Health matters: increasing the uptake of HIV testing
Published 1 December 2016
The scale of the problem
How common is HIV
An estimated 101,200 people were living with HIV in the UK in 2015. Of these, around 1 in 8 (13%) were unaware that they were living with the virus and may be at risk of passing it on.
The number of people being diagnosed with HIV in the UK has remained steady over the past few years. In 2015, 6,095 people (4,551 men and 1,537 women) were diagnosed with HIV in the UK, according to PHE figures. The equivalent figures for England were 5,512 (4,088 men and 1,417 women).
The HIV epidemic remains largely concentrated among gay, bisexual and other men who have sex with men (hereafter referred to as gay or bisexual men), and black African men and women. However, anyone can acquire HIV regardless of age, gender, ethnicity, sexuality or religion.
Just over half (54% or 3,320 of 6,095) of all new HIV diagnoses in 2015 were reported among gay or bisexual men. Although a slight decline from the 3,360 diagnoses in 2014, numbers remain high. This reflects high levels of HIV testing as well as ongoing transmission in this group. It is estimated that around 3,000 gay or bisexual men acquire HIV infection each year.
A total of 2,360 new diagnoses were reported in heterosexual men (1,010) and women (1,350) in 2015. This is about half the number of diagnoses made 10 years prior (4,340). The fall is largely due to changing migration patterns, with fewer people born in sub-Saharan Africa being diagnosed with HIV in the UK.
Over half of heterosexuals diagnosed in the UK are estimated to have acquired the virus while living in the UK.
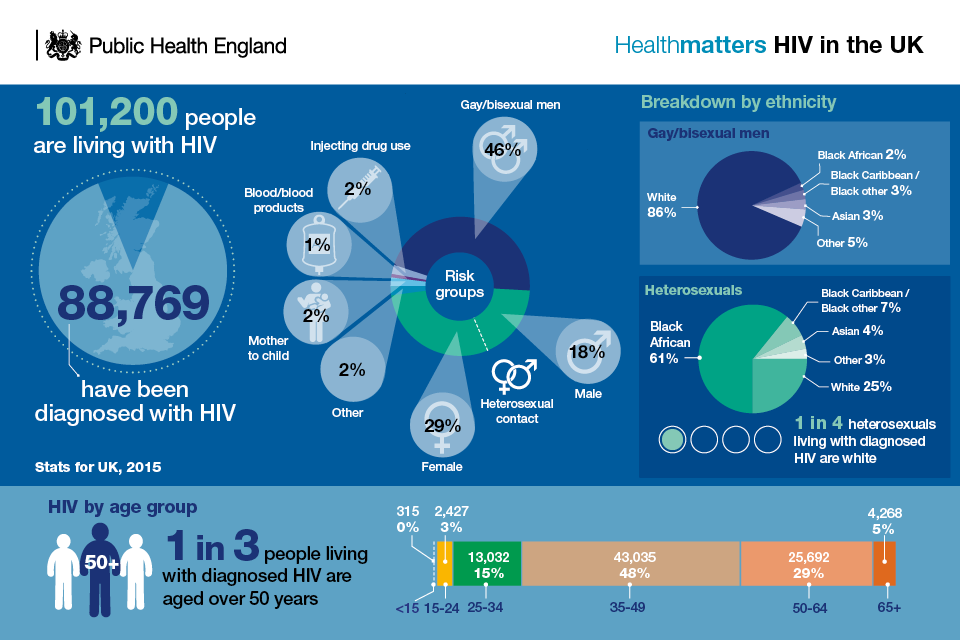
Infographic showing HIV statistics for the UK
Late diagnosis
Having an HIV infection is no longer a death sentence. Early diagnosis and effective treatment means that people with HIV are able to live a normal life well into old age.
However, 39% of adults with HIV were diagnosed at a late stage of infection in 2015.
