Shaping future support: the health and disability green paper
Updated 15 March 2023
Foreword
My priority as Minister for Disabled People is to make sure that disabled people and people with health conditions can lead the most independent lives possible and reach their full potential. As this Government’s 2019 manifesto set out, we must empower and support disabled people and be an ally. The benefits system is one important lever we have to achieve this.
Shaping Future Support: The Health and Disability Green Paper asks for your views on how the Government can help people to live more independently, including support to start, stay and succeed in work and ways we can improve the experience people have of the benefits system.
The experiences of disabled people and people with health conditions have shaped the ideas, proposals and questions in this Green Paper, following a significant programme of more than 40 events where people have shared with us their views on the benefits system and their priorities for change. I’d like to thank everyone who has contributed to these discussions for sharing your knowledge, experiences and enthusiasm.
We have heard that some people find it difficult to interact with the benefits system. They can feel afraid to access benefits and can find health assessments a difficult, long and challenging process. Shaping Future Support: The Health and Disability Green Paper sets out ways we could make our services easier to access, make our processes simpler and help build people’s trust.
We have already stopped reassessments for people with the most severe conditions that are unlikely to change. We propose ways to further reduce the number of unnecessary assessments, while continuing to ensure support is properly targeted. Alongside this, we propose ways of offering greater flexibility and simplicity in the way that assessments are delivered; including improving the evidence we use to make decisions from health assessments, and learn the lessons of coronavirus where we introduced telephone and video assessments
For people who need extra help to navigate the benefits system, we want to strengthen the role of advocacy so that they can get the right level of support and information first time. Where advocacy support is already available from other sources, we want to look at how we can make sure everybody who needs it has access to the same level of service.
The majority of people are satisfied with the assessment process, but for those who do want to appeal a decision, we must ensure this process is as easy and efficient as possible. That is why Shaping Future Support: The Health and Disability Green Paper explores further ways to improve the decision making and appeals process.
And we plan to make it quicker, simpler and easier for people approaching the end of their lives to claim benefits by changing the Special Rules for Terminal Illness. This change follows an evaluation where we heard the views of people nearing the end of their lives, their families and friends, the organisations supporting them and the healthcare professionals involved in their care. This will mirror the current definition of end of life used across the NHS and we will seek to raise awareness of this vital support.
I am proud that since 2013 we have witnessed record levels of disability employment, and significant progress has been made on our commitment for an additional 1 million more disabled people in work by 2027. Disabled people and people with health conditions are benefiting from intensive employment support through our Plan for Jobs, which builds on the more active support we have introduced through Universal Credit and our existing employment programmes. But there is still more we can do. Disabled people rightly want the same work opportunities that everyone else has access to. To meet that aspiration, we must make further positive changes, which is why this Green Paper explores how we could go further to help reduce the challenges disabled people can still face in starting, staying and succeeding in employment.
Shaping Future Support: The Health and Disability Green Paper represents an important step for improving the benefits system, increasing opportunities for employment and helping more people to lead independent lives. It is part of a wider package of support for disabled people that includes the National Disability Strategy which, for the first time, represents focus and collaboration across Government to set out a wide-ranging portfolio of practical changes we can take to help people in every aspect of daily life. Our Health Is Everyone’s Business consultation response also looks at how employers can support people at work.
I hope you will take the opportunity to have your say on all our proposals by responding to the consultation questions in Shaping Future Support: The Health and Disability Green Paper.
Justin Tomlinson
Minister for Disabled People
Executive Summary
1. The Government has ambitious plans to support disabled people and people with health conditions to achieve their full potential and live better for longer. This Green Paper, the National Disability Strategy and the Health is Everyone’s Business consultation response each form part of our holistic approach to supporting disabled people and people with health conditions to live independent lives and start, stay and succeed in employment.
2. The National Strategy calls for action across Government and wider society. This will look at how to address broader issues that can limit opportunities for disabled people.
3. Our response to the Health is Everyone’s Business consultation is being published with the Department of Health and Social Care. This will set about improving the support provided to employers and employees, to reduce the number of people we see leaving employment because of a disability or health condition.
4. Alongside this work, this Green Paper consults on the following aspects of our support for disabled people and people with health conditions:
- How well our services work for people, and what more we can do to make improvements and build trust.
- How effectively we are supporting people to start, stay and succeed in employment. We recognise that, where people are able to work, appropriate employment has a vital role to play in supporting good mental and physical health.
- How successful the changes we have made to the benefits system since 2010 have been. We consider whether we need to re-think any aspect of these changes or go further. We want to explore whether our current system encourages and supports people in the best way.
5. Throughout this Green Paper, we are guided by three priorities. These are:
- Enabling independent living;
- Improving employment outcomes; and
- Improving the experience of people using our services.
6. This Green Paper has been informed by the experiences of disabled people and people with health conditions who use our services. We have talked with hundreds of people and organisations to ensure that we know what is and is not working. This consultation focuses on those areas that we may need to change.
7. Alongside this, we have analysed existing data and evidence as well as carrying out new research. This has provided us with a detailed understanding of what is happening now. This evidence is shared throughout this Green Paper. It is available in more detail in the supporting data pack and in our published research.
8. We know that we can make more progress. We have already delivered changes to our services and support in the last ten years that have made a real difference. For example, we have delivered more employment support through Universal Credit (UC) and new employment programmes. By the end of 2019, the number and rate of disabled people in employment was the highest it has been since comparable records began in 2013[footnote 1].
9. We are proud of this Government’s commitment to supporting disabled people. However, the amount of public money we spend on benefits for disabled people and people with health conditions is growing every year, and it is vital we ensure that this money is spent in the most effective way possible.
10. In this Green Paper we consider how to address some of the short- and medium-term issues in health and disability benefits. These include:
- Improving signposting to wider services at an early stage. In particular, we want to improve signposting to health services, so that people are better able to access treatment and support;
- Testing advocacy for people who struggle the most to access and use the benefits system;
- Continuing to improve our employment support so that more people can start, stay and succeed in work. This is particularly important given the challenges we are seeing in the wider economy as a result of the coronavirus pandemic. This work includes exploring greater join-up between employment support and health services; and
- Improving the support for, and expectations of, employers, to help prevent people with a health condition or disability falling out of work;
- Exploring how to conduct assessments in different ways. This includes through the use of telephone and video assessments;
- Continuing to reduce repeat assessments where a person’s health is unlikely to change;
- Continuing to increase the quality and accuracy of the decisions we make on benefit entitlement;
- Exploring further improvements to our mandatory reconsideration and appeal processes; and
- Improving the information we use to make decisions. This includes securing better medical evidence to increase the speed and likelihood of people getting the correct level of support at the outset.
11. We also want to consider whether we should make more fundamental changes over the longer-term. We want to hear how the benefits system could be designed differently to help more people work and live independently and explore new approaches to providing support.
12. We want to hear from you about the approaches we should consider. Crucially, we want your views on whether we can achieve our ambition within the current structure of health and disability benefits or whether wider change is needed.
13. This consultation is an important step towards making changes that will improve our services, increase opportunities for employment and help more people to live independent lives. Our approach must be informed by different views and opinions, particularly those of disabled people and people with health conditions.
Introduction
14. This Government has ambitious plans to support and empower disabled people and people with health conditions. The National Disability Strategy will be published shortly. This will outline practical changes to tackle the day-to-day challenges disabled people face. It will also set out the Government’s vision to transform the lives of disabled people by taking action across Government and wider society.
15. This Green Paper will explore how the benefits system can better meet the needs of disabled people and people with health conditions. As such, it forms an important part of the Government’s wider plans and is this Department’s main contribution to the National Disability Strategy.
16. A number of publications led by other Departments, will also explore support for disabled people and people with health conditions, as follows:
- The Department of Health and Social Care is working to refresh the Autism Strategy. This will improve understanding of autism and the provision of services and support for autistic people. It will set out steps to enable more autistic people who are able to work to do so.
- The Department for Education will also publish a review of support for children with Special Educational Needs and Disabilities (SEND). This aims to ensure better outcomes for children and young people with SEND. It will consider ways to make sure the SEND system is consistent, high-quality, and integrated across education, health and care.
17. As well as being linked to work across government, this Green Paper builds on our earlier consultations. We published the 2016 Improving Lives Green Paper[footnote 2] and the 2017 response[footnote 3] with the Department of Health and Social Care. These looked at supporting disabled people and people with health conditions to remain in and return to work, improving assessments for benefits, and helping employers to recruit disabled people. We will follow up on the responses to this Green Paper with a White Paper in mid-2022. This will aim to set out how we can better enable people to take up work and live more independently, and outline the changes we want to make to the benefits system to better address structural and delivery challenges.
18. The 2019 Health is Everyone’s Business consultation[footnote 4], also published with the Department of Health and Social Care, looked at ways to encourage employers to support disabled people and people with health conditions at work. This focused on better and earlier information and support for employers and employees, to help prevent disabled people and people with health conditions losing their jobs through ill-health. We will shortly be publishing the Health is Everyone’s Business consultation response. While important progress is being made, we know there is more to do.
19. The coronavirus pandemic has affected how we live and work. Since spring 2020, we have been providing support in the midst of a public health emergency. More people than before have been claiming benefits: in the first six weeks of the UK Government’s response to the pandemic, we received over six times the normal number of claims for benefits, including Universal Credit (UC) and Employment and Support Allowance (ESA) [footnote 6]. Many disabled people and people with health conditions have been identified as clinically extremely vulnerable (CEV) and, as such, advised to shield for significant periods since the start of the pandemic. Since the pandemic began, we have rapidly adapted our ways of working to continue to support people. The UC system in particular has shown resilience and flexibility in how it has responded to the challenges posed by the pandemic.
20. By the end of 2019, the number and rate of disabled people in employment were the highest they have been since comparable records began in 2013[footnote 5]. As we come through these unprecedented challenges, we are still committed to getting 1 million more disabled people into work by 2027. The number of people needing our support is forecast to increase[footnote 7]. As we recover from the pandemic, we want to intensify our support for disabled people and people with health conditions.
The Scope of this Green Paper
21. This consultation focuses on the main benefits paid to disabled people and people with long-term health conditions of working age. These benefits fall into two groups:
- Benefits for people who have a health condition or disability that affects their ability to work and who are unemployed or on a low income. These benefits are ESA and UC.
- Benefits to help with some of the extra costs for disabled people and people with long-term health conditions. These are paid to people whether or not people have a job or income, and aim to support independent living. The main extra costs benefit is Personal Independence Payment (PIP), which is replacing Disability Living Allowance (DLA) for adults.
Employment and Support Allowance (ESA)
22. Until recently, ESA has been the main benefit paid to people who have a disability or health condition that affects their ability to work. People who receive ESA are placed in one of two groups. Where a person is able to prepare for work, that person will be placed in the Work-Related Activity Group (WRAG). People in the WRAG may be required to do things like write a CV or take part in confidence-building sessions. Alternatively, a person may be placed in the Support Group. Where someone is placed in the Support Group there is no obligation to take part in work-related activity. People in the Support Group receive an extra amount of benefit, on top of their main ESA payment.
23. There are two types of ESA: income-related ESA and contribution-based ESA. Contribution-based ESA is now known as New Style ESA[footnote 8], while income-related ESA (ESA (IR)) is being replaced by UC. In November 2020 952,260 people were claiming ESA (IR) and have not yet moved across to claim UC, while 809,590 people were receiving New Style ESA[footnote 9].
Universal Credit (UC)
24. UC is a benefit for working-age people who are unemployed or in low-paid work and who have limited savings. It was introduced in 2013 and is simplifying the benefits system by replacing six different benefits with one. A person does not need to be disabled or have a health condition to be able to claim the main UC payment (the standard allowance). Where a person who is eligible for the main UC payment has a health condition which affects their ability to work, that person may be found to have limited capability for work (LCW) or limited capability for work and work-related activity (LCWRA). People found to have LCWRA receive an extra amount of benefit in addition to the main UC payment.
25. We consider support for people claiming UC who have LCW and LCWRA in this Green Paper. We also consider people claiming UC with approved evidence of a health condition[footnote 10] as well as people claiming UC who are waiting for an assessment. Throughout this Green Paper we will refer to these people as people claiming UC with a health condition. People claiming UC with a health condition remain part of the overall UC caseload. 782,000 people of working age were claiming UC with a health condition in November 2020[footnote 11].
Personal Independent Payment (PIP)
26. Unlike UC and ESA, PIP aims to help people with the extra costs of a disability or long-term health condition. PIP is paid regardless of income or savings. The amount paid depends on the impact of a disability or health condition. PIP was introduced in 2013 to replace DLA for adults of working age to provide more support for the people who need it most. In November 2020 there were 2.5 million working-age people receiving extra costs benefits. The majority of these people are claiming PIP[footnote 12].
Other Support
27. In November 2020, 3.5 million working-age people were claiming at least one of PIP/DLA or are claiming ESA or UC with a health condition. Of these, 1.6 million working-age people claim PIP/DLA as well as ESA or UC with a health condition[footnote 13].
28. We use ‘functional assessments’ on PIP, ESA and UC LCW/LCWRA. A functional assessment is one which considers the impact of a health condition on a person’s ability to carry out activities, rather than just the health condition itself. The Work Capability Assessment (WCA) is used to help decide financial entitlement and employment support for ESA and UC. We use a separate assessment to determine entitlement for PIP.
29. As well as the payment of benefits, the help we offer working-age disabled people and people with health conditions includes employment support (for people claiming UC and ESA). In addition, mobility support is provided through the independent Motability scheme (for people receiving higher-rate PIP and DLA mobility payments) and support to apply for UC is available through the Help to Claim service.
30. Although the scope of this Green Paper is restricted to support for working-age disabled people and people with health conditions, many of the issues we explore will also resonate with older people who have similar needs. There are 284,000 people over State Pension age who receive PIP[footnote 14]. The benefits system also provides financial support for people over State Pension age through Attendance Allowance (AA). AA can help towards the extra costs faced by pensioners who require long-term care or supervision as a result of being disabled or having a health condition. Disabled people and people with health conditions may also have unpaid carers. We provide support for unpaid carers through Carer’s Allowance or extra amounts for carers in UC and other benefits[footnote 15]. As we consider the responses to this consultation we will look at the potential impacts on support for people with similar needs over State Pension age, and unpaid carers.
Why Change is Needed
31. Starting, staying and succeeding in work can be more difficult for many disabled people than non-disabled people. Disabled people and people with health conditions can also face other challenges which make it harder to live equal, independent lives.
32. Currently one in three people aged 16-64[footnote 16] in the UK has a long-term health condition and one in five people aged 16-64 in the UK is disabled[footnote 17]. The number of working-age people reporting a disability increased by 20% between 2013 and 2019[footnote 18], and is forecast to continue to grow[footnote 19]. The number of older working-age people has increased and, typically, people’s health declines with age. However, changes in the age of the working-age population do not fully explain the increase in the number of people claiming health and disability benefits. There are likely to be many factors, including the increase in the proportion of people reporting a mental health condition[footnote 20] [footnote 21]. In 2020 50% of working-age people receiving ESA and 41% of working-age people receiving PIP/DLA had a mental health condition as their main condition[footnote 22].
33. Spending on benefits for disabled people and people with long-term health conditions is currently the highest it has ever been[footnote 23]. In 2021/22 we are forecast to spend £33 billion to support working-age adults on PIP/DLA, ESA and people claiming UC with a health condition. Over the next five years this spending is forecast to continue to increase[footnote 24].
34. We want to make sure that money spent on supporting disabled people and people with health conditions has a positive impact on their lives. Spending on the main benefits claimed by disabled people and people with health conditions is at a record level[footnote 25] and there has been positive progress on outcomes. By the end of 2019, the number and rate of disabled people in employment were the highest they have been since comparable records began in 2013[footnote 26]. The difference between the employment rate of disabled people and the employment rate of non-disabled people, known as the disability employment gap, also reduced between 2013 and 2019[footnote 27].
35. Our ambition is to do more and go further to improve employment and independent living outcomes for disabled people and people with health conditions. This is not only good for the individual, but good for everyone. Having one extra disabled person in full-time work, rather than being out of work longer term, would mean Government could save and re-invest £15,000 a year[footnote 28].
36. We want to continue to reduce the disability employment gap, which currently stands at 28.6%[footnote 29]. According to the latest figures, 43% of people living in poverty live in a family where someone is disabled[footnote 30]. Disabled people and people with health conditions have told us that change is needed, as set out below.
Listening to Disabled People and People with Health Conditions
37. We have been listening to disabled people and people with health conditions. Their feedback has helped shape our proposals for change. To make sure we heard a range of views which reflect people’s lived experience, the Minister for Disabled People, Health and Work held a series of Green Paper events. Disabled people and people with health conditions, local support organisations, national charities, employers and think tanks have all taken part. To understand the needs of people living in different parts of Great Britain, we have held events in large towns and cities as well as in more rural and coastal areas. To continue listening to people during the pandemic, we have also held virtual events. More information about when, where and how these events have been conducted is provided in Annex A.
38. We have also collected evidence through research. In recent years, independent researchers have surveyed and interviewed thousands of people claiming health and disability benefits. This work has been done to understand more about people’s experiences of claiming benefits[footnote 31] and to establish where we can make improvements[footnote 32].
39. We are grateful to everyone who has attended these Green Paper events and taken part in research. We reflect on the insights that have been gathered in every chapter of this Green Paper. We will continue to listen to disabled people and people with health conditions throughout the consultation period and beyond.
Priorities for Change
40. The insights from Green Paper events have helped us develop three priorities for change. These priorities will help us to improve outcomes for disabled people and people with health conditions. The three priorities are:
- Enabling independent living;
- Improving employment outcomes; and
- Improving the experience of people using our services.
41. Each of these priorities is explained below.
Enabling independent living
42. Independent living is about extending opportunities, so disabled people and people with health conditions can achieve their full potential and live the lives they choose.
43. At present, we enable independent living mainly through the payment of benefits and the provision of employment support. People who receive higher-rate PIP or DLA mobility payments can also swap their payments to access mobility support through the independent Motability Scheme.
44. At Green Paper events people said that we could do more to make sure disabled people have equal access to the same opportunities as non-disabled people. People asked us to provide better and broader support to help meet the specific needs of disabled people and people with health conditions. This includes help to overcome obstacles to independent living, such as difficulties in accessing healthcare, issues with transport and a lack of suitable local jobs. People told us that government services need to be more accessible for disabled people, so that people can get the support they need. People said that we need to work harder to provide reasonable adjustments to the services provided by this Department. The support we offer could also be better joined-up, both internally (between different benefits) and externally (with services offered by other government departments and agencies, the NHS, local authorities and charities).
45. Our first priority is to support disabled people and people with health conditions to live independently and achieve their potential. This means that people should be provided with the right amount of financial support, given the opportunity to make their own choices, have equal access to services, be supported to access healthcare and treatment, and be able to participate in society on the same basis as other people.
Improving employment outcomes
46. We want disabled people and people with health conditions to have opportunities and live a full life. Being in appropriate work is good for health and being out of work can have a negative impact on people’s health[footnote 33]. We want to focus more on what disabled people and people with health conditions can do, rather than what they cannot. Through effective employment support we can help people improve their health and reach their potential.
47. The Government has committed to continue reducing the disability employment gap. We have also committed to see 1 million more disabled people in employment between 2017 and 2027. We want to do our best to make sure that disabled people and people with health conditions have the same opportunities as others to fulfil their potential. We want to help disabled people and people with health conditions to stay in work wherever possible. As set out in the Health is Everyone’s Business consultation[footnote 34], preventing people from falling out of work is a key part of our ambition. We also want to do more to help people prepare for and enter employment.
48. We already offer employment support to people claiming benefits such as UC and ESA. This is delivered through work coaches in jobcentres and employment support provision including the Work & Health Programme and Intensive Personalised Employment Support (IPES). We also support disabled people in work through Access to Work grants and work with employers to help them recruit and retain disabled people through the Disability Confident scheme.
49. At Green Paper events, disabled people and people with health conditions expressed a desire to contribute to society in such a way as to be able to balance working with managing their health. People recognise the value of employment but want us to take more account of their circumstances, including the impact of being disabled or having a health condition, and the restrictions of their local area. People would like support and training to be more tailored to their needs. Some people felt afraid of taking steps to prepare for or try out work in case this affected their benefits. People also asked for better support from employers and this Department to stay and succeed in work.
50. We have conducted research with disabled people and people with health conditions on ESA and UC[footnote 35] to understand their feelings about preparing for work and working. This showed that people felt health-related issues were often a challenge. People were worried that their health could make it difficult to find or keep a job, or that working could have a negative impact on their health.
51. The same research indicates that disabled people and people with health conditions do not always feel comfortable taking up our employment support. Some people who were not in work were concerned that doing paid work could risk them losing their benefits or having to reapply for benefits if a job did not work out. Some people felt worried about being left without income during the period between their benefit payments stopping and receiving the first wages from a new job[footnote 36].
52. Some of the people who took part in this research were claiming ESA rather than UC. UC is an in- and out-of-work benefit which helps to address some of the concerns people expressed. For example, UC allows people to try out work and stay on benefit in the knowledge that their benefit will continue if the job does not work out.
53. Our second priority is to reduce the difficulties disabled people and people with health conditions can still face in starting, staying and succeeding in employment. We want to offer better and more tailored employment support, whether people are in or out of work. We want to help prevent disabled people and people with health conditions from falling out of employment. We want to work with employers to improve employment outcomes wherever people may be able to work, now or in the future.
Improving the experience of disabled people and people with health conditions
54. Most people receiving services from this Department agree that we do what we say we will do, that we treat people fairly and that our staff are helpful, polite and respectful[footnote 37]. Where disabled people and people with health conditions have said their experience could be better, we want to take ambitious steps to improve.
55. At Green Paper events some people have said it is difficult to interact with us. People may feel afraid of having to use the benefits system. People sometimes struggle to apply for benefits and can find health assessments difficult. People said they did not always trust assessments, or the decisions that they led to. Where people challenge a benefit decision this can sometimes lead to a long and difficult process. A lack of trust can affect people’s willingness to accept offers of employment support.
56. Our third priority is to improve the experience of disabled people and people with health conditions by continually listening, learning and improving. We want to make our services easier to access and our processes simpler, where we can. We want to make improvements that will help build people’s trust. We want to explore ways to offer more and better support for the people who need it most.
Spending on Health and Disability Benefits
57. In the last seven years we have seen an increase of 20% in the number of working-age people reporting a disability[footnote 38]. In 2021/22 we are forecast to spend a record £58 billion of public money on benefits for disabled people and people with health conditions[footnote 39]. Of this, £33 billion is spent on working-age people in Great Britain, including spending devolved to the Scottish Government for working-age PIP and DLA. Between 2021/22 and 2025/26 we expect real terms[footnote 40] spending on Great Britain working-age health and disability benefits to increase from £33bn to £40bn[footnote 41], an increase of 20% and an increase in expenditure as a proportion of GDP over this time. We are proud of this Government’s commitment to supporting disabled people. However, it is vital to ensure that public money is spent in the most effective way possible.
58. The Government is committed to improving the lives of disabled people and people with health conditions. We want to help people overcome challenges to independent living. We also want to support people to move into work wherever possible. Rising spending on health and disability benefits suggests there is more to be done to enable people to live independent lives and work. We want to consider the support we currently offer and explore whether there may be better ways to provide support.
59. We must ensure that disabled people and people with health conditions are effectively supported. This Green Paper will consider whether the money we spend on supporting disabled people and people with health conditions is spent well. This includes ensuring that we have the right checks in place to make sure we are paying people the right amount of money for their particular circumstances. This is because we want to ensure that the health and disability benefits system is effective and sustainable in the future.
Across the United Kingdom
60. The UK Government is committed to improving the lives of disabled people and people with health conditions across the Union. We welcome views from people wherever they live, including in Northern Ireland. However, the specific areas covered in this Green Paper relate to Great Britain only.
61. This section sets out the extent to which this consultation will apply in each part of the UK. The Minister for Disabled People, Health and Work in the UK Government has overall responsibility for disabled people across the United Kingdom.
62. The UK Government is responsible for policies on employment support and social security in England and Wales, and shares that responsibility in Scotland with the Scottish Government. In Northern Ireland, these areas are the responsibility of the Northern Ireland Executive. The Department for Communities in Northern Ireland and the Department for Work and Pensions in Great Britain seek to maintain similar social security systems.
63. In Scotland, some parts of the social security system are devolved[footnote 42]. This includes PIP and DLA. These will be replaced over time by new Scottish Government benefits[footnote 43]. Once these new benefits have been introduced, the proposals relating to PIP and DLA considered in this Green Paper will not apply in Scotland. This includes the changes we propose to the Special Rules for Terminal Illness (SRTI) in PIP and DLA, which are outlined in Chapter 3 of this Green Paper[footnote 44]. The changes proposed for ESA and UC will apply in Scotland, since these benefits will remain the responsibility of the UK Government.
64. With respect to employment support, the Scottish Government has powers to set up contracted programmes to help disabled people into work. It has similar powers to support people who are at risk of long-term unemployment, provided this support lasts for 12 months or longer. The UK Government remains responsible for the support provided by Jobcentre Plus, and for other contracted employment support in Scotland. The proposals in this Green Paper apply in Scotland to areas which are reserved to the UK Government.
65. In Wales, employment support and social security are the responsibility of the UK Government. This means that the proposals in this Green Paper relating to those areas, including PIP and DLA, apply in Wales.
66. The case studies in Chapter 2 of this Green Paper provide insights on delivery in Scotland and Wales.
67. The Scottish and Welsh Governments are responsible for health, local government, education, skills and social care. Where the proposals set out in this Green Paper relate to these areas, the consultation and views will focus on what this means for England.
68. We remain committed to working with the Scottish and Welsh Governments, and with the Northern Ireland Executive, to consider how best to deliver support for disabled people and people with health conditions.
Summary
69. The three priorities of enabling independent living, improving employment outcomes and improving the experience of people using our services will be considered in each of the following chapters:
- In Chapter 1 we will explore ways to provide more support to help meet the needs of disabled people and people with health conditions and allow them to more easily access and use benefits and services.
- In Chapter 2 we will consider how to continue to improve employment support for disabled people and people with health conditions, and how to encourage people to take up that support, where possible.
- In Chapter 3 we will look at short-term improvements to our current services such as improvements to assessments and decision making, to improve the experience of disabled people.
- In Chapter 4 we will describe how we have been working with disabled people and people with health conditions, medical professionals, charities and academics to consider changes to future assessments, and explore alternative approaches.
- In Chapter 5 we will explore changes that could be made to the structure of the main benefits claimed by working-age disabled people and people with health conditions.
70. In each chapter, we want to hear your views on the areas for consultation. This Government and this Department have bold ambitions for disabled people and people with health conditions. This Green Paper is a crucial part of the action we are taking under the National Disability Strategy. Our priority now is to hear your suggestions on how to transform these ambitions into reality.
Chapter 1: Providing the Right Support
Chapter Summary
We have heard that people can sometimes find it difficult to access health and disability benefits and related support. In this chapter we explore how to improve this by:
- Improving signposting. In particular, we want to improve signposting to health services, so that people are better able to access treatment and support;
- Testing advocacy for people who struggle the most to access and use the benefit system; and
- Exploring further support for mobility needs.
Introduction
71. Each person is likely to have different support needs at different times. We want to do our best to make sure disabled people and people with health conditions have the right support to meet these needs and live independently.
72. Lots of support, including financial, health and employment support, is already available to disabled people and people with health conditions from a range of sources. Most people feel it is easy to access and use our services[footnote 45]. However, at Green Paper events, some people said that it can be difficult to know what wider support exists and how to access it. At the same events, we heard that it is not always clear which of our benefits people might be eligible for. People have also told us that our benefit forms can feel long, stressful and difficult to fill in. Finally, we have heard that the reasonable adjustments people ask for when using our services are not always provided.
73. We want to do more to ensure everyone has a smooth experience and can access the right help. To achieve that, in this chapter we will explore ways to help people access and use the current health and disability benefits system and wider services.
What We have Already Done
Improving reasonable adjustments
74. A reasonable adjustment is a change that removes or reduces the barriers disabled people face. We want to make sure that our services are fully accessible to support people and offer the reasonable adjustments that people need. For example, we have a visiting service for people who are not able to get to one of our assessment centres and we provide communications in alternative formats.
75. The Department already has in place a wide range of reasonable adjustments for disabled people. These include communications in braille, large print and electronic formats for visually impaired people, British Sign Language (BSL) interpretation for deaf and hard of hearing people, quiet rooms for autistic people, and coloured paper for dyslexic people. We also offer email as a reasonable adjustment for people who cannot access print or find it difficult to use the telephone to contact us.
76. We have been working with organisations for people with a learning disability to develop a Department for Work and Pensions (DWP) Easy Read standard and publish new Easy Read guides on topics such as Access to Work which are accessible online. Further Easy Read products for PIP and UC are also available on the UK Government website, GOV.UK.
77. We are continually working to improve the reasonable adjustments we provide. In October 2020, we completed the roll-out of the Video Relay Service across all benefits. This allows people who use BSL to contact us by telephone. We are also testing the introduction of Video Remote Interpreting in our services. This would allow BSL users to communicate with us through an interpreter on a video call.
78. We are working on improving how we collect and record alternative formats and reasonable adjustments on our systems so that people will not need to request a change to their communications more than once. We have also set up a Reasonable Adjustments Forum with disability charities, to continue to improve accessibility. We want everyone to get the support they need and would like to hear what more we could do.
Consultation question
What more could we do to improve reasonable adjustments to make sure that our services are accessible to disabled people?
Improvements to forms
79. We use forms to understand the challenges disabled people and people with health conditions face that affect their ability to work and live independently. For PIP, we have the PIP2 ‘How your disability affects you’ form. For UC and ESA, we use the UC50 and ESA50 ‘Capability for Work’ forms.
80. It can be difficult to explain the effects of a health condition or disability, as illustrated in the case study below.
Case study: The need to improve our forms
James, an unpaid carer, told us that if our forms were easier to understand, people would need to rely less on medical professionals to provide support when applying for benefits. The focus of the forms on what a person cannot do can often leave people feeling more vulnerable and less positive. Nothing prepares people for how complicated the forms are and what they are asking people to describe or prove. James said that he had to fill in 42 pages of information which took him two whole days. He had to send lots of emails and contact multiple healthcare professionals to obtain the necessary supporting evidence.
81. To address this, we commissioned research to understand more about how to improve our forms[footnote 47]. We are now making many of the changes that people asked for. Following the discussions that took place with disabled people and people with health conditions through research and at Green Paper events, we are improving our forms. For example, on the PIP2 form we are:
- Simplifying instructions and reducing repeated information;
- Adding examples that show how to explain the impact of certain conditions;
- Changing the descriptions of some activities to make it clearer how they relate to different conditions; and
- Explaining more clearly what happens after returning the form.
82. At Green Paper events, some people told us that they prefer online forms. During the coronavirus pandemic, we introduced an online New Style ESA claim service. We are developing a fully digital version of the UC50 ‘Capability for Work’ form. We are also developing an online PIP2 form which can be automatically saved and uploaded onto our systems. We hope to offer the improved digital PIP2 form by summer 2021. We will always offer alternatives to people who cannot access online forms.
Signposting and support to help people access benefits
83. Signposting means making people aware of other benefits and services which could help them, so that people can more easily access vital support. Signposting can be particularly helpful when people are claiming benefits for the first time. We already provide a range of support to 3.45 million disabled people and people with health conditions of working age, including through PIP and UC[footnote 48]. At Green Paper events, we heard that people would like more information, signposting and practical support to help meet their financial and health-related needs.
84. We have set out below examples of processes that are in place and changes underway which make it easier for people to identify and access relevant support:
- Improving information on GOV.UK – To help people access the relevant benefits online, we are making it easier for people to find information on GOV.UK. We know there is a lot of information on this website so people can struggle to know where to go for what they need. We are working with GOV.UK users, local partners and other organisations to improve the information we provide online.
- Signposting to other services – We want to find ways to signpost people to other support and services. For example, in the letter people receive with their PIP decision, we include information about other benefits, support and services that could be helpful. Work coaches also identify issues that could make it more difficult for people to start work, and find help to address these. This can include signposting people to local services and support for issues related to mental health, housing, debt management and wellbeing.
- Special Rules for Terminal Illness – Where people are nearing the end of their lives, it is important that the process for securing support is as simple as possible. Since the end of 2020 we have been offering a full benefit check on the PIP telephone service for people who have applied for PIP through the Special Rules for Terminal Illness. This identifies the financial support to which people may be entitled.
- Extra Support through Advanced Customer Support Senior Leaders (ACSSLs) – In 2020, we introduced a network of 31 ACSSLs. These roles are located throughout England, Scotland and Wales. Where people need extra support to access our benefits or services, ACSSLs support and signpost people to a range of local provision.
- Support through Help to Claim – Since April 2019, we have funded[footnote 49] Citizens Advice and Citizens Advice Scotland to successfully deliver our Help to Claim programme[footnote 50]. As illustrated in the case study below, ‘Help to Claim’ offers independent, tailored and practical support to help people make a UC claim and receive their first full payment on time.
Case study: Support through Help to Claim
Pauline had been on contribution-based ESA which came to an end after 12 months. She rang the ESA helpline and was told to apply for UC online. Pauline has poor mental health and is a carer for her disabled father. Pauline needs support with managing money and budgeting. She also struggles to use the internet and was unsure of her entitlement and was not able to start an application for UC online.
This situation was making her anxiety worse. A Help to Claim adviser was able to support Pauline, check her entitlement and help her through the application process. The adviser gave Pauline information so that she could check that her first UC payment was correct, as well as a number to call if she had any concerns at the beginning of her claim. Pauline was very grateful for the support she received to claim UC.
85. While we have made progress, we know more needs to be done. We want to go further to take account of and respond to people’s different needs and improve the experiences of people using our services. We would like to hear how signposting can help us to do this more effectively.
86. In particular, we know that access to appropriate health treatment is vital to enable people to live full and independent lives. Health-related issues can make it harder for people to take up employment support, as well as to start and stay in work. Because of this, we especially want to improve signposting to health services, so that people are better able to access treatment.
Consultation questions
What more information, advice or signposting is needed? How should this be provided?
Going Further
Testing advocacy support
87. At Green Paper events, we heard about the power of advocacy for disabled people and people with health conditions. Advocacy is more than signposting; it is about supporting each person to help ensure their needs are met. Many people can use the benefits system independently or have the help of friends, family, charities or other support networks[footnote 52]. People can also use Help to Claim for UC. For people who do not have that support, we want to test providing advocacy so that people can get the right level of support and information first time. Where advocacy support is already available from other sources, we want to look at how we can make sure everybody who needs it has access to the same level of service[footnote 53]. 88. Evidence supports what we have heard at Green Paper events: that extra support to help people navigate the benefits system can help change people’s lives[footnote 54]. To help us design and test advocacy support, we want to explore how it might look. We will explore in our test of the service whether it is feasible to deliver advocacy support and whether this offers value for money.
89. We recognise that improvement to our services is an important part of making the benefits system easier to use. Chapter 3 looks at what we could do to improve the experience of disabled people using our services. Providing advocacy would not be an alternative to these improvements but an additional form of support for people who need it.
How advocacy support might look
90. We suggest that advocacy support could be based on these principles:
- Advocacy could help people find information and provide practical support (such as filling in forms) but would also help people to have their voice heard on matters affecting them.
- This support would not be available for everyone; it would only be offered to the people who need it most. It could be for people who do not already have the support of charities and other organisations. Evidence suggests that advocacy could benefit disabled people in particular[footnote 55] but it would not need to be limited to disabled people. It could also be offered to other people who are not able to find their way through the benefits system without extra support.
- It should be delivered in a way that ensures it offers advice that people can trust.
- Advocacy should not duplicate existing support but fill gaps in provision. It should complement the help other organisations provide.
- It should be flexible enough to support people whenever they need help, and not just at the beginning of their claim. This will help meet the needs of vulnerable claimants.
- Advocacy should aim to help people to achieve certain outcomes rather than being open-ended, so that it helps people to become independent from the service[footnote 56].
- Advocacy could do more than just help people to access and use the benefits system. It could also provide support to address wider issues in people’s lives (such as access to health and care services, and housing) which we know can affect people’s ability to manage their health condition or disability.
91. We want to hear from people who could benefit from advocacy and their representatives to help us develop this test. We are keen to hear views on the principles we have proposed and would like to understand whether there is anything else we should consider.
Consultation questions
- Do you agree with the principles we have set out for advocacy support?
- How might we identify people who would benefit from advocacy?
- What kinds of support do you think people would want and expect from advocacy?
Exploring support for mobility needs
92. The ability to move around and make journeys is a key part of independent living. We currently provide mobility allowances through PIP and DLA. People can choose to spend these allowances however they wish.
93. A popular way to spend mobility allowances is through the independent Motability scheme. The Motability scheme, which is operated by the independent Motability charity, helps people meet their mobility and travel needs. It allows disabled people and people with health conditions to use their PIP/DLA higher-rate mobility allowance to lease a new affordable car, Wheelchair Accessible Vehicle, scooter or powered wheelchair. In 2020 1.8 million people were receiving the PIP Enhanced mobility or DLA Higher mobility award and were eligible for the Motability Scheme. In that year there were 635,000 customers using the scheme[footnote 57].
94. The charity which provides the Motability Scheme benefits from a range of tax concessions[footnote 58] and the direct transfer of mobility allowances[footnote 59]. This means that they are able to provide leases that are around 44% cheaper than they would be otherwise[footnote 60]. Currently, 34% of eligible people join the Motability Scheme[footnote 61]. The support provided by the scheme is illustrated in the case study below. We want to hear how disabled people and people with health conditions use their PIP and DLA mobility payments, particularly where people do not use Motability, and whether there is more we could do to support people’s mobility needs.
Case study: The Motability scheme
Nazmin, 37, has Arthrogryposis Multiplex Congenita. This is a condition that causes limb weakness. Nazmin decided to use her mobility allowance to join the Motability Scheme after she attended a regional driving assessment centre to find out which adaptations would enable her to drive a car herself.
Before I found out about Motability, I used to have to travel by taxi, but this wasn’t ideal as they were frequently late. This experience gave me the incentive to pass my driving test. The advisors at the driving assessment centre suggested what adaptations would be suitable for me and informed me about the Motability Scheme and the range of help that both it and the charity could provide me with.
Nazmin received a grant from Motability for adaptations to be added to her new vehicle. She has a hoist to help move her powered wheelchair in and out of the vehicle, a powered tailgate and hand controls.
Motability and the Motability Scheme have been an absolute godsend and continue to be so. It is incredibly hard to put into words just how much my vehicle has helped over the years and continues to help. I started using the Scheme in 2004 and in that time, it has enabled me to go to university and flourish within my studies. It enables me to go out to visit friends and family, hospital appointments and interviews. It enables me to work, to contribute to and feel part of society and to live a fulfilling life.
Consultation question
Are we meeting disabled people’s mobility needs? Please tell us why/why not.
Summary
95. We have listened to what people have told us at Green Paper events, through surveys and research. Although most people find our services easy to access[footnote 63], we know that some disabled people and people with health conditions can struggle to access benefits and use services. Because of this, we want to do more to help people find their way through the benefits system and access wider support. This includes improving signposting to other services, such as housing and health, and testing advocacy support.
96. We believe that together, improving signposting and offering advocacy could make it easier for people to use the benefits system and help meet their wider needs. Since being able to move around and travel freely is an important need for many disabled people, we also want to understand what more we can do to help people meet their mobility needs.
Chapter 2: Improving Employment Support
Chapter Summary
There has been good progress on disability employment since the 2016 Improving Lives Green Paper[footnote 64]. By the end of 2019, the number and rate of disabled people in employment were the highest they had been since comparable records began in 2013[footnote 65]. However, we want to go further to help more disabled people and people with health conditions prepare for, start, stay and succeed in work, where it is right for them. In this chapter we explore:
- Taking action now through early intervention. This means supporting people to stay in work and providing back-to-work support earlier to reduce the risk of people falling into long-term inactivity.
- How to ensure our that our jobcentres are welcoming and engaging, to encourage more people to take up our employment support. This includes using a new approach to conditionality. Our staff also need to be expert in providing and referring to employment support for disabled people and people with health conditions.
- Personalising employment support, recognising that one size does not fit all. We also ask what more we can do to encourage people in the Support Group/LCWRA to take up our voluntary employment support.
Introduction
97. Work has a vital role to play in supporting good mental and physical health[footnote 66]. It can also provide greater financial security and enable people to live independently. Improving employment outcomes for disabled people and people with health conditions can help unlock their talents, promote equal access to opportunity and contribute to the economy. This is why we want to reduce the difference between the employment rate of disabled and non-disabled people, which is known as the disability employment gap.
98. In 2017, we set a goal to see 1 million more disabled people in work by 2027[footnote 67]. In the three years since, the number of disabled people in work grew by 800,000[footnote 68]. The disability employment rate has also increased by 8.4% since comparable records began in 2014[footnote 69]. We now want to intensify our efforts to provide the support disabled people and people with health conditions need, when they need it. We remain committed to achieving the challenging goal of 1 million more disabled people in work and, once we have, we will consider how we can build on this success.
99. In this chapter we consider employment support for disabled people and people with health conditions. We also know that other factors, such as people’s experiences of assessments for benefits and the structure of the benefits system, can affect whether and how people move into and stay in work. These other factors will be considered in Chapters 4 and 5.
100. To improve employment outcomes for disabled people and people with health conditions, we want to support people who are out of work to start, stay and succeed in appropriate employment, wherever it is possible to do so. However, to achieve our goals, it is equally important that we support disabled people and people with health conditions in work to remain in employment. For full context, this chapter should be read alongside the Health is Everyone’s Business consultation[footnote 70]. This contained a range of proposals to support more disabled people and people with health conditions to stay in work. Evidence shows how important it is for an employer to support an employee who is at risk of, or on, long-term sickness absence. Providing more support sooner to employees and employers is vital to reduce the chance of people losing their jobs through ill health[footnote 71].
101. In the forthcoming response to the Health is Everyone’s Business consultation, which we will publish with the Department of Health and Social Care, we will set out our strategy for preventing ill health-related job loss. In this response, we will explain how we propose to improve information, advice and guidance on health, work and disability. This includes work by the Health and Safety Executive (HSE) to lead new guidance on how to manage sickness absence and support people to return to work.
102. In this chapter we explore early intervention. We want to provide back-to-work support earlier when people apply for out-of-work health and disability benefits, through jobcentres and our employment support programmes, in order to reduce the risk of long-term unemployment.
103. We also consider what more we can do to ensure disabled people and people with health conditions feel comfortable taking up our employment support. We look at how to make our jobcentres more welcoming and engaging. We set out the new way we are applying conditionality for disabled people and people with health conditions claiming out-of-work benefits[footnote 72]. Our staff also need to be expert in providing and referring to employment support in order to build trust with disabled people and people with health conditions.
104. Starting and staying in work can be particularly difficult for disabled people and people with health conditions. We know that one size does not fit all and people will have different support needs. Later in this chapter, we set out the wide range of tailored employment support that is available to help meet people’s specific needs. This includes approaches to support that join up employment and health services. We also ask how best to offer voluntary support to people in the ESA Support Group and people claiming UC who have LCWRA.
Early Intervention
105. Preventing people from falling out of work is crucial. Where ill health-related job loss does occur, it is vital to ensure that people can rapidly access appropriate support. We know that the longer someone is out of work, the greater the risk to their long-term health and wellbeing[footnote 73]. As well as exploring early intervention, improved guidance and greater support to help people stay in work, we want to set out changes to Access to Work and Disability Confident that will support employers and employees. We also want to explore providing earlier and more comprehensive support through jobcentres for people who have fallen out of work because of a health condition or disability. This support could be provided before people have a WCA. Where people are able to work, providing this extra support could enable a quicker return to appropriate employment.
Working to support employers
106. Employers play a vital role in supporting disabled people and people with health conditions to stay in work. Soon, we will publish our response to the Health is Everyone’s Business consultation with the Department of Health and Social Care. This focuses on better and earlier support for employers and employees, to help prevent people losing their jobs through ill-health. The response explains how we will clarify and improve information, advice and guidance for employers on health, work and disability. This includes a national information and advice service for employers.
107. The Health & Safety Executive (HSE) will also lead new guidance on sickness absence management and returns to work. We will take steps to improve access to quality occupational health services[footnote 74], particularly for people who work in small and medium-sized businesses.
108. We know that the proportion of people with a mental health condition is growing[footnote 75]. We have been working to help employers improve mental health in the workplace. This has included contributing to the Government’s plan[footnote 76] to prevent, mitigate and respond to the mental health impacts of the pandemic. In addition, we continue to support employer action to improve mental health at work through the Thriving at Work Leadership Council. This includes promoting the information and advice available via the Mental Health at Work website[footnote 77], which supports employers to manage the mental health of their staff.
109. Access to Work provides practical and financial support. It is designed to help people overcome barriers and cover the extra costs disabled people and people with health conditions can face in work, beyond those covered by reasonable adjustments. This support is illustrated in the case study below. It can include workplace assessments, providing support workers, specialist aids and equipment and travel to work costs.
Case study: Support provided by Access to Work
Deborah experiences light sensitivity, migraine and a number of musculoskeletal health conditions. Using equipment supplied through Access to Work has enabled Deborah to work effectively in an office.
I chose to apply online and this was a simple process to complete. Once received by Access to Work, an Advisor was allocated to myself who then got in touch to discuss my application further and explained the process step by step.
Using equipment supplied through Access to Work has helped tremendously.
I use an ergonomic split keyboard and a roller mouse, these offer me the ability to use my computer without exacerbating the pain in my wrist and hand. I also have forearm supports which clamp to my desk; these enable me to achieve a supported posture and reduce pressure on my wrists. I have an ergonomic chair with lumbar support; having the neck support allows me to lean back and stretch periodically throughout the day.
To enable me to work from home through the Access to Work Blended Offer Scheme, I was provided with an Electric Sit-Stand Desk, enabling me to stand or sit while working.
The combination of using all this specialist equipment ensures that I work in a comfortable position, allowing me to sit or stand as needed.
Deborah started working as a Customer Services Advisor with Manpower at EON in 2018. She is now employed as an Account Manager at EON.
110. We know from Green Paper events that Access to Work can be a lifeline for disabled people and people with health conditions. However, some people have found the application process difficult, and said that support can take too long to be provided. We are committed to making Access to Work a fully digital service that is innovative, visible and provides an improved experience. We are already making digital improvements which will speed up the payment process and reduce the time it takes to provide support.
111. We are working with disabled people, disabled people’s organisations and charities via the Access to Work Stakeholder Forum to develop an Access to Work Passport, which we will be testing during 2021. The passport will support disabled people when transitioning from education, leaving the armed forces or moving into employment for the first time. This will be a document that can be continually updated, setting out the needs of the passport holder to assist understanding by the employer and provide relevant support in the workplace. This will provide greater flexibility and reduce the need for repeated workplace assessments when changing job roles or working on time-limited contracts.
112. To provide greater flexibility for disabled people to decide where they work, we made changes to enable Access to Work support to be provided in more than one location. Recognising that many disabled people may want to take up freelance and contractor work opportunities, we have introduced a new flexible application process. This flexible application process will reduce bureaucracy and remove the need for repeated Access to Work applications when moving between contracts.
113. Disability Confident (DC) aims to help disabled people start, stay and succeed in work. It does this by helping employers to think differently about disability and take action to improve how they recruit and retain disabled employees[footnote 79]. We are continuing to increase the number of employers who are signed up to the Disability Confident scheme. In April 2019, 11,500 employers had signed up. By the end of March 2021 this had increased to more than 20,000. We are working with people to maximise opportunities through communications, newsletters, social media and network groups to encourage employers to take part in Disability Confident and to progress through the scheme. We are also taking steps to improve Disability Confident by making it easier for employers to sign up and provide their information online.
Consultation question
What more could we do to further support employers to improve work opportunities for disabled people through Access to Work and Disability Confident?
Providing more support before the Work Capability Assessment
114. Recent forecasts assume that the pandemic will lead to greater levels of economic inactivity, including health-related inactivity. As a result, 300,000 more people are forecast to claim UC with LCWRA and New Style ESA from 2022/23[footnote 80]. This can be expected to increase the demand for WCAs. However, the pandemic has also brought about a potentially lasting shift towards home working, which may present new opportunities for many disabled people and people with health conditions.
115. We want to tackle the predicted growth in health-related inactivity, because we know that the longer someone is out of work, the greater the risk to their long-term health and wellbeing[footnote 81]. To help reduce the chance of people being out of work in the long term, we want to explore offering earlier back-to-work support. This support would go beyond the existing ‘Health and Work Conversation’ which people take part in before their WCA takes place.
116. Where people have recently fallen out of work because of a health condition or disability, jobcentres could help people to consider appropriate employment opportunities and raise awareness of in-work support. This could involve more support from a person’s work coach, more often and earlier in the claim. This support would be tailored to each person’s needs. This could either be delivered by a work coach alone or with a Disability Employment Advisor. This will be explored further in Chapter 4, where we look at a separate employment and health discussion.
Consultation question
How can we support people who have fallen out of work to identify and consider suitable alternative work before their WCA?
Ensuring Jobcentres Are Welcoming, Engaging and Expert
117. In recent years we have undertaken research to help us understand what may be preventing people from taking up the support we offer. Through this research[footnote 82], and at Green Paper events, some disabled people and people with health conditions reported worrying that taking part in employment support or starting work might affect their benefit claim or lead to a sanction[footnote 83].
118. Through UC, people can start a new job and gradually increase their earnings without having to leave the benefit. This makes it easier for disabled people and people with health conditions to try out work without worrying about seeing a sudden drop in income.
119. In this section, we will look at building trust and engagement through our jobcentres. We will also consider the role of conditionality and the expertise of our staff.
Applying a new approach to conditionality
120. At Green Paper events, we have heard that people are nervous about engaging with employment support. Conditionality is the requirement for a person to do certain activities that will help that person move towards and into work if they are able. These activities are tailored to the person’s capability and circumstances, with requirements varying depending on which group or regime people are placed in. People who are waiting for a WCA may be asked to carry out work search on UC or work preparation on ESA. People who are found to have LCW (known as WRAG on ESA) will only be required to carry out work preparation activities; while people who are found to have LCWRA (Support Group on ESA) will not be asked to carry out any mandatory work-related activities.
121. Where activities are required, completing them is a requirement of receiving financial support. However, we will never apply a sanction where someone shows a good reason for not complying with this requirement. The activities should always be reasonable and should take account of a person’s disability, health condition and other circumstances.
122. Having listened to people’s views, we have rolled out a new approach to conditionality for disabled people and people with health conditions. This applies to:
- People claiming ESA in the WRAG;
- People who are claiming UC who have been found to have LCW or;
- People who are claiming UC or ESA, ahead of their WCA.
123. In September 2019, we started testing whether changing how activities are agreed can improve the relationship between a person and their work coach. The aim of the approach is to enable an honest and open conversation about what a person can do. We want people to feel engaged in their activity, understand why it is worthwhile and carry it out to the best of their ability, so people are more likely to move towards work, and into work, where possible.
124. Work coaches have the option of applying no mandatory requirements if they feel this is appropriate for the person’s individual circumstances, but instead are encouraged to set voluntary steps the person could take to move towards or into work. These could include, for example, developing a CV or looking for suitable jobs online. Using their discretion, work coaches apply mandatory requirements only if and when they are needed.
125. One of the reasons why this approach to conditionality was shown to be effective in testing was because work coaches were able to apply more tailored activities to help people prepare for and progress in work. Work coaches felt they were able to develop a better understanding of how best to support people through the new approach. They were able to make the best use of voluntary activities to stretch and encourage people, while introducing mandatory activities if necessary to ensure people remained engaged with their employment support. This new approach also reduced the risk of sanctions. We have now rolled this approach out nationally, subject to ongoing evaluation. We will continue to refine our approach on the basis of these findings.
Testing new support through Health Model Offices
126. We want to encourage people who are able to take up employment support to do so. We know that people value frequent contact with a trusted individual, who can identify and help people access extra support[footnote 84].
127. In 2019, we introduced Health Model Offices in 11 jobcentres across Great Britain. These aimed to test a wide range of initiatives including:
- Providing more intensive support to disabled people and people with health conditions;
- Adapting the physical environment in the jobcentre to better meet the needs of disabled people and people with health conditions;
- Improving links between jobcentres and health services, including by basing work coaches in GP surgeries and healthcare professionals in jobcentres; and
- Introducing new communication tools such as a map which outlines a person’s route through the benefits system. This helps to reassure people and encourage better communication.
128. The work of one of these Health Model Offices is highlighted in the case study below.
Case study: Leeds Eastgate jobcentre is one of the Health Model Offices which tested innovative tools and flexible approaches
- Meeting people in an environment where they feel more comfortable – this can involve meeting people in a private room in the jobcentre where it is quieter or in alternative locations to jobcentres such as in community hubs. A disabled person who had appointments with a work coach at the Headingley Community Hub in Leeds said: ‘It’s great to be seen in a relaxing, supporting environment with my work coach. I feel like a person not a number. I feel part of the process and that things are not just being done to me.’
- A Wellness Star –This tool was used to support conversations between work coaches and individuals on a range of areas such as their lifestyle, condition and aspirations for moving towards work. The tool helps measure progress towards goals and identify support needs. The aim is to encourage open and honest conversations and highlight areas where people need support.
- Flexibility – work coaches were given flexibility over the length of time they could spend with people. This helped work coaches build relationships. One work coach said “it means that we have time to build trust. We can explain how we can help and support individuals – it isn’t a one-size-fits-all approach.”
129. The work of the Health Model Offices has identified a number of initiatives which could improve the service we offer. These include making better use of the employment opportunities provided by Disability Confident employers for disabled young people (18-24) and young people with long-term health conditions, and testing the Access to Work adjustments checklist to support conversations with work coaches and employers around disability and adjustment support. Because of this, we want to continue exploring options such as more intensive support and the use of improved communication tools. We will continue this work to learn what more we can do to build trust and encourage people to access employment support.
130. Alongside the new approaches being tested in Health Model Offices[footnote 86], jobcentres have developed other local initiatives. These have been designed to improve the support for disabled people and people with health conditions, as illustrated in the case study below.
Case study: Improving support for autistic people
A number of Jobcentre districts have introduced improvements for autistic people. For example:
- Jobcentres in North London developed and organised Calm and Quiet sessions, including a toolkit for organising these in other jobcentres.
- In Bridgend Disability Employment Advisers DEAs worked in collaboration with Autism Wales to develop an online employability tool for autistic people.
- Jobcentres in Sunderland received a Gold Standard for Autism Acceptance Award in November 2020 in recognition of their work to improve the experience of autistic people.
- Aberdare Jobcentre went through National Autistic Society Wales approved accreditation to become an autism-friendly jobcentre, with all staff undertaking training to achieve accreditation. We will continue to improve staff awareness and skills, physical spaces and ways of working across the Jobcentre Plus network to ensure jobcentres are welcoming and supportive for autistic people.
Providing extra support for our staff
131. At Green Paper events we heard that our staff should continue to improve their understanding of how being disabled or having a health condition can affect the kinds of support and employment a person is able to access. We have been providing extra support to work coaches to ensure they can work with disabled people and people with health conditions in the most effective way.
132. Since 2018 we have delivered training to all our work coaches so they can acquire a better understanding of mental health. In 2019 we expanded on the Disability Employment Adviser (DEA) role and created a new DEA Leader role[footnote 88]. These roles are essential in building the skills and knowledge of work coaches and other colleagues, supporting disabled people and people with health conditions and influencing employer engagement in local communities. They also help staff deliver more personalised support. We are increasing the number of DEAs across Great Britain from 685 to 1000 from April 2021. Every work coach and every jobcentre has access to a DEA.
133. We know that specialist health expertise can help work coaches improve how they work with disabled people and people with health conditions. We recently tested three-way conversations between a disabled person, a work and health professional and their work coach, to see if occupational health expertise could improve the employment support we provide. We are continuing to explore how the expertise and knowledge of work and health professionals can improve the employment support we provide through jobcentres.
Case study: Supporting Will back into work in Scotland
Will is 52 years old and had worked for last 20 years as a head chef, but lost his job due to the coronavirus pandemic. He felt as though he couldn’t return to hospitality due to stress and severe back pain.
Will suffers from mental health issues and also has substance use problems. Will was also concerned about his elderly parents. His dad has cancer and his mum was struggling to cope and was reliant solely on Will which was causing his anxiety. He was overwhelmed by claiming benefits and was referred to a DEA at a jobcentre in Dumfries and Galloway for support. His DEA said:
Through our conversations Will expressed an interest in support and care work, which he had done many years ago. I arranged mental health support through NHS Co-Sync Health Improvement and Support Programme, as well as support for substance use. I also referred him to mPower, a support service for older people and a befriender was put in place for his mum, to have someone else she could talk to apart from Will. This gave him the time to concentrate on his next steps to employment.
I was able to talk Will through an application for a support worker role with Trust Housing. Will was called to interview and we did mock interviews over the phone. The Flexible Support Fund (FSF) helped Will get new interview clothes and he successfully got the job.
Will has now started work, and is loving it.
Consultation question
What further support or information would help work coaches to have more effective conversations with disabled people and people with health conditions?
Personalising Employment Support
134. Since publishing the Improving Lives Green Paper[footnote 90], we have invested in developing the evidence of what works, conducting trials and tests to explore how we can improve the employment support we offer. One size does not fit all. We know that support needs to be tailored to people’s circumstances. Effective support needs to take account of each person’s skills, experience and aspirations for work.
135. Evidence from the trials[footnote 91] [footnote 92], we have conducted and feedback from Green Paper events have also highlighted that employment support works best when:
- It is flexible and tailored to the individual;
- It starts before a person starts work and continues while they are in work;
- It is provided by someone the person trusts, who has the right skills and experience; and
- There is time to build a relationship with the person providing support.
Providing tailored support
136. Our employment support is flexible to cover a range of needs and is available to disabled people and people with health conditions in a variety of settings. It is designed to help people build their confidence, skills and experience through coaching and training, and to take steps towards and into work where people are able. Most of our provision can be accessed by disabled people and people with health conditions on a voluntary basis.
137. Information about the Government’s employment support programmes is provided in Annex B. Central to our offer is the one-to-one support delivered by work coaches and the extra support provided by DEAs through our Jobcentre Plus network. Work coaches also provide access to grants through the Flexible Support Fund which can cover the extra costs of moving into work such as travel costs and clothing. It can also fund additional suitable training or education to help a person move closer to or into sustained work.
138. We provide specialised support to disabled people and people with health conditions through our national employment support programmes. The Work and Health Programme was launched in England and Wales in 2017 and provides up to 15 months of pre-work support tailored to individual needs and further in-work support for up to 6 months. Through jobcentres we also refer people to employment support programmes run by the devolved administrations such as Fair Start Scotland, which is the Scottish Government’s equivalent to the Work and Health Programme.
Case study: Support with looking for work for Marie
Marie joined the Work and Health Programme for support looking for work on the Isle of Wight. Marie has a sight impairment and had been out of work for many years, so her confidence had dropped. Marie’s sight impairment made it difficult to job search and find the best employer for her. Marie’s adviser, Louise, helped Marie to explore job roles that she could do and the transferable skills that she had and supported her to apply for vacancies in her local area. Together they focused on what Marie could do rather than what she could not.
From day one of joining the programme Marie relentlessly pursued a job as a support worker and remained focused on achieving this with support from Louise. Marie built her confidence up with sea swimming. With support, Marie has now secured a job with Leonard Cheshire. The opportunity to learn, develop and grow in this role is really important to Marie.
139. For people with complex barriers who need more intensive, personalised support, we introduced the Intensive Personalised Employment Support (IPES) programme in 2019 in England and Wales. We are increasing places on IPES. This will help ensure that more disabled people and people with health conditions will be able to rapidly access appropriate, tailored support.
Case study: Personalised support for Ryan
Ryan has said, ‘I left college three years ago, and did a bit of volunteering and worked at a local supermarket for a short time, and was unemployed for about two years. My work coach Paul pointed me to this programme and said that the IPES programme will help find work for me. I suffer from social anxiety and depression and this programme helped me overcome this. I listened to Suky [an IPES Key Worker & Employment Engagement Consultant] and she helped find the placement for Tesco and gave me advice on the application forms and helped me complete them, gave me interview prep and guidance, helped support me with travel. This programme has helped with alternative means of work that I would not have looked at otherwise. This is no longer a placement, as Tesco has decided to offer temporary contracts instead of work experience.’
Ryan was successful in securing a temporary contract working for Tesco.
140. Support that is led and delivered locally can be effective in considering people’s needs in the context of the local labour market. Both jobcentres and our national programmes can help people identify and access other locally available support.
141. To make sure that the support we provide is as effective as possible, our current national programmes build on learning from previous programmes and the existing evidence base about what works. Robust evaluation is built into all of these programmes so that we can monitor their impact on outcomes as support is delivered.
142. We want to make sure these programmes are always developing and improving, taking account of evidence as it emerges. In particular, we want to explore how providing people who have more complex needs with intensive periods of focused support can help them move into work.
143. We want to provide more support in local services that disabled people and people with health conditions trust and use regularly. In addition, we want to continue to build on the experience of local providers, including the voluntary sector.
Consultation questions
- What has been your experience of receiving employment support? What was good about the support? Are there further improvements that could be made?
- How can we make the most of the knowledge and expertise of local organisations to support disabled people and people with health conditions into employment?
Providing support in health settings and other local support
144. We know that good work and good health are related[footnote 95]. Because of this, we want to continue to embed employment support within health services to provide more integrated and holistic support. Since 2015, working with the Department of Health and Social Care in England we have jointly invested in employment support in health settings which join up local support for people who are in and out of work. Initiatives that combine work and health services include:
- Employment Advice in NHS England’s Improving Access to Psychological Therapies (IAPT) service. This provides evidence-based psychological therapies to people with anxiety and depression. We have tripled the number of employment advisers within IAPT and currently fund these directly in approximately 40% of IAPT services across England. Therapists and employment advisers work together to consider ways to improve mental health, support people to remain in work while receiving treatment, get back to work if off sick or to find work, if out of work. More than half of the people using this service are in work.
- Individual Placement and Support (IPS). This is an evidence-based intervention used in the NHS to support people with severe mental health problems, to provide intensive support to place people with common mental and physical health conditions, alcohol and/or drug dependence in jobs and support them to stay there. We are continuing to fund IPS in our existing trial areas in England during 2021/22[footnote 96]. An important aim of the service, alongside helping people back into work, is to prevent ill health-related job loss. We have also been working with the Welsh Government and Betsi Cadwaladr University Health Board to test the integration of IPS employment support for people with common mental health conditions into the Welsh health system.
- For autistic people, people with a learning disability and people with severe mental health conditions, we also tested Local Supported Employment (LSE) in partnership with nine local authorities. LSE provides intensive one-to-one support to help people enter and stay in work. We will look to expand on LSE and work with people who access local authority social care to help them access Jobcentre Plus support.
145. Beyond central government a range of other organisations provide employment support for disabled people and people with health conditions. These include charities and social enterprises which can provide specialist services for people with different health conditions and disabilities; statutory services in England (such as the NHS); and services funded by the devolved administrations and local authorities.
146. Examples of employment support available for disabled people and people with health conditions include:
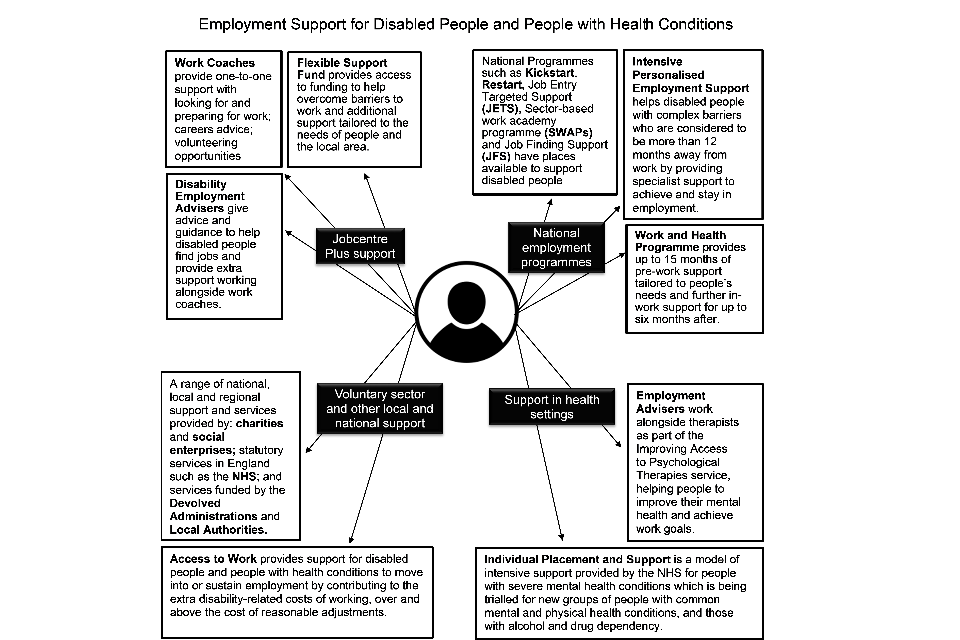
Jobcentre Plus Support
- Work Coaches provide one-to-one support with looking for and preparing for work, careers advice and volunteering opportunities.
- Flexible Support Fund provides access to funding to help overcome barriers to work and additional support tailored to the needs of people and the local area.
- Disability Employment Advisers give advice and guidance to help disabled people find jobs and provide extra support working alongside work coaches.
National Employment Programmes
- Work and Health Programme provides up to 15 months of pre-work support tailored to people’s needs and further in-work support for up to six months after.
- Intensive Personalised Employment Support helps disabled people with complex barriers who are considered to be more than 12 months away from work by providing specialist support to achieve and stay in employment.
- National Programmes such as Kickstart, Restart, Job Entry Targeted Support, Sector-based work academy programme (SWAP) and Job Finding Support have places available to support disabled people.
Support in health settings
- Employment Advisers work alongside therapists as part of the Improving Access to Psychological Therapies (IAPT) service, helping people to improve their mental health and achieve work goals.
- Individual Placement and Support is a model of intensive support provided by the NHS for people with severe mental health conditions which is being trialled for new groups of people with common mental and physical health conditions, and those with alcohol and drug dependency.
Voluntary sector and other local and national support
- A range of national, local and regional support and services provided by: charities and social enterprises; statutory services in England such as the NHS; and services funded by the devolved administrations and local authorities.
- Access to Work provides support for disabled people and people with health conditions to move into or sustain employment by contributing to the extra disability-related costs of working, over and above the cost of reasonable adjustments.
Case study: Support received by Gordon for anxiety and depression through the Improving Access to Psychological Therapies (IAPT) service
I was referred to the employment advice service as part of my treatment for anxiety and anxiety-related depression. Through counselling I have identified that a large majority of my “triggers” for anxiety are work-related. My referral took place after a significant restructure in my workplace and the process of being assessed for redundancy. I had a huge fear of becoming unemployed following my experience of a previous period out of work and the negative impact it had on my wellbeing.
I am pleased to say that I have secured a new role with my employer. The help I received from the IAPT employment adviser was hugely important and helped to coach me in answering interview questions for my new role without triggering my anxiety. I cannot overstate the power of being able to discuss mental health issues in the workplace honestly and openly with an adviser during a process like the one I have just been through; it has made a real difference to me.
Consultation question
What more could we do to work with other organisations and service providers, local authorities, health systems and the devolved administrations to provide employment support in health settings and join up local support?
Encouraging people in the Support Group or with LCWRA to take up support
144. We know that for many people claiming health and disability benefits, such as people in the ESA Support Group and people claiming UC with limited capability for work and work-related activity (LCWRA), work may not be a realistic option immediately because of the impact of their health condition. However, our research with people in these groups showed that one in five people (20%) wanted to work and thought they would be able to work at some point in the future, if the right job and the right support were available[footnote 98].
145. Employment support is available for people who are further away from work via jobcentres, our national programmes and programmes run by the devolved administrations. For people in the ESA Support Group and people claiming UC with LCWRA, participation in employment support is entirely voluntary. In practice, however, very few of these people take up our voluntary employment support and few move into work[footnote 99].
146. We know that being out of work has a negative impact on people’s health and wellbeing[footnote 100]. Recent forecasts[footnote 101] predict an increase in the number of people claiming working-age health and disability benefits. Many people who fall out of work because of a health condition could work in a new role if they had the right support, including healthcare and adjustments. We want to do everything we can to ensure people, including people in the ESA Support Group and people with LCWRA, are able to access the right employment support to take advantage of opportunities.
147. In Chapters 4 and 5 we will consider changes that could be made to assessments and to the benefits system that could better support and encourage disabled people and people with health conditions to start, stay and succeed in employment. We want to make changes so that, instead of focusing on the negative impact of a health condition or disability on a person’s ability to work, we focus more on what people can or could do.
148. In 2020[footnote 102] the Chancellor announced that the UK Shared Prosperity Fund (UKSPF) will help to create opportunity across the UK for people and places. The UKSPF seeks to support people who are furthest away from work, such as people in the LCWRA or ESA Support Group, to move towards or into employment.
149. We want to improve our employment support for people who are further away from work, building on the evidence we have gathered, with further tests[footnote 103]. We want to hear what disabled people and people with health conditions would like this support to include and how we can improve take-up.
Consultation question
What can we offer that would encourage people in the Support Group or LCWRA to take up our employment support?
Exploring digital employment support
150. At Green Paper events some people told us that interacting digitally, for example via video call, was a useful communication method. We also heard that, for some disabled people and people with health conditions, being able to access support remotely could work better for them. During the coronavirus pandemic, our work coaches have made greater use of digital methods such as the UC online journal and provided support via telephone rather than face-to-face.
151. However, we also know that some people do not have access to digital services or may struggle to use these. We want to learn from the way we have provided employment support during the pandemic and explore different ways to provide employment support. Where digital communication, conducted online, via video call or via telephone, does work for people, we have an opportunity to make our services more accessible. Therefore, we want to consider how employment support could be offered as part of a mixed offer combining digital and face-to-face options and explore how effective this support is.
Consultation questions
- Would you be happy to access employment support digitally? Please tell us why/why not.
- What should we consider when developing a digital support offer for disabled people and people with health conditions?
Supporting young disabled people into employment
152. We understand that moving into work can be more difficult for young disabled people and people with health conditions than for other young people. In 2020 we introduced the Kickstart Scheme[footnote 104], which will provide hundreds of thousands of young people with 6-month work placements with a local employer, funded by the Government. The Kickstart Scheme is available to young people between 16 and 24 years of age, including young disabled people and people with health conditions on UC.
153. Moving into work can be a particular challenge for young people with a learning disability. Supported internships give young people with a Education, Health and Care plans the opportunity to learn valuable skills in the workplace to help prepare for paid employment. We are committed to working with the Department for Education to make sure more young people can get support to move from education into work, including through supported internships.
154. The cross-government Special Educational Needs and Disabilities (SEND) Review, led by the Department for Education, is will consider how to successfully support young disabled people to move from school or college into work, if they are able.
Case study: Health, Wellbeing and Motivation in Wales
Samantha and Lawrence are both Disability Employment Advisors. Through a survey of people claiming benefits and discussions with work coaches, Samantha and Lawrence identified that there was an increase in the amount of 18-24 year olds suffering with anxiety and depression linked to the isolation caused by the pandemic.
They decided that people claiming benefits in this age group needed more support to assist them back into work and put together a business case to request extra support drawing on funding from the Flexible Support Fund.
This support was to be delivered virtually via Zoom and would include 12 group sessions. These sessions covered different topics such as managing worry and anxiety, interview skills, workplace behaviours and positivity.
As well as the 12 group Zoom sessions the young people attending had the opportunity to have three individual Zoom calls to talk about individual goals and three months of informal Zoom coffee and connect meeting so participants could continue to support each other.
This support was contracted out to local providers through the Flexible Support Fund and has been used in nine jobcentres across South Wales.
The programme has been received well by young people and has helped many rebuild their confidence when moving towards work.
Consultation question
How can we better support young disabled people who are moving out of education to find appropriate work?
Summary
155. Employment can have a positive impact on many people’s lives, so we want to do more to help disabled people and people with health conditions to start, stay and succeed in appropriate work, wherever possible. To be truly effective, we know a range of support is required, from early intervention to stop people falling out of work in the first place to effective back-to-work support when people do. In addition, employers have a critical role to play in creating inclusive workplaces where people can thrive.
156. Because we know health and employment are related, we want to do more to join up employment support with health services. Disabilities and health conditions affect people in different ways, so it is also clear that support needs to be personalised. We know that support has to be trusted and provided in settings where people feel comfortable taking it up. That is why we want to look at a range of options from continuing to make jobcentres more welcoming to asking what more can be done to encourage people in the ESA Support Group and with LCWRA to take up voluntary employment support. We want to hear how we can improve the support on offer for disabled people and people with health conditions.
Chapter 3: Improving our Current Services
Chapter Summary
Most people claiming health and disability benefits have a positive experience. Where this is not the case we want to hear how to do better. In this chapter we will consult on changes to key aspects of our current services. These are changes that can be implemented in the short-term. This chapter considers how we can:
- Improve the current system of assessments, such as through exploring different ways to conduct assessments and reducing unnecessary assessments;
- Improve our decisions, including by making sure that evidence is available earlier in the decision-making process;
- Better support people moving between child and adult benefits; and
- Provide improved support for people with serious health conditions, including people nearing the end of their lives.
Introduction
157. Research tells us most people are content with our services. 75% of people claiming ESA, 74% of people claiming PIP and 79% of people claiming UC[footnote 107] say they are ‘satisfied’ or ‘very satisfied’ with their overall experience[footnote 108]. However, we also know that a sizeable minority of people are not content. For example, 9% of PIP decisions[footnote 109] have been appealed through a tribunal. We want to ensure more people have a positive experience.
158. We are continually aiming to provide better services. We carry out research with the people who use our services and regularly request their feedback. This helps us identify and understand which issues to solve. We also monitor the impact of the changes we make, so that we can continue to make improvements.
159. We have also worked to rapidly adapt our services to respond to the coronavirus pandemic. In particular, we have made changes to the way that we conduct assessments. We want to learn from the work we have done, where we can, to offer improved services that will provide better support. We also need to consider how improvements affect public spending on benefits, to ensure our support for disabled people and people with health conditions continues to be affordable in the future.
Feedback from Green Paper events: improving our services
160. At Green Paper events, and through research[footnote 110], people told us which aspects of our services they thought needed to improve. People said that assessment reports were not always accurate and that this could lead to poor decisions being made. Some people found our application and assessment processes difficult and stressful. People sometimes had to provide the same information during the assessment process more than once. People felt Work Capability Assessments (WCAs) and PIP assessments were repetitive. People wanted more say in where their assessments took place. People felt repeat assessments were unnecessary where they had a condition that would not improve.
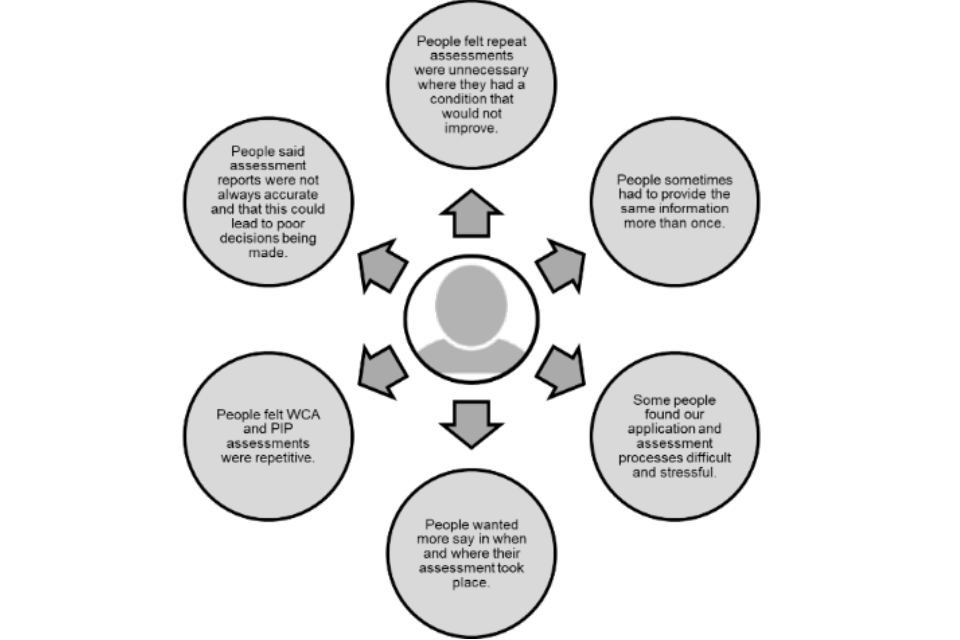
161. The lived experience of disabled people and people with health conditions is at the heart of our plans to make improvements. Throughout this chapter, we will seek views on what more we need to do to address the points that people have raised.
Improving Assessments
162. We use ‘functional assessments’ to help us determine entitlement for health and disability benefits. A functional assessment is one that considers the impact of a health condition on a person’s ability to carry out activities, rather than just the health condition itself.
163. The Department currently uses two separate functional assessments on health and disability benefits. These are the PIP assessment and the WCA. The WCA helps determine eligibility for ESA as well as whether someone has LCW or LCWRA on UC. Both the PIP assessment and the WCA use assessment criteria to assess a person’s ability to carry out activities and determine the appropriate level of support.
164. We have already made positive changes to assessments[footnote 111] and we know that many people now have a good assessment experience[footnote 112]. However, feedback from Green Paper events, and other evidence[footnote 113], suggests that some people continue to find assessments difficult and stressful. There are also a high number of tribunal appeals lodged following an assessment[footnote 114]. We want to do our best to ensure that the quality of assessments is always improving.
What we have learned about current assessments
165. Under the current system, nearly half the people claiming health and disability benefits claim ESA or UC with a health condition as well as PIP or, to a lesser extent, DLA[footnote 115]. In 2019, we announced[footnote 116] that we would test whether using one single assessment to combine the separate WCA and PIP assessments could improve the experience of people who claim both PIP and ESA/UC.
166. Our work has shown that even though many people have both a WCA and a PIP assessment, few people would benefit from a single assessment under the current system. One reason for this is that most people make their initial claims for the different benefits at different times. In 2016/17 only 4% of initial WCA and PIP assessments took place within 3 months of a claim for the other benefit[footnote 117]. Each benefit also has different rules about when the level of payment needs to be reviewed. In 2017/18 only 1% of PIP Award Reviews and ESA WCA reassessments occurred within 3 months of each other[footnote 118]. This means that the timings for the different types of assessments do not align.
167. Another reason why it would be difficult to combine the WCA and PIP assessments into one single assessment is that they are assessing different ways in which people’s disabilities and health conditions affect them. The PIP assessment tests whether a person is likely to incur extra costs, while the WCA tests the impact of a person’s condition on their ability to work. To test both these things in one single assessment under the current system would mean that the single assessment would take longer than an individual WCA or PIP assessment.
168. Because of these factors, we found that, under the current benefit structure, introducing a single assessment combining both the WCA and PIP assessments could make the assessment process longer and more complex. As a result, we do not believe that combining both assessments into a single assessment would improve people’s experience under the existing system[footnote 119]. We will however consider whether changes could be made to the structure of these benefits, which could allow for a single assessment, in Chapter 5.
169. During the coronavirus pandemic we made a number of temporary changes to our services, including the introduction of telephone assessments. These changes were necessary to keep people safe. Although these changes were not intended to be permanent, many people have welcomed them. Our work on the single assessment and the temporary changes made during the coronavirus pandemic have led us to identify ways to improve assessments now and in the future.
Introducing a new integrated health assessment service
170. In March 2019, we announced plans to develop an integrated health assessment service through our Health Transformation Programme[footnote 120]. This integrated service is different from the work on the single assessment. The integrated service will bring the assessments for PIP and UC/ESA onto a single, digital system. This will help make our processes more effective and efficient and improve people’s experience. For example, where people are willing to provide consent, the new system will allow us to share medical evidence more easily. This will help reduce the need for people to provide the same information more than once.
171. We will develop this new service on a small scale to begin with in a small area called the Departmental Transformation Area (DTA). The DTA will be a safe environment to test, adapt and learn from new ideas and processes. This approach will allow us to continually improve the new service and systems in a controlled way. We then plan to roll out improvements gradually at a greater scale, including with assessment providers. The first DTA location is in London and was launched on 21 April 2021.
172. The full scale of what the Health Transformation Programme can achieve is still developing. It will support the delivery of many of the improvements we have outlined in this Green Paper. For example, for some time, people going through a WCA have been able to have their face-to-face assessment audio-recorded. The Programme has now developed an approach to ensure PIP face-to-face assessments can also be audio-recorded, where a request is made in advance. In addition, we have started to offer audio-recording of telephone assessments for ESA, UC and PIP. We believe that audio-recording assessments will help improve trust in our decisions. Action is also being taken to test video assessments through the integrated assessment service, as set out in the next section.
Exploring different ways to conduct assessments
173. Before the coronavirus pandemic, where the necessary evidence was not available, a face-to-face assessment was usually carried out to gather the evidence needed. To develop our services and improve people’s experience we have been exploring different ways to conduct assessments.
Making greater use of triaging
173. In some cases[footnote 121], people are able to provide sufficient evidence to allow a paper-based assessment to be carried out instead of a face-to-face assessment. To make more decisions quickly and simply, and reduce the need for face-to-face assessments, we want to maximise the use of paper-based assessments and make greater use of triaging. We would like to explore whether we can make decisions in straightforward cases without the need for an assessment with and recommendation from a healthcare professional. Where there are only small amounts of missing evidence, we want to explore whether assessors can make robust recommendations by taking steps to gather that evidence, for example through a telephone call, instead of needing to conduct a face-to-face assessment. We want to test how to triage claims, so that people only have to go through face-to-face assessments where these are absolutely necessary.
Using telephone and video assessments
173. During the coronavirus pandemic, we have had to rapidly adapt how we deliver our services. We have not been able to conduct face-to-face assessments during most of this time. Therefore, as a temporary measure, we have been carrying out assessments by telephone. The feedback on telephone assessments has so far been positive[footnote 122]. In a recent survey, the majority of people who had a telephone assessment for PIP or for their WCA were ‘satisfied’ or ‘very satisfied’[footnote 123] [footnote 124].
175. We want to fully evaluate telephone assessments. It is important that people continue to receive consistent and accurate decisions whatever kind of assessment they go through.
176. We also want to explore whether we could offer assessments by video call. In the same survey, people were asked how comfortable they would feel taking part in a video assessment. Just over half (56%) of people said they would feel ‘comfortable’ or ‘very comfortable’ having their WCA or PIP assessment by video call.
177. Over 750 people have gone through a video assessment as part of a test which ran until the end of March 2021. Subject to an evaluation, we are now progressing plans to increase the number of video assessments as part of a pilot.
178. We would like to hear your views about the different ways to provide assessments. This will help shape our future health assessment service.
Consultation questions
- During the coronavirus pandemic we introduced assessments by telephone and video call as a temporary measure. In your view, in future, what mixture of methods should we use to conduct assessments?
- How could we improve telephone and video assessments, including making sure they are as accurate as possible?
Reducing repeat assessments
179. The impact of a disability or health condition can change over time. We conduct repeat assessments[footnote 125] to understand whether and how this impact has changed. Repeat assessments allow us to make sure people continue to receive the correct amount of financial support.
180. Reducing the number of repeat assessments disabled people must go through where a significant change in condition is unlikely is a key priority for Government[footnote 126]. At Green Paper events, disabled people have also told us that we should do more to reduce repeat assessments. This is illustrated in the case study below.
Case study: The need to reduce repeat assessments where a condition is unlikely to change
Gulnar has several health problems including cancer and heart conditions. She was asked to complete a review form as her previous PIP award was coming to an end.
Due to her conditions, Gulnar spends a lot of time at medical appointments. She also finds it difficult to get to an assessment centre. As a result, she was very unhappy about the prospect of having to go to a repeat PIP assessment. Her medical consultants were able to provide evidence that her condition was not going to improve. She felt this should have been sufficient for her PIP award to be renewed.
Gulnar was later awarded PIP following an assessment.
181. We have already made good progress in reducing repeat assessments. For example, through the Severe Conditions criteria, we have stopped repeat assessments on ESA/UC for people with the most severe and lifelong conditions. [footnote 128]
182. We have also made changes to help reduce the frequency of repeat assessments some people need to go through on PIP. We have ensured that people who receive the highest level of support whose needs will not improve, and most people over State Pension Age, receive an ongoing award of PIP with a ‘light touch’ review at the 10-year point. A review can take place sooner if a person’s needs change.
183. The Government’s 2019 manifesto set out to reduce the number of repeat assessments faced by disabled people, whose condition is unlikely to change. We have decided that better triaging and testing the Severe Disability Group (covered later in this chapter) will deliver this commitment more effectively than introducing a minimum award duration in PIP.
184. Going further, we would like to hear what more we could do to make sure that people do not have unnecessary repeat assessments where the impact of their condition is unlikely to change significantly.
Consultation question
What more could we do to reduce repeat assessments, where someone has a condition that is unlikely to change?
Improving Decision Making
185. The assessment process starts when a person makes a claim. This involves the person applying for the benefit and providing evidence to support their claim. Next there is an assessment by a work and health expert known as the assessor[footnote 129]. At this stage the assessor will produce a report based on a face-to-face assessment or a paper based review where there is enough evidence.
186. There will then be a decision, where a decision maker will consider the report and other evidence to make the decision. The person will then be informed of the decision. In order to improve this stage, we are implementing a new approach to give decision makers more time to gather evidence. We are also looking at how we can improve the quality of evidence provided.
187. If a person disagrees with the decision, they can ask for it to be looked at again during a process called a mandatory reconsideration (MR). To improve this stage, we have implemented the same approach to give decision-makers more time to gather evidence, which has seen the volume of appeals reduce.
188. The last stage is an appeal. Following an MR where the person still disagrees with their decision they can appeal to HM Courts and Tribunals Service (HMCTS). To improve this stage, we can change the decision based on any new evidence. If the person accepts the new decision this will mean there is no need to go through an appeal.
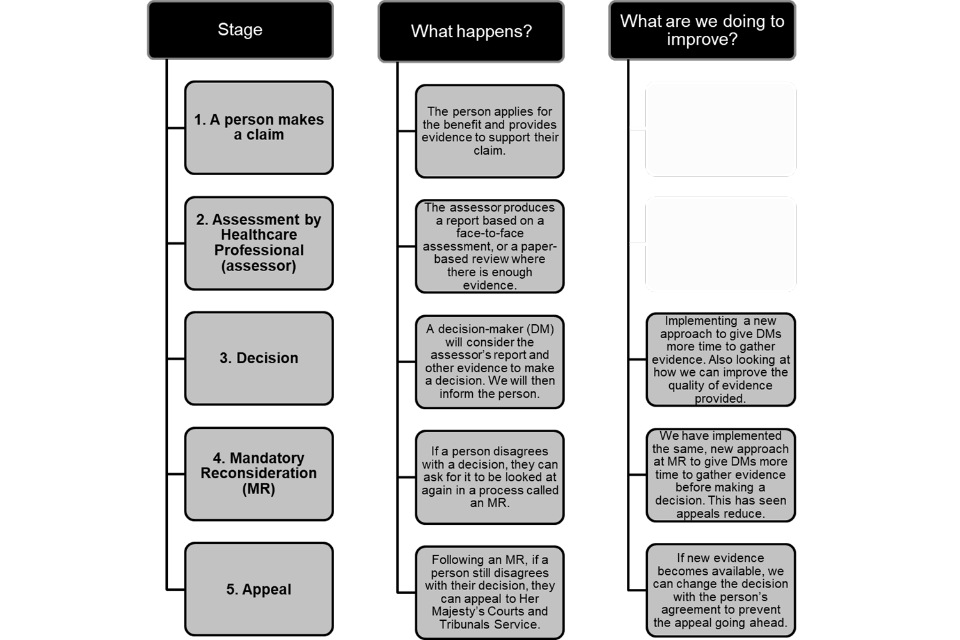
189. We know from Green Paper events that not everyone feels they receive the right decision after a health assessment. This can lead to a long and difficult process including an appeal to a tribunal. We have worked to improve the way we make decisions, but want to do more to improve the experience of disabled people and people with health conditions and, in doing so, build their trust.
190. MR is a key part of our decision-making process. If someone disagrees with a benefit decision, they have a legal right to request an MR. This means a different team of decision-makers will look at the decision again to see whether it should be changed. MR gives people an early opportunity to challenge our decisions. In this way, the MR process means that fewer decisions go to appeal.
The impact of holistic decision making
191. As part of our ongoing learning to understand how to improve decision making and reduce appeals, we gathered insights from HMCTS, DWP staff, disabled people, people with health conditions and disabled people’s organisations. This suggested that better quality evidence needs to be gathered earlier in the decision-making process.
192. To address this, in 2019 we started to adopt a holistic approach to decision-making. This was initially introduced on PIP at the MR stage. Holistic decision making allows our staff to take extra time, if needed, to make a decision on benefit entitlement following a health assessment. This extra time has often allowed more evidence to be provided to support the decision-making process. It has also allowed more time for our staff to listen to people claiming benefits and to help people understand the reasons why a decision has been made.
193. Since we introduced this new approach, the percentage of PIP decisions that we change at the MR stage has nearly doubled[footnote 130]. There has also been a decrease in the percentage of appeals lodged following an MR[footnote 131]. This is better for disabled people and people with health conditions, who often find the appeal process difficult and stressful. It is also more affordable for the Department because it means less money is spent on appeals.
194. Holistic decision making has since been introduced at MR for ESA and UC and we are now also using it to make the first decision about entitlement following a health assessment on ESA, PIP and UC. We hope this will mean that people are less likely to need to use MRs and appeals. We want to continue to improve our decision making and would like to hear what further changes we could make.
Case study: A holistic decision-making approach to Mandatory Reconsiderations (MRs)
One person who has benefited from our holistic decision-making approach is a person who has not worked for many years due to caring for her elderly parents. She has not claimed ESA before and was undertaking her first Work Capability Assessment (WCA). At assessment, she said that she could cope well with daily activities. The assessment report recommended that she was capable of working.
However, the work coach and case manager did not agree with this finding. They considered the person to have long-standing mental health issues for which she was not getting support and that she lacked insight into her ability to cope. They flagged this to the decision-maker (DM). When the DM made a decision assurance call the person revealed that she had been prompted to seek further help for her mental health recently by some friends and had been given a number for social services as she was not coping. Her mental state appeared very unusual on the call and she was very anxious, in contrast to the initial assessment. Given the deterioration in her mental state the DM felt that any further pressure, such as carrying out work-related activity, could potentially cause a further deterioration in her mental state.
Based on all the evidence available, the DM concluded that there would be a substantial risk to the person’s mental or physical health if she were found not to have limited capability for work and work-related activity. As a result, she was awarded ESA and placed in the Support Group. The holistic approach to decision-making led to the right outcome.
Improving the appeal lapsing process
195. We have also continued to improve the process where people appeal against our decisions. If new evidence or information becomes available after an appeal has been lodged, but before it is heard at a tribunal, we are able to change a decision and increase the award where appropriate. This is known as lapsing an appeal. We explore lapsing an appeal where we can so that people do not need to wait to go through the stress of a tribunal hearing.
196. In cases where the new decision does not give people the award that they had hoped for, but still gives people more than the previous decision, we will speak to the person or their representative[footnote 133] before changing the decision. If the person accepts the new decision the appeal will stop. It is still possible to appeal the new decision after it has been accepted but the appeal waiting time will start again[footnote 134]. Alternatively, if people are unhappy with the new decision when we explain it, we do not change the decision and the appeal continues.
197. We have developed new guidance for staff on lapsing appeals. We are also working with charities to improve how we communicate new decisions to people so that people are fully aware of how the new decision was reached and what the appeal rights are. We would like to hear further suggestions about how to improve appeal lapsing.
Consultation questions
- Decisions can be changed after an appeal has been lodged but before a tribunal hearing takes place. How can we improve the way we communicate a new decision in this situation?
- What other changes could we make to improve decision making?
Supporting People Moving between Child and Adult Benefits
198. At Green Paper events, and through other forums, people have told us that moving between child and adult benefits and services can be difficult. One example of this is where young people claiming Child DLA are invited to apply for PIP at the age of 16.
199. Child DLA and PIP are different benefits with different entitlement rules. This means that a young person who receives Child DLA may not always be entitled to PIP in the same way.
200. If a young person claiming Child DLA decides to apply for PIP, the young person will need to follow the same process and will be treated in the same way as anyone claiming PIP for the first time. This often includes having an assessment.
201. We would like to hear what changes could help improve the experience of young people and their families. For example, we could develop new guidance for the organisations and individuals supporting young people and their families, such as welfare rights organisations.
Consultation question
- How could we improve the experience when people claiming Child DLA are invited to apply for PIP?
Support for People with Serious Health Conditions
Changing the Special Rules for Terminal Illness (SRTI)
202. Currently, where a person is unlikely to live longer than six months, their claim to benefit can be fast-tracked and a face-to-face assessment is not required. The majority of people also receive the highest levels of benefit[footnote 135].
203. We conducted an evaluation[footnote 136] into how the benefits system supports people nearing the end of their lives. We heard views from people directly affected, their families and friends, the organisations supporting them and the healthcare professionals[footnote 137] involved in their care. There was a consensus to change the six-month rule and significant support from healthcare professionals for a 12-month, end of life approach.
204. We will therefore take forward legislation to change the six-month rule so that people who are believed to be in their final year of life will be able to make fast-tracked claims to the benefits system. This will support the delivery of a fair and compassionate system. It will also reflect the approach used by NHS England to identify when people are nearing the end of their lives (with similar approaches across the NHS in other parts of the UK). We believe this change will make accessing the benefits system easier and the rules simpler to understand. We will also consider ways to simplify the application process for people nearing the end of their lives.
205. This change will ensure more people receive vital support faster. Aligning with the existing NHS approach should also make it more straightforward for healthcare professionals to identify people who could access this support through the benefits system. It should make it easier to improve people’s awareness of the support available. These changes will also help improve consistency across services used by people nearing the end of their lives.
Testing a Severe Disability Group (SDG)
206. People who do not come within the special rules for terminal illness may still have severe and lifelong conditions that will not improve. These people are unlikely ever to work again and will always need extra financial support to live independently. Meeting the needs of people with such conditions is extremely important.
207. We want to test a new Severe Disability Group (SDG) so that these people can benefit from a simplified process without ever needing to complete a detailed application form or go through an assessment. This will build on existing successful measures such as the Severe Conditions Criteria[footnote 138] for ESA/UC.
208. The case study below highlights why we want to make changes to the assessment process, so that people with the most severe health conditions and disabilities can claim the benefits they are entitled to through a simpler process.
Case study: Who could the introduction of a Severe Disability Group help?
Ashley has a diagnosis of Motor Neurone Disease. She moved from receiving Disability Living Allowance (DLA) to Personal Independence Payment (PIP). She was very surprised to learn that she would be required to start the process of applying for PIP from the beginning. Motor Neurone Disease is a progressive and degenerative neurological condition that will never improve. Because of the impact of her condition, Ashley had already been assessed as eligible for the highest rates of DLA. Ashley thought that as the Department was already aware of her diagnosis, the transfer from receiving DLA to PIP would be a simple process to ‘rubberstamp’ her eligibility.
However, this was not the case. Ashley was required to fill out lengthy forms and provide extra supporting evidence. This whole process took several months to be completed, and included an assessor visiting Ashley at her home to gather further information to support her claim. Ashley found this extremely stressful. She could not understand the need for the home assessment as supporting documents and evidence had already been provided.
209. We expect that the decision to place someone in the SDG will be based on information from medical professionals. The SDG could apply to people on PIP, ESA and UC.
210. We are working with a group of health and social care professionals to help us develop the criteria for the SDG and identify the evidence that would be required to meet them. We will consult with charities and disabled people’s organisations on the criteria. We will also work directly with disabled people and people with health conditions to develop the service, and test the approach to make sure it delivers the improvements we are seeking. This test will look at whether the SDG achieves its goals while ensuring people receive the right level of benefit. We will consider the test results alongside the responses to this Green Paper when determining whether the policy should be rolled out further.
Summary
211. Most people have a positive experience of claiming benefits. For people who do not have that experience, we are listening to and acting on feedback so that everyone feels supported and able to rely on this Department.
212. We hope the changes that we have already made will mean disabled people and people with health conditions have a better experience of health assessments and feel more able to trust our decisions. We have also sought views on further changes.
213. These improvements are just the beginning. We know that we need to take bolder steps to help people live fully independent lives and to start, stay and succeed in work.
Chapter 4: Re-thinking Future Assessments to Support Better Outcomes
Chapter Summary
The outcome of an assessment can have a huge impact on someone’s life. In this chapter, we explain how we want to go further to make changes to future assessments, so that we can help more people live independent lives and work, where possible. Whereas the last chapter considered short-term changes to assessments to improve people’s experience, this chapter explores:
- Why we want to re-think health assessments, and the feedback and evidence that supports this;
- The objectives and principles for future assessments; and
- Proposals for future assessments.
Introduction
214. In this chapter, we look at the potential for making changes to future health assessments. These are longer-term changes, some of which would require changes to current legislation. We share insights we have gathered from disabled people and people with health conditions. We have also been listening to charities, healthcare professionals, think tanks and academics. This feedback, and evidence from research and analysis, has informed our development of objectives and proposals for future assessments.
215. We consulted on WCA reform in the 2016 Improving Lives Green Paper[footnote 140]. Most people said we should make changes, but there was no agreement on what changes should be made. Since then, as set out in Chapter 3, we have improved assessments and continue to do so. However, we believe that further changes are still needed. We would like to hear your views on what more we should do.
Feedback and Views on Assessments
216. To help us better understand the issues disabled people and people with health conditions face, we have been gathering feedback on assessments. This work has included:
- The creation of an Assessments Policy Forum. The forum is made up of a small number of academics, think tanks and disability charities. It has considered objectives and provided views on proposals for changing assessments. This group met nine times between April 2018 and May 2021.
- Gathering ideas through running specific policy development sessions and Green Paper events. This has allowed us to hear the views of disabled people and disability charities, as well as those of DWP staff and assessors who deliver the current service.
217. Most people have a good assessment experience[footnote 141], but we recognise the need to make improvements to assessments for the minority of people who do not. The case study below demonstrates the fear that some people can feel when going through an assessment, a Mandatory Reconsideration (MR) and an appeal. It illustrates the need for change.
218. At Green Paper events, we heard that:
- People want more flexibility: Some people said that assessments were too rigid. These did not take into consideration how conditions can change over time and often covered things that were not relevant to a person’s condition or circumstances.
- There needs to be more trust and confidence in assessment decisions: Some people felt their responses had not been accurately recorded and that the impact of conditions such as mental illness was not always fully recognised. Some people also said that the WCA was not always the best measure of someone’s capability for work.
Evidence for Making Changes to Assessments
219. Most people go through their PIP and ESA assessments without significant problems, but a sizeable minority do not[footnote 142]. Research shows that people claiming PIP had mixed views about assessments[footnote 143]. People have also asked why the assessment repeats the same questions that are asked in the forms people complete before the assessment[footnote 144].
220. The number of people found to have LCWRA and placed in the ESA Support Group following a WCA has increased over time, and continues to grow[footnote 145]. In November 2020, there were 1.9m people in the ESA Support Group or UC LCWRA. This means that 75% of all people claiming ESA or people on UC with a health condition are in the Support Group or LCWRA group[footnote 146]. As set out in Chapter 2, people in the ESA Support Group can volunteer for employment support, but few do. At Green Paper events and through research, people said this was due to feeling worried about preparing for work. Some people fear that preparing for work will trigger a WCA reassessment or result in a loss of benefits[footnote 147].
221. Research with people in the Support Group (and the UC equivalent group, the LCWRA) found that 20% of the people in these groups thought they could work in the future[footnote 148]. We want to change the current assessment process so it better identifies what people can do, rather than focusing on the limitations of disability or health condition.
222. People do not always trust the outcome of their health assessment. For example, between the introduction of PIP in 2013 and September 2020, 9% of people who received an initial PIP decision[footnote 149] lodged an appeal at a tribunal. To improve the experience of disabled people and people with health conditions, we want to explore making changes to assessments so that people have more confidence in our decisions and are less likely to feel the need to appeal a decision made after an assessment.
Our objectives for future assessments
223. We have developed a set of objectives for assessment reform with input from the Assessments Policy Forum group. We believe that future assessments should:
- Build trust through transparency and consistency: It is important that we deliver assessments that people can trust. Assessments must lead to the right decisions and outcomes. Decisions and outcomes must also be communicated in a way that is supportive and easy for people to understand.
- Form part of a personalised service: We want to make the best use of available evidence to understand a person’s needs. We want to make sure assessments are responsive to changing health conditions.
- Offer an improved experience: We want to do more to stop people having to repeatedly provide information or attend unnecessary repeat assessments.
- Improve employment and independent living outcomes: We want to encourage people to take up personalised support where possible. An improved assessment process should also help us make better decisions about what a person must do in return for benefit if required.
224. We also want to ensure that assessments provide value for money. We want to improve value for money by simplifying processes and delivering more efficient and effective services to ensure people receive their correct entitlement and know when to report changes. These services will target support at the people who need it most.
Separating the assessments for financial and employment support
225. In the 2016 Improving Lives Green Paper, we consulted on making changes to the WCA. We asked whether we should separate the assessment for financial support from the assessment for employment support. Most people who responded to that consultation agreed that separating these two elements was a good idea, but there was no agreement on how this should be done.
226. We believe that there are two clear advantages of separating these two elements:
- People can feel more confident about taking part in employment support knowing it will not affect the amount of benefit paid.
- Deciding who should receive additional payments due to the impact of a health condition or disability, and how much these payments should be, is very different to deciding what employment support a person needs. Trying to do both through one assessment is challenging.
227. In responses to the Improving Lives Green Paper, some people told us they were also concerned about how decisions would be made and whether work coaches would be able to set the right work search and work preparation requirements. We have used this feedback to help to develop our proposals.
A New Approach: Proposals for Future Assessments
228. Our proposals for future assessments aim to build greater trust and improve the quality of decision making. In Chapter 3, we explained that we want to explore developing criteria for a new Severe Disability Group (SDG) to identify people with the most severe health conditions and disabilities who could benefit from a simplified process and may not need to have an assessment to determine their eligibility for benefits. In this section we want to focus on two key questions:
- How can we improve the way that we assess entitlement for financial support? This includes exploring changes to the assessment criteria, how we use evidence and the role of assessors.
- How can we better decide what employment and health support a person receives, including what a person receiving UC or ESA must do to look for or prepare for work?
Assessment to determine financial support
229. We want the assessment process for financial support to be as simple as possible. This should help ensure that people can clearly understand the reason for and approach to an assessment, what evidence to provide and the outcome received.
230. Currently, ESA/UC and PIP use what we call ‘functional assessments’. A functional assessment is one which considers the needs that a person has that arise from their health condition or disability, rather than the health condition or disability itself.
231. The aim is to look at how health conditions and disabilities affect a person’s ability to work (for ESA/UC) or live independently (for PIP). Considering the needs arising from a person’s health condition or disability is a key feature of assessments. However, we have heard at Green Paper and other events that the criteria used in functional assessments may not always fully reflect how a disability or health condition impacts on daily living or finding work.
232. People need to be able to explain or provide evidence of how their condition affects them, not just at the time of the assessment, but from one day to another. This will help make sure we can be confident that we are giving support to the people who need it most.
233. Considering the impact of a person’s condition or disability on their ability to work or live independently is important. We believe that this should continue to be a part of assessments in the future.
Making changes to the assessment criteria
234. A lot has changed since the WCA and PIP assessment criteria were originally developed. At Green Paper events, people have also told us that the descriptors and activities used in the WCA[footnote 150] and PIP[footnote 151] assessments may not always capture certain kinds of health conditions or disabilities as well as they do others. We therefore want to consider whether any changes should be made to the WCA and PIP assessment criteria.
235. Both the WCA and the PIP assessments use descriptors to assess a person’s ability to carry out activities. Descriptors list a range of actions within each activity area which people may be able to perform with or without assistance. The activities and the descriptors together make up the assessment criteria.
236. We recognise the importance of ensuring that the activities equally capture the impact of all health conditions and disabilities on people’s daily lives, including fluctuating conditions. We also want to ensure that the definitions and descriptors used within the assessment criteria are clear.
237. Since the assessment criteria were introduced, some of the activities referred to may have become less of a barrier to independent living and employment. For example, new assistive technology has become available.
238. In relation to the WCA, we have seen a reduction in the disability employment gap between 2014 and 2019 (although there has been a small increase from 2020) [footnote 152]. The coronavirus pandemic has resulted in more people working flexibly, including working from home. This may mean that barriers to work have reduced.
239. We want our current assessment service to be more efficient and straightforward, so we would need to make any changes in a way that would not complicate or lengthen the assessment process. Our central aim is to ensure that assessments are fair and that people receive the level of benefit to which they are entitled.
Consultation questions
- Is there anything about the current PIP activities and descriptors that should be changed? (Yes/No/Don’t know)
- If yes, what changes to the PIP activities and descriptors should we consider?
- Is there anything about the current WCA activities and descriptors that should be changed? (Yes/No/Don’t know)
- If yes, what changes to the WCA activities and descriptors should we consider?
When responding to these questions, please consider the following:
- What the best way to capture the impacts of health conditions that fluctuate or vary might be;
- How we could ensure the activities and descriptors capture the impact of all health conditions and disabilities fairly;
- How we could simplify the assessment criteria; and
- Any possible PIP or WCA activities that are no longer a barrier or that are less of a barrier to employment or independent living, due to modern working practices and advances in assistive technology.
Supporting evidence for assessments
The role of evidence in WCA and PIP assessments
240. Access to the right evidence at the right time is key to each stage of the assessment process. The right evidence enables robust decisions to be made first time round, increasing people’s confidence in their decisions and reducing the number of challenges made through the Mandatory Reconsideration (MR) and appeal processes. However, collecting the right evidence can be difficult. Assessments are used to evaluate the needs arising from a health condition or disability, but there is currently no standard evidence source that can be used to confirm these needs apart from the assessment itself.
241. Most of the medical evidence currently gathered allows us to confirm a person’s medical condition. In most cases, this is not enough for us to be able to make a decision without an assessment. Further evidence from other health and social care professionals is helpful (for example from a social worker or a physiotherapist). However, many people do not have interactions with such professionals.
242. The most common form of evidence used for people receiving UC or ESA at the start of their claim is a fit note. This is evidence, usually from a person’s GP, which shows that a person has a health condition which means that the person cannot work or carry out their usual duties.
243. The use of the fit note in the WCA process can be confusing. A person might receive a fit note from their GP stating they are ‘unfit for work’ but then receive a decision from us following their WCA stating that the person is able to look for work. This can happen because the WCA assesses a person’s ability to carry out any form of work based on the specific activities and descriptors in the assessment criteria that are set out in law. GPs are not always familiar with these criteria. Instead, GPs often base their advice on whether a person can perform their current job, taking into consideration their health condition.
244. The case study below highlights the importance of getting the correct medical evidence at the right time and as early in the process as possible. This can help avoid the need for people to go through MR and appeals.
Case study: The challenges of accessing medical evidence
Eldon suffers from chronic depression, anxiety and paranoia. His application for Personal Independence Payment was initially unsuccessful.
Eldon was reluctant to ask the GP for evidence as he finds them unsympathetic. They previously produced a list of Eldon’s conditions and his repeat medications, which was not helpful to him.
Citizens Advice were able to assist Eldon to request further medical evidence, including an assessment that the complex needs team had already carried out, which was important to understand how Eldon’s condition affects his ability to cope with the demands of daily activities. Eldon submitted a claim for appeal with the additional medical evidence, which resulted in a successful appeal of his Personal Independence Payment entitlement.
245. We want to explore which evidence is most useful for making decisions and to understand when the evidence should be collected and from whom.
Consultation questions
- Should we seek evidence from other people, such as other health professionals or support organisations?
- What type of evidence would be most useful for making decisions following a WCA or PIP assessment, and should there be a standard way to collect it?
- How could we make sure the evidence we collect before a WCA or PIP assessment directly relates to a person’s ability to do certain things?
The role of assessors in the process to decide financial support
246. The role of assessors has been highlighted in research[footnote 155] as well as often being mentioned in the feedback we received. At Green Paper events we heard that:
- Some people did not feel the assessor had enough knowledge about certain conditions to be able to accurately assess them;
- Some people felt assessors had not accurately recorded what happened at the assessment; and
- Some people were concerned that their assessor had not always listened to the answers they gave.
247. People have told us they would like specialist assessors appropriate to their condition. There are a number of reasons why this would be difficult. Firstly, because specialists might not be available. Secondly, because many of the people claiming health and disability benefits have more than one condition.
248. Assessors already have access to specialist support so they can obtain advice on assessments if needed. However, we would like to explore whether there are circumstances where it could be helpful to bring in extra expertise to support assessors and decision-makers. We would like to understand whether this would improve outcomes and increase people’s trust and confidence in the decision being made.
Consultation question
How could we improve assessments or the specialist support available to assessors and decision-makers to better understand the impact of a person’s condition on their ability to work or live independently?
Reviewing financial support
249. Many health conditions change over time. We need to check people’s entitlement to make sure it is still appropriate. This might result in a higher or lower award depending on whether the impact of a person’s condition has got better or worse.
250. We need to make sure that we have the right checks in place to ensure we are paying people the right amount of money for their particular circumstances. We want to encourage people to keep their claims up to date. This will help minimise the risk of paying people too much or too little in benefits.
251. We have heard that repeat assessments can cause anxiety for people claiming health and disability benefits. In Chapter 3, we considered ways to reduce the number of repeat assessments a person must go through. In this chapter we want to explore whether there are other ways to review financial support that would be less stressful and enable people to provide a picture of how their condition may have changed over time.
252. We want to explore using a Health Impact Record (HIR) to do this so that people can record the impact of their condition throughout their claim, particularly where there has been a change. This might give someone a way to provide an ongoing self-assessment of their condition(s) and support needs. Other people in a person’s support network and potentially health professionals could contribute to the HIR as well as the person making the claim.
Consultation question
How can we make it easier for people to inform us if their condition or circumstances have changed so that a review of entitlement can be carried out at the right time?
Testing an employment and health discussion
253. We have explained that the separation of the assessment for financial support from a consideration of employment and other support could mean that more people are willing to take up support. This could lead to better employment and independent living outcomes.
254. We would like to explore whether a separate employment and health discussion could help people move closer to or into work if they are able. Work may also be part of the independent living objectives of many people who claim PIP, so this support could be offered to them. This discussion could be led by a work and health expert. This would be a conversation about the impact of a person’s condition on their ability to move towards work. The work and health expert and the person could also agree activities to be carried out to overcome challenges. The discussion would focus on what the person can do, rather than what they cannot. It could explore career goals, workplace support and signposting to other support.
255. We envisage that this discussion would lead to the development of an action plan. This could set out actions that could be shared with future employers or the person’s immediate support network. It could include things like workplace adjustments, where appropriate. It could involve support workers to provide encouragement to act on the positive steps outlined in the plan.
256. As a first step to understanding how an employment and health discussion might work we are exploring whether to test this within the existing system. This test will explore whether it is possible to deliver this discussion effectively and whether it would offer value for money. The following case studies illustrate how access to advice from a specialist healthcare professional can make a positive difference.
Case studies: Support from an Occupational Health Professionals (OHP)
Case study 1
After attending a WCA, Suzanne was asked to meet with an OHP by her Jobcentre Plus work coach. When Suzanne was introduced to Abby, an OHP, she was undergoing a series of tests for possible heart problems or rheumatoid arthritis. Suzanne’s mobility was severely limited and she was struggling with her day-to-day personal care. Suzanne was accompanied by her husband and they were both distressed when they came to see Abby. However, Abby was quickly able to offer Suzanne help and support which improved her daily life.
Abby identified that Suzanne needed assistance from Adult Social Care and so she put them in touch. Within five days, Adult Social Care organised for Suzanne to have a home visit and made adaptations to her home so that she could take care of herself more easily. This included changing the seating to give her more independence. Abby also helped Suzanne contact an organisation which gave her advice about staying in her existing home and helped her contact the council to request a more accessible home.
Suzanne said:
She [Abby] was very informative and her knowledge has made my life much easier. She has made a huge difference.
Case study 2
Annabel received support from an OHP who helped her set goals and move into employment. Annabel began claiming UC after being unemployed for 12 months. She experienced anxiety and depression and was coping with a very difficult home life. Annabel was spending much of her time trying to provide support to her mother who was clinically depressed and alcohol-dependent as well as to her younger brother who had developed a drug addiction. Annabel felt that she was unable to concentrate on herself and on what she needed to do to improve the quality of her own life.
Annabel’s work coach introduced her to an occupational therapist, as Annabel felt that getting a job may be helpful in providing her some stability in her life and improving her self-esteem.
The occupational therapist asked Annabel to complete a mind-mapping exercise where she considered her likes and dislikes and what ideas she had for moving forward. Annabel met with the occupational therapist a second time to discuss the exercise and the occupational therapist then gave her lots of practical advice on courses she was interested in. Together, they set clear goals to help Annabel move forward.
This extra support gave Annabel the confidence to apply to the University of Central Lancashire to do a foundation degree. She also updated her CV and started to apply for jobs. She was soon offered a role in retail and started working 19 hours per week. Annabel informed her work coach that she was very pleased to have a plan in place for the future. She felt positive that she’d been able to turn her life around and was finding the time to fulfil her own ambitions.
Consultation questions
- What could be included in a discussion to develop a more personalised employment and health support plan?
- What skills and experience should the person undertaking an employment and health discussion have?
Summary
257. In this chapter, we have explained why further changes to assessments are needed and explored bold proposals for change. We have:
- Described the work we have been doing with disabled people and people with health conditions, disability charities and others to hear about assessments and develop objectives for future assessments;
- Considered how to simplify and improve the assessments for financial support; and
- Explored a separate discussion for employment and health support.
Chapter 5: Exploring Ways to Improve the Design of the Benefits System
Chapter Summary
We are committed to improving the lives of disabled people and people with health conditions. Rising spending on health and disability benefits suggests there is more we can do to enable independent living and employment. We want to explore making bigger changes to the benefits system that will improve outcomes for disabled people and people with health conditions and that will also mean the system will be more affordable in the future.
In this chapter, we will:
- Consider major changes we have already made to the benefits disabled people and people with health conditions claim;
- Outline challenges within the current system and consider these in the context of how the extent and nature of disability is changing;
- Look at examples of how other countries provide support to disabled people; and
- Explore further, bigger changes that have the potential to improve outcomes and address the rising benefit spend. These are long-term changes that will:
- Help simplify the system;
- Better support more people into work, where appropriate;
- Help people manage changes in benefit entitlement; and
- More effectively support people with their extra costs. This includes looking at alternatives to financial support which could better enable independent living.
We want to provide help to overcome challenges to independent living, including by enabling more people to move into and progress in work where possible. Alongside supporting more disabled people and people with health conditions to enjoy the benefits of employment, this will ensure that the health and disability benefits system is affordable in the future, so that we can continue to provide support for the people who need it most.
Introduction
258. The benefits system is an important source of financial support for disabled people and people with health conditions. It also provides vital support when a person’s ability to work is affected. In total, 3.45 million working-age people claim UC with a health condition, receive ESA, PIP or DLA[footnote 158].
259. We want our benefits to help disabled people and people with health conditions to live independent lives. The benefits system should help and encourage people to start, stay and succeed in work, where possible. In addition, it should provide a safety net for people who cannot work due to the impact of a disability or health condition. It is also important that our support is effective and targeted. Going further, we want to be better able to connect people with the wider support they need, such as help to manage health and wellbeing. This will help ensure the best outcomes for disabled people and people with health conditions and ensure that public spending on benefits is affordable in the long-term.
260. In this chapter we outline previous changes to the benefits system and consider their impact. We also consider what more we can do to improve the system for disabled people and people with health conditions. We want to hear whether we need to make more changes to our benefits to deliver further improvements. If changes are needed, we want to hear what these changes should be.
Previous Changes to Benefits
261. We currently provide two main types of benefit for working-age disabled people and people with health conditions. These are:
-
Benefits that provide money to people who are either not in work or who are employed on low pay. Extra financial support may be awarded to people who are likely to spend longer out of work because of their disability or health condition. These type of benefits are called income replacement benefits and include UC and ESA. Eligibility to UC and income-related ESA (ESA(IR)) is entirely based on a person’s earnings and savings. People with savings over £16,000 may be able to claim contributory ESA (New Style ESA) if they have paid into the system to get support[footnote 159].
-
Benefits to provide money to help people meet the extra costs of a disability or health condition. For working-age people, this is mainly delivered through PIP, although some people still receive DLA. Eligibility for extra costs benefits is not affected by a person’s income or savings. It also is not affected by whether or not a person is working, or by how much a person has paid into the system, for example through National Insurance contributions.
262. Two major changes to health and disability benefits have been introduced within the last 10 years[footnote 160]. We have been replacing DLA for adults with PIP. We have also created UC to replace six different income-related benefits (including ESA (IR)) [footnote 161]. Contributory ESA has not been replaced by UC. This continues to exist alongside UC and is now called New Style ESA.
263. These changes were introduced to meet certain aims and to address challenges of the benefits being replaced. When considering whether further changes are needed, it is important to reflect on the aims and impact of changes made so far.
The introduction of PIP
264. PIP was introduced to replace DLA and was designed to improve:
- Consistency: to increase objectivity, PIP claims are assessed against fixed assessment criteria by an independent healthcare professional. Most people claiming PIP go through an assessment to determine the correct level of award. On DLA, only 5% of people had an assessment. Most DLA decisions were made using the information supplied in the application form, plus any medical evidence. Assessments enable people to give a clearer account of the impact of their health condition. They can also help draw out issues that might not otherwise have been identified
- Sustainability: to focus support on those people least able to participate in society. PIP features regular repeat assessments to ensure that people continue to receive the correct level of support. On DLA, more than 70% of people received an ongoing award. On PIP most awards are made for a fixed period. However, some people are given an ongoing award with a ‘light-touch’ review after 10 years.
- Fairness: to focus on the needs arising from the person’s health condition rather than the condition itself. PIP aims to treat different kinds of health conditions equally.
265. In terms of the extent to which PIP delivered the improvements we intended, there are some clear areas of success others where challenges remain.
266. As explained in Chapter 4, both the WCA and the PIP assessments use criteria to assess a person’s ability to carry out activities and determine the appropriate level of financial support. The assessment criteria used for PIP are more clearly defined than the criteria for DLA. We have also been successful in ensuring the impact of mental health conditions is better recognised. Under PIP, the proportion of people who have a mental health condition and are awarded the highest rate of benefit is almost six times higher than it was on DLA[footnote 162].
267. However, as discussed in Chapter 4, there are a number of challenges relating to assessments. Many of these apply to both the PIP assessment and the WCA, which is used on ESA and UC. For example, we know from Green Paper events that some people do not think the current system of repeat assessments is appropriate for people with conditions that are unlikely to change. The Department also faces challenges in delivering the number of assessments needed. On PIP, this is partly because the number of new claims was higher than the comparable number of new claims made to DLA before PIP was introduced[footnote 163]. Another reason why it is challenging to deliver the necessary volume of PIP assessments is that, unlike most ESA and UC awards, PIP awards are usually made for a fixed period. At the end of that period a repeat assessment (referred to on PIP as an ‘award review’) is usually needed to prevent the claim from going out of payment.
268. PIP has also faced a number of successful legal challenges. While it is normal for the courts to test new legislation, the extent of challenge and the success rate suggest that some aspects of the PIP assessment criteria would have benefitted from further testing before PIP was introduced. PIP is estimated to have increased spending by £1-2bn per year compared to DLA[footnote 164]. Implementing the required changes following successful legal cases is one of many reasons why the cost of PIP has increased.
The introduction of Universal Credit
269. UC was introduced to simplify the benefits system. It was designed to help people move into and progress in work, while also supporting the most vulnerable. UC replaces a range of benefits, including ESA(IR).
270. Both ESA(IR) and UC provide means-tested support for people on low incomes who have a disability or health condition that affects their ability to work. ESA was designed with three key objectives: to help people stay in work when they fall ill or become disabled; to increase the number of people leaving benefit to start work; and to better address the needs of people who require extra help and support.
271. The approach for people claiming UC with a health condition is similar to the approach used for ESA. A person’s capability for work and eligibility for a health-related financial top-up is determined by the outcome of a WCA. Many of the challenges to the WCA are explored in Chapter 4. In UC, this top-up is provided to people who are found to have LCWRA and is worth an extra £343 per month.
272. Compared to older benefits, UC has many features that aim to make it easier for people to move into work. It is for people both out of work and in work on a low income. On UC, people no longer need to switch between different benefits when they move into or out of work, change the number of hours they are working or how much they are earning. This means people can feel confident about being able to try out work on UC, without worrying about suddenly losing all of their benefit at once.
273. UC is designed to make work pay. Some people, including people who are disabled or have a health condition that affects their capability for work, have access to a work allowance. This means that people can earn more before their benefit payment is reduced. A person who has a work allowance can keep either £293 or £515 of the money they earn before the UC taper is applied. The taper reduces benefit in a consistent way. For every £1 earned, 63p is taken away from a person’s benefit amount, rather than the full £1. This means that people are better off by working, even a few hours, where possible.
274. We stopped taking new applications for ESA(IR) in January 2021[footnote 165]. In November there were 952,260[footnote 165] people still claiming ESA(IR). These people can make a new claim for UC should they wish to, or if they experience a change in their circumstances which prompts them to claim UC. It is not currently possible to make comparisons between people who receive UC with a health condition and people who receive ESA. This is because there are many differences between the people claiming the different benefits, such as the length of time people have been claiming the benefit.
Why Further Change is Needed
275. The examples outlined above demonstrate that making changes to benefits can bring opportunities and also challenges. In previous chapters we have explored potential areas for improvement within the current benefits system. We are confident that progressing these improvements will help us to better meet our objectives. However, we know that some people think changes within the current system ‘can only go so far’ and that a new approach is needed[footnote 166].
276. This section summarises what we have heard from disabled people, people with health conditions and the organisations supporting them. It provides further evidence on how effectively we are supporting disabled people and people with health conditions to start, stay and succeed work. In addition, we consider the further pressures on the future benefits system.
277. At Green Paper events, we heard that:
- The purpose of the different benefits can be confusing. Sometimes this means people do not know what they are entitled to;
- Some people worry that their benefits will be taken away as a result of preparing for work;
- There should be more flexibility for disabled people and people with health conditions moving into work and/or off benefits; and
- It can feel as if the benefits system takes a ‘one size fits all’ approach to meeting people’s needs. Some people want extra flexibility in the system.
278. We want to do more to support disabled people and people with health conditions to start, stay and succeed in employment. In recent years, there has been progress towards our goal of seeing 1 million more disabled people in work by 2027[footnote 167]. The latest figures show that the disability employment rate has increased by 8.4% since 2014[footnote 168]. However, the difference between the employment rate of disabled people and the employment rate of non-disabled people, known as the disability employment gap, still stands at 28.6%[footnote 169]. Chapter 2 looks at how we can improve the employment support available for disabled people and people with health conditions. In this chapter, we want to explore bigger changes to help improve employment outcomes.
279. We are seeing an increasing number of people being assessed as having LCWRA on UC or being placed in the ESA Support Group. These people are not required to look for or prepare for work. In 2012 it was forecast that by 2017/18, a total of 0.3m people would be in the Support Group (15% of all people receiving ESA). However, in 2018 there were 1.6m people in the Support Group (67% of all people receiving ESA). This has since increased to 1.9m people (75% of all people on ESA or people on UC with a health condition) in the Support Group or LCWRA[footnote 170].
280. Research with disabled people and people with health conditions shows that some people with LCWRA on UC or in the ESA Support Group would like to work, if the right job and the right support were available[footnote 171]. However, some people were concerned that doing paid work meant risking losing their benefits or having to reapply for benefits if a job did not work out. Some people were also worried about being left without income during the period between their benefit payments stopping and receiving their first wages from a new job[footnote 172].
281. It is likely that some of these concerns (highlighted both in our research and at Green Paper events) relate to older benefits, such as ESA(IR). As outlined previously, the introduction of UC aims to address several of these issues to better support people who are able and want to work.
282. We know that work not only benefits people financially. The evidence that appropriate work can bring health and wellbeing benefits is widely recognised. Evidence shows that, on average, people in work report higher levels of wellbeing than people who are out of work[footnote 173]. Being out of work is also associated with a range of poor health outcomes[footnote 174]. Because of this, we want more people to experience the benefits of working, where this is appropriate.
283. We also need to ensure that the money we spend on benefits makes a real difference to the lives of disabled people and people with health conditions. In 2019/20, we spent over £30bn on working-age health and disability benefits to support disabled people and people with health conditions[footnote 175]. This amount includes spending on benefits which are devolved to the Scottish Government. As the chart below highlights, spending on health and disability benefits for people of working-age will increase from £31bn to £40bn, a 20% increase in real terms, by 2025/26[footnote 176].
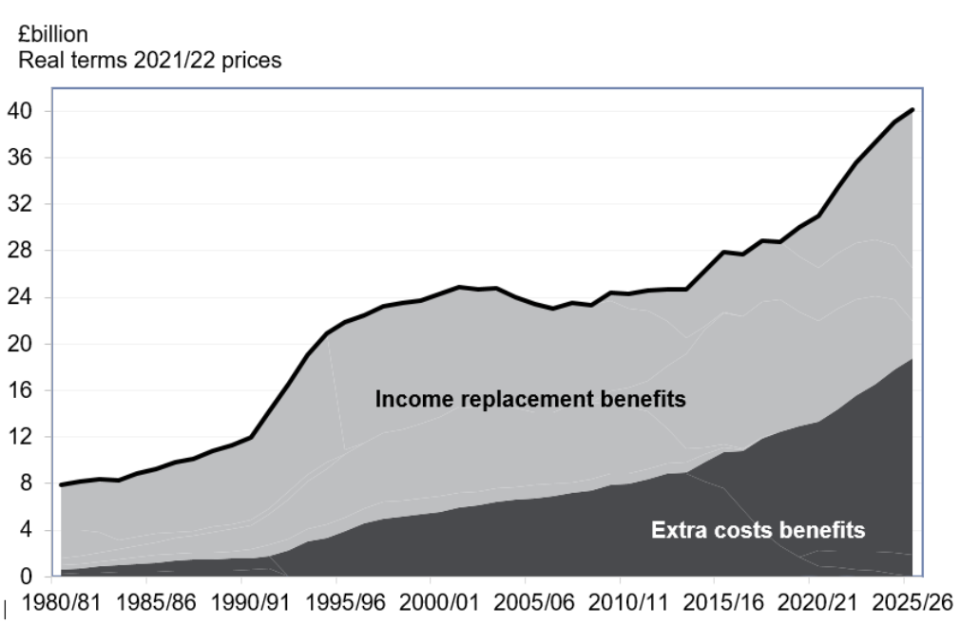
284. Adjusted to real term 2020/21 prices, in 1980/81 the combined spend on income replacement and extra costs benefits was around £8 billion – £500 million on extra costs and £7.5 billion on income replacement benefits. These both have gradually risen to reach a combined £31 billion by 2020/21 – £13 billion on extra costs and £18 billion on income replacement benefits. These are both forecast to continue to rise, reaching a combined £40 billion by 2025/26 – £19 billion on extra costs and £21 billion pounds on income replacement benefits.
285. £5 billion of the real terms[footnote 177] increase in forecasted spending is due to be spent on PIP and DLA. The remaining £4 billion of increased real terms spending is a result of higher than predicted spend on ESA and people claiming UC with a health condition[footnote 178].
286. Spending on health and disability benefits is growing for a number of reasons. The number of people who report a disability or health condition has increased[footnote 179]. Overall improvements in healthcare mean that the diagnosis and treatment of health conditions has improved and led to fewer years lived with disability at each age compared to 1990[footnote 181]. However, the number of older working-age people has increased, and typically people’s health declines with age. This means we can expect to see a greater number of older working-age people who are disabled or have a health condition. Access to treatment will continue to be key to improving people’s health and helping people to manage the impact of a health condition.
287. However, changes in the age and size of the working-age population do not fully explain the increase in the number of people claiming health and disability benefits. There are likely to be many factors, including the increase in the proportion of people reporting a mental health condition[footnote 182] [footnote 183]. Currently around half of all people receiving working-age health and disability benefits have a mental health condition as their main condition. For people receiving PIP or DLA the proportion of people with a mental and behavioural disorder as their main condition has increased from 25% in 2002 to 41% in 2020[footnote 184]. Evidence also shows that mental and physical health are closely linked. Around 30% of people with a long-term physical health condition have a mental health condition too[footnote 185].
288. Wider changes to the benefits system have contributed to the increased spend. Changes in the State Pension age mean that people now claim working-age benefits who would previously have claimed pension-age benefits. For PIP, people can then continue to receive this benefit beyond State Pension age. These changes suggest that the benefits system will face higher demand from disabled people and people with health conditions in the future.
289. We need to ensure that people are supported to live independent lives, moving into and progressing in work where possible. Ensuring that the benefits system is enabling this in an effective and affordable way is crucial given the scale of the challenge, both now and in the future. The benefits system also needs to adapt to the changing needs of disabled people, for example by responding to the increasing number of people with a mental health condition. We also know that some people will need support that goes beyond what this Department can provide, such as support from health services.
Comparing our Health and Disability Benefits to Other Countries’
290. In this chapter, we consider how other countries support disabled people and people with health conditions through the benefits system. International case studies are provided in Annex C. These case studies demonstrate the range of approaches that are taken across the world. We have included these to encourage thinking beyond our current benefits system.
291. Across all of these case studies, it is important to remember that there is no ‘perfect’ system. Other countries face many of the same challenges as we do and different approaches create their own challenges.
292. The countries we have looked at vary a lot in how they assess who is entitled to benefits and how these are paid. Each country also has a different system with different priorities on how to offer support. For example, many countries use insurance-based systems. In these countries people need to pay contributions into the system to be able to access support when they need it. This places more of a focus on rewarding past contributions and could mean that people who have not ‘paid in’ receive a reduced level of support. In contrast, in Great Britain in 2019/20, just 16% of the total amount of money spent on working-age health and disability benefits was paid through contribution-based benefits[footnote 186].
Should We Simplify the Benefits System?
293. As shown in the diagram below, around 1.6 million working-age people claim both support for income replacement (people claiming UC with a health condition and ESA) and extra costs (through PIP and, to a lesser extent, DLA). This means that around half of these people claim both types of benefit. The proportion of people claiming PIP or DLA who are also on ESA or claiming UC with a health condition has increased since 2013[footnote 187].
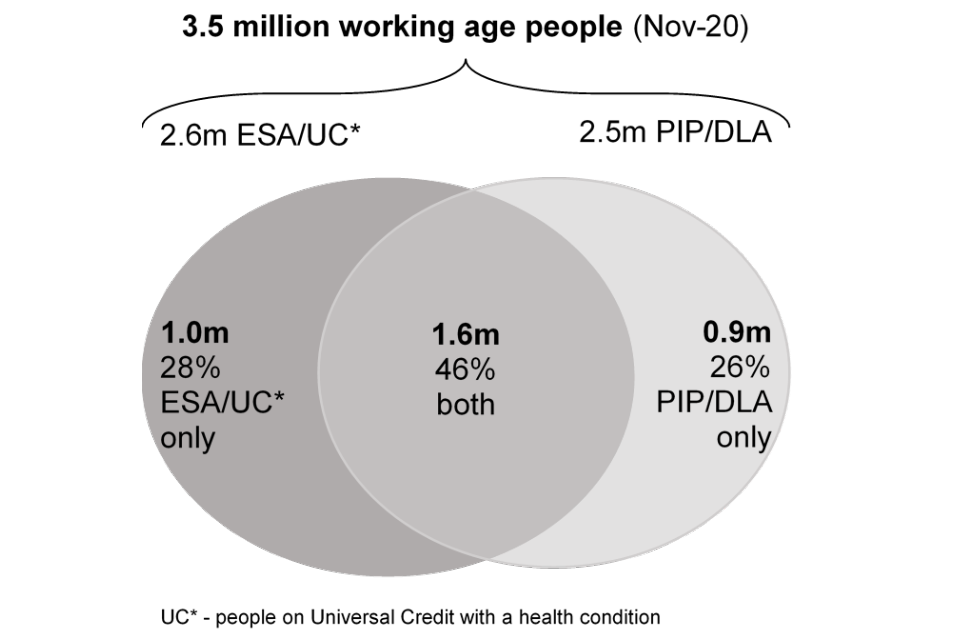
294. Some working-age people claim ESA/ UC with a health condition only, some claim PIP/DLA only and some claim both types of benefit: In total, 3.5 million people (as of November 2020) were in receipt of one or both of PIP or DLA and ESA, or on UC with a health condition. Of these, 1 million are in receipt of ESA or are people on UC with a health condition only, 900,000 are in receipt of PIP or DLA only and 1.6 million are in receipt of both PIP or DLA and ESA or UC with a health condition. This also means that 2.6 million people are in receipt of ESA or UC with a health condition and 2.5 million are in receipt of PIP or DLA.
295. People who are on PIP as well as claiming either ESA or UC with a health condition currently go through two separate application and assessment processes. This means that people sometimes feel the same information is requested twice. The different purposes of the separate benefits are also not always clear to people claiming them. Some people have told us that having to go through two separate processes can be confusing and difficult, as illustrated in the case study below.
Case study: Experiences of the current system
Teodora suffers from anxiety, severe depression and paranoia following the death of her child. As a result, Teodora’s family made a claim for Personal Independence Payment (PIP) to support her with some of the extra costs she faces. They also made a claim for Universal Credit (UC), as Teodora’s health conditions limit her ability to work.
Teodora’s partner found completing the forms extremely distressing due to the loss they had suffered and found he was repeating himself on both forms. Teodora also found the process distressing as she had to attend two face-to-face assessments.
296. At Green Paper events, people told us that there needs to be a simpler application and assessment process. Some people felt that having a single health and disability benefit would help achieve this. Other people were worried about all their financial support depending on the outcome of one assessment.
297. As discussed in Chapter 3, we have explored using one single assessment for both types of benefit. This has shown that introducing a single assessment into the current system would not be beneficial[footnote 189]. The benefits have been designed separately and each assessment considers different criteria. However, in the future, we could look to create a new single benefit. This could both provide support for disabled people and people with health conditions on low income and with extra costs. Alternatively, a new benefit could have different priorities or a different set of objectives to our current system. More focus could be put on supporting people with their extra costs, or on helping people to find and stay in work. Different countries prioritise these aims differently.
298. For example, we know that Switzerland’s disability benefits system provides less support for the extra costs of disability. It also has a greater focus on supporting people on low incomes to move back into work. It does this in a number of different ways, including through workplace adjustments, training courses and financial support (see case study 1 in Annex C).
299. If we were to introduce a new single benefit, depending on how this was designed and its objectives, it might be possible to use a single assessment. Alternatively, we might be able to simplify access to this new benefit in some other way.
Consultation question
How could we simplify the system for people applying for multiple health and disability benefits?
How Can We Better Support People into Work and Adjust to Changes?
300. The current health and disability benefits system provides different levels of financial support depending on the impact of a person’s health condition. As outlined earlier in this chapter, for ESA and UC this is assessed using the WCA. People found to have LCWRA on UC or placed in the Support Group on ESA are eligible for an additional award of benefit and are not required to look for or prepare for work. People found to have LCW on UC or placed in the WRAG on ESA do not receive any additional benefit compared to people applying with no health condition. However, people found to have LCW or placed in the WRAG are not required to look for work now, but do need to take steps to prepare for work.
301. For PIP, the assessment looks at how a person’s health condition affects their ability to carry out certain day-to-day tasks. This is used to determine the level of financial support a person will receive towards the extra costs of their disability. There are eight possible PIP award payment outcomes that are designed to contribute towards extra costs. These are paid at fixed amounts and via regular payments for the length of the award.
302. Having these different levels of payments aims to ensure that financial support is focused towards the people who need it most. However, it can mean that people are worried about the level of their benefit payment changing after an assessment. For example, the amount of benefit paid to a person claiming UC could be reduced by £343 per month if we find that the person is no longer eligible for the extra support that comes from having LCWRA. A change in financial circumstances also happens when people move between rates within PIP.
303. In France (see case study 2 in Annex C), ‘grace periods’ are used to address this. These are used when a person’s benefit entitlement changes and allow people time to adjust and prepare for work if needed. During a grace period, people continue to receive benefits at their old rate so that it is easier to adapt.
304. We know that once people are receiving benefits because of their limited capability to work, they are very unlikely to move off the benefit and into work. ESA data shows that only 1-2% of people in the WRAG and less than 1% of people in the Support Group leave the benefit each month[footnote 190].
305. We want disabled people and people with health conditions to feel supported in moving towards and into work where possible. As outlined earlier in this chapter, UC has been designed to encourage this. Everyone on UC and on ESA, including people found to have LCWRA or placed in the Support Group, is allowed to do some work while still receiving benefit. On ESA, a person can work up to 16 hours or earn up to £143 (after tax) a week before losing any of their benefit payment. On UC, people’s working hours are not restricted at all. People found to have LCW or LCWRA are also given a work allowance. On UC, earnings above these limits are subject to the taper discussed earlier. This means that people always keep a proportion of their benefits in addition to their earnings when carrying out paid work.
306. As discussed previously, our research suggests that some people who have LCWRA or are in the Support Group are worried that starting work could affect their financial position significantly or trigger a repeat assessment. People are also concerned about their ability to access benefits again quickly if a job does not work out[footnote 191].
307. Where people may be able to work, we want to provide encouragement to do so. We want to explore whether there are better ways to target financial support at people with the highest needs so that people do not feel discouraged from trying out work.
Consultation questions
- UC has many features, such as the work allowance and taper, that aim to make it easier for people to move into work. How can we ensure that disabled people and people with health conditions are aware of these features, and encourage people to try out work on UC?
- How could the current structure of benefits be changed to overcome people’s financial concerns about moving towards employment?
- How could the current structure of benefits be improved so people can better manage changes in benefit entitlement?
How Can We More Effectively Support People with Their Extra Costs?
308. PIP is designed to provide a financial contribution towards the extra costs that disabled people and people with health conditions can incur. The assessment considers a person’s ability to manage a range of daily activities. There are two categories or components PIP considers. The first is daily living, which includes activities such as preparing food and washing and bathing. The second is mobility, which includes planning and following journeys and moving around. Awards are determined by the number of points scored against each activity. PIP award payment outcomes are paid at fixed amounts and via regular payments for the length of the award. People can spend their PIP award freely with no restrictions.
309. Other countries take a different approach to supporting people with extra costs. New Zealand (see case study 3 in Annex C), for example, look more closely at the actual costs incurred and help people by providing exact amounts of financial support to cover these costs. Other countries, like Australia (see case study 4 in Annex C), use a more holistic assessment which looks at the wider needs of each person and considers what broader support could help people meet their goals.
310. We want to explore how the benefits system can better support people to live independent lives. This could be through improving awareness and/or access to aids, appliances and services. This could help improve people’s health or improve people’s ability to manage the impact of a disability or health condition. Given the increasing amount the Government spends on health and disability benefits, it is important that we do this in an efficient and targeted way.
311. The Motability scheme, which is run by the independent Motability Charity, is currently the only option where the Government allows disabled people to use some of their benefit payment to access goods or a service. This allows people who receive the enhanced rate of the PIP mobility component to swap all or part of it to hire a vehicle through the independent Motability scheme.
312. We could explore improving access to aids, appliances and services by allowing people to voluntarily swap all or part of their benefit payment for these. This could create a more personalised service than when benefits are just paid as financial support.
313. At Green Paper events, people told us that swapping a benefit payment for goods or services should always be optional. This is because a benefit payment lets people choose how to meet their specific needs.
314. There are some key things to consider when deciding whether to move to a system offering practical support. In Chapter 1, we heard that disabled people can find the system complex and confusing. Offering more options could make the system more complicated, especially where practical support is also offered by local authorities or the NHS. It may only be deliverable if a large number of disabled people are interested in similar types of support. If most people continued to opt for a financial payment, we might not be able to provide practical support in a cost-effective way.
Consultation questions
- While continuing to focus financial support on people who need it most, how could we more effectively support disabled people with their extra costs and to live independently?
- Should we explore options to make it easier for disabled people to access practical support such as aids, appliances or services, and why?
- What particular types of practical support should we help disabled people access?
Summary
315. In this chapter, we have asked for views on what the future of health and disability benefits should look like. This builds on a robust analysis of the health and disability benefit statistics and research as well as the conversations we have been having with disabled people and people with health conditions at Green Paper events.
316. We will consider the impact of any potential changes to the benefits system on the other benefits and support we provide for disabled people and people with health conditions. For example, changes to PIP, UC or ESA could affect benefits such as Carer’s Allowance and Attendance Allowance. We will look holistically at any changes we make, to avoid unintended consequences.
317. We are committed to making any changes collaboratively, working with and listening to the people who receive and rely on our benefits. Responses to this consultation will be used to shape the future of benefits claimed by disabled people and people with health conditions.
Conclusion
318. The Government is committed to transforming the lives of disabled people and people with health conditions. This is why we are publishing the National Disability Strategy, to take action across government and society to address challenges that limit people’s opportunities. The Green Paper forms part of this wider plan to transform the prospects of disabled people and people with health conditions. As we build back better from the coronavirus pandemic, it is more important than ever that the benefits system supports people when they need it most. By consulting on Government’s ambitious plans for change, this Green Paper has sought to start a conversation that puts disabled people and people with health conditions at its centre.
319. We know that many people are happy with the services we provide[footnote 192] but we want to do more. We have asked for views on how to improve health and disability support for working-age people. Through Green Paper events, we have gathered valuable insights. These have enabled us to set out how we believe the benefits system should: enable independent living; improve employment outcomes and improve the experience of disabled people and people with health conditions.
320. We heard at Green Paper events that people can sometimes find it difficult to interact with us. Disabled people and people with health conditions can feel afraid of the benefits system, do not always trust health assessments or the decisions that they lead to and, as a result, can be unwilling to accept offers of employment support and feel worried about starting work. We have set out what we want to do to make improvements in the future and asked for suggestions about the changes we should make.
- We have explored what more we can do to provide the right support to help disabled people and people with health conditions find their way through the benefits system.
- We have outlined how we want to continue to improve employment support and encourage more disabled people and people with health conditions to take up this support.
- We know that most people have a positive experience with this Department. Where that is not the case, we have considered what more we could do to improve our current services such as assessments and decision making.
- We have explored whether more fundamental changes could be made to future health assessments, to help more people find work and live independent lives.
- Finally, to deliver better outcomes, and because we want the support we provide to be affordable in the future, we have explored changes to the structure of the benefits system itself.
Working with Disabled People and People with Health Conditions
321. This Green Paper draws on a wide range of evidence and views. Independent research has been carried out with thousands of people claiming health and disability benefits. We regularly work with a range of charities. For this Green Paper, we have also held Green Paper events to hear directly from disabled people. A number of these events have been led by disability charities. More information about these events is provided in Annex A.
322. We know that working in partnership with the people who are directly affected by our decisions is crucial if we are to deliver better outcomes. We want to involve more disabled people and people with health conditions in shaping how we work. We will continue to listen in order to improve how we work in future, so that we can continue to make changes that will improve people’s lives.
Summary of Consultation Questions
Chapter 1: Providing the Right Support
- What more could we do to improve reasonable adjustments to make sure that our services are accessible to disabled people?
- What more information, advice or signposting is needed and how should this be provided?
- Do you agree with the principles we have set out for advocacy support?
- How might we identify people who would benefit from advocacy?
- What kinds of support do you think people would want and expect from advocacy?
- Are we meeting disabled people’s mobility needs? Please tell us why/why not.
Chapter 2: Improving Employment Support
- What more could we do to further support employers to improve work opportunities for disabled people through Access to Work and Disability Confident?
- How can we support people who have fallen out of work to identify and consider suitable alternative work before their Work Capability Assessment?
- What further support or information would help work coaches to have more effective conversations with disabled people and people with health conditions?
- What has been your experience of receiving employment support? What was good about the support? Are there further improvements that can be made?
- How can we make the most of the knowledge and expertise of local organisations to support disabled people and people with health conditions into employment?
- What more could we do to work with other organisations and services, such as local authorities, health systems, and health services offered in the devolved administrations, to provide and join up employment support in health settings?
- What can we offer that would encourage people in the Support Group or LCWRA to take up our employment support?
- Would you be happy to access employment support digitally? Please tell us why/why not.
- What should we consider when developing a digital support offer for disabled people and people with health conditions?
- How can we better support young disabled people and people with health conditions who are moving out of education to find appropriate work?
Chapter 3: Improving Our Current Services
- During the coronavirus pandemic we introduced assessments by telephone and video call as a temporary measure. In your view, in future, what mixture of methods should we use to conduct assessments?
- How could we improve telephone and video assessments, making sure they are as accurate as possible?
- What more could we do to reduce repeat assessments, where someone has a condition that is unlikely to change?
- Decisions can be changed after an appeal has been lodged but before a tribunal hearing takes place. How can we improve the way we communicate a new decision in this situation?
- What other changes could we make to improve decision making?
- How could we improve the experience when people claiming Child DLA are invited to apply for PIP?
Chapter 4: Re-thinking Future Assessments to Support Better Outcomes
- Is there anything about the current PIP activities and descriptors that should be changed? (Yes/No/Don’t know)
- If yes, what changes to the PIP activities and descriptors should we consider?
- Is there anything about the current WCA activities and descriptors that should be changed? (Yes/No/Don’t know)
- If yes, what changes to the WCA activities and descriptors should we consider?
When responding to these questions, please consider:
- What the best way to capture the impacts of health conditions that fluctuate might be.
- How we could ensure the activities and descriptors capture the impact of all health conditions and disabilities fairly;
- How we could simplify the assessment criteria; and
-
Any possible PIP or WCA activities that are no longer a barrier or that are less of a barrier to employment or independent living, due to modern working practices and advances in assistive technology.
- Should we seek evidence from other people, such as other health professionals and support organisations?
- What type of evidence would be most useful for making decisions following a WCA or PIP assessment, and should there be a standard way to collect it?
- How could we make sure the evidence we collect before a WCA or PIP assessment directly relates to a person’s ability to do certain things?
- How could we improve assessments or the specialist support available to assessors and decision-makers to better understand the impact of a person’s condition on their ability to work or live independently?
- How can we make it easier for people to inform us if their condition or circumstances have changed so that a review of entitlement can be carried out at the right time?
- What could be included in a discussion to develop a more personalised employment and health support plan?
- What skills and experience should the person undertaking an employment and health discussion have?
Chapter 5: Exploring Ways to Improve the Design of the Benefits System
- How could we simplify the system for people applying for multiple health and disability benefits?
- Universal Credit (UC) has many features, such as the work allowance and taper, that aim to make it easier for people to move into work. How can we ensure that disabled people and people with health conditions are aware of these features, and encourage people to try out work on UC?
- How could the current structure of benefits be changed to overcome people’s financial concerns about moving towards employment?
- How could the current structure of benefits be improved so people can better manage changes in benefit entitlement?
- While continuing to focus financial support on people who need it most, how could we more effectively support disabled people with their extra costs and to live independently?
- Should we explore options to make it easier for disabled people to access practical support such as aids, appliances or services, and why?
- What particular types of practical support should we help disabled people access?
Annex A: Green Paper Events
Background
On 25 June 2019, we announced that we would be launching a Green Paper to explore ways to improve support for disabled people and people with health conditions. Disabled people’s organisations and representatives told us that they wanted to work closely with us to develop the Green Paper. They also said that people using our services should be encouraged to share their experiences and priorities for change. As a result, disabled people and people with health conditions, and the organisations supporting them, have helped shape this Green Paper. This annex describes how people fed in their views[footnote 193].
October 2019 – March 2020: We heard from disabled people and people with health conditions in Bristol, Leeds, Milton Keynes, Birmingham, Whitehaven, Nantgarw and Wisbech.
Face-to-Face Events
On 4 July 2019 we held an event in London with representatives from charities, disabled people’s organisations, associations, think tanks and academics, to begin the conversation about the themes this Green Paper should cover.
Between October 2019 and March 2020 we organised a series of seven face-to-face events to allow conversations between DWP staff, disabled people and people with health conditions, their representatives and charity workers from various local and national organisations.
These events took place at a range of locations as shown in the map above. People drew upon their experiences (either of using our services, or of supporting others to use them) to identify what we did well, and make suggestions about where we could improve.
We designed the events to make sure that everyone was comfortable and had the opportunity to share their views and ideas. People talked about their interactions with us, from the application process, through to the assessment and ongoing support. We then asked people to discuss these issues in groups, to identify common experiences, and draw out the good and the bad. Finally, we encouraged people to take the best and worst of those shared experiences and develop them into ideas for improvement. People had lots of good ideas, big and small.
In October and November 2019 we also held three workshops in London and Birmingham. These were attended by our staff who work with disabled people and people with health conditions. At these events we heard about issues affecting their work. This allowed us to make sure that the experiences of our staff were reflected in the Green Paper.
Virtual Events
The outbreak of the coronavirus pandemic in March 2020 made it unsafe to hold further face-to-face events. We continued to hear from disabled people and people with health conditions in a series of virtual events led by the Minister for Disabled People, Health and Work.
In September 2020 we held two events for charity staff working in London and Scotland. We also held 13 virtual events led by the following charities. These charities arranged for disabled people and people with health conditions to take part in these events and tell us about their experiences:
- Scope, 21 July 2020;
- MS Society, 30 September 2020;
- Royal National Institute of Blind People (RNIB), 12 October 2020;
- Royal National Institute for Deaf People (RNID), 13 October 2020;
- Mind, 14 October 2020;
- Macmillan, 20 October 2020;
- Mencap, 21 October 2020;
- Citizens Advice, 3 November 2020;
- Ambitious About Autism, 16 November 2020;
- Motor Neurone Disease Association (MNDA), 17 November 2020;
- Sense, 14 January 2021;
- Marie Curie, 3 March 2021; and
- Headway, 24 March 2021.
We worked with these charities to create events that were fully accessible for the people attending. The main topics discussed included navigating the benefits system, assessments, and employment support. Some charities asked that events include special sections on other topics such as our response to the coronavirus pandemic and improvements to Access to Work.
Several of these events brought together people with the same health condition or disability. This helped us to understand the full range of experiences people have of the benefits system, and how we could improve the system to better meet people’s specific needs.
Between 5 and 15 disabled people attended each of these events. This allowed more time for people to fully explain their experiences. Where people were interested in providing feedback but were not able to attend, we asked for views in writing which we then put together with the feedback from the event.
On 20 July 2020 we discussed the Green Paper with the Disability Charities Consortium (DCC), which brings together representatives from the UK’s largest national disability organisations.
On 1 December 2020 we held an event with Anthony Mangnall MP, who arranged for representatives from charities and organisations operating in his constituency of Totness to attend and share their views. In February 2021 the Minister for Disabled People, Health and Work wrote to all MPs to offer them the opportunity to organise similar events for their constituents. In all we have run 14 events with a further nine planned.
On 8 December 2020 we held an event with representatives from health assessment providers. The purpose of this event was to hear the views of providers about how to improve assessments for disabled people and people with health conditions.
In January 2021 we also held 3 further virtual events with our staff whose roles require them to work closely with disabled people. These events helped to further develop our understanding of where we could make improvements that would better support disabled people and people with health conditions.
Regional Stakeholder Network
The Regional Stakeholder Network is made up of 225 disabled people, the organisations supporting them, their parents and carers. These are grouped in each of the 9 regions in England and led by regional chairs. This network allows people to share their views about the policies and services that affect them. It also provides a way for organisations across England to contribute views on government priorities and policies that affect disabled people. Between November 2020 and January 2021 we met with each of the regional groups to discuss the Green Paper and to hear views about what needs to change.
How we used feedback from Green Paper events
These Green Paper events gave us the chance to listen and hear first-hand about those aspects of our services that disabled people and people with health conditions find difficult, and to work with people to explore how we can improve.
After the events took place, we reviewed all the evidence, insights and ideas and drew out the key themes so that these could be considered throughout the Green Paper. We also shared this information with staff working across the Department to make sure the insights gathered could be taken into account in making wider changes to our services.
Annex B: Our Employment Support Programmes
| Programme / initiative | Description |
|---|---|
| Work and Health Programme (WHP) | By early 2018, the WHP was launched throughout England and Wales. By October 2022, the programme will have provided support to around 220,000 disabled people. Some of this support is devolved to our Local Government Partners in London and Manchester. The WHP aims to use the expertise of local organisations and offers up to 15 months of pre-work support that is tailored to individual needs. In-work support is also available for up to six months, if needed. Referrals are due to end in October 2022, with the option to extend for up to two years. We are considering how best to build on the programme including looking at evidence from a full evaluation. |
| Intensive Personalised Employment Support (IPES) | IPES provides a further level of intensive support to disabled people with complex barriers to work who are considered by DWP work coaches to be more than 12 months away from work. Support can be delivered for up to 21 months, including six months of intensive in-work support. IPES will provide support for 10,000 disabled people to find work over four years. Places on IPES will be increased by 25% from July 2021 to meet increased demand. |
| Local Supported Employment (LSE) | LSE has been developed to test ways of working with local authorities to support autistic people and people with a learning disability. We are looking to expand our offer of LSE through a Trailblazer. This will build on existing relationships with people who access social care through their Local Authority. It will enable a wider group of people who do not regularly attend jobcentres to access support. |
| Plan for Jobs | To support the UK’s economic recovery following the coronavirus pandemic, the Government has launched the Plan for Jobs[footnote 194] . This is a range of measures designed to ensure more people get tailored support to find work, including disabled people and people with health conditions. It includes programmes such as Kickstart, Restart, Job Entry Targeted Support (JETS), Sector-based work academy programme and Job Finding Support (JFS), which have places available to support disabled people. |
| Individual Placement and Support (IPS) | IPS is a model of intensive support which places people into work and provides support to stay there. We have been trialling IPS with people with common mental and physical health conditions, and people with drug and alcohol dependence. We will continue to fund IPS in our existing trial areas in 2021/2022, and expand IPS for people with drug and/or alcohol dependence to more local authority areas. |
| Employment Advice in Improving Access to Psychological Therapies (EA in IAPT) | NHS England’s IAPT provides evidence-based psychological therapies to people with anxiety and depression. We provide employment advice embedded in IAPT. We currently fund this directly in approximately 40% of IAPT services across England. Therapists and employment advisers work together to consider ways to improve mental health, support people to remain in work while receiving treatment, get back to work, if off sick, or to find work, if out of work. |
| Health is Everyone’s Business consultation response | The Government is publishing its response to the Health Is Everyone’s Business consultation, which focused on earlier, improved support for employers and employees, to support more disabled people and people with health conditions to remain in work. |
| Group Work | Group Work is a specialised job-search skills training course, designed to support people back into high-quality employment and protect the mental health and wellbeing of the people involved. Over the course of a week, trained group leaders deliver five, four-hour job skills modules to a group of 10 to 20 people. We conducted a trial of this approach between 2017 and 2018. An evaluation of the trial has found positive employment and health effects for people at greater disadvantage in the labour market, such as people with higher levels of anxiety. Many of these positive impacts still remain 12 months after the course.[footnote 195] |
| Access to Work | The 2019/20 support provided by Access to Work reached its highest ever number, with over 43,000 disabled people and people with health conditions receiving tailored and flexible support to do their job. Access to Work has continued to support underrepresented groups including people with mental health conditions. In 2019/20, 8,710 people with mental health conditions were awarded help from Access to Work. This was double the number of people helped the previous year. Government is looking to expand the reach of the scheme, improve the experience of people accessing funds and use the scheme to encourage innovation. Access to Work is adapting and flexing its offer. Government has introduced a new flexible offer to enable disabled people to work from more than one location and adapt to new working arrangements. A number of improvements have been made to the Access to Work service, including an online application, to enable disabled people and employers to choose a time that is convenient for them to make their application, a digital renewal process with a text or email reminder service to ensure continuity of support, updated Access to Work staff guidance and reflecting feedback. Changes have also been introduced to streamline the process and reduce the time it takes for people to receive payments. |
| Disability Confident | The Disability Confident scheme is continuing to encourage employers to think differently about the employment of disabled people. The scheme aims to provide employers with the knowledge, skills and confidence they need to attract, recruit and retain disabled people and provide support for disabled people to progress in the workplace. As of 30 April 2021, there were over 20,000 employers signed up to the scheme, covering over 11 million paid employees. |
Annex C: International Case Studies
Case Study 1: Switzerland
Everyone living or working in Switzerland is required to pay into the ‘Disability Insurance’ scheme, even people who are not in employment. Provided that three years of contributions have been completed, as well as other eligibility criteria, a disabled person with a long-term condition may be able to receive a disability pension. The amount of pension paid is determined, in particular, by the level of severity of the person’s disability.
The disability pension is very much a last resort. Instead, there is more focus in Switzerland on early rehabilitation measures. Best efforts are made to help disabled people maintain or improve their ability to work and/or perform everyday tasks. The goal is for people to be able to continue employment or carry out day-to-day tasks (such as household chores) as much as possible. Rehabilitation measures include things like adjustments to the workplace, training courses and daily cash benefits.
In Switzerland, there is also a cash benefit designed to contribute towards extra costs called ‘helplessness allowance’ Like PIP, it is designed for people who face additional costs because of their disability and is measured against their ability to complete, without assistance, certain day-to-day tasks such as dressing, getting out of bed or eating. Helplessness allowance is awarded only in exceptional circumstances and only to people who need personal assistance or regular care to perform those day-to-day tasks. Just 10% of people with a disability pension have a helplessness allowance.
Case Study 2: France
Other countries support people to start and stay in work in different ways. In France, people on the contribution-based system can continue to receive benefits for six months after starting work, regardless of earnings. After this, if earnings have not reached the level they were at before the person became unemployed, then benefits can continue to be paid, in addition to earnings. This payment is reduced accordingly as earnings increase. This is an example of how benefits systems can support people as their benefit entitlement changes, smoothing the transition to earned income.
Case Study 3: New Zealand
The New Zealand Disability Allowance aims to help people pay the ongoing, extra costs that arise from having a disability that is expected to last at least six months. Unlike PIP, people are not assessed and are grouped based on their health-related needs. Instead, the amount of Disability Allowance paid is determined based on the actual extra costs the person has as a result of their disability. The costs must be verified by the person’s health practitioner as being a result of the person’s disability, ongoing, as well as needed and of therapeutic value for the person. People who meet the income test then receive a weekly payment to cover these costs, up to a set maximum (NZ $66.11 (around £34) as of 1 April 2021). Below this, maximum payments are adjusted according to people’s actual costs related to their disability, rounded up to the nearest five cents. This helps ensure that the money is targeted at people’s specific costs.
Case study 4: Australia
Since 2013, Australia has supported eligible disabled people through the National Disability Insurance Scheme (NDIS). Aiming to ensure that eligible people receive individualised support based on their needs, a person on the scheme will see a plan developed which will set out the value of the funding to be provided by the NDIS. This is determined by the impact of the person’s disability on their ability to complete day-to-day activities. The funding provided in the person’s NDIS plan can be used to purchase goods, services and other support related to their needs to help them pursue their goals and aspirations. People can manage their NDIS funding in three ways:
- Self-management: Where people manage the funding themselves and provide receipts received directly from providers against their own NDIS plan;
- Plan-management: Where providers send receipts to a plan manager, selected by the person to manage their money. The plan manager will then organise payment to the provider for services delivered to the person;
- Agency-managed: Where the provider claims payment through the NDIA’s (National Disability Insurance Agency) online portal once support has been delivered. The NDIA pays providers directly on behalf of the person.
The NDIS will benefit around 500,000 Australians with permanent and significant disability by 2023.
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Department for Work & Pensions/Department of Health, Improving Lives: The Work, Health and Disability Green Paper, published October 2016. ↩
-
Department for Work & Pensions/Department of Health, Improving Lives: The Future of Work, Health and Disability, published November 2017. ↩
-
Health is Everyone’s Business: Proposals to reduce ill-health related job loss, published July 2019. ↩
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Between 16 March and the end of April 2020 there were over 1.8 million claims for Universal Credit, over 250,000 claims for Jobseeker’s Allowance and over 20,000 claims for Employment and Support Allowance. See: The Secretary of State’s Oral Statement to Parliament on DWP’s response to the coronavirus pandemic on 4 May 2020. ↩
-
Office for Budget Responsibility, Economic and Fiscal Outlook, published March 2021, pages 140-141 ↩
-
To be eligible for New Style ESA a person usually needs to have worked and paid and/or been credited with enough National Insurance contributions in the 2 or 3 years before making a claim. To be eligible for income-related ESA, a person must have income and savings below a certain level. ↩
-
DWP Benefit Expenditure and Caseload Tables, published March 2021. People with payment type of both income and contributions based are counted as contributions based. There are also 107,340 people on ESA who have no payment (Credits only). ↩
-
This usually takes the form of a valid Fit Note which has been provided by a person’s GP and has been approved by this Department. ↩
-
284,000 people claiming PIP are over State Pension age. Source: DWP Benefit Expenditure and Caseload Tables, published March 2021. ↩
-
The care needs of disabled people and people with long-term health conditions may be met formally through support provided by their local authority or more informally through an unpaid carer, often a family member. The benefits system can provide help and support to unpaid carers. This may be through receipt of a means-tested benefit, or it may be more specific where the hours of care provided meet the appropriate threshold, through Carer’s Allowance and/or additional amounts for carers in Universal Credit and other benefits. This support is “triggered” by the payment of specified benefits to the person being cared for. ↩
-
Data held for people aged 16-64 data pre-dates the increase in State Pension age to 66. ↩
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
The number of working-age people reporting a disability has increased from 6.7m in 2013 to 8.1m in 2019. Labour Force Survey, Oct-Dec 2013 to Oct-Dec 2019. ↩
-
Between 2019 and 2029 the total number of working-age people is expected to increase by 2.6 million people. The number of working-age people who are aged over 60 is expected to increase by 1.8 million. This means that working-age people over 60 are expected to account for 66% of the total increase in the working age population between 2019 and 2029. This is partly the result of the rise in the State Pension age from 65 in 2019 to 67 by 2028. Source: 2018-based National population projections, GB Principal projection, ONS. ↩
-
Blank ↩
-
These figures use the most recent outturn of 2019/20 based on real terms and with a 2021/22 benchmark. Source: DWP Benefit Expenditure and Caseload Tables, published March 2021. ↩
-
Based on DWP Benefit Expenditure and Caseload Tables, published March 2021, and includes spending on working age PIP and DLA devolved to the Scottish Government. See Green Paper evidence pack. ↩
-
DWP Benefit Expenditure and Caseload Tables, published March 2021. ↩
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Internal analysis based on DWP UC Social Cost Benefit Analysis Model. This estimate of exchequer savings is for a full time (35 hours per week) working individual on UC with the LCWRA award. This estimate does not change significantly if they are on LCW. They are single, over the age of 25, have no children and do not have caring responsibilities. They are earning the median hourly wage for someone with a disability (£10.63), taken from the ONS and are paying the average rent (social and private) for a single person with no children, taken from 2017 SHBE data. It assumes the individual is claiming UC when in and out of work and it compares being in work for 1 year to being out of work for 1 year. It excludes distributional and substitution effects. It does not account details of employment intervention/programme costs. Figure is in 21/22 prices. ↩
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
In 2019/20, 43% of people living in absolute poverty (before housing costs) lived in a family where someone was disabled. Source: Department for Work and Pensions, National Statistics, Households below average income: for financial years ending 1995 to 2020, published 25 March 2021 ↩
-
For example, Barry J, Blake M, Bridges L, Candy D, Carragher E, Duxbury K, Fowler H, Lambert C, Morris L (Ipsos MORI). Personal Independence Payment Claimant Research – Final Report. DWP Research Report 963; published September 2018. ↩
-
For example, Marcinkiewicz A, Lucey G, Pinto C, Taylor I, Taylor B, Cheesbrough S (NatCen Social Research). Claimant experience of telephone-based health assessments for PIP, ESA and UC. DWP Research Report; 2021. ↩
-
Gordon Waddell & Kim Burton, Is work good for your health and wellbeing? published 2006.. See also: Rueda S, Chambers L, Wilson M, Mustard C, et al. Association of returning to work with better health in working-aged adults: a systematic review. American Journal of Public Health, 2012; 102, 541–56.; Roelfs DJ, Shor E, Davidson KW, Schwartz JE. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Social Science & Medicine, 2011; 72(6), 840–854. ↩
-
Health is Everyone’s Business: Proposals to reduce ill-health related job loss, published July 2019. ↩
-
This research was conducted with people in the ESA Support Group and people claiming UC with limited capability for work and work-related activity. See: Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. ↩
-
Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. ↩
-
Department for Work and Pensions, Claimant Service and Experience Survey 2018 to 2019, published 20 July 2020. ↩
-
Labour Force Survey, Oct-Dec 2013 to Oct-Dec 2019. ↩
-
DWP Benefit Expenditure and Caseload Tables, published March 2021. ↩
-
Real terms – ‘Real terms’ refers to a value that has been adjusted to take into account the effects of inflation. For example, if you see a text that says ‘adjusted for inflation, it means the value of something in ‘real terms’. You can think of real terms as being comparable to ‘today’s prices’, regardless of what year is reported. ↩
-
This figure includes expenditure devolved to the Scottish government calculated for working age health and disability benefits, derived from Benefit expenditure and caseload tables retrieved 25 May 2021. ↩
-
The responsibility for additional-needs disability benefits, including PIP and DLA, and for weekly-paid industrial injuries benefits, transferred to the Scottish Government in April 2020. The responsibility for Carer’s Allowance transferred in September 2018. ↩
-
Starting with the replacement for DLA for children in 2021. ↩
-
DWP will deliver PIP and DLA on the Scottish Government’s behalf until the Scottish Government has built the capacity to deliver its replacement benefits. This is on the same basis that these benefits are delivered in England and Wales. The SRTI rules applicable in PIP and DLA will therefore apply in Scotland until the new Scottish benefits have been introduced. ↩
-
Department for Work and Pensions, Claimant Service and Experience Survey 2018 to 2019, published 20 July 2020. ↩
-
Provided by Motor Neurone Disease Association. ↩
-
Adams L, Tindle A, Greevy H, Stroud S, Gooding O (IFF Research), Claimant views on ways to improve PIP and ESA questionnaires. DWP Research Report 1001; 2021. ↩
-
For 2020/21, we funded Citizens Advice and Citizens Advice Scotland for up to £39m. For 2021/22, we are funding Citizens Advice and Citizens Advice Scotland for up to £37.5m. ↩
-
Citizens Advice, Annual Report 2019/20. Citizens Advice Scotland, Help to Claim Universal Credit. ↩
-
Provided by Citizens Advice. ↩
-
For example, a survey of people claiming PIP found that 59% of people sought help to complete the PIP2 form. The most common source of help was a friend or relative (33%), followed by help from a charity or support group, a social care professional or from Citizens Advice: Source: Barry J, Blake M, Bridges L, Candy D, Carragher E, Duxbury K, Fowler H, Lambert C, Morris L (Ipsos MORI). Personal Independence Payment Claimant Research – Final Report. DWP Research Report 963; published September 2018. ↩
-
Research shows that existing advocacy provision is geographically variable and may not be accessible for everybody who needs it. For example: Ruth Townsley, Anna Marriott and Linda Ward / Norah Fry Research Centre at the University of Bristol. (2009) Access to independent advocacy: an evidence review – Report for the Office for Disability Issues. ↩
-
O’Connor, N (2017), Making an Impact: The Public Value of Citizens Information Services in Ireland Brown, B (2014), Without advocacy – I don’t want to think about that: A summary of research exploring the value of Independent Advocacy and examining current advocacy provision in Scotland, Scottish Independent Advocacy Alliance; Carlsson, H (2014), Advocacy changed my life: Research into the impact of independent advocacy on the lives of people experiencing mental illness, Scottish Independent Advocacy Alliance. ↩
-
Dr Karen Newbigging, Dr Julie Ridley, June Sadd. (2016) “Commissioning advocacy under the Care Act: Emerging good practice” pub. Social Care Institute for Excellence (SCIE). ↩
-
Research shows that advocacy can help empower people, build self-confidence and help them make informed choices. For example: Chapman, Melanie, Susan Bannister, Julie Davies, Simon Fleming, Claire Graham, Andrea McMaster, Angela Seddon, Anita Wheldon, and Bridget Whittell. (IMCA) “Speaking up about Advocacy: Findings from a Partnership Research Project.” British Journal of Learning Disabilities 40, no. 1 (March 2012): 71–80 and Ailsa Stewart and Gillian MacIntyre. (2013) Advocacy: Models and effectiveness IRISS Insight 20. ↩
-
HMRC legislation does not limit the VAT and insurance premium tax reliefs to the Motability Scheme but to a provider of leases to disabled people, that predominantly serves disabled people and is the recipient of a direct transfer of mobility components from DWP. DWP legislation only provides for the direct transfer of mobility components under arrangements made or negotiated by Motability. DWP does not limit who Motability can negotiate with so if they entered into arrangements with another supplier, that supplier could also receive the direct transfer of mobility components and the associated tax reliefs. Motability currently only contract with Motability Operations. ↩
-
The Department currently transfers the PIP and DLA mobility component of qualifying claimants directly to Motability and this helps reduce Motability Operations’ credit risk. The Motability Scheme also benefits from VAT and insurance premium tax reliefs granted by HM Treasury. The combination of the tax reliefs, direct benefit transfers and Motability’s economy of scale enables them to provide leases to disabled customers, that are estimated at 44% cheaper than comparative private leases. ↩
-
National Audit Office, The Motability Scheme, published December 2018. ↩
-
Provided by Motability. ↩
-
Department for Work and Pensions, Claimant Service and Experience Survey 2018 to 2019, published 20 July 2020. ↩
-
Improving Lives: The Work, Health and Disability Green Paper, published October 2016. ↩
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Waddell G, Burton AK. Is work good for your health and wellbeing, 2006. Public Health England; Movement into Employment: Return on Investment Tool: Estimation of benefits from moving an individual from unemployment into sustainable employment, Published October 2017. ↩
-
Department for Work & Pensions/Department of Health, ‘Improving Lives: The Future of Work, Health and Disability’, published November 2017. ↩
-
Previously published figures for Q1 2020 showed that, in the first three years of the goal (between Q1 2017 and Q1 2020), the number of disabled people in employment increased by 800,000. Data for Q1 2020 is currently under review therefore this figure is subject to change. However, figures for the previous quarter (Q4 2019) - which are not directly comparable but are unaffected by the issue - also show that the number of disabled people in employment has increased by 800,000 since Q1 2017. 2017 is used as a reference point because this is when the 1 million ambition was set. Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Difference between the proportion of disabled people in employment in January-March 2014 compared to January-March 2021. Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Health is Everyone’s Business: Proposals to reduce ill-health related job loss, published July 2019. ↩
-
Dekkers-Sánchez, P.M., Hoving, J.L., Sluiter, J.K. and Frings-Dresen, M.H., 2008. Factors associated with long-term sick leave in sick-listed employees: a systematic review. Occupational and Environmental Medicine, 65(3), pp.153-157. ↩
-
This change will affect people who are claiming ESA in the Work-Related Activity Group (WRAG) and people claiming UC with limited capability for work (LCW) and in the Intensive Work Search Regime. ↩
-
Maier R, Egger A, Barth A, Winker R, Osterode W, Kundi M, Wolf C, Ruediger H. Effects of short- and long-term unemployment on physical work capacity and on serum cortisol. International Archives of Occupational and Environmental Health. 2006;79(3): 193–8.; Hämäläinen J, Poikolainen K, Isometsä E, Kaprio J, Heikkinen M, Lindeman S and Aro H. Major depressive episode related to long unemployment and frequent alcohol intoxication. Nordic Journal of Psychiatry. 2005;59 (6): 486–491.; Voss M, Nylén L, Floderus B, Diderichsen F, Terry P D (2004) Unemployment and Early Cause Specific Mortality: A Study Based on the Swedish Twin Registry. American Journal of Public Health 94 (12): 2155-2161. ↩
-
Occupational health teams help keep people well at work – physically and mentally. Occupational health services can help keep employees healthy and safe while in work and manage any risks in the workplace that are likely to give rise to work-related ill health. ↩
-
HM Government, COVID-19 Mental Health and Wellbeing Recovery Action Plan, published 27th March 2021. ↩
-
Provided by DWP Press Office. ↩
-
See Annex B for further information on Access to Work and Disability Confident. ↩
-
Office for Budget Responsibility, Economic and Fiscal Outlook, published November 2020. ↩
-
Maier R, Egger A, Barth A, Winker R, Osterode W, Kundi M, Wolf C, Ruediger H. Effects of short- and long-term unemployment on physical work capacity and on serum cortisol. International Archives of Occupational and Environmental Health. 2006;79(3): 193–8.; Hämäläinen J, Poikolainen K, Isometsä E, Kaprio J, Heikkinen M, Lindeman S and Aro H. Major depressive episode related to long unemployment and frequent alcohol intoxication. Nordic Journal of Psychiatry. 2005;59 (6): 486–491.; Voss M, Nylén L, Floderus B, Diderichsen F, Terry P D (2004) Unemployment and Early Cause Specific Mortality: A Study Based on the Swedish Twin Registry. American Journal of Public Health 94 (12): 2155-2161. ↩
-
Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. ↩
-
Sanctions are a temporary reduction of benefit. ↩
-
Benson A, Buchanan T, Crowley J, Davies M, Marcinkiewicz A, Rantanen K, Thompson B, Windle K (NatCen Social Research). Evaluation of the Personal Support Package. DWP Research Report; 2021. ↩
-
Case Study Provided by Leeds Eastgate (a DWP Health Model Office). ↩
-
Case Study Provided by Leeds Eastgate (a DWP Health Model Office). ↩
-
Provided by DWP Employers, Health and Inclusive Employment team ↩
-
DEA Leaders support their team of DEAs to deliver the best possible help for disabled people and work externally with GPs, the NHS, organisations and charities to build strong working partnerships. ↩
-
Provided by SWS Good News Stories. ↩
-
Department for Work & Pensions/Department of Health, Improving Lives: The Work, Health and Disability Green Paper, published October 2016. ↩
-
Benson A, Buchanan T, Crowley J, Davies M, Marcinkiewicz A, Rantanen K, Thompson B, Windle K (NatCen Social Research). Evaluation of the Personal Support Package. DWP Research Report; 2021. ↩
-
Department for Work & Pensions, Employment & Support Allowance: Evaluation of pilots to support Work-Related Activity Group customers with an 18 to 24-month re-referral period, published January 2019. ↩
-
Provided by Seetec Plus. ↩
-
Provided by the Shaw Trust. ↩
-
Waddell G, Burton AK. Is work good for your health and wellbeing, 2006. Public Health England; Movement into Employment: Return on Investment Tool: Estimation of benefits from moving an individual from unemployment into sustainable employment, Published October 2017. ↩
-
The IPS existing trial areas in England are Sheffield City Region and West Midlands Combined Authority. ↩
-
Provided by South Cumbria First Step and Lancashire and South Cumbria NHS trust. ↩
-
People claiming ESA in the Work-Related Activity Group (WRAG) and people claiming UC with limited capability for work (LCW) who were not in paid employment took part in a survey where they were asked to what extent they would like to find paid employment in the future (either full- or part-time). A majority of these (64%) said they would like to work to a great or some extent. See: Benson A, Buchanan T, Crowley J, Davies M, Marcinkiewicz A, Rantanen K, Thompson B, Windle K (NatCen Social Research). Evaluation of the Personal Support Package. DWP Research Report; 2021. ↩
-
Waddell G, Burton AK. Is work good for your health and wellbeing, 2006. ↩
-
Office for Budget Responsibility, Welfare trends report. Published 23 March 2021. ↩
-
HM Treasury, Spending Review 2020, published 25 November 2020. ↩
-
For example, see: Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. See also: Benson A, Buchanan T, Crowley J, Davies M, Marcinkiewicz A, Rantanen K, Thompson B, Windle K (NatCen Social Research). Evaluation of the Personal Support Package. DWP Research Report; 2021. ↩
-
Provided by Maesteg/Porthcawl jobcentre. ↩
-
Support was provided by an external provider specialising in the delivery of Health and Wellbeing Workshops. ↩
-
Please note this includes people claiming the Universal Credit standard allowance, not just people claiming UC with a health condition. ↩
-
Department for Work and Pensions, Claimant Service and Experience Survey 2018 to 2019, published 20 July 2020. ↩
-
Between the introduction of PIP in 2013 and March 2020, 4.1 million decisions have been made after a PIP assessment. 9% of these decisions (370,000) have been appealed. Source: Department for Work & Pensions, Personal Independence Payment statistics to January 2021, published 16 March 2021. ↩
-
We have undertaken independent research to understand people’s experiences of the benefit claims process. For example, see Barry J, Blake M, Bridges L, Candy D, Carragher E, Duxbury K, Fowler H, Lambert C, Morris L (Ipsos MORI). Personal Independence Payment Claimant Research – Final Report. DWP Research Report 963; published September 2018. See also: Adams L, Tindle A, Greevy H, Stroud S, Gooding O (IFF Research). Claimant views on ways to improve PIP and ESA questionnaires. DWP Research Report; 2021]. ↩
-
Department for Work & Pensions, Government’s Response to the Independent Review of the Work Capability Assessment - year five, published February 2015. ↩
-
Cabinet Office, Key Performance Indicators (KPIs) for Government’s Most Important Contracts, last updated 26 November 2020, Data for April to June 2020. ↩
-
House of Commons Work and Pensions Committee, PIP and ESA Assessments: Seventh Report of Session 2017-19, published 14 February 2018. ↩
-
For example, between the introduction of PIP in 2013 and March 2020, 4.1 million decisions have been made after a PIP assessment. 9% of these decisions (370,000) have been appealed. Source: Department for Work & Pensions, Personal Independence Payment statistics to January 2021, published 16 March 2021. ↩
-
Please see the Green Paper evidence pack for further information. ↩
-
Please see the Green Paper evidence pack for further information. ↩
-
See the Green Paper evidence pack for further information. Analysis showed that only a small proportion of people receiving ESA/UC and PIP could be assessed through a single assessment without fundamental reform. A single assessment could mean some people having to attend a third type of assessment alongside a repeat WCA and a PIP award review. ↩
-
For those who meet the criteria for the support group and the LCWRA and have sufficient evidence to be entitled to the highest rates of benefit on paper. Everyone else gets a telephone or face-to-face assessment so that they have the chance to present more evidence in person. ↩
-
Marcinkiewicz A, Lucey G, Pinto C, Taylor I, Taylor B, Cheesbrough S (NatCen Social Research). Claimant experience of telephone-based health assessments for PIP, ESA and UC. DWP Research Report; 2021. ↩
-
The feedback on telephone assessments has so far been positive. 75% of people on PIP and 94% of people on WCA (94%) were ‘satisfied’ or ‘very satisfied’. 45% of people who had a PIP telephone assessment preferred this kind of assessment, while 42% preferred face-to-face and 13% had no preference. Where people had a WCA by telephone, 62% preferred telephone assessments, 23% preferred face-to-face and 15% expressed no preference. ↩
-
The outcome of an assessment may affect people’s satisfaction rates and the type of assessment they would prefer. The differences in satisfaction rates for PIP and WCA telephone assessments may be partly explained by differences in the percentage of benefit awards (or other outcomes) that were made following these assessments. See: Marcinkiewicz A, Lucey G, Pinto C, Taylor I, Taylor B, Cheesbrough S (NatCen Social Research). Claimant experience of telephone-based health assessments for PIP, ESA and UC. DWP Research Report; 2021. ↩
-
We refer to ‘award reviews’ on PIP and ‘reassessments’ on the WCA. ↩
-
See the 2019 Conservative Manifesto. ↩
-
Provided by Citizens Advice. ↩
-
As of November 2020, 130,000 people receiving ESA have been exempted from routine reassessments, out of 1,240,000 who had been assessed since the introduction of the Severe Conditions criteria. See Green Paper evidence pack. ↩
-
The assessor is a professional who has knowledge of how a person’s health condition can improve their ability to move towards work, who can support them in overcoming barriers to work, and who has an understanding of the world of work. ↩
-
Between January 2019 and February 2020. See: Department for Work and Pensions, Personal Independence Payment: Official Statistics to January 2021, published 16 March 2021. ↩
-
Provided by the DWP Decision Making Team. ↩
-
When lapsing an appeal, DMs must contact formal representatives in the first instance and in any event must speak to them before revising the decision. Where the representative is informal, the DM should contact the claimant first but should allow time for them to speak to their representative to discuss the new decision if they wish to do so, before revising the decision. ↩
-
When a decision has been made, a person can accept the decision but still feel as though they want to appeal it. If they do this, the person will go back to the beginning of the appeals process. A new appeal will begin and the appeal waiting time will start again. ↩
-
In April 2021, 97% of PIP special rules claimants were receiving the highest possible award. ↩
-
Findings from the Evaluation of the Special Rules for Terminal Illness process. ↩
-
These professionals included GPs, hospital doctors and registered nurses (including professionals working in a role such as advanced nurse practitioner, Macmillan nurse, clinical specialist nurse or a practice nurse with expertise in long-term condition management). ↩
-
Provided by the Motor Neurone Disease Association. ↩
-
Department for Work & Pensions, Department of Health, Improving Lives: The Future of Work, Health and Disability, published November 2017. ↩
-
Cabinet Office, Key Performance Indicators (KPIs) for Government’s Most Important Contracts, last updated 26 November 2020, Data for April to June 2020. ↩
-
Work & Pensions Select Committee, PIP and ESA Assessments, February 2018. ↩
-
For example, while most claimants understood what was being asked of them at their assessment (80%) and agreed that they had enough time to explain how their condition affected them (74%), fewer people agreed that the measurements and functional tests were relevant and appropriate (60%): Barry J, Blake M, Bridges L, Candy D, Carragher E, Duxbury K, Fowler H, Lambert C, Morris L (Ipsos MORI). Personal Independence Payment Claimant Research – Final Report. ↩
-
Adams L, Tindle A, Greevy H, Stroud S, Gooding O (IFF Research). Claimant views on ways to improve PIP and ESA questionnaires. DWP Research Report; 2021. ↩
-
Latest data on StatXplore: November 2020: 79% of initial assessment decisions, December 2020: 75% of initial assessment decisions on ESA now place people in the Support Group. See: Stat-Xplore ESA WCA tables. ↩
-
Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. ↩
-
Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. ↩
-
Between the introduction of PIP in 2013 and September 2020, 4.2 million decisions have been made following a PIP assessment. 9% of people (380,000) who received a PIP decision lodged an appeal and 4.7% (200,000) of those decisions were overturned at tribunal. ↩
-
For information about the WCA descriptors information please refer to: Centre for Health and Disability Assessments, Revised WCA Handbook, published 6th October 2020, pages 77-142 and pages 169-173. ↩
-
For information about the PIP assessment descriptors please refer to: Department for Work & Pensions, PIP Assessment Guide Part 2: the assessment criteria, updated 17 September 2020. ↩
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Provided by Citizens Advice. ↩
-
On the whole, people claiming PIP were happy with the role of the assessor. However, while 89% agreed that the assessor treated them with dignity and respect, a lower proportion (71%) agreed the assessor understood their form and supporting evidence. Among the quarter of people claiming PIP (26%) who found the assessment more difficult than they expected, the main reasons were that the assessment was stressful (42%) or the assessor was seen as unhelpful and/or unfriendly (24%). Source: Barry J, Blake M, Bridges L, Candy D, Carragher E, Duxbury K, Fowler H, Lambert C, Morris L (Ipsos MORI). Personal Independence Payment Claimant Research – Final Report. DWP Research Report 963; published September 2018. ↩
-
Provided by Bexhill jobcentre. ↩
-
Provided by Clitheroe jobcentre. ↩
-
To claim New Style ESA a person must have been paid and/or been credited with NI contributions in the last 2 to 3 years (employed or self-employed). ↩
-
Following the Welfare Reform Act 2012. ↩
-
Universal Credit replaces Child Tax Credit, Housing Benefit, Income Support, income-based Jobseekers Allowance (JSA), income-related Employment and Support Allowance (ESA) and Working Tax Credit. ↩
-
35% of people who received the maximum PIP award in January 2021 have mental health recorded as their main condition (ICD classification) receive the maximum PIP award. The corresponding figure on DLA in February 2013, prior to the introduction of PIP, was 6%. Stat-Xplore, PIP Cases with Entitlement and DLA: Cases in Payment retrieved 2 June 2021. ↩
-
Most new applications for ESA (IR) were stopped in December 2018 with certain exceptions allowing some people to continue to apply until 29 January 2021 Available at: Stat-Xplore retrieved 28 May 2021. ↩ ↩2
-
Matthew Oakley, The Social Market Foundation supported by Scope, Time to Think Again: Disability benefits and support after Covid-19, published February 2021. ↩
-
2017 Conservative Manifesto ambition of getting 1 million more disabled people into employment by 2027. ↩
-
Difference between the proportion of disabled people in employment in October-December 2013 compared to October-December 2020. Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
Office for National Statistics, Table A08: Labour market status of disabled people, published 18 May 2021. 2013 is often used as a reference point for disability employment data as this is when the latest definition/ time series began. ↩
-
For example, a survey of people in the ESA Support Group (and UC equivalent) found that 20% of people in the Support Group (ESA) had a desire to do paid work in the future. See: Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. ↩
-
Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. ↩
-
Department for Work and Pensions/Department of Health and Social Care. Work, health and disability green paper: data pack, 2016. ↩
-
Waddell G, Burton, K. Is Work Good for Your Health and Wellbeing? London: The Stationery Office; 2006. ↩
-
Real terms – ‘Real terms’ refers to a value that has been adjusted to take into account the effects of inflation. For example, if you see a text that says ‘adjusted for inflation’, it means the value of something in ‘real terms’. ↩
-
Based on an age-weighted estimate of the population of Great Britain using disability rates for age bands from the 2018/19 Family Resources Survey, in 2018/19, 14.4 million (21%) of people reported a disability. This represents an increase from 11.3 million (19%) in 2008/09. ↩
-
The number of people claiming a mental health condition as well as a disability has increased from 24% in 2016/17 up to 27% in 2018/19. ↩
-
Public Health England: Chapter 3: trends in morbidity and risk factors 2018. ↩
-
In GB in 2021/22, £4.8 billion (14%) of working age health and disability benefits (ESA, UC Health, PIP and DLA) were paid through contributions based benefits. £14.3 billion (43%) was paid in means tested benefits, while £14.4 billion (43%) is neither means tested nor contributions based. These figures include expenditure devolved to the Scottish government calculated for working age health and disability benefits, derived from Benefit expenditure and caseload table retrieved 28 May 2021. ↩
-
From 43% in 2013 to 47% in 2020. ↩
-
Provided by Citizens Advice. ↩
-
Some people felt that starting paid employment might jeopardise their financial position. This was related to a perceived ‘pay gap’: the period between benefit payments ceasing and the first pay cheque from a new job being received, as well as to the possibility that employment might not work out, resulting in people subsequently struggling to re-apply for benefits (or struggling financially while their application was being processed). See: Adams L, Cartmell B, Coburn S, Dobie S, Stroud S, Svanaes S, Tindle I (IFF Research). The work aspirations and support needs of claimants in the ESA support group and Universal Credit equivalent. DWP Research Report 983; published February 2020. ↩
-
Department for Work and Pensions, Claimant Service and Experience Survey 2018 to 2019, published 20 July 2020. ↩
-
While many charities and disabled people’s organisations have helped us in this process and are listed here, this does not mean that they necessarily agree with the content or proposals in this Green Paper. ↩
