HPR volume 10 issue 27: news (19 August)
Updated 16 December 2016
1. Epidemiology of infectious syphilis in London
Key facts relating to the surveillance, prevention and control of syphilis in London are presented in PHE’s first Syphilis Epidemiology in London report, produced jointly by the agency’s Field Epidemiology Services and its integrated London Centre/regional office [1].
Based on a detailed analysis of data for 2015, the report finds that:
- 2,811 new cases of syphilis were diagnosed in London-borough residents in 2015, representing a 22% year-on-year increase over 2014
- in 14 London boroughs syphilis incidence increased by more than 100% between 2011 and 2015
- overall London accounts for the majority of syphilis cases in the UK – 56% of the national total – and has an incidence rate over three times the national rate
- the rate of diagnosis of new syphilis cases in London in 2015 was 32.9 cases per 100,000 population, compared with 9.3 cases for the country as a whole (see map below)
- 90% of cases in London were in men who have sex with men
Incidence of infectious syphilis increased in the late 1990s and has remained at elevated levels since. In the late 1990s and early 2000s, significant outbreaks were identified across the country (in Bristol, Peterborough and North Cambridgeshire, Manchester, London, Brighton and Newcastle), and in the East of England and in Yorkshire and Humber between 2012 and 2014. There is evidence of sustained transmission of syphilis continuing among sexually active populations in Manchester and Brighton, as well as in London. But syphilis in London now represents the most significant public health challenge, the new report notes.
The experience of investigation of recent STI outbreaks in MSM by PHE epidemiologists has informed the findings and recommendations made in the report. Investigations indicate, for example, that risk taking behaviours – including condomless sex, higher numbers of sexual partners, sero-adaptive behaviours (ie choosing a partner based on HIV status), chemsex (sex under the influence of recreational drugs), meeting sexual partners through social networking applications – are likely to be the main drivers of sustained transmission in syphilis in London among MSM.
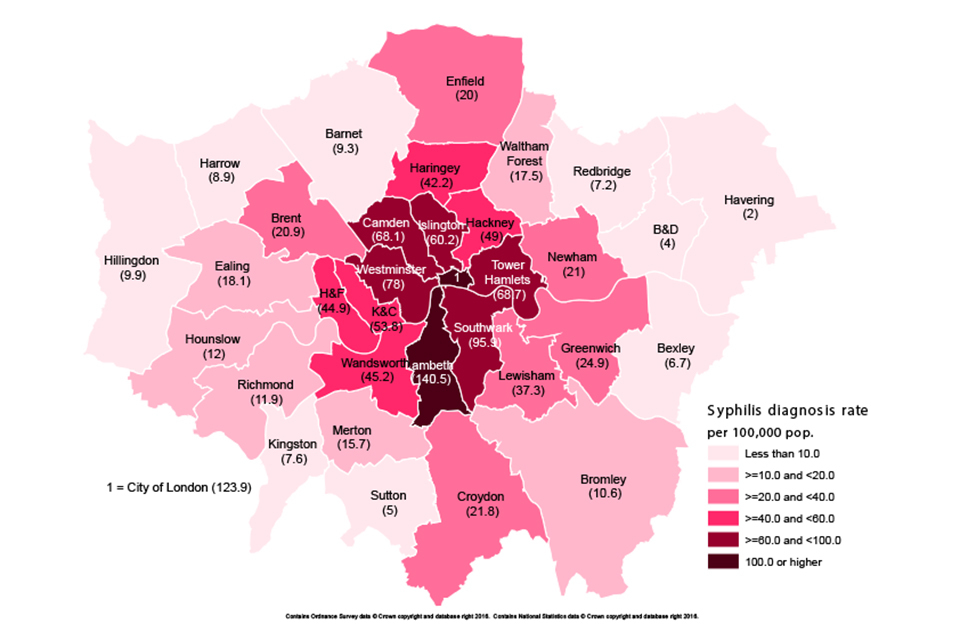
Map of syphilis rates per 100,000 residents by local authority in London (2015)
The report reiterates the principles of outbreak control and management – outlined in longstanding PHE (HPA) [3] and BASHH (British Association for Sexual Health and HIV) [4] guidelines (ie surveillance and intelligence capture; early testing and treatment of cases; robust contact tracing; health promotion to modify sexual risk behaviour, such as condom use; and continued monitoring and evaluation).
However, the authors express concern that the London epidemic has continued despite active campaigns to promote condom provision and use targeted towards MSM through a pan-London HIV prevention programme, and “in an area with a fully functioning sexual health care system where MSM have open access to testing and treatment”. They conclude that, “action needs to be taken by the health system as a whole….. This must bring together preventive action, raising awareness of the disease, improved diagnosis and earlier treatment with intervention at all parts of the care pathway”.
1.1 References
-
PHE (July 2016). Syphilis epidemiology in London: sustained high numbers of cases in men who have sex with men.
-
“PHE publishes report on syphilis”, PHE press release, 17 August.
-
PHE (2010). Guidance for managing STI outbreaks and incidents.
-
Kingston M, French P, Higgins S, McQuillan O, Sukthankar A, Scott C, et al (2016). UK national guidelines on the management of syphilis. Int J STD AIDS 27(6):421-46.
2. Zika virus – epidemiological update
The outbreak of Zika virus, primarily focussed in South and Central America and the Caribbean, continues. As of 18 August 2016, 57 countries, territories and areas have reported active Zika virus transmission in the last three months, including three British Overseas Territories (Anguilla, Turks and Caicos Islands, and the Cayman Islands). Many countries in the Americas are experiencing an expected seasonal decrease in reported cases [1]. However, based on the available evidence, the World Health Organization (WHO) does not consider there to be an overall decline in the outbreak [2].
On 29 July, the Florida Department of Health reported four cases of locally acquired mosquito transmitted Zika virus infection, representing the first autochthonous cases in the United States of America [3]. As of 18 August, a total of 35 cases have been reported. Health authorities in Florida believe active transmission of the Zika virus is restricted to one small area in Miami-Dade County [4]. This development was not unexpected, as Florida (along with many southern US states) has established populations of Aedes aegypti mosquitoes. Further cases in Florida, and other areas, are therefore likely during this transmission season. To date, no locally acquired mosquito transmitted cases of Zika have been reported in Europe.
2.1 Congenital Zika syndrome (CZS)
Cases of CZS have been reported by 17 countries, territories or areas to date. This includes four countries (USA, Slovenia, Spain and Canada) where cases born to mothers with a recent travel history to known affected countries have been reported. Brazilian authorities continue to report the majority of cases of CZS with 1,835 cases as of 13 August 2016 [5]. WHO still considers the Zika virus infection and its associated congenital and other neurological disorders to constitute a public health emergency of international concern (PHEIC).
2.2 UK diagnosed cases
In the UK, as of 17 August 2016, 72 PCR confirmed cases of Zika virus infection have been reported in travellers since 2015 [6]. Zika cases in the UK have travelled to the Caribbean and South America, areas with known intense transmission. More than two-thirds of cases have travelled to the Caribbean; the largest number reported travel to Jamaica (19), followed by Barbados, St Lucia, Grenada, and Trinidad and Tobago – all countries popular with UK travellers including those visiting friends and relatives. Of those that travelled to South America, most have reported travel to Colombia, Brazil and Venezuela.
2.3 Region of travel for Zika cases diagnosed in UK travellers since 2015 (as of 17 August 2016)
| Region of travel | Total |
|---|---|
| Caribbean | 50 |
| South America | 17 |
| Central America | 3 |
| More than one region | 2 |
| TOTAL | 72 |
2.4 Zika specific travel advice
Travel advice for people travelling to areas with Zika virus transmission has recently been updated [7]. Countries, territories or areas with active or past Zika infection are now classified into four risk categorisations (very low, low, moderate or high) based on the current and potential epidemiological situation [8].
An A-to-Z list of all countries, territories and areas that have reported Zika virus transmission since 2007, with their respective risk rating, is available on the PHE Zika virus: country specific risk webpage. This allows for Zika-specific travel advice to be tailored to the individual depending on (a) the Zika virus risk of their countries/territories/areas of travel and (b) whether the individual or their sexual partner is perceived as being at increased risk from complications of Zika virus infection (currently pregnant or planning pregnancy within eight weeks following travel). NaTHNaC’s Country Information Pages have been updated to reflect the Zika risk categories and corresponding advice for travellers and pregnant women [9].
Information and guidance documents on the PHE website are regularly reviewed and revised in light of new evidence. Please see the Zika virus collection for latest updates [10]. Health professionals and travellers should consult the country information pages on NaTHNaC’s Travelhealthpro website for the latest travel health advice for their destination [11].
2.5 References
- Pan American Health Organization, WHO Regional Office for the Americas (11 August 2016). Regional Zika epidemiological update (Americas).
- WHO. Zika virus situation reports.
- Florida Health Department (29 July 2016). Department of Health responds to local Zika cases.
- Florida Department of Health (18 August 2016). Department of Health daily Zika update.
- WHO (18 August 2016). Zika situation report.
- PHE website. Zika virus: epidemiology and cases diagnosed in the UK.
- PHE website. Zika virus: travel advice.
- PHE website. Zika virus (ZIKV): clinical and travel guidance.
- NaTHNaC Travel Health Pro website Country information pages
- PHE website. Zika virus (ZIKV): clinical and travel guidance.
- NaTHNaC Travel Health Pro website.
3. Candida auris in England: an update
Public Health England is continuing to monitor circulation of an emerging fungal pathogen,Candida auris, sporadic cases of which have been identified across the country, since August 2013, by the PHE Reference Mycology Laboratory.
A critical care unit in England has been managing an outbreak of C. auris since April 2015 [1] with 50 patients either colonised or infected to date, of which there have been nine candidaemias in eight patients. The hospital outbreak has been difficult to control, despite enhanced infection control interventions, including regular patient screening, environmental decontamination and ward closure. In addition, 12 patients have had C. auris detected since August 2013 in six further English NHS Trusts, five of whom had a bloodstream infection. Four additional patients have had C. auris detected through private laboratories in England.
C. auris isolates can be misidentified by commercial testing kits and equipment – most commonly as Candida haemulonii, Rhodotorula glutinis or Saccharomyces cerevisiae – so further work is advised if those species are identified, to ensure that they are not C. auris.
It is important that any Candida spp. isolates associated with invasive infections and isolates from superficial sites in patients from high intensity settings and those transferred from an affected hospital (UK or abroad) should be analysed to species level.
As knowledge on the epidemiology and prevalence in the UK is as yet limited, PHE is currently not in a position to make specific recommendations with regards to screening policy. However, C. auris screening could be considered for patients at risk for Candida disease.
Many local microbiology services will not have the facilities to test at this level and will have to refer onwards to their PHE Network Laboratory or to the PHE Mycology Reference Laboratory.
Further recommendations and guidance are available on the PHE website [2].
3.1 References
- “Candida auris identified in England”, HPR 10(21), 1 July 2016.
- PHE (27 June 2016). Guidance for the laboratory investigation, management and infection prevention and control for cases of Candida auris.
