Health matters: preventing STIs
Published 21 August 2019
Summary
This edition of Health Matters focuses on the prevention of 5 common sexually transmitted infections (STIs):
- gonorrhoea
- chlamydia
- syphilis
- genital herpes
- genital warts
It also covers the public health challenge of antimicrobial-resistant STIs, and the commissioning and improvement of sexual health services.
For more about HIV and increasing the uptake of HIV testing, read Health Matters: increasing the uptake of HIV testing.
Scale of the problem
Sexually transmitted infections (STIs) are a major public health concern. STIs are often considered to be stigmatising, and may seriously impact the health and wellbeing of affected individuals, as well as being costly to healthcare services.
If left undiagnosed and untreated, common STIs may cause complications and long-term health problems, including:
- pelvic inflammatory disease, ectopic pregnancy, postpartum endometriosis, infertility, and chronic abdominal pain in women
- adverse pregnancy outcomes - including abortion, intrauterine death, and premature delivery
- neonatal and infant infections and blindness
- urethral strictures and epididymitis in men
- genital malignancies, proctitis, colitis, and enteritis in men who have sex with men (MSM)
- cardiovascular and neurological damage
Increasing resistance and decreased susceptibility to antimicrobials used to treat STIs has reduced treatment options, and there are therefore emerging concerns - especially for gonorrhoea.
In 2011 in the UK, the estimated STI treatment costs were £620 million, excluding costs for HIV treatment.
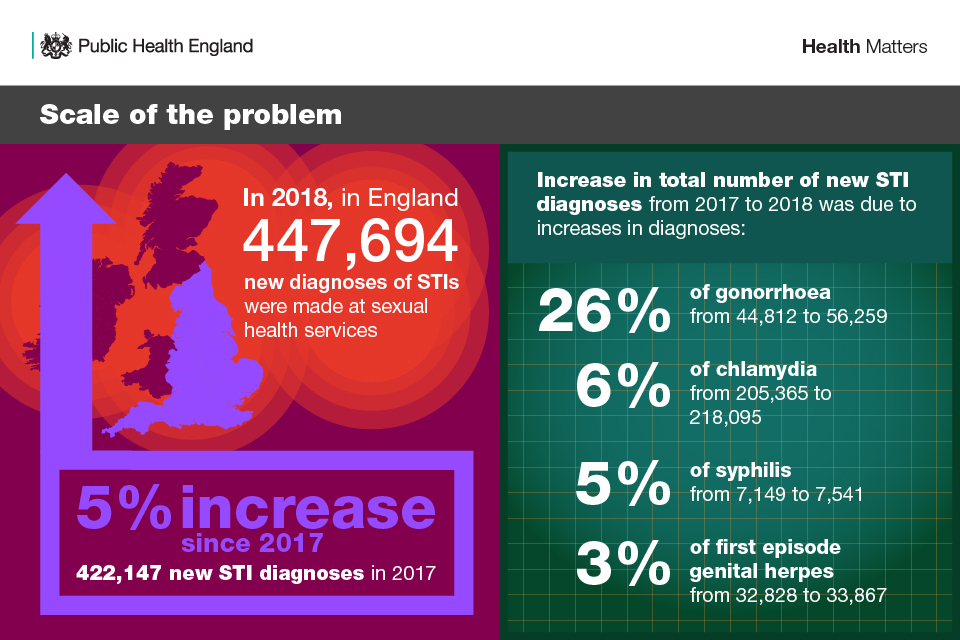
In 2018, there were 447,694 new diagnoses of STIs made at SHSs in England - a 5% increase since 2017 when 422,147 new STI diagnoses were made.
Of these, the most commonly diagnosed STIs were:
- chlamydia (49% of all new STI diagnoses)
- first episode genital warts (13%), gonorrhoea (13%)
- first episode genital herpes (8%)
The increase in the total number of new STIs compared to 2017 was due to a large increase in gonorrhoea (26%; from 44,812 to 56,259), and more moderate increases in diagnoses of:
- chlamydia (6%; from 205,365 to 218,095)
- syphilis (5%; from 7,149 to 7,541)
- first episode genital herpes (3%; from 32,828 to 33,867)
STIs: Scale of the problem
The rise in chlamydia is generated, in part, by the increasing positivity of tests delivered through the National Chlamydia Screening Programme (NCSP) but increasing transmission in people aged 25 years and older is also likely.
Gonorrhoea and syphilis have re-emerged as major public health concerns, especially among gay, bisexual and MSM. In 2018, 47% of gonorrhoea and 75% of syphilis diagnoses were in MSM.
Since 2009, gonorrhoea and syphilis diagnoses have risen by 249% (16,141 to 56,259) and 165% (2,847 to 7,541) overall, and by 643% (3,579 to 26,574) and 236% (1,692 to 5,681) among MSM.
Behavioural changes, including more condomless sex with new or casual partners, likely contribute to these trends. More modest increases in diagnoses for both infections have also occurred among heterosexuals since 2016.
Genital warts diagnoses decreased between 2017 and 2018 (a 3% decrease from 59,178 to 57,318), largely due to the substantial declines in younger women, the majority of whom would have received the quadrivalent human papilloma virus (HPV) vaccine when aged 12 or 13 years. The sustained decrease is also due to declines in similarly-aged heterosexual young men, which are likely attributable to substantial herd protection.
