Guide to abortion statistics, England and Wales: 2021
Updated 15 January 2026
Applies to England and Wales
Introduction
This report is a supplementary document to the main commentary section of the Abortion Statistics publication which presents statistics on abortions carried out in England and Wales in 2020. This document provides more detail on those statistics and is intended to give the legal context as well as a technical guide to the concepts and methodology used.
The Department of Health and Social Care (DHSC) has published abortion statistics annually since 2002. These are available in the Abortion statistics for England and Wales collection. As of 2022, abortion statistics are published by the Office for Health Improvement and Disparities (OHID), which is part of DHSC.
Statistics for years from 1968 to 1993 were published by the Office of Population Censuses and Surveys, then by their successor Office for National Statistics (ONS) from 1994 to 2001. The reports for years up to and including 2001 are available electronically on request to abortion.statistics@dhsc.gov.uk.
This publication is a National Statistic. It is a statutory requirement that National Statistics should be produced in accordance with the standards set out in the Code of Practice for Official Statistics. The UK Statistics Authority assesses all National Statistics for compliance with the Code of Practice. The last assessment of abortion statistics were published in February 2012 (PDF, 80KB) but there have been a number of internal reviews since, to ensure that the publication continues to meet the high standards required of a National Statistics publication.
The legislative context
The Abortion Act 1967, as amended by the Human Fertilisation and Embryology Act 1990, permits termination of a pregnancy by a registered medical practitioner subject to certain conditions. Legal requirements apply to the certification and notification of abortion procedures. Within the terms of the Abortion Act, only a registered practitioner can terminate a pregnancy. The doctor taking responsibility for the procedure is legally required to notify the Chief Medical Officer (CMO) of the abortion within 14 days of the termination, whether carried out in the NHS or an approved independent sector place and whether or not the woman is a UK resident. The Department of Health and Social Care provides a HSA4 form for this purpose.
Usually, any treatment for the termination of pregnancy can only be carried out in an NHS hospital or an independent clinic approved for the purpose by the Secretary of State; the only exceptions to this are in cases of emergency and in the case of early medical abortion up to 10 weeks gestation, where both medications can be taken at home (see later section on home use). After a pregnancy has reached 24 weeks gestation (defined as 24 weeks and 0 days and beyond), the abortion can only be carried out in an NHS hospital. Through contractual arrangements with NHS clinical commissioning groups (CCGs), a large number of approved independent sector clinics perform NHS-funded abortions. The main independent providers are British Pregnancy Advisory Service (BPAS), Marie Stopes International (MSI) and National Unplanned Pregnancy Advisory Service (NUPAS).
A legally induced abortion must be certified by 2 registered medical practitioners as justified under one or more of the following grounds:
-
the continuance of the pregnancy would involve risk to the life of the pregnant woman greater than if the pregnancy were terminated (Abortion Act, 1967 as amended, section 1(1)(c)) (Ground A)
-
the termination is necessary to prevent grave permanent injury to the physical or mental health of the pregnant woman (section 1(1)(b)) (Ground B)
-
the pregnancy has not exceeded its twenty-fourth week and that the continuance of the pregnancy would involve risk, greater than if the pregnancy were terminated, of injury to the physical or mental health of the pregnant woman (section 1(1)(a)) (Ground C)
-
the pregnancy has not exceeded its twenty-fourth week and that the continuance of the pregnancy would involve risk, greater than if the pregnancy were terminated, of injury to the physical or mental health of any existing children of the family of the pregnant woman (section 1(1)(a)) (Ground D)
-
there is a substantial risk that if the child were born it would suffer from such physical or mental abnormalities as to be seriously handicapped (section 1(1)(d)) (Ground E)
or, in an emergency, certified by the operating practitioner as immediately necessary:
-
to save the life of the pregnant woman (section 1(4)) (Ground F)
-
to prevent grave permanent injury to the physical or mental health of the pregnant woman (section 1(4)) (Ground G)
Recent changes to abortion legislation
Funding of abortions for women from Northern Ireland
On 29 June 2017, the government announced that it would fund – via the Government Equalities Office (GEO) – abortions for women ordinarily resident in Northern Ireland, where abortions were only available in very limited circumstances. The Central Booking System went live on 8 March 2018.
