Health matters: delivering the flu immunisation programme during the COVID-19 pandemic
Published 29 September 2020
Summary
This edition of Health Matters focuses on the national flu immunisation programme and the delivery of the 2020 to 2021 programme. This will be the largest national flu immunisation programme to date offering 30 million people a vaccine. This edition also covers co-infection of flu and COVID-19 and provides calls to action for the wider health economy and local authorities as we prepare for the first winter with co-circulation of flu and COVID-19.
The UK’s flu immunisation programme
The impact of flu
Flu occurs every winter in the UK and is a primary factor in NHS winter pressures. It impacts on those who become ill, the NHS services that provide direct care, and on the wider health and social care system that supports people in at-risk groups.
For most healthy people, flu is an unpleasant but usually self-limiting disease with recovery generally within a week. However, there is a higher risk of severe illness from flu for some at-risk groups, including:
-
older people
-
the very young
-
pregnant women
-
those with an underlying condition, such as chronic respiratory or cardiac disease
-
those who are immunosuppressed
-
people with a learning disability

An analysis by PHE of data from fatal flu cases in England during the 2010 to 2011 flu season gives an indication of the increased risk of death from flu complications for those in clinical risk groups.
Every year, flu has a major impact on the NHS during winter months and puts particular pressure on the urgent and emergency healthcare system. Between 2015 to 2016 and 2019 to 2020, over 11,000 people died from the flu annually in England, with the figure ranging from almost 4,000 deaths in the 2018 to 2019 season to more than 22,000 deaths in the 2017 to 2018 season.
Flu vaccination is one of the most effective interventions available to reduce pressure on the health and social care system each winter.
The aim of the programme
The aim of the annual national flu immunisation programme is to offer protection against flu and its complications to as many eligible people as possible, particularly those most at risk. All eligible groups should be vaccinated as soon as possible to ensure that they are protected before the flu virus circulates.
Protection can be achieved directly through individual immunisation, or indirectly through herd immunity, which is one of the major benefits of the childhood flu immunisation programme. Improving and extending the childhood programme is a primary focus in protecting the population from flu.
Another significant focus is ensuring that frontline health and social care workers are vaccinated.
Flu surveillance
Flu surveillance in the UK is undertaken throughout the year and collated by PHE’s Influenza Surveillance Team on behalf of the UK countries.
Weekly outputs are published between October and May. These collate data from a variety of sources to provide information on:
-
circulating flu strains
-
timing of flu activity
-
antiviral resistance
-
flu vaccine uptake (in-season and end-of-season)
-
vaccine effectiveness
This is also done to provide rapid estimates of flu-related burden within the community, on the NHS, and excess all-cause mortality.
Flu vaccine uptake
England’s flu immunisation programme started in the late 1960s, initially as a programme targeted at people in clinical risk groups. Over the years many more groups have become eligible, including everyone over the age of 65 years and, more recently, pregnant women. In 2013, the childhood influenza programme was launched with a phased introduction that has slowly expanded to reach children aged 2 to 3 years old, all primary school-aged children, and for the first time this year, children in secondary school Year 7.
In recent years, the UK countries (England, Scotland, Wales and Northern Ireland) have been among the European leaders for seasonal flu vaccine coverage rates. The European Centre for Disease Prevention and Control (ECDC)’s 2018 report on seasonal flu vaccination in EU/EEA Member States presents data that shows this is the case for:
-
older age groups
-
individuals with chronic medical conditions
-
pregnant women
-
healthcare workers
The UK is also one of the first countries to introduce the childhood programme, which has seen a year on year increase in uptake rates as the programme has been expanded to include more ages.
The highest flu vaccine uptake rates have consistently been amongst those aged 65 years and over. The UK also performs very well internationally in the uptake of the flu vaccine amongst frontline healthcare workers. We have also seen promising increases in vaccine uptake in primary school-aged children as the childhood programme becomes more established.
Due to the UK’s ageing population and the expansion of the programme to more eligible groups, more people are vaccinated every year.
We have seen the following increases in numbers of people vaccinated in the following cohorts from the 2013 to 2014 flu season to the 2019 to 2020 season.
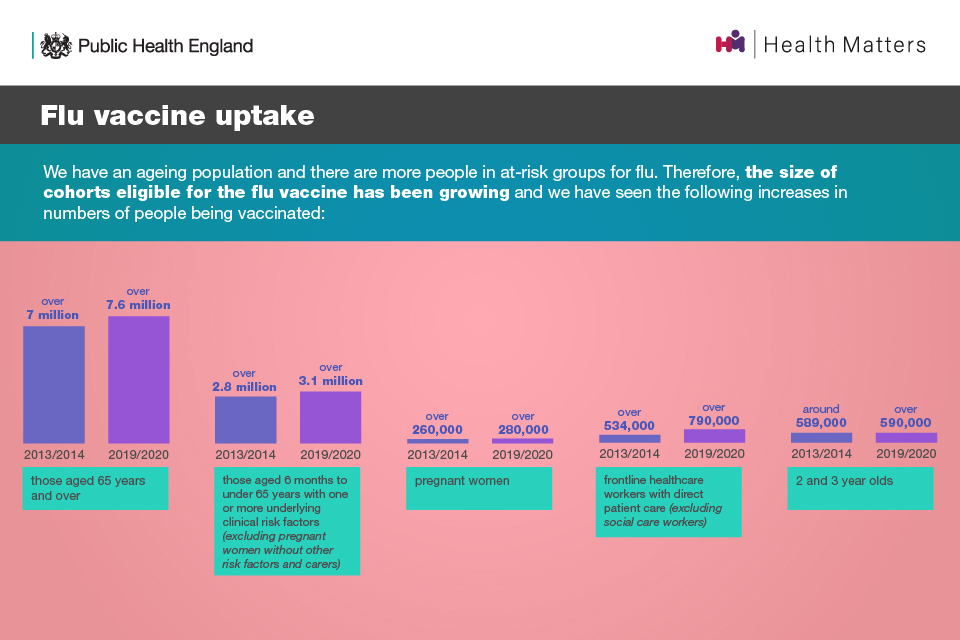
We have an ageing population and there are more people in at-risk groups for flu. Therefore, the size of cohorts eligible for the flu vaccine is growing and we have seen increases in numbers of people being vaccinated in groups such as people over 65.
More detailed vaccine uptake reports for each season, broken down by cohort, are also available.
Trends from 2012 to 2020
The following statistics demonstrate the flu vaccine uptake rates by cohort over recent years.
In those aged 65 years and over, uptake was:
-
72.4% in 2019 to 2020
-
72.0% in 2018 to 2019
-
72.6% in 2017 to 2018
-
70.5% in 2016 to 2017
-
71.0% in 2015 to 2016
-
72.7% in 2014 to 2015
-
73.2% in 2013 to 2014
-
73.4% in 2012 to 2013
In those aged 6 months to under 65 years with one or more underlying clinical risk factors (excluding pregnant women without other risk factors and carers), uptake was:
-
44.9% in 2019 to 2020
-
48.0% in 2018 to 2019
-
48.9% in 2017 to 2018
-
48.6% in 2016 to 2017
-
45.1% in 2015 to 2016
-
50.3% in 2014 to 2015
-
52.3% in 2013 to 2014
-
51.3% in 2012 to 2013
In pregnant women, uptake was:
-
43.7% in 2019 to 2020
-
45.2% in 2018 to 2019
-
47.2% in 2017 to 2018
-
44.9% in 2016 to 2017
-
42.3% in 2015 to 2016
-
44.1% in 2014 to 2015
-
39.8% in 2013 to 2014
-
40.3% in 2012 to 2013
In frontline healthcare workers with direct patient care, excluding social care workers, uptake was:
-
74.3% in 2019 to 2020
-
70.3% in 2018 to 2019
-
68.7% in 2017 to 2018
-
63.2% in 2016 to 2017
-
50.6% in 2015 to 2016
-
54.9% in 2014 to 2015
-
54.8% in 2013 to 2014
-
45.6% in 2012 to 2013
In children of primary school age, uptake was:
-
60.4% in 2019 to 2020 (Reception to Year 6)
-
60.8% in 2018 to 2019 (Reception to Year 5)
-
59.5% in 2017 to 2018 (Reception to Year 4)
-
55.4% in 2016 to 2017 (Years 1, 2 and 3)
-
53.6% in 2015 to 2016 (Years 1 and 2)
In GP-registered children aged 2 and 3 years old, uptake was:
-
43.8% in 2019 to 2020
-
44.9% in 2018 to 2019
-
42.8% for 2 year olds and 44.2% for 3 year olds in 2017 to 2018
-
38.9% for 2 year olds and 41.5% for 3 year olds in 2016 to 2017
-
35.4% for 2 year olds and 37.7% for 3 year olds in 2015 to 2016
-
38.5% for 2 year olds and 39.5% for 3 year olds in 2014 to 2015
-
42.6% for 2 year olds and 39.5% for 3 year olds in 2013 to 2014
Immunisation is the most effective intervention available to reduce harm from flu. It is important to increase flu vaccine uptake in eligible groups, including clinical risk groups, children, pregnant women and frontline health and social care workers.
The most recent flu vaccine uptake figures (2019 to 2020)
In the 2019 2020 season, over 15 million adults and children were vaccinated in England through the flu immunisation programme from the eligible population of 25 million. Vaccine uptake varied by cohort:
-
74.3% in frontline healthcare workers
-
72.4% in those aged 65 years and over
-
60.4% in primary school aged children (Reception to Year 6) with uptake in each school year group being the same or higher than in the 2018 to 2019 season
-
44.9% in those aged 6 months to under 65 years with one or more underlying clinical risk factors
-
43.8% in 2 and 3 year olds
-
43.7% in pregnant women
Useful resources:
The National Institute for Health and Care Excellence (NICE) have guidelines on increasing flu vaccine uptake and quality standards to support these.
Co-circulation of flu and COVID-19
This year, we are seeing the additional impact of COVID-19 on the NHS and social care system, and a winter where we may be faced with co-circulation of COVID-19 and flu. People most at risk from flu are also most vulnerable to COVID-19, so it is critical that we do all we can to help protect them this winter.
Public understanding of viruses is at an all-time high due to the pandemic and extensive discussion of prevention and vaccines in the media. There is also evidence that some people with underlying conditions, who traditionally have the lowest uptake, now recognise themselves as more vulnerable and have greater interest in the flu vaccine.
It is expected that there will be a higher demand for flu vaccination this season in all groups. A national supply of vaccine stock has been procured to ensure demand does not outstrip supply.
Co-infection of flu and COVID-19
PHE has recently published new research on the interactions between SARS-CoV-2 (the virus that causes COVID-19) and flu, and the impact of co-infection on disease severity. To our knowledge, this is the first epidemiological study that uses national-level data on both positive and negative COVID-19 and flu cases.
A total of 19,256 individuals were tested for both flu and COVID-19 between 20 January 2020 and 25 April 2020. In total:
-
58 had COVID-19 and flu co-infection
-
992 tested positive for flu and negative for COVID-19
-
4,443 tested positive for COVID-19 and negative for flu
-
13,763 tested negative for both COVID-19 and flu
In terms of mortality rates:
-
43.1% of those with co-infection died
-
26.9% of those who tested positive for only COVID-19 died
-
4.8% of those who tested positive for only flu died
-
8.7% of those who tested negative for both COVID-19 and flu died
Compared to those with neither flu nor COVID-19, the odds of death was:
-
5.92 times greater among those with co-infection
-
2.61 times greater among those with only COVID-19
-
slightly decreased among those with only flu
Those with co-infection were also 6.43 times more likely to be on a ventilator or die, and 6.33 times more likely to be admitted to the Intensive Care Unit or die.
The study found that the risk of testing positive for COVID-19 was 58% lower among positive flu cases, suggesting possible pathogenic competition between the 2 viruses.
Most of the COVID-19 tests were collected when the government policy was to test individuals on admission to hospital with lower respiratory tract infections and healthcare workers. Therefore, the majority of COVID-19 cases were individuals with moderate to severe symptoms, and mild cases are likely to be missed.

This year 30 million people are now eligible including, household contacts of those on the NHS shielded patients list; children of school Year 7 age; all health and social care workers who have direct contact with their patients; those aged 50-64 years.
Eligible groups, uptake ambitions for the 2020 to 2021 programme and increasing uptake
Eligibility in 2020 to 2021
In 2020 to 2021, groups eligible for the NHS funded flu immunisation programme include:
-
all children aged 2 to 11 years on 31 August 2020
-
those aged 6 months to under 65 years in clinical risk groups
-
those aged 65 years and over
-
those in long-stay residential care homes
-
the main carers of older or disabled people
-
close contacts of immunocompromised individuals
-
pregnant women
-
health and social care staff employed by a registered residential care or nursing home, registered domiciliary care provider or a voluntary managed hospice provider
Additionally, this year, the flu vaccination will be offered to:
-
household contacts of those on the NHS shielded patients list – specifically individuals who expect to share living accommodation with a shielded person on most days over the winter and for whom continuing close contact is unavoidable
-
children of school Year 7 age in secondary schools (those aged 11 years on 31 August 2020)
-
health and social care workers employed through Direct Payment (personal budgets) and or Personal Health Budgets (such as Personal Assistants) to deliver domiciliary care to patients and service users
The programme will be further extended from November and December 2020 to include the 50 to 64 year old age group. This extension is being phased to allow prioritisation of those in at-risk groups first.
Providers will be given notice in order to have services in place for any additional cohorts later in the season.
Useful resources:
The flu immunisation programme 2020 to 2021 letter provides further information on eligibility this season and actions to take to prepare for the vaccination campaign.
The flu vaccination winter 2020 to 2021: who should have it and why leaflet, and the protecting your child against flu leaflet for parents and carers of eligible children also provide further information.
Uptake ambitions for 2020 to 2021
25 million people were eligible for the flu vaccine in 2019 to 2020. This has been expanded to 30 million people for the 2020 to 2021 season.
PHE, NHS England and NHS Improvement (NHSEI), and the Department of Health and Social Care (DHSC) are calling for a concerted effort to significantly increase flu vaccination coverage this year and achieve a minimum of 75% uptake across all eligible groups. Where possible, it is expected that uptake will be higher than this. For frontline health and social care workers, there is an expectation that all should be offered the vaccine.
Many of the groups vulnerable to flu are also more vulnerable to COVID-19. Therefore, this year, it is important that we protect the health of those who are vulnerable to hospitalisation and death from COVID-19 by ensuring they do not get flu.

Many groups vulnerable to flu are also more vulnerable to COVID-19, making it more important than ever that a minimum of 75% uptake across all eligible groups is achieved this year.
Increasing uptake in underserved groups
It is essential to increase flu vaccination levels for underserved groups, including those living in the most deprived areas.
A study of population-level factors predicting variation in flu vaccine uptake in England in the 2015 to 2016 and 2016 to 2017 seasons found that:
-
adjusted uptake for 2 to 4-year-old children during both seasons was more than 11% lower in the most deprived decile
-
pregnant women in deprived areas had significantly lower uptake than in non-deprived areas
-
patients 16 to 64 years old at risk showed no significant variation in uptake by deprivation
-
patients 65 years and older had more than 3% higher vaccine uptake in the least deprived populations than the most deprived populations
Providers are expected to ensure they have robust plans in place for tackling health inequalities for all underserved groups, to ensure uptake is equitable compared to the population as a whole.
This requires high quality, dedicated and culturally competent engagement with local communities, employers and faith groups. To assist this process, PHE has published a leaflet on who should have the flu vaccine in winter 2020 to 2021 and a leaflet on protecting children against flu in a range of different languages.
For the first time this year, the NHS will implement a national call and recall service to remind people who are eligible, in addition to the usual correspondence that GPs send out inviting their patients for a flu vaccination. The national letters will be a reminder rather than an invite and will direct people to the types of service that are appropriate for their ‘cohort’ (for instance, over 65 years old to their registered GP, or a participating community pharmacy).
People with a learning disability will receive one of these reminder letters in Easy Read because they are also at increased risk from flu. They are eligible to get a free flu vaccine from their doctor or pharmacist, as are their carers, and it is important to increase uptake amongst them. PHE has easy read flu resources aimed at people who have, or care for someone with a learning disability. These resources provide advice on:
-
the flu virus and why you need a vaccine every year
-
signs of flu
-
the flu vaccine and where to get one
There will also be an addendum of easy read information on how to access services safely this year.
NHSEI is running a campaign aimed at encouraging people with a learning disability to have an annual health check and, as part of that, to have the flu vaccination. Two short films are being made to encourage people with a learning disability and their carers to get vaccinated and will be made available on the PHE Campaign Resource Centre when completed.
BAME communities
A study of flu vaccine uptake variation in England in the 2015 to 2016 and 2016 to 2017 seasons found that areas with the highest Muslim and Black, Asian and Minority Ethnic (BAME) populations had significantly higher vaccine uptake among patients aged 16 to under 65 years old in a clinical risk group.
However, recent evidence has suggested that COVID-19 may have a disproportionate impact on people from BAME groups. Therefore, it is more important that these groups are protected from flu and co-infection of flu and COVID-19 this year. This will require local authorities to continue strengthening their engagement work in communities to ensure that as many eligible people in BAME communities as possible are vaccinated.
PHE’s Disparities in the risk and outcomes from COVID-19 report details the evidence of the impact of COVID-19 on BAME communities.
Pregnant women
All pregnant women should have the flu vaccine to help protect themselves and their unborn child as women’s immune systems are naturally weakened during pregnancy. The flu vaccine can be given safely at any stage of pregnancy.
Pregnant women benefit from the flu vaccine because it will:
-
reduce the risk of complications such as pneumonia, particularly in the later stages of pregnancy
-
reduce the risk of miscarriage or having a baby born too soon or with a low birth weight
-
help protect their unborn child who after birth will continue to have some immunity to flu during the first few months of life
-
reduce the chance of the mother passing flu to her new baby
Find out more about flu vaccination for pregnant women in this suite of videos in this suite of videos:
NHSEI has asked Trust maternity departments to vaccinate pregnant women attending hospital appointments wherever possible in order to boost uptake in this cohort this year.
Frontline health and social care workers
In the 2019 to 2020 season, 74.3% of staff were vaccinated, an increase from 70.3% in 2018 to 2019. This is one of the highest rates in Europe, but we would like to do better this year.
All frontline health and social care workers should have the flu vaccine. This should be provided by their employer, who should:
-
commission a service which makes the vaccine accessible for all frontline staff
-
encourage staff to get vaccinated
-
monitor the delivery of their programmes
NHS England and NHS Improvement will continue to support vaccination of frontline staff working in social care settings. This scheme is intended to complement, not replace, any established occupational health schemes that employers have in place.
Eligibility covers those employed in registered residential care or nursing homes, registered domiciliary care providers, and voluntary managed hospice providers, who are directly involved in the care of vulnerable people who are at increased risk from exposure to flu.
The scheme has been expanded this year to improve access to health and social care workers employed through Direct Payment (personal budgets) and or Personal Health Budgets, such as Personal Assistants. These staff will be able to access the vaccine through community pharmacies or their registered general practice.
There has been a renewed push of the health and social care worker campaign to remind this group of the importance of getting vaccinated and doing so early in the season.
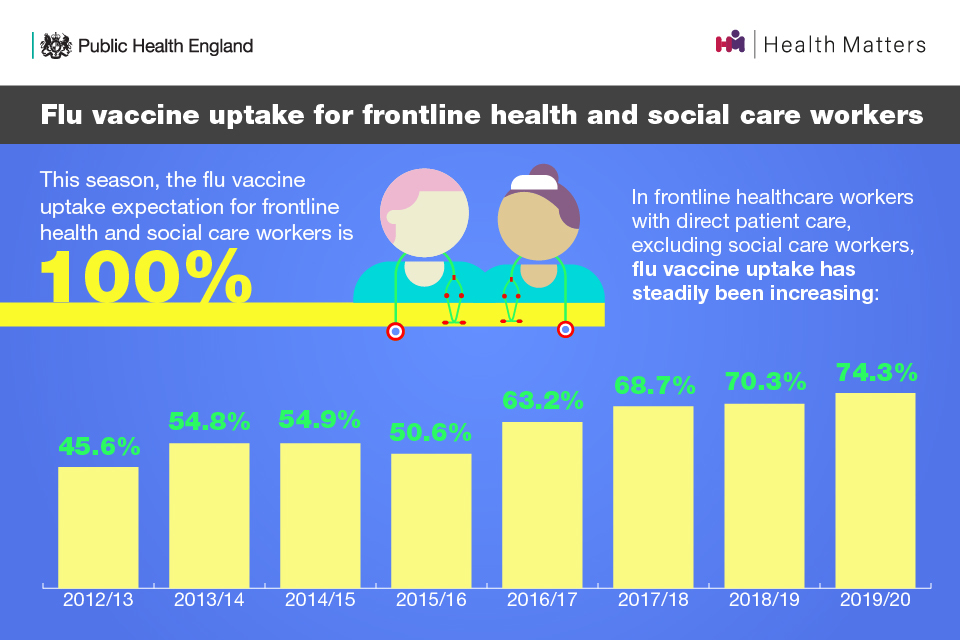
This season, the flu vaccine uptake expectation for frontline health and social care workers is 100%. In frontline healthcare workers with direct patient care, flu vaccine uptake has steadily been increasing, from 45.6% in 2012/13 to 74.3% in 2019/20.
Useful resources:
-
NHS England’s page on five components to increasing health and social care worker flu vaccinations
-
World Health Organization’s (WHO) report on how to implement seasonal influenza of health workers (published July 2019)
-
PHE’s toolkit of adaptable campaign assets available for NHS Trusts and social care organisations to use in their own staff vaccination campaigns
Childhood flu immunisation programme
Implementation of the childhood flu immunisation programme began in 2013, with pre-school children offered vaccination through GP practices and pilots for school aged children. In 2015 to 2016 the programme began in a phased roll-out nationally, starting with the youngest school-aged children first and was fully implemented for all primary school aged children in 2019 to 2020.
The UK is one of the only countries that has a childhood programme and we have seen a year on year increase of vaccine uptake in schools since its introduction. There is also evidence that the programme leads to a reduction of flu transmission in communities.