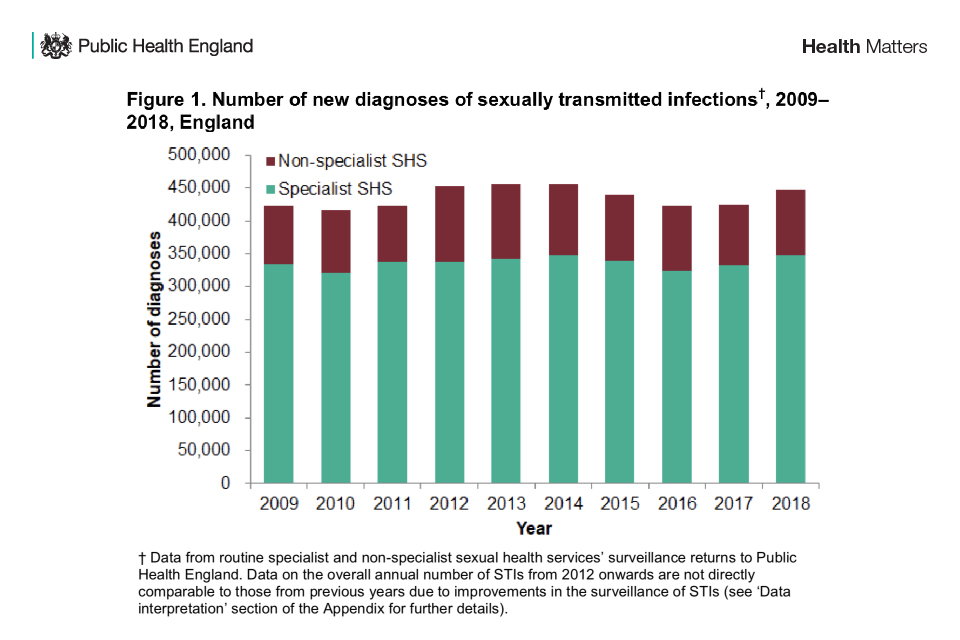
Number of new diagnoses of sexually transmitted infections, 2009-2018, England
SHSs include both specialist (level 3) and non-specialist (level 1 and 2) SHSs. Specialist SHSs refers to genitourinary medicine (GUM) and integrated GUM and sexual and reproductive health (SRH) services.
Non-specialist SHSs refers to:
- SRH services
- young people’s services
- online sexual health services
- termination of pregnancy services
- pharmacies
- outreach and general practice
- other community-based settings
Further details on the levels of sexual healthcare provision are included in the BASHH Standards for the Management of STIs (Appendix B).
In April 2019, PHE launched the updated specification of the GUMCAD STI Surveillance System to capture additional behavioural, clinical and partner notification information collected during sexual history taking, as recommended by the British Association for Sexual Health and HIV (BASHH).
The additional data will ensure that PHE can better understand the epidemiological causes of STI outbreaks and epidemics to improve the public health response and monitor and evaluate the NHS England funded trial of HIV pre-exposure prophylaxis (PrEP) and the future national programme of PrEP.
HIV
Although HIV testing is increasing, the number of all new HIV diagnoses has declined over the past decade, with a substantial decrease over the past 3 years. This recent reduction has been mostly driven by fewer HIV diagnoses among MSM, as a result of combination HIV prevention, including:
- HIV testing - particularly repeat testing among higher-risk men
- improvements in the initiation of anti-retroviral therapy
- treatment as prevention (TasP)
- PrEP
The underlying incidence of new HIV infections in MSM has been falling steadily since 2011 to 2012, largely driven by intensified TasP. It is too early to know the strength of any additional effect on HIV incidence of PrEP scale-up since 2016 to 2017. Furthermore, the scale-up of England’s PrEP Impact Trial has recently been magnified, with the agreement at the beginning of 2019 to double the number of places available to 26,000.
Decreases are also occurring in black African, black Caribbean and other heterosexual groups. Latest data, published in September 2018, show a total of 4,363 people were newly diagnosed with HIV in 2017 in the UK. This represents a 17% drop from the 5,280 diagnoses reported in 2016 and a 28% drop from the 6,043 diagnoses in 2015.
New data for 2018 will be released in September 2019.
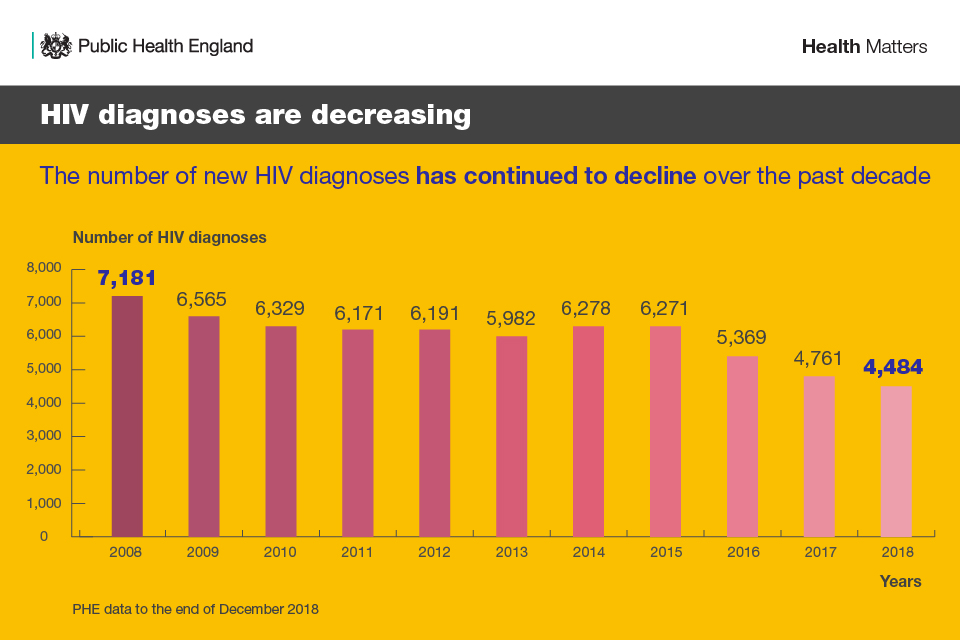
HIV diagnoses are decreasing - the number of new HIV diagnoses has continued to decline over the past decade
You can read more about HIV and increasing the uptake of HIV testing in this previous edition of Health Matters.
STIs and inequalities
The diagnosis rates of STIs remains greatest in young heterosexuals aged 15 to 24 years, black minority ethnic (BME) populations, MSM, and people residing in the most deprived areas in England.