This provision for Northern Irish women currently remains in place despite the decriminalisation of abortion in Northern Ireland. This followed a free vote by Westminster MPs in July 2019 during the period that the Northern Ireland Executive was suspended (effectively becoming law when the Executive did not reconvene before 21 October 2019). This required the Northern Ireland Office (NIO) to provide a framework for abortion services to come into effect from 31 March 2020.
On 19 May 2022, the Abortion (Northern Ireland) Regulations 2022 were laid, which remove barriers to commissioning and means that the Northern Ireland Department of Health no longer needs to seek Executive Committee approval in relation to commissioning abortion services. If the Northern Ireland Department of Health does not commission and fund abortion services, the regulations give the UK government power to do anything that a Northern Ireland Minister or department could do for the purpose of ensuring that abortion services are provided as decided by Parliament in 2019.
Methods of abortion
Different methods can be used to terminate a pregnancy, depending on the duration of gestation, and other circumstances relating to the individual woman. There is one principal medical method, involving the use of the abortifacient drug Mifegyne (mifepristone, also known as RU486).
Early medical abortion in the first 10 weeks of pregnancy requires the administration of 2 tablets. Medical abortions can also happen after the first 10 weeks of pregnancy, but this is less common.
The main surgical methods are:
- vacuum aspiration, recommended at up to 15 weeks gestation
- dilatation and evacuation (D and E) recommended where gestation is greater than 15 weeks
D and E may be used in combination with vacuum aspiration; such cases are recorded in the statistics as D and E.
Early medical abortions: home use
Women in Wales from late June 2018, and Women in England from late December 2018, can take the second of the 2 abortion pills, misoprostol, at home for early medical abortions. This brought England and Wales in line with Scotland, which allowed the second pill to be taken at home from October 2017. Before this change medical abortions could only be carried out in an approved NHS hospital or an independent clinic.
From 30 March 2020, the Secretary of State for Health and Social Care approved temporary measures in England to limit the transmission of COVID-19 by approving the use of both pills for early medical abortion, without the need to first attend a hospital or clinic. Similar measures were put in place by the Welsh Government’s Minister for Health and Social Services on 31 March 2020.
[Further details on home use are available on the Royal College of Obstetricians and Gynaecologists’ website. Data collection on HSA4 forms allows uptake of home use early medical abortions to be monitored.
Chlamydia screening
The HSA4 form also allows for the collection of data on whether women were screened for chlamydia.
The Royal College of Obstetricians and Gynaecologists recommend that all women undergoing an abortion should be screened for C. trachomatis and undergo a risk assessment for other sexually transmitted infections (STIs). Chlamydia is the most commonly diagnosed STI in England. Infection of varying degrees of severity may occur after medical or surgical abortion and is usually caused by pre-existing infection. Prophylactic antibiotic use and bacterial screening for lower genital tract infection reduces this risk.
Data quality
Validation
DHSC uses a thorough process for inspecting and recording the information received on the HSA4 forms in order to monitor compliance with the legislation and the extent to which best practice guidance from DHSC is followed. Selected forms are scrutinised by a medical practitioner who may request further detail from the patient's medical record via the terminating doctor. Further details of the checks that are made on the data are available.
Data collection
Not all the information collected on form HSA4 is necessary for statistical purposes and some of the information that is used to monitor the Abortion Act is not stored electronically other than on scanned images of the forms. The scanned images of the forms are part of the system for processing the forms and they are kept for a minimum of 3 years.
There is an example HSA4 form form online that outlines what information is collected, The following information is not stored in the statistical data sets:
- terminating and certifying doctors' names
- terminating and certifying doctors' addresses
- terminating doctor's GMC number
- patient name
- patient reference including NHS number
- patient address
- detail about any medical conditions (though information on medical conditions associated with the procedure are stored in the form of ICD10 Codes)
Derived fields
Some of the data used in the tables are derived variables. More detail about these calculations is shown below:
- reported Date of Termination is from the date of the surgical treatment or, for medical abortions, the date of misoprostol or other medical agent. If a feticide is used, this date takes priority. Under the temporary approval of both medications at home for early medical abortions the date misoprostol had been supplied is used
- age at Termination is taken from Reported Date of Termination (see above) minus date of birth. Age at termination is collected in whole years
- purchaser is derived from information given about how the abortion was funded (NHS or privately) together with clinic type (NHS hospital, independent sector, private hospital). For example, a privately funded abortion within an independent sector organisation will be 'privately funded' and an NHS funded abortion within an independent sector clinic will be 'NHS funded: independent sector'
- area of residence (CCG/LA/region) is derived from postcode of the woman's residence
Incomplete information and imputation
Incomplete and incorrectly completed forms are returned to practitioners for completion and clarification. In a very small number of cases (less than 1%), the information remains unavailable at the time of publication. For example, date of birth was missing from 37 records in 2021, gestation information from 83 records, postcodes from 56 records and grounds from 57 records.
For the purposes of constructing statistics, values for missing items are imputed. Records with missing ages were assigned to the 20 to 24 age group, as this is the modal (most common) age group, accounting for 25% of abortions. Missing gestations were imputed using mode gestation (under 24 week) for grounds and method. Missing postcodes were imputed with a random postcode from within the main local authority of other residents attending the same hospital or clinic. Missing grounds were imputed as ground C unless information on the form suggested otherwise, as this is the modal ground accounting for 98% of abortions.
Forms returned after the publication cut-off date
The 2021 figures in this annual bulletin are based on a snapshot of the records taken about 10 weeks prior to publication. A small number of notifications have been, and will continue to be, received after this cut-off date. While these additional notifications are processed and the information retained in line with our retention policy, they are not included in future statistical releases.
Under-reporting of Ground E notifications
Ground E abortions are those performed because of fetal abnormality at any gestation. The medical diagnoses are coded to ICD10.
During 2013, it was brought to DHSC's attention that the number of Ground E HSA4 notifications was lower than the number reported to the congenital anomaly registries. DHSC worked closely with the National Down's Syndrome Cytogenetic Register (NDSCR) to explore this discrepancy.
A matching exercise was carried out between the NDSCR data and DHSC notifications for 2011, 2012 and 2013 data. Results from the matching suggest that a DHSC notification was made for about 54% of NDSCR records and that almost half of Ground E notifications are missing. As recommended by the Royal College of Obstetricians and Gynaecologists, DHSC has been working with clinics to rectify this under-reporting. In December 2016 DHSC wrote to all Fetal Medicine Units, Antenatal Screening Midwives and administration staff reminding colleagues of doctors' responsibility to submit HSA4 forms to the relevant Chief Medical Officer. The letter was jointly signed by DHSC, the Royal College of Obstetricians and Gynaecologists and the Maternal and Fetal Health Medicine Society. However, despite some progress being made, it is likely there is still a significant undercount presented in the ground E notification tables in this publication, so overall figures related to ground E notifications should be treated with caution.
View results from this matching exercise in 2013.
Classification of Ground E notifications in the publication
Changes were made in the 2019 publication to the reporting of medical conditions for abortions performed under ground E, where we now only report the total number of mentions by medical condition. There can often be multiple reasons for an abortion for a fetal abnormality and previous publications reported both the principal medical condition, as well as the total number of mentions by medical condition.
However, where there are 2 or more medical conditions provided in free text by the terminating doctor, it is not always clear which is the medical principal medical condition.
From 2019, we therefore decided to show the reporting of medical conditions for ground E conditions by the mentions of the condition on the HSA4 form only. This has the benefit of being a consistent measure and allows us to monitor the total frequency that a condition is mentioned.
