Transcript: Prime Minister's speech to the Dementia 2012 conference
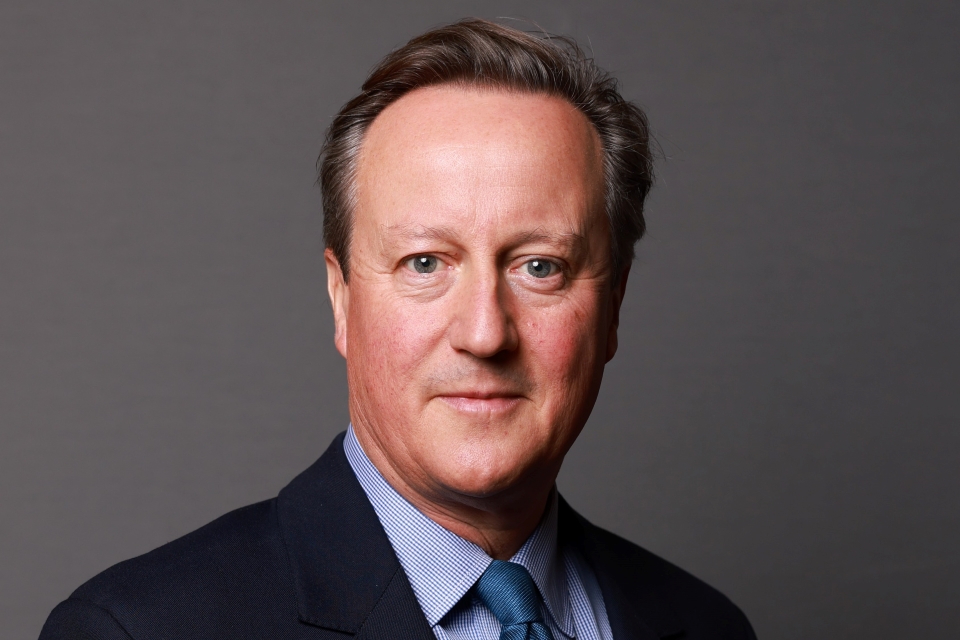
Prime Minister David Cameron's speech on dementia to the Dementia 2012 conference on Monday 26 March 2012.
Introduction
There are some challenges in our national life that get a lot of headlines, like the debt crisis.
But one of the greatest challenges of our time is what I’d call the quiet crisis…
…one that steals lives and tears at the hearts of families…
…but that relative to its impact is hardly acknowledged.
670,000 people in England are living with dementia today.
Each of these is someone like Enid Russell.
Twenty years ago Enid was diagnosed with dementia.
She’d been a mother, childcare worker and loving wife to George for many years.
George says that “she’s still the lovely Enid” he’s always loved….
…but - for the past four years - she no longer recognises her husband.
It is almost impossible to imagine seeing the one you love slip away from you while physically, they’re still there.
And every day, hundreds of thousands of these tragedies are playing out behind closed doors.
National fight-back
This is simply a terrible disease.
And it is a scandal that we as a country haven’t kept pace with it.
The level of diagnosis, understanding and awareness of dementia is shockingly low.
It is as though we’ve been in collective denial.
Already a quarter of hospital beds are occupied by someone with dementia.
Already the total cost of the disease is around £19 billion in England…
…that is higher than the costs of cancer, heart disease or stroke.
And in less than ten years, as we all live longer lives, the number of people with dementia will reach a million.
So my argument today is that we’ve got to treat this like the national crisis it is.
We need an all-out fight-back against this disease; one that cuts across society.
We did it with cancer in the 70s. With HIV in the 80s and 90s.
We fought the stigma, stepped up to the challenge and made massive in-roads into fighting these killers.
Now we’ve got to do the same with dementia.
This is a personal priority of mine, and it’s got an ambition to match.
That ambition: nothing less than for Britain to be a world leader in dementia research and care.
Misconceptions about dementia
Today I want to talk about what together we can do to get there.
But first I want to say something about the misconceptions surrounding dementia…
…because when you look at what’s held this country back from confronting this, you see a couple of big myths standing in the way.
There’s the myth that dementia is just an inevitable part of aging.
But it is not - it is caused by diseases like Alzheimer’s.
You can look at scans of the brain and see the physical impact it is having.
This is not age clouding the brain or forgetfulness.
It is a disease and we need to treat it as such.
Why has this held us back?
Because when something is shrouded in mystery, it tends to be taken less seriously, or it’s treated as inevitable.
That links to the second myth: that “nothing can be done”.
People often assume there are no drugs that can help, no coping strategies that work, no light on the horizon…
…so we’d better just shove it under the carpet as it’s too painful to contemplate.
But this does not do justice to the great strides that have been made.
There are points of light and hope.
There are medical developments.
There are many ways to make life easier.
National Dementia Strategy
So our challenge is to fight that ignorance and increase understanding.
Above all, to recognise that we can do much, much more both to treat dementia and to make life better for those who have it, and their families.
This is what our national dementia strategy is about.
We are ramping up the level of ambition…
…going further and faster across three areas.
First: making sure our health and social care systems are properly geared up to deal with this crisis.
Second: getting our whole society involved in the fight; communities, charities and businesses.
And third: radically stepping up research into cures and treatments.
Diagnosis
Let’s begin with the challenge in our public services.
The explosion in dementia has been a massive shock to the system in our NHS.
Every day doctors, nurses and health and care workers are doing a heroic job.
But there’s no doubt we’ve got to do better, right across the board.
That starts with better diagnosis.
Today only around 40 per cent of those with dementia know they have it.
Can you imagine if these were cancer diagnosis rates?
There would be a national outcry.
And dementia should be treated in just the same way…
…because just like most other diseases, it makes a real difference if you spot it early.
You can help people live independently for longer, even put the brakes on their decline.
Now some might say - that’s all very well, but the nature of this condition makes it difficult to diagnose.
Of course there are difficulties, but the evidence tells us we could be doing far better.
In Belfast diagnosis is at almost 70 per cent.
Here in England we’ve got neighbouring areas with massively different rates…
…in Sheffield 57 per cent; in East Riding - less than 80 miles away - it’s 29 per cent.
In the next few years I want to see a dramatic increase in these rates in every part of the country.
To help achieve that we’re doing a number of things.
Next year, every local area in the NHS will set out a clear, strong ambition for better diagnosis rates.
We’re going to run a major national awareness campaign…
…across TV, on our streets, in the press…
…telling people if they or their loved one is feeling worried about their memory then they should get it checked out.
And on top of that, from the age of 65, people are going to be made aware of memory clinics, of which there are hundreds round the country.
At their usual five-yearly health check, as well as when they normally see their GP, those at risk will be referred on - just as they would be with a heart problem.
Together with the Royal College of GPs we’re working to send a message to every surgery and clinic in the country that this is to be taken very seriously.
Hospital
We need that same surge of awareness running through our hospitals.
For someone with dementia, hospital can be a terrifying place.
The short term memory tends to go first.
That means the patient waking up in a place they don’t know.
They’re being examined by strangers. They’re away from familiar things.
All this is incredibly distressing.
Worse - it can accelerate their decline.
Shadia’s father was admitted to hospital with dementia.
Before arriving he was mobile, able to feed himself and could speak easily.
While in hospital he became bed-ridden, he was fed through a tube, then finally was unable to speak or move and passed away eight months later.
This is a tragic story. But it isn’t an isolated one.
The phrase that comes up time and again that people come out of hospital “a different person”.
So there are a couple of resolutions we’ve got to make.
We’ve got to make very clear that for people with dementia, hospital should be a last resort.
Our health reforms are going to help achieve that, by putting more power into the hands of clinicians.
Take the local doctor working in Devon.
She knows there are a few elderly ladies living in the village who have dementia.
She also knows that - as so often happens - they might forget to drink enough water, so they get dehydrated, get urinary tract infections and end up in hospital where they get worse.
But once she’s got the control over the budgets she’ll be in a better position to prevent that…
…to hire a local nurse to go into their homes and check they’re drinking enough water.
This is what we want more of: more thoughtfulness, more community care, more independence.
But of course there will be times when hospital is the only option.
That’s why the other resolution we’ve got to make is that care in hospitals and care homes must get much, much better.
The most important things in the NHS are not structures or systems.
They’re kindness. Care. Gentleness.
Nurses taking the time to chat to people, reassure them, ease their distress.
Making sure they have enough to eat and drink.
Every single patient with dementia has the right to be treated with that dignity and respect.
The best hospitals are already doing this. The rest need to catch up.
One of the ways we’ll make that happen is through getting the incentives right, and rewarding hospitals for providing good dementia care.
From next month - April 2012 - there will be a £54 million pot of funding on top of the normal tariff, to encourage hospitals to get to grips with dementia.
In the first year, that money - the so-called CQUIN payments - will be there for those who assess over-75 year-olds admitted to hospital to check for signs of dementia.
This isn’t some box-ticking exercise - it’s about actively trying to pick up people who may not realise they have dementia, so that they can be referred for diagnosis.
That’s the raising awareness stage.
Then from next year, we’ll have the raising standards stage.
The CQUIN payments will only go to those hospitals that show they are really stepping up to the plate on the quality of their dementia care.
That might be proper dementia training for nurses…
…or dementia-friendly wards with clearer signs and lights that are bright enough to make things less disorientating.
This is what our NHS has got to be…
…an institution that rewards excellence - that expects the very best - as though it were our own mother or father there in hospital.
Social care and carers
But without doubt, one of the biggest things we’ve got to get right in our public services is social care.
The overwhelming complaint today is helplessness.
People given little or no choice about the care they get at home.
In the dark about care homes.
And, of course, that real worry of losing control of the finances - even losing the home you’ve worked so hard for - in order to pay the care fees.
On the financial point, we know there are huge challenges.
We know people are suffering massive losses.
We are determined to do the right thing by these people…
…and when we publish the Care and Support white paper in the near future, we will be saying more about the wider reforms that are needed.
But here I want to say what we’re doing to improve the quality of care.
Put simply, our reforms are about ending the helplessness people feel.
Putting more power in their hands - so that just through the act of choosing; what care they have, what home they stay in - they can make things better.
So for those who get their care at home, we’re rolling out personal budgets and direct payments that put people in the driving seat.
I know from experience how incredibly frustrating it is when some distant official is telling you the kind of care package you need, where you should go and how it should be spent.
You think - hang on a minute - this is my family, my home, my life.
I know best what I need.
If it’s a different care agency people want - so be it.
If it’s a specialised kind of therapy - they should choose it.
We’re ending the nightmare of one-size-fits-all - and this is happening quite fast.
The most recent figures show almost 340,000 people were receiving their own personal budgets at the end of March last year.
By April next year, when personal budgets are available for everyone, that figure should have doubled.
This is a huge change that is already putting people with dementia - and their families - in control.
Another thing we’re doing to make life a lot easier is joining up the NHS and social care.
So often we hear how frustrating it is to give the same information over and over again, or nurses doing one thing, care workers another…
…when all people want is a system that works to accommodate them, not the other way round.
So this revolution in personal budgets is spreading to the NHS too.
We’re committed to offering them to 50,000 NHS continuing care patients by 2014, and we’re going to keep up that momentum - so more and more people get that tailored care they deserve.
The vision is for health and social care working much more seamlessly…
…social workers and GPs, nurses, care assistants and voluntary sector workers coming together around people to make sure their needs are met.
And for carers, we have done something else.
One of our very first acts in government, back when the coalition was formed, was a new respite fund.
£400 million to give these carers that breathing space that so often they desperately need.
This is about recognising, pure and simple, what an amazing thing these people do not just for their families, but for our country.
And for them - and those they care for - we need to put more power in their hands when it comes to care homes too.
We need a lot more information about what goes on.
Because when you think about it, it is quite ludicrous that you can get online and find out more about the hotel you’re going to stay in for a week than the care home your parent might live in for the rest of their life.
So to change that, two things are happening.
Ten of the most forward-thinking care providers - like Bupa and Barchester Healthcare - have come together to set out what good dementia care should look like….
… focusing on quality of life for people with dementia, not just the quality of care.
They’ve pledged to live up to these standards - and that’s going to be a badge of excellence, applying gentle peer pressure to all other care homes.
But to give these standards real bite, the other thing we’re doing is bringing in a whole new era of transparency in the care sector.
In the white paper we’re going to shine a light on the quality of care…
…in every care home and every home care agency.
There’s going to be feedback from family and friends. Hard information.
We’ve seen how transparency can transform public services and this is going to do the same for care.
Putting people in control. Forcing different providers to raise their game. An open, honest pursuit of excellence.
Whole society approach
So big new changes are coming in across our public services.
I wish this could be enough alone - that we could meet this challenge by focussing the NHS on dementia.
But the truth is we can’t.
Because dementia isn’t just about what happens in hospitals and care homes.
It’s about those with the condition getting confused about endless PIN numbers and passwords.
The carer almost breaking under the strain of holding down a job at the same time as looking after Dad.
The stigma people have.
As Philip Clarke, who has early onset dementia has said: “When you get diagnosed with Alzheimer’s suddenly you become a non-person…
…I’ve been an RAF officer and a university lecturer and suddenly the doctors are directing questions about me to my wife as though I’m not in the room.”
All these are problems our public services alone can’t reach.
So second, we need to go further and faster is in getting our whole society involved in the fight.
Already good things are happening.
Tesco has been working with the Alzheimer’s Society to run dementia road-shows.
HSBC are training up staff to recognise the condition and make banking a bit simpler accordingly.
Every day charities and volunteers undertake countless acts of kindness, like running dementia cafes where people can get together and get support.
This is just the kind of thoughtfulness we need much, much more of.
So we are issuing a call to action across society…
…for people to come forward and do more to help those with dementia.
Today I can announce that a whole load of businesses have already pledged their support - from Saga and Aviva to Lloyds, E:ON and Waitrose.
And communities are responding too.
The Alzheimers’ Society is leading a movement of dementia-friendly cities and towns across the country.
In Plymouth everyone from the Naval Base to the Raiders basketball team has joined forces.
Groups in York, Plymouth, Bradford, Sheffield, Leeds and Liverpool have come together to do their bit.
All this is incredibly heartening - and my message to everyone in this country…
…communities, businesses, individuals, charities, is that we need to see much more of it.
Research
Together we can help people live with dignity and live well.
But the ultimate goal has got to be prevention and cure.
That’s why going further and faster on medical research is our third big aim.
Too often the lack of a ‘wonder drug’ has led to defeatism, but huge advances have been made, with British scientists often leading the way.
After a hundred years of groping in the semi-dark, we’ve now got clear images of the brain.
…we have - thanks to research led by Britain - the clearest picture yet of the makeup of Alzheimer’s, opening the door to crucial treatment development.
Our work on the early detection of dementia is world-leading.
We have new ways to get drugs direct to the affected cells…
…and many other exciting breakthroughs.
At Eli Lilly UK they’re helping to take some of the clearest ever images of a live brain.
Just last month we heard the news that Aricept can be effective in the later stages of dementia as well as the early ones.
And we have something really exciting going on in this country today - the Bio Bank.
Already, 500,000 people have volunteered to take part.
That is half a million people who have provided blood samples, are regularly getting their blood pressure, vital signs, even their eating habits monitored, so we can join the dots and see how diseases like dementia get signalled really early on.
We want to use Bio-Bank to take brain scans of up to 100,000 people, allowing us to see the earliest stages of progression of Alzheimer’s and other diseases like never before.
Indeed, in the history of mankind we’ve never had so much information about what goes on in the brain.
There is hope - and I want Britain to be a world leader in turning that hope into something real.
We’ve got the first-class universities, the globally-respected doctors, a genuinely national health service.
All this gives us great advantages…
…but up to now, we haven’t made the most of them.
We currently spend over ten times more on researching cancer than we do dementia.
So today, I can make a big announcement on funding.
Though we are in a time when money is tight, this government has made a bold and important decision…
…to more than double the amount we spend on dementia research…
…from £26 million at the end of the last Parliament, to over £66 million at the end of this one.
Already we’ve got some of the world’s greatest research scientists working here and with this boost we want to see many more of them…
…attracted to this country in the knowledge that we are taking dementia seriously and we are putting our money where our mouth is.
Another major thing we’re going to have is a push for more people to get into clinical trials…
…more people getting that chance to get the very latest drugs.
Clinical trials have made a huge difference in the fight against cancer - and they can do the same with dementia.
Our ambition is this: at least 10 per cent of people with dementia should be able to take part in clinical trials - up around ten times from today.
Yes, this is ambitious - but like I say we have got to be…
…and in the coming years I want us to be working with countries across the world…
…collaborating on research, pooling the best talent, making this a global endeavour to find new treatments and cures.
Conclusion
So in hospitals and care homes, in communities, businesses and research labs I want a new energy to infuse this fight against dementia.
But to make sure this is a prolonged and winning fight…
…not just a spasm of well-meaning action…
…we have done something else: set up a dedicated Champion group for each strand of this strategy…
…to mobilise action, drive forward new ideas and to challenge and check that all these actions I’ve spoken about get done.
They’re headed by leaders with real experience in this field, from Dame Sally Davies to Angela Rippon and Sir Iain Carruthers…
…and in six months they are going to report back to me with progress.
Before this speech I met them and my message was clear: don’t stint on the ambition.
I want to see big ideas. Boldness.
And yes - hold our feet to the flames to get things done.
So though this is a painful subject, my message today is one of hope.
Increasingly people with dementia are being helped to live fuller lives.
On the horizon are new avenues for research.
And most importantly, there is that essential spirit of defiance that we in this room share…
…that together we’re not going to shrug our shoulders or be defeated by this…
…but instead we’re going to work relentlessly to improve lives, to help hundreds of thousands of families…
…to take the fight to dementia.