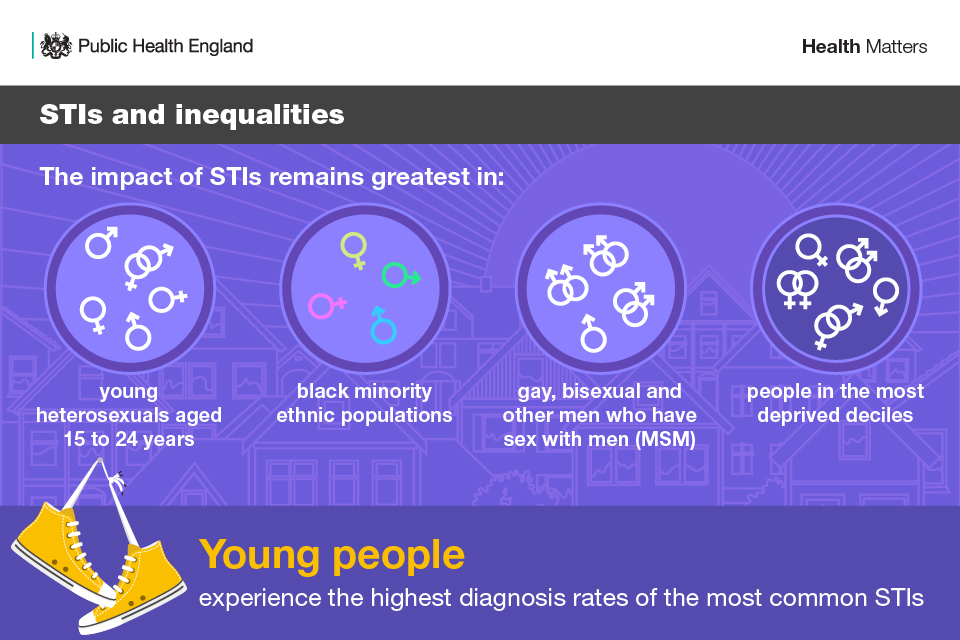
STIs and inequalities
Young people aged 15 to 24 years old experience the highest diagnosis rates of the most common STIs, likely due to higher rates of partner change. 61% (132,324 out of 218,095 cases) of chlamydia and 36% (20,453 out of 56,259 cases) of gonorrhoea diagnoses are among young people.
Young women are more likely to be diagnosed with an STI than young men, partly due to greater uptake of chlamydia screening through the NCSP, as well as sexual mixing between younger women and older male partners.
Of the 64,831 new STI diagnoses in MSM in 2018, gonorrhoea and chlamydia were most common at 41% and 29%, respectively. Among MSM, although the majority of syphilis, gonorrhoea and chlamydia diagnoses are in those who are HIV-negative or of unknown HIV status, the population diagnosis rates are 3-6 times higher in those diagnosed with HIV.
The rise in syphilis, gonorrhoea and chlamydia diagnoses among MSM is probably primarily associated with behavioural changes such as an increase in partner numbers and condomless anal intercourse with new or casual partners. For some MSM, chemsex and group sex facilitated by geosocial networking applications may have also contributed.
In 2015, PHE published a briefing for commissioners and providers of drug and alcohol services, which highlights issues relating to chemsex, including barriers and facilitators to help them plan services and understand, assess and meet the needs of their local population.
The core data set of the National Drug Treatment Monitoring System (NDTMS) has collected information on sexual orientation since 2016, under the categories:
- heterosexual
- gay and lesbian
- bisexual
- not stated
Every year, each local area receives a commissioning support data pack to assist with planning for drug prevention, treatment and recovery for adults. This includes client profile data for new treatment presentations in the previous year including by sexuality.
Local areas can also access NDTMS data relating to the drugs most commonly associated with chemsex through data available in the Local Authority Sexual Health, Reproductive Health and HIV Epidemiology Reports (LASERs), which are available on PHE’s HIV/STI web portal.
Although the majority of STI diagnoses (64%; 284,847 out of 447,694 cases) are in those of white ethnicity, the highest population diagnosis rates are among people of black Caribbean and black non-Caribbean or non-African ethnicity (any other black ethnicity).
This may be partly explained by higher rates of sexual partner change and concurrent partnerships among men of black Caribbean or any other black ethnicity.
2018 data show that the rate of gonorrhoea in people of black ethnicity people is 4 times that of the general population.
Rates of STIs are also strongly associated with socioeconomic deprivation (SED), with the highest rates found among people living in the most deprived areas of England.
SED, which is often more common in ethnic minorities, is a known determinant of poor sexual health outcomes. A study that investigated the interplay between SED and ethnicity on population-level rates of STIs in England found that while SED is a key determinant of poor sexual health, other cultural influences on sexual behaviour may contribute to STI risk exposure among ethnic groups.
The high STI rates seen among black ethnic communities are likely to be an outcome of the complex relationship between cultural, economic and behavioural factors.
Higher risk sexual behaviours
Higher risk sexual behaviours, such as condomless sex with casual or multiple partners, are affected by social norms, attitudes and health. To adequately plan preventative measures, it is important to examine trends and future trajectories of these risk behaviours, as well as their determinants such as alcohol and drug use and SED.
A study examining change in sexual lifestyles throughout the life course – using data from the three National Surveys of Sexual Attitudes and Lifestyles (Natsal) – found that sexual lifestyles in Britain have changed substantially in the past 60 years. This is influencing what we are seeing in terms of disease epidemiology.
For instance, the study found that sexual activity is continuing into later life, emphasising that attention to sexual health and wellbeing is required throughout the life-course.
Using the third Natsal (Natsal-3), another study investigated whether inequalities in STI rates across ethnic groups could be explained by differences in sexual behaviours, including age and sexual competence at sexual debut, partner numbers, and concurrency.
This study concluded that men of black Caribbean or any other black ethnicity were most likely to report higher numbers of recent sexual partners and concurrent partnerships. This, coupled with assortative sexual mixing patterns, may contribute to higher rates of bacterial STIs in these communities.
Data from the Natsal-3 survey also showed that people under the age of 25 years had higher rates of partner change than their older counterparts. This likely contributes to the higher diagnosis rates of bacterial STIs in the younger age group.
Evidence from Natsal-3 also showed that MSM are disproportionately affected by a broad range of higher-risk health behaviours and poor health outcomes. A bio-behavioural study of MSM in London found high rates of behaviours associated with increased risk of HIV/STI transmission, including:
- 3 in 5 reporting condomless sex with at least 1 casual partner in the previous 12 months
- 1 in 5 reporting having an STI in the previous 12 months
- 1 in 5 reporting chemsex in the last year
MSM also tend to report higher rates of partner change than heterosexual populations and are more likely to belong to complex, densely connected sexual networks that facilitate rapid STI transmission.
Despite this, it’s important to note that the number of new HIV diagnoses in MSM in London is declining.
PHE’s economic resources for sexual health
PHE’s Spend and Outcome Tool (SPOT) gives an overview of spend and outcomes across key areas of business for local authorities - and can be used to compare with other geographical areas and a range of benchmarks.
