HPR volume 13 issue 31: news (6 and 9 September)
Updated 20 December 2019
HIV in the UK: annual data release in summary
There were 4,484 new HIV diagnoses reported in 2018, a 6% decline relative to 2017, according to Public Health England ‘s (PHE’s) latest annual HIV data release [1,2], reported in this issue of the Health Protection Report (HPR) [3].
The decline in new diagnoses in 2018 was the third successive year-on-year decline, a trend, amounting to a 28% overall drop since 2015, that has been manifest in both heterosexual, and gay and bisexual, populations. The steepest falls have been seen among gay and bisexual men, where new diagnoses declined by 39% between 2015 and 2018.
Despite falling rates of new diagnoses there remain challenges in ensuring that more people are diagnosed early. Almost half (43%) of those newly diagnosed with HIV in 2018 were at a late stage of infection.
There was substantial variation between sub-populations in rates of late diagnosis; the late diagnosis proportion was 60% (372/621) among heterosexual men, 52% among black African adults (346/669), and 59% in those aged 50 and older (399/673).
The overall, continued decline in new diagnoses in the UK is largely due to the success of combination HIV prevention over the past decade, which includes HIV testing, condom provision, the scale-up of pre-exposure prophylaxis (PrEP) and anti-retroviral therapy (ART).
The HPR report notes that it is too early to determine the additional effect on HIV transmission and new HIV diagnoses of the scale-up of PrEP, which is the subject of a three-year trial which began in October 2017 and will culminate in 2020 [2].
Further epidemiological commentary relating to the fall in new diagnoses in 2018 will be contained in PHE’s annual HIV report to be published in November.
References
- GOV.UK (3 September 2019). HIV annual data tables [Official statistics].
- New HIV diagnoses fall by a third since 2015, PHE press release, 3 September 2019.
- Trends in new HIV diagnoses and in people receiving HIV-related care in the United Kingdom: data to the end of December 2018, HPR 13(31).
Annual review of infections in UK blood, tissue and organ donors
The joint NHS Blood and Transplant (NHSBT) and PHE epidemiology unit has published its annual review of research and data gathering activity entitled, Safe Supplies 2018: Monitor, Inform, Progress. [1,2]
The joint unit is responsible for the surveillance systems which report on infections in blood, tissue, cell and organ donations across the UK. This year’s review covers: the work done by the unit during 2018 in monitoring the effects of a change to donor selection criteria implemented in 2017; updated residual risk estimates; and a summary of reported transfusion-transmitted infections.
A combination of donor selection and donation testing is used by the UK’s blood services to maintain safety. Recently SaBTO, the Department of Health and Social Care’s expert committee on blood safety, reviewed donor selection policies related to sexual behaviours and made several recommendations to government. This resulted in the English, Welsh and Scottish blood services (in November 2017) changing their donor selection criteria, for the following donor categories, from a 12-month to a 3-month deferral since last sex: donors with partners who may be at increased risk of acquiring a blood-borne infection (for example, men who have sex with men; and commercial sex workers).
A year after these changes were implemented, current surveillance data suggest, there has been no resultant increase in non-compliant donors, nor any increase in recently acquired infections due to a known deferrable risk factor.
Of the almost 1.9 million whole blood and platelet donations made by around 1.2 million donors in the UK in 2018, only 602 were confirmed positive for the mandatory markers of infection and thus removed from the supply. Most confirmed positive donations were due to either past or chronic infections, only a small number of newly acquired or acute infections were identified. Most recent infections were due to syphilis, 7 were acute hepatitis B infections and 3 were recent HIV infections.
Residual risk and transfusion-transmitted infection
Of the 40 donors with recent infections in 2018, 6 did not fully disclose deferrable risks at the time of donation. The residual risk of not detecting a HBV, HCV or HIV window period donation on screening remained extremely low (one in 1 million donations tested). More information is available on the JPAC website. There was one confirmed HEV transfusion-transmitted infection (TTI) and one probable HBV TTI reported in 2018.
Bacterial screening of platelets is in place across all UK blood services with detection rates remaining relatively constant year-on-year. Among both apheresis and pooled platelets screened in 2018, the confirmed positive rate for each UK blood service was less than 0.1%, with most bacteria identified on screening originating from the skin.
Bacterial safety measures do not completely remove the risk of a positive unit being released so vigilance remains important. Transfusion-transmitted infections continue to be extremely rare and in 2018, among 97 incidents investigated by the blood services, there was one probable Staphylococcus epidermidis transmission reported to SHOT. It was not possible to confirm whether this was due to transfusion or reflected an ongoing infection in the patient.
Horizon scanning
Another role of the joint unit is in horizon scanning for infectious diseases that could potentially affect the safety of the UK blood supply, particularly new and emerging infections, in conjunction with colleagues across PHE and blood services across the world. Data contribute to risk assessments and may result in additional tests or changes to donor selection criteria being implemented; for example, the spread of West Nile Virus to Slovenia in 2018 resulted in an additional test being requested from donors returning from that country.
