[Withdrawn] Care data matters: a roadmap for better data for adult social care
Updated 4 May 2023
Applies to England
Foreword from the Minister of State for Care
Data matters in social care. It matters for making sure people get the right care, for planning how care is organised and for joining up health and social care services around people. It can make lives better and, ultimately, can save lives.
The coronavirus (COVID-19) pandemic taught us many lessons. One of those was the importance of having social care data. As COVID-19 took hold, we started collecting new data directly from care providers through a system known as the ‘Capacity Tracker’. This provided up to date information about what was happening in care homes and home care agencies and meant the government and local authorities could help those who provided care and support with the challenges they faced through that difficult time.
While some care providers, local authorities and other organisations are trailblazers in the use of data, digital tools and technology, overall adult social care as a sector lags behind healthcare. While we have come a long way in improving the data that we collect and use, there is still much more to do.
We are embarking on far-reaching reforms for social care. We want to increase the quantity and the quality of care available. To do that successfully and sustainably, we need better social care data, joined up health and social care records, and more use of digital technologies and innovation in care.
People at the Heart of Care outlined our plans for data, digital and technology within our 10-year vision for adult social care, and in June 2022 we published the health and care data strategy Data saves lives. This outlined our commitment to improving how social care data is collected, shared and used, so that people - both those who draw on care and support and unpaid carers - have access to timely information to make informed choices about care and support, and care professionals can improve the quality of care delivered.
Building on these commitments, we set out here our roadmap for achieving transformation of social care data. This document is primarily for local authorities and care providers and will be of interest to everyone in the adult social care sector who interacts with social care data. We want this to stimulate conversation about our collective priorities for data as a sector; we are seeking your views on the data you need, as care providers, local authorities, unpaid carers or people who draw on care and support (see Chapter 3, Give your feedback, to fill out the feedback form).
We are deliberately ambitious in our aims for transformation. If we get this right, we can make a real difference. By improving our use of data and digital technologies, we can deliver:
- more joined up care for people, with information shared effectively between professionals
- more time and resources for people who provide and commission care and support, so that time can be focused on providing high quality, personalised care and support
- greater understanding of people’s care journeys - whether that be for people who draw on care or unpaid carers - where data is used to identify good practice, areas for improvement and research into how care is commissioned, provided and integrated with healthcare
- better management and oversight of the health and care system at local, regional and national levels, to in turn provide better care and make more effective use of resources
Much of this work is already underway, led by central government working in partnership with people who draw on care and support, care providers, unpaid carers and local authorities. Many local data transformation initiatives are also being taken forward, such as the development of local and regional interactive analysis tools to strengthen monitoring of performance and outcomes. I very much welcome all this work, which demonstrates a strong commitment to change across the sector.
Going forward, we will work with stakeholders to identify the data that we propose to collect. We will design our data collections to meet the data needs of all stakeholders across the sector, while keeping these collections proportionate and minimising burden on those who provide data. We will make good quality and meaningful data available to all those who need it, to design and deliver high-quality care and to develop fresh insights into care needs in the short and longer-terms. We will support the sector to develop the digital and technology capabilities to facilitate change. And we will ceaselessly work to ensure that all data held is treated with the utmost respect for people’s privacy, that all data is protected in accordance with the law, and that the purposes for which data is used are always fair and transparent.
I am determined that we unlock the potential of data to enable high-quality care, improve outcomes and strengthen accountability. While I recognise that this is no mean feat, I am confident that, together, we can transform social care data and succeed in making a real and enduring difference to social care.
Chapter 1: our vision for adult social care data
Data and the insights they provide are fundamental to ensuring that people who draw on care and support can access high quality care and achieve the outcomes that matter to them. This document sets out our roadmap for improving how we collect, share and analyse data in adult social care.
It is written for people and organisations who interact with social care data. This includes dedicated staff in delivery and leadership roles who hold, use, and submit data, local authority staff wanting to understand how changes will help them meet their responsibilities, and organisations representing people accessing care and support.
This document is published as a first draft; we want to seek your views on the data you and the sector need to commission, deliver and oversee care and support, which will be used to develop the data framework further and shape the initiatives laid out in this framework. The finalised framework will be published by the end of 2023.
Within this roadmap:
- Chapter 1 sets out the importance of adult social care data and our vision for what we can achieve through the better use of data across the sector, through:
- streamlining and improving existing data collections
- establishing data collections and bridging data gaps
- improving data access to produce better insights
- driving sector digitisation, to streamline data flows including through the adoption of digital social care records
- Chapter 2 summarises the current adult social care data landscape, outlining the different data flows and data collections at both a national and local level, and the limitations that we are aiming to tackle, such as lack of data sharing and gaps in the data collected
- Chapter 3 sets out the importance of understanding data needs across the sector and the engagement we have done to date. It details our plans for further engagement with the sector, and includes a feedback questionnaire to help us understand what data is needed by people who draw on care and support, their families and unpaid carers, and those involved in the delivery and commissioning of social care in a professional capacity
- Chapter 4 sets out our roadmap for how and when we will transform adult social care data nationally by:
- streamlining and improving existing data collections to reduce duplication and burden of collection
- setting up new data collections to bridge data gaps
- improving how data is shared and disseminated
- digitising data across the sector
- Chapter 5 sets out how we will support the sector to have the capabilities to achieve our vision, outlining the guiding principles that we must adopt as a sector to facilitate this, and the initiatives underway to advance digital and technology across the sector that are critical to underpinning our success
This framework is focused on the work happening nationally to improve how we collect, use and analyse data as a sector. It is not intended as guidance on how people and organisations should interact with data daily but outlines initiatives that will ultimately improve and enhance their access to, and use of, data.
What we are trying to achieve
We want to unlock the potential of data and digital technologies to make a real difference to people who draw on care and support and unpaid carers. If we get this right, we can deliver the following outcomes.
Better joined up care for individuals
We want people who draw on care and support and unpaid carers to have the confidence that those who plan, commission and deliver their care have access to the right information, at the right time, to meet their needs. Through initiatives such as the introduction of digital social care records (DSCRs), we will reduce the need for people accessing services to repeatedly supply information about their care needs, while also minimising the risk of incorrect care, such as medication errors. Greater transparency will also empower people to make informed choices about their care by giving them access to reliable data about local care and support services and the quality of their care.
More staff time to care
For the staff who work tirelessly to deliver care and those in leadership roles, support from the right data infrastructure will give them access to the information they need to plan and deliver personalised care, improve the operation of services, develop the workforce and inform future planning. Data infrastructure that gathers and retains timely, accurate and accessible information on care needs will also free up staff time to focus on providing direct care and support.
Greater understanding of people’s care journeys
Better availability and more consistent use of data alongside improved technology will support effective integration across local health and care systems, by allowing health and care providers to share information more effectively and to monitor the quality and continuity of care across every person’s whole care journey. Better data will support local authorities in having the right information and tools needed to continue to meet their responsibilities, such as ensuring their local markets provide sufficient choice and capacity across the full range of social care provision and delivering their safeguarding responsibilities, by enabling them to identify risks of harm and reduce or prevent this, and to manage and monitor safeguarding concerns and enquiries.
Better management of the health and care system
Nationally, improved data will give government a better understanding of how to keep the public safe, to monitor the safety, quality and continuity of care, and to reach well-informed and well-targeted decisions to improve care and evaluate its impact. Data is also key to enabling transparency and accountability at every level - local, regional and national - and to inform research into how care can best be delivered locally and nationally.
Underpinning all our work on data are key principles of transparency, data security and efficiency. We want data collections to be transparent and impose minimal burden, while data is routinely made available to those who need it. We want people who access care and support and unpaid carers to trust that their information is well-managed and safely stored. Where data is used for care planning, or for innovation and research, we want this to be done with the highest respect for their privacy and in accordance with all legal requirements and safeguards.
Progress so far
We are not starting from scratch. The COVID-19 pandemic showed the potential of data to make a real difference. Prior to the pandemic, national social care data collections were limited in scope. They often took the form of aggregated returns submitted annually by local authorities and hence lacked consistent and timely data on elements of care. As an early response to the pandemic, we introduced emergency measures to collect new data from providers which enabled the sector and government to respond more swiftly to emerging problems and to provide insights to plan for the future. There are more lessons to learn from this, but the immediate benefit has been a step-change in our understanding of care and support and of the sector-wide benefits from better data sharing.
To embed these benefits and other lessons learned from the pandemic, we developed Data saves lives, setting out our strategy for harnessing the potential of data and driving innovation across health and care. Good progress has been made, with some real transformation already underway. For example:
- the introduction of a client level data set will, for the first time, link health and social care data, plugging the gaps in our knowledge of how people move between health and social care, how they experience these transitions and the resulting care outcomes. More than 50 local authorities are already voluntarily providing client level data (CLD), ahead of it becoming mandatory in April 2023
- we have also been working with NHS England (NHSE) to improve data standards and strengthen data safeguards, such as developing secure data environments (SDEs) to manage access to person level data. Alongside this, we have been working with providers, who have been dedicating efforts to promoting the adoption of digital social care records (DSCRs); approximately 50% of Care Quality Commission (CQC) registered providers now use DSCRs
- we have been working with providers, local authorities, people who access care and support and unpaid carers to strengthen the outcomes metrics in the Adult Social Care Outcomes Framework (ASCOF). Details of the first stage of updates to ASCOF are outlined in this framework. They now clearly set out the outcomes for people that we expect social care to achieve locally and nationally, in line with the Care Act 2014
Our roadmap
Achieving this transformation is only possible by working together across the sector to deliver the initiatives set out in this framework. Our roadmap (see Figure 1) demonstrates our important milestones over the next 5 years.
We recognise the challenges in doing this well - we must build confidence and trust among stakeholders in our plans for collecting and using data, by ensuring that it is done safely and securely, and that people have a say in how their data is used.
Figure 1: important milestones on our roadmap to transforming social care data
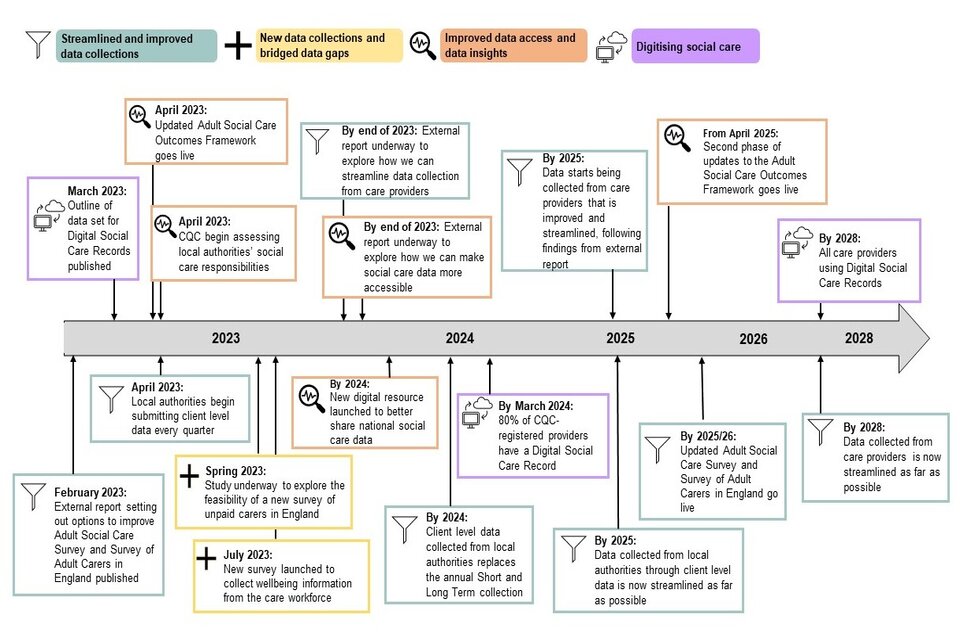
Description text for figure 1:
Milestones on the roadmap:
February 2023: discovery report identifying options to improve Adult Social Care Survey and Survey of Adult Carers in England (now published)
March 2023: outline of data set for digital social care records published
April 2023: strengthened metrics launched in Adult Social Care Outcomes Framework
April 2023: the Care Quality Commission begins assessments of local authorities’ social care responsibilities
April 2023: quarterly client level data submission is mandatory
Spring 2023: study underway to explore the feasibility of a new survey of unpaid carers
July 2023: the first wave of the new workforce staff survey is launched to collect wellbeing data directly from the workforce
By 2023: external report underway to explore how we can streamline data collection from care providers
By 2023: external report underway to explore how we can make social care data more accessible
By 2024: client level data collected from local authorities replaces the annual Short and Long Term collection
By March 2024: 80% of Care Quality Commission registered providers have access to a digital social care record
By 2024: new digital resource launched to better share national social care data
April 2025: the second phase of updates to the Adult Social Care Outcomes Framework goes live
By 2025: data collected from local authorities through client level data is now streamlined as far as possible
By 2025 to 2026: updated Adult Social Care Survey and Survey of Adult Carers in England go live
By 2028: data collected from care providers is now streamlined as far as possible
By 2028: all care providers using digital social care records
The milestones are grouped around themes of:
- streamlined and improved data collections
- new data collections and bridged data gaps
- improved data access and data insights
- digitising social care
Chapter 2: the current data collection landscape and its limitations
A considerable amount of data is already collected, stored and shared across adult social care. This chapter summarises this data landscape and its main limitations.
