise the relevance of independent and impartial advice and should consider carefully whether services should be provided by the local authority directly or by another agency, including independent providers.
The audiences for the information and advice service
3.15 Local authorities are responsible for ensuring that all adults including carers in their area with a need for information and advice about care and support are able to access it. This is a very broad group, extending much further than people who have an immediate need for care or support. It will only be achieved through working in partnership with the wider public and local advice and information providers.
3.16 People (carers included) who are likely to need information and advice include, but are not restricted to:
- people wanting to plan for their future care and support needs
- people who may develop care and support needs, or whose current care and support needs may become greater. Under the duty of prevention in Section 2 of the Act, local authorities are expected to take action to prevent, delay and/or reduce the care and support needs for these people (see chapter 2 on prevention)
- people who have not presented to local authorities for assessment but are likely to be in need of care and support. Local authorities are expected to take steps to identify such people and encourage them to come forward for an assessment of their needs (see chapter 2 on prevention)
- people who become known to the local authority (through referral, including self-referral), at first contact where an assessment of needs is being considered (see chapter 6 on assessments)
- people who are assessed by local authorities as currently being in need of care and support. Advice and information must be offered to these people irrespective of whether they have been assessed as having eligible needs which the local authority must meet (see chapter 6 on assessments)
- people whose eligible needs for care and support the local authority is currently meeting (whether the local authority is paying for some, all or none of the costs of meeting those needs) (see chapter 10 on care and support planning)
- people whose care and support or support plans are being reviewed (see chapter 13 on reviews of care and support plans)
- family members and carers of adults with care and support needs, (or those who are likely to develop care and support needs). Under Sections 2 of the Act, local authorities are expected to have regard to the importance of identifying carers and take action to reduce their needs for support (see chapter 6 on assessments)
- adults who are subject to adult safeguarding concerns (see chapter 14 on safeguarding)
- people who may benefit from financial information and advice on matters concerning care and support. Local authorities must have regard to the importance of identifying these people, to help them understand the financial costs of their care and support and access independent financial information and advice including from regulated financial advisers (see para. 3.49)
- care and support staff who have contact with and provide information and advice as part of their jobs
3.17 In providing information and advice, local authorities must recognise and respond to the specific requirements that carers have for both general and personal information and advice. A carer’s need for information and advice may be separate and distinct from information and advice for the person they are caring for. These distinct needs may be covered together, in a similar manner to the local authority combining an assessment of a person needing care and support with a carer’s assessment (where both the individuals concerned agree) (see chapter 6 on assessments), but may be more appropriately addressed separately. This may include information and advice on:
- breaks from caring
- the health and wellbeing of carers themselves
- caring and advice on wider family relationships
- carers’ financial and legal issues
- caring and employment
- caring and education
- a carer’s need for advocacy
Access to and quality of information and advice
3.18 The local authority must ensure that there is an accessible information and advice service that meets the needs of its population. Information and advice must be open to everyone who would benefit from it. People access information and advice from a wide variety of sources. The authority should take account of information standards published by the Information Standards Board for Health and Social Care under the provisions of the Health and Social Care Act 2012.
3.19 Local authorities should ensure that information supplied is clear. Information and advice should only be judged as clear if it is understood and able to be acted upon by the individual receiving it. Local authorities will need to take steps to evaluate and ensure that information and advice is understood and able to be acted upon.
3.20 Information and advice provided within the service should be accurate, up-to-date and consistent with other sources of information and advice. Staff providing information and advice within a local authority and other frontline staff should be aware of accessibility issues and be appropriately trained.
3.21 All reasonable efforts should be taken to ensure that information and advice provided meets the individual’s requirements, is comprehensive and is given at an early stage. Local authorities must seek to ensure that all relevant information is available to people for them to make the best informed decision in their particular circumstances, and omission or the withholding of information would be at odds with the duty as set out in the Act.
3.22 There are some circumstances where it is particularly important for information and advice to be impartially provided. Local authorities should consider when this might most effectively be provided by an independent source rather than by the local authority itself. This is particularly likely to be the case when people need advice about how and whether to question or challenge the decisions of the local authority or other statutory body.
What should be provided – information and advice content
3.23 In discharging this duty, local authorities must ensure that information and advice is provided on:
- the care and support system locally – about how the system works. An outline of what the ‘process’ may entail and the judgements that may need to be made. Including specific information on what the assessment process, eligibility, and review stage is, how to complain or make a formal appeal to the authority, what they involve and when independent advocacy should be provided and be widely available. This also includes wider information and advice to support individual wellbeing (see paragraph 3.25); the charging arrangements for care and support costs (utilising current and developing national resources (see paras. 3.68 to 3.69); how a person might plan for their future care and support needs and how to pay for them, including provision for the possibility that they may not have capacity to make decisions for themselves in the future
- how to access the care and support available locally – where, how and with whom to make contact, including information on how and where to request an assessment of needs, a review or to complain or appeal against a decision
- the choice of types of care and support, and the choice of care providers available in the local authority’s area – including prevention and reablement services and wider services that support wellbeing. Where possible this should include the likely costs to the person of the care and support services available to them. This should also include information on different types of service or support that allow people personal control over their care and support for example, details of Independent Service Funds, and direct payments (see chapter 4 on market shaping and commissioning)
- how to access independent financial advice on matters relating to care and support – about the extent of their personal responsibilities to pay for care and support, their rights to statutory financial and other support, locally and nationally, so that they understand what care and support they are entitled to from the local authority or other statutory providers. Including what information and advice people may wish to consider when making financial decisions about care so that they can make best use of their financial resources and are able to plan for their personal costs of care whether immediately or in the future (see paras. 3.25 to 3.26)
- how to raise concerns about the safety or wellbeing of an adult with care and support needs and also consider how to do the same for a carer with support needs (see paras. 3.53 to 3.54)
3.24 The breadth of the circumstances under which information and advice must be provided, and the overall duty to promote individual wellbeing, means that local authorities must ensure that the subject matters covered by their information and advice available to people in their areas go much further than a narrow definition of care and support and cover all those subject matters listed in paragraph 3.23 above. Depending on local circumstances, the service should also include, but not be limited to, information and advice on:
- available housing and housing-related support options for those with care and support needs
- effective treatment and support for health conditions, including Continuing Health Care arrangements
- availability and quality of health services
- availability of services that may help people remain independent for longer such as home improvement agencies, handyman or maintenance services
- availability of befriending services and other services to prevent social isolation
- availability of intermediate care entitlements such as aids and adaptations
- eligibility and applying for disability benefits and other types of benefits
- availability of employment support for disabled adults
- children’s social care services and transition
- availability of carers’ services and benefits
- sources of independent information, advice and advocacy
- the Court of Protection, power of attorney and becoming a deputy
- raise awareness of the need to plan for future care costs
- practical help with planning to meet future or current care costs
- accessible ways and support to help people understand the different types of abuse and its prevention
When information should be provided
3.25 Local authorities have a number of direct opportunities to provide – or signpost to – advice and information when people in need of care and support come into contact with them. These include:
- at first point of contact with the local authority
- as part of a needs or carer’s assessment, including joint continuing healthcare assessments
- during a period of reablement
- around and following financial assessment
- when considering a financial commitment such as a deferred payment agreement or top-up agreement
- during or following an adult safeguarding enquiry
- when considering take up of a personal budget and/or direct payment
- during the care and support planning process
- during the review of a person’s care and support plan
- when a person may be considering a move to another local authority area
- at points in transition, for example when people needing care or carers under 18 become adults and the systems for support may change
3.26 Local authorities, working with their partners must use the wider opportunities to provide targeted information and advice at key points in people’s contact with the care and support, health and other local services. These include, but are not limited to, known ‘trigger points’ during a person’s life such as:
- contact with other local authority services
- bereavement
- hospital entry and/or discharge
- diagnosis of health conditions – such as dementia, stroke or an acquired impairment for example
- consideration or review of continuing healthcare arrangements
- take-up of power of attorney
- applications to Court of Protection
- application for, or review of, disability benefits such as attendance allowance
- personal independence payments, and for carers allowance
- access to work interviews
- contact with local support groups, charities, or user-led organisations including carers
- groups and disabled person’s organisations
- contact with or use of private care and support services, including homes care
- change or loss of housing
- contact with the criminal justice system
- admission to or release from prison
- ‘Guidance Guarantee’ in the Pensions Act 2014
- retirement
Accessibility of information and advice
3.27 The local authority should ensure that products and materials (in all formats) are as accessible as possible for all potential users. Websites should meet specific standards such as the Web Content Accessibility Guidelines and guidance set out in the Government Digital Service’s (GDS) service manual, printed products should be produced to appropriate guidelines with important materials available in easy read, and telephone services should also be available to those with hearing impairments. Local authorities should particularly be aware of the needs of individuals with complex but relatively rare conditions, such as deaf-blindness.[footnote 4]
3.28 As required under the Equality Act 2010, reasonable adjustments should be made to ensure that disabled people have equal access to information and advice services. Reasonable adjustments could include the provision of information in accessible formats or with communication support.
3.29 Advice and information content should, where possible, be provided in the manner preferred by the person and will therefore often need to be available in a number of different formats. The duty in the Care Act will not be met through the use of digital channels alone, and information and advice channels are likely to include all of the following:
- face-to-face contact
- use of peer-to-peer contacts
- community settings
- advice and advocacy services
- telephone
- mass communications, and targeted use of leaflets, posters (for example: in GP surgeries)
- use of ‘free’ media such as newspaper, local radio stations, social media
- local authority’s own and other appropriate internet websites, including support for the self-assessment of needs
- third party internet content and applications
3.30 Some groups in need of information and advice about care and support may have particular requirements. Local authorities must ensure that their information and advice service has due regard to the needs of these people. These include, but are not limited to:
- people with sensory impairments, such as visual impairment, deafblind and hearing impaired
- people who do not have English as a first language
- people who are socially isolated
- people whose disabilities limit their physical mobility
- people with learning disabilities
- people with mental health problems
3.31 Some people, including some people with dementia, may benefit from an independent person to help them to access or avail themselves of necessary information and advice. Any such need for help to facilitate access to this universal information and advice needs to be considered in planning for delivery of the service, although the duty to make arrangements for an individual to have an independent advocate available to them in certain circumstances only applies in relation to an individual’s involvement in the assessment, planning and review processes. From the point of first contact with or referral to the authority consideration of the duty to provide for independent advocacy to support involvement in assessment, planning and reviews should be undertaken (see chapter 7 on independent advocacy).
Proportionality of information and advice
3.32 The type, extent and timing of information and advice provided should be appropriate to the needs of the person. More complex issues may require more intensive and more personalised information and advice, helping people to understand the choices available to them, while general enquiries may require a less intensive approach. It is also important that the right level of information and advice is provided at the right time, recognising that a person’s need for information or advice may vary depending on the circumstance. For example, providing a person with too much information, more than they can take in, perhaps at a time of crisis, can be counter-productive.
3.33 There are clear messages from past public consultations and from research that people ‘don’t know what they need to know’ in relation to their care and support. This can prevent them asking the right questions and can mask the articulation and identification of needs that they have, for which they could benefit from information and advice. All contact for information and advice should take account of this and be able to respond with an assessment of needs when appropriate (see chapter 6). [footnote 5]
3.34 Local authorities should help ensure that information and advice is proportionate to the needs of those for whom it is provided. This could include enabling access to the support of registered social work advice for those providing information and advice to people contacting the local authority. This can help ensure that the potential for complexity is recognised early on and the person receives help to access non-statutory services and/or initial statutory sector support proportionate to their needs.
3.35 In providing an information and advice service, local authorities must be providing more than just leaflets and web-based materials. The focus should be on enabling people to access what they need through a tailored range of services that assists people to navigate all points and aspects of their journey through care and support. In doing this, local authorities should think about how they are reaching out and joining up with other providers of information and advice to ensure the coherence of the overall ‘offer’ (see chapter 15 on integration and cooperation).
Financial information and advice
3.36 Financial information and advice is fundamental to enabling people to make well-informed choices about how they pay for their care. It is integral to a person’s consideration of how best to meet care and support needs, immediately or in the future. People with good and impartial financial information and advice have a better understanding of how their available resources can be used more flexibly to fund a wider range of care options.
3.37 Financial information and advice is considered in a separate section due to the sometimes specialist and complex nature of what can be needed. This section should be read in the context of the overarching chapter and all requirements set out in this chapter, for example on accessibility and proportionality, must also be applied to financial information and advice. As set out at the start of the chapter, when this section refers to ‘independent financial information and advice’ it means services independent of the local authority. Where it refers to ‘regulated’ financial advice it means advice from an organisation regulated by the FCA which can extend to individual recommendations about specific financial products.
3.38 The service that local authorities are required to establish and maintain must include financial information and advice on matters relevant to care and support. It should provide some of this information directly to people in its community. However, where it would not be appropriate for a local authority to provide it directly, the local authority must ensure that people are helped to understand how to access independent financial advice.
3.39 Care decisions are often made quickly and at a time of crisis, and they can often involve family and friends in the process. The local authority must have regard to the importance of identifying those who may benefit from financial advice or information as early as possible. This should be complemented by broader awareness raising about how care and support is funded. Local authorities may also include how care and support costs interact with retirement decisions. Actions taken by a local authority to do this should include:
- working with partners to get the right message to people in the authority’s area: those who develop care and support needs, their carers, families and friends
- working with partners to communicate messages about the benefits of financial information and advice for example with the voluntary sector, through hospitals, GPs, or solicitors who may be advising on wills or power of attorney
- considering a person’s need for financial information and advice when they make first contact with the authority and throughout the assessment, care and support planning and review processes
3.40 When making financial plans about how to pay for care and support, a person needs to have confidence in what to do in the present, a view ahead to the future and a plan for what to do if circumstances change. This long-term outlook means that people will want to access financial information and advice at different points in their journey to enable them to make sustainable plans to pay for their care. The local authority should provide a service that covers this breadth and that facilitates access to the full spectrum of financial information and advice – from basic budgeting tips to regulated advice – to ensure that people within its area who would benefit can access it. They should also be aware and provide for the fact that some people will be less able to protect themselves from theft, fraud and financial exploitations (see chapter 14 on safeguarding).
3.41 The local authority service should include the following aspects of financial information and advice:
- understanding care charges
- ways to pay
- money management
- making informed financial decisions
- facilitating access to independent financial information and advice
3.42 Before providing financial information or advice directly to a person the local authority should establish whether the person has a deputy of the Court of Protection or a person with Lasting Power of Attorney acting on their behalf.
Understanding care charges
3.43 The local authority must provide information to help people understand what they may have to pay, when and why and how it relates to people’s individual circumstances. This must include the charging framework for care and support, how contributions are calculated (from both assets and income) and the means tested support available; top-ups (see chapter 8 on charging); and how care and support choices may affect costs. In the case of top-ups, the local authority should ensure that someone is willing and able to pay for them – this information will be fundamental in helping with this. The local authority should use the knowledge it has of the local care market – types of care and local providers of information and advice – to complement and develop the overarching narrative on how care funding works at the national level. This would include both domiciliary and residential care.
Ways to pay
3.44 The local authority must provide people with information on the availability of different ways to pay for care including through income and assets (for example, pension or housing wealth), a deferred payment agreement (see chapter 9 on deferred payment agreements), a financial product or a combination of these things. Local authorities should seek to give information that would be particularly pertinent to a person’s individual circumstances and facilitate access to an independent source of information or advice where relevant. This will be of particular relevance where a person will be meeting the total cost of care and support themselves or may be considering taking out a deferred payment agreement (see chapter 9 on deferred payments) or purchasing a financial product.
Money management
3.45 Different people will need different levels of support from the local authority and other providers of information and advice depending on their financial capability, their care needs and the amount they are expected to contribute. At the lower end of the spectrum, people may just need some basic information and support to help them rebalance their finances in light of their changing circumstances. Topics may include welfare benefits, advice on good money management, help with basic budgeting and possibly on debt management. The local authority may be able to provide some of this information itself, for example on welfare benefits, but where it cannot, it should help people access it.
Making informed financial decisions
3.46 The local authority must support people to make informed, affordable and sustainable financial decisions about their care throughout all stages of their life. In many situations the role of the local authority will be to understand the circumstances of the person, understand their preferences and help them to access the tailored information and advice that they need to make well-informed decisions. Where a person lacks capacity, the authority must establish whether a person has a deputy of the Court of Protection or a person with Lasting Power of Attorney acting on their behalf.
3.47 The local authority must offer to consider a person’s specific circumstances and provide them with information about the methods of paying for their care and support that may be available to them. The local authority may consider the timing and context of any retirement decisions a person might be making and how this interacts with paying for their care and support. They should advise people of the ways to pay that others in similar circumstances would usually consider and the range of information and advice they should be considering to help make their decision.
3.48 To help people access the information and advice they need, the local authority should have a clear view of the information and advice services available locally and what they provide. The local authority should take a role in joining up information and advice organisations locally so they can work collaboratively. The local authority should help information and advice providers and people to understand the role of each information and advice provider so people can access the right provider at the right time and not be sent round in circles. Local authorities should provide and publicise links and information on access to wider sources of information and advice, including those available nationally.
3.49 Local authorities should ensure that staff, including front line staff, are able to support people to access the information and advice they need to make good financial decisions. Staff should have the knowledge to direct people to the financial information and advice they need, explaining the differences and potential benefits from seeking regulated or non-regulated financial advice.
Facilitating access to independent financial information and advice
3.50 A key role for local authorities, when it would be inappropriate to provide it itself, is to facilitate access to financial information and advice which is impartial and independent of a local authority. This should include both generic free and fee-based advice as well as services providing regulated forms of financial advice. ‘Facilitating access’ may include making people aware of specific sources of information and advice that are available and giving information about how to use them. Local authorities should make people aware which independent services may charge for the information and advice they provide. Local authorities should be able to actively describe the general benefits of independent information and advice and, based on what is known of an individual’s circumstance, be able to explain the reasons why it may be beneficial for a person to take independent financial advice.
3.51 Where a person may be considering taking regulated financial advice local authorities are not required or encouraged to make a direct referral to one individual independent financial adviser, but they should actively help and direct a person to a choice of advisers regulated by the Financial Conduct Authority with the appropriate qualifications and accreditation. The local authority should ensure that they do this on a transparent basis.
3.52 Further practice guidance is also available to support local authorities to facilitate access to independent financial information and advice.
Information and advice on adult safeguarding
3.53 The government expects local authorities and others to help people with care and support needs, who may be at risk of abuse or neglect as a result of those needs, keep safe. But this must not mean preventing them making their own choices and having control over their lives. Everyone in the community should understand the importance of safeguarding and help keep people safe (see chapter 14 on safeguarding).
3.54 The local authority must provide information and advice on how to raise concerns about the safety or wellbeing of an adult who has needs for care and support and should support public knowledge and awareness of different types of abuse and neglect, how to keep yourself physically, sexually, financially and emotionally safe, and how to support people to keep safe. The information and advice provided must also cover who to tell when there are concerns about abuse or neglect and what will happen when such concerns are raised, including information on how the local Safeguarding Adults Board works.
Complaints
3.55 Current complaints provision in relation to local authority social services is set out in regulations. [footnote 6] The provisions of the regulations mean that anyone who is dissatisfied with a decision made by the local authority would be able to make a complaint about that decision and have that complaint handled by the local authority. The local authority must make its own arrangements for dealing with complaints in accordance with the 2009 regulations. As an essential part of how the whole system operates, under the 2009 regulations the local authority’s arrangements must ensure that those who make complaints receive, as far as reasonably practicable, assistance to enable them to understand the complaints procedure or advice on where to obtain such assistance.
Reviewing and developing a plan or strategy
3.56 Local differences and different starting points will mean that each local authority will need to develop and implement a plan regarding their information and advice services that matches their circumstances and meets the needs of its population. The information and advice service should be aligned with wider local authority strategies such as market shaping and commissioning, and with joint area strategies with health. The development of such plans should have regard to some common principles, including:
- involving people who use services and carers, interested organisations and service providers in determining what is needed and how it is provided
- being available at the right time for people who need it, in a range of accessible formats and through a range of channels
- meeting the needs of all groups
- being clear, comprehensive and impartial
- be consistent, accurate and up-to-date
- meeting quality standards, such as the Advice Quality Standard
- being based on a detailed analysis of the needs of the local population served by the local authority
- being commissioned in tandem with other relevant support and independent advocacy services
- avoiding unnecessary duplication
- directing people to sources of further information
- be used to inform future planning
- ensuring appropriate quality assurance and review, including customer feedback to make sure that the service learns from experience and continuously improves
3.57 The plan should build on local and national best practice and make best use of national resources. These national resources include guidance on principles for local information and advice strategies, case studies and practice examples.
3.58 The local authority must exercise its functions under the Care Act, including the duty to provide an information and advice service, with a view to integrating care and support provision with health and health-related issues (including housing). It must also co-operate more generally with each of its relevant partners taking account of their respective functions (see chapter 15 on integration, cooperation and partnerships). The Local Government and Public Involvement in Health Act 2007 (as amended by the Health and Social Care Act 2012), provides that local authorities are under a duty to work with their local CCGs, and other partners through the Health and Wellbeing Board to undertake Joint Strategic Needs Assessments for their areas and to develop Joint Health and Wellbeing Strategies. Statutory Guidance published in March 2013 makes clear that the Joint Strategic Needs Assessment and Joint Health and Wellbeing Strategies must be published, and have specific regard to ‘what health and social care information the community needs, including how they access it and what support they may need to understand it’.
3.59 The development and implementation of a wider plan or strategy on the provision of information and advice on care and support should be led by the local authority, acting as the coordinator and where appropriate the commissioners of information and advice services.
3.60 The development of information and advice plans and their implementation should be an ongoing and dynamic process, involving all relevant stakeholders, rather than a one off occurrence. The plan and the resulting service should adapt to changing needs and as a result of feedback and learning on what works best. The plan should be reviewed at agreed intervals. As a minimum, the process of developing a local plan should include:
- engagement with people, carers and family members, to understand what is working and not working for them, their preferences and how their information advice and advocacy needs can best be met
- adopting a ‘co-production’ approach to their plan, involving user groups and people themselves, other appropriate statutory, commercial and voluntary sector service providers, and make public the plan once finalised
- mapping to understand the range of information, advice and advocacy services, including independent financial advice and different providers available
- coordination with other statutory bodies with an interest in care and support, including local CCGs, Health and Wellbeing Boards, local Healthwatch and neighbouring local authorities
- building into the plan opportunities to record, measure and assess the impact of information and advice services rather than simply service outputs
3.61 In deciding the types of information and advice services to be provided, each local authority will need to analyse and understand the specific needs of its population. Some of the factors and circumstances that local authorities should consider in doing this will often be identified in Joint Strategic Needs Assessments. These factors may include, but are not limited to:
- the ethnic composition of the local area, including languages used
- the identity and nature of hard to reach groups
- the split between those whose care and support is (or is likely to be) arranged or funded by the person and the state
- demographic trends relating to health and care needs, age and disability
- how people access information and advice at the moment and the quality of information and advice services
- an appropriate balance between the needs of its local population for information and the needs people will have for access to advice
- the current sufficiency of supply and the range of information and advice providers from different sectors (including their prospects for growth)
3.62 Local authorities should review and publish information about the effectiveness of the information and advice service locally, including customer satisfaction and may wish to build these into the local Joint Health and Wellbeing Strategies.
3.63 These actions will support local authorities to meet their duties for understanding and promoting the efficient and effective market of services for meeting care and support needs in its area (see chapter 4).
3.64 As part of their plans, local authorities should consider the persons and/or places most likely to come into contact with people in need of information and advice at these and other critical points in the person’s care and support journey. This may be another statutory party, such as a GP or other NHS professional, other professionals, such as a solicitor or funeral director, care and support and housing providers, or a local group, user-led or charitable organisation, rather than the local authority itself. Local authorities should consider whether independent sources of information and advice may in some circumstances be more trusted – and therefore more effective – than the local authority itself (see chapter 15, para. 15.71) [footnote 7].
3.65 In addition or instead of direct provision, local authorities should consider whether it is in a person’s best interests that they be signposted, directed or referred to independent sources of information and advice. In particular, people should be signposted to appropriate independent information and advice when they are entering into a legal agreement with a local authority or other third party, such as a deferred payment agreement or committing to a top-up, or they wish to question, challenge or appeal a decision of the local authority or other statutory body.
3.66 People often come into contact with care and support services and need to make important decisions at a time of crisis. A local authority plan should therefore allow for the urgent provision of information and advice when necessary. Local authorities should work with health organisations and other partners to provide targeted information and advice to people in these critical situations and where people have long-term health conditions such as dementia (see paragraph 3.26).
3.67 In their information and advice planning, local authorities will need to weigh up the likely demand and effectiveness of these different channels of communication, some of which will incur substantially higher costs than others. A plan that relies disproportionately on provision of information and advice through the authority’s website, or third party websites, is unlikely to meet the authority’s duty under the Act to establish and maintain a service to provide information and advice on care and support.
3.68 Local authorities will need to consider in their information and advice planning the appropriate interface and balance between local and national sources of information and advice. Where appropriate, local authorities should signpost or refer people to national sources of information and advice where these are recognised as the most useful source. Examples might include:
- the NHS Choices website [footnote 8] which contains a mix of textual content, videos, and tools such as the online quality profiles of registered care providers in local areas. Local authorities are encouraged to add local sources of information and advice to the online profiles and make sure their local registered care providers add information on the services and support they offer.
- NHS Choices website. Health A to Z, detailed information on specific health conditions and how/where to access health services
- Carers Direct – national telephone helpline: Telephone 0300 123 1053
- Money Advice Service
- the Care Quality Commission
- the Local Government Ombudsman
- consumer websites providing people with information and advice, including on managing their finances well, for example Which? Elderly Care
- national charities and/or advice services supporting people with disabilities or older people and those with expert knowledge of specific conditions (for example, deaf blind). For example, Age UK ; Independent Age; Alzheimer’s Society and Sense, and their national telephone advice/help lines
- national charities and advice services for carers, for example Carers UK or Age UK
- national resources related to housing, accommodation and housing related support, for example FirstStop Advice or Foundations
3.69 Some national providers, for example the Money Advice Service and NHS Choices, may also offer free access to tools, resources and information content that can be integrated into local authority websites or delivered in paper formats. Local authorities are encouraged to explore how they can make the most of cost-effective partnership opportunities with national providers. Referral or signposting to national sources should only occur where this is deemed to be in the best interests of the person and their circumstances and should not take the place of local services necessary for local authorities to discharge their duty under the Act. Local authorities will need to find the appropriate balance between local and national provision to cost-effectively meet their local need.
3.70 Information and advice, whether provided directly by a local authority or by third parties as part of the information and advice service that the local authority establishes and maintains, should be of a good standard and, where appropriate, delivered by trained or suitably qualified individuals.
4. Market shaping and commissioning of adult care and support
This chapter provides guidance on section 5 of the Care Act 2014 and covers:
- the principles which should underpin market-shaping and commissioning activity:
- focusing on outcomes and wellbeing
- promoting quality services, including through workforce development and remuneration and ensuring appropriately resourced care and support
- supporting sustainability
- ensuring choice
- co-production with partners
- the steps which local authorities should take to develop and implement local approaches to market-shaping and commissioning:
- designing strategies that meet local needs
- engaging with providers and local communities
- understanding the market
- facilitating the development of the market
- integrating their approach with local partners
- securing supply in the market and assuring its quality through contracting
4.1 High-quality, personalised care and support can only be achieved where there is a vibrant, responsive market of service providers. The role of the local authority is critical to achieving this, both through the actions it takes to commission services directly to meet needs and the broader understanding of and interactions it undertakes with, the wider market, for the benefit of all local people and communities.
4.2 The Care Act places new duties on local authorities to promote the efficient and effective operation of the market for adult care and support as a whole. This can be considered a duty to facilitate the market, in the sense of using a wide range of approaches to encourage and shape it, so that it meets the needs of all people in their area who need care and support, whether arranged or funded by the state, by the individual themselves, or in other ways. The ambition is for local authorities to influence and drive the pace of change for their whole market, leading to a sustainable and diverse range of care and support providers, continuously improving quality and choice, and delivering better, innovative and cost-effective outcomes that promote the wellbeing of people who need care and support.
4.3 The market for care and support services is part of a wider system in which much of the need for care and support is met by people’s own efforts, by their families, friends or other carers, and by community networks. Local authorities have a vital role in ensuring that universal services are available to the whole population and where necessary, tailored to meet the needs of those with additional support requirements (for example housing and leisure services). Market shaping and commissioning should aim to promote a market for care and support that should be seen as broadening, supplementing and supporting all these vital sources of care and support.
4.4 Local authorities should review the way they commission services, as this is a prime way to achieve effective market shaping and directly affects services for those whose needs are met by the local authority, including where funded wholly or partly by the state.
4.5 At a time of increasing pressure on public funds, changing patterns of needs, and increasing aspirations of citizens, together with momentum for integrated services, joint commissioning, and choice for individuals, it is suggested that fundamental changes to the way care and support services are arranged may be needed, driven through a transformation of the way services are led, considered and arranged (PDF, 1.18MB). Commissioning and market shaping are key levers for local authorities in designing and facilitating a healthy market of quality services.
Definitions
4.6 Market shaping means the local authority collaborating closely with other relevant partners, including people with care and support needs, carers and families, to encourage and facilitate the whole market in its area for care, support and related services. This includes services arranged and paid for by the state through the authority itself, those services paid by the state through direct payments, and those services arranged and paid for by individuals from whatever sources (sometimes called ‘self-funders’), and services paid for by a combination of these sources. Market shaping activity should stimulate a diverse range of appropriate high quality services (both in terms of the types of services and the types of provider organisation), and ensure the market as a whole remains vibrant and sustainable.
4.7 The core activities of market shaping are to engage with stakeholders to develop understanding of supply and demand and articulate likely trends that reflect people’s evolving needs and aspirations, and based on evidence, to signal to the market the types of services needed now and in the future to meet them, encourage innovation, investment and continuous improvement. It also includes working to ensure that those who purchase their own services are empowered to be effective consumers, for example by helping people who want to take direct payments make informed decisions about employing personal assistants. A local authority’s own commissioning practices are likely to have a significant influence on the market to achieve the desired outcomes, but other interventions may be needed, for example, incentivising innovation by user-led or third sector providers, possibly through grant funding.
4.8 Commissioning is the local authority’s cyclical activity to assess the needs of its local population for care and support services, determining what element of this needs to be arranged by the authority, then designing, delivering, monitoring and evaluating those services to ensure appropriate outcomes. From the 1990s onwards care services have been increasingly procured from the independent sector (for example, not directly commissioned from and provided by an authority itself) and covered all services that the authority arranged for people receiving state funding. Since 2007 when personalisation became a mainstream policy, commissioning has also covered activity to ensure that sufficient and appropriate services are available to meet the needs of growing numbers of people with personal budgets and direct payments. This has changed the commissioning role, as purchasing decisions have been increasingly devolved to individuals and families and direct procurement using block contracts has reduced. Commissioning has come to be shaped more by the outcomes commissioners and individuals identify, rather than volumes of activity expected and commissioners have sought to facilitate flexible arrangements with providers for other forms of service to support choice and control, such as Individual Service Funds (ISFs).
4.9 Procurement is the specific functions carried out by the local authority to buy or acquire the services which the local authority has a duty to arrange to meet people’s needs, to agreed quality standards so as to provide effective value for money to the public purse and deliver its commissioning strategy.
4.10 Contracting is the means by which that process is made legally binding. Contract management is the process that then ensures that the services continue to be delivered to the agreed quality standards. Commissioning encompasses procurement but includes the wider set of strategic activities.
4.11 This statutory guidance describes, at a high level, the themes and issues that local authorities should have regard to when carrying out duties to shape their local markets and commission services. Market shaping, commissioning, procurement and contracting are inter-related activities and the themes of this guidance will apply to each to a greater or lesser extent depending on the specific activity.
Principles of market-shaping and commissioning
Focusing on outcomes
4.12 Local authorities must ensure that the promotion of the wellbeing of individuals who need care and support, and the wellbeing of carers, and the outcomes they require, are central to all care and support functions in relation to individuals, emphasising the importance of enabling people to stay independent for as long as possible.
4.13 Local authorities will need to understand the outcomes which matter most to people in their area, and demonstrate that these outcomes are at the heart of their local strategies and approaches.
4.14 Local authorities should consider the Adult Social Care Outcomes Framework (ASCOF), in addition to any locally-collected information on outcomes and experiences (for example, from local consumer research), when framing outcomes for their locality and groups of people with care and support needs. Local authorities should have regard to guidance from the Think Local Act Personal (TLAP) partnership when framing outcomes for individuals, groups and their local population, in particular the Making It Real ‘I’ statements, which set out what good personalised care and support should look like from the perspective of people with care and support needs, carers and family members. Outcomes should be considered both in terms of outcomes for individuals and outcomes for groups of people and populations. Local authorities should consider the emerging revised Care Quality Commission standards for quality and any emerging national frameworks for defining outcomes. Local authorities may find the Chartered Institute of Housing’s Service Quality Tool for housing-related services useful. This builds on and updates the Quality Assessment Framework (QAF).
4.15 Local authorities should consider analysing and presenting local needs for services in terms of outcomes required. Local authorities should ensure that achieving better outcomes is central to its commissioning strategy and practices, and should be able to demonstrate that they are moving to contracting in a way that has an outcome basis at its heart. Local authorities should consider emerging best practice on outcomes-based commissioning.
4.16 Outcomes-based services mean developing service arrangements that are defined on the basis of an agreed set of outcomes either for an individual or a group of people. Moving to an outcomes-based approach therefore means changing the way services are bought: from units of provision to meet a specified need (for example, hours of care provided) to what is required to ensure specified measurable outcomes for people are met. The approach should emphasise prevention, enablement, ways of reducing loneliness and social isolation and promotion of independence as ways of achieving and exceeding desired outcomes, as well as choice in how people’s needs are met. Moving to an outcomes-based approach will need to recognise that some outcomes are challenging to assess and local authorities may wish to consider involving service providers when considering how service evaluations can be interpreted. Outcomes should be used as a principal measure for quality assurance of services.
4.17 In encouraging outcomes-based services, consideration should be given to how services are paid for. Local authorities should consider incorporating elements of ‘payments-by-outcomes’ mechanisms, where practical, to emphasise and embed this commissioning approach which is based on specifying the outcomes to be achieved, rather than the service outputs to be delivered. Whilst payments-by-outcomes may be theoretically the most appropriate approach for outcomes-based services, it is recognised that proxies for outcomes may be required to make the approach practical. For example, an outcome an authority may wish to measure might be someone’s personal outcome ‘I want to maintain a nutritious and balanced diet’, but a proxy measure that is observable, attributable and capable of being described, may be the person receiving help with meal preparation at agreed and specified times. Care logs documenting punctual assistance in meal preparation, in conjunction with positive feedback from the person receiving care about support received might be used as part of the basis of payment. It is also recognised that whilst these mechanisms are more commonplace in other types of commissioning, they are in their infancy for adult social care.
4.18 The design of any mechanism should, however, be introduced in cooperation with stakeholders and partners to ensure it is sustainable and ensure that innovation, and individual choice and control are not undermined. Any move to payments by outcomes should be achieved such that smaller, specialist, voluntary sector and community-based providers are not excluded from markets or disadvantaged, because for example, they did not have appropriate IT systems.
4.19 Local authorities should keep under review emerging ideas and best practice about outcomes based commissioning and payments by outcomes. For example:
Local authorities should have regard to the evolving guidance ‘Commissioning for Better Outcomes’ that was co-produced by the Department of Health, ADASS, LGA together with provider representatives and people with lived experience of care and support. This guidance is intended to support peer review and self-assessment of local authority commissioning, and represents a practical approach that underpins the themes of this statutory guidance.
4.20 Section 2 of the Care Act outlines local authorities’ role in preventing, reducing or delaying the need for care and support. This includes how the authority facilitates and commissions services and how it works with other local organisations to build community capital and make the most of the skills and resources already available in the area. [footnote 10] Local authorities should consider working not just with traditional public sector partners like health, but also with a range of other partners to engage with communities to understand how to prevent problems from arising. [footnote 11]
Promoting quality
4.21 Local authorities must facilitate markets that offer a diverse range of high-quality and appropriate services. In doing so, they must have regard to ensuring the continuous improvement of those services and encouraging a workforce which effectively underpins the market through:
The quality of services provided and the workforce providing them can have a significant effect on the wellbeing of people receiving care and support, and that of carers, and it is important to establish agreed understandable and clear criteria for quality and to ensure they are met.
4.22 When considering the quality of services, local authorities should be mindful of the capacity, capability, timeliness, continuity, reliability and flexibility of services delivered to support wellbeing, where appropriate, using the definitions that underpin the CQC’s fundamental standards of care as a minimum, and having regard to the ASCOF framework of population outcomes. High quality services should enable people who need care and support, and carers, to meet appropriate personal outcome measures, for example, a domiciliary care service which provides care 2 days a week so that a carer who normally provides care can go to work, is not a quality service if it is not available on the specified days, or the care workers do not arrive in time to allow the carer to get to work on time.
4.23 Local authorities should also consider other relevant national standards including those that are aspirational, for example, any developed by the National Institute of Health and Care Excellence (NICE). [footnote 12]
4.24 Local authorities should encourage a wide range of service provision to ensure that people have a choice of appropriate services; appropriateness is a fundamental part of quality. For example, a working age person should be able to choose care and support tailored for their situation, and not be faced with only a choice of facilities designed for older people, as this is unlikely to be appropriate to their situation, regardless of how high quality the facilities may be in their own contexts. Appropriate services will meet people’s needs and reasonable preferences.
4.25 When arranging services themselves, local authorities must ensure their commissioning practices and the services delivered on their behalf comply with the requirements of the Equality Act 2010, and do not discriminate against people with protected characteristics; this should include monitoring delivery against the requirements of that Act. When shaping markets for services, local authorities should work to ensure compliance with this Act for services provided in their area that are not arranged and/or paid for by them. Local authorities should consider care and support services for their appropriateness for people from different communities, cultures and beliefs.
4.26 Local authorities should encourage services that respond to the fluctuations and changes in people’s care and support needs, for example someone with fluctuating mobility or visual impairment. Local authorities should support the transition of services throughout the stages of people with care and support needs’ lives to ensure the services provided remain appropriate. This is particularly important, for example, for young people with care and support needs and young carers transitioning to adulthood.
Example: Ensuring provision of appropriate services
Young people move from children’s to adult care and support or providing support for situations where young carers become adults
For instance, many young people with learning disabilities leave full-time education at around this age and require new forms of care and support to live independently thereafter. Ensuring that services are made available to meet those needs is better for the quality of life of the young person in question. This could include things such as employment support, training, developing friendships or advice on housing options. It is equally important to think about ways of supporting carers at this time: some parent carers need extra support to juggle caring and paid work after their child leaves full time education. Loss of paid employment can have a significant impact on the carer’s wellbeing and self-esteem as well as a significant impact on the family’s financial circumstances. Similar issues can affect young carers. Taking a whole family approach to care and support planning that sets out a ‘five-day offer’ or appropriate supported living options for a young person, and support for a carer to manage an increased caring role (that allows them to stay in paid work if they wish to do so) can help families manage the transition and save money by avoiding unwanted out-of-county placements.
4.27 Local authorities should commission services having regard to the cost-effectiveness and value for money that the services offer for public funds. The Local Government Association Adult Social Care Efficiency Programme has advice on these issues and may be helpful.
4.28 People working in the care sector play a central role in providing high quality services. Local authorities must consider how to help foster, enhance and appropriately incentivise this vital workforce to underpin effective, high quality services. [footnote 13] [footnote 14]
4.29 Local authorities should consider, in particular, how to encourage training and development for the care and support workforce, including for the management of care services, through, for example, national standards recommended by Skills for Care:
- Care Quality Commission regulations
- care certificate
- manager induction standards
- national occupational standards
And have regard to funding available through grants to support the training of care workers in the independent sector:
- an example of collaborative training by Surrey, East Sussex & Brighton & Hove
- Workforce Development Fund
- Individual Employer Funding
- Workforce Development Innovation Fund
- Social Work - assessed and supported year in employment
Local authorities should consider encouraging the training and development of care worker staff to at least the standard of the emerging Care Certificate currently being developed by Health Education England, Skills for Care and Skills for Health.
4.30 When commissioning services, local authorities should assure themselves and have evidence that service providers deliver services through staff remunerated so as to retain an effective workforce. Remuneration must be at least sufficient to comply with the national minimum wage legislation for hourly pay or equivalent salary. This will include appropriate remuneration for any time spent travelling between appointments. Guidance on these issues can be found on the HMRC website.
4.31 When commissioning services, local authorities should assure themselves and have evidence that contract terms, conditions and fee levels for care and support services are appropriate to provide the delivery of the agreed care packages with agreed quality of care. This should support and promote the wellbeing of people who receive care and support, and allow for the service provider ability to meet statutory obligations to pay at least the national minimum wage and provide effective training and development of staff. It should also allow retention of staff commensurate with delivering services to the agreed quality, and encourage innovation and improvement. Local authorities should have regard to guidance on minimum fee levels necessary to provide this assurance, taking account of the local economic environment. This assurance should understand that reasonable fee levels allow for a reasonable rate of return by independent providers that is sufficient to allow the overall pool of efficient providers to remain sustainable in the long term. The following tools may be helpful as examples of possible approaches:
- Homecare Association’s Minimum Price for Homecare
- Laing and Buisson toolkit to understand fair price for residential care
- ADASS paying for care calculator
4.32 Local authorities should ensure that they themselves have functions and systems in place to fulfil their duties on market shaping and commissioning that are fit for purpose, with sufficient capacity and capability of trained and qualified staff to meet the requirements set out in the Care Act and this statutory guidance. In particular, local authorities should encourage relevant staff to be trained or developed to meet the National Skills Academy standards and programmes of training for care and support commissioners ‘Commissioning Now’, or equivalent, and appropriate standards for commissioning related services such as housing services where appropriate. Local authorities should consider the skills and capabilities needed to support new approaches to commissioning, for example, outcomes-based and integrated commissioning. Local authorities should have regard to the emerging skill levels and qualifications being developed for commissioning staff by Skills for Care.
Supporting sustainability
4.33 Local authorities must work to develop markets for care and support that - whilst recognising that individual providers may exit the market from time to time - ensure the overall provision of services remains healthy in terms of the sufficiency of adequate provision of high quality care and support needed to meet expected needs. This will ensure that there are a range of appropriate and high quality providers and services for people to choose from.
4.34 Local authorities should understand the business environment of the providers offering services in their area and seek to work with providers facing challenges and understand their risks. Where needed, based on expected trends, local authorities should consider encouraging service providers to adjust the extent and types of service provision. This could include signalling to the market as a whole the likely need to extend or expand services, encourage new entrants to the market in their area, or if appropriate, signal likely decrease in needs – for example, drawing attention to a possible reduction in care home needs, and changes in demand resulting from increasing uptake of direct payments. The process of developing and articulating a Market Position Statement or equivalent should be central to this process.
4.35 Local authorities should consider the impact of their own activities on the market as a whole, in particular the potential impact of their commissioning and re-commissioning decisions, and how services are packaged or combined for tendering, and where they may also be a supplier of care and support. The local authority may be the most significant purchaser of care and support in an area, and therefore its approach to commissioning will have an impact beyond those services which it contracts. Local authorities must not undertake any actions which may threaten the sustainability of the market as a whole, that is, the pool of providers able to deliver services of an appropriate quality, for example, by setting fee levels below an amount which is not sustainable for providers in the long-term.
4.36 Local authorities should have effective communications and relationships with providers in their area that should minimise risks of unexpected closures and failures, and have effective interaction and communication with the Care Quality Commission (CQC) about the larger and most difficult to replace providers that CQC will provide financial oversight for. Local authorities should review the intelligence they have about the sustainability of care providers drawn from market shaping, commissioning and contract management activities. [footnote 15] Where the authority believes there is a significant risk to a provider’s financial viability, and where they consider it would be in the best interests of service users, the authority should consider what assistance may be provided or brokered to help the provider return to viability, and consider what actions might be needed were that provider to fail. For example, where a local authority has arranged services for people with a provider that appears to be at risk, undertaking early planning to identify potential replacement service capacity. Where it is apparent to a local authority that a provider is likely to imminently fail financially, either through its own intelligence or through information from the CQC, the authority should prepare to take steps to ensure continuity of care and support for people who have their care and support provided by that provider (see chapter 5 on managing provider failure).
Ensuring choice
4.37 Local authorities must encourage a variety of different providers and different types of services. This is important in order to facilitate an effective open market, driving quality and cost-effectiveness so as to provide genuine choice to meet the range of needs and reasonable preferences of local people who need care and support services, including for people who choose to take direct payments, recognising, for example, the challenges presented in remote rural areas for low volume local services.
4.38 Local authorities must encourage a range of different approaches to services to ensure people have a genuine choice of different types of service. This may be achieved by encouraging different types of service provider organisation, for example, independent private providers, third sector, voluntary and community based organisations, including user-led organisations, mutual and small businesses. Local authorities should note that the involvement of people with specific lived experience of the type of needs being met, may lead to better outcomes for people who use services and carers as they directly empathise with service users. This should recognise that the different underpinning philosophies, cultural sensitivity and style of service of these organisations may be more suited to some people with care and support needs. Local authorities should consider encouraging and supporting providers or taking other steps to promote an appropriate balance of provision between types of provider, having regard to competition rules and the need for fairness and legal requirements for all potential providers who may wish to compete for contracts. The TLAP guidance commissioning for provider diversity may be helpful to commissioners.
4.39 When commissioning services to meet people’s eligible needs, where a local authority develops approved lists and frameworks that are used to limit the number of providers they work with, for example within a specific geographical area or for a particular service type to achieve strategic partnerships and value for money, the local authority must consider how to ensure that there is still a reasonable choice for people who need care and support.
4.40 For universally available services - for example, prevention - where the local authority does not have a duty to directly arrange services, it should have regard to facilitating this market through market shaping activity to encourage a diversity of service provision. If the authority decides to augment such universal services by directly contracting itself with one or more provider organisations, it should nevertheless continue to ensure that the overall mix of available services presents meaningful choice to people who need these services.
4.41 Local authorities should encourage a genuine choice of service type, not only a selection of providers offering similar services, encouraging, for example, a variety of different living options such as shared lives, extra care housing, supported living, support provided at home, and live-in domiciliary care as alternatives to homes care, and low volume and specialist services for people with less common needs. Local authorities may find the TLAP guidance ‘Top Tips: commissioning for market diversity’ helpful.
4.42 Choice for people who need care and support and carers should be interpreted widely. Local authorities should encourage choice over the way services are delivered, examples would include: developing arrangements so that care can be shared between an unpaid carer or relative and a paid care worker, a choice over when a service is delivered, choice over who is a person’s key care worker, arranging for providers to collaborate to ensure the right provision is available, for example, a private provider and a voluntary organisation working together, choice over when a service is delivered. [footnote 16]
4.43 Local authorities must have regard to ensuring a sufficiency of provision – in terms of both capacity and capability – to meet anticipated needs for all people in their area needing care and support – regardless of how they are funded. This will include regularly reviewing trends in needs including multiple and complex needs, outcomes sought and achieved, and trends in supply, anticipating the effects and trends in prevention and community-based assets, and through understanding and encouraging changes in the supply of services and providers’ business and investment decisions. [footnote 17]
4.44 When considering the sufficiency and diversity of service provision, local authorities should consider all types of service that are required to provide care and support for the local authority’s whole population, including, for example:
- support services and universal and community services that promote prevention
- domiciliary (home) care
- homes and other types of accommodation care
- nursing care
- live-in care services
- specialist care
- support for carers
- reablement services
- sheltered accommodation and supported living
- shared lives services
- other housing options
- community support
- counselling
- social work
- information, brokerage, advocacy and advice services
- direct payment support organisations
4.45 This will include keeping up to date with innovations and developments in services, networking through for example, the Association of Directors of Adult Social Services (ADASS), TLAP, and the Local Government Association (LGA).
4.46 Local authorities should facilitate the personalisation of care and support services, encouraging services (including small, local, specialised and personal assistant services that are highly tailored), to enable people to make meaningful choices and to take control of their support arrangements, regardless of service setting or how their personal budget is managed. Local authorities should have regard to the TLAP partnership agreement that sets out how shaping markets to meet people’s needs and aspirations, including housing options, can promote choice and control. Alongside the suitability of living accommodation in Section 1 of the Act, Local authorities should consider how they can encourage the development of accommodation options that can support choice and control and promote wellbeing. Personalised care and support services should be flexible so as to ensure people have choices over what they are supported with, when and how their support is provided and wherever possible, by whom. The mechanism of Individual Service Funds by service providers, which are applicable in many different service types, can help to secure these kinds of flexibilities for people and providers.
4.47 Local authorities should help people who fund their own services or receive direct payments, to ‘micro-commission’ care and support services and/or to pool their budgets, and should ensure a supporting infrastructure is available to help with these activities. Many local authorities, for example, are utilising web-based systems such as e-Marketplaces for people who are funding their own care or are receiving direct payments to be able to search for, consider and buy care and support services on-line, consider joint purchases with others. This often involves offering information and advice about, for example, the costs and quality of services and information to support safeguarding. This should include facilitating organisations that support people with direct payments and those whose care is funded independently from the local authority to become more informed and effective consumers and to overcome potential barriers such as help to recruit and employ personal assistants and to assist in overcoming problems and issues. This activity should help to match people’s wider needs with services.
4.48 Local authorities must facilitate information and advice to support people’s choices for care and support. This should include where appropriate through services to help people with care and support (PDF, 1.09MB) needs understand and access the systems and processes involved and to make effective choices. This is a key aspect of the new duty to establish and maintain a universal information and advice service locally as set out in Section 4 of the Care Act. Information and advice services should be reviewed for effectiveness using people’s experiences and feedback. This feedback forms part of the overall information a local authority considers about people’s needs and aspirations.
4.49 Local authorities should facilitate local markets to encourage a sufficiency of preventative, enablement and support services, including support for carers to make caring more sustainable, such as interpreters, signers and communicator guides, and other support services such as ‘telecare’, home maintenance and gardening that may assist people achieve more independence and supports the outcomes they want.
4.50 Local authorities should encourage flexible services to be developed and made available that support people who need care and support, and carers who need support, to take part in work, education or training. Services should be encouraged that allow carers who live in one local authority area but care for someone in another local authority area to access services easily, bearing in mind guidance on ordinary residence.
Co-production with stakeholders
4.51 Local authorities should pursue the principle that market shaping and commissioning should be shared endeavours, with commissioners working alongside people with care and support needs, carers, family members, care providers, representatives of care workers, relevant voluntary, user and other support organisations and the public to find shared and agreed solutions. This should be in line with the Building Capacity and Partnership in Care Agreement. The TLAP guidance on co-production may be helpful, in particular the web-based tool People not process – Co-production in Commissioning.
Developing local strategies
4.52 Commissioning and market shaping should be fundamental means for local authorities to facilitate effective services in their area and it is important that authorities develop evidence-based local strategies for how they exercise these functions, and align these with wider corporate planning. Local authorities should have in place published strategies that include plans that show how their legislative duties, corporate plans, analysis of local needs and requirements (integrated with the Joint Strategic Needs Assessment and Joint Health and Wellbeing Strategy), thorough engagement with people, carers and families, market and supply analysis, market structuring and interventions, resource allocations and procurement and contract management activities translate (now and in future) into appropriate high quality services that deliver identified outcomes for the people in their area and address any identified gaps. [footnote 18]
4.53 Since 2007 there has been a duty on local authorities and latterly clinical commissioning groups, through health and wellbeing boards, to undertake Joint Strategic Needs Assessments (JSNA). JSNA is a process that assesses and maps the needs and demand for health and care and support, supports the development of joint Health and Wellbeing Strategies to address needs, understands community assets and informs commissioning of local health and care and support services that together with community assets meet needs.
4.54 Market shaping and commissioning intentions should be cross-referenced to JSNA, and should be informed by an understanding of the needs and aspirations of the population and how services will adapt to meet them. Strategies should be informed by and emphasise preventative services that encourage independence and wellbeing, delaying or preventing the need for acute interventions. Statutory guidance on JSNA and Joint Health and Wellbeing Strategies (PDF, 180KB) was published in March 2013. The ambition is for market shaping and commissioning to be an integral part of understanding and delivering the whole health and care economy, and to reflect the range and diversity of communities and people with specific needs, in particular:
- people needing care and support themselves (through for example, consumer research)
- carers
- carer support organisations
- health professionals
- care and support managers and social workers (and representative organisations for these groups)
- relevant voluntary, user and other support organisations
- independent advocates
- the wider local population
- provider organisations (including where appropriate housing providers)
- other tiers of local government
4.55 A co-produced approach will stress the value of meaningful engagement with people at all stages, through design, delivery and evaluation, rather than simply as ‘feedback’. Local authorities should publish and make available their local strategies for market shaping and commissioning, giving an indication of timescales, milestones and frequency of activities, to support local accountability and engagement with the provider market and the public.
4.56 It is suggested that a local authority can best commence its duties under Sections 5 (market shaping and commissioning) and 48 to 52 (provider failure) of the Care Act by developing with providers and stakeholders a published Market Position Statement. It may be helpful for Market Position Statements from neighbouring local authority areas to be coordinated to ensure a degree of consistency for people who will use the documents; this is particularly true for urban areas.
4.57 Local authorities should review strategies related to care and support together with stakeholders to ensure they remain fit for purpose, learn lessons, and adapt to incorporate emerging best practice, noting that peer review has a strong track record in driving improvement. It is suggested that reporting against strategies for care and support should form part of the local authority’s Local Account.
4.58 Many public sector bodies, including local authorities, have radically transformed services by reconsidering commissioning in a strategic context. The Government’s Commissioning Academy is working to promote such transformational approaches and local authorities should have regard to the emerging best practice it is producing.
4.59 Developing a diverse market in care and support services can boost employment and create opportunities for local economic growth, through for example, increasing employment opportunities for working-age people receiving care and carers, and developing the capacity of the care workforce. Local authorities should consider how their strategies related to care and support can be embedded in wider local growth strategies, for example, engaging care providers in local enterprise partnerships.
4.60 Recognising that changes to adult care and support are taking place at a time of the need to deliver services from constrained resources, local authorities should have regard to best practice on efficiency and value for money, in particular the LGA’s Adult Social Care Efficiency Programme.
4.61 Local authority strategies should adhere to general standards, relevant laws and guidance, including the Committee of Standards in Public Life principles of accountability (PDF, 1MB), regularity and ensuring value for money alongside quality, and the HM Treasury guidance on managing public money.
4.62 Local authorities should develop standards on transparency and accountability to ensure citizens are able to contribute to and understand policy and review delivery. Standards should be in line with the codes of practice drawn up by the Department of Communities and Local Government.
4.63 Local authorities should take the lead to engage with a wide range of stakeholders and citizens in order to develop effective approaches to care and support, including through developing the JSNA and a Market Position Statement. While the duties under section 5 of the Care Act fall upon local authorities, successful market shaping is a shared endeavour that requires a range of coordinated action by commissioners and providers, working together with the citizen at the centre. Local authorities should engage and cooperate with stakeholders to reflect the range and diversity of communities and people with specific needs, for example:
- people needing care and support themselves and their representative organisations
- carers and their representative organisations
- health professionals
- social care managers and social workers
- independent advocates
- support organisations that help people who need care consider choices (including financial options)
- provider organisations (including where appropriate private housing providers and registered social landlords)
- the wider local population including individuals and communities who are less frequently heard (for example, LGBT communities where there may be a lack of data on care and support needs and preferences) or at risk from exclusion, including those who have communication issues and involving representatives of those who lack mental capacity [footnote 19].
4.64 Engagement with people needing care and support, people likely to need care and support, carers, independent advocates, families and friends, should emphasise understanding the needs of individuals and specific communities, what aspirations people have, what outcomes they would like to achieve, their views on existing services and how they would like services to be delivered in the future. [footnote 20] It should also seek to identify the types of support and resources or facilities available in the local community which may be relevant for meeting care and support needs, to help understand and build community capacity to reinforce the more formal, regulated provider market. In determining an approach to engagement, local authorities should consider methods that enable people to contribute meaningfully to:
- setting the strategic direction for market shaping and commissioning
- engaging in planning – using methods that support people to identify problems and solutions, rather than relying on ‘downstream’ consultation
- identifying outcomes and setting priorities for specific services
- setting measures of success and monitor on-going service delivery, including through the experience of people who use services and carers
- playing a leading role throughout tendering and procurement processes, from developing specifications to evaluating bids and selecting preferred providers
- contributing to reviews of services and strategies that relate to decommissioning decisions and areas for new investment
- managing any changes to service delivery, recognising that long-term relationships may have developed in the community and with individual people receiving care and support and carers
4.65 Engagement with service providers should emphasise understanding the organisation’s strategies, risks, plans, and encourage building trusting relationships and fostering improvement and innovation to better meet the needs of people in the area. Local authorities should consider engagement with significant suppliers of services to provider organisations, where this would help improve their understanding of markets, for example, engaging with employment and training services that might enable local authorities to gain access to frontline insights on care provision and the local workforce supply and training.
4.66 Local authorities should ensure that active engagement and consultation with local people is built into the development and review of their strategies for market shaping and commissioning, and is demonstrated to support local accountability (for example, via the Local Account).
4.67 Local authorities should engage positively with provider organisations to ensure fair play and necessary confidentiality. The Think Local Act Personal (TLAP) partnership has produced guidance that may assist in the process – Stronger Partnerships for Better Outcomes and Commissioning the future: start a new conversation. Local authorities may also find the IPC ‘Market shaping toolkit (MaST): supporting local authority and SME care provider innovation and collaboration’ useful in supporting positive engagement with providers.
4.68 Local authorities should make available to providers available routes to register concerns or complaints about engagement and commissioning activities. Local authorities should consider the adequacy and effectiveness of these routes and processes as part of their engagement and trust-building activities.
Undertaking market shaping and commissioning
Understanding the market
4.69 Local authorities must understand local markets and develop knowledge of current and future needs for care and support services, and, insofar as they are willing to share and discuss, understand providers’ business models and plans. This is important so that authorities can articulate likely trends in needs and signal to the market the likely future demand for different types of services for their market as a whole, and understand the local business environment, to support effective commissioning. Activities to understand the market should appropriately reflect an authority’s strategic plans for integrating health, social care and related services and will require the cooperation of those other parties, as well as other authorities in the region, to ensure a complete picture.
4.70 Local authorities (through an engagement process, in concert with commissioners for other services where appropriate) should understand and articulate the characteristics of current and future needs for services. This should include reference to underpinning demographics, drivers and trends, the aspirations, priorities and preferences of those who will need care and support, their families and carers, and the changing care and support needs of people as they progress through their lives. This should include an understanding of:
- people with existing care needs drawn from assessment records
- carers with existing care needs drawn from carers’ assessment records
- new care and support needs
- those whose care and support needs will transition from young people’s services to adult services
- those transitioning from working-age adults to services for older people
- people whose care and support needs may fluctuate
- people moving to higher needs and specialised care and support
- those that will no longer need care and support
4.71 It should include information and analysis of low incidence needs and multiple and complex conditions as well as more common conditions such as sensory loss. The RNIB has a tool to help local authorities scope the needs of people with sight impairment. It should also include information about likely changes in requirements for specialist housing required by people with care and support needs. The online tool SHOP@ developed by the Housing Learning and Improvement Network may be helpful.
4.72 Local authorities should have in place robust methods to collect, analyse and extrapolate this information about care and support needs, including as appropriate information about specific conditions (for example, neurological conditions such as Stroke, Parkinson’s, and Motor Neurone Disease), and multiple and complex needs. This should sit alongside information about providers’ intentions to deliver support over an appropriate timescale – likely to be at least 5 years into the future, with alignment to other strategic timeframes. Data collection should include information on the quality of services provided in order to support local authority duties to foster continuous improvement. This could be achieved, for example, by collecting and acting on feedback from people who receive care, their families and carers alongside information on the specific nature of the services people receive (for example, regularity and length of homecare visits). This will allow for an assessment of correlation between customer experience and service provision. Data collection must be sufficient to allow local authorities to meet their duties under the Equality Act 2010.
4.73 Local authorities should include in their engagement and analysis, services and support provided by voluntary, community services, supported housing providers, and other groups that make up ‘community assets’ and plan strategically to encourage, make best use of and grow these essential activities to integrate them with formal care and support services.
4.74 Local authorities should also seek to understand trends and changes to the levels of support that are provided by carers, and seek to develop support to meet their needs, noting that amongst other sources, census data include information on carers and their economic activity. Local authorities should understand the trends and likely changes to the needs of carers in employment, so as to better plan future support.
4.75 In order to understand future trends in needs and demands, local authorities should include an understanding of people who are or are likely to be both wholly or partly state funded, and people who are or are likely to be self-funding. It should also include an analysis of those self-funding people who are likely to move to state funding in the future.
4.76 The understanding of needs should also include an understanding of the likely demand for state-funded services that the local authority will need to commission directly, and state-funded services likely to be provided through direct payments and require individuals to ‘micro-commission’ services. Local authorities should also consider the extent to which people receiving services funded by the state may wish to ‘top up’ their provision to receive extra services or premium services – that is, the assessment of likely demand should be for services that people are likely to need and be prepared to pay for through top ups.
4.77 The assessment of needs should be integrated with the process of developing, refining and articulating a local authority’s Joint Strategic Needs Assessment. Where appropriate, needs should be articulated on an outcomes basis.
4.78 In order to gather the necessary information to shape its market, local authorities should engage with providers (including the local authority itself if it directly provides services) to seek to understand and model current and future levels of service provision supply, the potential for change in supply, and opportunities for change in the types of services provided and innovation possible to deliver better quality services and greater value for money. Local authorities should understand the characteristics of providers’ businesses, their business models, market concentration, investment plans. Information about both supply and expected demand for services should be made available publicly to help facilitate the market and empower communities and citizens when considering care and support. Smaller care providers should be included in engagement. Local authorities may find helpful the guidance Supporting Local Authority and SME Care Provider Innovation and Collaboration that was co-produced by the Department of Health with ADASS and LGA, provider organisations and people with lived experience.
4.79 Assessment of supply and potential demand should include an awareness and understanding of current and future service provision and potential demand from outside the local authority area where this is appropriate, for example in considering services to meet highly specialised and complex needs, care and support may not be available in the local authority area, but only from a small number of specialised providers in the country. Consideration should be given to whether such services might better be commissioned and facilitated regionally.
Facilitating the development of the market
4.80 Local authorities should collaborate with stakeholders and providers to bring together information about needs and demands for care and support with that about future supply, to understand for their whole market the implications for service delivery. This will include understanding and signalling to the market as a whole the need for the market to change to meet expected trends in needs, adapt to enhance diversity, choice, stability and sustainability, and consider geographic challenges for particular areas. To this picture, local authorities should add their own commissioning strategy and future likely resourcing for people receiving state-funding. Local authorities should consider co-ordinating these market shaping and related activities with other neighbouring authorities where this would facilitate better outcomes.
4.81 Local authorities should consider how to support and empower effective purchasing decisions by people who self-fund care or purchase services through direct payments, recognising that this can help deliver a more effective and responsive local market.
4.82 Local authorities should ensure that the market has sufficient signals, intelligence and understanding to react effectively and meet demand, a process often referred to as market structuring or signalling. Local authorities should publish, be transparent and engage with providers and stakeholders about the needs and supply analysis to assist this signalling. It is suggested that this is best achieved through the production and regular updating of a document like a Market Position Statement that clearly provides evidence and analysis and states the local authority’s intent. A Market Position Statement is intended to encourage a continuing dialogue between a local authority, stakeholders and providers where that dialogue results in an enhanced understanding by all parties is an important element of signalling to the market.
4.83 A Market Position Statement should contain information on: the local authority’s direction of travel and policy intent, key information and statistics on needs, demand and trends, (including for specialised services, personalisation, integration, housing, community services, information services and advocacy, and carers’ services), information from consumer research and other sources about people’s needs and wants, information to put the authority’s needs in a national context, an indication of current and future authority resourcing and financial forecasts, a summary of supply and demand, the authority’s ambitions for quality improvements and new types of services and innovations, and details of, or cross-references to the local authority’s own commissioning intentions, strategies and practices [footnote 22].
4.84 Developing and then making publicly available a Market Position Statement is one way a local authority can meet its duties to make available information about the local market, and demonstrates activity to meet the other parts of Section 5 of the Act. The DCMQC web pages include exemplar Market Position Statements and links to examples of good practice. Market Position Statements for care and support services should combine, cross-refer or otherwise complement other similar statements for related services, particularly where there is an integrated approach or ambition, for example, housing. The paper from the Housing Learning and Improvement Network on developing MPS for housing services may be helpful.
4.85 As part of developing and publishing a document like a Market Position Statement, local authorities should engage with stakeholders and partners to structure their markets. This could include:
- discussions with potential providers
- actively promoting best practice and models of care and support
- understanding the business planning cycles of providers
- aligning interactions and supporting the provider’s business planning
- identifying and addressing barriers to market entry for new providers
- facilitating entry to the market through advice and information
- streamlining the authority’s own procurement processes
- promoting diversification of provider organisations
- working with providers on an ‘open-book accounting’ approach [footnote 23] to cost current and future services and ensure provider sustainability
- supporting providers through wider local authority activity – planning, business support and regeneration
4.86 Local authorities may consider that market structuring activity – signalling to the market and providing assistance – is not achieving the strategic aims as quickly or as effectively as needed, and may wish to consider more direct interventions in the market. Market interventions may also be planned as part of the market shaping and commissioning strategies where there is an immediate need for intervention.
4.87 Market interventions could for example include: refocusing local authority business support initiatives onto the care and support sector, exploring how local care and support projects could attract capital investments and support and what guarantees may be needed, encouraging and supporting social enterprises, micro-enterprises, Community Interest Companies, and User-Led Organisations (for example, incentivising innovation by third sector providers, possibly through grant funding), exploring planning barriers and using planning law, offering access to training and development opportunities.
4.88 Local authorities should consider monitoring progress toward the ambitions set out in the Market Position Statement, and making that progress public along with information about its own commissioning decisions, as part of a commitment to transparency and accountability. This would demonstrate that the authority’s commissioning activity is in line with the ambition and direction of travel articulated in its Market Position Statement, and might be achieved by including this information in regular updates to the Market Position Statement.
Case Study Facilitating the market
Warwickshire Council’s Market Position Statement for Older People identified a significant growth in the number of people living with dementia in the county, coupled with a declining trend in the number of people accessing traditional day services in the previous 4 to 5 years. Day services provide stimulation for the person living with dementia as well as a break for the person’s carer.
Following this the Council undertook a full review of Dementia Community Support. This included evaluating the role of services funded by the NHS and the Council and also those provided directly by the voluntary and community sector.
The Council held an engagement event to establish what customers and carers want dementia Community Support services to look like and deliver. This identified the gaps between supply and demand in more detail and at a local level. The event also gathered information from providers and voluntary and community groups about the challenges of delivering services. Providers identified commissioning models which promote strong and stable service delivery whilst still allowing flexible responses to meet individual needs as particularly useful. As a result of this activity, the Council is now in the process of procuring a new service model for Dementia Community Support. The model will include information and advice, community services, building-based respite and specialist support.
Promoting integration with local partners
4.89 The Health and Social Care Act 2012 sets out specific obligations for the health system and its relationship with care and support services. It gives a duty to NHS England, clinical commissioning groups, Monitor and Health and Wellbeing Boards to make it easier for health and social care services to work together to improve outcomes for people. Section 3 of the Care Act places a corresponding duty on local authorities to carry out their care and support functions with the aim of integrating services with those provided by the NHS or other health-related services, such as housing.
4.90 Local authorities should also consider working with appropriate partners to develop integration with services related to care and support such as housing, employment services, transport, benefits and leisure services. Local authorities should prioritise integration activity in areas where there is evidence that effective integration of services materially improves people’s wellbeing, for example, end of life care, and should take account of the key national and local priorities and objectives of the Better Care Fund, for example, stopping people reaching crisis and reducing the emergency admissions to hospitals.
4.91 Integrated services built around an individual’s needs are often best delivered through the home. The suitability of living accommodation is a core component of an individual’s wellbeing and when developing integrated services, local authorities should consider the central role of housing within integration, with associated formal arrangements with housing and other partner organisations.
4.92 Local authorities should work towards providing integrated care and support, providing services that work together to provide better outcomes for individuals who need care and support and enhancing their wellbeing, noting that this will require the sharing of information about current and future needs and likely service provider’s responses to underpin a holistic approach to developing integrated care and support pathways. Further information can be found in the chapters of this statutory guidance on integration (chapters 15 to 18). NHS guidance and LGA case studies on integration may be helpful, together with the toolkit for integration developed by North West London Whole System Integrated Care (particularly chapter 7 on budget pooling, governance arrangements and commissioning issues in general).
4.93 Local authorities should consider with partners, the enabling activities, functions and processes that may facilitate effective integrated services. For example Bexley LA and CCG joint commissioning of preventative services. These will include consideration of: joint commissioning strategies, joint funding, pooled budgets, lead commissioning, collaborative commissioning, working with potential service providers to consider innovative ways of arranging and delivering services, and making connections to public health improvement.
Securing supply in the market and assuring its quality and value for money through contracting
4.94 Local authorities should consider best practice on commissioning services, for example the NAO guidance to ensure they deliver quality services with value for money. ‘Value for money’ means optimal use of resources to achieve intended outcomes, and must reference the quality of service delivered and the outcomes achieved for people’s wellbeing, and should not be solely based on achieving the lowest cost. Achieving value for money may mean arranging service provision collaboratively with other authorities, in order to secure viable, quality services that meet the demands identified, for example, low-volume services.
4.95 Commissioning and procurement practices must deliver services that meet the requirements of the Care Act and all related statutory guidance. Re-commissioning and replacing services represents a particular challenge and should be carried out so as to maintain quality and service delivery that supports the wellbeing of people who need care and support and carers, and guards against the risk of a discontinuity of care and support for those receiving services. For example, multiple contracts terminating around the same time may destabilise local markets if established providers lose significant business rapidly and staff do not transfer smoothly to new providers.
4.96 De-commissioning services where there is to be no replacement service should similarly be carried out so as to maintain the wellbeing of people who need care and support, and carers, and ensures that their eligible needs continue to be met.
4.97 Local authorities should consider the contract arrangements they make with providers to deliver services, including the range of block contracts, framework agreements, spot contracting or ‘any qualified provider’ approaches, to ensure that the approaches chosen do not have negative impacts on the sustainability, sufficiency, quality, diversity and value for money of the market as a whole – the pool of providers able to deliver services of appropriate quality.
4.98 A local authority’s own commissioning should be delivered through a professional and effective procurement, tendering and contract management, monitoring, evaluation and decommissioning process that must be focussed on providing appropriate high quality services to individuals to support their wellbeing and supporting the strategies for market shaping and commissioning, including all the themes set out in this guidance.
4.99 Local authorities should ensure that they understand relevant procurement legislation, and that their procurement arrangements are consistent with such legislation and best practice. Local authorities should be aware that there is significant flexibility in procurement practices to support effective engagement with provider organisations and support innovation in service delivery, potentially reducing risks and leading to cost-savings. The Office of Fair Trading produced guidance to help public purchasers understand the flexibilities so as to support service transformations through better commissioning. The Market Shaping Toolkit, produced by the Institute of Public Care includes a section summarising recent changes to procurement rules, including EU procurement rules and the implications for commissioners. Government has also produced guidance on when reserved contracts may be allowable for organisations employing a significant number of disabled people these documents may be helpful to commissioners.
4.100 Local authorities should ensure that their procurement and contract management and monitoring systems provide direct and effective links to care service managers and social workers to ensure the outcomes of service delivery matches individual’s care and support needs and that where the local authority arranges services, people are given a reasonable choice of provider. Contract management should take account of feedback from people receiving care and support.
4.101 Local authorities should ensure that where they arrange services, the assessed needs of a person with eligible care and support needs is translated into effective, appropriate commissioned services that are adequately resourced and meet the wellbeing principle of the Act. For example, short home-care visits of 15 minutes or less are not appropriate for people who need support with intimate care needs, though such visits may be appropriate for checking someone has returned home safely from visiting a day centre, or whether medication has been taken (but not the administration of medicine) or where they are requested as a matter of personal choice.
4.102 When commissioning services, local authorities should pay particular attention to ensuring that providers have clear arrangements in place to prevent abuse or neglect. This should include assuring themselves, through their contracting arrangements, that a provider is capable and competent in responding to allegations of abuse or neglect, including having robust processes in place to investigate the actions of members of staff. Local authorities should be clear what information they expect from providers (for example, where there are allegations of abuse, what action the provider is taking or has taken and what the outcome is) and where providers are expected to call upon local authorities to lead a Section 42 enquiry (where the management of the provider is implicated for instance), or to involve the CCG (for health matters) or police (for example, in the case of potential crimes). There should be clear agreement about how local partners work together on investigations and what their respective roles and responsibilities are.
4.103 When commissioning services, local authorities should undertake due diligence about the financial sustainability and effectiveness of potential providers to deliver services to agreed criteria for quality, and should assure themselves that any recent breaches of regulatory standards or relevant legislation by a potential provider have been corrected before considering them during tendering processes. For example, where a provider has previously been in breach of national minimum wage legislation, a local authority should consider every legal means of excluding them from the tendering process unless they have evidence that the provider’s policies and practice have changed to ensure permanent compliance.
4.104 Contracts should incentivise value for money, sustainability, innovation and continuous improvement in quality and actively reward improvement and added social value. Contracts and contract management should manage and eliminate poor performance and quality by providers and recognise and reward excellence.
4.105 Local authorities are under a duty to consider added social value when letting contracts through the Public Services (Social Value) Act 2012 and are required to consider how the services they procure, above relevant financial thresholds, might improve the economic, social and environmental wellbeing of the area. Local authorities should consider using this duty to promote added value in care and support both when letting contracts to deliver care and support, and for wider goods and services. This should include considering whether integrated services, voluntary and community services and ‘community capital’ could be enhanced, recognising that these community assets provide the bedrock of care and support that commissioned and bought services supplement. Local authorities should consider the range of funding mechanisms that are available to support market interventions to support community based organisations such as seed funding and grants.
4.106 All services delivered should adhere to national quality standards, with procedures in place to assure quality, safeguarding, consider complaints and commendations, and continuing value for money, referencing the CQC standards for quality and CQC quality ratings.
4.107 Local authorities may consider delegating some forms of contracting to brokers and people who use care and support to support personal choice for people who are not funded by the local authority and those taking direct payments, with appropriate systems in place to underpin the delivery of safe, effective appropriate high quality services through such routes. Where functions and activities are delegated, local authorities should ensure that appropriate elements of this statutory guidance are included in contractual conditions, for example, allowing engagement in developing Market Position Statements. Local authorities should also consider providing support to people who wish to use direct payments to help them make effective decisions through, for example, Direct Payment support organisations.
4.108 Local authority procurement and contract management activities should seek to minimise burdens on provider organisations and reduce duplications, where appropriate, using and sharing information, with for example the CQC.
4.109 Recognising that procurement is taking place against a backdrop of significant demand on commissioners to achieve improved value for money and make efficiencies, local authorities should consider emerging practice on achieving efficiencies without undermining the quality of care.
Further information/best practice
4.110 The different approaches provided in footnotes in this guidance are meant as illustrative examples rather than recommendations or endorsements.
4.111 The Department of Health funded a programme during 2013 to 2014 to support local authorities prepare for market shaping duties; further information is available on the Developing Care Markets for Quality and Choice programme website. The Department also funded a project to develop commissioning standards, Commissioning for Better Outcomes, which are designed to support local authorities, through peer challenge and self-assessment to move towards commissioning practices which underpins the themes of this statutory guidance.
4.112 The Developing Care Markets programme, Commissioning for Better Outcomes, and the market shaping toolkit develop the themes presented in this statutory guidance and will themselves point to examples of best practice and support tools that demonstrate how these themes have been introduced and delivered effectively.
5. Managing provider failure and other service interruptions
This chapter provides guidance on:
- Sections 19 and 48 to 57 of the Care Act 2014
- The Care and Support (Business Failure) Regulations 2015
This chapter covers:
- service interruptions because of business failure, this chapter explains what local authorities must do if a provider is unable to carry on because of business failure
- business failure involving a provider in the Care Quality Commission’s (CQC) market oversight regime. This section explains CQC’s role if business failure occurs and the link with the local authority’s temporary duty
- business failure involving a provider not in the CQC market oversight regime. This section explains what local authorities must do if the business failure involves a provider not in the CQC regime
- administration and other insolvency procedures. This section explains the relationship between local authorities and persons such as an Administrator appointed in insolvency proceedings
- service interruptions other than business failure. This section explains local authorities’ powers where a service is interrupted for other reasons
- the link with local authorities’ duties in respect of market shaping. This section explains how local authorities’ market shaping activities can play a part in effectively addressing service interruptions
- the need for contingency planning. This section explains how local authorities should consider having contingency plans in advance to address the service interruptions that pose the greatest risk locally
5.1 The possibility of interruptions to care and support services causes uncertainty and anxiety for people receiving services, their carers, family and friends. This guidance explains how the Care Act makes provision to ensure that, in such circumstances, the care and support needs of those receiving the service continue to be met. It describes local authorities’ powers and duties when services are at risk of interruption in general and, in particular, when the interruption is because a provider’s business has failed. It provides guidance to local authorities on the exercise of those powers and the discharge of those duties.
5.2 Interruptions can arise from a number of different causes. An example is when a provider of services faces commercial difficulties that put the continuation of their business under threat. In 2011, Southern Cross Healthcare, then the biggest provider of residential care services in the United Kingdom, ran into financial difficulties and it was possible the business would have to close down, putting services to residents at risk. While Southern Cross was a provider of services in all parts of the country, smaller local providers can also encounter commercial issues which cause uncertainty for people receiving care and support. Local authorities have an important role in situations where a provider is unable to continue to supply services because of business failure.
5.3 There are numerous other situations that can cause disruption to care and support services. Some may impact on the whole business – for example, a provider decides to close the business down – while others impact on a particular service – for example, a meningitis outbreak at a care home. Local authorities should use their powers to act in such cases, as set out below.
Definitions
5.4 ‘Business failure’ is defined in The Care and Support (Business Failure) Regulations 2015 (PDF, 45KB). These Regulations define what is meant by ‘business failure’ and explain the circumstances in which a person is to be treated as being unable to do something because of business failure. Business failure is defined by a list of different events such as the appointment of an administrator, the appointment of a receiver or an administrative receiver (the full list appears in the Regulations). Service interruption because of ‘business failure’ relates to the whole of the regulated activity and not to parts of it.
5.5 ‘Temporary duty’ or ‘duty’ means the duty on local authorities to meet needs in the case of business failure. ‘Temporary’ means the duty continues for as long as the local authority considers it necessary. The temporary duty applies regardless of whether a person is ordinarily resident in the authority’s area. The duty applies from the moment the authority becomes aware of the business failure. The actions to be taken by authorities will depend on the circumstances, and may include the provision of information. The duty is to meet needs but authorities have discretion as to how they meet those needs.
Service interruptions because of business failure
5.6 Business failure of a major provider is a rare and extreme event and does not automatically equate to closure of a service. It may have no impact on residents or the people who use the services. However, if a provider of any size is unable to continue because of business failure, the duties on local authorities are as follows.
5.7 Local authorities are under a temporary duty to meet people’s needs when a provider is unable to continue to carry on the relevant activity in question because of business failure. The duty applies when a service can no longer be provided and the reason for that is that the provider’s business has failed. If the provider’s business has failed but the service continues to be provided then the duty is not triggered. This often may happen in insolvency situations where an administrator is appointed and continues to run the service.
5.8 The duty applies where a failed provider was meeting needs in the authority’s area. It does not matter whether or not the authority has contracts with that provider, nor does it matter if all the people affected are self-funders (for example, arranging and paying for their own care). The duty is in respect of people receiving care by that provider in that authority’s area – it does not matter which local authority (if any) made the arrangements to provide services.
5.9 The needs that must be met are those that were being met by the provider immediately before the provider became unable to carry on the activity. Local authorities must ensure the needs are met but how that is done is for the local authority to decide, and there is significant flexibility in determining how to do so, as set out in section 8 of the Care Act. It is not necessary to meet those needs through exactly the same combination of services that were previously supplied. However, when deciding how needs will be met, local authorities must involve the person concerned, any carer that the person has, or anyone whom the person asks the authority to involve (see chapter 10 on care and support planning). Where the person lacks capacity to ask the authority to do that, the local authority must involve anyone who appears to the authority to be interested in the person’s welfare. Where a carer’s service is involved, local authorities must involve the carer and anyone the carer asks the authority to involve. The authority must take all reasonable steps to agree how needs should be met with the person concerned. It should seek to minimise disruption for people receiving care, in line with the wellbeing principle and, although authorities have discretion about how to meet needs, the aim should be to provide a service as similar as possible to the previous one.
5.10 An authority has the power, where it considers this necessary to discharge the temporary duty, to request that the provider, or anyone involved in the provider’s business as it thinks appropriate, to supply it with information that it needs. This may involve, for example, up-to-date records of the people who are receiving services from that provider, to help the local authority to identify those who may require its support.
5.11 The authority should act promptly to meet people’s needs. The lack of a needs or carer’s assessment or a financial assessment for a person must not be a barrier to action. Neither is it necessary to complete those assessments before or whilst taking action. Similarly, authorities must meet needs irrespective of whether those needs would meet the eligibility criteria. All people receiving services in the local authority’s area are to be treated the same. In particular, how someone pays for the costs of meeting their needs – for example, in full by the person themselves – must have no influence on whether the authority fulfils the duty. However, an authority may charge the person for the costs of meeting their needs, and it may also charge another local authority which was previously meeting those needs, if it temporarily meets the needs of a person who is not ordinarily resident in its area. The charge must cover only the actual cost incurred by the authority in meeting the needs. No charge must be made for the provision of information and advice to the person.
5.12 The Care Act imposes certain restrictions on the provision of health services by local authorities and these apply to meeting needs in provider failure cases (section 52(7)). A local authority may not meet needs in provider failure cases by, for example, providing NHS Continuing Healthcare (NHS CHC). Where the failed provider’s clientele consists of persons in receipt of NHS CHC, unless their needs appear to have changed, it would be reasonable for the local authority to conclude that it was not necessary to do anything to meet those needs. This is because the duty to provide NHS CHC falls on the NHS and local authorities cannot provide it. The duties of the NHS in such situations are covered elsewhere and as such are beyond the scope of this guidance. Authorities should refer to the Standing Rules (the National Health Service Commissioning Board and Clinical Commissioning Groups (Responsibilities and Standing Rules) Regulations 2012, as amended); and to the national framework for NHS Continuing Healthcare and NHS-funded nursing care and the NHS-Funded Nursing Care Best Practice Guidance for further guidance.
5.13 In fulfilling this function, authorities must follow the general duties to cooperate (see chapter 15). Where a person is not ordinarily resident in an authority’s area, that authority must cooperate with the authority which was arranging for the needs to be met previously (for example, before the provider became unable to carry on because of business failure). The duty of cooperation applies equally where the needs being met previously were paid for (in full or in part) by another authority through a direct payment to the person concerned.
5.14 Authorities that disagree on whether and/or how the law (for example, section 48) applies in these circumstances may apply to the Secretary of State for a determination of a dispute under the procedure that applies to disputes over ordinary residence or continuity of care (see chapters 19 and 20).
5.15 All of the duties on local authorities described above apply equally if the needs the authority must meet were, at the time the provider became unable to carry on because of business failure, being met under arrangements made by local authorities in Wales, Scotland or Northern Ireland under the legislation that applies in those countries. English local authorities may recover from their counterparts in Wales, Scotland and Northern Ireland the costs incurred in meeting the person’s needs. If applicable, English authorities can also recover costs from the person themselves (other than the costs of needs being met or funded by the authorities mentioned above).
5.16 Disputes between authorities in England, Wales, Scotland or Northern Ireland about whether or how the temporary duty applies in cross-border situations are to be resolved under the legislation governing disputes about cross-border placements in Schedule 1 and the relevant regulations (see chapter 22).
Business failure involving a provider in the CQC oversight regime
5.17 In April 2015, the financial ‘health’ of certain care and support providers became subject to monitoring by the Care Quality Commission (CQC). The Care and Support (Market Oversight Criteria) Regulations 2015 set out the entry criteria for a provider to fall within the regime. These are intended to be providers which, because of their size, geographic concentration or other factors, would be difficult for one or more local authorities to replace, and therefore where national oversight is required. CQC will determine which providers satisfy the criteria using data available to it. It will notify the providers which meet the entry criteria.
5.18 CQC must then assess the financial sustainability of the provider’s business. If it assesses there is a significant risk to the financial sustainability of the provider’s business, there are certain actions CQC may take with that provider (none of which involve local authorities).
5.19 Where CQC is satisfied that a provider in the regime is likely to become unable to continue with their activity because of business failure, it is required to tell the local authorities which it thinks will be required to carry out the temporary duty, so that they can prepare for the local consequences of the business failure. CQC will inform local authorities once it is satisfied the provider is unlikely to be able to carry on because of business failure. CQC’s trigger to contact authorities is that it believes the whole of the regulated activity in respect of which the provider is registered is likely to fail, not parts of it. It is not required to make contact with authorities if, say, a single home owned by the provider in the regime is likely to fail because it is unprofitable and the CQC is not satisfied that this will lead to the whole of the provider’s relevant regulated activity becoming unable to continue. In these circumstances, it is the provider’s responsibility to wind down and close the service in line with its contractual obligations and it is expected that providers would do so in a planned way that does not interrupt people’s care.
5.20 Where CQC considers it necessary to do so to help a local authority to carry out the temporary duty, it may request the provider to provide it with information and CQC must then give the information, and any further relevant information it holds, to the local authorities affected. If the CQC is of the view that a provider is likely to become unable to continue with its activity because of business failure, the CQC should work closely together with the affected local authorities to help them fulfil their temporary duty. In exercising its market oversight functions, CQC must have regard to the need to minimise the burdens it imposes on others.
Business failure involving a provider not in the CQC oversight regime
5.21 Regulations set out the entry criteria into the CQC regime. It will be for CQC to apply those regulations and decide which providers are included. There are many thousands of providers in England and only a relatively small number of providers fall in the regime. The providers outside the regime will in the main be those with small and medium size businesses.
5.22 The temporary duty on local authorities to meet needs in the case of business failure applies regardless of whether the provider is in the market oversight regime. Despite the CQC having a market oversight responsibility, local authorities have responsibility to ensure continuity of care in respect of business failure of all registered providers.
Administration and other insolvency procedures
5.23 Business failure (as defined) will usually involve an official being appointed for example, an Administrator to oversee the insolvency proceedings. An Administrator represents the interests of the creditors of the provider that has failed and will typically try to rescue the company as a going concern. In these circumstances, the service will usually continue to be provided, and the exercise of local authorities’ temporary duties may not be called for. It is not for local authorities to become involved in the commercial aspects of the insolvency, but they should cooperate with the Administrator if requested. Local authorities should, insofar as it does not adversely affect people’s safety and wellbeing, support efforts to maintain service provision by, for example, not prematurely withdrawing people from the service that is affected, or ceasing to commission that service.
Service interruptions other than business failure
5.25 Sections 18 and 20 of the Care Act set out when a local authority must meet a person’s eligible needs. They place duties on the local authority. If the circumstances described in the sections apply and the needs are eligible, the local authority must meet the needs in question. These duties apply whether or not business failure is at issue.
5.26 Section 19 of the Care Act covers the circumstances where care and support needs may be met for example, circumstances where no duties arise under section 18 but the local authority may nevertheless meet an adult’s needs. In particular, section 19(3) permits a local authority to meet needs which appear to it to be urgent. In this context, ‘urgent’ takes its everyday meaning, subject to interpretation by the courts, and may be related to, for example, time, severity. This is likely to be the case in many situations where services are interrupted but business failure is not the cause. The power in section 19(3) can be exercised in order to meet urgent needs without having first conducted a needs assessment, financial assessment or eligibility criteria determination. The local authority may meet urgent needs regardless of whether the adult is ordinary resident in its area. This means the local authority can act quickly if circumstances warrant. The power to meet urgent needs is not limited by reference to services delivered by particular providers and is thus available where urgent needs arise as a result of service failure of an unregistered provider (for example, a provider of an unregulated social care activity). The power may also be used in the context of quality failings of providers if that is causing people to have urgent needs.
5.27 This section gives local authorities a power to act to meet needs, but it does not require that authorities must act. Whether or not to act is a decision for the authority itself but authorities should consider the examples which follow.
5.28 In relation to service interruption, circumstances that might lead to the exercise of the power include where the continued provision of care and support to those receiving services is in imminent jeopardy and there is no likelihood of returning to a ‘business as usual’ situation in the immediate future, leading to urgent needs. Not all situations where a service has been interrupted or closed will merit local authority involvement because not all cases will result in adults having urgent needs. For example, if a care home closes and residents have agreed to the provider’s plans to move the residents to a nearby care home that the provider also owns, local authorities will not necessarily have to become actively involved as urgent needs might not arise. On the other hand, the local authority might wish to be satisfied that the alternative home can adequately meet the urgent needs. Whether to act under this power is a judgement for the local authority to make in the first instance.
5.29 If a provider has not failed, it is primarily the provider’s responsibility to meet the needs of individuals receiving care in accordance with its contractual liabilities. The local authority may wish to be involved to help with this. The power provides an ultimate backstop for use where the provider cannot or will not meet its responsibilities, and where the authority judges that the needs of individuals are urgent (and where the local authority is not already under a duty to meet the adult’s needs, for example under section 18).
5.30 A service closure may be temporary (for example, unforeseen absence of qualified staff) or permanent (for example, the home is to be sold on for use as a hotel). Similarly, an emergency closure or planned closure may be involved. What matters in deciding whether to meet needs is whether the needs of the people affected appear to be urgent. For example, the sale of a provider’s business may be a positive development for residents, service users and commissioners alike and may not lead to urgent needs. These powers are not intended to inhibit the effective operation of a market in improving choice, quality and investment.
5.31 Where the local authority does get involved in ensuring needs continue to be met, that involvement might be short-lived (for example, the giving of advice) or enduring over some months (for example, overseeing the movement of residents following the closure of several homes owned by the same provider). Acts of God (for example, flooding) or complications with suppliers (for example, a nursing agency refuses to continue to provide qualified staff) should not in themselves automatically be considered to trigger the use of the power. In all cases, the test is whether the local authority considers there is an urgent need to be met.
5.32 When considering action in relation to service interruption or closure, there is a balance to be struck. On the one hand, if local authorities know there is a serious risk to the continued provision of a service, they may consider not using that service temporarily or reassigning people using that service to an alternative service. On the other hand, it may be possible and justifiable for the local authority to act in a way that maximises the provider’s chances of continuing to provide the service and avoiding a business failure. Local authorities should weigh the consequences of their actions before deciding how to respond, in particular, how their actions might impact on the likelihood of the service continuing. Certain actions may increase the risk of precipitating the business failure.
5.33 In summary, each service interruption should be considered on its facts and assessed by the local authority through a process of risk assessment. It is for the local authority to decide if it will act to meet a person’s needs for care and support which appear to it to be urgent. In exercising this judgement the local authority must act lawfully, including taking decisions that are reasonable.
The link with local authorities’ duties in respect of market shaping
5.34 Section 5 and the associated guidance sets out authorities’ duties to promote the efficient and effective operation of the local market in care and support services (see chapter 4). Central to this function is the need to ensure that the authority has, and makes available, information about the providers of care and support services in its area and the types of services they provide. This gathering of market intelligence is equally relevant to authorities’ responses to business failure and other service interruptions. Where alternative services are to be put in place, an effective response requires a thorough knowledge of the market, which providers provide which services, the quality of each provider’s services and where there is spare capacity in service provision. In anticipating potential service interruptions, there is also a need to know the vulnerabilities in the operation of the market. For example, is there only one local provider of a particular service and no alternatives exist locally, or does one provider cater for a substantial part of the local market and alternative capacity could not be found easily? Service interruptions involving such providers are likely to be more difficult to address. Local authorities should have knowledge of market vulnerabilities, market capacity and capabilities such as this in order to respond effectively to service interruptions.
5.35 Local authorities should understand how providers in their area are coping with the current trading conditions through discussions with the providers themselves. Authorities can achieve this without the collection of detailed financial metrics, accounts and business plans that CQC might utilise in respect of the major corporate providers in the regime. The business failure of providers outside the CQC regime will be on a smaller scale, usually with lesser impact, and local authorities should take a proportionate approach to anticipating or getting early warning of business failure. Local authorities may find the Cordis Bright guidance and toolkit: Assessing care market and provider sustainability helpful in developing a proportionate approach. Given CQC is responsible for monitoring the financial sustainability of providers falling within the market oversight scheme, it is not necessary for authorities also to ask for detailed financial information from these providers.
The need for contingency planning
5.36 Most service interruptions are on a small scale and are easily managed but service interruptions on a large scale pose far greater problems. If a provider which operates nationwide fails, few local authorities are likely to be able to respond effectively on their own. Local authorities should consider how they would respond to different service interruptions and, where the involvement of neighbouring authorities would be essential in order to maintain services, ensure effective liaison and information sharing arrangements are set up in advance. Close cooperation between authorities may be particularly required where an authority has a substantial number of people placed within its area by other authorities.
5.37 As part of contingency planning, authorities should discuss with local providers which services they would be willing and able to provide if the need arose because another local provider had failed. This should help to facilitate a prompt response that would help to maintain continuity of care for the people affected. Through its market shaping activities, authorities should encourage trust between the parties so that effective relationships exist where urgent needs are to be met.
5.38 Service interruptions are often the cause of much anxiety and media attention. Local authorities should have the capacity to react quickly to any media reporting of service interruptions, whether large scale or small, if uncertainty and anxiety are to be minimised.
5.39 Local authorities should consider how to undertake contingency planning most effectively at a local level, to ensure preparedness for possible service interruptions in the future. Service interruptions are often unforeseen and require rapid response. Local authorities should review which service interruptions pose the greatest risk in their locality and consider developing contingency plans in advance, in conjunction with local partners. This may include regional activity with other local authorities in the same area, where risks are better shared between a number of neighbouring authorities.
5.40 Local authorities already plan and manage challenging situations as a matter of course, for example, school closures from public health outbreaks or the impact of extreme weather. The aim should be that contingency planning for social care sits alongside authorities’ other emergency planning activities.
5.41 Local authorities may find it useful to consider the Local Government Information Unit guide, Care and continuity: contingency planning for provider failure.
First contact and identifying needs
This section includes the following chapters:
6. Assessment and eligibility
This chapter provides guidance on:
- Sections 9 to 13 of the Care Act 2014
- the Care and Support (Assessment) Regulations 2014
- the Care and Support (Eligibility Criteria) Regulations 2015
This chapter covers:
- the purpose of needs and carers’ assessments; refusal of assessment; first contact and relevant safeguarding, advocacy and capacity duties; supporting the person’s involvement in the assessment; taking a preventative approach and looking at a person’s strengths
- the importance of appropriate and proportionate assessment, including supporting the person through the process, enabling supported self-assessment, combining assessments and referring to NHS Continuing Healthcare where appropriate
- taking into account the wider picture by considering fluctuating needs and the impact on the whole family
- the importance of having assessors appropriately trained and with the experience and knowledge necessary to carry out the assessment, including specialist assessments for those who are deafblind
- carrying out integrated assessment where a person has other needs, for example where the person also has health as well as care and support needs; keeping records and delegating assessments
- the eligibility framework to ensure that there is clarity and consistency around local authority determinations on eligibility
Assessment
6.1 The assessment and eligibility process is one of the most important elements of the care and support system. The assessment is one of the key interactions between a local authority and an individual, whether an adult needing care or a carer. The process must be person-centred throughout, involving the person and supporting them to have choice and control.
6.2 The assessment process starts from when local authorities begin to collect information about the person, and will be an integral part of the person’s journey through the care and support system as their needs change. It should not just be seen as a gateway to care and support, but should be a critical intervention in its own right, which can help people to understand their situation and the needs they have, to reduce or delay the onset of greater needs, and to access support when they require it. It can also help people to understand their strengths and capabilities, and the support available to them in the community and through other networks and services.
6.3 An ‘assessment’ must always be appropriate and proportionate. It may come in different formats and can be carried out in various ways, including but not limited to:
- a face-to-face assessment between the person and an assessor, whose professional role and qualifications may vary depending on the circumstances, but who must always be appropriately trained and have the right skills and knowledge
- a supported self-assessment, which should use similar assessment materials as used in other forms of needs or carers’ assessments, but where the person completes the assessment themselves and the local authority assures itself that it is an accurate reflection of the person’s needs (for example, by consulting with other relevant professionals and people who know the person with their consent)
- an online or phone assessment, which can be a proportionate way of carrying out assessments (for example where the person’s needs are less complex or where the person is already known to the local authority and it is carrying out an assessment following a change in their needs or circumstances)
- a joint assessment, where relevant agencies work together to avoid the person undergoing multiple assessments (including assessments in a prison, where local authorities may need to put particular emphasis on cross-agency cooperation and sharing of expertise)
- a combined assessment, where an adult’s assessment is combined with a carer’s assessment and/or an assessment relating to a child so that interrelated needs are properly captured and the process is as efficient as possible
6.4 People may approach a local authority for an assessment, or be referred by a third party, for a number of reasons. The ‘assessment’ which they receive must follow the core statutory obligations, but the process is flexible and can be adapted to best fit with the person’s needs, wishes and goals. The nature of the assessment will not always be the same for all people, and depending on the circumstances, it could range from an initial contact or triage process which helps a person with lower needs to access support in their local community, to a more intensive, ongoing process which requires the input of a number of professionals over a longer period of time.
6.5 The aim of the assessment is to identify what needs the person may have and what outcomes they are looking to achieve to maintain or improve their wellbeing. The outcome of the assessment is to provide a full picture of the individual’s needs so that a local authority can provide an appropriate response at the right time to meet the level of the person’s needs. This might range from offering guidance and information to arranging for services to meet those needs. The assessment may be the only contact the local authority has with the individual at that point in time, so it is critical that the most is made of this opportunity.
6.6 The assessment and eligibility process provides a framework to identify any level of need for care and support so that local authorities can consider how to provide a proportionate response at the right time, based on the individual’s needs. Prevention and early intervention are placed at the heart of the care and support system, and even if a person has needs that are not eligible at that time, the local authority must consider providing information and advice or other preventative services. Local authorities must also consider the person’s own strengths or if any other support might be available in the community to meet those needs. The assessment and eligibility framework provides for ongoing engagement with the person so where they have eligible needs they are involved in the arrangements put in place to deliver the outcomes they want to achieve.
6.7 To provide a comprehensive assessment, the assessor must be appropriately trained. Registered social workers and occupational therapists can provide important support and may be involved in complex assessments which indicate a wide range of needs, risks and strengths that may require a coordinated response from a variety of statutory and community services. Or they may be involved at the point of first contact to advise on whether preventative services would be more appropriate at that time.
6.8 Some of the duties and powers detailed in this chapter apply to children and young carers in transition as well as to adults (for more information on transition, (see chapter 16 on Transition to adult care and support).
The purpose of an assessment
6.9 The purpose of an assessment is to identify the person’s needs and how these impact on their wellbeing, and the outcomes that the person wishes to achieve in their day-to-day life. The assessment will support the determination of whether needs are eligible for care and support from the local authority, and understanding how the provision of care and support may assist the adult in achieving their desired outcomes. An assessment must be person-centred, involving the individual and any carer that the adult has, or any other person they might want involved. An adult with care needs could for example ask for their GP or a district nurse to be contacted to provide information relevant to their needs.
6.10 An assessment must seek to establish the total extent of needs before the local authority considers the person’s eligibility for care and support and what types of care and support can help to meet those needs. This must include looking at the impact of the adult’s needs on their wellbeing and whether meeting these needs will help the adult achieve their desired outcomes. The assessment process also provides the opportunity for local authorities to take a holistic view of the person’s needs in the context of their wider support network. Local authorities must consider how the adult, their support network and the wider community can contribute towards meeting the outcomes the person wants to achieve.
6.11 An individual may be unable to request an assessment or may struggle to express their needs. The local authority must in these situations carry out supported decision making, helping the person to be as involved as possible in the assessment, and must carry out a capacity assessment. The requirements of the Mental Capacity Act and access to an Independent Mental Capacity Advocate apply for all those who may lack capacity.
6.12 Eligibility determinations must be made on the basis of an assessment, and cannot be made without having first carried out an assessment. Once an eligibility determination has been made, and the local authority has determined whether it will meet the person’s needs (whether eligible or not), it must then carry out a financial assessment if it wishes to charge the adult and confirm that the adult is ordinarily resident in the authority. The eligibility determination cannot take place until an assessment has been completed, except in cases where the local authority is meeting urgent needs. The financial assessment may in practice run parallel to the needs assessment, but it must never influence an assessment of needs. Local authorities must inform individuals that a financial assessment will determine whether or not they pay towards their care and support, but this must have no bearing on the assessment process itself.
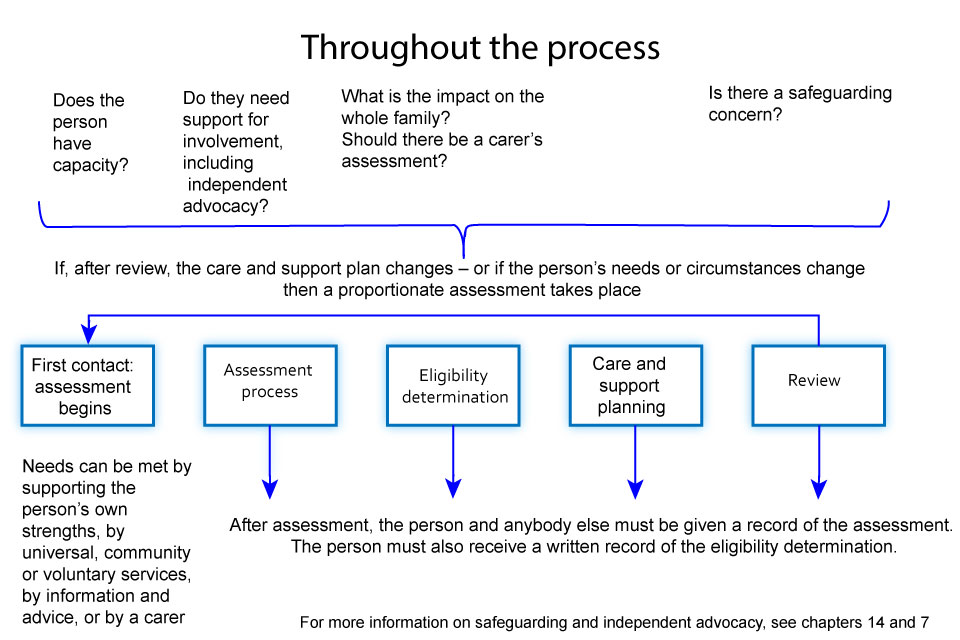
Needs assessment
6.13 Local authorities must undertake an assessment for any adult with an appearance of need for care and support, regardless of whether or not the local authority thinks the individual has eligible needs or of their financial situation.
6.14 Wherever an individual expresses a need, or any challenges and difficulties they face because of their condition(s), the local authority should ensure that it has established the impact of that on the individual’s day-to-day life. The local authority must also consider whether the individual’s needs impact upon their wellbeing beyond the ways identified by the individual. For example where an adult expresses a need regarding their physical condition and mobility, the local authority must establish the impact of this on the adult’s desired outcomes; and must also consider whether their need(s) have further consequences on their wider wellbeing such as on their personal health or the suitability of their living accommodation.
6.15 During the assessment, local authorities must consider all of the adult’s care and support needs, regardless of any support being provided by a carer. Where the adult has a carer, information on the care that they are providing can be captured during assessment, but it must not influence the eligibility determination. After the eligibility determination has been reached, if the needs are eligible or the local authority otherwise intends to meet them, the care which a carer is providing can be taken into account during the care and support planning stage. The local authority is not required to meet any needs which are being met by a carer who is willing and able to do so, but it should record where that is the case. This ensures that the entirety of the adult’s needs are identified and the local authority can respond appropriately if the carer feels unable or unwilling to carry out some or all of the caring they were previously providing.
Carer’s assessment
6.16 Where an individual provides or intends to provide care for another adult and it appears that the carer may have any level of needs for support, local authorities must carry out a carer’s assessment. Where an adult provides care under contract (for example, for employment) or as part of voluntary work, they should not normally be regarded as a carer, and so the local authority would not be required to carry out the assessment.
6.17 There may be circumstances where the adult providing care, either under contract or through voluntary work, is also providing care for the same adult outside of those arrangements. In such a circumstance, the local authority must consider whether to carry out a carer’s assessment for that part of the care they are not providing on a contractual or voluntary basis. There may also be cases where the person providing care does so as voluntary work or under contract, but the nature of their relationship with the person cared for is such that they ought to be considered as a carer within the scope of the Act. The local authority has the power to carry out an assessment in such cases, if it judges that there is reason to do so.
6.18 Carers’ assessments must seek to establish not only the carer’s needs for support, but also the sustainability of the caring role itself, which includes both the practical and emotional support the carer provides to the adult. Therefore, where the local authority is carrying out a carer’s assessment, it must include in its assessment a consideration of the carer’s potential future needs for support. Factored into this must be a consideration of whether the carer is, and will continue to be, able and willing to care for the adult needing care. Some carers may need support in recognising issues around sustainability, and in recognising their own needs. This will allow local authorities to make a realistic evaluation of the carer’s present and future needs for support and whether the caring relationship is sustainable. Where appropriate these views should be sought in a separate conversation independent from the adult’s needs assessment.
6.19 The carer’s assessment must also consider the outcomes that the carer wants to achieve in their daily life, their activities beyond their caring responsibilities, and the impact of caring upon those activities. This includes considering the impact of caring responsibilities on a carer’s desire and ability to work and to partake in education, training or recreational activities, such as having time to themselves. This impact should be considered in both a short-term immediate sense but also the impact of caring responsibilities over a longer term, cumulative sense.
Refusal of assessment
6.20 An adult with possible care and support needs or a carer may choose to refuse to have an assessment. The person may choose not to have an assessment because they do not feel that they need care or they may not want local authority support. In such circumstances local authorities are not required to carry out an assessment. However, where the local authority identifies that an adult lacks mental capacity and that carrying out a needs assessment would be in the adult’s best interests, the local authority is required to do so. The same applies where the local authorities identifies that an adult is experiencing, or is at risk of experiencing, abuse or neglect. Where the adult who is or is at risk of abuse or neglect has capacity and is still refusing an assessment, local authorities must undertake an assessment so far as possible and document this. They should continue to keep in contact with the adult and carry out an assessment if the adult changes their mind, and asks them to do so.
6.21 In instances where an individual has refused a needs or carer’s assessment but at a later time requests that an assessment is carried out, the local authority must do so. Additionally, where an individual previously refused an assessment and the local authority establishes that the adult or carer’s needs or circumstances have changed, the local authority must consider whether it is required to offer an assessment, unless the person continues to refuse.
First contact with the authority
6.22 The assessment process starts from when local authorities start to collect information about the person. From their very first contact with the local authority, the person must be given as much information as possible about the assessment process, as early as possible, to ensure a personalised approach to the assessment. This should include detail of what can be expected during the assessment process (such as the format and timescale of assessment, complaints processes and possible access to independent advocacy) and allow them to be as involved in the process as possible. Local authorities must ensure that this information is in an accessible format for those to whom it is provided. For example, Braille may be an appropriate format for many with partial-sightedness or who are blind. Some formats are less accessible for certain groups, such as online platforms for those with particular sensory impairments.
6.23 From this early stage local authorities should consider whether the individual would have substantial difficulty in being involved in the assessment process and if so consider the need for independent advocacy (see chapter 7). Local authorities should also consider whether the person may have difficulty communicating (for example those with Autistic Spectrum Disorder or Profound and Multiple Learning Disabilities) and whether a specialist or interpreter may be needed to support communication. For information on reasonable adjustments, see the Equality Act 2010
6.24 Getting the initial response right can save time and costs on assessment later. Some local authorities have found that putting in place a single access point for all new requests and people currently receiving care can speed up and simplify the process for people approaching the authority; and can also free up time for professional staff to focus on more complex cases.
6.25 Local authorities should not, however, remove people from the process too early. Early or targeted interventions such as universal services, a period of reablement and providing equipment or minor household adaptions can delay an adult’s needs from progressing. The first contact with the authority, which triggers the requirement to assess, may lead to a pause in the assessment process to allow such interventions to take place and for any benefit to the adult to be determined. Local authorities must ensure that their staff are sufficiently trained and equipped to make the appropriate judgements needed to steer individuals seeking support towards information and advice, preventative services or a more detailed care and support assessment, or all of these. They must also be able to identify a person who may lack mental capacity and to act accordingly.
6.26 The Care Act provides local authorities with the powers to meet urgent needs where they have not completed an assessment. Authorities may meet urgent need for care and support regardless of the person’s ordinary residence. See the Care Act 2014, Section 19. Where an individual with urgent needs approaches or is referred to the local authority, the local authority should provide an immediate response and meet the individual’s care and support needs. For example, where an individual’s condition deteriorates rapidly or they have an accident, they will need a swift response to ensure their needs are met. In some cases, the appropriate response may be that the local authority will meet the adult’s needs. In other cases, an immediate referral may be the best way to meet a person’s urgent needs, for example by completing the NHS Continuing Healthcare Fast Track Pathway Tool. Following this initial response, the individual should be informed that a more detailed needs assessment, and any subsequent processes, will follow. Once the local authority has ensured these urgent needs are met, it can then consider details such as the person’s ordinary residence and finances.
6.27 Staff who are involved in this first contact must have the appropriate training and should have the benefit of access to professional support from social workers, occupational therapists and other relevant experts as appropriate, to support the identification of any underlying conditions or to ensure that complex needs are identified early and that people are signposted appropriately.
6.28 Local authorities must ensure that any adult with an appearance of care and support needs, and any carer with an appearance of need for support, receives a proportionate assessment which identifies their level of needs. Where appropriate, an assessment may be carried out over the phone or online. In adopting such approaches, local authorities should consider whether the proposed means of carrying out the assessment poses any challenges or risks for certain groups, particularly when assuring itself that it has fulfilled its duties around safeguarding, independent advocacy, and assessing mental capacity. Where there is concern about a person’s capacity to make a decision, for example as a result of a mental impairment such as those with dementia, acquired brain injury, learning disabilities or mental health needs, a face-to-face assessment should be arranged. Local authorities have a duty of care to carry out an assessment in a way that enables them to recognise the needs of those who may not be able to put these into words. Local authorities must ensure that assessors have the skills, knowledge and competence to carry out the assessment in question, and this applies to all assessments regardless of the format they take.
6.29 An assessment should be carried out over an appropriate and reasonable timescale taking into account the urgency of needs and a consideration of any fluctuation in those needs. Local authorities should inform the individual of an indicative timescale over which their assessment will be conducted and keep the person informed throughout the assessment process.
Supporting the person’s involvement in the assessment
6.30 Putting the person at the heart of the assessment process is crucial to understanding the person’s needs, outcomes and wellbeing, and delivering better care and support. The local authority must involve the person being assessed in the process as they are best placed to judge their own wellbeing. In the case of an adult with care and support needs, the local authority must also involve any carer the person has (which may be more than one carer), and in all cases, the authority must also involve any other person requested. The local authority should have processes in place, and suitably trained staff, to ensure the involvement of these parties, so that their perspective and experience supports a better understanding of the needs, outcomes and wellbeing.
6.31 Where local authorities identify that an adult is unable to engage effectively in the assessment process independently, it should seek to involve somebody who can assist the adult in engaging with the process and helping them to articulate their preferred outcomes and needs as early as possible. This will include some people with mental impairments who will nevertheless have capacity to engage in the assessment alongside the local authority. They may require assistance whereby the local authority provides an assessment, tailored to their circumstances, their needs and their ability to engage. They should be supported in understanding the assessment process and assisted to make decisions wherever possible.
6.32 Where there is concern about a person’s capacity to make a specific decision, for example as a result of a mental impairment such as dementia, acquired brain injury or learning disabilities, then an assessment of capacity should be carried out under the Mental Capacity Act (MCA). Those who may lack capacity will need extra support to identify and communicate their needs and make subsequent decisions, and may need an Independent Mental Capacity Advocate. The more serious the needs, the more support people may need to identify their impact and the consequences. Professional qualified staff, such as social workers, can advise and support assessors when they are carrying out an assessment with a person who may lack capacity.
Independent advocates
6.33 At the point of first contact, request or referral (including self-referral), local authorities must seek to ascertain whether an individual is able to be involved in their assessment and local authorities must therefore consider whether the individual has substantial difficulty in doing so. Local authorities must consider whether the adult would experience substantial difficulty in any of these 4 areas: understanding the information provided; retaining the information; using or weighing up the information as part of the process of being involved; and communicating the person’s views, wishes or feelings. Where a person has substantial difficulty in any of these 4 areas, then they need assistance (see chapter 7, on independent advocacy).
6.34 If a person does have substantial difficulty, the local authority must find someone appropriate and independent to support and represent the person, for the purpose of facilitating their involvement. This should be done as early as possible in the assessment process so that the individual’s involvement can be supported throughout all stages of the process. Individuals may require help to understand information provided, assistance in weighing up the information, and support in communicating their wishes and preferences. Where there is a family member or friend who is willing and able to facilitate the person’s involvement effectively, and who is acceptable to the individual and judged appropriate by the local authority, they may be asked to support the individual in the assessment process. Where there is no one thought to be appropriate for this role – either because there is no family member or friend willing and available, or if the individual does not want them to be a part of the assessment – the local authority must appoint an independent advocate.