SPOT can be a useful tool for local authorities who are interested in comparing spend data on sexual and reproductive health with sexual and reproductive health outcomes. The practical guidance to SPOT for improving sexual and reproductive health provides a step by step guide for local authorities who choose to use this tool.
PHE also has a Health Economics Evidence Resource, which summarises cost-effectiveness evidence for sexual health interventions.
Preventing and reducing common STIs
Prevention is central to achieving good sexual health outcomes and entails changes that reduce the risk of poor sexual health outcomes and activities that encourage healthy behaviours. Education, condom use, diagnosis and treatment are key interventions for their prevention and control.
Prime responsibility for prevention rests with local authorities who commission and support a range of prevention work, often working collaboratively with PHE and the NHS.
Access to SHSs
Open access to SHSs (in person or online) that provide rapid treatment and partner notification can reduce the risk of STI complications and infection spread. It is important that local and national services for the prevention, diagnosis, treatment and care of STIs are available to the general population, but target groups with greater sexual health needs.
The total number of consultations at SHSs in England - attendances at physical clinics or through electronic SHSs (eSHSs) – increased by 7% between 2017 and 2018, from 3,337,677 to 3,561,548 consultations. This continues the increasing trend seen between 2014 and 2018, during which there was a 15% increase in the number of consultations.
Over this same time period, the total number of sexual health screens (tests for chlamydia, gonorrhoea, syphilis and HIV) increased by 22%, from 1,603,744 in 2014 to 1,955,108 in 2018.
Despite increases in SHS attendances and testing nationally, there is some variability regionally. Between 2017 and 2018, there were small declines in attendances at SHSs in the North East (1%) and South East (2%). The STI testing rate indicator on PHE’s Sexual and Reproductive Health Profiles can be used to explore these regional variations.
Furthermore, BASHH has set a standard that 80% of eligible attendees should be tested for HIV, but only 12% of specialist SHSs meet this standard.
A national mystery shopper survey found that the majority of SHSs could offer an appointment within 48 hours. 83% of 220 UK clinics in 2015 responding (of a total of 248) offered patients contacting by telephone an appointment within 48 hours, compared with 74% in 2014.
However, access to specialist SHSs has worsened for those with symptoms suggestive of an acute STI and is significantly poorer for asymptomatic women. For patients with acute symptoms, the proportion of appointments offered within 48 hours fell from 96% in 2014 to 91% in 2015. Among asymptomatic patients, women were significantly less likely to be offered an appointment within 48 hours than men (53% and 77%, respectively). There was no determinable difference in access associated with service tendering.
Professional bodies are responsible for clinical standards alongside the National Institute for Health and Care Excellence (NICE), which form part of the Department of Health and Social Care’s (DHSC) national template service specification. These documents are designed for use by local authorities in public health commissioning services including SHSs.
Education
International evidence is clear that comprehensive relationships and sex education (RSE) protects young people from STIs and unplanned pregnancy, as well as some of the behaviours that make them more at risk, including non-consensual sex. Natsal-3 found young people who cited school as their main source of RSE were less likely to acquire an STI or experience an unplanned pregnancy.
From September 2020, legislation requires all schools in England to provide:
- relationships education at primary level
- RSE at secondary level
- health education in both
Relationships, sex and health education (RSHE) applies to all schools including academies, faith schools and the independent sector.
Statutory status provides a unique opportunity to embed primary prevention on all sexual and reproductive health issues, equipping young people with the skills and knowledge they need to look after their own sexual health, including understanding the benefits of condom use and testing.
Statutory guidance for schools, published by the Department for Education (DfE) in June 2019, specifically requires that students at secondary level learn about:
- the prevalence of some STIs and the impact they can have on those who acquire them
- how the different STIs, including HIV and AIDs, are transmitted
- how risk can be reduced through safer sex (including through condom use)
- the importance of and facts about testing and treatment
- how to get further advice, including how and where to access confidential sexual and reproductive health advice and treatment
PHE will be working closely with DfE and local authorities to support schools prepare for and deliver statutory RSHE. This will include providing local authorities with evidence-based information and local sexual and reproductive health data relevant to their populations.
National sexual health promotion
PHE’s national HIV Prevention and Sexual Health Promotion programme supports national and local health promotion activities to improve sexual and reproductive health and prevent HIV.
Sexwise is a sexual health and reproductive health information programme that seeks to provide clear, impartial, up-to-date information for the general public and healthcare professionals, to enable informed sexual health choices and support healthy sexual behaviour.
Protect Against STIs Use a Condom is a sexual health campaign launched by PHE in 2017, to encourage condom use by young adults aged 16-to-24 years to reduce the rates of STIs. It aims to raise awareness of the serious consequences of STIs, as well as normalise and encourage condom use. See the range of campaign advertising and images.
PHE also commissions specialist programmes to address HIV prevention and sexual health improvement, including multimedia and local outreach programmes.
National HIV Testing Week is a part of the national HIV Prevention England Programme aimed at MSM, black African communities and other groups in whom there is a higher or emerging burden of infection.
PHE recognises that voluntary and community organisations play a key role in tackling STIs and improving HIV and sexual health. In 2015, PHE set up an HIV Prevention Innovation Fund, and in 2019 and 2020 the fund has been expanded to support projects that offer new and innovative ways of improving reproductive and sexual health (including STI prevention), as well as HIV.
The new Reproductive Health, Sexual Health and HIV Innovation Fund is a grant scheme which aims to reduce the impact of HIV and improve sexual and reproductive health in England by supporting voluntary sector organisations to deliver innovative interventions.
The fund supports volunteer organisations spearheading new, innovative community-led interventions through:
- online campaigns
- outreach
- patient support
- testing and media
- art projects.
To date, the fund has supported 46 projects across England and reached over 170,000 people in 2018.
National Chlamydia Screening Programme (NCSP)
The NCSP provides opportunistic screening to sexually active young people aged 15-to-24 years. The aim of the programme is to control chlamydia through early detection and treatment of asymptomatic infection, so reducing onward transmission and the consequences of untreated infection.
In 2018, through the NCSP, a total of 1,304,113 chlamydia tests were carried out among young people aged 15 to 24 years in England. This was a 1% decline since 2017 and a 22% decline since 2014. Due to an increase in the proportion testing positive, this resulted in 131,269 chlamydia diagnoses in this age group, a 2% increase since 2017.