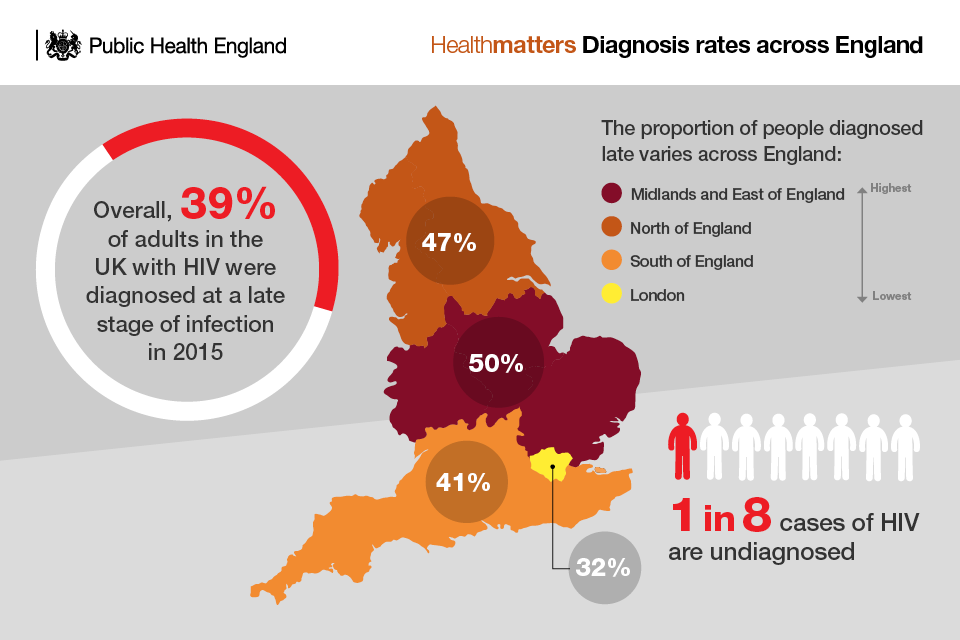
Infographic showing HIV diagnosis rates across England
Someone is considered to have been diagnosed late if they have a CD4 count below 350 cells per mm³ within 3 months of diagnosis.
Late HIV diagnoses are more common among those diagnosed later in life. In 2015, 55% of those aged 50 to 64 years were diagnosed late, with 63% among those aged 65 years and over. This not only reflects the fact that older people may be living with HIV for longer before they are diagnosed but also continuing transmission among older age groups. It is estimated that about half of people diagnosed with HIV at age 50 years and over acquired their infection whilst aged over 50.
People who are diagnosed late have a 10-fold risk of mortality within the first year of diagnosis compared to those diagnosed promptly (3.2% compared to 0.36%). The majority of the 594 people living with HIV who died in 2015 were diagnosed late. Just under half of these deaths were likely to be AIDS-related.