Appropriate and proportionate assessments
6.35 The assessment must be person-centred throughout. Local authorities must find out the extent to which the person being assessed wishes to be involved in the assessment and should meet those wishes as far as is practicable do so, as the person is best placed to understand the impact of their condition(s) on their outcomes and wellbeing.
6.36 An assessment should be a collaborative process and it is therefore essential that the process is transparent and understandable so that the individual is able to:
- develop an understanding of the assessment process
- develop an understanding of the implications of the assessment process on their condition(s) and situation
- understand their own needs, the outcomes they want to achieve and the impact of their needs on their own wellbeing to allow them to engage effectively with the assessment process
- start to identify the options that are available to them to meet those outcomes and to support their independence and wellbeing
- understand the basis on which decisions are reached
6.37 To support the person’s involvement, the local authority should establish the individual’s communication needs and seek to adapt the assessment process accordingly. In doing so local authorities must provide information about the assessment process in an accessible format.
6.38 To help the adult with needs for care and support, or the carer, prepare for the assessment the local authority should provide in advance, and in an accessible format, the list of questions to be covered in the assessment. This will help the individual or carer prepare for their assessment and think through what their needs are and the outcomes they want to achieve.
6.39 Some people being assessed may have severe communication needs, such as people with Profound and Multiple Learning Disabilities, Autistic Spectrum Disorder, or those who are deaf or blind. Such individuals may require the support of a specialist interpreter to help them to communicate and engage in the assessment.
6.40 Local authorities should also consider the impact of the assessment process itself on the individual’s condition(s). People may feel uncertain and worried about what an assessment involves and may find the process itself to be strenuous. Local authorities should therefore give consideration to the preferences of the individual with regards to the timing, location and medium of the assessment.
6.41 The assessment should be designed to reflect the wishes of the person being assessed, taking into account their presenting need and their circumstances. An assessment process which benefits an individual in one instance may not necessarily be as effective for another. Local authorities should recognise this and in order to maintain a person-centred approach, local authorities must ensure that assessments are flexible to each individual case.
6.42 In carrying out a proportionate assessment local authorities must have regard to:
a) The person’s wishes and preferences and desired outcomes. For example, an individual who pays for their own care may wish to receive local authority support with accessing a particular service, but may not want the same interaction with the authority as someone who wants greater support.
b) The severity and overall extent of the person’s needs. For example, an individual with more complex needs will require a more detailed assessment, potentially involving a number of professionals. A person with lower needs may require a less intensive response.
c) The potential fluctuation of a person’s needs, both adults and carers. For example, where the local authority is aware that an adult’s needs fluctuate over time, the assessment carried out at a particular moment may take into account the adult’s history to get a complete picture of the person’s needs.
6.43 Each local authority may decide to use an assessment tool to help collect information about the adult or carer and details of their wishes and feeling and their desired outcomes and needs. Where a local authority has decided that a person does not need a more detailed assessment, it should consider which elements of the assessment tool it should use and which are not necessary. When carrying out a proportionate assessment the assessor should continue to look for the appearance of further needs which may be the result of an underlying condition. Where the assessor believes that the person’s presenting needs may be as a result of or a part of wider needs then the local authority should undertake a more detailed assessment and refer the person to other services such as housing or the NHS if necessary. For example, the Brain Injury Rehabilitation Trust has produced the Brain Injury Needs Indicator, which is a tool that can be used as part of the assessment to help identify deficits of people with a suspected or diagnosed acquired brain injury.
Supported self-assessment
6.44 A supported self-assessment is an assessment carried out jointly by the adult with care and support needs or carer and the local authority. It places the individual in control of the assessment process to a point where they themselves complete their assessment form. Whilst it is the person filling in the assessment form, the duty to assess the person’s needs, and in doing so ensure that they are accurate and complete, remains with the local authority. Local authorities can offer individuals a supported self-assessment, and must do so if the adult or carer is able, willing and has capacity to undertake it. If the person does not wish to self-assess, then the local authority must undertake an assessment following one of the other processes outlined above.
6.45 In order to support the person in carrying out a supported self-assessment, the local authority must give them any relevant information it has either about the person themselves or, for a carer’s self-assessment, about the individual they care for. This is so that the person undertaking the assessment has a full picture of their care and support history and is equipped with the same information an assessor would have when undertaking an assessment. Before sharing any information, the local authority must ensure that the person consents to that information being shared. If the person lacks capacity, information must only be shared where the local authority is satisfied that doing so is in the person’s best interests. In the case of a young carer, the local authority must also consider whether it is appropriate to share the information about the person the young carer cares for (see chapter 16).
6.46 Once the person has completed the assessment, the local authority must ensure that it is an accurate and complete reflection of the person’s needs, outcomes, and the impact of needs on their wellbeing. The process of a supported self-assessment begins with first contact and is only complete when this assurance has been secured. Until the process of assurance is complete and the local authority has ensured that it is accurate, it will not have discharged its duties under section 9 of the Care Act. Where the person carrying out a supported self-assessment jointly with the local authority requires a specialist, for example people who are deafblind, then the professional leading this assurance process must be seen as the ‘assessor’ and so must have specific training and expertise relating to the individual’s needs. When assuring itself that a self-assessment is comprehensive a local authority should not look to repeat the full assessment process again.
6.47 In assuring self-assessments local authorities may consider it useful to seek the views of those who are in regular contact with the person self-assessing, such as their carer(s) or other appropriate people from their support network, and any professional involved in providing care such as a housing support officer, a GP, a treating clinician, a district nurse, a rehabilitation officer or relevant prison staff. In doing this, the local authority should first seek the person’s consent. This may be helpful in allowing local authorities to build an understanding of the individual’s desires, outcomes, needs, and the impact on their wellbeing.
6.48 The person should be asked to complete a similar assessment questionnaire that the authority uses in their needs or carers’ assessments, which must assess the person’s needs, their outcomes, and the impact of their needs on their wellbeing. The assessment questionnaire can be the same as the one used by local authority assessors or adapted to cover the same questions but made easier for the person to use and understand. Local authorities must also ensure they fulfil other relevant duties under the Act when supporting and assuring a person’s self-assessment, such as those around independent advocacy. If at any point the local authority suspects that a person is experiencing, or is at risk of, abuse and neglect, it must begin a safeguarding enquiry (see chapter 14).
6.49 Before offering a supported self-assessment local authorities must ensure that the individual has capacity to fully assess and reflect their own needs. Local authorities must establish the individual’s mental capacity in accordance with the Mental Capacity Act.
6.50 If a local authority considers a person may lack capacity to understand and carry out a self-assessment, they must carry out a capacity assessment. If this shows that the person lacks the capacity to carry out a self-assessment, then the self-assessment should not be offered.
6.51 Where local authorities have established that the adult has capacity to undertake a self-assessment but experiences substantial difficulty in understanding, retaining and using the relevant information in relation to their self-assessment, they may wish to involve their carer or any other member of their family or support network in their self-assessment. Where the adult does not have the support required from a carer or family member who is willing and able to facilitate the person’s involvement effectively and who is acceptable to the individual and judged appropriate by the local authority, the local authority must provide an independent advocate to assist them in their self-assessment. When a person who would otherwise receive a specialist assessment (for example, someone who is deafblind) chooses to undertake a self-assessment, the local authority must involve a person who has specific training and expertise when assuring that the person’s assessment taken as a whole reflects the overall needs of the individual concerned.
6.52 Local authorities should ensure that self-assessments are completed in suitable time periods. If there is a delay in the person returning the self-assessment form the authority should assure itself that this is not because the person’s condition(s) have deteriorated and is unable to complete the self-assessment.
6.53 The local authority, once it has assured itself that the self-assessment has accurately captured the person’s needs, must make an eligibility determination. Where appropriate this may include taking into account the person’s own view. Although the local authority and the individual are working jointly to ascertain needs and eligibility, the final decision regarding eligibility will rest with the local authority. In all cases, the authority must inform the person of their eligibility judgement and why the local authority has reached the eligibility determination that it has. It must also discuss what needs are eligible and discuss how these might be met. Where the authority determines that the person has needs that are not eligible it must provide advice and information on what services are available in the community that can support the person in meeting those needs.
Safeguarding
6.54 Where a person is at risk of abuse or neglect, it is important that local authorities act swiftly and put in place an effective response. When carrying out an assessment local authorities must consider the impact of the adult’s needs on their wellbeing. If it appears to local authorities that the person is experiencing, or at risk of, abuse or neglect, they must carry out a safeguarding enquiry and decide with the adult in question what action, if any, is necessary and by whom (see chapter 14).
6.55 The decision to carry out a safeguarding enquiry does not depend on the person’s eligibility, but should be taken wherever there is reasonable cause to think that the person is experiencing, or is at risk of, abuse or neglect. Where this is the case, a local authority must carry out (or request others to carry out) whatever enquiries it thinks are necessary in order to decide whether any further action is necessary.
6.56 Where the actions required to protect the adult can be met by local authorities, they should take appropriate action. In some cases, safeguarding enquiries may result in the provision of care and support (under either section 18 or 19 of the Care Act), or the provision of preventative services (under section 2) or information and advice (under section 4). In the majority of cases the response will involve other agencies, for example, a safeguarding enquiry may result in referrals to the police, a change of accommodation, or action by CQC.
6.57 Where the adult has care and support needs, local authorities must continue to carry out a needs assessment and determine whether they have eligible needs, and if so, how these will be met. The assessment for care and support should run parallel to the safeguarding enquiry and the enquiry should not disrupt the assessment process or the local authority meeting eligible needs.
Fluctuating needs
6.58 As the condition(s) of the individual at the time of the assessment may not be entirely indicative of their needs more generally, local authorities must consider whether the individual’s current level of need is likely to fluctuate and what their on-going needs for care and support are likely to be. This is the case both for short-term fluctuations, which may be over the course of the day, and longer term changes in the level of the person’s needs. In establishing the on-going level of need local authorities must consider the person’s care and support history over a suitable period of time, both the frequency and degree of fluctuation. The local authority may also take into account at this point what fluctuations in need can be reasonably expected based on experience of others with a similar condition. It is important to recognise the benefit of adopting this comprehensive approach to assessment as the consideration of an individual’s wider wellbeing may allow local authorities to provide types of care and support, or information and advice which delay or prevent the development of further needs in the future.
6.59 The assessment should also include a consideration of the individual’s wider care and support needs. This may include types of care and support the individual has received in the past and their general medical history, which may be indicative of their current care and support needs.
Focusing on preventing needs
6.60 The assessment and eligibility framework should be a key element of any prevention strategies authorities put in place. It is during the assessment where local authorities can identify needs that could be reduced, or where escalation could be delayed, and help people improve their wellbeing by providing specific preventive services, or information and advice on other universal services available locally. Early interventions can prevent or delay a person’s needs from progressing.
6.61 In parallel with assessing a person’s needs, local authorities must consider the benefits of approaches which delay or prevent the development of needs in individuals. This applies to both people with current needs that may be reduced or met through available universal services in the community, and those without needs who may otherwise require care and support in the future. This could include directing people to services such as community support groups which ensure that people feel supported, including an ability to participate in their local community. It may also include helping the person to access services which the local authority provides as part of its universal offer on prevention. Local authorities can also support the person in understanding other types of support available to them, such as within their own support networks, for example to seek to promote access to appropriate employment, education or training, which can be an effective way of maintaining independence. Such interventions at an early stage will help to sustain the independence and wellbeing of people (see chapter 2 on prevention and chapter 3 on information and advice).
6.62 Where the local authority judges that the person may benefit from such types of support, it should take steps to support the person to access those services. The local authority may ‘pause’ the assessment process to allow time for the benefits of such activities to be realised, so that the final assessment of need (and determination of eligibility) is based on the remaining needs which have not been met through such interventions. For example, if the local authority believes that a person may benefit from a short-term reablement service which is available locally, it may put that in place and complete the assessment following the provision of that service.
Considering the person’s strengths and capabilities
6.63 At the same time as carrying out the assessment, the local authority must consider what else other than the provision of care and support might assist the person in meeting the outcomes they want to achieve. In considering what else might help, authorities should consider the person’s own strengths and capabilities, and what support might be available from their wider support network or within the community to help. Strengths-based approaches might include co-production of services with people who are receiving care and support to foster mutual support networks. Encouraging people to use their gifts and strengths in a community setting could involve developing residents’ groups and appropriate training to support people in developing their skills.
6.64 Local authorities might also consider the ways a person’s cultural and spiritual networks can support them in meeting needs and building strengths, and explore this with the person. Any suggestion that support could be available from family and friends should be considered in light of their appropriateness, willingness and ability to provide any additional support and the impact on them of doing so. It must also be based on the agreement of the adult or carer in question.
Considering the person’s strengths: a case study
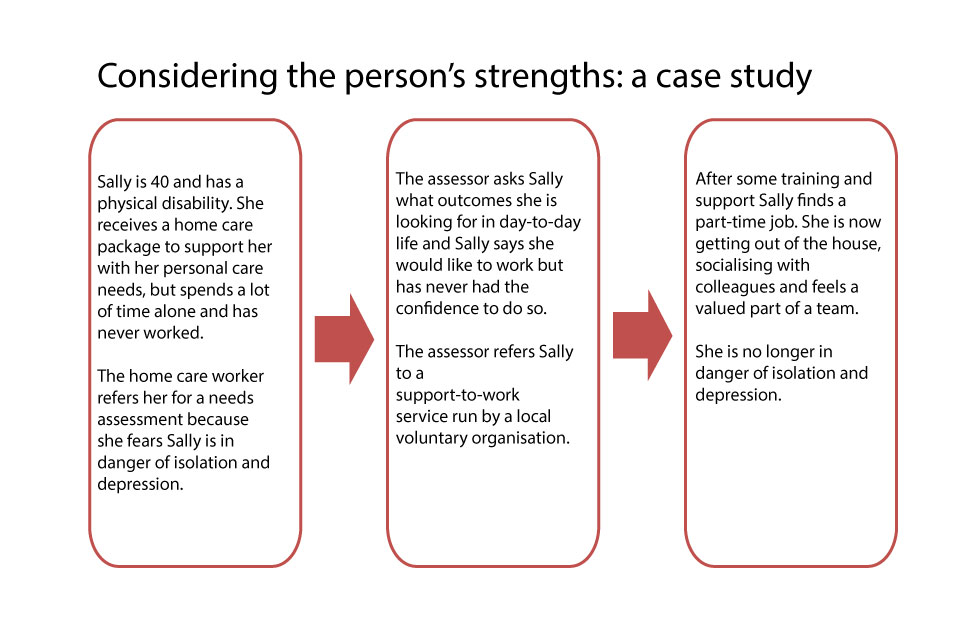
Whole family approach
6.65 The intention of the whole family approach is for local authorities to take a holistic view of the person’s needs and to identify how the adult’s needs for care and support impact on family members or others in their support network.
6.66 During the assessment the local authority must consider the impact of the person’s needs for care and support on family members or other people the authority may feel appropriate. This will require the authority to identify anyone who may be part of the person’s wider network of care and support.
6.67 In considering the impact of the person’s needs on those around them, the local authority must consider whether or not the provision of any information and advice would be beneficial to those people they have identified. For example, this may include signposting to any support services in the local community.
6.68 The local authority must also identify any children who are involved in providing care. The authority may become aware that the child is carrying out a caring role through the assessment of the person needing care or their carer, or informed through family members or a school. Identification of a young carer in the family should result in an offer of a needs assessment for the adult requiring care and support and, where appropriate, the local authority must consider whether the child or young carer should be referred for a young carer’s assessment or a needs assessment under the Children Act 1989, or a young carer’s assessment under section 63 of the Care Act. Local authorities should ensure that adults’ and children’s care and support services work together to ensure the assessment is effective – for example by sharing expertise and linking processes.
6.69 When carrying out an adult’s or carer’s assessment, if it appears that a child is involved in providing care the local authority must consider:
- the impact of the person’s needs on the young carer’s wellbeing, welfare, education and development
- whether any of the caring responsibilities the young carer is undertaking are inappropriate
6.70 An assessment should take into account the parenting responsibilities of the person as well as the impact of the adult’s needs for care and support on the young carer.
6.71 Local authorities must also consider whether any of the caring tasks the child is undertaking are inappropriate. They should consider how supporting the adult with needs for care and support can prevent the young carer from undertaking excessive or inappropriate care and support responsibilities. A young carer becomes vulnerable when their caring role risks impacting upon their emotional or physical wellbeing or their prospects in education and life. This might include:
- preventing the young carer from accessing education, for example because the adult’s needs for care and support result in the young carer’s regular absence from school or impacts upon their learning
- preventing the young carer from building relationships and friendships
- impacting upon any other aspect of the young carer’s wellbeing
6.72 Inappropriate caring responsibilities should be considered as anything which is likely to have an impact on the child’s health, wellbeing or education, or which can be considered unsuitable in light of the child’s circumstances and may include:
- personal care such as bathing and toileting
- carrying out strenuous physical tasks such as lifting
- administering medication
- maintaining the family budget
- emotional support to the adult
6.73 When a local authority is determining whether the tasks a child carries out are inappropriate, it should also take into account the child’s own view wherever appropriate.
Combining assessments
6.74 Local authorities may combine an assessment of an adult needing care and support or of a carer with any other assessment it is carrying out either of that person or another where both the individual and carer agree, and the consent condition is met in relation to a child. This will also avoid the authority carrying out 2 separate assessments when the 2 assessments are intrinsically linked. If either of the individuals concerned does not agree to a combined assessment, then the assessments must be carried out separately.
Integrated assessments
6.75 People may have needs that are met by various bodies. Therefore, a holistic approach to assessment which aims to bring together all of the person’s needs may need the input of different professionals such as adult care and support, children’s services, housing, experts in the voluntary sector, relevant professionals in the criminal justice system, health or mental health professionals.
6.76 A local authority may carry out a needs or carer’s assessment jointly with another body carrying out any other assessment in relation to the person concerned, provided that person agrees. In doing so, the authority may integrate or align assessment processes in order to better fit around the needs of the individual. An integrated approach may involve working together with relevant professionals on a single assessment. It may also include putting processes in place to ensure that the person is referred for other assessments such as an assessment for after-care needs under the Mental Health Act 1983. In some settings, for example in prisons, local authorities should engage relevant professionals early to ensure assessors are prepared for carrying out an assessment in that environment.
6.77 Where more than one agency is assessing a person, they should all work closely together to prevent that person having to undergo a number of assessments at different times, which can be distressing and confusing.
6.78 Where a person has both health and care and support needs, local authorities and the NHS should work together effectively to deliver a high quality, coordinated assessment. To achieve this, local authorities should:
- shape the process around the person, involving the person and considering their experience when coordinating an integrated assessment
- work with other professionals to ensure the person’s health and care services are aligned. This will require flexibility of systems where possible, for example when sharing information. It will also be strengthened by a culture of common values and objectives at frontline level - joint visits can be helpful here
- link together various care and support plans to set out a single, shared care pathway, for example when following the Care Programme Approach for people with a severe mental disorder who need multi-agency support or intensive intervention, under the direction of a named care coordinator. See chapter 34 of the revised Code of Practice Mental Health Act 1983. A multi-agency approach is particularly important where people are enrolled on the Proactive Care Programme, which was introduced through the Avoiding Unplanned Emergency Admissions Enhanced Service in the 2014 to 2015 GP Contract.
6.79 The local authority may carry out the care and support assessment jointly with any other assessment, and can also undertake the other assessment on behalf of the other body, where this is agreed. Where an assessment involves a body from outside of the local authority, the local authority should provide any resources or facilities which may be required to carry out the assessment. Sharing resources may include the provision of facilities or relative information relating to the person being assessed. (See chapters 15-18 on Integration and Partnership Working).
NHS Continuing Healthcare
6.80 Where it appears that a person may be eligible for NHS Continuing Healthcare (NHS CHC), local authorities must notify the relevant Clinical Commissioning Group (CCG). NHS CHC is a package of on-going care that is arranged and funded solely by the NHS where the individual has been found to have a ‘primary health need’ as set out in the national framework for NHS Continuing Healthcare and NHS-funded nursing care. Such care is provided to individuals aged 18 or over, to meet needs that have arisen as a result of disability, accident or illness. Eligibility for NHS CHC places no limits on the settings in which the package of support can be offered or on the type of service delivery.
6.81 Whilst local authorities have a duty to carry out an assessment where a person has an appearance of needs and a duty to meet eligible needs, local authorities cannot arrange services that are the responsibility of the NHS (for example, care provided by registered nurses and services that the NHS has to provide because the individual is eligible for NHS CHC). However, the local authority may provide or arrange healthcare services where they are incidental or ancillary to doing something else to meet needs for care and support and the service or facility in question is of a nature that a local authority could be expected to provide. Ultimate responsibility for arranging and monitoring the services required to meet the needs of those who qualify for NHS CHC rests with the NHS.
6.82 Individuals may require care and support provided by their local authority and/or services arranged by CCGs. Local authorities and CCGs therefore have a responsibility to ensure that the assessment of eligibility for care and support and CHC respectively take place in a timely and consistent manner. If, following an assessment for NHS CHC, a person is not found to be eligible for NHS CHC, the NHS may still have a responsibility to contribute to that person’s health needs – either by directly commissioning services or by part-funding the package of support. Where a package of support is commissioned or funded by both a local authority and a CCG, this is known as a joint package of care. A joint package of care could include NHS-funded nursing care and other NHS services that are beyond the powers of a local authority to meet. The joint package could also involve the CCG and the local authority both contributing to the cost of the care package, or the CCG commissioning part of the package. Joint packages of care may be provided in a nursing or care home, or in a person’s own home, and could be by way of joint personal budget.
6.83 Local authorities and CCGs in each local area must agree a local disputes resolution process to resolve cases where there is a dispute between them about eligibility for NHS CHC, the apportionment of funding in joint funded care and support packages, or the operation of refunds guidance. Disputes should not delay the provision of the care package, and the process should make clear how funding will be provided pending resolution of the dispute. Where disputes relate to local authorities and CCGs in different geographical areas, the disputes resolution process of the responsible CCG should normally be used in order to ensure resolution in a robust and timely manner. This should include agreement on how funding will be provided during the dispute, and arrangements for reimbursement to the agencies involved once the dispute is resolved.
Roles and responsibilities
6.84 Assessments can be carried out by a range of professionals including registered social workers, occupational therapists and rehabilitation officers. Registered social workers and occupational therapists are considered to be 2 of the key professions in adult care and support. Local authorities should consider how adults who need care, carers, and assessors have access to registered social care practitioners, such as social workers or occupational therapists.
Training
6.85 It is essential that the assessment is carried out to the highest quality. The assessment must: identify the person’s needs, outcomes and how these impact on their wellbeing; consider the person’s strengths and capabilities; and consider what universal services might help the person improve their wellbeing. Local authorities must ensure that their staff have the required skills, knowledge and competence to undertake assessments and that this is maintained. This applies no matter how the assessment is carried out, including first contact, any assessment over the phone or online, or self-assessments where the person carrying out the assurance will need to have the appropriate training.
6.86 Local authorities must ensure that assessors are appropriately trained and competent whenever they carry out an assessment. This means ensuring that assessors undergo regular, up-to-date training on an ongoing basis. The training must be appropriate to the assessment, both the format of assessment and the condition(s) and circumstances of the person being assessed. They must also have the skills and knowledge to carry out an assessment of needs that relate to a specific condition or circumstances requiring expert insight, for example when assessing an individual who has autism, learning disabilities, mental health needs or dementia. This training must be maintained throughout their career. As part of maintaining their registration, social workers and occupational therapists are required to evidence their Continuing Professional Development.
6.87 When assessing particularly complex or multiple needs, an assessor may require the support of an expert to carry out the assessment, to ensure that the person’s needs are fully captured. Local authorities should consider whether additional relevant expertise is required on a case-by-case basis, taking into account the nature of the needs of the individual, and the skills of those carrying out the assessment. The local authority must ensure that the person is able to be involved as far as possible, for example by providing an interpreter where a person has a particular condition affecting communication – such as autism, blindness, or deafness. See the Equality Act for necessary provisions around reasonable adjustments.
6.88 Where the assessor does not have the necessary knowledge of a particular condition or circumstance, they must consult someone who has relevant expertise. This is to ensure that the assessor can ask the right questions relating to the condition and interpret these appropriately to identify underlying needs. A person with relevant expertise can be considered as somebody who, either through training or experience, has acquired knowledge or skill of the particular condition or circumstance. Such a person may be a doctor or health professional, or an expert from the voluntary sector, but there is no obligation for the local authority to source an expert from an outside body if the expertise is available in house.
6.89 The Department of Health has published guidance for certain groups of adults that refer to their assessment for care and support. Two specific areas are for people who are deafblind and people with autism and these pieces of guidance should be read with this guidance. Think Autism 2014, the April 2014 update to Fulfilling and Rewarding Lives, the strategy for adults with autism in England (2010), sets out that local authorities should:
- make basic autism training available for all staff working in health and social care
- develop or provide specialist training for those in roles that have a direct impact on access to services for adults with autism
- include quality autism awareness training within general equality and diversity training programmes across public services
6.90 The Care Act strengthens this guidance in relation to assessors having specialised training to assess an adult with autism. The Act places a legal requirement on local authorities that all assessors must have the skills, knowledge and competence to carry out the assessment in question. Where an assessor does not have experience in a particular condition (such as autism, learning disabilities, mental health needs or other conditions), they must consult someone with relevant experience. This is so that the person being assessed is involved throughout the process and their needs, outcomes and the impact of needs on their wellbeing are all accurately identified.
Assessment for people who are deafblind
6.91 Local authorities must ensure that an expert is involved in the assessment of adults who are deafblind, including where a deafblind person is carrying out a supported self-assessment jointly with the authority. People are regarded as deafblind ‘if their combined sight and hearing impairment causes difficulties with communication, access to information and mobility. This includes people with a progressive sight and hearing loss’ (Think Dual Sensory, Department of Health, 1995).
6.92 During an assessment if there is the appearance of both sensory impairments, even if when taken separately each sensory impairment appears relatively mild, the assessor must consider whether the person is deafblind as defined above. If a person is deafblind, this must trigger a specialist assessment. This specialist assessment must be carried out by an assessor or team that has training of at least QCF or OCN level 3, or above where the person has higher or more complex needs.
6.93 Training and expertise should in particular include; communication, one-to-one human contact, social interaction and emotional wellbeing, support with mobility, assistive technology and rehabilitation. The type and degree of specialism required should be judged on a case by case basis, according to the extent of the person’s condition and their communication needs. Local authorities should also recognise that deafblindness is a dual sensory condition which requires a knowledge and understanding of the 2 respective conditions in unison, which cannot be replicated by taking an individual approach to both senses.
6.94 The combined loss of sight and hearing can have a significant impact upon the individual even where they are not profoundly deaf and totally blind, as it is the impact of one impairment upon the other which causes difficulties. Deafblindness can have significant impact on the adult’s independence and their ability to achieve their desired outcomes. In particular deafblindness may have impact on the adult’s:
- autonomy and ability to maintain choice and control
- health and safety and daily routine
- involvement in education, work, family and social life
6.95 Local authorities should recognise that adults may not define themselves as deafblind. Instead they may describe their vision and hearing loss in terms which indicate that they have significant difficulty in their day-to-day lives. The assessment must therefore take the initiative to establish maximum possible communication with the adult to ensure that individuals are as fully engaged as possible and have the opportunity to express their wishes and desired outcomes. This is particularly important where the person is carrying out a supported self-assessment jointly with the local authority. The person ensuring that the self-assessment is a complete and accurate reflection of needs must have specific training and expertise that will enable maximum possible communication and an accurate and complete assessment.
6.96 Whilst the person carrying out the assessment must have the suitable training and expertise, it may not be possible for them to carry out the assessment without an interpreter, for instance where the adult uses sign language. Therefore, where necessary a qualified interpreter with training appropriate for the deafblind adult’s communication should be used. It is not normally appropriate to use a family member or carer as an interpreter, though sometimes this is appropriate, for instance where the adult’s communication is idiosyncratic or personal to them and would only be understood by those close to them. This should only take place where the adult agrees or – if they lack capacity – where it is in their best interests.
6.97 The assessment should take into account both the current and future needs of the person being assessed, particularly where the adult’s deafblindness is at risk of deteriorating. In such cases the adult may benefit from learning alternative forms of communication before their condition has deteriorated to a point where their current or preferred form of communication is no longer suitable.
Record keeping
6.98 Following their assessment, individuals must be given a record of their needs or carer’s assessment. A copy must also be shared with anybody else that the individual requests the local authority to share a copy with. Where an independent advocate, an Independent Mental Capacity Advocate or an Independent Mental Health Advocate is involved in supporting the individual, the local authority should keep the advocate informed so that they can support the person to understand the outcome of the assessment and its implications.
Delegating assessments
6.99 Local authorities can delegate the majority of their care and support functions, including assessment (see chapter 18). In doing so they must ensure that the body carrying out an assessment complies with all the requirements and fulfils all relevant duties under the Act and regulations (such as providing an independent advocate – (see chapter 7). Anything done by the body carrying out an assessment is treated as if done by the local authority. In respect of duties surrounding non-delegated functions, such as safeguarding (see chapter 14), local authorities must have appropriate processes in place to ensure they fulfill these functions, for example agreeing with the body that the local authority is notified if a safeguarding issue is spotted.
Eligibility
6.100 The national eligibility criteria set a minimum threshold for adult care and support needs and carer support needs which local authorities must meet. All local authorities must comply with this national threshold. Authorities can also decide to meet needs that are not deemed to be eligible if they chose to do so.
6.101 The introduction of a national eligibility threshold provides more transparency on what level of need is eligible. More clarity will support authorities in deciding whether the earlier provision of information and advice or preventative services would delay a person from developing needs which meet the eligibility criteria or whether longer-term care and support might be needed. It should also help the person needing care or their carer to think more broadly about what support might be available in the local community or through their support network to meet their needs and support the outcomes they want to achieve.
What is the national eligibility threshold for adults needing care?
6.102 The eligibility threshold for adults with care and support needs is set out in the Care and Support (Eligibility Criteria) Regulations 2015 (the ‘Eligibility Regulations’). The threshold is based on identifying how a person’s needs affect their ability to achieve relevant outcomes, and how this impacts on their wellbeing.
6.103 In considering whether an adult with care and support needs has eligible needs, local authorities must consider whether:
- the adult’s needs arise from or are related to a physical or mental impairment or illness
- as a result of the adult’s needs the adult is unable to achieve 2 or more of the specified outcomes (which are described in the guidance below)
- as a consequence of being unable to achieve these outcomes there is, or there is likely to be, a significant impact on the adult’s wellbeing
An adult’s needs are only eligible where they meet all 3 of these conditions.
Interpreting the eligibility criteria
6.104 The adult’s needs arise from or are related to a physical or mental impairment or illness. The first condition that local authorities must be satisfied about is that the adult’s needs for care and support are due to a physical or mental impairment or illness and that they are not caused by other circumstantial factors. Local authorities must consider at this stage if the adult has a condition as a result of either physical, mental, sensory, learning or cognitive disabilities or illnesses, substance misuse or brain injury. The authority should base their judgment on the assessment of the adult and a formal diagnosis of the condition should not be required.
As a result of the adult’s needs, the adult is unable to achieve 2 or more of the outcomes set out in the regulations
6.105 The second condition that authorities must consider is whether the adult is ‘unable’ to achieve 2 or more of the outcomes set out in the regulations. Authorities must also be aware that the regulations provide that ‘being unable’ to achieve an outcome includes any of the following circumstances, where the adult:
- is unable to achieve the outcome without assistance. This would include where an adult would be unable to do so even when assistance is provided. It also includes where the adult may need prompting for example, some adults may be physically able to wash but need reminding of the importance of personal hygiene
- is able to achieve the outcome without assistance but doing so causes the adult significant pain, distress or anxiety. For example, an older person with severe arthritis may be able to prepare a meal, but doing so will leave them in severe pain and unable to eat the meal
- is able to achieve the outcome without assistance, but doing so endangers or is likely to endanger the health or safety of the adult, or of others – for example, if the health or safety of another member of the family, including any child, could be endangered when an adult attempts to complete a task or an activity without relevant support
- is able to achieve the outcome without assistance but takes significantly longer than would normally be expected. For example, an adult with a physical disability is able to dress themselves in the morning, but it takes them a long time to do this, leaves them exhausted and prevents them from achieving other outcomes
6.106 The Eligibility Regulations set out a range of outcomes. Local authorities must consider whether the adult is unable to achieve 2 or more of these outcomes when making the eligibility determination. The following section of the guidance provides examples of how local authorities should consider each outcome set out in the Eligibility Regulations (which do not constitute an exhaustive list) when determining the adult’s eligibility for care and support:
a) Managing and maintaining nutrition - local authorities should consider whether the adult has access to food and drink to maintain nutrition, and that the adult is able to prepare and consume the food and drink.
b) Maintaining personal hygiene - local authorities should, for example, consider the adult’s ability to wash themselves and launder their clothes.
c) Managing toilet needs - local authorities should consider the adult’s ability to access and use a toilet and manage their toilet needs.
d) Being appropriately clothed - local authorities should consider the adult’s ability to dress themselves and to be appropriately dressed, for instance in relation to the weather to maintain their health.
e) Being able to make use of the home safely - local authorities should consider the adult’s ability to move around the home safely, which could for example include getting up steps, using kitchen facilities or accessing the bathroom. This should also include the immediate environment around the home such as access to the property, for example steps leading up to the home.
f) Maintaining a habitable home environment - local authorities should consider whether the condition of the adult’s home is sufficiently clean and maintained to be safe. A habitable home is safe and has essential amenities. An adult may require support to sustain their occupancy of the home and to maintain amenities, such as water, electricity and gas.
g) Developing and maintaining family or other personal relationships - local authorities should consider whether the adult is lonely or isolated, either because their needs prevent them from maintaining the personal relationships they have or because their needs prevent them from developing new relationships.
h) Accessing and engaging in work, training, education or volunteering - local authorities should consider whether the adult has an opportunity to apply themselves and contribute to society through work, training, education or volunteering, subject to their own wishes in this regard. This includes the physical access to any facility and support with the participation in the relevant activity.
i) Making use of necessary facilities or services in the local community including public transport and recreational facilities or services - local authorities should consider the adult’s ability to get around in the community safely and consider their ability to use such facilities as public transport, shops or recreational facilities when considering the impact on their wellbeing. Local authorities do not have responsibility for the provision of NHS services such as patient transport, however they should consider needs for support when the adult is attending healthcare appointments.
j) Carrying out any caring responsibilities the adult has for a child - local authorities should consider any parenting or other caring responsibilities the person has. The adult may for example be a step-parent with caring responsibilities for their spouse’s children.
As a consequence there is, or there is likely to be, a significant impact on the adult’s wellbeing
6.107 The third condition that must be met is that local authorities must consider whether the adult’s needs and their inability to achieve the outcomes above cause or risk causing a significant impact on their wellbeing. The meaning of wellbeing is set out in Section 1 of the Care Act and more detail is described in chapter 1 of this guidance.
6.108 Local authorities must determine how the adult’s inability to achieve the outcomes above impacts on their wellbeing. Where the adult is unable to achieve more than one of the outcomes, the local authority does not need to consider the impact of each individually, but should consider whether the cumulative effect of being unable to achieve those outcomes is one of a ‘significant impact on wellbeing’. In doing so, local authorities should also consider whether:
- the adult’s inability to achieve the outcomes above impacts on at least one of the areas of wellbeing (as described in Section 1 of the Act and chapter 1 of this guidance) in a significant way
- the effect of the impact on a number of the areas of wellbeing mean that there is a significant impact on the adult’s overall wellbeing
6.109 The term ‘significant’ is not defined by the regulations, and must therefore be understood to have its everyday meaning. Local authorities will have to consider whether the adult’s needs and their consequent inability to achieve the relevant outcomes will have an important, consequential effect on their daily lives, their independence and their wellbeing.
6.110 In making this judgment, local authorities should look to understand the adult’s needs in the context of what is important to him or her. Needs may affect different people differently, because what is important to the individual’s wellbeing may not be the same in all cases. Circumstances which create a significant impact on the wellbeing of one individual may not have the same effect on another.
6.111 The table below illustrates the interplay of the 3 conditions above, the outcomes listed in the eligibility regulations and the wellbeing principle, which is broken down into areas of wellbeing in (see chapter 1: Promoting wellbeing).
Eligibility decision process
1. Needs
The adult’s needs arise from or are related to a physical or mental impairment or illness.
2. Outcomes
As a result of the needs, the adult is unable to achieve 2 or more of the following:
- a) managing and maintaining nutrition
- b) maintaining personal hygiene
- c) managing toilet needs
- d) being appropriately clothed
- e) maintaining a habitable home environment
- f) being able to make use of the home safely
- g) developing and maintaining family or other personal relationships
- h) accessing and engaging in work, training, education or volunteering
- i) making use of necessary facilities or services in the local community including public transport and recreational facilities or services
- j) carrying out any caring responsibilities the adult has for a child
3. Wellbeing
As a consequence, there is or is likely to be a significant impact on the adult’s wellbeing, including the following:
- a) personal dignity (including treatment of the individual with respect)
- b) physical and mental health and emotional wellbeing
- c) protection from abuse and neglect
- d) control by the individual over day-to-day life (including over care and support provided and the way it is provided)
- e) participation in work, education, training or recreation
- f) social and economic wellbeing
- g) domestic, family and personal relationships
- h) suitability of living accommodation
- i) the individual’s contribution to society
6.112 The case studies which follow demonstrate examples of how eligibility determinations may be made. The purpose of these case studies is to illustrate eligibility on the basis of significant impact on wellbeing where the person has needs caused by a physical or mental impairment or illness which mean they are unable to achieve 2 or more outcomes specified in the Eligibility Regulations. Significant impact on wellbeing is personal, so although 2 people are in similar circumstances, the impact on their wellbeing is different.
Case Study 1: John (eligible)
John is 32 and has been referred by his mother for an assessment, who is concerned for John and his future. John is unemployed and lives with his mother and she is getting to an age where she realises that she might not be able to provide the same level of care and support for her son as she has done so far. John is able to manage his own personal care, but his mother does all the housework for both of them. John feels increasingly isolated and will not leave the house without his mother. It is important to John that he is intellectually stimulated and there is a chess club nearby which he would like to join, but John does not feel confident about this due to his anxiety in social situations.
Needs
Adult on the autistic spectrum.
Outcomes
John has severe difficulties socialising and co-operating with other people.
He only has transactional exchanges and cannot maintain eye contact. John knows that others feel uneasy around him, and spends a lot of his time alone. As a result, John is unable to achieve the following outcomes: Developing and maintaining family or other personal relationships and making use of necessary facilities and services in the community.
Impact on wellbeing
John is too anxious to initiate developing friendships on his own although he would like to and he feels lonely and depressed most of the time. His nervousness also affects his ability to take advantage of facilities in the community, which could help him feel less lonely. Feeling anxious and lonely has a significant impact on his wellbeing
Decision: Eligible
Next Actions
John’s local authority thinks John’s needs are eligible. Both John and the local authority agree that the most effective way of meeting John’s needs is to develop his confidence to join the chess club. John uses his personal budget to pay for a support worker to accompany him to an autism social skills group, and to the chess club and to travel with him on the bus to get there.
John’s local authority notes that John’s mother could need support too and offers her a carer’s assessment.
Case study 2: Dave (not eligible)
Dave is 32 and has been referred by his mother for an assessment, who is concerned for Dave and his future. Dave lives with his mother and she is getting to an age where she realises that she might not be able to provide the same level of care and support for her son as she has done so far.
Dave is able to manage his own personal care, but his mother does all the housework for both of them. Dave also works, but would like to get a job that is a better match for his intellectual abilities as his current job does not make the most of his numerical skills. Dave’s social contact is mainly online because he feels more comfortable communicating this way and he spends a lot of time in his room on his computer.
Category
Adult on the autistic spectrum.
Needs
Dave struggles severely in social situations leading to difficulties accessing work and cooperating with other people. He only has transactional exchanges with others and cannot maintain eye contact. Dave knows that others feel uneasy around him and spends a lot of his time alone.
Impact on wellbeing
Dave is not in ideal employment, but has access to and is engaged in work. This has some impact on his wellbeing but not to a significant extent.
Dave prefers to socialise with people online. It emerges from conversations with Dave that he has access to those personal relationships that he considers essential. Dave is contributing to society, has contact with others, is in employment and is able to look after himself.
Decision: Not Eligible
Dave has difficulties doing some of the things that many other people would think should be a natural part of daily living and he is unable to participate in recreational activities in a conventional sense. Those aspects of his wellbeing that are affected by the needs caused by his autism are not so significantly affected that Dave’s overall wellbeing is at risk.
The local authority decides that Dave’s needs are not eligible, because they do not have a significant effect on his wellbeing despite his mother’s concerns.
Next Actions
The local authority records Dave’s assessment and sends him a copy. They include information about a local autism support group. Dave’s local authority notes that Dave’s mother could well need support and offers her a carer’s assessment.
Fluctuating needs
6.113 Individuals with fluctuating needs may have needs which are not apparent at the time of the assessment, but may have arisen in the past and are likely to arise again in the future. Therefore local authorities must consider an individual’s need over an appropriate period of time to ensure that all of their needs have been accounted for when eligibility is being determined. Where fluctuating needs are apparent, this should also be factored into the care plan, detailing the steps local authorities will take to meet needs in circumstances where these fluctuate. For example, an adult with a mental illness, which has been managed in the past 8 months but which could deteriorate, if circumstances in the adult’s life change. In such situations, local authorities must consider the nature of the adult’s needs have been over the past year to get a complete picture of the adult’s level of need.
6.114 When considering the type of needs an adult may have, local authorities should note that there is no hierarchy of needs or of the areas of wellbeing as described in chapter 1 of this guidance.
Considering needs met by carers in eligibility determinations
6.115 The eligibility determination must be made based on the adult’s needs and how these impact on their wellbeing. Authorities must only take consideration of whether the adult has a carer, or what needs may be met by a carer after the eligibility determination when a care and support plan is prepared. The determination must be based solely on the adult’s needs and if an adult does have a carer, the care they are providing will be taken into account when considering whether the needs must be met. Local authorities are not required to meet any eligible needs which are being met by a carer, but those needs should be recognised and recorded as eligible during the assessment process. This is to ensure that should there be a breakdown in the caring relationship, the needs are already identified as eligible, and therefore local authorities must take steps to meet them without further assessment.
What is the national eligibility threshold for carers?
6.116 Carers can be eligible for support in their own right. The national eligibility threshold for carers is also set out in the Care and Support (Eligibility Criteria) Regulations 2015. The threshold is based on the impact a carer’s needs for support has on their wellbeing.
6.117 In considering whether a carer has eligible needs, local authorities must consider whether:
- the needs arise as a consequence of providing necessary care for an adult
- the effect of the carer’s needs is that any of the circumstances specified in the Eligibility Regulations apply to the carer
- as a consequence of that fact there is, or there is likely to be, a significant impact on the carer’s wellbeing
A carer’s needs are only eligible where they meet all 3 of these conditions.
Interpreting the carers’ eligibility criteria
The needs arise as a consequence of providing necessary care for an adult
6.118 Local authorities must consider whether the carer’s need for support arises because they are providing care to an adult. Carers can be eligible for support whether or not the adult for whom they care has eligible needs. The eligibility determination must be made based on the carer’s needs and how these impact on their wellbeing. The determination should be made without consideration of whether or not the adult the carer cares for, has eligible needs.
6.119 The carer must also be providing necessary care. If the carer is providing care and support for needs which the adult is capable of meeting themselves, the carer may not be providing necessary support. In such cases, local authorities should provide information and advice to the adult and carer about how the adult can use their own strengths or services available in the community to meet their needs.
The effect of the carer’s needs is that any of the circumstances specified in the Eligibility Regulations apply to the carer
6.120 The second condition that authorities must consider is whether the carer’s physical or mental health is either deteriorating or is at risk of doing so, or whether the carer is unable to achieve any of a list of other outcomes which may apply.
6.121 Authorities must be aware that the regulations provide that ‘being unable’ to achieve outcomes, includes circumstances where the carer:
- is unable to achieve the outcome without assistance. This includes where the carer would be unable to achieve an outcome even if assistance were provided. A carer might, for example, be unable to fulfill their parental responsibilities unless they receive support in their caring role
- is able to achieve the outcome without assistance, but doing so causes or is likely to cause significant pain, distress or anxiety. A carer might for example be able to care for the adult and undertake fulltime employment, but if doing both, this causes the carer significant distress, the carer should not be considered able to engage in employment
- is able to achieve the outcome without assistance but doing so is likely to endanger the health or safety of the carer or any adults or children for whom the carer provides care. A carer might for example be able to provide care for their family and deliver necessary care for the adult, but, where this endangers the adult with care and support needs, for example, because the adult receiving care would have to be left alone while other responsibilities are met, the carer should not be considered able to meet the outcome of caring for their family
6.122 The Eligibility Regulations set out a range of outcomes. Local authorities must consider whether the carer is able to achieve these outcomes or if due to the nature of their needs they are unable to achieve any of the outcomes. The carer will have eligible needs met if they are unable to achieve any of these outcomes and as a result there is, or there is likely to be, a significant impact on their wellbeing.
6.123 The following section of the guidance provides examples of how local authorities should consider the outcomes set out in the Eligibility Regulations when they determine whether a carer meets the eligibility criteria. To be eligible, a carer must be unable to achieve any of the following outcomes:
| Criteria | Examples of how to interpret the criteria |
|---|---|
| (i) carrying out any caring responsibilities the carer has for a child | Local authorities should consider any parenting or other caring responsibilities the carer has for a child in addition to their caring role for the adult. For example, the carer might be a grandparent with caring responsibilities for their grandchildren while the grandchildren’s parents are at work. |
| (ii) providing care to other persons for whom the carer provides care | Local authorities should consider any additional caring responsibilities the carer may have for other adults. For example, a carer may also have caring responsibilities for a parent in addition to caring for the adult with care and support needs. |
| (iii) maintaining a habitable home environment | Local authorities should consider whether the condition of the carer’s home is safe and an appropriate environment to live in and whether it presents a significant risk to the carer’s wellbeing. A habitable home should be safe and have essential amenities such as water, electricity and gas. |
| (iv) managing and maintaining nutrition | Local authorities should consider whether the carer has the time to do essential shopping and to prepare meals for themselves and their family. |
| (v) developing and maintaining family or other significant personal relationships | Local authorities should consider whether the carer is in a position where their caring role prevents them from maintaining key relationships with family and friends or from developing new relationships where the carer does not already have other personal relationships. |
| (vi) engaging in work, training, education or volunteering | Local authorities should consider whether the carer can continue in their job, and contribute to society, apply themselves in education, volunteer to support civil society or have the opportunity to get a job, if they are not in employment. |
| (vii) making use of necessary facilities or services in the local community | Local authorities should consider whether the carer has an opportunity to make use of the local community’s services and facilities and for example consider whether the carer has time to use recreational facilities such as gyms or swimming pools. |
| (viii) engaging in recreational activities | Local authorities should consider whether the carer has leisure time, which might for example be some free time to read or engage in a hobby. |
As a consequence of that fact there is, or there is likely to be, a significant impact on the carer’s wellbeing
6.124 The third condition that must be met is that local authorities must consider whether the carer’s needs and their inability to achieve the outcomes above present a significant impact on the carer’s wellbeing. ‘Wellbeing’ is defined by referring to examples of specific areas in Section 1 of the Care Act (see chapter 1). In doing so, local authorities should consider whether:
- the carer’s needs and inability to achieve the outcomes impact on an area of the carer’s wellbeing in a significant way
- the impact on a number of the areas of wellbeing is such that they have a significant impact on an adult’s overall wellbeing
6.125 The term ‘significant’ is not defined by the Regulations, and must therefore be understood to have its everyday meaning. Local authorities will have to consider whether the carer’s needs and their inability to achieve the outcomes will have an important, consequential effect on their daily lives, their independence and their own wellbeing.
6.126 In making this judgment, local authorities should look to understand the carer’s needs in the context of what is important to them. The impact of needs may affect different carers differently, because what is important to the individual’s wellbeing may not be the same in all cases. Circumstances which create a significant impact on the wellbeing of one individual may not have the same effect on another.
6.127 When considering the type of needs a carer may have, local authorities should note that there is no hierarchy of needs or of the areas of wellbeing as described in chapter 1 of the guidance.
6.128 The following illustrates the interplay of the outcomes listed in the eligibility regulations and the wellbeing principle, which is broken down into areas of wellbeing in Chapter 1 of this guidance.
Carers’ eligibility decision process
1. Needs
The needs arise as a consequence of providing necessary care to an adult, and the carer is ‘unable’ to achieve the following:
2. Outcomes
As a result of the carer’s needs, either:
- the carer’s physical; or mental health is, or is at risk of, deteriorating
- the carer is unable to achieve any of the following outcomes:
- carrying out any caring responsibilities the carer has for a child
- providing care to other persons for whom the carer provides care
- maintaining a habitable home environment
- managing and maintaining nutrition
- developing and maintaining family or other significant personal relationships
- accessing and engaging in work, training, education or volunteering
- making use of necessary facilities or services in the local community including recreational facilities or services
- engaging in recreational activities
3. Wellbeing
As a consequence, there is or is likely to be a significant impact on the carer’s wellbeing, including:
- personal dignity (including treatment of the individual with respect)
- physical and mental health and emotional wellbeing
- protection from abuse and neglect
- control by the individual over day-to-day life (including over care and support provided and the way it is provided)
- participation in work, education, training or recreation
- social and economic wellbeing
- domestic, family and personal relationships
- suitability of living accommodation
- the individual’s contribution to society
6.129 The case studies which follow demonstrate examples of how eligibility determinations may be made. The purpose of these case studies is to illustrate eligibility on the basis of significant impact on wellbeing where the carer has needs caused by providing necessary care. Significant impact on wellbeing is personal, so although 2 people are in similar circumstances, the impact on their wellbeing is different.
Case Study 1: Deirdre (not eligible)
Deirdre is 58 and has been caring for her neighbour for the past 6 years. Deirdre has been coping with her caring responsibilities, which include checking in on her neighbour, doing her shopping and cleaning and helping her with the cooking every other day.
Deirdre works 20 hours a week at the local school, and she is also helping her daughter by picking up her grandchild after school. Deirdre’s son is concerned that she is taking on too much and notices that she is tired. Deirdre’s son persuades her to ask the local authority for a carer’s assessment.
Caring responsibilities
Neighbour with COPD.
Outcomes
Deirdre enjoys the variety that her working life and caring role provide. She would like to be able to spend more time with her grandchild in the afternoons, but recognises that there is a balance between doing this and caring for her neighbour. Deirdre’s needs impact on the following outcomes:
- carrying out caring responsibilities the carer has for a child
- engaging in recreational activities
Impact on wellbeing
Deirdre’s needs are impacting on a few outcomes.
Deirdre enjoys her caring responsibility for her grandchild and would like more free time. On the other hand, her caring roles are fulfilling so although Deirdre is tired at the end of the day, her local authority does not think her wellbeing is significantly affected.
Decision: Not Eligible
The local authority decides that Deirdre is not eligible because her wellbeing is not significantly affected.
Next actions
The local authority recognises that Deirdre could do with some advice to help her manage her day so that she can find some time for herself and so she does not get tired. They advise on how she may reduce some of her tasks such as sitting down with her neighbour to order their food shopping online rather than carrying them home. They make contact with a local carers’ organisation and the local authority makes sure Deirdre is able to access it. The organisation is able to provide additional advice.
Case study 2: Sam (eligible)
Sam is 38 and cares for his mother who has early-stage dementia. Sam’s mother has telecare, but he still checks in on her daily, and does her shopping, cooking and laundry. Sam is a divorced father of 2 children, who live with him every other week. Sam works fulltime in an IT company and has come forward for an assessment as he is starting to feel unable to cope with his various responsibilities in the weeks when he looks after his children. Sam has made an arrangement with his employer that he can work longer hours on the weeks when the children are with their mother and fewer when he has the children.
Caring responsibilitie
Mother with early stage dementia.
Outcomes
Sam wants to spend more time with his children and for instance be able to free up an hour in the afternoon to help them with their homework, so it doesn’t have to be done in the evening when the children are tired. Sam’s needs impact on the following outcomes:
- carrying out caring responsibilities the carer has for a child
- engaging in recreational activities
Impact on wellbeing
Sam’s responsibilities impact on a few important outcomes. Sam is starting to feel like he is failing as a parent and it affects the relationship he has with his children, his ex-wife, and his mother. He also worries that his ability to stay in work would be in jeopardy unless he receives support. Sam seems quite stressed and anxious.
Decision: Eligible
The local authority decides that Sam’s fluctuating needs are eligible for support, because it perceives that they have a significant impact on his wellbeing. If the local authority supports Sam to maintain his current role, everyone is better off, because Sam can stay in employment, sustain his family relationships and provide security for his mother.
Next actions
The local authority gives Sam a direct payment which he uses to pay for a care worker to come in for 3 days every other week to check on his mother and make her a meal. This gives Sam more time to spend with his children, doing homework with them and spending some more relaxed time with them.
The local authority directs Sam to a carers’ organisation which provides Sam with information about his rights at work and how to speak to his employers.
Fluctuating needs
6.130 Carers with fluctuating needs may have needs which are not apparent at the time of the assessment, but may have arisen in the past and are likely to arise again in the future. Therefore local authorities must consider an individual’s need over an appropriate period of time to ensure that all of their needs have been accounted for when the eligibility is being determined. Where fluctuating needs are apparent, this should also be factored into the care plan, detailing the steps local authorities will take to meet needs in circumstances where these fluctuate. For example, a carer could be caring for an adult with a mental illness, who has managed their condition well in the past 8 months, but who could deteriorate, if circumstances in the adult’s life change. In such situations, local authorities must consider how the carer’s needs change as a result of the fluctuation in the needs of the person they are caring for. Authorities must get a complete picture of the carer’s level of need over an appropriate period.
6.132 The level of a carer’s need can also fluctuate irrespective of whether the needs of the adult for whom they care, fluctuate. For example, if the carer is a parent of school children, they may not have the same level of need for support during term time as during school holidays.
What must local authorities do after the eligibility determination?
6.132 When the eligibility determination has been made, local authorities must provide the person to whom the determination relates (whether that is an adult with care and support needs, or a carer with support needs) with a copy of their decision.
6.133 Where the person is found to have no eligible needs, local authorities must provide information and advice on what can be done to meet or reduce the needs (for example what support might be available in the community to help the adult or carer) and what can be done to prevent or delay the development of needs in the future. Local authorities should consider how this package of information can be tailored to the needs which the person does have, with the aim of delaying deterioration and preventing future needs, and reflect the availability of local support (see also chapter 2 on preventative services and chapter 3 on information and advice).
6.134 If the adult has some eligible needs, the local authority must:
- agree with the adult which of their needs they would like the local authority to meet. The person may not wish to have support in relation to all their needs – they may, for example, intend to arrange alternative services themselves to meet some needs. Others may not wish for the local authority to meet any of their needs, but approach the authority only for the purposes of determining eligible needs
- consider how the local authority may meet those needs. This does not replace or pre-empt the care and support planning process (see chapters 10 –13), but is an early consideration of the potential support options, in order to determine whether some of those may be services for which the local authority makes a charge. Where that is the case, the local authority must carry out a financial assessment (see chapter 8).
- establish whether the person meets the ordinary residence requirement. This applies differently for adults with care and support needs and for carers. In the case of the adult, they must be ordinarily resident in the authority’s area. In the case of the carer, the person for whom they care must be ordinarily resident in the authority’s area. This is because carers’ needs are met by local authorities where the adult with the needs for care and support lives, not the authority where the carer lives. Determining ordinary residence at this stage should not lead to a delay in meeting eligible needs - more guidance on ordinary residence can be found in chapter 19
7. Independent advocacy
This chapter provides guidance on:
- Sections 67 and 68 of the Care Act 2014
- the Care and Support (Independent Advocacy) Regulations 2014
This chapter covers:
- local authorities’ responsibilities to provide independent advocacy
- matters which a local authority must consider in deciding whether an individual would experience substantial difficulty in being involved with care and support ‘process’ or safeguarding
- circumstances in which an advocate must be provided
- the role of the advocate and how independent advocates are to carry out their functions
7.1 The purpose of this section of guidance is to ensure that local authorities fully understand their duties in relation to the provision of independent advocacy and to assist them in carrying out these duties effectively.
7.2 There are duties to arrange an independent advocate for all adults, as part of their own assessment and care planning and care reviews and to those in their role as carers. It also applies to children who are approaching the transition to adult care and support, when a child’s needs assessment is carried out, and when a young carer’s assessment is undertaken.
7.3 There is also a separate duty to arrange an independent advocate for adults who are subject to a safeguarding enquiry or Safeguarding Adults Review (SAR).
7.4 Local authorities must arrange an independent advocate to facilitate the involvement of a person in their assessment, in the preparation of their care and support plan and in the review of their care plan, as well as in safeguarding enquiries and SARs if 2 conditions are met. That if an independent advocate were not provided then the person would have substantial difficulty in being fully involved in these processes and second, there is no appropriate individual available to support and represent the person’s wishes who is not paid or professionally engaged in providing care or treatment to the person or their carer. The role of the independent advocate is to support and represent the person and to facilitate their involvement in the key processes and interactions with the local authority and other organisations as required for the safeguarding enquiry or SAR.
7.5 Everyone should have access to information and advice on care and support and keeping safe from abuse or neglect (see chapters 3 and 14). Prior to making contact with the local authority, there may be some people who require independent advocacy to access that information and advice. Local authorities will need to consider such needs in ensuring that the information and advice service is accessible. Subsequently, once a person has contacted the local authority, or come to the local authority’s attention as a result of a safeguarding concern, they must be actively involved in identifying their needs through assessment, in developing their care and support plan, and in leading their care reviews, where relevant, and being involved in any safeguarding enquiry or SAR. The aim of the duty to provide advocacy is to enable people who have substantial difficulty in being involved in these processes to be supported in that involvement as fully as possible, and where necessary to be represented by an advocate who speaks on their behalf. The Equality Act 2010, requires that reasonable adjustments should be made to ensure that disabled people have equal access to information and advice services. Provision of such adjustments, information in different formats for example, may reduce or remove a substantial difficulty a person may have in being involved. The ultimate aim is for people’s wishes, feelings and needs to be at the heart of the assessment, care planning and review processes. This needs to be just as true for those who are the subject of a safeguarding enquiry or safeguarding adult review (SAR).
Advocacy and the duty to involve
7.6 Local authorities must involve people in decisions made about them and their care and support or where there is to be a safeguarding enquiry or SAR. Involvement requires the local authority helping people to understand how they can be involved, how they can contribute and take part and sometimes lead or direct the process. People should be active partners in the key care and support processes of assessment, care and support and support planning, review and any enquiries in relation to abuse or neglect. No matter how complex a person’s needs, local authorities are required to involve people, to help them express their wishes and feelings, to support them to weigh up options, and to make their own decisions.
7.7 The duty to involve applies in all settings, including for those people living in the community, in care homes or, apart from safeguarding enquiries and SARs, [footnote 24] in prisons, for example.
7.8 Local authorities must form a judgment about whether a person has substantial difficulty in being involved with these processes. If it is thought that they do, and that there is no appropriate individual to support and represent them for the purpose of facilitating their involvement, then the local authority must arrange for an independent advocate to support and represent the person.
7.9 Many of the people who qualify for advocacy under the Care Act will also qualify for advocacy under the Mental Capacity Act 2005. The same advocate can provide support as an advocate under the Care Act and under the Mental Capacity Act. This is to enable the person to receive seamless advocacy and not to have to repeat their story to different advocates. Under whichever legislation the advocate providing support is acting, they should meet the appropriate requirements for an advocate under that legislation.
Judging ‘substantial difficulty’ in being involved
7.10 Local authorities must consider for each person, whether they would have substantial difficulty in engaging with the local authority care and support processes. The Care Act defines 4 areas in any one of which a substantial difficulty might be found, which are set out below. Understanding relevant information
7.11 The first area to consider is ‘understanding relevant information’. Many people can be supported to understand relevant information, if it is presented appropriately and if time is taken to explain it. Some people, however, will not be able to understand relevant information, for example if they have mid-stage or advanced dementia.
Retaining information
7.12 The second area to consider is ‘retaining information’. If a person is unable to retain information long enough to be able to weigh up options and make decisions, then they are likely to have substantial difficulty in engaging and being involved in the process.
Using or weighing the information as part of engaging
7.13 The third area is ‘using or weighing the information as part of the process of being involved.’ A person must be able to weigh up information, in order to participate fully and express preferences for or choose between options. For example, they need to be able to weigh up the advantages and disadvantages of moving into a care home or terminating an undermining relationship. If they are unable to do this, they will have substantial difficulty in engaging and being involved in the process.
Communicating their views, wishes and feelings
7.14 The fourth area involves ‘communicating their views, wishes and feelings’. A person must be able to communicate their views, wishes and feelings whether by talking, writing, signing or any other means, to aid the decision process and to make priorities clear. If they are unable to do this, they will have substantial difficulty in engaging and being involved in the process.
7.15 For example, a person with mid-stage or advanced dementia, significant learning disabilities, a brain injury or mental ill health may be considered to have substantial difficulty in communicating their views, wishes and feelings. But equally a person with Asperger’s may be considered, as may a frail older person who does not have any diagnosis but is confused as a result of an infection, or a person who is near the end of their life and appears disengaged from involvement and decision-making. Within this context, it is the person’s ability to communicate their views, wishes and feelings which is fundamental to their involvement rather than the diagnosis or specific condition.
7.16 Both the Care Act and the Mental Capacity Act recognise the same areas of difficulty, and both require a person with these difficulties to be supported and represented, either by family or friends, or by an advocate in order to communicate their views, wishes and feelings.
Case Study
Stephen sustained a brain injury in a fall; he has completed 6 months in a specialist residential rehabilitation setting and the next step is an assessment of need for his continuing support.
Prior to this, the social worker telephones Stephen’s treating clinician who confirms that because of his brain injury, Stephen lacks insight into the effects this has had on him and he also has difficulty processing lots of information quickly – this is a common symptom of brain injury.
Therefore the social worker decides on an initial short meeting to determine Stephen’s needs and knows her first step will be to evaluate if Stephen has difficulty understanding and therefore being involved in the assessment process. If so, support could come from a carer, family member or friend or Mental Capacity Advocate, as she is aware lack of insight does not necessarily determine lack of capacity.
The social worker notes that Stephen is able to retain information about who she is and why she is meeting with him. He is articulate and can converse well about his plans for the future which includes detailed plans to meet up with friends and return to work again. However, a pre-assessment conversation with his mother, confirms that his friendship group has significantly diminished as his friends find it difficult to understand the differences in his behaviour since his fall and doubts whether he will be able to return to full-time employment. The social worker judges that because Stephen lacks insight into his personal relationships and future plans, he may well also have trouble estimating his true care and support needs. At this point the social worker decides that Stephen would have substantial difficulty in being fully involved in the rest of the assessment process and would therefore benefit from assistance.
Stephen is adamant that he wants to act and make decisions independently of his mother, though he is happy for her to inform the assessment process. The social worker decides that Stephen’s mother would not be an appropriate person under the Care Act to support his involvement in the needs assessment. The social worker talks to Stephen about how an independent advocate could help him make sure his views, beliefs, wishes and aspirations are taken into account in the assessment, and with his agreement, arranges for an independent advocate with specialist brain injury training to support him. The independent advocate meets Stephen but also talks to his mother to get a true picture of Stephen’s current needs and wishes and to ascertain the differences between how Stephen is now and prior to acquiring his brain injury. The social worker carries out the needs assessment with Stephen who is supported by his independent advocate, and with Stephen’s approval, input from his mother.
When the duty to provide independent advocacy applies
Assessment of needs
7.17 From the point of first contact, request or referral (including self-referral) for an assessment, the local authority must involve the person (see chapter 6 on Assessment). They must initially consider the best way of involving the person in the assessment processes, which is appropriate and proportionate to the person’s needs and circumstances. In some cases this may be relatively brief, in others it may consist of a series of interviews, in the person’s own home or other care settings, over a period of time.
7.18 At the start of the assessment process, if it appears to the local authority that a person has care and support or support needs, and throughout any subsequent part of the process, the local authority must judge whether a person has substantial difficulty in involvement with the assessment, the care and support planning or review processes. The identification of a potential need for advocacy may arise through the process, from the person themselves, carers or family. Where an authority has outsourced or commissioned all or some of this process, the authority will maintain overall responsibility for this judgement.
7.19 Where the local authority considers that a person has substantial difficulty in engaging with the assessment process, then they must consider whether there is anyone appropriate who can support the person be fully involved. This might for example be a carer (who is not professionally engaged or remunerated), a family member or friend. If there is no one appropriate, then the local authority must arrange for an independent advocate. The advocate must support and represent the person in the assessment, in the care and support planning, and the review. This applies to the following:
- a needs assessment under section 9 of the Care Act
- a carer’s assessment under section 10
- the preparation of a care and support plan or support plan under section 25
- a review of care and support plan or support plan under section 27
- a child’s needs assessment under section 58
- a child’s carer’s assessment under section 60 (therefore some people below 16 years of age)
- a young carer’s assessment under section 63
- safeguarding under section 68
7.20 As part of the assessment and the care and support plan, the local authority must have regard to the need to help protect people from abuse and neglect. They should assist the person to identify any risks and ways to manage them. They should also assist the person to decide how much risk they can manage. The local authority must also have regard to ensuring that any restriction on the person’s rights or freedom is kept to the minimum necessary. Restrictions should be carefully considered and frequently reviewed. Any potential deprivation of liberty must be authorised, either by a Deprivation of Liberty Authorisation by the local authority or the Court of Protection under the Deprivation of Liberty Safeguards in the Mental Capacity Act.
7.21 Where it appears that a person may be eligible for NHS Continuing Healthcare (NHS CHC), local authorities must notify the relevant NHS body. NHS CHC is a package of ongoing care that is arranged and funded solely by the NHS where the individual has complex ongoing healthcare needs of a type or quantity such that they are found to have a ‘primary health need’ as set out in the national framework for NHS Continuing Healthcare and NHS-funded nursing care. Where an individual is not eligible for NHS CHC, local authorities still have a duty to carry out an assessment of needs where a person has an appearance of needs and a duty to meet those eligible needs (see chapter 6 on assessment) and therefore have a consequential duty to consider the need for an independent advocate to support the person’s involvement in that assessment. This guidance applies equally to those people whose needs are being jointly assessed by the NHS and the local authority or where a package of support is, planned, commissioned or funded by both a local authority and a Clinical Commissioning Group (CCG), known as a joint package of care.
7.22 These processes and arrangements have historically been difficult for individuals, their carers, family or friends, to understand and be involved in. Local authorities (with CCGs) will therefore want to consider the benefits of providing access to independent advice or independent advocacy for those who do not have substantial difficulty and/or those who have an appropriate person to support their involvement. Effective joint commissioning arrangements would involve:
- dealing with the person holistically, providing a seamless service and avoiding duplication
- reducing communication break-down
- involvement of the person, family and carers
- effective partnership working for health and social care addressing needs together
- improved communication and continued care to achieve joint outcomes
7.23 Under the Mental Health Act 1983 (MHA) certain people, known as ‘qualifying patients’, are entitled to the help and support from an Independent Mental Health Advocate (IMHA). Section 117 of the MHA places a duty on the NHS and local authorities to provide aftercare and this will usually involve a joint assessment (often under the Care Programme Approach) including an assessment of the person’s care and support needs, a care and support or support plan and subsequent review (which may reach a decision that a person is no longer in need of aftercare). Those people who do not retain a right to an IMHA, whose care and support needs are being assessed, planned or reviewed should be considered for an advocate under the Care Act, if they have substantial difficulty in being involved and if there is no appropriate person to support their involvement (see paragraph 7.32).
Safeguarding enquiries and safeguarding adult reviews (SARs)
7.24 The local authority must arrange, where necessary, for an independent advocate to support and represent an adult who is the subject of a safeguarding enquiry or a safeguarding adult review. Where an independent advocate has already been arranged under s67 Care Act or under MCA 2005 then, unless inappropriate, the same advocate should be used.
7.25 Effective safeguarding is about seeking to promote an adult’s rights as well as about protecting their physical safety and taking action to prevent the occurrence or reoccurrence of abuse or neglect. It enables the adult to understand both the risk of abuse and actions that she or he can take, or ask others to take, to mitigate that risk.
7.26 There is increasing case law on adult safeguarding from the Court of Protection which advocates and practitioners should be aware.
7.27 If a safeguarding enquiry needs to start urgently then it can begin before an advocate is appointed but one must be appointed as soon as possible. All agencies need to know how the services of an advocate can be accessed and what their role is.
7.28 It is critical in this particularly sensitive area (whether an enquiry or a SAR) that the adult is supported in what may feel a daunting process which may lead to some very difficult decisions. An individual who is thought to have been abused or neglected may be so demoralised, frightened, embarrassed or upset that independent advocacy provided under section 68 to help them to be involved will be crucial.
Case Study Lynette
Lynette, who has learning disabilities, lives in a care home. A support worker contacted the local authority because another resident, Fred, has come into Lynette’s room late at night shouting on several occasions and most recently was seen pushing her. A safeguarding enquiry is started and the local authority appoint an independent advocate to support Lynette as they are concerned that she cannot express herself easily. When interviewed by the social worker Lynette cannot describe what happened. The social worker and advocate agree that the advocate will help Lynette to communicate how she feels.
The advocate spends time with Lynette. She explains what is happening and communicates with Lynette about different people that she lives with, including using photos, finding out more about her feelings. Lynette appears to be generally happy around the house and when going out, but is very distressed when she sees Fred in person, or even when she sees a picture of him. The advocate makes clear to the Local Authority what Lynette has communicated.
The local authority finds that whilst there is no doubt that Fred did what was reported, he may have done so as a result of his own confusion and distress. They agree a proposal from the registered manager of the care home that alarms will be put on Fred’s door and staffing numbers increased to prevent a recurrence. The local authority agrees to review the situation after some weeks during which time the advocate stays in contact with Lynette in order to understand the impact of this decision on Lynette. The advocate finds that Lynette remains distressed by Fred’s presence. She is concerned that the measures in place are not sufficient and writes this in a report to the local authority detailing what Lynette has communicated about where she lives and about Fred. The local authority agrees to look at what further action may be needed which might include considering whether Lynette and Fred should continue to share accommodation.
The main aspect of wellbeing promoted is protection from abuse and neglect, but also personal dignity and emotional wellbeing. The local authority has also demonstrated its regard for Lynette’s views, wishes, feelings and beliefs.
Continuity of care and ordinary residence
7.29 The local authority which is carrying out the assessment, planning or review of the plan is responsible for considering whether an advocate is required. In the case of a person who is receiving care and support from one local authority and decides to move and live in another authority, the responsibility will move with the care and support assessment (see chapter 20). For a person whose care and support is being provided out of area (in a type of accommodation set out in the section on ordinary residence (see chapter 19) it will be the authority in which the person is ordinarily resident. Understanding of local communities may be an important consideration, so the advocacy/advocate should wherever possible be from the area where the person is resident at the time of the assessment, planning or review.
Consequences for local authorities
The local authority should have local policies to clarify the appointing of advocates:
- from advocacy services out of their area that they may not have a direct commissioning relationship with (as it currently is with Independent Mental Capacity Advocate (IMCA))
- for people placed out of area temporarily
- for people who move from one area to another following an assessment and care and support planning in which an advocate is involved (the same advocate should be involved wherever practicable)
Care and support reviews
7.30 The local authority must involve the person, their carer and any other individual that the person wants to be involved in any review of their care and support plan, and take all reasonable steps to agree any changes (see chapter 13).
7.31 Local authorities must consider whether an advocate is required to facilitate the person’s involvement in the review of a care and support plan and, if appropriate, appoint an advocate. This applies regardless of whether an advocate was involved at an earlier stage. Examples of when an advocate may be appointed at this stage despite not previously being involved include:
- the person’s ability to be involved in the process without an advocate has changed
- the circumstances have changed (for example, the person’s involvement was previously facilitated by a relative who is no longer able to perform that role)
- an advocate should have been involved at the care and support planning stage and was not
- the requirement to involve an advocate at the care and support planning stage did not exist at that time
Judgements made by the local authority
An appropriate individual to facilitate the person’s involvement
7.32 Local authorities must consider whether there is an appropriate individual (or individuals) who can facilitate a person’s involvement in the assessment, planning or review processes, and this includes 3 specific considerations.
7.33 First, it cannot be someone who is already providing the person with care or treatment in a professional capacity or on a paid basis (regardless of who employs or pays for them). That means it cannot be, for example, the person’s GP, nurse, key worker or care and support worker.
Case study: Janice
Janice is 43 and cares for her mother Sheena who is 72 who has advanced Parkinson’s and increasing cognitive and communication difficulties. Janice cares for her mother in excess of 40 hours per week. Janice gave up work to care for her mother 5 years ago, and using her direct payment Sheena pays her daughter for 8 hours per week for care and support, including helping her with personal care, cooking meals and grocery shopping. Sheena preferred this to paying someone else – she prefers not to have strangers in the house and finds that others often do not understand her needs. As Janice is caring for her mother for many more hours than this, Janice has received a carers assessment and receives her own carers personal budget which she uses for breaks such as her weekly aerobics class which she finds helps her keep in touch with her friends, stay healthy, and deal with stress.
There is no-one else available to act as an appropriate individual to support Sheena in decision making. Both Sheena and Janice would be happy for Janice to take on this role. However, as Janice received a payment, she would not be regarded as an appropriate individual, though the guidance states that good practice should ensure Janice’s views are sought as Sheena has made clear that she wishes this to happen.
7.34 Second the person’s wish not to be supported by that individual should be respected. Where a person does not wish to be supported by a relative, for example, perhaps because they wish to be moving towards independence from their family, then the local authority cannot consider the relative appropriate. The person’s wish not to be supported by that individual should be respected and if the person has capacity, or is competent to consent, the person’s wishes must be followed. If the person has been judged to lack the capacity to make a decision, then the local authority must be satisfied that it is in a person’s best interests to be supported and represented by the individual.
Case study
If the person already has an advocate, whose role so far has been to support the person on matters not under the Care Act, who is able and willing to facilitate their involvement in the assessment, planning and review processes then they may be an appropriate individual to support the person’s involvement and represent them. They would be acting as an appropriate person rather than an independent advocate under the Care Act. If, however, that advocate fulfils the requirements for an independent advocate under the Care Act then they can be appointed as such.
Additionally, if an advocate is required under the Mental Capacity Act, and the local authority is going to appoint the same person to be that advocate, then the instruction, appointment and qualification of the advocate must also meet the requirements of the Mental Capacity Act.
7.35 Third, the appropriate individual is expected to support and represent the person and to facilitate their involvement in the processes. It is unlikely that some people will be able to fulfil this role easily, for instance a family member who lives at a distance and who only has occasional contact with the person, a spouse who also finds it difficult to understand the local authority processes, a friend who expresses strong opinions of her own prior to finding out those of the individual concerned, or a housebound parent. It is not sufficient to know the person well or to love them deeply; the role of the appropriate individual is to support the person’s active involvement with the local authority processes (see chapter 6).
Case study: Jacinta
Jacinta is 26 and lives with her mother and father. She has 2 siblings aged 28 and 23 who have left the family home. Jacinta would also like to move to living more independently. Jacinta has moderate learning disabilities and finds it hard to retain information. Jacinta’s parents are very worried that she won’t be able to cope living in her own home and are against her doing so. In these circumstances Jacinta’s parents would not be ‘an appropriate person’ who could effectively represent and support her involvement.
Case study: Brian
Brian is 84 and has advancing dementia. He lives alone in the house he owns. Brian has very limited mobility, has frequent falls and has difficulty in remembering to take medication and to eat. He has periods when he is confused and weighing up the longer term advantages and disadvantages of this care and support options, but has been judged to retain ‘capacity’ Brian says he feels very lonely. Social services are already providing some domiciliary care for which Brian is charged. The local authority is reviewing Brian’s care plan. Brian’s daughter and son in law who have had little contact with Brian over the past few years and will inherit the house are adamant that he can cope at home and does not need to go into a care home. In these circumstances, in addition to a lack of recent contact, there could be a conflict of interests and Brian’s relatives would not be ‘an appropriate person’.
7.36 It will clearly not be suitable for a person to be regarded as an appropriate individual where they are implicated in any enquiry of abuse or neglect or have been judged by a SAR to have failed to prevent an abuse or neglect.
7.37 Sometimes the local authority will not know at the point of first contact or at an early stage of the assessment whether there is someone appropriate to assist the person in engaging. They may need to appoint an advocate, and find later that there is an appropriate person in the person’s own network. The advocate can at that stage ‘hand over’ to the appropriate person. Alternatively, the local authority may agree with the individual, the appropriate person and the advocate that it would be beneficial for the advocate to continue their role, though this is not a specific requirement under the legislation. Equally, it is possible that the local authority will consider someone appropriate who may then turn out to have difficulties in supporting the person to engage and be involved in the process. The local authority must at that point arrange for an advocate.
7.38 There may also be some cases where the local authority considers that a person needs the support of both a family member and an advocate; perhaps because the family member can provide a lot of information but not enough support, or because while there is a close relationship, there may be a conflict of interest with the relative, for example in relation to inheritance of the home.
7.39 If the local authority decides that they are required to appoint an independent advocate as the person does not have friends or family who can facilitate their involvement, the local authority must still consult with those friends or family members when the person asks them to (see chapter 6 on assessment).
7.40 It is the local authority’s decision as to whether a family member or friend can act as an appropriate person to facilitate the individual’s involvement. It is the local authority’s responsibility to communicate this decision to the individual’s friends and family where this may have been in question and whenever appropriate. The overall aim should be for people who need advocacy to be identified and when relevant, receive consistent support as early as possible and throughout the assessment, the care and support planning and the review processes.
7.41 The local authority may be carrying out assessments of 2 people in the same household. If both people agree to have the same advocate, and if the local authority consider there is no conflict of interest between the individuals or either of the individuals and the advocate, then the same advocate may support and represent the 2 people. For example, if they both wish to be supported to live together in their own home, then it may make sense for one advocate to support both. But where for example one wishes for the other to be moved away, there may be a conflict of interest and 2 advocates will be needed. If any of the people involved – the people being assessed or taking part in care and support or support planning or the advocate – consider that it would be better to have different advocates, then separate advocates should be provided.
The exceptions: provision of an advocate even where they have family or others who can facilitate the person’s involvement.
7.42 In general, a person who has substantial difficulty in being involved in their assessment, plan and review, will only become eligible for an advocate where there is no one appropriate to support their involvement. The exceptions are:
- where the exercising of the assessment or planning function might result in placement in NHS-funded provision in either a hospital for a period exceeding 4 weeks or in a care home for a period of 8 weeks or more and the local authority believes that it would be in the best interests of the individual to arrange an advocate
- where there is a disagreement, relating to the individual, between the local authority and the appropriate person whose role it would be to facilitate the individual’s involvement, and the local authority and the appropriate person agree that the involvement of an independent advocate would be beneficial to the individual
Who can act as an advocate?
7.43 Advocates must have:
A suitable level of appropriate experience
This may, for example, be in non-instructed advocacy or in working with those groups of people who may have substantial difficulty in engaging with assessments and care and support planning
Appropriate training
This may, for example, initially be training in advocacy (non-instructed and instructed) or dementia, or working with people with learning disabilities. Once appointed, all independent advocates should be expected to work towards the National Qualification in Independent Advocacy (level 3) within a year of being appointed, and to achieve it in a reasonable amount of time
Competency in the task
This will require the advocacy organisation assuring itself that the advocates who work for it are all competent and have regular training and assessment
Integrity and good character
This might be assessed through: interview and selection processes; seeking and scrutinising references prior to employment and on-going DBS checks [footnote 25]
The ability to work independently of the local authority or body carrying out assessments, planning or
reviews on the local authority’s behalf
This would include the ability to make a judgement about what a person is communicating and what is in a person’s best interests, as opposed to in a local authority’s best interests, and to act accordingly to represent this
Arrangements for regular supervision
This will require that the person meets regularly and sufficiently frequently with a person with a good understanding of independent advocacy who is able to guide their practice and develop their competence
7.44 The third updated version on the Advocacy Quality Performance Mark (QPM) was published on 3 April 2014 by the National Development Team for Inclusion (NDTi). The QPM is a tool for providers of independent advocacy to show their commitment and ability to provide high quality advocacy services - essential for people to have their voices heard, to exercise choice and control and to live independently.
7.45 To prevent potential conflict of interest, the independent advocate must not be working for the local authority, or for an organisation that is commissioned to carry out assessments, care and support plans or reviews for the local authority unless the potential conflict of interests is adequately addressed within the organisation’s structure (for example a different group within a company or through an effective ‘firewall’, as in the banking industry). In certain circumstances, in addition to their role under the Care Act, an advocate may assist an individual to develop their own care or support plan if requested to by the individual, but they cannot be the person to authorise the support plan or to approve care and support plans or reviews on behalf of the authority. Nor can an advocate be appointed if they are providing care or treatment to the individual in a professional or a paid capacity.
The role of the independent advocate
7.46 It is intended that advocates will decide the best way of supporting and representing the person they are advocating for, always with regard to the wellbeing and interest (including their views, beliefs and wishes) of the person concerned. This may involve creative approaches, for example, supporting someone to show film to help explain their needs, wishes or preferences.
Case study: Kate
Kate has profound and multiple learning disabilities. She doesn’t use formal communication such as words or signs. She communicates using body language and facial expressions. In her assessment, Kate’s independent advocate supports her to show some film of her visiting a local market, enjoying the colours and sounds around her. In this way, Kate is able to show the assessor some of the things that are important to her.
7.47 In addition, where practicable, they are expected to meet the person in private. Where a person has capacity, the advocate should ask and obtain their written consent to look at their records and to talk to their carer, family, friends, care or support worker and others who can provide information about their needs and wishes, their beliefs and values. Where a person does not have capacity to decide whether an advocate should look at their relevant records or talk to their family and friends, then the advocate should consult the records and the family and others as appropriate, but consulting the family and others only where the advocate considers this is in the person’s best interests. The Care Act allows advocates to examine and take copies of relevant records in certain circumstances. This mirrors the powers of an Independent Mental Capacity Advocate.
7.48 Acting as an advocate for a person who has substantial difficulty in engaging with care and support or safeguarding processes is a responsible position. It includes:
- assisting a person to understand the assessment, care and support planning and review and safeguarding processes. This requires advocates to understand local authority policies, and other agencies roles, and processes, the available assessment tools, the planning options, and the options available at the review of a care or support plan are required and good practice in safeguarding enquiries and SARs. It may involve advocates spending considerable time with the individual, considering their communications needs, their wishes and feelings and their life story, and using all this to assist the person to be involved and where possible to make decisions
- assisting a person to communicate their views, wishes and feelings to the staff who are carrying out an assessment or developing a care or support plan or reviewing an existing plan or to communicate their views, wishes and feelings to the staff who are carrying out safeguarding enquiries or reviews
- assisting a person to understand how their needs can be met by the local authority or otherwise – understanding for example how a care and support and support plan can be personalised, how it can be tailored to meet specific needs, how it can be creative, inclusive, and how it can be used to promote a person’s rights to liberty and to family life
- assisting the person to make decisions about their care and support arrangements – assisting them to weigh up various care and support options and to choose the ones that best meet the person’s needs and wishes.
- assisting the person to understand their rights under the Care Act – for an assessment which considers their wishes and feelings and which considers the views of other people; their right to have their eligible needs met, and to have a care or support plan that reflects their needs and their preferences, and in relation to safeguarding, understanding their right to have their concerns about abuse taken seriously and responded to appropriately. Also assisting the person to understand their wider rights, including their rights to liberty and family life. A person’s rights are complemented by the local authority’s duties, for example to involve the person, to meet needs in a way that is least restrictive of a person’s rights
- assisting a person to challenge a decision or process made by the local authority; and where a person cannot challenge the decision even with assistance, then to challenge it on their behalf
7.49 In terms of safeguarding there are some particular important issues for advocates to address. These include assisting a person to:
- decide what outcomes/changes they want
- understand the behaviour of others that are abusive /neglectful
- understand which actions of their own may expose them to avoidable abuse or neglect
- understand what actions that they can take to safeguard themselves
- understand what advice and help they can expect from others, including the criminal justice system
- understand what parts of the process are completely or partially within their control
- explain what help they want to avoid reoccurrence and also recover from the experience
Representing
7.50 There will be times when an advocate will have concerns about how the local authority has acted or what decision has been made or what outcome is proposed. The advocate must write a report outlining their concerns for the local authority. The local authority should convene a meeting with the advocate to consider the concerns and provide a written response to the advocate following the meeting.
7.51 Where the individual does not have capacity, or is not otherwise able, to challenge a decision, the advocate must challenge any decision where they believe the decision is inconsistent with the local authority’s duty to promote the individual’s wellbeing.
7.52 Where a person has been assisted and supported and nevertheless remains unable to make their own representations or their own decisions, the independent advocate must use what information they have collected and found, and make the representations on behalf of the person. They must ‘advocate’ on their behalf, to put their case, to scrutinise the options, to question the plans if they do not appear to meet all eligible needs or do not meet them in a way that fits with the person’s wishes and feelings, or are not the least restrictive of the person’s life, and to challenge local authority decisions where necessary. The ultimate goal of this representation is to secure a person’s rights, promote the individual’s well-being and ensure that their wishes are taken fully into account.
The role of the local authority in supporting the advocate
7.53 The local authority is expected to recognise that an advocate’s duty is to support and represent a person who has substantial difficulty in engaging with the local authority processes. The local authority must take into account any representations made by an advocate. The local authority must provide a written response to a report from an advocate which outlines concerns about how the local authority has acted or what decision has been made or what outcome is proposed. The local authority should understand that the advocate’s role incorporates ‘challenge’ on behalf of the individual.
7.54 The local authority is responsible for ensuring that the relevant people who work for the authority are aware of the advocacy service and the authority’s duty to provide such services (see chapter 3 on information and advice). It may engage with advocates to support this awareness raising.
7.55 The local authority should consider including the identification and referral of those people likely to benefit from independent advocacy (during assessment, care and support planning, review and safeguarding) through the care and support services they may commission. In doing so, the local authority should engage with domiciliary and residential care and support workers and agencies.
7.56 The local authority should take reasonable steps to assist the advocate in carrying out their role. For example, they should let other agencies know that an advocate is supporting a person, facilitating access to the person and to the records [footnote 26], they should propose a reasonable timetable for the assessment and the care and support plan (taking into consideration the needs of the person), and where the advocate wishes to consult family, friends or paid staff, the timetable should allow this. They should keep the advocate informed of any developments and of the outcome of the assessment and the care and support plan.
7.57 The local authority may make reasonable requests of the advocate for information or for meetings both in relation to particular individuals and in relation to the advocate’s work more generally, and the independent advocate should comply with these.
7.58 The local authority must meet its duties in relation to working with an Independent Mental Capacity Advocate (IMCA) provided under the Mental Capacity Act as well as those in relation to an advocate under the Care Act when the advocate is acting in both roles. These duties have been closely aligned so as to facilitate this.
Availability of advocacy services to people in the area
7.59 All local authorities must ensure that there is sufficient provision of independent advocacy to meet their obligations under the Care Act. There should be sufficient independent advocates available for all people who qualify, and it will be unlawful not to provide someone who qualifies with an advocate (see also chapter 4).
7.60 Advocacy should be seamless for people who qualify, so that they can benefit from the support of one advocate for their whole experience of care or safeguarding work. It rarely makes sense to have one advocate for assessment and another for care and support planning; the 2 are interrelated, and people who have substantial difficulty in engaging should not be expected to have to tell their story repeatedly to different advocates.
7.61 The Local Government and Public Involvement in Health Act 2007 (as amended by the Health and Social Care Act 2012), provides that local authorities are under a duty to work with their local CCGs, and other partners through the Health and Wellbeing Board to undertake Joint Strategic Needs Assessments for their areas and to develop Joint Health and wellbeing Strategies. Statutory Guidance, published in March 2013 makes clear that the Joint Strategic Needs Assessment and Joint Health and Wellbeing Strategies must be published, and have specific regard to: ‘what health and social care information the community needs, including how they access it and what support they may need to understand it’.
7.62 Local authorities should be aware of and build on the current availability of independent advocacy services in its local area.
7.63 Independent advocacy under the duty flowing from the Care Act is similar in many ways to independent advocacy under the Mental Capacity Act (MCA). Regulations have been designed to enable independent advocates to be able to carry out both roles. For both:
- the independent advocate’s role is to support and represent people
- the independent advocate’s role is primarily to work with people who do not have anyone appropriate to support and represent them
- the independent advocates require a similar skill set
- regulations about the appointment and training of advocates are similar
- local authorities are under a duty to consider representations made by both independent advocates
- independent advocates will need to be well known and accessible
- independent advocates may challenge local authority decisions
- people who qualify for an Independent Mental Capacity Advocate (an IMCA) in relation to the care planning and care review – as that planning may result in an eligible change of accommodation decision – will (in nearly all cases) also qualify for independent advocacy under the Care Act. The provisions of the Care Act are however wider and apply to care planning irrespective of whether it may result in a change of accommodation decision. People for whom there is a power to instruct an IMCA in relation to care review will (in nearly all cases) also qualify for independent advocacy under the Care Act. The Care Act however creates a duty rather than a power in relation to advocacy and care reviews
7.64 However, the duty to provide independent advocacy under the Care Act is broader and provides support to:
- people who have capacity but who have substantial difficulty in being involved in the care and support ‘processes’
- people in relation to their assessment and/or care and support planning regardless of whether a change of accommodation is being considered for the person
- people in relation to the review of a care and/or support plan
- people in relation to safeguarding processes (though IMCAs may be involved if the authority has exercised its discretionary power under the MCA and appointed an IMCA if protective measures are being proposed for a person who lacks capacity, at the time to make the relevant decisions or understand their consequences)
- carers who have substantial difficulty in engaging – whether or not they have capacity
- people for whom there is someone who is appropriate to consult for the purpose of best interests decisions under the Mental Capacity Act, but who is not able and/or willing to facilitate the person’s involvement in the local authority process
- adults who are subject to a safeguarding enquiry or SAR
7.65 Frequently a person will be entitled to an advocate under the Care Act and then, as the process continues it will be identified that there is a duty to provide an advocate (IMCA) under the Mental Capacity Act. This will occur for example when during the process of assessment or care and support planning it is identified that a decision needs to be taken about the person’s long-term accommodation. It would be unhelpful to the individual and to the local authority for a new advocate to be appointed at that stage. It would be better that the advocate who is appointed in the first instance is qualified to act under the Mental Capacity Act (as IMCAs) and the Care Act and that the commissioning arrangements enable this to occur.
7.66 Local authorities do not have to commission one organisation to provide all types of statutory and non-statutory advocacy. But there may be advantages of working with one organisation or working through one liaison point for a consortium of advocacy providers:
- it is better for the person receiving the support
- it is easier for those carrying out assessment and care planning to work with one advocate per individual rather than two
- it is easier for the local authority to manage and monitor one contract rather than 2
Charging and financial assessment
This section includes chapters:
8. Charging and financial assessment
This chapter provides guidance on:
- Sections 14, 17 and 69-70 of the Care Act 2014
- the Care and Support (Charging and Assessment of Resources) Regulations 2014
- the Care and Support and Aftercare (Choice of Accommodation) Regulations 2014
This chapter covers:
- common issues for charging
- charging for care and support in a care home
- choice of accommodation when arranging care in a residential setting
- making additional payments for preferred accommodation
- charging for home care and support in a person’s own home
- charging for support to carers
- requesting local authority support to meet eligible needs
This chapter must be read in conjunction with Annexes A to F, which provide further technical and detailed information.
8.1 The Care Act provides a single legal framework for charging for care and support under sections 14 and 17. It enables a local authority to decide whether or not to charge a person when it is arranging to meet a person’s care and support needs or a carer’s support needs.
8.2 Where a local authority arranges care and support to meet a person’s needs, it may charge the adult, except where the local authority is required to arrange care and support free of charge. The new framework is intended to make charging fairer and more clearly understood by everyone. The overarching principle is that people should only be required to pay what they can afford. People will be entitled to financial support based on a means-test and some will be entitled to free care. The framework is therefore based on the following principles that local authorities should take into account when making decisions on charging. The principles are that the approach to charging for care and support needs should:
- ensure that people are not charged more than it is reasonably practicable for them to pay
- be comprehensive, to reduce variation in the way people are assessed and charged
- be clear and transparent, so people know what they will be charged
- promote wellbeing, social inclusion, and support the vision of personalisation, independence, choice and control
- support carers to look after their own health and wellbeing and to care effectively and safely
- be person-focused, reflecting the variety of care and caring journeys and the variety of options available to meet their needs
- apply the charging rules equally so those with similar needs or services are treated the same and minimise anomalies between different care settings
- encourage and enable those who wish to stay in or take up employment, education or training or plan for the future costs of meeting their needs to do so
- be sustainable for local authorities in the long-term
8.3 Alongside this, local authorities should ensure there is sufficient information and advice available in a suitable format for the person’s needs, in line with the Equality Act 2010 (in particular for those with a sensory impairment, with learning disabilities or for whom English is not their first language), to ensure that they or their representative are able to understand any contributions they are asked to make. Local authorities should also make the person or their representative aware of the availability of independent financial information and advice.
Common issues for charging
8.4 Local authorities have a duty to arrange care and support for those with eligible needs, and a power to meet both eligible and non-eligible needs. In all cases, a local authority has the discretion to choose whether or not to charge under section 14 of the Care Act following a person’s needs assessment. Where it decides to charge, it must follow the Care and Support (Charging and Assessment of Resources) regulations and have regard to the guidance. The detail of how to charge is different depending on whether someone is receiving care in a care home, or their own home, or another setting. However, they share some common elements, which are set out in the following section.
8.5 The different approaches exist to reflect that the delivery model for care homes is relatively uniform across the country and it is therefore sensible to provide a single model for charging purposes. However, other models of care generally see a greater variety of approaches and innovation that we wish to continue.
8.6 Where a local authority chooses to charge, regulations determine the maximum amount a local authority can charge a person.
8.7 Only in care homes, where the financial assessment identifies that a person’s resources exceed the capital limits, is a local authority precluded from paying towards the costs of care. Therefore, local authorities should develop and maintain a policy setting out how they will charge people in settings other than care homes. In deciding what it is reasonable to charge, local authorities must ensure that they do not charge more than is permitted under the regulations and as set out in this guidance.
8.8 The subsequent guidance and the supporting annexes assume that the appropriate assessment of needs has been carried out and the local authority has chosen to charge. It therefore provides detail on how to conduct the financial assessment for that person. The local authority has no power to assess couples or civil partners according to their joint resources. Each person must therefore be treated individually. (For further guidance on assessment of needs see Chapter 6.)
8.9 Where a person lacks capacity, they may still be assessed as being able to contribute towards the cost of their care. However, a local authority must put in place policies regarding how they communicate, how they carry out financial assessments and how they collect any debts that take into consideration the capacity of the person as well as any illness or condition. Local authorities are expected to use their social work skills both to communicate with people and also to design a system that works with, and for, very vulnerable people. Sometimes it is useful to consult with and engage with family members; however, family members may not have the legal right to access the person’s bank accounts. Where possible, local authorities should work with someone who has the legal authority to make financial decisions on behalf of a person who lacks capacity. If there is no such person, then an approach to the Court of Protection is required.
8.10 The charging rules also apply equally to people in prison. Whilst prisoners have restricted access to paid employment and benefits (and earnings in prison are to be disregarded for the purposes of the financial assessments), any capital assets, savings and pensions will need specific consideration as set out in this chapter and relevant annexes. (For more information on prisons and approved premises see Chapter 17).
Capital limits
8.11 The financial limit, known as the ‘upper capital limit’, exists for the purposes of the financial assessment. This sets out at what point a person is entitled to access local authority support to meet their eligible needs. Full detail is set out in Annex B, and the local authority must read that guidance before undertaking a financial assessment.
8.12 The upper capital limit is currently set at £23,250. Below this level, a person can seek means-tested support from the local authority. This means that the local authority will undertake a financial assessment of the person’s assets and will make a charge based on what the person can afford to pay. In the financial assessment capital below the lower capital limit – currently set at £14,250 – is not taken into account in the assessment of what a person can pay in tariff income assessed against their capital. Where a person’s resources are below the lower capital limit of £14,250 they will not need to contribute to the cost of their care and support from their capital. However, for adults receiving care and support in locations other than in a care home the limits of £23,250 and £14,250 are simply minimums and local authorities have discretion to set their own higher capital limits if they wish, provided they are no lower than £23,250 for the upper limit and £14,250 for the lower limit.
8.13 A person with more in capital than the upper capital limit can ask their local authority to arrange their care and support for them. Where the person’s needs are to be met by care in a care home, the local authority may choose to meet those needs and arrange the care, but is not required to do so. In other cases, the authority must meet the eligible needs if requested. However, these people are not entitled to receive any financial assistance from their local authority and in any case, may pay the full cost of their care and support until their capital falls below the upper capital limit.
8.14 The local authority must not charge for certain types of care and support which must be arranged free.
These are:
- intermediate care, including reablement, which must be provided free of charge for up to 6 weeks. However, local authorities must have regard to the guidance on preventative support set out in Chapter 2. This sets out that neither should have a strict time limit but should reflect the needs of the person. Local authorities therefore may wish to apply their discretion to offer this free of charge for longer than 6 weeks where there are clear preventative benefits, such as when a person has recently become visually impaired
- community equipment (aids and minor adaptations). Aids must be provided free of charge whether provided to meet or prevent/delay needs. A minor adaptation is one costing £1,000 or less
- care and support provided to people with Creutzfeldt-Jacob Disease
- after-care services/support provided under section 117 of the Mental Health Act 1983
- any service or part of service which the NHS is under a duty to provide. This includes Continuing Healthcare and the NHS contribution to Registered Nursing Care
- more broadly, any services which a local authority is under a duty to provide through other legislation may not be charged for under the Care Act 2014
- assessment of needs and care planning may also not be charged for, since these processes do not constitute ‘meeting needs’
Carrying out a financial assessment
8.15 The legal framework for charging is set out in Sections 14 and 17 of the Care Act. When choosing to charge, a local authority must not charge more than the cost that it incurs in meeting the assessed needs of the person. It also cannot recover any administration fee relating to arranging that care and support. The only exception is in the case of a person with eligible needs and assets above the upper capital limit who has asked the local authority to arrange their care and support on their behalf. In such cases, the local authority may apply an administration fee to cover its costs. However, (see paragraphs 8.55 to 8.60 below) this must not be higher than the cost the local authority has incurred in arranging that care and support. This approach must also apply if the local authority has involved other organisations to deliver its duties in any way.
8.16 Where a local authority has decided to charge, except where a light touch assessment is permissible (see paragraph 8.22 below), it must carry out a financial assessment of what the person can afford to pay and, once complete, it must give a written record of that assessment to the person. This could be provided alongside a person’s care and support plan or separately, including via online means. It should explain how the assessment has been carried out, what the charge will be and how often it will be made, and if there is any fluctuation in charges, the reason. The local authority should ensure that this is provided in a manner that the person can easily understand, in line with its duties on providing information and advice.
8.17 In carrying out the assessment, the local authority must have regard to the detailed guidance set out in Annexes B and C that set out how both capital and income should be treated. A local authority must regularly reassess a person’s ability to meet the cost of any charges to take account of any changes to their resources. This is likely to be on an annual basis, but may vary according to individual circumstances. However, this should take place if there is a change in circumstance or at the request of the person.
8.18 At the time of the assessment of care and support needs, the local authority must establish whether the person has the capacity to take part in the assessment. If the person lacks capacity, the local authority must find out if the person has any of the following as the appropriate person will need to be involved:
- enduring power of attorney (EPA)
- lasting power of attorney (LPA) for property and affairs
- lasting power of attorney (LPA) for health and welfare
- property and affairs deputyship under the Court of Protection
- any other person dealing with that person’s affairs (for example, someone who has been given appointeeship by the Department for Work and Pensions (DWP) for the purpose of benefits payments)
8.19 People who lack capacity to give consent to a financial assessment and who do not have any of the above people with authority to be involved in their affairs, may require the appointment of a property and affairs deputyship. Family members can apply for this to the Court of Protection or the local authority can apply if there is no family involved in the care of the person. While this takes some weeks, it then enables the person appointed to access information about bank accounts and financial affairs. A person with dementia for example should not be ‘forced’ to undertake a financial assessment, to sign documents they can no longer understand and should not be punished for any incomplete information that is elicited from them. The local authority should be working with an EPA, a LPA or a deputy instead.
8.20 In the financial assessment, the person’s capital is taken into account unless it is subject to one of the disregards set out in Schedule 2 to the regulations and described in Annex B. The main examples of capital are property and savings. Where the person receiving care and support has capital at or below the upper capital limit (currently £23,250), but more than the lower capital limit (currently £14,250), they may be charged £1 per week for every £250 in capital between the 2 amounts. This is called ‘tariff income’. For example, if a person has £4,000 above the lower capital limit, they are charged a tariff income of £16 per week.
8.21 In assessing what a person can afford to pay, a local authority must take into account their income. However, to help encourage people to remain in or take up employment, with the benefits this has for a person’s well-being, earnings from current employment must be disregarded when working out how much they can pay. There are different approaches to how income is treated depending on whether a person is in a care home or receiving care and support in their own home. Full details are set out in Annex C on the treatment of income in care homes and other settings.
8.21a) As part of the Armed Forces Covenant, the government has committed to making sure veterans are not disadvantaged by their service and when appropriate receive special consideration. To support veterans injured on active service, payments to veterans under the War Pension Scheme, with the exception of Constant Attendance Allowance which is specifically intended to pay for care, must be disregarded in the assessment of what a veteran can pay for care from 10 April 2017. This brings payments to veterans under the War Pension Scheme into line with Guaranteed Income Payments under the Armed Forces Compensation Scheme which have been disregarded since October 2012.
‘Light-touch’ financial assessments
8.22 In some circumstances, a local authority may choose to treat a person as if a financial assessment had been carried out. In order to do so, the local authority must be satisfied on the basis of evidence provided by the person that they can afford, and will continue to be able to afford, any charges due. This is known as a ‘light-touch’ financial assessment.
8.23 The main circumstances in which a local authority may consider carrying out a light-touch financial assessment are:
- a) Where a person has significant financial resources, and does not wish to undergo a full financial assessment for personal reasons, but wishes nonetheless to access local authority support in meeting their needs. In these situations the local authority may accept other evidence in lieu of carrying out the financial assessment and consider the person to have financial resources above the upper limit.
- b) Where the local authority charges a small or nominal amount for a particular service (for example, for subsidised services) which a person is clearly able to meet and would clearly have the relevant minimum income left, and carrying out a financial assessment would be disproportionate.
- c) When an individual is in receipt of benefits which demonstrate that they would not be able to contribute towards their care and support costs. This might include income from Jobseeker’s Allowance.
8.24 Ways a local authority may be satisfied that a person is able to afford any charges due might include evidence that a person has either:
- a) property clearly worth more than the upper capital limit, where they are the sole owner or it is clear what their share is
- b) savings clearly worth more than the upper capital limit
- c) sufficient income left following the charge due
8.25 Where the local authority is going to meet the person’s needs, and it proposes to undertake a light-touch financial assessment, it should take steps to assure itself that the person concerned is willing, and will continue to be willing, to pay all charges due. It must also remember that it is responsible for ensuring that people are not charged more than it is reasonable for them to pay. Where a person does not agree to the charges that they have been assessed as being able to afford to pay under this route, a full financial assessment may be needed.
8.26 When deciding whether or not to undertake a light-touch financial assessment, a local authority should consider both the level of the charge it proposes to make, as well as the evidence or other certification the person is able to provide. They must also inform the person when a light-touch assessment has taken place and make clear that the person has the right to request a full financial assessment should they so wish, as well as making sure they have access to sufficient information and advice, including the option of independent financial information and advice.
Deprivation of assets and debts
8.27 People with care and support needs are free to spend their income and assets as they see fit, including making gifts to friends and family. This is important for promoting their wellbeing and enabling them to live fulfilling and independent lives. However, it is also important that people pay their fair contribution towards their care and support costs.
8.28 There are some cases where a person may have tried to deliberately avoid paying for care and support costs through depriving themselves of assets – either capital or income. Where a local authority believes they have evidence to support this, it must read Annex E concerning the deprivation of assets. In such cases, the local authority may either charge the person as if they still possessed the asset or, if the asset has been transferred to someone else, seek to recover the lost income from charges from that person. However, the local authority cannot recover more than the person gained from the transfer.
8.29 Where a person has accrued a debt, the local authority may use its powers under the Care Act to recover that debt. In deciding how to proceed, the local authority should consider the circumstances of the case before deciding a course of action. For example, a local authority should consider whether this was a deliberate avoidance of payment or due to circumstances beyond the person’s control.
8.30 Ultimately, the local authority may institute County Court proceedings to recover the debt. However, they should only use this power after other reasonable alternatives for recovering the debt have been exhausted. Further details on how to pursue debts are set out in Annex D.
Charging for care and support in a care home
8.31 This section must be read in conjunction with Annex B on the treatment of capital and Annex C on the treatment of income in care homes.
8.32 Where a local authority has decided to charge and undertaken the financial assessment, it should support the person to identify options of how best to pay any charge. This may include offering the person a deferred payment agreement. In such cases, chapter 9 of the guidance must be considered.
8.33 Where a local authority is meeting needs by arranging a care home, it is responsible for contracting with the provider. It is also responsible for paying the full amount, including where a ‘top-up’ fee is being paid. However, where all parties are agreed it may choose to allow the person to pay the provider directly for the ‘top-up’ where this is permitted. In doing so it should remember that multiple contracts risk confusion and that the local authority may be unable to assure itself that it is meeting its responsibilities under the additional cost provisions in the Care Act. Local authorities must ensure they read the guidance at Annex A on the use of ‘top-up’ fees.
8.34 Where a person is a short-term or temporary resident there is a degree of discretion or modified charging rules to take account of this.
-
A short-term resident is someone provided with accommodation in a care home for a period not exceeding 8 weeks, for example where a person is placed in a care home to provide respite care. Where a person is a short-term resident a local authority may choose to assess and charge them based on the rules for care or support arranged other than in a care home.
-
A temporary resident is someone whose stay in a care home is unlikely to exceed 52 weeks or, in exceptional circumstances, is unlikely to substantially exceed 52 weeks. Because a temporary resident is expected to return home their main or only home is usually disregarded in the assessment of whether and what they can afford to pay. In addition, for example, certain housing-related costs are also disregarded in the financial assessment.
8.35 People in a care home will contribute most of their income, excluding their earnings, towards the cost of their care and support. However, a local authority must leave the person with a specified amount of their own income so that the person has money to spend on personal items such as clothes and other items that are not part of their care. This is known as the personal expenses allowance (PEA). This is in addition to any income the person receives from earnings. Ministers have the power to adjust the PEA. Any changes are communicated by Local Authority Circular and are binding. Local authorities have discretion to apply a higher income allowance in individual cases, for example where the person needs to contribute towards the cost of maintaining their former home. Further detail is set out in Annex C.
Choice of accommodation
8.36 Where the care planning process has determined that a person’s needs are best met in a care home, the local authority must provide for the person’s preferred choice of accommodation, subject to certain conditions. This also extends to shared lives, supported living and extra care housing settings. Determining the appropriate type of accommodation should be made with the adult as part of the care and support planning process, therefore this choice only applies between providers of the same type.
8.37 The local authority must ensure that the person has a genuine choice of accommodation. It must ensure that at least one accommodation option is available and affordable within the person’s personal budget and it should ensure that there is more than one of those options. However, a person must also be able to choose alternative options, including a more expensive setting, where a third party or in certain circumstances the resident is willing and able to pay the additional cost (‘top-up’). However, an additional payment must always be optional and never as a result of commissioning failures leading to a lack of choice. Detailed guidance is set out in Annex A which a local authority must have regard to.
Charging for care and support in other care settings including a person’s own home
8.38 This section should be read in conjunction with the regulations and Annex B on the treatment of capital and Annex C on the treatment of income in non-residential care.
8.39 These charging arrangements cover any setting for meeting care and support needs outside of a care home. For example, care and support received in a person’s own home, and in other accommodation settings such as in extra care housing, supported living accommodation or shared lives arrangements.
8.40 The intent of the regulations and guidance is to support local authorities to assess what a person can afford to contribute towards their care costs. Local authorities should also consider how to use their discretion to support the principles of care and support charging.
8.41 This guidance does not make any presumption that local authorities will charge for care and support provided outside care homes, but enables them to continue to allow discretion.
8.42 Because a person who receives care and support outside a care home will need to pay their daily living costs such as rent, food and utilities, the charging rules must ensure they have enough money to meet these costs. After charging, a person must be left with the minimum income guarantee (MIG), as set out in the Care and Support (Charging and Assessment of Resources) Regulation 2014. In addition, where a person receives benefits to meet their disability needs that do not meet the eligibility criteria for local authority care and support, the charging arrangements should ensure that they keep enough money to cover the cost of meeting these disability-related costs.
8.43 Additionally, the financial assessment of their capital must exclude the value of the property which they occupy as their main or only home. Beyond this, the rules on what capital must be disregarded are the same for all types of care and support. However, local authorities have flexibility within this framework; for example, they may choose to disregard additional sources of income, set maximum charges, or charge a person a percentage of their disposable income. This will help support local authorities to take account of local circumstances and promote integration and innovation.
8.44 Although local authorities have this discretion, this should not lead to 2 people with similar needs, and receiving similar types of care and support, being charged differently.
8.45 Local authorities should develop and maintain a policy on how they wish to apply this discretion locally. In designing this policy local authorities should consider the objectives of care and support charging and how it can:
- ensure that people are not charged more than it is reasonably practicable for them to pay
- be comprehensive, to reduce variation in the way people are assessed and charged
- be clear and transparent, so people know what they will be charged
- promote wellbeing, social inclusion, and support the vision of personalisation, independence, choice and control
- support carers to look after their own health and wellbeing and to care effectively and safely
- be person-focused, reflecting the variety of care and caring journeys and the variety of options available to meet their needs
- apply the charging rules equally so those with similar needs or services are treated the same and minimise anomalies between different care settings
- encourage and enable those who wish to stay in or take up employment, education or training or plan for the future costs of meeting their needs to do so
- be sustainable for local authorities in the long-term
- administer a charging policy for people who lack capacity or are losing capacity in a way that considers what capacity remains and their rights
8.46 Local authorities should consult people with care and support needs when deciding how to exercise this discretion. In doing this, local authorities should consider how to protect a person’s income. The government considers that it is inconsistent with promoting independent living to assume, without further consideration, that all of a person’s income above the minimum income guarantee (MIG) is available to be taken in charges.
8.47 Local authorities should therefore consider whether it is appropriate to set a maximum percentage of disposable income (over and above the guaranteed minimum income) which may be taken into account in charges.
8.48 Local authorities should also consider whether it is appropriate to set a maximum charge, for example these might be set as a maximum percentage of care home charges in a local area. This could help ensure that people are encouraged to remain in in their own homes, promoting individual wellbeing and independence.
Charging for support to carers
8.49 Where a carer has eligible support needs of their own, the local authority has a duty, or in some cases a power, to arrange support to meet their needs. Where a local authority is meeting the needs of a carer by providing a service directly to a carer, for example a relaxation class or driving lessons, it has the power to charge the carer. However, a local authority must not charge a carer for care and support provided directly to the person they care for under any circumstances.
8.50 Local authorities are not required to charge a carer for support and indeed in many cases it would be a false economy to do so. When deciding whether to charge, and in determining what an appropriate charge is, a local authority should consider how it wishes to express the way it values carers within its local community as partners in care, and recognise the significant contribution carers make. Carers help to maintain the health and wellbeing of the person they care for, support this person’s independence and enable them to stay in their own homes for longer. In many cases of course, carers voluntarily meet eligible needs that the local authority would otherwise be required to meet. Local authorities should consider carefully the likely impact of any charges on carers, particularly in terms of their willingness and ability to continue their caring responsibilities. It may be that there are circumstances where a nominal charge may be appropriate, for example to provide for a service which is subsidised but for which the carer may still pay a small charge, such as a gym class. Ultimately, a local authority should ensure that any charges do not negatively impact on a carer’s ability to look after their own health and wellbeing and to care effectively and safely.
8.51 While charging carers may be appropriate in some circumstances, it is very unlikely to be efficient to systematically charge carers for meeting their eligible needs. This is because excessive charges are likely to lead to carers refusing support, which in turn will lead to carer breakdown and local authorities having to meet more eligible needs of people currently cared for voluntarily. As an example, work carried out by Surrey County Council found that if even 10% of people with care and support needs in families supported by carers presented to the council with eligible needs as a result of carer breakdown, the resulting cost would be 3 times the current total budget for carer support. The ADASS produced the Economic Case for Investment in Carers, a short factsheet for local authorities to use in considering whether to put in place a policy of charging carers, setting out the evidence that charging would be a false economy.
8.52 Local authorities may also wish to consider whether charging is proportionate when carers’ assessments are undertaken for small scale help. There is a risk that financial assessments might become the most costly part of the process and something that is administratively burdensome.
8.53 Where a local authority takes the decision to charge a carer, it must do so in accordance with the non-residential charging rules. In doing so, it should usually carry out a financial assessment to ensure that any charges are affordable. However, it may be more likely, in the case of a carer, that the carer and the local authority will agree that a full financial assessment would be disproportionate as carers often face significantly lower charges.
8.54 In such cases, a local authority may choose to treat a carer as if a financial assessment has been carried out. When deciding whether or not to undertake a light-touch financial assessment, a local authority should consider both the level of the charge it proposes to make as well as the evidence the person is able to provide that they will be able to afford the charge. They must also inform the person when a light-touch assessment has taken place and make clear from the outset that the person has the right to request a full financial assessment should they so wish.
8.55 A carer’s assessment may identify that the carer’s needs for support could be met by arranging time away from the person they care for, for instance so that they can stay on top of other aspects of their lives, and that in order to achieve this services need to be provided to support the cared-for person in their absence. Such services would be provided direct to the cared-for person, even though they may meet the needs of both parties and may have been identified through the carer’s assessment. The local authority may not charge the carer for these services, and any charges should be based on the local authority’s policy on charging for non-residential care and support.
Requesting local authority support to meet eligible needs
8.56 People with eligible needs and financial assets above the upper capital limit may ask the local authority to meet their needs. This could be for a variety of reasons such as the person finding the system too difficult to navigate, or wishing to take advantage of the local authority’s knowledge of the local market of care and support services. Where the person asks the local authority to meet their eligible needs, and it is anticipated that their needs will be met by a care home placement, then the local authority may choose to meet their needs, but is not required to do so. In other cases, where the needs are to be met by care and support of some other type, the local authority must meet those eligible needs.
8.57 Local authorities should therefore take steps to make people aware that they have the right to request the local authority to meet their needs, in certain circumstances even when they have resources above the financial limits and would not be entitled to financial support with any charges. They should also be clear that this right does not extend to needs met by a care home placement, although local authorities may choose to apply the same approach locally. Local authorities should also offer support to people in meeting their own needs, including providing information and advice on different options, and may offer to arrange contracts with providers.
8.58 Where the person’s resources are above the financial limit, the person’s entitlement to local authority support in meeting their needs may be dependent on the request having been made. Therefore it is important that the person, and any carer, advocate or other person they wish to involve, are aware of this ability and the consequences for their care and support. The local authority must make clear to the person that they may be liable to pay an arrangement fee in addition to the costs of meeting their needs to cover the costs of putting in place the care and support required.
8.59 Arrangement fees charged by local authorities must cover only the costs that the local authorities actually incur in arranging care. Arrangement fees should take account of the cost of negotiating and/or managing the contract with a provider and cover any administration costs incurred. Where a local authority chooses to meet the needs of a person with resources above the financial limit who requires a care home placement, it must not charge an arrangement fee. This is because it would support that person under its power (rather than its duty) to meet needs, and the ability to charge the arrangement fee applies only to circumstances when the authority is required to meet needs.
8.60 Local authorities must not charge people for a financial assessment, a needs assessment or the preparation of a care and support plan.
8.61 It may be appropriate for local authorities to charge a flat rate fee for arranging care. This can help ensure people have clarity about the costs they will face if they ask the local authority to arrange their care. However, such flat rate costs must be set at a level where they do not exceed the costs the local authority actually incurs.
8.62 The information provided to the person following a financial assessment should include information on the right to request the local authority to meet their needs – and how they would be charged – and the advice and support that is available to help people make arrangements to meet their own needs whatever type of support they require.
8.63 A local authority will be under a duty to meet a person’s eligible needs when requested to do so and their needs are to be met by care and support other than in a care home. However, where the person has resources above the financial limits the local authority may charge the person for the full cost of their care and support. In such circumstances, the person remains responsible for paying for the cost of their care and support, but the local authority takes on the responsibility for meeting those needs. This means that the local authority may for example provide or arrange care and support, or make a direct payment which may be a paper based exercise, or some combination of these. Further information on how, to ‘meet needs’ and the options available is provided in chapter 10.
8.64 The local authority must assure itself that whilst the person remains responsible for paying for their own care, they have sufficient assets for the arrangements that it puts in place to remain both affordable and sustainable. The local authority should also take steps to avoid disputes and additional liabilities by securing a person’s agreement in writing to pay the costs that they are responsible for in meeting their needs, including payments to providers. Local authorities should make similar arrangements with any third parties that agree to contribute towards these costs.
Pension reforms
8.65 Reforms to defined contribution pensions came into effect from April 2015. The aim of the reforms is to provide people with much greater flexibility in how they fund later life. The government expects there to be a range of new products that people will use to manage and access money from their pensions as and when they need it, and where possible, these should be treated similarly to existing drawdown products for charging purposes.
8.66 The Pension wise service helps people to make informed choices at the point of retirement. This will include information and advice on later life, including the risk that they may need care and support in the future, and will have to pay for it.
8.67 For the purposes of charging, a local authority must follow the guidance set out on the treatment of income and capital in Annexes B and C and treat a person’s assets accordingly. Where a person has chosen to withdraw funds from their pension pot and manage it directly, for example combining it with other assets rather than through a pensions product, this may be treated as capital under the rules laid out in Annex B.
Complaints
8.68 A person may wish to make a complaint about any aspect of the financial assessment or how a local authority has chosen to charge. A local authority must make clear what its complaints procedure is and provide information and advice on how to lodge a complaint.
8.69 Complaints about the level of charge levied by a local authority are subject to the usual care and support complaints procedure as set out in The Local Authority Social Services and NHS Complaints (England) Regulations 2009.
8.70 Where a local authority has established a special panel or fast track review processes to deal with financial assessment/charging issues, they should remind the person that they still have access to the statutory complaints procedure.
9. Deferred payment agreements
This chapter provides guidance on:
- sections 34-36 of the Care Act 2014
- the Care and Support (Deferred Payment) Regulations 2014 (as amended by the Care and Support (Deferred Payment)(Amendment) Regulations 2017) [see note 1]
This chapter covers:
- who to offer a deferred payment to
- provision of information and advice before making a deferred payment agreement
- how much can be deferred, and security for the agreement
- interest rate for the deferral and administrative charges
- making the agreement, responsibilities while the agreement is in place and termination of the agreement
Note 1
The legislation that underpinned deferred payment agreements (DPAs) did not work as intended. It meant that local authorities (LAs) in England were not required to offer DPAs to eligible individuals unless they were meeting that individual’s needs or believed they would meet their needs if asked. We therefore made amendments to the Care and Support (Deferred Payment) Regulations 2014 so that LAs are now required to enter into a ‘loan-type’ DPA with individuals who qualify for one but whose needs the LA is not meeting. This chapter was amended on 12 February 2018 to reflect these changes in the law and to provide greater clarity on the types of DPAs that can be offered (see paragraphs 9.3, 9.7 and 9.10 to 9.13).
Definitions
9.1 ‘Care costs’ – all costs charged to a person by a care provider, including any top-ups and core care costs. This includes the costs associated with the provision of supported accommodation.
9.2 ‘Top ups’ – this term has the usual meaning accorded to it within the care and support sector, but for the avoidance of doubt, top ups are costs due to a local authority under Section 30 of the Care Act or costs for the provision of the type of care referred to in Section 34(3)(a) of the Care Act.
Introduction
9.3 The establishment of the universal deferred payment scheme means that people should not be forced to sell their home in their lifetime to pay for their care. By entering into a deferred payment agreement, a local authority agrees to:
- defer the payment of charges due to it from the adult, for the costs of meeting needs in a care home or supported living accommodation
or
- defer the repayment of a loan to the adult in instalments, to cover the costs of care and support in a care home or supported living accommodation
Deferring payment can help people to delay the need to sell their home, and provides peace of mind during a time that can be challenging (or even a crisis point) for them and their loved ones as they make the transition into care.
9.4 A deferred payment agreement can provide additional flexibility for when and how someone pays for their care and support. It should be stressed from the outset that the payment for care and support is deferred and not ‘written off’. The costs of provision of care and support will have to be repaid by the individual (or a third party on their behalf) at a later date.
9.5 The scheme is universally available throughout England, and local authorities are required to offer deferred payment agreements to people who meet certain criteria governing eligibility set out in paragraph 9.7 below (the qualifying criteria) for the scheme. Local authorities need to ensure that adequate security is in place for the amount being deferred, so that they can be confident that the amount deferred will be repaid in the future. Local authorities are also encouraged to offer the scheme more widely to anyone they feel would benefit who does not fully meet the criteria.
9.6 A deferral can last until death. However, many people choose to use a deferred payment agreement as a ‘bridging loan’ to give them time and flexibility to sell their home when they choose to do so. This is entirely up to the individual to decide. Further details on deferred payment agreements are set out in the sections below.
Who to offer deferred payment agreements to
Qualifying criteria for deferred payment agreements
9.7 Deferred payment agreements are designed to prevent people from being forced to sell their home in their lifetime to meet the cost of their care. Local authorities must offer them to people who meet the criteria below and who are able to provide adequate security (see section entitled ‘Obtaining Security’ below). Subject to these criteria they must offer them to people who have their needs met by the local authority, and also people who meet their own needs. The regulations provide that someone must be offered a deferred payment agreement if they meet all of the following criteria at the point of applying for a deferred payment agreement. Broadly, they are that the:
- a) person is ordinarily resident in the local authority area or present in the area but of no settled residence; or ordinarily resident in another local authority area but the local authority has determined that they will or would meet the individual’s care needs under section 19 of the Care Act if asked to do so [see note 2]
- b) person has needs which are to be met by the provision of care in a care home. This is determined when someone is assessed as having care and support needs [see note 3] which the local authority considers should be met through a care home placement
- c) person has less than (or equal to) £23,250 in assets excluding the value of their main or only home (for example, in savings, other non-housing assets and housing assets other than their main or only home)
- d) person’s home is not disregarded [see note 4]; for example, it is not occupied by a spouse or dependent relative as defined in regulations on charging for care and support (for example, someone whose home is taken into account in the local authority financial assessment and so might need to be sold)
Note 2
Where a local authority is meeting an individual’s care and support needs under section 19(2) of the Care Act.
Note 3
When someone is arranging their own care and support and the authority has not performed an assessment, this condition is satisfied when someone would be assessed as having eligible needs were the authority to have carried out such an assessment.
Note 4
Disregarded for the purposes of the financial assessment carried out under section 17 of the Act.
9.8 As well as providing protection for people facing the prospect of having to sell their home to pay for care, deferred payment agreements can offer valuable flexibility, giving people greater choice over how they pay their care costs. Local authorities are, at their discretion, permitted to be more generous than these criteria and offer deferred payment agreements to people who do not meet criteria b, c or d in section 9.7. In deciding whether someone who does not meet all of the criteria above should still be offered a deferred payment, some considerations a local authority may wish to take into account include (but are not limited to):
- a) whether meeting care costs would leave someone with very few accessible assets (this might include assets which cannot quickly or easily be liquidated or converted to cash)
- b) if someone would like to use wealth tied up in their home to fund more than just their core care costs and purchase affordable top-ups (see further guidance on ‘How much can be deferred’, paragraph 9.36)
- c) whether someone has any other accessible means to help them meet the cost of their care and support
- d) if a person is narrowly not entitled to a deferred payment agreement given the criteria above, for example because they have slightly more than the £23,250 asset threshold. This should include people who are likely to meet the criteria in the near future
9.9 Local authorities may also at their discretion enter into deferred payment agreements with people whose care and support is provided in supported living accommodation. The local authority should not exercise this discretion unless the person intends to retain their former home and pay the associated care and accommodation rental costs from their deferred payment. Further details on precisely what qualifies as supported living accommodation are set out in regulations. Deferred payment agreements cannot be entered into to finance mortgage payments on supported living accommodation.
Types of deferred payment agreement
9.10 Deferred payment agreements can take 2 forms:
- the local authority pays the care home or supported living accommodation directly and defers the charges due to it from the individual (traditional type)
- the individual pays the care provider for their care and the local authority loans them the cost of care in instalments less any contributions the individual contributes from other sources (loan type)
9.11 When considering their approach as to when or whether to offer loan or traditional type deferred payment agreements, local authorities should have regard to their duties under the Care Act, including their duties under the well-being principle and their market duties. Local authorities cannot refuse to enter into a loan-type deferred payment agreement if the qualifying criteria are met and the individual requests it (subject to paragraphs 9.14 to 9.17 below).
9.12 The local authority must comply with all relevant legislation and act under the guidance.
9.13 In all cases, a local authority is only required to enter into a deferred payment agreement to cover the costs of care and support which it considers necessary.
Permission to refuse a deferred payment agreement
9.14 A local authority must offer a deferred payment to someone meeting the qualifying criteria for deferred payment agreements and who is able to provide adequate security for the debt (obtaining a first land registry charge on their property, see ‘Obtaining security’ at paragraph 9.58); and may offer a deferred payment agreement to others who do not meet the criteria, at their discretion.
9.15 There are, however, certain circumstances in which a local authority may refuse a request for a deferred payment agreement (‘permission to refuse’), even if a person meets the qualifying criteria and the local authority would otherwise be required to offer the person an agreement. This permission (or discretion) to refuse is intended to provide local authorities with a reasonable safeguard against default or non-repayment of debt.
9.16 A local authority may refuse a deferred payment agreement despite someone meeting the qualifying criteria:
- a) where a local authority is unable to secure a first charge on the person’s property
- b) where someone is seeking a top up [see note 5]
- c) where a person does not agree to the terms and conditions of the agreement, for example a requirement to insure and maintain the property
Note 5
In these situations, a local authority should still seek to offer a deferred payment agreement but should be guided by principles in the section ‘How much to defer’, to determine a maximum amount that is sustainable (or reflects their core care costs without any top-ups) and agree a deferral. The person can then choose whether they wish to agree
9.17 In any of the above circumstances, a local authority should consider whether to exercise its discretion to offer a deferred payment anyway (for example, if a person’s property is uninsurable but has a high land value, the local authority may choose to accept charges against this land as security instead).
Circumstances in which local authorities may stop deferring care costs or making payments under a loan-type agreement
9.18 There are also circumstances where a local authority may refuse to defer or loan any more charges for a person who has an active deferred payment agreement. Local authorities cannot demand repayment in these circumstances, and repayment is still subject to the usual terms of termination, as set out in the section entitled ‘termination of the agreement’ below.
9.19 The local authority should provide a minimum of 30 days’ advance notice that further deferrals or loans will cease; and should provide the person with an indication of how their care costs will need to be met in future. Depending on their circumstances, the person may either receive local authority support in meeting the costs of their care, or may be required to meet their costs from their income and assets. Local authorities exercising these powers to cease deferring additional amounts should consider their decision to do so whilst considering the person’s circumstances and their overarching duties under the well-being principle.
9.20 Circumstances in which a local authority may refuse to defer or loan any more charges include[footnote 25]:
- a) when a person’s total assets fall below the level of the means-test (see chapter 8), and the person becomes eligible for local authority support in paying for their care
- b) where a person no longer has need for care in a care home (or where appropriate supported living accommodation)
- c) if a person breaches certain predefined terms of their contract (which must be clearly set out in the contract) and the local authority’s attempts to resolve the breach are unsuccessful and the contract has specified that the authority will stop making further payments in such a case
- d) if, under the charging regulations (see also chapter 8), the property becomes disregarded for any reason and the person consequently qualifies for local authority support in paying for their care, including but not limited to:
- (i) where a spouse or dependent relative (as defined in charging regulations) has moved into the property after the agreement has been made, where this means the person is eligible for local authority support in paying for care and no longer requires a deferred payment agreement
- (ii) where a relative who was living in the property at the time of the agreement subsequently becomes a dependent relative (as defined in charging regulations). The local authority may cease further deferrals at this point
9.21 Local authorities should not exercise these discretionary powers if a person would, as a result, be unable to pay any tariff income due to the local authority from their non-housing assets.
9.22 Local authorities must also cease deferring or loaning further amounts when a person has reached the ‘equity limit’ that they are allowed to defer (see ‘how much can be deferred’ below); or when a person is no longer receiving care and support in either a care home setting or in supported living accommodation. This also applies when the value of the security has dropped and so the equity limit has been reached earlier than expected. [footnote 26]
Case study 1
Lucille develops a need for a care home placement. She lives alone and is the sole owner of her home. Her home is valued at £165,000, and she has £15,000 in savings. Lucille meets the qualifying criteria for a deferred payment.
Information and advice
9.23 Under the Care Act, local authorities have responsibilities to provide information and advice about people’s care and support. These extend to deferred payment schemes as well. This chapter should be read in combination with chapter 3 (‘Information and Advice’).
9.24 In order to be able to make well-informed choices, it is essential that people access appropriate information and advice before taking out a deferred payment agreement (DPA). It is also important that people are kept informed about their DPA throughout the course of the agreement, and that they (and the executor of their estate where appropriate) receive the necessary information upon termination of the agreement.
9.25 Information and advice requirements prior to taking out a DPA are discussed in this section; requirements on local authorities while the DPA is in place are discussed in a separate section below (see ‘the local authority’s responsibilities whilst the agreement is in place’); and the section entitled ‘termination of the agreement’ addresses the responsibilities on the local authority when the agreement is concluded. The requirements on local authorities to offer and facilitate access to financial information and advice on other options for paying for care are discussed in chapter 3.
9.26 Deferred payment agreements are often made during a time that is demanding for a person and their loved ones – a period when they are making a transition into a care home. People may need additional support during this period, and the local authority has a role in providing this support and facilitating their transition, particularly if their transition to care is made rapidly and/or at an unexpected point. The local authority must provide information in a way which is clear and easy to understand, and it should be designed to ease the process of transition for people, their carers and their families.
9.27 Carers and families often assist people in making decisions about their care and how they pay for it. Local authorities should as appropriate invite carers and/or families to participate in discussions, and should also provide them with all the information that would otherwise be given to the person they care for, subject (where required)[footnote 29] to the consent of the person with care and support needs (if they have capacity) or someone else with appropriate authorisation. In doing this, they must ensure compliance with mental capacity and data protection legislation, and the other duties pertaining to information and advice set out in chapter 3 of this guidance.
9.28 As a deferred payment agreement can take some time to set up and agree, it is important that both the local authority and the individual consider any potential issues around mental capacity. Where a person may lack capacity to request a deferred payment, a deputy or attorney (a person with a relevant enduring power of attorney or lasting power of attorney) may request a deferred payment on their behalf. If a family member requests a deferred payment and they do not have the legal power to act on behalf of the person, then the person and the family member should receive information and advice on how to obtain this, through lasting power of attorney and deputyships. Where the local authority is the deputy for a person, then the local authority deputy may apply for deferred payments where this is in the best interests of the person. Local authorities must not enter into deferred payment agreements with a person lacking the requisite mental capacity unless the proper arrangements are in place.
9.29 Local authorities and the person applying for a deferred payment (who has capacity) may also want to consider any potential issues around loss of capacity. The local authority should where appropriate provide the person with information and advice on options for deputyship, legal power of attorney and advocacy. If a local authority and the person do discuss the issue, the local authority should confirm what would happen were the person to lose capacity and not have made their own arrangements. Further advice on capacity and financial arrangements is contained in the guidance on debt recovery in Annex D (a deferred payment being effectively a consensually-accruing debt to the local authority).
9.30 If a local authority identifies someone who may benefit from or be eligible for a DPA or a person approaches them for information, the local authority must tell them about the DPA scheme and how it works. This explanation should, at a minimum:
- set out clearly that the fees are being deferred or delayed and must still be paid back at a later date, for example through the sale of the home (potentially after the individual’s death)
- explain the types of security that a local authority is prepared to accept (as set out by each local authority in a publicly – available policy; see the section entitled ‘Obtaining Security’ below for further details)
- explain that if a home is used as security, the home may need to be sold at a later date to repay the amount due
- explain that the total amount they can defer will be governed by an equity limit (discussed in the section entitled ‘How much can be deferred’ below) which may change if the value of their security changes
- explain the circumstances where the local authority may cease to defer further amounts (such as when the person qualifies for local authority support in paying for their care), and the circumstances where the local authority has to stop deferring further amounts (such as when the person reaches their equity limit)
- explain if and how interest will be charged on any amount deferred
- explain that they may be liable to pay administrative charges
- explain what happens on termination of the agreement, how the loan becomes due and their options for repayment
- explain what happens if they do not repay the amount due
- set out the qualifying criteria for a DPA
- detail the requirements that must be adhered to during the course of the DPA
- explain the implications that a deferred payment agreement may have on their income, their benefit entitlements, and charging
- provide an overview of some potential advantages and disadvantages of taking out a DPA, and explain that there are other options for paying for their care that they may wish to consider
- note the existence of the 12-week disregard, which will afford those who qualify for it some additional time to consider their options in paying for care
- suggest that people may want to consider taking independent financial advice (including flagging the existence of regulated financial advice), in line with the guidance set out in chapter 3
9.31 Local authorities should provide easy to read information about how the scheme works. This may be in the form of a standardised information sheet.
9.32 Local authorities must provide this information and advice in formats that ensure compliance with the requirements of the Equality Act 2010 (in particular, they must ensure where appropriate that the information is accessible to the sensory impaired, people with learning disabilities, and people for whom English is not their first language). Further clarifications on information and advice requirements are detailed in chapter 3.
9.33 Where relevant, local authorities should provide information and advice on DPAs at the earliest appropriate opportunity during the period of the 12-week disregard[footnote 28]. Local authorities should aim to ensure that people are able to make a smooth transition from the 12-week disregard to the DPA if they opt to enter into an agreement. This means ensuring as far as possible that a DPA is available by the first day of week 13.
9.34 Local authorities should advise people (where appropriate) that they will need to consider how they plan to use, maintain and insure their property if they take out a DPA; that is whether they wish to rent, to prepare for sale, or to leave it vacant for a period. The local authority should advise if it intends to place conditions on how the property is maintained whilst the DPA is in place (authorities will usually include requirements for people to maintain and insure their homes in the terms and conditions of a deferred payment agreement; see the section entitled ‘Making the Agreement’ for further details).
9.35 Local authorities should develop basic information and advice for homeowners on how they may choose to use their property when they enter care, for example information on how they may go about renting their property, and the potential impact on other people living in the property if a sale is required after their death. They should signpost people to more specialist organisations who can provide further advice on this issue, including information about their legal responsibilities as landlords and their obligations to any potential tenants.
Case study 2
Lucille’s son Buster has been providing informal care and support to her, and has heard of the deferred payments scheme. When Lucille decides she may benefit from a care home placement, her son suggests they approach her local authority together for information and advice about deferred payment agreements.
Her local authority provides them both with a printed information sheet setting out further details on the authority’s deferred payment scheme, and also provides them with contact details of some national and local services who provide financial information and advice
Lucille is interested in renting her property whilst residing in a care home. The local authority has an existing housing advice service, so signposts Lucille to them for further advice on lettings. The local authority’s standard information sheet also includes information on how her rental income may be used to pay for her care and support.
How much can be deferred?
9.36 In principle, a person should be able to defer the entirety of their care costs; subject to any contribution the local authority is allowed to require from the person’s income. The local authority will need to consider whether a person can provide adequate security for the deferred payment agreement (see next section entitled ‘Obtaining Security’ – usually this requirement for ‘adequate security’ will be fulfilled by securing their deferred payment agreement against their property).
9.37 If the person is considering a top-up, the local authority should also consider whether the amount or size of the deferral requested is sustainable given the equity available from their chosen form of security. A discussion of sustainability may be helpful in all cases to ensure the person is aware of how much care their chosen form of security would afford them.
9.38 Three elements will dictate how much a person will defer, each of which is discussed below:
- a) The amount of equity a person has available in their chosen form of security (usually their property)
- b) The amount a person is contributing to their care costs from other sources, including income and (where they choose to) any contribution from savings, a financial product or a third-party
- c) The total care costs a person will face, including any top-ups the person might be seeking
9.39 Local authorities should also satisfy themselves that any top-up they agree to is sufficiently sustainable. Some guidance for local authorities in assessing whether a top-up is sustainable is provided below.
Equity Limit
9.40 When considering the equity available, local authorities must be guided by an ‘equity limit’ for the total amount that can be deferred and ensure that the amount deferred does not rise above this limit. The equity limit will leave some equity remaining in the security used for the DPA – this will both act as a buffer to cover any subsequent interest which continues to accrue, and will provide a small ‘cushion’ in case of small variations in value of the security. In the majority of cases a property will be used as security, so the equity limit will provide a cushion against changes in house prices. When calculating progress towards the equity limit, the local authority must also include any interest and/or fees to be deferred.
9.41 If the person intends to secure their deferred payment agreement with a property, local authorities must obtain a valuation of the property. Reasonable property valuation costs are included in the list of administration charges that local authorities can pass on to people, should they wish to do so. People may request an independent assessment of the property’s value (in addition to the local authority’s valuation). If an independent assessment finds a substantially differing value to the local authority’s valuation, the local authority and person should discuss and agree an appropriate valuation prior to proceeding with the agreement.
9.42 Where a property is used as security to offer a deferred payment agreement, the equity limit must be set at the value of the property minus 10%, minus £14,250 (for financial year 2015 to 2016, this is in line with the lower capital limit) and the amount of encumbrance secured on it. This limit provides some protection to local authorities against changes in the value of the security (such as possible house price fluctuations) and the risk that they may not be able to recoup the full amount owed, but also should mean that people qualify for local authority support if they deplete the equity available in their property (and are consequently not at risk of having to sell their home to pay for care).[footnote 29]
9.43 Local authorities should, when someone is approaching or reaches the point at which they have deferred 70% of the value of their chosen security, review the cost of their care with the person, discuss when the person might be eligible for any means tested support, discuss the implications for any top-up they might currently have, and consider jointly whether a deferred payment agreement continues to be the best way for someone to meet these costs.
9.44 The following example illustrates the equity limit principle.
Case study 3: The equity limit
Lucille decides to secure her deferred payment agreement with her house, which is worth £165,000. The amount of equity available will be the value of the property minus 10%, minus a further £14,250 (the lower capital limit).
£165,000 – £16,500 – £14,250 = £134,250
Therefore, her ‘equity limit’ for the total amount she could defer would consequently be £134,250, which would leave £30,750 in equity in her home.
9.45 Local authorities must not allow additional amounts to be deferred beyond the equity limit, and must refuse to defer care costs beyond this (see section above entitled ‘permission to refuse’). However, interest can still accrue beyond this point, and administrative charges can still be deferred.
Contributing to care costs from other sources
9.46 A person may meet the costs of their care and support from a combination of any of 4 primary sources:
- income, including pension income (see chapter 8 for definition of income)
- savings or other assets they might have access to, this might include any contributions from a third party
- a financial product designed to pay for long-term care
- a deferred payment agreement which enables them to pay for their care at a later date out of assets (usually their home)
9.47 The share of care costs that someone defers will depend on the amount they will be paying from the other sources listed above.
9.48 Local authorities may require a contribution towards care costs from a person’s income, but the person has a right to retain a proportion of their income (the ‘disposable income allowance’). The disposable income allowance is a fixed amount (up to £144 per week) of a person’s income which the local authority must allow the person to retain (if the person wants to retain it). The local authority can require the person to contribute the rest of their income, but must allow the person to retain as much of their disposable income allowance as they want to.
9.49 A person may choose to keep less of their income than the disposable income allowance. This might be advantageous to the person as they would be contributing more to the costs of their care from their income, and consequently reducing the amount they are deferring (and accruing less debt to their local authority overall). However this must be entirely at the individual’s decision and the local authority must not compel someone to retain less than the disposable income allowance if the person wants to retain the full amount.
9.50 If a person decides to rent out their property during the course of their DPA, a local authority should permit that person to retain a percentage of any rental income they possess. Local authorities may want to consider whether to offer other incentives to individuals to encourage rental of properties, though the decision as to whether or not to rent a property must be the person’s and theirs alone.
9.51 A person may also contribute to their care costs from payments by a third party (including any contributions available from a financial product) or from their savings. Contributing to care costs from another source would be beneficial for a person as it would reduce the amount they are deferring (and hence reduce their overall debt to the local authority). A local authority must not compel a person to contribute to their deferral from these sources.
Case study 4
Lucille identifies a care home placement that meets her care and support needs, costing £540 per week. She has an income provided by her pension of £230 per week. Lucille decides not to rent her home as she intends to sell it within the year.
Based on this provisional estimate of her care costs, Lucille would contribute £86 (230 –144) per week from her income, and her weekly deferral would be £454.
Care costs
9.52 Before considering in detail how much they will be deferring, a person and usually the local authority should have a rough idea of their likely care costs as a result of the care planning process. Someone may wish to vary their care package (or any top-ups they may be considering) following consideration of what they could afford with a deferred payment agreement, but should approach the process with an approximate idea of what their care costs are likely to be.
9.53 In principle, people should be able to defer their full care costs including any top-ups.[footnote 32] At a minimum, when local authorities are required to offer a deferred payment agreement they must allow someone to defer their ‘core’ care costs. To ensure sustainability of the deferral, local authorities have discretion over the amount people are permitted to top-up.[footnote 33] Local authorities should consider any request for top-ups, but retain discretion over whether or not to agree to a given top-up. Local authorities should accept any top-up deemed to be reasonable given considerations of affordability, sustainability and available equity. Local authorities should be mindful of the duties set out in relation to top-ups and additional costs in the care and support and aftercare (Choice of Accommodation) regulations 2014.
Sustainability
9.54 When deciding on the amount to be deferred in a discretionary deferred payment agreement (particularly when considering top-ups), both parties should consider a range of factors to satisfy themselves that the arrangement is sustainable including:
- the likely period the person would want a DPA for (if they intend to use it as a ‘bridging loan’);
- the equity available
- the sustainability of a person’s contributions from their savings (if they are making one)
- the flexibility to meet future care needs
- the period of time a person would be able to defer their care costs for
9.55 Deferred payment agreements should prevent people from having to sell their home in their lifetime to pay for their care. Local authorities should discuss with the person the projected limit of what their equity could cover, given their projected care costs, and how their care costs might change over time. This may include a discussion of when they are likely to reach any of the income thresholds and may begin to qualify for local authority support in paying for their care. If the person is requesting a top-up, it is important that the local authority discusses what might happen to any top-up requested if the person reaches the equity limit and moves on to local authority support in paying for their care, and ensures that a written agreement is in place (see Annex A: Choice of accommodation and additional payments). In particular, the local authority should make the person aware that once they have reached the equity limit, the local authority may not be willing to fund their top-up, and the person may need to find other ways to pay for it or be prepared for a change in their care package.
9.56 Local authorities and individuals should also consider the length of time that a person’s intended contribution to care costs from savings would last, if they intend to contribute to their care costs from their savings. This should include consideration of the impact on their care if a person’s savings are depleted (normally this would involve increasing the amount the person is deferring).
9.57 An important factor in the sustainability of a deferred payment agreement will be any future care and support needs someone might face, and local authorities and people should consider allowing flexibility for changes in circumstance, including possible escalations of needs, when deciding how much someone should defer. Local authorities and people should factor any potential changes in circumstances into their considerations of sustainability.
9.58 The department has developed a tool to aid local authorities in assessing sustainability. Local authorities may use this tool to aid discussions and decisions about the amount to be deferred, but local authorities retain final responsibility for (and have discretion over) decisions taken about the agreements they enter into.
9.59 When agreement has been reached between a person and the local authority as to how much they want to defer, the local authority must ensure this is clearly and unambiguously set out in the deferred payment agreement. Further details on what happens once an amount has been agreed are set out in the section entitled ‘making the agreement’ below.
9.60 The amount being deferred should be reviewed on a regular basis to ensure the deferred amount does not exceed the equity limit as discussed above.[footnote 32] Local authorities should have particular regard to the amount deferred as it approaches the equity limit.
9.61 Further details of local authorities’ responsibilities during the course of the DPA are set out in the relevant section below.
Case study 5
Lucille discusses her care home fees with the local authority. Based on the equity available in her home (£134,250, as set out in Case study 3 above), Lucille could afford her weekly deferral of £454 for around 5 years. Given an average length of stay in a care home care of 19.7 months (source: BUPA 2010, cited in Laing and Buisson 2012/13), the local authority deems her projected care costs to be sustainable.
Lucille enquires as to the cost of a room with a garden view. This would increase her weekly deferral to £525 which she could afford for around four and a half years. The local authority deems this to be sustainable, so agrees to Lucille’s requested top-up.
Obtaining security
9.62 A local authority must have adequate security in place when entering into a deferred payment agreement. The regulations set out one form of security that local authorities must accept, and also provide wider discretion for local authorities to accept other forms of security as they see fit. Local authorities should consider whether another type of security could be provided if a person cannot secure their deferred payment agreement with a charge on a property.
9.63 One form of ‘adequate security’ would be the local authority securing a first legal mortgage charge against a property on the Land Register. Local authorities must accept a first legal mortgage charge as adequate security and local authorities must offer a deferred payment to someone who meets the qualifying criteria for the scheme where the local authority is able to secure a first legal mortgage charge on the property.
9.64 In cases where an agreement is to be secured with a jointly-owned property, local authorities must seek both owners’ consent (and agreement) to a charge being placed on the property. Both owners will need to be signatories to the charge agreement, and the co-owner will need to agree not to object to the sale of the property for the purpose of repaying the debt due to the local authority (following the same procedure as in the case where an individual is the sole owner of a property).
9.65 The local authority must obtain similar consent to a charge being created against the property from any other person who has a beneficial interest in the property.
9.66 Under the discretionary scheme, local authorities have discretion to decide what else may constitute ‘adequate security’ for a deferred payment agreement, in cases where a first charge cannot be secured. A local authority’s decision should be based on an explicit and publicly-accessible policy of what other types of security they are willing to consider in addition to a first charge, but local authorities may consider the merits of each case individually. Other forms of security a local authority may choose to consider include (but are not limited to):
- a third-party guarantor – subject to the guarantor having / offering an appropriate form of security
- a solicitor’s undertaking letter
- a valuable object such as a painting or other piece of art
- an agreement to repay the amount deferred from the proceeds of a life assurance policy
9.67 A local authority has full discretion in individual cases to refuse a deferred payment agreement if it is not satisfied that adequate security is in place.[footnote 33]
9.68 The security should also be revalued when the amount deferred equals or exceeds 50% of the value of the security to assess any potential change in the value (and consequently the person’s ‘equity limit’ should be reassessed in turn). After this revaluation, local authorities should revalue the security periodically to monitor any potential further changes in value. If in either case there has been any substantial change the local authority should review the amount being deferred as well, as set out in the section ‘how much can be deferred’ above.
Interest rate and administration charge
9.69 The deferred payment agreement scheme is intended to be run on a cost-neutral basis, with local authorities able to recoup the costs associated with deferring fees by charging interest. Local authorities can also recoup the administrative costs associated with DPAs, including legal and ongoing running costs, via administration charges which can be passed on to the individual. Administration charges and interest can be added on to the total amount deferred as they are accrued, although a person may request to pay these separately if they choose. The agreement must make clear that all fees deferred, alongside any interest and administrative charges incurred, must be repaid by the person in full. The local authority must also notify the individual in writing whenever they are liable for an administration charge.
9.70 Local authorities will have the ability to charge interest on any amount deferred, including any administration charge deferred. This is to cover the cost of lending and the risks to local authorities associated with lending, for example the risk of default. Where local authorities charge interest this must not exceed the maximum amount specified in regulations. A local authority may (but is not required to) charge the nationally-set maximum interest rate. The same interest rate must be charged on all deferred payments within a local authority.[footnote 34]
9.71 The national maximum interest rate will change every 6 months on 1st January and 1st July. It will track the market gilts rate specified in the most recently published report by the Office of Budget Responsibility (OBR) plus a 0.15% default component. For example, gilt rate 1% plus 0.15% equals a maximum interest rate of 1.15%. The market gilt rate is currently published in the Economic and Fiscal Outlook, which is usually published twice-yearly on the OBR website. The figures can be found in the ‘Determinants of the fiscal forecast’ table, in the Economic and Fiscal Outlook.
Local authorities must ensure that any changes to the national maximum rate are reflected within their authority and are applied to any agreements they have entered into (unless they are already charging less than the national maximum). Individual agreements must also contain adequate terms and conditions to ensure that the interest rate within any given agreement does not exceed the nationally set maximum.
9.72 In extremely rare circumstances (such as a severe economic shock), government may need to make new regulations to change the maximum interest rate which local authorities are permitted to charge before the next January or July change date. These powers would only be exercised as a last resort.
9.73 Local authorities must inform people before they make the agreement if interest will be charged, what interest rates are currently set at, and when interest rates are likely to change. This is to enable people to make well-informed decisions about whether a deferred payment agreement is the best way for them to meet the costs of their care.
9.74 The interest charged and added to the deferred amount will be compounded, and local authorities should ensure when making the agreement that individuals understand that interest will accrue on a compound basis.
9.75 Interest can accrue on the amount deferred even once someone has reached the ‘equity limit’ (see ‘how much can be deferred’ above). It can also accrue after someone has died up until the point at which the deferred amount is repaid to the local authority. If the local authority cannot recover the debt and seeks to pursue this through the County Court system (as discussed in Annex D on debt recovery), the local authority may charge the higher County Court rate of interest.
9.76 Local authorities must set their administration charge at a reasonable level, and this level must not be more than the actual costs incurred by the local authority in provision of the Universal Deferred Payment Scheme, as set out in regulations. Relevant costs may include (but are not limited to) the costs incurred by a local authority whilst:
- registering a legal charge with the Land Registry against the title of the property, including Land Registry search charges and any identity checks required
- undertaking relevant postage, printing and telecommunications
- costs of time spent by those providing the service
- cost of valuation and re-valuation of the property
- costs for removal of charges against property
- overheads, including where appropriate (shares of) payroll, audit, management costs, legal service
9.77 Local authorities should maintain a publicly-available list of administration charges that a person may be liable to pay. It is good practice to separate charges into a fixed set-up fee for deferred payment agreements, reflective of the costs incurred by the local authority in setting up and securing a typical deferred payment agreement, and other reasonable one-time fees during the course of the agreement (reflecting actual charges incurred in the course of the agreement).
Making the agreement
9.78 Where someone chooses to enter into a deferred payment agreement, local authorities should aim to have the agreement finalised and in place by the end of the 12-week disregard period (where applicable) (see Annex B: Treatment of capital), or within 12 weeks of the person approaching the local authority regarding DPAs in other circumstances.
9.79 Decisions on a person’s care and support package, the amount they intend to defer, the security they intend to use and the terms of the agreement should only be taken following discussion between the local authority and the individual. Once agreement in principle has been reached between the local authority and the person, it is the local authority’s responsibility to transpose the details agreed into a deferred payment agreement, taking the legal form of a contract between the local authority and the person.
9.80 The local authority should provide a hard copy of the deferred payment agreement to the person, and they should be provided with reasonable time to read and consider the agreement, including time for the individual to query any clauses and discuss the agreement further with the local authority.
9.81 The agreement must clearly set out all terms, conditions and information necessary to enable the person to ascertain his or her rights and obligations under the agreement. These include:
- a) terms to explain how the interest will be calculated and that it will be compounded if it is to be added to the deferred amount
- b) information as to administrative costs the individual might be liable for
- c) terms to explain how the adult may exercise his or her right to terminate the agreement, which should explain the process for and consequences of terminating the agreement and specify what notice should be given (see the section entitled ‘terminating the agreement’ below)
- d) terms to explain the circumstances in which the local authority might refuse to defer or loan further fees (either when it is required to stop, for example if the person has already reached their ‘equity limit’, or when it has powers to stop, such as when a person qualifies for local authority support in paying for their care; as set out in the ‘how much can be deferred’ and ‘permission to refuse’ sections above)
- e) that the local authority will secure their debt either by placing a legal (Land Registry) charge against the property, or by some other means specified
- f) a term requiring the local authority to provide the person with a written statement every 6 months and within 28 days of request by the person, setting out how much the person owes to the authority and the cost to them of repaying the debt
- g) a term which explains that the maximum amount which may be deferred is the equity limit and that this is likely to vary over time
- h) a term which requires the local authority to give the adult 30 days written notice of the date on which they are likely to reach the equity limit
- i) a term which requires the adult to obtain the consent of the local authority for any person to occupy the property
- j) an explanation that the local authority will stop deferring its charges and making advances under a loan agreement if the person no longer receives care and support in a care home or supported living accommodation or if the local authority no longer considers that the adult’s needs should be met in such accommodation
9.82 If the agreement is not for the deferral of charges due to the authority (that is, a loan-type agreement), the agreement must also contain:
- a) a term to make clear that the authority will make advances of the loan to the adult in instalments
- b) a term to make clear that the purpose of the loan is to pay for costs of care and support in a care home or supported living accommodation. This should explain:
- (i) the consequences of any failure by the adult to pay those costs of care and support; and
- (ii) that the adult must inform the local authority if he or she no longer receives or intends to receive care in such accommodation.
9.83 The agreement should also stipulate:
- a) the value of any accrued or possible administrative charges, and where possible a breakdown of their calculation
- b) the means of redress if either party feels the other has broken the terms of the agreement
- c) the person’s responsibilities regarding maintenance and insurance of their home
- d) the person’s responsibility to notify the local authority of any change to their income, home or care and support
- e) the person’s responsibility to notify the local authority if they intend to rent or sell their property and if someone has gained or may gain a beneficial interest in their property
- f) the local authority’s responsibility to give the person 30 days written notice if it intends to cease to defer charges (or make loan instalments) under the agreement
- g) a clear explanation of the consequences of taking out a DPA for the person and their property, including anybody who may reside in the property
- h) the equity limit of their security (as discussed above in the section entitled ‘how much can be deferred’) and the scope for this to change upon revaluation of the security used for the DPA
- i) the process for varying any part of the agreement
- j) the process by which the local authority can require a re-valuation of a person’s chosen form of security
9.84 Local authorities should ensure at a minimum that people sign or clearly and verifiably affirm they have received adequate information on options for paying for their care, that they understand how the DPA works and understand the agreement they are entering into; and that they have had the opportunity to ask questions about the contract. A term reflecting this should be included in the agreement itself.
9.85 Local authorities will need to consider whether the deferred payment agreements they enter into are regulated credit agreements to which the Consumer Credit Act 1974 (CCA) and Financial Services and Markets Act 2000 (FSMA) apply.
9.86 The scope of ‘regulated credit agreements’ is set out in article 60B of the Financial Services and Markets Act 2000 (Regulated Activities) Order 2001 (RAO). A credit agreement is regulated unless exempt, and there are a number of exemptions in articles 60C to 60H of the RAO. It is likely that most DPAs will fall within such an exemption. If the agreement is regulated, it will need to comply with all applicable requirements of the CCA. In addition, the local authority will need a relevant permission from the Financial Conduct Authority (FCA), and to comply with the FCA’s rules and principles, unless the exclusion in article 72G of the RAO applies ( if the credit agreement is within the scope of the Consumer Credit Directive FCA authorisation is required).
9.87 All deferred payment agreements will be subject to the Unfair Terms in Consumer Contracts Regulations 1999, so the terms will have to be written in plain, intelligible English and will not be binding if they are unfair to the borrowers. Local authorities will also have to ensure that they do not contravene the Consumer Protection from Unfair Trading Regulations 2008.
9.88 Under Section 79 of the Care Act, local authorities may delegate responsibility for deferred payment agreements to another body. This could potentially allow a number of local authorities to combine their collective resources and offer a regional solution tailored to the local conditions and the administrative burden they face. If a local authority chooses to exercise their powers for delegation, the local authority must satisfy itself that the body taking on responsibility for DPAs is complying with all appropriate regulations and guidance (including but not limited to those governing deferred payments). Any and all duties in this guidance document, in the regulations and in the relevant sections of the Care Act apply equally to any delegated authority as they do to local authorities. The local authority should also seek feedback from people entering into DPAs to satisfy themselves that the service being provided meets the standards expected of the local authority. In the case of delegation of responsibility, the local authority remains ultimately responsible for (and liable for) the DPA.
The local authority’s responsibilities whilst the agreement is in place
9.89 Local authorities must at a minimum provide people with 6-monthly written updates of the amount of fees deferred, of interest and administrative charges accrued to date, and of the total amount due and the equity remaining in the home (the ‘equity limit’ discussed in the section entitled at ‘how much can be deferred’ above). Local authorities should also provide the person with a statement on request within 28 days. Local authorities may provide updates on a more frequent basis at their discretion. The update should set out the amount deferred during the previous period, alongside the total amount deferred to date, and should also include a projection of how quickly someone would deplete all equity remaining in their chosen form of security up to their equity limit.
9.90 Local authorities should reassess the value of the chosen form of security once the amount deferred exceeds 50% of the security (and periodically thereafter), and adjust the equity limit and review the amount deferred if the value has changed.
9.91 Local authorities may offer people a way to check their statement at any point in the year via an online facility.
9.92 Local authorities may choose to develop advice and guidance around maintaining a home, renting, and income. Local authorities may also offer services/ products to help the person meet the requirements for maintenance and insurance, but cannot compel a person to take on their product. Local authorities must accept reasonable alternative maintenance and insurance services.
Case study 6:
For illustrative purposes, we have used an interest rate of 3.5%. After 6 months, Lucille receives her first statement. It confirms she has deferred a total of £13,900, including £110 in interest and £100 in administration fees.
At this point, the local authority revalues her property and finds its value has increased to £170,000. Based on the amount deferred and her care costs, her equity would afford her just over 4 and a half more years’ care at this price.
Contractual responsibilities on the individual whilst the agreement is in place
9.93 The deferred payment agreement sets out various contractual requirements on the individual as well as on the local authority. These are set out briefly in sections above, but the person’s consequent responsibilities are recapped in more detail in the paragraphs below.
9.94 If the local authority is exercising its right to require the adult to make a contribution from income, it should include in the legal agreement provisions requiring the person to notify the local authority of any changes in their income.
9.95 The agreement should also contain provisions requiring the adult to notify the authority of changes in their need for care and support, if those changes are ones which will mean that the authority must or is entitled to stop making further instalments under the agreement or to alter the amount of the instalments.
9.96 Similarly if the agreement has been entered into on the basis that the adult’s property has not been disregarded for the purposes of the financial assessment in section 17 and it is a term of the agreement that the local authority will cease making or reduce the amount of instalments it makes, the agreement should require the person to inform the authority of changes which mean that the property may be disregarded.
9.97 The local authority should include in a contract provisions requiring someone to ensure that appropriate arrangements are in place to maintain their home whilst they are in care. In particular, the contract should require that their home is maintained adequately, and require someone to have in place an arrangement for regular maintenance to take place. Local authorities should also require the person to have adequate insurance for their property. If their home is to be left empty for an extended period of time, the person will need to ensure their insurance covers this adequately and that any terms required by the insurer are met.
9.98 The local authority must include in a contract provisions which require the person to obtain the authority’s consent before allowing someone to move into the property after the agreement has been made. In these circumstances, the local authority may (if it is reasonable to do so) require written consent from the person which places the debt owed to the local authority above any beneficial interest they may accrue in the property.
Termination of agreement
9.99 A deferred payment agreement can be terminated in 3 ways:
- a) at any time by the individual, or someone acting on their behalf, by repaying the full amount due (this can happen during a person’s lifetime or when the agreement is terminated through the deferred payment agreement holder’s death)
- b) when the property (or form of security) is sold and the authority is repaid [see note 6]
- c) when the person dies and the amount is repaid to the local authority from their estate
Note 6
In the case that a deferred payment agreement is agreed on the basis of a form of security other than property, local authorities will need to make provision in the agreement for conclusion of the deferred payment agreement in the event that the given security is disposed of/comes to fruition.
9.100 All 3 scenarios for the termination of the agreement are discussed below, alongside the various options for repayment. On termination, the full amount due (including care costs, any interest accrued and any administrative or legal fees charged) must be paid to the local authority.
9.101 If a person decides to sell their home, they should notify the local authority during the sale process. They will be required to pay the amount due to the local authority from the proceeds of the sale, and the local authority will be required to relinquish the charge on their property.
9.102 A person may decide to repay the amount due to the local authority from another source, or a third party may elect to repay the amount due on behalf of the individual. In either case, the local authority should be notified of the person’s/the third party’s intention in writing, and the local authority must relinquish the charge on the property on receipt of the full amount due.
9.103 If the deferred payment is terminated due to the person’s death, the amount due to the local authority must be either paid out of the estate or paid by a third party. A person’s family or a third party may wish to settle the debt to the local authority by other means of repayment (as may be the case if the family wanted to avoid having to sell the property or means of security), and the local authority must accept an alternative means of payment in this case, provided this payment covers the full amount due to the local authority.
9.104 The executor of the will or administrator of the estate can decide how the amount due is to be paid; either from the person’s estate (usually via the sale of the house or potentially via a life assurance policy) or from a third party source.
9.105 A local authority should wait at least 2 weeks following the person’s death before approaching the executor with a full breakdown of the total amount deferred (but a family member or the executor can approach the local authority to resolve the outstanding amount due prior to this point).
9.106 Responsibility for arranging for repayment of the amount due (in the case of payment from the estate) falls to the executor of the will.
9.107 Interest will continue to accrue on the amount owed to the local authority after the individual’s death and until the amount due to the local authority is repaid in full.
9.108 If terminated through a person’s death, the amount owed to a local authority under a deferred payment agreement falls due 90 days after the person has died. After this 90-day period, if a local authority concludes active steps to repay the debt are not being taken, for example if the sale is not progressing and a local authority has actively sought to resolve the situation (or the local authority concludes the executor is wilfully obstructing sale of the property), the local authority may enter into legal proceedings to reclaim the amount due to it. Further information on debt recovery is included at Annex D of this guidance.
9.109 In whichever circumstance an agreement is terminated, the full amount due to the local authority must be repaid to cover all costs accrued under the agreement, and the person (and/or the third party where appropriate) must be provided with a full breakdown of how the amount due has been calculated. Once the amount has been paid, the local authority should provide the individual with confirmation that the agreement has been concluded, and confirm (where appropriate) that the charge against the property has been removed.
Person-centred care and support planning
This section includes chapters 10 to 13 and has information on:
- 10. Care and support planning
- 11. Personal budgets
- 12. Direct payments
- 13. Review of care and support plans
10. Care and support planning
This chapter provides guidance on sections 24 and 25 of the Care Act 2014, and includes:
- when to undertake care and support planning
- what it means to ‘meet needs’, and considerations in deciding how to meet needs
- how to undertake care and support planning, and support planning
- production of the plan
- Involving the person
- authorising others (including the person) to prepare the plan
- care planning for people who lack capacity
- minimising and authorising a deprivation of liberty (DOL) for people who lack capacity
- combining plans
- sign-off and assurance
- protecting property of adults being cared for away from home
10.1 Care and support should put people in control of their care, with the support that they need to enhance their wellbeing and improve their connections to family, friends and community. A vital part of this process for people with ongoing needs which the local authority is going to meet is the care and support plan or support plan in the case of carers (henceforth referred to as ‘the plan’).
10.2 The person must be genuinely involved and influential throughout the planning process, and should be given every opportunity to take joint ownership of the development of the plan with the local authority if they wish, and the local authority agrees. There should be a default assumption that the person, with support if necessary, will play a strong pro-active role in planning if they choose to. Indeed, it should be made clear that the plan ‘belongs’ to the person it is intended for, with the local authority role being to ensure the production and sign-off of the plan to ensure that it is appropriate to meet the identified needs.
10.3 The personal budget in the plan will give everyone clear information regarding the costs of their care and support and the amount that the local authority will make available, in order to help people to make better informed decisions as to how needs will be met. The ability to meet needs by taking a direct payment must be clearly explained to the person in a way that works best for them, so that they can make an informed decision about the level of choice and control they wish to take over their care and support. This should mean offering the choice more than once in the process and enabling that choice by providing examples of how others have used direct payments, including via direct peer support, for example from user-led organisations.
10.4 Some people will need assistance to make plans and decisions, and to be involved in the planning process. The modern care and support system should routinely enable supported decision making, where options and choices are presented simply and clearly. Independent advocates (if used) must be instructed early in the assessment and planning process for those who have substantial difficulty in engaging with the care system, and have no other means of accessing appropriate support through friends or relatives to facilitate their involvement. If the person’s substantial difficulty only becomes apparent during the assessment, an advocate must be instructed as soon as this becomes known (see chapter 7).
10.5 Ultimately, the guiding principle in the development of the plan is that this process should be person-centred and person-led, in order to meet the needs and achieve the outcomes of the person in ways that work best for them as an individual or as part of a family. Both the process and the outcomes should be built holistically around people’s wishes and feelings, their needs, values and aspirations, irrespective of the extent to which they choose or are able to actively direct the process.
Definitions
10.6 This chapter applies to people in need of care and support and carers equally, unless specifically stated. It should be read in conjunction with the other chapters in this section (personal budgets, direct payments and review of care plans).
10.7 Unless otherwise stated, this chapter (and subsequent chapters in the section of ‘Person Centred Care and Support Planning’) applies to everyone whose needs are being met by the local authority, regardless of the setting in which the needs are met. For example, people in care homes must also receive a care and support plan and personal budget.
10.8 For the purposes of this chapter ‘the plan’ means either the care and support plan (in the case of adults with care and support needs) or the support plan (in the case of carers). When to undertake care and support planning, and support planning
10.9 Following the needs and carer’s assessment and determination of eligibility (see chapter 6), a plan must be provided where a local authority is required to meet needs under section 18 or 20(1) of the Care Act, or decides to meet needs under section 19(1) or (2) and 20(6) of the Act. Where a local authority is required to meet needs under section 117 of the Mental Health Act 1983 this chapter should be read in conjunction with chapter 34 of the Mental Health Act 1983 Code of Practice (on the Care Programme Approach) and Refocusing the Care Programme Approach.
What does it mean to ‘meet needs’?
10.10 ‘Meeting needs’ is an important concept under the Act and moves away from the previous terminology of ‘providing services’. This enables a greater variety of approaches in how needs can be met, developed through care and support planning as described in this chapter. The concept of ‘meeting needs’ is intended to be broader than a duty to provide or arrange a particular service. Because a person’s needs are specific to them, there are many ways in which their needs can be met. The intention behind the legislation is to encourage this diversity, rather than point to a service or solution that may be neither what is best nor what the person wants. The purpose of the care and support planning process is to agree how a person’s needs should be met, and therefore how the local authority will discharge its duty, or its power, to do so.
10.11 There are a number of broad options for how needs could be met, and the use of one or more of these will depend on the circumstances. Section 8(2) of the Act gives some examples of ways of meeting needs, and would cover:
- the local authority directly providing some type of support, for example by providing a reablement or short-term respite service
- making a direct payment, which allows the person to purchase their own care and support
- some combination of the above, for example the local authority arranging a homecare service whilst also providing a direct payment to meet other needs
10.12 Where the local authority provides or arranges for care and support, the type of support may itself take many forms. These may include more traditional ‘service’ options, such as care homes or homecare, but may also include other types of support such as assistive technology in the home or equipment/adaptations, and approaches to meeting needs should be inclusive of less intensive or service-focused options.
10.13 Needs may be met through types of care and support which are available universally, including those which are not directly provided by the local authority. For example, in some cases needs could be met by a service which is also made available as part of a local authority’s plans for preventing or reducing needs for care and support (under Section 2 of the Act). Needs could also be met, for example, by putting a person in contact with a local community group or voluntary sector organisation.
10.14 The examples of how needs can be met listed in the Act are not exhaustive, but cover the most common means of meeting needs. In addition, there are other methods which may be suitable for meeting a person’s needs, for example by arranging an individual service fund (see chapter 11 on personal budgets which also includes detail on individual service funds). This is a budget held by a provider, rather than by the local authority or the individual. The local authority makes a payment to the provider, which then holds a budget over which the individual has control.
10.15 The local authority may also consider whether it can effectively meet a person’s needs by ‘brokering’ a service on behalf of an individual in certain cases. ‘Brokering’ services are commonly offered by organisations which are independent of the local authority, and may be accessed by any person wishing to find care. However, the local authority may also provide such support where it meets a person’s needs. ‘Brokering’ would involve the local authority supporting an individual to make a choice about the provider of their care, and to enter into a contract with that provider. The local authority would not need to hold the contract with the provider, but would be required to assure itself that the chosen provider and terms of the contract were appropriate to meet the person’s needs.
10.16 The local authority would remain under the duty to meet a person’s eligible needs, and so would need to be satisfied both that this was an effective way of meeting those needs, and that the person was in agreement to this approach being used. It is likely that ‘brokering’ would only be an effective way of meeting a person’s needs in exceptional circumstances, for example where a person is fully funding their own care and wishes to retain control of the contract with their provider, but wants the local authority to meet their needs and the local authority has agreed to do so. If there is a risk that a person’s needs would not be met effectively by means of ‘brokering’, the local authority should discount it as an option and proceed with other ways of meeting that person’s needs, such as direct commissioning of services from a provider. In considering such an option, the local authority should also have regard to the likelihood of the person continuing to be willing and able to manage such arrangements in the future, including their ability to pay the charges due (for example, to mitigate against a future loss of capacity or disposal of their assets, such that the local authority may be required to take over the contract with the provider). The local authority would continue to support the person in meeting any other needs, offering ongoing support and keeping the arrangements under review to ensure that the needs were met. The person would have a care and support plan as usual.
10.17 The individual’s position in this approach would in some respects be akin to a person who had taken a direct payment to commission their own services, in that they would hold their own contract with a provider whilst the local authority is under a duty to meet their needs.
10.18 The difference would be that in the case of a direct payment, the money for commissioning the service comes from the local authority, whereas in the case of ‘brokering’ it comes from the individual directly. This option, therefore, would only likely be of use for meeting the needs of people who are fully funding their own care but ask the local authority to meet their eligible needs, and who are not using alternative arrangements such as an individual service fund.
Case study: Using discretionary powers to meet needs
Mrs Pascal, who is frail and elderly, was admitted to hospital after a fall. The hospital has established that Mrs Pascal currently has no care and support plan in place and made contact with the local authority to arrange a needs assessment. The local authority assesses that she has eligible needs which will be best met in a care home setting.
The local authority undertakes a financial assessment which finds that Mrs Pascal’s finances are above the limit for financial support from the local authority. The authority provides her with information and advice about her options. Mrs Pascal expresses extreme nervousness about seeking a placement on her own as she has struggled with managing her personal finances in recent times and does not have any family who are able to support her.
After a consultation, both Mrs Pascal and her local authority agree that support with arranging and managing a care placement would be beneficial for her wellbeing and would adequately meet her eligible needs. The authority arranges for Mrs Pascal to meet a trusted brokerage organisation which discusses her needs and arranges a contract with a care home on behalf of Mrs Pascal that she is very happy with.
Considerations in meeting needs
10.19 However the local authority is meeting needs, the principles in this chapter should be followed, such as ensuring the process is person-centred, and involving and taking all reasonable steps to agree the plan with the person.
10.20 The local authority must take into consideration the individual’s preferences. The authority should consider the person’s goals in approaching the authority for support, and the level or nature of support desired. Where the person wishes to take more control over their own care and support, this should be reflected in the route taken. Similarly, where the person asks for more local authority support (for example, because they lack the skills or confidence to engage with the provider market and do not have family or friends who are willing and/or able to support them with this), the authority should respond accordingly in the decision taken about how needs will be met.
Relationship with other services
10.21 Local authorities should also have regard to how needs may be met beyond the provision, or arrangement, of services by the authority. A person may already be in receipt of care and support which meets their needs (whether self-funded and arranged or not). For example, needs may be met by a carer, in an educational establishment or by another institution other than the local authority. In these circumstances the local authority remains under a duty to meet the person’s eligible needs. If however, the alternative means of meeting the needs is in place and the authority is satisfied that this alternative means is, in fact, meeting the person’s eligible needs, then the authority may not actually have to arrange or provide any services to comply with that duty.
10.22 However, the local authority should nonetheless record those needs through the assessment process, determine whether the needs meet the eligibility criteria and keep under review whether the authority needs to do anything in order to comply with its duty to meet the person’s eligible needs (for example, if the alternative services being provided to meet the needs cease or the authority is no longer satisfied that the alternative services adequately meet the person’s needs).
10.23 Sections 21 to 23 of the Act set out the limitations on the circumstances in which local authorities may meet care and support needs. In particular, they make clear that local authorities must not meet needs by providing or arranging any health service or facility which is required to be provided by the NHS, or doing anything under the Housing Act 1996. The aim of these provisions is to avoid duplication in the provision of services and facilities, and provide clarity about the limits of care and support, and the circumstances in which care and support should be provided as opposed to health services or housing services (or vice versa).
10.24 There may be other services to which a person is entitled under other legislation (but which could also be provided as part of the provision of care and support), which a local authority is not specifically prohibited from providing under the Act. Where there is a risk of overlapping entitlements (for example, where 2 different organisations may be under a duty to provide a service in relation to the same needs), local authorities should take steps to support the individual to access the support to which they are entitled under other legislation. This may include, for example, helping the person to access some disability-related benefits and allowances. It may also include working with the housing authority to ensure that there is a clear process in place for access to disabled facilities grants to avoid the risk of duplication of work in meeting the same needs.
10.25 The duty to meet eligible needs is not discharged just because a person has another entitlement to a different service which could meet those needs, but of which they are not availing themselves. The needs remain ‘unmet’ (and so the local authority remains under a duty to meet them) until those needs are actually met by the relevant service bring provided or arranged. Local authorities should therefore consider how to inform and advise people on accessing any such entitlements at the earliest stage possible, as well as working collaboratively with other local services to share information.
Needs met by a carer
10.26 Local authorities are not under a duty to meet any needs that are being met by a carer. The local authority must identify, during the assessment process, those needs which are being met by a carer at that time, and determine whether those needs would be eligible. But any eligible needs met by a carer are not required to be met by the local authority, for so long as the carer continues to do so. The local authority should record in the care and support plan which needs are being met by a carer, and should consider putting in place plans to respond to any breakdown in the caring relationship.
Other considerations
10.27 In determining how to meet needs, the local authority may also take into reasonable consideration its own finances and budgetary position, and must comply with its related public law duties. This includes the importance of ensuring that the funding available to the local authority is sufficient to meet the needs of the entire local population. The local authority may reasonably consider how to balance that requirement with the duty to meet the eligible needs of an individual in determining how an individual’s needs should be met (but not whether those needs are met). However, the local authority should not set arbitrary upper limits on the costs it is willing to pay to meet needs through certain routes – doing so would not deliver an approach that is person-centred or compatible with public law principles. The authority may take decisions on a case-by-case basis which weigh up the total costs of different potential options for meeting needs, and include the cost as a relevant factor in deciding between suitable alternative options for meeting needs. This does not mean choosing the cheapest option; but the one which delivers the outcomes desired for the best value.
Non-eligible needs
10.28 Where the local authority is not required to meet needs, it nonetheless may use its powers to meet any other needs. This may include, for example, meeting needs which are not ‘eligible’ (for example, those which do not meet the eligibility criteria), or meeting eligible needs in circumstances where the duty does not apply (for example, where the person is ordinarily resident in another area). Where the local authority exercises such a power to meet other needs, the same duties would apply regarding the next steps, and therefore a plan must be provided.
10.29 If the local authority decides not to use its powers to meet other needs, it must give the person written explanation for taking this decision, and should give a copy to their advocate if the person requests. If the person cannot request this, then a copy should be given to the person’s advocate or appropriate individual if this in the best interests of the person. This explanation must also include information and advice on how the person can reduce or delay their needs in future. This should be personal and specific advice based on the person’s needs assessment and not a generalised reference to prevention services or signpost to a general web-site. For example, this should involve consideration of alternative ways in which a person could reduce or delay their care and support needs, including signposting to support within the local community. Authorities may choose to provide this information after the eligibility determination, in which case this need not be repeated again. At whatever stage this is done, in all cases the person must be given a written explanation of why their needs are not being met. The explanation provided to the person must be personal to and should be accessible for the person.
10.30 Where a local authority is meeting some needs, but not others, a combination of the 2 approaches above must be followed. The person must receive a care and support plan for the needs the local authority is required, or decides to meet that accords to the Act and this guidance, and which also includes a tailored package of information and advice on how to delay and/or prevent the needs the local authority is not meeting. This information should be given to the person in a format accessible to them so they are clear what needs are being met by the local authority.
How to undertake care and support planning, and support planning
10.31 The plan must detail the needs to be met and how the needs will be met, and will link back to the outcomes that the adult wishes to achieve in day-to-day life as identified in the assessment process and to the wellbeing principle in the Act. This should reflect the individual’s wishes, their needs and aspirations, and what is important to and for them, where this is reasonable. [footnote 37] This process is central to the provision of person-centred care and support that provides people with choice and control over how to meet their needs. The local authority should encourage creativity in planning how to meet needs, and refrain from judging unusual decisions as long as these are determined to meet needs in a reasonable way.
10.32 The guiding principle therefore is that the person be actively involved and is given every opportunity to influence the planning and subsequent content of the plan in conjunction with the local authority, with support if needed. Joint planning does not mean a 50:50 split; the person can take a bigger share of the planning where this is appropriate and the person wishes to do so. A further principle is that planning should be proportionate. The person should not be required to go through lengthy processes which limit their ability to be actively involved, unless there are very strong reasons to add in elements of process and decision-making. Wherever possible the person should be able to be fully involved in the development of their plan, and any revision if circumstances change, with minimum process.
Production of the plan
10.33 The plan should be person-centred, with an emphasis on the individual having every reasonable opportunity to be involved in the planning to the extent that they choose and are able. This requires the local authority to ensure that information is available in a way that is meaningful to the person, and that they have support and time to consider their options. A named contact or lead professional should be considered both as part of care planning, and in the final plan, so that the person knows how to contact the local authority. The planning choices offered should range from support for the person, to jointly develop their plan with the local authority alone or with their family, friends or whoever they may wish to involve (this might include web-based resources, written information and peer support), through to one-to-one support from a paid professional, such as a social worker which may be the same person who undertook the assessment.
10.34 Where the person has substantial difficulty in being actively involved with the planning process, and they have no family and friends who are able to facilitate the person’s involvement in the plan, the local authority must provide an independent advocate to represent and support the person to facilitate their involvement (see chapter 7). Likewise, where a person with specific expertise or training in a particular condition (for example, deafblindness) has carried out the assessment, someone with similar knowledge (and preferably the same person to ensure continuity) should also be involved in production of the plan.
10.35 In ensuring that the process is person-centred, the local authority should ensure that any staff responsible for developing the plan with the person are trained in the Mental Capacity Act if appropriate, familiar with best practice, and that there is sufficient local availability of independent advocacy and peer support, including access to social work advice.
10.36 When developing the plan, there are certain elements that must always be incorporated in the final plan, [unless excluded by the Care and Support (Personal Budget Exclusion of Costs) Regulations 2014]. These are:
- the needs identified by the assessment
- whether, and to what extent, the needs meet the eligibility criteria
- the needs that the authority is going to meet, and how it intends to do so
- for a person needing care, for which of the desired outcomes care and support could be relevant
- for a carer, the outcomes the carer wishes to achieve, and their wishes around providing care, work, education and recreation where support could be relevant
- the personal budget (see chapter 11)
- information and advice on what can be done to reduce the needs in question, and to prevent or delay the development of needs in the future
- where needs are being met via a direct payment (see chapter 12), the needs to be met via the direct payment and the amount and frequency of the payments
10.37 These requirements should not encourage lengthy process where this is not necessary, or fixed decisions that cannot be changed easily. The maximum flexibility should be incorporated to allow adjustment and creativity, for example by allowing people to include personal elements into their plan which are important to them (but which the local authority is not under a duty to meet), or by developing the plan in a format that works for the person rather than a standard template.
10.38 Consideration of the needs to be met should take a holistic approach that covers aspects such as the person’s wishes and aspirations in their daily and community life, rather than a narrow view purely designed to meet personal care needs.
10.39 Consideration of needs should also include the extent to which the needs or a person’s other circumstances may mean that they are at risk of abuse or neglect. The planning process may bring to light new information that suggests a safeguarding issue, and therefore lead to a requirement to carry out a safeguarding enquiry (see chapter 14). Where such an enquiry leads to further specific interventions being put in place to address a safeguarding issue, this may be included in the care and support plan.
10.40 In considering the person’s needs and how they may be met, the local authority must take into consideration any needs that are being met by a carer. The person may have assessed eligible needs which are being met by a carer at the time of the plan – in these cases the carer must be involved in the planning process. Provided the carer remains willing and able to continue caring, the local authority is not required to meet those needs. However, the local authority should record the carer’s willingness to provide care and the extent of this in the plan of the person and also the carer, so that the authority is able to respond to any changes in circumstances (for instance, a breakdown in the caring relationship) more effectively. Where the carer also has eligible needs, the local authority should consider combining the plans of the adult requiring care and the carer, if all parties agree, and establish if the carer requires an independent advocate.
10.41 Local authorities should have regard to how universal services and community-based and/or unpaid support could contribute to the factors in the plan, including support that promotes mental and emotional wellbeing and builds social connections and capital. This may require additional learning and development skills and competencies for social workers and care workers which local authorities should provide.
10.42 Authorities are free, and are indeed encouraged, to include additional elements in the plan where this is proportionate to the needs to be met and agreed with the person the plan is intended for. For example, some people may value having an anticipated review date built into their plan in order for them to be aware of when the review will take place. As detailed in the review chapter, it is the expectation that the plan is reviewed no later than every 12 months, although a light-touch review should be considered 6-8 weeks after the plan and personal budget have been signed off.
10.43 The plan should be proportionate to the needs to be met, and should reflect the person’s wishes, preferences and aspirations. However, local authorities should be aware that a ‘proportionate’ plan does not equate to a light-touch approach, as in many cases a proportionate plan will require a more detailed and thorough examination of needs, how these will be met and how this connects with the outcomes that the adult wishes to achieve in day-to-day life.
10.44 For example, the person may have fluctuating needs, in which case the plan should make comprehensive provisions to accommodate for this, as well as indicate what contingencies are in place in the event of a sudden change or emergency. This should be an integral part of the care and support planning process, and not something decided when someone reaches a crisis point. Furthermore, specific consideration should be given to how planning is conducted in end of life care.
10.45 In all cases, additional content to the plan must be agreed with the adult and any other person that the adult requests, and should be guided by the person the plan is intended for. There should also be no restriction or limit on the type of information that the plan contains, as long as this is relevant to the person’s needs and/or outcomes. It should also be possible for the person to develop their plan in a format that makes sense to them, rather than this being dictated by the recording requirements of the local authority.
Case study: Fluctuating needs
Miss S has Multiple Sclerosis and requires a frame or wheelchair for mobility. Miss S suffers badly with fatigue, but for the majority of the time she feels able to cope with daily life with a small amount of care and support. However, during relapses she has been unable to sit up, walk or transfer, has lost the use of an arm or lost hervision completely. This can last for a few weeks, and happens 2 or 3 times a year; requiring 24 hour support for all daily activities.
In the past, Miss S was hospitalised during relapses as she was unable to cope at home. However, for the past 3 years, she has received a care and support package that include direct payments which allows her to save up one month’s worth of 24 hour care for when she needs it, and this is detailed in the care and support plan.
Miss S can now instantly access the extra support she needs without reassessment and has reassurance that she will be able to put plans in place to cope with any fluctuating needs. She has not been hospitalised since.
10.46 In developing the plan, the local authority must inform the person which, if any, of their needs may be met by a direct payment (see chapter 12). In addition to this, the local authority should provide the person (and/or their independent advocate or any other individual supporting the person, if relevant and if the person wishes this) with appropriate information and advice concerning the usage of direct payments, how they differ from traditional services, and how the local authority will administer the payment (for example an explanation of the direct payment agreement or contract, and how it will be monitored). This advice should also include detail such as:
- the ability for someone else (such as a carer) to receive and manage the direct payment on behalf of the person
- the ability to request to pay a close family member to provide care and/or administration and management of the direct payment if the local authority determines this to be necessary
- the difference between purchasing regulated and unregulated services (for example regarding personal assistants)
- explanation of responsibilities that come with being an employer, managing the payment, and monitoring arrangements and how these can be managed locally without being a burden
- signposting to direct payment support and support organisations available; in the area (for example, employment, payroll, admin support, personal assistants, peer support)
- that there is no curtailment of choice on how to use the direct payment (within reason), with the aim to encourage innovation
- local examples and links to people successfully using direct payment in similar circumstances to the person (providing these groups agree)
- the option to have needs met by a mixed package of direct payments and other forms of support or arrangements
10.47 This information provided upfront should assist the person to decide whether they wish to request a direct payment to meet some or all of their needs and should also be available at various points in the process to ensure people have the best opportunities possible to consider how direct payments may be of benefit to them. However the person chooses to have their needs met, whether by direct payment, by the provision of local authority-arranged or directly provided care and support, or third-party provision, or a mix of these, there should be no constraint on how the needs are met as long as this is reasonable. The local authority has to satisfy itself that the decision is an appropriate and legal way to meet needs, and should take steps to avoid the decision being made on the assumption that the views of the professional are more valid than those of the person. Above all, the local authority should refrain from any action that could be seen to restrict choice and impede flexibility.
10.48 It is important that people are allowed to be very flexible to choose innovative forms of care and support, from a diverse range of sources, including quality providers but also ‘non-service’ options such as Information and Communication Technologies (ICT) equipment, club membership, and massage. Lists of allowable purchases should be avoided as the range of possibilities should be very wide and will be beyond what the local authority is able to list at any point in time. While many authorities may choose to operate lists of quality accredited providers to help people choose (for example some authorities include trading standards-style ‘buy with confidence’ approaches) the use of such lists should not be mandated as the only choice offer to people. Limited lists of ‘prescribed providers’ that are only offered to the person on a ‘take it or leave it’ basis do not fit with the government’s vision of personalised care and should be avoided.
Involving the person
10.49 In addition to taking all reasonable steps to agree how needs are to be met, the local authority must also involve the person the plan is intended for, the carer (if there is one), and/or any other person the adult requests to be involved. Where the person lacks capacity to ask the authority to do that, the local authority must involve any person who appears to the authority to be interested in the welfare of the person and should involve any person who would be able to contribute useful information. An independent advocate must be provided if section 67 of the Act applies (see chapter 7). The person, and their carers, will have the best understanding of how the needs identified fit into the person’s life as a whole and connect to their overall wellbeing (see chapter 1). They are well placed to consider and identify which care and support options would best fit into their lifestyle and help them to achieve the day to day outcomes they identified during the assessment process. In practice, local authorities should give consideration to include a prompt to the person during the initial stages of the planning process to ask whether there is anyone else that the person wishes to be involved. Where the person lacks capacity, the local authority should make a best interests decision about who else should be involved.
10.50 The level of involvement should be agreed with the individual and any other party they wish to involve and should reflect their needs and preferences. This may entail local authorities involving the person through regular planning meetings, or there may be instances where remote involvement is just as effective, such as over the telephone, through video conferencing, or other means. In other circumstances, local authorities will need to seek the support of speech and language therapists or other specialists such as interpreters. Some people will need little help to be involved, others will need much more. Social workers or other relevant professionals should have a discussion with the person to get a sense of their confidence to take a lead in the process and what support they feel they need to be meaningfully involved.
10.51 The person should be supported to understand what is being discussed and what options are available for them. The local authority should make sure that a person’s lack of confidence to take a lead in the process should not limit the extent to which they can play an active role, if they wish to do so. In all cases, people should be allowed to gain support from individuals who they choose to assist their involvement in the planning process. Where they have substantial difficulty in being actively involved in the process, then they should be assisted by a family member or friend. If the person already has an advocate, whose role has been to support the person on matters not under the Care Act, then it may be appropriate for them to support the individual’s involvement and represent them. However, if an advocate is required under the Mental Capacity Act 2005 (MCA) as well as the Care Act, then the instruction, appointment and qualification of the advocate must meet the requirements of the MCA.
10.52 The local authority must instruct an independent advocate if there is no one to represent and support the person’s involvement (see chapter 7). This duty arises if the person would, without the representation and support of an independent advocate, experience substantial difficulty in any of the following:
- understanding relevant information
- retaining that information
- using or weighing that information as part of the process of being involved
- communicating their views, wishes or feelings (whether by talking, using sign language, or any other means)
10.53 For example, there may be cases where a person who has substantial difficulty in the above, has no family or friend who can help, and therefore requires an independent advocate to understand the relevant information provided by the local authority, and to be able to use it to effectively plan for their care and support.
10.54 Genuine involvement will aid the development of the plan, increase the likelihood that the options selected will effectively support the adult in achieving the outcomes that matter to them, and may limit disputes as people involved will be fully aware and have agreed to decisions made. Local authorities should ensure that staff have appropriate learning and development opportunities in order to be able to facilitate involvement in the development of the plan.
Authorising others (including the person) to prepare the plan jointly with the local authority
10.55 As stated earlier in this guidance, it is important that local authorities give people every opportunity to prepare their own plan in conjunction with the local authority if they wish.
10.56 Where a plan is being jointly prepared by the local authority and the person whose plan it is, or the local authority and a third party, the local authority should ensure that relevant information is shared securely, promptly and in accordance to the Data Protection Act to allow the plan to be prepared in a timely fashion.
10.57 A partnership approach should be taken, where each partner knows their role and the parties supported to identify options and choose between them. For example, the person may need help to weigh up different service options to understand what each involves and to be able to choose the most appropriate and least restrictive option possible.
10.58 The local authority should also consider cases or circumstances where it may not be appropriate to jointly prepare the plan. For example, a person may not wish their family to be involved, or the authority may be aware that family members may have conflicting interests, or the person may have asked the local authority to prepare the plan with someone who lives far away from the person and even with the assistance of email, phone and other methods of communication is unable to prepare the plan in a timely fashion. The test for allowing the person and others to prepare the plan jointly with the local authority should start with the presumption that the person at the heart of the care plan should give consent for others to do so; and should also have safeguarding principles embedded to ensure that there is no conflict of interest between the person and the third party they wish to involve to prepare the plan jointly with. Where a person lacks capacity and cannot consent to third parties jointly preparing the plan, the local authority must always act in the best interests of the person requiring care and support.
Planning for people who lack capacity
10.59 Good, person-centred care planning is particularly important for people with the most complex needs. Many people receiving care and support have mental impairments, such as dementia or learning disabilities, mental health needs or brain injuries. The principles of the Care Act apply equally to them, in addition to the principles and requirements of the Mental Capacity Act 2005 (MCA) if the person lacks capacity (see also chapter 7 on independent advocacy).
10.60 The MCA requires local authorities to assume that people have capacity and can make decisions for themselves, unless otherwise established. Every adult has the right to make his or her own decisions in respect of his or her care plan, and must be assumed to have capacity to do so unless it is proved otherwise. This means that local authorities cannot assume that someone cannot make a decision for themselves just because they have a particular medical condition or disability.
10.61 The local authority must support the person to understand and weigh up information, to offer choices and help people to exercise informed choice. A person must be given all practicable help to make the specific decision before being assessed as lacking capacity to make their own decisions.
10.62 Local authorities must understand that people have the right to make what others might regard as an unwise or unusual decision. Everyone has their own values, beliefs and preferences which may not be the same as those of other people. People cannot be treated as lacking capacity for that reason. Sometimes the care and support plan may have unusual aspects; the question to explore is whether it will meet the assessed needs and lead to the desired outcomes.
10.63 If a local authority thinks a person may lack capacity to make a decision or a plan, even after they have offered them all practicable support, a social worker or other suitably qualified professional should carry out a capacity assessment in relation to the specific decision to be made. For example, the local authority may assess whether the person has the capacity to decide whether family members should be involved in their care planning or whether the person has the capacity to decide on whether a particular support option will meet their needs.
10.64 Where an individual has been assessed as lacking capacity to make a particular decision, then the local authority must commence care planning in the person’s best interests under the meaning of the MCA. Furthermore a person making a decision concerning a plan on behalf of a person who lacks capacity must consider whether it is possible to make a decision or a plan in a way that would be less restrictive of the person’s rights and freedoms of action. Any restriction must be in the person’s best interests and necessary to prevent harm to the person, and a proportionate response to the likelihood of the person suffering harm and the seriousness of that harm.
10.65 The duty to involve the person remains throughout the process. If lack of capacity is established, it is still important that the person is involved as far as possible in making decisions. Planning should always be done with the person and not for them; should always start by the identification of their wishes, feelings, values and aspirations, not just their needs, and should always consider their wellbeing in the wider context of their rights to security, to liberty, and to family life.
10.66 Where a person has substantial difficulty in being fully involved in their care planning or lacks capacity to agree and consent to the care plan, they may be supported by family members or friends. If a person has no family or friend who is able to facilitate the person’s involvement available and willing to do so, then an independent advocate must be appointed. A friend or family member is not appropriate to facilitate the person’s involvement if the person has capacity to decide who they wish to support them and chooses not to be supported by that individual. If the person lacks such capacity, then the local authority must decide on the suitability of the friend or family member to act in the person’s best interests. The role of the independent advocate is to:
- support and represent the person to facilitate their involvement in decision-making in the care planning process
- assist the person in communicating their wishes, feelings, value and aspirations where possible
- to challenge the local authority’s decisions if necessary to represent the person’s wishes or to promote the person’s wellbeing and rights to security, liberty and family life
Minimising and authorising deprivation of liberty (DOL) for people who lack capacity
10.67 In line with the least restrictive principle in the MCA, local authorities and others drawing up plans must minimise planned restrictions and restraints on the person as much as possible. Sections 5 and 6 of the MCA provides legal protection for acts of restraint only if the act is necessary to prevent harm to the person, a proportionate response to the likelihood of the person suffering harm and the seriousness of that harm, and in the person’s best interests. Planned restrictions and restraints must be documented and reported to a social worker to agree. Disagreements should be resolved through formal Best Interests meetings, involving a wide range of people, including family members and/or an advocate to support and represent the person.
10.68 However, if the degree and intensity of restrictions and restraints are so significant that they amount to a deprivation of liberty, this must be authorised under the Deprivation of Liberty Safeguards (DOLS) under the MCA.
10.69 Developing effective person-centred processes for planning in line with the guidance and the Act in general may in most cases avoid circumstances where a deprivation of liberty will arise.
10.70 The difference between a deprivation of liberty and restraint is one of degree, intensity and duration, not necessarily nature or substance. The Supreme Court has clarified that there is a deprivation of liberty for the purposes of Article 5 of the European Convention on Human Rights in the following circumstances: the person is under continuous supervision and control and is not free to leave, and the person lacks capacity to consent to those arrangements. [footnote 38] The precise scope of the term ‘deprivation of liberty’ is not fixed. It develops over time in accordance with case law.
10.71 In DOLS cases, MCA/DOLS staff and the independent advocate must go through the following steps when conducting the care planning process:
- familiarise themselves with the provisions of the MCA, particularly the 5 principles and specifically the ‘least restrictive’ principle
- when designing and implementing new care and support plans for people lacking capacity, be alert to any restrictions and restraint which may be a degree or intensity that means a person is being, or is likely to be, deprived of their liberty (following the revised test supplied by the Supreme Court)
- where a potential deprivation of liberty is identified at the planning or commissioning care stage, a full exploration of the alternative ways of providing the care and/or treatment should be undertaken, in order to identify any less restrictive ways of providing that care which will avoid a deprivation of liberty
- where the plan for an individual lacking capacity will unavoidably result in a deprivation of liberty judged to be in the person’s best interests, this must be authorised before being implemented
10.72 If the person will be accommodated in a hospital or care home, the local authority can issue a deprivation of liberty authorisation under Schedule 1A to the MCA (DOL authorisation). If the person will be accommodated in other settings, a Court of Protection Order under the MCA to authorise the deprivation of liberty is needed. If the independent advocate is concerned that there is a risk of deprivation of liberty which has not been authorised, the advocate should raise this with the local authority. The advocate may make an application to the Court of Protection (with the Court’s permission) if they are dissatisfied with the local authority’s response.
Combining plans
10.73 Local authorities should not develop plans in isolation from other plans (such as plans of carers or family members, or Education, Health and Care plans) and should have regard to all of the person’s needs and outcomes when developing a plan, rather than just their care and support needs. [footnote 39]
10.74 The local authority should attempt to establish where other plans are present, or are being conducted and seek to combine plans, if appropriate. This should be considered early on in the planning process (at the same time as considering the person’s needs and how they can be met in a holistic way) to ensure that the package of care and support is developed in a way that fits with what support is already being received or developed. For example, this may be where the plan can be combined with a plan being developed to meet other needs, or where a plan might usefully be combined with that of a carer, or family member. In all circumstances, the plan should only be combined if all parties to whom it is relevant agree and understand the implications of sharing data and information. It is the responsibility of the local authority to obtain consent from all parties involved, and the combination of plans should aim to maximize outcomes for all involved.
10.75 Where one of the plans to be combined is for a child (below 18 years old), the child must have capacity to agree to the combination, or if lacking capacity, the local authority must be satisfied that the combination of plans would be in the child’s best interests. Often it will be; but where there is a conflict of interest (for example a parent does not wish to support their 17 year old daughter’s wish for greater independence) it may not be (see chapter 16 on transition to adult care and support).
10.76 The local authority may be undertaking care and or support planning for 2 people in the same household who require independent advocacy to facilitate their involvement. If both people have the capacity to consent to having the same advocate, and the advocate and the local authority both consider there is no conflict of interest, then the same advocate may support and represent the 2 people. If either person lacks the capacity to consent to having the same advocate, the advocate and local authority must both consider that using the same advocate would not raise a conflict of interest and would be in the best interests of both persons (see chapter 7).
10.77 Consideration should also be given to how plans could be combined where budgets are pooled, either with people in the same household, or between members of a community with similar care needs where this is appropriate and all parties agree (see chapter 11 on personal budgets). Pooling arrangements should not be restricted to individuals using the same provider. Networks of pooling arrangements should be encouraged to bring groups of people together in a more effective manner.
10.78 Where it has been agreed to combine the plan with plans relating to other people, it is important that the individual aspects of each person’s plan are not lost in the process of combining plans. The combined plan should reflect the individual needs and circumstance for each person involved, as well as any areas where a joint approach has been agreed to meet needs in a more effective way.
10.79 One key area where plans can be combined cases where the person is receiving both local authority care and support and NHS health care is an example would be a person with mental disorder who meets the criteria for care and support under the multi-agency Care Programme Approach. The introduction of personal health budgets in health, similar to personal budgets in social care, provides a powerful tool to enable integrated health and care provision which focuses on what matters most to the person. Local authorities should provide information to the person of the benefits of combining health and social care support, and seek to work with health colleagues to combine health and care plans wherever possible.
10.80 In combining plans, whether among people or organisations (such as health, education or housing), it is vital to avoid duplicating process or introducing multiple monitoring regimes. Information sharing should be rapid and seek to minimise bureaucracy. Local authorities should work alongside health and other professionals (such as housing) where plans are combined to establish a ‘lead’ organisation who undertakes monitoring and assurance of the combined plan (this may also involve appointing a lead professional and detailing this in the plan so the person knows who to contact when plans are combined). Particular consideration should be given to ensuring that processes are aligned, coherent and streamlined, to avoid confusing the person with different systems (see Chapter 14 on integration and cooperation).
Sign-off and assurance
10.81 The local authority must take all reasonable steps to agree with the person the manner in which the plan details how needs will be met, before the authority signs off the plan. Therefore, it should not introduce measures that place any undue burden on the person, especially where the person or third party is preparing the plan in conjunction with the local authority. The local authority should therefore avoid developing processes that undermine the joint preparation of plans, such as excessive quality control. For example, a local authority may have arrangements or contract with outside organisations/individuals to provide peer support for planning. If so, an important part of this contract should be around having agreement as to non-restrictive approaches that enhance the quality of plans and the local authority’s trust in the detail as well as removing issues that can cause delay and problems.
10.82 The local authority’s role where the person or third-party are undertaking the preparation of the plan jointly with the local authority includes overseeing and providing guidance for the completion of the plan; and ensuring that the plan sufficiently meets needs, is appropriate and represents the best balance between value for money and maximisation of outcomes for the person. For example, this may involve providing materials and approaches to support people jointly preparing the plan with the local authority. Where the local authority is preparing the plan on behalf of the person, or delegating this to a third-party to do so, the best interests of the person must be reflected throughout.
10.83 The local authority must take all reasonable steps to reach agreement with the person for whom the plan is being prepared. Wherever possible, local authority sign-off should occur when the person, any third party involved in the preparation of the plan and the local authority have agreed on the factors within the plan, including the final personal budget amount (which may have been subject to change during the planning process), and how the needs in question will be met. This is a key part of the planning process and the agreement should be recorded and a copy placed within the plan. Where an independent advocate has been involved, they should not be asked to sign off the plan – this is the responsibility of the local authority.
10.84 While there is no defined timescale for the completion of the care and support planning process, the plan should be completed in a timely fashion, proportionate to the needs to be met. Local authorities must ensure that sufficient time is taken to ensure the plan is appropriate to meet the needs in question, and is agreed by the person the plan is intended for. The planning process should not unduly delay needs being met.
10.85 Due regard should be taken to the use of approval panels in both the timeliness and bureaucracy of the planning and sign-off process. In some cases, panels may be an appropriate governance mechanism to sign-off large or unique personal budget allocations and/or plans. Where used, panels should be appropriately skilled and trained, and local authorities should refrain from creating or using panels that seek to amend planning decisions, micro-manage the planning process or are in place purely for financial reasons. Local authorities should consider how to delegate responsibility to their staff to ensure sign-off takes place at the most appropriate level. In cases or circumstances where a panel is to be used, and where an expert assessor has been involved in the care and support journey, the same person or another person with similar expertise should be part of the panel to ensure decisions take into account complex or specialist issues.
10.86 In the event that the plan cannot be agreed with the person, or any other person involved, the local authority should state the reasons for this and the steps which must be taken to ensure that the plan is signed-off. This may require going back to earlier elements of the planning process. People must not be left without support while a dispute is resolved. If a dispute still remains, and the local authority feels that it has taken all reasonable steps to address the situation, it should direct the person to the local complaints procedure. However, by conducting person-centred planning and ensuring genuine involvement throughout, this situation should be avoided.
10.87 Upon completion of the plan, the local authority must give a copy of the final plan which should be in a format that is accessible to the person for whom the plan is intended, any other person they request to receive a copy, and their independent advocate if they have one and the person agrees. This should not restrict local authorities from making the draft plan available throughout the planning process; indeed in cases where a person is preparing the plan in conjunction with the local authority, the plan should be in their possession. Consideration should also be given to sharing key points of the final plan with other professionals and supporters, with the person’s consent (for example, as part of the person’s health record), or sharing the plan in the best interests of a person who lacks capacity to decide on this matter.
Protecting property of adults being cared for away from home
10.88 Local authorities must take all reasonable steps to protect the moveable property of an adult with care and support needs who is being cared for away from home, in a hospital or in accommodation such as a care home, and who cannot arrange to protect their property themselves; this could include their pets as well as their personal property (for example, private possessions and furniture). Local authorities must act where it believes that if it does not take action there is a risk of moveable property being lost or damaged.
10.89 For example, protecting property may include arranging for pets to be looked after when securing premises for someone who is having their care and support needs provided away from home in a care home or hospital, and who has not been able to make other arrangements for the care of their home or pets.
10.90 In order to protect moveable property in these circumstances the local authority may enter the property, at reasonable times, with the adult’s consent; but reasonable prior notice to enter should be given. If the adult lacks the capacity to give consent to the local authority entering the property, consent should be sought from a person authorised under the Mental Capacity Act 2005 to give consent on the adult’s behalf. This might be:
- an attorney (also known as a donee with lasting power of attorney) that is someone appointed under the Mental Capacity Act 2005 who has the legal right to make decisions (for example, decisions about their care and support) within the scope of their authority on behalf of the person (the donor) who made the power of attorney
- a deputy (also known as a court-appointed deputy) that is a person appointed by the Court of Protection under the Mental Capacity Act 2005 to take specified decisions on behalf of someone who lacks capacity to take those decisions themselves
- the Court of Protection
10.91 If the adult in question lacks capacity and no other person has been authorised to act on their behalf, then the local authority must act in the best interests of the adult in accordance with section 4 of the Mental Capacity Act 2005.
10.92 If a third party tries to stop an authorised entry into the home then they will be committing an offence, unless they can give a good reason for why they are obstructing the local authority in protecting the adult’s property. Committing such an offence could, on conviction by a Magistrates’ Court, lead to the person being fined up to a maximum fine not exceeding level 4 on the standard scale. If a local authority intends to enter a home then it must give written authorisation to an officer of the council and that person must be able to produce it if asked for.
10.93 The local authority has no power to apply for a warrant to carry out their duties to protect property. The enforcement power is prosecution for unreasonable obstruction. However, if the Court decides the obstruction is reasonable then the local authority would have no further power to force entry.
10.94 This duty on the local authority lasts until the adult in question returns home or makes their own arrangements for the protection of property or until there is no other danger of loss or damage to property; whichever happens first. Often a one off event is required such as the re-homing of pets or ensuring that the property is secured. However, if costs are incurred or if there are ongoing costs the local authority can recover any reasonable expenses they incur in protecting property under this duty from the adult whose property they are protecting.
Links to external resources
- Care and Support Planning Guide
- Delivering Care and Support Planning Guide (PDF, 2.59MB)
- Essential criteria of support planning
- Good practice in support planning and brokerage, PPF, 2008
- Peer support and personalisation
- Planning together – peer support and self-directed support
- Support planning and brokerage with older people and people with mental health difficulties
- Rethinking support planning – ideas for an alternative approach
- Empower and enable – a people led approach to support planning
- Individual Service Funds and contracting for flexible support (PDF, 2.26MB)
- Using Individual Service Funds to deliver personalised care and support
- Personal health Budget Toolkit
- Employing your own care and support
- A toolkit to help you employ your own personal assistants
- The Common Core Principles to Self Care
- Personal budgets and mental health
- PHB Toolkit:Implementing effective care planning
- Carers’ rights
- Involve Me: involving people with profound and multiple learning disabilities in decision making
- At a glance 42: Personalisation briefing: Implications for lesbian, gay, bisexual and transgendered (LGBT) people
- Personalisation through person-centre planning
11. Personal budgets
This chapter provides guidance on Section 26 of the Care Act 2014 and the Care and Support (Personal Budget Exclusion of Costs) Regulations 2014, including:
- the personal budget
- elements of the personal budget
- elements of care and support that are excluded from the personal budget
- calculating the personal budget
- agreeing the final budget
- use of the personal budget
- use of a carer’s personal budget
- carers’ personal budgets where the adult being cared for does not have eligible needs
- appeals/disputes
11.1 Personal budgets are a key part of the government’s aspirations for a person-centred care and support system. Independent research shows that where implemented well, personal budgets can improve outcomes and deliver better value for money. [footnote 40] [footnote 41] [footnote 42] [footnote 43]
11.2 The Act places personal budgets into law for the first time, making them the norm for people with care and support needs.
11.3 The personal budget is the mechanism that, in conjunction with the care and support plan, or support plan, enables the person, and their advocate if they have one, to exercise greater choice and take control over how their care and support needs are met. It means:
- knowing, before care and support planning begins, an estimate of how much money will be available to meet a person’s assessed needs and, with the final personal budget, having clear information about the total amount of the budget, including proportion the local authority will pay, and what amount (if any) the person will pay
- being able to choose from a range of options for how the money is managed, including direct payments, the local authority managing the budget and a provider or third party managing the budget on the individual’s behalf (an individual service fund), or a combination of these approaches
- having a choice over who is involved in developing the care and support plan for how the personal budget will be spent, including from family or friends
- having greater choice and control over the way the personal budget is used to purchase care and support, and from whom
11.4 It is vital that the process used to establish the personal budget is transparent so that people are clear how their budget was calculated, and the method used is robust so that people have confidence that the personal budget allocation is correct and therefore sufficient to meet their care and support needs. The allocation of a clear upfront indicative (or ‘ball-park’) allocation at the start of the planning process will help people to develop the plan and make appropriate choices over how their needs are met.
11.5 The process of allocating the personal budget should be completed in a timely manner, proportionate to the needs to be met. At all times the person should be informed where they are in the care planning process, what will happen next and the likely timeframes.
11.6 This chapter applies to people in need of care and support and carers equally, unless specifically stated.
The personal budget
11.7 Everyone whose needs are met by the local authority, whether those needs are eligible, or if the authority has chosen to meet other needs, must receive a personal budget as part of the care and support plan, or support plan. The personal budget is an important tool that gives the person clear information regarding the money that has been allocated to meet the needs identified in the assessment and recorded in the plan. An indicative amount should be shared with the person, and anybody else involved, at the start of care and support planning, with the final amount of the personal budget confirmed through this process. The detail of how the personal budget will be used is set out in the care and support plan, or support plan. At all times, the wishes of the person must be considered and respected. For example, the personal budget should not assume that people are forced to accept specific care options, such as moving into care homes, against their will because this is perceived to be the cheapest option.
11.8 This allows the person, and anybody else the person wishes, to make informed decisions about how to meet their care and support needs. The person can choose for the personal budget allocation to remain with the local authority to arrange care and support on the person’s behalf, and in line with their wishes. Alternatively, if available locally, it can be placed with a third-party provider on the same basis, often called an individual service fund (ISF). Where an ISF-type arrangement is not available locally, the local authority should explore arrangements to develop this offer, and should be receptive to requests from personal budget recipients to create these arrangements with specified providers.
11.9 There may also be cases where a person prefers to use a mixed package of care and support. For example, this may be a direct payment to the person for some of their needs, with the remainder of the personal budget used to meet needs via local authority or third-party provision, or any combination of the above. The method of allocating the personal budget should be decided and agreed during the care and support planning process (see chapter 10). It is important that these arrangements can be subsequently adjusted if the person wishes this, with the minimum of procedure. The process for allocating and agreeing the personal budget via the planning process should be as straightforward and as timely as possible so that the person can access the budget without significant delay.
Elements of the personal budget
11.10 The personal budget must always be an amount sufficient to meet the person’s care and support needs, and must include the cost to the local authority of meeting the person’s needs which the local authority is under a duty to meet, or has exercised its power to do so. This overall cost must then be broken down into the amount the person must pay, following the financial assessment, and the remainder of the budget that the authority will pay.
11.11 The personal budget may also set out other amounts of public money that the person is receiving, such as money provided through a personal health budget. Local authorities should consider requests from individuals to present their personal budget in this way. Integrated health and care, and integration of other aspects of public support are the long-term vision of the government. This will provide the individual with a seamless experience, and can help to remove unnecessary bureaucracy and duplication that may exist where a person’s needs are met through money from multiple funding streams.
11.12 Local authorities must carry out their care and support responsibilities with a view to promoting integration with health and other related services (such as housing), and therefore should take a lead in driving the integration of support services for their population. For example, this may involve agreeing with partner organisations how to integrate budgets and to what extent, and the establishment of a lead organisation that agrees to oversee monitoring and assurance of all budgets the person is receiving.
11.13 Where a local authority is meeting the eligible needs of a person whose financial resources are above the financial limit, but who has requested the local authority meet their needs, the local authority may make a charge for putting in place the necessary arrangements to meet needs (see chapter 8 on charging and financial assessment). Where this occurs, the local authority should consider how best to set this information out to the person, in a format accessible to them. This fee is not part of the personal budget, since it does not relate directly to meeting needs, but it may be presented alongside the budget to help the person understand the total charges to be paid. For example, a local authority may wish to specify this in both the plan and the personal budget for the person so all parties are clear on how costs are allocated.
11.14 Similarly, there will be cases where a person or a third party on their behalf is making an additional payment (or a ‘top-up’) in order to be able to secure the care and support of their choice, where this costs more than the local authority would pay for such a type of care. In these cases, the additional payment does not form part of the personal budget, since the budget must reflect the costs to the local authority of meeting the needs. However, the local authority should consider how best to present this information to the individual, so that the total amount of charges paid is clear, and the link to the personal budget amount is understood.
Elements of care and support that are excluded from the personal budget
11.15 Regulations set out the cases or circumstances where the costs of meeting the needs of care and support do not have to be incorporated into the personal budget. Because both the care and support plan and personal budget are mechanisms to enable people to have greater choice and control over their care and support, there are not many instances where this exclusion will apply.
11.16 The Care and Support (Personal Budget Exclusion of Costs) Regulations 2014 set out that the provision of intermediate care and reablement services, for which the local authority cannot or chooses not to make a charge [footnote 44] must be excluded from the personal budget. This will mean that where either intermediate care or reablement is being provided to meet needs (for example, under section 18, 19 or 20 of the Act) the cost of this must not be included in the personal budget.
11.17 Intermediate care services are usually provided to patients, often older people, after leaving hospital or when they are at risk of being sent to hospital. The services are a link between places such as hospitals and people’s homes, and between different areas of the health and social care system – community services, hospitals, GPs and social care. ‘Reablement’ is a particular type of intermediate care, which has a stronger focus on helping the person to regain skills and capabilities to reduce their needs, in particular through the use of therapy or minor adaptations. There is a tendency for the terms ‘reablement’, ‘rehabilitation’ and ‘intermediate care’ to be used interchangeably. The National Audit of Intermediate Care categorises 4 types of intermediate care: crisis response – services providing short-term care (up to 48 hours); home-based intermediate care – services provided to people in their own homes by a team with different specialities but mainly health professionals such as nurses and therapists; bed-based intermediate care – services delivered away from home, for example, in a community hospital; and reablement – services to help people live independently, provided in the person’s own home by a team of mainly social care professionals (see chapter 2 – preventing, reducing or delaying needs).
11.18 Three of the 4 types of intermediate care have historically been clinician-led and provided by health staff, with reablement being provided by local authorities. However, these are not concrete, mutually-exclusive categories – and, furthermore, with greater integration and co-operation between health and local authorities, there should be greater use of qualified staff from health and social care working together to provide intermediate care.
11.19 Local authorities should not include additional elements that would not normally be classified as intermediate care or reablement into this exclusion. Indeed, the Act restricts the regulations into specifying only care and support which the local authority cannot charge for, or chooses not to charge for. This ensures that long-term care and support will always be part of the personal budget, and in future, count towards the cap on care costs. Also, broader rehabilitation services could be included to an individual to meet identified health needs as part of a joint personal budget across health and social care.
11.20 Intermediate care/reablement should usually be provided as a free, universal service under section 2 of the Act, and therefore would not contribute to the personal budget amount. However, in some circumstances, a local authority may choose to combine either service with aspects of care and support to meet eligible or ongoing needs, which would require a personal budget to be developed. Removing the cost of provision of intermediate care/reablement from the personal budget in these scenarios ensures that the allocation of both services is applied uniformly across all local authorities, and in future people progress towards the cap on care costs in a fair and consistent way.
11.21 In cases where intermediate care/ reablement is provided to meet needs under section 18 or 20(1) or under section 19(1) or 20(6), either in isolation or combined with longer-term care and support, the plan should describe what the package consists of and how long it will last. This will help the person understand what is being provided to meet their needs. However, the person should not receive a personal budget, unless there are other forms of care and support being provided under these sections. In these cases, the personal budget amount must not include the cost of intermediate care/reablement which are provided free of charge.
Calculating the personal budget
11.22 It is important to have a consistent method for calculating personal budgets that provides an early indication of the appropriate amount to meet the identified needs to be used at the beginning of the planning process. Local authorities should ensure that the method used for calculating the personal budget produces equitable outcomes to ensure fairness in care and support packages regardless of the environment in which care and support takes place, for example, in a care home or someone’s own home. Local authorities should not have arbitrary ceilings to personal budgets that result in people being forced to accept to move into care homes against their will.
11.23 There are many variations of systems used to arrive at personal budget amounts, ranging from complex algorithmic-based resource allocation systems (RAS), to more ‘ready-reckoner’ approaches. Complex RAS models of allocation may not work for all client groups, especially where people have multiple complex needs, or where needs are comparatively costly to meet, such as in the case of deaf-blind people. It is important that these factors are taken into account, and that a ‘one size fits all’ approach to resource allocation is not taken. If a RAS model is being used, local authorities should consider alternative approaches where the process may be more suitable to particular client groups to ensure that the personal budget is an appropriate amount to meet needs.
11.24 Regardless of the process used, the most important principles in setting the personal budget are transparency, timeliness and sufficiency. This will ensure that the person, their carer, and their independent advocate if they have one, is fully aware of how their budget was calculated, that they know the amount at a stage which enables them to effectively engage in care and support planning, and that they can have confidence that the amount includes all relevant costs that will be sufficient to meet their identified needs in the way set out in the plan. The local authority should also explain that the initial indicative allowance can be increased or decreased depending on the decisions made during the development of the plan. This should prevent disputes from arising, but it must also be possible for the person, carer or independent advocate (on the person’s behalf) to challenge the local authority on the sufficiency of the final amount. These principles apply to both the indicative upfront budget and the final signed=off personal budget that forms part of the care and support plan.
Transparency
Authorities should make their allocation processes publicly available as part of their general information offer, or ideally provide this on a bespoke basis for each person the authority is supporting in a format accessible to them. This will ensure that people fully understand how the personal budget has been calculated, both in the indicative amount and the final personal budget allocation. Where a complex RAS process is used, local authorities should pay particular consideration to how they will meet this transparency principle, to ensure people are clear how the personal budget was derived.
Timeliness
It is crucial when calculating the personal budget to arrive at an upfront allocation which can be used to inform the start of the care and support planning process. This ‘indicative budget’ will enable the person to plan how the needs are met. After refinement during the planning process, this indicative amount is then adjusted to be the amount that is sufficient to meet the needs which the local authority is required to meet under section 18 or 20(1), or decides to meet under section 19(1) or (2) or 20(6). This adjusted amount then forms the personal budget recorded in the care plan.
Sufficiency
The amount that the local authority calculates as the personal budget must be sufficient to meet the person’s needs which the local authority is required to meet under section 18 or 20(1), or decides to meet under section 19(1) or (2) or 20(6) and must also take into account the reasonable preferences to meet needs as detailed in the care and support plan, or support plan.
11.25 The Act states the personal budget must be an amount that is the cost to the local authority of meeting the person’s needs. In establishing the ‘cost to the local authority’, consideration should therefore be given to local market intelligence and costs of local quality provision to ensure that the personal budget reflects local market conditions and that appropriate care that meets needs can be obtained for the amount specified in the budget. To further aid the transparency principle, these cost assumptions should be shared with the person so they are aware of how their personal budget was established. Consideration should also be given as to whether the personal budget is sufficient where needs will be met via direct payments, especially around any other costs that may be required to meet needs or ensure people are complying with legal requirements associated with becoming an employer (see chapter 12). There may be concern that the ‘cost to the local authority’ results in the direct payment being a lesser amount than is required to purchase care and support from the local market due to local authority bulk purchasing and block contract arrangements. However, by basing the personal budget on the cost of quality local provision, this concern should be allayed.
11.26 However, a request for needs to be met via a direct payment does not mean that there is no limit on the amount attributed to the personal budget. There may be cases where it is more appropriate to meet needs via directly-provided care and support, rather than by making a direct payment. For example, where there is no local market for a particular kind of care and support that the person wishes to use the direct payment for, except for services provided by the local authority. It may also be the case where the costs of an alternate provider arranged via a direct payment would be more than the for what the local authority would be able to arrange the same support, whilst achieving the same outcomes for the individual.
11.27 In all circumstances, consideration should be given to the expected outcomes of each potential delivery route. It may be that by raising the personal budget to allow a direct payment from a particular provider, it is expected to deliver much better outcomes than local authority delivered care and support, or there may be other dynamics such as the preferred option reducing the need for travel costs, or out of hours care. In addition, efficiencies to the local authority (for example through an individual making their own arrangements) should also be considered. Decisions should therefore be based on outcomes and value for money, rather than purely financially motivated.
11.28 In cases where making a direct payment is a more expensive option to meet needs, the care plan should be reviewed to ensure that it is accurate and that the personal budget allocation is correct. The authority should work with the person, their carer and independent advocate (if there is one) to agree on how best to meet their care and support needs. It may be that the person can take a mixture of direct payment and local authority-arranged care and support, or the local authority can work with the person to discuss alternate uses for the personal budget. Essentially, these discussions will take place during the planning process and local authorities should ensure that their staff are appropriately trained to support personalised care and support, and to facilitate decision-making.
Example: Costs of direct payments 1
Andrew has chosen to meet his needs by receiving care and support from a PA. The local authority has a block contract with an agency which has been providing support to Andrew twice per week. Andrew would now like more flexibility in the times at which he receives support in order to better meet his needs by allowing him to undertake other activities and consider employment.
He therefore requests a direct payment so that he can make his own arrangements with another agency, which is happy to arrange a much more flexible and personalised service, providing Andrew with the same care worker on each occasion, and at a time that works best for him.
The cost to the local authority of the block contracted services is £13.50 per hour. However, the more flexible support costs £18 per hour (inclusive of other employment costs). The local authority therefore increases Andrew’s direct payment from £67.50 to £90 per week to allow him to continue to receive the care he requires. The solution through a direct payment delivers better outcomes for Andrew and therefore the additional cost is reasonable and seen as value for money as it may delay future needs developing.
The local authority also agrees it is more efficient for them to allow Andrew to arrange and commission the hours he wants to receive support and handle the invoicing himself.
Example: Costs of direct payments 2
Following George’s assessment of needs, the local authority work out an indicative personal budget of £135 per week, based on their block contract rate of £13.50 per hour as an indication of the potential costs to meet his needs.
During care planning, George states that he has a neighbour that has recently trained to become a personal assistant, and George indicates a preference to use a direct payment to employ the neighbour instead of an arranged service.
The local authority is satisfied that George will be able to manage the direct payment, and that he understands his responsibilities as an employer. George wants to pay the PA above the living wage and has provisionally agreed a hourly rate of £9 per hour.
The local authority agrees to this as George agrees that it will meet his needs and outcomes. The final personal budget is adjusted to £110 per week which factors in the new hourly rate, plus an additional allowance for employment responsibilities (PAYE, NI, insurance)
Use of the personal budget
11.29 The person should have the maximum possible range of options for managing the personal budget, including how it is spent and how it is utilised. Directing spend is as important for those choosing the council-managed option or individual service fund as for those choosing direct payments. Evidence suggests that people using council-managed personal budgets are currently not achieving the same level of outcomes as those using direct payments, and in too many cases do not even know they have been allocated a personal budget.
11.30 There are 3 main ways in which a personal budget can be deployed:
- as a managed account held by the local authority with support provided in line with the persons wishes
- as a managed account held by a third party (often called an individual service fund or ISF) with support provided in line with the persons wishes [footnote 45]
- as a direct payment
11.31 In addition, a person may choose a ‘mixed package’ that includes elements of some or all 3 of the approaches above. Local authorities must ensure that whatever way the personal budget is used, the decision is recorded in the plan and the person is given as much flexibility and choice as is reasonably practicable in how their needs are met. The mixed package approach can be a useful option for people who are moving to direct payments for the first time. This allows a phased introduction of the direct payment, giving the person time to adapt to the direct payment arrangements.
11.32 Where ISF approaches to personal budget management are available locally, the local authority should provide people with information and advice on how the ISF arrangement works and any contractual requirements, how the provider(s) will manage the budget on behalf of the person, and advice on what to do if a dispute arises. Consideration should be given to using real local examples that illustrate how other people have benefitted from ISF arrangements.
11.33 Where there are no ISF arrangements available locally, the local authority should consider establishing this as an offer for people. Additionally, the local authority should reasonably consider any request from a person for an ISF arrangement with a specified provider.
Examples: Using individual service funds
Sally really enjoys dancing and night clubs and she needs support for this. Sally’s ISF arrangement with her provider has given her the flexibility to employ staff that also like to do this, and they are paid time and a half after 11:00pm. The ISF arrangement also allows Sally to convert ‘standard hours’ into ‘enhanced hours’, for example, 6 standard hours equals 4 enhanced hours. Sally can plan late nights out knowing what it ‘costs’ from her allocation of 24 standard hours support, which is calculated from her personal budget.
Brian’s ISF arrangement with his provider allows him to save up and then convert the hours of his support into money to purchase personal trainer time at a local gym.
In addition to promoting wellbeing in the areas of emotional and social wellbeing and personal relationships, these arrangements also demonstrate the local authority’s regard for the importance of beginning with the assumption that an individual is best-placed to judge their own wellbeing.
11.34 Local authorities should also give consideration to how choice could be increased by people pooling their budgets together. For example, this may include pooling budgets of people living in the same household such as an adult and carer, or pooling budgets of people within a community with similar care and support needs, or aspirations. Pooling budgets in circumstances such as this may deliver increased choice, especially where managed budgets are concerned. Developing networks of ‘budget poolers’ could help create dynamic groups of people working together to meet needs.
11.35 Evidence suggests that in most cases people need to know the amount of their budget, be able to choose how it is managed, and have maximum flexibility in how it is used to achieve the best outcomes. Therefore the process and practice for personal budgets should follow the key principles of self-directed support. Local authorities should aim to develop a range of means to enable anyone to make good use of direct payments and where people choose other options, should ensure local practice that maximises choice and control (for example use of Individual Service Funds). Local authorities should also take care not to inadvertently limit options and choices. For example ‘pre-paid cards’ can be a good option for some people using direct payments, but must not be used to constrain choice or be only available for use with a restricted list of providers.
Use of a carer’s personal budget
11.36 Specific consideration should be given to how a personal budget will be used by carers. The Act specifies that a carer’s need for support can be met by providing care to the person they care for. However, decisions on for whom a particular service is to be provided may affect issues such as whether the service is chargeable, and who is liable to pay any charges. It is therefore important that it is clear to all individuals involved whose needs are intended to be met by a particular type of support, to whom the support will be provided directly, and therefore who may pay any charges due. Where a service is provided directly to the adult needing care, even though it is to meet the carer’s needs, then that adult would be liable to pay any charge, and must agree to doing so. Section 14 of the Act makes clear that where the needs are met by providing care and support direct to the adult needing care, the charge may not be imposed on the carer.
11.37 Decisions on which services are provided to meet carers’ needs, and which are provided to meet the needs of the adult for whom they care, will therefore impact on which individual’s personal budget includes the costs of meeting those needs. Local authorities should make this decision as part of the care planning process, in discussion with the individuals concerned, and should consider whether joint plans (and therefore joint personal budgets) for the 2 individuals may be of benefit.
