Health matters: health economics - making the most of your budget
Published 27 July 2018
Summary
This edition of Health matters focuses on local authorities, NHS commissioners and healthcare providers making better evidence-based commissioning decisions, and getting the most from their budget using easy to use health economic tools, resources and core principles.
Scale of the problem
Growing demands on the NHS, local authorities and wider society
The population of England has increased steadily over recent decades. At the same time the population has also been ageing and in 2017, the number of people aged 85 years and over was more than 3 times greater than it was in 1971. This increase is largely due to an increase in average life expectancy, which is a public health success story, and trends in the number of people born 85 or more years ago.
The number of people aged 85 years and over is expected to increase substantially in the future. As reported in the latest Health Profile for England, in 2017 there were 1.35 million people aged 85 and over in England. By 2031 (when ‘baby boomers’ born after World War 2 move into this age group) the figure could reach just over 2 million.
People are living longer than at the start of the century, but the increase in healthy life expectancy (or years spent in good health) has not kept pace with life expectancy. Therefore people are spending more years in poor health, particularly in the more deprived parts of the country. In the period 2014 to 2016, males lived 16.2 years in poor health, while females lived 19.3 years in poor health.
You can read more about this in this previous edition of Health matters on productive healthy ageing.
The current situation
Evidence shows that prevention and early intervention are effective in improving or maintaining health and represent good value for money. Not only do well-chosen interventions implemented at a scale help to avoid poor health and reduce the growth in demand on the NHS, they can also reduce pressure on other public services and support economic growth.

Through regular conversations PHE’s Health Economics team has with the NHS, local government and national government, they are regularly reminded of 2 points:
- firstly, health and social care budgets must work harder and harder, year on year, inevitably leading to conversations within the NHS and local government about which initiatives provide the best value for money or even save public money.
- secondly, there is still work to be done to demonstrate where health economics can be applied. This includes de-mystifying certain terms such as ‘ROI’, ‘cost-effectiveness’ and ‘cost-saving’ for the widest possible audience, particularly as the nature and level of health funding will continue to be a key public debate.
In recent years, there have been developments in the economic evidence related to public health, and there are a growing number of tools to translate this evidence into insight that can be applied for local systems and to inform national policy. PHE and the National Institute for Health and Care Excellence (NICE) have published a wide range of such tools and summaries of the available evidence.
Return on Investment
Return on Investment (ROI), in simple terms, encompasses the range of approaches that assess the value generated by an investment, compared to the resources put in.
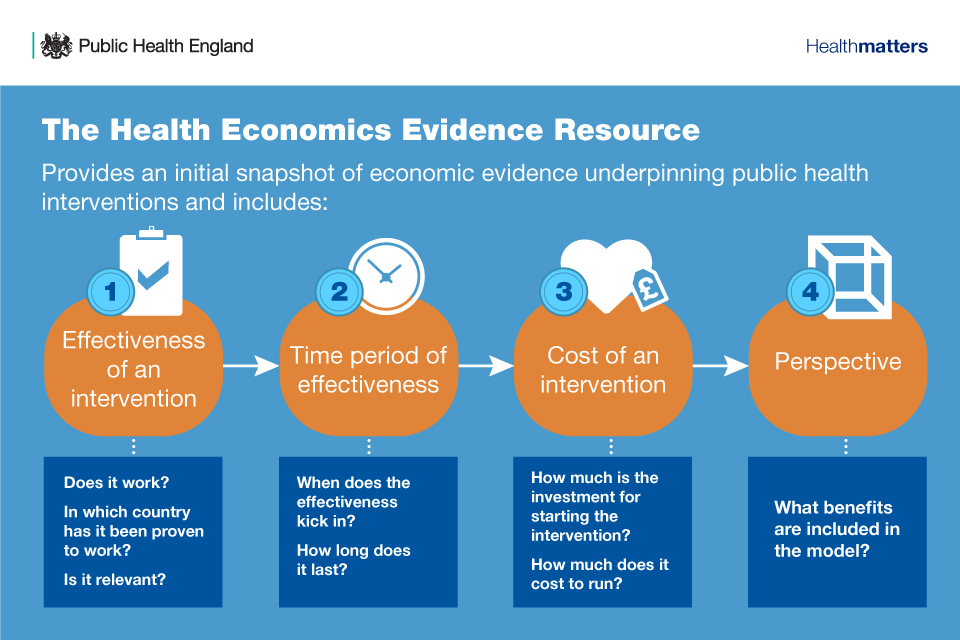
Whilst preventing people from becoming ill has an intrinsic value to individuals, families and society, there are some main building blocks that are required when undertaking any economic evaluation including:
- effectiveness – whether an intervention works, including looking at which countries and with which population groups it has worked to understand if it is relevant to your setting
- time period of effectiveness – when does the impact kick in and how long does it last?
- cost of the intervention - both the investment to set it up and the ongoing running costs, this will then help to assess the cost-effectiveness or ROI
- perspective of the analysis – specific costs and benefits are included and to whom, typically involves longer and broader societal perspective to quantify health benefits and place a value on these alongside other benefits
Adopting a societal approach for quantifying the cost of unhealthy behaviours allows us to consider all the potential impacts on society. This approach is also in line with guidance from HM Treasury’s ‘Green Book’, which sets out how to evaluate policies, projects and programmes.
Ideally, all the costs and benefits that fall on society and the economy as a result of unhealthy behaviours would be quantified, but this is not always possible. This is often due to a lack of data availability or a methodology to monetise specific impacts.
There is a common misunderstanding and misuse of the term ‘return on investment’ and its conflation with ‘cost saving’ to public services, usually the NHS. When the question “are public health interventions ‘cost-saving’?” is asked, it is often taken to mean “does the intervention deliver cashable financial savings to government budgets in the short term?”.
In 2017 PHE’s Chief Economist wrote a response to a paper which looked at this topic in depth – ‘Return on investment of public health interventions: a systematic review’. The response concluded that overall, PHE supports the conclusions of this review that public health expenditure is relatively cost-effective compared with healthcare expenditure, and that cuts to public health budgets represent a false economy.
These statements must be interpreted as relating to overall societal costs and benefits, including the value of long-term health benefits, as well as financial savings to government budgets.
Some public health interventions, such as the ‘Home assessment and modification falls prevention programme’ discussed below, can be ‘cost-saving’ in the sense of delivering short-term cashable savings to government budgets. However, most analysis into the ROI of public health programmes looks at overall social costs and benefits, which are longer-term savings.
It is important to understand that short-term cost savings are a high bar to set for public health interventions. Further, it’s not all about cost saving – the aim of public policy is not solely to achieve maximum savings to public sector budgets, but also to improve people’s health and wellbeing and reduce health inequalities.
Why is it necessary to make the economic case for investment in prevention?
Video: Why is it necessary to make the economic case for investment in prevention?
Overcoming the barriers to getting involved in health economics
There is also a common misconception that it is difficult to get involved in health economics, and that it requires being qualified in the subject area to apply the relevant techniques to decision making. This is certainly not the case, and there is a wide range of support available to dispel these myths, including those provided by PHE’s Health Economics team and support from local PHE Centres.
To help with the use of health economics resources and ideas, PHE has developed 2 e-learning modules, which provide an introduction to basic health economics. These modules were developed alongside Health Education England and are hosted on the e-Learning for Healthcare website. Registration is required to access the material, however, it is completely free.
By carrying out surveys and workshops in local areas, we can see that time constraints are a barrier to carrying out economic analysis. It is also clear that some colleagues have had negative experiences with ROI tools in the past, and therefore may see the process as over-complicated.
Over the last year or so, PHE has introduced a range of new health economics tools and reports and whilst we still strive to make further usability improvements, we believe they are more user-friendly than ever before.
Through dialogue with users, we are listening to what they find helpful and less helpful, and taking steps to improve our products. There are common themes and approaches to overcoming some of these barriers and increasing the use of health economics tools and resources that are not used enough, including sharing best practice among users. This would enable learning from others in terms of what has worked and what has not. The team are actively collecting these case studies, including those included as part of this edition of Health Matters.
Other things the team are doing to overcome these perceived barriers include:
- raising awareness of the tools and resources available
- improving the look and feel of the tools to be user friendly and intuitive
- running webinars to support the rollout of new tools and resources
- greater tailoring of results from the tools to be specific to local areas
- working with local PHE centres to ensure they are equipped to support users
- providing introductory Health Economics e-learning modules
Pressure on local authorities and commissioners
All local authorities and local public health teams are under budget pressures and are facing increasingly challenging decisions over what services to invest in and disinvest from.
It is known that this support is needed and that professionals want to make robust and transparent decisions, as local areas have asked PHE for support in making decisions across public health programmes. There is a demand for tools that help provide rationale and answer the question “how did you decide on investment or disinvestment decisions?”.
This is an important issue for local areas who want to reduce the need to make funding decisions based on historical spending trends, or the need to make disinvestment decisions based on reducing all programme budgets by the same percentage; which is commonly known as ‘salami slicing’.
Health economics forms an important part of the decision making process. If local people or organisations want answers on the way decisions were made, the use of health economics tools and processes can in part provide the necessary rationale and evidence base. However, there are of course other factors, such as equity, that must also be considered.
How to get the most from your budget
Changing needs and context mean that local authorities must frequently review which public health services they provide for their population. Whether the decision to be made is around particular interventions or a wider review of allocating resources across programmes, there are health economics resources that can help.
For decisions around specific interventions, going straight to the HEER and ROI tools (discussed below) may be the best option. However, for a wider review of how resources are spent across programmes, PHE’s Health Economics team recommends that public health teams should start with a coherent prioritisation process.
This process should involve questioning the current state of programmes being delivered, which programmes could offer greatest value, and analysing other considerations such as population needs, political acceptability, health inequalities, and links to the health system.
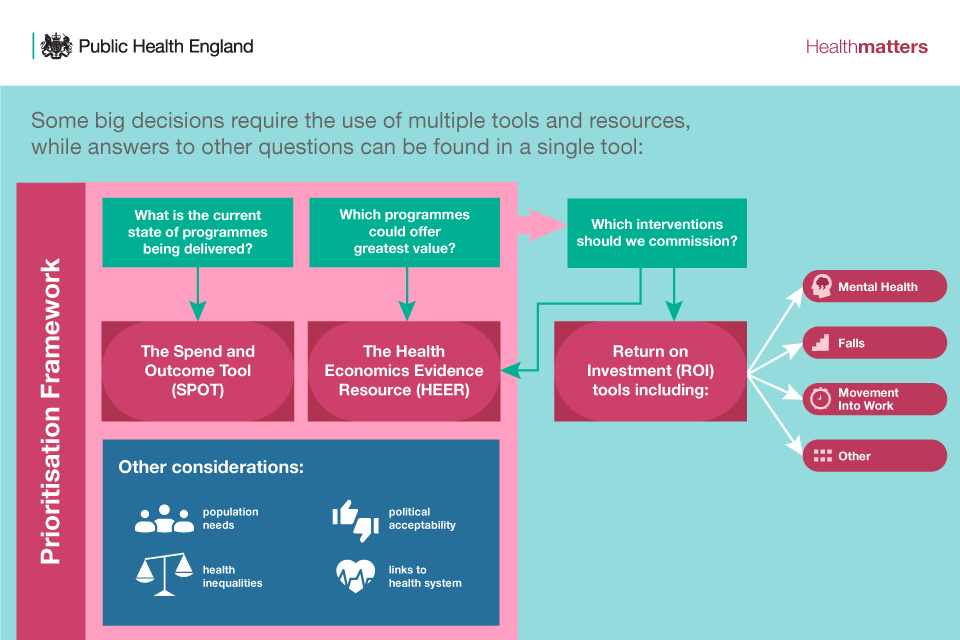
The Prioritisation Framework is the first resource that should be applied for initial guidance on which public health concerns and programmes to focus efforts, time and funds on.
The SPOT and HEER resources feed into the Prioritisation Framework to help answer some of the specific questions around current programmes, impact and value.
The Prioritisation Framework also allows for wider consideration, like those listed above, to be factored into decision making. After the Prioritisation Framework has helped areas consider how to use their budget at programme level, the ROI tools for specific topic areas should be used to identify the cost-effectiveness of particular interventions, and therefore which interventions should be invested in or disinvested from.
What health economic tools and resources have PHE made available?
Video: What health economic tools and resources have PHE made available?
The following sections discuss the details of these health economics resources, and how they can each help in making commissioning decisions.
Prioritisation Framework
What it is and how it works
PHE developed the Prioritisation Framework as a planning tool to help local authorities and decision makers make transparent, evidence-based spending decisions on how to split their budget across multiple public health programmes. The new Prioritisation Framework was published in March 2018.
The framework doesn’t prescribe how budgets should be allocated between programmes but instead allows users to break down big decisions into smaller manageable pieces. The framework also offers a structure through which open, frank and evidence-based discussions can take place between multiple stakeholders.
This greatly simplifies the process of undertaking a systematic prioritisation exercise and ensures that the resulting recommendations are backed by consensus.
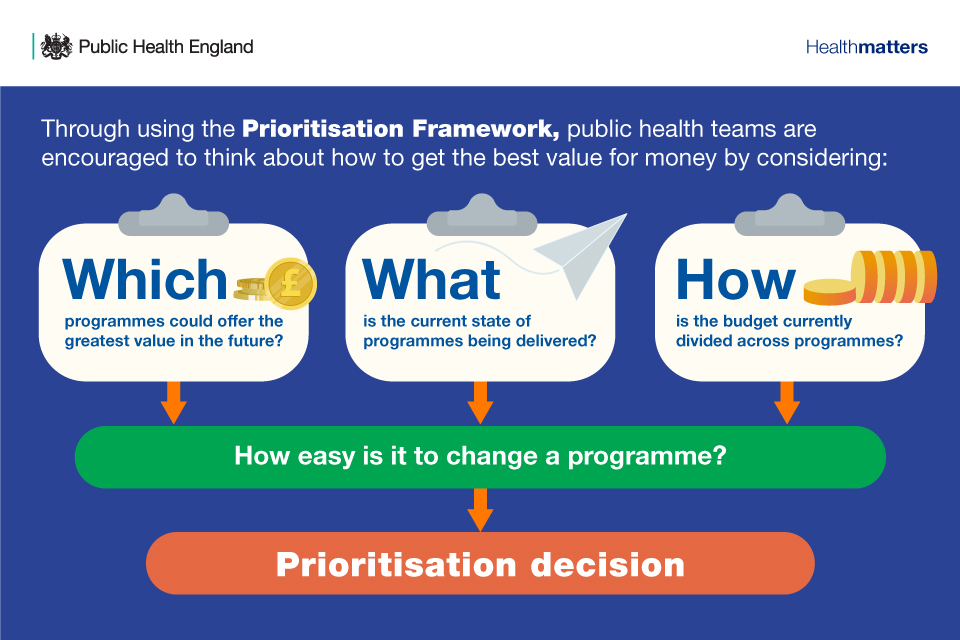
By using the framework, public health teams are encouraged to think about how to get the best value for money by considering:
- potential – what value could be achieved and which programmes could offer the greatest value in the future?
- current – what do our programmes look like relative to those in other comparable areas?
- budget – how do we use our resources at the minute?
Strategic, operational and political considerations are then brought into play to determine which changes are feasible to make. The final outcomes are recommendations on whether to increase, decrease or maintain spend in each programme area, underpinned by a strong supporting narrative developed over the course of the process.
Understanding the ‘potential’ and ‘current’ state of public health programmes is done through multi-criteria decision analysis (MCDA). MCDA might sound complicated, but it is actually a way of simplifying decision making by explicitly defining what you are trying to achieve, how important each outcome is relative to others, and how well options move you towards your goal.
MCDA is a recognised technique that has been used extensively by organisations around the world, both in health but also much more widely. Further guidance on MCDA can be found in this guide from the Ministry of Housing, Communities and Local Government.
Why it is needed
To simplify the increasing burden and complexity of decision making that local authorities and commissioners are facing, the Prioritisation Framework helps to build a consensus so that when investment decisions are made, they are based on a clear set of criteria. Also, if local areas need to disinvest or re-allocate funds, then the framework can provide clarity and transparency on how these decisions were taken.
How it was developed
The idea to develop the Prioritisation Framework emerged in 2015 when Directors of Public Health from the North East asked their local PHE Centre for support to identify areas where public health spending could be reduced, in a transparent manner that ensured the best outcome for local people. The resulting process was implemented and developed by South Tyneside and Gateshead local authorities.
Since then, PHE has been working with a number of local authorities to co-produce a tool which captures and builds on that approach; the Prioritisation Framework. This included initial conversations about the functionality of the framework, in-depth interviews after a prototype was developed, and finally live-testing in 4 areas.
How it works in practical terms: using the Prioritisation Framework in your area
A small team of people are needed to commit to supporting the prioritisation process. A ‘process owner’ (usually a senior member of the public health team) needs to take responsibility for leading the process and completing the Prioritisation Framework.
A commitment of around 5 months is required to complete the process, although experience of local authorities who have conducted a prioritisation exercise suggests that it requires 5 to 10 days of a person’s work, spread across the team.
To help areas use the framework, local PHE Centres can provide advice and assistance with various activities, including:
- getting you up to speed with the principles of prioritisation
- planning how to conduct the process locally
- providing ongoing advice throughout the exercise
- connecting you with other areas which have already undergone the process
As more local authorities use the framework, PHE’s national Health Economics team will assess the types of guidance and support that are most helpful. However, it is important to note that the new Prioritisation Framework does not require in-depth health economics knowledge as it’s very much a strategic tool.
The Prioritisation Framework tool contains extensive guidance to help local areas complete each stage. To further assist teams who use the tool, PHE has produced a range of guidance and worked examples, which are available on request from the Health Economics team by emailing healtheconomics@phe.gov.uk.
Several local authorities who have used the Prioritisation Framework summarised their experiences in a recently recorded webinar below.
SPOT: Comparing spend and outcomes
The Spend and Outcome Tool (SPOT) is an interactive product that allows both local authorities and clinical commissioning groups (CCGs) to see how much is being spent, and the outcomes across a range of public health interventions, as well as wider areas of spend such as education, housing and roads. This allows comparisons to be made across public health programmes, which might be used as part of a prioritisation exercise. The SPOT tool also allows comparisons against other local authorities or CCGs.
SPOT does not estimate value for money or ROI, although it can be used alongside ROI tools. Instead, the tool provides insight and understanding of the relationship between spend and outcomes by identifying areas where there is a significant variation that warrants further investigation.
By using SPOT, public health teams and commissioners can:
- compare spending and outcomes against that of other local authorities or CCGs
- look at spend against a selection of outcomes across public health interventions and frameworks, including the Public Health Outcomes Framework
- identify programmes with outcomes that are significantly different to similar local authorities or CCGs, which may need more analysis
- use the tool alongside ROI and health economics tools
SPOT was updated in June 2018, and a video introduction to the use of it is available on the SPOT website.
Health Economics Evidence Resource (HEER)
The Health Economics Evidence Resource (HEER) tool is an interactive resource where economic evidence is collated and summarised by PHE’s Health Economics team. The HEER shows the best available evidence on the cost-effectiveness and ROI of interventions from published literature that is quality assured by PHE, to help both locally and nationally in developing the economic case for investing in prevention.
The HEER is an initial snapshot and currently focuses on the areas of the public health grant, but there are plans to update and expand this resource.
Each piece of evidence is summarised across over 20 criteria to provide details on how the results were created and to highlight the inputs and assumptions used in the original studies. This allows users to understand the relevance and apply the evidence to their local setting. Users can search the tool on any of these criteria to browse and refine the evidence most relevant to their needs. Outputs from the tool can also readily be downloaded in a PDF format for use elsewhere.
The cost-effectiveness of specific topic areas
PHE’s Health Economics team has produced a number of resources that can be used to estimate the value of investing in prevention and early diagnosis in your area. The best available evidence on costs, savings, and health benefits for specific topic areas in a single place is pulled together, thus simplifying the process of commissioning cost-effective services. These tools allow local areas to see what the impact of scaling up or rolling out new interventions for their specific population.
The following section covers three interactive ROI tools produced by PHE:
- mental health service
- falls prevention
- movement into employment
Additional tools are currently in development, and information on the other available interactive tools can be found here.
These include:
- Colorectal cancer
- NHS Diabetes Prevention Programme
- End of life care
- Weight management
- Oral health in pre-school children
- Musculoskeletal conditions
- Best Start in Life
- Air pollution
1. Mental health service
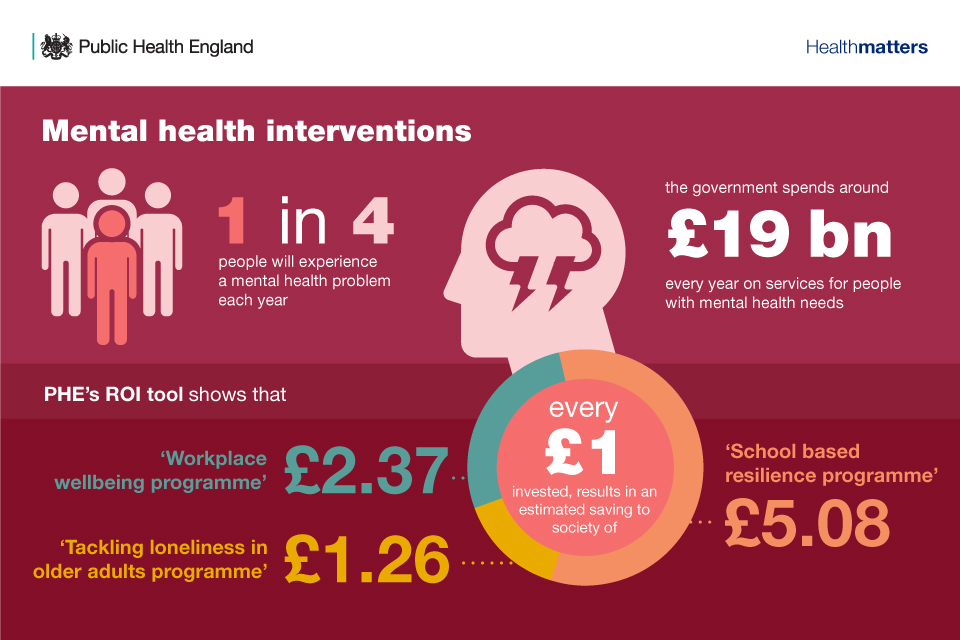
In the UK, approximately 1 in 4 adults experience at least one diagnosable mental health problem in any given year, and 10% of children aged 5 to 16 have significant mental health difficulties.
The health, social and economic consequences of poor mental health are substantial. In England, the government spends around £19 billion every year within and beyond the health system on dedicated services for people with mental health needs. The NHS alone spent almost £9.2 billion in 2015 to 2016 on mental health problems, and the mental health planned spend at CCG level was 12.5% of their overall budgetary allocation in 2015 to 2016.
Many people who have poor mental health also have other physical health problems, which accrue further social and economic consequences. Further, those with poor mental health experience reduced chances of being in employment or finishing school, college or university, and it increases costs in places such as schools and workplaces.
These substantial impacts mean that there is a strong economic case – as well as a health and moral case – for investing in actions to promote better mental health and reduce the risk of developing mental health problems.
There is clear evidence proving that a range of prevention activities promote good mental health and reduce some of the impacts of poor mental health. These actions have also been shown to be cost-effective as a good way of spending money on activities that improve health outcomes, that is, they yield a good ROI. This evidence is summarised in PHE’s commissioning report.
1.1 PHE’s ROI tool
PHE has a mental health promotion ROI tool, which:
- builds on the evidence in the commissioning report on cost-effective services for promotion of mental health and wellbeing and prevention of mental ill-health
- can be adapted to local conditions
- presents results showing the economic benefits of each intervention
The tool reports the ROI to health and other sectors from investment in 8 different interventions, and results can be tailored to local settings.
These interventions include:
- KiVa bullying intervention, which addresses bullying targeted at children and young people
- school-based resilience programme
- workplace wellbeing programme, which promotes mental health and wellbeing in the workplace
- workplace stress intervention, which prevents stress, depression and anxiety problems
- protecting the mental health of people with long-term physical health problems such as diabetes and heart disease
- addressing loneliness to protect the mental health of older people
- providing debt advice to protect mental health
- suicide and self-harm prevention
PHE’s primary focus is the health and social care perspective, including benefits relating to reduced impacts of co-morbidities if these can be identified, but it is also important to be aware of wider public purse and societal perspectives.
The suite of ROI resources that support local commissioners in designing and implementing mental health and wellbeing support services can be found here. The commissioning report provides details on the interventions listed above, and the tool guide provides users with step-by-step instructions and guidance on how to use the tool.
These resources can also be used by local authorities, CCGs, Health and Wellbeing Boards and their local partners (for example schools, employers, police) to improve the provision of mental health services.
1.2 Findings
On a national level, some of the main findings from the tool are that for every £1 invested, there is an ROI of:
- £1.58 for the KiVa bullying intervention
- £5.08 for the school based resilience programme
- £2.37 for the workplace wellbeing programme
- £2.00 for the workplace stress intervention
- £1.52 for the intervention protecting the mental health of people with long-term physical health problems
- £1.26 for the intervention addressing loneliness in older people
- £2.60 for the programme providing debt advice
- £39.11 for the suicide prevention intervention (over 10 years)
2. Falls prevention
Falls are very common, with around a third of people aged 65 and over experiencing a fall each year, increasing to half of those aged 80 and over. In around 5% of cases, a fall leads to fracture – one of the most serious MSK problems seen in the older population – and hospitalisation. This is very costly for health services and the wider economy, as well as having a detrimental impact on the health and independence of the individual.
There are around 255,000 falls-related emergency hospital admissions in England among patients aged 65 years and over each year. Further, an audit by the Royal College of Physicians found that fractures and falls in people aged 65 and over account for over 4 million hospital beds each year in England. It is estimated that fragility fractures cost the UK around £4.4 billion, of which 25% is for social care.
Therefore, preventing falls is important for helping to maintain the independence and wellbeing of older people and their carers, as well as our health and social care services.
2.1 PHE’s ROI tool
This is why PHE developed a falls prevention ROI tool, which will help to assess ROI for a number of falls prevention interventions for older people where there was supporting evidence around both clinical and cost-effectiveness. People involved in local policy setting and commissioning, as well as those leading falls programmes in local government, can use the tool to report the ROI for a number of interventions to support investment in falls prevention in their area.
The tool allows the user to select one of the following 4 interventions and input information specific to their area to calculate the ROI:
- Otago Strength and Balance programme
- Falls Management Exercise (FaME)
- Tai Chi or Tai Ji Quan
- Home Assessment and Modification (HAM)
As with all of the ROI tools, it’s only possible to include interventions where there is sufficient clinical and/or cost-effectiveness evidence needed to support the analysis.
2.2 Findings
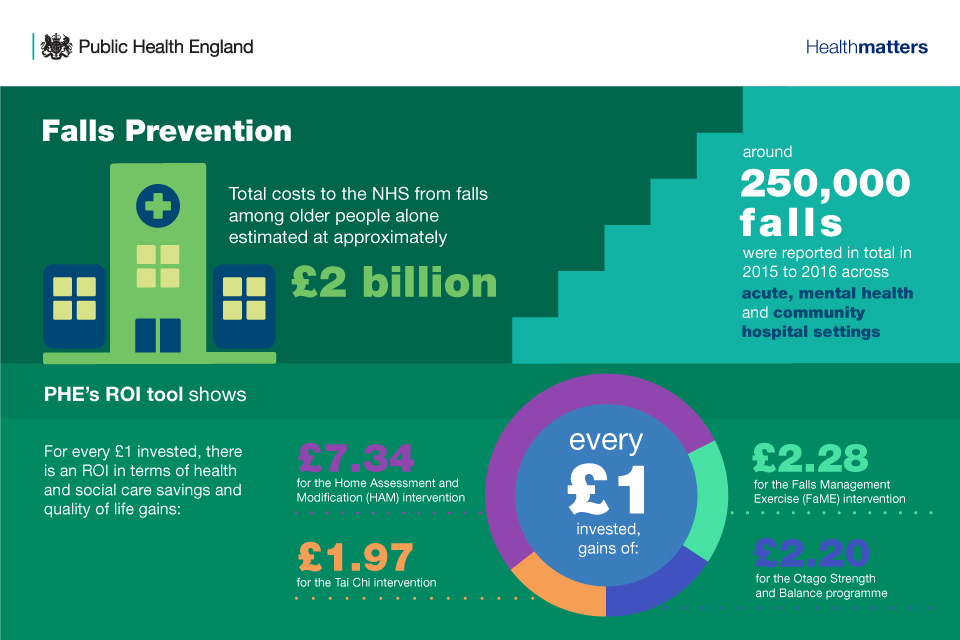
On a national level some of the main findings from the tool are:
- every £1 spent on the HAM intervention saves around £3.17 on health care and social care costs
- two of the interventions, Otago and FaME, virtually achieve financial breakeven – they fall just short of saving as much as they cost to deliver with ROI of £0.95 and £0.99 respectively
- when the quality and quantity of life is considered, all interventions have a positive ROI – for every £1 invested, there is an ROI in terms of health and social care savings and quality of life gains of:
- £7.34 for the HAM intervention
- £2.28 for the FaME intervention
- £2.20 for the Otago Strength and Balance programme
- £1.97 for the Tai Chi intervention
All of the interventions differ in terms of the populations they target. The HAM intervention achieves the greatest ROI, which may be explained by the fact it targets those who have already experienced a fall and therefore are at higher risk of falling.
3. Movement into employment
Unemployment is a significant factor that affects individual wellbeing, with negative impacts going beyond the effects of income. Being out of work is damaging to health and wellbeing, regardless of age, gender, ethnicity or region, and the longer period of unemployment, the worse the impact, according to the What Works Centre for Wellbeing.
There is a significant body of evidence specifically on mental health, showing a decline due to unemployment. However, on the contrary, mental health problems, whether work-related or not, are a key cause of worklessness.
One in four adults experience poor mental health each year, and half of those claiming Employment and Support Allowance do so on the basis of a mental health claim. As a result, mental health is a mainstream issue for our welfare system.
There are economic and social arguments that work is one of the most effective ways to improve the wellbeing of individuals and their communities, and a healthy population is one that has the potential to be a healthy and productive workforce for industry. This, and the fact that combined costs from worklessness and sickness absence amount to over £100 billion annually, make a strong economic case for greater action.
There has been some progress over the past 5 years, with the evidence base developing around which health and work interventions are most likely to have an impact and how cost effective they are. However, better investment in tackling worklessness will likely lead to better outcomes for the individuals transitioning into employment, their families and their wider local communities. An effective programme that helps individuals to move into work cannot be designed without addressing the impact of poor mental health on the ability of many to find work.
It is important that health and work are seen as 2 sides of the same coin. Whilst being in work is beneficial to our mental and physical health and wellbeing, good health is important to allow individuals to obtain and remain in employment, and to be happy and productive within the workplace. Having a healthy workforce greatly benefits communities and businesses as it leads to positive labour market outcomes, including productivity and reduced absenteeism. Helping people with health issues to move into and stay in employment is a significant part of the economic success and wellbeing of every community.
3.1 PHE’s ROI tool
PHE’s movement into employment ROI tool is an interactive tool that supports the case for investment in Health and Work interventions at local level, for commissioning organisations such as:
- local authorities
- CCGs
- Jobcentre Plus
- charities and others
The tool supports both local commissioners and national policymakers to assess the health and financial benefits for individuals, the exchequer and wider society of helping people in their area back into work. This subsequently aids both those considering implementing interventions in order to help people move from unemployment or economic inactivity to employment and those who are attempting to make the case for investment in this area. It also enables commissioning organisations to work together to commission interventions that will support those with poor mental health into employment.
Find out more about how the tool was constructed and its main findings in PHE’s Estimation of benefits from moving individuals into employment report.
3.2 Findings
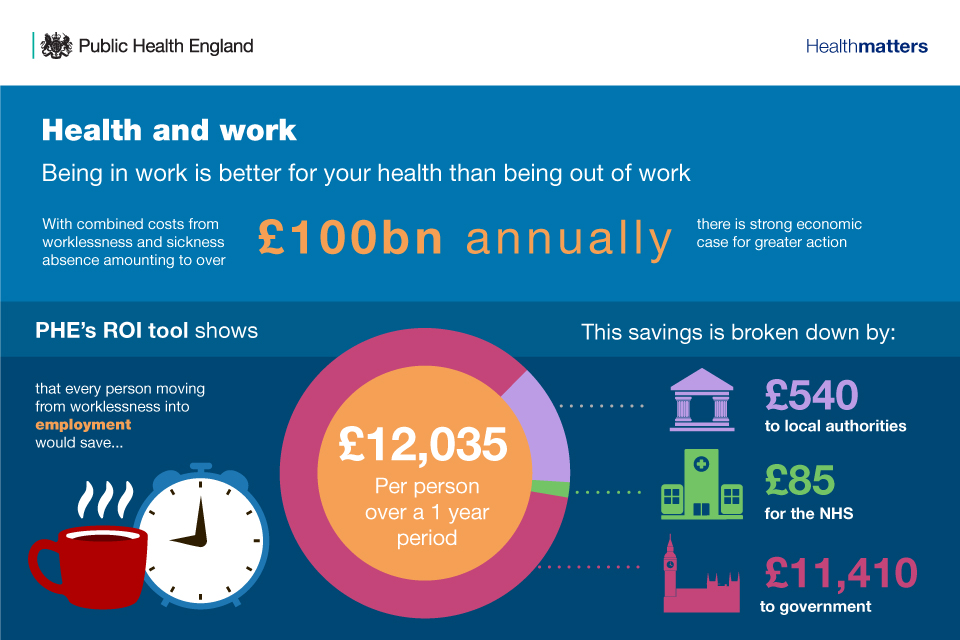
On a national level, some of the main findings from the tool are that for every person moving from worklessness into employment, £12,035 is saved over a 1 year period and this is broken down by:
- £11,410 to government
- £540 to local authorities
- £85 for the NHS
Where we are now versus where we want to be
The current situation local authorities, in particular, are facing involves increasing budget constraints and challenging decisions over which public health programmes to invest in and disinvest from. As such, these teams often still have to rely on looking at historical spending trends and salami slicing of budgets as means of making commissioning decisions. There are also factors such as political pressures and perceived barriers to getting involved in health economics, which push them to make decisions that are not necessarily the most beneficial for the health of their population.
What we would like to move towards is local authorities and their public health teams, NHS commissioners, and healthcare providers being able to make commissioning decisions that are evidence-based, transparent and defensible. PHE’s Health Economics team is continuing to develop resources that help provide the rationale behind these decisions and guide decision makers towards commissioning in a manner that leads to the most impactful outcomes.
We would like to see more and more local public health teams adopting these tools in their prioritisation and commissioning processes, and providing PHE’s Health Economics team with feedback as to how they have helped and how they can improve.
Who do we need to influence when making the case for investing in prevention?
Video: Who do we need to influence when making the case for investing in prevention?
PHE’s Health Economics team will have a stand at the PHE Annual Conference on 11 and 12 September 2018. Please visit the stand to find out more about any of the health economics tools and resources directly from the members of the team.
Resources
Download supporting references.
Download the Health matters infographics.
Read the Health matters blog.
Watch Health matters videos.
Read case study: Use of health economics tools by Shropshire Public Health.
Read case study: Public Health Budget Prioritisation in Durham.