National data collections and publications
Currently there are over 50 national data collections (see Annex A), which centrally collect social care information from across the sector. Some of this data is collected primarily for operational purposes, to support the commissioning, management and delivery of care, and to help organisations meet their statutory duties such as safeguarding adults. For example, the Capacity Tracker collects national real-time data on key areas such as care home vacancy, and the Adult Social Care Finance Return (ASC-FR) collects data on local authority spending on social care.
Many of these national collections feed into publications or other outputs such as data insight dashboards. For example, Capacity Tracker data is published as part of the monthly Statistics for adult social care publication, alongside data on COVID-19 testing in care settings. Most national data is currently only published annually. Annex A lists the outputs for each national data collection.
Local data collections and publications
Local authorities and providers carry out many local and regional data collections to support a range of uses, such as quality and risk monitoring, understanding capacity, identifying areas for improvement, and supporting local authorities in meeting their statutory duties. For example, local authorities in the north-west are already sharing their spend and placement data to compare their own performance with that of their region, to support better and more efficient commissioning. Integrated care systems (ICSs) and integrated care boards (ICBs) also use national data collections as a source of information.
Box 1: how data flows through collections from the adult social care sector
Data collections are formed by a series of steps that come together to create a data flow. Data collections often involve more than one person or organisation who may have a role in submitting, collecting or holding data (see Glossary for a definition of terms).
Figure 2: how data flows through collections in the adult social care sector

Description text for figure 2:
Data is collected from people and organisations across the sector. These include:
- individuals who draw on care and support
- care providers and their staff
- carers who provide informal or unpaid care
- local authorities and care commissioners
Data about experiences and delivery of care is recorded either through management systems, information returns or surveys.
This data is received and used by national government departments, local governments, research organisations and care providers. Data is then stored in over 50 national data collections across 12 different organisations (such as NHSE, the Office for National Statistics (ONS), the CQC and local authorities). These data collections are then shared publicly or within organisations.
Limitations of the current data landscape
The adult social care data landscape has changed in recent years. We have seen improved timeliness and accessibility of data, but there are still many limitations. The Office for Statistics Regulation (OSR) highlighted in its 2020 report on adult social care statistics that the sector was hindered by the lack of good quality data and identified 3 key areas of focus:
- lack of leadership and collaboration
- significant gaps in data that is collected
- a lack of accessibility, coherence, quality, timeliness and granularity of existing data
Work to date
Over the past year, we have engaged with the sector to explore these limitations in greater detail. We set up a data governance board, supported by advisory boards and task and finish groups, and we held a series of workshops and surveys to develop the provider dataset. This engagement has identified 5 important areas, which echo the OSR’s findings (see Figure 3).
Figure 3: the limitations of adult social care data
As these limitations are interlinked and span the sector, we need a systematic approach to addressing them. The sector has already started collaborating to overcome these barriers, as outlined in the following chapters.

Description text for figure 3:
The 5 limitations identified are:
- limited digitisation: approximately 50% of social care providers have digital care records. Providers highlighted the lack of digital infrastructure as one of their main challenges, with the use of paper records increasing the burden of data management and sharing
- lack of data availability: data and information is not always accessible to the right people or at the right time, so individuals and their families have to repeat information. This leads to support not being tailored to needs, the workforce not having access to information needed to deliver the right care, and national and local government being unable to have proper oversight and the necessary information for decision-making
- duplication of data collected: a lack of data sharing means data is often collected more than once. Reducing this can free up staff time to focus on delivering the best possible care
- lack of standardisation and harmonisation in how data is collected: due to the nature of social care being delivered by various people and organisations, data sources are numerous. Differences in practices can lead to inconsistent data insights that inform people’s decisions
- gaps in the data collected: gaps exist in social care data, indicating that not all data needs are being met. This leads to those across the sector not having appropriate or reliable information to make informed decisions
Chapter 3: the sector’s data needs
To ensure that the right data is collected, held and shared across social care, it is vital that we have a clear understanding of the data that people and organisations need. We are seeking your views on several questions to help us do this.
Data needs differ across the sector according to the user, from individuals to providers to local government to policymakers, and will also change over time. We have seen this during the COVID-19 pandemic, where data collections were continually refined to meet the evolving data needs of the local and national pandemic response.
This need for flexibility has informed our approach to data, which is grounded in the principle of continuously reviewing data needs and adjusting data collection as needed (see Figure 4).
