Guidance for breast screening mammographers
Updated 24 July 2025
Applies to England
For most women attending breast screening, the mammographer will be the only health care professional they encounter. The mammographer has a primary role to play in the woman’s experience, satisfaction and continued acceptance of the service.
Mammographers have a role in ensuring women understand the importance of breast awareness in between screening invitations.
The needs of individual women and their circumstances must be recognised to ensure a satisfactory and positive screening experience. High uptake is necessary to help reduce mortality from breast cancer in the screening population.
Mammography staff are responsible for producing images of the highest quality to enable cancer detection rates to be maximised. They are also responsible for providing the best possible care for women attending screening and assessment, to promote wellbeing and to encourage regular attendance.
The term ‘mammographer’ includes:
- registered radiographers, who are regulated by the Health and Care Professions Council
- mammography assistant practitioners
The purpose of these guidelines is to encourage best practice by mammographic staff to achieve the NHS breast screening programe (BSP) objectives and standards.
These guidelines give clear and detailed information on radiographic aspects of breast screening quality assurance:
- providing a framework for audit and for identifying, reporting and resolving problems
- supporting continuous improvement in quality for all radiographic aspects of breast screening service delivery
- promoting the development of a learning culture within breast screening
- promoting best practice, effective training and continuing professional development (CPD)
The guidelines should be used in conjunction with other relevant guidance and regulatory frameworks. These include but are not limited to:
- consolidated standards for the NHS breast screening programme
- routine quality control tests for full-field digital mammography systems
- the Ionising Radiation (Medical Exposure) Regulations (IRMER)
- the data protection act
- the Society and College of Radiographers (SoR) guidance
- the Health and Care Professions Council (HCPC) standards of conduct, performance and ethics
- screening women with breast implants
- surveillance screening of higher risk women
- ageX trial
The guidelines are for:
- all mammographers in the NHS BSP
- radiography line managers and superintendents
- breast screening unit quality control leads
- professional clinical advisors (PCAs) for radiography
- directors of breast screening
- breast screening programme managers
They are also useful for:
- NHS trust managers
- regional screening quality assurance services (SQAS)
- medical physics services
- radiographic support workers
- professional bodies relating to breast screening
- commissioners and screening and immunisation area teams
- training organisations and universities
- public interest groups
- patient advice and liaison services (PALS) or equivalent
- all other screening unit staff
At unit level and individual level, use the guidelines to help inform practice around:
- self-appraisal and reflective practice
- peer review
- the audit of individual performance and to inform appraisal
- the development of personal development plans
- induction and training
- informing organisational development and business management processes
- mammography in the NHS BSP
At regional level, the guidelines should be used by radiographic PCAs to inform:
- the audit of unit mammographic performance
- reporting unit mammographic performance
- giving support, information and advice to mammographers
- the identification of resource issues to inform organisational development and business planning processes
Radiographic PCAs should encourage the use of these guidelines in the everyday working practice of breast screening mammographers.
While the guidelines are designed for the breast screening programme in England, it is recognised that they may be helpful for mammographers working in Northern Ireland, Wales and Scotland. These mammographers should be aware that legislation in their countries may vary from that presented in this document.
The 4-tier structure and related roles
There are currently 4 levels of mammographic practice within the NHS BSP. Each level of practice has specific roles and responsibilities.
Assistant practitioner (AP): main functions
APs work to current scope of practice. They are a supervised workforce under the supervision of a state registered practitioner. This supervision may be either direct or indirect. The education and training of assistant practitioners should support the development of a practice focused, competent individual.
Most APs work in screening, although some may also work in symptomatic services and assessment clinics. As breast care services are re-aligned, there may be the opportunity for APs to expand their scope of practice. This must be on the understanding that they have undertaken the additional education and training necessary for them to fulfil this role. They will continue to work under protocols and the supervision of a radiographer practitioner. The employing authority must be advised of their additional duties and expanded scope of practice.
Radiographic practitioner
Registered radiographers at the practitioner level undertake a broad portfolio of diagnostic examinations in the delivery of care for clinical imaging. The practitioner is an integral member of the clinical imaging team delivering high quality clinical care.
Radiographer practitioners specialising in mammography perform all aspects of screening and assessment mammography. They supervise students, trainee mammographers and APs as required.
Advanced practitioner: main functions
Advanced clinical practice incorporating various clinical competencies is delivered by experienced registered healthcare practitioners. It is a level of practice characterised by a high level of autonomy and complex decision-making. This is underpinned by a master’s level award or equivalent that encompass the 4 pillars of clinical practice, management and leadership, education and research, with demonstration of core and area specific competence.
Advanced practice clinical skills may include:
- mammographic image reading; all mammographic image readers are required to participate in Personal Performance in Mammographic Screening (PERFORMS) and they should attend MDTs regularly
- clinical examination
- breast ultrasound
- interventional procedures
- stereotactic-guided interventional procedures
- health promotion and audit
- team or professional leadership
- practice and service development
- education and training
- research and development
The knowledge, understanding and skills required for this role are stated in the Education and Career Framework for the Radiography Workforce
Consultant practitioner: main functions
The Department of Health (DH) defines a consultant allied health professional (AHP) as an individual who provides clinical leadership within a specialism, bringing strategic direction, innovation and influence through practice, research and education. In radiography, AHP posts were developed at a time of medical consultant shortages. They were not designed as a replacement but to enhance service delivery by:
- providing better outcomes for patients by improving quality and services
- providing a new career opportunity to help retain experienced staff and recognise their clinical contribution
- strengthening professional leadership
Consultant practitioners work autonomously and are involved in clinical decision making about women under their care. Their job description must include all 4 core domains of consultant practice as outlined in the generic guidance for Allied Health Professional Consultant roles.
