Alcohol and drug treatment in secure settings: statistics summary 2017 to 2018
Published 17 January 2019
1. Overview
This National Drug Treatment Monitoring System (NDTMS) statistics report presents information on specialist treatment interventions for drugs and alcohol misuse in secure settings during 2017 to 2018. The report contains information on adults (aged 18 and over) in contact with treatment services in prisons, including youth offender institutions (YOIs) for 18 to 21 year olds, and immigration removal centres (IRCs).
There is a separate section on young people receiving treatment within the children and young people’s secure estate, including welfare-only children’s homes.
Trend data on people receiving substance misuse treatment in these settings has been included for the first time.
Many people experience difficulties with, and receive treatment for, drugs or alcohol or both. While they often share many similarities, they also have clear differences, so this report divides people in treatment into 4 substance groups:
- opiate - people who are dependent on or have problems with opiates, mainly heroin
- non-opiate only - people who are dependent on or have problems with non-opiate drugs, such as cannabis, crack and ecstasy
- non-opiate and alcohol - people who are dependent on or have problems with both non-opiate drugs and alcohol
- alcohol only - people who are dependent on or have problems with alcohol but don’t have problems with any other substances
Figure 1: Numbers in treatment by main substance group: 2017 to 2018
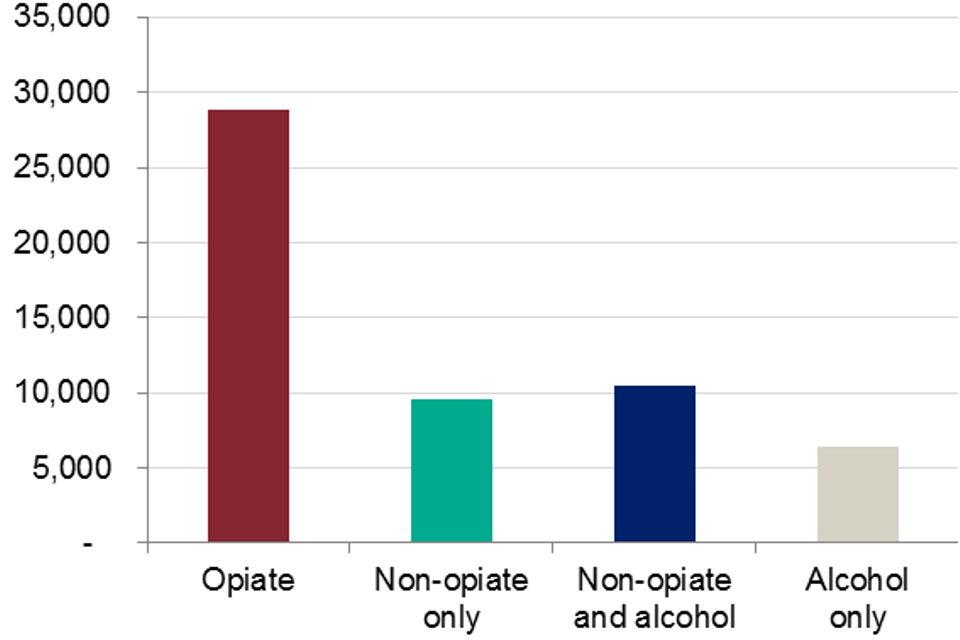
Bar graph showing the numbers of people in treatment in prisons by the four main substance groups in 2017 to 2018
Figure 2: Percentages in treatment by main substance group: 2017 to 2018
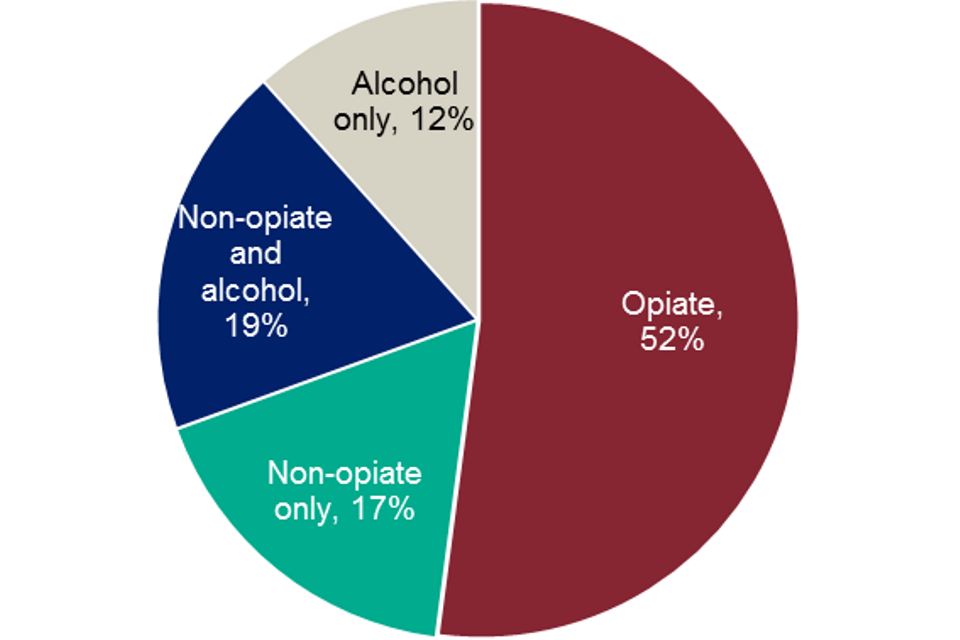
Pie chart showing the percentages of people in treatment in prisons by the four main substance groups in 2017 to 2018
2. Adults in secure settings
2.1 Numbers in treatment and substance use
During 2017 to 2018 there were data recording issues in some prisons in the West Midlands that resulted in an undercount of adults in treatment in that region. Because of this, the numbers of adults in treatment in England will also be undercounted and therefore it is not possible to make direct comparisons to previous years.
In 2017 to 2018, the number of adults (aged 18 and over) accessing treatment in a secure setting was 55,413. Most of those (96%, or 53,109) accessed structured treatment in a prison setting; either in a local, training, high security or open prison. People accessing treatment in prisons and IRCs were primarily treated for opiate use (53%, or 28,246, and 58%, or 318, respectively), while YOIs mostly treated those with non-opiate drug use (77%, or 1,353).
Just over half of all adults in treatment in a secure setting in 2017-18 reported problematic use of opiates (52%, or 28,859). Seven in ten opiate clients (70%, or 20,066) reported problems with crack cocaine and just over a fifth (21%, or 6,150) reported problematic benzodiazepine use. Nearly a third of opiate users also reported problems with alcohol use (31%, or 8,909).
After opiates, alcohol was the next most common substance (25,828, or 47% of adults in treatment). The majority (63%, or 12,674) of people in the non-opiate group were in treatment for problematic cannabis use (68%, or 6,552, of non-opiate only; 58%, or 6,122, of non-opiate and alcohol clients).
The next most common substances were powder cocaine (49%, or 5,126 of non-opiate and alcohol clients and 38%, or 3,646 of non-opiate only clients), followed by amphetamines (8%, or 1,636) and benzodiazepines (6%, or 1,147).
Almost one in ten adults in treatment said they had a problem with new psychoactive substances (NPS) (8.8%, or 4,868). This figure is the proportion of adults entering treatment with problematic NPS use and is not necessarily a reflection of overall NPS use in adult secure settings.
2.2 Age
As in community treatment, adults in treatment for alcohol only or opiate use in secure settings tended to be older than those treated for other substances. The median age of people in the alcohol only group at the first point of contact with treatment was 38 years and 36 years for the opiate group (46 years and 40 years in community treatment, respectively).
People in the non-opiate and alcohol and non-opiate only groups had median ages which were lower, at 30 years and 28 years respectively (the medians are 34 years and 30 years in community treatment).
2.3 Gender
Gender proportions in the total treatment population in adult secure settings were 90% male (49,791) and 10% female (5,622), double the proportion of women within the total prison population, shown in the HM Prison and Probation Service (HMPPS) offender equalities annual report. Problematic opiate use was reported by half of the male treatment population (50%, or 24,712). Almost three-quarters (74%, or 4,147) of women in treatment were being treated for opiate use.
2.4 Ethnicity
The largest ethnic group in treatment were recorded as white British (79%, 42,904). No other ethnic group made up more than 3% of the total treatment population, although 6% of those in the non-opiate only group were Caribbean (578).
2.5 Parental status
Information on the parental status of adults in treatment has been introduced in this report for the first time this year. Where reported, just over half of all adults (54%, or 28,682) were either a parent or had children living with them prior to coming into the secure setting. This is very similar to the parental status of people entering community treatment in the same period, where 51% were a parent or had children living with them.
2.6 Mental health
Information on whether a person in treatment has a mental health need has also been introduced into this report for the first time this year. The proportion of people entering alcohol and drug treatment who had a mental health need other than substance misuse, (which was identified and reported by healthcare services), was 32% (16,542).
The numbers ranged from 25% (2,242) in the non-opiate only group to 36% (9,694) in the opiate group. The proportion of people entering community alcohol and drug services who needed mental health treatment was 41% in the same period.
2.7 Time to start treatment
The median time between a person entering an adult secure setting and getting a triage assessment for substance misuse treatment was 1 day. Nearly all (96%, or 34,368) adults started their first treatment intervention within 3 weeks of being assessed but would usually start treatment immediately if it was clinically appropriate to do so.
2.8 Treatment interventions
The majority (61%, or 53,613) of treatment interventions received by adults in treatment were structured psychosocial interventions. The remaining interventions were pharmacological interventions: 26% (22,793) to address opiate use, 9% (7,952) for alcohol and 4% (3,119) to address other drug misuse. These would generally be provided alongside a psychosocial component to help support an individual’s recovery, as recommended by the UK drug treatment clinical guidelines.
Almost all people in treatment in secure settings (93%, or 51,559) in 2017 to 2018 received psychosocial interventions. 5% (2,705) received pharmacological interventions only and 2% (1,149) either did not start an intervention or an intervention was not recorded.
The majority of people (94%, or 25,725) were receiving continuous prescribing for less than one year, which reflects the relatively short periods they spent incarcerated. Overall, the average (median) length of continuous prescribing was 48 days but ranged from 8 days for people in the alcohol only group to 59 days for the opiate group.
2.9 Treatment exits and successful completions
The number of adults leaving treatment was 34,834. Around a third (30%, or 10,343) of those completed their treatment programme.
The lowest rate of successful completion was among opiate users (18%, or 3,060), compared with 41% to 44% for the other 3 substance groups. The majority of people in the opiate group discharged from treatment were referred to treatment services in the community on release (61%, or 10,593, of discharged opiate clients). A lower proportion of alcohol only (31%, or 1,434), non-opiate and alcohol group (24%, or 1,555) and non-opiate only group (23%, or 1,426) had the same referral to community treatment.
Dropout rates for people in treatment in secure settings, across all substance groups, were low (5% or less).
Continuity of care between treatment services in prisons and the community is monitored by the Public Health Outcomes Framework (PHOF) indicator 2.16. This indicator reported that in 2017to 2018, 32.1% of adult prisoners who needed ongoing treatment successfully engaged with community-based treatment within 21 days of release.
2.10 Deaths
There were 43 people who died while in contact with treatment services in a secure setting, which is less than 0.1% of all adults accessing treatment in the secure estate.
Over half (58%) of the 43 deaths were in the opiate group (25 deaths) and almost a third (30%) were in the non-opiate client groups (13 deaths). Females accounted for 5% (2 deaths) of the total deaths among adults in treatment.
2.11 Trends in adults in treatment in secure settings
Due to the data compliance issues in the West Midlands during 2017 to 2018 and the resulting national undercount, it is not possible to make direct comparisons to previously published data.
To be able to report more representative trends over time the West Midlands data has been removed from both the 2017 to 2018 adult data in this section as well as from the preceding years that are also reported here.
Adults in treatment
Overall, there was a 4.6% reduction of adults in treatment in 2017 to 2018 compared with the previous year. The majority of the decrease was seen within the non-opiate only (9%) and alcohol only (14%) groups. The HMPPS offender equalities annual report shows that there have been fluctuations in the overall male and female prison populations in 2017 to 2018 and the combined population of both was 3% lower on 31 March 2018 than it was on 31 March 2017.
Substance use by people starting treatment
There was a decrease in adults starting treatment in 2017 to 2018 (6% lower than the previous year). This decrease was seen across all substance groups; the largest falls being in the alcohol only and non-opiate and alcohol groups (14% decrease and 8% decrease respectively).
The proportion of people entering treatment in 2017 to 2018 who reported problematic crack cocaine use alongside opiate use has risen year on year (from 26% in 2015 to 2016 to 36% in 2017 to 2018), as has the proportion of those starting treatment for crack cocaine without opiates (from 5% in 2015 to 2016 to 7% in 2017 to 2018).
This increase mirrors a similar rise among people starting community treatment for crack cocaine use and opiate use within the same period (from 14% in 2015 to 2016 to 18% in 2017 to 2018) and the rise in the proportion of adults being treated for crack cocaine (but not opiate) problems (an increase of 1% between 2015 to 2016 and 2017 to 2018).
Conversely, the proportion of people entering treatment for opiate problems, who didn’t also have crack problems, has fallen year on year (from 22% in 2015 to 2016, to 14% in 2017 to 2018).
The proportion of people entering treatment for other substances has also decreased from last year, with the largest drops seen for people entering treatment for problems with alcohol (down 3%), cannabis (down 2%) and benzodiazepines (down 3%).
The number and proportion of people starting treatment in prison for new psychoactive substances (NPS) has continued to increase. Almost one in ten adults in treatment stated they had a problem with this in 2017 to 2018 (8.5%). The proportion has increased from 5.7% in 2015 to 2016 where 3,037 individuals reported problematic NPS use. This is the opposite to the trend in community treatment, where numbers in treatment for NPS have decreased from 2,728 in 2015 to 2016, to 2,074 in 2017 to 2018 (only 0.8% of the treatment population), a fall in volume of 24%.
These figures are the number of adults being treated for problematic NPS use and do not necessarily reflect overall NPS use in adult secure settings.
Treatment exits and successful completions
The proportion of adults leaving treatment after successfully completing their treatment free of dependence increased in 2017 to 2018 to 31% (from 28% in 2016 to 2017 and 24% in 2015 to 2016). Adults successfully engaging in community treatment within 21 days of release also increased to 32.1% in 2017 to 2018 (30.3% in 2016 to 2017).
Deaths
The number of adults who died while in contact with treatment services in 2017 to 2018 decreased 36% from 2016 to 2017, with all substance groups seeing falls. This decrease is in line with Ministry of Justice statistics which show decreases in the rate of male and female deaths per 1,000 prison population in 2017 (calendar year), and the total numbers of deaths in prison 17% lower than in 2016.
People with opiate problems have continued to be the most at risk, with over half of all deaths in treatment being in that substance group. However, the large numbers of deaths in the non-opiate and alcohol groups in 2016 to 2017 has decreased markedly, with a fall from 12 to 6 people in 2017 to 2018.
3. Young people in secure settings
There were 1,352 young people in specialist substance misuse treatment in secure settings in 2017 to 2018. The majority (72%) of young people in treatment in secure settings were in YOIs, with a further 16% in secure children’s homes, 6% in secure training centres and 5% in welfare only homes.
3.1 Age, gender and ethnicity
Approximately 92% of young people in treatment were male. Males tended to be slightly older (17 years) compared to females (16 years). Nearly two thirds (61%) were recorded as white British and white and black Caribbean was the next largest ethnic group (9%). Other groups represented no more than 4% of the total treatment population.
3.2 Substance use by young people
Cannabis was the most common substance reported by young people in treatment in secure settings (91% of all in treatment). Just under half said they problematic alcohol use (47%), followed by nicotine (22%), and powder cocaine (16%).
3.3 Time to treatment start
The majority (89%) of young people received a triage assessment within one week of arriving in a secure setting and, of those starting treatment, most (85%) started their first intervention within one week of triage.
3.4 Treatment interventions
Most young people starting treatment received a harm reduction intervention (85%). Motivational interviewing (52%) and relapse prevention (23%) were the next 2 most common interventions received. One percent of young people in treatment in secure settings received a pharmacological intervention.
3.5 Treatment exits and completions
Of the 931 young people in secure settings who left treatment nearly a quarter (22%) completed their treatment in custody. Half (50%) were released from custody and were referred for further treatment in the community while 14% were transferred to another establishment with the intention that their treatment would continue. Seven percent declined further treatment and the remaining 6% either dropped out or withdrew from treatment.
There were no deaths among young people in secure settings while they were in specialist substance misuse treatment.