Further information
Individuals interested in donating blood should visit blood.co.uk or call 0300 123 2323 for further information.
To join the organ donor register visit www.organdonation.nhs.uk.
Further information about the data held by the NHSBT and PHE joint epidemiology unit is available from epidemiology@nhsbt.nhs.uk.
References
-
GOV.UK (28 August 2019). Safe supplies: annual review.
-
NHSBT (August 2019). Annual review of the NHS Blood and Transplant (NHSBT) and Public Health England (PHE) epidemiology unit’s data and research activity.
EVD outbreak in eastern DRC: thirteenth update
The Ebola virus disease (EVD) outbreak in the Democratic Republic of the Congo (DRC) continues into its fourteenth month. During August 2019, there was little change in transmission intensity and further geographical spread with 4 new health zones and a third province reporting their first cases.
As of 3 September 2019, 2,940 confirmed and 109 probable cases had been reported in North Kivu, Ituri and South Kivu provinces [1]. Of these, 2,050 had died but over 900 patients survived the infection. Between 1 and 31 August, 307 newly confirmed cases were reported, the lowest monthly total since March 2019.
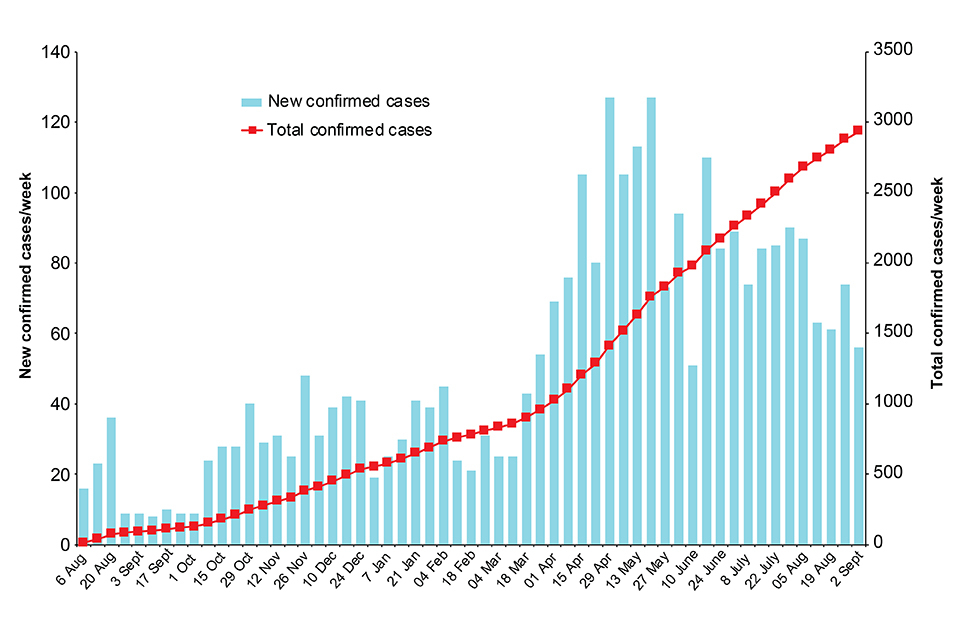
New and total confirmed cases by week. Data provided by WHO.
The first cases in South Kivu province were 2 individuals (mother and child) who had had contact with a confirmed case in Beni (North Kivu) before travelling south to Mwenga health zone [2]. In total, 6 cases were confirmed here in 2 family clusters, the second of which followed a nosocomial transmission [3].
On 29 August 2019, a new EVD case was confirmed in Uganda [4]. The patient was a young child who had been exposed and developed symptoms in DRC and was taken by her mother to seek medical care in Uganda. She was detected at the Mpondwe-Kasindi border point and immediately transported to an Ebola Treatment Centre in Kasese district (Uganda). There have not been any further cases associated with this incident in Uganda to date.
There are 29 affected Health Zones in the 3 affected provinces.
Outbreak response activities continue to be intermittently hampered by security incidents and there is ongoing uncertainty regarding the completeness of surveillance and detection of all new cases.
The risk to the UK public remains very low to negligible. The situation is being monitored closely and the risk assessment regularly reviewed.
Further information sources
- GOV.UK Ebola virus disease: clinical management and guidance
- NaTHNaC website travel advice Travel Health Pro website
- WHO website EVD homepage Ebola virus disease
- FCO travel advice DRC advice
References
- WHO Dashboard (updated daily).
- WHO Africa (20 August 2019). External Situation Report 55.
- WHO Africa (1 September 2019). External Situation Report 57.
- Uganda Ministry of Health, 30 August 2019.
Infection reports in this issue
This issue includes:
