Physical activity: applying All Our Health
Updated 10 March 2022
The Public Health England team leading this policy transitioned into the Office for Health Improvement and Disparities (OHID) on 1 October 2021.
Introduction
This guide is part of ‘All Our Health’, a resource which helps health professionals prevent ill health and promote wellbeing as part of their everyday practise. The information below will help front-line health and care staff use their trusted relationships with patients, families and communities to promote the benefits of physical activity.
We also recommend important actions that managers and staff holding strategic roles can take.
View the full range of ‘All Our Health’ topics
Access the physical activity e-learning session
An interactive e-learning version of this topic is now available to use.
The Office for Health Improvement and Disparities (OHID) and Health Education England’s ‘e-Learning for Healthcare’ have developed this content to increase the confidence and skills of health and care professionals, to embed prevention in their day-to-day practise.
Why promote physical activity in your professional practice?
Physical inactivity is associated with 1 in 6 deaths in the UK and is estimated to cost the UK £7.4 billion annually (including £0.9 billion to the NHS alone).
Unfortunately, our population is around 20% less active than in the 1960s. If current trends continue, it will be 35% less active by 2030.
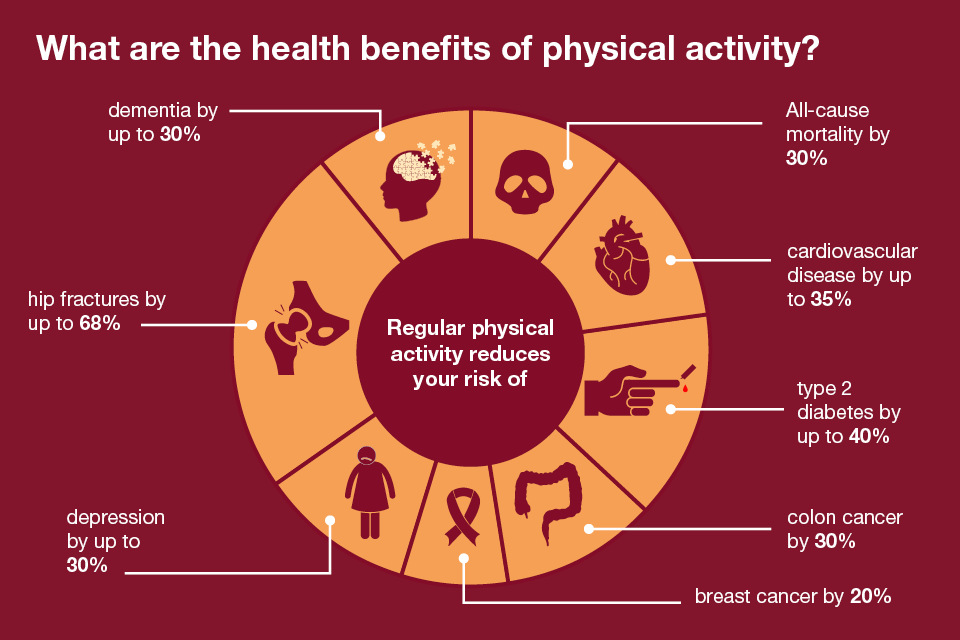
Many people don’t realise that physical activity has significant benefits for health, both physical and mental, and can help to prevent and manage over 20 chronic conditions and diseases, including some cancers, heart disease, type 2 diabetes and depression.
Health benefits of physical activity
Around 1 in 3 (34%) of men and 1 in 2 (42%) of women are not active enough for good health.
Men are more likely to report being active at the recommended level than women.
Physical activity varies with age and life stage. People tend to get less active with age, especially in older years.
And people with disabilities or long-term conditions are twice as likely not to be active enough for good health.
However, one in four people would be more active if advised by a healthcare professional so this presents a unique opportunity for you to support people to be more active.
The UK Chief Medical Officers’ Guidelines recommend each week adults do:
- at least 150 minutes moderate intensity activity, 75 minutes’ vigorous activity, or a mixture of both
- strengthening activities on two days
- reducing extended periods of sitting
Core principles for healthcare professionals
This ‘All Our Health’ physical activity information has been created to help all health professionals:
- understand specific activities and interventions that can prevent physical inactivity
- think about the resources and services available in your area that can help people get active
Taking action
If you’re a front-line health professional:
- speak to your patients about the benefits of physical activity and risks of inactivity, referring them to information or services if necessary
- read our blogs about brief advice, motivational interviewing and health coaching to help you have non-judgemental conversations tailored to individual patients
- find out about the resources and services in your area that can help people get active, such as local referral pathways, including exercise/activity on referral schemes
- read the NHS resource Walking for health
- read our blogs about the type of local services that may be available and how to find them
- familiarise yourself with key physical activity messages and understand where to access trusted advice for your patients – we recommend NHS Choices which has information for adults, older people, children and people with disabilities
- promote physical activity campaigns like Change4Life (information for children) and Better Health (for adults aged 40 to 60)
- offer online activities or health apps such as Better Health’s ACTIVE10 which encourages 10 minutes of brisk walking every day or ‘Couch to 5k’ which helps people take up running
- become a physical activity role model; increasing your own activity levels will improve your own health and make it easier for you to discuss physical activity with other people
If you’re a team leader or manager:
- ensure the teams you manage are aware of physical activity services and interventions in your local area
- promote a team culture where staff know that they should talk to their patients about healthy lifestyles – ‘Making Every Contact Count’ initiatives should include physical activity
- create a culture where all staff understand the benefits of measuring their impact and demonstrating the value of their work
- consider working within your own organisation, or with local businesses, to promote active workplaces
- encourage high-level, executive staff to act as physical activity role models
If you’re a senior or strategic leader:
- work to ensure physical activity is promoted prominently within commissioned healthcare services
- include physical activity in health and wellbeing boards’ Joint Strategic Needs Assessment (JSNA)
- consider the physical activity needs of the local workforce to create a culture change towards a more active workforce
- look at the education and training needs of the workforce, to equip them to deliver high-quality physical activity advice and interventions
- encourage high-level, executive staff to act as physical activity role models
Understanding local needs
The Physical Activity Data Sources document provides information on what can be found in each data source, including geographical areas reported (including national, regional and local authority), demographics of respondents (age, sex, ethnicity, sexuality, socio-economic status, religion, disability) and frequency of updates to the data.
The 2 main sources of national level physical activity data are the Health Survey for England (HSE) and the Active Lives Survey (ALS).
The HSE is used by central government to monitor trends in the national physical activity estimates, with most recent data available from HSE 2016. Data from ALS is used for the Public Health Outcomes Framework and Physical Activity tools to support local monitoring of performance against the government’s Sport Strategy and Chief Medical Officer guidelines, with PHE producing physical activity estimates for each local authority in England.
Measuring impact
As a health professional there are a range of reasons why it makes sense to measure your impact and demonstrate the value of your contribution. This could be about sharing what has worked well in order to benefit your colleagues and local people, or help you with your professional development.
The general practice physical activity questionnaire (GPPAQ) is a simple, validated screening tool to assess adult physical activity and the associated risk of cardiovascular disease and all-cause mortality within primary care.
The Everyday Interactions measuring impact toolkit provides a quick, straightforward and easy way for health care professionals to record and measure their public health impact in a uniform and comparable way.
The physical activity impact pathway is recommended for healthcare professionals to record and measure actions undertaken as part of routine care which impact on physical activity levels.
Further reading, resources and good practice
Advice for patients and the public
- NHS Choices has a range of information and support to help people get and keep fit
- Better Health has information and support to help people stay active
- Active 10 app helps individuals build 10 minutes of brisk walking into their routine
- Couch to 5k helps people take up running
- the Activity Alliance provides advice for disabled people to get active
Professional resources and tools
The UK CMOs’ Start active, stay active report on physical activity provides detail and evidence on the recommended guidelines for physical activity and is supported by a number of infographics showing the guidelines and the benefits, including:
- physical activity for pregnant women infographic and evidence briefing
- physical activity for children and young people (aged 5 to 18)
- physical activity for early years (birth to 5 years old)
- physical activity for disabled adults
OHID has created a longer-length physical activity and health e-learning course to help healthcare professionals to champion physical activity across the life course. The course covers the science, the UK Chief Medical Officers’ physical activity guidelines, the underpinning evidence base and how to incorporate physical activity into daily clinical care. It also includes a resource on motivational interviewing.
NICE guidance and pathways are available to support evidence based practice to promote physical activity.
OHID and BMJ Learning have published 8 modules on physical activity in the treatment of long-term conditions, as well as one on motivational interviewing in brief consultations.
OHID provides free peer training and online resources to healthcare professionals, via the Moving Healthcare Professionals Programme, to empower them with the skills and confidence to have quality conversations with patients about physical activity.
Moving Medicine is a free, online resource for healthcare professionals to promote and support patients with long-term conditions to get more active. Led by the Faculty of Sport and Exercise Medicine UK (FSEM), in partnership with Public Health England and Sport England, the toolkit provides what is needed for a 1-minute, 5-minute and longer conversations with patients.
Macmillan Cancer Support’s Move More is a guide to helping people with cancer to be more active, with ongoing digital support.
Parkrun organises free weekly 5k run events.
Good practice examples
- The ‘Everybody active, every day’ framework to embed physical activity into daily life includes:
- ‘Everybody active, every day: what works, the evidence’ to support a range of interventions
- ‘Identifying what works for local physical inactivity interventions’ summarises the methods and findings of a national call for local practice to increase physical activity
- Everybody active, every day: 5 years on shows how the strategy has been implemented
- ‘Moving at scale – promising practice and practical guidance on evaluation of physical activity programmes in the UK’ is a national review of local case studies by ukactive Research Institute, the National Centre for Sport and Exercise Medicine and PHE