11.38 Local authorities should consider how to align personal budgets where they are meeting the needs of both the carer and the adult needing care concurrently. Where an adult has eligible needs for care and support, and has a personal budget and care and support plan in their own right, and the carer’s needs can be met, in part or in full, by the provision of care and support to that person needing care, then this kind of provision should be incorporated into the plan and personal budget of the person with care needs, as well as being detailed in a care and support plan for the carer.
Examples: Flexible use of a carer’s personal budget
Conor has been caring for his wife, who is in a wheelchair with ME and arthritis, for the last 9 years. He does all the cooking, driving and general household duties for their household. Conor received a personal budget which he requested in the form of a direct payment from his local authority for a laptop to enable him to be in more regular contact through Skype with family in the US. This now enables Conor to stay connected with family he cannot afford to fly and see. This family support helps Connor with his ongoing caring role.
Divya has 4 young children and provides care for her father who is nearing the end of his life. Her father receives a direct payment, which he used to pay a family member for a period of time to give his daughter a break from her caring role. Divya received a carers’ direct payment, which she uses for her children to attend summer play schemes so that she get some free time to meet with friends and socialise when the family member providers care to her father. This gives Divya regular breaks from caring which are important to the family unit.
11.39 ‘Replacement care’ may be needed to enable a carer to look after their own health and wellbeing alongside caring responsibilities, and to take a break from caring. For example, this may enable them to attend their own health appointments, or go shopping and pursue other recreational activities. It might be that regular replacement care overnight is needed so that the carer can catch up on their own sleep. In other circumstances, longer periods of replacement care may be needed, for example to enable carers to have a longer break from caring responsibilities or to balance caring with education or paid employment. In these circumstances, where the form of the replacement care is essentially a homecare service provided to the adult needing care that enables the carer to take a break, it should be considered a service provided to the cared-for person, and thus must be charged to them, not the carer.
11.40 The carer’s personal budget must be an amount that enables the carer to meet their needs to continue to fulfil their caring role, and takes into account the outcomes that the carer wishes to achieve in their day to day life. This includes their wishes and/or aspirations concerning paid employment, education, training or recreation if the provision of support can contribute to the achievement of those outcomes. The manner in which the personal budget will be used to meet the carer’s needs should be agreed as part of the planning process.
11.41 Local authorities must have regard to the wellbeing principle of the Act, as it may be the case that the carer needs a break from caring responsibilities to look after their own physical/mental health and emotional wellbeing, social and economic wellbeing and to spend time with other members of the family and personal relationships. Whether or not there is a need for replacement care, carers may need support to help them to look after their own wellbeing. This may be, for example, a course of relaxation classes, training on stress management, gym or leisure centre membership, adult learning, development of new work skills or refreshing existing skills (so they might be able to stay in paid employment alongside caring or take up return to paid work), pursuit of hobbies such as the purchase of a garden shed, or purchase of a laptop so they can stay in touch with family and friends.
Carers’ personal budgets where the adult being cared for does not have eligible needs
11.42 The Act makes clear that the local authority is able to meet the carer’s needs by providing a service directly to the adult needing care. However, there may be instances where the adult being cared for does not have eligible needs, so does not have their own personal budget or care plan. In these cases, the carer must still receive a support plan which covers their needs, and how they will be met. This would specify how the carer’s needs are going to be met (for example, via replacement care to the adult needing care), and the personal budget would be for the costs of meeting the carer’s needs.
11.43 The adult needing care would not receive a personal budget or care plan, because no matter what the service is in practice, it is designed to meet the carer’s needs. However, it is essential that the person requiring care is involved in the decision-making process and agrees with the intended course of action.
11.44 In situations such as these, the carer could request a direct payment, and use that to commission their own replacement care from an agency, rather than using an arranged service from the local authority or a third party. The local authority should take steps to ensure that the wishes of the adult requiring care are taken into account during these decisions. For example, the adult requiring care may not want to receive replacement care in this manner.
11.45 If such a type of replacement care is charged for (and it may not be), then it would be the adult needing care that would pay, not the carer, because they are the direct recipient of the service. This is in part why it is so important that the adult needing care agrees to receiving that type of care. The decisions taken by the carer and adult requiring care and charging implications should be agreed and recorded in the support plan. If a dispute arises and the person refused to pay the charge, the local authority must, as far as it is feasible, identify some other way of supporting the carer.
11.46 For the purposes of charging, the personal budget which the carer receives must specify the costs to the local authority and the costs to the adult, based on the charging guidance (see chapter 8). In this case, ‘the adult’ refers to the carer, because they are the adult whose needs are being met. However, in instances where replacement care is being provided, the carer should not be charged; if charges are due to be paid then these have to be met by the adult needing care. Any such charges would not be recorded in the personal budget, but should be set out clearly and agreed by those concerned.
Disputes
11.47 The local authority should take all reasonable steps to limit disputes regarding the personal budget allocation. This will include through effective care and support planning, and transparency in the personal budget allocation process. Additionally, many disputes may be avoided by informing people of the timescales that are likely to be involved in different stages of the process. Keeping people informed how their case is progressing may help limit the number of disputes.
11.48 Current complaints provision for care and support is set out in regulations. [footnote 46] The provisions of the regulations mean that anyone who is dissatisfied with a decision made by the local authority can make a complaint about that decision and have that complaint handled by the local authority. The local authority must make its own arrangements for dealing with complaints in accordance with the 2009 regulations.
Links to external resources
- Adult social care minimum process framework
- The seven steps to being in control of my support
- Enabling risk, ensuring safety - self-directed support and personal budgets
- Self-directed support process - what good looks like
- Making resource allocation work in a financial environment
- Keeping personal budgets personal – learning from the experiences of older people, people with mental health problems and their carers
- Financial management of personal budgets
- Personal budgets – taking stock, moving forward
- Individual Serviced Funds (ISFs) and contracting for flexible support (PDF, 2.26MB)
- Integrating personal budgets - early learning, PHB Toolkit
- Integrating personal budgets - myths and misconceptions
- Progressing personalisation – a review of personal budgets and direct payments for carers
- Making it real - making progress towards personalised, community based support
- Choice and Control for All
- Improving personal budgets for older people
- Self-directed support: reducing process, increasing choice and control
- Resource Allocation Systems (RAS) Challenge
- Paths to personalisation in mental health
- 2nd National Personal Budget Survey
- Making it real for carers
12. Direct payments
This chapter covers:
- making direct payments available
- considerations for adults with and without capacity
- administering, monitoring and reviewing direct payments
- using the direct payment
- paying family members
- short-term and long-term care in a care home
- becoming an employer
- direct payments and hospital stays
- direct payments for local authority services
- direct payments in the form of pre-payment cards
- harmonisation of direct payments
- terminating direct payments
12.1 Direct payments are monetary payments made to individuals who request to receive one to meet some or all of their eligible care and support needs. The legislative context for direct payments is set out in the Care Act, Section 117(2C) of the Mental Health Act 1983 (the 1983 Act) and the Care and Support (Direct Payments) Regulations 2014.
12.2 Direct payments have been in use in adult care and support since the mid-1990s and they remain the Government’s preferred mechanism for personalised care and support. They provide independence, choice and control by enabling people to commission their own care and support in order to meet their eligible needs. [footnote 47]
12.3 Direct payments, along with personal budgets and personalised care planning, mandated for the first time in the Care Act, provide the platform with which to deliver a modern care and support system. People should be encouraged to take ownership of their care planning, and be free to choose how their needs are met, whether through local authority or third-party provision, by direct payments, or a combination of the 3 approaches.
12.4 For direct payments to have the maximum impact, the processes involved in administering and monitoring the payment should incorporate the minimal elements to allow the local authority to fulfil its statutory responsibilities. These processes must not restrict choice or stifle innovation by requiring that the adult’s needs are met by a particular provider, and must not place undue burdens on people to provide information to the local authority. An effective monitoring process should also go beyond financial monitoring, and include aspects such as identifying wider risks and issues, for example non-payment of tax, and provision of employers’ liability insurance where this is appropriate.
12.5 The local authority also has a key role in ensuring that people are given relevant and timely information about direct payments, so that they can make a decision whether to request a payment, and, if doing so, are supported to use and manage the payment appropriately. The route to a direct payment is for a person to request one, but the local authority should support the person’s right to make this request by providing information and advice as detailed above. People must not be forced to take a direct payment against their will, but instead be informed of the choices available to them.
12.6 This chapter should be read in conjunction with the sections on care and support planning and personal budgets (see chapters 10 and 11), and applies to people in need of care and support and carers equally, unless specifically stated.
Making direct payments available
12.7 The availability of direct payments should be included in the universal information service that all local authorities are required to provide. This should set out:
- what direct payments are
- how to request one including the use of nominated and authorised persons to manage the payment
- explanation of the direct payment agreement and how the local authority will monitor the use of the direct payment
- the responsibilities involved in managing a direct payment and being an employer;
- making arrangements with social care providers
- signposting to local organisations (such as user-led organisations and micro-enterprises) and the local authority’s own internal support, who offer support to direct payment holders, and information on local providers
- case studies and evidence on how direct payments can be used locally to innovatively meet needs [footnote 48]
12.8 This will allow people to be fully aware what direct payments are and whether they are something that are of interest. In addition to this general information, authorities must also explain to people what needs could be met by direct payments during the care and support planning process.
12.9 Local authorities have a crucial role to play in promoting the use of direct payments, and enabling people to make requests to receive direct payments in an efficient way. However, the gateway to receiving a direct payment must always be through the request from the person. Local authorities must not force people to take a direct payment against their will, or allow people to be placed in a situation where the direct payment is the only way to receive personalised care and support. However, local authorities are encouraged to prompt people to consider direct payments and how they could be used to meet needs.
Steps following a request to receive direct payments
12.10 It is expected that most requests to receive direct payments will occur during the care planning stage as this is when authorities must inform the person of the needs that could be met via direct payments. However, local authorities must consider requests for direct payments made at any time, and have clear and swift processes in place to respond to the requests. For example, a person may request a direct payment before a scheduled or anticipated review. In these cases, the local authority must assess the request on the same basis as a request made during care planning. In practice, it may be convenient to consider the request at the same time as a review of the care plan. In these cases, the review should be brought forward so as not to delay the consideration of the direct payment request (see chapter 13 on reviews). The steps to follow after receiving a request for a direct payment will depend on whether the person has been assessed as having capacity to make a decision about direct payments or not, which should have taken place at the assessment of needs (see chapter 6).
Assessing capacity
The following considerations should be made when assessing capacity:
- does the person have a general understanding of what decisions they need to make and how they need to make them?
- does the person have a general understanding of the consequences of making, or not making the decision?
- is the person able to understand, retain, use and weigh up all relevant information to support the decision?
- can the person communicate the decision? (this may involve the use of a specialist or independent advocate)
- is there need to bring in additional expertise to aid the assessment?
12.11 Mental capacity is the ability to make a decision. Under the 2005 Mental Capacity Act, a person lacks capacity in relation to a matter if, at the material time, they are unable to make a decision in relation to the matter because of an impairment of, or a disturbance in the functioning of, the mind or brain.
12.12 Assessments of capacity must always be made on a case-by-case basis, in relation to the specific decision to be made. Assumptions should not be made due to the existence of a particular condition, nor on whole groups of people.
12.13 Consideration should also be given to whether capacity is constant or likely to fluctuate. Where it is clear that fluctuating capacity is a known issue, or likely to be, this should be covered in the care plan which details the steps to take where capacity fluctuates. The Care and Support (Direct Payments) Regulations 2014 allow for direct payments to continue to be made in cases of fluctuating capacity (see paras. 12.67-12.68 on terminating direct payments).
Adults with capacity
12.14 Where the local authority is satisfied that the person has capacity to make a request for direct payments to cover some or all of their care needs, it must consider each of the 4 conditions in section 31 of the Care Act. These conditions need to be met in their entirety; a failure in one would result in the request to receive a direct payment being declined. The conditions are:
- the adult has capacity to make the request, and where there is a nominated person, that person agrees to receive the payments
- the local authority is not prohibited by regulations under section 33 from meeting the adult’s needs by making direct payments to the adult or nominated person
- the local authority is satisfied that the adult or nominated person is capable of managing direct payments either by himself or herself, or with whatever help the authority thinks the adult or nominated person will be able to access
- the local authority is satisfied that making direct payments to the adult or nominated person is an appropriate way to meet the needs in question
12.15 The authority must clarify at the earliest stage possible where the request originates from. The Care Act provides a power to enable direct payments to be made to the person in need of care and support, or a nominated person acting on their behalf if the adult so requests. Where a nominated person has been requested to receive the direct payment, the authority should involve the nominated person in any appropriate stages of the care planning journey, such as the development of the care plan, as long as the person with care needs agrees to this. Where the person does not specifically request this involvement, the local authority should consider whether to encourage the person to make that request. During this process, the nominated person should receive information regarding the local authorities direct payments processes, as well as information and advice on using and managing the direct payment, so that the nominated person understands their legal obligations as the direct payment recipient to act in the best interests of the person requiring care and support (see paras. 12.48-12.51 on becoming an employer). The local authority must also satisfy itself that the nominated person meets the conditions in Section 31 of the Act.
Adults lacking capacity
12.16 In cases where the person in need of care and support has been assessed as lacking capacity to request the direct payment, an authorised person can request the direct payment on the person’s behalf. In these cases, the local authority must satisfy itself that the person meets the 5 conditions as set out in section 32 of the Care Act.
12.17 As with direct payments for people with capacity, each of these conditions must be met in their entirety. Failure to meet any of the conditions would result in the request being declined. The conditions are:
- where the person is not authorised under the Mental Capacity Act 2005 but there is at least one person who is so authorised, that person who is authorised supports the person’s request
- the local authority is not prohibited by regulations under section 33 from meeting the adult’s needs by making direct payments to the authorised person, and if regulations under that section give the local authority discretion to decide not to meet the adult’s needs by making direct payments to the authorised person, it does not exercise that discretion
- the local authority is satisfied that the authorised person will act in the adult’s best interests in arranging for the provision of the care and support for which the direct payments under this section would be used
- the local authority is satisfied that the authorised person is capable of managing direct payment by himself or herself, or with whatever help the authority thinks the authorised person will be able to access
- the local authority is satisfied that making direct payments to the authorised person is an appropriate way to meet the needs in question
Consideration of the request
12.18 After considering the suitability of the person requesting the direct payment against the appropriate conditions in the Care Act, the local authority must make a determination whether to provide a direct payment. Where accepted, the decision should be recorded in the care plan, or support plan. Where refused, the person or person making the request should be provided with written reasons that explain the decision, and be made aware of how to appeal the decision through the local complaints process.
12.19 The Care Act defines one of the conditions to be met is that the direct payment is an appropriate way to meet the needs in question (or, in respect of after-care services, an appropriate way to discharge its duty under section 117 of the 1983 Act). [footnote 49] Local authorities must not use this condition to arbitrarily decline a request for a direct payment. For example, there may be instances where a person is obliged to receive services as a condition of mental health legislation (including a community treatment order, guardianship or leave of absence from hospital under the Mental Health Act or provisions in other mental health legislation). In these cases, although the person is being obliged to receive services rather than choosing to present for services, it may still be appropriate to give the person the responsibility of meeting their needs via a direct payment, if this is what is requested. Particular consideration should be given to these cases when applying the conditions set out in the Act. In all cases, appropriateness is for local authorities to determine, although it is expected that in general, direct payments are an appropriate way to meet most care and support needs.
12.20 However, there may be cases where a direct payment is not appropriate to meet needs. The Regulations set out that direct payments cannot be made to people subject to a court order for a drug or alcohol treatment program or similar schemes (schedule 1 of the Regulations).
12.21 A further condition is that the local authority must be satisfied that the person is able to manage the direct payment by him or herself, or with whatever help or support the person will be able to access. Local authorities should therefore take all reasonable steps to provide this support to whoever may require it. To comply with this, many local authorities have contracts with voluntary or user-led organisations that provide support and advice to direct payment holders, or to people interested in receiving direct payments. This condition should not be used to deny a person from receiving a direct payment without consideration of support needs. Consideration should also be given to involving a specialist assessor in determination of support requirements, in particular if one was used earlier in the care and support process (such as assessment).
12.22 In all cases, the consideration of the request should be concluded in as timely a manner as possible. Where the request for a direct payment has been declined, the person in need of care and support, and any other person involved in the request (for example, nominated or authorised person) should (subject to Data Protection Act requirements) receive the reasons in a format that is accessible to them. This should set out which of the conditions in the Care Act have not been met, the reasons as to why they have not been met, and what the person may need to do in the future to obtain a positive decision. The consideration stage should be performed as quickly as is reasonably practicable, and the local authority must provide interim arrangements to meet care and support needs to cover the period in question.
Case Study: Making direct payments support accessible
Abdul is a deafblind man; to communicate he prefers to use Braille, Deafblind Manual and email. He directly employs several staff through direct payments. He receives payroll support from his local direct payments support service. Abdul suggested ways to make direct payments management accessible to him. He communicates with the support service mainly via email but they also use Typetalk.
At the end of the month, Abdul emails the support service with details of the hours that his staff have worked. The support service work out any deductions from pay (such as National Insurance and Income Tax) and email him to tell him how much he should pay the staff via cheque. They then send him pay slips to be given to staff. The envelope that the payslips are sent in has 2 staples in the corner so that he knows who the letter is from. The payslips themselves are labelled in Braille so that he knows which staff to give them to.
Each quarter, the support service tells him how much he needs to pay on behalf of his employees in National Insurance and Income Tax. The service also fills in quarterly Inland Revenue paperwork. At the end of the year, the support service sends relevant information to the council, so that they are aware of how the direct payments are being spent.
Abdul has taken on only some of the responsibilities of employing people; he has delegated some tasks to the support service. Control still remains with Abdul and confidentiality is maintained by using accessible labelling. In terms of the wellbeing principle, the local authority has promoted Abdul’s control over his day-to-day life.
12.23 Where the request has been declined, the local authority should continue the care planning process so that it can seek to agree with the person how best to meet the needs, without the use of direct payments (see chapter 10 on care and support planning).
Administering direct payments
12.24 The local authority must be satisfied that the direct payment is being used to meet the care and support needs set out in the plan, and should therefore have systems in place to proportionally monitor direct payment usage to ensure effective use of public money. The Care and Support (Direct Payments) Regulations 2014 set out that the local authority must review the making of direct payments initially within 6 months, and thereafter every 12 months, and must not require information to be provided more often and in more detail than is reasonably required for the purpose of enabling the authority to know that making direct payment is still an appropriate way of meeting the needs, and that conditions upon which it is made are met. Local authorities should not design systems that place a disproportionate reporting burden upon the individual. The reporting system should not clash with the policy intention of direct payments to encourage greater autonomy, flexibility and innovation. For example, people should not be requested to duplicate information or have onerous monitoring requirements placed upon them. Monitoring should be proportionate to the needs to be met and the care package. Thus local authorities should have regard to lowering monitoring requirements for people that have been managing direct payments without issues for a long period.
12.25 The amount of the direct payment is derived from the personal budget as set out in the care and support plan, or support plan, and thus must be an amount which is sufficient to meet the needs the local authority has a duty or power to meet. The direct payment amount will reflect whether the person is required to make any financial contributions, or is requesting a direct payment for only a part of their care and support requirements. Local authorities cannot require financial contributions for a direct payment for after care services under the MHA; these must be provided without charge.
Example: Reduced monitoring
Gina has a stable condition and has been successfully managing her direct payment for over 2 years. The local authority therefore decides to reduce monitoring to the lowest level due to the low perceived risk (while still complying with the required review in the Act and Regulations). Gina is now considered to have the skills and experience to manage on her own unless the local authority request otherwise or information suggested otherwise comes to the attention of the local authority.
12.26 It is ultimately for authorities to decide whether payments are made on a gross or net basis in consultation with appropriate stakeholders. However, local authorities who operate systems of providing gross direct payments should consider the benefits of moving to net payments as these reduce transaction and process costs for both the authority and the person receiving the direct payment. [footnote 50]
12.27 The local authority should have regard to whether there will be costs such as recruitment costs, Employers’ National Insurance Contributions, and any other costs by reason of the way in which the adult’s needs will be met with the direct payment. [footnote 51] If these costs will be incurred their amount must be included in the personal budget (and thus direct payment) if it is appropriate for the adult to meet the needs in a way which incurs the costs. Some local authorities include one-off payments within the direct payment to cover these factors. In addition, other authorities have commissioned support services such as brokerage, payroll and employment advice as part of their general direct payment offer.
12.28 Where a direct payment recipient is using their payment to employ a personal assistant (PA) or other staff, the local authority should ensure that there are clear plans in place of how needs will be met in the event of the PA being absent, for example due to sickness, maternity or holiday. Local authorities still have a duty to ensure needs are being met, even if the person makes their own arrangements via the direct payment, so contingencies may be needed. Where appropriate, these should be detailed in the care and support plan, or support plan.
12.29 Specific information should also be given to people about the requirements to have plans in place for redundancy payments due to circumstances such as moving home, a change in care and support needs, or the result of the death of the direct payment holder, or care recipient. If the person meets needs by directly employing someone, they will be responsible for all costs of employment including redundancy payments and this should be made clear to people as part of the information and advice process before a decision is made whether to request direct payments. The local authority must ensure that the direct payment is sufficient to meet these costs if it is appropriate for the adult to meet their needs by employing someone.
12.30 Normally, if someone dies any employment liabilities will be met by the person’s estate, but with direct payments local authorities and adults have freedom to develop their own arrangements for dealing with this issue. This could include using any unspent direct payment to contribute to any redundancy costs, having insurance in place that covers redundancy, or the local authority agreeing to cover redundancy payments through the direct payment amount.
12.31 Whatever arrangements are made it is important that the local authority and direct payment holder are both clear as to their responsibilities in this regard to avoid any disputes at a sensitive time for family and carers. Decisions made should be recorded in care plans.
12.32 Local authorities should also consider how to recover unspent direct payments if the recipient dies. For example, if someone wishes to pay an agency in advance for its services, the local authority should bear in mind that it may be difficult to recover money paid for services that were not in fact delivered. Local authorities should also consider, if the direct payment recipient does leave unspent funds to be recovered, that before their death the direct payment recipient may have incurred liabilities that should legitimately be paid for using the direct payments (for example, they received services for which payment had not been made at the time of death). Local authorities may need to consider any redundancy costs payable to personal assistants and be prepared to provide advice on how these might be met. As with other costs the personal budget must be a sufficient amount to meet the person’s needs, including the provision of any redundancy costs, if appropriate to meet needs, and subject to other arrangements that may have been made.
12.33 Local authorities should ensure all direct payment recipients are supported and given information in regards to having the correct insurance cover in place. Direct payments recipients should be given support to understand the benefits that insurance cover can provide, and the direct payment should therefore include an amount to cover the cost of employers’ liability insurance and any other insurance that is required in order that the person can meet their needs in the way specified in the care plan.
12.34 The local authority must also have regard to where the direct payment can be integrated with other forms of public funding, such as personal health budget direct payments. Where this is apparent, the local authority should take steps to work with partners to combine the payments, as long as the person and all parties agree. For example, the local authority could agree with the NHS that the social care and health direct payments are combined and that the monitoring is performed solely by one organisation, reporting to the other as appropriate. This will avoid the person having multiple bank accounts, and having to supply similar information to public bodies to account for direct payment spend, while allowing both bodies to meet their statutory responsibilities.
Using the direct payment
Paying family members
12.35 The direct payment is designed to be used flexibly and innovatively and there should be no unreasonable restriction placed on the use of the payment, as long as it is being used to meet eligible care and support needs.
Example: Direct Payment to pay a family member for administration support
David has been using direct payments to meet his needs for some time, and has used private agencies to provide payroll and administration support, funded by a one-off annual payment as part of his personal budget allocation. David’s wife, Gill provides care for him and is increasingly becoming more hands-on in arranging multiple PAs to visit and other administrative tasks as David’s care needs have begun to fluctuate.
They jointly approach the local authority to request that Gill undertake the administration support instead of the agency as they want to take complete control of the payment and care arrangements so that they can best meet David’s fluctuating needs and ensure that appropriate care is organized.
The local authority considers that Gill would be able to manage this aspect of the payment, and jointly revises the care plan to detail the aspects of the payment, and what services Gill will undertake to the agreement of all concerned. The personal budget is also revised accordingly.
The family now has complete control of the payment, Gill is reimbursed for her time in supporting David with his direct payment and the local authority is able to make a saving in the one-off support allocation as there are no provider overheads to pay. In promoting David’s wellbeing, the local authority has demonstrated regard for the balance between promoting an individual’s wellbeing and that of people who are involved in caring for them. It has given Gill increased control in a way that David is comfortable with and supports.
12.36 The 2009 Direct Payment Regulations excluded the payment from being used to pay for care from a close family member living in the same household, except where the local authority determined this to be necessary. [footnote 52] While the Care and Support (Direct Payments) Regulations 2014 maintain this provision regarding paying a family member living in the same household for care, it provides a distinction between ‘care’ and ‘administration/management’ of the direct payment. This allows people to pay a close family member living in the same household to provide management and/or administrative support to the direct payment holder in cases where the local authority determines this to be necessary. This is intended to reflect the fact that in some cases, especially where there are multiple complex needs, the direct payment amount may be substantial.
Example: Direct payment paid to a family member where necessary
James has severe learning difficulties as well as various physical disabilities. He has serious trust issues and a unique way of communicating that only his family, through years of care as a child, can understand. The local authority agrees that using a direct payment to pay for care from his parents is necessary as it is the best way to meet James’s needs and outcomes.
12.37 The management and administration of a large payment, along with organising care and support can be a complex and time consuming task. This allows family members performing this task to be paid a proportion of the direct payment, similar to what many direct payment holders pay to third-party support organisations, as long as the local authority allows this.
12.38 This is not intended to be income replacement, and people interested in requesting this option should be informed of tax and employment implications, any impacts upon other benefits and given (or signposted to) information and advice to help them decide. The local authority should be satisfied that it is necessary to make the payment to the family member to provide this service and that the direct payment will only be used for administration and management of the payment. The circumstances and payment amount should be decided and agreed with the person requiring care and support, the family member, local authority and any other person (for example, advocate), with the local authority taking steps to ensure all parties agree.
12.39 These decisions should be recorded in the care plan and include the amount of the payments, their frequency and the activities that are covered. This arrangement must also be taken into account during allocation of the personal budget so that the amount remains sufficient to meet the person’s needs.
12.40 Local authorities will need to have in place agreement between all parties about what steps to take in case of a dispute regarding the management of the payment by a household family member. This will be especially relevant where the person providing administrative and management is also the nominated or authorised direct payment recipient. It would not be appropriate to allow this where there is a risk that the direct payment may be abused, or there are other sensitivities such as potential safeguarding issues.
Short-term care in a care home
12.41 Direct payments cannot currently be used to pay for people to live in long-term care home placements. They can be made to enable people to purchase for themselves a short stay in care homes, provided that the stay does not exceed a period of 4 consecutive weeks in any 12-month period. This could be used to provide a respite break for a carer, for example.
12.42 The Regulations specify that where the interim period between 2 stays in care homes is less than 4 weeks, then the 2 stays should be added together to make a cumulative total, which should also not exceed 4 weeks if it is to be paid for with direct payments. On the other hand, if 2 stays in care homes are more than 4 weeks apart then they are not added together.
12.43 Once a direct payment recipient has had 4 consecutive weeks in care homes, or 2 or more periods separated by less than 4 weeks which added together total 4 weeks, then they cannot use their direct payments to pay for any more home services care until 12 months have passed from the start of the 4-week period. On the other hand, as long as each stay is less than 4 weeks and there is an interim period of at least 4 weeks between 2 or more stays which added together exceed 4 weeks, then the service recipient may use their direct payments to pay for residential breaks throughout the year.
Example: Direct Payments for short-term residential care
Mrs. H has one week in a care home every 6 weeks. Because each week in a care home is more than 4 weeks a part, they are not added together. The cumulative total is only one week and the 4-week limit is never reached.
Peter has 3 weeks in a care home, 2 weeks at home and then another week in a care home. The 2 episodes of time in a care home are less than 4 weeks apart and so they are added together making 4 weeks in total. Peter cannot use his direct payments to purchase any more care home services within a 12-month period.
12.44 People can receive additional weeks in a care home once they have reached the 4-week maximum. They cannot purchase the stay using their direct payments, but if the local authority and the person agrees that a longer stay is needed, it can still arrange and fund stays for the person. There is no restriction on the length of time for which the local authority may arrange such accommodation for someone (see chapter 8 for guidance on choice of accommodation).
12.45 The time limit is imposed to promote people’s independence and to encourage them to remain at home rather than moving into long-term home placement. Where a person is constantly using the direct payment to pay for a short-term care home stays, the local authority should consider whether to conduct a review to ensure that the care plan is still meeting needs.
Long-term care in a care home
12.46 People who are living in care homes may receive direct payments in relation to non-residential care services. For example, they may have temporary access to direct payments to try out independent living arrangements before making a commitment to moving out of their care home. Direct payments can also be used by people living in care homes to take part in day-time activities. This can be particularly empowering for young people in transition (see chapter 16).
12.47 Direct payments cannot currently be used to secure long-term stays in a care home. Approaches to the use of direct payments in care homes have been trialled in a number of local authorities which were designated trailblazers and specified in the regulations The learning from this trailblazer programme will be used to develop additional statutory guidance for local authorities when direct payments for long-term stays in care homes is introduced for all local authorities in 2020. Trailblazers were asked if they wished to remain on the schedule of those local authorities not prohibited from making a direct payment for the purposes of securing long term care in a care home until national rollout in 2020 and the regulations were amended accordingly.
Becoming an employer
12.48 Local authorities should give people clear advice as to their responsibilities when managing direct payments, and whether the person in receipt of direct payments needs to register with HM Revenue & Customs (HMRC) as an employer. Becoming an employer carries with it certain responsibilities and obligations, in particular to HMRC and people need to be aware of these before agreeing to take up a direct payment. Disability and tax – a guide provides information on being an employer.
12.49 The local authority should consider using the proportionality principle, whether to carry out checks to make sure any PAYE income tax and National Insurance contributions deducted from an employee’s pay is in turn paid over to HMRC, and that employment payments do not breach the national minimum wage and conform to pension requirements if eligible. Some people may not need this check to be performed, but it may be more appropriate in other cases and conform to pension requirements if eligible. [footnote 53]
Where it becomes clear that payments, or returns detailing employee information deductions, have not been made, or that the individual is failing to meet their obligations as an employer generally, the direct payment scheme should be reviewed and consideration given to whether alternative arrangements that result in the direct payment recipient no longer acting as the employer need to be made. Not doing so may result in the individual building up arrears of tax and National Insurance due to HMRC, which may then lead to enforcement action to recover any debt. This situation should be able to be avoided by effective monitoring where appropriate, and by providing clear, accessible upfront information about the responsibilities of becoming an employer. Many local authorities have commissioned voluntary and charity organisations to provide support to direct payment holders on these matters.
12.50 Many people are interested in using the direct payment to become an employer, for example, directly employing a personal assistant (PA). In these instances, the local authority should ensure that the person is given appropriate information and advice that explains the difference between a regulated and unregulated provider to help the person make a fully informed decision on how best to meet their needs. Where a direct payment is made under section 32 of the Act and to comply with the regulations, the local authority must also ensure that the authorised person is aware of how to access Disclosure and Barring Service Checks (DBS – previously CRB checks) on individuals they wish to employ, for example by ensuring that a check has been made by the agency providing the service, the local authority, or by another body. Individuals cannot apply for DBS checks on other individuals, and the local authority should make people aware of this, and the importance of thorough checks and employment references in the recruitment process.
12.51 Where a person wishes to directly employ their own PA, the local authority should also have regard to the guidance published by Skills for Care detailing minimum levels of support for individual employers and PAs. This guidance recommends local authorities should provide on-going support through access to training activities in a variety of ways and promote the Workforce Development Fund. It also proposes that local authorities promote apprenticeships for PAs.
Direct payments and hospital stays
12.52 There may often be occasions when direct payment holders require a stay in hospital. However, this should not mean that the direct payment must be suspended while the individual is in hospital. Where the direct payment recipient is also the person requiring care and support, consideration should be given to how the direct payment may be used in hospital to meet non-health needs or to ensure employment arrangements are maintained. Suspending or even terminating the payment could result in the person having to break the employment contract with a trusted personal assistant, causing distress and a lack of continuity of care when discharged from hospital.
12.53 In these cases, the local authority should explore with the person, their carer and the NHS the options to ensure that both the health and care and support needs of the person are being fully met in the best way possible. For example, the person may prefer the personal assistant to visit hospital to help with personal care matters. This may be especially so where there has been a long relationship between the direct payment holder and the personal assistant. This should not interfere with the medical duties of hospital personnel, but be tailored to work alongside health provision.
12.54 In some cases, the nominated or authorised person managing the direct payment may require a hospital stay. In these cases, the authority must conduct an urgent review to ensure that the person continues to receive care and support to meet their needs. This may be through a temporary nominated/ authorised person, or through short-term authority arranged care and support.
Example: Using a direct payment whilst in hospital
Peter is deafblind and is required to stay in hospital for an operation. Whilst the hospital pays for an interpreter for the medical interventions, Peter needs additional support to be able to move around the ward, and to communicate informally with staff and his family. The local authority and the NHS Trust agree that Peter’s communicator guide continues to support him in hospital, and is paid for via the direct payment, as it was when Peter was at home. Personal and medical care is provided by NHS staff but Peter’s communicator guide is on hand to provide specialist communication and guiding support to make his hospital stay is as comfortable as possible.
Direct payments for local authority services
12.55 As a general rule, direct payments should not be used to pay for local authority-provided services from the ‘home’ local authority. Where a person wishes to receive care and support from their local authority, it should be easier and less burdensome to provide the service direct to the person. This will also avoid possible conflicts of interest where the local authority is providing the direct payment, but also promoting their services for people to purchase.
12.56 There may be cases where the local authority exercises discretion to provide care and support by receiving a direct payment amount, for example this could be where a person who is using direct payments wants to make a one-off purchase from the local authority such as a place in day care. In these cases, the local authority should take into account the wishes of the person requiring care and support when making a decision. In one off cases such as these, it may be less burdensome to accept the direct payment amount, rather than providing the service and then reducing the personal budget and direct payment accordingly.
Example: Local authority provided service
Graham has a direct payment for the full amount of his personal budget allowance. He decides to use a local authority run day service on an infrequent basis and requests to pay for it with his direct payment so that he retains flexibility about when he attends. The local authority service is able to agree to this request and has systems already in place to take payments as self-funders often use the service. The authority advise Graham that if he wishes to use the day service on a frequent basis (for example, once a week) it would be better to provide the service to him direct, and to reduce the direct payment amount accordingly.
12.57 This does not preclude people from using their direct payment to purchase care and support from a different local authority. For example, a person may live close to authority boundaries and another local authority could provide a particular service that their ‘home’ authority does not provide.
Direct payments in the form of pre-paid or pre-payment cards
12.58 Many local authorities have been developing the use of pre-paid cards as a mechanism to allow direct payments without the need for a separate bank account, or to ease the financial management of the payment. Whilst the use of such cards can be a useful step from managed services to direct payments, they should not be provided as the only option to take a direct payment The offer of a ‘traditional’ direct payment paid into a bank account should always be available if this is what the person requests and this is appropriate to meet needs. Consideration should be given to the benefit gained from this arrangement as opposed to receiving the payment via a pre-paid card.
12.59 It is also important that where a pre-paid card system is used, the person is still free to exercise choice and control. For example, there should not be blanket restrictions on cash withdrawals from pre-paid cards which could limit choice and control. The card must not be linked solely to an online market-place that only contains selected providers in which to choose from. Local authorities should therefore give consideration to how they develop card systems that encourage flexibility and innovation, and consider consulting care and support user groups on any proposed changes to direct payment processes.
Harmonisation of direct payments
12.60 In circumstances where it is in the person’s interest to combine the plan and budget with another form of state support (such as personal health budgets), and the person agrees that plans should be combined, the local authority should give consideration to whether the person is receiving direct payments from partner organisations, such as the NHS. If so, attempts should be made to harmonise the direct payments so that the person does not have multiple payments each with their own monitoring regime. For example, the local authority could work with the NHS partner to agree on a ‘lead organisation’ that oversees the overall budget and monitors the direct payments to ensure they are being to meet both health and care needs, while still allowing both bodies to satisfy themselves of their statutory responsibilities.
Reviewing direct payments
12.61 In addition to monitoring direct payments generally to ensure they are being used to meet care and support needs, the Regulations set out that local authorities must also review the making of the direct payment within the first 6 months of making the first payment. This provision is intended to be used for direct payments made under the powers in the Care Act, rather than pre-existing ones.
12.62 This review is intended to be light-touch to ensure that the person is comfortable with using the direct payment, and experiencing no initial issues. It should ideally be incorporated within the initial review of the care and support plan 6-8 weeks after sign-off and include elements such as managing and using the direct payment and a discussion to consider any long-term support arrangements that may be appropriate such as payroll, insurance cover and third party support. Local authorities should ensure that reviewing officers are appropriately trained to review direct payments (for example are familiar with financial procedures and employment laws) This review is not intended to be a full review of the person’s care and support plan. However, if this review raises concerns or requires actions that affect the detail recorded in the care plan, then a full review of the plan would need to be carried out.
12.63 If the direct payment recipient is employing people, the local authority should as part of the review, consider checking, if appropriate, to ensure the individual is fulfilling their responsibilities as the employer, in particular that they are submitting PAYE returns to HMRC as well as paying tax and National Insurance deductions made to HMRC.
12.64 The Regulations also set out that following the 6-month review, the local authority must then review the making of the direct payment no later than every 12 months. In practice, after the initial 6-month review period, local authorities may wish to consider aligning the annual review of the direct payment with the general review of the care plan. This will reduce bureaucracy and allow the local authority to review both at the same time.
12.65 Where a direct payment is being allocated to a nominated/authorised person, or where there may be a family carer being paid for administrative support, the review should incorporate all of these parties as well as the person in need of care and support. This will ensure that the local authority receives views from everyone involved in the direct payment, so that it can satisfy itself that there are no initial issues that require resolving.
12.66 The outcome of the review should be written down, and a copy given to all parties. Where there are issues that require resolving, the resolution method should be agreed with all parties involved, as far as is reasonably practicable. Where appropriate, local authorities should advise people of their rights to access the local authority complaints procedure.
Terminating direct payments
12.67 Direct payments should only be terminated as a last resort, or where there is clear and serious contradiction of the Regulations or where the conditions in sections 31 or 32 of the Act are no longer met (except in cases of fluctuating capacity – see sections below). Local authorities should take all reasonable steps to address any situations without the termination of the payment. Effective, but proportionate monitoring processes will help local authorities to spot any potential issues before a termination is necessary.
12.68 If terminating a direct payment, the local authority must ensure there is no gap in the provision of care support. Where a decision has been made to terminate a direct payment, the local authority should conduct a revision of the care and support plan, or support plan, to ensure that the plan is appropriate to meet the needs in question (see Chapter 13 on reviews).
Reasons for discontinuing direct payments
12.69 A person to whom direct payments are made, whether to purchase support for themselves or on behalf of someone else, may decide at any time that they no longer wish to continue receiving direct payments. In these cases, the local authority should ensure there are no outstanding contractual liabilities, and conduct a review of the care plan to consider alternate arrangements to meet needs.
12.70 The Care Act also sets out that a local authority shall cease making direct payments if the person no longer appears to be capable of managing the direct payments or of managing them with whatever support is necessary.
12.71 Direct payments should be discontinued when a person no longer needs the support for which the direct payments are made. This might happen in situations where the direct payments are for short-term packages when leaving care home or hospital. Direct payments for after-care services under section 117 of the Mental Health Act would also cease once the clinical commissioning group and local authority are satisfied that the person concerned is no longer in need of such services.
12.72 There may be circumstances in which the local authority discontinues direct payments temporarily. An example might be when an individual does not require assistance for a short period because their condition improves and they do not require the care and support that the direct payments are intended to secure. The local authority will need to discuss with the person, their carer, and any other person how best to manage this. The person should be allowed to resume responsibility for their own care after the interruption, if that remains their wish, unless there has been a change of circumstances which means that the conditions in the Act and/or Regulations are no longer met. If there is a change of circumstances that affects the care plan/support plan the local authority must revise the plan to ensure that it is still meeting needs (see Chapter 13).
12.73 The local authority might also discontinue payments if the person fails to comply with a condition imposed under regulations to which the direct payments are subject or if for some reason the local authority no longer believes it is appropriate to make the direct payments. For example, the local authority might discontinue the direct payment if it is apparent that they have not been used to achieve the outcomes of the care plan.
12.74 The 2009 Direct Payment regulations set out that direct payments must not be provided under certain conditions, such as where the recipient is placed by the courts under a condition or requirement relating to a drug and/or alcohol dependency. The Care and Support (Direct Payments) Regulations 2014 retain this universal restriction. The groups and conditions remain substantially the same as the 2009 regulations and are set out in the schedule to the 2014 regulations.
12.75 Where direct payments are discontinued as a result of criminal justice legislative provisions, the local authority should make timely arrangements for services to be provided in lieu of the direct payments, to ensure continuity of support.
Discontinuing direct payments in the case of persons with capacity to consent
12.76 Where someone with capacity was receiving direct payments but then loses capacity to consent, the local authority should discontinue direct payments to that person and consider making payments to an authorised person instead. In the interim, the local authority should make alternative arrangements to ensure continuity of support for the person concerned.
12.77 If the local authority believes the loss of capacity to consent to be temporary, it may continue to make payments if there is someone else who is willing to manage payments on the person’s behalf. This situation should be treated as strictly temporary and closely monitored to ensure that, once the person has regained capacity, they are able to exercise overall control over the direct payments as before. If the person’s loss of capacity to consent becomes prolonged, then the local authority should consider making more formal arrangements for an authorised person to take over receipt of the direct payments on that person’s behalf. The local authority should make clear that the arrangement is designed to be temporary, so that the person managing the direct payment does not enter into any long-term contractual arrangements.
Discontinuing direct payments in the case of persons lacking capacity to consent
12.78 Direct payments must be discontinued if the local authority is no longer satisfied for whatever reason that the authorised person is acting in the best interests of the beneficiary, within the meaning of the 2005 Act. The local authority might also wish to discontinue the direct payments if it has sufficient reason to believe that the conditions imposed under regulations on the authorised person are not being met. The authority may wish to consider if someone else can act as an authorised person for the person lacking capacity, or whether it will have to arrange services for them in place of the direct payments.
12.79 Direct payments under section 32 of the Act must be discontinued where the local authority has reason to believe that someone who had lacked capacity to consent to direct payments has now regained that capacity on a long-term or permanent basis. The authority should not terminate direct payments to the authorised person before beginning to make direct payments to the service recipient themselves or to arrange services for them, according to their wishes. If the local authority is satisfied that the regaining of capacity will only be temporary, then it can continue to make direct payments to the authorised person if during the period that the adult has the capacity to make the request and is capable of managing the direct payment, the adult will manage the payments for him or herself.
How to discontinue direct payments
12.80 In all cases, as soon as possible the local authority should discuss with individuals, their carers and any person managing the direct payments if it is considering discontinuing direct payments to them, in order to explore all available options before making the final decision to terminate the direct payments. For example, if ability to manage is an issue, the individual should be given an opportunity to demonstrate that they can continue to manage direct payments, albeit with greater support if appropriate. The local authority should not automatically assume when problems arise that the only solution is to discontinue or end direct payments.
12.81 If the local authority does decide to withdraw direct payments, it will need to conduct a review of the plan and agree alternative care and support provision with the person, their carer and independent advocate if they have one, unless the withdrawal was following a review after which the local authority concluded that the services were no longer needed A minimum period of notice should be established that will normally be given before direct payments are discontinued. This should be included in the information to be provided to people who are considering receiving direct payments.
12.82 It will be extremely unlikely that a local authority will discontinue direct payments without giving notice, although in serious cases this may be warranted (for example, the authorised person is not acting in the best interests of the person). Local authorities should explain to people, before they begin to receive direct payments, the exceptional circumstances in which this might occur and discuss with them the implications this has for the arrangements that individuals might make.
12.83 If direct payments are discontinued, some people may find themselves with ongoing contractual responsibilities or having to terminate contracts for services (including possibly making employees redundant). Local authorities should take reasonable steps to make people aware of the potential consequences if direct payments end, and any obligations they may have.
12.84 There may be circumstances where the person has lost the capacity to manage the direct payment and there is no-one else to manage the payment on their behalf, or where a person needs additional support to terminate arrangements. In these cases the local authority should have regard as to whether it needs to step in or provide support to ensure that any contractual arrangements are appropriately terminated to ensure that additional costs are not incurred.
Links to external resources
- Direct payments in healthcare - a practical guide
- Employee information
- Register as an employer
- Introduction to PAYE
- Information on taking on a new employee
- Guidance for anyone taking on a personal assistant
- Best practice in direct payments support - a guide for commissioners
- Self-Directed Support: Reducing process, increasing choice and control
- PA toolkit
13. Review of care and support plans
This chapter provides guidance on section 27 of the Care Act 2014 and covers:
- review of the care and support plan, support plan
- keeping plans under review generally
- planned and unplanned review
- considering a request for a review of a care plan, support plan
- considering a review
- revision of the care and support plan, support plan
- timeliness and regularity of reviews
13.1 Ensuring all people with a care and support plan, or support plan have the opportunity to reflect on what is working, what is not working and what might need to change is an important part of the planning process. It ensures that plans are kept up to date and relevant to the person’s needs and aspirations, provides confidence in the system and mitigates the risks of people entering a crisis situation.
13.2 The review process should be person-centred and outcomes-focused, as well as accessible and proportionate to the needs to be met. The process must involve the person needing care and also the carer where feasible, and consideration must be given whether to involve an independent advocate who local authorities are required to supply in the circumstances specified in the Act.
13.3 Reviewing intended outcomes detailed in the plan is the means by which the local authority complies with its ongoing responsibility towards people with care and support needs. The duty on the local authority therefore is to ensure that a review occurs, and if needed, a revision follows this. Consideration should also be given to authorising others to conduct a review – this could include the person themselves or carer, a third party (such as a provider) or another professional, with the local authority adopting an assurance and sign-off approach.
13.4 The review will help to identify if the person’s needs have changed and can in such circumstances lead to a reassessment. It should also identify other circumstances which may have changed, and follow safeguarding principles in ensuring that the person is not at risk of abuse or neglect. The review must not be used as a mechanism to arbitrarily reduce the level of a person’s personal budget.
13.5 In many cases, the review and revision of the plan should be intrinsically linked; it should not be possible to decide whether to revise a plan without a thorough review to ascertain if a revision is necessary, and in the best interests of the person. In addition, where a review is being undertaken where a person has a carer, the local authority should consider whether the carer’s support plan requires reviewing, too. 13.6 However, there are occasions when a change to a plan is required but there has been no change in the levels of need (for example, a carer may change the times when they are available to support). In addition, there can be small changes in need, at times temporary, which can be accommodated within the established personal budget.
13.7 In these circumstances, it may not be appropriate for the person to go through a full review and revision of the plan. The local authority should respond to these ‘light-touch’ requests in a proportionate and reasonable way.
13.8 Where the local authority is satisfied that a revision is necessary, it must work through the assessment and care planning processes as detailed in sections 9-12 and 25 of the Act to the extent that it thinks appropriate (see chapter 6).
13.9 This chapter applies to people in need of care and support and carers equally, unless specifically stated. As many of the same principles apply to both care and support planning and reviews, this chapter should be read in conjunction with chapter 10 on care and support planning. Where a plan is for a person with mental health problems, this chapter should be read in conjunction with chapter 34 of the Mental Health Act 1983 Code of Practice (on the Care Programme Approach) and Refocusing the Care Programme Approach.
Review of the care and support plan, support plan
Keeping plans under review generally
13.10 Keeping plans under review is an essential element of the planning process. Without a system of regular reviews, plans could become quickly out of date meaning that people are not obtaining the care and support required to meet their needs. Plans may also identify outcomes that the person wants to achieve which are progressive or time limited, so a periodic review is vital to ensure that the plan remains relevant to their goals and aspirations.
13.11 The Act specifies that plans must be kept under review generally. Therefore, local authorities should establish systems that allow the proportionate monitoring of both care and support plans and support plans to ensure that needs are continuing to be met. This system should also include seeking cooperation with other health and care professionals who may be able to inform the authority of any concerns about the ability of the plan to meet needs (see chapter 15 on integration and cooperation).
13.12 The review should be a positive opportunity to take stock and consider if the plan is enabling the person to meet their needs and achieve their aspirations. The process should not be overly-complex or bureaucratic, and should cover these broad elements, which should be communicated to the person before the review process begins:
- have the person’s circumstances and/or care and support or support needs changed?
- what is working in the plan, what is not working, and what might need to change?
- have the outcomes identified in the plan been achieved or not?
- does the person have new outcomes they want to meet?
- could improvements be made to achieve better outcomes?
- is the person’s personal budget enabling them to meet their needs and the outcomes identified in their plan?
- is the current method of managing it still the best one for what they want to achieve, for example, should direct payments be considered (see chapter 11 on personal budgets)?
- is the personal budget still meeting the sufficiency test?
- are there any changes in the person’s informal and community support networks which might impact negatively or positively on the plan?
- have there been any changes to the person’s needs or circumstances which might mean they are at risk of abuse or neglect?
- is the person, carer, independent advocate satisfied with the plan?
13.13 There are several different routes to reviewing a care and support or support plan including:
- a planned review (the date for which was set with the individual during care and support or support planning, or through general monitoring)
- an unplanned review (which results from a change in needs or circumstance that the local authority becomes aware of, for example, a fall or hospital admission)
- a requested review (where the person with the care and support or support plan, or their carer, family member, advocate or other interested party makes a request that a review is conducted. This may also be as the result of a change in needs or circumstances)
Planned reviews
13.14 During the planning process, the person and their social worker, or relevant professional may have discussed when it might be useful to review the plan and therefore agree to record this date in the plan. This may be valuable to people in the care system so that they can anticipate when the review will take place, rather than the review being an unexpected experience. It also fits with the Government’s view of personalised care and support, as the person may have a view as to a suitable time-frame for the review to occur. Additionally, setting out anticipated review dates may help authorities with future workload planning.
13.15 Even in cases with anticipated review dates, this should not reduce the requirement of the local authority to keep the plan under review generally. The first planned review should be an initial ‘light touch’ review of the planning arrangements 6-8 weeks after sign-off of the personal budget and plan. Where relevant, this should also be combined with an initial review of direct payment arrangements. This will provide reassurance to all parties that the plan is working as intended, and will help to identify any teething problems. In addition, where plans are combined with other plans (for example the plan of a carer, or education, housing, and health and care plans which may be reviewed annually) the local authority should be aware of the review arrangements with these other plans and seek to align reviews together.
13.16 Local authorities should have regard to ensuring the planned review is proportionate to the circumstances, the value of the personal budget and any risks identified. In a similar way to care and support or support planning, there should be a range of review options available, which may include self-review, peer-led review, reviews conducted remotely, or face to face reviews with a social worker or other relevant professional. For example, where the person has a stable, longstanding support package with fixed or long-term outcomes, they may wish to complete a self-review at the planned time which is then submitted to the local authority to sign-off, rather than have a face to face review with their social worker. This does not preclude their requesting a review at another time or a face to face review being needed if there is an unplanned change in needs or circumstances.
13.17 In all instances, the method of review should, wherever reasonably possible, be agreed with the person and must involve the adult to whom the plan relates, any carer the adult has and any person the adult asks the authority to involve. The local authority should take all appropriate measures to ensure their involvement and the involvement of other people if appropriate, such as an independent advocate where this is required by the circumstances specified in the Act.
13.18 Furthermore, if a person is recorded as having a mental impairment and lacking capacity to make some decisions, then the local authority should consider carefully when it will be appropriate for the next review to take place. In these instances, making appropriate use of a social worker as the lead professional should be encouraged. Where conditions are progressive, and the person’s health is deteriorating, reviews may need to be much more frequent. Similarly where a person has few or no family members or friends involved in supporting them, the risks are higher, and again, reviews or monitoring may need to be more frequent. It may beneficial to put a ‘duty to request a review’ into commissioned services so that employees are required to inform the local authority if they think that there is a need for a review. Where this occurs, the person should still be involved in the review process to ensure their views are taken account of.
Unplanned reviews
13.19 If there is any information or evidence that suggests that circumstances have changed in a way that may affect the efficacy, appropriateness or content of the plan, then the local authority should immediately conduct a review to ascertain whether the plan requires revision. For example this could be where a carer is no longer able to provide the same level of care, there is evidence of a deterioration of the person’s physical or mental wellbeing or the local authority receives a safeguarding alert. During the review process, the person the plan is intended for, or the person acting on their behalf should be kept fully involved and informed of what is occurring, the timescales involved and any likely consequences. This will help to alleviate anxiety at a time where things in the person’s life may have changed substantially.
Considering a request for a review of a plan
13.20 In addition to the duty on local authorities to keep plans under review generally, the Act provides a duty on the local authority to conduct a review if a request for one is made by the adult or a person acting on the adult’s behalf. [footnote 54] Local authorities should provide information and advice to people at the planning stage about how to make a request for a review. This process should be accessible and include multiple routes to make a request – phone, email, or text for example. The information given to people should also set out what happens after a request is made, and the timescales involved in the process.
13.21 The request process should be accessible and streamlined, with local authorities acting promptly after a request has been received. Consideration should also be given to the accessibility needs of the local population. This may, for example, include multiple language versions, and non-internet routes to request for people who may not have access to the internet, or in areas of digital exclusion. Local authorities should also consider the role that local community and voluntary organisations can play to help people log requests.
13.22 The right to request a review applies not just to the person receiving the care, but to others supporting them or interested in their wellbeing. For example a person with advanced dementia may not be able to request a review, but a relative or a neighbour may want to draw the attention of the local authority to a deterioration in the person’s condition. The local authority should consider the request even if it is not made by the adult or their carer.
Considering a review
13.23 Upon receipt of a request to conduct a review, the local authority must consider this and judge the merits of conducting a review. In most cases, it is the expectation that a review should be performed unless the authority is reasonably satisfied that the plan remains sufficient, or the request is frivolous, or is made on the basis of inaccurate information, or is a complaint; for example where a person lodges multiple requests for a review in a short period of time and there is no reason to believe that the person’s needs have changed. Local authorities should clearly set out the process that will be used to consider requests.
13.24 In considering whether to undertake a review the authority must involve the person, carer and anyone else the person requests to be involved where feasible. The local authority will need to identify those who may have significant difficulty in being fully involved in the decision to review and when there is no appropriate person who can represent or support their involvement and consider the duty to provide independent advocacy (see also chapter 7 on advocacy).
Example: Accepting a renewal request
A local authority receives an email from a relative of an older person receiving care and support at home. The email provides details that the older person’s condition is deteriorating and supplies evidence of recent visits to the GP. The local authority therefore decides to review their care and support plan to ensure that it continues to meet their needs.
Example: Declining a renewal request
A local authority receives a phone call from Mr X. He is angry as he feels that he has needs that have not been identified in his care plan and requests a review of the plan. The authority has on a separate recent occasion reviewed his plan, when it came to the conclusion that no revision was necessary and informed Mr X of the decision and the reasons for it. Therefore, the local authority declines the request in this case and provides a written explanation to Mr X, informing hi m of an anticipated date of when it will be formally reviewing the plan together with information on its complaints procedure.
13.25 Where a decision is made not to conduct a review following a request, the local authority should set out the reasons for not accepting the request in a format accessible to the person, along with details of how to pursue the matter if the person remains unsatisfied. In most cases, it would be helpful for this to set out that the authority will continue to monitor the plan to ensure that it remains fit for purpose, and that the decision does not affect the right to make a future request for review. Although not mandatory, it may also be prudent for the local authority to set out when the person can expect a formal review of the plan.
Revision of the care and support plan, support plan
13.26 Where a decision has been made following a review that a revision is necessary, the authority should inform the person, or a person acting on their behalf of the decision and what this will involve. Where the person has substantial difficulty in being actively involved with the review, and where there are no family or friends to help them to engage, an independent advocate must be involved (see also chapter 7 on advocacy).
13.27 When revising the plan the local authority must involve the person, their carer and any other persons the adult may want involved, and their advocate where the person qualifies for one. The local authority must take all reasonable steps to agree the revision. The revision should wherever possible follow the process used in the assessment and care planning stages. Indeed, the local authority must if satisfied that the circumstances have changed in a way that affects a care and support or support plan, carry out a needs or carer’s assessment and financial assessment, and then revise the plan and personal budget accordingly. The assessment process following a review should not start from the beginning of the process but pick up from what is already known about the person and should be proportionate. [footnote 55]
13.28 In some cases a complete change of the plan may be required, whereas in others minor adjustments may be needed. In either case, the following aspects of care planning should be followed:
- the person’s wishes and feelings should be identified as far as possible and they should be supported to be involved
- the revision should be proportionate to the needs to be met
- where the plan was produced in combination with other plans, this should be considered at the revision stage
- the person, carer or person acting on their behalf should be allowed to self-plan in conjunction with the local authority where appropriate
- the development of the revised plan must be made with the involvement of the adult/carer, and any person the adult asks the authority to involve
- any additional elements that were incorporated into the original plan should be replicated in the revised plan where appropriate and agreed by all parties
- there needs to be clarity on the sign-off process, especially where the revised plan is prepared by the person and the local authority
13.29 Particular attention should be taken if the revisions to the plan propose increased restraints or restrictions on a person who has not got the capacity to agree them. This may become a deprivation of liberty, which requires appropriate safeguards to be in place. The local authority should have policies to address how these are recognised and responded to, and the social worker, occupational therapist or other relevant social care qualified professional or Mental Capacity lead should be involved, as well as an advocate.
13.30 The local authority must consider in all cases whether an independent advocate may be required to facilitate the person’s involvement in the revision of the plan. Where the plan was produced with the assistance of an independent advocate, then consideration should be given to whether an independent advocate is also required for the revision of the plan. In these scenarios, the advocate would ideally be the same person to ensure consistency and continuity with the case details. Likewise, where a specialist assessor has been used previously in the care and support journey, the local authority should have regard to whether they need to employ the expertise of the assessor in the review.
Timeliness and regularity of reviews
13.31 In the absence of any request of a review, or any indication that circumstances may have changed, the local authority should conduct a periodic review of plan. As stated earlier, this could be indicated at the planning stage by including an anticipated review date to allow for future planning. In addition, local authorities may wish to align the periodic review of the plan, with the compulsory review of the direct payment arrangements, where this is appropriate.
13.32 It is the expectation that authorities should conduct a review of the plan no later than every 12 months, although a light-touch review should be considered 6– 8 weeks after agreement and sign-off of the plan and personal budget, to ensure that the arrangements are accurate and there are no initial issues to be aware of. This light-touch review should also be considered after revision of an existing plan to ensure that the new plan is working as intended, and in cases where a person chooses a direct payment, should be aligned with the review of the making of the direct payment (see chapter 12 on direct payments).
13.33 The periodic review should be proportionate to the needs to be met, and the process should not contain any surprises for the person concerned. Periodic reviews and reviews in general must not be used to arbitrarily reduce a care and support package. Such behaviour would be unlawful under the Act as the personal budget must always be an amount appropriate to meet the person’s needs. Any reduction to a personal budget should be the result of a change in need or circumstance.
13.34 The review should be performed as quickly as is reasonably practicable. As with care and support planning, it is expected that in most cases the revision of the plan should be completed in a timely manner proportionate to the needs to be met. Where there is an urgent need to intervene, local authorities should consider implementing interim packages to urgently meet needs while the plan is revised. However, local authorities should work with the person to avoid such circumstances wherever possible by ensuring that any potential emergency needs are identified as part of the care and support planning stage and planned for accordingly.
Links to external resources
- Delivering Care and Support Planning Guide (PDF, 2.59MB)
- Outcome focused reviews – a practical guide
Safeguarding
14. Safeguarding
This chapter provides guidance on sections 42 to 46 of the Care Act 2014 and covers:
- adult safeguarding: what it is and why it matters
- abuse and neglect
- understanding what they are and spotting the signs
- reporting and responding to abuse and neglect
- carers and adult safeguarding
- adult safeguarding procedures
- local authority’s role and multi-agency working
- criminal offences and adult safeguarding
- safeguarding enquiries
- Safeguarding Adults Boards
- Safeguarding Adults Reviews
- information sharing, confidentiality and record keeping
- roles, responsibilities and training in local authorities, the NHS and other agencies
14.1 The chapter replaces the ‘No Secrets’ guidance.
14.2 The safeguarding duties apply to an adult who:
- has needs for care and support (whether or not the local authority is meeting any of those needs)
- is experiencing, or at risk of, abuse or neglect
- as a result of those care and support needs is unable to protect themselves from either the risk of, or the experience of abuse or neglect
14.3 The adult experiencing, or at risk of abuse or neglect will hereafter be referred to as ‘the adult’ throughout this chapter.
14.4 The safeguarding duties have a legal effect in relation to organisations other than the local authority on for example the NHS and the Police.
14.5 Where someone is 18 or over but is still receiving children’s services and a safeguarding issue is raised, the matter should be dealt with through adult safeguarding arrangements. For example, this could occur when a young person with substantial and complex needs continues to be supported in a residential educational setting until the age of 25 (see also chapter 16). Where appropriate, adult safeguarding services should involve the local authority’s children’s safeguarding colleagues as well as any relevant partners (for example, the Police or NHS) or other persons relevant to the case. However, the level of needs is not relevant, and the young adult does not need to have eligible needs for care and support under the Care Act, or be receiving any particular service from the local authority, in order for the safeguarding duties to apply – so long as the conditions set out in paragraph 14.2 are met.
14.6 Local authority statutory adult safeguarding duties apply equally to those adults with care and support needs regardless of whether those needs are being met, regardless of whether the adult lacks mental capacity or not, and regardless of setting, other than prisons and approved premises where prison governors and National Offender Management Service (NOMS) respectively have responsibility. However, senior representatives of those services may sit on the Safeguarding Adults Board and play an important role in the strategic development of adult safeguarding locally. Additionally, they may ask for advice from the local authority when faced with a safeguarding issue that they are finding particularly challenging.
Adult safeguarding – what it is and why it matters
14.7 Safeguarding means protecting an adult’s right to live in safety, free from abuse and neglect. It is about people and organisations working together to prevent and stop both the risks and experience of abuse or neglect, while at the same time making sure that the adult’s wellbeing is promoted including, where appropriate, having regard to their views, wishes, feelings and beliefs in deciding on any action. This must recognise that adults sometimes have complex interpersonal relationships and may be ambivalent, unclear or unrealistic about their personal circumstances.
14.8 Organisations should always promote the adult’s wellbeing in their safeguarding arrangements. People have complex lives and being safe is only one of the things they want for themselves. Professionals should work with the adult to establish what being safe means to them and how that can be best achieved. Professionals and other staff should not be advocating ‘safety’ measures that do not take account of individual well-being, as defined in Section 1 of the Care Act.
14.9 Safeguarding is not a substitute for:
- providers’ responsibilities to provide safe and high quality care and support
- commissioners regularly assuring themselves of the safety and effectiveness of commissioned services
- the Care Quality Commission (CQC) ensuring that regulated providers comply with the fundamental standards of care or by taking enforcement action
- the core duties of the police to prevent and detect crime and protect life and property
14.10 The Care Act requires that each local authority must:
- make enquiries, or cause others to do so, if it believes an adult is experiencing, or is at risk of, abuse or neglect (see para. 14.16 onwards). An enquiry should establish whether any action needs to be taken to prevent or stop abuse or neglect and if so, by who.
- set up a Safeguarding Adults Board (SAB) (see para. 14.133 onwards)
- arrange, where appropriate, for an independent advocate to represent and support an adult who is the subject of a safeguarding enquiry or Safeguarding Adult Review (SAR) where the adult has ‘substantial difficulty’ in being involved in the process and where there is no other suitable person to represent and support them (see chapter 7 on advocacy)
- co-operate with each of its relevant partners (as set out in Section 6 of the Care Act) in order to protect the adult. In their turn each relevant partner must also co-operate with the local authority.
14.11 The aims of adult safeguarding are to:
- prevent harm and reduce the risk of abuse or neglect to adults with care and support needs
- stop abuse or neglect wherever possible
- safeguard adults in a way that supports them in making choices and having control about how they want to live
- promote an approach that concentrates on improving life for the adults concerned
- raise public awareness so that communities as a whole, alongside professionals, play their part in preventing, identifying and responding to abuse and neglect
- provide information and support in accessible ways to help people understand the different types of abuse, how to stay safe and what to do to raise a concern about the safety or well-being of an adult
- address what has caused the abuse or neglect
14.12 In order to achieve these aims, it is necessary to:
- ensure that everyone, both individuals and organisations, are clear about their roles and responsibilities
- create strong multi-agency partnerships that provide timely and effective prevention of and responses to abuse or neglect
- support the development of a positive learning environment across these partnerships and at all levels within them to help break down cultures that are risk-averse and seek to scapegoat or blame practitioners
- enable access to mainstream community resources such as accessible leisure facilities, safe town centres and community groups that can reduce the social and physical isolation which in itself may increase the risk of abuse or neglect
- clarify how responses to safeguarding concerns deriving from the poor quality and inadequacy of service provision, including patient safety in the health sector, should be responded to
14.13 The following 6 principles apply to all sectors and settings including care and support services, further education colleges, commissioning, regulation and provision of health and care services, social work, healthcare, welfare benefits, housing, wider local authority functions and the criminal justice system. The principles should inform the ways in which professionals and other staff work with adults. The principles can also help SABs, and organisations more widely, by using them to examine and improve their local arrangements.
Six key principles underpin all adult safeguarding work
Empowerment
People being supported and encouraged to make their own decisions and informed consent.
I am asked what I want as the outcomes from the safeguarding process and these directly inform what happens.
Prevention
It is better to take action before harm occurs.
I receive clear and simple information about what abuse is, how to recognise the signs and what I can do to seek help.
Proportionality
The least intrusive response appropriate to the risk presented.
I am sure that the professionals will work in my interest, as I see them and they will only get involved as much as needed.
Protection
Support and representation for those in greatest need.
I get help and support to report abuse and neglect. I get help so that I am able to take part in the safeguarding process to the extent to which I want.
Partnership
Local solutions through services working with their communities. Communities have a part to play in preventing, detecting and reporting neglect and abuse.
I know that staff treat any personal and sensitive information in confidence, only sharing what is helpful and necessary. I am confident that professionals will work together and with me to get the best result for me.
Accountability
Accountability and transparency in delivering safeguarding.
I understand the role of everyone involved in my life and so do they.
Making safeguarding personal
14.14 In addition to these principles, it is also important that all safeguarding partners take a broad community approach to establishing safeguarding arrangements. It is vital that all organisations recognise that adult safeguarding arrangements are there to protect individuals. We all have different preferences, histories, circumstances and life-styles, so it is unhelpful to prescribe a process that must be followed whenever a concern is raised; and the case study below helps illustrate this.
Case study
Two brothers with mild learning disabilities lived in their family home, where they had remained following the death of their parents some time previously. Large amounts of rubbish had accumulated both in the garden and inside the house, with cleanliness and self-neglect also an issue. They had been targeted by fraudsters, resulting in criminal investigation and conviction of those responsible, but the brothers had refused subsequent services from adult social care and their case had been closed.
They had, however, had a good relationship with their social worker, and as concerns about their health and wellbeing continued it was decided that the social worker would maintain contact, calling in every couple of weeks to see how they were, and offer any help needed, on their terms. After almost a year, through the gradual building of trust and understanding, the brothers asked to be considered for supported housing; with the social worker’s help they improved the state of their house enough to sell it, and moved to a living environment in which practical support could be provided.
14.15 Making safeguarding personal means it should be person-led and outcome-focused. It engages the person in a conversation about how best to respond to their safeguarding situation in a way that enhances involvement, choice and control as well as improving quality of life, wellbeing and safety. Nevertheless, there are key issues that local authorities and their partners should consider. See diagrams 1A and 1B after para. 14.92 if they suspect or are made aware of abuse or neglect. See paragraph 14.231 for more detail about what such guidelines should cover.
What constitutes abuse and neglect?
14.16 This section considers the different types and patterns of abuse and neglect and the different circumstances in which they may take place. This is not intended to be an exhaustive list but an illustrative guide as to the sort of behaviour which could give rise to a safeguarding concern. This chapter also contains a number of illustrative case studies showing the action that was taken to help the adult stay or become safe.
14.17 Local authorities should not limit their view of what constitutes abuse or neglect, as they can take many forms and the circumstances of the individual case should always be considered; although the criteria at paragraph 14.2 will need to be met before the issue is considered as a safeguarding concern. Exploitation, in particular, is a common theme in the following list of the types of abuse and neglect.
Physical abuse including:
- assault
- hitting
- slapping
- pushing
- misuse of medication
- restraint
- inappropriate physical sanctions
Domestic violence including:
- psychological
- physical
- sexual
- financial
- emotional abuse
- so called ‘honour’ based violence
Sexual abuse including:
- rape
- indecent exposure
- sexual harassment
- inappropriate looking or touching
- sexual teasing or innuendo
- sexual photography
- subjection to pornography or witnessing sexual acts
- indecent exposure
- sexual assault
- sexual acts to which the adult has not consented or was pressured into consenting
Psychological abuse including:
- emotional abuse
- threats of harm or abandonment
- deprivation of contact
- humiliation
- blaming
- controlling
- intimidation
- coercion
- harassment
- verbal abuse
- cyber bullying
- isolation
- unreasonable and unjustified withdrawal of services or supportive networks
Financial or material abuse including:
- theft
- fraud
- internet scamming
- coercion in relation to an adult’s financial affairs or arrangements, including in connection with wills, property, inheritance or financial transactions
- the misuse or misappropriation of property, possessions or benefits
Modern slavery encompasses:
- slavery
- human trafficking
- forced labour and domestic servitude.
- traffickers and slave masters using whatever means they have at their disposal to coerce, deceive and force individuals into a life of abuse, servitude and inhumane treatment
Read Modern slavery: how the UK is leading the fight (PDF. 543KB) for further information.
Discriminatory abuse including forms of:
- harassment
- slurs or similar treatment:
- because of race
- gender and gender identity
- age
- disability
- sexual orientation
- religion
Read Discrimination: your rights for further information.
Organisational abuse
Including neglect and poor care practice within an institution or specific care setting such as a hospital or care home, for example, or in relation to care provided in one’s own home. This may range from one off incidents to on-going ill-treatment. It can be through neglect or poor professional practice as a result of the structure, policies, processes and practices within an organisation.
Neglect and acts of omission including:
- ignoring medical
- emotional or physical care needs
- failure to provide access to appropriate health, care and support or educational services
- the withholding of the necessities of life, such as medication, adequate nutrition and heating
Self-neglect
This covers a wide range of behaviour neglecting to care for one’s personal hygiene, health or surroundings and includes behaviour such as hoarding. It should be noted that self-neglect may not prompt a section 42 enquiry. An assessment should be made on a case by case basis. A decision on whether a response is required under safeguarding will depend on the adult’s ability to protect themselves by controlling their own behaviour. There may come a point when they are no longer able to do this, without external support.
14.18 Incidents of abuse may be one-off or multiple, and affect one person or more. Professionals and others should look beyond single incidents or individuals to identify patterns of harm, just as the CCG, as the regulator of service quality, does when it looks at the quality of care in health and care services. Repeated instances of poor care may be an indication of more serious problems and of what we now describe as organisational abuse. In order to see these patterns it is important that information is recorded and appropriately shared.
14.19 Patterns of abuse vary and include:
- serial abuse, in which the perpetrator seeks out and ‘grooms’ individuals. Sexual abuse sometimes falls into this pattern as do some forms of financial abuse
- long-term abuse, in the context of an ongoing family relationship such as domestic violence between spouses or generations or persistent psychological abuse
- opportunistic abuse, such as theft occurring because money or jewellery has been left lying around
Domestic abuse
14.20 The cross-government definition of domestic violence and abuse is: any incident or pattern of incidents of controlling, coercive, threatening behaviour, violence or abuse between those aged 16 or over who are, or have been, intimate partners or family members regardless of gender or sexuality. The abuse can encompass, but is not limited to:
- psychological
- sexual
- financial
- emotional
14.21 A new offence of coercive and controlling behaviour in intimate and familial relationships was introduced into the Serious Crime Act 2015. The offence will impose a maximum 5 years imprisonment, a fine or both.
14.22 The offence closes a gap in the law around patterns of coercive and controlling behaviour during a relationship between intimate partners, former partners who still live together, or family members, sending a clear message that it is wrong to violate the trust of those closest to you, providing better protection to victims experiencing continuous abuse and allowing for earlier identification, intervention and prevention.
14.23 The offence criminalising coercive or controlling behaviour was commenced on 29 December 2015. Read the accompanying statutory guidance for further information.
Financial abuse
14.24 Financial abuse is the main form of abuse investigated by the Office of the Public Guardian both amongst adults and children at risk. Financial recorded abuse can occur in isolation, but as research has shown, where there are other forms of abuse, there is likely to be financial abuse occurring. Although this is not always the case, everyone should also be aware of this possibility.
14.25 Potential indicators of financial abuse (PDF, 471KB) include:
- change in living conditions
- lack of heating, clothing or food
- inability to pay bills/unexplained shortage of money
- unexplained withdrawals from an account
- unexplained loss/misplacement of financial documents
- the recent addition of authorised signers on a client or donor’s signature card
- sudden or unexpected changes in a will or other financial documents
14.26 This is not an exhaustive list, nor do these examples prove that there is actual abuse occurring. However, they do indicate that a closer look and possible investigation may be needed. Read report on The Financial Abuse of Older People (PDF, 471KB)
Case study
Mrs B is an 88 year old woman with dementia who was admitted to a care home from hospital following a fall. Mrs B appointed her only daughter G, to act for her under a Lasting Power of Attorney in relation to her property and financial affairs.
Mrs B’s former home was sold and she became liable to pay the full fees of her care home. Mrs B’s daughter failed to pay the fees and arrears built up, until the home made a referral to the local authority, which in turn alerted the Office of the Public Guardian (OPG).
The OPG carried out an investigation and discovered that G was not providing her mother with any money for clothing or toiletries, which were being provided by the home from its own stocks. A visit and discussion with Mrs B revealed that she was unable to participate in any activities or outings arranged by the home, which she dearly wished to do. Her room was bare of any personal effects and she had limited stocks of underwear and nightwear.
The Police were alerted and interviewed G, who admitted using the proceeds of the mother’s house for her own benefit. The OPG applied to the Court of Protection for suspension of the power of attorney and the appointment of a deputy, who was able to seek recovery of funds and ensure Mrs B’s needs were met.
14.27 The above case study highlights the need for local authorities not to underestimate the potential impact of financial abuse. It could significantly threaten an adult’s health and wellbeing. Most financial abuse is also capable of amounting to theft or fraud and would be a matter for the police to investigate. It may also require attention and collaboration from a wider group of organisations, including shops and financial institutions such as banks.
14.28 Internet scams, postal scams and doorstep crime are more often than not, targeted at adults at risk and all are forms of financial abuse. These scams are becoming ever more sophisticated and elaborate. For example:
- internet scammers can build very convincing websites
- people can be referred to a website to check the caller’s legitimacy but this may be a copy of a legitimate website
- postal scams are massed-produced letters which are made to look like personal letters or important documents
- doorstep criminals call unannounced at the adult’s home under the guise of legitimate business and offering to fix an often non-existent problem with their property. sometimes they pose as police officers or someone in a position of authority
14.29 In all cases this is financial abuse and the adult at risk can be persuaded to part with large sums of money and in some cases their life savings. These instances should always be reported to the local police service and local authority Trading Standards Services for investigation. The SAB will need to consider how to involve local Trading Standards in its work.
14.30 These scams and crimes can seriously affect the health, including mental health, of an adult at risk. Agencies working together cab better protect adults at risk. Failure to do so can result in an increased cost to the state, especially if the adult at risk loses their income and independence.
14.31 Where the abuse is perpetrated by someone who has the authority to manage an adult’s money, the relevant body should be informed - for example, the Office of the Public Guardian for deputies or attorneys (see para 14.61) and Department for Work and Pensions (DWP) in relation to appointees.
14.32 If anyone has concerns that a DWP appointee is acting incorrectly, they should contact the DWP immediately. Note that the DWP can get things done more quickly if it also has a National Insurance number in addition to a name and address. However, people should not delay acting because they do not know an adult’s National Insurance number. The important thing is to alert DWP to their concerns. If DWP knows that the person is also known to the local authority, then it should also inform the relevant authority.
Who abuses and neglects adults?
14.33 Anyone can perpetrate abuse or neglect, including:
- spouses/partners
- other family members
- neighbours
- friends
- acquaintances
- local residents
- people who deliberately exploit adults they perceive as vulnerable to abuse
- paid staff or professionals and volunteers
- strangers
14.34 While a lot of attention is paid, for example, to targeted fraud or internet scams perpetrated by complete strangers, it is far more likely that the person responsible for abuse is known to the adult and is in a position of trust and power. Read the report on Abuse of Vulnerable Adults in England for more information.
14.35 Abuse can happen anywhere: for example, in someone’s own home, in a public place, in hospital, in a care home or in college. It can take place when an adult lives alone or with others.
Spotting signs of abuse and neglect
14.36 Workers across a wide range of organisations need to be vigilant about adult safeguarding concerns in all walks of life including, amongst others in health and social care, welfare, policing, banking, fire and rescue services and trading standards; leisure services, faith groups, and housing. GPs, in particular, are often well-placed to notice changes in an adult that may indicate they are being abused or neglected. Findings from serious case reviews have sometimes stated that if professionals or other staff had acted upon their concerns or sought more information, then death or serious harm might have been prevented. The following example illustrates that someone who might not typically be thought of, in this case the neighbour, does in fact have an important role to play in identifying when an adult is at risk.
Case study
Mr A is in his 40s, and lives in a housing association flat, with little family contact. His mental health is relatively stable, following a previous period of hospitalisation and he has visits from a mental health support worker.
He rarely goes out, but he allows people into his accommodation because of his loneliness. The police were alerted by Mr A’s neighbours to several domestic disturbances. His accommodation had been targeted by a number of local people and he had become subjected to verbal, financial and sometime physical abuse. Although Mr A initially insisted they were his friends, he did indicate he was frightened; he attended a case conference with representatives from adult social care, mental health services and the police, from which emerged a plan to strengthen his own self-protective ability as well as to deal with the present abuse.
Mr A has made different arrangements for managing his money so that he does not accumulate large sums at home. A community-based visiting service has been engaged to keep him company through visits to his home, and with time his support worker aims to help get involved in social activities that will bring more positive contacts to allay the loneliness that Mr A sees as his main challenge.
14.37 Anyone can witness or become aware of information suggesting that abuse and neglect is occurring. The matter may, for example, be raised by a worried neighbour (see above case study), a concerned bank cashier, a GP, a welfare benefits officer, a housing support worker or a nurse on a ward. Primary care staff may be particularly well-placed to spot abuse and neglect, as in many cases they may be the only professionals with whom the adult has contact. The adult may say or do things that hint that all is not well. It may come in the form of a complaint, a call for a police response, an expression of concern, or come to light during a needs assessment. Regardless of how the safeguarding concern is identified, everyone should understand what to do, and where to go locally to get help and advice. It is vital that professionals, other staff and members of the public are vigilant on behalf of those unable to protect themselves. This will include:
- knowing about different types of abuse and neglect and their signs
- supporting adults to keep safe
- knowing who to tell about suspected abuse or neglect
- supporting adults to think and weigh up the risks and benefits of different options when exercising choice and control
14.38 Awareness campaigns for the general public and multi-agency training for all staff will contribute to achieving these objectives.
Reporting and responding to abuse and neglect
14.39 It is important to understand the circumstances of abuse, including the wider context such as whether others may be at risk of abuse, whether there is any emerging pattern of abuse, whether others have witnessed abuse and the role of family members and paid staff or professionals.
14.40 The circumstances surrounding any actual or suspected case of abuse or neglect will inform the response. For example, it is important to recognise that abuse or neglect may be unintentional and may arise because a carer is struggling to care for another person. This makes the need to take action no less important, but in such circumstances, an appropriate response could be a support package for the carer and monitoring. However, the primary focus must still be how to safeguard the adult.
14.41 In other circumstances where the safeguarding concerns arise from abuse or neglect, then it would not only be necessary to immediately consider what steps are needed to protect the adult but also whether to refer the matter to the police to consider whether a criminal investigation would be required or is appropriate. It should be remembered that abuse may consist of a single or repeated act. It may be physical, verbal or psychological, an act of neglect or an omission to act. Defining abuse can be complex but it can involve an intentional, reckless, deliberate or dishonest act by the perpetrator. In any case where you encounter abuse and you are uncertain about your next steps, you should contact the police for advice.
14.42 The nature and timing of the intervention and who is best placed to lead will be, in part, determined by the circumstances. For example, where there is poor, neglectful care or practice, resulting in pressure sores for example, then an employer-led disciplinary response may be more appropriate; but this situation will need additional responses such as clinical intervention to improve the care given immediately and a clinical audit of practice. Commissioning or regulatory enforcement action may also be appropriate.
14.43 Early sharing of information is the key to providing an effective response where there are emerging concerns (see sections on information sharing, para. 14.179) and confidentiality, para. 14.186). To ensure effective safeguarding arrangements:
-
1. All organisations must have arrangements in place which set out clearly the processes and the principles for sharing information between each other, with other professionals and the SAB; this could be via an Information Sharing Agreement to formalise the arrangements.
-
2. No professional should assume that someone else will pass on information which they think may be critical to the safety and wellbeing of the adult. If a professional has concerns about the adult’s welfare and believes they are suffering or likely to suffer abuse or neglect, then they should share the information with the local authority and, or, the police if they believe or suspect that a crime has been committed.
14.44 Local authorities may choose to undertake safeguarding enquiries for people where there is not a section 42 enquiry duty, if the local authority believes it is proportionate to do so, and will enable the local authority to promote the person’s wellbeing and support a preventative agenda.
Carers and safeguarding
14.45 Circumstances in which a carer (for example, a family member or friend) could be involved in a situation that may require a safeguarding response include:
- a carer may witness or speak up about abuse or neglect
- a carer may experience intentional or unintentional harm from the adult they are trying to support or from professionals and organisations they are in contact with
- a carer may unintentionally or intentionally harm or neglect the adult they support on their own or with others
14.46 Assessment of both the carer and the adult they care for must include consideration of the wellbeing of both people. Section 1 of the Care Act includes protection from abuse and neglect as part of the definition of wellbeing. As such, a needs or carer’s assessment is an important opportunity to explore the individuals’ circumstances and consider whether it would be possible to provide information, or support that prevents abuse or neglect from occurring, for example, by providing training to the carer about the condition that the adult they care for has or to support them to care more safely. Where that is necessary the local authority should make arrangements for providing it.
14.47 If a carer speaks up about abuse or neglect, it is essential that they are listened to and that where appropriate a safeguarding enquiry is undertaken and other agencies are involved as appropriate.
14.48 If a carer experiences intentional or unintentional harm from the adult they are supporting, or if a carer unintentionally or intentionally harms or neglects the adult they support, consideration should be given to:
- whether, as part of the assessment and support planning process for the carer and, or, the adult they care for, support can be provided that removes or mitigates the risk of abuse. For example, the provision of training or information or other support that minimises the stress experienced by the carer. In some circumstances the carer may need to have independent representation or advocacy; in others, a carer may benefit from having such support if they are under great stress or similar
- whether other agencies should be involved; in some circumstances where a criminal offence is suspected this will include alerting the police, or in others the primary healthcare services may need to be involved in monitoring
14.49 Other key considerations in relation to carers should include:
- involving carers in safeguarding enquiries relating to the adult they care for, as appropriate
- whether or not joint assessment is appropriate in each individual circumstance
- the risk factors that may increase the likelihood of abuse or neglect occurring
- whether a change in circumstance changes the risk of abuse or neglect occurring
14.50 A change in circumstance should also trigger the review of the care and support plan and, or, support plan. Further information about these considerations can be found in an ADASS paper on carers and safeguarding.
Case study
Mrs D lives with her husband, B. B has a long term brain injury which affects his mood, behaviour and his ability to manage close family relationships. This has often led to him shouting and hitting out at his wife, who is also his main informal carer. Mrs D told a professional who was involved in supporting her that she was becoming increasingly frightened by B’s physical and verbal outbursts and at times feared for her personal safety.
Other family members were unaware of the extent of the harm and that Mrs D was exhausted and considering leaving the situation. The local authority became involved.
The situation presented significant personal risk to Mrs D but there was also a risk of fragmenting relationships if the local authority staff were not sensitive to the needs of the whole family. The practitioner, under supervision from her social work manager invested time in meeting with Mrs D to explore her preferences around managing her safety and how information about the situation would be communicated with the wider family and with B. This presented dilemmas around balancing the local authority’s duty of care towards
Mrs D with her wishes to remain in the situation with B. Placing emphasis on the latter inevitably meant that Mrs D would not be entirely free from the risk of harm but allowed the practitioner to explore help and support options which would enable Mrs D to manage and sustain her safety at a level which was acceptable to her.
The practitioner received regular supervision to allow time to reflect on the support being offered and to ensure that it was ‘person centred’. The outcome for Mrs D was that she was able to continue to care for B by working in partnership with the local authority. The practitioner offered advice about how to safely access help in an emergency and helped her to develop strategies to manage her own safety – this included staff building rapport with B, building on his strengths and desire to participate in social activities outside the family home. The effect of this was that some of the trigger points of him being at home with his wife for sustained periods during the day were reduced because he was there less.
Mrs D also had a number of pre-existing support avenues, including counselling and a good relationship with her son and her friends. The situation will be reviewed regularly with Mrs D but for the time being she feels much more able to manage.
Adult safeguarding procedures
14.51 In order to respond appropriately where abuse or neglect may be taking place, anyone in contact with the adult, whether in a volunteer or paid role, must understand their own role and responsibility and have access to practical and legal guidance, advice and support. This will include understanding local inter-agency policies and procedures.
14.52 In any organisation, there should be adult safeguarding policies and procedures. These should reflect this statutory guidance and the decision making tree diagram 1B (following para. 14.92) and are for use locally to support the reduction or removal of safeguarding risks, as well as to secure any support to protect the adult and, where necessary, to help the adult recover and develop resilience. Such policies and procedures should assist those working with adults how to develop swift and personalised safeguarding responses and how to involve adults in this decision making. This, in turn, should encourage proportionate responses and improve outcomes for the people concerned. Procedures may include:
- a statement of purpose relating to promoting wellbeing, preventing harm and responding effectively if concerns are raised
- a statement of roles and responsibility, authority and accountability sufficiently specific to ensure that all staff and volunteers understand their role and limitations
- a statement of the procedures for dealing with allegations of abuse, including those for dealing with emergencies by ensuring immediate safety, the processes for initially assessing abuse and neglect and deciding when intervention is appropriate, and the arrangements for reporting to the police, urgently when necessary
- a full list of points of referral indicating how to access support and advice at all times, whether in normal working hours or outside them, with a comprehensive list of contact addresses and telephone numbers, including relevant national and local voluntary bodies
- an indication of how to record allegations of abuse and neglect, any enquiry and all subsequent action
- a list of sources of expert advice
- a full description of channels of inter-agency communication and procedures for information sharing and for decision making
- a list of all services which might offer access to support or redress
- how professional disagreements are resolved especially with regard to whether decisions should be made, enquiries undertaken for example
14.53 The SAB should keep policies and procedures under review and report on these in the annual report as necessary. Procedures should be updated to incorporate learning from published research, peer reviews, case law and lessons from recent cases and Safeguarding Adults Reviews. The procedures should also include the provisions of the law – criminal, civil and statutory – relevant to adult safeguarding. This should include local or agency specific information about obtaining legal advice and access to appropriate remedies.
14.54 The Care Act requires that each local authority must arrange for an independent advocate to represent and support an adult who is the subject of a safeguarding enquiry or Safeguarding Adult Review where the adult has ‘substantial difficulty’ in being involved in the process and where there is no other suitable person to represent and support them (see Chapter 7).
The Mental Capacity Act 2005
14.55 People must be assumed to have capacity to make their own decisions and be given all practicable help before anyone treats them as not being able to make their own decisions. Where an adult is found to lack capacity to make a decision then any action taken, or any decision made for, or on their behalf, must be made in their best interests.
14.56 Professionals and other staff need to understand and always work in line with the Mental Capacity Act 2005 (MCA). They should use their professional judgement and balance many competing views. They will need considerable guidance and support from their employers if they are to help adults manage risk in ways and put them in control of decision-making if possible.
14.57 Regular face-to-face supervision from skilled managers is essential to enable staff to work confidently and competently in difficult and sensitive situations.
14.58 Mental capacity is frequently raised in relation to adult safeguarding. The requirement to apply the MCA in adult safeguarding enquiries challenges many professionals and requires utmost care, particularly where it appears an adult has capacity for making specific decisions that nevertheless places them at risk of being abused or neglected.
14.59 The MCA created the criminal offences of ill-treatment and wilful neglect in respect of people who lack the ability to make decisions. The offences can be committed by anyone responsible for that adult’s care and support – paid staff but also family carers as well as people who have the legal authority to act on that adult’s behalf (for example, persons with power of attorney or Court-appointed deputies).
14.60 These offences are punishable by fines or imprisonment. Ill-treatment covers both deliberate acts of ill-treatment and also those acts which are reckless which results in ill-treatment. Wilful neglect requires a serious departure from the required standards of treatment and usually means that a person has deliberately failed to carry out an act that they knew they were under a duty to perform.
14.61 Abuse by an attorney or deputy: If someone has concerns about the actions of an attorney acting under a registered enduring power of attorney (EPA) or lasting power of attorney (LPA), or a deputy appointed by the Court of Protection, they should contact the Office of the Public Guardian (OPG). The OPG can investigate the actions of a Deputy or Attorney and can also refer concerns to other relevant agencies. When it makes a referral, the OPG will make sure that the relevant agency keeps it informed of the action it takes. The OPG can also make an application to the Court of Protection if it needs to take possible action against the attorney or deputy. Whilst the OPG primarily investigates financial abuse, it is important to note that that it also has a duty to investigate concerns about the actions of an attorney acting under a health and welfare Lasting Power of Attorney or a personal welfare deputy. The OPG can investigate concerns about an attorney acting under a registered EPA or LPA, regardless of the adult’s capacity to make decisions. Read about the role and powers of the OPG and its policy in relation to adult safeguarding.
Multi-agency safeguarding role
Preventing abuse and neglect
14.62 The provisions of the Care Act are intended to promote and secure wellbeing. Under the definition of wellbeing (see Chapter 1, Para 1.5), it is made clear that protection from abuse and neglect is a fundamental part of that. Identification and management of risk is an essential part of the assessment process; the risk to an adult of abuse or neglect should be considered at this point.
14.63 Local authorities must cooperate with each of their relevant partners, as described in section 6(7) of the Care Act, and those partners must also cooperate with the local authority, in the exercise of their functions relevant to care and support including those to protect adults (see also chapter 15 which sets out general responsibilities in relation to co-operation).
14.64 Relevant partners of a local authority include any other local authority with whom they agree it would be appropriate to co-operate (for example, neighbouring authorities with whom they provide joint shared services) and the following agencies or bodies who operate within the local authority’s area including:
- NHS England
- CCGs
- NHS trusts and NHS foundation trusts
- Department for Work and Pensions
- the police
- prisons
- probation services
14.65 Local authorities must also co-operate with such other agencies or bodies as it considers appropriate in the exercise of its adult safeguarding functions, including (but not limited to) those listed in section 6(3):
- general practitioners
- dentists
- pharmacists
- NHS hospitals
- housing, health and care providers
14.66 Agencies should stress the need for preventing abuse and neglect wherever possible. Observant professionals and other staff making early, positive interventions with individuals and families can make a huge difference to their lives, preventing the deterioration of a situation or breakdown of a support network. It is often when people become increasingly isolated and cut off from families and friends that they become extremely vulnerable to abuse and neglect. Agencies should implement robust risk management processes in order to prevent concerns escalating to a crisis point and requiring intervention under safeguarding adult procedures.
14.67 Partners should ensure that they have the mechanisms in place that enable early identification and assessment of risk through timely information sharing and targeted multi-agency intervention. Multi-agency safeguarding hubs may be one model to support this but are not the only one. Policies and strategies for safeguarding adults should include measures to minimise the circumstances, including isolation, which make adults vulnerable to abuse.
Case study
Miss P’s mental health social worker became concerned when she had received reports that 2 of Miss P’s associates were visiting more regularly and sometimes staying over at her flat. Miss P was being coerced into prostitution and reportedly being physically assaulted by one of the men visiting her flat. There was also concern that she was being financially exploited. Miss P’s lack of understanding of how to protect herself when livng alone was exacerbated by her mental health needs and consequent inability to set safe boundaries with the people she was associating with.
The social worker recognised that the most appropriate way to enable Miss P to manage the risk of harm was to involve Miss P’s family, which she agreed to, and other professionals to develop and coordinate a plan which would enable her to continue living independently but provide a safety net for when the risk of harm became heightened. Guided initially by Miss P’s wish for the 2 men to stay away from her, the social worker initiated a planning meeting between supportive family members and other professionals such as the police, domestic violence workers, support workers and housing officers. Although Miss P herself felt unable to attend the planning meeting, her social worker ensured that her views were included and helped guide the plan. The meeting allowed family and professionals to work in partnership, to openly share information about the risks and to plan what support Miss P needed to safely maintain her independence.
Tasks were divided between the police, family members and specialist support workers. The social worker had a role in ensuring that the plan was coordinated properly and that Miss P was fully aware of everyone’s role. Miss P’s family were crucial to the success of the plan as they had always supported her and were able to advocate for her needs.
They also had a trusting relationship with her and were able to notify the police and other professionals if they thought that the risk to Miss P was increasing. The police played an active role in monitoring and preventing criminal activity towards Miss P and ensured that they kept all of the other professionals and family up to date with what was happening. Miss P is working with a domestic violence specialist to help her develop personal strategies to keep safer and her support worker is helping her to build resilience through community support and activities.
Responding to abuse and neglect in a regulated care setting
14.68 It is important that all partners are clear where responsibility lies where abuse or neglect is carried out by employees or in a regulated setting, such as a care home, hospital, or college. The first responsibility to act must be with the employing organisation as provider of the service. However, social workers or counsellors may need to be involved in order to support the adult to recover.
14.69 When an employer is aware of abuse or neglect in their organisation, then they are under a duty to correct this and protect the adult from harm as soon as possible and inform the local authority, CQC and CCG where the latter is the commissioner. Where a local authority has reasonable cause to suspect that an adult may be experiencing or at risk of abuse or neglect, then it is still under a duty to make (or cause to be made) whatever enquiries it thinks necessary to decide what if any action needs to be taken and by whom. The local authority may well be reassured by the employer’s response so that no further action is required. However, a local authority would have to satisfy itself that an employer’s response has been sufficient to deal with the safeguarding issue and, if not, to undertake any enquiry of its own and any appropriate follow up action (for example, referral to CQC, professional regulators).
14.70 The employer should investigate any concern (and provide any additional support that the adult may need) unless there is compelling reason why it is inappropriate or unsafe to do this. For example, this could be a serious conflict of interest on the part of the employer, concerns having been raised about non-effective past enquiries or serious, multiple concerns, or a matter that requires investigation by the police.
14.71 An example of a conflict of interest where it is better for an external person to be appointed to investigate may be the case of a family-run business where institutional abuse is alleged, or where the manager or owner of the service is implicated. The circumstances where an external person would be required should be set out in the local multi-agency procedures. All those carrying out such enquiries should have received appropriate training.
14.72 There should be a clear understanding between partners at a local level when other agencies such as the local authority, CQC or CCG need to be notified or involved and what role they have. ADASS, CQC, LGA, NPCC (formerly ACPO) and NHS England have jointly produced a high level guide on these roles and responsibilities. [footnote 56] The focus should be on promoting the wellbeing of those adults at risk.
14.73 Commissioners of care or other professionals should only use safeguarding procedures in a way that reflects the principles above not as a means of intimidating providers or families. Transparency, open-mindedness and timeliness are important features of fair and effective safeguarding enquiries. CQC and commissioners have alternative means of raising standards of service, including support for staff training, contract compliance and, in the case of CQC; enforcement powers may be used.
14.74 Commissioners should encourage an open culture around safeguarding, working in partnership with providers to ensure the best outcome for the adult. A disciplinary investigation, and potentially a hearing, may result in the employer taking informal or formal measures which may include dismissal and possibly referral to the Disclosure and Barring Service.
14.75 If someone is removed by being either dismissed or redeployed to a non-regulated activity, from their role providing regulated activity following a safeguarding incident, or a person leaves their role (resignation, retirement) to avoid a disciplinary hearing following a safeguarding incident and the employer/volunteer organisation feels they would have dismissed the person based on the information they hold, the regulated activity provider has a legal duty to refer to the Disclosure and Barring Service. If an agency or personnel supplier has provided the person, then the legal duty sits with that agency. In circumstances where these actions are not undertaken then the local authority can make such a referral.
Local authority’s role in carrying out enquiries
14.76 Local authorities must make enquiries, or cause others to do so, if they reasonably suspect an adult who meets the criteria at paragraph 14.2 is, or is at risk of, being abused or neglected.
14.77 An enquiry is the action taken or instigated by the local authority in response to a concern that abuse or neglect may be taking place. An enquiry could range from a conversation with the adult, or if they lack capacity, or have substantial difficulty in understanding the enquiry their representative or advocate, prior to initiating a formal enquiry under section 42, right through to a much more formal multi-agency plan or course of action. Whatever the course of subsequent action, the professional concerned should record the concern, the adult’s views, wishes, and any immediate action has taken and the reasons for those actions.
14.78 The purpose of the enquiry is to decide whether or not the local authority or another organisation, or person, should do something to help and protect the adult. If the local authority decides that another organisation should make the enquiry, for example a care provider, then the local authority should be clear about timescales, the need to know the outcomes of the enquiry and what action will follow if this is not done.
14.79 What happens as a result of an enquiry should reflect the adult‘s wishes wherever possible, as stated by them or by their representative or advocate. If they lack capacity it should be in their best interests if they are not able to make the decision, and be proportionate to the level of concern.
14.80 The adult should always be involved from the beginning of the enquiry unless there are exceptional circumstances that would increase the risk of abuse. If the adult has substantial difficulty in being involved, and where there is no one appropriate to support them, then the local authority must arrange for an independent advocate to represent them for the purpose of facilitating their involvement.
14.81 Professionals and other staff need to handle enquiries in a sensitive and skilled way to ensure distress to the adult is minimised. It is likely that many enquiries will require the input and supervision of a social worker, particularly the more complex situations and to support the adult to realise the outcomes they want and to reach a resolution or recovery. For example, where abuse or neglect is suspected within a family or informal relationship it is likely that a social worker will be the most appropriate lead. Personal and family relationships within community settings can prove both difficult and complex to assess and intervene in. The dynamics of personal relationships can be extremely difficult to judge and rebalance. For example, an adult may make a choice to be in a relationship that causes them emotional distress which outweighs, for them, the unhappiness of not maintaining the relationship.
14.82 Whilst work with the adult may frequently require the input of a social worker, other aspects of enquiries may be best undertaken by others with more appropriate skills and knowledge. For example, health professionals should undertake enquiries and treatment plans relating to medicines management or pressure sores.
Criminal offences and adult safeguarding
14.83 Everyone is entitled to the protection of the law and access to justice. Behaviour which amounts to abuse and neglect, for example physical or sexual assault or rape, psychological abuse or hate crime, wilful neglect, unlawful imprisonment, theft and fraud and certain forms of discrimination also often constitute specific criminal offences under various pieces of legislation. Although the local authority has the lead role in making enquiries, where criminal activity is suspected, then the early involvement of the police is likely to have benefits in many cases.
Case study
Miss Y is a young woman with a learning disability with limited support from her family and was not engaged with health and social care services. Miss Y was befriended by an individual who took her to parties where she was given drugs and alcohol and forced to have sex with different men. Sometimes she would be given money or gifts in return for having sex with the men.
Miss Y disclosed this to a social worker and it was discovered that there were a number of young people and vulnerable adults who were being sexually exploited by multiple perpetrators. Miss Y lacked mental capacity in order to be able to consent to having sex, as well as in relation to her accommodation, finances or personal safety.
The perpetrators sought out Miss Y and others because of their perceived vulnerability – whether that was because of their isolated situation and social circumstances coupled with age, disability, mental illness, or their previous history as a victim of abuse. The process to safeguard Miss Y involved a coordinated response between the police, social care, health and voluntary and community sector organisations.
This included the police investigating the perpetrators for rape, sexual assault, trafficking and drug offences. The Court of Protection and Deprivation of Liberty Safeguards were also used initially to safeguard Miss Y.
14.84 For the purpose of court proceedings, a witness is competent if they can understand the questions and respond in a way that the court can understand. Police have a duty under legislation to assist those witnesses who are vulnerable and intimidated. A range of special measures are available to facilitate the gathering and giving of evidence by vulnerable and intimidated witnesses. Consideration of specials measures should occur from the onset of a police investigation. In particular:
- immediate referral or consultation with the police will enable the police to establish whether a criminal act has been committed and this will give an opportunity of determining if, and at what stage, the police need to become involved further and undertake a criminal investigation
- the police have powers to initiate specific protective actions which may apply, such as Domestic Violence Protection Orders (DVPO)
- a higher standard of proof is required in criminal proceedings (‘beyond reasonable doubt’) than in disciplinary or regulatory proceedings (where the test is the balance of probabilities) and so early contact with police may assist in obtaining and securing evidence and witness statements
- early involvement of the police will help ensure that forensic evidence is not lost or contaminated
- police officers need to have considerable skill in investigating and interviewing adults with a range of disabilities and communication needs if early involvement is to prevent the adult being interviewed unnecessarily on subsequent occasions. Research has found that sometimes evidence from victims and witnesses with learning disabilities is discounted. This may also be true of others such as people with dementia. It is crucial that reasonable adjustments are made and appropriate support given, so people can get equal access to justice
- police investigations should be coordinated with health and social care enquiries but they may take priority
- guidance should include reference to support relating to criminal justice matters which is available locally from such organisations as Victim Support and court preparation schemes
- some witnesses will need protection
- the police may be able to get victim support in place
14.85 Special Measures were introduced through legislation in the Youth Justice and Criminal Evidence Act 1999 (YJCEA) and include a range of measures to support witnesses to give their best evidence and to help reduce some of the anxiety when attending court. Measures in place include the use of screens around the witness box, the use of live-link or recorded evidence-in-chief and the use of an intermediary to help witnesses understand the questions they are being asked and to give their answers accurately.
14.86 Vulnerable adult witnesses (S.16 YJCEA) have one of the following:
- mental disorder
- learning disability
- physical disability
14.87 These witnesses are only eligible for special measures if the quality of evidence that is given by them is likely to be diminished by reason of the disorder or disability.
14.88 Intimidated Witnesses (S17 YJCEA 99): Intimidated witnesses are defined by Section 17 of the Act as those whose quality of evidence is likely to be diminished by reason of fear or distress. In determining whether a witness falls into this category the court takes account of:
- the nature and alleged circumstances of the offence
- the age of the witness
- the social and cultural background and ethnic origins of the witness
- the domestic and employment circumstances of the witness
- any religious beliefs or political opinions of the witness
- any behaviour towards the witness by the accused or third party.
14.89 Also falling into this category are:
- complainants in cases of sexual assault
- witnesses to specified gun and knife offences
- victims of and witnesses to domestic violence, racially motivated crime, crime motivated by reasons relating to religion, homophobic crime, gang related violence and repeat victimisation
- those who are older and frail
- the families of homicide victims
14.90 Registered Intermediaries (RIs) have been facilitating communication with vulnerable witnesses in the criminal justice system in England and Wales since 2004.
14.91 A criminal investigation by the police takes priority over all other enquiries, although a multi-agency approach should be agreed to ensure that the interests and personal wishes of the adult will be considered throughout, even if they do not wish to provide any evidence or support a prosecution. The welfare of the adult and others, including children, is paramount and requires continued risk assessment to ensure the outcome is in their interests and enhances their wellbeing.
14.92 If the adult has the mental capacity to make informed decisions about their safety and they do not want any action to be taken, this does not preclude the sharing of information with relevant professional colleagues. This is to enable professionals to assess the risk of harm and to be confident that the adult is not being unduly influenced, coerced or intimidated and is aware of all the options. This will also enable professionals to check the safety and validity of decisions made. It is good practice to inform the adult that this action is being taken unless doing so would increase the risk of harm.
Case study
Mr P has mild learning disabilities. The safeguarding concern was financial and other abuse and neglect by his brother, with whom he lived. His support worker had noticed that Mr P had begun to appear agitated and anxious, that he looked increasingly unkempt and that he was often without money; then he suddenly stopped attending his day centre.
When the support worker and the safeguarding officer followed up, Mr P told them that at times he was not allowed out at all by his brother and was confined to his bedroom. He was only allowed to use the bathroom when his brother said he could, and often didn’t get enough to eat. He was also very worried because his bank card no longer worked, and he had no money, so couldn’t buy food for himself.
Mr P consented to move to temporary accommodation, and a case conference was held, which he attended with an advocate. At his request a move to a supported living flat was arranged and his belongings were retrieved from his brother’s property. His bank account had been emptied by his brother, so he has made new arrangements for his money.
The police are investigating both the financial abuse and the harm Mr P suffered at his brother’s hands. He has begun to talk about his experiences and is gradually regaining his confidence.
Information gathering
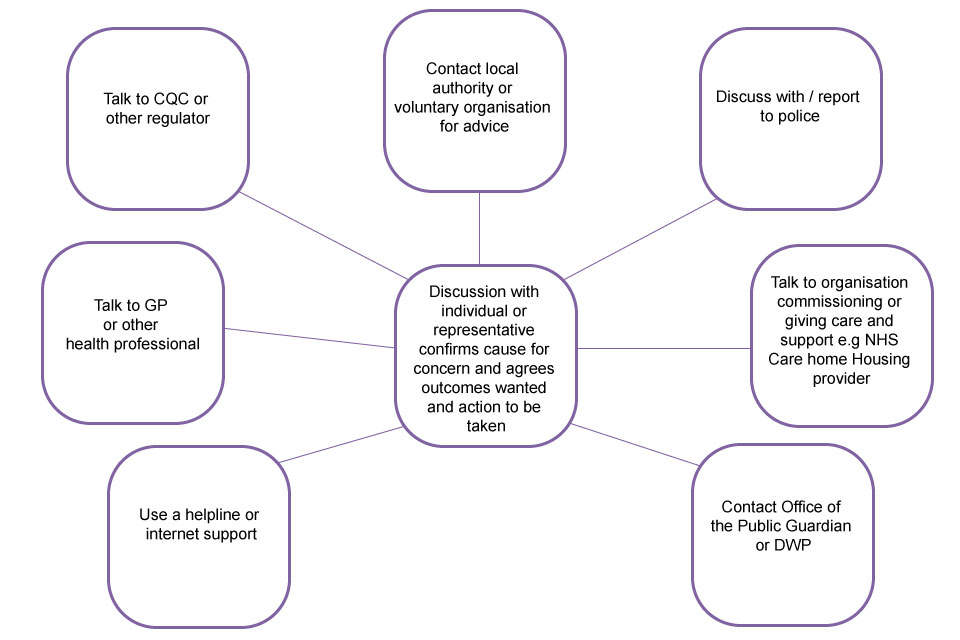
If the issue cannot be resolved through these means or the adult remains at risk of abuse or neglect (real or suspected) then the local authority’s enquiry duty under section 42 continues until it decides what action is necessary to protect the adult and by whom and ensures itself that this action has been taken.
Principles for local decision making process:
- empowerment: presumption of person led decisions and informed consent
- prevention: it is better to take action before harm occurs
- proportionate and least intrusive response appropriate to the risk presented
- protection: support and representation for those in greatest need
- partnership: local solutions through services working with their communities
- communities: have a part to play in preventing, detecting and reporting neglect and abuse
- accountability and transparency in delivering safeguarding
- feeding back whenever possible
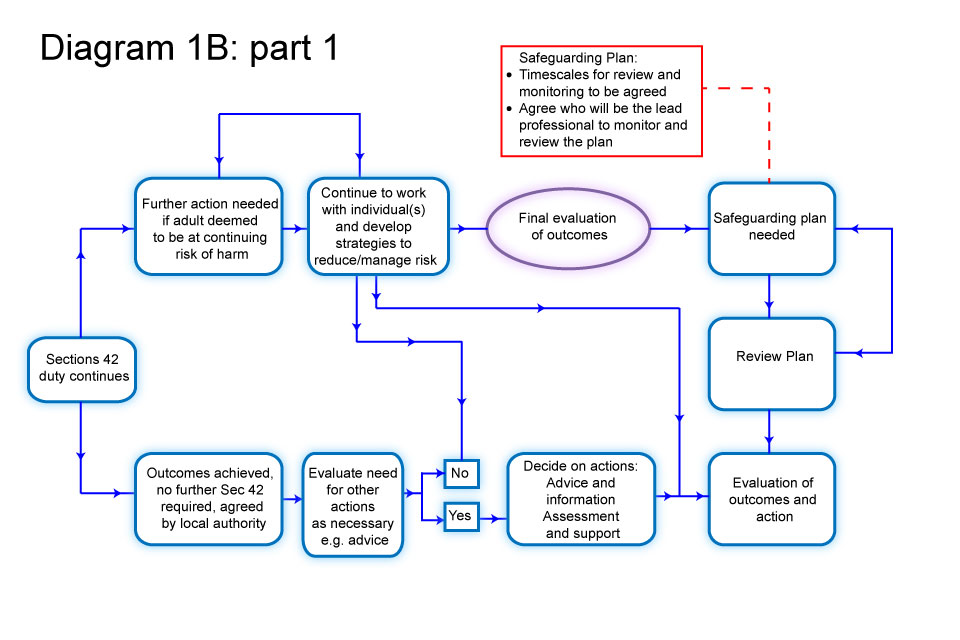
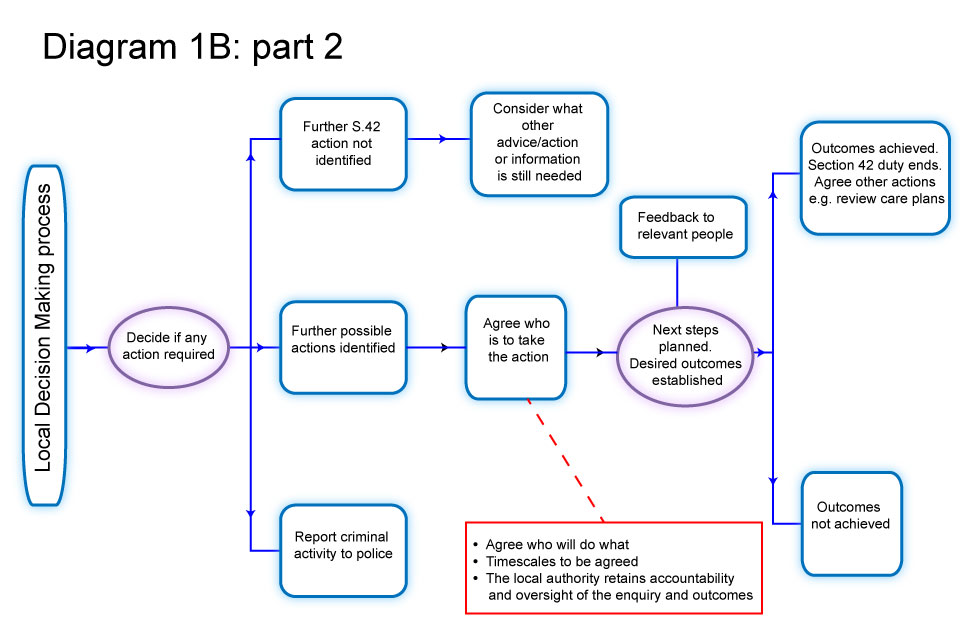
Procedures for responding in individual cases
When should an enquiry take place?
14.93 Local authorities must make enquiries, or cause another agency to do so, whenever abuse or neglect are suspected in relation to an adult and the local authority thinks it necessary to enable it to decide what (if any) action is needed to help and protect the adult. The scope of that enquiry, who leads it and its nature, and how long it takes, will depend on the particular circumstances. It will usually start with asking the adult their view and wishes which will often determine what next steps to take. Everyone involved in an enquiry must focus on improving the adult’s well-being and work together to that shared aim. At this stage, the local authority also has a duty to consider whether the adult requires an independent advocate to represent and support the adult in the enquiry. See diagrams 1A and 1B following para. 14.92, which highlight appropriate pauses for reflection, consideration and professional judgment and reflect the different routes and actions that might be taken.
Objectives of an enquiry
14.94 The objectives of an enquiry into abuse or neglect are to:
- establish facts
- ascertain the adult’s views and wishes
- assess the needs of the adult for protection, support and redress and how they might be met
- protect from the abuse and neglect, in accordance with the wishes of the adult;
- make decisions as to what follow-up action should be taken with regard to the person or organisation responsible for the abuse or neglect
- enable the adult to achieve resolution and recovery
14.95 The first priority should always be to ensure the safety and well-being of the adult. The adult should experience the safeguarding process as empowering and supportive. Practitioners should wherever practicable seek the consent of the adult before taking action. However, there may be circumstances when consent cannot be obtained because the adult lacks the capacity to give it, but it is in their best interests to undertake an enquiry. Whether or not the adult has capacity to give consent, action may need to be taken if others are or will be put at risk if nothing is done or where it is in the public interest to take action because a criminal offence has occurred. It is the responsibility of all staff and members of the public to act on any suspicion or evidence of abuse or neglect and to pass on their concerns to a responsible person or agency.
From BMA adult safeguarding toolkit:
…where a competent adult explicitly refuses any supporting intervention, this should normally be respected. Exceptions to this may be where a criminal offence may have taken place or where there may be a significant risk of harm to a third party. If, for example, there may be an abusive adult in a position of authority in relation to other vulnerable adults [sic], it may be appropriate to breach confidentiality and disclose information to an appropriate authority. Where a criminal offence is suspected it may also be necessary to take legal advice. Ongoing support should also be offered. Because an adult initially refuses the offer of assistance he or she should not therefore be lost to or abandoned by relevant services. The situation should be monitored and the individual informed that she or he can take up the offer of assistance at any time.
What should an enquiry take into account?
14.96 The wishes of the adult are very important, particularly where they have capacity to make decisions about their safeguarding. The wishes of those that lack capacity are of equal importance. Wishes need to be balanced alongside wider considerations such as the level of risk or risk to others including any children affected. All adults at risk, regardless of whether they have capacity or not may want highly intrusive help, such as the barring of a person from their home, or a person to be brought to justice or they may wish to be helped in less intrusive ways, such as through the provision of advice as to the various options available to them and the risks and advantages of these various options.
14.97 Where an adult lacks capacity to make decisions about their safeguarding plans, then a range of options should be identified, which help the adult stay as much in control of their life as possible. Wherever possible, the adult should be supported to recognise risks and to manage them. Safeguarding plans should empower the adult as far as possible to make choices and to develop their own capability to respond to them.
14.98 Any intervention in family or personal relationships needs to be carefully considered. While abusive relationships never contribute to the wellbeing of an adult, interventions which remove all contact with family members may also be experienced as abusive interventions and risk breaching the adult’s right to family life if not justified or proportionate. Safeguarding needs to recognise that the right to safety needs to be balanced with other rights, such as rights to liberty and autonomy, and rights to family life. Action might be primarily supportive or therapeutic, or it might involve the application of civil orders, sanctions, suspension, regulatory activity or criminal prosecution, disciplinary action or de-registration from a professional body.
14.99 It is important, when considering the management of any intervention or enquiry, to approach reports of incidents or allegations with an open mind. In considering how to respond the following factors need to be considered:
- the adult’s needs for care and support
- the adult’s risk of abuse or neglect
- the adult’s ability to protect themselves or the ability of their networks to increase the support they offer
- the impact on the adult, their wishes
- the possible impact on important relationships
- potential of action and increasing risk to the adult
- the risk of repeated or increasingly serious acts involving children, or another adult at risk of abuse or neglect
- the responsibility of the person or organisation that has caused the abuse or neglect
- research evidence to support any intervention
Who can carry out an enquiry?
14.100 Although the local authority is the lead agency for making enquiries, it may require others to undertake them. The specific circumstances will often determine who the right person is to begin an enquiry. In many cases a professional who already knows the adult will be the best person. They may be a social worker, a housing support worker, a GP or other health worker such as a community nurse. The local authority retains the responsibility for ensuring that the enquiry is referred to the right place and is acted upon. The local authority, in its lead and coordinating role, should assure itself that the enquiry satisfies its duty under section 42 to decide what action (if any) is necessary to help and protect the adult and by whom and to ensure that such action is taken when necessary. In this role if the local authority has asked someone else to make enquiries, it is able to challenge the body making the enquiry if it considers that the process and/or outcome is unsatisfactory.
14.101 Where a crime is suspected and referred to the police, then the police must lead the criminal investigations, with the local authority’s support where appropriate, for example by providing information and assistance. The local authority has an ongoing duty to promote the wellbeing of the adult in these circumstances.
Case study
Mr A is 24 and has autism and a mild learning disability. He is a very friendly and sociable young man, who is prone to waving and talking to most people he comes across and who sees everyone as a potential friend. However, he struggles to read the intentions of others and is easily led astray and manipulated.
He lives next door to a pub, where he knows the staff and the regulars. He also lives close to his GP and is able to access his most frequently visited places. He does, however, like to walk into town to talk to people he meets out and about. On such occasions he has been repeatedly tricked into stealing items from a newsagent by a group of teenagers and given large amounts of money away to strangers he strikes up conversations with. Due to his previous experiences, Mr A was identified during a needs assessment as being at risk of abuse and neglect and a safeguarding enquiry was triggered.
The council found that, although Mr A was not currently experiencing abuse or neglect, he remained highly vulnerable to abuse due to his being well-known in his area as someone as easy to manipulate.
To assure his safety in the future, a safeguarding plan was agreed between Mr A and a social worker. This focused on developing his social skills and understanding of relationships and boundaries and the social worker worked with Mr A to consider various support options such as having a buddy or circle of support.
The social worker put Mr A in touch with an autism social group which provided sessions on skills for staying safe. As the group was based in town, Mr A’s plan also included a support worker to accompany him. After the first 5 sessions Mr A was able to attend himself but continued to meet with his support worker on a monthly basis as part of the risk management strategy set out in his safeguarding plan.
14.102 Employers must ensure that staff, including volunteers, are trained in recognising the symptoms of abuse or neglect, how to respond and where to go for advice and assistance. These are best written down in shared policy documents that can be easily understood and used by all the key organisations.
14.103 Employers must also ensure all staff keep accurate records, stating what the facts are and what are the known opinions of professionals and others and differentiating between fact and opinion. It is vital that the views of the adult are sought and recorded. These should include the outcomes that the adult wants, such as feeling safe at home, access to community facilities, restricted or no contact with certain individuals or pursuing the matter through the criminal justice system.
What happens after an enquiry?
14.104 Once the wishes of the adult have been ascertained and an initial enquiry undertaken, discussions should be undertaken with them as to whether further enquiry is needed and what further action could be taken.
14.105 That action could take a number of courses: it could include disciplinary, complaints or criminal investigations or work by contracts managers and CQC to improve care standards. Those discussions should enable the adult to understand what their options might be and how their wishes might best be realised. Social workers must be able to set out both the civil and criminal justice approaches that are open and other approaches that might help to promote their wellbeing, such as therapeutic or family work, mediation and conflict resolution, peer or circles of support. In complex domestic circumstances, it may take the adult some time to gain the confidence and self-esteem to protect themselves and take action and their wishes may change. The police, health service and others may need to be involved to help ensure these wishes are realised.
Safeguarding plans
14.106 Once the facts have been established, a further discussion of the needs and wishes of the adult is likely to take place. This could be focused safeguarding planning to enable the adult to achieve resolution or recovery, or fuller assessments by health and social care agencies (for example, a needs assessment under the Care Act). This will entail joint discussion, decision taking and planning with the adult for their future safety and well-being. This applies if it is concluded that the allegation is true or otherwise, as many enquiries may be inconclusive.
14.107 The local authority must determine what further action is necessary. Where the local authority determines that it should itself take further action (for example, a protection plan), then the authority would be under a duty to do so.
14.108 The MCA is clear that local authorities must presume that an adult has the capacity to make a decision until there is a reason to suspect that capacity is in some way compromised; the adult is best placed to make choices about their wellbeing which may involve taking certain risks. Of course, where the adult may lack capacity to make decisions about arrangements for enquiries or managing any abusive situation, then their capacity must always be assessed and any decision made in their best interests. If the adult has the capacity to make decisions in this area of their life and declines assistance, this can limit the intervention that organisations can make. The focus should therefore be, on harm reduction. It should not however limit the action that may be required to protect others who are at risk of harm. The potential for ‘undue influence’ will need to be considered if relevant. If the adult is thought to be refusing intervention on the grounds of duress then action must be taken.
14.109 In order to make sound decisions, the adult’s emotional, physical, intellectual and mental capacity in relation to self-determination and consent and any intimidation, misuse of authority or undue influence will have to be assessed. Read the guidance on the Mental Capacity Act: making decisions for information.
Taking action
14.110 Once enquiries are completed, the outcome should be notified to the local authority which should then determine with the adult what, if any, further action is necessary and acceptable. It is for the local authority to determine the appropriateness of the outcome of the enquiry. One outcome of the enquiry may be the formulation of agreed action for the adult which should be recorded on their care plan. This will be the responsibility of the relevant agencies to implement.
14.111 In relation to the adult, this should set out:
- what steps are to be taken to assure their safety in future
- the provision of any support, treatment or therapy including on-going advocacy
- any modifications needed in the way services are provided (for example, same gender care or placement; appointment of an OPG deputy)
- how best to support the adult through any action they take to seek justice or redress;
- any on-going risk management strategy as appropriate
- any action to be taken in relation to the person or organisation that has caused the concern
Person alleged to be responsible for abuse or neglect
14.112 When a complaint or allegation has been made against a member of staff, including people employed by the adult, they should be made aware of their rights under employment legislation and any internal disciplinary procedures.
14.113 Where the person who is alleged to have carried out the abuse themselves has care and support needs and is unable to understand the significance of questions put to them or their replies, they should be assured of their right to the support of an ‘appropriate’ adult if they are questioned in relation to a suspected crime by the police under the Police and Criminal Evidence Act 1984 (PACE). Victims of crime and witnesses may also require the support of an ‘appropriate’ adult. Read government policy documents about helping victims of crime.
14.114 Under the MCA, people who lack capacity and are alleged to be responsible for abuse, are entitled to the help of an Independent Mental Capacity Advocate, to support and represent them in the enquiries that are taking place. This is separate from the decision whether or not to provide the victim of abuse with an independent advocate under the Care Act.
14.115 The Police and Crown Prosecution Service (CPS) should agree procedures with the local authority, care providers, housing providers, and the NHS/CCG to cover the following situations:
- action pending the outcome of the police and the employer’s investigations
- action following a decision to prosecute an individual
- action following a decision not to prosecute
- action pending trial
- responses to both acquittal and conviction
14.116 Employers who are also providers or commissioners of care and support not only have a duty to the adult, but also a responsibility to take action in relation to the employee when allegations of abuse are made against them. Employers should ensure that their disciplinary procedures are compatible with the responsibility to protect adults at risk of abuse or neglect.
14.117 With regard to abuse, neglect and misconduct within a professional relationship, codes of professional conduct and/or employment contracts should be followed and should determine the action that can be taken. Robust employment practices, with checkable references and recent DBS checks are important. Reports of abuse, neglect and misconduct should be investigated and evidence collected.
14.118 Where appropriate, employers should report workers to the statutory and other bodies responsible for professional regulation such as the General Medical Council and the Nursing and Midwifery Council. If someone is removed from their role providing regulated activity following a safeguarding incident the regulated activity provider (or if the person has been provided by an agency or personnel supplier, the legal duty sits with them) has a legal duty to refer to the Disclosure and Barring Service. The legal duty to refer to the Disclosure and Barring Service also applies where a person leaves their role to avoid a disciplinary hearing following a safeguarding incident and the employer/volunteer organisation feels they would have dismissed the person based on the information they hold.
14.119 The standard of proof for prosecution is ‘beyond reasonable doubt’. The standard of proof for internal disciplinary procedures and for discretionary barring consideration by the Disclosure and Barring Service (DBS) and the Vetting and Barring Board is usually the civil standard of ‘on the balance of probabilities’. This means that when criminal procedures are concluded without action being taken this does not automatically mean that regulatory or disciplinary procedures should cease or not be considered. In any event there is a legal duty to make a safeguarding referral to DBS if a person is dismissed or removed from their role due to harm to a child or a vulnerable adult.
Allegations against people in positions of trust
14.120 The local authority’s relevant partners, as set out in section 6 (7) of the Care Act, and those providing universal care and support services, should have clear policies in line with those from the safeguarding adults board for dealing with allegations against people who work, in either a paid or unpaid capacity, with adults with care and support needs. Such policies should make a clear distinction between an allegation, a concern about the quality of care or practice or a complaint.
14.121 Safeguarding adults boards need to establish and agree a framework and process for how allegations against people working with adults with care and support needs (for example, those in positions of trust) should be notified and responded to. Whilst the focus of safeguarding adults work is to safeguard one or more identified adults with care and support needs, there are occasions when incidents are reported that do not involve an adult at risk, but indicate, nevertheless, that a risk may be posed to adults at risk by a person in a position of trust.
14.122 Where such concerns are raised about someone who works with adults with care and support needs, it will be necessary for the employer (or student body or voluntary organisation) to assess any potential risk to adults with care and support needs who use their services, and, if necessary, to take action to safeguard those adults.
14.123 Examples of such concerns could include allegations that relate to a person who works with adults with care and support needs who has:
- behaved in a way that has harmed, or may have harmed an adult or child
- possibly committed a criminal offence against, or related to, an adult or child
- behaved towards an adult or child in a way that indicates they may pose a risk of harm to adults with care and support needs
14.124 When a person’s conduct towards an adult may impact on their suitability to work with or continue to work with children, this must be referred to the local authority’s designated officer.
14.125 If a local authority is given information about such concerns they should give careful consideration to what information should be shared with employers (or student body or voluntary organisation) to enable risk assessment.
14.126 Employers, student bodies and voluntary organisations should have clear procedures in place setting out the process, including timescales, for investigation and what support and advice will be available to individuals against whom allegations have been made. Any allegation against people who work with adults should be reported immediately to a senior manager within the organisation. Employers, student bodies and voluntary organisations should have their own sources of advice (including legal advice) in place for dealing with such concerns.
14.127 If an organisation removes an individual (paid worker or unpaid volunteer) from work with an adult with care and support needs (or would have, had the person not left first) because the person poses a risk of harm to adults, the organisation must make a referral to the Disclosure and Barring Service. It is an offence to fail to make a referral without good reason.
14.128 Allegations against people who work with adults at risk must not be dealt with in isolation. Any corresponding action necessary to address the welfare of adults with care and support needs should be taken without delay and in a coordinated manner, to prevent the need for further safeguarding in future.
14.129 Local authorities should ensure that their safeguarding information and advice services are clear about the responsibilities of employers, student bodies and voluntary organisations, in such cases, and signpost them to their own procedures and legal advice appropriately. Information and advice services should also be equipped to advise on appropriate information sharing and the duty to cooperate under Section 6 of the Care Act.
14.130 Local authorities should ensure that there are appropriate arrangements in place to effectively liaise with the police and other agencies to monitor the progress of cases and ensure that they are dealt with as quickly as possible, consistent with a thorough and fair process.
14.131 Decisions on sharing information must be justifiable and proportionate, based on the potential or actual harm to adults or children at risk and the rationale for decision-making should always be recorded.
14.132 When sharing information about adults, children and young people at risk between agencies it should only be shared:
- where relevant and necessary, not simply all the information held
- with the relevant people who need all or some of the information
- when there is a specific need for the information to be shared at that time
Safeguarding Adults Boards
14.133 Each local authority must set up a Safeguarding Adults Board (SAB). The main objective of a SAB is to assure itself that local safeguarding arrangements and partners act to help and protect adults in its area who meet the criteria set out at paragraph 14.2.
14.134 The SAB has a strategic role that is greater than the sum of the operational duties of the core partners. It oversees and leads adult safeguarding across the locality and will be interested in a range of matters that contribute to the prevention of abuse and neglect. These will include the safety of patients in its local health services, quality of local care and support services, effectiveness of prisons and approved premises in safeguarding offenders and awareness and responsiveness of further education services. The SAB will need intelligence on safeguarding in all providers of health and social care in its locality (not just those with whom its members commission or contract). It is important that SAB partners feel able to challenge each other and other organisations where it believes that their actions or inactions are increasing the risk of abuse or neglect. This will include commissioners, as well as providers of services.
14.135 The SAB can be an important source of advice and assistance, for example in helping others improve their safeguarding mechanisms. It is important that the SAB has effective links with other key partnerships in the locality and share relevant information and work plans. They should consciously cooperate to reduce any duplication and maximise any efficiency, particularly as objectives and membership is likely to overlap.
14.136 A SAB has 3 core duties:
- it must publish a strategic plan for each financial year that sets how it will meet its main objective and what the members will do to achieve this. The plan must be developed with local community involvement, and the SAB must consult the local Healthwatch organisation. The plan should be evidence based and make use of all available evidence and intelligence from partners to form and develop its plan
- it must publish an annual report detailing what the SAB has done during the year to achieve its main objective and implement its strategic plan, and what each member has done to implement the strategy as well as detailing the findings of any safeguarding adults reviews and subsequent action
- it must conduct any safeguarding adults review in accordance with Section 44 of the Act.
14.137 Safeguarding requires collaboration between partners in order to create a framework of inter-agency arrangements. Local authorities and their relevant partners must collaborate and work together as set out in the co-operation duties in the Care Act and, in doing so, must, where appropriate, also consider the wishes and feelings of the adult on whose behalf they are working.
14.138 Local authorities may cooperate with any other body they consider appropriate where it is relevant to their care and support functions. The lead agency with responsibility for coordinating adult safeguarding arrangements is the local authority, but all the members of the SAB should designate a lead officer. Other agencies should also consider the benefits of having a lead for adult safeguarding
14.139 Each SAB should:
- identify the role, responsibility, authority and accountability with regard to the action each agency and professional group should take to ensure the protection of adults
- establish ways of analysing and interrogating data on safeguarding notifications that increase the SAB’s understanding of prevalence of abuse and neglect locally that builds up a picture over time
- establish how it will hold partners to account and gain assurance of the effectiveness of its arrangements
- determine its arrangements for peer review and self-audit
- establish mechanisms for developing policies and strategies for protecting adults which should be formulated, not only in collaboration and consultation with all relevant agencies but also take account of the views of adults who have needs for care and support, their families, advocates and carer representatives
- develop preventative strategies that aim to reduce instances of abuse and neglect in its area
- identify types of circumstances giving grounds for concern and when they should be considered as a referral to the local authority as an enquiry
- formulate guidance about the arrangements for managing adult safeguarding, and dealing with complaints, grievances and professional and administrative malpractice in relation to safeguarding adults
- develop strategies to deal with the impact of issues of race, ethnicity, religion, gender and gender orientation, sexual orientation, age, disadvantage and disability on abuse and neglect
- balance the requirements of confidentiality with the consideration that, to protect adults, it may be necessary to share information on a ‘need-to-know basis’
- identify mechanisms for monitoring and reviewing the implementation and impact of policy and training
- carry out safeguarding adult reviews and determine any publication arrangements;
- produce a strategic plan and an annual report
- evidence how SAB members have challenged one another and held other boards to account
- promote multi-agency training and consider any specialist training that may be required. Consider any scope to jointly commission some training with other partnerships, such as the Community Safety Partnership
14.140 Strategies for the prevention of abuse and neglect is a core responsibility of a SAB and it should have an overview of how this is taking place in the area and how this work ties in with the Health and Wellbeing Board’s, Quality Surveillance Group’s (QSG), Community Safety Partnership’s and CQC’s stated approach and practice. This could be about commissioners and the regulator, together with providers, acting to address poor quality care and the intelligence that indicates there is risk that care may be deteriorating and becoming abusive or neglectful. It could also be about addressing hate crime or anti-social behaviour in a particular neighbourhood. The SAB will need to have effective links and communication across a number of networks in order to make this work effectively.
14.141 Within the context of the duties set out at paragraph 14.2, safeguarding partnerships can be a positive means of addressing issues of self-neglect. The SAB is a multi-agency group that is the appropriate forum where strategic discussions can take place on dealing with what are often complex and challenging situations for practitioners and managers as well as communities more broadly.
Case study
Recent research has identified ways of working that can have positive outcomes for those who self-neglect. [footnote 57]
Mr M, in his 70s, lives in an upper-floor council flat, and had hoarded over many years: his own possessions, items inherited from his family home, and materials he had collected from skips and building sites in case they came in useful. The material was piled from floor to ceiling in every room, and Mr M lived in a burrow tunnelled through the middle, with no lighting or heating, apart from a gas stove. Finally, after years of hiding in privacy, Mr M had realised that work being carried out on the building would lead to his living conditions being discovered. Mr M himself recounted how hard it had been for him to invite access to his home, how ashamed and scared he was, and how important his hoard was to him, having learnt as a child of the war never to waste anything.
Through working closely together, Mr M, his support worker and experienced contractors have been able gradually to remove from his flat a very large volume of hoarded material and bring improvements to his home environment. It has taken time and patience, courage and faith, and a strong relationship based on trust. The worker has not judged Mr M, and has worked at his pace, positively affirming his progress. Both Mr M and his support worker acknowledge his low self-esteem, and have connected with his doctor and mental health services. The worker has recognised the need to replace what Mr M is giving up, and has encouraged activities that reflect his interests. Mr M has valued the worker’s honesty, kindness and sensitivity, his ability to listen and the respect and reciprocity within their relationship.
14.142 Members of a SAB are expected to consider what assistance they can provide in supporting the Board in its work. This might be through payment to the local authority or to a joint fund established by the local authority to provide, for example, secretariat functions for the Board. Members might also support the work of the SAB by providing administrative help, premises for meetings or holding training sessions. It is in all core partners’ interests to have an effective SAB that is resourced adequately to carry out its functions.
14.143 Local SABs decide how they operate but they must ensure that their arrangements will be able to deliver the duties and functions under Schedule 2 of the Care Act.
14.144 The arrangements that the SAB needs to create include for example, how often it meets, the appointment of the chair, any sub-groups to it and other practical arrangements. It also needs to be clear about how it will seek feedback from the local community, particularly those adults who have been involved in a safeguarding enquiry.
Membership of safeguarding adults boards
14.145 The information about how the SAB works should be easily accessible to partner organisations and to the general public. The following organisations must be represented on the Board:
- the local authority which set it up
- the CCGs in the local authority’s area
- the chief officer of police in the local authority’s area
14.146 SABs may also include such other organisations and individuals as the establishing local authority considers appropriate having consulted its SAB partners from the CCG and police. The SAB may wish to invite additional partners to some meetings depending on the specific focus or to participate in its work more generally. Examples include:
- ambulance and fire services
- representatives of providers of health and social care services, including independent providers
- Department for Work and Pensions
- representatives of housing providers, housing support providers, probation and prison services
- general practitioners
- representatives of further education colleges
- members of user, advocacy and carer groups
- local healthwatch
- Care Quality Commission
- representatives of children’s safeguarding boards
- trading standards
14.147 This is not a definitive list, but SABs should assure themselves that the Board has the involvement of all partners necessary to effectively carry out its duties. Additionally, there may also be effective links that can be made with related partnerships to maximise impact and minimise duplication and which would reflect the reality and interconnectivities of local partnerships. There are strong synergies between the work of many of these bodies, particularly when looking at a broader family agenda as well as opportunities for efficiencies in taking forward work. The following example illustrates how a safeguarding children’s board and the domestic abuse board work collaboratively to commission and deliver training.
Example
A SAB has worked with the domestic abuse Board to develop a Multi-Agency Risk Assessment Conference (MARAC) e-learning package and to commission training in line with the domestic abuse training standards, such as: domestic abuse basic awareness; domestic abuse enhanced awareness; Domestic Abuse, Stalking and Harassment (DASH) and; MARAC awareness.
14.148 Partnerships may include:
- community safety partnerships
- local children safeguarding boards
- health and wellbeing boards
- quality surveillance groups
- clinical commissioning group boards
- health overview and scrutiny committees (OSCs)

14.149 The local authority which establishes the SAB must ensure that between them, all members of the SAB have the requisite skills and experience necessary for the SAB to act effectively and efficiently to safeguard adults in its area. For example, a social worker’s ability to understand the individual within complex social networks and other systems makes social work input a vital component in SAB arrangements; but the SAB will also require access to medical, nursing and legal expertise. Members who attend in a professional and managerial capacity should be:
- able to present issues clearly in writing and in person
- experienced in the work of their organisation
- knowledgeable about the local area and population
- able to explain their organisation’s priorities
- able to promote the aims of the SAB
- able to commit their organisation to agreed actions
- have a thorough understanding of abuse and neglect and its impact
- understand the pressures facing front line practitioners
14.150 Although it is not a requirement, the local authority should consider appointing an independent chair to the SAB who is not an employee or a member of an agency that is a member of the SAB. The chair has a critical role to lead collaboratively, give advice, support and encouragement but also to offer constructive challenge and hold main partner agencies to account and ensure that interfaces with other strategic functions are effective whilst also acting as a spokesperson for the SAB. An independent chair can provide additional reassurance that the Board has some independence from the local authority and other partners. The chair will be accountable to the chief executive of the local authority as the lead body responsible for establishing the SAB but should be appointed by the local authority in the name of the SAB having consulted all its statutory partners. There is a clear expectation that chairs will keep up to date with, and promote, good practice, developments in case law and research and any other relevant material.
14.151 The SAB must develop clear policies and processes that have been agreed with other interested parties, and that reflect the local service arrangements, roles and responsibilities. It will promote multi-agency training that ensures a common understanding of abuse and neglect, appropriate responses and agree how to work together. Policies will state what organisations and individuals are expected to do where they suspect abuse or neglect. The SAB should also consider any specialist training that is required. A key part of the SAB’s role will be to develop preventative strategies and aiming to reduce instances of abuse and neglect in its area. Members of the SAB should also be clear about how they will contribute the financial and human resources of their organisation to both preventing and responding to abuse and neglect.
SAB strategic plans
14.152 The SAB must publish its strategic plan each financial year. This plan should address both short and longer-term actions and it must set out how it will help adults in its area and what actions each member of the SAB will take to deliver the strategic plan and protect better. This plan could cover 3-5 years in order to enable the Board to plan ahead as long as it is reviewed and updated annually.
14.153 When it is preparing the plan, the SAB must consult the local Healthwatch and involve the local community. The local community has a role to play in the recognition and prevention of abuse and neglect but active and on-going work with the community is needed to tap into this source of support.
14.154 SABs must understand the many and potentially different concerns of the various groups that make up its local community. These might include such things as scams targeted at older householders, bullying and harassment of disabled people, hate crime directed at those with mental health problems, cyber bullying and the sexual exploitation of people who may lack the capacity to understand that they have the right to say no. In order to make the plan understood as widely as possible, it should be free from jargon and written in plain English with an easy read version available.
SAB annual reports
14.155 After the end of each financial year, the SAB must publish an annual report that must clearly state what both the SAB and its members have done to carry out and deliver the objectives and other content of its strategic plan. The reports should have prominence on each core member’s website and be made available to other agencies.
14.156 Specifically, the annual report must provide information about any safeguarding adults reviews (SARs) that the SAB has arranged which are ongoing or have reported in the year (regardless whether they commenced in that year). The report must state what the SAB has done to act on the findings of completed SARs or, where it has decided not to act on a finding, why not.
14.157 The annual report must set out how the SAB is monitoring progress against its policies and intentions to deliver its strategic plan. The SAB should consider the following in coming to its conclusions:
- evidence of community awareness of adult abuse and neglect and how to respond
- analysis of safeguarding data to better understand the reasons that lie behind local data returns and use the information to improve the strategic plan and operational arrangements
- what adults who have experienced the process say and the extent to which the outcomes they wanted (their wishes) have been realised
- what front line practitioners say about outcomes for adults and about their ability to work in a personalised way with those adults
- better reporting of abuse and neglect
- evidence of success of strategies to prevent abuse or neglect
- feedback from local Healthwatch, adults who use care and support services and carers, community groups, advocates, service providers and other partners
- how successful adult safeguarding is at linking with other parts of the system, for example children’s safeguarding, domestic violence, community safety
- the impact of training carried out in this area and analysis of future need; and
- how well agencies are co-operating and collaborating
14.158 Safeguarding forms one of the domains in the Adult Social Care Outcomes Framework (ASCOF). The 2014 to 2015 publication announced the development of a national measure on safeguarding outcomes – one of the first to focus on those who have been through an adult safeguarding enquiry and their views on how the enquiry was dealt with. A set of questions was developed and cognitively tested which formed the basis of a successful pilot survey undertaken by around 40 local authorities in Summer 2014. The report detailing the conclusions of the work and the recommendations for next steps can be found on HSCIC’s website. The Data and Outcomes Board (DOB) are supportive of the conclusions of the work and continue to wish to see the associated ASCOF measure taken forward. Given the resource implications and further development required to ensure the most appropriate measure is found, the indicator will remain a placeholder in forthcoming ASCOF frameworks. The materials and documentation required for local authorities to run the survey independently can be found on HSCIC’s website. Local authorities are encouraged to use them in their safeguarding processes to understand the experience of those involved in the safeguarding enquiry.
14.159 The report is meant to be a document that can be read and understood by anyone. Most SABs are likely to publish these reports on their websites. SABs should consider making the report available in a variety of media. SABs will need to establish ways of publicising the report and actively seeking feedback from communities.
14.160 Every SAB must send a copy of its report to:
- the chief executive and leader of the local authority
- the police and crime commissioner and the chief constable
- the local healthwatch
- the chair of the health and wellbeing board
14.161 It is expected that those organisations will fully consider the contents of the report and how they can improve their contributions to both safeguarding throughout their own organisation and to the joint work of the Board.
Safeguarding adults reviews (SARs)
14.162 SABs must arrange a SAR when an adult in its area dies as a result of abuse or neglect, whether known or suspected, and there is concern that partner agencies could have worked more effectively to protect the adult.
14.163 SABs must also arrange a SAR if an adult in its area has not died, but the SAB knows or suspects that the adult has experienced serious abuse or neglect. In the context of SARs, something can be considered serious abuse or neglect where, for example the individual would have been likely to have died but for an intervention, or has suffered permanent harm or has reduced capacity or quality of life (whether because of physical or psychological effects) as a result of the abuse or neglect. SABs are free to arrange for a SAR in any other situations involving an adult in its area with needs for care and support.
14.164 The SAB should be primarily concerned with weighing up what type of ‘review’ process will promote effective learning and improvement action to prevent future deaths or serious harm occurring again. This may be where a case can provide useful insights into the way organisations are working together to prevent and reduce abuse and neglect of adults. SARs may also be used to explore examples of good practice where this is likely to identify lessons that can be applied to future cases.
Case study
At the age of 72 years, Ms W, although registered disabled, was an active member in her community often seen helping at community events and visiting the local shops and swimming pool. Ms W had a fall in her home which left her lacking in confidence and fearful that she would fall again. As the winter approached, Ms W spent more time alone at home only venturing to the corner shop to buy groceries. As time passed her house came in disrepair and unhygienic as local youths began throw rubbish, including dog faeces into her front garden.
Within a 5 month period Ms W made 7 complaints to the police about anti-social behaviour in her local area, and on 2 occasions was the victim of criminal damage to the front of her house, where her wheelchair accessibility ramp has been painted by graffiti. The police made a referral to social services. As a result, Ms W was placed on a waiting list for a support service.
Four weeks after she was last seen Ms W committed suicide. A Serious Case Review (SCR) was convened according to the local policy that stated ‘the purpose of an SCR is not to reinvestigate or to apportion blame, but to establish whether there are lessons to be learnt from the circumstances of the case about the way in which local professionals and agencies work together to safeguard vulnerable adults. The published report and recommendations which followed demonstrated the lessons from this case. The resultant action plan included:
- strengthened relationships and information sharing between police officers, health and the local authority
- clear lines of reporting and joint working arrangements with the community safety partnerships
- a robust multi-agency training plan
- a targeted community programme to address anti-social behaviour
- the development of a ‘people’s panel’ as a sub group to the Safeguarding Adults Board which includes people who access services, carers and voluntary groups
- the development of a ‘stay safe’ programme involving local shops where adults at risk of abuse may report their concerns to a trusted member if their community
14.165 Early discussions need to take place with the adult, family and friends to agree how they wish to be involved. The adult who is the subject of any SAR need not have been in receipt of care and support services for the SAB to arrange a review in relation to them.
14.166 SARs should reflect the 6 safeguarding principles. SABs should agree Terms of Reference for any SAR they arrange and these should be published and openly available. When undertaking SARs the records should either be anonymised through redaction or consent should be sought.
14.167 The following principles should be applied by SABs and their partner organisations to all reviews:
- there should be a culture of continuous learning and improvement across the organisations that work together to safeguard and promote the wellbeing and empowerment of adults, identifying opportunities to draw on what works and promote good practice
- the approach taken to reviews should be proportionate according to the scale and level of complexity of the issues being examined
- reviews of serious cases should be led by individuals who are independent of the case under review and of the organisations whose actions are being reviewed
- professionals should be involved fully in reviews and invited to contribute their perspectives without fear of being blamed for actions they took in good faith
- families should be invited to contribute to reviews. They should understand how they are going to be involved and their expectations should be managed appropriately and sensitively
14.168 SARs should seek to determine what the relevant agencies and individuals involved in the case might have done differently that could have prevented harm or death. This is so that lessons can be learned from the case and those lessons applied to future cases to prevent similar harm occurring again. Its purpose is not to hold any individual or organisation to account. Other processes exist for that, including criminal proceedings, disciplinary procedures, employment law and systems of service and professional regulation, such as CQC and the Nursing and Midwifery Council, the Health and Care Professions Council, and the General Medical Council.
14.169 It is vital, if individuals and organisations are to be able to learn lessons from the past, that reviews are trusted and safe experiences that encourage honesty, transparency and sharing of information to obtain maximum benefit from them. If individuals and their organisations are fearful of SARs their response will be defensive and their participation guarded and partial.
14.170 The process for undertaking SARs should be determined locally according to the specific circumstances of individual circumstances. No one model will be applicable for all cases. The focus must be on what needs to happen to achieve understanding, remedial action and, very often, answers for families and friends of adults who have died or been seriously abused or neglected. The recommendations and action plans from a SAR need to be followed through by the SAB.
14.171 The SAB should ensure that there is appropriate involvement in the review process of professionals and organisations who were involved with the adult. The SAR should also communicate with the adult and, or, their family. In some cases it may be helpful to communicate with the person who caused the abuse or neglect.
14.172 It is expected that those undertaking a SAR will have appropriate skills and experience which should include:
- strong leadership and ability to motivate others
- expert facilitation skills and ability to handle multiple perspectives and potentially sensitive and complex group dynamics
- collaborative problem solving experience and knowledge of participative approaches
- good analytic skills and ability to manage qualitative data
- safeguarding knowledge
- inclined to promote an open, reflective learning culture
14.173 The SAB should aim for completion of a SAR within a reasonable period of time and in any event within 6 months of initiating it, unless there are good reasons for a longer period being required; for example, because of potential prejudice to related court proceedings. Every effort should be made while the SAR is in progress to capture points from the case about improvements needed; and to take corrective action.
Links with other reviews
14.174 When victims of domestic homicide are aged between 16 and 18, there are separate requirements in statutory guidance for both a child Serious Case Review (SCR) and a Domestic Homicide Review (DHR). Where such reviews may be relevant to SAR (for example, because they concern the same perpetrator), consideration should be given to how SARs, DHRs and SCRs can be managed in parallel in the most effective manner possible so that organisations and professionals can learn from the case. For example, considering whether some aspects of the reviews can be commissioned jointly so as to reduce duplication of work for the organisations involved.
14.175 In setting up a SAR the SAB should also consider how the process can dovetail with any other relevant investigations that are running parallel, such as a child SCR or DHR, a criminal investigation or an inquest.
14.176 It may be helpful when running a SAR and DHR or child SCR in parallel to establish at the outset all the relevant areas that need to be addressed, to reduce potential for duplication for families and staff. Any SAR will need to take account of a coroner‘s inquiry, and, or, any criminal investigation related to the case, including disclosure issues, to ensure that relevant information can be shared without incurring significant delay in the review process. It will be the responsibility of the manager of the SAR to ensure contact is made with the Chair of any parallel process in order to minimise avoidable duplication.
Findings from SARs
14.177 The SAB should include the findings from any SAR in its Annual Report and what actions it has taken, or intends to take in relation to those findings. Where the SAB decides not to implement an action then it must state the reason for that decision in the Annual Report. All documentation the SAB receives from registered providers which is relevant to CQC’s regulatory functions will be given to the CQC.
14.178 SAR reports should:
- provide a sound analysis of what happened, why and what action needs to be taken to prevent a reoccurrence, if possible
- be written in plain English
- contain findings of practical value to organisations and professionals
14.179 In the interest of transparency and disseminating learning the SAB should consider publishing the reports within the legal parameters about confidentiality.
Information sharing
Record-keeping
14.180 Good record keeping is a vital component of professional practice. Whenever a complaint or allegation of abuse is made, all agencies should keep clear and accurate records and each agency should identify procedures for incorporating, on receipt of a complaint or allegation, all relevant records into a file to record all action taken. When abuse or neglect is raised managers need to look for past incidents, concerns, risks and patterns. We know that in many situations, abuse and neglect arise from a range of incidents over a period of time. In the case of providers registered with CQC, records of these should be available to service commissioners and the CQC so they can take the necessary action.
14.181 Staff should be given clear direction as to what information should be recorded and in what format. The following questions are a guide:
- What information do staff need to know in order to provide a high quality response to the adult concerned?
- What information do staff need to know in order to keep adults safe under the service’s duty to protect people from harm?
- What information is not necessary?
- What is the basis for any decision to share (or not) information with a third party?
14.182 Records should be kept in such a way that the information can easily be collated for local use and national data collections.
14.183 All agencies should identify arrangements, consistent with principles and rules of fairness, confidentiality and data protection for making records available to those adults affected by, and subject to, an enquiry. If the alleged abuser is using care and support themselves, then information about their involvement in an adult safeguarding enquiry, including the outcome, should be included in their case record. If it is assessed that the individual continues to pose a threat to other people then this should be included in any information that is passed on to service providers or other people who need to know.
14.184 In order to carry out its functions, SABs will need access to information that a wide number of people or other organisations may hold. Some of these may be SAB members, such as the NHS and the police. Others will not be, such as private health and care providers or housing providers/housing support providers or education providers.
14.185 In the past, there have been instances where the withholding of information has prevented organisations being fully able to understand what ‘went wrong’ and so has hindered them identifying, to the best of their ability, the lessons to be applied to prevent or reduce the risks of such cases reoccurring. If someone knows that abuse or neglect is happening they must act upon that knowledge, not wait to be asked for information.
14.186 An SAB may request a person to supply information to it or to another person. The person who receives the request must provide the information to the SAB if:
- the request is made in order to enable or assist the SAB to do its job
- the request is made of a person who is likely to have relevant information and then either:
- the information requested relates to the person to whom the request is made and their functions or activities
- the information requested has already been supplied to another person subject to an SAB request for information
Confidentiality
14.187 Agencies should draw up a common agreement relating to confidentiality and setting out the principles governing the sharing of information, based on the welfare of the adult or of other potentially affected adults. Any agreement should be consistent with the principles set out in the Caldicott Review published 2013 (PDF, 777KB) ensuring that:
- information will only be shared on a ‘need to know’ basis when it is in the interests of the adult
- confidentiality must not be confused with secrecy
- informed consent should be obtained but, if this is not possible and other adults are at risk of abuse or neglect, it may be necessary to override the requirement
- it is inappropriate for agencies to give assurances of absolute confidentiality in cases where there are concerns about abuse, particularly in those situations when other adults may be at risk
14.188 Where an adult has refused to consent to information being disclosed for these purposes, then practitioners must consider whether there is an overriding public interest that would justify information sharing (for example, because there is a risk that others are at risk of serious harm) and wherever possible, the appropriate Caldicott Guardian should be involved. Confidentiality: NHS Code of Practice sets out guidance on public interest disclosure.
14.189 Decisions about who needs to know and what needs to be known should be taken on a case by case basis, within agency policies and the constraints of the legal framework.
14.190 Principles of confidentiality designed to safeguard and promote the interests of an adult should not be confused with those designed to protect the management interests of an organisation. These have a legitimate role but must never be allowed to conflict with the welfare of an adult. If it appears to an employee or person in a similar role that such confidentiality rules may be operating against the interests of the adult then a duty arises to make full disclosure in the public interest.
14.191 In certain circumstances, it will be necessary to exchange or disclose personal information which will need to be in accordance with the law on confidentiality and the Data Protection Act 1998 where this applies. The Home Office and the Office of the Information Commissioner have issued general guidance on the preparation and use of information sharing protocols. Information for staff, people who use care and support, carers and the general public
14.192 Information in a range of media should be produced in different, user-friendly formats for people with care and support needs and their carers. These should explain clearly what abuse is and also how to express concern and make a complaint. Adults with care and support needs and carers should be informed that their concern or complaint will be taken seriously, be dealt with independently and that they will be kept involved in the process to the degree that they wish to be. They should be reassured that they will receive help and support in taking action on their own behalf. They should also be advised that they can nominate an advocate or representative to speak and act on their behalf if they wish.
14.193 If an adult has no appropriate person to support them and has substantial difficulty in being involved in the local authority processes, they must be informed of their right to an independent advocate. Where appropriate local authorities should provide information on access to appropriate services such as how to obtain independent legal advice or counselling services for example. The involvement of adults at risk in developing such communication is sensible.
14.194 A number of local SABs or multi-agency safeguarding hubs (MASHs) have developed helpful and accessible information aimed at adults in order that they can protect themselves from abuse, such as the London Borough of Barnet’s ‘Say NO to Abuse booklet. Barnet has also produced a booklet, ‘What happens after you report abuse’.
14.195 All commissioners or providers of services in the public, voluntary or private sectors should disseminate information about the multi-agency policy and procedures. Staff should be made aware through internal guidelines of what to do when they suspect or encounter abuse of adults in vulnerable situations. This should be incorporated in staff manuals or handbooks detailing terms and conditions of appointment and other employment procedures so that individual staff members will be aware of their responsibilities in relation to safeguarding adults.
Example
Camden has developed a leaflet for carers about the harm they may experience when caring for a relative or friend and the harm they may cause. This was developed in partnership with carers’ organisations and carers themselves, and remains a partnership owned publication.
14.196 This information should emphasise that all those who express concern will be treated seriously and will receive a positive response from managers.
Local roles and responsibilities
14.197 Roles and responsibilities should be clear and collaboration should take place at all the following levels:
- operational
- supervisory line management
- practice leadership
- strategic leadership within the senior management team
- corporate/cross authority
- chief officers/chief executives
- local authority members and local police and crime commissioners
- commissioners
- providers of services
- voluntary organisations
- regulated professionals
Front line
14.198 Operational front line staff are responsible for identifying and responding to allegations of abuse and substandard practice. Staff at operational level need to share a common view of what types of behaviour may be abuse or neglect and what to do as an initial response to a suspicion or allegation that it is or has occurred. This includes GPs. It is employers’ and commissioners’ duty to set these out clearly and reinforce regularly.
14.199 It is not for front line staff to second-guess the outcome of an enquiry in deciding whether or not to share their concerns. There should be effective and well-publicised ways of escalating concerns where immediate line managers do not take action in response to a concern being raised.
14.200 Concerns about abuse or neglect must be reported whatever the source of harm is. It is imperative that poor or neglectful care is brought to the immediate attention of managers and responded to swiftly, including ensuring immediate safety and well-being of the adult. Where the source of abuse or neglect is a member of staff it is for the employer to take immediate action and record what they have done and why (similarly for volunteers and or students).
14.201 There should be clear arrangements in place about what each agency should contribute at this level. These will cover approaches to enquiries and subsequent courses of action. The local authority is responsible for ensuring effective co-ordination at this level.
Case study
A resident at a local care home told the district nurse that staff members spoke disrespectfully to her and that there were episodes of her waiting a long time for the call bell to be answered when wanting to use the commode. The resident wished to leave the home as she was very unhappy with the treatment she was receiving, and was regularly distressed and tearful.
The resident was reluctant for a formal safeguarding enquiry to take place, but did agree that the issues could be discussed with the manager. The district nurse negotiated some actions with the manager to promote good practice and address the issues that had been raised. When the district nurse reviewed the situation; the manager at the care home had dealt with the issues appropriately and devised an action plan. The resident stated that she was now happy at the care home – staff ‘couldn’t be more helpful’ - and she no longer wanted to move.
Line managers’ supervision
14.202 Skilful and knowledgeable supervision focused on outcomes for adults is critically important in safeguarding work. Managers have a central role in ensuring high standards of practice and that practitioners are properly equipped and supported. It is important to recognise that dealing with situations involving abuse and neglect can be stressful and distressing for staff and workplace support should be available.
14.203 Managers need to develop good working relationships with their counterparts in other agencies to improve cooperation locally and swiftly address any differences or difficulties that arise between front line staff or managers.
14.204 They should have access to legal advice when proposed interventions, such as the proposed stopping of contact between family members, or if it is unclear whether proposed serious and/or invasive medical treatment is likely to be in the best interests of the adult who lacks capacity to consent, require applications to the Court of Protection. Practice leadership
14.205 All social workers undertaking work with adults should have access to a source of additional advice and guidance particularly in complex and contentious situations. Principal social workers are often well-placed to perform this role or to ensure that appropriate practice supervision is available.
14.206 Principal social workers in the local authority are responsible for providing professional leadership for social work practice in their organisation and organisations undertaking statutory responsibilities on behalf of the local authority. Practice leaders/principal social workers should ensure that practice is in line with this guidance.
14.207 Making safeguarding personal represents a fundamental shift in social work practice and underpins all healthcare delivery in relation to safeguarding, with a focus on the person not the process. As the professional lead for social work, principal social workers and senior healthcare safeguarding professionals should have a broad knowledge base on safeguarding and making safeguarding personal and are confident in its application in their own and others’ work.
14.208 All providers of healthcare should have in place named professionals, who are a source of additional advice and support in complex and contentious cases within their organisation. There should be a designated professional lead in the CCG, who is a source of advice and support to the governing body in relation to the safeguarding of individuals and is able to act as the lead in the management of complex cases.
14.209 All commissioners and providers of healthcare should ensure that staff have the necessary competences and that training in place to ensure that their staff are able to deliver the service in relation to the safeguarding of individuals. This is strengthened by the development of the safeguarding adults: roles and competences for health care staff - intercollegiate document, which details the levels of training and competencies required for the different groups of staff in the organisations.
14.210 Many of the police investigators involved in safeguarding investigations specially trained for that role and work in specialist units. Each of those units has a set of arrangements to help provide advice and guidance to ensure that a thorough investigation takes place in order to achieve successful outcomes for the individual.
14.211 The police service itself has identified ways that enable non specialist officers to seek advice from supervisors at every stage of the safeguarding process, even when specialist departments are unavailable. Strategic leadership within the senior management team
14.212 Each SAB member agency - local authority, clinical commissioning groups and police, should identify a senior manager to take a lead role in the organisational and in inter-agency arrangements, including the SAB. In order for the Board to be an effective decision-making body providing leadership and accountability, members need to be sufficiently senior within their organisation and have the authority to commit the required resources and able to make strategic decisions. To achieve effective working relationships, based on trust and transparency, the members will need to understand the contexts and restraints within which their counterparts work.
14.213 All police forces in England and Wales have a head of public protection that has strategic management responsibility for all aspects of protecting people in vulnerable situations, including adults at risk. The role of the head of public protection is to build an effective working team and develop a multi-agency approach into alleged offences involving people in vulnerable circumstances. They will also have responsibility for managing and developing policy that ensures standardised processes of investigation and working practice throughout each force. The police and clinical commissioning groups are now represented at a strategic level on every local safeguarding adults board and contact details for the individuals concerned will be available to the Board and all Board members.
Corporate/cross authority roles
14.214 To ensure effective partnership working, each organisation must recognise and accept its role and functions in relation to adult safeguarding. These should be set out in the SAB’s strategic plan as well as its own communication channels. They should also have protocols for mediation and family group conferences and for various forms of dispute resolution.
Chief Officers and Chief Executives
14.215 As chief officer for the leading adult safeguarding agency, the Director of Adult Social Services (DASS) has a particularly important leadership and challenge role to play in adult safeguarding.
14.216 Responsible for promoting prevention, early intervention and partnership working is a key part of a DASS’s role and also critical in the development of effective safeguarding. Taking a personalised approach to adult safeguarding requires a DASS promoting a culture that is person-centred, supports choice and control and aims to tackle inequalities.
14.217 However, all officers, including the chief executive of the local authority, NHS and police chief officers and executives should lead and promote the development of initiatives to improve the prevention, identification and response to abuse and neglect. They need to be aware of and able to respond to national developments and ask searching questions within their own organisations to assure themselves that their systems and practices are effective in recognising and preventing abuse and neglect. The Chief Officers must sign off their organisation’s contributions to the Strategic Plan and Annual reports
14.218 Chief officers should receive regular briefings of case law from the Court of Protection and the High Courts.
Local authority members
14.219 Local authority members need to have a good understanding of the range of abuse and neglect issues that can affect adults and of the importance of balancing safeguarding with empowerment. Local authority members need to understand prevention, proportionate interventions, and the dangers of risk adverse practice and the importance of upholding human rights. Some SABs include elected members and this is one way of increasing awareness of members and ownership at a political level. Others take the view that members are more able to hold their officers to account if they have not been party to Board decision making, though they should always be aware of the work of the SAB. Managers must ensure that members are aware of any critical local issues, whether of an individual nature, matters affecting a service or a particular part of the community.
14.220 In addition, Local Authority Health Scrutiny Functions, such as the Council’s Health Overview and Scrutiny Committee, Health and Wellbeing Boards (HWBs) and Community Safety Partnerships can play a valuable role in assuring local safeguarding measures, and ensuring that SABs are accountable to local communities. Similarly, local Health and Wellbeing Boards provide leadership to the local health and wellbeing system; ensure strong partnership working between local government and the local NHS; and ensure that the needs and views of local communities are represented. HWBs can therefore play a key role in assurance and accountability of SABs and local safeguarding measures. Equally SABs may on occasion challenge the decisions of HWBs from that perspective.
Commissioners
14.221 Commissioners from the local authority, NHS and CCGs are all vital to promoting adult safeguarding. Commissioners have a responsibility to assure themselves of the quality and safety of the organisations they place contracts with and ensure that those contracts have explicit clauses that holds the providers to account for preventing and dealing promptly and appropriately with any example of abuse and neglect.
Providers of services
14.222 All service providers, including housing and housing support providers, should have clear operational policies and procedures that reflect the framework set by the SABs in consultation with them. This should include what circumstances would lead to the need to report outside their own chain of line management, including outside their organisation to the local authority. They need to share information with relevant partners such as the local authority even where they are taking action themselves. Providers should be informed of any allegation against them or their staff and treated with courtesy and openness at all times. It is of critical importance that allegations are handled sensitively and in a timely way both to stop any abuse and neglect but also to ensure a fair and transparent process. It is in no-one’s interests to unnecessarily prolong enquiries. However some complex issues may take time to resolve.
Voluntary organisations
14.223 Voluntary organisations need to work with commissioners and the SAB to agree how their role fits alongside the statutory agencies and how they should work together. This will be of particular importance where they are offering information and advice, independent advocacy, and support or counselling services in safeguarding situations. This will include telephone or on-line services. Additionally, many voluntary organisations also provide care and support services, including personal care. All voluntary organisations that work with adults need to have safeguarding procedures and lead officers.
Regulated professionals
14.224 Staff governed by professional regulation (for example, social workers, doctors, allied health professionals and nurses) should understand how their professional standards and requirements underpin their organisational roles to prevent, recognise and respond to abuse and neglect.
Recruitment and training for staff and volunteers
14.225 The SAB should ensure that relevant partners provide training for staff and volunteers on the policy, procedures and professional practices that are in place locally, which reflects their roles and responsibilities in safeguarding adult arrangements. Employers, student bodies and voluntary organisations should also undertake this, recognising their critical role in preventing and detecting abuse. This should include:
- basic mandatory induction training with respect to awareness of spotting signs of abuse and the duty to report
- more detailed awareness training, including training on recognition of abuse and responsibilities with respect to the procedures in their particular agency
- specialist training for those who will be undertaking enquiries, and managers; and, training for elected members and others for example, healthwatch members
- post qualifying or advanced training for those who work with more complex enquiries and responses or who act as their organisation’s expert in a particular field, for example in relation to legal or social work, those who provide medical or nursing advice to the organisation or the Board
14.226 Training should take place at all levels in an organisation and be updated regularly to reflect current best practice. To ensure that practice is consistent – no staff group should be excluded. Training should include issues relating to staff safety within a Health and Safety framework and also include volunteers. In a context of personalisation, boards should seek assurances that directly employed staff (for example, Personal Assistants) have access to training and advice on safeguarding.
14.227 Training is a continuing responsibility and should be provided as a rolling programme. Whilst training may be undertaken on a joint basis and the SAB has an overview of the standards and content, it is the responsibility of each organisation to ensure the effective delivery of safeguarding training to its own staff.
14.228 Regular face-to-face supervision and reflective practice, from skilled managers is essential to support staff, and to enable staff to work confidently and competently with difficult and sensitive situations.
Rigorous recruitment practices relevant to safeguarding
14.229 There are 3 levels of a Disclosure and Barring Service (DBS) check. Each contains different information and the eligibility for each check is set out in law. They are:
Standard check
This allows employers to access the criminal record history of people working, or seeking to work, in certain positions, especially those that involve working with children or adults in specific situations. A standard check discloses details of an individual’s convictions, cautions, reprimands and warnings recorded on police systems and includes both ‘spent’ and ‘unspent’ convictions.
Enhanced check
This discloses the same information provided on a Standard certificate, together with any local police information that the police believe is relevant and ought to be disclosed.
Enhanced with barred list check
This check includes the same level of disclosure as the enhanced check, plus a check of the appropriate barred lists. An individual may only be checked against the children’s and adults’ barred lists if their job falls within the definition of ‘regulated activity’ with children and/or adults under the Safeguarding Vulnerable Groups Act 2006, as amended by the Protection of Freedoms Act 2012. It should be noted that in ‘signing off’ or agreeing a personal budget or personal health budget a local authority may add conditions such as a DBS check as part of its risk assessment of safeguarding in specific cases. The local authority may also require personal budget holders using Direct Payments to specify whom they are employing to the local authority.
14.230 Skills for Care has produced a recruitment and retention toolkit for the adult care and support sector. ‘Finders Keepers’ is designed to help care providers, particularly smaller organisations, to improve the ways they recruit staff and retain them. Internal guidelines for all staff
14.231 Provider agencies should produce for their staff a set of internal guidelines which relate clearly to the multiagency policy and which set out the responsibilities of all staff to operate within it. These should include guidance on:
- identifying adults who are particularly at risk
- recognising risk from different sources and in different situations and recognising abusive or neglectful behaviour from other service users, colleagues, and family members
- routes for making a referral and channels of communication within and beyond the agency
- organisational and individual responsibilities for whistleblowing
- assurances of protection for whistle blowers
- working within best practice as specified in contracts
- working within and co-operating with regulatory mechanisms
- working within agreed operational guidelines to maintain best practice in relation to:
- challenging or distressing behaviour
- personal and intimate care
- control and restraint
- gender identity and sexual orientation
- medication
- handling of people’s money
- risk assessment and management (read risk guidance for people living with dementia)
14.232 Internal guidelines should also explain the rights of staff and how employers will respond where abuse is alleged against them within either a criminal or disciplinary context.
Integration and partnership working
This section includes chapters 15,16, 17 and 18 and has information on:
- 15. Integration, cooperation and partnerships
- 16. Transition to adult care and support
- 17. Prisons, approved premises and bail accommodation
- 18. Delegation of local authority functions
15. Integration, cooperation and partnerships
This chapter provides guidance on:
- Sections 3, 6, 7, 22, 23, 74 and Schedule 3 of the Care Act 2014
- the Care and Support (Provision of Health Services) Regulations 2014
- the Care and Support (Discharge of Hospital Patients) Regulations 2014
This chapter covers:
-
integrating care and support with other local services:
- strategic planning
- integrating service provision and combining and aligning processes
-
cooperation of partner organisations:
- general duty to cooperate
- who must cooperate
- cooperation within local authorities
- cooperating in specific cases
-
working with the NHS:
- the boundary between the NHS and care and support
- delayed transfers of care from hospitals
- working with housing authorities and providers
- working with welfare and employment support
15.1 For people to receive high quality health and care and support, local organisations need to work in a more joined-up way, to eliminate the disjointed care that is a source of frustration to people and staff, and which often results in poor care, with a negative impact on health and wellbeing. The vision is for integrated care and support that is person-centred, tailored to the needs and preferences of those needing care and support, carers and families.
15.2 Sections 3, 6 and 7 of the Act require that:
- local authorities must carry out their care and support responsibilities with the aim of promoting greater integration with NHS and other health-related services
- local authorities and their relevant partners must cooperate generally in performing their functions related to care and support; and, supplementary to this,
- in specific individual cases, local authorities and their partners must cooperate in performing their respective functions relating to care and support and carers wherever they can
Integrating care and support with other local services
15.3 Local authorities must carry out their care and support responsibilities with the aim of joining-up the services provided or other actions taken with those provided by the NHS and other health-related services (for example, housing or leisure services). This general requirement applies to all the local authority’s care and support functions for adults with needs for care and support and for carers, including in relation to preventing needs (see chapter 2), providing information and advice (see chapter 3) shaping and facilitating the market of service providers (see chapter 4), safeguarding (see chapter 14), cross-border placements (see chapter 21), and transition to adult care and support (see chapter 16).
15.4 This duty applies where the local authority considers that the integration of services will:
- promote the wellbeing of adults with care and support needs or of carers in its area
- contribute to the prevention or delay of the development of needs of people
- improve the quality of care and support in the local authority’s area, including the outcomes that are achieved for local people
15.5 The local authority is not solely responsible for promoting integration with the NHS, and this responsibility reflects similar duties placed on NHS England and clinical commissioning groups (CCGs) to promote integration with care and support. Under the NHS Act, NHS England must encourage partnership arrangements between CCGs and local authorities where it considers this would ensure the integrated provision of health services and that this would improve the quality of services or reduce inequalities. Similarly, every CCG has a duty to exercise its functions with a view to securing that health services are provided in an integrated way, where this would improve the quality of health and/or reduce inequalities in access or outcomes. The Care Act adds further coherence by placing an equivalent duty on local authorities to integrate care and support provision with health services and health related services, for example housing (see paragraphs 15.7-15.8 below about the integration of health and health related services).
15.6 There are a number of ways in which local authorities can fulfil this duty at the strategic level; at the level of individual service; and in combining and aligning processes. Some examples are discussed below.
Case study: Promoting the integration of housing, health and social care across Leicestershire
District Councils in Leicestershire have taken a strategic approach to working with county wide providers on priority issues, including housing, health and wellbeing. A District Chief Executive leads across the 7 District Councils working with a network of senior managers in each individual council. This has built the influence and credibility of District Councils with health and social care leaders who now have an increasing understanding of the vital role housing and housing based services play in the delivery of better outcomes for vulnerable people. The Housing Offer to Health in Leicestershire is built into the County`s Better Care Fund priorities and work is underway across health, social care and housing in the following key areas:
Housing’s Hospital to Home discharge pathway: looking to place housing options expertise within the day-day discharge assessment and planning work of both acute and mental health providers so that the planning and decisions around an individual’s hospital discharge includes early consideration, and actioning of appropriate and supportive housing options. * establishing an integrated service to provide practical support to people in their own homes across all tenures so that aids, equipment, adaptations, handy person services and energy efficiency interventions are available and delivered quickly. Through this we hope to reduce the time taken to provide practical help to individual people with care and support needs, reduce process costs for services paid for through the public purse and support vulnerable people to access the low level practical support that helps them remain independently at home.
Establishing a locality based approach to prevention and housing based support which includes Local Area Co-ordination, Timebanking and delivery of low level support services to vulnerable older people through a mixture of community volunteers and multi-skilled workers.
The district councils are therefore promoting wellbeing in the area of suitability of accommodation at population level, providing a basis for promoting individual wellbeing via transfers of care and universal preventative services.
Strategic planning
Integration with health and health-related services
15.7 A local authority must promote integration between care and support provision, health and health related services, with the aim of joining up services. To ensure greater integration of services, a local authority should consider the different mechanisms through which it can promote integration, for example;
a) Planning
Using adult care and support and public health data to understand the profile of the population and the needs of that population. For example, using information from the local Joint Strategic Needs Assessments to consider the wider need of that population in relation to housing (see chapter 2 for further guidance in relation to prevention). The needs of older and vulnerable residents should be reflected within local authorities’ development plans with reference to local requirements for inclusive mainstream housing and specialist accommodation and/or housing services. As part of this, local authorities can share population level data with partners to enable greater integration.
b) Commissioning
Building on joint strategic needs assessments, joint commissioning can ensure better outcomes for populations in an area. A local authority may wish to have housing represented at the Health and Wellbeing Board/Clinical Commissioning Groups (CCGs) making a visible and effective link between preventative spend (including housing related) and preventing acute/crisis interventions. Ways to achieve this include jointly-commissioned advice services covering healthcare and housing, and services like housing-related support that can provide a range of preventative interventions alongside care.
c) Assessment and information and advice
This may include integrating an assessment with information and advice about housing options on where to live, and adaptations to the home, care and related finance to help develop a care plan (if necessary), and understand housing choices reflecting the person’s strengths and capabilities to help achieve their desired outcomes. There may be occasions where non-social care professional (for example, a housing staff) knows the person best, and with their agreement may be able to contribute to the assessment process or provide information. As part of care and support planning (se chapter 10) a local area could introduce a single care plan for an individual spanning health, care and housing that is owned and directed by that person.
d) Delivery or provision of care and support
That is integrated with an assessment of the home, including general upkeep or scope for aids and adaptations, community equipment of other modifications could reduce the risk to health, help maintain independence or support reablement or recovery. For example, some specialist housing associations and home improvement agencies may offer a support service which could form part of a jointly agreed support plan. A housing assessment should form part of any assessment process, in terms of suitability, access, safety, repair, heating and lighting (for example, efficiency).
Joint strategic needs assessment
15.8 Local authorities and clinical commissioning groups already have an equal and joint duty to prepare Joint Strategic Needs Assessments (JSNAs) and Joint Health and Wellbeing Strategies (JHWS) through health and wellbeing boards. JSNAs are local assessments of current and future health and care needs that could be met by the local authority, CCGs or the NHS Commissioning Board, or other partners. JHWSs are shared strategies for meeting those needs, which set out the actions that each partner will take individually and collectively.
15.9 Joint Strategic Needs Assessments and Joint Health and Wellbeing Strategies are therefore key means by which local authorities work with CCGs to identify and plan to meet the care and support needs of the local population, including carers. JHWSs can help health and care and support services to be joined up with each other and with health-related services. Local Authorities and CCGs can include in their JHWSs a statement of how arrangements for the provision of health, social care and health-related services might be better integrated.
15.10 Under the Act, local authorities must exercise its care and support functions with a view to ensuring integration with health and health-related services if doing so would achieve any or all of the objectives set in paragraph 15.4 above (promoting wellbeing; preventing or delaying needs; improving the quality of care). The JHWSs should also set the local context and frame the discussion with partners on how different organisations can work together to align and integrate services. However, local authorities should bear in mind that carrying out the JSNA and JWHS on their own will not be sufficient to fulfil the requirement to promote integration; it will be the agreed actions which follow the strategies and plans that will have the greatest impact on integration and on the experience and outcomes of people.
Integrating service provision and combining and aligning processes
15.11 There are many ways in which local authorities can integrate care and support provision with that of health and related provision locally. Different areas are likely to find success in different models. Whilst some areas may pursue for integrated organisational structures, or shared funding arrangements, others may join up teams of frontline professionals to promote multi-disciplinary working. There is no required format or mechanism for integrating provision, and local authorities should consider and develop their strategy jointly with partners.
15.12 At the strategic level, there are many examples of how local authorities can integrate services including:
The use of ‘pooled budgets’
Which bring together funding from different organisations to invest jointly in delivering agreed, shared outcomes. For example, the Better Care Fund, which provides local authorities and CCGs with a shared fund to invest in agreed local priorities which support health and care and support, will be a key opportunity to promote integration in provision to ensure access to, and availability of, a range of preventative care and support services in the community.
The development of joint commissioning arrangements
To achieve health and wellbeing outcomes across traditional service boundaries of housing, health, care and support.
Integrated management or provision of services.
This could, for example, include jointly funding home adaptations to ensure people with changing care needs are able to maximize their independence and live well at home for longer.
15.13 In terms of working practices to encourage greater integration at an individual level, this could include recruiting and training individual care coordinators who are responsible for planning how to meet an adult’s needs through a number of service providers. Another example could be in relation to working with people who are being discharged from hospital, where staff from more than one body may be involved with providing or arranging care and support to allow the person to return home and live independently. As with other examples of integration, this would not necessarily require structural integration – for example, organisations merging – but a seamless service, from the point of view of the person, could be delivered by staff working together more effectively, for example, integrating an assessment with information and advice about housing options, or co-locating housing support workers in health and care settings like GPs surgeries or hospitals. (see paragraphs 15.54-15.75 on housing and integration).
Case study: Promoting the integration and social care with regards to carers support in Torbay and Southern Devon Health and Care NHS Trust
Torbay, a ‘Care Trust’ or organisation responsible for health and social takes a ‘whole system’ approach to the identification and support of carers. They worked with clinicians in primary care and the acute trust to develop an evidence base to show the positive impact early support and access to services has on carers’ health and wellbeing. This led to recognition that carer support is the joint responsibility of primary and acute health services and social care as well as an understanding that carers can be a ‘reluctant audience’ and may not identify themselves until in crisis.
Torbay has used joint CQUINs (commissioning for quality and innovation payments) to drive change. They developed a model founded on having Carers Support Workers at key points in the carer’s journey in all GP practices, in the Acute Hospital Discharge team and in specialist community teams such as Mental Health and Substance Misuse. These workers provide easy access to support, advice to other practitioners, and signpost carers through the system. They also target key staff groups for development; for example the 2013/14 focus has been on training and encouraging district and community nurses to identify and signpost carers to support. This has significantly increased referrals as well as raised awareness.
A pathway exercise was undertaken with staff and carers to map the carer’s journey through the whole system and the points at which engagement did, or could, happen. This has led to changes such as Carer Contact Cards, which includes key information on where carers can get support, in all discharge folders and a new Carers Policy for Torbay Hospital.
Providing simple, easy to access services for all carers such as Signpost’s information service, a Torbay carers’ register and carer education programmes, that are not subject to eligibility criteria and has brought carers into support much earlier therefore reducing crises.
15.14 Local authorities, together with their partners, should consider combining or aligning key processes in the care and support journey, where there may be benefit to the individual concerned from linking more effectively. Combined assessments should only take place in suitable circumstances and where assessors are trained to do so. For example, combining assessments may allow for a clearer picture of the person’s needs holistically, and for a single point of contact with the person to promote consistency of experience, so that provision of different types of support can be aligned. A number of assessments could be carried out on the same person, for example a care and support needs assessment, health assessment and continuing healthcare assessments. Where it is not practicable for assessments to be conducted by the same professional, it may nonetheless be possible to align processes to support a better experience, for example, the second or third assessor could be obliged to read the first assessment (provided there is a lawful basis for sharing the information) and not ask any information that has already been collected, or the different bodies could work together to develop a single, compatible assessment tool. Local authorities have powers to carry out assessments jointly with other parties, or to de-delegate the function in its entirety.
Co-operation of partner organisations
15.15 All public organisations should work together and co-operate where needed, in order to ensure a focus on the care and support (including carers’ support) and health and health-related needs of their local population. Whilst there are some local services where the local authority must actively promote integration, in other cases it must nonetheless co-operate with relevant local and national partners.
15.16 Co-operation between partners should be a general principle for all those concerned, and all should understand the reasons why co-operation is important for those people involved. The Act sets out 5 aims of co-operation between partners which are relevant to care and support, although it should be noted that the purposes of co-operation are not limited to these matters:
- promoting the wellbeing of adults needing care and support and of carers
- improving the quality of care and support for adults and support for carers (including the outcomes from such provision)
- smoothing the transition from children’s to adults’ services
- protecting adults with care and support needs who are currently experiencing or at risk of abuse or neglect
- identifying lessons to be learned from cases where adults with needs for care and support have experienced serious abuse or neglect
15.17 The processes and systems behind the areas noted above, as well as how working with partners is integral to achieving the best outcomes, are set out in more detail in other chapters of this guidance.
15.18 Local authorities and relevant partners must co-operate when exercising any respective functions which are relevant to care and support. This requirement relates to organisations existing functions only, and the Act does not confer new functions.
15.19 ‘Co-operation’, like integration, can be achieved through a number of means, and is intended to require the adoption of a common principle, rather than to prescribe any specific tasks. There are a number of powers which local authorities may use to promote joint working. For example, local authorities may share information with other partners, or provide staff, services or other resources to partners to improve co-operation. Some of the actions may be the same as those undertaken to promote integration, for example under section 75 of the NHS Act 2006, a local authority may contribute to a ‘pooled budget’ with an NHS body - a shared fund out of which payments can be made to meet agreed priorities.
15.20 Other actions may be specific to particular circumstances or the needs of a specific group, for example the local authority co-operating with prisons in its area to develop a joint strategy for meeting the care and support needs of prisoners.
Who must co-operate?
15.21 The local authority must co-operate with each of its relevant partners, and the partners must also co-operate with the local authority, in relation to relevant functions. The Act specifies the ‘relevant partners’ who have a reciprocal responsibility to co-operate. These are:
- other local authorities within the area (for example, in multi-tier authority areas, this will be a district council)
- any other local authority which would be appropriate to co-operate with in a particular set of circumstances (for example, another authority which is arranging care for a person in the home area)
- NHS bodies in the authority’s area (including the primary care, CCGs, any hospital trusts and NHS England, where it commissions health care locally) [see paragraphs 15.29-15.53 about care and support and the NHS]
- local offices of the Department for Work and Pensions, such as Job Centre Plus (see para. 15.73 about care and support, welfare and employment)
- police services in the local authority areas and prisons and probation services in the local area [see chapter 17 on care and support in Prisons]
15.22 In addition, there may be other persons or bodies with whom a local authority should co-operate if it considers this appropriate when exercising care and support functions, in particular independent or private sector organisations. Examples include, but are not limited to, care and support providers, NHS primary health providers, independent hospitals and private registered providers of social housing, the Care Quality Commission and regulators of health and social care professionals. In these cases, the local authority should consider what degree of co-operation is required, and what mechanisms it may have in place to ensure mutual co-operation (for example, via contractual means).
Ensuring co-operation within local authorities
15.23 Local authorities fulfil a range of different functions that have an impact on the health and wellbeing of individuals, in addition to their care and support responsibilities (for example, children’s services, housing, public health). It is therefore important that, in addition to ensuring co-operation between the local authority and its external partners, there is internal co-operation between the different local authority officers and professionals who provide these services. Local authorities must make arrangements to ensure co-operation between its officers responsible for adult care and support, housing, public health and children’s services, and should also consider how such arrangements may also be applied to other relevant local authority responsibilities, such as education, planning and transport. Arrangements that local authorities could make to ensure co-operation between officers include offering training and establishing systems for information sharing or multi-disciplinary teams.
15.24 For example, it is important that local authority officers responsible for housing work in co-operation with adult care and support, given that housing and suitability of living accommodation play a significant role in supporting a person to meet their needs and can help to delay that person’s deterioration. Similarly, the transition from children’s social care to adult care and support will require local authority officers in the respective departments to co-operate to share information, prepare for transition, and ensure the young person’s needs are met on reaching the age of 18. Co-operation is also needed where there are children at risk of taking on inappropriate caring roles. In these cases local authorities should be referring children for a young carer’s assessment under the Children Act and under the Care Act where the conditions in section 63 apply. Joint working with the Director of Public Health will be important when, for example, developing joint health and wellbeing strategies, and designing and commissioning preventative services.
Co-operating with partners in specific cases
15.25 Co-operation in relation to care and support functions should form part of a local authority and partners’ general strategic thinking, which should, in turn, inform how they exercise these functions day-to-day. However, there will be individual cases where more specific co-operation will be required, and a local authority or partner will need to explicitly ask one another for co-operation, for example, by requesting specific action in an individual case. The Care Act provides an express duty for the local authority and partner to ask each other for co-operation in individual cases.
15.26 Where a local authority or partner requests co-operation from each other in relation to a particular individual case, the local authority or relevant partner must co-operate as requested, unless doing so would be incompatible with their own duties or have an adverse effect on the exercise of their functions.
15.27 This mechanism is intended to support partners with a means of identifying specific cases in which more targeted co-operation is required. In practice, it may be the case that general working protocols and relationships between organisations mean that this further process is not required. However, there will be situations that arise which that necessitate a more tailored response to fit around the person concerned. This might include, for example:
- when a person is planning to move from one area to another, and the authorities involved require co-operation to support that move
- when an assessment of care and support needs identified other needs that should be assessed (for instance, health needs that may indicate eligibility for NHS Continuing Healthcare)
- when a local authority is carrying out a safeguarding enquiry or review, and requires the support of another organisation
15.28 Where the local authority or relevant partner decide to use this mechanism, they should notify the other in writing, making clear the relevant Care Act provisions. If the local authority or the relevant partner decide not to co-operate with a request, then they must write to the other, setting out reasons for not doing so. Local authorities and their relevant partners must respond to requests to cooperate under their general public law duties to act reasonably, and failure to respond within a reasonable time frame could be subject to judicial review.
Working with the NHS
The boundary between care and support and the NHS
15.29 Local authorities must carry out an assessment where someone appears to have needs for care and support. It has a duty to meet those needs for care and support that meet the eligibility criteria. Similarly, in the case of carers, the local authority must carry out an assessment if a carer appears to have, or is likely to have, needs for support and it has a duty to meet those needs for support that meet the eligibility criteria. However, local authorities cannot lawfully meet needs in either case by providing or arranging services that are legally the responsibility of the NHS.
15.30 In order to support joint working, it is important that all partners involved are clear about their own responsibilities, and how they fit together. Section 22 of the Care Act sets out the limits on what a local authority may provide by way of healthcare and so, in effect, sets the boundary between the responsibilities of local authorities for the provision of care and support, and those of the NHS for the provision of health care.
15.31 Where the NHS has a clear legal responsibility to provide a particular service, then the local authority may not do so. This general rule is intended to provide clarity and avoid overlaps, and to maintain the existing legal boundary. However, there is an exception to this general rule, in that the local authority may provide some limited healthcare services as part of a package of care and support, but only where the services provided are ‘incidental or ancillary’ (that is, relatively minor, and part of a broader package), and where the services are the type of support that an authority whose primary responsibility if to provide social services could be expected to provide.
15.32 The 2 most obvious relevant examples of healthcare that are clearly the responsibility of the NHS (and thus not something a local authority may provide) are nursing care provided by registered nurses, and services that the NHS has to provide because the individual is eligible for NHS Continuing Healthcare.
15.33 NHS Continuing Healthcare is a package of ongoing care that is arranged and funded solely by the health service for individuals outside a hospital setting who have complex ongoing healthcare needs, of a type or quantity such that they are found to have a ‘primary health need’. Such care is provided to people aged 18 or over, to meet needs that have arisen as a result of disability, accident or illness. NHS Continuing Healthcare is not dependent on a person’s condition or diagnosis, but is based on their specific physical or mental health needs.
15.34 Where the person has a ‘primary health need’ as set out in regulations and as determined following an assessment of need under national guidance in the national framework for NHS Continuing Healthcare and NHS-funded nursing care (‘the national framework’), it is the responsibility of the health service to meet all assessed health and associated care and support needs, including suitable accommodation, if that is part of the overall need.
15.35 The national framework sets out a process for the NHS, working together with its local authority partners wherever practicable, to assess health needs, decide on eligibility for NHS Continuing Healthcare, and provide that assessed care. ‘NHS-funded Nursing Care’, is the funding provided by the NHS to care homes providing nursing, to support the provision of nursing care by a registered nurse. If an individual does not qualify for NHS Continuing Healthcare, the need for care from a registered nurse must be determined. If the person has such a need and it is determined that their overall needs would be most appropriately met in a care home providing nursing care, then this would lead to eligibility for NHS-funded Nursing Care. Once the need for such care is agreed, a CCG (or in some cases NHS England) must pay a flat-rate contribution to the care home towards registered nursing care costs.
15.36 The regulations and guidance referred to above, set out how the ‘primary health need’ test takes account of the limits of local authority responsibility. Although the regulations and guidance pre-date the coming into force of the Care Act 2014, the limits of local authority responsibility have not been changed by the Care Act 2014.
Supporting discharge of hospital patients with care and support
15.37 The provisions on the discharge of hospital patients with care and support needs are contained in Schedule 3 to the Care Act 2014 and the Care and Support (Discharge of Hospital Patients) Regulations 2014 (‘the Regulations’). These provisions enable the NHS to seek reimbursement from local authorities where they consider it necessary in order to assist the NHS and local authorities in working together effectively and efficiently to plan the safe and timely discharge of NHS hospital patients from NHS acute medical care facilities to local authority care and support. The purpose of these provisions is to maintain the existing scope of the reimbursement regime but to update existing provisions to reflect the current NHS and care and support landscape. Also, in light of the drive to improve integration between health and social care provision the recovery of any reimbursement has now been placed on a discretionary rather than mandatory footing.
15.38 Schedule 3 to the Care Act covers:
- the scope of the hospital discharge regime and the definition of the patients to whom it applies
- the notifications which an NHS body must give a local authority where the NHS considers that it is not likely to be safe to discharge the patient unless arrangements for meeting the patient’s needs for care and support are put in place
- the period for which an NHS body can consider seeking reimbursement from a local authority, where that local authority has not fulfilled its requirements to assess or put in place care and support to meet needs, or (where applicable) to meet carers’ needs for support, within the time periods set such that the patient’s discharge from hospital is delayed
15.39 The Regulations and this guidance both set out further details of the form and content of what the various types of NHS notification notices must and should contain to ensure the local authority has relevant information to comply with its requirements to undertake assessments, and to put in place any arrangements necessary for meeting any of the patient’s care and support needs, or where applicable, the carer’s needs for support. They set out the circumstances when assessment notices and discharge notices must be withdrawn, and determine the period and amount of any reimbursement liability which a local authority may be required to pay the NHS for any delay in the transfer of care.
15.40 This guidance seeks to support the effective implementation of the requirements of these regulations. However, it does not address the wider practice issues associated with planning safe and effective discharge which apply to all cases of hospital discharge regardless of they whether they fall within the scope of these provisions or not. In relation to all cases, both NHS and local authorities should, using the best evidence available, develop and apply local protocols that ensure that all patients receive appropriate and safe discharge procedures.
Reimbursement as part of the wider duties to co-operate and promote integration
15.41 The NHS may seek reimbursement from local authorities for a delayed transfer of care in the circumstances set out in Schedule 3 to the Care Act and its Regulations. The potential for reimbursement liability is intended to act as an incentive to improve joint working between the NHS and local government, but should not be seen in isolation. It is a part of a wider picture in which joint and integrated working is embedded in the Act. The opportunity to seek collaborative solutions to address barriers locally in the first instance is reflected in the use of these reimbursements being made discretionary: see paragraphs 4(1) and (2) of Schedule 3 to the Act.
15.42 NHS and local authorities should develop and adopt collaborative approaches to working together in order to reduce the number of delayed days where a patient is ready to be transferred from NHS acute medical care to other settings regardless of whether the patient falls within the scope of the reimbursement regime. Both the NHS and local authorities owe a common law duty of care to the people within their care. The duties to cooperate in the Care Act 2014 also apply to all transfers of care.
15.43 The majority of delayed discharge days are attributable to the NHS and because the issues behind them are within their gift to address, it is important that NHS organisations consider what actions they need to take to support reductions in delayed discharges for which the cause is wholly within the health sector. NHS organisations should report the days for as long as the delay occurs. This reporting is required irrespective of whether the patient concerned has potential social care needs and whether the patient comes within the scope of the potential reimbursement arrangements or not.
To whom do the discharge of hospital patients provisions apply?
15.44 The discharge of hospital patients provisions only apply to NHS hospital patients in England who are receiving acute care, and who the NHS considers are likely to have care and support needs after discharge from hospital and who have not otherwise been expressly excluded. However, even where a patient falls outside the scope of these provisions, this does not means that the NHS and local authorities should not be working together to deliver the safe and timely discharge of all hospital patients with care and support needs.) More detail on the key criteria is set out below:
NHS Hospital Patient in England
A hospital patient is a person who is ordinarily resident in England who is accommodated in an NHS hospital in England, or in an independent hospital in the United Kingdom under arrangements made by an English NHS body.
Adult Care and Support Needs
In terms of age, the discharge of hospital patient provisions do not apply in respect of patients who will be under the age of 18 at the proposed date of discharge, as they will have their relevant care and support needs met by children’s social services provided under other provisions (for example, the Children Act 1989).
Acute Care
The provisions only apply to patients who are receiving, have received or can reasonably be expected to receive, acute care. Acute care means intensive medical treatment provided by or under the supervision of a consultant that lasts for a limited period after which the person receiving the treatment no longer benefits from it.
NHS hospital patients to whom the provisions do not apply
15.45 The following cases are excluded from the reimbursement regime under the Care Act:
Mental health care
Mental health care means psychiatric services, or other services provided for the purpose of preventing, diagnosing or treating illness, the arrangements for which are the primary responsibility of a consultant psychiatrist. However, if the patient is receiving treatment in an acute setting for a physical condition and is under the care of an acute medical consultant but has post-care needs that relate, for example, to their dementia, the case could fall within the scope of the discharge of hospital patient provisions. If a person is admitted with a physical condition but during their stay is subsequently transferred to the care of a consultant psychiatrist, then delays to that person’s discharge would not count towards any potential reimbursement.
Private patients
As the regime only applies to NHS patients, the Discharge of Hospital provisions do not apply to patients who have given an undertaking to pay for their care in an NHS hospital or who are accommodated at an independent hospital under private arrangements. However, patients who are admitted to NHS hospitals as private patients but who subsequently elect to change their status and become NHS patients while still receiving acute medical treatment fall within the scope of the Act from the point at which they start to be treated as NHS patients.
Other
In addition, palliative care, maternity care, intermediate care and care provided for recuperation or rehabilitation are excluded from the definition of acute care.
Patients in independent hospitals receiving NHS-commissioned acute care
15.46 NHS patients can receive acute treatment which is arranged and funded by an NHS body, but which takes place in an independent sector hospital. As such they are NHS patients, and can fall within the Discharge of Hospital Patient provisions if they also satisfy the criteria set out above.
15.47 The duty to issue notices will apply in respect of these cases, as may the potential for the NHS to seek reimbursement from the local authority for any delayed transfers of care. The Act allows an NHS body which has commissioned acute treatment at an independent hospital within the UK to make arrangements for the independent provider to issue assessment or discharge notifications on its behalf. This means that independent providers can take decisions such as whether the patient is likely to need care and support services, when the patient is to be discharged, what follow-up health needs they may have. However, the NHS body will retain ultimate responsibility for the functions, including any claim for reimbursement that might be appropriate. Working with housing authorities and providers
15.48 Housing or suitable living accommodation is a place which is safe, healthy and suitable for the needs of a person, so as to contribute to promoting physical and emotional health and wellbeing and social connections. For example, a healthy home would be dry, warm and insulated and a safe home would meet particular needs (for example, of an older person). Housing refers to the home and the neighbourhood where people live, and to the wider housing sector including staff and services around these homes.
15.49 Suitable living accommodation includes all places where people live; for example a house, flat, other general dwelling or an adult placement or other specialist housing.
15.50 Housing and the provision of suitable accommodation should be considered when considering the provision of care and support and carers’ support. The setting in which a person lives, and its suitability to their specific needs can have a major impact on the extent and means to which their care and support needs can be met, or prevented, over time. Housing is therefore a crucial health-related service which is to be integrated with care and support and health services to promote the wellbeing of adults and carers and improve the quality of services offered.
15.51 Local authorities have broad powers to provide different types of accommodation in order to meet people’s needs for care and support. The Care Act is clear that suitable accommodation can be one way of meeting care and supports needs. However, the Act is also clear on the limits of responsibilities and relationship between care and support and housing legislation, to ensure that there is no overlap or confusion. Section 23 of the Care Act clarifies the existing boundary in law between care and support relevant housing legislation, such as the Housing Act 1996. Where a local authority is required to meet accommodation related needs under housing legislation as set out in the Housing Act 1996 or under any other legislation specified in regulations (and in the case of 2 tier authorities it would include ‘another local authority’) then the local authority must meet those needs under that housing legislation. Where housing forms part of the solution to meeting a person’s needs for care and support, or preventing needs for care and support, then a local authority may include this in the care or support plan even though the housing element itself is provided under housing legislation. Any care or support needed to supplement housing is covered by this Act.
15.52 The purpose of this is to clarify the boundary in law between a local authority’s care and support function and its housing function. It does not prevent joint working, and it does not prevent local authorities in the care and support role from providing more specific services such as housing adaptations, or from working jointly with housing authorities.
15.53 Housing plays a critical role in enabling people to live independently and in helping carers to support others more effectively. Poor or inappropriate housing can put the health and wellbeing of people at risk, where as a suitable home can reduce the needs for care and support and contribute to preventing or delaying the development of such needs. Housing services should be used to help promote an individual’s wellbeing, in which people in need of care and support and carers can build a full and active life. Suitability of living accommodation is one of the matters local authorities must take into account as part of their duty to promote an individual’s wellbeing.
15.54 Consideration of housing issues in relation to a local authority’s reasonability is an integral part of the health and care system and a local authority’s responsibility for care and support. This could be in relation to a local authority’s duty on prevention (see chapter 2) or through the duty to assess an adult or carer’s needs for care and support (see chapter 6), or in providing advice and information (see chapter 3).
15.55 Enabling individuals to recognise their own skills, ambitions and priorities and developing personal and community connections in relation to housing needs can help promote an individual’s wellbeing. Supporting people through the provision of good quality information and advice can help people make early choices about their housing options and related services in advance of a potential crisis. This avoids making such decisions when a person is in crisis or when such decisions have to be taken by relatives or carers. People can be helped to stay independent longer through adaptations and modifications to their homes or extra care or support being offered in their home.
15.56 Health, care and support and housing services should centre on the individual and family, by helping them to articulate the outcomes they want to achieve a local authority can consider what support it can provide in or through the home.
Considering accommodation within the wellbeing principle
15.57 Local authorities have a general duty to promote an individual’s wellbeing when carrying out their care and support functions. The Act is clear that one specific component of wellbeing is the suitability of living accommodation. A local authority should consider suitable living accommodation in looking at a person’s needs and desired outcomes.
15.58 Housing has a vital role to play in other areas relating to a person’s wellbeing. For example access to a safe settled home underpins personal dignity. A safe suitable home can contribute to physical and mental wellbeing and can provide control over day to day life and protection from abuse and neglect. A home or suitable living accommodation can enable participation in work or education, social interactions and family relationships.
15.59 In relation to housing, a local authority can make an important contribution to an individual’s wellbeing, for example by providing and signposting information that allows people to address care and support needs through specific housing related support services, or through joint planning and commissioning that enables local authorities to provide (or arrange for the provision of) housing and care services or housing adaptations to meet the needs of the local population.
Housing to support prevention of needs
15.60 In many cases, the best way to promote someone’s wellbeing will be through preventative measures that allow people to live as independently as possible for as long as possible.
15.61 A local authority must provide or arrange for the provision of services that contribute towards preventing, reducing or delaying the needs for care and support (see chapter 2). Housing and housing related support can be a way to prevent needs for care and support, or to delay deterioration over time. Getting housing right and helping people to choose the right housing options for them can help to prevent falls, prevent hospital admissions and readmissions, reduce the need for care and support, improve wellbeing, and help maintain independence at home.
15.62 Housing and housing services can play a significant part in prevention, for example, from a design/physical perspective, accessibility, having adequate heating and lighting, identifying and removing hazards or by identifying a person who needs to be on the housing register. In addition, housing related support, for example, services that help people develop their capacity to live in the community, live independently in accommodation, or sustain their capacity to do so, such as help with welfare benefits, developing budgeting skills, help with developing social networks or taking up education, training and employment opportunities can prevent, reduce or delay the needs for care and support. Community equipment, along with telecare, aids and adaptations can support reablement, promote independence contributing to preventing the needs for care and support.
15.63 A local authority may wish to draw on the assistance of the housing authority and local housing services. Housing-related support staff and scheme managers can contribute to prevention, for example by being alert to early signs of ill health, for example, dementia, and signposting or supporting individuals to access community resources which may prevent, reduce or delay the need for care and support or a move into residential care.
15.64 The links between living in cold and damp homes and poor health and wellbeing are well-evidenced. Local authorities may wish to consider the opportunities to prevent the escalation of health and care and support needs through the delivery or facilitation of affordable warmth measures to help achieve health and wellbeing outcomes.
Integrating information and advice on housing
15.65 A local authority must establish and maintain a service for providing information and advice relating to care and support, and this must include advice on relevant housing and housing services which meet care and support needs. The authority is not required to provide all elements of this service, rather, they are expected under this duty to understand, co-ordinate and make effective use of other statutory, voluntary and or private sector information and advice resources within their area in order to deliver more integrated information and advice.
15.66 A person-centred approach to information and advice will consider the person’s strengths and capabilities and the information or advice that will help them to achieve their ambitions. Information and advice should include services in the home that bring health, care and housing services together. This means that information and advice on housing, on adaptations to the current home, or alternative housing options or housing related services should be included. This will enable a person to choose how best they can meet or prevent their needs for care and support. (See chapter 3 on information and advice).
15.67 A person using care and support or carer should be supported to make fully informed decisions about how to prevent or meet their needs for care and support. A local authority should make use of information and advice that is already available at local and national levels. Examples of some national resources are:
15.68 People’s care and support needs, their housing circumstances and financial resources are closely interconnected. It is only with full knowledge of the care and support options open to them, including possible housing options and the related financial implications that people will be able to exercise informed choice. For example, some people with their families have made early decisions about moving into residential care possibly sooner than is necessary. Information and advice about the full range of accommodation/housing options and how these might be funded can contribute to more informed decision making for individuals and can extend independent living.
Case study: Putting health back into housing
The Gloucestershire Affordable Housing Landlords’ Forum (GAHLF), comprising of the 7 leading local housing providers in the county, have set out an ‘offer’ to the Health and Wellbeing Board that demonstrates how each is working to improve the quality of life of their residents, the neighbourhoods and wider communities, by investing in new homes, supporting independent living, developing the community and supporting older and vulnerable people.
£12 million is being invested, by Stroud District Council, over 5 years, to improve the quality of housing stock and reduce fuel poverty for tenants. Stroud has been upgrading the heating supply in properties not currently served by mains gas. Many properties have electric storage heating which does not give the same level of control and is more expensive than gas or renewable energy. Dryleaze Court is a Supported Housing unit where 5 properties have had mains gas installed this year. At the same time, the team has also installed uPVC privacy panels, replaced porches with insulated cavity brick walls and fitted new double-glazed windows. The works have improved tenants’ quality of life, helping them to live more comfortably and reduce their fuel bills. All in all, over the 3 years ending March 2013, GAHLF has improved over 14,900 homes, with an estimated savings to the NHS of around £1.4 million per annum.
- Putting Health Back into Housing (PDF, 11.7MB)
- Case Study – Commissioning Advice Services in Portsmouth
Working with employment and welfare services
15.69 The Disability and Health Employment Strategy identified that many disabled people and people with health conditions, particularly those with more complex needs, receive a range of different services at local level, for example, care and support, primary and secondary health services, as well as support offered by Jobcentre Plus and contracted providers. It highlighted feedback from stakeholders that the support on offer at a local level to disabled people and people with health conditions can be confusing and inconsistent and often results in them having to give the same information to different services.
15.70 Local authorities must establish and maintain an information and advice service, but they are not required to provide all elements of this service. Rather, local authorities are expected to understand, co-ordinate and make effective use of other statutory, voluntary and/or private sector information and advice resources available to people within their areas. The information and advice available to the local population should include information and advice on eligibility and applying for disability benefits and other types of benefits and, on the availability of employment support for disabled adults.
15.71 Different people will need different levels of support from the local authority and other providers of financial information and advice depending on their capability, their care needs and their financial circumstances. People may just need some basic information and support to help them rebalance their finances in light of their changing circumstances. Topics may include welfare benefits, advice on good money management, help with basic budgeting and possibly on debt management. The local authority may be able to provide some of this information itself, for example of welfare benefits, but where it cannot, it should work with partner organisations to help people access it.
15.72 Local authorities, working with their partners, must also use the wider opportunities to provide targeted information and advice at key points in people’s contact with the care and support, health and other local services. This should include application for disability benefits such as Attendance Allowance and Personal Independence Payments, and for Carers Allowance and access to work interviews. Considering individual employment, training and education needs
15.73 In addition to considering how to join up care and support at a local level, local authorities must consider education, training and employment when working with individuals. In particular:
- local authorities must promote wellbeing when carrying out care and support functions, or making a decision in relation to a person. This applies equally to people with care and support needs and their carers. In some specific circumstances, it also applies to children, their carers and to young carers (when they are subject to the transition assessments discussed in chapter 16). The definition of wellbeing includes participation in work education and training. As such local authorities must consider whether participation in work, education or training is a relevant consideration when they are promoting wellbeing.
- local authorities, when carrying out a needs assessment, carer’s assessment or child’s carer’s assessment must have regard to whether the carer works or wishes to do so, and whether the carer is participating in or wishes to participate in education, training or recreation and this should be reflected, as appropriate in the way their needs are met. Local authorities and the Department for Work and Pensions should cooperate to ensure people are given appropriate employment support and opportunities – in particular where this is a person’s preferred outcome. This should include consideration of how direct payments may be used for employment support.
- sections 37 and 38 of the Act support people to move, including to pursue employment opportunities or move closer to family members. Local authorities must ensure continuity of care and support when people move between areas so that they can move without the fear that they will be left without the care and support they need (see chapter 20).
Sources of information
15.74 The integration clauses mirrors similar duties placed on Clinical Commissioning Groups and NHS England. There are a number of relevant documents that local authorities may find of interest:
- the Functions of Clinical Commissioning Groups
- Statutory Guidance on Joint Strategic Needs Assessments and Joint Health and Wellbeing Strategies See part 4: Promoting integration between services
- National Voices, a national coalition of health and social care charities, have produced a narrative for person-centred co-ordinated care and support, showing what this would look like from the perspective of people with care and support needs (PDF, 149KB)
15.75 The following links provide further sources of information in relation to housing service and practical examples which support integration with care and support on a local level:
- Getting to grips with integration: making housing count
- Developing your local housing offer for health and care
- Housing health and safety rating system (HHSRS) guidance
- Hospital to Home: Resource Pack
16. Transition to adult care and support
This chapter provides guidance on:
- Sections 58 to 66 of the Care Act
- The Care and Support (Children’s Carers) Regulations 2014.
This chapter covers:
- when a transition assessment must be carried out
- identifying young people who are not already receiving children’s services
- adult carers and young carers
- features of a transition assessment
- cooperation between professionals and organisation
- providing information and advice once a transition assessment is completed
- provision of age appropriate local services and resources
- after the young person in question turns 18
- combining EHC plans with care and support plans after the age of 18
- continuity of care after the age of 18
- safeguarding after the age of 18
- ordinary residence and transition to higher education
- transition from children’s to adult NHS Continuing Healthcare
16.1 Effective person-centred transition planning is essential to help young people and their families prepare for adulthood. Transition to adult care and support comes at a time when a lot of change can take place in a young person’s life. It can also mean changes to the care and support they receive from education, health and care services, or involvement with new agencies such as those who provide support for housing, employment or further education and training.
16.2 The years in which a young person is approaching adulthood should be full of opportunity. Some of the life outcomes that matter for young people approaching adulthood and their families, may include (but are not limited to):
- paid employment
- good health
- completing exams or moving to further education
- independent living (choice and control over one’s life and good housing options)
- social inclusion (friends, relationships and community)
16.3 The wellbeing of each young person or carer must be taken into account so that assessment and planning is based around the individual needs, wishes, and outcomes which matter to that person (see chapter 1 on the wellbeing principle). Historically, there has sometimes been a lack of effective planning for people using children’s services who are approaching adulthood. Looked-after children, young people with disabilities, and carers are often among the groups of people with the lowest life chances. Early conversations provide an opportunity for young people and their families to reflect on their strengths, needs and desired outcomes, and to plan ahead for how they will achieve their goals.
16.4 Professionals from different agencies, families, friends and the wider community should work together in a coordinated manner around each young person or carer to help raise their aspirations and achieve the outcomes that matter to them. The purpose of carrying out transition assessments is to provide young people and their families with information so that they know what to expect in the future and can prepare for adulthood.
16.5 Transition assessments can in themselves be of benefit in providing solutions that do not necessarily involve the provision of services, and which may aid planning that helps to prevent, reduce or delay the development of needs for care or support. The local authorities’ own commissioning and procurement practices should take account of wider market shaping duties and therefore transition assessments should focus outcomes and well–being (see section 2.15 on Market shaping and commissioning). Transition assessments will also allow local authorities to better understand the needs of people in their population, and to plan resources and commission services for young people and carers accordingly.
Definitions
16.6 The Care Act contains provisions to help preparation for adulthood for 3 particular groups of people - children, young carers and child’s carers. See list of definitions below:
Child
In the context of this chapter, a child is most probably a young person in their teenage years preparing for their adult life. This chapter therefore uses the term ‘young person’ for people under 18 with care and support needs who are approaching transition, rather than the legal term ‘child’ contained in the Care Act itself.
Young person
see above
Adult carer
An adult carer of a young person preparing for adulthood, this is equivalent to the term ‘child’s carer’ in the Care Act itself.
Young carer
A young carer under 18 preparing for adulthood themselves.
Young person or carer
This is the general term in the chapter for all 3 groups – young people, adult carers and young carers. Where something does not apply to all 3 groups, the specific groups to whom it does apply are specified using the terms above.
Transition assessment
Each group has their own specific transition assessment respectively; a child’s needs assessment, a young carer’s assessment, and a child’s carer’s assessment. The term used in this chapter for all 3 is ‘transition assessment’.
Likely need
The duty to conduct a transition assessment applies when someone is likely to have needs for care and support (or support as a carer) under the Care Act when they or the person they care for transitions to the adult system.
Significant benefit
A transition assessment must be conducted for all those who have likely needs (see above), however the timing of this assessment will depend on when it is of significant benefit to the young person or carer. This will generally be at the point when their needs for care and support as an adult can be predicted reasonably confidently, but will also depend on a range of other factors discussed in the section below ‘When a transition assessment must be carried out’.
When a transition assessment must be carried out
16.7 Transition assessments should take place at the right time for the young person or carer and at a point when the local authority can be reasonably confident about what the young person’s or carer’s needs for care or support will look like after the young person in question turns 18. There is no set age when young people reach this point; every young person and their family are different, and as such, transition assessments should take place when it is most appropriate for them.
16.8 Local authorities must carry out a transition assessment of anyone in the 3 groups when there is significant benefit to the young person or carer in doing so, and if they are likely to have needs for care or support after turning 18. The provisions in the Care Act relating to transition to adult care and support are not only for those who are already receiving children’s services, but for anyone who is likely to have needs for adult care and support after turning 18.
16.9 That a young person or carer is ‘likely to have needs’ means they have any likely appearance of any need for care and support as an adult – not just those needs that will be deemed eligible under the adult statute. It is highly likely that young people and carers who are in receipt of children’s services would be ‘likely to have needs’ in this context, and local authorities should therefore carry out a transition assessment for those who are receiving children’s services as they approach adulthood, so that they have information about what to expect when they become an adult.
16.10 When considering if it is of ‘significant benefit’ to assess, the local authority should consider the circumstances of the young person or carer, and whether it is an appropriate time for the young person or carer to undertake an assessment which helps them to prepare for adulthood. The consideration of ‘significant benefit’ is not related to the level of a young person or carer’s needs, but rather to the timing of the transition assessment. When considering whether it is of significant benefit to assess, a local authority should consider factors which may contribute to establishing the right time to assess (including but not limited to the following):
- the stage they have reached at school and any upcoming exams
- whether the young person or carer wishes to enter further/higher education or training
- whether the young person or carer wishes to get a job when they become a young adult
- whether the young person is planning to move out of their parental home into their own accommodation
- whether the young person will have care leaver status when they become 18
- whether the carer of a young person wishes to remain in or return to employment when the young person leaves full time education
- the time it may take to carry out an assessment
- the time it may take to plan and put in place the adult care and support
- any relevant family circumstances
- any planned medical treatment
16.11 For young people with special educational needs (SEN) who have an Education, Health and Care (EHC) plan under the Children and Families Act, preparation for adulthood must begin from year 9 - see Special Educational needs & Disability (SEND) Code of Practice ‘Preparing for Adulthood’ . The transition assessment should be undertaken as part of one of the annual statutory reviews of the EHC plan, and should inform a plan for the transition from children’s to adult care and support.
16.12 Equally for those without EHC plans, early conversations with local authorities about preparation for adulthood are beneficial – when these conversations begin to take place will depend on individual circumstances. For care leavers, local authorities should consider using the statutory Pathway Planning process as the opportunity to carry out a transition assessment where appropriate.
16.13 Local authorities should not carry out the transition assessment at inappropriate times in a young person’s life, such as when they are sitting their exams and it would cause disruption. The SEND Code of Practice similarly states that local authorities must minimise disruption to the child and their family – for example by combining multiple appointments where possible. Local authorities should seek to agree the best time for assessments and planning with the young person or carer, and where appropriate, their family and any other relevant partners.
16.14 A young person or carer, or someone acting on their behalf, has the right to request a transition assessment. The local authority must consider such requests and whether the likely need and significant benefit conditions apply – and if so it must undertake a transition assessment. If the local authority thinks these conditions do not apply and refuses an assessment on that basis, it must provide its reasons for this in writing in a timely manner, and it must provide information and advice on what can be done to prevent or delay the development of needs for support.
16.15 Where it is judged by the local authority that the young person or carer is likely to have needs for care and support after turning 18, but that it is not yet of significant benefit to carry out a transition assessment, the local authority should consider indicating (when providing its written reasons for refusing the assessment) when it believes the assessment will be of significant benefit. In these circumstances, the onus is on the local authority to contact the young person or carer to agree the timing of the transition assessment, rather than leaving the young person or carer in uncertainty or having to make repeated requests for an assessment.
Case study: When a transition assessment is of ‘significant benefit’ – Isabelle’s story
Isabelle is 15 years old with complex needs. She attends a residential school on a 38-week basis funded by education and social services. Care and support is currently required on the weekends and in holidays. Isabelle’s parents have approached the local authority requesting a transition assessment around the time of her 16th birthday. Initially the local authority’s reaction is that this is too soon to be of significant benefit. Since the support from school can continue until she is 19, they feel transition will be straightforward as adult services simply need to begin funding the package which is already in place.
However, when they talk in more detail to the school and the parents they realise that when Isabelle leaves school at 19 it will not be appropriate for her to live with her parents and she will require substantial supported living support and a college placement. Due to the nature of Isabelle’s needs, she will need a lengthy transition in order to get used to new staff, a new environment and a new educational setting. The college has also indicated that that they will need up to a year to plan for her start.
It is therefore of significant benefit for the transition assessment to take place around the age of 16, looking at both the funding for support from age 18 – 19 and the longer-term options. Once the assessment has identified the support Isabelle will be entitled to on leaving school, the planning process can begin and suitable support can be put in place by the time she leaves school.
If a transition assessment were to take place later, the local authority would be at risk of not promoting wellbeing in the areas of family relationships (because Isabelle could temporarily need to live with her parents while solutions are found at the last minute, which would not be appropriate) and control over day-to-day life (because Isabelle would very likely not have the same range of choices if planning and preparation were to be truncated).
16.16 Where someone is refused (or they themselves refuse) a transition assessment, but at a later time makes a request for an assessment, the local authority must again consider whether the likely need and significant benefit conditions apply, and carry out an assessment if so. In more complex cases, it can take some time not only to carry out the assessment itself but to plan and put in place care and support. Social workers will often be the most appropriate lead professionals for complex cases. Transition assessments should be carried out early enough to ensure that the right care and support is in place when the young person moves to adult care and support.
16.17 When transition assessments take place too late and care and support is arranged in a hurry, it can result in care and support which does not best meet the young person or carer’s needs – and sometimes at greater financial cost to the local authority than if it had been planned properly in advance.
Identifying young people and young carers who are not already receiving children’s services
16.18 Most young people who receive transition assessments will be children in need under the Children Act 1989 and will already be known to local authorities. However, local authorities should consider how they can identify young people who are not receiving children’s services who are likely to have care and support needs as an adult. Key examples include:
- young people with degenerative conditions
- young people (for example with autism) whose needs have been largely met by their educational institution, but who once they leave, will require their needs to be met in some other way
- young people detained in the youth justice system who will move to the adult custodial estate
- young carers whose parents have needs below the local authority’s eligibility threshold but may nevertheless require advice or support to fulfil their potential, for example a child with deaf parents who is undertaking communication support
- young people and young carers receiving Children and Adolescent Mental Health Services (CAMHS) may also require care and support as adults even if they did not receive children’s services from the local authority
16.19 Even if they are not eligible for services, a transition assessment with good information and advice about support in the community can be particularly helpful for these groups as they are less likely to be aware of support available in the community.
16.20 Often when young people who have not been in contact with children’s services present to the local authority as a young adult, they do so with a high level of need for care and support. Local authorities should consider how to establish mechanisms in partnership with local educational institutions, health services and other agencies to identify these groups as early as possible in order to plan and prevent the development of care and support needs. (see chapter 15 on cooperation and integration and SEND Code Of Practice chapter 4 on joint commissioning, making effective relationships.
Adult carers and young carers
16.21 Preparation for adulthood will involve not only assessing how the needs of young people change as they approach adulthood but also how carers’, young carers’ and other family members’ needs might change. Local authorities must assess the needs of an adult carer where there is a likely need for support after the child turns 18 and it is of significant benefit to the carer to do so. For instance, some carers of disabled children are able to remain in employment with minimal support while the child has been in school. However, once the young person leaves education, it may be the case that the carer’s needs for support increase, and additional support and planning is required from the local authority to allow the carer to stay in employment.
16.22 The SEND Code of Practice sets out the importance of full-time programmes for young people aged 16 and over. For instance, some sixth forms or colleges offer 5 day placements which allow parents to remain in employment full time. However, for young people who do not have this opportunity, for example if their college offers only 3 day placements, transition assessments should consider if there is other provision and support for the young person such as volunteering, community participation or training which not only allows the carer to remain in full time employment, but also fulfils the young person’s wishes or equips them to live more independently as an adult (see chapter 4 on market shaping and SEND Code of Practice chapter 8 on preparation for adulthood).
16.23 Local authorities must also assess the needs of young carers as they approach adulthood. For instance, many young carers feel that they cannot go to university or enter employment because of their caring responsibilities. Transition assessments and planning must consider how to support young carers to prepare for adulthood and how to raise and fulfil their aspirations.
16.24 Local authorities must consider the impact on other members of the family (or other people the authority may feel appropriate) of the person receiving care and support. This will require the authority to identify anyone who may be part of the person’s wider network of care and support. For example, caring responsibilities could have an impact on siblings’ school work, or their aspirations to go to university. Young carers’ assessments should include an indication of how any care and support plan for the person(s) they care for would change as a result of the young carer’s change in circumstances. For example, if a young carer has an opportunity to go to university away from home, the local authority should indicate how it would meet the eligible needs of any family members that were previously being met by the young carer.
Features of a transition assessment
16.25 The transition assessment should support the young person and their family to plan for the future, by providing them with information about what they can expect. All transition assessments must include an assessment of:
- current needs for care and support and how these impact on wellbeing
- whether the child or carer is likely to have needs for care and support after the child in question becomes 18
- if so, what those needs are likely to be, and which are likely to be eligible needs
- the outcomes the young person or carer wishes to achieve in day-to-day life and how care and support (and other matters) can contribute to achieving them
16.26 Transition assessments for young carers or adult carers must also specifically consider whether the carer:
- is able to care now and after the child in question turns 18
- is willing to care now and will continue to after 18
- works or wishes to do so
- is or wishes to participate in education, training or recreation
16.27 The same requirements and principles apply for carrying out transition assessments as for other needs assessments under the adult statute (chapter 6 sets out the requirements and principles for carrying out needs assessments under the adult statute).
16.28 For example, assessments must include an assessment of the outcomes, views and wishes that matter to the child or carer in question, and an assessment of their strengths and capabilities. The power to join up assessments also applies, so for example if an adult is caring for a 17 year-old in transition and a 12 year-old, the local authority could combine:
- the child’s needs assessment of the 17 year old under the Care Act
- any assessment of the 17 year old’s needs under section 17 of the Children Act
- any assessment of the 12 year old’s needs under section 17 of the Children Act
- the child’s carer’s assessment of the adult under the Care Act
- the parent carer assessment of the adult under the Children and Families Act
16.29 The young person or carer in question must be involved in the assessment for it to be person centred and reflect their views and wishes. The assessment must also involve anyone else who the young person or carer wants to involve in the assessment. For example, many young people will want their parents involved in their process.
16.30 Transition assessments will often represent a very different context to that which the person is accustomed, so ensuring that people have general information and advice about adult care and support will sometimes be a prerequisite for giving more detailed information and advice. For example, the right to self-assessment applies as with other assessments under the Care Act (see chapter 6), however there is the important caveat that for children, the local authority must ensure that a self-assessment is appropriate. This means for example ensuring that a young carer conducting a self-assessment is clear about the support available both to them and the person(s) they care for, avoiding a situation where the young carer assumes the default of continuing in the same caring role through ignorance of other options.
16.31 When sharing information with a young carer about the person they care for a supported self-assessment during transition, local authorities must satisfy themselves that it is appropriate for the young carer to have the information. They must have regard to all circumstances in taking this decision, especially the age of the young carer, however each case will be different and there is no one age at which a young carer is necessarily old enough to receive information. Local authorities must ensure that the adult consents to have their information shared in this way.
16.32 Transition assessments should be carried out in a reasonable timescale. Local authorities should inform the young person or carer of an indicative timescale over which the assessment will be conducted and keep them informed.
16.33 While like all assessments transition assessments must identify all a person’s needs for care and support, they should be proportionate to that person’s needs. For someone with a low level of need, an assessment might be light-touch, but in many cases, more thorough examination will be required to establish a person’s needs fully.
16.34 Transition assessments should consider the immediate short-term outcomes that a child or carer wants to achieve as well as the medium and longer-term aspirations for their life. Progress towards achieving outcomes should be monitored.
16.35 EHC plans must be person-centred, and must focus on preparation for adulthood from Year 9. Therefore, for young people with EHC plans, transition assessments should build on the plans which will already contain information about the person, their aspirations and progress towards achieving their desired outcomes.
16.36 Similarly, for young people and carers who do not have an EHC plan, but who already have other plans under children’s legislation, the transition assessment should build on existing information.
16.37 In all cases, the young person or carer in question must agree to the assessment where they have mental capacity and are competent to agree. Where a young person or carer lacks mental capacity or is not competent to agree, the local authority must be satisfied that an assessment is in their best interests. Everyone has the right to refuse a transition assessment, however the local authority must undertake an assessment regardless if it suspects that a child is experiencing or at risk of abuse or neglect.
16.38 The right of young people to make decisions is subject to their capacity to do so as set out in the Mental Capacity Act 2005. The underlying principle of the Act is to ensure that those who lack capacity are supported to make as many decisions for themselves as possible, and that any decision made or action taken on their behalf, is done so in their best interests. This is a necessity if the transition assessment is to be person-centred.
16.39 For young people below the age of 16, local authorities will need to establish a young person’s competence using the test of ‘Gillick competence’ (whether they are able to understand a proposed treatment or procedure). Where the young person is not competent, a person with parental responsibility will need to be involved in their transition assessment, – or an independent advocate provided if there is no one appropriate to act on their behalf (either with or without parental responsibility).
16.40 The Care Act places a duty on local authorities to provide an independent advocate to facilitate the involvement in the transition assessment where the person in question would experience substantial difficulty in understanding the necessary information or in communicating their views, wishes and feelings – and if there is nobody else appropriate to act on their behalf (see chapter 7 for more detail on the provision independent advocacy). This duty applies for all young people or carers who meet the criteria, regardless of whether they lack mental capacity as defined under the Mental Capacity Act.
Co-operation between professionals and organisations
16.41 People with complex needs for care and support may have several professionals involved in their lives, and numerous assessments from multiple organisations. For children with special educational needs, the Children and Families Act 2014 brings these assessments together into a coordinated Education, Health and Care (EHC) Plan (see SEND Code of Practice, Chapter 9).
16.42 Local authorities must cooperate with relevant partners, and this duty is reciprocal (see chapter 15 on cooperation). This includes an explicit requirement which states that children and adult services must cooperate for the purposes of transition to adult care and support. Often, staff working in children’s services will have built relationships and knowledge about the young person or carer in question over a number of years. As young people and carers prepare for adulthood, children’s services and adults’ services should work together to pass on this knowledge and build new relationships in advance of transition.
16.43 Local authorities should have a clear understanding of their responsibilities, including funding arrangements, for young people and carers who are moving from children’s to adult services. Disputes between different departments within a local authority about who is responsible can be time consuming and can sometimes result in disruption to the young person or carer.
16.44 Local authorities must also co-operate with relevant external agencies including local GP practices, housing providers and educational institutions. Again, this duty is reciprocal. This co-operation is crucial to help ensure that assessments and planning are person-centred. Furthermore, local health services or schools are vital to identifying young people and carers who may not already be in contact with local authorities.
16.45 It can be frustrating for children and families who have to attend multiple appointments for assessments, and who have to give out the same information repeatedly. The SEND Code of Practice highlights the importance of the ‘tell us once’ approach to gathering information for assessments and this will be important in other contexts as well. Local authorities should consult with the young person and their family to discuss what arrangements they would prefer for assessments and reviews.
16.46 The local authority should ensure that all relevant partners are involved in transition planning where they are involved in the person’s care and support. Equally, the local authority should be involved in transition planning led by another organisation, for example a child and adolescent mental health service, where there are also likely to be needs for adult care and support.