This change applies to the ground E section of the publication and Tables 9a, 12f and 12h specifically.
Complications
Data on complications should be treated with caution. It is not possible to fully verify complications recorded on HSA4 forms and complications that occur after discharge may not be always be recorded. At the end of 2018, the government amended the approval for the class of place where abortion drugs can be administered for the second stage of early medical abortion to include the place in England where a pregnant woman has her permanent address or usually resides ("home use") and from late March 2020 temporary measures have allowed women in England and Wales to administer both pills from home without first attending a clinic or hospital to help limit the transmission of COVID-19. This means that for terminations where either both or the second stage was administered at home, complications may be less likely to be recorded on the HSA4. OHID is currently undertaking a project to review the system of recording abortion complications data to address this going forward.
Statistical methods used in this publication
Population estimates used for rates of abortion
Abortion rates are calculated using the conventional age range for women in their child-bearing years, 15 to 44.
Abortion rates per 1,000 women for 2021 at a national level and at CCG level were calculated using the mid-2020 population estimates for England, Wales, England and Wales, clinical commissioning groups and Locality Office, as published at 25 June 2021. Rates for earlier years were calculated using the latest population estimates available at the time the relevant annual reports were produced and have not been revised, either by using population estimates for the year in question or by using updated population estimates.
Deriving age standardised rates of abortion
Age standardised rates allow comparison between populations which may contain different proportions of people of different ages. The European Standard Population (ESP) is a widely used artificial population structure for the calculation of directly age standardised rates. The replacement of the ESP first used in 1976 with an updated version published in 2013 means that figures using the 1976 and 2013 ESPs are not comparable. Information about this change in methods can be found on the ONS website.
The effect of implementing the 2013 ESP for abortion age standardised rates is small. The vast majority of abortions occur within the age range 15 to 44. The 1976 ESP assumed equal populations at each single age between 15 to 44 (see Annex table 1 below). The 2013 ESP made only a small change to the populations within age range 15 to 44 such that although not equal, it remains fairly uniform. Thus, the 2013 ESP brings the abortion age standardised rates down by about 4% in recent years and 2% in earlier years. The time series using 2013 ESP age standardised rates back dated to 1968 is presented in Table 1 of the detailed tables.
The formulae used to calculate the age-standardised abortion rates are given below:
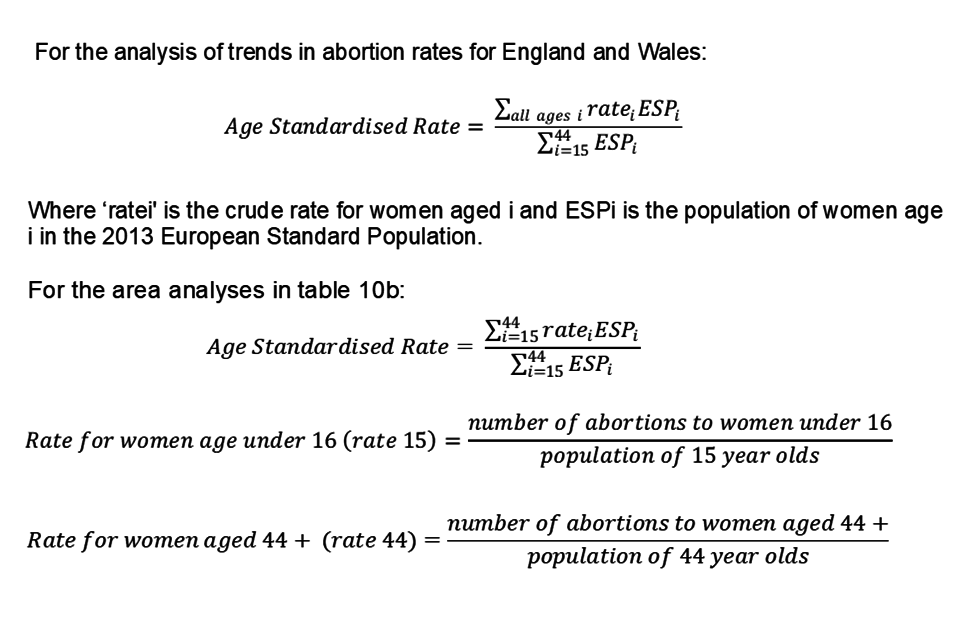
For the analysis of trends in abortion rates for England and Wales:
Age standardised rate is equal to the sum of crude rate for women multiplied by the population of women in the 2013 European standard population for women of all ages, divided by the sum of population of woman aged between 15 and 44 in the 2013 European Standard Population.