Why HIV testing is important
PHE wants to reduce late HIV diagnoses through improving the coverage and uptake of HIV testing. Improving HIV testing coverage and uptake will help to:
- eliminate all AIDS-related deaths
- diagnose HIV before people become unwell
- reduce HIV transmission by:
- decreasing the number of people living with an undiagnosed HIV infection
- increasing the number of people successfully treated so that they are no longer infectious
It will also help to ensure that the UK meets all aspects of the United Nations UNAIDS 90:90:90 vision for 2020, to end the AIDS epidemic by 2030. This calls for:
- 90% of people living with HIV to be diagnosed
- 90% of those diagnosed to receive treatment
- 90% of those treated to be virally suppressed
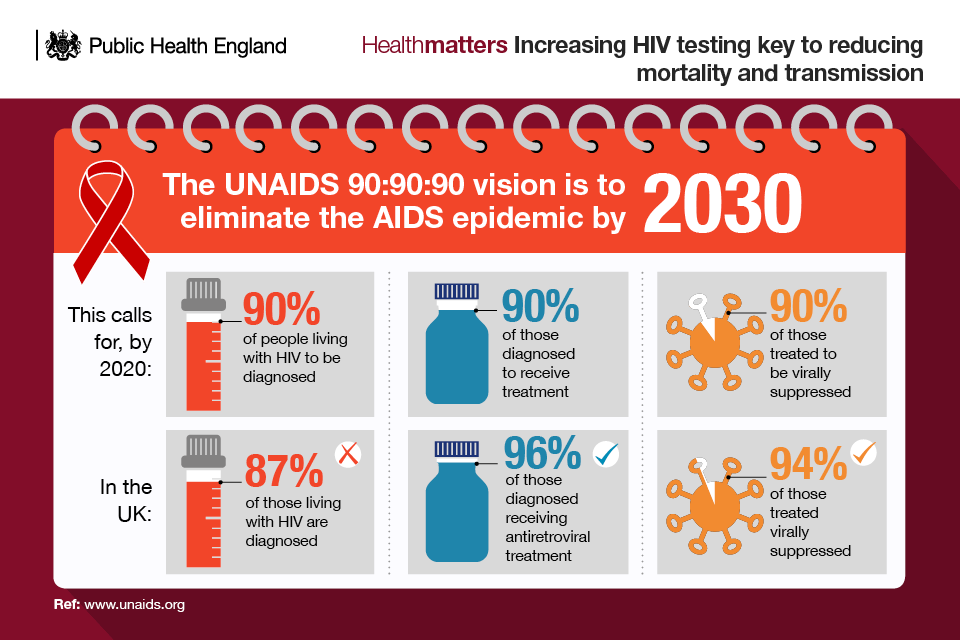
Infographic describing the UNAIDS 90, 90, 90 vision to eliminate the AIDS epidemic by 2030
In 2015, the number of people diagnosed with HIV reached 87%, with treatment coverage at 96% and viral suppression at 94%. Cumulatively, this means that the substantive UNAIDS target of 73% has been surpassed in the UK, reaching 78% in 2015.
Now is the time for collaborative action to address the first target and work towards 90% of people living with HIV being diagnosed.
Increasing HIV testing uptake will also help commissioners in public health and the NHS to deliver reductions in health inequalities, given that HIV disproportionately affects minority groups such as gay or bisexual men and black Africans.
Opinion leader panel discussion on increasing the uptake of HIV testing
Opinion leader panel discussion on increasing the uptake of HIV testing
What testing involves
Testing is the only way to find out if an individual has HIV and is central to prevention efforts to eliminate AIDS-related deaths and to reduce HIV transmission.
It has never been easier to have an HIV test. The test itself usually involves taking a blood sample, which is then sent off to a laboratory for testing. Other tests that use a finger-prick or saliva sample are also available.
HIV tests are available free and confidentially from:
- sexual health clinics
- HIV testing centres
- GP practices
- secondary care services
- some pharmacies
- an antenatal clinic if you are pregnant
- local drugs agencies if you are an injecting drug user
The charity NAM has an online HIV test finder to locate testing services in your local area.
More than 1.1 million HIV tests were carried out in specialist sexual health clinics (GUM clinics and integrated GUM or sexual and reproductive health services) in England in 2015. This identified 2,850 people with new HIV diagnoses.
HIV testing in specialist sexual health clinics has increased steadily over the last 5 years, including a 47% increase in HIV testing among gay, bisexual and other men who have sex with men (gay or bisexual men).
PHE advises that gay or bisexual men have an HIV and STI screen at least annually, and every 3 months if having unprotected sex with new or casual partners.
Persons born in a high prevalence country are advised to have an HIV test and a regular HIV and STI screen if having unprotected sex with new or casual partners.
People who test HIV positive are rapidly linked to specialised services; 97% of those newly diagnosed are linked to care within 3 months of diagnosis.
Self-sampling
PHE has co-commissioned a national HIV self-sampling service through the website www.freetesting.hiv, in partnership with 85 local authorities.
The aim of this service is to provide a cost effective and clinically robust remote HIV sampling service for sexually active individuals aged 16 years and over. Emphasis is placed on increasing HIV testing among most at-risk groups including gay or bisexual men and black African populations (and other black communities at increased risk of HIV).
The service, which complements other local HIV testing services, operates at no financial expense to the service user and is independent from other STI remote sampling and testing services.
PHE is funding all home sampling kits dispatched between 7 November 2016 and 8 January 2017 in support of National HIV Testing Week – to try and reach even more people at risk.
The original objective was to distribute 50,000 kits in its first year and over 40,000 kits have been delivered to date, reporting a 1.1% reactive rate.
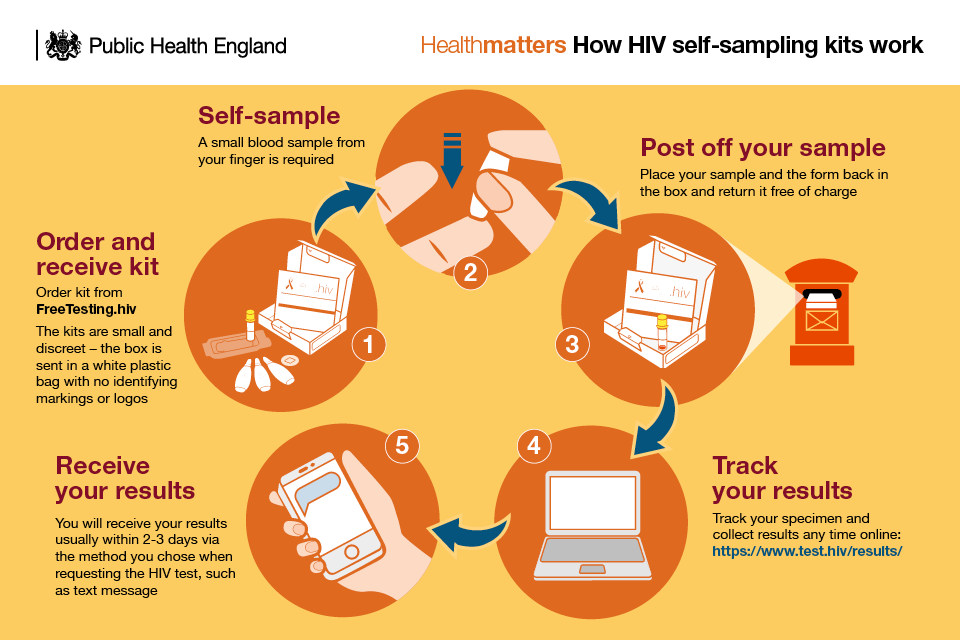
Infographic showing how HIV self-sampling kits work
Self-testing
Self-testing kits for HIV are also available. With HIV self-test kits, an individual will take a sample, test it themselves and obtain their result immediately without the need to send the sample to a laboratory.
The window period for self-testing kits is 3 months. This means a self-testing kit is not guaranteed to pick up an infection that has been acquired in the previous 3 months.