The review process aims to assess data quality needs, for example whether data with national statistic status is required, or whether raw unchecked data will be sufficient. It also aims to ensure that changes to collections are made only if there is significant benefit and if adequate notice can be given to data providers and collectors, to help manage data burdens.
Figure 4: using data needs to strengthen data flows

Description text for figure 4:
Data life cycle: review data needs and adjust data collection accordingly
First, identify data needs.
Next, review existing data flows.
Implement new or revised data flows as necessary, or remove flows which are no longer needed.
Monitor data flows.
Make improvements if needed.
Begin cycle again by identifying data needs.
Developing our understanding of data needs
We are working with the sector to develop a thorough understanding of the data needs of providers, unpaid carers, people who draw on care and support (including those who fund their own care), local and central government, and other relevant organisations. We need to be clear on what we need to know and why.
Work to date
We have begun work to identify and capture the data that we and the sector already know we need. This includes its purpose - such as operational delivery, policy, strategic planning, innovation - and its characteristics, such as frequency, scope and nature.
Our engagement has been carried out with stakeholders including providers, local authorities, ICBs and ICSs through workshops and a survey. We plan to continue to seek views from other stakeholders, including people who draw on care and support.
A common theme identified with stakeholders was the need for more and better operational data, but each set of stakeholders also had specific requests. For example, some providers highlighted the need for outcomes and benchmarking data, while local authorities, ICSs and ICBs emphasised the importance of workforce data and data-sharing across local areas, in addition to data on outcomes and quality of care.
These discussions with stakeholders identified some key overarching themes and categories that social care data needs can be grouped into:
- data on the population, characteristics, needs and outcomes of people who draw on care and support including self-funders
- data on the quality of care and support, including safeguarding, early intervention and integration of health and care services
- data on the supply of care services, local authority commissioning and accountability, and markets, including occupancy, capacity, discharge and strategic planning
- data on the social care workforce
- data on the population of unpaid carers
- information on contingency planning and infectious disease control measures
We are working with the sector to develop this list of themes further, to ensure there are no gaps, and to understand the detailed data requirements against each theme. Some initial examples of some stakeholder’s data needs are set out in Box 2. We will build on these select examples to thoroughly map all data needs for each set of stakeholders against each theme listed above, to be published in full as part of this framework by the end of 2023.
We will then review existing sources of data and their fitness for purpose, and identify where new collections are required. We will also consider how future changes, for example social care reform, may impact these data needs.
Box 2: examples of data needs across the sector
Data needs of unpaid carers and people who draw on care and support
People who draw on care and support and unpaid carers should have access to timely, high-quality data to improve care quality and inform choices about their care and support, and have confidence that those delivering their care also have this information, including:
- personal information: for both people who draw on care and support and unpaid carers, access to their own information about their individual health and care and the ability to give access to everyone supporting them, including unpaid carers
- local information: access to data about the type and quality of local care and support services to make better informed choices about care, support, and preferences, as well as access to user-friendly and up-to-date information to provide respite and support for unpaid carers
Data needs for providers surrounding care markets and supply of services
For providers, data is needed regarding the care market to support delivery of continuity and quality of care services and enable the care market to respond quickly to changing demands. This broadly covers the following areas:
- local authority commissioning practices: including data on capacity, market sustainability and hospital discharge with care arrangements data
- information on those using the provider’s services: access to individual level data, aggregates of safeguarding data to assess resource constraints, shared feedback from people who draw on the provider’s services, risk assessments, detailed care plans, outcomes information to understand the journey of the care user
- oversight of the market: customisable reports to support benchmarking (such as hours of overtime paid, hours of employee time paid, hours of absence recorded, vaccination rates and the ratio of private to local authority funded beds and room availability), data on local authority spend including prices paid for care across local areas, information on market resilience and financial stability of the market, and data to inform future strategic planning and promote innovation in care provision
Data needs of local government surrounding unpaid carers
Broadly, local government needs the following data to ensure the right support is being offered, to manage demand for services and to improve services locally:
- demographics and characteristics of unpaid carers: size and location of the population including those not receiving formal support from their local authority, age, gender, ethnicity, employment status
- formal support for unpaid carers: access to carers assessments, waiting times for carers assessment and support, the number of unpaid carers receiving support, types/duration/frequency of support, hours of care provided per week
- outcomes for unpaid carers: their health and wellbeing, quality of life, employment activity
- satisfaction with services among unpaid carers: particularly those in contact with and receiving support from their local authority
Data needs of central and local government surrounding the workforce
Broadly, central and local government need the following data at a local authority level to gain a true picture of the workforce, to support decision making and to ensure the right funding, resources and policies are in place to cultivate a robust, resilient and professional workforce:
- demographics and characteristics of care workforce: as far as practicable, comprehensive data such as on the age, gender, ethnicity, disability, pregnancy, and maternity
- workforce size, capacity, and employment characteristics: data on the current size of the workforce across different settings and roles, hours worked, vacancy rates, turnover rates, levels of absence, contract types and terms and conditions
- career paths and progression: current skills and qualifications, uptake of training, reasons for recruitment and retention, progression through a care career path, reasons for exiting the sector, pay rates and pay progression
- outcomes of the workforce: wellbeing and work-related quality of life (including measures of job satisfaction or attachment)
Give your feedback
We are seeking views from people and organisations on the data they need.
We would like to hear from:
- members of the public, including:
- unpaid carers
- adults who draw on support and care
- friends and relatives of someone who draws on support and care
- others with an interest in adult social care
- care professionals and others involved in delivering or commissioning care, including:
- local and central government staff
- those in leadership roles
- volunteers
- researchers
Fill in the feedback form (submit responses by 31 July 2023)
This feedback will help us set up and manage data collection, dissemination and analysis to enable these needs to be met. A summary of the feedback will be published as part of the final version of this framework. This will include details of the data needs of people and organisations in relation to the themes outlined above and our plans for addressing data gaps. All answers will be made anonymous and no personal information will be shared.
There will be further opportunities to engage on these questions throughout 2023.
Chapter 4: improving adult social care data
In this chapter, we build on the details provided in Data saves lives covering some of the most transformative projects led by central government. These aim to:
- streamline and improve existing data collections through:
- developing a provider level data collection and national minimum dataset
- rolling out client level data collected from local authorities, moving from aggregate to non-identifiable person level data
- strengthening the Adult Social Care Survey and Survey of Adult Carers in England to ensure they are fit for purpose
- establish data collections and bridge data gaps by:
- implementing a social care workforce survey to understand wellbeing and quality of life among the formal social care workforce
- developing a survey of unpaid carers to broaden the scope of information on unpaid carers beyond those receiving support from their local authority
- improve data access to produce better insights by:
- improving social care data sharing and dissemination via a new social care data access solution
- improving how we monitor outcomes through strengthening ASCOF
- improving the use of data and insight through CQC’s assessments of local authority performance
- extending our use of secondary data to generate better evidence
- drive sector digitisation, to streamline data flows including through the adoption of digital social care records
Streamlining and improving data collections
The benefits of better data are recognised by sector stakeholders such as the Association of Directors of Adult Social Services (ADASS) and the Local Government Association (LGA), who are supporting the development of major data initiatives led by national and local government. This section outlines how we are working with them and the sector to improve, adapt and integrate existing data collections.
Provider level data collection
Data collected from providers offers the most timely and direct intelligence on how the commissioning and delivery of care is operating.
The Capacity Tracker is currently the department’s main source of adult social care provider data. Its remit was extended at the start of the pandemic to gather COVID-19-related data. A subset of data in the Capacity Tracker was made mandatory from 31 July 2022, in recognition of the value of the information it collects.[footnote 1] There is a growing need to review and update this collection to keep it relevant and to minimise burdens.
Provider data is also collected through CQC’s provider information returns (PIRs), by Skills for Care as part of their Adult Social Care Workforce Data Set (ASC-WDS) and by other organisations to inform and monitor local operations. As a result, providers often submit the same data through different collections, incurring unnecessary burdens and causing data reconciliation issues for those comparing across sources.
We are developing a minimum dataset, which will improve and streamline how we and other organisations collect data from providers. This project is co-led by the department and NHS England’s digital policy unit NHS Transformation Directorate (NHSTD). Beginning from end of 2023, this will deliver a core provider dataset. Data collection will be increasingly streamlined through DSCRs to reduce burdens on providers. The minimum dataset will fold existing provider data flows into a single collection designed to meet all user needs and to fill existing gaps, such as on home care capacity.
To date, we have engaged with stakeholders, including care providers, local authorities and ICSs to identify what data is currently collected from providers, how it is used and data gaps, and begun work to commission the discovery.
Provider level data collection milestones
Project milestones by 2023:
- commission a discovery on how to best streamline provider level data flows and share the data with stakeholders, including the development of a roadmap to develop and transition to the new collection system
- building on the discovery, begin development of a new long-term, streamlined approach to data collection that streamlines existing flows and improves availability of data. Continued engagement on the development of DSCRs throughout
- continued stakeholder engagement to develop the minimum dataset and begin piloting a subset of it
Project milestones by 2025:
- data starts being collected following transition to the new long-term streamlined data collection system, based on findings of the discovery work
- progressive streamlining of data extraction, in line with sector digitisation and expansion of DSCRs
- iterative review of the minimum data set in line with automated data extraction from other data flows
Project milestones by 2028:
- the project will be completed: data collection will now be in place for the whole sector and streamlined from DSCRs and other sources
Client level data
CLD has the potential to transform our understanding of pathways and interactions of people in social care and their experiences and outcomes, as for the first time it will enable health and care data to be linked.
CLD responds to the need for timely and granular data on local authority activity and service delivery. It is intended to replace the annual Short and Long Term (SALT) publication of aggregated local authority data, which places a significant data collation burden on local authorities and does not provide timely or detailed data.
As of January 2023, 58 local authorities were voluntarily submitting CLD as part of the pilot collection. From April 2023, quarterly CLD collection will be mandatory; in the long term, CLD is intended to replace SALT.
This will support in-depth analysis of the delivery, quality and integration of local health and care services. It will allow people’s journeys - which will be non-identifiable - to be tracked through health and care, and it will allow for much greater understanding of people’s outcomes and how the system is working for individuals. This will enable local and central government to understand people’s needs in greater detail, to plan and improve the quality of care and support, while also enabling local authorities, ICBs and ICSs to undertake benchmarking, market oversight and care planning.
We are working in parallel with the roll-out of digitised care records by NHS England to enhance integration of health and care, by standardising terminology and supporting interoperability across health and care systems.
Client level data milestones
Project milestones by 2023:
- from April 2023 quarterly collection will be mandated
Project milestones by 2024:
- CLD will replace the annual SALT collection, to provide social care activity statistics
- CLD will be shared with the sector by ASC data access product
- there will be a review of CLD
Project milestones by 2025:
- submission of CLD will become automated and the project will be completed
The Adult Social Care Survey (ASCS) and the Survey of Adult Carers in England (SACE)
The Adult Social Care Survey (ASCS) and the Survey of Adult Carers in England (SACE) are the primary sources of information and insight into people’s experiences of, and satisfaction with, care services.
These surveys were established before the Care Act 2014 and therefore do not cover all groups of people within scope of that Act, such as those who access care and support on a short-term basis. We are committed to revising the surveys, including their methodologies and collection mechanisms, to ensure that they ask the right questions of a broad group of people who draw on care and support, while keeping burdens proportionate.
We have begun developing the surveys, including scoping options for reviewing the questionnaires, increasing accessibility through easy-reads and simplifying the collection mechanism. An initial discovery phase for this work was completed by Ipsos; the final discovery report is published alongside this framework (see Annex C). Further development will continue in 2023, with the revised surveys intended to be launched for the 2025 to 2026 ASCS cycle.