For the area analyses in tables 10b: age standardised rate is equal to the sum of crude rate for women multiplied by the population of women in the 2013 European standard population for women between the ages of 15 and 44, divided by the sum of population of woman aged between 15 and 44 in the 2013 European Standard Population.
Rates for women age under 16 (for example, 15) is equal to the number of abortions to women under 16 divide by the population of 15 year olds.
Rates for women age 44 and over (for example, 44) is equal to the number of abortions to women aged 44 and over divide by the population of 44 year olds.
Table 1: European Standardised Population (ESP)
| Age group | 1976 ESP | 2013 ESP |
|---|---|---|
| Under 1 | 1,600 | 1,000 |
| 1 to 4 | 6,400 | 4,000 |
| 5 to 9 | 7,000 | 5,500 |
| 10 to 14 | 7,000 | 5,500 |
| 15 to 19 | 7,000 | 5,500 |
| 20 to 24 | 7,000 | 6,000 |
| 25 to 29 | 7,000 | 6,000 |
| 30 to 34 | 7,000 | 6,500 |
| 35 to 39 | 7,000 | 7,000 |
| 40 to 44 | 7,000 | 7,000 |
| 45 to 49 | 7,000 | 7,000 |
| 50 to 54 | 7,000 | 7,000 |
| 55 to 59 | 6,000 | 6,500 |
| 60 to 64 | 5,000 | 6,000 |
| 65 to 69 | 4,000 | 5,500 |
| 70 to 74 | 3,000 | 5,000 |
| 75 to 79 | 2,000 | 4,000 |
| 80 to 84 | 1,000 | 2,500 |
| 85 and over | 1,000 | - |
| 85 to 89 | - | 1,500 |
| 90 to 94 | - | 800 |
| 95 and over | - | 200 |
| Total | 100,000 | 100,000 |
Source: Eurostat
Confidence intervals
The figures recorded in this report are the outcome of a stochastic process – that is, they are influenced by chance or random processes such as fertilisation. Each recorded figure is only one of a range of results that could have occurred under the same circumstances if those random processes had led to different outcomes. It is often the underlying circumstances or process that is of interest and the actual value observed gives only an imprecise estimate of this 'underlying risk'. For example, users are often interested in understanding whether there has been a change in rates of abortion, perhaps reflecting a change in the prevalence of risky sexual behaviour, a change in attitudes towards the options available in pregnancy or a change in access to services. To assess this, it is necessary to determine if the observed change is one that is unlikely to be the result of random fluctuation and therefore offers evidence that a real change has occurred.
A confidence interval can be calculated around each observed value, which gives a range in which the expected or average value resulting from the underlying process is likely to fall. The 95% confidence intervals have been calculated for some of the observed values in tables 10a, 10b, and 10c. These are known as such, because if it were possible to repeat the underlying process under the same conditions a large number of times (that is, 'rerun' the year over and over again), 95% of the confidence intervals calculated in this way would contain the average value from those runs. When assessing the observed results for the year, it is usual to assume that there is only a 5% chance that the expected or average value falls outside the 95% confidence interval.
The confidence interval may be used to compare an estimate against a target or benchmark value. If the target or benchmark value is outside the confidence interval it can be inferred that the difference between the estimate and the target is statistically significant at the 95% confidence level.
Confidence intervals are also often used to compare 2 observed values (for example, abortion rates within 2 regions.) Sometimes in such cases statistical testing is undertaken by seeing if the 2 confidence intervals overlap. This is quick and easy to do, but not necessarily conclusive: while it is safe to assume that non-overlapping confidence intervals indicate a statistically significant difference, it is not always the case that overlapping confidence intervals do not.
The method for estimating a confidence interval varies depending on whether it is for a percentage, count, crude rate or standardised rate. The methods used are those detailed in the Association of Public Health Observatories' Technical Briefing 3: Commonly used public health statistics and their confidence intervals.
For example, the 95% confidence interval associated with:
- the figure of 209,917 for the total number of abortions of residents in England and Wales is 209,020 to 210,817 (Table 10a)
- the age standardised rate of 18.2 abortions per 1,000 resident women aged 15 to 44 in England and Wales is 18.1 to 18.3 (Table 10b)
Disclosure control
All official statistics activities and outputs are subject to the UK Statistics Authority Code of Practice for Official Statistics, the Statistics and Registration Services Act 2007, the Data Protection Act 2018 and the General Data Protection Regulation (GDPR) (2016/679). The GDPR and the Data Protection Act 2018 replaced the 1998 Act from 25 May 2018.
The disclosure control policy applied to Abortion statistics is consistent with this legislation. DHSC will publish more detailed information on the policy for disclosure control for abortion statistics in due course.
Perturbed values in tables 10 and 11
In Tables 10 and 11, values in 6 local authorities have been randomly perturbed to prevent disclosing numbers of abortions in areas with very small population sizes that lie in the intersections of local authorities and clinical commissioning groups (CCG). This allows the values to be presented for these local authorities rather than being supressed as in previous years. A review of local authorities is conducted for each annual publication to ensure that perturbation is necessary and is correctly applied.
These local authority pairs were York and North Yorkshire, Buckinghamshire and Oxfordshire, and Stoke-on-Trent and Staffordshire. Values have been randomly perturbed by a number between -5 and +5, excluding 0. While these adjustments affect the values and total within these local authorities the overall totals at National level are preserved. The level of adjustment has a minor impact on the local authorities total – the minimum total for any local authorities is around 500, so each individual adjustment would be a maximum change of 1%.
A patient record was randomly selected in a local authority requiring perturbation in each age category (Under 18, 18 to 19, 20 to 24, 25 to 29, 30 to 34, 35 and over) and each funding category (NHS funded, NHS Independently funded, privately funded). Each of these records was allocated a value at random (uniform probability) from -5 to +5, excluding 0.
A corresponding record was randomly selected from the adjacent local authority in each of the age and funding categories. These records were randomly selected from records with matching age category, funding category, gestation group, method, and previous abortions. The corresponding record was weighted inversely, for example if the first record was assigned +2, the corresponding record would be -2. This ensured that relative proportions in these groups were retained through the tables.
These records were weighted in the dataset such that the perturbed values feed through all calculations relating to these local authorities. For example, a record allocated a 2 for perturbing would be weighted twice as much as other data points in the analysis.
Worked example:
-
in LA1, there are 10 records for women aged \<18, one of these is randomly selected, and assigned a random weighting from -5 to +5, excluding 0 – for example a weighting of 2
-
this record, has gestation 3 to 9 weeks, was surgical, had zero previous abortions and was NHS Independently funded
-
in LA2, there are 12 records for women <18, of those there are 7 records with gestation 3 to 9 weeks, surgical method, had zero previous abortions and NHS Independently funded. One of these 7 is picked at random, and assigned the opposite weighting, for example -2
-
this is repeated for each age category and each funding category
Table 2a: example to show local authority totals before perturbing
| Local authority | Total abortions | NHS funding | NHS independent funding | Privately funded |
|---|---|---|---|---|
| LA1 | 600 | 200 | 200 | 200 |
| LA2 | 600 | 200 | 200 | 200 |
Table 2b: example to show perturbed values
| Local authority | Total abortions | NHS funding | NHS independent funding | Privately funded |
|---|---|---|---|---|
| LA1 | 2 | 1 | 4 | -3 |
| LA2 | -2 | -1 | -4 | 3 |
Table 2c: example to show final local authority totals after perturbing
| Local authority | Total abortions | NHS funding | NHS independent funding | Privately funded |
|---|---|---|---|---|
| LA1 | 602 | 201 | 204 | 197 |
| LA2 | 598 | 199 | 196 | 203 |
Geographical coding and naming
This publication includes statistical analysis by Clinical Commissioning Groups (England) and Local Health Boards (Wales) in Tables 10a, 10b, 11a and 11b.