Increasing opportunities for testing
Normalise testing
To encourage more people to get tested, HIV testing services should communicate that:
- HIV is no longer a fatal infection but a chronic manageable disease
- treatment is available that allows the vast majority of people with HIV infection to be considered non-infectious
- regular HIV testing should be seen as a routine healthy behaviour and it has never been easier to have an HIV test
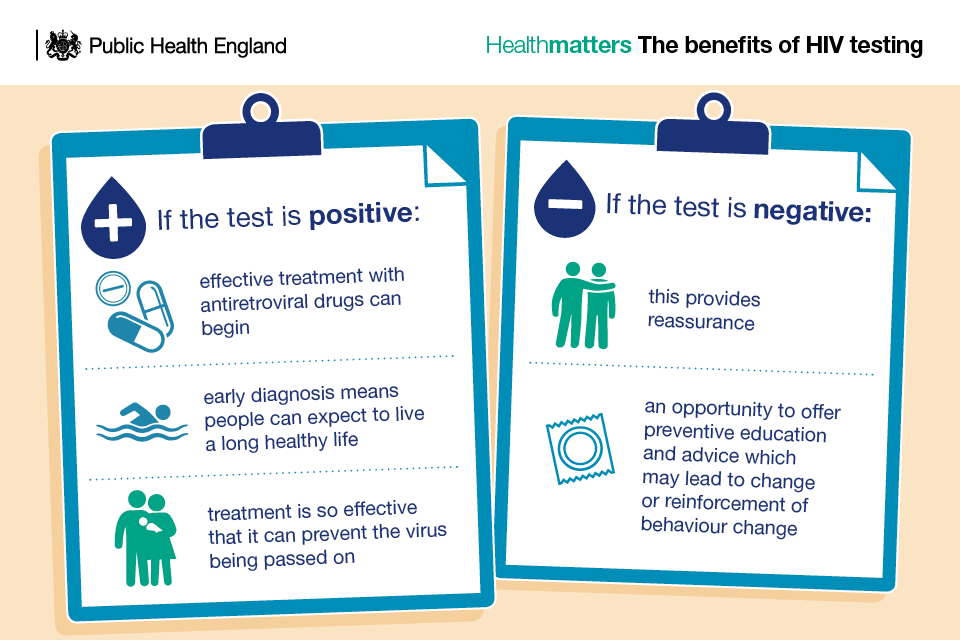
Infographic showing the benefits of HIV testing
Understand local need
It is essential that services are aware of the prevalence of HIV in their local area and the potential demand for HIV testing.
NICE has worked with PHE to develop new HIV guidance that defines a prevalence of between 2 and 5 diagnosed HIV cases per 1,000 people aged 15 to 59 as being a high prevalence area that may require additional testing interventions.
The guidance also defines areas with extremely high prevalence as having a diagnosed HIV prevalence of 5 or more per 1,000 people aged 15 to 59 years.
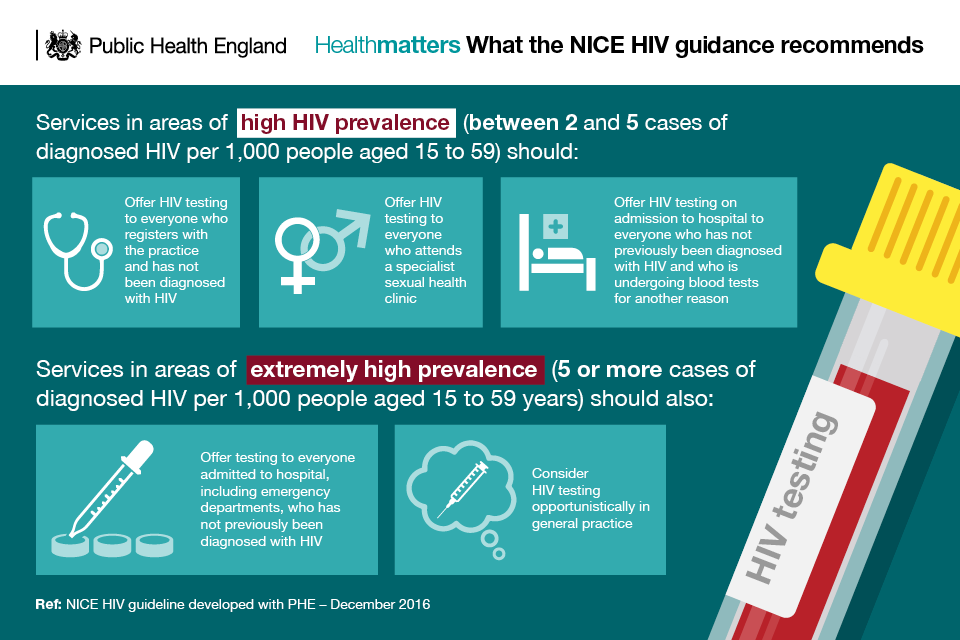
Infographic showing what the NICE HIV guidance recommends
In areas of high and extremely high prevalence, HIV testing should be offered to everyone who has not previously been diagnosed with HIV and who:
- registers with their GP practice or
- is undergoing blood tests for another reason and has not had an HIV test in the previous year
In extremely high prevalence areas, services should consider HIV testing opportunistically.