Despite reduced testing, there has been an increase in diagnoses, which could in part be a result of better targeting of young people most at risk.
Non-specialist SHSs are the largest provider of chlamydia testing, but in 2018, 55% of chlamydia diagnoses were made in specialist SHSs.
However, there have been significant changes in service provision across the country, including the increased availability of eSHSs. As such, eSHS tests increased by 54% between 2017 and 2018, now accounting for 17% of tests and contributing the second largest number of diagnoses (14%).
Chlamydia screening is commissioned by local government in a variety of health and non-health settings including online testing. The chlamydia care pathway supports commissioners and providers with data and examples of best practice to inform local action.
PHE commissioned a group of external experts to review programme policy on the NCSP. This expert peer review group has made a number of recommendations and PHE plans to consult on resulting changes to proposed revisions to NCSP policy.
PHE’s Sexually transmitted infections and screening for chlamydia in England: 2018 report provides further information on chlamydia testing coverage, detection rates and test positivity.
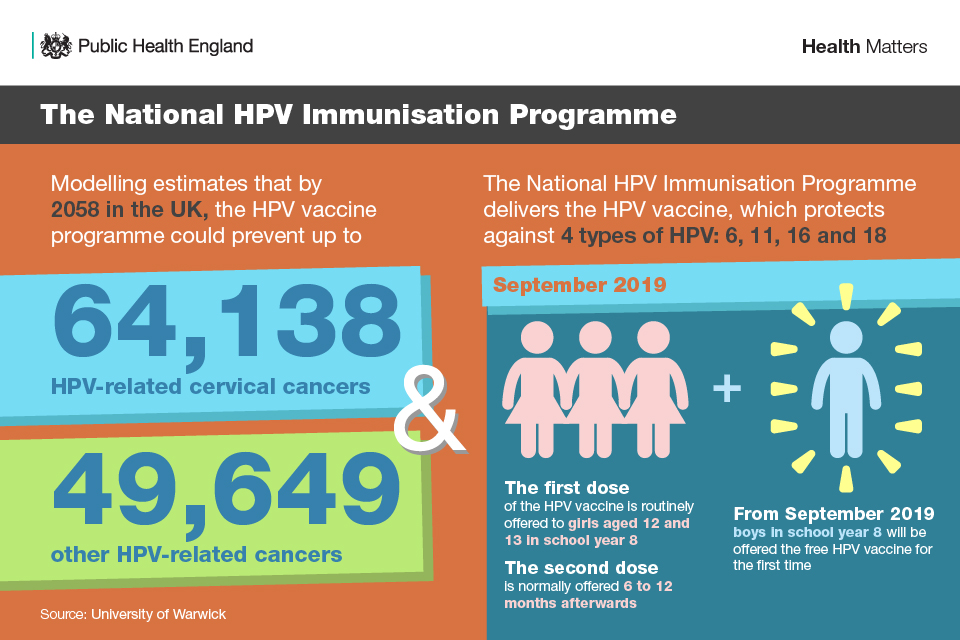
The National HPV Immunisation Programme
There are over 100 types of HPV, of which around 40 types infect the genitals. HPV infections are very common and most people will get an infection (caught through any kind of sexual contact with another infected person) at some point in their lives. The majority of these infections will naturally clear up without treatment, but if they don’t, they can lead to HPV-related disease.
Some genital HPV types are categorised as high-risk as they are linked to the development of cancers including cervical, anal and genital cancers, as well as cancers of the head and neck. Other low-risk HPV types cause genital warts.
The National HPV Immunisation Programme delivers the HPV vaccine, which protects against 4 types of HPV (6, 11, 16 and 18). These include both high- and low-risk types responsible for the majority of cervical cancers and genital warts.
The National HPV Immunisation Programme
The adolescent programme is commissioned locally by screening and immunisation teams for delivery by school immunisation providers. The first dose of the HPV vaccine is routinely offered to girls aged 12 and 13 in school year 8 and the second dose is normally offered 6 to 12 months afterwards.
In July 2019, it was announced that from September 2019, boys in school year 8 will be offered the HPV vaccine for the first time as part of the National HPV Immunisation Programme.
Offering the vaccine to boys will not only protect them, but also prevents more cases of HPV-related cancers in girls and reduces the overall burden of these cancers in both men and women in the future.
It is estimated that by 2058 in the UK, the HPV vaccine currently being used may prevent up to 64,138 HPV-related cervical cancers and 49,649 other HPV-related cancers.
There is also a national HPV vaccination programme for MSM, which began in April 2018. The purpose of this programme is to offer the vaccine to MSM aged up to and including 45 years who are attending SHSs and or HIV clinics. PHE has a clinical and operational guidance document with information on the MSM programme.
Syphilis Action Plan
The continued increase in syphilis cases and the potential for severe disease necessitate a strengthening of preventive measures. A wide range of measures to control transmission already exists, but the continued increase in cases suggests that these are not being consistently applied.
PHE has published a Syphilis Action Plan, which, to help reduce the impact of syphilis on the main affected populations, brings together existing evidence, national guidelines and best practice for:
- clinicians
- public health specialists
- specialty societies
- service commissioners
A successful response to the current increase in syphilis incidence is dependent upon optimising 4 prevention pillars fundamental to syphilis control and prevention:
- increase testing frequency of higher-risk MSM and re-testing of syphilis cases after treatment
- deliver partner notification to BASHH standards
- maintain high antenatal screening coverage and vigilance for syphilis throughout antenatal care
- sustain targeted health promotion
These pillars need to be underpinned by maintaining professional awareness and knowledge of syphilis, improving epidemiological intelligence and developing diagnostics and research.