16.47 Agencies should agree how to organise processes so that all the relevant professionals are able to contribute. For example, this might involve arranging a multi-disciplinary team meeting with the young person or carer. However, it may not always be possible for all the professionals from different agencies to be present at appointments, but where this is the case, they should still be able to contribute. Transition assessments must be person-centred, which means that contributions by different agencies should reflect the views of the person to whom the assessment relates.
16.48 The local authority may also combine a transition assessment with any other assessment it is carrying out (see examples in para. 16.28), or it may carry out assessments jointly with, or on behalf of, another body. All such cases must meet the consent condition around mental capacity or the competence condition set out above (para. 16.37) to be carried out jointly. For example, transition assessments should be combined with existing EHC assessments unless there are specific circumstances to prevent it.
16.49 Many people value having one designated person who coordinates assessments and transition planning across different agencies, and helps them to navigate through numerous systems and processes that can sometimes be complicated. Often there is a natural lead professional involved in a young person’s care who fulfils this role and local authorities should consider formalising this by designating a named person to co-ordinate transition assessment and planning across different agencies. Local authorities may also wish to consider specialist posts in their workforce to carry out this co-ordination function for people who are preparing for adulthood and interacting with multiple agencies.
16.50 This co-ordinating role, sometimes referred to as a ‘key working’ or ‘care coordination’, can not only help to deliver person-centred, integrated care, but can also help to reduce bureaucracy and duplication for local authorities, the NHS and other agencies. Care coordinators are also often able to build close relationships with young people and families and can act as a valuable provider of information and advice both to the families and to local authorities. Care leavers will have Personal Advisers to provide support, for example by providing advice or signposting the young person to services. The Personal Adviser will be a natural lead in many cases to coordinate a transition from children’s to adult care and support where relevant.
Case study: Person-centred transition planning, involving multiple agencies - Matthew’s story:
To ensure that Matthew was fully involved in the transition process, 4 planning sessions were held with his Transition Officer and facilitated by an outside agency that had expertise in person-centred planning. Matthew’s aspirations were to live independently in his own home and to have paid employment in an office.
It was vital to Matthew’s preparation for adulthood that he was given information about what support he would be eligible for after 18 in order to plan for sustainable employment and to ensure the appropriate support would be available to enable Matthew to live independently. This involved considering:
- whether he would still have a Personal Budget
- support with travel training
- job coaching
- support to live independently, developing appropriate housing options locally
Matthew and his family worked with the local authority and the housing association to identify a suitable home for him. The housing association then bought the house for Matthew and another young man to live in, with a carer. This whole process took over 3 years. Early, person-centred planning has been crucial to Matthew achieving his goals. Without adequate transition planning, the local authority would not have been able to promote Matthew’s wellbeing in terms of participation in work, suitability of accommodation, or control over day-to-day life.
Watch Matthew’s Story: a short film
On completion of the transition assessment – providing information and advice
16.51 Having carried out a transition assessment, the local authority must give an indication of which needs are likely to be eligible needs (and which are not likely to be eligible) once the young person in question turns 18, to ensure that the young person or carer understands the care and support they are likely to receive and can plan accordingly.
16.52 There is a particularly important role for local authorities in ensuring that young people and carers understand their likely situation when they reach adulthood. The different systems for children’s and adult care and support mean that there will be circumstances in which needs that were being met by children’s services may not be eligible needs under the adult system. Adult care and support is also subject to means-testing and charging.
16.53 It is critical that families are able to understand what support they are likely to receive when the young person or carer is in the adult system, and that the transition period is planned and managed as far in advance as is practical and useful to the individual to ensure that there is not a sudden gap in meeting the young person’s or carer’s needs. Where the transition assessment identifies needs that are likely to be eligible, local authorities should consider providing an indicative personal budget, so that young people, carers and their families are able to plan their care and support before entering the adult system (see SEN code of practice for further information about right to a personal budget for people with EHC plans, and chapter 11 for personal budgets under the Care Act).
16.54 For any needs that are not eligible under the adult statute, local authorities must provide information and advice on how those needs can be met, and how they can be prevented from getting worse. Information and advice must be accessible and proportionate to whoever needs it and must consider individual circumstances. For example when providing information and advice to young people and young carers, it is often more effective if information is given face-to-face from a trusted source, such as the young person’s care coordinator.
16.55 The Children and Families Act 2014 requires local authorities to publish a local offer, which includes provision of information and advice for children’s social care in their local area, including specific requirements for young people who are preparing for adulthood (see chapter 4 of SEND Code of Practice). The Care Act places a similar duty on local authorities to provide information and advice about adult care and support (see chapter 3 on the provision of information and advice).
16.56 Given the similar requirements on both children and adult services to provide information and advice that is easily accessible, local authorities should consider jointly commissioning and delivering their information and advice services for both children’s and adult care and support as part of their requirement to work together to smooth the transition between children and adult services.
16.57 The local authority and relevant partners should consider building on a transition assessment to create a person-centred transition plan that sets out the information in the assessment, along with a plan for the transition to adult care and support, including key milestones for achieving the young person or carer’s desired outcomes. An advantage of a transition plan is that it is easier to update and refine without undertaking a new assessment – transition assessments and plans should be reviewed regularly to take account of changes both in circumstances and desired outcomes. The priorities of young people and young carers will often change a lot during their adolescent years, and plans should be updated frequently enough to reflect this. Local authorities should also accept reasonable requests from young people and their families to review transition plans (see Chapter 13 for further on reviews of care plans).
Links to example templates of transition plans:
16.58 In the case of an adult carer, if the local authority has identified needs through a transition assessment which could be met by adult services, it may meet these needs under the Care Act in advance of the child being cared for turning 18. In deciding whether to do this the local authority must have regard to what support the adult carer is receiving under children’s legislation. If the local authority decides to meet the adult carer’s needs through adult services, as for anyone else under the adult legislation, the adult carer must receive a support plan and a personal budget – as well as a financial assessment if they are subject to charges for the support they will receive. A local authority may not meet an adult carer’s needs for support under section the Care Act by providing care and support to the child cared for – this will always happen under children’s legislation.
Provision of age-appropriate local services and resources
16.59 The Care Act requires local authorities to arrange preventative services, and to ensure a diverse range of quality providers of care and support in their local area. There are similar requirements in relation to the Local Offer in the Children and Families Act (see chapter 4 on market shaping).
16.60 Promoting a local market that offers a choice of high quality services will include having regard to the needs of young people and young carers transferring from children’s services after turning 18. In order to prepare to live independently as adults, many young people leaving full-time education will require different types of care and support to that which is typically provided to children or older people. For young adults with care and support needs or young adult carers, this might include things such as advice on housing options, support to help them live in their own home or job training.
16.61 Given the clear similarities in the statutory requirements under both Acts, local authorities should consider jointly planning and commissioning these services where there is potential to make better use of resources. It can cause significant disruption to young people and their families if they would prefer to stay local but are forced to travel out of area due to lack of adequate local provision. This will also often result in high transport costs and high costs of out-of-area placements.
After the young person or carer turns 18
16.62 There is no obligation on local authorities to implement the move from children’s social care to adult care and support as soon as someone turns 18. Very few moves will take place on the day of someone’s 18th birthday. For the most part, the move to adult services begins at the end of a school term or another similar milestone, and in many cases should be a staged process over several months or years.
16.63 In advance of the move taking place, the local authority must decide whether to treat the transition assessment as a needs or carers assessment under the Care Act (for example, an assessment for the adult care and support system as set out in chapter 6). In making this decision the local authority must have regard to when the transition assessment was carried out and whether the person’s circumstances have changed.
16.64 If the local authority will meet the young person’s or carer’s needs under the Care Act after they have turned 18 (based either on the existing transition assessment or a new needs assessment if necessary), the local authority must undertake the care planning process as for other adults – including creating a care and support plan and producing a personal budget as set out in chapters 10 and 11. Local authorities should ensure that this happens early enough that a package of care and support is in place at the time of transition.
Combining EHC plans and care and support plans after the age of 18
16.65 Where young people aged 18 or over continue to have EHC plans under the Children and Families Act 2014, and they make the move to adult care and support, the care and support aspects of the EHC plan will be provided under the Care Act. The statutory care and support plan must form the basis of the ‘care’ element of the EHC plan (chapter 10 sets out the requirements and guidance for care and support plans).
16.66 Under the Children and Families Act, EHC plans must clearly set out the care and support which is reasonably required by the learning difficulties and disabilities that result in the young person having SEN. For people over 18 with a care and support plan, this will be those elements of their care and support which are directly related to their SEN. EHC plans may also include other care and support that is in the care and support plan, but the elements that are directly related to SEN should always be clearly marked out separately as they will be of particular relevance to the rest of the EHC plan.
Continuity of care after the age of 18
16.67 Young people and their carers have sometimes faced a gap in provision of care and support when they turn 18, and this can be distressing and disruptive to their lives. Local authorities must not allow a gap in care and support when young people and carers move from children’s to adult services.
16.68 If transition assessment and planning is carried out as it should be, there should not be any gap in provision of care and support. However, if adult care and support is not in place on a young person’s 18th birthday, and they or their carer have been receiving services under children’s legislation, the local authority must continue providing services until the relevant steps have been taken, so that there is no gap in provision. The ‘relevant steps’ are if the local authority:
- concludes that the person does not have needs for adult care and support
- concludes that the person does have such needs and begins to meet some or all of them (the local authority will not always meet all of a person’s needs – certain needs are sometimes met by carers or other organisations)
- concludes that the person does have such needs but decides they are not going to meet any of those needs (for instance, because their needs do not meet the eligibility criteria under the Care Act 2014)
16.69 In order to reach such a conclusion, the local authority must have conducted a transition assessment (that they will use as a needs or carers assessment under the adult statute). Where a transition assessment was not conducted and should have been (or where the young person’s circumstances have changed), the local authority must carry out an adult needs or carer’s assessment as described in chapter 6.
16.70 In the case of care leavers, the Staying Put guidance states that local authorities may choose to extend foster placements beyond the age of 18. All local authorities must have a Staying Put policy to ensure transition from care to independence and adulthood that is similar for care leavers to that which most young people experience, and is based on need and not on age alone.
16.71 For some people with complex SEN and care needs, local authorities and their partners may decide that children’s services are the best way to meet a person’s needs - even after they have turned 18. Both the Care Act 2014 and the Children and Families Act 2014 allow for this.
16.72 The Children and Families Act enables local authorities to continue children’s services beyond age 18 and up to 25 for young people with EHC plans if they need longer to complete or consolidate their education and training and achieve the outcomes set out in their plan. Under the Care Act 2014, if, having carried out a transition assessment, it is agreed that the best decision for the young person is to continue to receive children’s services, the local authority may choose to do so. Children and adults’ services must work together, and any decision to continue children’s services after the child turns 18 will require agreement between children and adult services.
16.73 Where a person over 18 is still receiving services under children’s legislation through their EHC plan and the EHC plan ceases, the transition assessment and planning process must be undertaken as set out elsewhere in this chapter. Where this has not happened at the point of transition, the requirement under the Care Act to continue children’s services (as set out above) applies.
16.74 Both the Children and Families Act 2014 and the Care Act 2014 also require young people and their parents to be fully involved making decisions about their care and support. This includes decisions about the most appropriate time to make the transition to adult services. The EHC plan or any transition plan should set out how this will happen, who is involved and what support will be provided to make sure the transition is as seamless as possible.
Safeguarding after the age 18
16.75 Where someone is over 18 but still receiving children’s services and a safeguarding issue is raised, the matter should be dealt with as a matter of course by the adult safeguarding team. Where appropriate, they should involve the local authority’s children’s safeguarding colleagues as well as any relevant partners (for example, police or NHS) or other persons relevant to the case. The same approach should apply for complaints or appeals, as well as where someone is moving to a different local authority area after receiving a transition assessment but before moving to adult care and support.
Ordinary residence and transition to Higher Education
16.76 Where a young person is intending to move to a higher or further education institution which is out of the area where they were receiving children’s services, they will usually remain ordinarily resident in the area where their parents live (or the local authority area which had responsibility for them as a child). However, this is not always the case and Chapter 19 and Annex H contain more detailed guidance about ordinary residence principles when young people move from children’s to adult services (see para. 19.16), and when they move away to university. This includes example case studies to help local authorities in making decisions about which area is responsible - it will be an important aspect of transition planning to confirm as early as possible where someone will be ordinarily resident as an adult.
16.77 Where a young person or carer wishes to attend a higher or further education institution, local authorities should help them identify a suitable institution as part of transition planning (if they have not done so already). Once an offer has been accepted, local authorities should ensure the relevant institution is made aware as soon as possible of the young person’s or carer’s needs and desired outcomes and discuss a plan for meeting them. As set out in the SEN code of practice, an EHC plan will cease if someone progresses to further or higher education, but a care and support plan is likely to be required thereafter.
16.78 Wherever possible, this should be a conversation involving the young person or carer, anyone else they wish to involve, the local authority, and the institution – as well as the local authority where the institution is located where appropriate. All higher and further education institutions have clear duties and responsibilities under the Equality Act 2010 with regard to ensuring that disabled students do not face discrimination or less favourable treatment whilst applying to, and studying in these institutions. They are likely to have a learning support team or similar that can lead transition discussions on their behalf. These conversations should also ensure young people and carers are aware of their rights to the Disabled Students Allowance and student loans.
16.79 The objective should be to ensure that there will be an appropriate package of care and support in place from the day the young person or carer starts at the institution. In many cases a young person or carer studying at university will have a dual location, for example coming home to stay with the parents during weekends or holidays. Where this is the case, local authorities must ensure their needs are met all year round.
Transition from children’s to adult NHS Continuing Healthcare
16.80 Clinical Commissioning Groups (CCGs) should use the national framework for NHS Continuing Healthcare and supporting guidance and tools (especially the Decision Support Tool) to determine what on-going care services people aged 18 years or over should receive. The framework sets out that CCGs should ensure that adult NHS Continuing Healthcare is appropriately represented at all transition planning meetings to do with individual young people whose needs suggest that there may be potential eligibility. CCGs and LAs should have systems in place to ensure that appropriate referrals are made whenever either organisation is supporting a young person who, on reaching adulthood, may have a need for services from the other agency.
16.81 The framework sets out best practice for the timing of transition steps as follows:
- children’s services should identify young people with likely needs for NHS CHC and notify the relevant CCGs when such a young person turns 14
- there should be a formal referral for adult NHS CHC screening at 16
- there should be a decision in principle at 17 so that a package of care can be in place once the person turns 18 (or later if agreed more appropriate)
16.82 Where a young person has been receiving children’s continuing health care from a relevant CCG, it is likely that they will continue to be eligible for a package of adult NHS CHC when they reach the age of 18. Where their needs have changed such that they are assessed as no longer requiring such a package, they should be advised of their non-eligibility and of their right to request an independent review and mediation (see 16.83 below). The CCG should continue to participate in the transition process, in order to ensure an appropriate transfer of responsibilities, including consideration of whether they should be commissioning, funding or providing services towards a joint package of care.
16.83 As set out above, where it will benefit a young person with an EHC plan, local authorities have the power to continue to provide children’s services past a young person’s 18th birthday for as long as is deemed necessary. Where there is a change in CHC provision, this needs to be recorded in the young person’s EHC plan, where they have one, and advised of their rights to ask the local authority for mediation (this is in the SEND Code of Practice and applicable up to age 25).
Links to external resources
- Code of Practice for Children with Special Educational Needs & Disability
- Preparing for Adulthood
- Together for Short Lives
- Transition Information Network
17. Prisons, approved premises and bail accommodation
This chapter provides guidance on section 76 of the Care Act 2014. It also provides guidance on other sections of the Act where they relate to care and support for adults in prison, approved premises and bail accommodation and those released from custody.
This chapter covers:
- information sharing
- assessments of need
- assessments of a carer’s needs
- charging and assessing financial resources
- next steps after assessments
- direct payments and deferred payment agreements
- continuity of care and support when an adult moves or is released
- partnerships and interdependencies
- end of life care
- safeguarding adults at risk of abuse or neglect
- transition from children’s to adult care and support
- independent advocacy support
- complaints
- standards and assessments
17.1 People in custody or custodial settings who have needs for care and support should be able to access the care they need, just like anyone else. In the past, the responsibilities for meeting the needs of prisoners have been unclear, and this has led to confusion between local authorities, prisons and other organisations. This has created difficulties in ensuring people’s eligible needs are met.
17.2 Prisoners can often have complex health and care needs and experience poorer health and mental health outcomes than the general population. Evidence demonstrates higher prevalence among the adult prison population of mental illness, substance misuse and learning disabilities than in the general population. Access to good integrated health and care support will be particularly important for these groups. Section 76 of the Care Act sets out to clarify local responsibilities, and to describe how the partners involved should work together.
17.3 Throughout this chapter, references to custody or custodial settings relate to prisons, approved premises and other bail accommodation. It can also apply to people aged over 18 years in young offender institutions, secure children’s homes and secure training centres. Please see the Definitions section below. People bailed to a particular address in criminal proceedings are, like those in prison or approved premises, treated for the purposes of the Care Act as ordinarily resident in the local authority where they are required to reside and the provisions in the Care Act apply accordingly.
17.4 The guidance in this chapter relates only to custodial settings in England.
17.5 The Act and this chapter apply to adults who are detained or residing in a custodial setting. For the purposes of the Act, adults detained or residing in a custodial setting are treated as if they were ordinarily resident in the area where the custodial setting is located.
17.6 Where prisoners have previously been detained under sections 47 and 48 of the Mental Health Act 1983 and transferred back to prison, their entitlement to section 117 aftercare should be dealt with in the same way as it would be in the community, apart from any provisions which are disapplied in custodial settings, such as direct payments and choice of accommodation, which are set out in more detail below. Section 117(3), as amended by the Care Act 2014, will apply in determining which local authority is responsible for commissioning or providing the section 117 after-care.
17.7 If the person was ordinarily resident in the area of a local authority immediately before being detained in hospital, that local authority will be responsible for the after-care while the person is in prison and upon their release from prison (see Chapter 19 for further detail on determination). However, if the person was not ordinarily resident in any area immediately before detention, the local authority responsible will be where the person is resident or where they have been discharged (for example, the local authority responsible for the prison to which the person has been discharged). The local authority will be jointly responsible for after-care with NHS England while the person is in prison.
17.8 This chapter of the guidance does not apply to individuals aged under 18 years. Details of where to find information on provision for children can be found at the end of this chapter. Please refer to paras. 17.70-17.71 of this chapter for information about transition from children’s to adult care and support in custodial settings. For further detail, please see chapter 16 of this guidance on transition from children’s to adult care and support.
17.9 All adults in custody, as well as offenders and defendants in the community, should expect the same level of care and support as the rest of the population. This principle of equivalence of care forms the basis of the policy intent for the Act and this guidance. This is crucial in ensuring that those in need of care and support achieve the outcomes that matter to them, and that will support them to live as independently as possible at the end of their detention. In addition to ensuring that individual needs are met, this will contribute to the effectiveness of rehabilitation and improve community safety.
17.10 Local authorities are responsible for the assessment of all adults who are in custody in their area and who appear to be in need of care and support, regardless of which area the individual came from or where they will be released to. If an individual is transferred to another custodial establishment in a different local authority area this responsibility will transfer to the new area. The prison or approved premises to which an individual is allocated is a matter for the Ministry of Justice.
17.11 Local authorities should also be aware that prisoners, especially those serving long sentences, may develop eligible needs over time whilst in prison. Local authorities should consider how best to provide information and advice to both individuals and establishments on what can be done to prevent or delay the development of care and support needs. In doing so it is important to consider the level of access to electronic media and the most appropriate format, such as easy-read leaflets, of information and advice in custodial settings, and the custodial environment in which the care and support is to be provided.
17.12 Not all local authority areas contain prisons or approved premises. Those that do will assume responsibility for the eligible needs of the people residing in these sites. However, all local authorities will be responsible for continuity of care for offenders with a package of care coming into their area on release from prison. Provision of care and support, where an adult has eligible needs, should be provided in line with chapter 6 of this guidance once these individuals move into the community. Early engagement in the resettlement plan of the local authority in the area to which the person is returning will reduce delays, particularly when resettlement is in a new area due to the nature of the original offence. Similarly local authorities must support continuity of care for any of their residents moving into custody. Either party may use the mechanism to require co-operation to support working in an individual case, set out in chapter 15.
17.13 Local authorities, provider organisations and their staff working in custodial settings should abide by all rules and practices for that establishment, including (but not restricted to) security policies such as restricted items and searches on entry, equality and safeguarding procedures.
Definitions
A) Prison
This has the same meaning as the Prison Act 1952, section 53(1). A reference to a prison includes a reference to a young offender institution, secure training centre or secure children’s home (see Care Act section 76(11)(a)). A reference to a governor, director or controller of a prison includes a reference to the governor, director or controller of a young offender institution, to the governor, director or monitor of a secure training centre and to the manager of a secure children’s home (see Care Act section 76(11)(b)). A reference to a prison officer or prisoner custody officer includes a reference to a prison officer or prisoner custody officer as a young offender institution, to an officer or custody officer at a secure training centre and to a member of staff at a secure children’s home (see Care Act section 76(11)(c)).
B) Approved Premises
Premises approved as accommodation under section 13 of the Offender Management Act 2007 for the supervision and rehabilitation of offenders, and for people on bail. They are usually supervised hostel-type accommodation.
C) National Offender Management Service (NOMS)
An executive agency of the Ministry of Justice, its role is to commission and provide offender services in the community and in custody in England and Wales, ensuring best value for money from public resources. NOMS works to protect the public and reduce reoffending by delivering the punishment and orders of the courts and supporting rehabilitation by helping offenders to change their lives.
D) National Probation Service (NPS) and Community Rehabilitation Companies (CRCs)
The Transforming Rehabilitation reforms are putting in place a new system of offender management and rehabilitation across England and Wales. The NPS is responsible for conducting all initial offender assessments for risk of harm, and allocating offenders to either the NPS or CRCs. It will manage all offenders who pose a high risk of serious harm to the public (including those whose risk level escalates during their period of supervision), offenders who have committed the most serious sexual and violent offences (including those managed under Multi Agency Public Protection Arrangements), foreign nationals who meet the criteria for deportation, and a small number of exceptional public interest cases. The 21 CRCs are responsible for managing the majority of offenders in the community (most low to medium risk offenders), The NPS sits within the National Offender Management Service, while the 21 CRCs will be run in the public sector until contracts with new providers are awarded.
E) HM Inspectorate of Prisons for England and Wales (HMI Prisons)
An independent inspectorate which reports on conditions for and treatment of those in prison, young offender institutions and immigration detention facilities.
F) HM Inspectorate of Probation for England and Wales
An independent inspectorate on the effectiveness of work with adults, children and young people who have offended aimed at reducing reoffending and protecting the public.
G) Prisons and Probation Ombudsman (PPO)
The PPO investigates complaints from prisoners, those on probation and those held in immigration removal centres. The Ombudsman also investigates all deaths that occur among prisoners, immigration detainees and the residents of approved premises.|
17.14 Local authorities should ensure the security of information held on people who are in custodial settings, and should develop agreements consistent with policies and procedures of Ministry of Justice and the National Offender Management Service and with relevant legislation which enable appropriate information sharing on individuals, including the sharing of information about risk to the prisoner and others where this is relevant.
17.15 If a local authority is providing care and support for a person in the community and that person is subsequently remanded or sentenced to custody, or bailed to an approved premises, or required to live in approved premises as part of a community sentence, the local authority should share details of the most recent assessment and care and support plan to the relevant custodial setting and the local authority in which it is based so that care and support may continue.
17.16 It is unlikely that local authorities will know when an individual is remanded or sentenced to custody in a new local authority area. Prisons and/or prison health services should inform local authorities when someone they believe has care and support needs arrives at their establishment. Either party may use the mechanism to require co-operation to support working in an individual case, set out in chapter 15. Local authorities may also receive requests for information from managers of custodial settings or probation services when an individual who has already received care and support in the community is remanded or sentenced to custody. Local authorities should take all reasonable steps to provide the information requested as soon as practicable after receiving the request.
Assessments of need
17.17 Where a local authority is made aware that an adult in a custodial setting may have care and support needs, they must carry out an assessment as they would for someone in the community. The standards and approach to assessment and determination of need set out in chapter 6 should apply to individuals within custodial settings, just as they would for people in the community, bearing in mind that an adult with care and support needs will no longer have the benefit of support they may have relied upon in the community. It is likely that there will be complexities for carrying out assessments in custodial settings and consideration should be given to how such assessments will be carried out in an efficient way for all involved (for example making appointments and consideration of the number and type of staff required to be involved).
17.18 The local authority may also combine a needs assessment with any other assessment it is carrying out, or it may carry out assessments jointly with, or on behalf of another body, for example prisoners’ health assessments.
17.19 Local authorities should consider processes for identifying people in custodial settings who are likely to have or to develop care and support needs. Reception screening and health assessments are key opportunities to establish whether an individual has been receiving care and support before entering custody. Existing processes such as interviews for court purposes conducted by the National Probation Service could be used to obtain information about current social care needs. This information follows the individual into the custodial setting and can be used to enable appropriate links to local authorities. This also applies to people with low level needs who are being supported in the community by local authority community services. Sharing this information will enable continuity of care in the custodial setting. Further guidance will be issued to prison and approved premises managers regarding sharing information with local authorities and partnership working.
17.20 Local authorities should aim to conduct assessments of those who appear to have care and support needs promptly following receipt of the referral from managers of custodial settings or the prison’s health providers. People in a custodial setting have a right to self-refer for an assessment (as described in chapter 6 of this guidance) and local authorities should work with the managers of the custodial setting to consider how to facilitate and respond to self-referrals. The local authority should provide appropriate types of care and support prior to completion of the assessment where it is clear the person has urgent needs (as per section 19 (3) of the Care Act).
17.21 If someone in a custodial setting refuses a needs assessment the local authority is not required to carry out the assessment, subject to the same conditions as in the community. That is, this does not apply if:
- the person lacks the capacity to refuse and the local authority believes that the assessment will be in their best interests; or
- the person is experiencing, or is at risk of, abuse or neglect (see chapter 6 on assessment).
17.22 Once a local authority has assessed an individual in custody as needing care and support they must then determine if some or all of these needs meet the eligibility criteria. Where an individual does not meet the eligibility criteria, the local authority must then give him or her written information about:
- what can be done to meet or reduce needs and what services are available; and
- what can be done to prevent or delay the development of needs for care and support in the future.
17.23 The threshold for the provision of care and support does not change in custodial settings and will be the same as described in chapter 6. When an individual is in a custodial setting, this should not in any way affect the assessment and recording of eligible needs. Whilst the setting in which the care and support will be provided is likely to be different from community or other settings, and this should be taken into account when considering how to meet the need for care and support as part of the care planning process, the extent and nature of need should be identified before taking into account the environment in which the individual lives. This is particularly important when individuals move between prisons and/or from prison into the community. Services which support the best outcomes which can be achieved should be provided where the built environment necessarily limits the type or quality of care and support which can be provided. If a safeguarding issue is identified then the prison or approved premises management needs to be notified in accordance with NOMS policy on adult safeguarding.
17.24 For any needs that are not eligible under the Act, local authorities must provide information and advice to the individual on how those needs can be met, and how they can be prevented from getting worse (as per Section 13 (5) of the Care Act). It is good practice to copy this information to managers of custodial settings, with the person’s consent as this may be relevant to how the individual is managed in the custodial setting.
17.25 Prisoners, especially those serving long sentences, may develop eligible needs over time. Local authorities should consider how best to provide information and advice to both individuals and establishments on what can be done to prevent or delay the development of care and support needs. In doing so it is important to consider the prison regime and the environment, as well as the individual’s capacity to understand the information that is being provided. Individuals in custodial settings, like people in the community, may benefit from low level preventative support and information and advice that will help them maintain their own health and wellbeing.
17.26 The right to a choice of accommodation does not apply to those in a custodial setting except when an individual is preparing for release or resettlement in the community. Release into an approved premises amounts to moving from one custodial setting to another.
17.27 It is important that, where appropriate, individuals in custodial settings, maintain links with their families, subject to consideration of the best interests of the individual and to public protection requirements which may limit family contact. While it may not always be possible or appropriate to involve family members directly in assessment or care planning, individuals should be asked whether they would like to involve others in their assessment or care planning.
17.28 If it is not possible to involve families directly, the local authority should ask the individual concerned whether they would like others to be informed that an assessment is taking place, the outcome of that assessment and whether they should see the care and support plan.
Assessments of a carer’s needs
17.29 It is not the intention of the Care Act that any prisoner, resident of approved premises or staff in prisons or approved premises should take on the role of carer as defined by the Act and should therefore not in general be entitled to a carer’s assessment. Separate guidance will be issued to prison and approved premises staff on the role of prisoners and residents of approved premises in providing assistance to others.
Charging and assessing financial resources
17.30 Those in custodial settings will be subject to a financial assessment to determine how much they may pay towards the cost of their care and support, as they would be in the community (see chapter 8). Consideration should be given to the best way of handling financial assessments, taking into account the resources required. In particular local authorities should consider how ‘light touch’ assessments could be carried out where a person is unlikely to be required to contribute towards the cost of their care and support. As indicated previously, a high proportion of the prison population have a mental health problem or learning disability and they may have a poor understanding of their personal finances. Therefore forms and questions must be accessible and support provided to enable the individual to complete the financial assessment. Should the person not meet the eligibility threshold for local authority support, but they wish to purchase care services, this request should be referred for decision to NOMS.
Next steps after assessment
17.31 The local authority should ensure that all relevant partners are involved in care and support planning and take part in joint planning with health partners.
17.32 Where a local authority is required to meet needs it must prepare a care and support plan for the person concerned and involve the individual to decide how to have their needs met. The local authority should also speak to others concerned with the person’s health and wellbeing, including prison staff, probation Offender Managers, staff of approved premises and health care staff, to ensure integration of care, and fit with the custodial regime as appropriate, including enabling access to regime services such as libraries and education. Any safeguarding issues are to be addressed in the care and support plan.
17.33 Whilst every effort should be made to put people in control of their care and for them to be actively involved and influential throughout the planning process (see chapter 10 on care and support planning), this should be discussed with the individual and recorded as part of the care planning process. However, the plan must contain the elements defined in the Act, including the allocated personal budget. This will ensure that the person is clear about the needs to be met, the cost attributed to meeting those needs and how, if applicable, the custodial regime limited the individual’s choice and control.
17.34 Local authorities should aim to ensure that consent is given so that individual care plans are shared with other providers of custodial and resettlement services including custodial services, probation service providers including Community Rehabilitation Companies, prison healthcare providers and managers of approved premises. For residents of approved premises, the local authority should always liaise with the responsible Offender Manager in probation services.
17.35 For those assessed as being in need of equipment or adaptations to their living accommodation to meet their needs, local authorities should make it clear to individuals that the custodial regime may limit the range of care options available and some, such as direct payments, do not apply in a custodial setting. Where an individual’s ability to exercise choice and control is limited by the custodial regime, authorities should discuss with their partners in prisons, approved premises and health care services where responsibility lies. Where this relates to fixtures and fittings (for example, a grab rail or a ramp), it will usually be for the prison to deliver this. But for specialised and moveable items such as beds and hoists, then it may be the local authority that is responsible. Aids for individuals, as defined in the Care and Support (Preventing Needs for Care and Support) Regulations 2014, are the responsibility of the local authority, whilst more significant adaptations would the responsibility of the custodial establishment. Further guidance on responsibility of custodial services for equipment aids and adaptations will be issued by NOMS. Custody services, healthcare providers and local authorities should agree local responsibilities.
17.36 Local authorities may commission or arrange for others to provide care and support services, or delegate the function to another party (see chapter 18 on delegation). Local authorities should consider how this fits alongside the commissioning of health and substance misuse services in prison directly commissioned by NHS England and the commissioning of education services by the Skills Funding Agency. If such an arrangement is implemented, local authorities should consider retaining the functions relating to requirements for continuity of care between settings and must retain the functions in relation to charging and safeguarding. Local authorities should make sure that any other party commissioned to provide care and support is aware of the policies and procedures to be followed when working in a custodial environment.
17.37 Care and support plans for those in custodial settings will be subject to the same review processes as all other plans (see chapter 13). Local authorities should also review an individual’s care and support plan each time they enter custody from the community, or are released from custody.
17.38 People in custody may experience episodes of hospital care, for example following an incident such as a stroke. Local authorities should co-operate with hospital staff and prison health service providers and commissioners to prevent delays in discharge from hospital and support a timely return to custody.
Direct payments
17.39 Any references to direct payments in the Act or this guidance will not apply in prisons and approved premises. Direct payments may not be made to people in custodial settings.
17.40 17Individuals in bail accommodation and approved premises who have not yet been convicted are entitled to direct payments, as they would have been whilst in their own homes. For more information, see chapter 12 on direct payments.
Continuity of care and support when an adult moves
17.41 Individuals in custody with care and support needs must have continuity of care where they are moved to another custodial setting or where they are being released from prison and are moving back in to the community. To ensure that the individual continues to receive care during the move, local authorities should follow a similar process to that set out in chapter 20 on continuity of care.
17.42 Individuals in custody cannot be said to be ordinarily resident there because the concept of ordinary residence relies on the person voluntarily living there and those in custody have not chosen to live there. As such, they might remain ordinarily resident where they previously resided. It is the local authority where the custodial setting is situated which is responsible for assessments, services under Part 1 of the Care Act in relation to an individual in custody. Where the adult is being released from prison, their ordinary residence will generally be in the authority where they intend to live on a permanent basis, but see also paragraphs 17.55-17.58.
17.43 There will be circumstances where the process to ensure continuity of care will need to differ, for example when a prisoner is moved between establishments or when they are released in another area because of the nature of their offence. The prison or approved premises to which an individual is allocated is a matter for the Ministry of Justice, and individuals may be moved between different custodial settings. In such cases, the Governor of the prison or a representative, should inform the local authority in which the prison is located (the first authority) that the adult is to be moved or is being released to a new area as soon as practicable. If this is a move to a custodial setting or release into the community in the same authority, then the first authority will remain responsible for meeting the individual’s care and support needs. Where the new custodial setting or the community, if being released, is in a different local authority area (second authority), the first authority must inform the second authority of the move once it has been told by the prison.
17.44 The prison, both local authorities and where practicable, the individual, should work together to ensure that the adult’s care is continued during the move. It is good practice for the first and second local authority (and the transferring and receiving prisons where appropriate) to have a named member of staff to lead on arrangements for individuals during the transfer. Both local authorities must share the relevant information as set out in chapter 20 on continuity of care, including their care and support plan.
17.45 The second authority should assess the individual before they are moved, but this may not always be possible as the authority could be informed of the transfer at short notice. In such circumstances the second authority must continue to meet the care and support needs that the first authority was meeting. It must continue to meet these needs until it has carried out its own assessment.
17.46 The requirements outlined in this guidance only apply to custodial settings in England. (Guidance to cover prisoners who are moved to Scotland, Wales or Northern Ireland is still to be developed.)
17.47 Under the Transforming Rehabilitation Programme, all prisons in England and Wales will be designated as either resettlement or non-resettlement prisons. Due to the nature of resettlement prisons, it is likely that they will experience a high turnover of prisoners and it is particularly important that the care needs of those serving short term sentences are identified and responded to.
People leaving prison: ordinary residence
17.48 The deeming provisions in section 39 of the Care Act, which provide that in most circumstances a person’s ordinary residence is retained where they have their needs met in certain types of accommodation in another local authority area, do not apply to people who are leaving prison. However, local authorities can reasonably follow the approach set out in section 39 for people who are due for release from prison. Therefore, where a person requires a specified type of accommodation (see chapter 19 on ordinary residence) to be arranged to meet their eligible needs on release from prison, local authorities should start from a presumption that they remain ordinarily resident in the area in which they were ordinarily resident before the start of their sentence.
17.49 However, determining an offender’s ordinary residence on release from prison will not always be straightforward and each case must be considered on an individual basis. For example, it may not be possible for an offender to return to their prior local authority area due to the history of their case and any risks associated with a return to that area.
17.50 In situations where an offender is likely to have needs for care and support services on release from prison or approved premises and their place of ordinary residence is unclear and/or they express an intention to settle in a new local authority area, the local authority to which they plan to move should take responsibility for carrying out the needs assessment.
17.51 Given the difficulties associated with determining some offenders’ ordinary residence on release, prisons or approved premises, the probation provider (NPS or CRC) and the local authority providing care and support should initiate joint planning for release in advance. Early involvement of all agencies, particularly providers of probation services, should ensure that the resettlement plan is sustainable in the local authority area where the individual will reside. Prisons and probation services should support assessment and care and support planning for those offenders who will require care and support services on their release from prison.
Partnerships and interdependencies
17.52 It is essential that local arrangements for the delivery of care and support are made in partnership with health and education commissioners and providers within a custodial environment, as well as the NPS and CRCs so that those with eligible needs experience integrated services. This should take account of the need for close working with prison staff and regime service (see chapter 15 on integration and cooperation).
17.53 Consideration should be given to the duty to promote integration contained in section 3 of the Act. This includes health and health related services provided by prisons and providers of probation services. In support of this, local authorities should consider the value of regular inter-agency meetings with all those involved in the person’s care and support.
17.54 Local authorities should ensure that contracts with providers of care and support cover staff supervision and that staff are supported to deliver high quality services in custodial settings. As part of their responsibilities for shaping and facilitating the market in care and support services, local authorities should work with prisons and approved premises to develop and test contingency plans to cover the event of provider failure. These plans should be aligned with wider prison and local authority business continuity and contingency planning (see Chapter 4 on market shaping and commissioning and Chapter 5 provider failure).
End of life care
17.55 The provision of care and support for those in custodial settings extends to those who reach the end of life whilst in prison. For this provision of palliative care, some will transfer to a local hospital, hospice or care home or move to an alternative prison where a more suitable environment is available. In these cases, responsibility for care and support will pass to the NHS or new local authority, once the individual arrives at the new location. Approved Premises are not in general a suitable location for the provision of end of life care.
17.56 Prison managers and health care providers should consider informing local authorities when a prisoner receives a terminal diagnosis or when the condition of such a patient deteriorates significantly. Information could be shared with local authorities for the purpose of offender management under s.14 of the Offender Management Act 2007. The individual’s consent should be obtained where possible.
17.57 Where it is not possible to obtain consent to share the information, managers of custodial settings and health care providers should make an individual assessment of the nature of the information and the requirements of the Data Protection Act 1998.
17.58 Local authorities should work with the prison healthcare provider to ensure that the care and support needs of the prisoner are met throughout the provision of end of life care.
NHS Continuing Healthcare
17.59 NHS Continuing Healthcare is a package of ongoing care that is arranged and funded solely by the health service for individuals outside a hospital setting who have ongoing healthcare needs of a type and quantity that they have been found to have a ‘primary health need’. Such care is provided to people aged 18 or over, to meet needs that have arisen as a result of disability, accident or illness. NHS Continuing Healthcare is not dependent on a person’s condition or diagnosis, but is based on their specific care needs.
17.60 Section 22 of the Care Act sets out the limits on what a local authority may provide by way of healthcare and so, in effect, sets the boundary between the responsibilities of local authorities for the provision of care and support, and those of the NHS for the provision of health care. In order to support joint working, it is important that all partners involved are clear about their own responsibilities, and how this sits together (see chapter 15 for more detail). NHS England is responsible for commissioning healthcare for prisoners, where necessary this includes NHS Continuing Healthcare.
Safeguarding adults at risk of abuse or neglect
17.61 Local authority and care provider staff must understand what to do where they have a concern about abuse and neglect of an adult in custody. The prison must ensure that it has clear safeguarding policies and procedures that are explained to all visiting staff. Prison and probation staff may approach the local authority for advice and assistance in individual cases although the local authority will not have the legal duty to lead enquiries in any custodial setting.
17.62 Local authorities should consider inviting prison and probation staff to be members of Safeguarding Adult Boards. The inclusion of prison and probation staff on safeguarding adult boards should be agreed with all statutory board members. The Safeguarding Adult Board can act as a forum for members to exchange advice and expertise to assist prison and probation staff in ensuring that all people in custodial settings are safeguarded. PSI 16/2015 Adult Safeguarding in Prisons contains guidance for prison governors on engaging with local Adult Safeguarding Boards .
Transition from children’s to adult care and support
17.63 Local authorities should be aware of children and young people in Young Offender Institutions, Secure Children’s Homes, Secure Training Centres or other places of detention as well as children and young people in the youth justice system, who are likely to have eligible needs for care and support as adults, and are approaching their eighteenth birthday. Local authorities should ensure that appropriate arrangements are in place to identify these young people and ensure they receive a transition assessment when appropriate. See chapter 16.
17.64 This also applies where an offender moves from the youth custodial estate to the adult custodial estate, which may include a change in the responsible local authority. A request for an assessment can be made on the young person’s behalf by the professional responsible for their care in the Young Offenders’ Institution, Secure Children’s Home or Secure Training Centre. Good communication between professionals, institutions and local authorities is essential to prepare for transfer and ensure a smooth transition.
Care leavers
17.65 If a young person is entitled to support and services as a care leaver, this status remains unchanged while in custody and the local authority that looked after the young person retains responsibility for providing leaving care services during his/her time in custody and on release.
17.66 Responsibilities for planning continuing support applies to all care leavers until they reach the age of 21 or, if they are being helped with education or training, to the end of the agreed programme of education or training (which can take them beyond their 25th birthday).
17.67 Good communication is essential between the local authority responsible for leaving care services and the local authority responsible for providing care and support in custody.
Independent advocacy support
17.68 Adults in custody are entitled to the support of an independent advocate during needs assessments and care and support planning and reviews of plans if they would have significant difficulty in being involved in the process. It is the local authority’s duty to arrange an independent advocate, as they would for an individual in the community. See chapter 7 of this guidance for further details.
17.69 Local authorities should agree with managers of custodial establishments how the advocacy scheme will work in their establishments. Local arrangements for peers or prison officers to provide advocacy support or signpost people in custody have a role. However, this does not fulfil the requirement under the Act for independent advocacy support.
Complaints and appeals
17.70 Local authorities should provide information to those in custodial settings on how to make complaints, and seek redress about provision of care and support services.
17.71 Managers of custodial settings should inform local authorities where an offender wishes to make a complaint as soon as they are made aware. A prisoner may choose to complain or appeal by alternative methods, such as by letter or telephone to the care and support provider. This correspondence should be processed in the same way as all other appeals and complaints once received by local authorities.
17.72 Current complaints provision for care and support is set out in regulations. . The provisions of the regulations mean that anyone who is dissatisfied with a decision made by the local authority would be able to make a complaint about that decision and have that complaint handled by the local authority. The local authority must make its own arrangements for dealing with complaints in accordance with the 2009 regulations.
17.73 Section 72 of the Care Act 2014, which relates to an appeals system for reviewing care and support decisions made by local authorities, has not yet come into effect. While the government does not intend to introduce such a system imminently, we are keeping it under review.
Standards and assessments
17.74 The Prisons and Probation Ombudsman (PPO) conducts investigations in prisons following complaints about prison services, as well as deaths in custody or other significant events. The PPO will commission a relevant body to assist their investigations where it is felt that an aspect of care and support provision has contributed to the event. Local authorities should co-operate with any investigations as required.
17.75 The party commissioned by the PPO will investigate any relevant aspect of care and support provision and report back to the PPO for inclusion in the final report.
17.76 Both prisons and probation services are inspected by HM Inspectorate of Prisons and HM Inspectorate of Probation. Local authorities should make any relevant assessments and other documents available to inspecting bodies as part of the investigation.
17.77 Local authorities will receive copies of all investigation reports that are relevant to them. It is good practice for local authorities to contribute to the responses and action plans in conjunction with NOMS managers, prison managers and health care providers and commissioners. This could include work to prevent and reduce reoffending, and to prevent harm to others or to the offender.
17.78 Local authorities should co-operate with and attend any inquests that are held following a death in custody, where they are requested to do so or they have relevant information.
Links to other sources of information/products which support implementation
18. Delegation of local authority functions
This chapter provides guidance on section 79 of the Care Act 2014.
This chapter covers:
- overview of the policy
- local authorities retain ultimate responsibility for how its functions are carried out
- importance of contracts
- which functions may not be delegated
- the difference between outsourcing a legal function and activities relating to the function
- conflicts of interest
18.1 Part 1 of the Care Act sets out local authorities’ functions and responsibilities for care and support. Sometimes external organisations might be better placed than the local authority itself to carry out some of its care and support functions. For instance, an outside organisation might specialise in carrying out assessments or care and support planning for certain disability groups, where the local authority does not have the in-house expertise. External organisations might also be able to provide additional capacity to carry out care and support functions.
18.2 The Care Act allows local authorities to delegate some, but not all, of their care and support functions to other parties. This power to delegate is intended to allow flexibility for local approaches to be developed in delivering care and support, and to allow local authorities to work more efficiently and innovatively, and provide better quality care and support to local populations.
18.3 As with all care and support, individual wellbeing should be central to any decision to delegate a function. Local authorities should not delegate its functions simply to gain efficiency where this is to the detriment of the wellbeing of people using care and support.
18.4 Local Authorities retain ultimate responsibility for how its functions are carried out. Delegation does not absolve the local authority of its legal responsibilities. When a local authority delegates any of its functions, it retains ultimate responsibility for how the function is carried out. The Care Act is clear that anything done (or not done) by the third party in carrying out the function, is to be treated as if it has been done (or not done) by the local authority itself. This is a core principle of allowing delegation of care and support functions.
18.5 The power to delegate functions in the Care Act does not supersede the pre-existing ability for NHS and local authorities to enter into prescribed partnership arrangements under Section 75 NHS Act 2006. This means that local authorities can enter into partnership arrangements with the NHS for the NHS to carry out a local authority’s ‘health-related functions’ (as set out in the NHS Bodies and Local Authorities Partnership Arrangements Regulations 2000.
This includes authorisation for NHS bodies to exercise those health-related functions, including safeguarding functions, that local authorities are prohibited from delegating under the Care Act. In fact all care and support functions under the Care Act (for example, under Part 1) can be included in such partnership arrangements except for certain functions. Charging and carrying out financial assessments can only be the subject of partnership arrangements where there are also partnership arrangements in place to meet needs under section 18 of 19 of the Care Act.
Similarly, charging for prevention functions (section 2 of the Care Act) can only be the subject of partnership arrangements if there are also partnership arrangements in respect of those functions. Functions under section 78 (guidance) and 69 (debt recovery) cannot be the subject of partnership arrangements at all. The local authority would still remain legally responsible for its functions when they are carried out via partnership arrangements, as with delegated functions.
18.6 People using care and support will always have a means of redress against the local authority for how any of its functions under Part 1 of the Act are carried out. For example, a local authority might delegate needs assessments to another organisation, which has its own procedures for handling complaints. If the adult to whom the assessment relates has a complaint about the way in which it was carried out, the adult might choose to take it up with the organisation in question. However, if this does not satisfy the adult, or if the adult simply chooses to complain directly to the local authority, the local authority will remain responsible for addressing the complaint.
18.7 In delegating care and support functions, local authorities should have regard to the local authority version of the NHS information governance toolkit, in particular ensuring that all formal contractual arrangements include compliance with information governance requirements (requirement 12-146).
Importance of contracts
18.8 The success of a policy by a local authority to delegate its functions to a third party will be determined to a large extent, by the strength and quality of the contracts that the local authorities make with the delegated third party. Local authorities should therefore ensure that contracts are drafted by staff with the necessary skills and competencies to do so. Local authorities should consider the findings of the Social Work Practice pilot scheme , which tested approaches to delegation, when considering how to construct contracts.
18.9 Through the terms of their contracts with authorised third parties, local authorities have the power to impose conditions on how the function is carried out. For example, when delegating assessments the local authority could choose to require that assessments must be carried out by people with a particular training or expertise, and that the training must be kept up to date.
18.10 The delegated organisation will be liable to the local authority for any breach of the contract, and as such this is the mechanism through which local authorities are able to ensure that its functions are carried out properly, and through which they may hold the contractor to account.
18.11 Where a local authority uses its power under the Act to authorise another party to carry out its care and support functions, it should specify how long the authorisation lasts, and it should make clear that it may revoke the authorisation at any time during that period.
18.12 Local authorities should put in place monitoring arrangements so that they can assure themselves that functions that have been delegated, are being carried out in an appropriate manner. This should involve building good working relationships which allow local authorities to guide third parties about how they are exercising the functions, but equally for the local authority to learn about innovations and knowledge that third parties may be able to provide.
18.13 Since care and support functions are public functions, they must be carried out in a way that is compatible with all of the local authority’s legal obligations. For example, the local authority would be liable for any breach by the delegated party, of its legal obligations under the Human Rights Act or the Data Protection Act. Local authorities should therefore draw up its contracts so as to ensure that third parties carry out functions in a way that is compatible with all of their legal obligations.
18.14 Although local authorities retain overall responsibility for how its functions are carried out, delegated organisations will be responsible for any criminal proceedings brought against them.
18.15 Local authorities are able to choose the extent to which they delegate their functions. For example, they could authorise an external party to carry out all the elements of the function, including for example taking final decisions, or it can limit the steps the authorised organisation may take, leaving any final decisions to the local authority. Local authorities should make clear in its contracts with authorised parties, the extent to which the function is being delegated.
18.16 The fact that a local authority delegates its functions does not mean that it cannot also continue to exercise that function itself. So, for instance the local authority could ask a specialist mental health organisation to carry out care and support planning for people with specific mental health conditions, but it may choose to do care and support planning for people with other mental health conditions itself. Or it may choose to offer people a choice between itself and the external organisation.
Which care and support functions may not be delegated?
18.17 The Care Act does not allow certain functions to be delegated. These are:
Integration and cooperation
Local authorities must cooperate and integrate with local partners. Delegating these functions would not be compatible with meeting their duties to work together with other agencies. However, local authorities should take steps to ensure that authorised parties co-operate with other partners, work in a way which supports integration, and is consistent with their own responsibilities.
Adult safeguarding
The Care Act puts in place a legal framework for adult safeguarding, including the establishment of Safeguarding Adults Boards (SABs), carrying out safeguarding adult reviews and making safeguarding enquiries. Since the local authority must be one of the members of SABs, and it must take the lead role in adult safeguarding, it may not delegate these statutory functions to another party. However, it may commission or arrange for other parties to carry out certain related activities (see paragraph 18.19 below).
Power to charge
The Care Act gives local authorities the power to charge people for care and support in certain circumstances. Local policies relating to what can and cannot be charged for must rightly remain a decision of the local authority, and therefore the Act does not permit local authorities to delegate this decision to outside parties. However, it may commission or arrange for other parties to carry out related activities. What is the difference between delegating a statutory care and support function and commissioning other related activities?
18.18 For those functions which may not be delegated (outlined in paragraph 18.15 above), as well as other functions which may be delegated, local authorities may wish to use outside expertise to assist in carrying out practical activities to support it in discharging those functions, rather than fully or formally delegating the function itself to be carried out by another party.
18.19 There can be some uncertainty about the difference between delegation of a statutory care and support function and commissioning, arranging or outsourcing other procedural activities relating to a function. Local authorities should seek legal advice about whether the activity it is seeking to commission another party to undertake is a legal function under Part 1 of the Act or not.
18.20 For example, as set out above local authorities may not delegate their functions relating to establishing Safeguarding Adult Boards, making safeguarding enquiries or arranging safeguarding reviews. However, the enquiry duty is for local authorities to make enquiries or cause them to be made, so a local authority can still have arrangements whereby a third party is asked to undertake the enquiries where necessary. So while a local authority can ask others to carry out an actual enquiry, it cannot delegate its responsibility for ensuring that this happens and ensuring that, where necessary, any appropriate action is taken.
18.21 Similarly, it may decide to authorise an external agency to run a contact centre for people to report safeguarding incidents, and manage referrals to the local authority. It may be that the contact centre is not carrying out the local authority’s statutory functions (although its activities are related to the functions), and as such the local authority would not require any legal authority to outsource these activities, so may choose to do so.
18.22 Another example is the local authorities’ function which allows them discretion over charging people for care and support. The Act does not allow delegation of this decision to other organisations. As such the local authority itself must decide its charging policies. However, local authorities may commission an external agency to carry out the administration, billing and collection of fees for care and support on its behalf. These activities may not be classed as care and support functions under the Care Act, even though they are related to the charging function. It should be noted that the care and support function relating to financial assessments (section 17 of the Act) may be delegated.
Conflicts of interest
18.23 There might be instances where there is the potential for a conflict of interest when delegating functions. For example, when the same external organisation carries out care and support planning, but also provides the resulting care and support that is set out in the plan. Local authorities should consider whether the delegation of its functions could give rise to any potential conflict and should avoid delegating their functions where they deem that there would be an inappropriate conflict.
18.24 Local authorities should consider imposing conditions in their contracts with delegated parties to mitigate against the risk of any potential conflicts. For example, the local authority may choose to delegate care and support planning, but retain the final decision-making, including signing off the amount of the personal budget (see chapter 10 on care and support planning and chapter 11 on personal budgets). Local authorities should also consider including conditions that allow the contract to be revoked at any time, if having authorised an external party to exercise its functions, a conflict becomes apparent.
Conflict of interest relating to making direct payments
18.25 The Act places various functions on local authorities relating to the provision of direct payments. These functions include determining whether someone is capable of managing a direct payment, being satisfied that the direct payment is being used in a way that is meeting the person’s needs, and monitoring this periodically. Local authorities may choose to delegate these functions. For example, where an authorised external party is carrying out care and support planning, the local authority may decide that the direct payment functions could also usefully be delegated to that party (see chapter 12 on direct payments).
18.26 The Act also gives local authorities the function of making direct payments to people, that is, paying them money to meet their care and support needs. This function may also be delegated to an external party. However, where local authorities delegate their functions relating to assessment of needs or calculation of personal budgets to an external party, they should not allow that same party to make direct payments. In these cases, the actual payment of money should be made directly from the local authority to the adult or carer. This is because it is not appropriate for an external party to determine both how public funds are to be spent, as well as handling and those funds. This is in line with standard anti-fraud practice.
Case Study: Delegation of local authority care and support functions
A local authority has agreed a contract with a local user-led organisation (ULO), to carry out specialist needs assessments and care and support planning for people with learning disabilities. The expertise provided by the ULO allows for better interaction with the people undergoing assessments and a better understanding of their needs, resulting in more accurate and person-centred needs assessments.
The ULO’s specialist knowledge of local facilities, befriending groups and employment schemes allows them to broker more personalised care and support planning which allows the person’s needs to be met in a number of imaginative ways which support local people with learning disabilities to live independently, improves their wellbeing – and often with less costly care packages.
As part of the delegation, the local authority builds a good working relationship with the ULO, as it needs to monitor how the needs of the adults to whom they have a responsibility are being met. The local authority realises that the ULO has had some difficulty in advising its clients on employment laws for people who are employing personal assistants with their direct payments. The local authority has much experience of providing this type of advice to people with disabilities, and provides support to the ULO to help with this aspect of function.
Through the delegation, the local authority has been able to build its knowledge of specialist resources in its area that it did not previously know about, and has been able to learn about new practices in carrying out assessments and planning care and support packages more imaginatively and efficiently – learning which it is able to apply to other groups of people with care and support needs.
The more personalised assessment and care planning has resulted in fewer reviews of care plans. More people with learning disabilities in the area are supported to live independently for longer which results in better outcomes for them while simultaneously reducing costs to the local authority. The local authority has thus been able to use effective delegation as a way of promoting the wellbeing of its local population.
Moving between areas: inter-local authority and cross-border issues
This section contains chapters:
19. Ordinary residence
This chapter provides guidance on:
- Sections 39-41 of the Care Act 2014
- The Care and Support (Ordinary Residence) (Specified Accommodation) Regulations 2014
- The Care and Support (Disputes Between Local Authorities) Regulations 2014
This chapter covers:
- how ordinary residence affects the legal framework in the Care Act
- how to determine ordinary residence
- change in approach to determining ordinary residence disputes following the Supreme Court Judgment in R (on the application of Cornwall Council) v Secretary of State for Health
- determining ordinary residence when a person moves into certain types of accommodation out of area
- disputes between local authorities and the process for seeking a determination by the Secretary of State for Health or appointed person
- further information around ordinary residence and relevant scenarios (see annexes H)
19.1 It is critical to the effective operation of the care and support system that local authorities understand for which people they are responsible; and that people themselves know who to contact when they need care and support. Many of a local authority’s care and support responsibilities relate to the entire local population (for instance, in relation to information and advice or preventive services). However, when it comes to determining which individuals have needs which a local authority is required to meet, the local authority is only required to meet needs in respect of an adult who is ‘ordinarily resident’ in their area (or is present there but has no settled residence (see heading ‘People with no Settled Residence’ below).
19.2 Ordinary residence is crucial in deciding which local authority is required to meet the care and support needs of adults and their carers. Whether the person is ‘ordinarily resident’ in the area of the local authority is a key test in determining where responsibilities lie between local authorities for the funding and provision of care and support.
19.3 Ordinary residence is not a new concept – it has been used in care and support for many years. However, there have been in the past and will continue to be cases in which it is difficult to establish precisely where a person is ordinarily resident, and this guidance is intended to help resolve such situations. The Care Act also extends the principle of ‘deeming’ certain people to be ordinarily resident in a particular local authority’s area when some types of accommodation are arranged for them in another area, and the guidance also describes how these provisions should be put into practice. Local authorities cannot escape the effect of the deeming provision where they are under a duty to provide or to arrange for the provision of services (see para. 55 of R(Greenwich) v Secretary of State and Bexley (2006) EWHC 2576).
19.4 This chapter of the guidance should also be read with Annexes H1-H8, which provide further detailed guidance on specific situations and circumstances which may arise, and where the question of ordinary residence may be unclear.
How does ordinary residence affect the provision of care and support?
19.5 Ordinary residence is one of the key tests which must be met to establish whether a local authority is required to meet a person’s eligible needs. It is therefore crucial that local authorities establish at the appropriate time whether a person is ordinarily resident in their area, and whether such duties arise.
19.6 The test for ordinary residence, which determines which local authority would be responsible for meeting needs, applies differently in relation to adults with needs for care and support and carers. For adults with care and support needs, the local authority in which the adult is ordinarily resident will be responsible for meeting their eligible needs. For carers, however, the responsible local authority will be the one where the adult for whom they care is ordinarily resident.
19.7 Establishing responsibility for the provision of care and support for carers, therefore, requires the local authority to consider the ordinary residence of the adult needing care. However, there may be some cases where the carer provides care for more than one person in different local authority areas.
19.8 Where there is more than one local authority involved, those authorities should consider how best to cooperate on and share the provision of support. For example, where there are services or interventions that directly relate to the caring responsibilities towards one individual (for example, equipment installed in the carer’s home to accommodate one of the people), then it would be a straightforward matter of the relevant authority being responsible. Where that same piece of equipment serves for other people cared-for, then the local authorities concerned should agree how to arrange the package. There might be an agreement to jointly fund the support for the carer, or the authorities concerned may agree that one takes overall responsibility for certain aspects. For example, one might lead on reviews because it is geographically closer to the carer’s home.
19.9 The Care Act contains all the necessary powers for joint assessments and support planning, plus the duties to co-operate to provide a mechanism for one of the authorities to require the cooperation of the other, if needed.
19.10 Local authorities must determine whether an individual is ordinarily resident in their area following the needs or carer’s assessment, and after determining whether the person has eligible needs (see chapter 6).
19.11 The determination of ordinary residence must not delay the process of meeting needs. In cases where ordinary residence is not certain, the local authority should meet the individual’s needs first, and then resolve the question of ordinary residence subsequently. This is particularly the case where there may be a dispute between 2 or more local authorities.
How to determine ordinary residence
19.12 The local authority’s responsibility for meeting a person’s eligible needs under the Care Act is based on the concept of ordinary residence. However, there is no definition of ordinary residence in the Care Act. Therefore, the term should be given its ordinary and natural meaning.
19.13 In most cases, establishing the person’s ordinary residence is a straightforward matter. However, this is not always the case. There will be circumstances in which ordinary residence is not as clear cut, for example when people spend their time in more than one area, or move between areas. Where uncertainties arise, local authorities should always consider each case on its own merits.
19.14 The concept of ordinary residence involves questions of both fact and degree. Factors such as time, intention and continuity (each of which may be given different weight according to the context) have to be taken into account. The courts have considered the meaning of ordinary residence and the leading case is that of Shah v London Borough of Barnet (1983). In this case, Lord Scarman stated that:
unless … it can be shown that the statutory framework or the legal context in which the words are used requires a different meaning I unhesitatingly subscribe to the view that ordinarily resident refers to a man’s abode in a particular place or country which he has adopted voluntarily and for settled purposes as part of the regular order of his life for the time being, whether of short or long duration.
19.15 Local authorities must always have regard to this case when determining the ordinary residence of adults who have capacity to make their own decisions about where they wish to live. Local authorities should in particular apply the principle that ordinary residence is the place the person has voluntarily adopted for a settled purpose, whether for a short or long duration. Ordinary residence can be acquired as soon as the person moves to an area, if their move is voluntary and for settled purposes, irrespective of whether they own, or have an interest in a property in another local authority area. There is no minimum period in which a person has to be living in a particular place for them to be considered ordinarily resident there, because it depends on the nature and quality of the connection with the new place.
19.16 For people who lack capacity to make decisions about their accommodation and for children transitioning into adult social care services, the judgment in the case of R (on the application of Cornwall Council) Secretary of State & Ors [2015] UKSC46 (Cornwall) is appropriate because a person’s lack of mental capacity may mean that they are not able to voluntarily adopt a particular place of residence. [footnote 58]
Change in approach to determining ordinary residence disputes following the Supreme Court Judgment in R (on the application of Cornwall Council) v Secretary of State for Health
19.17 This statutory guidance sets out the changes to the approach to determining ordinary residence (OR) disputes between local authorities in relation to:
- adults who lack capacity to decide where to live and;
- looked after children [footnote 58] transitioning to certain adult social care and other accommodation
19.18 This follows the judgment that was handed down on 8 July 2015 in the Supreme Court, in the case of R (on the application of Cornwall Council) v Secretary of State [2015] UKSC 46 (‘Cornwall’). This case concerned the OR determination made by the Secretary of State in March 2012 that on 26 December 2004 (the day before PH’s 18th birthday), PH was ordinarily resident in Cornwall where his parents lived. In reaching this determination the Secretary of State applied his understanding of the law as decided in the case of R v Waltham Forest ex p. Vale (1985) (‘Vale’) in respect of the tests to apply to determine the ordinary residence of adults who lack capacity to decide where to live.
19.19 Cornwall council sought a judicial review of the determination. The determination was upheld by the High Court but reversed by the Court of Appeal who held that PH was ordinarily resident in South Gloucestershire where he had been placed as a child by Wiltshire and had lived for 14 years with his foster carers.
19.20 The decision was appealed to the Supreme Court who held that PH was ordinarily resident in Wiltshire, the authority which had placed him in South Gloucestershire.
19.21 Broadly, the Court made this decision because of the broad similarity between the deeming provisions in children’s and adult legislation, the underlying purpose of which was that an authority should not be able to export its responsibility for providing the necessary accommodation by exporting the person who is in need of it. Thus the Court said that:
- A person who is placed by local authority A in accommodation in the area of local authority B under the Children Act 1989 (the 1989 Act) and remains there until he or she becomes 18 is to be regarded on reaching 18 as remaining ordinarily resident in local authority A for the purpose of the deeming provisions in the National Assistance Act 1948. [footnote 59]
- The department’s reliance on the case of Vale [footnote 60] to substitute an alternative test of ordinary residence, based on ‘the seat of (his) [footnote 61] decision-making’, or otherwise on his relationship with his parents and their home, in relation to adults lacking capacity to decide where to live depended on a misunderstanding of that judgment.
19.22 Changes to the approach to ordinary residence reflecting the above findings are detailed below.
Cases where a person lacks capacity to decide where to live
19.23 All issues relating to mental capacity should be decided with reference to the Mental Capacity Act 2005 (the 2005 Act) [footnote 62]. Under this Act, it must be assumed that adults have capacity to make their own decisions, including decisions relating to their accommodation and care, unless it is established to the contrary.
19.24 The test for capacity is specific to each decision at the time it needs to be made, and a person may have capacity to make some decisions but not others. It is not necessary for a person to understand local authority funding arrangements to have capacity to decide where they want to live.
19.25 If it can be shown that a person lacks capacity to make a particular decision, the 2005 Act makes clear how decisions should be made for that person. For example, if a person lacks capacity to decide where to live, a best interests’ decision about their accommodation should be made under the 2005 Act. Under section 1(5) of the 2005 Act, any act done, or decision made (which would include a decision relating to where a person without capacity should live), must be done or made in the best interests of the person who lacks capacity. Section 4 of the 2005 Act sets out how to work out the best interests of a person who lacks capacity and provides a checklist of factors for this purpose.
19.26 Where a person lacks the capacity to decide where to live and uncertainties arise about their place of ordinary residence, direct application of the test in Shah will not assist since the Shah test requires the voluntary adoption of a place.
19.27 The Supreme Court judgment in Cornwall made clear that the essential criterion in the language of the statute [footnote 63] ‘is the residence of the subject and the nature of that residence’.
19.28 At paragraph 51, the judgment says in relation to the Secretary of State’s argument that the adult’s OR must be taken to be that of his parents as follows:
‘There might be force in these approaches from a policy point of view, since they would reflect the importance of the link between the responsible authority and those in practice representing the interests of the individual concerned. They are however impossible to reconcile with the language of the statute, under which it is the residence of the subject, and the nature of that residence, which provide the essential criterion…..’
19.29 At paragraph 47, the judgment refers to the attributes of the residence objectively viewed.
19.30 At paragraph 49, the judgment refers to an: assessment of the duration and quality of actual residence.
19.31 At paragraphs 47 and 52, the judgment refers to residence being ‘sufficiently settled’.
19.32 Therefore with regard to establishing the ordinary residence of adults who lack capacity, local authorities should adopt the Shah approach, but place no regard to the fact that the adult, by reason of their lack of capacity cannot be expected to be living there voluntarily. This involves considering all the facts, such as the place of the person’s physical presence, their purpose for living there, the person’s connection with the area, their duration of residence there and the person’s views, wishes and feelings (insofar as these are ascertainable and relevant) to establish whether the purpose of the residence has a sufficient degree of continuity to be described as settled, whether of long or short duration.
19.33 Physical presence provides a starting point for considering ordinary residence but does not necessarily equate to ordinary residence - a person could be physically present in an area but of no settled residence. This is covered in paragraphs 19.44 to 19.46 of the Care Act statutory guidance.
19.34 In certain situations, ordinary residence could be deemed to be in a different area to that in which a person is physically present. This is covered in paragraphs 19.44 to 19.59 of the Care Act statutory guidance and in the section below on looked after children transitioning to adult social care services.
19.35 Other situations such as temporary absences and people having more than one home are covered in paragraphs 19.70 to 19.74 of the Care Act statutory guidance.
19.36 The issue of duration is covered in paragraph 19.15 of the Care Act statutory guidance.
Looked after children transitioning to adult social care services
19.37 Prior to Cornwall, the department’s approach was to start with a presumption that, for the purposes of the 1948 Act, a looked after child who had been placed in accommodation out of area under the 1989 Act retained the ordinary residence of the local authority who had made the placement under the 1989 Act upon turning 18. That presumption could be rebutted by the circumstances of the case. In Cornwall, the Supreme Court held that a looked after child who had been placed in foster care in local authority A by local authority B under the 1989 Act and who was ordinarily resident in local authority B for the purposes of the 1989 Act, continued to be ordinarily resident in local authority B when he reached 18 for the purposes of deeming provisions [footnote 64] in the 1948 Act The Supreme Court set out that the underlying purpose behind deeming provisions in both children’s and adult legislation is that: ‘an authority should not be able to export its responsibility for providing the necessary accommodation by exporting the person who is in need of it.’ [footnote 65]
19.38 This means that for the purposes of the 2014 Act, and where relevant, the 1948 Act [footnote 66], any person who moves from accommodation provided under the 1989 Act to accommodation provided under the 1948 Act or 2014 Act, which is accommodation to which the deeming provisions under the 1948 Act or the 2014 Act apply, remains OR in the local authority in which they were ordinarily resident under the Children Act. This includes a situation where a child has been placed out of area under the 1989 Act as a looked after child and requires residential accommodation under the 1948 Act or the 2014 Act at age 18 as well as leaving care support under the 1989 Act.
19.39 The accommodation to which the adult deeming provisions apply is:
- ‘specified accommodation’ for the purpose of section 39 of the 2014 Act [footnote 67] in circumstances where the adult’s needs can be met only if they are living in accommodation of a specified type. The types currently specified are: care homes, shared lives scheme accommodation and supported living accommodation [footnote 68]
- NHS accommodation within the meaning of section 39 of the 2014 Act [footnote 69]
- residential accommodation under Part 3 of the 1948 Act
- NHS accommodation within the meaning of section 24 of the 1948 Act [footnote 70]
Accommodation to which deeming provisions do not apply
19.40 The above guidance on looked after children who have been placed in residential accommodation out of area under the 1989 Act and who transition to adult social care services applies where the person is provided with the specified accommodation as set out above for example, accommodation to which deeming provisions under the 2014 Act apply. It also applies to accommodation to which deeming provisions under the 1948 Act apply. In cases where those deeming provisions do not apply, although the provisions of the
19.41 Children Act normally no longer apply once a young person reaches 18 [footnote 71] local authorities should start from a presumption that for the purposes of the 1948 Act or the 2014 Act the young person remains ordinarily resident in the local authority in which they were ordinarily resident under the 1989 Act. However, this is only a starting point and if the young person remains in the area in which he was placed as a child or moves to a new local authority area the presumption may be rebutted by the circumstances of the individual’s case and the application of the Shah test.
Historic matters
19.42 In relation to historic matters, the position on OR might have been understood to be different to that which it would have been under the principles established in the Cornwall judgment, whether following a determination of a dispute or otherwise. If local authorities have concerns about this, they are advised to seek their own legal advice. When considering their options, the department would encourage LAs to have regard to the need to act in the interests of good fiscal administration.
Case studies; where a person lacks capacity to decide where to live
Mary is 30 years of age. She has severe learning disabilities. A best interests assessment under the Mental Capacity Act 2005 (the 2005 Act) has established that Mary lacks the capacity to make her own decisions, including decisions relating to her accommodation and care. Up until July 2015, she lived with her mum in a 2 bedroom property that her mum rented from a private landlord in local authority A. Mary’s mum has a serious condition that over the years has been getting progressively worse. This had caused her mum, over the past few years to spend longer and longer recovering in hospital. In May 2015, this culminated in local authority A, offering and subsequently carrying out a carers assessment for Mary’s mum that identified that she could no longer care for Mary. Local authority A thought about increasing Mary’s care package. However, local authority A spoke to Mary, her social worker, her mum and Mary’s sister about where would be best for Mary to live. All parties agreed that Mary should go to live with her sister in the area of local authority B. Local authority A helped organise the discussions with the family, they also reassessed her needs and agreed to continue to provide Mary’s domiciliary care. Local authority A also informed local authority B that Mary would be moving in to its area. Although in a different local authority area, the accommodation was not far from Mary’s her mum’s flat and very close to the hospital where her mum is often admitted. Mary settled very well in her new home with her sister and her family. Over the past year she has made friends with the family next door to her sister and a week after she moved she started attending the local church group and has become part of that community.
However in July 2016, a dispute arose between local authorities A and B as to who is the responsible authority for the provision of Mary’s care. Local authority, A who had been providing Mary with some domiciliary care, now argue that local authority B should now be the responsible authority as this is where Mary is currently resident, and has a connection with the area.
As Mary is not in specified accommodation and the ‘deeming’ provision in section 39 of the Care Act does not apply, Mary’s ordinary residence falls to be determined on its ordinary and natural meaning. As Mary lacks capacity, this should be approached based on the Shah test of ‘settled purpose’ without requiring voluntariness by evaluating the quality of the residence. This involves considering all the facts, including the place of physical presence, the purpose for living there, the connection with the area, the duration of residence there and the person’s views, wishes and feelings to establish whether the purpose of the residence has a sufficient degree of continuity to be properly described as settled, whether for short or long duration. In this case, Mary physically lives in local authority B. Mary is happy living with her sister and has formed connections with the area through the friends she has made and the activities she participates in. To all extents, therefore, Mary’s residence in local authority B has a settled purpose. Therefore, Mary’s ordinary residence would have transferred to local authority B when she moved to that area to live with her sister.
Karolina is 22 years old. She suffers from a severe learning disability. An assessment under the Mental Capacity Act 2005 (‘the 2005 Act’) had determined that she lacked the capacity to decide where to live.
Karolina received services from local authority A as a child, under the 1989 Act in the area of local authority B. When she became 18 it was considered in her best interests to place her in supported living accommodation in local authority area C. Local authority A continued to pay and provide her care. She attends a local day care centre, has forged a bond with her flatmates and attends the local church every Sunday.
Local authority A is in dispute with local authority B and C over Karolina’s care and support. It maintains that either of those local authorities is responsible for the provision of her care. Local authority B and C dispute this, as local authority A placed Karolina in local authority B and C.
If the placement was made under the 1948 Act, Karolina’s place of ordinary residence would be in the area of local authority C. This is because under the 1948 Act the placement would have been made to a type of accommodation (supported living accommodation) where the deeming provisions under that Act would not apply. However, although the provisions of the 1989 Act normally no longer apply once Karolina reaches 18, the local authorities in question could reasonably start from a presumption that Karolina remains ordinarily resident in local authority A as the local authority that had responsibility for her under the 1989 Act. However, the local authorities would also have to consider whether this presumption could be rebutted by the facts and the application of the Shah test. Karolina does not have capacity to decide where to live so she cannot be expected to live somewhere voluntarily. All the facts have to be considered including the fact that Karolina is physically present in local authority C, the move was made for settled purposes as the long term intention was for her to live more independently and she has established links ties in the area of local authority C. Therefore, in line with the Shah test, Karolina has acquired an ordinary residence in local authority C: the starting presumption that she is ordinarily resident in local authority A can be rebutted.
However if the placement was made under the 2014 Act then the deeming provisions under that Act would apply and when read with the deeming provisions under the 1989 Act, ordinary residence would remain in local authority A in line with the Cornwall judgment.
Case studies: Transition from accommodation under the 1989 Act to accommodation under the 2014 Act
Donna is taken into care by local authority A at the age of eight. She is placed with foster carers living in local authority B and therefore under the Children Act is deemed to be ordinarily resident in local authority A. She has learning disabilities, and she has capacity to decide where to live. Upon turning 18, in March 2016, she wishes to remain living in local authority B. The foster carers in local authority B agree to sign a Staying Put licence agreement in order that she can remain with them for a year. Donna has ongoing care and support needs and will need to be supported by an adult learning disability team. Her needs will be met under the 2014 Act. Local authority A is claiming that Donna is now ordinarily resident in local authority B and that local authority B should meet and fund her care and support needs as an adult. If Donna has chosen to remain living in local authority area B in a type of accommodation that is not specified in regulations under section 39 of the 2014 Act - the Care and Support (Ordinary Residence) (Specified Accommodation) Regulations 2014 (the accommodation regulations), Donna’s place of residence will be in the area of local authority B.
The local authorities in question could reasonably start from a presumption that Donna remains ordinarily resident in local authority A as the local authority that had responsibility for her under the 1989 Act. However, this presumption can be rebutted by the facts and the application of the Shah test. Donna has capacity to decide where to live and has chosen to remain in local authority B. She has lived in local authority B for around ten years, is well settled there and is expected to continue to live there on a long term basis. Therefore, in line with the Shah test, Donna has acquired an ordinary residence in local authority B. But if Donna is in a specified type of accommodation as set out in the 2014 Act and the accommodation regulations, for example shared lives scheme accommodation, where her care and support needs can only be met whilst she is in a specified type of accommodation, then she will be deemed to be ordinarily resident in the area in which she was ordinarily resident immediately before she began to live in a specified type of accommodation, that is to say, the area of local authority A. For the purposes of the 1989 Act she was, at that time, deemed to be ordinarily resident in local authority A. Although that deeming provision applied in determining ordinary residence for the purpose of the 1989 Act, this will also apply in relation to the deeming provision in the 2014 Act. This is on the basis of the principles in Cornwall that there is a broad similarity between the deeming provisions in the children’s and adult legislation, the underlying purpose of which are that an authority should not be able to export its responsibility for providing the necessary accommodation by exporting the person who is in need of it.
Sunil is 18 years old and has physical and learning disabilities. Since the age of 10 he has been accommodated in a specialist residential school under section 20 of the 1989 Act. The school is located in local authority B but paid for by local authority A, the local authority where his family live and where he lived before he went to school. For the purposes of the 1989 Act, Sunil is the responsibility of local authority A.
Now that Sunil is 18, he is ready to leave school. His needs are assessed and it is decided that he should move in to a house with three other people in a supported living tenancy. As Sunil has capacity to make some decisions for himself, he is able to express a desire to remain living in local authority B, near his friends from school and within the local community to which he feels he now belongs. Therefore, at the end of the school year he moves into his new home in local authority B and his accommodation changes from being provided under the 1989 Act to being provided under the 2014 Act.
At this point, local authority B falls into dispute with local authority A over Sunil’s ordinary residence. Local authority B’s view is that Sunil should remain the responsibility of local authority A. However, local authority A argues that their duty to Sunil ended when he left school and moved into accommodation under the 2014 Act in local authority B’s area and that he has become ordinarily resident in local authority B.
Supported living is a type of accommodation specified in regulations under section 39 of the 2014 Act, Sunil’s care and support needs can only be met if he is living in accommodation of that type and his needs are being under the 2014 Act whilst he is in that accommodation therefore for the purposes of Part 1 of that Act, Sunil’s ordinary residence is deemed to be in the area in which he was ordinarily resident immediately before moving into that accommodation for example, immediately before he became 18. For the purposes of the 1989 Act he was, at that time, deemed to be ordinarily resident in local authority A. Although that deeming provision applied in determining ordinary residence for the purpose of the 1989 Act, this will also apply in relation to the deeming provision in the 2014 Act and local authority A will be ‘deemed’ as Sunil’s place of ordinary residence even though he is not living in that area. This is on the basis of the principles in Cornwall that there is a broad similarity between the deeming provisions in the children’s and adult legislation, the underlying purpose of which are that an authority should not be able to export its responsibility for providing the necessary accommodation by exporting the person who is in need of it.
Persons of no settled residence
19.43 Where doubts arise in respect of a person’s ordinary residence, it is usually possible for local authorities to decide that the person has resided in one place long enough, or has sufficiently firm intentions in relation to that place, to have acquired an ordinary residence there. Therefore, it should only be in rare circumstances that local authorities conclude that someone is of no settled residence. For example, if a person has clearly and intentionally left their previous residence and moved to stay elsewhere on a temporary basis during which time their circumstances change, a local authority may conclude the person to be of no settled residence.
19.44 Sections 18 and 20 of the Care Act make clear that local authorities have a duty to meet the eligible needs of people if they are present in its area but of no settled residence. In this regard, people who have no settled residence, but are physically present in the local authority’s area, should be treated in the same way as those who are ordinarily resident.
19.45 A local authority may conclude that a person arriving from abroad is of no settled residence, including those people who are returning to England after a period of residing abroad and who have given up their previous home in this country. For further information on people returning to England after living abroad, see Annex H, paras. 31-34 (British citizens resuming permanent residence in England after a period abroad).
Case study: Persons of no settled residence
David is 20 years old and has a physical disability together with mild learning disabilities. Until 4 months ago, he lived with his family in local authority A. However, his family relationship broke down and his parents asked him to leave their home for good. They have since changed the locks on their house.
He sought help from local authority A and was placed in a care home for young people with disabilities located in local authority A. This placement was made on a short-term basis until a more permanent solution for David could be found in a supported living type accommodation with his own tenancy. However, David chose to leave the care home after a few weeks and stayed with friends in local authority B for a short period. However, he has recently presented at local authority B seeking accommodation on the basis that he is a destitute adult who is in need of care and attention. Local authority B provides David with care home accommodation but falls into dispute with local authority A over his place of ordinary residence.
Local authority B contends that David remains ordinarily resident in local authority A, given his previous residence there and his recent discharge from their care. Local authority A argues that David has acquired a new ordinary residence in local authority B.
As David is being provided with a type of accommodation by local authority B, as specified by the regulations, S39 (1) (a) applies. Therefore, he is deemed to continue to be ordinarily resident in the area in which he was ordinarily resident immediately before the care home accommodation was provided for him. The day before David presented at local authority B he was staying with friends in that local authority area. His friends made it clear that this was a short-term temporary arrangement, to prevent him becoming homeless upon leaving the care home in local authority A. He had not built up any community ties within the area of local authority B; nor had he chosen to reside in local authority B voluntarily and for settled purposes. Therefore, under the [Shah] test, David has not acquired an ordinary residence in local authority B.
However, nor does it appear that David has retained his ordinary residence in local authority A where he lived with his parents. He left the care home in local authority A intentionally and has no settled residence to which he can return. As David appears not to have been ordinarily resident in either local authority A or local authority B immediately before he presented at local authority B and was provided with accommodation, it is decided that he is a person of no settled residence. Section 18 of the Care Act 2014 makes clear that local authorities have a duty to meet the needs of someone, if they are present in its area but of no settled residence. Local authority B is therefore the authority responsible for David’s eligible care and support needs and can therefore treat David as if he were ordinarily resident in their area and provide him with accommodation.
Ordinary residence when arranging care and support in another area
19.46 There may be some cases where the local authority considers that the person’s care and support needs can only be met if they are living in a specified type of accommodation. This could be in a care home, or other kinds of premises that are specified in the legislation (see para. 19.28 for the types of accommodation specified). If the specified accommodation in which the care is provided is located in the area of another authority, it is important that there is no question as to which local authority is responsible for meeting the person’s needs.
19.47 Section 39 of the Care Act, and the specified accommodation regulations made under it [footnote 72] set out what should happen in these cases, and specify which local authority is responsible for the person’s care and support. Together, these create the principle that the person placed ‘out of area’ is deemed to continue to be ordinarily resident in the area of the first authority, and does not acquire an ordinary residence in the ‘host’ or second authority. The local authority which arranges the care in the specified accommodation, therefore, retains responsibility for meeting the person’s needs.
19.48 The specified accommodation regulations specify the types of accommodation to which this provision applies. The specified accommodation regulations explicitly set out 3 types of accommodation:
- nursing homes/care homes: accommodation which includes either nursing care or personal care
-
supported living/extra care housing this is either:
- specialist or adapted accommodation: this means accommodation which includes features that have been built in or changed to in order to meet the needs of adults with care and support needs. This may include safety systems and features which enable accessibility and navigation around the accommodation and minimise the risk of harm, as appropriate to the individual
- accommodation which is intended for occupation by adults with care and support needs, in which personal care is also available, usually from a different provider
- shared lives schemes: accommodation which is provided together with care and support for an adult by a shared lives carer, approved by the scheme, in the shared lives carer’s home under the terms of an agreement between the adult, the carer and any local authority responsible for making the arrangement. The shared lives carer will normally be providing personal care but they will not need to provide it in every case.
19.49 Where an adult’s care and support needs can only be met if they are living in one of the specified types of accommodation and the accommodation arranged is in another area, then the principle of ‘deeming’ ordinary residence applies. This means that the adult is treated as remaining ordinarily resident in the area where they were resident immediately before the local authority began to provide or arrange care and support in any type of specified accommodation. The consequence of this is that the local authority which first provided that care and support will remain responsible for meeting the person’s eligible needs, and responsibility does not transfer to the authority in whose area the accommodation is physically located. However, in circumstances where the person moves to accommodation in a different area of their own volition, without the local authority making the arrangements, they would be likely to acquire ordinary residence in the area of the authority where the new accommodation is situated. The deeming rule does not apply where a person has chosen to arrange their own care in a type of specified accommodation in another area, and then later asks for local authority support.
19.50 Need should be judged to be ‘able to be met’ or of a kind that ‘can be met only’ through a specified type of accommodation where the local authority has made this decision following an assessment and a care and support planning process involving the person. Decisions on how needs are to be met, made in the latter process and recorded in the care and support plan, should evidence that needs can only be met in that manner. Where the outcome of the care planning process is a decision to meet needs in one of the specified types of accommodation and it is the local authority’s view it should be assumed that needs can only be met in that type of accommodation for the purposes of ‘deeming’ ordinary residence. This should be clearly recorded in the care and support plan. The local authority is not required to demonstrate that needs cannot be met by any other type of support. The local authority must have assessed those needs in order to make such a decision - the ‘deeming’ principle therefore does not apply to cases where a person arranges their own accommodation and the local authority does not meet their needs.
19.51 The first local authority’s responsibility will continue in this way for as long as the person’s eligible needs are met by a specified type of accommodation. This will include situations where the person moves between care and support provided in different specified types of accommodation in another (or more than one other) area.
19.52 As an example, if the first authority arranges care and support in one type of accommodation in the area of the second authority (for example in a shared lives scheme or a care home) and the person’s needs change, leading to them moving into another type of accommodation still in the second authority’s area (for example a supported living scheme), the person would continue to be ordinarily resident in the area of the first authority, and that authority would remain responsible for the care and support. However, should the person’s needs no longer require the care and support to be provided in a specified type of accommodation, then it is likely that their ordinary residence will change, and the first local authority will no longer retain responsibility.
19.53 As part of their involvement in the planning process, where the local authority is arranging the person’s accommodation the person will also have a right to make a choice about their preferred accommodation (see chapter 8 and Annex A on choice of accommodation). This right allows the person to make a choice about a particular individual provider, including where that provider is located. Provided that certain conditions are met, the local authority must arrange for the preferred accommodation. The ordinary residence rules described above will apply when the person’s preferred accommodation is in the area of another local authority.
19.54 The ordinary residence ‘deeming’ principle applies most commonly where the local authority provides or arranges care and support in the accommodation directly. However, the principle also applies where a person takes a direct payment and arranges their own care (since the local authority is still meeting their needs). In such cases, the individual has the choice over how their needs are met, and arranges their own care and support. If the care plan stipulates that person’s needs can be met only if the adult is living in one of the specified types of accommodation and the person chooses to arrange that accommodation [footnote 73] in the area of a local authority which is not the one making the direct payments then the same principle would apply; the local authority which is meeting the person’s care and support needs by making direct payments would retain responsibility. However, if the person chose accommodation that is outside what was specified in the care plan or of a type of accommodation not specified in the regulations, then the ‘deeming’ principle would not apply.
19.55 At present, direct payments may not be made to meet needs by the provision of long-term care and support in a care home. However, the individual may request a direct payment to meet needs for other types of accommodation specified in the regulations. Where someone chooses a type of supported living accommodation, the direct payment would be for the care but usually not the accommodation. Local authorities should therefore ensure that they have in place effective, proportionate processes for recording how the individual chooses to meet their needs. More information on direct payments can be found in chapter 12.
19.56 If a local authority arranges care and support in a type of accommodation as specified in the regulations in another area, or becomes aware that an individual with a direct payment has done so themselves, the authority should inform the host authority, to ensure the host authority is aware of the person in their area. The first authority should ensure that satisfactory arrangements are made before the accommodation begins for any necessary support services which are provided locally, such as day care, and that clear agreements are in place for funding all aspects of the person’s care and support.
19.57 In practice, the first local authority may enter into agreements to allow the authority where the accommodation is located to carry out functions on its behalf. This may particularly be the case where the accommodation is located some distance away, and some functions can be performed more effectively locally. For example a carer may live in a different authority from the person he or she is caring for. Local authorities may make arrangements to reimburse to each other, any costs occurred through such agreements
19.58 There may be occasions where a provider chooses to change the type of care which it provides, for instance to de-register a property as a care home and to redesign the service as a supported living scheme. Where the person remains living at the same property, and their needs continue to be met by the new service, then ordinary residence should not be affected, and the duty to meet needs will remain with the first authority. This will occur even if the person temporarily moves to another address whilst any changes to the property occur.
NHS accommodation
19.59 Where a person goes into hospital, or other NHS accommodation, there may be questions over where they are ordinarily resident, especially if they are subsequently discharged into a different local authority area. For this reason, the Care Act makes clear what should happen in these circumstances.
19.60 A person for whom NHS accommodation is provided is to be treated as being ordinarily resident in the local authority where they were ordinarily resident before the NHS accommodation was provided. This means that where a person, for example, goes into hospital, they are treated as ordinarily resident in the area where they were living before they went into hospital. This applies regardless of the length of stay in the hospital, and means that responsibility for the person’s care and support does not transfer to the area of the hospital, if this is different from the area in which the person was ordinarily resident previously.
19.61 This requirement also applies to NHS accommodation in Northern Ireland, Scotland and Wales. If a person who is ordinarily resident in England goes into hospital in Scotland, Wales or Northern Ireland, their ordinary residence will remain in England (in the local authority in which they ordinarily resided before going into hospital) for the purposes of responsibility for the adult’s care and support.
Mental health after-care
19.62 Under section 117 of the Mental Health Act 1983 (the 1983 Act), local authorities together with CCGs [footnote 74] have a joint duty to arrange the provision of mental health after-care services for people who have been detained in hospital for treatment under certain sections of the 1983 Act. [footnote 75] After-care services must have both the purposes of ‘meeting a need arising from or related to the person’s mental disorder’ and ‘reducing the risk of a deterioration of the person’s mental condition and, accordingly, reducing the risk of the person requiring admission to a hospital again for treatment for mental disorder.’ The range of services which can be provided is broad. [footnote 76]
19.63 The duty on local authorities to commission or provide mental health after-care rests with the local authority for the area in which the person concerned was ordinarily resident immediately before they were detained under the 1983 Act, even if the person becomes ordinarily resident in another area after leaving hospital.
19.64 Although any change in the patient’s ordinary residence after discharge will affect the local authority responsible for their social care services, it will not affect the local authority responsible for commissioning the patient’s section 117 after-care. Under section 117 of the 1983 Act, as amended by the Care Act 2014, if a person is ordinarily resident in local authority area (A) immediately before detention under the 1983 Act, and moves on discharge to local authority area (B) and moves again to local authority area (C), local authority (A) will remain responsible for providing or commissioning their after-care. However, if the patient, having become ordinarily resident after discharge in local authority area (B) or (C), is subsequently detained in hospital for treatment again, the local authority in whose area the person was ordinarily resident immediately before their subsequent admission (local authority (B) or (C)) will be responsible for their after-care when they are discharged from hospital.
19.65 If, however, a patient is not ordinarily resident in England or Wales immediately before being detained, the local authority responsible for commissioning the patient’s after-care will be the one for the area in which the patient is resident. Only if that cannot be established, either, will the responsible local authority be the one for the area to which the patient is sent on discharge. However, local authorities should only determine that a person is not resident anywhere as a last resort.
19.66 Section 39(4) of the Care Act is a deeming provision that applies to any person who is provided with accommodation as part of their after-care. The effect of section 39(4) is that the person is deemed, for the purposes of Part 1 of the Care Act, to be ordinarily resident in the area of the local authority responsible for the person’s after-care. Section 39(4) will apply to any person who receives after-care on leaving hospital on or after 1 April 2015, irrespective of the date that they were discharged from detention under any of the relevant provisions cited in section 117(1).
19.67 There are several provisions in the Care Act (section 39(1)-(3) and (5)-(7) and paragraph 2 of Schedule 1) which deem a person to be ordinarily resident in a particular local authority’s area in specified circumstances for the purposes of Part 1 of the Act. These deeming provisions do not apply to section 117 of the 1983 Act, nor have they been incorporated into section 117 of the 1983 Act.
19.68 If there is a dispute between local authorities in England about where the person was ordinarily resident immediately before being detained, this will be determined by the process set out in section 40 of the Care Act. Disputes between a local authority in England and a local authority in Wales will be determined by the Secretary of State for Health or the Welsh Ministers. The Secretary of State and the Welsh Ministers have published arrangements for determining which of them will determine such disputes.
Other common situations
Temporary absences
19.69 Having established ordinary residence in a particular place, this should not be affected by the individual taking a temporary absence from the area. [footnote 77] The courts have held that temporary or accidental absences, including for example holidays or hospital visits in another area, [footnote 78] should not break the continuity of ordinary residence, and local authorities should take this into account.
19.70 The fact that the person may be temporarily away from the local authority in which they are ordinarily resident, does not preclude them from receiving any type of care and support from another local authority if they become in urgent need (see Annex H1 for further guidance regarding persons in urgent need). Local authorities have powers in the Care Act to meet the needs of people who are known to be ordinarily resident in another area, at their discretion and subject to their informing the authority where the person is ordinarily resident.
People with more than one home
19.71 Although in general terms it may be possible for a person to have more than one ordinary residence (for example, a person who divides their time equally between 2 homes), this is not possible for the purposes of the Care Act. The purpose of the ordinary residence test in the Act is to determine which single local authority has responsibility for meeting a person’s eligible needs, and this purpose would be defeated if a person could have more than one ordinary residence.
19.72 If a person appears genuinely to divide their time equally between 2 homes, it would be necessary to establish (from all of the circumstances) to which of the 2 homes the person has the stronger link. Where this is the case, it would be the responsibility of the local authority in whose area the person is ordinarily resident, to provide or arrange care and support to meet the needs during the time the person is temporarily away at their second home.
19.73 Further scenarios which may occur are set out in Annex H, and may be used by local authorities to support cases where there may be uncertainty as to an individual’s ordinary residence.
People who arrange and fund their own care
19.74 People who self-fund and arrange their own care (self funders) and who choose to move to another area and then find that their funds have depleted can apply to the local authority area that they have moved to in order to have their needs assessed. If it is decided that they have eligible needs for care and support, the person’s ordinary residence will be in the place where they moved to and not the first authority (for further information on self-funders, see annex H, paras. 21-23).
Resolving ordinary residence and continuity of care disputes
19.75 In the majority of cases, determining ordinary residence should be straightforward. However, there will be occasions where a person’s residency status is more complicated to establish.
19.76 A question as to a person’s ordinary residence can only arise where 2 or more local authorities are in dispute about the place of ordinary residence of a person. In such a case, the authorities may apply for a determination to the Secretary of State or appointed person. Where the local authorities concerned are in agreement about a person’s ordinary residence, but the person is unhappy with the decision, the person would have to pursue this with the authorities concerned and could not apply to the Secretary of State or an appointed person for a determination.
19.77 The Care and Support (Disputes Between Local Authorities) Regulations 2014 (the regulations), set out the procedures local authorities must follow when disputes arise between local authorities regarding a person’s ordinary residence. When a dispute between 2 or more local authorities occurs, local authorities must take all reasonable steps to resolve the dispute between themselves. It is critical that the person does not go without the care they need, should local authorities be in dispute. The local authority that is meeting the needs of the adult or the carer on the date that the dispute arises, must continue to do so until the dispute is resolved. If no local authority is currently meeting the person’s needs, then the local authority where the person is living or is physically present must accept responsibility until the dispute is resolved. The local authority which has accepted provisional responsibility is referred to as the ‘the lead authority’.
19.78 The lead authority must identify all the authorities involved in the dispute and co-ordinate an ongoing dialogue between all parties involved. The parties involved must provide the lead authority with contact details of a named person in relation to the dispute. The lead authority must be responsible for the co-ordination of any information that may be relevant to the dispute and keep all parties informed of any developments that may be relevant to the dispute. The lead authority must also keep the person, or their carer if appropriate, fully informed of dispute in question and of progress regarding any resolution.
19.79 If, having followed the procedure set out in the disputes regulations, the authorities are still unable to resolve a particular dispute, the lead authority must apply for a determination to the Secretary of State or appointed person. This should be done as soon as the local authorities agree that they are unable to resolve it and in any event no later than 4 months of the date the dispute first arose. The provisional acceptance of responsibility by the lead authority will not influence any determination made by the Secretary of State.
Process for seeking a determination
19.80 The regulations place a duty on the parties involved in the dispute to provide specified information to the Secretary of State or appointed person. It is the lead local authority that makes a request in writing to the Secretary of State or appointed person, together with a statement of facts and other documentation. The statement of facts must include certain specified information as set out in the regulations. Local authorities should endeavour to produce a statement of facts that is jointly agreed. If the parties cannot agree on particular information, they should make clear what information the parties say is agreed, what information the parties say is in dispute and, as regards the latter, what the parties’ respective versions of the facts are. Local authorities should ensure that all documents sent to the Secretary of State or appointed person are in an indexed paginated bundle. Copies of any further documents required will need to be added to the index for insertion into the bundle. All applications for determinations by the Secretary of State should be sent by email to OrdinaryResidenceReferrals@dhsc.gov.uk (preferred) or by post to:
The Department of Health and Social Care
Social Care Oversight Team
3rd Floor
39 Victoria Street
Westminster
London
SW1H 0EU
19.81 Local authorities may wish to seek legal advice before making an application for a determination, although they are not required to do so. Local authorities may, in addition to the required documentation, provide a separate legal submission. Such submissions must be submitted to the Secretary of State no later than 14 days from the date of the request for a determination. Where legal submissions are submitted, these should be exchanged between the local authorities in dispute and evidence of this should be supplied to the Secretary of State.
19.82 The Secretary of State or appointed person will not allow ordinary residence disputes to run on indefinitely once they have been referred for a determination. The Secretary of State – or appointed person – once satisfied that the parties have had adequate opportunity to make representations, will proceed to make a determination. Any local authority failing to have due regard to a determination by the Secretary of State or appointed person, would put itself at risk of a legal challenge by the resident or their representative or the other local authorities to the dispute.
19.83 If during a determination of the ordinary residence dispute by the Secretary of State or appointed person, a local authority in dispute is asked to provide further information to the Secretary of State or appointed person, that local authority must provide that information without delay.
19.84 If the local authorities involved in the dispute reach an agreement whilst the Secretary of State is considering the determination, they should notify the Department of Health and Social Care at the above address. Both parties must confirm that the dispute has been resolved after which the determination will be closed down.
19.85 If a determination by the Secretary of State or an appointed person subsequently finds another local authority to be the authority of ordinary residence, the lead local authority may recover costs from the authority which should have been providing the relevant care and support.
19.86 Regardless of when the Secretary of State is asked to make a determination, it will be made in accordance with the law that was in force at the relevant date, in respect of which ordinary residence falls to be determined. Therefore, where ordinary residence is to be determined in respect of a period which falls before 1st April 2015, then the determination will be made in accordance with Part 3 of the National Assistance Act 1948 (the 1948 Act). If, in respect of a period on or after 1st April 2015, then the determination will be made in accordance with the Care Act. Any question as to a person’s ordinary residence arising under the 1948 Act which is to be determined by the Secretary of State on or after 1 April 2015 is to be determined in accordance with section 40 of the 2014 Act (disputes about ordinary residence) and the new dispute procedure under the Care Act is to be followed [footnote 79].
19.87 The Department of Health and Social Care makes available anonymised copies of determinations it has made. Each case must be considered in light of its own particular facts, but past determinations may provide local authorities with useful guidance when faced with similar circumstances.
Financial adjustments between local authorities
19.88 Sometimes a local authority has been paying for a person’s care and support, but it later becomes apparent (for example as a result of an ordinary residence determination) that the person is in fact ordinarily resident elsewhere. In these circumstances the local authority which has been paying for that person’s care may reclaim the costs from the local authority where the person was ordinarily resident.
19.89 This can occur in cases where it is not clear initially where the person is ordinarily resident. In order to ensure that the individual does not experience any delay to their care due to uncertainty over their ordinary residence, local authorities should be able to recover any losses due to initial errors or delays in deciding where a person is ordinarily resident. This also extends to costs spent supporting the carer of the person whose ordinary residence was in dispute.
Reconsidering disputes
19.90 Local authorities may ask the Secretary of State or appointed person to reconsider the original determination by way of a review. As a consequence of this, a different determination may be substituted. This may mean that payments made from one local authority to another as a consequence of the first determination will need to be repaid.
19.91 Any review of the determination must begin within 3 months of the date of the original determination. So, any local authority seeking a review must ensure that their request is received by the Secretary of State or appointed person no later than 3 months from the date of the determination. This is needed to ensure clarity and fairness in the process and minimise the amount of time taken for the dispute to be resolved.
When seeking a review a local authority should provide the Secretary of State or appointed person with the legal arguments it relies on, within its request for a review. At the same time as seeking a review the local authority should notify the other local authority/authorities who are party to the dispute that it has sought a review, and provide the local authority/authorities with a copy of its request for a review and any legal arguments it relies on.
A local authority who has been notified of a review should submit any legal arguments that it intends to rely on within 14 days from that notification.
Where local authorities dispute whether a review should take place at all, then the Secretary of State or appointed person will consider the local authorities’ views and reach a decision on whether to proceed with the review. If the decision is to proceed, the 14 days to provide legal arguments start from the date of that decision.
20.Continuity of care
This section provides guidance on:
- Sections 37-38 of the Care Act 2014
- The Care and Support (Continuity of Care) Regulations 2014
This chapter covers:
- making an informed decision to move to a different local authority; confirming intention to move; supporting people to be fully involved in the process
- what local authorities take into account when they are planning the move with people
- how to ensure continuity of the person’s care if the second local authority has not carried out an assessment ahead of the day of the move
- what happens if a person does not move
20.1 People with care and support needs may decide to move home just like anyone else, such as to be closer to family or to pursue education or employment opportunities, or because they want to live in another area. Where they do decide to move to a new area and as a result their ordinary residence status changes (see chapter 19 on ordinary residence), it is important to ensure that care and support is in place during the move, so the person’s wellbeing is maintained.
20.2 In circumstances where a person is receiving local authority support and moves within their current local authority (for example, moving between homes in the same area), they would remain ordinarily resident within that authority and it must continue to meet their needs. Where the person chooses to live in a different local authority area, the local authority that is currently arranging care and support and the authority to which they are moving must work together to ensure that there is no interruption to the person’s care and support.
20.3 The continuity of care chapter sets out the process local authorities must follow to ensure that the person’s care and support continues, without disruption, during and after the move. These procedures also apply where the person’s carer is receiving support and will continue to care for the adult after they have moved. In addition to meeting their responsibilities in these sections, authorities are reminded that the other requirements of Part 1 of the Act apply during this process, and authorities should refer to the guidance on wellbeing, prevention, information and advice, integration, assessment and eligibility, and care and support planning.
20.4 The aim of this process is to ensure that the person with care and support needs will be able to move with the confidence that arrangements to meet their needs will be in place on the day of the move. Local authorities are expected to achieve continuity of care by ensuring that the second authority has completed a needs assessment and developed a care and support plan for the individual prior to the day of the move. It is possible that the second local authority might be unable to complete a needs assessment prior to the day of the move due to the logistics of assessing a person a long distance away or because they want to assess the adult in their new home. If the second authority has not carried out the assessment prior to the move, it must continue to meet the needs and take into account outcomes identified in the adult’s current care and support plan until it has carried out its own assessment.
20.5 The key to ensuring that the adult’s care is continued is through both local authorities working together and that the adult and their carer, if they are continuing to care for the adult, are at the centre of the process.
Definitions
20.6 For the purpose of this chapter the following meaning applies:
Adult
Means the person who needs care and support, and is or is intending to move to another authority.
Carer(s)
refers to any carer(s) that the person may have who has decided to continue to care for the adult after they have moved to the new area|.
New carer
Refers to any new person who will take over the caring role when the adult moves to the new area.
Person or individual
Refer to both the adult needing care and support and the carer.
First authority
The local authority where the person lives and is ordinarily resident prior to moving.
Second authority
The local authority the person is wishing to move to.
Assessment
Refers to both a needs assessment and a carer’s assessment.
Making an informed decision to move to a different local authority
20.7 When contemplating the possibility of moving, an adult may want to find out information about the care and support available in one or more authorities. Local authorities may already make much of this information publicly available in accordance with its general duties under the Care Act (see chapter 3), and they should provide any extra information requested by the adult and where relevant, their carer.
20.8 Local authorities can provide the adult and their carer with relevant information or advice to help inform their decision. When providing relevant information and advice, local authorities should guard against influence over the final decision. The authorities can, for example, provide advice on the implications for the individual’s care and support (and their carer’s support), but the final decision on whether or not to move is for the adult and, if relevant, the carer to make.
20.9 The prompt provision of this information will help the adult make an informed decision and assist the process if the adult decides that they want to move.
Confirming the intention to move
20.10 The continuity of care process starts when the second authority is notified of the adult’s intention to move. Local authorities may find out about the person’s intention to move from the individual directly or through someone acting on their behalf, who may contact either the first authority or the second authority to tell them of their intentions. If the person has approached the first authority and informed them of their intention to move, the first authority should make contact with the second authority to tell them that the person is planning on moving to their area.
20.11 When the person has confirmed their intention to move with the second authority, the authority must assure itself that the person’s intention is genuine. This is because the duties in the Act flow from this point.
20.12 To assure itself that the intention is genuine, the second authority should:
- establish and maintain contact with the person and their carer to keep abreast of their intentions to move
- continue to speak with the first authority to get their view on the person’s intentions
- ask if the person has any information or contacts that can help to establish their intention
20.13 When the second authority is satisfied that the person’s intentions to move are genuine, it must provide the adult and the carer if also intending to move, with accessible information about the care and support available in its area. This should include but is not limited to, details about:
- the types of care and support available to people with similar needs, so the adult can know how they are likely to be affected by differences in the range of services available
- support for carers
- the local care market and organisations that could meet their needs
- the local authority’s charging policy, including any charges which the person may be expected to meet for particular services in that area
20.14 Where the person moving currently receives a direct payment to meet some or all of their needs, the first authority should advise the person that they will need to consider how to meet any contractual arrangements put in place for the provision of their care and support. For instance, any contracts a person may have with personal assistants who may not be moving with them.
Supporting people to be fully involved
20.15 The person may request assistance from either the first or second authority in helping them understand the implications of their move on their care and support, and the authority should ensure that they have access to all relevant information and advice. This should include consideration of the need for an independent advocate in helping the person to weigh up their options (see chapter 7 on advocacy).
20.16 There will be situations where the adult may lack capacity to make a decision about a move, but the family wish to move the adult closer to where they live.
20.17 The local authority must in these situations first carry out supported decision making, supporting the adult to be as involved as possible and must carry out a capacity assessment and where necessary then take ‘best interests’ decisions. The requirements of the Mental Capacity Act 2005 apply to all those who may lack capacity.
Preparing for the move
20.18 Once the second authority has assured itself that the adult’s and where relevant the carer’s intentions to move are genuine, it must inform the first authority. At this stage, both authorities should identify a named staff member to lead on the case and be the ongoing contact during the move. These contacts should make themselves known to the person and lead on the sharing of information and maintaining contact on progress towards arranging the care and support for the adult and support for the carer. These contacts should be jointly responsible for facilitating continuity of care within an acceptable timeframe, taking into consideration the circumstances behind the adult’s intention to move, such as a job opportunity.
20.19 The second authority must provide the adult and carer with any relevant information that it did not supply when the person was considering whether to move.
20.20 When the first authority has been notified by the second authority that it is satisfied that the person’s intention to move is genuine, the first authority must provide it with:
- a copy of the person’s most recent care and support plan
- a copy of the most recent support plan where the person’s carer is moving with them
- any other information relating to the person or the carer (whether or not the carer has needs for support), that the second authority may request
20.21 The information the second authority may request may include the most recent needs assessment if the person’s needs are not likely to change as a result of the move, the adult’s financial assessment, any safeguarding plan that have been completed for the individual, and, where a Deprivation of Liberty has been authorised for a person who is moving to a new local authority area, then a new referral for a Deprivation of Liberty must be made to the new local authority. [footnote 80]
People receiving services under children’s legislation
20.22 The continuity of care provisions will not apply for people receiving services under children’s legislation. Where such a person has had a transition assessment (see chapter 16) but is moving area before the actual transition to adult care and support takes place, the first local authority should ensure that the second is provided with a copy of the assessment and any resulting transition plan. Similarly, where a child’s carer is having needs met by adult care and support in advance of the child turning 18 (following a transition assessment), the first local authority should ensure that the second is provided with a copy of the assessment and the carer’s support plan.
Assessment and care and support planning
20.23 If the person has substantial difficulty and requires help to be fully involved in the assessment or care planning process and there is no other suitable person who can support them, the Act requires that they must be provided with an independent advocate. In this case the advocate should be provided by the second authority because it takes over the responsibility for carrying out the assessment and care planning with the individual (see chapter 7).
20.24 The second authority must contact the adult and the carer to carry out an assessment and to discuss how arrangements might be made. The second authority should also consider whether the person might be moving to be closer to a new carer and whether that new carer would benefit from an assessment.
20.25 Throughout the assessment process, the first authority must keep in contact with the second authority about progress being made towards arranging necessary care and support for the day of the move. The first authority must also keep the adult and the carer informed and involved of progress so that they have confidence in the process. This should include involving them in any relevant meetings about the move. Meetings may not always be face-to-face where there are long distances between the local authorities involved. Having this 3-way contact will keep the individuals at the centre of the process, and help ensure that arrangements are in place on the day of the move.
20.26 All assessments, for adults with care and support needs and carers, must be carried out in line with the processes described in chapter 6 of this guidance. The adult and the carer, and anyone else requested, must be involved in the respective assessments. The assessments must identify the person’s needs and the outcomes they want to achieve. These could be the same as the outcomes the first authority was meeting or they could have changed with the person’s circumstances.
20.27 The assessment must consider whether any preventative services or advice and information would help either person meet those outcomes. The assessments should also consider the individuals’ own strengths and capabilities and whether support might be available from family, friends or within the new community to achieve their outcomes. In carrying out the assessments, the second authority must take into account the previous care and support plan (or support plan) which has been provided by the first authority.
20.28 Following the assessment and after determining whether the adult or carer has eligible needs, the second authority must involve the adult, the carer and any other individual the person requests, in the development of their care and support plan, or the carer’s support plan as relevant, and take all reasonable steps to agree the plan. The development of the care and support plan or carer’s support plan should include consideration of whether the person would like to receive a direct payment. Further guidance on care and support planning is provided in chapter 10.
20.29 The second authority should agree the adult’s care and support plan and carer’s support plan, including any personal budget, in advance of the move to ensure that arrangements are in place when the person moves into the new area. This should be shared with the individuals before the move so that they are clear how their needs will be met, and this must also set out any differences between the person’s original plan and their new care and support or support plan. Such differences could arise where the range of services in one local authority differs from the range of services in another. The second authority must also explain to the adult or carer where there are any differences in their needs.
20.30 The care and support plan should include arrangements for the entire day of the move. This should be agreed by the adult, the carers (existing and new as relevant) and both authorities. The first authority should remain responsible for meeting the care and support needs the person has in their original home and when moving. The second authority is responsible for providing care and support when the person and their carer move in to the new area. The person moving is responsible for organising and paying for moving their belongings and furniture to their new home.
20.31 In considering the person’s personal budget, the second authority should take into consideration any differences between the costs of making arrangements in the second authority compared with the first authority and provide explanation for such a difference where relevant. Where there is a difference in the amount of the personal budget, this should be explained to the person. It should also look to ensure that the person’s direct payment is in place in a timely manner since, for example, the person moving may have a personal assistant that is also moving and will require payment.
Integration
20.32 The adult and their carer may have health needs as well as care and support needs. Both local authorities should work with their local clinical commissioning groups (CCGs) to ensure that all of the adult’s and carer’s health and care needs are being dealt with in a joined-up way. Guidance to CCGs is set out in Who Pays? Determining Responsibility for Payments to Providers (PDF, 326KB).
20.33 If the person also has health needs, the second authority should carry out the assessment jointly with their local CCG. Alternatively, if the CCG agrees, the second authority can carry out the assessment on its behalf. Having a joint assessment ensures that all of the person’s needs are being assessed and the second authority can work together with the CCG to prepare a joint plan to meet the adult’s care and support and health needs. Where relevant, the local authority may use the cooperation procedures set out in the Care Act to require cooperation from the CCG, or other relevant partners, in supporting with the move (for further detail on these procedures, see chapter 15).
20.34 Providing joint care and support and health plans will avoid duplication of processes and the need for multiple monitoring regimes. Information should be shared as quickly as possible with the minimum of bureaucracy. Local authorities should work alongside health and other professionals where plans are developed jointly to establish a ‘lead’ organisation which undertakes monitoring and assurance of the combined plan. Consideration should be given to whether a person should receive a personal budget and a personal health budget to support integration of services. More information about personal budgets, including how to integrate them with personal health budgets can be found in chapter 11.
Equipment and adaptations
20.35 Many people with care and support needs will also have equipment installed and adaptations made to their home. Where the first authority has provided equipment, it should move with the person to the second authority where this is the person’s preference and it is still required and doing so is the most cost-effective solution. This should apply whatever the original cost of the item. In deciding whether the equipment should move with the person, the local authorities should discuss this with the individual and consider whether they still want it and whether it is suitable for their new home. Consideration will also have to be given to the contract for maintenance of the equipment and whether the equipment is due to be replaced.
20.36 As adaptations are fitted based on the person’s accommodation, it may be more practicable for the second authority to organise the installation of any adaptations. For example, walls need to be checked for the correct fixing of rails.
20.37 Where the person has a piece of equipment on long-term loan from the NHS, the second local authority should discuss with the relevant NHS body. The parties are jointly responsible for ensuring that the person has adequate equipment when they move (see chapter 15 on cooperation and integration).
Copy of documentation
20.38 The second authority must provide the adult and the carer and anyone else requested with a copy of their assessments. This must include a written explanation where it has assessed the needs as being different to those in the care and support plan or the carer’s support plan provided by the first authority. The second authority must also provide a written explanation if the adult’s or carer’s personal budget is different to that provided by the first authority.
What happens if the second authority has not carried out an assessment before the day of the move?