ACSC and SACE milestones
Project milestones by 2023 to 2024:
- assessment of options for revising ASCS and SACE
- development of revised surveys
Project milestones by 2025 to 2026:
- revised ASCS and SACE are in place for 2025 to 2026 cycles
Establishing new data collections and bridging data gaps
The following collections propose to address specific data gaps remaining after existing collections have been improved. Any new burdens resulting from these will be assessed and addressed as an integral part of their development processes.
Adult social care workforce employee survey
While detailed worker level data is collected through Skills for Care’s ASC-WDS, gaps currently exist around workforce wellbeing and work-related quality of life. ASC-WDS data is also collected from employers, which may make it less suitable for capturing more sensitive information, including some demographics (for example religion or sexual orientation), which may not always be readily disclosed to employers.
Measuring workforce work-related quality of life and wellbeing is a long-term policy interest, as improvements in workforce wellbeing play a role in increased productivity (as improved wellbeing is associated with fewer days of sickness absence) and improvements in retention (as staff are more likely to stay in their role if supported), as well as being an important outcome itself. Richer and better data on demographics and the experiences of the workforce will also provide us with the means to:
- assess equality impacts within the workforce
- evaluate workforce reforms
These data gaps are best filled through a direct, employee-level survey. However, existing omnibus surveys, including flagship labour market and business surveys run by the ONS, are limited - in part, by their small sample of social care workers, but also because potential classification issues and other differences can result in very different definitions and estimates of the care workforce compared to those obtained from the ASC-WDS.
To address this, we are developing a workforce employee-level survey to collect data directly from care staff. We have now commissioned the design and roll out of the survey; we expect the first wave of data will be collected by July 2023.
Survey of unpaid carers
While various sources capture information on unpaid carers, they lack consistency and coverage. For example, SACE only covers carers known by local authorities to be caring for someone who has been in recent contact with their local authority.
The department will undertake a feasibility study for a new regular survey focused on unpaid carers. This will explore how a survey could be representative of all unpaid carers and aspects of unpaid care provision, to fill a crucial evidence gap and provide an updated and more accurate estimate of the number of unpaid carers and their lived experience. The feasibility study will also consider how any new survey would sit alongside the existing SACE.
Improving data access and strengthening data insights
It is vital that we also strengthen how we as a sector use and share data, improving the insights and evidence we can obtain including through linking to wider health data where possible, and disseminating these back to all who would benefit.
Improving social care data sharing and dissemination through a new social care data access solution
Currently, social care data is not always accessible or shared at the right time or with the right people. During the COVID-19 pandemic, the department developed a COVID-19 dashboard to collate and share key infectious disease monitoring data with local authorities. Providers are also able to view their data in Capacity Tracker and use this for benchmarking purposes as is done through ASC-WDS; we are working with providers to improve and strengthen the data they can view in both the Capacity Tracker and other digital access products, and we will explore whether extra data sources can be added to this view to offer a richer source of data to providers.
These existing digital products have shown the potential benefits of a centralised approach to data sharing that is co-designed with those who use data. We want to build on this and develop a new digital product that will support all actors in the system to access social care data. It is our ambition that the product will host existing and new national social care collections, such as client level data. We will be taking a user-centred design approach to build the product, starting with a discovery in early 2023 that will scope stakeholder and end-user needs. The discovery will help us to identify and evaluate the options that would best satisfy the requirements identified.
The development of the product will be designed with those who will interact with it and aim to reduce the burdens and costs associated with data processing, data analysis and data storage across the sector. This will make data sharing more accessible and enable more people and organisations to unlock the value of data for the delivery of good quality care.
Social care data access platform milestones
Project milestones by 2023:
- the user research discovery will be commissioned to scope sector requirements
- prototype will be developed to demonstrate concept
Project milestones by 2024:
- the digital product will go live, this will share access to social care data and analysis
Improving how we monitor outcomes through ASCOF
Measuring the outcomes of people who draw on care and support, unpaid carers and the professionals delivering care through ASCOF is vital for tracking whether services are providing the best care and support.
We want ASCOF to demonstrate how social care enables people to achieve the outcomes that matter most to them and meets their needs, setting out the outcomes that we as central government expect social care to deliver both locally and nationally. Given upcoming changes to data over the next few years that will transform the potential of outcomes metrics, including the mandatory collection of CLD, we are committed to delivering updates to ASCOF in 2 phases.
Alongside the publication of this data framework, we have launched the first update to ASCOF, which will go live from April 2023 and the first annual publication with data will be in October 2024. This update ensures ASCOF reflects the Care Act 2014 and refocuses ASCOF on 6 priority outcomes, removing and strengthening existing metrics to reflect the latest available data (see Annex B).
We will continue working with stakeholders, including people with lived experience, to develop the second phase of the refresh, over the next few years. This will seek to utilise new data streams coming online, such as updates to SACE and ASCS, and explore metrics that will better reflect the full suite of people’s outcomes, such as their emotional wellbeing.
Sat alongside CQC’s single assessment framework, used to set out CQC’s view and assessment of the quality of health and social care, the metrics will strengthen transparency and accountability, providing a stronger lens on the performance of social care and its success in delivering good outcomes for all.
Case study: using data insights to benchmark
Devon County Council has developed tools such as using PowerBI for benchmarking performance, such as comparing ASCOF indicators against other comparable authorities or regions. These tools enable the council to drill down into survey data to better understand people’s lived experience.
The council’s annual report also includes benchmarking of activity, cost and spend data, which informs financial planning and provides an evidence base to develop their strategies and delivery plans. The council have now developed over 100 PowerBI tools using national and local data to inform their performance management, needs analysis, market shaping and other activities.
Improving the use of data and insight through CQC’s local authority assurance
The Health and Care Act 2022 conferred a new duty on CQC to assess the performance of local authorities’ delivery of certain care functions (to be set out in regulations), as set out under the Care Act 2014. CQC have been working with local government, the care sector and people with care and support needs to develop a framework for these assessments, drawing on a range of evidence.
Inspectors need access to data at a local authority-level to use as evidence in making these assessments. CQC is exploring the datasets and metrics at this level currently held or published by their organisation and others in the sector and their suitability to be used as part of CQC’s assessments. CQC is working with the department, along with other stakeholders, to ensure the development of future data collections and indicator development limits duplication and promotes consistency. Publishing data and insight at a local authority-level will also help increase transparency, by providing the public with information about the performance of local services.
CQC’s duties to assess local authorities are due to commence in April 2023, with an initial baselining period. An initial set of indicators is being developed, using existing data. These will be reviewed as the system rolls out to ensure that they are providing the information needed.
Extending our use of secondary data to generate better evidence
A breadth of wider, secondary data collections exists in social care in addition to primary use data collections; these are wider data collections that are not specific to adult social care, but account for approximately 60% of current national collections (see Glossary for further information). These could be shared and used more widely, to fill existing data and evidence gaps. For example, ONS is further developing our understanding of the size and composition of the social care workforce in England, which can be used to inform the direction of future research. In a recent blog post on Taking care of the carers: why good workforce data matters in supporting social care, ONS stated that Skills for Care’s workforce report is the most comprehensive publicly available source of workforce statistics, but ONS recognised the need for further work to address evidence gaps. The ONS census analysis plans also include analysis on unpaid care and geography, protected characteristics, health, economic activity and life expectancy. Outputs of this work will be published by ONS in due course.
NHSE is also changing how health and social care data is made available for research and analysis, moving away from data sharing to a model of data access through the implementation of SDEs. This aims to enable analysts and researchers to harness the potential of health and social care data, which will facilitate research intended for the public good whilst ensuring the highest privacy and ethics standards are upheld.
We will continue to work with other government departments to support, promote and make best use of their social care data: for example, working with the Department for Work and Pensions to better understand Carers Allowance data.
External research projects also provide useful evidence and insights which can inform social care policy and delivery. For example, DACHA (Developing research resources and minimum data set for care homes; adoption and use) is an NIHR Applied Research Collaboration East of England study (running from November 2019 to November 2023), which aims to establish what data is needed to support research, service development and innovation in care homes, and to synthesise existing data to deliver an agreed minimum data set. The VIVALDI study (running from June 2020 to March 2023), led by UCL with Four Seasons Healthcare and Department of Health and Social Care (DHSC), aims to establish how many care home staff and residents have been infected with COVID-19, and to better understand how the virus spreads in care homes to inform national policy decisions around testing and prevention in care homes. We must continue to support the development of such research projects and use the evidence and insights they provide to inform decision-making at all levels.
Digitising adult social care data through digital social care records
Our vision for the use of social care data is supported by the widespread uptake of digital systems. This includes the adoption of DSCRs to improve the safety and quality of care by reducing time spent by care workers and managers on administrative tasks (for example by automating data extraction from existing collections) and providing access to the information they need to provide the right care. This will promote closer integration between health and social care.
This work supports the overall trend towards digitisation in the sector. Around 50% of CQC registered providers currently have a DCSR, up from 45% in March 2022 (CQC data, September 2022). As this proportion grows, it is vital that digital systems and the data they generate are consistent (including making use of existing data standards where possible) and aligned. We are supporting providers to procure technology of the right standard and with the right capability by publishing a list of assured suppliers, draft standards, and a capabilities roadmap for DSCR suppliers. We are also commissioning exploratory work on a Social Care Integration Platform (SCIP) to help structured information exchange between health and social care. Our target is for 80% of CQC registered providers to have access to a DSCR by March 2024, with an interim target of 60% by March 2023.
To support this, we are:
- delivering funding directly to ICSs to support uptake of assured DSCRs through the Digital transformation fund by blending implementation and commercial support for providers
- providing appropriate and secure access to GP records for authorised social care staff, such as registered home managers and care staff who need the information to deliver direct care - we are also working to expand the use of GP Connect and developing DSCR interoperability standards with shared care records, to enable integration and sharing of information across health and social care settings
- enabling providers to record and access standardised information for direct care, including care plans, and direct care needs assessments. The DSCR Minimum Operational Data Set (MODS) will establish a list of required fields that DSCRs must capture for CQC registered care providers. This will support the delivery of direct care, increase interoperability with system suppliers, and improve planning for personalised care and support. Assured DSCR suppliers will adopt and embed MODS in the records used by their providers
- collecting provider level data, through the DSCR Minimum Dataset for Reporting. This will form a subset of the provider data minimum dataset (outlined earlier in this chapter). The Minimum Dataset for Reporting will establish a list of required fields that DSCRs must capture for CQC registered care providers. This will support the reporting of management information to plan and improve services, and to provide data relevant to help DHSC, local authorities and regulators understand care quality and inform public policy
We are continuing to engage with stakeholders, including care workers and assured DSCR suppliers, as we iteratively develop the MODS. We plan to make a minimal viable product available through the Digital Social Care Data Catalogue by March 2023.
Digital social care records key milestones
Project milestones by 2023:
- publication of a minimal viable product for DSCR MODS
- MDS begins being recorded via DSCRs
Project milestones by 2024:
- 80% of providers will access DSCRs
Project milestones by 2025:
- expansion of DSCRs to include provider level data collection and further iterations of MODS
Project milestones by 2028:
- all CQC registered providers have access to a DSCR, collecting data that is shared via interoperability standards to support improved health and care outcomes for people
Chapter 5: making our vision a reality
Over the coming years, the projects set out in this roadmap will take us further on our journey to unlock the value of data in adult social care. To achieve this, we must be guided by the same principles and have the right infrastructure in place.