Antimicrobial resistance in STIs
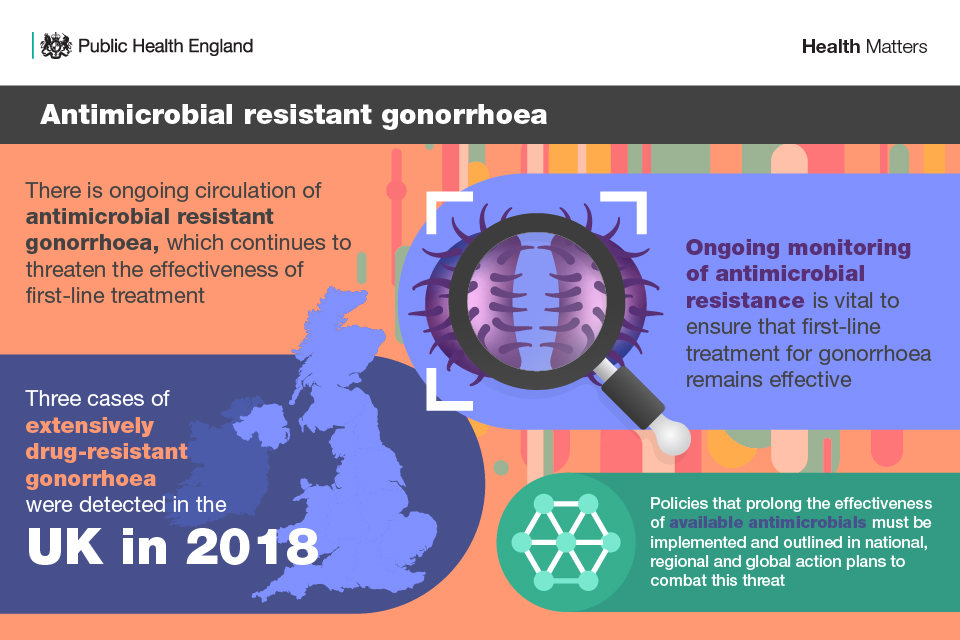
Antimicrobial resistant gonorrhoea
The large increase in gonorrhoea diagnoses in England between 2017 and 2018 is a public health challenge.
The emergence and circulation of antimicrobial resistance (AMR) in Neisseria gonorrhoeae (the bacterium which causes gonorrhoea) is a global concern, as there are no classes of antimicrobials to which gonorrhoea has not developed resistance.
In response to increasing resistance to azithromycin, current first-line gonorrhoea treatment in the UK was recently changed from dual therapy of ceftriaxone with azithromycin to monotherapy with ceftriaxone at a higher dose. Fortunately, ceftriaxone resistance remains rare in the UK, with only sporadic cases reported to date.
However, in 2018, a case of N. gonorrhoeae with extensive drug resistance (XDR), including ceftriaxone resistance, was detected in a UK resident man who had acquired the infection in Thailand. Later that year, 2 additional cases of an identical strain were detected in Australia, highlighting the likelihood of global dissemination of the XDR strain.
Subsequently, 2 cases unrelated to the previous cases but with similar resistance profiles were detected in 2 women in different regions of England, both of whom had overlapping sexual networks with UK residents who had travelled to Spain.
These extensively-drug resistant cases were extremely challenging to treat as they were resistant to ceftriaxone and most other drugs used for treating gonorrhoea.
Antimicrobial resistant gonorrhoea
While azithromycin is no longer recommended as first-line therapy, in some cases it is still an antimicrobial option for treating gonorrhoea. However, between 2016 and 2017, the prevalence of azithromycin resistant-gonorrhoea increased from 4.7% to 9.2%.
Additionally, circulation of a strain of N. gonorrhoeae with high-level resistance to azithromycin (HLAziR) in England persists. Cases emerged among heterosexuals in Leeds but spread across England and into sexual networks of MSM as the outbreak progressed. Studies using whole-genome sequencing indicated sustained transmission of N. gonorrhoeae with the HLAziR phenotype on a national scale.
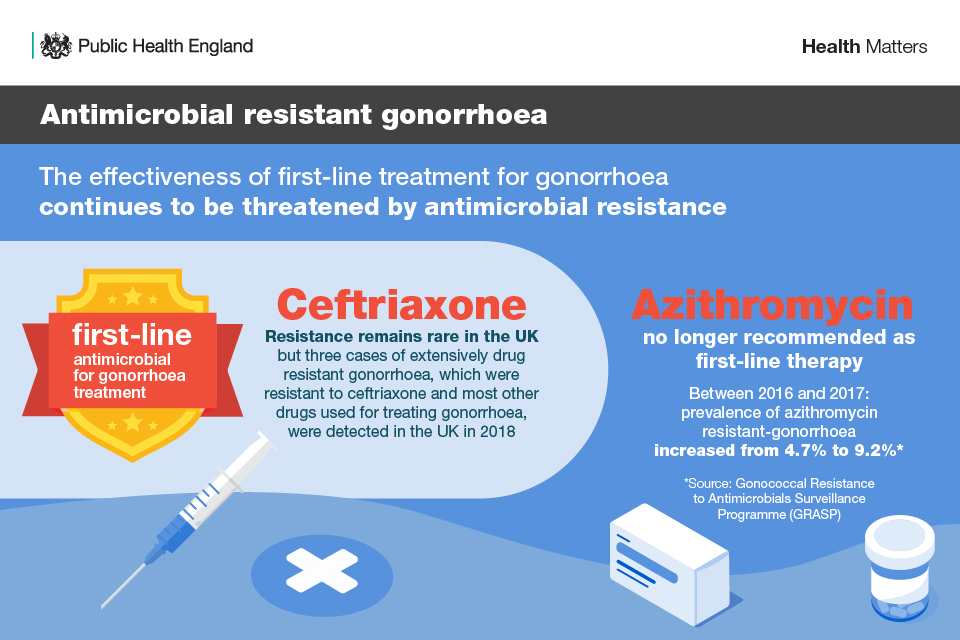
Antimicrobial resistant gonorrhoea - ceftriaxone and azithromycin
To detect any further importations or local circulation of multi- or extensively-drug resistant strains, clinical laboratories should continue to refer N. gonorrhoeae isolates with resistance to ceftriaxone to the PHE Bacteriology Reference Department at PHE Colindale for confirmation.
General Practitioners should refer all suspected cases of gonorrhoea to specialist SHSs for appropriate management.
Ongoing monitoring of AMR is vital to ensuring that first-line treatment for gonorrhoea remains effective, as patterns of resistance can change rapidly. Ineffective treatment facilitates onward transmission and development of adverse sequelae.
Additionally, policies that prolong the effectiveness of available antimicrobials must be implemented and outlined in national, regional and global actions plans to combat this threat.
PHE, the European Centre for Disease Prevention and Control, and the World Health Organization (WHO) have action or response plans in place to control the spread and impact of AMR in N gonorrhoeae.
Antimicrobial resistant Mycoplasma genitalium
Mycoplasma genitalium infection is an STI that is being increasingly recognised as a public health concern due to high levels of AMR. M. genitalium is thought to affect 1% to 2% of the general population, and anywhere between 4% and 38% of people who attend STI clinics.
Co-infection of M. genitalium with other STIs, such as chlamydia, is common and rates are higher in younger people of both sexes and in older age groups of men. It is also more common in people of non-white ethnicity.
The management of M. genitalium infection remains a challenge worldwide, and current treatments are associated with the emergence of multidrug-resistant M. genitalium strains. Further clinical trials are required to formulate and optimise treatment regimens, as newer drugs have shown potential for clinical cure but their inappropriate use may further hamper attempts to manage multidrug-resistant strains.
It is also important for health professionals and local practitioners to be aware of current guidelines and recommended treatment regimens. BASHH has a NICE-accredited national guideline for the diagnosis and management of the infection.
Asymptomatic screening is not recommended. Whilst the guideline sets out recommendations for best practice based on current evidence, not all clinics will currently have access to M. genitalium testing.
A pilot study has been conducted by PHE to determine local estimates of the prevalence of M. genitalium resistance in SHS attendees in England. The findings of this study are due to be published by the end of 2019.
Funding and commissioning SHSs
Responsibility for commissioning sexual health, reproductive health and HIV services is shared across local authorities, clinical commissioning groups (CCGs) and NHS England. These shared responsibilities require a whole system approach to commissioning of these services, and PHE and others have published a range of guidance to support this.
Read Making it work: a guide to whole system commissioning for sexual health, reproductive health and HIV – a joint PHE, Local Government Association (LGA) and DHSC publication.
LGA also have case studies of sexual health commissioning in local government that can be referred to for guidance.
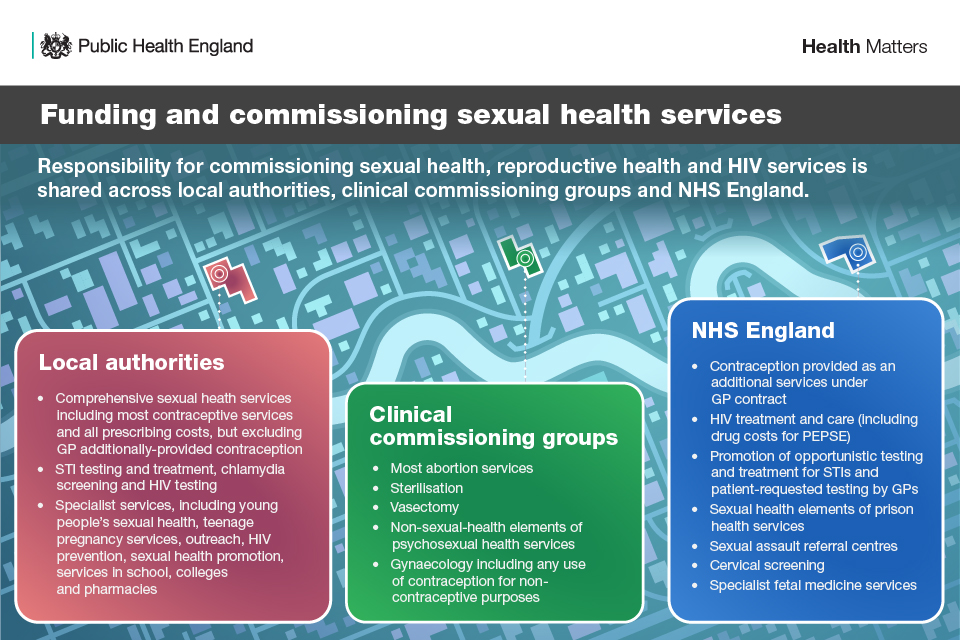
Funding and commissioning sexual health services
In 2016, PHE – with the Association of Directors of Public Health (ADPH) and supported by NHS England and NHS Clinical Commissioners – undertook a review of sexual health, reproductive health and HIV commissioning and surveyed local authorities, NHS England and CCGs.
The survey identified the main challenges faced by commissioners and providers. In response to these findings, PHE and partner agencies developed a commissioning action plan, with 5 areas of action that are intended to improve commissioning:
- reduce fragmentation of commissioning and reduce contracting barriers
- support commissioners in the delivery of effective commissioning
- build capability in commissioning
- provide evidence and data to support commissioning and the monitoring of outcomes
- ensure that sexual health, reproductive health and HIV commissioning is explicitly considered within the development of the new funding mechanisms for public health
Funding cuts
Given reductions in the public health grant, local authority spending on sexual health has fallen significantly, with a 14% reduction in real terms between 2013 to 2014 and 2017 to 2018. Spend fell by £41 million (7%) between 2014 to 2015 and 2016 to 2017 for mandated SHSs, and by £16.8 million (24%) for non-prescribed sexual health functions spending, including prevention. These cuts have occurred together with increasing attendances at services.
Local authorities have brought a greater focus on contracting for SHSs, and often achieved improvements in value for money. However, there has been significant variation in local authorities’ funding decisions across the country, and variation often does not reflect local need. Between 2013 to 2014 and 2017 to 2018, a total of 18 (12%) local authorities increased their total spend on SHSs, while 133 (88%) decreased it.
Providers and commissioners have said that the challenge with persistent funding cuts is the negative impact it has on delivering fit-for-purpose and high-quality services. They have also said that it affects their ability to focus on anything beyond the minimum requirements - mandated STI testing, treatment services and contraception services.
Feedback on cuts to funding for prevention activities and wider supportive services indicate that an adverse consequence of this is the reduction of outreach services for vulnerable groups. PHE has recognised that this funding must be sufficient and adequate in order to deliver and improve SHSs.
National (HIV self-sampling) and local online services are being implemented to help manage overall increases in demand for services, particularly among lower risk and asymptomatic patients. As these services develop, they have the potential to reach groups not currently engaged with clinic services, but there is also the risk they widen inequalities. Therefore, monitoring and evaluation of these services is critical.