20.39 The second local authority is generally expected to have carried out their needs assessment of the persons moving prior to the day of the move. However, there may be occasions where the authority has not carried out the assessments or has completed the assessments but has not made arrangements to have support in place. This might happen where the second authority wants to assess the person in their new home and consider if their needs have changed, for example because they have started a new job or are now in education, or they have moved to be closer to family. The second authority must still have made contact with the adult and their carer in advance of the move.
20.40 Where the full assessment has not taken place prior to the move, the second authority must put in place arrangements that meet the adult’s or carer’s needs for care and support as identified by the first authority. These arrangements must be in place on the day of the move and continue until the second authority has carried out its own assessment and put in place a care and support plan which has been developed with the person (see Chapters 6-10).
20.41 The second authority must involve the adult and carer, and any relevant independent advocate, as well as any other individual that either person may request, when deciding how to meet the care and support needs in the interim period. The authority must take all reasonable steps to agree these temporary arrangements with the relevant person.
Matters local authorities must have regard to when making arrangements
20.42 The Care and Support (Continuity of Care) Regulations 2014 require the second authority to have regard to the following matters when meeting the person’s needs in advance of carrying out their own assessment:
Care and support plan
The adult’s care and support plan, and the carer’s support plan if the carer is also moving, which were provided by the first authority. The second authority should discuss with the adult and the carer how to meet their eligible needs and any other needs that the first authority was meeting that are not deemed as eligible but were included in either plan.
Outcomes
Whether the outcomes that the adult and the carer were achieving in day-to-day life in their first authority are the outcomes they want to achieve in the new authority, or whether their aims have changed because of the move.
Preferences and views
The preferences and views of the adult and the carer on how their needs are met during the interim period.
20.43 The second authority must also consider any significant difference to the person’s circumstances where that change may impact on the individual’s wellbeing, including:
Support from a carer
Whether the adult is currently receiving support from a carer and whether that carer is also moving with them. Where the carer is not moving the second authority must consider how to meet any needs previously met by the carer, even if the first authority was not providing any service in relation to those needs.
Suitability of accommodation
Where the new accommodation is significantly different from the original accommodation and this changes the response needed to meet the needs. For example, the adult may move from a ground floor flat to a first floor flat and now need assistance to manage stairs.
Where the person has received equipment or had adaptations installed in their original home by the first authority, the procedures set out in paras. 20.35-20.37 should be followed.
Access to services and facilities
Where the services and facilities in the new area are different, and in particular fewer than those in the originating area; for example access to food deliveries or other food outlets, access to public transport, or access to leisure or recreational facilities, the person’s workplace. A move from an urban to a rural environment could bring this about.
Access to other types of support
Where the person was receiving support from friends, neighbours or the wider community and this may not readily be available in their new area.
- where the person makes use of universal services such as local authority day services, drop in support, or befriending schemes, and these are not available in the new area
20.44 If the person has substantial difficulty in being fully involved in the assessment, care planning or review process the second authority should consider whether the person needs an independent advocate or whether their original advocate is moving with them (see chapter 7 on advocacy).
20.45 The second authority should ascertain this information from relevant documentation sent to them or by talking to the individuals involved, and the first authority.
20.46 The adult or carer should not be on an interim care and support (or support) package for a prolonged period of time as a tailored care and support (or support) plan must be put in place. The second authority should carry out the assessment in a timely manner.
When the adult does not move or the move is delayed
20.47 There are a range of reasons why a person might not move on the designated day. This may be, for example, because they have become unwell, there has been a delay in exchanging contracts. Where there has been a delay because of unforeseen circumstances, both authorities should maintain contact with the person to ensure that arrangements are in place for the new date of the move.
20.48 If the person’s move is delayed and they remain resident in the area of the first authority, they will normally continue to be ordinarily resident in that area and so the first authority will remain responsible for meeting the person’s and the carer’s needs. Both local authorities may have incurred some expense in putting arrangements in place before the move was delayed. In such circumstances each of the authorities should consider agreeing to cutting their losses incurred in preparing continuity of care.
20.49 In circumstances where the second authority has not assessed the person prior to the move and is planning to meet needs based on their original care and support plan, but it transpires that the individual does not move to the second authority (and so the first authority remains responsible for providing care and support), the Care Act does provide for the second authority to be able to recover any costs it incurred from the first authority. In deciding whether to recover these costs the second authority may want to consider, for example, whether the first authority was aware that the person was not going to move and had not told the second authority or whether the first authority was not aware and was unable to advise the second authority not to make arrangements. The second authority should consider whether it would be reasonable to recover their costs depending on the circumstances of the case.
Disputes about ordinary residence and continuity of care
20.50 Where local authorities are in dispute over application of the continuity of care provisions, the authorities who are parties to the dispute must not allow their dispute to prevent, delay or adversely affect the meeting of the person’s needs. Where the authorities cannot resolve their differences, the steps described in chapter 19 on ordinary residence disputes must be taken to ensure that the person is unaffected by the dispute and will continue to receive care for the needs that were identified by the first local authority.
Making complaints
20.51 It is important that individuals have confidence in the assessment process and the wider care and support system. Therefore any individual should be able to make a complaint and challenge decisions where they believe a wrong decision has been made in their case. Current complaints provision for care and support is set out in regulations Local Authority Social Services and NHS Complaints Regulations 2009, made under powers in Sections 113 to 115 of the Health and Social Care (Community Health and Standards Act) 2003. The provisions of the regulations mean that anyone who is dissatisfied with a decision made by the local authority would be able to make a complaint about that decision and have that complaint handled by the local authority. The local authority must make its own arrangements for dealing with complaints in accordance with the Local Authority Social Services and National Health Service (England) Complaints Regulations 2009 No. 309.
21. Cross-border placements
This chapter provides guidance on:
- Section 39 of and Schedule 1 to the Care Act 2014
- The Care and Support (Cross-border Placements and Business Failure: Temporary Duty) (Dispute Resolution) Regulations 2014
This chapter covers:
- responsibilities of local authorities or Health and Social Care (HSC) Trusts in Northern Ireland, with respect to placing individuals into care home accommodation in different territories of the UK
- those matters local authorities (or HSC trusts) should have regard to when considering, planning and carrying out a cross-border placement
- process for resolving disputes that may arise in relation to a cross-border placement
Definitions
21.1 First authority: the local authority or HSC trust which places the individual in a cross-border residential placement
21.2 Second authority: that local authority or HSC trust into whose area the individual is placed or to be placed
Principles and purpose of cross-border placements
Purpose
21.3 People’s health and wellbeing are likely to be improved if they are close to a support network of friends and family. In a small number of cases an individual’s friends and family may be located in a different country of the UK from that in which they reside.
21.4 In the production of a care and support plan, [footnote 81] the authority [footnote 82] and the individual concerned may reach the conclusion that the individual’s wellbeing is best achieved by a placement into care home accommodation (‘a residential placement’) in a different country of the UK. Schedule 1 to the Care Act sets out certain principles governing cross-border residential care placements.
21.5 As a general rule, responsibility for individuals who are placed in cross-border residential care remains with the first authority. This guidance sets out how the first and second authorities should work together in the interests of individuals receiving care and support through a cross-border residential placement.
Principles
21.6 The 4 administrations of the UK (England, Scotland, Wales and Northern Ireland) have worked together to agree Schedule 1 and this accompanying guidance. Underpinning this close co-operation have been 2 guiding principles that those involved in making cross-border residential care placements should abide by.
A person-centred process
21.7 The underlying rationale behind Schedule 1 is to improve the wellbeing of individuals who may benefit from a cross-border residential care placement. If an authority, in creating an individual’s tailored care and support plan, believes a cross-border placement could be appropriate they should discuss this with the individual and/or their representative. In making the resulting arrangements, authorities should and in certain cases, must have regard to views, wishes, feelings and beliefs of the individual (see chapter 1 on promoting wellbeing).
Reciprocity and cooperation
21.8 The smooth functioning of cross-border arrangements is in the interests of all parties – and most importantly the interests of those in need of a residential placement – in all authorities and territories of the UK. It is not envisaged that authorities will suffer significant added financial disadvantage by making cross-border placements. All authorities are expected to co-operate fully and communicate properly. In the circumstances where individuals may need care and support from the second authority (for example, in the event of unforeseen and urgent circumstances such as provider failure) the second authority may have a duty to meet such needs and there should be no delay in the discharge of such a duty (arrangements to recoup costs can always be made subsequently).
21.9 Local authorities in England making a cross-border placement should be aware that in general the duties specified in the Act, and this statutory guidance, apply to cross-border placements as they apply to placements within an authority’s own area. This guidance applies to cross-border placements of any duration.
Cross-border residential placements
21.10 Authorities should follow the following broad process for making cross-border residential placements. Authorities may wish to adapt this process to fit their needs; but in general, authorities should aim to follow, as far as possible, the processes set out below.
21.11 Authorities may wish to designate a lead official for information and advice relating to cross-border placements and to act as a contact point.
21.12 These steps should be followed whenever a cross-border residential placement is arranged by an authority, regardless of whether it is paid for by that authority or by the individual.
Step 1: care and support planning
21.13 A need for a cross-border residential care placement will be determined as part of the overall care and support plan prepared by the authority, in partnership with the individual concerned.
21.14 Authorities should, in assessing care and support needs, establish what support networks (for example, friends and family) the individual concerned has in their current place of residence. In discussions with the individual and other relevant parties, enquiries should be made as to whether a support network exists elsewhere. Alternatively, the individual (or their family or friends) may proactively raise a desire to move to an area with a greater support network160 or to move to an area for other reasons.
21.15 Authorities should give due consideration as to how to reflect cross-border discussions with the individual in the care and support planning process (see chapter 10 on care and support planning for further information).
21.16 Where it emerges that residential care in a different territory of the UK may be appropriate for meeting the person’s needs, the authority should inform the individual concerned (and/ or their representative) of the potential availability of a cross-border placement if the individual (and/ or their representative) has not already raised this themselves.
21.17 Should the individual wish to pursue the potential for a cross-border placement, the authority will need to consider carefully the pros and cons. Questions the authority may wish to address could include:
- Would the support network in the area of the proposed new placement improve (or at least maintain) the individual’s wellbeing?
- What effect might the change of location have on the individual’s wellbeing? How well are they likely to adapt to their new surroundings?
- Is the individual in receipt of any specialist health care? Will the locality of the proposed new placement allow for the satisfactory continuation of this treatment?
- Where the individual lacks the mental capacity to decide where to live, who is the individual’s representative? The representative should be consulted and in certain cases there will be a duty to involve such persons in carrying out a needs assessment. [footnote 83] [footnote 84]
21.18 With the permission of the individual concerned (or their representative), the authority should approach the friends and/or family of the individual concerned who are resident in the area of the proposed new placement (and, any friends and/ or family in the area of their current residence) to seek their views on the perceived benefits of the placement and any concerns they may have.
21.19 Should a cross-border placement still appear to be in the interests of the individual’s wellbeing the authority should take steps to investigate which providers in the proposed new placement area exist and which are likely to be able to meet the needs of the individual. The authority should conduct all necessary checks and exercise due diligence as it would with any other residential placement.
21.20 In preparing a care and support plan, authorities should (and in England must) involve the individual, any carer of the individual, and any person whom the individual asks the authority to involve or, where the individual lacks capacity to ask the authority to involve others, any person who appears to the authority to be interested in the individual’s welfare. In involving the individual, the authority should (and in England must) take all reasonable steps to reach agreement with the individual about how the authority should meet the needs in question.
21.21 The individual should be kept informed and involved throughout the process. Their views on suitable providers should be sought and their agreement checked before a final decision is made. The benefits of advocacy in supporting the individual to express their wishes should be considered throughout and relevant duties met (see chapter 7 on advocacy).
21.22 The individual should also be informed of the likelihood of the first authority giving notification of the placement to the second authority, seeking that authority’s assistance with management of the placement or with discharge of other functions, for example reviews, and of what this would involve. Where, for example, this would involve the sharing of information or the gathering of information by the second authority on behalf of the first, (see next section) the individual should be informed of this at the outset and their consent sought.
21.23 Authorities should strive to offer people a choice of placements. [footnote 85]
Step 2: initial liaison between first and second authority
21.24 Once the placement has been agreed in principle (with the individual concerned and/or their representative) and the authority has identified a potential provider they should immediately contact the authority in whose area the placement will be made.
21.25 The first authority should:
- notify the second authority of its intention to make a cross-border residential care placement
- provide a provisional date on which it intends for the individual concerned to commence their placement
- provide the second authority with details of the proposed provider
- seek that authority’s views on the suitability of the residential accommodation
21.26 The initial contact can be made by telephone, but should be confirmed in writing.
21.27 The second authority has no power to ‘block’ a residential care placement into its area as the first authority contracts directly with the provider. In the event of the second authority objecting to the proposed placement, all reasonable steps should be taken by the first authority to resolve the issues concerned before making the placement.
21.28 Following the initial contact and any subsequent discussions (and provided no obstacles to the placement taking place have been identified) the first authority should write to the second authority confirming the conclusions of the discussions and setting out a timetable of key milestones up to the placement commencing.
21.29 The first authority should inform the provider that the placement is proposed – in the same way as with any residential placement. The first authority should ensure that the provider is aware that this will be a cross-border placement.
21.30 The first authority should contact the individual concerned and/or their representative to confirm that the placement can go ahead and to seek their final agreement. The first authority should also notify any family/friends that the individual has given permission and/ or requested to be kept informed.
21.31 The first authority should make all those arrangements that it would normally make in organising a residential care placement in its own area.
Step 3: arrangements for ongoing management of placement
21.32 A key necessity is for the first authority to consider with the second authority, arrangements for the on-going management of the placement and assistance with the performance of relevant care and support functions.
21.33 The first authority will retain responsibility for the individual and the management and review of their placement. In this regard, the authority’s responsibilities to the individual are no different than they would be if the individual was placed with a provider in the authority’s own area.
21.34 However, it is recognised that the practicalities of day-to-day management of a placement potentially hundreds of miles distant from the authority may prove difficult.
21.35 As such, the first authority may wish to make arrangements for the second authority to assist with the day-to-day placement management functions for example where urgent in-person liaison is required with the provider and/or individual concerned, or with regular care reviews which are for the first authority to perform (in accordance with its statutory obligations), [footnote 86] but with which the second authority may be able to assist (for example, by gathering information necessary for the review and passing this to the first authority to make a decision).
21.36 It should be made clear that ultimate responsibility for exercising the functions remains with the first authority (they are obtaining assistance with the performance of these functions or, where applicable, authorising the exercise of functions on their behalf).
21.37 Any such arrangement should be detailed in writing – being clear as to what role the second authority is to play and for how long. Clarity should also be provided on the regularity of any reporting to the first authority and any payment involved for services provided by the second authority.
Step 4: confirmation of placement
21.38 When the placement has been confirmed, the first authority should notify the second authority and detail in writing all the arrangements made with the second authority for assistance with on-going placement management and other matters. The first authority should also confirm the date at which the placement will begin.
21.39 The second authority should acknowledge receipt of these documents/information and give its agreement to the arrangements in writing.
21.40 The first authority should provide the individual concerned and/or their representative with contact details (including whom to contact during an emergency) for both the first and second authority. If required, it is expected that the first authority will be responsible for organising suitable transport, and for the costs of it, to take the individual and their belongings to their new placement.
21.41 As would be the case normally, the first authority will normally be responsible for closing off previous placements or making other necessary arrangements regarding the individual’s prior residence.
Other issues to be considered during the organisation of a placement
Timeliness of organising and making a placement
21.42 Steps 1 to 4 should be conducted in a timely manner; the time taken should be proportionate to the circumstances.
Self-arranged placements
21.43 This guidance does not apply in relation to individuals who arrange their own care. Individuals who arrange and pay for their own care will normally become ordinarily resident in and/or the responsibility of the area to which they move. This guidance does apply to individuals who pay for their own care where that care (cross border placement) is arranged by an authority.
Issues that may arise once a placement has commenced
Where the individual requires a stay in NHS accommodation
21.44 Should the individual placed cross-border need to go into NHS accommodation for any period of time then this stay will not interrupt the position regarding ordinary residence or responsibility deemed under Schedule 1.
21.45 If, while the individual is in NHS accommodation, a ‘retention’ fee is payable to the care provider to ensure the individual’s place is secured, this will be the responsibility of the first authority.
Where the individual requires NHS-funded nursing care
21.46 Should the individual being placed require NHS-funded nursing care, the arrangements for delivering this should be discussed between the first authority, the NHS body delivering the care, the NHS body funding the care and the care provider prior to the placement commencing. Early (indeed advance) engagement with the NHS in such circumstances is important in ensuring smooth and integrated provision of services in cross-border placements. The NHS body (likely the Clinical Commissioning Group) responsible for paying for the care in cross-border placements will need to ensure it follows the procedure in the NHS standing rules, including considering whether the person in question qualifies for a higher level of care, for example, NHS Continuing Healthcare
21.47 Where the need for nursing care becomes evident after the placement has commenced, the relevant authorities should work together to ensure this is provided without delay.
21.48 The 4 administrations of the UK have reached separate bilateral agreements as to which administration shall bear the cost of NHS funded nursing care required for individuals placed cross-border into residential accommodation.
21.49 In the event of cross-border placements between England and Scotland or between England and Northern Ireland (in either direction) the health service of the country of the first authority will be responsible for nursing costs. (In England therefore, the individual’s responsible Clinical Commissioning Group will pay the costs.) The NHS standing rules have been amended to facilitate this. The first authority should inform the CCG of the arrangements being made and their formal consent sought. It is not expected that the CCG would withhold consent – any change in costs associated with the care would be likely to be negligible.
21.50 In the event of a cross-border placement between England and Wales (in either direction), the second authority’s health service will be responsible for the costs of NHS nursing care. However, in the event of a cross-border placement between Wales and Scotland, Wales and Northern Ireland, or between Scotland and Northern Ireland, the first authority’s health service will retain responsibility for the costs of NHS funded nursing care.
Where the individual’s care needs change during the placement
21.51 In the event that an individual’s care and support needs change during the course of the placement, these should be picked up in the course of a review and the care and support plan amended as needed.
21.52 The first authority retains responsibility for review and amendment of the individual’s care and support plan, although it may have agreed with the second authority that the latter will assist it in certain ways. In this case, clarity and communication will be important as to each authority’s roles (see chapter 13 for more information on reviews of care and support plans and chapter 18 for more information on delegation of local authority functions).
Handling complaints
21.53 If the complaint relates to the care provider, it should normally be made to the provider in the first instance and dealt with according to the complaints process of the provider as governed by the applicable legislation, which will normally be the legislation of the administration into which the individual has been placed.
21.54 If the complaint relates to NHS care, it should be dealt with according to the legislation governing such complaints in the relevant territory of the UK.
21.55 Complaints regarding the first authority should be dealt with by the first authority in accordance with the relevant legislation of that territory of the UK. As should complaints regarding the care and support plan. Complaints regarding the second authority should be dealt with by the second authority.
21.56 If referral to the health ombudsmen is necessary this should be made to the ombudsmen whose investigation the provider or authority in question is subject to, in accordance with the governing legislation. See subsequent section for how to deal with a dispute that might arise between 2 or more authorities.
Reporting arrangements
21.57 There is no legal requirement for authorities to notify national authorities that a cross-border placement has taken place. However, as UK-wide cross-border placements will generally be a new occurrence, it will be sensible to record the number of placements occurring to best inform future application of the policy. Therefore, authorities should record the number of placements made into their area from other territories of the UK and vice versa.
Disputes between authorities
21.58 If authorities have regard to and apply the suggested process and procedures outlined above and, more importantly, if the first and second authority work together in a spirit of reciprocity and cooperation and promptly communicate in order to ensure matters go smoothly, then there should be no need for dispute resolution. A dispute is most likely to occur because of lack of communication or following a communication breakdown/misunderstanding between first and second authority during the process of arranging the placement.
21.59 The 4 administrations of the UK have worked together on the contents of specific regulations governing the process of resolving a dispute. These regulations cover all disputes that arise about the application of paragraphs 1 to 4 of Schedule 1 to the Act (general non-transfer of responsibility in the case of placements).
21.60 The Regulations under Schedule 1 state:
- a dispute must not be allowed to prevent, interrupt, delay or otherwise adversely affect the meeting of an individual’s care and support needs [footnote 87]
- the authority in whose area the individual is living at the date the dispute arises is the lead authority for the purposes of duties relating to coordination and management of the dispute
21.61 In the event of a dispute between 2 authorities where the individual is living in the area of one of those authorities when the dispute is referred, the Ministers/Northern Ireland Department (NID) in whose jurisdiction that area lies would determine the dispute. In the event of other disputes between authorities, the Ministers/NID in whose jurisdiction those authorities sit would decide between themselves as to who would determine the dispute.
21.62 Before a dispute is referred to the relevant Ministers/NID, the authorities concerned must take a number of steps. These include the following. The lead authority must:
- co-ordinate the discharge of duties by the authorities in dispute
- take steps to obtain relevant information from those authorities
- disclose relevant information to those authorities
21.63 Authorities in dispute must:
- take all reasonable steps to resolve the dispute between themselves
- co-operate with each other in the discharge of their duties
21.64 Each authority in dispute must:
- engage in constructive dialogue with other authorities to bring about a speedy resolution
- comply with any reasonable request made by the lead authority to supply information
21.65 The regulations specify the requisite contents of a dispute referral as follows. When a dispute is referred, the following must be provided:
- a letter signed by the lead authority stating that the dispute is being referred and identifying the provision of the Act which the dispute is about
- a statement of the facts
- copies of related correspondence
21.66 The statement of facts must include:
- details of the needs of the individual to whom the dispute relates
- which authority, if any, has met those needs, how they have been met and the relevant statutory provision
- any relevant steps taken in relation to the individual
- an explanation of the nature of the dispute
- details of the individual’s place of residence and any former relevant residence
- chronology of events leading up to the referral
- details of steps authorities have taken to resolve dispute
- where the individual’s mental capacity is relevant, relevant supporting information
21.67 The authorities in dispute may make legal submissions and if they do, they must send a copy to the other authorities in dispute, and provide evidence that they have done so.
21.68 The Responsible Person (for example, Minister or Northern Ireland Department) to whom the dispute has been referred must:
- consult other responsible persons (for example, Ministers or Northern Ireland Department) in determining the dispute
- notify those responsible persons of their determination
Provider failure
21.69 In the event that a provider with which cross-border arrangements for an individual have been made or funded fails and is unable to carry on the care activity as a result, the authority in whose area that individual’s care and support needs were being met has duties to ensure those needs continue to be met for so long as that authority considers it necessary.
21.70 Close communication and cooperation between the first and second authority throughout will be important. The temporary duty to meet needs in the event of provider failure will apply to authorities in England and Northern Ireland but is not expected to apply to local authorities in Wales until April 2016.
21.71 In the event of provider failure in Scotland, local authorities are required to perform duties provided for under Part 2 of the Social Work (Scotland) Act 1968 as specified in regulations made by the Secretary of State under paragraphs 1(6) and (7), 2(9) and (10) and 4(5) and (6) of Schedule 1 to the Care Act 2014.
21.72 The Act enables the authority hosting the placement to recover costs from the authority which made or funded the arrangements. This power will be commenced in relation to local authorities in Wales at the same time as the temporary duty is commenced in relation to them.
21.73 If a dispute later emerges, for example regarding costs incurred as a result of the provider failure situation, then the Schedule 1 dispute regulations described above will apply.
Cross-border arrangements for other care settings
21.74 Schedule 1 covers cross border placements into care homes.
21.75 It also applies to a placement into England which consists of shared lives scheme accommodation or supported living accommodation (for example, where the second authority is in England).
21.76 It does not cover shared lives and supported-living arrangements made by a first authority in England for a placement into a second authority in Scotland, Wales or Northern Ireland.
21.77 Schedule 1 makes provision for regulation-making powers with respect to applying cross-border principles to accommodation provided by means of direct payments and/ or cases where services other than accommodation are arranged by a local authority.
21.78 The UK Government and the Devolved Administrations will be keeping under review the possibility of exercising these regulation-making powers, in light of the implementation of residential cross-border placements and policy developments across all UK administrations.
Case Study: Frances
Frances is a 78 year old lady with severe arthritis who lives alone in south London. Frances slips whilst walking down her stairs and breaks a wrist and leg. Frances is admitted to a local general hospital. At the hospital, Francis is visited by Ray, a local authority social services member, who conducts a needs assessment. During the assessment, Ray asks Frances about her support network – does she have any friends and/or family nearby? Frances says her best friend passed away last year. She has one son but he lives outside Edinburgh with his young family.
When Ray re-visits Frances, he informs her that she is eligible for care and support. He also says, that whilst a number of options exist, it is Ray’s opinion, that Frances’s severe arthritis now means she is unable to live independently and that a care home may be the best way forward. Frances agrees. She expresses relief that she will not have to return home alone but is anxious at moving to an unfamiliar setting.
Ray asks Frances whether she has considered moving to be nearer her son. Frances says yes, but has previously dismissed the idea because she didn’t want to get in the way. Ray asks whether a move to a care home near her son might be attractive. The local authority would take care of the arrangements and her son and his family could visit more easily. Frances is keen to take this further. Ray asks Frances’s permission to contact her son. Frances agrees.
Ray contacts Frances’s son, Ian. Ian says he wishes he could visit Frances more often but with 2 young children and a busy job it is hard to do so. Ian phones every few days and says he knows Frances has been feeling down since her friend passed away. Ian’s house is too small to accommodate Frances and is empty all day so no-one would be available to support Frances. Ray explains the possibility of a cross-border placement for Frances into a care home close to Ian. Ian says he would find this very attractive. Frances has always enjoyed her visits to Scotland before, especially seeing her grandchildren. Ian agrees to talk to Frances about the possibility.
Ray hears from Frances the next day – she and her son would like to go forward with a cross-border placement. Ray researches possible care homes close to Ian, taking Frances’s preferences into account and selects 3 possibilities which Frances, in conference with Ian, pick from. The preferred home is in a suburban area similar to that in which Frances currently lives and close to a church – Frances is a regular church-goer. Ray contacts the care home provider and confirms availability and fees and informs the provider that this would be a cross-border placement.
Ray phones his opposite number, Rhian, in the Edinburgh local authority where the care home is based. Ray informs Rhian that it appears likely a cross-border placement will take place. Rhian says she knows the care home in question and the standard of care is good based on inspectorate findings. Ray thanks her and follows up in writing with the provisional date when the placement will occur and details of the care provider identified. Over the next week, arrangements for the placement are firmed up. Ray draws up an agreement as to how Frances’s care will be managed on a day-to-day basis with assistance from Rhian’s authority. Rhian has agreed that her local authority will take on several roles including providing assistance and information so that the local authority can fulfil its responsibilities. Rhian’s team agree to help to carry out regular care reviews by gathering and reporting information back to Ray’s local authority as ultimate decision-maker. Rhian also agrees that her local authority will provide support in an emergency situation.
Other areas
This section contains chapter:
22. Sight registers
This chapter provides guidance on:
- section 77 of the Care Act 2014
- The Care and Support (Registers) Regulations 2014
This chapter covers:
- registration
- certification
- transferring and retaining the certificate of vision impairment (cvi)
- making contact
- continuity of care
- care planning
- rehabilitation
- care and support for deafblind children and adults
- other registers
22.1 Local authorities must keep a register of people who are severely sight impaired and sight impaired.
22.2 Registration is voluntary, however individuals should be encouraged to consent to inclusion on the register as it may assist them in accessing other concessions and benefits. The data which local authorities are provided on registration are also of benefit in service planning for health and care and support. However, individuals’ access to care and support is not dependent upon registration, and those with eligible needs for care and support should continue to receive it regardless of whether they consent to inclusion on the register.
22.3 Local authorities should help health and social care organisations to work together to meet the needs of people who have sight loss, for example, ensuring that care and support services know what help somebody needs in their home when they leave hospital. Timely assessment and care and support that is integrated with health care and person-centred offer the potential to make improvements in experience and outcomes of people who are sight impaired, as well as improving system efficiency.
Registration
22.4 Local authorities must keep a register of people who are severely sight impaired and sight impaired. Local authorities may wish to use this opportunity to bring forward information from existing registers and update details, for example, to check if the information on the register is still current, for example a person may have moved out of the area. If the person consents to registration they will be included on the local authority’s register and be provided with a registration card. The registers can also be used by the local authority to ensure that information about services is made accessible to that person for example to ask if support could be given to assist them to participate in electoral events.
22.5 The Certificate of Vision Impairment (CVI) formally certifies someone as being sight impaired or as severely sight impaired. Where the patient has given their consent, a copy of the CVI should be sent to the relevant local authority by the hospital staff. However, people in receipt of a CVI should not be added to the local register until they have given their specific consent to the local authority for registration. If the person has given consent he or she may then be registered. Local authorities may take the date of certification given on the CVI as the effective date of registration. However, if consent has not been given, the person should still be offered a needs assessment.
22.6 The CVI is an important source of information for local authorities in relation to their registration duties. Local authorities should satisfy themselves that the CVI is completed correctly and it contains valid signatures as required (currently the consultant ophthalmologist and the patient) when receiving a hard copy of the form. Electronic versions and paper copies of CVIs should be accepted for registration.
22.7 People who agree to be registered may be entitled to some benefits, for example, an increase in personal tax allowance, a reduction in the cost of a TV license, a free bus pass and parking concessions under the Blue Badge Scheme. It is important that strong links exist between local authorities, health services and voluntary organisations to identify those who may benefit from registration.
Vision Strategy
22.8 Schedule 2 of the 1989 Children Act requires local authorities to keep registers of disabled children, which must include children with sight impairments.
Certification
22.9 The CVI is issued by a consultant ophthalmologist to the patient certifying as sight impaired or severely sight impaired. The DH guidelines in the Certificate of Vision Impairment: Explanatory Notes for Consultant Ophthalmologists and Hospital Eye Clinic Staff states who should be certified as severely sight impaired and sight impaired.
22.10 Certification is not the final stage, but often it is the point when people begin to accept the severity of their sight loss and get access to practical and emotional support.
22.11 It is expected that NHS services will keep the completed certificate, signed by the consultant and the patient, for their records. Where the patient has given their consent, a copy of the certificate should be sent to the relevant local authority and the patient’s GP within 5 working days of its completion. The ‘Certificate of Vision Impairment Explanatory Notes for Consultant Ophthalmologists and Hospital Eye Clinic Staff provides information on this.
22.12 The Public Health Outcomes Framework (Domain 4: Healthcare public health and preventing premature mortality) has the overarching objective to reduce numbers of people living with preventable ill health and people dying prematurely and has the ‘preventable sight loss’ indicator. The CVI is the key data source for the preventable sight loss indicator and, where the patient has given their consent, a copy of the form is also sent to Moorfields Eye Hospital for epidemiological analysis of cases where sight loss is due to age-related macular degeneration, glaucoma, diabetic retinopathy and any other cause.
22.13 The Certifications Office at Moorfields Eye Hospital receives the CVIs from hospitals across England and Wales for anonymised analysis by age, sex, visual status, location and ethnicity. These figures are reported to Public Health England so for example diabetic screening programmes can monitor the numbers of newly certified people in their areas with potentially avoidable eye disease. NHS Digital (previously the Health and Social Care Information Centre) will be issuing their latest report on certification data covering the period 1 April 2016 to 31 March 2017 in the latter part of 2017.
22.14 Local authorities should note that there will also be people who have a reduced/low vision but do not meet the criteria for certification who may need to be considered in service planning.
Transferring and retaining the CVI
22.15 The CVIs should be kept until the person moves to another area or has passed away. In the event of a person’s death, the local authority should keep the CVI for at least 3 years after the person’s death as it may be necessary for tax purposes to establish if a deceased person was registered with a local authority.
Making contact
22.16 Upon receipt of the CVI, the local authority should make contact with the person issued with the CVI within 2 weeks to arrange their inclusion on the local authority’s register (with the person’s informed consent) and offer individuals a registration card as identified on the CVI registration form. Where there is an appearance of need for care and support, local authorities must arrange an assessment of their needs in a timely manner.
22.17 To minimise unnecessary costs and maximise the ability of people who have sight impairment, they should have early access to information and advice in an accessible format so that they can adapt to their situation as quickly as possible and obtain any aids and support that will help them to manage their lives better.
Continuity of care
22.18 A person may decide to move home and live in another local authority area. In such circumstances local authorities must follow the process which is set out in chapter 20. This is aimed at ensuring that the person’s care and support needs will continue to be met during their move. The process requires the original authority to provide the authority the person is moving to with relevant information to support the move such as a copy of the person’s care and support plan, their latest assessment, and any other documentation the second authority requests. This should include a copy of their CVI. The second authority should register the person with the person’s consent on their register, and the former authority should remove that person’s name to avoid duplication.
Care planning
22.19 Providing excellent services for blind and partially sighted people – A guide for local authorities, published by Royal National Institute for Blind People (RNIB) and Action for Blind People, is a good practice guide that helps inform local authorities’ understanding of the extent and impact of sight impairment, the main causes and risk factors and the effects on people’s lives.
22.20 A vital part of modern care and support is the care and support plan. Having carried out a needs assessment, local authorities must prepare a care and support plan for everyone with eligible needs or other needs which the local authority is going to meet. Where someone has sight loss, this should be recorded in the care and support plan. Further details are set out in chapter 10 of this guidance. Rehabilitation
22.21 Local authorities should consider securing specialist qualified rehabilitation and assessment provision (whether in-house, or contracted through a third party), to ensure that the needs of people with sight loss are correctly identified and their independence maximised. Certain aspects of independence training with severely sight impaired and sight impaired people require careful risk management and should only be undertaken by professionals with relevant experience and training. This type of rehabilitation should be provided to the person for a period appropriate to meet their needs. This will help the person to gain new skills, for example, when training to use a white cane. As aspects of rehabilitation for people with sight loss are distinct from reablement, refer to the Association of Directors of Adults Social Services’ (ADASS) position statement of December 2013.
22.22 This makes it clear that rehabilitation for sight impaired people is a specific form of reablement. However, there are some intrinsic characteristics which define rehabilitation as being distinct from other forms of reablement. It is therefore not appropriate to take a one-size-fits-all approach, and local authorities need to ensure that individual needs are met appropriately.
Care and support for Deafblind children and adults
22.23 This guidance relates to adults with sight impairment only. Guidance in relation to care and support for deafblind children and adults is issued separately under different legal powers, and should be considered in parallel.
Other registers
22.24 Local authorities may also establish and maintain a register of people living in their area that have a disability (a physical or mental impairment which has a substantial and long-term adverse effect on their ability to carry out normal day-to-day activities) or who need care and support or are likely to do so in the future.
22.25 Inclusion on registers is voluntary and with the individual’s informed consent. However local authorities should encourage individual’s consent to inclusion on the register as such registers may support the establishment of an accurate and useful local record of people whose needs may change over time, for example:
- someone with a progressive long-term condition whose needs may increase over time
- when the person on whom they are mainly dependent for their care has stopped providing care
- those who are ordinarily resident but may be receiving temporary care and support out of area, or in-patient treatment in health services, but who are likely to require care and support on their discharge or return
22.26 For information on ordinary residence and out of area placements see chapter 19 of this guidance. This information can help local authorities to plan and commission services appropriately for those who need or are anticipated in the future to need care and support. This information could be useful, for example, in helping the local authority to meet its obligation to take steps to prevent reduce or delay needs, which requires local authorities to consider the importance of identifying adults whose needs are not being met and to arrange the provision of local preventative services, facilities and resources for its population. It may also support the local authority to undertake its ‘market shaping’ function, which requires the local authority to consider identifying current and future needs and how providers might meet that demand. For further detail see chapter 4 of this guidance.
22.27 Local authorities may wish to link the information collected to the Joint Strategic Needs Assessments (JSNAs) as well as the Joint Health and Wellbeing Strategies. They may also, as part of local JSNA and Health and Wellbeing Strategy development, want to look at this information alongside complementary information from other partners, for example, information drawn appropriately from registers of people with learning disabilities or particular health conditions which are held by GPs, in order to produce a comprehensive and accurate shared local picture.
Links to other relevant guidance and documentation
- the benefits of registering as blind or partially sighted (PDF, 157KB)
- Adult UK sight loss pathway
- ADASS position statement on visual impairment rehabilitation in the context of personalisation
- DH guidelines in Certificate of Vision Impairment: Explanatory Notes for Consultant Ophthalmologists and Hospital Eye Clinic Staff
- Health and Social Care Information Centre (HSCIC) publishes the number of people registered with councils with Adult Social Services Responsibilities in England
- Seeing it my way is a universal quality and outcomes framework for the information, advice and practical support that people with sight loss have identified as most important to them.
Annexes
This section contains:
- Annex A: Choice of accommodation and additional payments
- Annex B: Treatment of capital
- Annex C: Treatment of income
- Annex D: Recovery of debts
- Annex E: Deprivation of assets
- Annex F: Temporary and short-term residents in care homes
- Annex G: The process for managing transfers of care from hospital for patients with care and support needs
- Annex H: Ordinary residence
- Annex I: Repeals and revocations
- Annex J:Glossary
Annex A: Choice of accommodation and additional payments
This annex covers:
- choice of accommodation when arranging care and support in an accommodation setting
- making additional payments for preferred accommodation
1) A person’s ability to make an informed choice is an important element of the care and support system. This must extend to where the care and support planning process has determined that a person needs to live in a specific type of accommodation to meet their care and support needs.
2) The care and support planning process will have determined what type of accommodation will best suit the person’s needs. This could be, for example, a care home, shared lives or extra care housing. Where the type of accommodation is one of those specified in regulations, the person will have a right to choose the particular provider or location, subject to certain conditions. Where this is the case, the following guidance should be applied and in doing so, local authorities should have regard to the following principles:
- good communication of clear information and advice to ensure well informed decisions
- a consistent approach to ensure genuine choice
- clear and transparent arrangements for choice and any ‘top-up’ arrangements
- clear understanding of potential consequences should ‘top-up’ arrangements fail with clear exit strategies
- the choice is suitable to the person’s needs
3) Local authorities must also remember that the regulations and guidance on choice of accommodation and additional costs apply equally to those entering care for the first time, those who have already been placed by a local authority, and those who have been self-funders, but because of diminishing resources are on the verge of needing local authority support.
4) Local authorities should also be mindful of their duties under Section 1 of the Care Act 2014 to promote individual wellbeing. Further detail is available in Chapter 1.
Choice of accommodation
5) Where a local authority is responsible for meeting a person’s care and support needs and their needs have been assessed as requiring a particular type of accommodation in order to ensure that they are met, the person must have the right to choose between different providers of that type of accommodation provided that:
- the accommodation is suitable in relation to the person’s assessed needs
- to do so would not cost the local authority more than the amount specified in the adult’s personal budget for accommodation of that type
- the accommodation is available
- the provider of the accommodation is willing to enter into a contract with the local authority to provide the care at the rate identified in the person’s personal budget on the local authority’s terms and conditions
6) This choice must not be limited to those settings or individual providers with which the local authority already contracts with or operates, or those that are within that local authority’s geographical boundary. It must be a genuine choice across the appropriate provision.
7) If a person chooses to be placed in a setting that is outside the local authority’s area, the local authority must still arrange for their preferred care. In doing so, the local authority should have regard to the cost of care in that area when setting a person’s personal budget. Local authorities should also read the guidance on ordinary residence in chapter 19.
Suitability of accommodation
8) In exercising a choice, a local authority must ensure that the accommodation is suitable to meet a person’s assessed needs and identified outcomes established as part of the care and support planning process.
9) People are able to express a preference about the setting in which their needs are met through the care and support planning process. This process considers both the person’s needs and preferences and detailed guidance is set out in Chapter 10. Once this is agreed, the choice is between different settings, not different types. For example, a person cannot exercise the right to a choice of accommodation to choose a shared lives scheme when the care and support planning process, which involves the person, has assessed their needs as needing to be met in a care home.
Cost
10) The care and support planning process will identify how best to meet a person’s needs. As part of that, the local authority must provide the person with a personal budget, except in cases or circumstances set out in the Care Act (Personal Budget) Regulations. The Personal Budget is an important tool that provides clear information on the cost of meeting the person’s needs. Further guidance on how to undertake care and support planning and calculate a personal budget is set out in Chapters 10 and 11.
11) The personal budget is defined as the cost to the local authority of meeting the person’s needs which the local authority chooses or is required to meet. However, the local authority should take into consideration cases or circumstances where this ‘cost to the local authority’ may need to be adjusted to ensure that needs are met. For example, a person may have specific dietary requirements that can only be met in specific settings. In all cases the local authority must have regard to the actual cost of good quality care in deciding the personal budget to ensure that the amount is one that reflects local market conditions. This should also reflect other factors such as the person’s circumstances and the availability of provision. In addition, the local authority should not set arbitrary amounts or ceilings for particular types of accommodation that do not reflect a fair cost of care. Guidance on market shaping and commissioning is set out in Chapter 4. Local authorities must also have regard to the guidance on personal budgets in Chapter 11, and in particular paras. 11.22-11.24 on calculating the personal budget.
12) A person must not be asked to pay a ‘top-up’ towards the cost of their accommodation because of market inadequacies or commissioning failures and must ensure there is a genuine choice. The local authority therefore must ensure that at least one option is available that is affordable within a person’s personal budget and should ensure that there is more than one. If no preference has been expressed and no suitable accommodation is available at the amount identified in a personal budget, the local authority must arrange care in a more expensive setting and adjust the budget accordingly to ensure that needs are met. In such circumstances, the local authority must not ask for the payment of a ‘top-up’ fee. Only when a person has chosen a more expensive accommodation can a ‘top-up’ payment be sought. Paras. 20 and 21 set out guidance on additional costs.
Availability
13) Local authorities have specific duties to shape and facilitate the market of care and support services locally, including ensuring sufficient supply. As a result, a person should not have to wait for their assessed needs to be met. However, in some cases, a short wait may be unavoidable, particularly when a person has chosen a particular setting that is not immediately available. This may include putting in place temporary arrangements – taking in to account the person’s preferences and securing their agreement – and placing the person on the waiting list of their preferred choice of provider for example. It should be remembered however that such arrangements can be unsettling for the person and should be avoided wherever possible.
14) In such cases, the local authority must ensure that in the interim adequate alternative services are provided and set out how long the interim arrangement may last for. In establishing any temporary arrangements, the local authority must provide the person with clear information in writing on the detail of the arrangements as part of their care and support plan. As a minimum this should include the likely duration of the arrangement, information on the operation of the waiting list for their preferred setting alongside any other information that may be relevant. If any interim arrangements exceed 12 weeks, the person may be reassessed to ensure that both the interim and the preferred option are still able to meet the person’s needs and that remains their choice.
15) Where a person contributes to the cost of their care following a financial assessment they must not be asked to pay more than their assessment shows they can afford.
16) In some cases a person may decide that they wish to remain in the interim setting, even if their preferred setting subsequently becomes available. If the setting where they are temporarily resident is able to accommodate the arrangement on a permanent basis this should be arranged and they should be removed from the waiting list of their original preferred setting. Before doing so, the local authority must make clear the consequences of that choice, including any financial implications.
Choice that cannot be met and refusal of arrangements
17) Whilst a local authority should do everything it can to meet a person’s choice, inevitably there will be some instances where a choice cannot be met, for example if the provider does not have capacity to accommodate the person. In such cases, a local authority must set out in writing why it has not been able to meet that choice and should offer suitable alternatives. It should also set out the detail of the local authority’s complaints procedure and if and when the decision may be reviewed.
18) A local authority must do everything it can to take into account a person’s circumstances and preferences when arranging care. However, in all but a very small number of cases, such as where a person is being placed under guardianship under Section 7 of the Mental Health Act 1983, a person has a right to refuse to enter a setting whether that is on an interim or permanent basis. Where a person unreasonably refuses the arrangements, a local authority is entitled to consider that is has fulfilled its statutory duty to meet needs and may then inform the person in writing that as a result they need to make their own arrangements. This should be a step of last resort and local authorities should consider the risks posed by such an approach, for both the authority itself and the person concerned. Should the person contact the local authority again at a later date, the local authority should reassess the needs as necessary and re-open the care and support planning process.
Contractual terms and conditions
19) In supporting a person’s choice of setting, the local authority may need to enter into a contract with a provider that they do not currently have an arrangement with. In doing so, they should ensure that the contractual conditions are broadly the same as those they would negotiate with any other provider whilst taking account of the individual circumstances. Strict or unreasonable conditions should not be used as a means to avoid or deter the arrangement.
Additional costs or ‘top-up’ payments
20) In some cases, a person may actively choose a setting that is more expensive than the amount identified for the provision of the accommodation in the personal budget. Where they have chosen a setting that costs more than this, an arrangement will need to be made as to how the difference will be met. This is known as an additional cost or ‘top-up’ payment and is the difference between the amount specified in the personal budget and the actual cost. In such cases, the local authority must arrange for them to be placed there, provided a third party, or in certain circumstances the person in need of care and support, is willing and able to meet the additional cost.
21) The following sections of guidance only apply where the person has chosen a more expensive setting. Where someone is placed in a more expensive setting solely because the local authority has been unable to make arrangements at the anticipated cost, the personal budget must reflect this amount. The person would then contribute towards this personal budget according to the financial assessment. The additional cost provisions must not apply in such circumstances.
Agreeing a ‘top-up’ fee
22) Having chosen a setting that is more expensive, based on good information and advice, the local authority should ensure that the person understands the full implications of this choice, remembering that this is often a point of crisis. This should include for example that a third party, or in certain circumstances the person needing care and support, will need to meet the additional cost of that setting for the full duration of their stay and that should the additional cost not be met they may be moved to an alternative setting.
23) The local authority must ensure that the person paying the ‘top-up’ is willing and able to meet the additional cost for the likely duration of the arrangement, recognising that this may be for some time into the future. Therefore it must ensure that the person paying the ‘top-up’ enters into a written agreement with the local authority, agreeing to meet that cost. The agreement must, as a minimum, include the following:
- the additional amount to be paid
- the amount specified for the accommodation in the person’s personal budget
- the frequency of the payments
- to whom the payments are to be made
- provisions for reviewing the agreement
- a statement on the consequences of ceasing to make payments
- a statement on the effect of any increases in charges that a provider may make
- a statement on the effect of any changes in the financial circumstances of the person paying the ‘top-up’
24) Before entering into the agreement, the local authority must provide the person paying the ‘top-up’ with sufficient information and advice to ensure that they understand the terms and conditions, including actively considering the provision of independent financial information and advice. Further detail on each of these points is set out below.
25) Ultimately, if the arrangements for a ‘top-up’ were to fail for any reason, the local authority would need to meet the cost or make alternative arrangements, subject to a needs assessment. Further details are set out below in the consequences of ceasing to make payments. Local authorities should therefore maintain an overview of all ‘top-up’ agreements and should deter arrangements for ‘top-up’ payments to be paid directly to a provider.
The amount to be paid
26) The amount of the ‘top-up’ should be the difference between the actual costs of the preferred provider and the amount that the local authority would have set in a personal budget or local mental health after-care limit to meet the person’s eligible needs by arranging or providing accommodation of the same type. When considering the cost of care in its area, the local authority is likely to identify a range of costs which apply to different circumstances and settings. For the purposes of agreeing a ‘top-up’ fee the local authority must consider what personal budget it would have set at the time care and support is needed. It should not automatically default to the cheapest rate or to any other arbitrary figure.
Frequency of payments
27) In agreeing any ‘top-up’ arrangement, the local authority must clearly set out how often such payments need to be made, for example, on a weekly or monthly basis.
Responsibility for costs and to whom the payments are made
28) When entering into a contract to provide care in a setting that is more expensive than the amount identified in the personal budget, the local authority is responsible for the total cost of that placement. This means that if there is a break down in the arrangement of a ‘top-up’, for instance if the person making the ‘top-up’ ceases to make the agreed payments, then the local authority would be liable for the fees until it has either recovered the additional costs it incurs or made alternative arrangements to meet the cared for person’s needs.
29) In terms of securing the funds needed to meet the total cost of the care (including the ‘top-up’ element) a local authority has 3 options, except where it is being funded by a deferred payment agreement, in which case it is added to the amount owed. In choosing which option to take it will need to consider the individual circumstances of the case, and should be able to assure itself of the security of the arrangements and that there is no undue pressure on the person making the ‘top-up’ payment to increase the level of payment. Whichever option it chooses, it remains responsible for the total amount. The 3 options are:
- treat the ‘top-up’ payment as part of the person’s income and therefore recover the costs from the person concerned through the financial assessment (where the ‘top-up’ payments are being made by a third party rather than the cared for person, this is on the assumption that the third party makes the payment to the person with care needs)
- agree with the person, the third party paying the ‘top-up’ (if this is not the cared for person) and the provider that payment for the ‘top-up’ element can be made directly to the provider with the local authority paying the remainder. However, as stated earlier, this is not recommended.
- the person making the ‘top-up’ payments pays the ‘top-up’ amount to the local authority. The local authority then pays the full amount to the provider
30) In the cas of people with eligible needs who pay in full for their own care and support who asks the local authority to arrange their care, refer to paragraph 41.
Provisions for reviewing the agreement
31) As with any financial arrangement, an agreement to make a ‘top-up’ payment must be reviewed. A local authority must set out in writing details of how the arrangements will be reviewed, what may trigger a review, and circumstances when any party can request a review.
32) Local authorities should also consider how often it may be appropriate to review the arrangements. In doing so it should bear in mind how often it reviews other financial arrangements, such as deferred payment agreements. These should take place at least annually and in line with wider reviews of the financial assessment.
Consequences of ceasing to make payments
33) The local authority must make clear in writing the consequences should there be a break down in the arrangement to meet the cost of the ‘top-up’. This should include that the person may be moved to an alternative accommodation where this would be suitable to meet their needs and affordable within the personal budget or local mental health after-care limit. As with any change of circumstance, a local authority must undertake a new assessment before considering this course of action, including consideration of a requirement for an assessment of health needs, and have regard to the person’s wellbeing.
Price increases
34) Arrangements will need to be reviewed from time to time, for example in response to any changes in circumstances of the cared for person, the person making the ‘top-up’ payments (if this is different from the cared for person), local authority commissioning arrangements or a change in provider costs. However, these changes may not occur together and a local authority must set out in writing how these changes will be dealt with.
35) The local authority must clearly set out in writing to the person or persons concerned its approach to how any increased costs may be shared. This should also include details of how agreement will be reached on the sharing of any price increases. This should also state that there is no guarantee that these increased costs will automatically be shared evenly should the provider’s costs rise more quickly than the amount the local authority would have increased the personal budget or local mental health after-care limit and there is an alternative option that would be affordable within that budget.
36) A local authority may wish to negotiate any future prices rises with the provider at the time of entering into a contract. This can help provide clarity for adults and providers and help ensure that the top up remains affordable.
37) The local authority should also make clear that where the person has a change in circumstances that requires a new financial assessment and this results in a change in the level of contribution the person themself makes, this may not reduce the need for a ‘top-up’ payment.
Consequences of changes in circumstances of the person making the ‘top-up’ payment
38) The person making the ‘top-up’ payment could see an unexpected change in their financial circumstances that will impact their ability to continue to pay the ‘top-up’ fee. Where a person is unable to continue making ‘top-up’ payments, the local authority may seek to recover any outstanding debt and has the power to make alternative arrangements to meet a person’s needs, subject to a needs assessment. The local authority must set out in writing how it will respond to such a change and what the responsibilities of the person making the ‘top-up’ payment are in terms of informing the local authority of the change in circumstances.
First party ‘top ups’
39) The person whose needs are to be met by the accommodation may themselves choose to make a ‘top-up’ payment only in the following circumstances:
- where they are subject to a 12-week property disregard (See chapter 8 on Charging)
- where they have a deferred payment agreement in place with the local authority. Where this is the case, the terms of the agreement should reflect this arrangement. For further guidance on deferred payment agreements see Chapter 9.
- where they are receiving accommodation provided under S117 for mental health aftercare
People who are unable to make their own choice
40) There will be cases where a person lacks capacity to express a choice for themselves. Local authorities should therefore act on the choices expressed by the person’s advocate, carer or legal guardian in the same way they would on the person’s own wishes, unless in the local authority’s opinion it would be against the best interests of the person.
Self-funders who ask the local authority to arrange their care
41) The Care Act 2014 enables a person who can afford to pay for their own care and support in full to ask the local authority to arrange their care on their behalf. Where the person requires care in a care home to meet their needs, the local authority may choose to respond to the person’s request by meeting their needs. Where the person requires some other type of care, including other types of accommodation to which the right to a choice applies, the local authority must meet those needs. In such circumstances, whether because the authority chooses to meet needs in a care home, or is required to meet needs in some other type of accommodation, the same rules on choice must apply.
42) In supporting self-funders to arrange care, the local authority may choose to enter into a contract with the preferred provider, or may broker the contract on behalf of the person. Where the local authority is arranging and managing the contract with the provider, it should ensure that there are clear arrangements in place as to how the costs will be met, including any ‘top-up’ element.
43) Ultimately, the local authority should assure itself that robust contractual arrangements are in place in such circumstances that clearly set out where responsibilities for costs lie and ensure that the person understands those arrangements. Self-funders will have to pay for the costs of their care and support including, in cases where they choose a setting that is more expensive than the amount identified in their personal budget, the top-up element of the costs of that setting.
Choice of accommodation and mental health after-care
44) Regulations made under section 117A of the Mental Health Act 1983 enable persons who qualify for after-care under section 117 to express a preference for particular accommodation if accommodation of the types specified in the regulations is to be provided as part of that after-care. Local authorities are required to provide or arrange the provision of the preferred accommodation if the conditions in the regulations are met.
45) The regulations give people who receive mental health after-care broadly the same rights to choice of accommodation as someone who receives care and support under the Care Act 2014. But some differences arise because after-care is provided free of charge and, as the legislative requirement for a care and support plan under the Care Act 2014 does not apply to section 117 after-care, the care plan should instead be drawn up under guidance on the Care Programme Approach (CPA). Care planning under the CPA should, if accommodation is an issue, include identifying the type of accommodation which is suitable for the person’s needs and affording them the right to choice of accommodation set out in the regulations made under section 117A. The person should be fully involved in the care planning process.
46) An adult has the right to choose accommodation provided that:
- the preferred accommodation is of the same type that the local authority has decided to provide or arrange
- it is suitable for the person’s needs
- it is available (see guidance in paras. 13-16) for mental health after-care purposes (‘assessed needs’ means needs identified in the CPA care plan)
- where the accommodation is not provided by the local authority, the provider of the accommodation agrees to provide the accommodation to the person on the local authority’s terms (see guidance in para. 18)
47) The principles in paras. 5, 6, 7 and 40 apply equally where a local authority is providing, or arranging the provision of, accommodation in discharge of its after-care duty. The guidance in paras. 17 and 18 applies when the preferred choice cannot be met.
48) Where the cost of the person’s preferred accommodation is more than the local authority would provide in a personal budget or local mental health after-care limit to meet the person’s needs, then the local authority must arrange for them to be placed there, provided that either the person or a third party is willing and able to meet the additional cost.
49) The guidance in paras. 20 to 38 applies where the adult has chosen more expensive accommodation. For the purposes of section 117 after-care, however, references to a third party should be read as including the adult receiving the after-care (because an adult can also meet the additional cost when a local authority is providing, or arranging for the provision of accommodation in discharge of the after-care duty).
50) In securing the funds needed to meet the additional cost, one of the following will apply:
- a local authority may agree with the person and the provider, and in cases where a third party is paying the ‘top-up’, agree with that third party, that payment for the additional cost can be made directly to the provider with the local authority paying the remainder
- the person or the third party pays the ‘top-up’ amount to the local authority. The local authority then pays the full amount to the provider
Information and advice
51) For individuals to be able to exercise genuine choice they need information about the options open to them. They should be given clear and balanced information with which to make the best choice of accommodation. The local authority should explain to individuals their rights under the Care Act. Individuals should be told explicitly that they may allow the local authority to make a decision about accommodation on their behalf, or, if they wish, they are free to choose any accommodation subject to the constraints set out in the regulations.
52) Under Section 4 of the Care Act 2014 a local authority must establish and maintain a service for providing people in its area with information and advice in relation to care and support. This must include information and advice about the different care providers available in the local area to enable choice as well as information and advice to help people to understand care charges, different ways to pay and money management. Local authorities should also have a role in facilitating access to financial information and advice provided independently of the local authority, including regulated information and advice where appropriate; to support people in making informed financial decisions. This may be particularly appropriate when a person is considering paying a top-up to help them to understand what they would be paying the top-up for and come to a judgment about whether it would represent good value for money.
53) Where a ‘top-up’ arrangement is being entered in to, all parties should fully understand their responsibilities, liabilities and the consequences of the arrangements. A local authority must provide the third party with sufficient information and advice to support them to understand the terms of the proposed written agreement before entering in to it. Local authorities must also have regard to the general guidance on Information and Advice set out in Chapter 3.
Complaints
54) Complaints about how choice or any ‘top-up’ arrangement is exercise by the local authority fall within the scope of the local authority’s statutory complaints procedure.
Annex B: Treatment of capital
This annex covers:
The treatment of capital when conducting a financial assessment in all circumstances.
1) This section of the guidance applies where a local authority has chosen to charge a person for the services it is arranging and therefore must undertake a financial assessment. When doing so, it must assess the income and capital of the person. This annex covers the treatment of capital and should be read in conjunction with Annex C on the treatment of income. The details of the sources capital which local authorities must disregard are set out in regulations.
2) The financial assessment will need to look across all of a person’s assets – both capital and income – decide which is capital and which is income, and assess those assets according to the regulations and guidance. A local authority therefore must also refer to Annex C on the treatment of income and Annex E on deprivation of assets before conducting a financial assessment. The treatment of income will vary depending on the type of setting a person is receiving care in. The treatment of capital, as set out in this annex, is broadly the same for all settings. Where there is a distinction between care homes and all other settings, this is clearly set out.
3) In assessing what a person can afford to contribute a local authority must apply the upper and lower capital limits. The upper capital limit is currently set at £23,250 and the lower capital limit at £14,250.
4) A person with assets above the upper capital limit will be deemed to be able to afford the full cost of their care. Those with capital between the lower and upper capital limit will be deemed as able to make a contribution, known as ‘tariff income’, from their capital. Any capital below the lower capital limit should be disregarded. Further details are set out in paras. 24 to 27.
Defining capital
What is capital?
5) Capital can mean many different things and the intention is not to give a definitive definition here as a local authority will need to consult the regulations and consider the individual asset on its merits. In general it refers to financial resources available for use and tends to be from sources that are considered more durable than money in the sense that they can generate a return.
6) The following list gives examples of capital. This list is intended as a guide and is not exhaustive:
- (a) buildings
- (b) land
- (c) National Savings Certificates and Ulster Savings Certificates
- (d) Premium Bonds
- (e) stocks and shares
- (f) capital held by the Court of Protection or a Deputy appointed by that Court
- (g) any savings held in:
- (i) building society accounts
- (ii) bank current accounts, deposit accounts or special investment accounts. This includes savings held in the National Savings Bank, Girobank and Trustee Savings Bank.
- (iii) SAYE schemes
- (iv) unit trusts
- (v) co-operatives share accounts.
- (vi) cash
- h) trust funds
7) It is important that people are not charged twice on the same resources. Therefore, resources should only be treated as income or capital but not both. If a person has saved money from their income then those savings should normally be treated as capital. However they should not be assessed as both income and capital in the same period. Therefore in the period when they are received as income, the resource should be disregarded as capital.
Cases where it is not clear whether a payment is capital or income
8) In assessing a person’s assets it may not be immediately clear where a resource is capital or income, particularly where a person is due to receive planned payments. In order to guide a local authority’s decision, in general, a planned payment of capital is one which is:
- (a) not in respect of a specified period
- (b) not intended to form part of a series of payments
9) Local authorities should also have regard to the guidance on capital treated as income at paragraph 55.
Who owns the capital?
10) A capital asset is normally defined as belonging to the person in whose name it is held, the legal owner. However in some cases this may be disputed and/or beneficial ownership argued. Beneficial ownership is where someone enjoys the benefits of ownership, even though the title of the asset is held by someone else or where they directly or indirectly have the power to vote or influence a transaction regarding a particular asset. In most cases the person will be both the legal and beneficial owner.
11) Where ownership is disputed, a local authority should seek written evidence to prove where the ownership lies. If a person states they are holding capital for someone else, the local authority should obtain evidence of the arrangement, the origin of the capital and intentions for its future use and return to its rightful owner.
Example of capital dispute: 1
Arlene has £14,000 in a building society account in her own name. She says that £3,000 is set aside for her granddaughter’s education. Unfortunately there is no deed of trust or other legal arrangement which would prevent Arlene using the whole amount herself. She is therefore treated as the beneficial owner of the whole amount.
Example of capital dispute: 2
Lisa has £10,000 in a bank account in her own name and shares valued at £6,500. She provides evidence to show that the shares were purchased on behalf of her son who is abroad and that they will be transferred to her son when he returns to the UK. Although Lisa is the legal owner, she is holding the shares in trust for her son who is the beneficial owner. Only the £10,000 is therefore treated as Lisa’s capital.
12) Where a person has joint beneficial ownership of capital, except where there is evidence that the person own an unequal share, the total value should be divided equally between the joint owners and the person should be treated as owning an equal share. Once the person is in sole possession of their actual share, they can be treated as owning that actual amount.
13) In some cases a person may be the legal owner of a property but not the beneficial owner of a property. In other words, they have no rights to the proceeds of any sale. In such circumstances the property must not be taken into account.
Calculating the value of capital
14) A local authority will need to work out what value a capital asset has in order to take account of it in the financial assessment. Other than National Savings Certificates, valuation must be the current market or surrender value of the capital asset, for example, property, whichever is higher, minus the following:
- (a) 10% of the value if there will be any actual expenses involved in selling the asset. This must be expenses connected with the actual sale and not simply the realisation of the asset. For example the costs to withdraw funds from a bank account are not expenses of sale, but legal fees to sell a property would be
- (b) any outstanding debts secured on the asset, for example a mortgage
15) A capital asset may have a current market value, for example stocks or shares, or a surrender value, for example premium bonds. The current market value will be the price a willing buyer would pay to a willing seller. The way the market value is obtained will depend on the type of asset held.
16) If the person and the assessing officer both agree that after deducting any relevant amounts set out in paragraph 14 that the total value of the person’s capital is more than the upper capital limit of £23,250, or less then the lower capital limit of £14,250, then it is not necessary to obtain a precise valuation. If there are any disputes, a precise valuation should be obtained. However, the local authority should bear in mind how close someone is to the upper capital limit when deciding whether or not to obtain a precise valuation.
17) Where a precise valuation is required, a professional valuer should be asked to provide a current market valuation. Once the asset is sold, the capital value to be taken into account is the actual amount realised from the sale, minus any actual expenses of the sale.
18) Where the value of a property is disputed, the aim should be to resolve this as quickly as possible. Local authorities should try to obtain an independent valuation of the person’s beneficial share of the property within the 12-week disregard period where a person is in a care home. This will enable local authorities to work out what charges a person should pay and enable the person, or their representative, to consider whether to seek a deferred payment agreement.
19) The value of National Savings Certificates (and Ulster Savings Certificates) (Premium Bonds) is assessed in the same way as other capital assets. A valuation for savings certificates can be obtained by contacting the NS&I helpline on 0845 964 5000. An alternative method to get the value of National Savings Certificates is to use the NS&I online calculator. To enable an accurate value for the savings certificates the person must provide details of the:
- certificate issue number(s)
- purchase price
- date of purchase
Assets held abroad
20) Where capital is held abroad and all of it can be transferred to the UK, its value in the other country should be obtained and taken into account less any appropriate deductions under paragraph 14. Where capital is held jointly, it should be treated the same as if it were held jointly within the UK. The detail will depend on the conditions for transfer to the UK.
21) Where the capital cannot be wholly transferred to the UK due to the rules of that country, for example currency restrictions, the local authority should require evidence confirming this fact. Examples of acceptable evidence could include documentation from a bank, government official or solicitor in either this country or the country where the capital is held.
22) Where some restriction is in place, a local authority should seek evidence showing what the asset is, what its value is and to understand the nature and terms of the restriction so that should this change, the amount can be taken into account. It should also take into account the value that a willing buyer would pay in the UK for those assets, but be aware that it may be less than the market or surrender value in the foreign country.
Capital not immediately realisable
23) Capital which is not immediately realisable due to notice periods, for example National Savings Bank investment accounts or Premium Bonds, should be taken into account in the normal way at its face value. This will be the value at the time of the financial assessment. It may need to be confirmed and adjusted when the capital is realised. If the person chooses not to release the capital, the value at the time of assessment should be used and it should be reassessed at intervals in the normal way.
Capital limits
Upper and lower capital limits
24) The capital limits set out at what point a person is able to access local authority support and how much support they receive. However, local authorities have discretion to set higher capital limits for people receiving care other than in a care home. Subject to the above the local authority must apply the capital limits. The capital limits for financial year 2015 to 2016 are:
- (a) upper capital limit: £23,250
- (b) lower capital limit: £14,250
25) If a person clearly has capital in excess of the upper capital limit, there is no need to make a wider assessment. If a person is near the upper capital limit, the local authority should be mindful of the need to plan ahead for when assets have been spent down and a person may therefore fall below the upper capital limit.
This will help reduce burdens on both the local authority and the person from needing to repeat the financial assessment within a short timeframe.
26) The capital which a person has below the lower capital limit must be disregarded in the calculation of tariff income (see below).
Tariff income
27) Where a person has assets between the lower and upper capital limits the local authority must apply tariff income. This assumes that for every £250 of capital, or part thereof, a person is able to afford to contribute £1 per week towards the cost of their eligible care needs.
Example of tariff income
Nora has capital of £18,100. This is £3,850 above the lower capital limit of £14,250. Dividing the £3,850 by £250 produces a figure of £15.40. When calculating tariff income, the amount is always rounded up. This therefore gives a tariff income of £16 per week.
Notional capital
28) In some circumstances a person may be treated as possessing a capital asset even where they do not actually possess it. This is called notional capital.
29) Notional capital may be capital which:
- (a) would be available to the person if they applied for it
- (b) is paid to a third party in respect of the person
- (c) the person has deprived themselves of in order to reduce the amount of charge they have to pay for their care
30) A person’s capital should therefore be the total of both actual and notional capital. However, if a person has actual capital above the upper capital limit, it may not be necessary to consider notional capital.
31) Where a person has been assessed as having notional capital, the value of this must be reduced over time. The rule is that the value of notional capital must be reduced weekly by the difference between the weekly rate the person is paying for their care and the weekly rate they would have paid if notional capital did not apply.
Example of diminishing notional capital
Hayley is receiving care and support in a care home. She is assessed as having notional capital of £20,000 plus actual capital of £6,000. This means her assets are above the upper capital limit and she needs to pay the full cost of her care and support at £400 per week.
The notional capital should therefore be reduced by the difference between the sum Hayley is paying (£400) and would have paid without the notional capital (£100).
If she did not have the notional capital it would not affect her ability to pay. This is as she has an income of £120.40 and a personal allowance of £24.40 per week and would therefore be assessed as being able to pay £100.
32) Where a person is benefiting from the 12-week property disregard and has chosen to pay a ‘top-up’ fee from their capital resources between the upper and lower capital limits, the level of tariff income that applies during those 12 weeks is the same as it would be if the person were not using the capital to ‘top-up’.
Capital disregarded
33) The following capital assets must be disregarded:
- (a) property in specified circumstances (see paragraph 34)
- (b) the surrender value of any:
- (i) life insurance policy
- (ii) annuity
- (c) payments of training bonuses of up to £200
- (d) payments in kind from a charity
- (e) any personal possessions such as paintings or antiques, unless they were purchased with the intention of reducing capital in order to avoid care and support charges (Schedule 2, para. 13)
- (f) any capital which is to be treated as income or student loans
- (g) any payment from:
- (i) Macfarlane Trust
- (ii) Macfarlane (Special Payments) Trust
- (iii) Macfarlane (Special Payment) (No 2) Trust
- (iv) Caxton Foundation
- (v) The Fund (payments to non-haemophiliacs infected with HIV)
- (vi) Eileen Trust
- (vii) MFET Trust
- (viii) Independent Living Fund (2006)
- (ix) Skipton Fund
- (x) London Bombings Relief Charitable Fund
- (xi) Scottish Infected Blood Support Scheme
- (xii) an approved blood scheme (this is a scheme approved by the Secretary of State, or trust established with funds provided by the Secretary of State, to provide compensation in respect of a person having been infected from contaminated blood products)
- (xiii) London Emergencies Trust
- (xiv) We Love Manchester Emergency Fund
- (xiv) any payment made under or by a trust, established for the purpose of giving relief and assistance to disabled persons whose disabilities were caused by the fact that during their mother’s pregnancy she had taken a preparation containing the drug known as Thalidomide, and which is approved by the Secretary of State (the Thalidomide Trust)
- (xv) the scheme established by the government for former British child migrants in response to the Investigation Report on Child Migration Programmes by the Independent Inquiry into Child Sexual Abuse published on 1 March 2018, made to a former child migrant
- (xvi) any payment made for the purpose of providing compensation or support in respect of the fire on 14 June 2017 at Grenfell Tower
- (xvii) any payment made by the Post Office or the Secretary of State for the purpose of providing compensation or support which is in connection with the failings of the Horizon system, or otherwise payable following the judgment in Bates and Others v Post Office Ltd ((No. 3) “Common Issues”)
- (xviii) any payment made under the Windrush Compensation Scheme (Expenditure) Act 2020
- (xix) any payment from a scheme established or approved by the Secretary of State for the purpose of providing compensation in respect of historic institutional child abuse in the UK
- (xx) any payment from the Victims of Overseas Terrorism Compensation Scheme established by the Ministry of Justice in 2012 under section 47 of the Crime and Security Act 2010
- (xxi) any payment made under the Vaccine Damage Payments Act 1979
- (xxii) Lesbian, Gay, Bisexual and Transgender Financial Recognition Scheme
- (xxiii) any payment made under section 133(1) of the Criminal Justice Act 1988 or any other payment made by the Secretary of State, the Scottish Ministers or, in Northern Ireland, the Department of Justice, for the purpose of compensating a person for a miscarriage of justice arising from criminal proceedings
- (h) the value of funds held in trust or administered by a court which derive from a payment for personal injury to the person. For example, the vaccine damage and criminal injuries compensation funds
- (i) the value of a right to receive:
- (i) income under an annuity
- (ii) outstanding instalments under an agreement to repay a capital sum
- (iii) payment under a trust where the funds derive from a personal injury
- (iv) income under a life interest or a life-rent
- (v) income (including earnings) payable in a country outside the UK which cannot be transferred to the UK
- (vi) an occupational pension
- (vii) any rent. Please note however that this does not necessarily mean the income is disregarded. Please see Annex C for guidance on the treatment of income.
- (j) capital derived from an award of damages for personal injury which is administered by a court or which can only be disposed of by a court order or direction
- (k) the value of the right to receive any income under an annuity purchased pursuant to any agreement or court order to make payments in consequence of personal injury or from funds derived from a payment in consequence of a personal injury and any surrender value of such an annuity
- (l) periodic payments in consequence of personal injury pursuant to a court order or agreement to the extent that they are not a payment of income and area treated as income (and disregarded in the calculation of income)
- (m) any Social Fund payment
- (n) refund of tax on interest on a loan which was obtained to acquire an interest in a home or for repairs or improvements to the home
- (o) any capital resources which the person has no rights to as yet, but which will come into his possession at a later date, for example on reaching a certain age
- (p) payments from the Department of Work and Pensions to compensate for the loss of entitlement to Housing Benefit or Housing Benefit Supplement
- (q) the amount of any bank charges or commission paid to convert capital from foreign currency to sterling
- (r) payments to jurors or witnesses for court attendance (but not compensation for loss of earnings or benefit)
- (s) community charge rebate/council tax rebate
- (t) money deposited with a Housing Association as a condition of occupying a dwelling
- (u) any Child Support Maintenance Payment
- (v) the value of any ex-gratia payments made on or after 1 February 2001 by the Secretary of State in consequence of a person’s, or person’s spouse or civil partner’s imprisonment or internment by the Japanese during the Second World War
- (w) any payment made by a local authority under the Adoption and Children Act 2002 (under section 2(b)(b) or 3 of this act)
- (x) the value of any ex-gratia payments from the Skipton Fund made by the Secretary of State for Health to people infected with Hepatitis C as a result of NHS treatment with blood or blood products
- (y) payments made under a trust established out of funds provided by the Secretary of State for Health in respect of persons suffering from variant Creutzfeldt-Jakob disease to the victim or their partner (at the time of death of the victim)
- (z) any payments under Section 2, 3 or 7 of the Age-Related Payments Act 2004 or Age Related Payments Regulations 2005 (SI No 1983)
- (aa) any payments made under section 63(6)(b) of the Health Services and Public Health Act 1968 to a person to meet childcare costs where he or she is undertaking instruction connected with the health service by virtue of arrangements made under that section
- (bb) any payment made in accordance with regulations under Section 14F of the Children Act 1989 to a resident who is a prospective special guardian or special guardian, whether income or capital
Example of disregarded capital
Mr T is a former Far East prisoner of war and receives a £10,000 ex-gratia payment as a result of his imprisonment. He now requires care and support and has a total of £25,000 in capital. When calculating how much capital should be taken into account, the local authority must disregard the first £10,000 – the value of the ex-gratia payment.
The normal capital rules are then applied to the remaining £15,000. In this case, the first £14,250 would be completely disregarded in addition to the £10,000. Tariff income would therefore only be applied to the remaining £750 giving a charge of £3.
Property disregards
34) In the following circumstances the value of the person’s main or only home must be disregarded:
- (a) where the person is receiving care in a setting that is not a care home
- (b) if the person’s stay in a care home is temporary and they either:
- (i) intend to return to that property and that property is still available to them
- (ii) are taking reasonable steps to dispose of the property in order to acquire another more suitable property to return to
- (c) where the person no longer occupies the property but it is occupied in part or whole as their main or only home by any of the people listed below, the mandatory disregard only applies where the property has been continuously occupied since before the person went into a care home (for discretionary disregards see below):
- (i) the persons partner, former partner or civil partner, except where they are estranged
- (ii) a lone parent who is the person’s estranged or divorced partner;
- (iii) a relative as defined in paragraph 35 of the person or member of the person’s family who is either:
- 1) aged 60 or over
- 2) is a child of the resident aged under 18
- 3) is incapacitated
35) For the purposes of the disregard a relative is defined as including any of the following:
- (a) parent (including an adoptive parent)
- (b) parent-in-law
- (c) son (including an adoptive son)
- (d) son-in-law
- (e) daughter (including an adoptive daughter)
- (f) daughter-in-law
- (g) step-parent
- (h) step-son
- (i) step-daughter
- (j) brother
- (k) sister
- (l) grandparent
- (m) grandchild
- (n) uncle
- (o) aunt
- (p) nephew
- (q) niece
- (r) the spouse, civil partner or unmarried partner of (a) to (k) inclusive
36) A member of the person’s family is defined as someone who is living with the qualifying relative as part of an unmarried couple, married to or in a civil partnership.
37) For the purposes of the disregard the meaning of ‘incapacitated’ is not closely defined. However, it will be reasonable to conclude that a relative is incapacitated if one of the following conditions apply:
- (a) the relative is receiving one (or more) of the following benefits: incapacity benefit, severe disablement allowance, disability living allowance, personal independence payments, armed forces independence payments, attendance allowance, constant attendance allowance, or a similar benefit
- (b) the relative does not receive any disability related benefit but their degree of incapacity is equivalent to that required to qualify for such a benefit. Medical or other evidence may be needed before a decision is reached
38) For the purpose of the property disregard, the meaning of ‘occupy’ is not closely defined. In most cases it will be obvious whether or not the property is occupied by a qualifying relative as their main or only home. However, there will be some cases where this may not be clear and the local authority should undertake a factual inquiry weighing up all relevant factors in order to reach a decision. An emotional attachment to the property alone is not sufficient for the disregard to apply.
39) Circumstances where it may be unclear might include where a qualifying relative has to live elsewhere for the purposes of their employment, for example a member of the armed services or the diplomatic service. Whilst they live elsewhere in order to undertake their employment, the property remains their main or only home. Another example may be someone serving a prison sentence. It would not be reasonable to regard the prison as the person’s main or only home and they may well intend to return to the property in question at the end of their sentence. In such circumstances the local authority may wish to consider the qualifying relative’s length of sentence and the likelihood of them returning to the property. Essentially the qualifying relative is occupying the property but is not physically present.
Example of emotional attachment to a property
Bea is 62 years old and lives with her family in Kent. Her father Patrick is a widower who has been living in the family home in Teddington that she and her sister grew up in and where she occasionally stays to help her father. Patrick has been assessed as having eligible care and support needs that are best met by moving into a care home.
Although Bea is over the age of 60, the family home is not her main or only home and the property is therefore not disregarded.
Example of occupying a property when not physically present
Matt is 60 years old and has been living overseas for the past 10 years due to his job in the diplomatic service. When he is in England, he lives at the family home he grew up in. His father Ken has been assessed as having eligible care and support needs that are best met by moving into a care home. In Ken’s financial assessment, the value of his property is disregarded as his son Matt is a qualifying relative that occupies the property as his main or only home. Although Matt is not physically present at the property at the point Ken moves into the care home, his alternative accommodation is only as a result of his employment and the family home is his main home.
40) The local authority will need to take account of the individual circumstances of each case. However, it may be helpful to consider the following factors in making a decision:
- does the relative currently occupy another property?
- if the relative has somewhere else to live do they own or rent the property (for example, how secure/permanent is it?)
- if the relative is not physically present is there evidence of a firm intention to return to or live in the property
- where does the relative pay council tax?
- where is the relative registered to vote?
- where is the relative registered with a doctor?
- are the relatives belongings located in the property?
- is there evidence that the relative has a physical connection with the property?
41) A property must be disregarded where the relative meets the qualifying conditions (for example, is aged 60 or over or is incapacitated) and has occupied the property as their main or only home since before the resident entered the care home.
Discretionary disregard
42) A local authority may also use its discretion to apply a property disregard in other circumstances. However, the local authority will need to balance this discretion with ensuring a person’s assets are not maintained at public expense. An example where it may be appropriate to apply the disregard is where it is the sole residence of someone who has given up their own home in order to care for the person who is now in a care home or is perhaps the elderly companion of the person.
Example of local authority discretion to apply a property disregard
Jayne has the early signs of dementia but wishes to continue living in her own home. She is not assessed as having eligible needs, but would benefit from some occasional support. Her best friend Penny gives up her own home to move in with Jayne. At this point, there is no suggestion that Jayne may need care in a care home.
After 5 years Jayne’s dementia has reached the point where she needs a far greater level of care and support and following an assessment it is agreed her needs would best be met in a care home. On moving into the care home, the local authority uses its discretion to apply the property disregard as this has now become Penny’s main or only home.
43) A property may be disregarded when a qualifying relative moves into the property after the resident enters a care home. Where this happens the local authority will need to consider all the relevant factors in deciding whether the property must be disregarded. Factors such as the timing and purpose of the move may be relevant to establishing if the property is the relative’s main or only home. The purpose of the disregard in these circumstances is to safeguard certain categories of people from the risk of homelessness.
44) The local authority should consider if the principle reason for the move is that it is necessary to ensure the relative has somewhere to live as their main or only home. A disregard would not be appropriate, for example where a person moves into a property solely to protect the family inheritance. Local authorities need to ensure that people are not needlessly maintained at public expense. A local authority will need to take account of the individual circumstances of each case; however, it may be helpful to consider the factors listed above for the mandatory disregard plus the following additional factors in making a decision:
- was the relative occupying another property as their main or only home at the time of the previous financial assessment?
- could the relative have reasonably expected to have the property taken into account at the time they moved into the property?
- would failure to disregard the property result in the eligible relative becoming homeless?
- would failure to disregard the property negatively impact on the eligible relatives own health and wellbeing?
Example of local authority discretion to apply a property disregard where the qualifying person moves into the property after the resident entered the care home
Fred’s family home is unoccupied because his father has died and his mother is in a care home and Fred and his siblings have their own homes. The property is subject to a deferred payments agreement. Fred has a serious accident and becomes incapacitated. As a result he unable to work or pay for his existing home. He has nowhere else to live so he moves into the family home which becomes his only home. In the circumstances, the local authority exercises its discretion to disregard the property.
Example of local authority discretion to apply a property disregard
Hilda is 63 and lives in a rented flat. Her brother, Stephen, has recently died and his wife, Charlotte, has moved in to a care home. Hilda suddenly loses her job and finds she unable to afford to live in her rented flat. As a result, Hilda moves into Stephen and Charlotte’s house and this becomes her only home. In the circumstances, the local authority exercises its discretion to disregard the property.
‘12-week property disregard’
45) An important aim of the charging framework is to prevent people being forced to sell their home at a time of crisis. The regulations under the Care Act 2014 therefore create space for people to make decisions as to how to meet their contribution to the cost of their eligible care needs. A local authority must therefore disregard the value of a person’s main or only home for 12 weeks in the following circumstances:
(a) when they first enter a care home as a permanent resident
(b) when a property disregard other than the 12-week property disregard unexpectedly ends because the qualifying relative has died or moved into a care home
46) In addition, a local authority has discretion to choose to apply the disregard when there is a sudden and unexpected change in the person’s financial circumstances. In deciding whether to do so, the local authority will want to consider the individual circumstances of the case. Such circumstances might include a fall in share prices or an unanticipated debt. An example is given below.
Example of the end of a property disregard
Win and Ern have been married for 60 years and brought a home together. 18 months ago, Win moved into a care home as a result of dementia. During her financial assessment, the value of the home she shared with Ern was disregarded as Ern is her husband, was over 60 years old and still lived in the property. Ern has been in good health and there is no reason to anticipate a sudden change in circumstance. Unfortunately Ern suffers a heart attack and passes away, leaving the property to Win. There is no longer an eligible person living in the property, meaning its value can now be taken into account in what Win can afford to contribute to the cost of her care.
Given this was unplanned for, Win and her family need time to consider what the best option might be. The 12 week disregard would therefore be applied.
Example of an unexpected change in financial circumstances
Harry is a widower who owns his own home. Ten months ago he moved into a care home as a self-funder. He has been meeting the bulk of his costs from shares he received as part of his redundancy package. Due to an unexpected event, the value of his shared is suddenly reduced by half, meaning he is unable to meet the cost of his care.
Although already in a care home and likely to remain responsible for paying for this care, Harry approaches the local authority for assistance and to seek a Deferred Payment Agreement. During the financial assessment the local authority agrees that the circumstances could not have been foreseen and uses its discretion to disregard the value of his property for the first 12 weeks. This provides Harry with the space he needs to make arrangements for the Deferred Payment Agreement to be put in place and enable him to continue to meet the cost of his care.
‘26-week disregard’
47) The following capital assets must be disregarded for at least 26 weeks in a financial assessment. However, a local authority may choose to apply the disregard for longer where it considers this appropriate. For example where a person is taking legal steps to occupy premises as their home, but the legal processes take more than 26 weeks to complete.
a) Assets of any business owned or part-owned by the person in which they were a self-employed worker and has stopped work due to some disease or disablement but intends to take up work again when they are fit to do so. Where the person is in a care home, this should apply from the date they first took up residence. [Schedule 2 Paragraph 9]
b) Money acquired specifically for repairs to or replacement of the person’s home or personal possessions provided it is used for that purpose. This should apply from the date the funds were received. [Schedule 2 Paragraph 12]
c) Premises which the person intends to occupy as their home where they have started legal proceedings to obtain possession. This should be from the date legal advice was first sought or proceedings first commenced. [Schedule 2 Paragraph 22]
d) Premises which the person intends to occupy as their home where essential repairs or alterations are required. This should apply from the date the person takes action to effect the repairs. [Schedule 2 Paragraph 21]
e) Capital received from the sale of a former home where the capital is to be used by the person to buy another home. This should apply from the date of completion of the sale. [Schedule 2 Paragraph 6]
f) Money deposited with a Housing Association which is to be used by the person to purchase another home. This should apply from the date on which the money was deposited. [Schedule 2 Paragraph 11]
g) Grant made under a Housing Act which is to be used by the person to purchase a home or pay for repairs to make the home habitable. This should apply from the date the grant is received [Schedule 4 Paragraph 22]
‘52-week disregard’
48) The following payments of capital must be disregarded for a maximum of 52 weeks from the date they are received:
-
(a) the balance of any arrears of or any compensation due to non-payment of:
- (i) mobility supplement
- (ii) Attendance Allowance
- (iii) Constant Attendance Allowance
- (iv) Disability Living Allowance / Personal Independence Payment
- (v) Exceptionally Severe Disablement Allowance
- (vi) Severe Disablement Occupational Allowance
- (vii) Armed forces service pension based on need for attendance
- (viii) Pension under the Personal Injuries (Civilians) Scheme 1983, based on the need for attendance
- (ix) Income Support/Pension Credit
- (x) Minimum Income Guarantee
- (xi) Working Tax Credit
- (xii) Child Tax Credit
- (xiii) Housing Benefit
- (xiv) Universal Credit
- (xv) special payments to pre-1973 war widows
As the above payments will be paid for specific periods, they should be treated as income over the period for which they are payable. Any money left over after the period for which they are treated as income has elapsed should be treated as capital. [Schedule 2 Paragraphs 10 and 11]
- (b) payments or refunds for:
- (i) NHS glasses, dental treatment or patient’s travelling expenses
- (ii) cash equivalent of free milk and vitamins
- (iii) expenses in connection with prison visits. [Schedule 2 Paragraph 22]
- (c) Personal Injury Payments
Example of a disregard for 52 weeks
During his financial assessment it is identified that Colin is eligible for Pension Credit but is not currently claiming the support. He is therefore assessed as being able to pay £75 per week towards the cost of his care. Colin tells the local authority that he will apply for Pension Credit. It is explained to him that the level of what he can afford to contribute will be reassessed once he started receiving the additional support. If the payments are backdated, his contributions to the cost of his care will also be backdated and he may therefore need to make an additional payment to meet any arrears. Colin therefore chooses to pay £90 per week. After six weeks, arrears of Pension Credit at £35 per week (£210) are received. What Colin can afford to contribute is reassessed and he is now asked to pay £110 per week. As Colin has been paying £15 a week more than required, he only owes £120 rather than the full £210 of Pension Credit arrears. The remaining £90 of arrears payments should therefore be treated as capital and disregarded
‘2-year disregard’
49) Local authorities must disregard payments made under a trust established out of funds by the Secretary of State for Health in respect of vCJD to either a:
-
(a) member of the victim’s family for 2 years from the date of death of the victim (or from the date of payment from the trust if later)
-
(b) dependent child or young person until they turn 18 [Schedule 2 Paragraph 27]
Other disregards
50) In some cases a person’s assets may be tied up in a business that they own or part-own. Where a person is taking steps to realise their share of the assets, these should be disregarded during the process. However, the person should be required to show that it is their clear intention to realise the asset as soon as practicable. In order to show their intent, the local authority should request the following information:
- (a) a description of the nature of the business asset
- (b) the person’s estimate of the length of time necessary to realise the asset or their share of it
- (c) t statement of what, if any, steps have been taken to realise the asset, what these were and what is intended in the near future
- (d) any other relevant evidence, for example the person’s health, receivership, liquidation, estate agent’s confirmation of placing any property on the market
51) Where the person has provided this information to show that steps are being taken to realise the value of the asset, the local authority must disregard the value for a period that it considers to be reasonable. In deciding what is reasonable it should take into account the length of time of any legal processes that may be needed.
52) Where the person has no immediate intention of attempting to realise the business asset, its capital value should be taken into account in the financial assessment. Where a business is jointly owned, this should apply only to the person’s share.
Treatment of investment bonds
53) The treatment of investment bonds is currently complex. This is in part because of the differing products that are on offer. As such, local authorities may wish to seek advice from their legal departments.
54) Where an investment bond includes one or more element of life insurance policies that contain cashing-in rights by way of options for total or partial surrender, then the value of those rights must be disregarded as a capital asset in the financial assessment.
Capital treated as income
55) The following capital payments should be treated as income. Local authorities therefore must have regard to Annex C before conducting their assessments:
- (a) any payment under an annuity.
- (b) capital paid by instalment where the total of:
- (i) the instalments outstanding at the time the person first becomes liable to pay for their care, or in the case of a person in temporary care whom the local authority had previously decided not to charge, the first day on which the local authority decided to charge
- (ii) the amount of other capital held by the resident is over £16,000. If it is £16,000 or less, each instalment should be treated as capital [Regulation 16]
Earnings
56) Any income of the person derived from employment must be treated as earnings and not taken into account in the financial assessment.
Income treated as capital
57) The following types of income should be treated as capital:
- (a) any refund of income tax charged on profits of a business or earnings of an employed earner; Any holiday pay payable by an employer more than 4 weeks after the termination or interruption of employment
- (b) income derived from a capital asset, for example, building society interest or dividends from shares. This should be treated as capital from the date it is normally due to be paid to the person. This does not apply to income from certain disregarded capital
- (c) any advance of earnings or loan made to an employed earner by the employer if the person is still in work. This is as the payment does not form part of the employee’s regular income and would have to be repaid
- (d) any bounty payment paid at intervals of at least one year from employment as:
- (i) a part time fireman
- (ii) an auxiliary coastguard
- (iii) a part time lifeboat man
- (iv) a member of the territorial or reserve forces
- (e) charitable and voluntary payments which are neither made regularly nor due to be made regularly, apart from certain exemptions such as payments from AIDS trusts. Payments will include those made by a third party to the person to support the clearing of charges for accommodation
- (f) any payments of arrears of contributions by a local authority to a custodian towards the cost of accommodation and maintenance of a child [Regulation 18]
Capital available on application
58) In some instances a person may need to apply for access to capital assets but has not yet done so. In such circumstances this capital should be treated as already belonging to the person except in the following instances:
- (a) capital held in a discretionary trust
- (b) capital held in a trust derived from a payment in consequence of a personal injury
- (c) capital derived from an award of damages for personal injury which is administered by a court
- (d) any loan which could be raised against a capital asset which is disregarded, for example the home. [Regulation 21(2)]
59) A local authority should distinguish between:
-
(a) capital already owned by the person but which in order to access they must make an application for. For example:
- (i) money held by the person’s solicitor
- (ii) Premium Bonds
- (iii) National Savings Certificates
- (iv) money held by the registrar of a county court which will be released on application
-
(b) capital not owned by the person that will become theirs on application, for example an unclaimed Premium Bond win. This should be treated as notional capital. [Regulation 21(2)]
60) Where a local authority treats capital available on application as notional capital they should do so only from the date at which it could be acquired by the person. [Regulation 21(2)]
61) April 2015 saw much greater flexibility introduced regarding how people can access their defined contribution pensions, including enabling them to access their full pension pot. As a result, when applying notional income to a defined contribution pension this should be calculated as the maximum income that would be available if the person had taken out an annuity. Further guidance is provided in paragraph 25 of Annex C.
Annex C: Treatment of income
This annex covers the treatment of income when conducting a financial assessment in all circumstances. This is divided into:
- care homes
- all other settings
The purpose of this annex is to provide local authorities with detailed guidance on how to apply to the Care and Support (Charging and Assessment of Resources) Regulations 2014, in terms of how to treat different types of income when calculating what a person can afford to contribute to the cost of their eligible care needs.
1) This section of the guidance only applies where a local authority has chosen to charge a person for the services it is arranging and therefore must undertake a financial assessment. When doing so, it must assess the income and capital of the person.
2) There are differences in how income is treated in a care home and in all other settings. Charging a person in a care home is provided for in a consistent national framework. When charging a person in all other settings, a local authority has more discretion to enable it to take account of local practices and innovations. The guidance sets out the common issues and then those particular to each setting. Local authorities must read this guidance in all circumstances.
3) This annex covers the treatment of income and should be read in conjunction with Annex B on the treatment of capital. The detail of the sources of income which local authorities must disregard are set out in the regulations which accompany this guidance.
Common issues
4) The following section sets out the issues common to charging for all settings.
5) Only the income of the cared-for person can be taken into account in the financial assessment of what they can afford to pay for their care and support. Where this person receives income as one of a couple, the starting presumption is that the cared-for person has an equal share of the income. A local authority should also consider the implications for the cared-for person’s partner.
6) Income is net of any tax or National Insurance contributions.
7) Income will always be taken into account unless it is disregarded under the regulations. Income that is disregarded will either be:
- (a) partially disregarded
- (b) fully disregarded
8) In all cases, irrespective of setting, employed and self-employed earnings are fully disregarded. [Regulation 14]
9) Earnings in relation to an employed earner are any remuneration or profit from employment. This will include:
- (a) any bonus or commission
- (b) any payment in lieu of remuneration except any periodic sum paid to the person on account of the termination of their employment by reason of redundancy
- (c) any payments in lieu of notice or any lump sum payment intended as compensation for the loss of employment but only in so far as it represents loss of income
- (d) any holiday pay except any payable more than four weeks after the termination or interruption of employment
- (e) any payment by way of a retainer
- (f) any payment made by the person’s employer in respect of any expenses not wholly, exclusively and necessarily incurred in the performance of the duties of employment, including any payment made by the person’s employer in respect of travelling expenses incurred by the person between their home and the place of employment and expenses incurred by the person under arrangements made for the care of a member of the person’s family owing to the person’s absence from home
- (g) any award of compensation made under section 112(4) or 117(3)(a) of the Employment Rights Act 1996 (remedies and compensation for unfair dismissal)
- (h) any such sum as is referred to in section 112 of the Social Security Contributions and Benefits Act 1992 (certain sums to be earnings for social security purposes)
- (i) any statutory sick pay, statutory maternity pay, statutory paternity pay or statutory adoption pay, or a corresponding payment under any enactment having effect in Northern Ireland
- (j) any remuneration paid by or on behalf of an employer to the person who for the time being is on maternity leave, paternity leave or adoption leave or is absent from work because of illness
- (k) the amount of any payment by way of a non-cash voucher which has been taken into account in the computation of a person’s earnings in accordance with Part 5 of Schedule 3 to the Social Security (Contributions) Regulations 2001
10) Earnings in relation to an employed earner do not include:
- (a) any payment in kind, with the exception of any non-cash voucher which has been taken into account in the computation of the person’s earnings – as referred to above
- (b) any payment made by an employer for expenses wholly, exclusively and necessarily incurred in the performance of the duties of the employment
- (c) any occupational/personal pension
11) Earnings in the case of employment as a self-employed earner mean the gross receipts of the employment. This includes any allowance paid under section 2 of the Employment and Training Act 1973 or section 2 of the Enterprise and New Towns (Scotland) Act 1990 to the person for the purpose of assisting the person in carrying on his business.
12) Earnings in the case of employment as a self-employed earner do not include:
- (a) any payment to the person by way of a charge for board and lodging accommodation provided by the person
- (b) any sports award
13) Earnings also include any payment provided to prisoners to encourage and reward their constructive participation in the regime of the establishment, this may include payment for working, education or participation in other related activities.
Benefits
14) Local authorities may take most of the benefits people receive into account. Those they must disregard are listed below. However, they need to ensure that in addition to the minimum guaranteed income or personal expenses allowance – details of which are set out below – people retain enough of their benefits to pay for things to meet those needs not being met by the local authority.
15) Any income from the following sources must be fully disregarded:
- (a) Direct Payments
- (b) Guaranteed Income Payments made to veterans under the Armed Forces Compensation Scheme
- (c) War Pension Scheme payments made to veterans with the exception of Constant Attendance Allowance payments
- (d) the mobility component of Disability Living Allowance
- (e) the mobility component of Personal Independence Payments
16) Any income from the following benefits must be taken into account when considering what a person can afford to pay from their income towards the cost of their care and support in a care home:
- (a) Attendance Allowance, including Constant Attendance Allowance and Exceptionally Severe Disablement Allowance
- (b) Bereavement Allowance
- (c) Carers Allowance
- (d) Disability Living Allowance (Care component)
- (e) Employment and Support Allowance or the benefits this replaces such as Severe Disablement Allowance and Incapacity Benefit
- (f) Income Support
- (g) Industrial Injuries Disablement Benefit or equivalent benefits
- (h) Jobseeker’s Allowance
- (i) Maternity Allowance
- (j) Pension Credit
- (k) Personal Independence Payment (Daily Living component)
- (l) State Pension
- (m) Universal Credit
17) Working Tax Credits must be taken into account when considering what a person can afford to pay from their income towards the cost of their care in a care home. However, they should be disregarded in the calculation of income for care and support arranged other than in a care home.
18) Where any Social Security benefit payment has been reduced (other than a reduction because of voluntary unemployment), for example because of an earlier overpayment, the amount taken into account should be the gross amount of the benefit before reduction.
Annuity and pension income
19) An annuity is a type of pension product that provides a regular income for a number of years in return for an investment. Such products are usually purchased at retirement in order to provide a regular income. While the capital is disregarded, any income from an annuity must be taken fully into account except where it is:
- (a) purchased with a loan secured on the person’s main or only home
- (b) a gallantry award such as the Victoria Cross Annuity or George Cross Annuity
20) Where a person has a spouse or civil partner they do not live with, and is paying at least half of the value of their occupational pension, personal pension or retirement annuity to their spouse or civil partner for their maintenance, the local authority must disregard an amount equal to 50% of the pension or annuity income concerned.
21) For those who have purchased an annuity with a loan secured on their main or only home, this is known as a ‘home income plan’. Under these schemes, a person has purchased the annuity against the value of their home – similarly to a Deferred Payment Agreement.
22) In order to qualify for the disregard, one of the annuitants must still be occupying the property as their main or only home. This may happen where a couple has jointly purchased an annuity and only one of them has moved into a care home. If this is not the case, the disregard must not be applied.
23) Where the disregard is applied, only the following aspects may be disregarded:
- (a) the net weekly interest on the loan where income tax is deductible from the interest
- (b) the gross weekly interest on the loan in any other case
24) Before applying the disregard, the following conditions must be met:
- (a) the loan must have been made as part of a scheme that required that at least 90% of that loan be used to purchase the annuity
- (b) the annuity ends with the life of the person who obtained the loan, or where there are 2 or more annuitants (including the person who obtained the loan), with the life of the last surviving annuitant
- (c) the person who obtained the loan or one of the other annuitants is liable to pay the interest on the loan
- (d) the person who obtained the loan (or each of the annuitant where there are more than one) must have reached the age of 65 at the time the loan was made
- (e) the loan was secured on a property in Great Britain and the person who obtained the loan (or one of the other annuitants) owns an estate or interest in that property
- (f) the person who obtained the loan or one of the other annuitant occupies the property as their main or only home at the time the interest is paid
25) Where the person is using part of the income to repay the loan, the amount paid as interest must be disregarded. If the payments the person makes on the loan are interest only and the person qualifies for tax relief on the interest they pay, disregard the net interest. Otherwise, disregard the gross interest.
26) Reforms to defined contribution pensions came into effect from April 2015. The aim of the reforms is to provide people with much greater flexibility in how they fund later life. This may lead to changes in how people use the money in their pension fund. The rules for how to assess pension income for the purposes of charging are:
- (a) if a person has removed the funds and placed them in another product or savings account, they should be treated according to the rules for that product
- (b) if a person is only drawing a minimal income, or choosing not to draw income, then a local authority can apply notional income. This must be the maximum income that could be drawn under an annuity product. If applying maximum notional income, any actual income should be disregarded to avoid double counting
- (c) if a person is drawing down an income that is higher than the maximum available under an annuity product, the actual income that is being drawn down should be taken into account
Mortgage protection insurance policies
27) Any income from an insurance policy is usually taken into account. In the case of mortgage protection policies where the income is specifically intended to support the person to acquire or retain an interest in their main or only home or to support them to make repairs or improvements to their main or only home it must be disregarded. However, the income must be being used to meet the repayments on the loan. The amount of income from a mortgage protection insurance policy that should be disregarded is the weekly sum of (a+b+c) listed below:
- a) the amount which covers the interest on the loan
- b) the amount of the repayment which reduced the capital outstanding
- c) the amount of the premium due on the policy
28) It should be remembered that Income Support and Pension Credit may be adjusted to take account of the income from the policy.
Other income that must be fully disregarded
29) Any income from the following sources must be fully disregarded:
- (a) Armed Forces Independence Payments and Mobility Supplement
- (b) Child Support Maintenance Payments and Child Benefit, except where the accommodation is arranged under the Care Act in which the adult and child both live
- (c) Child Tax Credit
- (d) Council Tax Reduction Schemes where this involves a payment to the person
- (e) Disability Living Allowance (Mobility Component) and Mobility Supplement
- (f) Christmas bonus
- (g) dependency increases paid with certain benefits
- (h) Discretionary Trust
- (i) Gallantry Awards
- (j) Guardian’s Allowance
- (k) Guaranteed Income Payments made to Veterans under the Armed Forces Compensation Scheme
- (l) Payments made to Veterans under the War Pension Scheme with the exception of Constant Attendance Allowance
- (m) Income frozen abroad
- (n) income in kind
- (o) pensioners Christmas payments
- (p) Personal Independence Payment (Mobility Component) and Mobility Supplement
- (q) personal injury trust, including those administered by a Court
- (r) resettlement benefit
- (s) savings credit disregard
- (t) Social Fund payments (including winter fuel payments)
- (u) war widows and widowers special payments
- (v) any payments received as a holder of the Victoria Cross, George Cross or equivalent
- (w) any grants or loans paid for the purposes of education; and
- (x) payments made in relation to training for employment.
- (y) any payment from:
- (i) Macfarlane Trust
- (ii) Macfarlane (Special Payments) Trust
- (iii) Macfarlane (Special Payment) (No 2) Trust
- (iv) Caxton Foundation
- (v) The Fund (payments to non-haemophiliacs infected with HIV)
- (vi) Eileen Trust
- (vii) MFET Limited
- (viii) Independent Living Fund (2006)
- (ix) Skipton Fund
- (x) London Bombings Relief Charitable Fund
- (xi) Scottish Infected Blood Support Scheme
- (xii) an approved blood scheme (this is a scheme approved by the Secretary of State, or trust established with funds provided by the Secretary of State, to provide compensation in respect of a person having been infected from contaminated blood products)
- (xiii) London Emergencies Trust
- (xiv) We Love Manchester Emergency Fund
- (xv) any payment made for the purpose of providing compensation or support in respect of the fire on 14 June 2017 at Grenfell Tower
- (xvi) any payment made by the Post Office or the Secretary of State for the purpose of providing compensation or support which is in connection with the failings of the Horizon system, or otherwise payable following the judgment in Bates and Others v Post Office Ltd ((No. 3) “Common Issues”)
- (xvii) any payment made under the Windrush Compensation Scheme (Expenditure) Act 2020
- (xviii) any payment from a scheme established or approved by the Secretary of State for the purpose of providing compensation in respect of historic institutional child abuse in the UK
- (xix) any payment made under the Vaccine Damage Payments Act 1979
- (xx) any payment from the Victims of Overseas Terrorism Compensation Scheme established by the Ministry of Justice in 2012 under section 47 of the Crime and Security Act 2010
- (xxi) Lesbian, Gay, Bisexual and Transgender Financial Recognition Scheme
- (xxii) any payment made under section 133(1) of the Criminal Justice Act 1988 or any other payment made by the Secretary of State, the Scottish Ministers or, in Northern Ireland, the Department of Justice, for the purpose of compensating a person for a miscarriage of justice arising from criminal proceedings
- (xxiii) payments by local authorities in relation to placed or supported children
Savings credit
30) For people receiving care and support other than in a care home, the savings credit the adult receives should be fully disregarded.
Charitable and voluntary payments
31) Charitable payments are not necessarily made by recognised charity, but could come from charitable motives. The individual circumstances of the payment will need to be taken into account before making a decision. In general a charitable or voluntary payment which is not made regularly is treated as capital.
32) Charitable and voluntary payments that are made regularly must be fully disregarded.
Partially disregarded income
33) The following income is partially disregarded:
- (a) the first £10 per week of War Widows and War Widowers pension, survivors Guaranteed Income Payments from the Armed Forces Compensation Scheme, Civilian War Injury pension, any War Disablement pension paid to non-veterans and payments to victims of National Socialist persecution (paid under German or Austrian law)
- (b) a savings disregard based on qualifying is made to people as follows:
For individuals:
- where a person is in receipt of qualifying income of less than £133.82 per week there will be no Savings Disregard made
- where a person is in receipt of qualifying income between £133.82 and £155.60 per week the savings disregard is made, which will equal the actual amount of the savings credit received or a sum of £5.75 whichever is less
- where a person is in receipt of qualifying income in excess of £155.60 per week, and a savings credit reward is in payment, a flat rate savings disregard of £5.75 per week is made irrespective of how much the savings credit payment is
- where a person has qualifying income above the limit for receiving a savings credit reward (around £190.00 but could be higher if the person is severely disabled, has caring responsibilities or certain housing costs) a flat rate savings disregard of £5.75 is made
For couples:
- where a person is part of a couple (including a civil partnership) and is in receipt of qualifying income of less than £212.97 per week there will be no savings disregard made
- where a person who is part of a couple (including a civil partnership) and is in receipt of qualifying income between £212.97 and £237.55 per week the savings disregard is made, which will equal the actual amount of the savings credit received or a sum of £8.60 whichever is less
- where a person who is part of a couple (including a civil partnership) and is in receipt of qualifying income in excess of £237.55 per week, and a savings credit reward is in payment, a flat rate savings disregard of £8.60 per week is made irrespective of how much the savings credit payment is
- where a person who is part of a couple (including a civil partnership) and has qualifying income above the limit for receiving savings credit (around £278.00 but could be higher if the person is severely disabled, has caring responsibilities or certain housing costs) a flat rate savings disregard of £8.60 is made
The values of £155.60 and £237.55 above represent the standard minimum guarantee for an individual and couple respectively. These amounts are increased to an appropriate minimum guarantee where individuals and couples qualify as severely disabled or as carers because of receipt of qualifying benefits.
Notional income
34) In some circumstances a person may be treated as having income that they do not actually have. This is known as notional income. This might include for example income that would be available on application but has not been applied for, income that is due but has not been received or income that the person has deliberately deprived themselves of for the purpose of reducing the amount they are liable to pay for their care. For guidance on deprivation of assets, see Annex E. In all cases the local authority must satisfy itself that the income would or should have been available to the person.
35) Notional income should also be applied where a person who has reached pension credit qualifying age and has a personal pension plan but has not purchased an annuity or arranged to draw down the equivalent maximum annuity income that would be available from the plan. Notional income should be applied in line with paragraph 25 above. Estimates of the notional income can be received from the pension provider or from estimates provided by the Government Actuary’s Department.
Example of notional income
Andrew is 70 and is living in a care home. He has not been receiving his occupational pension to which he would have been entitled to from age 65. After contacting his former employer, they state Andrew will be paid the entire pension due from age 65. The local authority can therefore apply notional income from age 65.
36) Where notional income is included in a financial assessment, it should be treated the same way as actual income. Therefore any income that would usually be disregarded should continue to be so.
37) Notional income should be calculated from the date it could be expected to be acquired if an application had been made. In doing so, a local authority should assume the application was made when it first became aware of the possibility and take account of any time limits which may limit the period of arrears.
Example of notional income in relation to new pension flexibilities
Ben has a pension fund worth £30,000. He has taken the opportunity to access this flexibly and as a result is only drawing down £5 a week as income at the point he begins to receive care and support. The equivalent maximum annuity income would be £120 per week. For the purposes of the financial assessment, the local authority can assume an income £120 per week.
38) However, there are some exemptions and the following sources of income must not be treated as notional income:
- (a) income payable under a discretionary trust
- (b) income payable under a trust derived from a payment made as a result of a personal injury where the income would be available but has not yet been applied for
- (c) income from capital resulting from an award of damages for personal injury that is administered by a court
- (d) occupational pension which is not being paid because:
- (i) the trustees or managers of the scheme have suspended or ceased payments due to an insufficiency of resources
- (ii) the trustees or managers of the scheme have insufficient resources available to them to meet the scheme’s liabilities in full
- (e) Working Tax Credit
Disability-related expenditure
39) Where disability-related benefits are taken into account, the local authority should make an assessment and allow the person to keep enough benefit to pay for necessary disability-related expenditure to meet any needs which are not being met by the local authority.
40) In assessing disability-related expenditure, local authorities should include the following. However, it should also be noted that this list is not intended to be exhaustive and any reasonable additional costs directly related to a person’s disability should be included:
- (a) payment for any community alarm system
- (b) costs of any privately arranged care services required, including respite care
- (c) costs of any specialist items needed to meet the person’s disability needs, for example:
- (i) Day or night care which is not being arranged by the local authority
- (ii) specialist washing powders or laundry
- (iii) additional costs of special dietary needs due to illness or disability (the person may be asked for permission to approach their GP in cases of doubt)
- (iv) special clothing or footwear, for example, where this needs to be specially made; or additional wear and tear to clothing and footwear caused by disability
- (v) additional costs of bedding, for example, because of incontinence
- (vi) any heating costs, or metered costs of water, above the average levels for the area and housing type
- (vii) occasioned by age, medical condition or disability
- (viii) reasonable costs of basic garden maintenance, cleaning, or domestic help, if necessitated by the individual’s disability and not met by social services
- (ix) purchase, maintenance, and repair of disability-related equipment, including equipment or transport needed to enter or remain in work; this may include IT costs, where necessitated by the disability; reasonable hire costs of equipment may be included, if due to waiting for supply of equipment from the local council
- (x) personal assistance costs, including any household or other necessary costs arising for the person
- (xi) internet access for example for blind and partially sighted people
- (xii) other transport costs necessitated by illness or disability, including costs of transport to day centres, over and above the mobility component of DLA or PIP, if in payment and available for these costs. In some cases, it may be reasonable for a council not to take account of claimed transport costs – if, for example, a suitable, cheaper form of transport, for example, council-provided transport to day centres is available, but has not been used
- (xiii) in other cases, it may be reasonable for a council not to allow for items where a reasonable alternative is available at lesser cost. For example, a council might adopt a policy not to allow for the private purchase cost of continence pads, where these are available from the NHS
41) The care plan may be a good starting point for considering what is necessary disability-related expenditure. However, flexibility is needed. What is disability-related expenditure should not be limited to what is necessary for care and support. For example, above average heating costs should be considered.
Example of disability related expenditure
Zach is visually impaired and describes the internet as a portal into the seeing world – in enabling him to access information that sighted people take for granted. For example he explains that if a sighted person wants to access information they can go to a library, pick up a book or buy an appropriate magazine that provides them with the information they need.
The internet is also a portal into shopping. For example without the internet if Zach wanted to shop for clothes, food or a gift he would have to wait until a friend or family member could accompany him on a trip out, he would be held by their schedule and they would then have to explain what goods were on offer, what an item looked like, the colour and would inevitably be based on the opinion and advice of said friend. A sighted person would be able to go into a shop when their schedule suits and consider what purchase to make on their own. The internet provides Zach with the freedom and independence to do these things on his own.
Care homes
42) The following section deals with those who are receiving care and support in a care home only.
Personal expenses allowance
43) The local authority must leave the person with a minimum amount of income. This is known as the Personal Expenses Allowance (PEA) and the amount is set out in regulations and updates sent via a local authority circular. Anything above this may be taken into account in determining charges.
44) The PEA is not a benefit but the amount of a person’s own income that they must be left with after charges have been deducted. However, where a person has no income, the local authority is not responsible for providing one. However, the local authority should support the person to access any relevant state benefits or independent advocacy service.
45) The purpose of the PEA is to ensure that a person has money to spend as they wish. It must not be used to cover any aspect of their care and support that have been contracted for by the local authority and/or assessed as necessary to meet the person’s eligible needs. This money is for the person to spend as they wish and any pressure from a local authority or provider to do otherwise is not permitted.
46) There may be some circumstances where it would not be appropriate for the local authority to leave a person only with the personal expenses allowance after charges. For example:
a) Where a person has a dependent child the local authority should consider the needs of the child in determining how much income a person should be left with after charges. This applies whether the child is living with the person or not.
b) Where a person is paying half their occupational or personal pension or retirement annuity to a spouse or civil partner who is not living in the same care home, the local authority must disregard this money. This does not automatically apply to unmarried couples although the local authority may wish to exercise its discretion in individual cases.
c) Where a person is temporarily in a care home and is a member of a couple – whether married or unmarried – the local authority should disregard any Income Support or Pension Credit awarded to pay for home commitments and should consider the needs of the person at home in setting the personal expenses allowance. It should also consider disregarding other costs related to maintain the couple’s home (see below).
d) Where a person’s property has been disregarded the local authority should consider whether the PEA is sufficient to enable the person to meet any resultant costs. For example, allowances should be made for fixed payments (like mortgages, rent and Council Tax), building insurance, utility costs (gas, electricity and water, including basic heating during the winter) and reasonable property maintenance costs.
e) Where a person has moved to local authority support and has a deferred payment agreement (DPA) in place, the local authority should ensure the person retains sufficient resources to maintain and insure the property in line with the disposable income allowance (DIA).
All other settings
47) As all earnings must be disregarded, this leaves other sources of income such as benefits, pensions and payments from other products.
Minimum income guarantee
48) Local authorities must ensure that a person’s income is not reduced below a specified level after charges have been deducted. The amounts are set out in the Care and Support (Charging and Assessment of Resources) Regulations. However, this is only a minimum and local authorities have discretion to set a higher level if they wish. This approach will lead to greater consistency between the charging framework and established income protections under the income support rules. We will keep this under review and seek to update the charging framework in line with the roll-out of Personal Independence Payments and updating/repeal of the income support rules.
49) The purpose of the minimum income guarantee is to promote independence and social inclusion and ensure that they have sufficient funds to meet basic needs such as purchasing food, utility costs or insurance. This must be after any housing costs such as rent and council tax net of any benefits provided to support these costs – and after any disability related expenditure. For example, a council tenant will have water rates as part of a rent service charge whilst a private or housing association tenant will not.