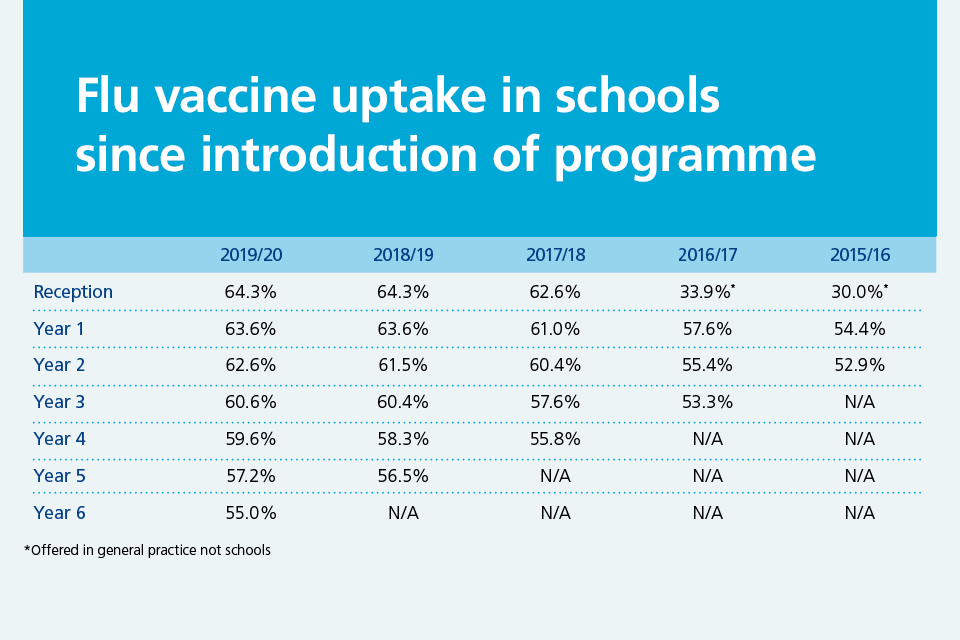
Flu vaccine uptake in schools has increased in all school years since its introduction in 2015/16.
Research into the first 3 years of the childhood programme compared the differences between pilot areas (where the entire primary school age cohort was offered vaccination) to non-pilot areas. These include reductions in:
-
GP consultations for flu-like illness
-
swab positivity in primary care
-
laboratory-confirmed hospitalisations
-
percentage of respiratory emergency department attendances
Flu immunisation programme 2020 to 2021 in schools
The flu vaccination programme in schools will be going ahead in the autumn term. The uptake ambition for children for the 2020 to 2021 season is at least 75%.
This year as part of our wider planning for winter, PHE has secured additional vaccine to enable the childhood programme to be extended into Year 7 in secondary schools.
In 2020 to 2021, children will be offered vaccination in general practice or through a schools provider as follows:
-
all those aged 2 and 3 years old on 31 August 2020 (date of birth on or after 1 September 2016 and on or before 31 August 2018) will be offered vaccine in general practice
-
all primary school children and Year 7 in secondary school (date of birth on or after 1 September 2008 and on or before 31 August 2016) will be offered through a school age immunisation service
All children in clinical risk groups should also be offered the flu vaccine, from the age of 6 months onwards.
Children will be vaccinated using a nasal spray. Children in clinical risk groups who are contraindicated to the nasal spray will be given an injected vaccine, as will all children in clinical risk groups aged 6 months to less than 2 years as the nasal spray is not licensed for children below 2 years of age.
For those parents who refuse the nasal spray for their children because of the porcine gelatine content, there may be an alternative offer of an injected vaccine that does not contain porcine gelatine from November 2020, subject to vaccine supply.
For the school programme, social distancing measures will create additional challenges. Where possible, it is expected that the school estate will still be used in the event of any local school closures.
Benefits of the school flu immunisation programme
The main purpose of the school flu immunisation programme is to reduce transmission in the community, as children can pass flu on to immediate family and the wider community, many of whom may be in at-risk groups.
The children themselves also benefit from the protection the vaccine provides, which leads to a healthy school environment, reduces school absence and reduces the impact on the NHS due to flu-related A&E attendances and hospital admissions.

Benefits of extending the programme to Year 7 children, include protect them against flu, reducing absences; healthy working environment; reduced likelihood of confusing symptoms with COVID-19; opportunity to include vaccination in the curriculum.
PHE has a range of resources that informs the childhood flu immunisation programme.