Improving the commissioning process is not the sole solution. There is a need to look carefully at a wide range of issues in conjunction with improving commissioning. Together with the STI prevention efforts outlined above these include:
- how to affect behavioural change
- targeted use of marketing
- tackling skills shortages in clinical staff
- ongoing education
The NHS Long Term Plan and commissioning review
Following a review of commissioning arrangements for sexual health and other local authority-commissioned public health services, as set out in paragraph 2.4 in the NHS Long Term Plan, Secretary of State for Health and Social Care Matt Hancock confirmed in June 2019 that there would be no change to the commissioning responsibilities of both local government and the NHS.
The review also recommended that the NHS work much more closely with local authorities on public health, to ensure that commissioning is more joined-up and prevention is embedded into a wider range of health services.
Similar claims about the issues around fragmentation were made in 2008. This is why it is particularly important to work in partnership across commissioners and providers.
The Prevention Green Paper explains that government would like to see the NHS and local authorities working more closely - at both the national and local level - to make collaborative commissioning the norm, building on best practice from across the country.
The Green Paper sets out that the shift towards Integrated Care Systems (ICSs) creates the opportunity to co-commission an integrated sexual and reproductive health service. Some areas, such as Hampshire, are already doing this and, throughout the review, it was made apparent that there are different ways of taking collaborative commissioning forward and local areas must decide what suits them best.
The document encourages more areas to use their existing powers and levers to develop joint approaches. This may include more consistent co-commissioning arrangements and making the best use of Health and Wellbeing Boards.
This case study exemplifies how collaborative commissioning of SHSs was carried out in Teesside.
Government is also considering calls from the Health and Social Care Committee (HSCC) and others to develop a new Sexual and Reproductive Health Strategy for England. A full response to the select committee report is being published shortly.
The Green Paper requests views on the development of a new strategy, and the top 3 areas that any new strategy should prioritise.
Call to action
Preparing for RSE
In order to prepare for the implementation of relationships education and RSE at primary and secondary level, it is important for local authorities to ensure all schools in their area have the details of their local sexual and reproductive health services.
Local authorities can also promote the RSE briefing for councillors, published by PHE, LGA, RSE Hub, and the Sex Education Forum. The Roadmap to Statutory RSE, published by the Sex Education Forum and PSHE Association, should also be promoted as it provides practical advice on preparing for the statutory RSE that will come into effect from September 2020.
Health promotion and condom use
There is NICE guidance on condom distribution schemes for:
- local authority commissioners of SHSs
- providers of condom distribution schemes
- practitioners working in specialist and general SHSs
The guideline includes recommendations on:
- targeting services
- multicomponent condom distribution schemes for young people in health, education, youth and outreach settings
- single component schemes
PHE and Brook have also published a Condom-Card Scheme guide, which showcases 6 years of practitioners’ experience commissioning, developing and providing these schemes.
Resources such as the NHS’ Find Free Condoms services should be promoted.
Data and evidence
PHE recognises the need for information in support of commissioning and will continue to support local systems by providing a wide range of data and information. Extensive information provided by PHE is in the form of:
- sexual and reproductive health profiles
- local authority sexual health epidemiology reports (LASERS)
- HIV/STI web portal reports
- national trends in gonococcal AMR and the proportion of local laboratories performing sensitivity testing according to national standards
- Sexual health, reproductive health and HIV in England: a guide to local and national data
As detailed above, PHE also has health economics tools that can be used by local authorities and commissioners to inform their decisions around commissioning SHSs and other interventions that enable good sexual health outcomes. These include:
PHE will support commissioners and providers to identify the ‘best way’ to achieve the desired outcome. Evaluating interventions is a key tool to see the impact of the changes made locally and add to the evidence base that others can draw on.
To this end, PHE has published a suite of evaluation resources for sexual health, reproductive health and HIV, including an introductory guide, workbook, and menu of output and outcome measures.
Commissioning
In order to ensure robust sexual health services and care pathways for service users, collaborative and whole-system working between commissioners is essential.
The commissioning survey action plan identified a range of actions for PHE and partner agencies to take forward, including publication of further guidance and supporting local areas to pilot approaches to collaborative commissioning. The evaluation of these pilots will be shared with local areas.
Further guidance: Commissioning local HIV sexual and reproductive health services and Public health services non-mandatory contract
Read this blog on supporting sexual health commissioning to find out more.
The LGA will shortly be publishing a further range of case studies of collaborative working at local levels. Many areas are working together effectively and local areas are encouraged to learn from these experiences and also to feed into the Green Paper consultation on what more can be done to help local authorities and NHS bodies work well together and to suggest priorities for a new Sexual and Reproductive Health Strategy for England.
Testing and treatment
BASHH recommends that at least 97% of people with needs related to STIs are offered a sexual health screen when they attend SHSs. This is essential to control the transmission of STIs such as gonorrhoea and syphilis.
PHE encourages local areas to ensure chlamydia screening is delivered as effectively and efficiently as possible through the chlamydia care pathway.
The pathway provides commissioners and providers with a supported and systematic approach to evaluating local chlamydia activities with the aim of improving outcomes for users and services.
It also allows local areas to explore and review local chlamydia activities and to create and instigate data-driven action plans to improve service provision and outcomes.
The National HIV Self-Sampling Service is delivered through a framework commissioned by PHE. Local authorities can choose to sign up to the framework to commission online HIV self-sampling services for their residents.
Self-sampling involves a person taking their own sample using a specimen collection kit and sending it to a laboratory for testing. The results are then communicated to the individual directly, usually via text message for negative results and telephone for reactive results.
From November 2019, the service will also give local authorities the option to include syphilis testing for their residents. During national campaigns, such as National HIV Testing week, PHE funds the HIV self-sampling service to ensure it is open to all residents in England during the national campaign period. From 2019, syphilis will be an option during this period.
Managing outbreaks and incidents
PHE has developed national guidance to support local teams to investigate STI outbreaks and incidents, which provides:
- information on planning an outbreak control strategy
- detection systems
- roles and responsibilities
- capacity and resources needed
- communications
- processes for investigation, control and evaluation once an outbreak control team has been convened
PHE also recommends that all suspected treatment failures for gonorrhoea, chlamydia, Mycoplasma genitalium, and Trichomonas vaginalis should be reported to PHE via the HIV/STI web portal.
Clinical services or laboratories that identify potentially highly resistant or unusual cases of STIs, or faulty diagnostic tests, should report and refer relevant specimens to PHE’s national reference laboratory for further investigation.
Resources
Health matters case studies contain information on projects and approaches that have been put in place to improve public health:
