Wellbeing and mental health: Applying All Our Health
Updated 28 February 2022
The Public Health England team leading this policy transitioned into the Office for Health Improvement and Disparities (OHID) on 1 October 2021.
Introduction
This guide is part of ‘All Our Health’, a resource which helps health professionals prevent ill health and promote wellbeing as part of their everyday practice. The information below will help front-line health and care professionals use their trusted relationships with patients, families and communities to improve their mental health and wellbeing.
We also recommend important actions that managers and staff holding strategic roles can take.
View the full range of ‘All Our Health’ topics.
Access the mental health and wellbeing e-learning session
An interactive e-learning version of this topic is now available to use. The Office for Health Improvement and Disparities (OHID) and Health Education England’s ‘e-Learning for Healthcare’ have developed this content to increase the confidence and skills of health and care professionals, to embed prevention in their day-to-day practice.
Promoting mental health in your professional practice
Mental health problems are common, with 1 in 6 adults reporting a common mental health disorder, such as anxiety, and there are close to 551,000 people in England with more severe mental illness (SMI) such as schizophrenia or bipolar disorder.[footnote 1]
Problems are often hidden, stigma is still widespread, and many people are not receiving support to access services.
Together with substance misuse, mental illness accounts for 21.3% of the total burden of disease in England.[footnote 2] Poor mental health is estimated to carry an economic and social cost of £105 billion a year in England.[footnote 3]
Mental health problems and suicide can be preventable. Promoting good mental health will impact on physical health and many other aspects of people’s lives.

Mental health promotion
The World Health Organisation (WHO) defines mental health as ‘a state of wellbeing in which the individual realises his or her abilities, can cope with the normal stresses of life, work productively and fruitfully, and is able to make a contribution to his or her community’.[footnote 4]
Our mental health influences our physical health, as well as our capability to lead a healthy lifestyle and to manage and recover from physical health conditions.[footnote 5]
People with physical health problems, especially long-term conditions, are at increased risk of poor mental health - particularly depression and anxiety.[footnote 6] Around 30% of people with any long-term physical health condition also have a mental health problem.[footnote 7] Poor mental health, in turn, exacerbates some long-term conditions, such as chronic pain.[footnote 8]
Preventing mental health problems
Mental health problems start early in life. Half of all mental health problems have been established by the age of 14, rising to 75% by age 24.[footnote 9]
Impact of COVID-19
Public Health England has been monitoring population mental health throughout the pandemic using a range of surveys close to real-time data. This shows that self-reported mental health and wellbeing at a population level (including in anxiety, stress and depression) has worsened during the pandemic and remains worse than pre-pandemic levels.
The following groups have been found to be most at risk from poor mental health:
- children and young people with particular characteristics
- young adults aged 18 to 34
- women (especially lone mothers)
- women experiencing domestic violence
- adults living alone
- adults with pre-existing mental health conditions
- adults with caring responsibilities[
- adults with low income
- adults who have experienced loss of income since the onset of the pandemic
- adults working in small businesses or are self-employed
- front line health and social care professionals
- adults with long-term physical health conditions
- older adults recommended to shield or with multi-morbidities
- children and men from certain minority ethnic backgrounds
- adults with COVID-19 symptoms
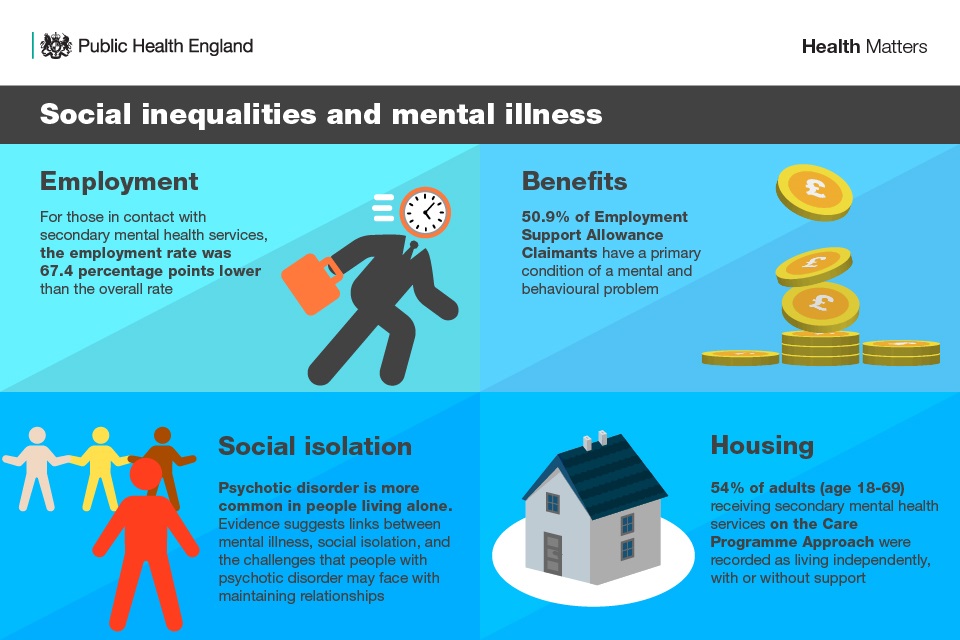
Social risk factors include poverty, migration, extreme stress, exposure to violence (domestic, sexual and gender-based), emergency and conflict situations, natural disasters, trauma, and low social support, increase risk for poor mental health and specific disorders.[footnote 10]
Across the UK, those in the poorest fifth of the population are twice as likely to be at risk of developing mental health problems as those on an average income.[footnote 11]
Children who have been neglected are more likely to experience mental health problems including depression, post-traumatic stress disorder, attention deficit and hyperactivity disorder.
Preventing suicide
In 2019, there were 5,691 suicides registered in England and Wales. Men are 3 times more likely to die by suicide than women, and suicide is the leading cause of death in men under 50 and women under 35.
Only 28% of all suicides include people who had contact with mental health services in the 12 months prior to death,[footnote 12] and those who are bereaved are at increased risk themselves. However, many people have had contact with other services.
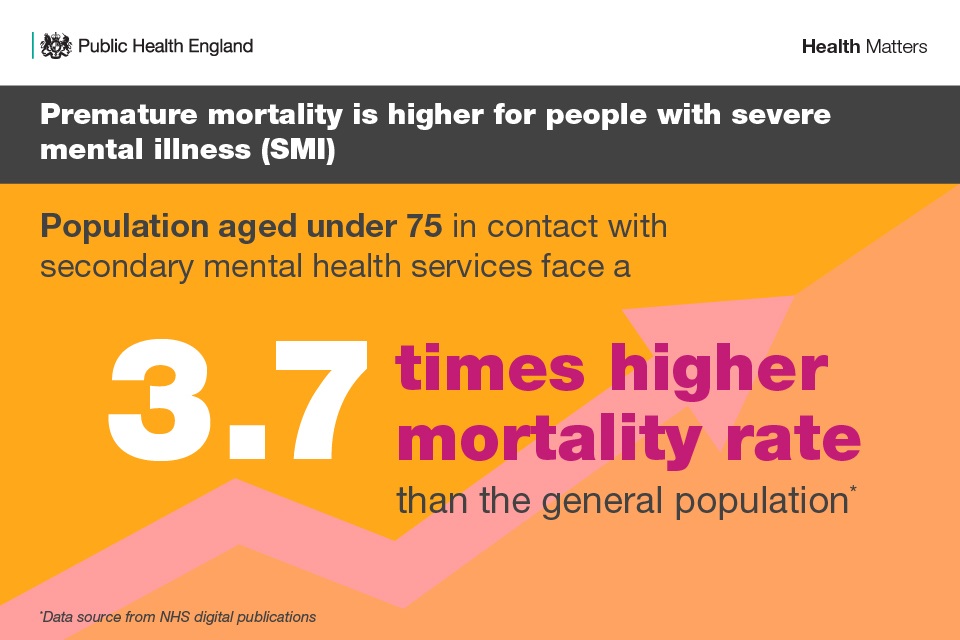
Improving the physical health of people with mental health problems
People with severe mental illness (SMI) such as bipolar disorder or schizophrenia have a life expectancy up to 20 years less than the general population,[footnote 13] and the gap is widening.[footnote 14] This is mostly from preventable physical health problems, such as cardiovascular disease.[footnote 9] It is estimated that for people with SMI, 2 in 3 deaths are due to physical illnesses and can be prevented.[footnote 9]
An adult (aged 15 to 74) with a serious mental illness is 1.8 times more likely to have 3 or more physical health conditions when compared to the general population, and a young adult (aged 15 to 34) with SMI is 5.1 times more likely to have 3 or more physical health conditions than the general population.[footnote 15]
Loneliness and lack of social interaction are also risk factors for physical and mental health – these factors increase risk of premature mortality by 30%.
Core principles for healthcare professionals
Healthcare professionals can provide advice and support to people of all ages (presenting with any issue) and work to:
- meet the patient’s mental health and wellbeing needs
- help identify those at risk of poor mental health
- prevent mental health problems from developing or worsening
- prevent suicide
When working with patients who have existing mental health problems, they can:
- ensure their physical health needs are met
- support their social needs
Taking action
Front-line health professionals
Front-line health professionals can:
- use the ‘Make every contact count’ resource, and take every opportunity to have brief conversations with people about making positive changes
- incorporate psychological aspects of care within all care pathways
- identify risk factors and symptoms of mental health problems
- signpost and refer appropriately[footnote 16]
- identify risk factors and indicators for potential self-harm and suicide and support individuals who may present with suicidal thoughts and refer appropriately[footnote 15]
- guide individuals with existing mental health problems through health promotion advice - and support them to access services to improve their physical health and wellbeing (screening, health checks)
- use basic coaching techniques to support an individual who may be experiencing mental distress
Psychological First Aid (PFA) is a globally recommended training for supporting people during crisis and emergency situations. These 2 courses equip staff, volunteers and community members to provide practical and emotional support, as well as recognising people at risk of distress:
Team leaders or managers
Team leaders or managers can:
- identify staff learning and development needs in relation to mental health and wellbeing - and provide access to appropriate training
- build prevention and mental health promotion into day-to-day work
- work collaboratively with colleagues and other teams, to raise awareness of mental health and reduce the stigma associated with mental illness
- provide and promote healthier lifestyle choices within mental health settings - including healthier food options, access to physical activities, and support to reduce and stop smoking
- work with other local services to meet people’s social needs - for example housing, employment and welfare
- provide a psychologically safe environment for patients, visitors and staff and promote mental health in the workplace[footnote 17]
Senior or strategic leaders
Senior or strategic leaders can:
-
understand the mental health needs of your local population using OHID’s Better Mental Health: JSNA toolkit
-
sign up to the Prevention Concordat for Better Mental Health. This is part of a wider drive to secure an increase in the implementation of public mental health approaches across the whole system
-
develop integrated systems to identify and support people with long term conditions who may experience mental health problems and to reduce the premature mortality of people with mental illness
-
work with community members, patient groups and other stakeholders to support collaborative action on improving mental health and wellbeing and reducing stigma associated with mental illness, including coproduction and community approaches
Understanding local needs
OHID’s Better Mental Health: JSNA toolkit links mental health data, policy and knowledge to help planners understand needs within the local population and assess local services.
The Mental Health and Wellbeing JSNA knowledge guide provides an overview of the areas to consider when thinking about the mental health needs in a local area, with a focus on understanding place factors and population groups across the life course.
These are accompanied by a Mental Health and Wellbeing JSNA data profile and a report on key features of a good Mental Health JSNA.
Measuring impact
Preventing mental health problems and suicide and promoting mental health will impact on overall life expectancy and healthy life expectancy.
There are a number of indicators in the Public Health Outcomes Framework related to mental health and wellbeing. These include:
- school readiness
- adults in contact with secondary mental health services - who live in stable and appropriate accommodation, and are in employment
- sickness absence rate
- domestic abuse
- violent crime (including sexual violence)
- statutory homeless
- social isolation
- child development at 2 to 2.5 years
- emotional wellbeing of looked after children
- self-harm
- self-reported wellbeing
- excess mortality in adults with serious mental illness
- suicide rate
- health-related quality of life for older people
The Everyday Interactions: measuring public health impact provides a quick, straightforward and easy way for health and care professionals to record and measure their public health impact in a uniform and comparable way.
The ultimate measure of physical health outcomes for people with mental health problems is an increased life expectancy and healthy life expectancy.
The CQUIN 2017 to 2019 by NHS England, focuses on improving physical healthcare to reduce premature mortality in people with serious mental illness (PSMI).
The CQUIN was introduced to support NHS England’s commitment to reduce the 20-year premature mortality rate in people with serious mental illness through improved assessment, treatment interventions, and communication between clinicians in primary and secondary care services.
The CQUIN for 2020 to 2021 now also includes a secure mental health services indicator.
The achieving healthy weight in adult secure mental health services CQUIN 2019 to 2020 by NHS England, aims to support a service environment and a systems approach to healthy lifestyles that takes account of the complexities of obesity for patients in adult secure mental health services.
The national Health Matters: preventing ill health from alcohol and tobacco use has the potential to reduce the risk of physical health conditions such as heart disease, as well as reduce future hospital admissions.
Data from the CQUIN’s first year of operation shows some improvements in the proportion of patients with mental health problems, who are being routinely screened and offered support for these health risks but there is wide variation across Mental Health Trusts.
Quality and Outcomes Framework (QOF) 2017 to 2018 includes several indicators relating to the physical health of people on the primary care register, for people with serious mental illness (patients with schizophrenia, bipolar affective disorder and other psychoses).
These indicators help to identify, for example:
- people with SMI who have a comprehensive care plan documented in their record in the preceding 12 months
- people with SMI who have a record of blood pressure in the preceding 12 months
- percentage of patients with SMI who have a record of alcohol consumption in the preceding 12 months
- females aged 25 to 64 years with SMI, whose notes record that a cervical screening test has been performed in the preceding 5 years
Physical health screening and monitoring is no longer the sole responsibility of physical healthcare professionals such as GPs and practice nurses in primary care services. Every health and care professional has a role to look after the whole person. This integrated approach is supported by Bringing together physical and mental health: A new frontier for integrated care.
Further reading, resources and good practice
There are several programmes and campaigns that offer advice for patients and the public.
Better Health is a nationwide programme that supports adults in making simple changes that can have a huge influence on their health, such as through eating well, moving more, drinking less and quitting smoking.
Better Health – Every Mind Matters is a national campaign and digital platform which launched in October 2019 with the aim of equipping people to take simple, early steps to look after their mental health, improve their mental wellbeing and support others.
In September 2020, the Better Health – Every Mind Matters campaign was relaunched to provide NHS-endorsed tips and advice to help children and young people’s mental wellbeing, and equip parents and carers with the knowledge to support them.
NHS.UK is the UK’s biggest health information service which provides advice, tips and tools to help you make the best choices about your health and wellbeing.
Equally Well UK is an initiative which seeks to promote and support collaborative action to improve physical health among people with a mental illness.
MindEd is a free educational resource on children and young people’s mental health, that is aimed at parents, carers and anyone who volunteers or works with young people.
Professional resources and tools
The Public mental health collection provides a range of resources to support national and local organisations to improve the public’s mental health.
The Health matters: reducing inequalities in mental illness outlines actions that local areas can take to reduce health inequalities experienced by people living with mental illness.
Suicide prevention resources and guidance provides help for local authorities, public health and care professionals, police forces, and others to prevent suicides in their areas.
Prevention concordat for Better Mental Health provides resources to help local areas with prevention planning arrangements. They are aimed at health and wellbeing boards, local authorities, clinical commissioning groups, integrated care systems and sustainability and transformation partnerships.
The Public mental health leadership and workforce framework can inform and influence the development of public health leadership and the workforce in relation to mental health.
Online tools intelligence and data provide up to date data and information about local mental health outcomes, risk factors and needs, as well as assets.
What Works Wellbeing collaborates with OHID and provides evidence, guidance and discussion papers on numerous topics.
Mental Health for Employers is a series of joint OHID and Business in the Community toolkits that provide free, online to help every organisation support the mental health and wellbeing of its employees
The Improving the mental health of children and young people report supports local commissioners that describe the importance of children and young people’s mental health and wellbeing, the case for investing and evidence of what works to improve local services.
Children and young people’s mental health: prevention evidence is a summary report and outputs from a review of evidence for universal approaches to improving children and young people’s mental health and wellbeing.
Suicide prevention case studies and information sheets on the National Suicide Prevention Alliance website.
Zero Suicide Awareness (ZSA) Training is a short online course which aims to give you the skills and confidence to help someone who may be considering suicide. It also works toward breaking the stigma around suicide, encouraging people to have open conversations about their mental health.