For schools:
For the local healthcare teams that go into schools:
For healthcare practitioners:
Delivering the flu immunisation programme during the COVID-19 pandemic
Effective plans for delivering the 2020 to 2021 programme
For the 2020 to 2021 flu season, it is more important than ever that effective plans are in place to protect those at risk, prevent ill-health and minimise further impact on the NHS and social care.
An important part of planning is ensuring there is a sufficient supply of vaccines. As usual, providers will have ordered flu vaccine directly from manufacturers for all cohorts apart from children. This season, it is expected that there will be increased demand for flu vaccine across all cohorts and the programme is being expanded to make more groups eligible for a free vaccine.
To support this, the Department of Health and Social Care (DHSC) has procured additional national supply of flu vaccine.
PHE has procured vaccines for use in the childhood programme, and additional stock has been procured for this season. These are:
-
the live attenuated influenza vaccine (LAIV) administered as a nasal spray and suitable for use in children aged 2 to less than 18 years except where contraindicated
-
the injectable egg-grown Quadrivalent Influence Vaccine (QIVe) for children in clinical risk groups for whom LAIV is unsuitable due to contraindication or age
Children in clinical risk groups who are contraindicated to LAIV and are aged 9 years and over who access the vaccine through general practice should ideally be offered the cell-based Quadrivalent Influenza Vaccine (QIVc) from the practice’s locally procured vaccine stocks. GP practices offering QIVc to these children will be reimbursed by NHSEI.
Useful resources:
The flu immunisations programme 2020 to 2021 letter sent out in August 2020 also includes a summary table of which flu vaccines to offer to the different eligible groups.
Relevant information is also provided in the national flu immunisation programme for 2020 to 2021 slide-set and the childhood flu immunisation programme for 2020 to 2021 slide-set.
Social distancing and other measures
This year, there may be concern that leaving home and travelling to clinics may increase exposure to COVID-19 and result in people avoiding going for the flu vaccine. If there are local lockdowns, it will be important that people are aware that they should continue to access flu vaccination services (unless they are symptomatic or self-isolating).
People, especially those on the NHS Shielded Patient List, will need reassurance that appropriate measures are in place to keep them safe from COVID-19.
Providers will be expected to deliver the programme according to social distancing guidelines.
Standard operating procedures in the context of COVID-19 have been issued for:
In line with these procedures and guidance, there is a range of ways of delivering the flu immunisation programme that should be considered, which should include:
-
careful appointment planning to minimise waiting times and maintain social distancing when attending
-
providing patients with information in advance of their appointment to explain what to expect
-
recalling at-risk patients if they do not attend in line with contract requirements
-
social distancing innovations such as drive-in vaccinations and ‘car as waiting room’ models, if possible
-
the use of domiciliary visits for those on the Shielded Patient List who are high risk for COVID-19
This year, some providers will be using different venues for their flu clinics. For example, vaccinations may take place in the GP surgery car park, a sports venue or another large venue. This is to enable a large number of people to be vaccinated at each clinic and can assist with minimising the risk of COVID-19 infection.
Providers should be prepared to make adjustments to the programme in the face of any local restrictions to ensure those at highest risk can continue to be vaccinated.
Social distancing, face coverings and other hygiene measures in place to stop COVID-19 should, in theory, also have an impact on flu transmission. These measures may have helped in countries like Australia, where the flu season has been milder than expected this year.
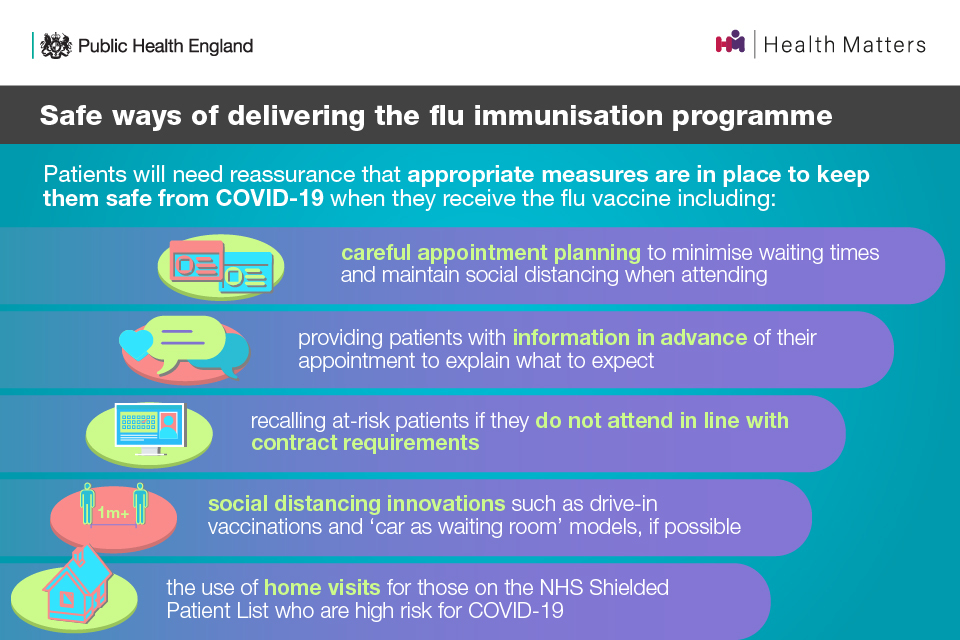
Safe ways of delivering the flu immunisation programme include appointment planning to minimise waiting times, social distancing innovations, providing patients with information in advance of their appointment.
