National intelligence network on drug health harms briefing: December 2018
Updated 13 January 2020
This briefing is based on a meeting of the national intelligence network (NIN) on the health harms associated with drug use. The NIN is made up of representatives from drug treatment services, local authority public health and commissioning teams and national professional and membership bodies. Network meetings are chaired by Dr Michael Kelleher, consultant addictions specialist and clinical lead for Lambeth Addictions at the South London and Maudsley NHS Foundation Trust.
1. Drug-related deaths
Drug-related death rates in England and in Wales continue to be among the highest recorded in Europe. In August, the Office for National Statistics (ONS) published the latest data on registration of drug-related deaths and substances for 2017. To coincide with the statistical release, ONS also published the results of its deep dive study into coroners’ records in England.
1.1 Drug-related deaths in England: findings from ONS data and coroners’ deep dive
Martin White (Public Health England)
Deaths categorised as drug misuse deaths (which covers drugs controlled by the Misuse of Drugs Act) and heroin-related deaths (which account for around 50% of drug misuse deaths) fell by 3% between 2016 and 2017. These were the first decreases in these categories since 2012. However, the numbers of deaths remain historically high. There have been more than 2,300 drug misuse deaths and around 1,100 heroin deaths each year from 2015 to 2017.
The widely-reported deaths involving carfentanyl in 2016 and 2017 are included in the ONS-reported figure of 31 fentanyl analogue deaths, although not all of those deaths have been registered yet so more are expected to appear in next year’s ONS figures.
Registrations where cocaine is mentioned on the death certificate have continued to increase among all age groups since 2010. There were 406 deaths registered in 2017, compared to 139 in 2010. In around a quarter of deaths registered in 2017, cocaine was the only drug mentioned and over half involved an opiate.
Mentions of GABAergic drugs (pregabalin and gabapentin) also increased. These drugs are particularly linked to deaths in conjunction with opiates.
Registrations of drug misuse deaths among women, although still at a lower rate (24.6) than for men (63.4) increased again in 2017 continuing a long-term increasing trend.
There are continuing large regional variations both in overall drug misuse death rates and the scale of increases in recent years, with the regions in the north (North East, North West and Yorkshire and the Humber) having the highest rates.
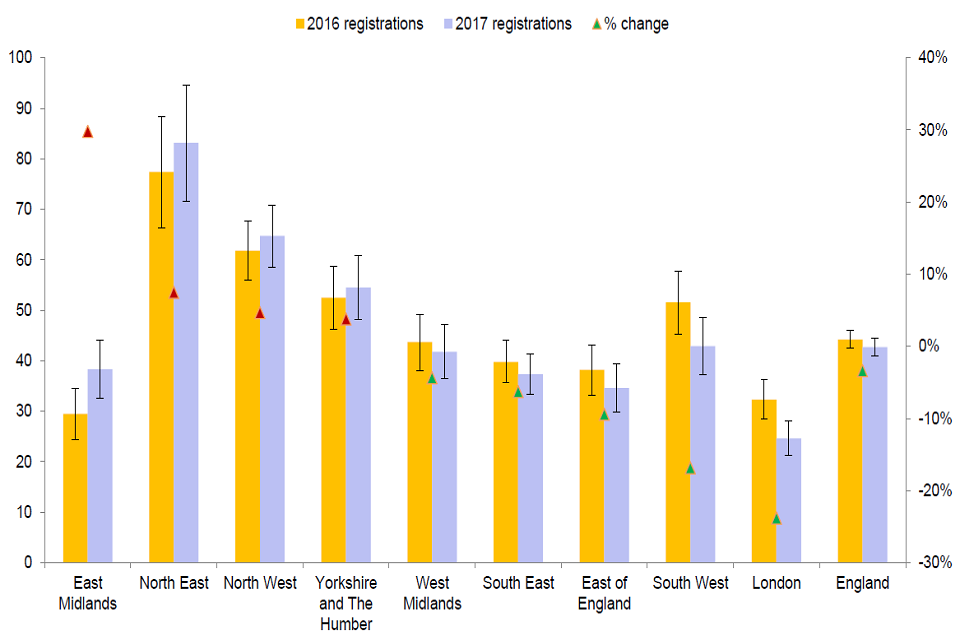
Graph shows large regional variations both in overall drug misuse death rates and the scale of increases in recent years.