PHE’s Sexual Health and Reproductive Health Profiles can help local authorities and NHS services identify whether they are in a high prevalence area and provide further data on:
- late diagnosis rates
- HIV testing uptake and coverage in sexual health clinics
Innovative approaches to testing
PHE is funding 13 projects that offer new and innovative ways of delivering HIV prevention via The National HIV Prevention Innovation Fund. The successful projects all target groups at high risk and are supported by their local authority.
This includes programmes to introduce HIV testing into new settings, engaging with workplaces and faith leaders to involve them in the delivery of HIV prevention work and providing new digital solutions to enable easier contact tracing and partner notification.
Raise awareness of HIV testing
Implementing social marketing campaigns is an essential component for raising awareness. The national HIV prevention programme is building on the assets and engagement of previous campaigns, while rejuvenating new efforts with creative and innovative features based on the latest strategies in commercial media, social marketing and health promotion.
The ‘It Starts with Me’ annual summer campaign (May to August) aims to reduce new infections though condom promotion and reduce undiagnosed HIV infection through increased testing. It aims to engage people with a call to action related to condom use, risk reduction and HIV testing.
PHE commissioned an evaluation of the ‘It Starts with Me’ campaign, which was conducted after National HIV Testing week in 2015. This found that among those who had seen the campaign:
- 29% of gay or bisexual men reported getting tested as a result
- 21% of black Africans reported getting tested as a result
- 19% of gay or bisexual men reported ordering an HIV self-sampling kit
National HIV Testing Week (November) raises awareness of the importance of HIV testing as well as motivating clinical and voluntary sector providers to increase opportunities to test – be it in clinical settings, in primary care, through community-based rapid testing or via postal testing. The ultimate goal is to increase regular HIV testing in the most affected groups.
HIV Prevention England’s resource centre provides free promotional materials, such as leaflets and posters, to organisations engaged in HIV prevention and testing work in England.
An example of a regional approach is the London-wide sexual health campaign Do It London. This programme, a collaboration of all 33 local authorities in London, aims to increase HIV testing and promote safer sex to all residents in the capital.
Reducing barriers to HIV testing
The guidance from NICE outlines a number of ways to address barriers to HIV testing that testing services should consider, including:
- advertising HIV testing in settings that offer it and making people aware that healthcare professionals welcome the opportunity to discuss HIV testing
- being able to discuss HIV symptoms and the implications of a positive or a negative test
- being familiar with existing referral pathways so that people who test positive receive prompt and appropriate support
- providing appropriate information if someone tests negative, including details of where to get free condoms and how to access local behavioural and preventive interventions
Stigma around HIV
Stigma around HIV and sexual behaviour can be a barrier to testing and may dissuade people from getting tested on a regular basis. Those responsible for HIV testing should emphasise that testing is free and confidential and that there is no obligation to disclose your status to your employer or insurance company.
NICE stresses the importance of recognising and being sensitive to the cultural issues facing different groups, such as black Africans who may be less used to preventive health services and advice, or may fear isolation and social exclusion if they test positive for HIV.
Barriers to HIV testing among health professionals
Barriers to HIV testing are not just an issue for at-risk groups. Health professionals in general practice can be prevented from offering HIV testing by the misconception that:
- general practice is not funded to provide HIV testing
- HIV testing is complicated and too expensive
- testing will scare patients unnecessarily
- sexual health clinics are more confidential and a better setting for testing
- there is a lack of time to discuss HIV testing with patients
The Medical Foundation for HIV and Sexual Health (MEDFASH) has more information on commonly-cited barriers and challenges among health professionals in general practice, and resources to help increase HIV testing in general practice.
During 2016 to 2017, the Royal College for General Practitioners is working with the Terrence Higgins Trust to focus on prioritising sexual and reproductive health and HIV care in primary care. This includes a programme of education for the entire primary care workforce including practice nurses, reception staff and medical staff, using face-to-face interventions, on-line training and events.
Specific projects will be developed based upon increasing HIV testing, enhancing patient care for people living with HIV and addressing HIV stigma.
Call to action
There is no doubt that a step change is required in order to reduce the rate of new HIV infections in England and regain some of the ground that has arguably been lost in recent years. This will require new ideas and ways of working, as well as a more joined-up approach across the system.
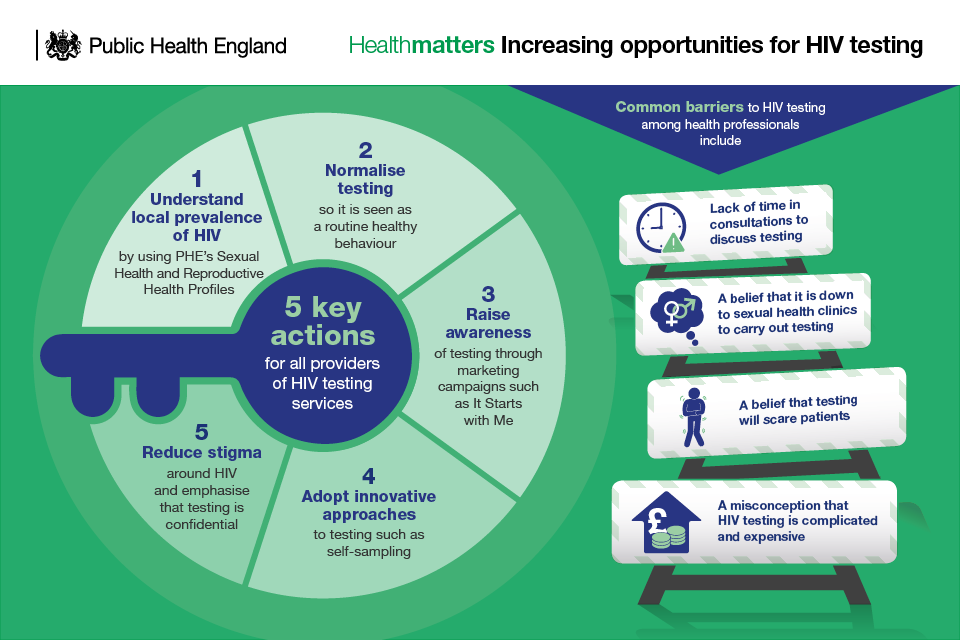
Infographic about increasing the opportunities for HIV testing
Local authorities
By building on the links already in place with local health and social care and voluntary sector providers, local authorities are well positioned to promote HIV testing among local at-risk populations.
They can do this through:
- leadership
- sharing of local intelligence
- promoting the Making Every Contact Count initiative
- identifying and working with relevant NHS and community services to improve access to services
Read a case study about the London HIV Prevention programme.
Local areas should also ensure that interventions to increase the uptake of HIV testing are hosted by, or advertised at, venues that encourage or facilitate sex (such as some saunas, websites, or geospatial apps that allow people to find sexual partners in their proximity). This should be in addition to general community-based HIV health promotion.
Read a case study about digital vending technology and HIV self-testing.
GP practices
GP surgeries should use or modify existing resources, for example TV screens, to help raise awareness of where HIV testing is available, including self-sampling.
They should also offer and recommend HIV testing, based on local prevalence and how it affects different groups and communities.
In all areas, GP practices should offer and recommend HIV testing to everyone who:
- has symptoms that may indicate HIV or HIV is part of the differential diagnosis (for example, infectious mononucleosis-like syndrome), in line with HIV in Europe’s HIV indicator conditions
- is known to be from a country or group with a high rate of HIV infection
- if male, discloses that they have sex with men, or is known to have sex with men, and has not had an HIV test in the previous year
- is a trans woman who has sex with men and has not had an HIV test in the previous year
- reports sexual contact (either abroad or in the UK) with someone from a country with a high rate of HIV
- discloses high-risk sexual practices, for example the practice known as ‘chemsex’
- is diagnosed with, or requests testing for, a sexually transmitted infection
- reports a history of injecting drug use
- discloses that they are the sexual partner of someone known to be HIV positive, or of someone at high risk of HIV (for example, female sexual contacts of men who have sex with men)
In areas of high and extremely high prevalence, also offer and recommend HIV testing to everyone who has not previously been diagnosed with HIV and who:
- registers with the practice
- is undergoing blood tests for another reason and has not had an HIV test in the previous year
In areas of extremely high prevalence, consider HIV testing opportunistically (whether bloods are being taken for another reason or not), based on clinical judgement.
Secondary and emergency care
The NICE guideline on HIV recommends routinely offering and recommending an HIV test to everyone attending their first appointment at drug dependency programmes, termination of pregnancy services, and services providing treatment for:
- hepatitis B
- hepatitis C
- lymphoma
- tuberculosis
In areas of high and extremely high prevalence, services should offer and recommend HIV testing on admission to hospital, including emergency departments, to everyone who has not previously been diagnosed with HIV and who is undergoing blood tests for another reason.
Additionally, in areas of extremely high prevalence, services should offer and recommend HIV testing on admission to hospital, including emergency departments, to everyone who has not previously been diagnosed with HIV.
Specialist sexual health clinics
Specialist sexual health services (including genitourinary medicine) should offer and recommend an HIV test to everyone who attends for testing or treatment.
HIV test coverage among eligible people attending specialist sexual health clinics in England was 67%. This low coverage level meant that 16,271 black Africans, 14,548 people born in high prevalence countries and 13,381 gay or bisexual men attended a specialist sexual health clinic but did not receive an HIV test.
PHE’s HIV testing report states that specialist sexual health clinics should improve the notification and testing of sexual partners of people with HIV. HIV partner notification had the highest positivity rates of all HIV testing activities (5.3%), but only 97 HIV diagnoses were reported through this system.
Positivity rates were highest in clinics in extremely high prevalence areas, where 10% of those tested through HIV partner notification were diagnosed with HIV. However, these clinics had the lowest partner notification testing ratios (contacts tested/new HIV diagnoses) in the country (0.2).
Specialist sexual health clinics should look to increase HIV testing among women in particular. Women attending specialist sexual health clinics were less likely to be offered (82%) or to receive (59%) an HIV test than men (90% and 78%, respectively). These lower rates include black African women whose HIV positivity rates were 18 times higher than other women attendees (1.8% v.s. 0.1%).
Read a case study about using a web-chat facility to promote HIV prevention support.
Community testing services or third sector
Testing services should be set up in:
- areas with a high prevalence or extremely high prevalence of HIV, using venues such as pharmacies or voluntary sector premises
- venues where there may be high-risk sexual behaviour, for example public sex environments, or where people at high risk may gather, such as nightclubs, saunas and festivals
It is important to recognise that not all community settings are appropriate for providing testing services; it is important that the setting allows for testing to be undertaken in a secluded or private area.
It is also important that people who decline or are unable to consent to a test are offered information about other local testing services, including self-sampling.
Read a case study about using community pharmacists to provide HIV testing in Cumbria.
Read the Health matters blog.