Access useful resources about immunisation from across the health system:
-
NHS England’s clinical guidance for healthcare professionals on maintaining immunisation programmes during COVID-19
-
PHE’s guidance on flu immunisation training to support healthcare professionals during the COVID-19 pandemic
-
The Royal College of General Practitioners’ Delivering Mass Vaccinations During COVID-19 report for General Practice
Infection prevention and control when administering vaccines
Premises that are administering the flu vaccine should follow the recommended infection prevention and control (IPC) guidance.
People who are displaying COVID-19 symptoms or are self-isolating because they are confirmed COVID-19 cases, or contacts of suspected or confirmed COVID-19 cases, should not attend until they have recovered and completed the required isolation period.
Healthcare professionals who administer the vaccine are required to wear the recommended personal protective equipment (PPE) in line with the government’s guidance. The IPC principles in this guidance apply to all health and care settings, including acute, mental health and learning disabilities, primary care (including community pharmacies) and care homes.
Further information on IPC measures is provided in the Information for Healthcare Practitioner documents, which will be updated prior to and during the season as required.
PHE’s promotional flu campaigns
Flu vaccination messaging in the context of the COVID-19 pandemic
This year, the flu immunisation programme will be supported with PHE’s new public-facing Marketing and Communications campaigns. Resources for both the Marketing and Communications campaigns are available to download and order from the PHE Campaign Resource Centre.
The campaigns will encourage take-up amongst eligible groups, as well as playing a critical role in providing reassurance that people attending flu vaccine clinics can do so safely and measures are in place to protect them from COVID-19.
Marketing campaign
PHE, working in partnership with NHS England and NHS Improvement, will launch a new marketing campaign in early October 2020 to drive uptake of the flu vaccination among all eligible groups.
In response to COVID-19, activity will be significantly scaled up this year to address new audiences and increased operational complexity. Partnerships with local authorities, GP practices, charities and other organisations will be used to extend the reach of the campaign and provide advocacy from trusted voices.
Make use of the Health and Social Care Workers Flu Immunisation marketing webinar and presentation slides.
Call to action
All frontline health and social care workers should:
- ensure you get vaccinated – there is an expectation that 100% of frontline health and social care workers should be offered the flu vaccine
GP practices and community pharmacists should:
-
educate patients, particularly those in at-risk groups, about the appropriate response to the occurrence of flu-like illness and other illness (including COVID-19)
-
ensure all those eligible for the flu vaccine are invited personally to receive their vaccine
-
have robust plans in place for tackling health inequalities for all underserved groups to ensure equality of access, including BAME and other hard-to-reach communities
-
ensure COVID-19 safe measures are in place (system for physically getting people in to the clinic and vaccinated in a secure way)
-
wear the recommended PPE in line with the government’s current Infection Prevention and Control guidance
Local authorities should:
-
ensure high quality, dedicated and culturally competent engagement with local communities, employers and faith groups to ensure uptake in BAME communities is equitable compared to population as a whole
-
provide appropriate advocacy with key stakeholders and challenge to local arrangements to ensure access to flu vaccination and to improve its uptake by eligible populations
-
provide leadership, together with local resilience partners to respond appropriately to local incidents and outbreaks of flu infection
-
promote uptake of flu vaccination among eligible groups, either directly or through local providers
-
promote uptake of flu vaccination among staff providing care for people in residential or nursing care, either directly or through local providers
Employers of NHS and social care staff should:
-
manage and have oversight of the flu vaccination campaign and infection control measures for their frontline staff
-
support providers to ensure access to flu vaccination and to maximise uptake among those eligible to receive it