50) Separate guidance applies when determining an appropriate contribution from income under a deferred payment agreement.
Annex D: Recovery of debts
This annex covers:
- the principles underpinning the approach to debt recovery
- options for debt recovery
- processes around debt recovery
1) The Care Act 2014 introduces a modern legal framework for the recovery of any debts that may have accrued as a result of a local authority meeting a person’s eligible care and support needs. Section 22 of the Health and Social Services and Social Security Act (HASSASSA) 1983 was revoked from April 2015 and no new debts can be recovered under that provision. New powers are provided under Section 69 of the Care Act that provides equal protection to both the local authority and the person. Section 70 of the Care Act also provides a local authority with the power to recover charges from a third party where a person has transferred assets to them in order to avoid paying charges for care and support.
2) The reason for the change is that the powers under HASSASSA are unilateral. They allow a local authority to place a charge against a person’s property but do not give the person from whom the recovery of the debt is being pursued the opportunity to seek alternative means for payment. The new powers under Section 69 of the Care Act provide equal protection for both the local authority and the person.
3) Ultimately the Care Act enables a local authority to make a claim to the county court for a judgment in order to recover the debt. As a first port of call, a local authority must offer a person the option of a DPA in order to recover the debt wherever the person could be offered a DPA, and can only make an application to the court should this be refused. In practice, local authorities will wish to consider the full range of options in order to secure the contributions owed to them. This section of the guidance is designed to cover both the alternative options a local authority may wish to consider and what to do should a case proceed to the county court. Implementation support tools will be provided to accompany this guidance and local authorities should consider the information offered in these tools alongside the guidance.
4) Whilst this is a change for social service departments of local authorities, this is not completely new for local authorities as a whole. Local authorities already have set processes for recovering other debts that are owed to it such as rent arrears which may provide some useful experience, and social services departments will want to consider how the new legislation fits with the wider approach of their local authority. Whilst adding the recovery of debts that arise as a result of the provision of care and support services to central teams would be a viable option, given the nature of the client group and the potentially much larger size of the debt, local authorities may wish to consider the merits of embedding their approach within their social care teams. If doing so, they will need to ensure that this function is adequately resourced with clear lines of responsibility for making decisions on taking claims forward as well as ensuring that local authority staff tasked with following up debts are able to effectively liaise with social care practitioners before taking action. In either case a local authority will need to ensure that adequate records are maintained to support a debt to be recovered.
5) When designing their system for debt recovery in social care, local authorities should be aware of the population they are dealing with. Unlike council tax or rent arrears debt, the local authority is not dealing with the general population. Much of this is debt is likely to be from a move into care homes of very frail people in their 80s and 90s, many with dementia. All debt recovery systems should be designed with a full understanding of the needs and capacities of this population to engage with the system being designed.
Principles underpinning the approach to debt recovery
6) The recovery of debts from those who are receiving care and support is a sensitive issue given the potentially vulnerable nature of the client group and local authority’s ultimate responsibility to meet needs. There could also be a variety of reasons why the person has not paid the assessed charge, for example, there could be issues around diminishing capacity, an administrative error or they may have needed to enter hospital meaning they may not have been able to notify the local authority of the change in circumstances or are not easily able to arrange payments. Given this, local authorities will want to bear in mind the following principles when approaching the recovery of debts:
- possible debts must be discussed with the person or their representative
- the local authority must act reasonably
- arrangements for debt repayments should be agreed between the relevant parties
- repayments must be affordable
- court action should only be considered after all other reasonable avenues have been exhausted
7) Local authorities should clearly discuss with the person or their representative at the outset that care and support is a chargeable service and that where the person has been assessed as being able to afford to do so, they will be required to contribute to the cost of that care. It should also be explained that this means there will be invoices and that an agreement should be reached as to whom the invoices are sent, and if the person wishes, that their agreement and authority is obtained for the use of an agent.
8) Local authorities should also bear in mind that they are bound by the public law principle of acting reasonably at all times and must act in accordance with human rights legislation, as well as the wellbeing principle set out in the Care Act. Given this, a local authority will wish to consider all other reasonable avenues before utilising the powers provided under the Act.
9) Before pursing any course of action the local authority should consider whether it is appropriate to recover the debt – although it has the power to do so, and in many cases will wish to do, it does not have to or indeed it may wish to only recover part of the debt. Such circumstances may include:
- where the amount of the debt is small and the costs of recovery would be disproportionate
- the person or their representative could not reasonably have been aware that the asset in question needed to be included in the financial assessment.
10) It should also consider how different approaches might impact on a person’s wellbeing, in line with a local authority’s general duty to promote a person’s wellbeing.
Timing of debt recovery
11) The point at which a debt becomes due continues to be the date at which the sum becomes due to the local authority. This means that, for example, if a bill was sent giving 30 days to pay, the payment becomes due on day 30. For any debts that have accrued prior to the commencement of the Care Act 2014 the time period for recovering that debt continues to be three years as previously set out under Section 56 of the National Assistance Act 1948 as any change to this would be retrospective and unfair. For any new debts that occur after the commencement of the Care Act 2014, the time period to recover debts has been extended to 6 years from the date when the sum became due to the local authority. Where a debt is taking some time to be recovered, provided legal proceedings have issued within the limitation period, enforcement can continue. If it has not, the debt must be written off.
Options to recover debt
12) Local authorities should consider the full range of options available to recover the debt. This is particularly important as if the claim does end up in the court they are likely to consider what efforts have been made to resolve the issue first. Whilst it is at the discretion of the Court to award costs, if no effort has been made to reach an agreement first a judge may hold this against the local authority when considering making an order for payment of the costs in the case. The greater the person’s need, the more effort should be made to resolve the issue positively through the use of effective social work skills. Options may include negotiation, using an advocate to help the person understand the options available to them, supporting the family to gain a power of attorney or deputyship, the local authority itself applying to be a deputy or the use of independent mediation. Local authorities should have regard to Practice Direction – Pre-Action Conduct guidance published by the Ministry of Justice.
13) As a first step, the local authority should contact the person or their representative in an effort to ascertain why the contribution to their care and support costs has not been met. In the first instance this is likely to be by phone, but may also include written communication in an appropriate format or a visit. This should not be a tick box exercise and there should be more than one effort to contact the person by each of these routes in order to simply and quickly address the issue if possible, whilst balancing the need to minimise further delays.
14) In some cases the issue will be easily resolved as a result of the contact, either through the amount being paid or from the offer of a DPA, where appropriate and further detail on this is set out below. However, some cases will be more complex. For example if a person does not meet the eligibility criteria for a DPA, a DPA is refused or there remains a dispute about the amount. Or a person may be unhappy about being placed in a care home and wish to return home, or could be depressed, have mental health needs or dementia. In many cases, social work assistance may be required.
15) The local authority must establish whether the person has the mental capacity to make financial decisions. This is important as a person who lacks capacity to make financial decisions is in a different legal position from someone who has capacity. While both may be liable for their debt, the way to proceed to recover the debt is different.
16) Where a person has mental capacity to make financial decisions, the local authority can proceed to the county court but does have alternative options and should consider these. These can include:
a) Negotiating an agreement: This could be through dealing directly with the person or their representative to broker a solution. This can be done by the local authority which may well support a better outcome, but in some circumstance this may be better led by an independent person such as an advisor or solicitor. In some cases it may be useful to involve an independent advocate to support the person to understand the options available to them.
b) Mediation:
This is where an independent third party assists those involved to reach an agreement. This could be carried out by a professional mediation service, but could also be carried out by anyone who is not involved in the issue, such as an independent social worker or a local voluntary organisation. It is important to understand that it is the people involved, not the mediator, who decide the course of action.
c) Arbitration:
This involves an independent arbitrator hearing both sides of the issue and making a decision on behalf of the parties that will resolve the issue. Local authorities should be aware that arbitration is usually binding on both sides and therefore cannot usually take the case to court after the arbitrator has made a decision.
Diminishing or lack of mental capacity
17) In some cases a debt may have accrued as a result of diminishing or a lack of mental capacity. In such cases, the local authority may need to involve their safeguarding teams. It is estimated by the Alzheimer’s Society that some 80% of people who enter into care homes have dementia. This means that many of those who are being placed in care homes may lack capacity to make financial decisions, and may have not been able to understand financial assessment forms, or the requests for payments. Social workers should be asked to carry out a decision specific capacity assessment where there is a diagnosis of mental impairment or mental disorder, or where the person’s engagement with care planning shows they may lack capacity to make some decisions.
18) The better the local authority’s understanding and application of the Mental Capacity Act 2005, the easier it is to prevent debts from building up and the easier it is to recover them. Where people with dementia or with learning disabilities have relevant mental capacity assessments on file, and where they also have appointed attorneys or deputies to make financial decisions with them or for them, or friends to support them in care planning, the local authority will be clearer about who to involve in financial decision making. This should help lead to less debt, and where it does occur, make it easier to recover.
19) Where a person has an attorney for property and financial affairs or a deputy, these roles give the attorney or deputy the legal authority to make financial decisions on behalf of the person, and require them to consider and engage with any debt recovery on behalf of the person. The local authority can use all the above methods with the attorney or deputy. They can negotiate an agreement, they can offer mediation, or they can use arbitration to recover the debt.
20) Where the person lacking capacity has no attorney or deputy and has substantial debts, then an application for a deputy is required. The application has to be made to the Court of Protection. Where there are family involved with the person, they may make the application to become a deputy. Where the local authority has an in house or contracted deputyship service, and there is no family, this service should make the application. Otherwise the social worker can make the application for the Court to appoint a deputy. While this process may take some weeks, it leads to the appointment of someone who has the legal authority both to make financial decisions and also to execute them – for example, to access bank accounts and make payments. The local authority should also consider the risk of a conflict of interest where it applies to take on a property and financial affairs deputyship.
21) Local authorities should not send threatening letters demanding payment. They should always seek to establish who has the legal authority to make financial decisions and engage with that person.
Recovering debt and deferred payment agreements
22) Where a debt has accrued and a person could be offered a DPA, the local authority must offer the person or their attorney or deputy the option of repaying the debt through a DPA as set out in Section 69(2) of the Care Act 2014. A person could be offered a DPA if they are receiving care in a care home or are renting an extra care property, and the person has a form of security adequate to cover the DPA (usually a property).
23) The local authority is only required to offer the DPA for the amount of the accrued debt and is not obliged to defer any future costs; [footnote 88] however it may wish to consider allowing the person to defer further payments so as to avoid any further accrual of debts.
24) This option is likely to be attractive to a person as the interest rate for DPAs is set by regulations and is lower than the maximum amount the county court can apply. It will also avoid the person needing to meet the costs of the local authority if the county court finds against them. It is also likely to be attractive for a local authority as it will ensure that the debt is secured, is at less risk of default and is likely to be quicker to secure. If a DPA is agreed upon, a local authority must have regard to the guidance set out in Chapter 9.
25) Only where a person refuses the option of a DPA or does not meet the eligibility criteria can a local authority seek to enforce the debt via an application to the county court. A local authority should therefore make sure a refusal, along with the reason, is recorded appropriately.
26) Where a person lacks capacity to make financial decisions, for example because they have severe dementia, and they have substantial debts to the local authority or are likely to accrue them, then the local authority should ask the family to apply for a deputyship. Where there is no family or they choose not to, the local authority should apply for one before they proceed to the county court, bearing in mind the risks of a conflict of interest.
Issuing a claim and subsequent enforcement through the county court
27) Where all other reasonable avenues have been exhausted, a local authority may wish to proceed to the county court in order to recover the debt owed. The county court has been chosen to enable all the parties involved to have an equal say regarding the debt that has accrued.
Getting started
28) Before making a claim, local authorities should read the HM Courts and Tribunal Services (HMCTS) leaflet EX302 How do I make a court claim? and comply with the Practice Direction – Pre-Action Conduct published by the Ministry of Justice The Court will require the local authority to prove the legal basis for their claim. Therefore before applying to the court, local authorities should consult and engage their legal departments and collect the necessary evidence.
29) Issue of claim and other processes, including enforcement, attract a court fee. The level of the fee will vary depending on the amount that is being sought and will vary depending on whether the claim is being issued online or by paper. Details setting out the level of fees can be found in the HMCTS leaflet EX50 Civil and Family Court Fees. Whilst there is an upfront cost to a local authority to meet this fee, if an order or judgment is made in favour of the local authority, the Court may add the fee to the debt recoverable. Any other pre-issue fees the local authority wishes to recover should be included in the claim form. If a solicitor is acting for the local authority, fixed costs may be claimed.
30) In order to make a claim, the local authority will need to fill out the relevant form. This can be done either on paper or online. Conditions apply for claims started online, including that the claim must be for a specified sum of money (under £100,000); that it cannot be against more than 2 people; and it cannot be against a known protected party or child, this includes a person who lacks capacity. Local authorities will also wish to note that fees are often reduced for online applications. Access to the Money Claim online service and registration for an account with the UK Government Gateway is required. The paper based claim form N1 and notes for guidance N1A and N1C can be downloaded from the HMCTS website. It is important that these guidance notes are read carefully. It is at this point that initial fees are required to be paid. If making a paper application this will need to be by cash or cheque and online, by credit or debit card.
31) In order for a local authority to claim interest on the debt, they must include the following text from leaflet EX302: in the section of the form entitled ‘Particulars of claim’:
The claimant claims interest under section 69 of the County Courts Act 1984 at the rate of [8]% a year from [date when the money became owed to you] to [date you are issuing the claim] of £[amount] as well as interest, at the same rate, up to the date of judgment or when the money is paid (if this is earlier) at a daily rate of [daily rate of interest].
32) Once the court has issued the claim, a Notice of Issue will be sent to the local authority and a copy of the claim to the person the local authority is seeking to recover contributions from. The person will then have the options of not responding to the claim, admitting the full amount of the claim, or defending the claim. If no response is received to the claim, or if the person admits part or the whole amount of the claim, and the local authority accepts the part admission, they may request the court to enter judgment against the person. The local authority may then commence enforcement proceedings if the person does not pay the judgment. If the claim is defended or the person does not accept the part admission, the claim will proceed to the next stage and further details are set out below.
33) If the person is a protected party, the local authority may only issue and serve the claim. At this point, any person who lacks capacity to litigate will need to have a litigation friend appointed which involves a separate application. It is the responsibility of the local authority to inform the court that there is a need for a litigation friend. Where the person has a relevant attorney or deputy, that person may be appointed as a litigation friend with the permission of the court. Ultimately it is the court that will appoint the litigation friend. Where a person does not have a relevant attorney or deputy, in making the first step to respond to the claim, the person seeking to become the litigation friend may file a certificate of suitability stating that they satisfy the conditions set out in Part 21 of the Civil Procedure Rules.
34) The role of the litigation friend is to represent the person in court. They may therefore raise any issue that the person would such as disputing the debt, seek alternative arrangements to repaying the debt or raise any other issues they consider relevant to the question of the debt. It is therefore important that the local authority has acted properly in relation to the person who lacks capacity and there is no evidence of any perceived harassment. This must be with regard to both care and debt recovery.
What next?
35) Local authorities should read the HMCTS leaflet EX304, I’ve started a claim in court – what happens next? which sets out the different next steps depending on the person’s response. In all cases, except where steps are being taken in relation to the appointment of a litigation friend, a local authority cannot take any action until the date by which the person must reply to the claim has passed. This date is specified on the Notice of Issue, but the period may be extended by 14 days if the person files an Acknowledgement of Service. The court will inform the person if an acknowledgement is filed.
36) The leaflet sets out details of the action the local authority should take depending on the response from the person. These are:
- how to request a judgment by default if no reply to the claim is received. If a request is not made within 6 months, the claim will be stayed until an application to lift the stay is made
- how to request judgment if the claim is admitted in part or in full
- the next steps if the claim is defended
- how to request issue of enforcement proceedings if the judgment is not paid
37) It is important to remember to check the dates set by the court for response at each stage of the process. If a date is missed, your claim may be stopped – known as ‘stayed’ – and the only way to continue the claim after this period is to apply to the court for an order to lift the stay, for which there may be a fee. This is known as a relief from sanctions which comes with strict criteria and may not always be granted. A local authority will therefore want to ensure it does not miss these dates. The rules in respect of sanctions are set out in Part 3 of the Civil Procedure Rules.
38) If a claim is defended, it will be provisionally allocated to one of three tracks based solely on the value of the claim. These are:
- the small claims track for claims under £10,000
- the fast track for claims of £10,000 – £25,000
- the multi-track for claims over £25,000
39) At this point both the local authority and the person will be directed to complete and return a Directions questionnaire. If the case is allocated to the multi-track, the court will also require the local authority to file a costs budget. Where the case is allocated to the small claims track and both parties indicate they wish to use the in house mediation scheme provided by the HMCTS the mediator will contact the parties with a view to resolving the dispute. If the parties do not wish to use the service or the claim is allocated to one of the other tracks, the claim will be sent to a county court hearing centre. A preference can be indicated on the claim form and Directions questionnaire.
40) On receipt at the county court hearing centre the papers will be referred to a judge for directions. Depending on the value and complexity of the claim the judge will confirm or may change the track allocation. The court may give directions for case management of the proceedings and a hearing may be fixed. In some instances, a further listing and hearing fee will be payable.
Receiving a county court judgment or order
41) Once a final judgment or order has been made, it is not possible to add any further debts that may have accrued. Local authorities will therefore need to think carefully about what steps can be put in place to ensure t#hat a person is able to meet their assessed contribution towards the cost of their care and support. Should debts continue to accrue, a local authority will need to begin the debt recovery process afresh.
Enforcing the judgment or order
42) Where there is a court order or judgment for payment, but the person has not complied with it, the local authority may choose to enforce the order. The HMCTS leaflet EX321 I have a judgment but the defendant hasn’t paid sets out the various options. It is important to note that the court will only issue enforcement proceedings at the request of the local authority.
43) There are various methods of enforcement and local authorities will wish to think carefully about which may be the most appropriate taking into account the person’s circumstances and their own responsibilities to the person. The most appropriate are likely to be one of the following:
- a warrant or writ of control
- an attachment of earnings order
- a third party debt order
- a charging order
44) A warrant or writ of control essentially enables enforcement agents or officers to take control of goods from the person’s home or business. If the order is for £5,000 or less, an application for a warrant of control may be made to the county court. If the order is for over £5,000 the local authority may apply to the High Court for a writ of control.
45) An attachment of earnings order allows for the periodic deduction of monies by the person’s employer (where they are known). It cannot be used if a person is unemployed or self-employed. An application may also be made to the court for deductions to be made from other earnings such as a pension. Earnings are disregarded during the financial assessment of what a person can afford to contribute towards the cost of their care so in some instances, this may be an option.
46) A third party debt order will instruct a third party such as a financial institution that holds a bank or building society account for the person to pay out the available funds, less that financial institution’s fees, to the local authority. The process will only be successful if there are monies in the account on the day the financial institution receives the court order. Third party debt orders may not be made where the account is held in the name of more than one person. Savings are taken into account in the financial assessment of what someone can afford to contribute towards the cost of their care and this may therefore be a suitable option in some cases.
47) A charging order places a charge on a property or other assets owned by the person in order to secure the debt. This means that, just as with a DPA, payment will only be realised when the property or assets are disposed of. A further claim must be made for an order for sale to enforce the charging order. Where a person owns their own property this is likely to be the most viable option for recovering the debt. It is similar to a DPA in that a charge is secured against the person’s property but by order of the court. The charge is usually a first charge unless other charges such as a mortgage are already registered against the property.
48) Further detail on both third party debt and charging orders can be found in the HMCTS leaflet EX325, Third party debt and charging orders – how do I ask for an order?
Other routes
49) Local authorities may also want to consider what other options may be available to support them in the recovery of debts. For example, Section 423 of the Insolvency Act 1986 provides additional routes to recover debts where a person may has transferred or sold their assets to a third party at a price that is lower than the market value with the intention of putting those assets out of reach or, or prejudicing the interests of, someone who may wish to bring a claim against that person. In considering the options, a local authority should seek the advice of its legal department.
Further information
50) HMCTS have developed a number of leaflets to help guide anyone through the court process.
A summary of those already referred to in this guidance and others that may be of use are listed below:
- EX301: I’m in a dispute – what can I do?
- EX302: How do I make a court claim?
- EX304: I’ve started a claim in court – what happens next?
- EX305 and EX306: Small claims track, fast track and multi-track claims in civil courts
- EX321: I have a judgment but the defendant hasn’t paid
- EX325: Third-party debt and charging orders – how do I ask for an order?
- EX50: Civil and family court fees
Complaints
51) A person may wish to make a complaint about any aspect of the way a local authority uses its powers under the Care Act. A local authority must therefore make clear what its complaints procedure is and provide information and advice on how to lodge a complaint and set out details of how to contact the Local Government Ombudsman.
Annex E: Deprivation of assets
This annex covers:
- the deprivation of capital in order to avoid or reduce care and support charges
- the deprivation of income in order to avoid or reduce care and support charges
The purpose of this annex is to provide local authorities with detailed guidance on how to respond when they suspect that a person has deliberately deprived themselves of assets in order to avoid or decrease the amount they are asked to pay towards any care and support charges. For the purposes of this section, ‘assets’ mean capital and/or income.
Setting the context
1) A local authority can choose whether or not to charge a person where it is meeting needs. Where it thinks it would charge the person for meeting at least some of the needs, it must carry out a financial assessment which may be a light touch assessment where appropriate.
2) The financial assessment will need to look across all of a person’s assets – both capital and income – decide which is which and assess those assets according to the regulations and guidance. A local authority therefore must also refer to Annex C on the treatment of income and Annex B on the treatment of capital before conducting a financial assessment.
3) When undertaking or reviewing a financial assessment a local authority may identify circumstances that suggest that a person may have deliberately deprived themselves of assets in order to reduce the level of the contribution towards the cost of their care. In such circumstances, the local authority should have regard to this guidance. Clearly, local authorities should treat this issue with sensitivity and care.
4) People should be treated with dignity and respect and be able to spend the money they have saved as they wish – it is their money after all. Whilst the Care Act 2014 represents an important step forward in redefining the partnership between the state and the individual, it is important that people pay the contribution to their care costs that they are responsible for. This is important to the overall affordability of the care and support system. A local authority should therefore ensure that people are not rewarded for trying to avoid paying their assessed contribution.
5) But deprivation should not be automatically assumed, there may be valid reasons why someone no longer has an asset and a local authority should ensure it fully explore this first. However, the overall principle should be that when a person has tried to deprive themselves of assets, this should not affect the amount of local authority support they receive.
What is meant by deprivation of assets?
6) Deprivation of assets means where a person has intentionally deprived or decreased their overall assets in order to reduce the amount they are charged towards their care. This means that they must have known that they needed care and support and have reduced their assets in order to reduce the contribution they are asked to make towards the cost of that care and support.
7) Where this has been done to remove a debt that would otherwise remain, even if that is not immediately due, this must not be considered as deprivation.
Has deprivation of capital occurred?
8) It is up to the person to prove to the local authority that they no longer have the asset. If they are not able to, the local authority must assess them as if they still had the asset. For capital assets, acceptable evidence of their disposal would be:
- (a) a trust deed
- (b) deed of gift
- (c) receipts for expenditure
- (d) proof that debts have been repaid
9) A person can deprive themselves of capital in many ways, but common approaches may be:
- (a) a lump-sum payment to someone else, for example as a gift
- (b) substantial expenditure has been incurred suddenly and is out of character with previous spending
- (c) the title deeds of a property have been transferred to someone else
- (d) assets have been put in to a trust that cannot be revoked
- (e) assets have been converted into another form that would be subject to a disregard under the financial assessment, for example personal possessions
- (f) assets have been reduced by living extravagantly, for example gambling
- (g) assets have been used to purchase an investment bond with life insurance
10) However, this will not be deliberate in all cases. Questions of deprivation therefore should only be considered where the person ceases to possess assets that would have otherwise been taken into account for the purposes of the financial assessment or has turned the asset into one that is now disregarded.
Example of where deprivation has not occurred
Max has moved into a care home and has a 50% interest in a property that continues to be occupied by his civil partner, David. The value of the property is disregarded whilst David lives there, but he decides to move to a smaller property that he can better manage and so sells their shared home to fund this.
At the time the property is sold, Max’s 50% share of the proceeds could be taken into account in the financial assessment, but, in order to ensure that David is able to purchase the smaller property, Max makes part of his share of the proceeds from the sale available.
In such circumstance, it would not be reasonable to treat Max as having deprived himself of capital in order to reduce his care home charges.
Example of assets to be considered
Emma gives her daughter Imogen a painting worth £2,000 the week before she enters care home. The local authority should not consider this as deprivation as the item is a personal possession and would not have been taken into account in her financial assessment.
However, if Emma had purchased the painting immediately prior to entering a care home to give to her daughter with £2,000 previously in a savings account, deprivation should be considered.
11) There may be many reasons for a person depriving themselves of an asset. A local authority should therefore consider the following before deciding whether deprivation for the purpose of avoiding care and support charges has occurred:
- (a) whether avoiding the care and support charge was a significant motivation in the timing of the disposal of the asset; at the point the capital was disposed of could the person have a reasonable expectation of the need for care and support?
- (b) did the person have a reasonable expectation of needing to contribute to the cost of their eligible care needs?
12) For example, it would be unreasonable to decide that a person had disposed of an asset in order to reduce the level of charges for their care and support needs if at the time the disposal took place they were fit and healthy and could not have foreseen the need for care and support.
Example of assets to be considered
Mrs Kapoor has £18,000 in a building society and uses £10,500 to purchase a car. Two weeks later she enters a care home and gives the car to her daughter Juhie.
If Mrs Kapoor knew when she purchased the car that she would be moving to a care home, then deprivation should be considered. However, all the circumstances must be taken into account so if Mrs Kapoor was admitted as an emergency and had no reason to think she may need care and support when she purchased the car, this should not be considered as deprivation.
Has deprivation of income occurred?
13) It is also possible for a person to deliberately deprive themselves of income. For example, they could give away or sell the right to an income from an occupational pension.
14) It is up to the person to prove to the local authority that they no longer have the income. Where a local authority considers that a person may have deprived themselves of income, they may treat them as possessing notional income.
15) The local authority will need to determine whether deliberate deprivation of income has occurred. In doing so it should consider:
- (a) was it the person’s income?
- (b) what was the purpose of the disposal of the income?
- (c) the timing of the disposal of the income (at the point the income was disposed of could the person have a reasonable expectation of the need for care and support?)
16) In some circumstances the income may have been converted into capital. The local authority should consider what tariff income may be applied to the capital and whether the subsequent charge is less or more than the person would have paid without the change.
Local authority investigations
17) In some cases a local authority may wish to conduct its own investigations into whether deprivation of assets has occurred rather than relying solely on the declaration of the person. There is separate guidance under the Regulation of Investigatory Powers Act 2000 that has recently been updated. That sets out the limits to local authority powers to investigate and local authorities should have regard to it before considering any investigations.
What happens where deprivation of assets has occurred?
18) If a local authority decides that a person has deliberately deprived themselves of assets in order to avoid or reduce a charge for care and support, they will first need to decide whether to treat that person as still having the asset for the purposes of the financial assessment and charge them accordingly.
19) As a first step, a local authority should seek to charge the person as if the deprivation had not occurred. This means assuming they still own the asset and treating it as notional capital or notional income.
20) If the person in depriving themselves of an actual resource has converted that resource into another of lesser value, the person should be treated as notionally possessing the difference between the value of the new resources and the one which it replaced. For example, if the value of personal possessions acquired is less than the sum spent on them, the difference should be treated as notional resource.
Recovering charges from a third party
21) Where the person has transferred the asset to a third party to avoid the charge, the third party is liable to pay the local authority the difference between what it would have charged and did charge the person receiving care. However, the third party is not liable to pay anything which exceeds the benefit they have received from the transfer.
22) If the person has transferred funds to more than one third party, each of those people is liable to pay the local authority the difference between what it would have charged or did charge the person receiving care in proportion to the amount they received.
23) As with any other debt, the local authority can use the county court process to recover debts, but this should only be used after other avenues have been exhausted. When pursing the recovery of charges from a third party, a local authority must read Annex D on debt recovery.
Example of liability of a third party
Mrs Tong has £23,250 in her savings account. This is the total of her assets. One week before entering care she gives her daughters Louisa and Jenny and her son Frank £7,750 each. This was with the sole intention of avoiding care and support charges.
Had Mrs Tong not given the money away, the first £14,250 would have been disregarded and she would have been charged a tariff income on her assets between £14,250 and £23,250. Assuming £1 for every £250 of assets, this means Mrs Tong should have paid £36 per week towards the cost of her care.
After 10 weeks of care, Mrs Tong should have contributed £360. This means Louisa, Jenny and Frank are each liable for £120 towards the cost of their mother’s care.
Annex F: Temporary and short-term residents in care homes
This annex covers how to undertake a financial assessment of someone who is temporarily placed in a care home
Setting the context
1) Following an assessment of a person’s eligible care and support needs a decision may be taken that the person would benefit from a temporary stay in a care home. This could be for a number of reasons such as providing respite care to a carer or to provide a period of more intense support owing to an additional, but temporary, care need.
2) The financial assessment of what they can afford to contribute to the cost of their care and support needs must be undertaken with regard to the following guidance.
3) The financial assessment must be based on the individual resources of the person. However a local authority should give regard to any partner or spouse remaining at home and ensure they are left with a basic level of income support or pension credit to which they may be entitled in their own right.
Who is a temporary resident?
4) A temporary resident is defined as a person whose need to stay in a care home is intended to last for a limited period of time and where there is a plan to return home. The person’s stay should be unlikely to exceed 52 weeks, or in exceptional circumstances, unlikely to substantially exceed 52 weeks.
5) A decision to treat a person as a temporary resident must be agreed with the person and/or their representative and written into their care plan.
6) In some cases a person may enter a care home with the intention of a permanent stay but a change in circumstances could result in it being temporary. In such cases the local authority should treat the person as temporary from the date of admission for the purposes of charging.
7) Similarly a stay which was initially intended to be temporary could become permanent. In such cases, the financial assessment of the person as a permanent resident should only be from the date that the care plan is amended and agreed with the person and/or their representative.
Charging
8) A local authority can choose whether or not to charge a person where it is arranging to meet needs. In the case of a short-term resident in a care home, the local authority has discretion to assess and charge as if the person were having needs met other than by the provision of accommodation in a care home.
Assessing ability to pay
9) Once a local authority has decided to charge a person and it has been agreed that they are a temporary resident, the local authority must undertake the financial assessment in accordance with the following guidance.
Capital
10) The person’s main or only home must be disregarded where the person:
- (a) Intends to return to that property as their main or only home and it remains available to them
- (b) Has taken steps to dispose of the home in order to acquire one that is more suitable and intends to return to that property
11) Any other capital assets should be treated in the same way as for permanent residents. Guidance is set out in Annex B.
Income and earnings
12) Both income and earnings should be treated in the same way as for permanent residents, as set out in Annex C on income. However, any additional amounts the person may need so they can maintain their home during their temporary stay so that it is in a fit condition for them to return to must be disregarded. Such expenses may include, but are not limited to, ground rent, service charges, water rates or insurance premiums.
13) However, the local authority should also take into account the following additional points.
14) Where Attendance Allowance or Disability Living Allowance is being received, these should be completely disregarded. However, a local authority should note that eligibility for both these benefits ceases after 4 weeks of local authority support and they should make sure they consider the impact on the person’s ability to maintain their home.
15) Where a stay in a care home is temporary, the amount of an Income Support or Pension Credit a person receives will usually remain the same as they will be treated as normally residing in their own home. However, any severe disability premium or enhanced disability premium that may have been included will no longer be paid if the Disability Living Allowance or Attendance Allowance has ceased. There are special rules for Income Support and income related Employment Support Allowance where one member of a couple enters a care home for a temporary period. This should be taken into account in considering what a person can afford to pay.
16) If Housing Benefit is paid to the person, this should be disregarded as they will still be responsible for meeting any costs associate with their main or only home.
17) The local authority should also disregard any other payment the person receives in order to meet the cost of their housing and/or to support independent living. For example this may include payments to provide warden support, emergency alarms or the meeting of cleaning costs where the person or someone in the household is unable to do this themselves.
18) The local authority should also consider whether any payments to support the cost of housing and/or independent living are sufficient to cover the person’s commitments during their temporary stay. This might be as these costs were met from earnings, which are disregarded, that are not being accrued during the temporary stay. In such cases, the local authority should calculate the additional cost and disregard this amount.
19) Where a person is sub-letting their property, this should be disregarded where the person occupies the property as their main or only home as they intend to return to the property.
20) Alternatively a person may have a boarder living in their property. A boarder is someone for whom at least one cooked meal is provided. Where a person has income from a boarder, the first £20 of the income should be ignored plus half of any balance over £20.
Annex G: The process for managing transfers of care from hospital for patients with care and support needs
This annex covers:
- overview of the requirements of the regulations
- legibility of notices
- assessment notices (including content, withdrawal and time to carry out assessment)
- interaction with NHS Continuing Healthcare
- discharge notices (including content, withdrawal and timing of discharge notice)
- delayed discharge reimbursement
- days exempt from payment liability
- ordinary residence
- dispute resolution
- sign-off of data between the NHS and local authority
- reporting of all delayed transfers of care days
- data and information
- patient and carer consultation
- patient choice
1) The Care and Support (Discharge of Hospital Patients) Regulations 2014 set out:
- the details of what the NHS body responsible for a relevant patient must include in the assessment notice that it issues, so that the local authority can then comply with its requirements to undertake assessments and put in place any arrangements necessary for meeting any of the patient’s care and support needs or where applicable the carer’s needs
- the minimum period that the local authority has to undertake the assessment
- the details of what must be included in the discharge notice
- the minimum period of notice that the NHS must give the local authority in terms of a relevant patient’s discharge
- the circumstances when an assessment notice and a discharge notice must be withdrawn
- the period and amount of any reimbursement liability which a local authority may be required to pay the NHS for any delayed discharge
2) The regulations also set out what is to happen when a local authority disputes that the patient is ordinarily resident in its area and to recover expenditure incurred as a result.
Legibility of notices
3) All notices issued by the relevant NHS body must be provided in writing to local authorities. This means that each notice (whether an assessment notice, discharge notice or withdrawal notice) must be in a legible form capable of being reproduced (for example, capable of being photocopied, emailed or faxed). Any notice which is not reasonably legible would therefore not be valid. In order to ensure the legibility of all notification notices, the NHS body who issues the notice should type or print the notices and use a digital format wherever possible. This ensures that the receiving local authority can read the information it requires to comply with its duties and helps to prove that a notice has been issued if ever this was disputed.
4) However, while it is important to establish an audit trail, the system which NHS bodies and local authorities set up around issuing notices should not impede good working practice. Where hospitals and local authorities are already operating joint discharge teams, which are often co-located in the same office with access to a shared database, an update to the database may be all that is required.
Assessment notices
5) The NHS is required to issue a notice to the local authority where they consider that an NHS hospital patient in receipt of acute care may need care and support as part of supporting a transfer from an acute setting regardless of whether they intend to claim reimbursement. The relevant local authority who the NHS must notify is the one in which the patient is ordinarily resident or, if it is not possible to determine ordinary residence, the local authority area in which the hospital is situated.
6) The vast majority of people admitted to hospital will not require care and support on discharge. It is important, therefore, that NHS organisations do not issue assessment notices in a precautionary and/or routine way without having satisfied themselves that there is a reasonable prospect that there may be a need for care and support for which arrangements may need to be made in order to ensure a safe discharge.
7) A locally agreed protocol between the NHS and local authorities which allows NHS staff to identify those likely to need care and support on discharge will provide help and advice as to when a patient should be considered to have possible care and support needs, in order to ensure the NHS issue assessment notices appropriately.
8) However, the relevant NHS body must issue an assessment notice where it considers that a patient may require care and support on discharge and the local authority must or may be required to meet such needs. Before issuing any assessment notice, the NHS must consult with the patient and, where applicable, the carer. This is to avoid unnecessary assessments where, for example, the patient wishes to make private arrangements for care and support without the involvement of the local authority. Before issuing an assessment notice, the NHS body must have considered NHS Continuing Healthcare and, if appropriate, completed any assessment of eligibility for NHS Continuing Healthcare.
Whether or not an NHS body can or must issue an assessment notice depends on which of the following scenarios applies in relation to NHS Continuing Healthcare:
a) Where an individual may require care and support from the local authority but is no longer a hospital patient at the time their NHS Continuing Healthcare eligibility decision is made, then an Assessment Notice is not required in order to make the necessary referral to the local authority.
b) Where an individual is still a hospital patient at the time their NHS Continuing Healthcare eligibility decision is made, if the decision is that the individual is not eligible, then an Assessment Notice must be issued if the NHS consider that the individual may require care and support from the local authority as part of supporting their transfer from the hospital setting.
c) Where an individual has been discharged from hospital into NHS-funded intermediate care to support their recovery before a decision is made whether or not to consider them for NHS Continuing Healthcare, if that subsequent decision is that the individual is not eligible for NHS Continuing Healthcare, then the NHS may decide to notify the local authority of further care and support needs for this individual (but this would not need to be through issuing an Assessment Notice).
d) Where the individual has an existing package or placement which all relevant parties agree can still safely and appropriately meet their needs without any changes, then they should be discharged back to this placement and/or package under existing funding arrangements. An Assessment Notice would not need to be issued. In such circumstances any screening (with a checklist) for NHS Continuing Healthcare, if required, should take place within 6 weeks of the individual returning to the place from which they were admitted to hospital.
In order to consider NHS Continuing Healthcare, the NHS body must either:
a) be clear that there is no need for NHS Continuing Healthcare at this point in time; where relevant, this decision and its reasons should be recorded and, if there is doubt between practitioners, an NHS Continuing Healthcare Checklist should be undertaken
b) screen (with a checklist) for NHS Continuing Healthcare
c) undertake a full assessment of eligibility for NHS Continuing Healthcare
Where the NHS considers that the patient may have a need for NHS Continuing Healthcare (b and c above), it must, before issuing an Assessment Notice, have:
a) carried out either a checklist and/or NHS Continuing Healthcare assessment first
b) made a decision as to what (if any) services the NHS is to provide to the patient after discharge
c) informed the local authority of these details
For further guidance on the interaction between hospital discharge and an assessment of eligibility (including screening with a checklist) for NHS Continuing Healthcare, reference should be made to the national framework for NHS Continuing Healthcare (paragraphs 108 to 117 of the 2018 national framework or practice guidance note 13 in the 2012 national framework).
Where applicable, the NHS body must also have made a decision on what services the NHS will be providing when issuing a discharge notice.
Timescales for NHS to issue an assessment notice
9) In general, the NHS should seek to give the local authority as much notice as possible of a patient’s impending discharge. This is so the local authority has as much notice as possible of its duty to undertake a needs and (where applicable) carer’s assessment. Local agreements should be in place between NHS bodies, local authorities and other relevant partners that set out each organisation’s role and how responsibilities are to be exercised, including intermediate or interim arrangements for step-down or sub-acute care, in order to achieve timely and safe hospital discharge.
10) However, an assessment notice must not be issued more than 7 days before the patient is expected to be admitted into hospital. This is so the notice is not provided too far in advance of admission to avoid the risk of wasting preliminary planning in the event that the patient’s condition changes. A balance should be struck between giving the local authority early notice of the need to undertake an assessment of the patient and the risk that the patient’s condition may change significantly such that any early planning needs to be reviewed.
11) Accordingly, if the NHS is able either to issue an assessment notice up to 7 days before the date of the patient’s admission into hospital and/or have a good indication of the likely proposed discharge date which is unlikely to change, then the NHS should issue the assessment notice as soon as possible.
Content of assessment notice
12) The information contained in an assessment notification is intended to be minimal, both to reflect patient confidentiality requirements and to minimise bureaucracy – it is only the trigger for assessment and care planning.
13) The assessment notice must state that it is an assessment notice given under paragraph1(1) of Schedule 3 to the Care Act 2014. This is so the local authority is aware of the consequences that could flow from the receipt of the assessment notice (for example, that it has to take steps to assess the patient and (where applicable) the patient’s carer and put in place any arrangements to meet those needs it proposes to meet. Ultimately if the local authority fails to carry out such steps then the local authority may, in certain circumstances, be liable to pay the NHS for any delayed discharge period.
14) The assessment notice must include the following:
- the name of the patient
- the patient’s NHS number
- if given before the patient’s admission, the expected date of admission and the name of the hospital in which the patient is being accommodated
- an indication of the patient’s discharge date, if known
- a statement:
- (a) that the NHS body that has given the assessment notice (‘the NHS body’) has complied with the requirement to consult the patient and, where feasible, any carer the patient has
- (b) that the NHS body has considered whether or not to provide the patient with NHS Continuing Healthcare and the result of that consideration. So, where the NHS considers that the patient may have needs for continuing health care to be met by the NHS after discharge, then it must have (i) carried out a continuing health care assessment first and (ii) made a decision as to what (if any) services the NHS is to provide to the patient after discharge and (iii) informed the local authority of these details.
- (c) as to whether the patient or carer has objected to the giving of the notice
- (d) the name and contact details of the person at the hospital who will be responsible for liaising with the local authority in relation to the patient’s discharge from that hospital. This must be one or a combination of the person’s telephone number and/or their work based e-mail address.
15) The requirements above are intended to make the assessment notice process work more effectively, including the requirements to include the patient’s NHS number and also the contact details of the person at the hospital who will be responsible for liaising with the local authority in relation to the patient’s discharge from that hospital.
16) These requirements may be built on at a local level to produce a form that meets the agreed needs of the NHS and local authority. Although not exhaustive, local systems might also want to include on the assessment notice the patient’s address and the lead clinician’s details. The following list provides a model that the NHS might want to use:
NOTICE OF REQUEST FOR Assessment under The Care and Support (Discharge of Hospital Patients) Regulations 2014
- Name
- Date of birth
- Address*
- NHS number
- Expected date of admission (where known)
- Expected date of discharge (where known)
- Name and contact details of the carer (where applicable)*
- Name and contact details of the person at the hospital liaising with the local authority
-
Patient’s lead clinician at hospital*
- please confirm the following:
- the patient has been consulted with regarding the assessment
- (where applicable and feasible) carer has been consulted regarding the assessment
- (where applicable) an assessment of their continuing healthcare needs has been completed and a decision that they are not eligible has been made
- the patient has not objected to the giving of the assessment notice
- the carer has not objected to the giving of the assessment notice
Those marked with an * are not legal requirements but should be included where known, as a matter of good practice.
Timescales for local authorities’ responsibilities to carry out assessments
17) On receiving an assessment notice, the local authority must carry out a need assessment of the patient and (where applicable) a carer’s assessment so as to determine, in the first place, whether it considers that the patient and where applicable, carer has needs. If so, the local authority must then determine whether any of these identified needs meet the eligibility criteria and if so, then how it proposes to meet any (if at all) of those needs. The local authority must inform the NHS of the outcome of its assessment and decisions.
18) To avoid any risk of reimbursement liability, the local authority must carry out a needs assessment and put in place any arrangements for meeting such needs that it proposes to meet in relation to a patient and, where applicable, carer, before ‘the relevant day’. The relevant day is either the date upon which the NHS proposes to discharge the patient (as contained in the discharge notice – see below) or the minimum period, whichever is the later.
19) The minimum period is 2 days after the local authority has received an assessment notice or is treated as having received an assessment notice.
20) Any assessment notice which is given after 2pm on any day is treated as being given on the following day.
21) The following examples show how these timescales work.
Example 1
The NHS issues an assessment notice to the local authority at 1pm on Monday. The assessment notice must specify the date of the proposed discharge date. The earliest date which would be permitted is 2 days after the date the assessment notice is given (although a later proposed discharge date could be set out in the discharge notice.) This means that in order to avoid any risk of reimbursement liability, Wednesday would be the earliest day by which the local authority would need to have carried out the assessment and put in place any care and support services and, where applicable, carers’ services that it proposes to meet.
Example 2
The NHS issues an assessment notice to the local authority at 3pm on Monday. The assessment notice is treated as having been given on the following day, Tuesday. This would mean that if no later discharge notice were given in the assessment notice, then Thursday would be the earliest day by which the local authority would need to have carried out the assessment and put in place any care and support services and, where applicable, carers’ services that it proposes to meet if it were to avoid the risk of any reimbursement liability. Again, the assessment notice and later the discharge notice (see below) could set out a proposed discharge date after Thursday, in which case this would be the actual deadline by which the local authority would be required to have carried out the assessment and put in place any care and support and carers’ service that is proposes to meet in order to avoid the risk of incurring any reimbursement liability.
Assessment notice withdrawal
22) The NHS body which issued the assessment notice may withdraw that assessment notice at any time. Once an assessment notice has been withdrawn by the NHS, this means that the local authority that has been given the assessment notice is no longer required to comply with the requirements to assess or, where an assessment has been carried out, to put in place arrangements to meet some or all of the patient’s care and support needs. Once an assessment notice is withdrawn no liability to the local authority can accrue after that date. This is even if a discharge notice has been subsequently issued. But any liability which may have accrued before the withdrawal of the assessment notice is unaffected.
23) There are a number of circumstances when the NHS must withdraw an assessment notice. These are where:
- the NHS body considers that it is likely to be safe to discharge the patient without arrangements being put in place for the meeting of the patient’s needs for care and support or (where applicable) the carer’s needs for support
- the NHS body considers that the patient’s on-going need is for NHS Continuing Healthcare
- following the decision as to which (if any) services the relevant local authority will make available to the patient or (where applicable) carer, the NHS body still considers that it is unlikely to be safe to discharge the patient from hospital unless further arrangements are put in place for the meeting of the patient’s care and support needs or (where applicable) the carer’s needs for support
- the patient’s proposed treatment is cancelled or postponed
- the NHS body has become aware that the relevant authority is not required to carry out any assessment because the patient has refused a needs assessment or (where applicable) the carer has refused a carer’s assessment
- the NHS body becomes aware that either one of the following applies:
- the patient’s ordinary residence has changed since the assessment notice was given
- the notice was given to a local authority other than the one in whose area the patient is ordinarily resident
24) The regulations do not prescribe what a withdrawal notice must contain. However, it must be in writing, and local systems should be established to ensure that the withdrawal notice provides sufficient information for both the NHS and local authority to be clear as to which patient and assessment notice the withdrawal notice refers to, and the reason(s) as to why the assessment notice is being withdrawn. In the context of identifying the person, mirroring either in full or part what is required for the assessment notice itself should be considered.
Discharge notices
25) Patients and carers should be informed of the discharge date at the same time as or before the local authority. In addition, hospital staff may give the local authority an early indication of when discharge is likely as part of helping their planning.
26) Where the NHS has issued an assessment notice to a local authority (so as to require the local authority to assess a patient’s care and support needs to facilitate a transfer of care), it must also give written notice to the local authority of the proposed date of the patient’s discharge notwithstanding that it included the proposed discharge date in the assessment notice. This is known as a discharge notice and its purpose is to confirm the discharge date as it either may not have been previously known at the time of the issue of the assessment notice or may have subsequently changed since the assessment notice was issued.
27) The NHS could not seek to recover any reimbursement from the local authority in respect of a patient’s delayed transfer of care unless it has first issued both an assessment notice and a discharge notice.
Content of a discharge notice
28) A discharge notice must contain:
- the name of the patient
- the patient’s NHS number
- the name of the hospital in which the patient is being accommodated
- the name and contact details (telephone and/or email) of the person at the hospital who is responsible for liaising with the relevant authority in relation to the patient’s discharge from hospital
- the date on which it is proposed that the patient be discharged
- a statement confirming that the patient and, where appropriate, the carer has been informed of the date on which it is proposed that the patient be discharged
- a statement that the discharge notice is given under paragraph 2(1)(b) of Schedule 3 to the Act. This is to make it clear that the notice is a formal ‘discharge notice’ for the purposes of the Discharge of Hospital Patient provisions
Timing of discharge notice
29) To ensure that a local authority receives fair advance warning of the discharge, the NHS body must issue a discharge notice indicating the date of the patient’s proposed discharge. The minimum discharge notification allowed is at least one day before the proposed discharge date. Again, where the discharge notice is issued after 2pm, it will not be treated as having been served until the next day.
30) Taking the examples above:
Example 1
The NHS issues an assessment notice to the local authority at 1pm on Monday. The assessment notice must specify the date of the proposed discharge date where known. The earliest discharge date which would be permitted to be specified is 2 days after the date the assessment notice is given (although the proposed discharge date can be later than this) for example, Wednesday. This means that where the minimum period were to apply, the discharge notice must be issued no later than Tuesday.
Example 2
The NHS issues an assessment notice to the local authority at 3pm on Monday. The assessment notice is treated as having been given on the following day, Tuesday. This would mean that if the minimum period were to apply then Thursday would be the earliest date by which the local authority would need to have carried out the assessment and put in place any care and support services and, where applicable, carers’ services that it proposes to meet if it were to avoid any risk of reimbursement liability. So, this means the discharge notice must be issued no later than Wednesday.
31) The NHS body can issue the discharge notification with a much longer period of advance warning if appropriate and it should continue to seek to provide the local authority with as much notice of the proposed discharge date as possible. However, it will need to consider the likelihood of such a date being inaccurate and then the potential need to withdraw and reissue the discharge notification in the event the patient’s condition changes in the meantime.
32) The NHS body is required to inform the local authority, by way of a withdrawal notice withdrawing the discharge notice, when it considers that it is no longer likely to be safe to discharge the patient on the proposed discharge date for any reason other than the fact that it would be likely to be unsafe to discharge the patient because the local authority has not taken the require steps. So, for example, the NHS must inform the local authority of changes in circumstances affecting the discharge date, for instance if the patient’s medical condition changes or the patient dies.
33) The NHS should also consider the appropriateness of issuing the assessment and discharge notices too closely together, as this may result in extremely short time frames for local authorities to put in place what may be complex and comprehensive packages of care, which will also need to be subject to discussion with the patient and/or their carer. This potentially could lead to decisions being made, which while supporting a safe discharge may not be in the best long-term interests of the patient.
Withdrawal of discharge notice
34) The NHS body which issued the discharge notice to a local authority may withdraw that discharge notice at any time. Such a withdrawal must also be in writing. It is important that the NHS body informs the local authority as soon as possible of a withdrawal of a discharge notice so that the local authority is not unnecessarily expending resources arranging a discharge on a date, which is no longer correct.
35) A discharge notice must be withdrawn where the NHS body considers that it is no longer likely to be safe to discharge the patient from hospital on the proposed discharge date.
36) However, this does not apply where the reasons for withdrawal are that the local authority has not taken the steps required to inform the NHS body of the outcome of the assessment the needs of the patient (and the carer, where applicable), and whether it Intends to put in place care and support to meet any eligible needs.
37) Local systems should be established to ensure that the withdrawal notice provides sufficient information for both the NHS and local authority to be clear who the person is that the notice refers to, and the reason(s) as to why it is being withdrawn. In the context of identifying the patient, mirroring either in full or part what is required for the discharge notice itself should be considered.
38) Once a discharge notice is withdrawn, no further liability for the local authority to pay the NHS for any delayed transfer of care arises.
Delayed discharge reimbursement
39) While reimbursement remains available for use by the NHS body, they and local authorities are encouraged to use the provisions on the discharge of hospital patients (such as the issue of assessment and discharge notices) to seek to focus on effective joint working so as to improve the care of those people whose needs span both NHS and local authority care settings. While reimbursement is a potential way of exposing local difficulties in the relationship between the NHS body and the local authority, NHS bodies should not use reimbursement as the first approach to address any local difficulties around delayed transfers of care.
40) The NHS will only be able to seek any reimbursement from the local authority arising from a delayed transfer of care, if the NHS has first sent both an assessment notice and a discharge notice to the local authority, but the local authority has then either not carried out an assessment or put arrangements in place for the meeting of care and support and, where applicable, carer’s needs which it proposes to meet by the end of the relevant day (for example, the proposed delayed discharge date in the discharge notice or the minimum period and it is for this reason alone that there has been a delay in the patient’s delayed transfer of care.
41) In these circumstances, it is then in the NHS’s discretion whether to recover payments for reimbursable delayed discharge days. In terms of the level of reimbursement, the regulations provide that:
- for local authorities outside London, the penalty amount per day will be £130
- for London authorities, the penalty amount per day will be £155
42) The amounts above have risen in line with the Consumer Price Index (CPI) measure of inflation since 2003, and the higher rate only applies to local authorities in London.
43) The period for which liability can be sought, if the NHS so chooses, starts on the day after the relevant day for example, after the date of the proposed discharge date contained in the discharge notice or the minimum period which is, at the earliest, 2 days after the assessment notice is given.
44) It then ends on the earliest date as to when any of the following occurs:
- the NHS withdraws either the assessment notice or the discharge notice
- the local authority notifies the NHS that it has now carried out the assessment and put in place arrangements for meeting any of the needs it proposes to meet in respect of that patient or where applicable carer
- the local authority is no longer required to put arrangements in place either because the patient informs the local authority that they have made alternative arrangements for care and support and ,where applicable, the carer informs the local authority that they have made alternative arrangements for their support
- the patient discharges themselves
- the NHS decided that the patient now needs to remain in hospital for a further course of treatment
- the patient dies
Days exempt from payment liability
45) It is intended that both the NHS and local authorities should have established systems in place by April 2015 that provide for 7-day coverage. Accordingly, the exemptions that previously existed for weekends and Bank Holidays are no longer to apply and as such all days become potentially reimbursable. However, a day is not to be treated as a day for which a local authority could be liable for reimbursement when the local authority has by 11am that day put in place arrangements for meeting some or all of the needs that it proposes to meet in relation to the patient and, where applicable, the carer.
46) Also, no liability will arise for any day where the NHS considers that the patient is not able to be discharged because they have suffered a deterioration in their condition on that date so that it would not be safe to discharge them even if the local authority had put in place arrangements for meeting the patient’s care and support and, where applicable, the carer’s needs.
47) If the patient’s deterioration becomes more established such that the patient requires a further course of treatment in hospital, and it would be unsafe to discharge the patient then the NHS body must withdraw the discharge notice and should consider withdrawing the assessment notice.
Ordinary residence
48) The NHS should serve the assessment notice on the local authority where the patient is ordinarily resident or where the patient has no settled address, the local authority in which the hospital is located. Where a local authority disputes the assertion that they are responsible for that individual based on ordinary residence, they must in the period of dispute still comply with the requirements of the Regulations in terms of providing an assessment and any care and support provision which is identified as being needed to secure a safe transfer from one care setting to another.
Dispute resolution
49) Where any dispute arises because a local authority disputes that the patient is ordinarily resident in its area (so that it should not be the local authority to whom an assessment notice is given), then that local authority must accept provisional responsibility and undertake the steps required under the discharge of hospital patient provisions. If no agreement can be reached on ordinary residence, it must then seek a determination as the patient’s ordinary residence from the Secretary of State or an appointed representative. Further information on this process can be found within the ordinary residence regulations, which have also been established as part of the Care Act 2014.
50) All other disputes in relation to delayed discharge payments (for example: whether to seek reimbursement, whether the day should be counted as a day of delayed discharge period) should be resolved between the NHS body and local authority. Where they cannot be resolved then resolution would have to be way of an application for judicial review to the High Court.
Sign-off of data between the NHS and local authority
51) As set out in existing guidance, the NHS organisation must ensure that before reporting days attributable to care and support that it has verified their accuracy with the local authority, irrespective of whether the NHS body is seeking reimbursement or not. This should happen in advance of them being reported into the formal system so that any errors can be identified and addressed. The system by which this happens is for local determination, although it is expected that it would be the relevant Director of Adult Social Services or their nominated representative who would be the local authority point of contact for this.
Reporting of all DTOC days
52) Irrespective of whether the delayed days fall into the reimbursement category or not, they must be reported by the relevant NHS body, this is reflected in the NHS Operational Guidance delivered via SitRep. These days include any person with a delayed discharge at any point in the given month, as well as that those patients who meet the Delayed Transfers of Care (DTOC) definition on the last Thursday of each month. In terms of definition, DTOC mean that individuals are in a setting that is recognised as not being appropriate for the care they need. This potentially contributes to worse outcomes for the individual, particularly in the context of their quality of life, as well as placing additional and sometimes costly burdens on the NHS and local government. The definition of a DTOC provided for within SitRep is when a patient is ready for transfer after being in receipt of acute care but is still occupying a bed even though:
- clinical decision has been made that a patient is ready for transfer
- a multi-disciplinary team decision (involving the NHS body and the local authority) has been made that a patient is ready for transfer
- the patient is safe to discharge/transfer
Data and information
53) The exchange of data needed for the purposes of NHS bodies and local authorities carrying out their respective functions is allowed in accordance with the common laws of confidentiality and data protection legislation. It is the responsibility of the individual bodies to ensure they have robust data protection safeguards in place to ensure a patient’s personal data is kept secure and only used for the purposes that it is required (for example, seen by those it needs to be seen by on a needs to know basis).
Patient and carer involvement
54) It is fundamental that both the NHS body and the local authority involve the patient and, if appropriate, their carer about their current and ongoing care and support needs. In doing this, it should have already undertaken an assessment of the patient’s capacity to participate in an informed way in these discussions and, where they do not believe that the capacity exists, they should move forward by taking account of other existing regulation and guidance such as for example the Mental Capacity Act.
Other relevant considerations
55) Other provisions and requirements under the Care Act may also be relevant to considerations arising to the discharge of hospital patients with care and support needs. Reference should be made to these, most notably those relating to:
- wellbeing
- prevention
- assessment and care planning
- carers
- duty to co-operate
- integration
- safeguarding
- ordinary residence
- continuity of care
Annex H: Ordinary residence
People with ‘urgent needs’
1) A person who is ordinarily resident in one local authority area may become in urgent need of accommodation whilst they are in another local authority area. The Care Act provides local authorities with powers [footnote 89] to meet the person’s needs in such urgent cases, if the adult (or in the case of a carer, the adult for whom they care) is known to be ordinary resident in the area of another local authority.
2) For example, an urgent need for accommodation may arise where a person with severe learning disabilities is on holiday or visiting someone with their carer in another area, and the carer unexpectedly has to be taken to hospital. In this case, the person with learning disabilities may be without assistance and/or unable to care for himself or herself, and may become in urgent need of accommodation, albeit on a short-term basis. Similarly, an urgent need may arise where an older person, who is ordinarily resident in one local authority area, stays with their family in another local authority area during a holiday period, but the caring responsibilities prove too much for the family and they seek assistance from their local authority on the basis that their relative is in urgent need.
3) In circumstances where a person who is ordinarily resident in one local authority area becomes in urgent need in another local authority area, the person’s local authority of ordinary residence would have a duty to meet the person’s eligible needs. However, since it is unlikely to be practicable for that authority to meet urgent needs, the local authority ‘of the moment’ (for example, where the person is physically present at the time) should exercise their power to meet the urgent needs and provide the necessary accommodation, even if only on a temporary basis. The local authority of the moment should, in carrying out any assessment of needs and providing any necessary accommodation, inform the local authority where the person is ordinarily resident that it is doing so.
4) The local authority of the moment is not required to seek the consent of the local authority where the person is ordinarily resident, in deciding whether and how to exercise the power to meet urgent needs. However, it should notify the other authority of its intention to do so, to ensure that information is shared on the individual case. The local authorities concerned may come to an agreement about sharing or transferring the costs involved in meeting urgent needs. For instance, the local authority of the moment, which is providing the accommodation, may recover some or all of the costs of the accommodation from the local authority where the person is ordinarily resident (and where the duty to meet needs would otherwise fall).
5) On rare occasions, a person with urgent needs who has been provided with accommodation by the local authority of the moment may be unable to return to their own local authority because of a change in circumstances. In this situation, decisions relating to ordinary residence must be made on an individual basis: the local authority of the moment and the person’s local authority of ordinary residence would need to consider all the facts of the case to determine whether the person’s ordinary residence had changed.
6) A local authority may also meet a person’s needs through the provision of accommodation, where the person is not ordinarily resident in that area, even if the needs themselves are not considered to be urgent.
7) For example, a local authority (local authority A) may need to provide accommodation on behalf of another (local authority B) in a situation where a person has been discharged from hospital and needs accommodation but wishes to remain living in the local authority in which he or she received hospital treatment, perhaps to be near family members. In these circumstances, local authority A, where the person was living on discharge from hospital could provide the accommodation, with the notification of his or her local authority of ordinary residence (local authority B). However, if the person subsequently intended to remain in local authority A indefinitely, then their place of ordinary residence would move to local authority A.
People who are party to deferred payment agreements
8) Deferred payment agreements are designed to prevent people from being forced to sell their home in their lifetime to pay for the costs of their care. They also extend choice, providing people with additional flexibility over how they meet the cost of their care.
9) An individual enters into an agreement with their local authority by which payment for their care and support is ‘deferred’, being paid in the interim period by the local authority. The money owed to the local authority is subsequently repaid either when the home is sold, from the person’s estate, or when the amount due is repaid to the local authority. The local authority could be repaid by either the person with the deferred payment agreement or by a third party. The individual grants the local authority a charge over their property for the purposes of security and to facilitate reclamation of the amount due to the local authority.
10) The regulations and guidance require local authorities to offer deferred payments in certain circumstances, and give local authorities discretion to offer deferred payments in other situations. For further information on deferred payments please see chapter 9 of the guidance.
11) It is the local authority in which the person is ordinarily resident that has responsibility for offering and making arrangements for a deferred payment agreement. That local authority then remains responsible for the deferred payment agreement until the agreement is concluded.
12) Information about deferred payment agreements should be offered when a person approaches a local authority, or at the time the person decides to enter a care home accommodation. Where a person is initially accommodated under the 12-week property disregard, the information should be given and arrangements made during this 12-week period. For details on this please see Annex B and the treatment of capital.
13) For example, where a person who is ordinarily resident in the area of local authority A chooses to meet their care and support needs in a care home in the area of local authority B, and the value of that person’s home is being disregarded for 12 weeks, (see Annex H3 – People who are accommodated under the 12 week property disregard), local authority A should offer the person the option of having a deferred payment during the 12-week period. If the person accepts the offer and enters into a deferred payment agreement, local authority A remains responsible for funding their care (minus any contributions from means-tested income and assets).
People who are accommodated under the 12 week property disregard
14) An important aim of the charging framework is to prevent people being forced to sell their home at a time of crisis. The framework therefore creates the space for people who are at risk of needing to sell their home to meet the cost of their care to make informed decisions on how best to do that. This means that a local authority must disregard the value of a person’s main or only home when the value of their non-housing assets are below the upper capital limit of £23,250 for a period of 12 weeks from when a person either:
- first enters a care home
- where an alternative property disregard is unexpectedly lost
15) A local authority also has discretion to choose to apply the disregard where a person has a sudden and unexpected change in their financial circumstances. In doing so, it must consider the individual circumstances of the case.
16) This is known as the ‘12 week property disregard’ and full details are set out in Annex B on the Treatment of Capital.
17) During the 12 week disregard period, the person receives local authority support where they are ordinarily resident. The local authority may place the person in a care home in the area of another local authority, for example because they have expressed a desire to be near family members. However, the placing authority remains the responsible authority during this period.
18) At the end of 12 weeks, the value of the person’s home is taken into account (unless it is subject of an alternative disregard. See Annex B). This may result in the person becoming liable to pay for all of the costs of their care and choosing to enter into a private contract with the care home for the provision of their care on a permanent basis, rather than continuing to be provided with accommodation by their placing authority. In such a case the person would be likely to acquire an ordinary residence in the new area, in line with the settled purpose test in Shah.
19) If the person’s needs or circumstances change and they subsequently require additional or different care and support, including care home support, they should approach the local authority where their care home is situated. However, if they enter into a deferred payment agreement with the original authority or there is another reason such as lack of mental capacity as to why they were unable to enter into a private contract with the care home, they will remain the responsibility of the original authority.
20) If a person arranges for their care and support needs to be met in a care home without regard to the local authority but subsequently contact the local authority in order to receive support, it is likely that they would have acquired ordinary residence in the area in which their care home is situated. If this is the case, it would be the local authority in whose area the care home is situated which would be responsible for funding the person’s accommodation.
People who have sufficient funds to pay for their own care and accommodation
21) When a person moves into permanent accommodation in a new local authority area under private arrangements, and is paying for their own care, they usually acquire an ordinary residence in this new area. If so, and if their needs subsequently change, meaning that they require other types of care and support, (or if their financial circumstances change so that they would not have to pay for all of the costs of their care and support, if their needs were met by a local authority) they may approach the local authority in which their accommodation is situated. That local authority will be responsible for assessing whether it should meet their needs. The person will be ordinarily resident in the local authority area where the person’s care home is situated.
22) Sometimes, a person with sufficient means to pay for their accommodation in a care home, who was intending to arrange their own care, may not be able to enter into a private agreement with a care home. If this is because they do not have the mental capacity to do so and they either have no attorney or deputy to act on their behalf, or another person in a position to do so, the local authority must meet their needs. Therefore if their assessed needs are required to be met by the provision of accommodation in a care home, the local authority must provide that accommodation (and it will do so by arranging for an independent care home provider to provide it) for which the authority may charge the adult.[footnote 90]
23) In other cases, the person may have capacity, but is not able to manage the making of the arrangements without assistance. In these circumstances the authority may provide information, advice and guidance, or refer the person to an independent broker (someone who can help them find and negotiate terms with a care home). Alternatively, under section 19 of the Care Act, it may decide to meet the person’s needs by arranging the accommodation (which it will normally do by arranging for an independent care home provider to provide the accommodation). The local authority should consider doing so where the person’s wellbeing would otherwise be adversely affected, in particular where there is no one else able to act on their behalf. In either case, if the person’s needs which the local authority is meeting can only be met in a type of specified accommodation, the person would remain ordinarily resident in their placing local authority, even if the accommodation arranged by it is in another local authority area. In such circumstances, if the person’s needs change, or their financial resources change so that they may not have to pay the local authority all of the costs for meeting their needs, they should approach the local authority which has arranged the placement and is currently meeting their needs.
Example 1: people who are arranging and paying for their care home placement
Wendy is 82 years old and very frail. Following a fall and a stay in hospital, she is assessed as having eligible needs for care and support under the Care Act. A financial assessment undertaken by her local authority, local authority A, concludes that she does not qualify for local authority financial assistance.
Wendy wants to arrange her own care and support, but does want some help in choosing the right care home. Local authority A provides advice to Wendy and her family on care homes in Local authority A and surrounding areas and help her to select a home that best meets her requirements. The care home is located in local authority B, as Wendy has expressed a desire to move closer to her family. Wendy moves into the care home as a self-funder and signs a contract with the care home for the provision of her care.
Sometime after Wendy moves into the care home, her savings fall below the capital limit and she approaches local authority A for support. She is advised by local authority A that she is no longer ordinarily resident in their local authority and that she should seek financial assistance from local authority B. Local authority B conducts a needs assessment and agrees Wendy’s needs can only be met in residential accommodation like the care home she is living in and agrees to meet the costs, but immediately falls into dispute with local authority A over her place of ordinary residence and therefore which local authority should pay the costs. Local authority B disagrees with A’s argument that Wendy has acquired an ordinary residence in their area and contends that she remains the responsibility of local authority A as that is where she has lived for most of her life.
Under the Care Act, Wendy is deemed to continue to be ordinarily resident in the area in which she was ordinarily resident immediately before her accommodation was provided by a local authority under the Act. Immediately before Wendy was provided accommodation, she was living in the same care home, but was responsible for paying for her own care. She had voluntarily left local authority A and moved to the care home in local authority B, which she had adopted voluntarily and for settled purposes. Therefore, Wendy is found to be ordinarily resident in local authority B.
Example 2: a local authority uses discretionary powers to meet a person’s needs by arranging a care home in another local authority area
Ewan is a frail and older man who has been referred to his local authority for a needs assessment following a hospital admission after a house fire at the bungalow which he owns. His resources are assessed as above the financial limit. The injuries he sustains have resulted in a physical disability, which compounded by his frailty mean he has eligible care and support needs which can only be met in a care home. Ewan has no other family.
His only friends are in a care home in a neighbouring local authority. Ewan is well enough to leave hospital but is finding it difficult to come to terms with his situation. When the local authority he lives in (local authority A) offers information and advice about his options, he asks if they could arrange his care directly in a care home in a neighbouring local authority (local authority B) so he can be with his friends. Local authority A decides to use its powers under section 19 of the Act to meet his needs by arranging a contract between themselves and the care home provider of Ewan’s choice in local authority B, and arrange to recover the costs from him. Once this arrangement is put in place, Ewan had been ordinarily resident in local authority A immediately before his accommodation was provided by that authority in a care home in local authority B, he therefore remains ordinarily resident in local authority A. Local authority A currently has a contract with the care home and recovers the amount from Ewan.
A year later Ewan becomes eligible for social care funding because his resources have depleted, though, following a needs assessment, his needs have not significantly changed. Local authority A continues to be responsible for meeting his needs, and is required to fund them in accordance with charging regulations.
NHS Continuing Healthcare
24) NHS Continuing Healthcare (NHS CHC) is a package of ongoing health and care and support that is arranged and funded solely by the NHS where the individual has been found to have a ‘primary health need’, as set out in the national framework for NHS CHC and NHS-funded nursing care. Such care is provided to people aged 18 or over, to meet needs that have arisen as a result of disability, accident or illness. Eligibility for NHS CHC places no limits on the settings in which the package of support can be offered or on the type of services provided.
25) Where an individual is eligible for NHS CHC, the relevant Clinical Commissioning Group (CCG) is responsible for care planning, commissioning health and care and support services, and for case management. Local authorities will continue to have a wider role, for example in relation to safeguarding responsibilities. However, if a review of a person’s care and support needs subsequently determines that the individual is no longer eligible for NHS CHC – perhaps because they needed intensive health and care following an operation and they have now recovered – the NHS ceases to be responsible for the provision of the person’s care and support. Instead, the responsibility for the provision of care and support to meet eligible needs falls to the local authority in which the person is ordinarily resident.
26) Where a person has been provided with NHS accommodation as part of a package of NHS CHC, then prior ordinary residence is retained. Therefore, where a person is placed in a care home (or other accommodation funded by the NHS) in another local authority area for the purpose of receiving NHS CHC, they continue to be ordinarily resident in the local authority area in which they were ordinarily resident before entering the NHS accommodation. Where a CCG places a person in such accommodation, it should inform the person’s local authority of ordinary residence and, if the person is placed ‘out of area’, it is also good practice for the CCG to inform the local authority of ordinary residence in which local authority the care home is located.
27) Where a person is accommodated in a care home as part of their package of NHS CHC, it is possible that they may cease to be eligible for NHS CHC, but still need to remain in the care home, or to be provided with accommodation elsewhere. In such a case, the local authority in whose area the person was ordinarily resident immediately before being provided with NHS accommodation would be the authority responsible for arranging care and support to meet the person’s eligible needs, and for funding the person’s accommodation, subject to any financial assessment.
Example: a person is discharged from NHS Continuing Healthcare
Maureen is 72 years old. Three years ago, she suffered a stroke which left her severely disabled with complex care needs. She was assessed as needing NHS CHC and was moved from hospital to a rehabilitation unit within an independent sector care home in local authority B. This placement was fully funded by Maureen’s CCG. Before her stroke, Maureen had lived with her husband in local authority A.
A recent reassessment of Maureen’s needs concludes that she is no longer eligible for NHS CHC, but has eligible needs for care and support and requires accommodation under the Care Act instead. The care home in which Maureen has been living offers her a place on a long-term basis and all those involved in her care agree that this arrangement best meets Maureen’s needs.
Local authority B agrees to fund the placement on a ‘without prejudice’ basis but immediately falls into dispute with local authority A over Maureen’s place of ordinary residence. Local authority B contends that Maureen remains ordinarily resident in local authority A, where she had been living with her husband before her placement at the care home began. Local authority A argues that Maureen has acquired an ordinary residence in local authority B due to the length of time she has spent at the care home. In this situation, when Maureen first enters the care home she is receiving NHS CHC. Therefore, whilst
Maureen is receiving NHS CHC at the care home she remains ordinarily resident in local authority A, where she was living before her stroke.
Once Maureen’s NHS CHC ceases and she is instead provided with accommodation under the Care Act, she is deemed to be ordinarily resident in the area in which she was ordinarily resident immediately before the accommodation was provided. Immediately before Maureen was provided with accommodation she was living in the care home but was still ordinarily resident in local authority A. Therefore, Maureen remains ordinarily resident in local authority A.
28) Under section 9 of the Care Act, local authorities have a duty to assess the needs of any person who appears to have needs for care and support. If it becomes apparent during the course of the assessment that the person has health needs, the local authority should notify the person’s CCG and invite them to assist in the assessment.
29) It is the responsibility of the local authority in which the person is ordinarily resident to provide any care and support identified as necessary to meet eligible needs, in the light of the assessment. Any health services identified by the assessment should be met by the person’s CCG. CCGs and local authorities should work in partnership to agree their respective responsibilities in relation to the provision of the joint package of care.
30) Where a person is placed in accommodation out of area, they remain ordinarily resident in the area of the placing local authority and the placing authority remains responsible for the provision of any other care and support services required. However, the person’s GP may be based in the area in which they are living, and it is this CCG that is responsible for the provision any health services. This may mean that a local authority and a CCG located several miles apart, need to work together to provide a joint package of health and care and support. In the case of a person in receipt of NHS Continuing Healthcare, the placing CCG remains responsible for the provision of care, even where the person changes their GP practice.
British citizens resuming permanent residence in England after period abroad
31) British citizens returning to England after a period of residing abroad (who had given up their previous home in this country) are entitled to an assessment as soon as they return if they appear to have needs for care and support.
32) Accordingly, a returning British citizen would usually acquire an ordinary residence in the area in which they chose to locate, if their intention was to stay living there for settled purposes. For example, they may have family in a particular area and choose to settle there for that reason or they may have no particular reason to locate in a given area. As long as they can demonstrate an intention to remain in the place they are living for settled purposes, they are able to acquire an ordinary residence there.
33) However, if a returning citizen presents to a local authority on their return to England but has no particular intention to settle in that area, the local authority may decide they may be found to be of ‘no settled residence’ and/or in ‘urgent need’ (see heading ‘People with Urgent Needs’). Each case should be decided on an individual basis.
34) It should be noted that ordinary residence can be acquired as soon as a person moves to an area, if their move is voluntary and for settled purposes. There is no minimum period in which a person has to be living in a particular place for them to be considered ordinarily resident there, because it depends on the nature and quality of the connection with the new place.
Armed forces veterans and the families of armed forces personnel
35) The ordinary residence provisions apply to armed forces veterans and the families of armed forces personnel in active service in the same way as they apply to other people. If veterans have needs for care and support upon leaving the forces, they would usually acquire an ordinary residence in the area to which they chose to locate. If a veteran does not have a permanent place to live on leaving the forces or does not have a settled purpose in relation to where they are living, they may be found to be of ‘no settled residence’ and/ or in ‘urgent need’. If the person is found to be of no settled residence, then the local authority in which they are physically present will be responsible for meeting their eligible needs for care and support. If the person is determined to have urgent needs, then the same local authority should consider using its powers to meet those needs, in advance of establishing where the person’s ordinary residence lies.
36) Where family members (who are 18 or over) of armed forces personnel in active service need care and support, their ordinary residence would fall to be assessed and they would generally be ordinarily resident in the area in which they were living. If the member of the armed forces was subsequently posted to another area of the country, the Shah test would again apply and the family member in need of services would usually acquire an ordinary residence in the area to which they were posted. However, if the family member was in receipt of accommodation, prior to the posting and was placed in accommodation in the new area by their original authority in order to be near their family, they would remain ordinarily resident in the area of the placing authority.
37) In the event of a service family returning from overseas, the ordinary residence of any family members (aged 18 or over) requiring care and support would be assessed and they would usually acquire an ordinary residence in the area in which they chose to reside for settled purposes. If the family had no settled purpose in relation to where they were living, the family member in need of services may be found to be of ‘no settled residence’ and/or in ‘urgent need’.
Young people in transition from children’s services to adult care and support
38) Children who are in need of care and support, including children who are ‘looked after’, [footnote 91] are provided with accommodation and/or services under the Children Act 1989 (the ‘1989 Act’). They may also be provided with care and support under the Chronically Sick and Disabled Persons Act 1970 (the ‘1970 Act’), though they receive universal services such as access to schools and primary health care in the same way as all other children. When a young person with care and support needs reaches the age of 18, the duty on local authorities to provide accommodation and services under the 1989 Act ceases. From their 18th birthday, care and support is generally under the Care Act 2014. This is provided by the local authority in which the young person is ordinarily resident.
39) The Department of Health is currently considering the policy implications in relation to the determination of OR disputes for children transitioning into adult social care services, in the light of the judgment - handed down on 8 July - in the case of R (on the application of Cornwall Council) Secretary of State & Ors [2015] UKSC46 (‘Cornwall’). New guidance will be provided in due course.
Care leavers and the 1989 Act
40) Where a child’s ‘looked after status’ under the 1989 Act ends, the local authority which was formerly responsible for them might retain some duties under the 1989 Act, after they reach the age of 18. These young people are referred to as ‘young people eligible for care leaving services’ or ‘care leavers’.
41) In order to provide care leavers with the assistance they need to achieve their aspirations, local authorities must allocate a personal adviser and work with a care leaver to maintain a pathway plan that sets out the support and services available (which may include assistance with education or training). This support may continue until the young person reaches the age of 21 or for longer if they remain in an approved programme of education or training [footnote 92]. Where a young person qualifies for advice and assistance under section 24 of the 1989 Act, the local authority may be required to advise and befriend him or her. They may also be required to give him or her assistance in kind and, exceptionally, by providing accommodation or cash.
42) A local authority which is responsible for providing support to a care leaver is not under a general duty to provide accommodation. Therefore, when a care leaver with assessed care and support needs reaches the age of 18 and requires residential accommodation, their accommodation is usually provided under the 2014 Act, by their local authority of ordinary residence. However, in 2014, the government introduced a duty on local authorities to support those care leavers aged 18 and eligible for care leaving services, who want to stay with their former foster parents until their 21st birthday, known as ‘Staying Put’.
43) There are, however, certain powers and duties to provide accommodation to care leavers in particular cases under the 1989 Act. Under section 24B(5) of the 1989 Act, local authorities have a duty to provide certain young people who qualify for advice and assistance under section 24 of the 1989 Act with vacation accommodation if they are in full-time further or higher education and their term-time accommodation is not available. They also have a power to provide assistance during term-time, such as expenses to cover travel or equipment costs and expenses incurred by the young person in living near the place where he or she is studying.
44) Local authorities do not have a duty to provide accommodation to care leavers during term time. Such accommodation is funded by whatever mainstream funding sources are available to support higher education students. Nor is there a duty under the 1989 Act to provide care and support in the home to care leavers who are in higher education – such services would be provided under the 2014 Act by the local authority of ordinary residence.
45) Local authorities also have a power to provide accommodation under section 24A(5) of the 1989 Act to a young person whom they are advising and befriending under section 24A. Such accommodation may only be provided in exceptional circumstances and if, in the circumstances, assistance may not be given under section 24B (vacation accommodation). A young person who is eligible for care home accommodation under the 2014 Act would be unlikely to be regarded as being in ‘exceptional circumstances’.
Other provisions under which an ordinary residence determination can be sought
Schedule 3 to the Care Act 2014
46) Schedule 3 to the Care Act places a duty on local authorities and the NHS to work together to ensure the safe hospital discharge of people with care and support needs. Where a person remains in hospital because a local authority has not carried out an assessment or put in place arrangements to meet the care and support that it proposes to meet in order to ensure that the person can be safely discharged from hospital, the local authority may be liable to pay the relevant NHS body a charge per day of delay.
47) Schedule 3 to the Care Act requires NHS bodies to take reasonable steps to ensure that eligibility for NHS Continuing Healthcare is assessed in all cases where it appears to the NHS body that the person may have a need for such care, in consultation, where it considers it appropriate, with the local authority appearing to the NHS body to be the authority in whose area the patient is ordinarily resident.
48) Where it is not likely to be safe to discharge a hospital patient unless arrangements for meeting their care and support are put in place, the NHS body must notify the patient’s local authority of this. Under the Care Act, it is the local authority in which the patient appears to the NHS body to be ordinarily resident. Or where a person is not ordinarily resident in any local authority, for example, a person of ‘no settled residence’, the Care Act provides that it is the local authority in which the hospital is situated that the NHS body must notify. Once notification has been received, the local authority must arrange for an assessment of the person’s need for care and support to be carried out and for the provision of any services.
49) If a local authority receives notification from the NHS body of a person who it believes is ordinarily resident in another local authority area, it should inform the NHS body that has issued the notification immediately. If the NHS body agrees that the person is ordinarily resident elsewhere, it should withdraw the notification and re-issue it to the correct local authority. If the NHS body does not agree that the person is ordinarily resident elsewhere, the local authority in receipt of the notification must proceed with carrying out the assessment and arranging for the provision of any necessary care and support. A person ready for discharge from hospital should not remain in hospital for longer than necessary because 2 or more local authorities have fallen into dispute about the person’s place of ordinary residence.
50) Where a local authority has provisionally accepted responsibility for a person discharged from hospital but remains in dispute with one or more local authorities over the person’s ordinary residence in relation to which authority should reimburse the NHS body for the person’s delayed discharge, a determination from the Secretary of State can be sought under section 40 of the Care Act. Determinations should only be sought as a last resort: local authorities should take all steps necessary to resolve the disputes themselves first.
The Mental Capacity Act 2005 Deprivation of Liberty Safeguards
51) The Deprivation of Liberty Safeguards (MCA DoLS) [footnote 93] in the Mental Capacity Act 2005 (‘the 2005 Act’) provide a framework for authorising the deprivation of liberty of people who lack the capacity to consent to arrangements made for their care or treatment (in either a hospital or care home [footnote 99]) and who meet the qualifying requirements in Schedule A1, including that they need to be deprived of liberty in their own best interests, and to prevent harm to them, and that the deprivation of liberty is a proportionate response to the likelihood and seriousness of that harm.[footnote 94]
52) Under the MCA DoLS, the ‘managing authority’ of a hospital or care home must request a standard authorisation from a local authority (a ‘supervisory body’) if they believe an adult will, or will be likely to be, deprived of their liberty in hospital or care home setting within the next 28 days.
53) In most cases, it should be possible to obtain a standard authorisation in advance of deprivation of liberty occurring. Where this is not possible and a person needs to be deprived of their liberty in their own best interests before the standard authorisation process can be completed, the managing authority must give itself an urgent authorisation and apply to the supervisory body for a standard authorisation to be issued within 7 calendar days.
54) Where a person needs to be deprived of liberty in a care home in England or Wales, the 2005 Act provides that the supervisory body is always the local authority in which the person is ordinarily resident.[footnote 95] This remains the case regardless of whether the person has been placed in the care home in another authority’s area by the local authority or a CCG.
55) If a person is arranging and paying for their care under private arrangements, they usually acquire an ordinary residence in the area in which their care home is located. Therefore, the local authority in which the care home is located will be the supervisory body.[footnote 96]
56) Where a person is not ordinarily resident in any local authority (for example a person of ‘no settled residence’), the 2005 Act provides that it is the local authority in which the care home is situated that becomes the supervisory body (see paragraph 18(2) of Schedule A1 to the 2005 Act).
57) Under paragraph 183 of Schedule A1 to the 2005 Act, the ‘deeming’ provisions in section 39(1) of the Care Act apply for the purposes of determining where a person is ordinarily resident so that the local authority that is the supervisory body can be identified. A person remains ordinarily resident in the area of the local authority (A) in which the person is ordinarily resident before that local authority (A) places the person in the area of authority (B) in an arrangement that amounts to a deprivation of liberty. Therefore the placing local authority remains the supervisory body.
58) If a person needs to be deprived of liberty in a care home upon their discharge from hospital, and the care home applies for a standard authorisation in advance, [footnote 97] whilst the person is still in hospital (as would be good practice in this situation), it is the local authority in which the person was ordinarily resident before their admission to hospital which is responsible for acting as the supervisory body. This remains the case even where it is planned that the person will be discharged from hospital to a care home located in another local authority area.
59) If the person arranges and pays for their own care in that care home (usually a deputy appointed by the Court of Protection under the 2005 Act would enter into a contract with the care home on their behalf), they would generally acquire an ordinary residence in the area in which their care home is located (the area of local authority (B). However, if the person does not yet reside in the care home when the care home applies for the standard authorisation, they are not yet ordinarily resident in the area for local authority (B), despite any imminent plans to move there. Whilst the person remains in hospital, they remain ordinarily resident where they were before admission to hospital (the area of local authority A) until they are discharged from hospital. In these circumstances, the supervisory body is local authority (A).
60) Section 39(5) of the Care Act applies to all NHS accommodation and not just hospitals. This means that where a person is placed in a care home ‘out of area’ by a CCG under NHS CHC arrangements, they remain ordinarily resident in the area in which they were ordinarily resident before being provided with NHS CHC. Therefore, if the person in receipt of NHS CHC subsequently needs to be deprived of their liberty, it is the local authority in which they were ordinarily resident immediately before being provided with NHS CHC that is the responsible supervisory body for the purposes of DoLS.
61) Where 2 or more local authorities dispute the person’s ordinary residence for the purpose of identifying which authority is the supervisory body, the 2005 Act provides that disputes may be determined by the Secretary of State or appointed person, or by the Welsh Ministers where they cannot be resolved locally. Disputes between a local authority in England and a local authority in Wales, are determined by the Secretary of State or Welsh Ministers under cross-border arrangements made under paragraph 183(4) of Schedule A1 to the 2005 Act.
62) A determination under the 2005 Act can only be sought in relation to ordinary residence disputes that arise in connection with which local authority is the responsible supervisory body for the purpose of giving (and potentially reviewing) a standard authorisation. Where ordinary residence disputes occur in relation to the general provision of care accommodation or services, determinations should be sought under section 40 of the Care Act.
63) Regulations made under the 2005 Act [footnote 98] put in place arrangements where there are disputes between local authorities in England over the ordinary residence of a person and who is the supervisory body arising when the managing authority of a care home or hospital requests a standard authorisation from a local authority; or any person requests the local authority to decide whether or not there is an unauthorised deprivation of liberty in a care home or hospital. They set out that, in the event of a dispute occurring, the local authority which receives the request for a standard authorisation must act as the supervisory body until the dispute is resolved, unless another local authority agrees to perform this role.
Example: moving from hospital to a care home under a standard authorisation
Geeta is 86 years old and has dementia. She lives on her own in local authority A but receives some care and support at home. She requires a routine operation to remove gallstones and is admitted to hospital in local authority B.
During Geeta’s stay in hospital she becomes increasingly confused and starts to wander, making various attempts to leave the ward. To ensure that Geeta can continue to receive essential treatment, her doctors and nursing staff feel it would be in her best interests to prevent her from leaving.
As Geeta is having her movements so restricted as to amount to a deprivation of liberty, and does not have capacity to consent to these arrangements, hospital staff place Geeta under an urgent authorisation and apply to local authority B, the local authority for the area in which the hospital is located, for a standard authorisation to last for the remainder of her hospital stay. Local authority B gives the standard authorisation.
Geeta recovers well from her operation but remains very confused. In preparation for her hospital discharge, she is assessed by a multi-disciplinary team; it is found that she does not have capacity to decide where she should live and a best-interests decision is made that concludes she is no longer able to live independently in the community and recommends that she enters a care home. A place in a care home specialising in dementia care is found for Geeta in neighbouring local authority C. Due to Geeta’s worsening dementia and the fact that she is unable to consent to living in the care home, the care home manager feels she will need to be deprived of her liberty as soon as she enters the care home, at least for the short-term until she settles in.
The care home manager requests a standard authorisation from local authority B, the area in which the hospital is located, mistakenly believing that local authority B is Geeta’s local authority of ordinary residence. Local authority B immediately falls into dispute with local authority A over Geeta’s ordinary residence and which authority should act as the supervisory body. Local authority C also becomes involved in the dispute.
Local authority A argues that local authority C should be the supervisory body. Its argument is based on the fact that the standard authorisation would begin as soon as Geeta moves into the care home in local authority C, at which point she will become ordinarily resident there. Local authority B argues that Geeta has not acquired an ordinary residence in their local authority during her hospital stay and, as such, local authority A or C should be the supervisory body. Finally, local authority C argues that, as Geeta is still in hospital and has not yet moved to their local authority area, she cannot be ordinarily resident in local authority C, despite her impending move.
As local authority B has received the request for the standard authorisation, it is obliged to act as the supervisory body until the dispute is resolved, as required by the Mental Capacity (Deprivation of Liberty: Standard Authorisations, Assessments and Ordinary Residence) Regulations 2008. However, local authority C feels strongly that local authority B is not the correct authority to give the standard authorisation and agrees to take on the supervisory body role until the question of Geeta’s ordinary residence is decided.
To determine Geeta’s ordinary residence for purpose of identifying the responsible supervisory body, paragraph 182 of Schedule A1 to the 2005 Act sets out that the supervisory body is the local authority in which the person is ordinarily resident. Therefore, Geeta’s ordinary residence must be established at the point in time when the care home manager requested the standard authorisation.
At the time of the request, Geeta is in hospital in local authority B. Therefore, whilst Geeta is in hospital in local authority B, she remains ordinarily resident in local authority A. When Geeta moves to the care home in local authority C her ordinary residence will not change because local authority A was the area she was living in for settled purposes before she went to the care home. Local authority A is also the supervisory body responsible for considering the request for the standard authorisation.
MCA DoLS authorisations should be given for as short a time as possible. It would be sensible for local authority A to grant a short standard authorisation so her situation can be reviewed once she moves to the care home. If the review concludes that a further standard authorisation is in Geeta’s best interests, the care home should request a fresh standard authorisation from the supervisory body, Geeta’s local authority of ordinary residence, local authority A. This is because while Geeta remains in receipt of services her ordinary residence does not change and remains with local authority A where she was living immediately before she was admitted to hospital.
Annex I: Repeals and revocations
Some of the important legal provisions and existing statutory guidance which are to be replaced by the Care Act 2014 and the associated regulations and guidance are summarised below. Where existing provisions relate to jurisdictions other than England, the provisions will be disapplied so that they no longer relate to English local authorities. Where provisions relate to children as well as adults, they will be disapplied in relation to adults, but will remain in force in relation to children.
The repeals and revocations required will be provided for by Orders under the Care Act. The final detail of which precise provisions are to be replaced is to be confirmed during the consultation process. The tables below are not therefore a final position, but intended to given an indication of the scope of the Act, and the main existing provisions which are to be affected.
Primary legislation to be repealed or disapplied
Title of legislation to be repealed, in whole or in part
- National Assistance Act 1948
- Health Services and Public Health Act 1968
- Local Authority Social Services Act 1970
- Chronically Sick and Disabled Persons Act 1970
- Health and Social Services and Social Security Adjudications Act 1983
- Disabled Persons (Services, Consultation and Representation) Act 1986
- National Health Service and Community Care Act 1990
- Carers (Recognition and Services) Act 1995
- Carers and Disabled Children Act 2000
- Health and Social Care Act 2001
- Community Care (Delayed Discharges) Act 2003
- Carers (Equal Opportunities) Act 2004
- National Health Service Act 2006
Secondary legislation to be revoked
Title of instruments to be revoked, in whole or in part
- Approvals and directions under S.21(1) NAA 1948 (LAC (93)10) National Assistance (Assessment of Resources) Regulations 1992
- National Assistance Act 1948 (Choice of Accommodation) Directions 1992
- National Assistance (Residential Accommodation) (Relevant Contributions) Regulations 2001
- National Assistance (Residential Accommodation) (Additional Payments and Assessment of Resources) Regulations 2001
- Delayed Discharges (Mental Health Care) (England) Order 2003
- Delayed Discharges (England) Regulations 2003
- National Assistance (Sums for Personal Requirements) Regulations 2003
- Community Care (Delayed Discharges) Act (Qualifying Services) Regulations 2003
- Community Care Assessment Directions 2004
- Community Care, Services for Carers and Children’s Services (Direct Payments) (England) Regulations 2009
- NHS Continuing Healthcare (Responsibilities) Directions 2009
- Ordinary Residence Disputes (National Assistance Act 1948) Directions 2010
Statutory guidance to be cancelled
Title of guidance to be cancelled
- Prioritising need in the context of Putting People First: a whole system approach to eligibility for social care (2010)
- Fairer Charging Policies for Home Care and other non-residential Social Services (2013) and LAC (2001)32
- Charging for residential accommodation guidance (CRAG) (2014)
- Guidance on direct payments for community care, services for carers and children’s services (2009)
- The Personal Care at Home Act 2010 and Charging for Reablement (LAC (2010)6) Charging for residential accommodation guidance (CRAG) (2014)
- Identifying the ordinary residence of people in need of community care services (2013) Transforming Adult Social Care (LAC (2009)1)
- Guidance on National Assistance Act 1948 (Choice of Accommodation) Directions 1992 and National
- Assistance (Residential Accommodation) (Additional Payments) Regulations 2001 (LAC (2004)20)
- The Community Care (Delayed Discharges) Act 2003 guidance for implementation (LAC (2003)21)
- Fair Access to Care Services (FACS): Guidance on eligibility criteria for adult social care (2002)
- Carers and people with parental responsibility for disabled children (2001)
- No secrets: guidance on developing and implementing multi-agency policies and procedures to protect vulnerable adults from abuse (2000)
- Caring for people: community care in the next decade and beyond (1990)
Annex J: Glossary
This glossary refers to key terms used throughout the guidance. More specific terms that are relevant to individual chapters are defined in the section to which they relate. Definitions of more common terms can be found on Think Local Act Personal’s care and support ‘jargon buster
Act of Parliament
If the House of Commons and the House of Lords agree proposals for a new law (called a Bill), and it then receives Royal Assent from the monarch, it becomes an Act of Parliament.
Adult
Any person over the age of 18 years.
Adult with care and support needs
A person over the age of 18 years who has a need for care and support (see below). Depending on the context, this could be an adult receiving a particular care and support service, or an adult who has such needs but are not receiving a service (for example, someone coming forward for an assessment).
Assessment
This is what a local authority does to find out the information so that it can decide whether a person needs care and support to help them live their day-to-day lives. A carer can also have an assessment.
Care and support
The mixture of practical, financial and emotional support for adults who need extra help to manage their lives and be independent – including older people, people with a disability or long-term illness, people with mental health problems, and carers. Care and support includes assessment of people’s needs, provision of services and the allocation of funds to enable a person to purchase their own care and support. It could include care home, home care, personal assistants, day services, or the provision of aids and adaptations.
Carer
Somebody who provides support or who looks after a family member, partner or friend who needs help because of their age, physical or mental illness, or disability. This would not usually include someone paid or employed to carry out that role, or someone who is a volunteer.
Commissioners
The people or organisations that arrange the care and support that is available in an area to meet the needs of the population.
Direct payment
Payments made directly to someone in need of care and support by their local authority to allow the person greater choice and flexibility about how their care is delivered.
Domiciliary care
Also known as home care or non-residential care, it enables people to remain independent and living in their own homes.
Duty
This is something that the law says that someone (in this case, usually a local authority) must do, and that if they do not follow may result in legal challenge.
Local authority
An administrative unit of local government.
Person/people
This is used to refer to an individual or individuals. It may include carers as well as adults with care and support needs.
Personal budget
This is a statement that sets out the cost to the local authority of meeting an adult’s care needs. It includes the amount that the adult must pay towards that cost themselves (on the basis of their financial assessment), as well as any amount that the local authority must pay.
Primary legislation
This a general term used to describe the main laws passed by Parliament, usually called Acts of Parliament.
Provider
An individual, institution, or agency that provides health, care and/or support services to people.
Provisions
The contents of a legal instrument, like an Act or regulations.
Regulations (see also secondary legislation)
A type of secondary legislation made under an Act of Parliament, setting out extra details that help the Act to be implemented.
Self-neglect
Where someone demonstrates lack of care for themselves and or their environment and refuses assistance or services. It can be long-standing or recent.
- non-hospital NHS accommodation (within the meaning of article 12 of the Health and Social Care Act 2008 (Commencement No. 15, Consequential Amendments and Transitional and Savings Provisions) Order 2010) which has been provided since immediately before 19th April 2010;
- shared lives scheme accommodation (within the meaning of regulation 4 of the Care and Support (Ordinary Residence) (Specified Accommodation) Regulations 2014); or
- supported living accommodation (within the meaning of regulation 5 of those Regulations),
- for as long as the provision of that accommodation continues.
a) the National Health Service Act 2006 b) the National Health Service (Wales) Act 2006 c) the National Health Service (Scotland) Act 1978 d) Article 5(1) of the Health and Personal Social Services (Northern Ireland) Order 1972
-
The Department of Health commissioned the Association of Directors of Adult Social Services (ADASS) carer policy network to produce Efficient and Effective Interventions to support carers, which summarises the key elements of this guidance that apply to carers and sets out relevant good practice in each case. This can be found at http://www.local.gov.uk/care-support-reform/-/journal_content/56/10180/7115304/ARTICLE ↩
-
ADASS position statement on visual impairment rehabilitation in the context of personalisation (Dec 2013) ↩
-
SEN Code of Practice (Department of Health, 2014). [https://www.gov.uk/government/publications/send-code-of-practice-0-to-25] (https://www.gov.uk/government/publications/send-code-of-practice-0-to-25) ↩
-
Social care for deafblind adults and children LAC(DH)(2009)6 [under review] http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Lettersandcirculars/LocalAuthorityCirculars/DH_101114 ↩
-
See chapter 6 – assessment – on first contact ↩
-
Local Authority Social Services and NHS Complaints Regulations 2009, made under powers in Sections 113 to 115 of the Health and Social Care (Community Health and Standards) Act 2003. ↩
-
See Integration chapter example in para 15.71 et seq. ↩
-
All NHS Choices web content can be syndicated and used in local systems allowing for automatic updating of information http://www.nhs.uk/CarersDirect/Pages/CarersDirectHome.aspx ↩
-
For example, the Campaign to End Loneliness toolkit for health and wellbeing boards may be helpful: http://www.campaigntoendloneliness.org/for-local-government-and-healthcare/ ↩
-
An example of preventative services effectively, taken from the Leeds Market Position Statement on Leeds Community Equipment Service, Telecare and Care Ring Services, can be found at: http://www.leeds.gov.uk/docs/LeedsAdultsMPS2012.pdf; there are also examples in the LGA final report on adult social care efficiency programme: http://www.local.gov.uk/documents/10180/11779/LGA+Adult+Social+Care+Efficiency+Programme+-+the+final+report/8e042c7f-7de4-4e42-8824-f7dc88ade15d Arthritis Research UK is developing a musculoskeletal (MSK) calculator to provide local estimates of the number of people with musculoskeletal conditions in England, for use in the planning of healthcare services and public health programmes for local populations. ↩
-
For example, NG21: ‘Home care: delivering personal care and practical support to older people living in their own homes’ published in September 2015 https://www.nice.org.uk/guidance/ng21 ↩
-
How to commission the adult social care workforce – North-West Joint Improvement Programme: http://ipc.brookes.ac.uk/publications/pdf/How_to_Commission_the_Adult_Social_Care_Workforce.pdf ↩
-
See Skill for Care resource on Workforce Redesign: http://www.skillsforcare.org.uk/NMDS-SC-intelligence-research-and-innovation/Workforce-redesign/Workforce-redesign.aspx ↩
-
Cordis Bright has produced guidance and a toolkit which provides a methodology (continued on next page) for assessing local market sustainability which local authorities may find helpful: http://www.cordisbright.co.uk/news/post.php?s=social-care-market-sustainability ↩
-
Shared Lives Plus/Community Catalyst guidance on commissioning for provider diversity. An example of a commissioning intervention to encourage diversity: http://sharedlivesplus.invisionzone.com/index.php?/files/file/184-commissioning-for-provider-diversity/ ↩
-
MENCAP guidance on commissioning for people with profound and multiple learning disabilities: http://www.mencap.org.uk/sites/default/files/documents/Raising-our-sights-Commissioning%20guide.pdf ↩
-
Examples of local authority strategies, development with stakeholders, links to JSNA, review processes, roles & responsibilities: http://www.hscic.gov.uk/jsna http://www.thinklocalactpersonal.org.uk/_library/Resources/Personalisation/Personalisation_advice/298683_Uses_of_Resources.pdf ↩
-
The recommendations of the all-party parliamentary group dementia report, ‘Building on the National Dementia Strategy: Change, progress and priorities’ may be helpful http://www.alzheimers.org.uk/site/scripts/download_info.php?fileID=2249 ↩
-
Example of engagement with people using care and support: Warwickshire transformation assembly http://www.warwickshire.gov.uk/transformationassembly ↩
-
See for example Warwickshire County Council’s older people needs assessment projection a multi factor demographic, demand and finance model: http://apps.warwickshire.gov.uk/api/documents/WCCC-568-330 (N.B. published version includes only limited financial information) ↩
-
typically sharing cost information between parties, sometimes with a third party acting as a broker – who surveys, anonymises, and analyses cost data from providers and arrives at a reasonable cost (based on weighted averages, and removing statistical outliers) ↩
-
Note: The advocacy duty under S68 in relation to a safeguarding enquiry and SAR would not apply to prisoners: see section 76(7) and (9) ↩
-
subject to necessary amendments being made to definition of ‘regulated activity related to vulnerable adults’ in Schedule 4 of Safeguarding Vulnerable Groups Act 2006. ↩ ↩2
-
Subject to the laws, principles and obligations that govern how organisations should handle confidential information http://www.hscic.gov.uk/confguideorg ↩ ↩2
-
Not all information about a person’s care will necessarily be confidential, so local authorities will need to apply data protection legislation to consider where seeking consent is and is not required ↩ ↩2
-
The equity limit has been formulated such that, by this point in time, the person should qualify for full local authority support in paying for their care. ↩
-
Subject to any contribution from a person’s income, as discussed above. ↩ ↩2
-
As deferred payment agreements with top-up elements would fall under local authorities’ discretionary powers, local authorities also retain broader overarching discretion as to whether to enter into any agreement involving a top-up. ↩ ↩2
-
Annually may suffice, or more frequently if needs change or the value of the person’s security changes substantially. ↩
-
Reasonableness is to be agreed during care planning and should take into account what is possible using the indicative personal budget as a guide (see chapter 11). However, this does not prevent the plan from detailing wider aspirations and wishes that may not form the person’s eligible needs which the local authority is required to meet, but nonetheless are still important to the person. ↩
-
P v Cheshire West and Chester Council and another; P and Q v Surrey County Council [2014] UKSC 19 ↩
-
The Department of Health commissioned the ADASS carer policy network to produce The Care Act and Whole-Family Approaches sets out best practice approaches to thinking ‘whole family’ in assessment, planning and review processes – as well as the combined legal framework with children’s legislation that underpins this. ↩
-
Glendinning, C. et al., Evaluation of the Individual Budgets Pilot Programme, IBSEN, York, 2008. ↩
-
Audit Commission, Improving Value For Money in Adult Social Care, 2011. 36% of councils cited personalisation as a driver of better value for money in 2009/10. This rises to 45 per cent for 2010/11. Better value came mostly from improved outcomes, not saving ↩
-
Audit Commission, Financial Management of Personal Budgets, 2010. ↩
-
Ipsos Mori, Users of Social Care Budgets, July 2011. ↩
-
The Care and Support (Charging and Assessment of Resources) Regulations 2014 state that intermediate care (including reablement) cannot be charged for, for the first 6 weeks. However, the charging guidance clearly sets out that, in line with the guidance on prevention, that neither should have a strict time limit but should reflect the needs of the person. Local authorities may therefore wish to apply their discretion to offer this free of charge for longer than 6 weeks where there are clear preventative benefits such as when a person has recently become visually impaired. ↩
-
Choice and control for all the role of individual service funds in delivering personalised care and support, Groundswell Partnership, 2012. ↩
-
Local Authority Social Services and NHS Complaints Regulations 2009, made under powers in Sections 113 to 115 of the Health and Social Care (Community Health and Standards Act) 2003. ↩
-
In this guidance, references to care and support to meet an adult’s eligible needs include care and support provided or commissioned by a local authority to discharge its duty under section 117 of the 1983 Act. References in this guidance to sections 31 and 32 of the Act also apply in respect of after-care services (as those sections are modified by Part 1 of Schedule 4 to the Act). ↩
-
A nominated person is anyone who agrees to manage a direct payment on behalf of the person with care needs. An authorised person is someone who agrees to manage a direct payment for a person who lacks capacity according to the Mental Capacity Act 2005. ↩
-
See sections 31(7) and 32(9) of the Act as modified respectively by paragraph (4) and (9) of Part 1 of Schedule 4 to the Act. ↩
-
Gross payments are for the full direct payment amount, and the local authority then recovers any applicable charges from the person. A net direct payment is allocated after any appropriate charges have been subtracted, and is generally seen as the easiest and most efficient way to administer direct payments. ↩
-
Employers (including direct payment holders) will be required to comply with the duty to automatically enrol eligible workers into a qualifying workplace pension scheme and to meet the minimum contributions required by law. More information for is available on the Pension Regulator website. ↩
-
This does not include family members that live elsewhere to the direct payment recipient (for example, it is allowed to pay a family member to provide care, as long as that member does not live in the same household) ↩
-
Employers (including direct payment holders) will be required to comply with the duty to automatically enrol eligible workers into a qualifying workplace pension scheme and to meet the minimum contributions required by law. More information for is available on the Pension Regulator website ↩
-
A similar provision exists in the Children & Families Act, where those with education, health and care (EHC) plans have a right to request a review of their EHC plan (as can others on their behalf). This will include any adult care components set out in the plan ↩
-
This process may be referred to as a ‘re-assessment’. As noted above, this should not be a new assessment from the beginning of the care and support process, but should be a proportionate assessment that takes into consideration what is already known of the person and incorporates revised elements as appropriate. A ‘re-assessment’ cannot occur without the local authority first conducting a review and then deciding that a revision of a plan is necessary. ↩
-
Safeguarding adults: Roles and responsibilities in health and care services (PDF, 315KB) ↩
-
Braye, S., Orr, D. and Preston-Shoot, M. Self-neglect Policy and Practice: Building an Evidence Base for Adult Social Care ↩
-
For example, deeming provisions in adult legislation provided that where a person is provided with residential accommodation under Part 3 of the 1948 Act, they are deemed to continue to be ordinarily resident in the area (if any) in which they were ordinarily resident immediately before the residential accommodation was provided. ↩ ↩2
-
These provide that where a person is provided with residential accommodation under Part 3 of the 1948 Act, they are deemed to continue to be ordinarily resident in the area (if any) in which they were ordinarily resident immediately before the residential accommodation was provided. ↩
-
R v Waltham Forest LBC ex parte Vale (1985) ↩
-
For example of the adult in question ↩
-
The Mental Capacity Act 2005 Code of Practice is available at the following address: https://www.gov.uk/government/publications/mental-capacity-act-code-of-practice ↩
-
the 1948 Act ↩
-
These provide that where a person is provided with residential accommodation under Part 3 of the 1948 Act, they are deemed to continue to be ordinarily resident in the area (if any) in which they were ordinarily resident immediately before the residential accommodation was provided. ↩
-
Paragraph 54 of the Supreme Court judgment. ↩
-
The relevant provisions of the National Assistance Act 1948 have been disapplied in relation to England by S.I. 2015/914. However, under article 3(3) of that S.I., despite the amendments made by that S.I., provisions of the 1948 Act that operate in relation to, or by reference to, support or services provided, or payments towards the cost of support or services made, before or on or after 1 April 2015 and anything done under such provision, continue to have effect for the purposes of that support or those services or payments. Also, by virtue of transitional provisions, any question as to a person’s ordinary residence arising under the 1948 Act which is to be determined by the Secretary of State on or after 1 April 2015 is to be determined in accordance with section 40 of the 2014 Act (disputes about ordinary residence). ↩
-
Section 39 provides that where an adult has needs for care and support which can be met only if they are living in accommodation of a type specified in regulations (specified type), and the adult is living in accommodation in England of a specified type, they are to be treated for the purposes of Part 1 of the Act as ordinarily resident in the area where they were ordinarily resident immediately before beginning to live in accommodation of a specified type, or (where the adult was of no settled residence at that time), in the area in which they were present at that time. By virtue of transitional provisions, section 39 does not have effect in relation to a person who, immediately before the relevant date in relation to that person, is being provided with — ↩
-
See the Care and Support (Ordinary Residence) (Specified Accommodation) Regulations 2014. Those types are specified only if the adult’s needs are being met under Part 1 of the Care Act while living in that type of accommodation. ↩
-
See the Care and Support (Ordinary Residence) (Specified Accommodation) Regulations 2014. Those types are specified only if the adult’s needs are being met under Part 1 of the Care Act while living in that type of accommodation. ↩
-
Section 39(6) of the 2014 Act provides that NHS accommodation means accommodation under either: ↩
-
Where a child’s ‘looked after status’ under the 1989 Act ends, the local authority which was formerly responsible for them might retain some duties under the 1989 Act, after they reach the age of 18. These young people are referred to as ‘young people eligible for care leaving services’ or ‘care leavers’. ↩
-
The Care and Support (Ordinary Residence) (Specified Accommodation) Regulations. ↩
-
Care and Support (Ordinary Residence) (Specified Accommodation)) Regulations 2014 ↩
-
Regulations made under section 117 may impose the duty of a CCG on another CCG or on NHS England instead. At the time of publication, see regulations 14 and 15 of the National Health Service Commissioning Board and Clinical Commissioning Groups (Responsibilities and Standing Rules) Regulations 2012/2996. ↩
-
These are patients who leave hospital after being detained on the basis of an application under section 3, a hospital order under section 37, or a hospital direction under section 45A, or a transfer direction under section 47 or 48. ↩
-
For detailed information on mental health after-care, see the Code of Practice Mental Health Act 1983 ↩
-
Levene v Inland Revenue Commissioners (1928) AC 217 ↩
-
Fox v Stirk 1970 2 QB 463 ↩
-
Article 5 of the Care Act (Transitional Provision) Order 2015 (S.I. 2015/995) ↩
-
Further detail can be found in Deprivation of Liberty Safeguards, Mental Capacity Act 2005 Code of Practice. ↩
-
In Wales, the requirement to prepare a care and support plan will be commenced under the Social Services and Well-being (Wales) Act in April 2016. Until then, references in this document to ‘care and support plans’ should be understood to refer to existing care management arrangements. ↩
-
Authority = Local Authority in England, Wales and Scotland. HSC Trust in Northern Ireland ↩
-
Cross-border placements could occur where a person is living at home or where they are already living in residential care accommodation. ↩
-
See section 9 of the Care Act as to the duties on English local authorities in relation to the assessment of adults’ needs for care and support. Section 9(5) imposes a duty to involve the adult, any carer the adult has, any person whom the adult asks the authority to involve, or where the adult lacks capacity to ask the authority to involve, any person who appears to the authority to be interested in the adult’s welfare. Under section 9(6) English authorities must also consider whether and, if so, to what extent, matters other than the provision of care and support could contribute to the achievement of the outcomes the adult wishes to achieve. ↩
-
See section 9(5) of the Act as to the duties on English local authorities to involve persons in carrying out needs assessments. ↩
-
See section 27 of the Act as to the review of care and support plans by English local authorities. See section 79 as to delegation of functions by such authorities and the chapter in this guidance on delegation. ↩
-
See further the meaning of ‘needs’ in relation to the 4 territories under the regulations. ↩
-
The local authority can exercise its discretion under the care act to refuse to agree to defer any further care costs, whilst securing any already-accrued debt. However, if the person meets the criteria governing eligibility for deferred payments, the LA must agree to defer future care costs. ↩
-
Sections 19(3) and 20(6) provide powers which can be used for meeting urgent needs for adults with care and support needs and carers respectively. ↩
-
See section 8 of the Care Act 2014. A local authority may meet needs by providing the service (accommodation) itself, however, most local authorities do not do so but meet a person’s needs for accommodation in a care home by arranging for another person to provide it. ↩
-
A child who is ‘looked after’ is defined in section 22(1) of the Children Act 1989 and this term means broadly that a child is in a local authority’s care by virtue of a care order or is provided with accommodation by a local authority in the exercise of their social services functions. ↩
-
See section 23CA of the 1989 Act which was inserted by the Children and Young Persons Act 2008, where a former relevant child resumes a programme of training up to age 25, they are entitled to continuing support from a leaving care personal adviser allocated by their authority of ordinary residence under the 1989 Act. ↩
-
The Mental Capacity Act Deprivation of Liberty Safeguards were inserted into the Mental Capacity Act 2005 by section 50 and Schedules 7,8 and 9 to the Mental Health Act 2007 which inserted Schedules A1 and 1A into the 2005 Act. ↩
-
Applications may be made to the Court of Protection under the 2005 Act to authorise deprivation of liberty in settings other than hospital or care homes. ↩
-
See the best interests requirement paragraph 16 of Schedule A1 to the 2005 Act ↩
-
Paragraph 18(2(1) of Schedule A1 to the 2005 Act. ↩
-
Paragraph 18(2) of Schedule A1 to the 2005 Act ↩
-
A standard authorisation comes into force when it is given, or at any later time specified in the authorisation: paragraph 52 of Schedule A1 to the 2005 Act. ↩
-
Part 6 of The Mental Capacity (Deprivation of Liberty: Standard Authorisations, Assessments and Ordinary Residence) Regulations 2008 (S.I. 2008/1858) as amended by article 11 of, and paragraph 118 of Schedule 2 of the National Treatment Agency (Abolition) and the Health and Social Care Act 2012 (Consequential, Transitional and Saving Provisions) Order 2013 (S.I. 2013/235). These Regulations apply only to England. ↩