NHS England’s House of Care includes emotional and psychological support, in particular, the mental health and wellbeing of people with ‘physical’ health problems.
The Mental Health Core Skills Education and Training Framework (PDF, 1.49MB) is for staff who need general mental health awareness or have contact with people experiencing a mental health problem.
Training and information for practice and community nurses in mental health and wellbeing is provided by the Charlie Waller Memorial Trust.
Five Ways to Wellbeing is a solution-focussed framework for working with individuals to take steps to improve their mental wellbeing.
Mental health awareness eLearning is a short programme aims to raise the awareness of mental health amongst health care staff.
Making Every Contact Count (MECC) brief intervention training.
Psychological First Aid: Supporting Children and Young People supports children and young people’s mental health during emergencies and crisis situations.
COVID-19: Psychological First Aid helps people with different needs to cope with the emotional impact of COVID-19.
Guidance on measuring impact when delivering brief advice on mental wellbeing.
Physical healthcare for people with mental health problems is evidence-based information to help mental health nurses improve the physical health and wellbeing of people living with mental health problems.
Breaking Down the Barriers aims to support the NHS workforce by providing awareness training materials to enhance existing skills, knowledge for early recognition, assessment, management and signposting of mental and physical health needs of patients.
NHS England has produced a practical toolkit (PDF, 889KB) for mental health trusts and commissioners, designed to help them improve the physical health of patients with serious mental illness. The toolkit looks at different approaches to implementing the Lester screening tool.
Health Education England have produced mental health crisis learning resources (PDF, 235KB) in partnership with Healthy Teen Minds. These resources have been designed by young people working with professionals, allowing you to hear from them directly about what helps in a moment of crisis. The tools complement existing training and education, and aims to build an individual’s confidence to have effective conversations and provide personalised support to a young person in a mental crisis.
Good practice examples
Smoke-free implementation in the Sheffield NHS trust is reducing harm from tobacco to service users and staff, addressing complex implementation challenges.
Implementing ‘Preventing ill health by risky behaviours’ is a commissioning for quality and innovation (CQUIN) allows South London and Maudsley NHS Foundation Trust to refocus on alcohol screening and interventions.
Improving Physical Health for people experiencing Serious Mental Illness (SMI) – Bradford is a physical health template developed by Primary and Secondary Care with academic and data quality support. It provides a systematic way to record all necessary cardiometabolic metrics as well as a host of other information relating to screening. It could be seen as the practical way to deliver the Lester tool, which has been incorporated into the template with the help of NHSIQ.
-
Quality and Outcomes Framework, Achievement, prevalence and exceptions data - 2017-18. ↩
-
The economic and social costs of mental health problems in 2009/10. ↩
-
World Health Organization. Strengthening mental health promotion. Geneva: WHO; 2001. ↩
-
Bell R. 2017. Psychosocial pathways and health outcomes. London: UCL/PHE. ↩
-
Naylor C, Parsonage M, McDaid D and others. (2012) Long term conditions and mental health – the cost of co-morbidities. (PDF, 240KB) Accessed 20 July 2018. ↩
-
Health profiles for England 2018 Ref: Naylor C, Parsonage M, McDaid D and others. (2012) Long term conditions and mental health – the cost of co-morbidities. ↩
-
Health profiles for England 2018 Ref: Arnow BA, Hunkeler EM, Blasey CM and others. (2016) Comorbid depression, chronic pain, and disability in primary care. Pschosom Med 68(2): 262 to 268. ↩
-
The Five-year Forward View for Mental Health – A report from the independent Mental Health Taskforce to the NHS in England (PDF, 2.6MB). ↩ ↩2 ↩3
-
Mental Health Foundation. Tackling poverty for good mental health. ↩
-
Chesney E and others. ‘Risks of all-cause and suicide mortality in mental disorders: a meta-review’ World Psychiatry 2014: volume 13, issue 2, pages 153 to 160. ↩
-
HEE. 2018 Self harm and suicide prevention competence framework. ↩ ↩2
-
HEE/Skills for Health. Mental health core skills and knowledge framework. (PDF, 1.49MB) 2016. ↩
-
Business in the Community. Mental health for employers toolkit. ↩