Principles for moving forward
Our guiding principles for transforming adult social care data
To achieve our vision, we must all be guided by common principles for how we collect, hold and make data available. Our commitment is that:
- data will be collected once and made available to those who need it, to avoid national and local government collecting the same data separately from care providers, unpaid carers and those who access care and support
- data will routinely be shared back with data suppliers wherever possible, in an accessible manner appropriate to the needs of different data users for additional insights and benchmarking purposes
- the option for automated data collection methods as an alternative to manual collection will be available wherever possible, to minimise the data collection burdens on data suppliers
- frequency of data collection will be the minimum needed to meet data needs
- data collections will be based on data already held by a data supplier, wherever possible, and where new or amended data is required, it will be kept to a minimum
- feedback will be sought from relevant stakeholders wherever possible, prior to finalising the details of new or amending existing collections
- the collection of very granular data will be kept to a minimum where such data is not held in digital format and therefore would present a significant burden on providers to submit manually. If individual level data is being collected, providers will not be expected to bear the burden of anonymising or pseudo-anonymising such data, rather this will be considered when identifying an appropriate data collection mechanism
- information will be processed and made available safely and securely, and only processed in accordance with the legal framework, including data protection legislation, with respect for people’s privacy and with due regard to their consent. Reasons for providing access to data will be transparent, open, and understood
- access to data for research and analysis will be made available through SDEs, which will ensure that the highest standards of security, privacy and transparency are upheld
- changes to new and existing data collections will be reviewed and approved by the relevant governance structures, to ensure changes are appropriate and proportionate
Critical underpinnings for success
Advancements in digital and technology across the sector are critical to underpinning transformation - Box 3 outlines the work being led by NHSTD that supports this.
Box 3: supporting digitisation in social care
Developing standards, access and interoperability
Too often the care workforce interacts with disparate systems, searching for information in outdated formats and relying on partial or inaccurate information. Standards are key to ensuring technology and systems exist to support the sector. They can reduce burdens and improve the delivery of care, while interoperability facilitates data sharing and implementation of emerging technologies as an extension of existing systems. An early version of a Standards directory service to find nationally recognised data standards for use in health and social care is now available. Feedback from the sector is welcome and should be sent to england.interop.standards@nhs.net.
Additional progress on data standards and access across government includes:
- work by the Data Standards Authority, which establishes standards to make it easier to access and use data across government
- the Government Data Quality Framework, which provides a consistent approach to managing data quality across government
- work by NHSE is being done to move away from data sharing to a model of data access through the implementation of SDEs
Better social care data terminology
We are developing a Digital Social Care Data Catalogue. This will provide a suite of resources that list, consolidate, and standardise existing terminology resources, datasets, standards and controlled vocabularies across health and social care, with a particular focus on adult social care. A data dictionary will provide the foundational vocabulary for projects such as CLD and the Minimum Operational Data Set for DSCRs. The first 1.0 release of this development is scheduled to go live in March 2023.
‘What good looks like’ digital working framework for social care
NHSTD is also developing a What Good Looks Like framework for social care, which will provide guidance for local authorities and providers on what good digital working looks like. This framework will set out success measures for social care, including key principles to achieve this and real-life case studies. The framework is due to be published in the spring. This will be a partner framework to the NHS What Good Looks Like framework
Improving cyber security standards
The Better Security, Better Care programme provides both national and local support through 28 local support organisations, to help providers to complete the Data Security and Protection Toolkit (DSPT). The DSPT is an online self-assessment tool that helps health and care organisations provide assurances on practising good data security and ensures personal information is being handled correctly
Governance
Governance structures are in place to provide oversight and approval of information standards, changes to data collections and extractions across health and social care.
The Data Alliance Partnership brings together key national organisations representing local authorities and providers from across health and social care and is focused on placing a minimal burden on the frontline. Wherever changes to adult social care data or standards affecting adult social care data are introduced, the partnership will review and ultimately provide approval for the collection to be added to a single list of approved data collections.
The Data and Outcomes Board is the sub-board of the Data Alliance Partnership Board for adult social care data. It reviews and approves any new or amended data collections or standards and is responsible for approving adult social care additions and amendments to the Single Data List, which lists the required datasets that local government must submit to central government. It also has a role in providing strategic advice to the department on adult social care data issues.
Any future changes will be approved by these governance structures, ensuring that they are appropriate and proportionate.
Next steps
To deliver our commitments set out in this draft framework, we must work together with people and organisations across the sector. We will:
- continue to work in partnership with stakeholders across the sector, including local government, care providers, people who draw on care and support and unpaid carers and other organisations to develop and design the initiatives set out in this framework, including reviewing existing data collections
- work across government, including with NHSE and other government departments, to seek ways to maximise the sharing of existing and new data
- further develop our commitments and do so openly, involving stakeholders through regular engagement
We will publish the final version of this framework by the end of 2023, reflecting on the feedback provided in the survey. You can provide feedback on this matter via the link provided until 31 July 2023.
Glossary
Data collection: the process of collecting information about specific subjects, which is a result of a data flow.
Survey data: information collected through the process of questioning a targeted sample of participants (individuals or organisations).
Operational data: information produced by an organisation’s day to day operational business processes.
Data flow: process by which a data collection is generated, starting from the subject of the data and ends with the entity holding that data.
Data subject: the people or organisation who the data is about.
Data submitter: the people or organisation who submit data or information.
Data collector: the organisation that runs the collection process and requests the data from the data submitter.
Data controller: the organisation that has overall responsibility for the data that is stored. They control who can access the data and how it can be accessed.
Primary use data: data that has been generated by a data collection tool (for example, surveys, interviews, experiments) specially designed for understanding and solving the problem at hand. In this context, these are individual collections tailored to adult social care, and account for approximately 40% of current national level adult social care collections, such as the data collected via the Capacity Tracker or by CQC.
Secondary use data: second-hand data that already exists and is generated by another organisation for another purpose. The data does not directly relate to the problem at hand but can still be used to inform it. In this context, these are wider collections that are not specific to adult social care and account for approximately 60% of current national collections. For example, the Office for National Statistic’s Census data identifies the number of care home residents and unpaid carers.
-
Under section 277A of the Health and Social Care Act 2012 as inserted by section 99 of the Health and Care Act 2022. ↩