In England, clinical commissioning groups (CCGs) commission most of the hospital and community NHS services in the local areas for which they are responsible.
In 2021, NHS England granted approval for 9 mergers between CCGs, resulting in 106 CCGs in total. More information regarding these changes can be found on the NHS website.
On 1 April 2013 CCGs assumed commissioning of termination of pregnancy services under the health system reforms. Further information on the Coding and Naming for Statistical Geographies is available.
In Wales, NHS services are delivered through 7 Local Health Boards (LHBs). This is the first time we have published abortions by LHBs; we would appreciate your feedback on this additional breakdown including how you use these statistics. Send feedback to abortion.statistics@dhsc.gov.uk.
Index of multiple deprivation
From 2017, the abortion statistics publication has included an analysis by index of multiple deprivation (IMD). The report previously featured IMD deciles based on England and Wales combined data. However, following consultation with the ONS, we changed this in 2019 to cover only English Indices of Deprivation. From 2022, the abortion statistics publication includes analysis by IMD for England and Wales separately.
Both the English and Welsh indices of deprivation measure relative deprivation in small areas in England and Wales respectively. These small areas are called lower-layer super output areas. The English IMD is based on deprivation across 7 weighted domains (or types) of deprivation, while the Welsh IMD is based on deprivation across 8 weighted domains of deprivation. Examples of domains of deprivation include education, health, and housing. The weight given to each domain also differs between the English and Welsh IMD. For this publication, the IMD is divided into 10 equal deciles, with decile 1 being the most deprived and decile 10 the least deprived.
The English and Welsh IMD should not be compared as each country measures deprivation differently.
The English IMD data comes from the Ministry of Housing, Communities and Local Government (now known as the Department for Levelling Up, Housing and Communities), while the Welsh IMD data comes from the Welsh government. English and Welsh population data are from the ONS. In both cases, these 2 data sources are linked to the abortion data using the lower layer super output areas. It is therefore possible to categorise women who have had abortions by age, geography and IMD decile, and to calculate rates for these categories, for women between the ages 15 to 44 years.
For further information about the indices see the English index of multiple deprivation and Welsh index of multiple deprivation.
Rounding
Percentages are subject to rounding and totals may not agree with the sum of the component figures shown. Rates are also rounded.
Symbols
The following symbols are used in the tables:
[z] = not applicable
[x] = suppressed value to protect patient confidentiality
Further information
Enquiries
Enquiries about the data or requests for further information should be addressed to:
Abortion Statistics
Department of Health and Social Care
39 Victoria Street
London
SW1H 0EU
Email: abortion.statistics@dhsc.gov.uk
Extracts from this publication may be reproduced provided a reference to the source is given.
Useful links
View this bulletin for 2021 and previous bulletins for 2011 to 2020.
View previous bulletins for 2002 to 2010.
Data for 1991 to 2001 can be sent by email on request.
Information about previous disclosure control protocol published on 9 June 2015
Information on abortions carried out in Scotland
Information about the release of abortion statistics in Scotland
Facts and figures about abortion in the European Region
Information on the incidence and recent trends in legal abortion worldwide
Conception statistics for England and Wales
Statistics on the National Chlamydia Screening Programme
The British Isles Network of Congenital (BINOCAR) collect and publish data on terminations of pregnancy for fetal anomaly.