The role should include the 4 domains of:
- expert clinical practice
- professional leadership and consultancy
- education training and development, and practice and service development
- research and evaluation
There are numerous variations in titles and pay bandings in consultant and advanced practitioner roles. The NHS BSP recommends breast units adhere as closely as possible to the 4-tier structure, nomenclature and guidance when considering staffing levels and skill mix to support service delivery.
Quality assurance framework
Responsibilities for quality assurance (QA)
The screening quality assurance service (SQAS) in the NHS BSP provides a framework for mammographers to:
- understand individual and unit performance relating to quality of mammography and cancer detection
- develop their performance in all areas relating to radiographic aspects of breast screening
- identify educational and development needs
- improve understanding of the breast screening programme and the mammographer’s role in the team
- understand that mammographic QA and quality control (QC) are the responsibility of all mammographers in the service and are monitored closely by radiography managers and other staff with delegated responsibility
Regional QA activity – the PCA for radiography
The PCA for radiography within each region is responsible for leading on mammographic quality assurance. This requires an in-depth knowledge of the practices and processes for delivering excellent patient care. The role helps the SQAS to deliver effective assurance of the mammographic quality of screening services and includes peer review, support and advice.
The primary aspects of the role include:
- providing ongoing, expert regular and ad-hoc advice to the regional QA service
- advising on areas of concern and potential incidents
- audit of mammographic performance at QA visits
- acting as a primary source of advice in their area of expertise to the national portfolio lead and national programme manager
- supporting and facilitating in the development and/or delivery of education and training resources as required
- chairing the regional radiographers professional group which shares best practice and is attended by superintendent radiographers/radiographic managers from each service in the region
- supporting national working to develop the screening QA service
- supporting the revision of guidance relating to mammography
Regional QA activity: multi-disciplinary quality assurance visits
These take place at intervals prescribed by the SQAS and examine all aspects of screening programme performance. They involve monitoring whether services have achieved acceptable standards (as a minimum), identifying variance from these standards and supporting professionals working in the local programme to maintain and improve standards.
Each service has a visit which includes satellite units. Visits include examination of a ‘right results’ process and mammographic reviews of performance. The radiography PCA will review a minimum of 5 clients’ images per mammographer using the national image quality assessment tool (which sets out the criteria for the review). The radiographic questionnaire for QA visits is currently available from the local SQAS team.
Any recommendations concerning mammographic performance will be published in a formal visit report.
The programme specific operating model for quality assurance of breast screening programmes is published on the GOV.UK website.
Local QA activity: the screening service quality control lead
The unit QC lead should:
- oversee monitoring of the mammographic image quality in the unit in conjunction with the radiography manager
- ensure that technical and clinical QC data are shared with the radiography manager and all staff to enable outcomes to be used for continuous improvement and to inform education and development
- monitor technical recall and technical repeat examinations and ensure action plans are developed where performance requires improvement with the radiography manager
- ensure compliance with radiographic QC guidelines, liaise with medical physics colleagues and discuss outcomes of equipment testing, ensuring remedial actions are completed as necessary
- take action when tolerances are exceeded
- understand and implement the process for suspending equipment when necessary
- maintain strong close links with the regional SQAS and the radiography PCA
- have appropriate training and knowledge to undertake the role
- identify their own educational and development needs through appraisal and a development review process, and seek to address such needs
- work within employers’ health and safety framework, including trade union representatives where needed, to ensure that all mammographers in the unit have the best possible working environment conducive to their health and welfare
- recognise, investigate and take appropriate action when system failures are identified and work to resolve them
Clinical and Professional Group (CPG) for Radiography
This is a national group to promote excellence in radiographic practice in the NHS BSP. Its primary aims include:
- giving expert advice to PHE which leads NHS screening programmes on important operational aspects for radiography in relation to best practice in the programme
- advising on aspects of programme delivery which require further consideration by the Advisory Committee for Breast Cancer Screening (ACBCS)
- undertaking work as requested by the ACBCS
- supporting PHE to produce new guidance or revise existing guidance
- analyse data relating to mammography to advise on best practice
- highlight the need for education or training where required
- producing an annual work programme to be agreed with PHE
Membership of the group includes the national programme manager, national SQAS portfolio lead, selected SQAS PCAs and additional senior experts in the field.
Representatives from Scotland, Wales and Northern Ireland may attend and contribute as observers.
Core breast screening standards for mammographers
Core programme standards for mammographers working in the NHS BSP are:
- to achieve optimum image quality
- to limit radiation dose
- to minimise the number of repeat examinations
Excellence in mammographic practice will contribute to the achievement of a range of core programme standards in addition to those listed above. The full list of standards can be found in the screening standards for the NHS breast screening programme.
Achieving optimum image quality with as low a radiation dose as possible requires mammographers, medical physics services, and equipment service personnel to work closely together.
Repeat rates
Mammographers should minimise the number of women undergoing repeat examinations. This includes technical repeats (TPs) and technical recalls (TCs).
Mammographers have a responsibility to undertake regular audit of repeat examinations and should review their own performance against unit and regional performance as well as against national standards. A high rate may identify equipment problems or indicate a training need. In addition to investigating TP and TC rates which do not comply with the national standards, unusually low rates should also be investigated because they can arise from under-reporting or ‘under-calling’ (a tendency to accept sub-standard images).
The NHS BSP good practice guide on collecting, monitoring and reporting repeat examinations should be followed to standardise practice.
The lead radiographer or radiography manager is responsible for ensuring that the collection and monitoring of TC and TP data, including repeat reasons, is undertaken. The information should be carefully analysed and discussed regularly with the regional radiographic PCA.
Health and safety
Mammographers are responsible for ensuring that the screening environment is safe for themselves and for women attending screening. All mammographers must understand and adhere to local health and safety rules and regulations. It is their responsibility to make sure that they are up to date with all relevant policies and procedures, guidance and legislative requirements. These will include:
- local procedures for medical physics checks, including acceptance tests and QC checks
- local procedures for regular checking of all equipment, including mobile units, for wear and tear
- local rules for the use of ionising radiation
- local infection control procedures
- local procedures for dealing with women who become unexpectedly ill during screening
- control of substances hazardous to health (COSHH) regulations
- regulations on electrical safety
- fire regulations
- safe working practices for manual handling
- procedures for reporting health and safety issues or causes for concern (incident reporting systems)
- being up to date with employer’s requirements for mandatory training
This is not an exhaustive list and there may be additional employer protocols and policies.
Mammographic Practice
Informed choice in breast screening
The breast screening programme invitation leaflet and breast screening easy guide support women in making an informed choice about whether to attend for breast screening. Current thinking and legal and professional frameworks in the area of informed choice and consent are subject to change, so mammographers have a professional responsibility to keep their knowledge up to date in this as in all areas of their practice (HCPC standards).
Informed consent to mammography
If a woman attends for breast screening, this implies consent. A woman may withdraw this at any time during the examination. If the woman expresses any misgivings or uncertainties about participating in screening, the mammographer should do everything possible to sensitively address these concerns at the time. Assistant practitioners should refer to their supervising registered radiographer whenever they are unable to answer questions fully or are asked about issues beyond their scope of practice. It may not always be possible to resolve all concerns in the context of a short appointment. Postponement of screening to allow the woman time to consider whether to attend may occasionally be appropriate.
An explanation of the mammographic procedure before it is performed must include the use and implications of radiation and compression. For consent to be valid, it must be given voluntarily (without pressure from others), as part of an informed choice, and the woman must have the capacity to consent. Capacity means they can understand and use information about the procedure, including benefits and risks. It is the radiographer’s professional judgement to decide if consent has been given prior to, and maintained throughout, the examination. If consent is withdrawn at any stage, the examination must be stopped and cessation of the examination documented.
Assistant practitioners and consent
Assistant practitioners who are trained via an accredited or approved academic programme and are competency-assessed may take consent to mammography as one of the responsibilities delegated to them by registered radiographers. However, this is limited to women who are co-operative and able to communicate their consent. If consent is in doubt, the supervising registered radiographer must be consulted.
Information needs for women being screened
To facilitate both informed choice in screening and informed consent to mammographic examinations, mammographers must to be able to provide information about:
- the benefits and harms of screening
- any research trials on screening women
- where to access further information about breast screening
- the screening test, including radiation risk and compression
- the limitations of mammography in the presence of breast implants
- the implications of being unable to achieve adequate positioning for a full examination (for example in women with limited mobility)
- the results process
- self-referral for screening for women aged 71 or over
- breast awareness and reporting any concerns to a GP
Confidentiality
Mammographers must ensure that:
- privacy and confidentiality are maintained in accordance with employer protocols
- local protocols for maintaining the security of patient identifiable data should be followed
- mammographers follow PHE’s policy on data collection and confidentiality and disclosure of information
- mammographers undertake information governance training according to local employer arrangements
Mammography equipment and fault reporting
Screening services and the National Coordinating Centre for the Physics of Mammography (NCCPM)
The NCCPM has oversight of the performance of all mammography equipment in the NHS BSP.
The NCCPM:
- maintains a database of equipment used by the NHS BSP
- monitors all equipment faults in the NHS BSP
- meets with manufacturers and servicing agents to discuss with them problems with equipment nationally
- works collaboratively with NHS BSP colleagues to evaluate new equipment
A review of NHS BSP equipment and equipment faults is prepared every 6 months and published internally by the NHS BSP and is distributed via SQAS to all services.
Responsibilities of services to report to the NCCPM
Units must report all equipment faults to the NCCPM using the prescribed format within required timescales. Any actual or potential serious equipment fault should be reported immediately through their local employer reporting system. The Medicines and Healthcare Products Regulatory Agency (MRHA), SQAS, NCCPM and national breast screening programme manager should also be informed as soon as possible.
Performing the mammogram
Introduction
The female breast is composed of soft tissues with inherently low radiographic contrast and little variation in attenuation coefficients. A highly sensitive and sophisticated form of diagnostic radiography is therefore required to demonstrate abnormal pathology reliably and consistently. Mammography has been described as “the science of imaging, and the art of positioning”.
Successful mammography is dependent on the performance of the equipment, the expertise of the mammographer and the co-operation of the woman. The skills of the mammographer and various factors associated with the woman undergoing the examination affect the quality of the mammogram. These include:
- the composition and size of the breast
- the woman’s physical and psychological attributes
A good quality mammogram shows all the breast tissue with high levels of detail and clarity. In addition to obtaining valid informed consent, mammographers must seek to ensure that:
- the woman’s identity is confirmed in line with local protocols by an active 3-point procedure such as full name, date of birth and first line of the address (IRMER guidance)
- where barriers to informed consent or establishing identity exist (for example, if English is not the woman’s first language) appropriate support is obtained according to local service provision
- all women feel confident that they have the ability to stop the procedure at any point
- if there is difficulty establishing informed consent, and/or any withdrawal of consent, this is clearly documented
- women with breast implants are given an explanation of the limitations of mammography for them (a breast implants and breast screening national leaflet is available)
- all women receive an explanation about receiving results and on breast awareness between screening appointments
- all women are informed about the importance of reporting any changes noticed between screening episodes to their GP
- any significant signs and symptoms reported by the woman are recorded and will be uploaded onto the national breast IT system
- the woman is informed about the potential of recall for further tests in assessment
- signs and symptoms observed by the mammographer should not be discussed with the woman but details should be uploaded onto the IT national database
- following the final screening appointment the woman is informed that she can self-refer for screening in 3 years’ time if she wants to (by contacting her local breast screening unit direct)
Partial mammography
Where it is not possible to perform a complete examination and (in the mammographer’s professional judgement) a complete examination would not be achievable if repeated, the mammographer should explain this to the woman and provide the NHS information leaflet on incomplete mammography. Partial mammography should be recorded on the the National Breast Screening System (NBSS) so that a partial results letter can be generated.
If the operator can screen at least half of 1 breast, in any view, the examination can be clinically justified. A mammogram must not be categorised as ‘partial mammogram’ if additional, repeat or recall views would complete the mammogram. Assistant practitioners will need to involve a supervising registered radiographer in these situations.
Subcutaneous mastectomy
If a woman has had a subcutaneous mastectomy with implants, it is not necessary to perform mammography on that breast as all breast tissue should have been removed. The other breast should be screened as usual.
Avoiding musculoskeletal strain when performing mammography
Work related repetitive strain injury (RSI) and musculoskeletal disorders (MSKD) may encompass a wide range of inflammatory and degenerative diseases and disorders and are a major occupational hazard for mammographers. Due to the repetitive nature of breast imaging within the NHS BSP and the fact that undertaking a mammogram is a physical activity, great care should be taken to support the wellbeing of mammography staff. This is a shared responsibility of the individual and the employer. Employers must ensure comprehensive risk assessments are performed of the workload, equipment and ergonomic requirements of the mammographic procedures.
Consideration should be given to the rotation between screening and assessment clinics and include additional tasks where appropriate (for example film reading, health and safety or QA). Mammographers should be involved in risk assessments and must comply with training requirements or other control measures.
In deciding which equipment to use, consideration should be given to the ergonomic suitability of the systems. Mammography staff should be trained on and familiar with using the equipment effectively and ensure that high image quality is obtained without compromising their own health.
Clinical image quality and image quality assessment
When evaluating both the medio-lateral oblique (MLO) and cranio-caudal (CC) images, the following criteria are used to judge the quality of the images.
Image annotations
The following annotations should be clearly shown and must be correct:
- woman’s identification details
- anatomical markers (left or right)
- positional markers (MLO, CC, and so on)
- mammographer identification
- date and time of examination
- organisation identifier
In addition, sufficient exposure information must be recorded to enable clinical radiation dose calculations to be performed. The required information is normally captured in the ‘digital imaging and communication in medicine’ (DICOM) header of each image. The manufacturers’ dose calculations presented in the header and on the image are not currently suitable for clinical dose audit.
Correct exposure
Overexposure is difficult to detect visually in digital imaging, where image appearance is heavily influenced by system technological factors. This heightens the importance of radiation dose monitoring through clinical audit.
Under-exposure leads to ‘noisy’ or grainy images and this should be recognised when assessing image quality.
Image contrast
Image contrast varies according to specific manufacturers’ digital processing algorithms. It is influenced by beam quality, so the mammographer must pay attention to this even in the context of sophisticated automatic exposure control (AEC) systems. While brightness and contrast preferences vary, a team approach is required via QC testing to optimise these to maximise cancer detection. Images should be checked for adequate greyscale range to maximise visibility of anatomical structures.
Where problems with image noise, brightness or contrast are detected, attention should be paid to effective compression, as well as correct operation of the AEC and correct positioning of the breast over the area of the detector used by the system to set exposure parameters.
Compression and image sharpness
Compression is important in minimising radiation dose, movement blur, geometric unsharpness and overlapping tissue shadows. The breast should be lifted and the tissue spread while compression is applied to enable optimal demonstration on the mammogram. The compression should be applied slowly and gently to ensure that the breast is held firmly in position, and continuing client consent must be checked during the procedure.
Images should be checked for absence of movement blur and for evidence of effective compression. Effective compression is evidenced by features such as separated and well demarcated ‘Cooper’s Ligaments’ and evenly spread glandular tissue.
Compression force levels will depend on the compressibility of the breast and on levels of breast tenderness and acceptance of compression by the woman. Effective compression depends not only on the exertion of sufficient force but on the quality of positioning. Poor positioning may also lead to higher than necessary compression force being used to achieve tissue immobilisation.
Skin folds
Images should be checked for skin creases and folds and whether these pose significant risk to accurate image interpretation. Optimal positioning and smoothing of the skin will help avoid the inclusion of skin folds in the imaging field.
Other artefacts
Images should be checked for any artefacts which may cause difficulties for image interpretation. These may include:
- the woman’s hair, chin, shoulder or other breast
- jewellery
- deodorant or other cosmetic residues
- artefacts arising from the imaging system’s hardware or software
Nipple in profile
This is important in order to demonstrate the retro-areolar area of the breast clearly on the mammograms. The nipple should normally be demonstrated in profile on at least one of the views of each breast. If it is judged that image interpretation will be difficult even with unilateral failure to profile the nipple, an additional image should be acquired.
Symmetry
Although images can be manipulated to be symmetrically aligned on the reporting station (to aid accurate image interpretation), the images should match as mirror images prior to manipulation. This will demonstrate correct positioning and to ensure that the AEC is aligned to the same part of each breast.
Specific criteria for MLO images
The specific criteria for assessing MLO images (see figure 1) are:
- correct patient ID and markers
- appropriate exposure
- adequate compression to hold breast firmly – no movement
- image sharp
- no artefacts obscuring image
- no obscuring skin folds
- nipple in profile (should normally be demonstrated in at least one view)
- pectoral muscle to nipple level or posterior nipple line (PNL)
- pectoral muscle at appropriate angle
- inframammary angle shown clearly
- symmetrical images
- whole breast imaged
Pectoral muscle to nipple level or PNL
The inferior extent of the pectoral muscle shadow should reach nipple level whenever possible, to ensure that the posterior aspect of the breast is fully included on the image. However, extensive anatomical variations between women mean that this is not always possible. Compliance with a less stringent standard whereby the pectoral muscle meets the PNL should be considered sufficient as long as other indicators of whole breast inclusion are present. The PNL is ‘drawn’ at 90 degrees to the anterior aspect of the pectoral muscle shadow, from the nipple to the anterior border of the pectoral muscle or, if the pectoral length criterion is not met, it will meet the back of the image without traversing the pectoral muscle.
Pectoral muscle at appropriate angle
The pectoral muscle should be at an appropriate angle to maximise inclusion of the axillary tail of the breast tissue without impeding effective compression of the breast disc. This angle varies according to the physical constitution of the individual.
Inframammary angle shown clearly
The inframammary angle should be clearly shown without overlapping chest wall tissue. This indicates that the breast has been lifted and that the postero-inferior part of the breast has been imaged.

An exmaple of an mediolateral oblique (MLO) image
Specific criteria for CC images
The specific criteria for assessing CC images (see figure 2) are:
- correct patient ID and markers
- appropriate exposure
- adequate compression to hold breast firmly – no movement
- image sharp
- no artefacts obscuring image
- no obscuring skin folds
- nipple in profile (should normally be demonstrated in at least one view)
- medial border demonstrated
- back of breast clearly shown with some medial, central and lateral
- some axillary tail shown
- whole breast imaged
- absence of artefacts covering the image
- symmetrical images
The CC view should show as much of the breast as possible. A correctly performed CC view will show virtually all of the breast except the extreme axillary tail. The breast should be presented as straight with no lateral or medial rotation and no ‘rolling’ to one side or the other.
The CC view should demonstrate:
- the medial border of the breast – ideally, although not always possible, the skin will be shown curving between the breast and the chest wall to evidence inclusion of the posterior extent of the medial breast tissue
- some of the axillary tail of the breast – this is evidenced by a tail-shaped lateral aspect, ideally of the glandular tissue as well as the skin surface
- pectoral muscle shadow shown on the posterior edge of the breast on some CC views depending on anatomical characteristics – if shown, this should be central and may only be achievable
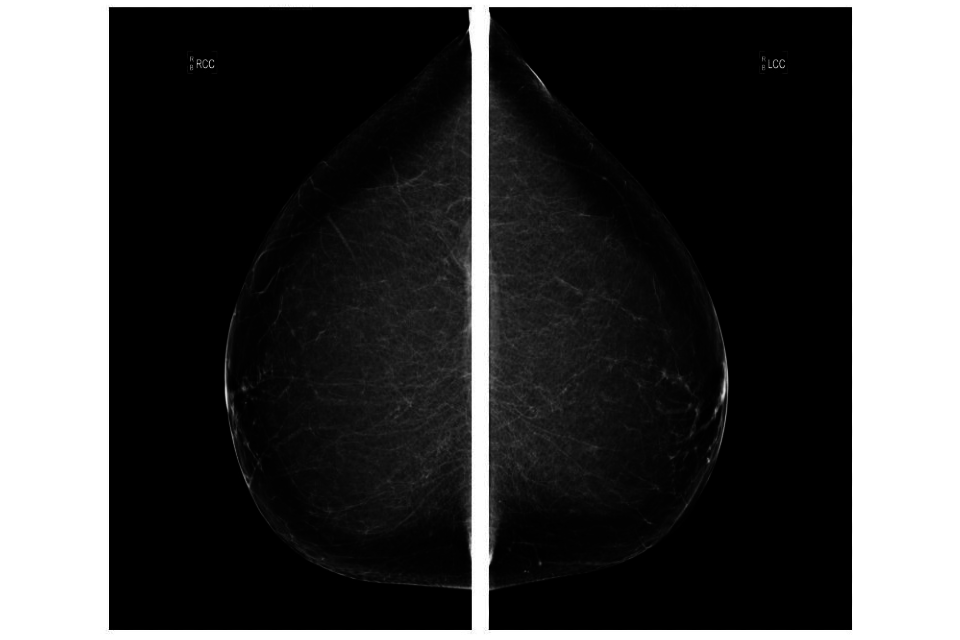
An example of a cranio-caudal (CC) image
Inadequate images
MLO or CC images are judged to be inadequate for radiological interpretation for one or more of the following reasons if:
- part of the breast is not imaged
- the image is blurred or unsharp to a degree likely to hinder accurate image interpretation
- the nipple in profile in neither view and/or the retro-areolar area is insufficiently clear to enable accurate image interpretation
- the exposure is incorrect such that noise or poor contrast or brightness is likely to impede accurate image interpretation
- artefacts obscure breast tissue
- skin folds obscure breast tissue
- annotation is inadequate or incorrect (in this case repeats are only required if it is impossible to verify the identity the individual/projection)
Monitoring clinical image quality
Regular monitoring and audit of mammographic technique is essential. The mammographer must carry out image assessment against the criteria laid down for the MLO and CC images.
The NHS BSP mammographic image assessment tool is mandatory for use within the programme for image review at individual, peer and department levels. Image review for individual staff is also reviewed at QA visits. The ‘perfect/good/moderate/inadequate’ (PGMI) or ‘excellent/acceptable/repeat’ (EAR) methods to examine image quality are no longer acceptable.
An audit of a minimum of 20 mammograms every 2 months should be undertaken at service level.
Underperformance in clinical image quality
Where underperformance of an individual is identified, the radiography manager should:
- identify and discuss possible solutions
- initiate informal discussions with the individual concerned to identify any possible underlying causes, such as working practices or personal or health problems
- set out and agree an action plan with a specified time scale, which may include additional training, mentoring, review of working practices and/or advice from the occupational health department on health related issues
- document, review and feedback against an agreed remedial action plan with the member of staff within the specified timescale
Where performance does not improve, further advice may be sought from the SQAS team and local service improvement policies should be consulted and followed.
Specific client groups
Clinical signs and symptoms
The mammographer should note if an individual presents with:
- a recent lump in the breast (a long-standing lump which has been previously investigated and diagnosed need not be recalled unless the client reports a change in the lump)
- distortion or change in the shape of the breast (a mass may be palpable)
- nipple eczema (this includes recent eczema that has just healed)
- recent nipple inversion (this may be caused by cancer and requires assessment; it is important that mammographers are aware of the various nipple appearances, skin tethering or dimpling, a mass may be palpable)
- nipple discharge (unilateral multiple duct discharge, whether bloody or not, is highly unlikely to be related to malignancy – bilateral multiple duct discharge is very unlikely to be of significance)
The mammographer should note down on the clinical sheet and the breast screening computer system any significant or relevant symptoms which are reported by a woman. If the mammographer observes a clinical sign which is not mentioned by the woman, this should also be recorded on the computer system.
It is important to clearly identify whether the observation has been raised by the woman or the mammographer. The mammographer is not required to undertake a clinical examination of the breasts, only to record reported or observed significant signs or symptoms. Where the mammographer only has observed a clinical sign, this information should not be shared with the woman being screened during the screening examination. At this stage, the observation has not been clinically or mammographically confirmed.
Women who have identified a symptom should be informed that they may receive a normal screening result. Mammographers should advise that if they notice further change in their symptom and become more worried following screening, they should seek advice from their GP.
Application of the equality act in breast screening
Under the Equality Act, certain duties are expected of all public organisations. These are:
- to eliminate unlawful discrimination, harassment, victimisation and any other conduct prohibited by the Act
- to advance equality of opportunity between people who share a protected characteristic and people who do not share it
- to foster good relations between people who share a protected characteristic and people who do not share it
Having ‘due regard’ means consciously thinking about these duties as part of the decision-making process. This means that consideration of equality issues must influence the decisions reached by public bodies. These include how they act as employers, how they develop, evaluate and review policy, how they design, deliver and evaluate services, and how they commission and procure from others.
Mammographers must ensure they:
- remove or minimise disadvantages suffered by people due to their protected characteristics
- meet the needs of people with protected characteristics
- encourage people with protected characteristics to participate in public life or in other activities where their participation is low
Fostering good relations involves tackling prejudice and promoting understanding between people who share a protected characteristic and others. Complying with the Equality Act may involve supporting some people more than others, as far as this is allowed by discrimination law.
Screening appointments for clients with additional needs
Women with physical disabilities
Mammographers should be aware of and respect women with additional needs such as physical disabilities. Appropriate facilities should be available to ensure that their visit to the breast screening unit is as acceptable as possible. This usually means offering an appointment at a static unit that allows easier access for women with physical disabilities, more space for carers or other supporters who may accompany the woman.
Every effort should be made to image women with a physical disability and to produce images of diagnostic quality. However, this may not always be possible for women who have limited mobility in their upper bodies or who are unable to support their upper bodies unaided.
Women with learning disabilities
Women with learning disabilities have the same entitlement as other women to breast screening. The NHS BSP has a responsibility to ensure that women with a learning disability:
- have access to breast screening easy read information to enable them to make their own decision about whether to attend for breast screening
- know what to expect when they attend for screening
- understand the possible consequences of breast screening and the need to be breast aware
Women with English as a second language
Women from differing cultural backgrounds and for whom English is not a first language may have support from local link workers or advocates within the employing provider. This is preferable to using family members where possible. Mammographers should be aware of what support is available locally for their clients should it be needed.
Gender reassignment clients
Individuals who are undergoing female to male gender reassignment will continue to be invited for breast screening so long as they are registered as a woman. The exceptions are if they ask to be ceased from the programme or have had a bilateral mastectomy.
Individuals who are undergoing male to female gender reassignment may be screened by asking their GP to request a screening appointment on their behalf. Individuals who are registered with a gender of indeterminate or female are included in screening batch lists and will be sent a screening invitation unless they ask to be ceased from the programme. Information on NHS population screening for transgender and non-binary people is available.
Imaging with breast implants
Guidance on screening women with breast implants is available. The Eklund technique must be used and should only be undertaken by a registered mammography practitioner. Training and information can be accessed via the DVD for imaging the augmented breast which has been provided by the NHS BSP to all breast screening services.
Screening women with implanted medical devices
The following examinations should only be undertaken by a HCPC-registered radiography practitioner.
Pacemakers
Pacemakers are not affected by the x-rays used for mammography. If the pacemaker is in the pectoral region (some are abdominal), the radiographer should adjust the x-ray equipment to make the woman as comfortable as possible and avoid pressure on the pacemaker or wires. The radiographer should never attempt to move or manipulate the pacemaker. Care must be taken not to compress the pacemaker while taking the mammogram. Depending on the position of the pacemaker, it may be difficult to image the breast adequately. Sometimes only a partial mammogram may be obtained. This should be explained to the client and the appropriate results letter sent.
Partial mammography should not be assumed for people with pacemakers. In many cases radiographers will achieve a high diagnostic image regardless of the pacemaker placement.

A diagram of a chest with a pacemaker, with the pacemaker pulse generator, lead in right atrium and lead in right ventricle all labelled.
Women with pacemakers may be advised to attend a static site rather than a mobile unit to enable more time to be allocated for the examination.
If ultrasound is used for women recalled for assessment, then care must be taken not to place the ultrasound probe over the pacemaker implant site. The energy from the probe may adversely affect the pacemaker operation.
Magnetic resonance imaging (MRI) is contraindicated for women with pacemakers unless there is clear evidence that the pacemaker is MRI compatible.
Other implanted medical devices should be dealt with in a similar manner.
Hickman (central) lines
A Hickman line is a tube that goes into the chest and directly into one of the major blood vessels. The end of a Hickman line hangs out of the chest and is usually sealed off with a cap. It is inserted to enable chemotherapy to be administered. Once the treatment is completed the line is removed.

A diagram of a chest with a Hickman line, with the heart, collar bone, connection for drips or syringes and the point where the central line enters the body all labelled.
If a woman attends for screening and has a Hickman line, mammography can be undertaken but care should be taken not to dislodge the line. It is common to see tunnelled lines with a subcutaneous port.
It is appropriate to discuss the risks of mammography with the woman and rebook the screening appointment when the line has been removed.
Pregnancy and lactation
There is no significant radiation dose to the foetus from mammography from a radiation protection point of view and there is no requirement to enquire about pregnancy before imaging. Screening should be suspended until 3 months after lactation stops. This is regulated by IRMER guidance.
Staffing, training and continuing professional development
Staffing levels
It is important that appropriate staffing levels are maintained to ensure that the quality of the service is not compromised. The minimum screening examination for women attending the NHS BSP is 2 views at all screens, and 6-minute appointments are acceptable for most routine screening of women up to their 71st birthday depending on uptake.
Screening services should specify the number of mammographers needed, and should take account of the local configuration of services, the local skill mix and local employer risk assessments. Consideration should be given to ensure there is rotation of staff between screening and assessment clinics and other duties to avoid working consecutive days in screening to avoid MSKD. This is not always possible due to staffing levels and combination of staffing groups.
To maintain clinical competence, mammographers should work a minimum of 2 days per week in the screening programme.
Table 1 (below) provides a guide to staffing levels for delivery of a screening service. Staffing levels are given as whole time equivalent (WTE) per 10,000 eligible women and are for mammography screening and assessment clinics only.
| Level of uptake (%) | Suggested staffing (WTE per 10,000 eligible women) |
|---|---|
| Up to 75 | 1.3 |
| 76 to 85 | 1.5 |
| 86 to 90 | 1.6 |
These staffing levels should allow for:
- rest breaks
- rotation through screening and assessment clinics
- participation in CPD activities
- participation in QC and QA activities including audit and review procedures
- cover for sickness and holiday absence
- attendance at multidisciplinary meetings
- participation in audit, service evaluation and research projects
- participation in QA roles
- link roles (such as infection control link, special needs link, manual handling link)
- mandatory training
- parenting leave
- supervision and mentoring sessions
The staffing levels are for mammographers required within screening and assessment clinics only. Symptomatic mammography, family history and symptomatic ‘fast track’ clinics are funded separately from screening and should not be included in the calculation of staffing levels for screening service delivery. Any other advanced practice, QA or managerial posts will require additional staff to undertake these roles. Where staff undertake additional roles and responsibilities, protected time should be allocated to ensure this is achievable to a high standard and to maintain service delivery.
Performance and development review
Regular review of professional performance is essential to ensure that high quality imaging is both achieved and maintained for each individual member of staff. The mammographers in the breast screening programme should receive regular feedback on their performance. This is achieved by participation in formal appraisal and performance review schemes, through informal discussions within the breast screening team and by peer review. Regular peer review of clinical image quality should be conducted in order to offer support and encouragement to colleagues to maintain high standards of mammography.
NHS BSP training programmes
Assistant practitioners
Assistant practitioners should be trained through an accredited higher education route such as a foundation degree or other suitable provision that has been approved by the SoR. This is to ensure they maintain standards of practice and perform CPD. All training undertaken in mammography requires participants to meet the National Occupational Standards for mammography.
Radiographer practitioners
Registered radiographers wanting to specialise in mammography and work within the NHS BSP must successfully complete a postgraduate course in mammography. Courses are run by national training centres in collaboration with universities. All courses are accredited and validated by an external body.
In-house training is not acceptable as an alternative to an accredited or approved course. Training will ensure that mammographers are technically expert and well informed to respond to the individual needs of the woman and ensure quality service delivery.
Advanced practitioner
To train in advanced practice, qualified radiographer practitioners must undertake additional post graduate qualifications at level 7 (master’s level). The choice of module will reflect the clinical skills required by the service. These courses are run by the national training centres and are supported by colleagues internally at their service until competency in the skill is proven.
Consultant practitioners
Advanced practitioners who want to become consultant practitioners must have a full master’s degree (MSc or MA) or be working towards the qualification. The SoR guidance supports development to doctorate level education.
IRMER training of practitioners and operators
Professional training will ensure that topics specified in IRMER guidance are covered for mammographers working in the NHS BSP (see Summary of IRMER responsibilities).
All operators must demonstrate competency in the use of mammographic equipment.
Employers are expected to ensure that relevant staff have continuing education and training in new techniques and radiation protection as appropriate.
Records of training must be maintained by the employer and be available for inspection.
Continuing professional development
In order to remain registered with the HCPC radiographers must maintain a continuous, up-to-date and accurate record of their CPD activities. They must be able to demonstrate that their CPD contributes to the quality of practice and service delivery. HCPC registered radiographers must present a written profile explaining how they meet the HCPC standards for CPD (if requested from the HCPC).
SoR guidance defines continuing professional development (CPD) for all mammographers.
To achieve and maintain accreditation with the SoR, assistant practitioners, advanced practitioners, consultant practitioners and practice educators must record and submit their CPD to the college.
Mammographers should support and encourage the development and education of students and other learners within their environment.
Extended roles and skill mix
Radiographers who extend their roles must be aware that they are legally responsible for their actions. Accountability means being answerable for decisions about work and being professionally responsible for the standard of practice.
Tasks must be delegated appropriately by the relevant medical practitioner and the employer must officially approve any role extension via the appropriate clinical governance process or at a minuted board level meeting.
The role extension must be clearly reflected in the current job description. Appropriate delegation of tasks means that the person to whom the task is delegated must be:
- aware of their responsibilities and has a clear job description identifying the extended role and responsibilities
- working within clear protocols and guidelines
- educated, trained and assessed as competent via an accredited/approved route
- supervised and mentored appropriately
- carrying out regular audits of their own work
- working to the agreed clinical standards
- taking responsibility for their actions
Practitioners working at all levels must work within their recognised scope of practice. Failure to comply may challenge the vicarious liability accepted by the organisation, and the individual’s own professional indemnity insurance covering their working practices.
Summary of IRMER responsibilities
Employer’s responsibilities
The employer is the trust or service provider. They should:
- ensure written procedures are in place and that staff follow them, including procedures covering patient identification, QA programme, assessment of patient dose, diagnostic reference levels and evaluating exposures (reporting)
- formally entitle the referrers and IRMER practitioners to act in these roles
- ensure that IRMER practitioners and operators are appropriately trained
Referrers and IRMER practitioners must be registered healthcare professionals and details must be written into an employer’s procedures.
Referrer’s responsibilities
The referrer is:
- the director of screening or lead radiologist
- the second reader of screening mammogram (or third reader if there is arbitration)
The referrer will:
- invite eligible women for screening
- recall women for assessment where appropriate
A radiographer may act as referrer if a woman attends for screening without a letter, provided local referral criteria are met and details must be written into an employer’s procedures.
IRMER practitioner’s responsibilities
An IRMER practitioner is:
- a consultant radiologist, breast physician or radiographer
- staff listed above, and operators following guidelines
The IRMER practitioner will:
- justify medical exposures by considering potential diagnostic net benefit (to individuals or society), any individual detriment, and any alternative techniques involving less or no radiation
- authorise exposures (by a signature), that is, confirm that they are justified
- together with the operator ensure that radiation dose is as low as reasonably practicable
For assessment, the IRMER practitioner is the lead clinician of the assessment clinic.
Operators’ responsibilities
Operators are:
- radiographers and assistant practitioners with approved training
- radiographers, assistant practitioners, picture archiving and communication system (PACS) managers
- radiologists, breast clinicians and radiographers trained to read screening mammograms
- medical physics staff (testing)
- radiographers and assistant practitioners (routine QC)
Operators:
- carry out practical aspects of exposures, including optimising exposures (ensuring doses are as low as reasonably practicable, with acceptable image quality)
- select exposure parameters, position clients and take exposures
- store images or send to PACS
- read and report mammograms
- test X-ray systems