Public Health England (PHE) analysts have matched ONS death data to national drug treatment monitoring system (NDTMS) data. This shows that the proportion in drug treatment when they died has remained reasonably stable in recent years (just under one-quarter of opiate deaths), as has the proportion with no record of treatment in the past year (just under two-thirds).
As part of a wider programme of work for the 2016 PHE inquiry into drug-related deaths, PHE commissioned a deep dive study into coroners’ reports. The study was carried out on a sample of 115 drug misuse deaths, with ONS staff visiting 7 coroners’ offices across England to review the available records in detail and record selected additional information using a structured electronic questionnaire. The sample included both suicides and unintentional overdose deaths.
There were several recommendations in the report, mainly for PHE, ONS and the Chief Coroner and the Coroner’s Society.
- PHE should consider the issues raised that relate to clinical practice and specific risk factors, such as taking drugs without anyone else present and consuming many different types of drug alongside alcohol, in consultation with leading government and academic stakeholders.
- ONS should continue to explore large-scale data linkage of death registrations with the NHS and other administrative data sources, such as prescriptions. ONS should also design both cross-sectional and longitudinal analyses to contribute to understanding of the patterns of drug misuse, causal relationships, and the individual pathways of those who die of drug-related causes.
- ONS, PHE, the Chief Coroner and the Coroners’ Society should work together to promote the value of coroners’ records as a source of information, which can help to prevent future deaths through public health research, including by providing information and guidance to coroners and their staff.
- ONS, the Chief Coroner and the Coroners’ Society, the Ministry of Justice and General Register Office, should work together to promote the completeness and consistency of coroners’ reports of details of deaths to ONS.
- ONS and PHE should consider further applications of this deep dive approach to improve understanding of causes of death, particularly to identify emerging issues and gain qualitative insights, but only where the expected benefit justifies such a resource-intensive commitment.
1.2 Drug deaths’ monitoring in Wales in 2017
Josie Smith (Public Health Wales)
The rate of drug-related deaths in Wales is higher than the English average – only surpassed by the regional rates in the north-east and north-west.
Although heroin deaths stabilised in 2017 there had been a big increase between 2014 and 2016. Cocaine deaths have continued to increase over the past few years.
In 2014, Public Health Wales published guidance on implementing reviews of fatal and non-fatal drug poisonings and collected data through the Harm Reduction Database (HRD) Wales.
The reviews aim to identify gaps in service provision and recommend changes to policies and practices. The information gathered can help to spot new trends in substance use, risk behaviour and changes in harms related to specific substances.
The increase in first responders using naloxone has resulted in a reduction in deaths among homeless people in hostels.
Data from the HRD showed that 69% of fatal cases were reported as having a history of mental health illness or suicidal and self-harming behaviour. Primary care and mental health services respond very well to coroner requests for personal information.
2. Shooting Up: infections among people who inject drugs
Stephanie Migchelsen (Public Health England)
PHE’s annual Shooting Up report describes the extent of infections among people who inject drugs (PWID) in England (and the rest of the United Kingdom (UK)) and highlights new developments and recent initiatives to tackle infections.
People who inject drugs are the group most affected by hepatitis C in the UK. The latest data from the unlinked anonymous monitoring survey of people who inject drugs shows that hepatitis C prevalence in England remains high (prevalence has been just over 50% since 2013) and there are significant levels of transmission among this group.
One quarter of PWID are currently living with a hepatitis C infection and only approximately half of those infected are aware of their hepatitis C virus infection. The increasing availability of the new directly acting antiviral (DAA) drugs provides an opportunity to reduce morbidity and mortality from hepatitis C, and to decrease the risk of transmission.
The uptake of the hepatitis B vaccination in England has slowed in recent years among younger people (64% in under 25 year olds) and people who have recently started injecting (57%).
HIV levels remain very low among people who inject drugs in England (around 1%). Although most people who inject drugs have been diagnosed and are accessing HIV care, their HIV is often diagnosed at a late stage.
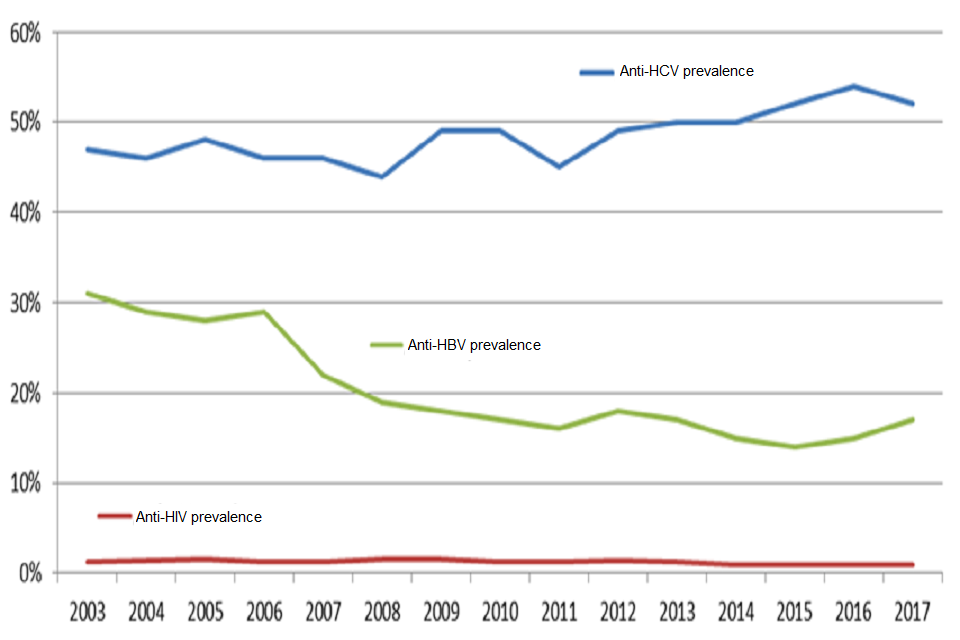
Graph shows the percentage of people who inject drugs that are living with hepatitis C, hepatitis B and HIV infections.
Bacterial infections continue to be a problem with around half of PWID having a recent symptom of a bacterial infection. Drug treatment services can help PWID avoid many of these infections by improving simple messaging around general hygiene. Incidents of methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible Staphylococcus aureus (MSSA) have increased.
Injecting practice data shows an increase in groin injecting. This might be because there is a large group of older injectors who do not have many veins they can still inject into and because, in some parts of the country, public injecting appears to be more prevalent. Public injecting can lead to people injecting into their groin as it is deemed to be quicker and more discreet than injecting into an arm.
There are also concerns about a continued increase in crack injection in 2017. This increase is particularly marked in Wales, East of England, south-east, south-west and East Midlands.
If necessary, local authority commissioners need to maintain and expand the provision of effective harm reduction interventions to reduce risk, and prevent and treat infections. These interventions include needle and syringe programmes (NSP), opioid substitution treatment (OST) and other treatments for drug misuse and dependence. Vaccinations and diagnostic tests for infections need to be routinely and regularly offered to people who inject or have injected drugs before. Where a person has tested positive for one of the infections, drug services need effective care pathways and provide access to treatment.
3. Drug health harms in prisons
Public Health England’s national health and justice team sits in the alcohol, drugs, tobacco and justice division in the health improvement directorate. It is the World Health Organization’s collaborating centre on prison healthcare and also links to the health and justice health protection network and the devolved administrations partnerships.
3.1 PHE’s partnership work in health and justice: focus on drug-related health harms
Eamonn O’Moore (Public Health England)
The shared objectives of Public Health England and national health and justice partners are to:
- improve health and wellbeing of people in contact with the criminal justice system and reduce health inequalities
- reduce re-offending and support rehabilitation by addressing health-related drivers of offending behaviour
- support access to and continuity of care across health and justice care pathways
Public health aims to reduce offending by addressing adverse childhood experiences, exclusion from education, poverty, unemployment and mental health. And to reduce re-offending by addressing recovery support, access to primary care, continuity of care and support through training, education, employment and housing.
PHE’s priorities, as set out in the national partnership agreement for prison healthcare 2018-2021, are to continue work to:
- reduce the impact of substance misuse (including from the use of new psychoactive substances)
- address the risks and harms associated with substance misuse
- ensure the right help is available at the right time
3.2 Infections: drug associated health harms for people in the criminal justice system
Maciej Czachorowski (Public Health England)
Health protection is a priority across all prescribed places of detention (PPD). Surveillance data on the number of disease outbreaks and their impact is collected centrally by the national health and justice team and this helps to inform operational responses.
The latest PHE health and justice report shows that rates for blood-borne viruses (BBV) and tuberculosis are far higher in the prison population compared to community primary care and the general population.

Graphic shows that rates for blood-borne viruses and tuberculosis are far higher in the prison population compared to community primary care and the general population.
Since opt-out testing has been implemented in prisons, prison BBV testing has increased by 700%. Some initiatives include:
- peer-to-peer programmes
- identifying lead BBV nurses in prison
- introducing a standardised test offer
- improving performance management and metrics
- awareness building
- reducing stigma
More information on this work is in PHE’s Infection Inside International publication.
3.3 Drug associated health harms for people in prison: an international perspective
Sunita Sturup-Toft (Public Health England)
The World Health Organization’s regional office for Europe wants to develop a universal indicator set to collect data on people and services in prison. This will give us a better understanding of prisoners’ health status, enable international comparisons and track trends over time.
This includes monitoring of:
- screening for drug use
- prevalence of injecting drug use
- availability of harm reduction interventions and treatment
- prevention strategies
To standardise data collection, the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) has developed the European questionnaire for drug use in prisons (EQDP) and accompanying methodological guidelines.
The EMCDDA’s 2018 trend spotter study reported new psychoactive substances (NPS) in prisons in 22 European Union countries. Long-term drug users switching to NPS in prison and younger people starting their drug use in prisons were the 2 main groups identified as NPS users.
4. Public Health England update
Pete Burkinshaw, Steve Taylor, Laura Pechey and Rob Wolstenholme (Public Health England) updated the network on recent PHE activity on drug-related health harms.
Adult substance misuse treatment statistics 2017 to 2018
PHE published annual statistics on alcohol and drug misuse treatment for adults from the national drug treatment monitoring system (NDTMS).
In the statistics for 2017 to 2018:
- overall numbers in drug and alcohol treatment continue to fall
- the decrease in overall numbers in treatment is driven mainly by the numbers of people in treatment for alcohol alone
- there is a continuing fall in numbers of people in treatment for opiates (down 4% on the previous year) but they still make up the largest proportion of people in treatment (53%)
- the number of people being treated for crack increased by 18% from the previous year
- crack treatment numbers are up by 44% over the last 2 years and the increases were seen in all age groups except 65 years and over
Buprenorphine supply issue and high price continue
PHE has written to directors of public health to update on the buprenorphine availability and price issue that has continued. Changes in the market have meant that pharmacists have had to supply branded buprenorphine which is more expensive than the generic product.
Due to changed market conditions, drug treatment services and their commissioners will see increased drugs bills continuing into 2019.
Hepatitis B vaccine shortage ends
PHE has closed the incident set up in response to the shortage of hepatitis B vaccine as there is no longer a shortage.
A system of prioritisation (which had meant healthcare professionals treating people who inject drugs as a priority group for access to the vaccine) is no longer required because there are now adequate supplies. PHE staff in the National Infection Service will continue to have regular meetings with the manufacturers beyond the closure of the incident to identify and resolve any specific supply issues.
Crack deep dive
PHE and the Home Office undertook a rapid enquiry on crack use to improve national and local understanding of the reasons behind the recent increases in crack use.
The enquiry will inform local action and responses to increased crack use.
Over the summer, PHE and Home Office staff visited 6 areas across the country, interviewing and gathering intelligence from service users, drug workers and police officers. Findings will be available early next year.
Scottish representatives at this meeting spoke about how although there were areas where people used crack and heroin together, there was a particular problem with intravenous powder cocaine use in Glasgow.
Network members from Newcastle spoke about an increase in crack use in the pubs and clubs where stimulants are already popular.
Fentanyl exposure and toxicology advice
In August, PHE published advice to protect first-responders from exposure to fentanyl. The advice outlines what law enforcement, fire, rescue, paramedic and emergency department personnel, need to know when encountering fentanyl and what action they should take.
PHE is working on advice for local authorities on the importance of commissioning comprehensive and competent toxicology services that are able to test for and detect unusual drugs, like new potent opioids.
Nasal naloxone now available
Nasal naloxone, Nyxoid, is now available to order through AAH Pharmaceuticals. Packs of 2 single-dose nasal spray devices cost £27.50. There is no direct training available to support roll-out but there are educational materials and other information on the UK Nyxoid website. Nasal naloxone is not covered by the 2015 legislation that allows drug services to supply naloxone without a prescription but PHE is working with other agencies to make it available on the same terms as injectable naloxone.
Network members from Bristol were keen to point out that although there was a good level of naloxone provision in the city, many drug users did not carry it. It is likely that for some frontline workers and carers, there would be more interest in carrying nasal naloxone.
Report Illicit Drug Reactions (RIDR)
RIDR is a joint project between PHE and the Medicines and Healthcare products Regulatory Agency (MHRA) for health professionals to report new and emerging adverse effects of new psychoactive substances (NPS) and other drugs. The pilot aims to reduce the length of time between drug-related health harms emerging and developing effective clinical responses.
Since March 2017, there have been 347 reports, primarily from prisons and hospitals. In the last quarter, synthetic cannabinoid receptor agonists (SCRAs) featured in half of the reports.
Nervous system and psychiatric disorders are the most commonly reported adverse reactions across substances.
Providers and commissioners can support RIDR by both encouraging staff to report relevant cases to RIDR and access the RIDR dashboard.
Please contact Laura Pechey to discuss any ideas for how to promote and embed RIDR reporting and dashboard use in frontline services.
Homelessness strategy and audit
PHE is working with the Ministry of Housing, Communities and Local Government, the Department of Health and Social Care and NHS England to take forward the commitments in the Rough Sleeping Strategy, published in August 2018.
One of these is a rapid audit, followed by a deep dive, of integrated health services (focusing on mental health, substance misuse and physical health) for rough sleepers in the 83 rough sleeping initiative areas.
Latest commissioning support packs published
PHE has published its annual commissioning support packs to help commissioners and local authorities assess and plan alcohol, drugs and tobacco prevention and treatment interventions for adults and children.
Trial of individual placement and support for employment
The trial of individual placement and support (IPS) for employment was the main recommendation from Dame Carol Black’s report looking at the links between substance dependence (and obesity) and the benefits system.
IPS-AD (alcohol and drugs) is the first large scale, multi-site randomised-controlled trial of IPS internationally in drug and alcohol treatment services. It is being funded jointly by the Department for Work and Pensions and the Department of Health and Social Care and runs until March 2020, with the evaluation report due by March 2021.
The trial went live in May in 7 local authority areas (Birmingham, Brighton and Hove, Blackpool, Derbyshire, Haringey, Sheffield and Staffordshire) and they have recruited approximately 850 participants to date.
