Personal protective equipment (PPE) strategy: stabilise and build resilience
Updated 29 September 2020
Applies to England
Foreword from the Secretary of State
Protecting those who protect us has been one of our most important goals in our fight against COVID-19.
We have strained every sinew to get NHS and social care staff the personal protective equipment (PPE) they need, so they can do their important jobs safely and with confidence.
During the coronavirus pandemic, we’ve needed to expand our PPE supply chain from 226 NHS trusts in England to over 58,000 different settings, including care homes, hospices and community care organisations.
This has meant we needed a Herculean logistical effort, of unprecedented scale and complexity, to make sure our healthcare heroes get what they need.
We’ve had to create a whole new logistics network from scratch, bringing to bear the experience and expertise of the NHS, industry and the armed forces.
The Department of Health and Social Care (DHSC) has distributed over 3.5 billion PPE items for use by health and social care services in England; and this strategy shows the work we are doing to put ourselves in the strongest possible position ahead of winter.
This winter presents a particular challenge, as we may need to deal with COVID-19 along with the usual pressures that the season will bring.
This strategy sets out how we can put ourselves in the strongest possible position. Through getting a clearer view of demand, developing a more resilient and diverse supply chain, and building up our stockpile of PPE.
We have now also established a strong domestic supply base, transforming our ability to respond to a crisis and providing greater resilience for any second wave.
The work outlined in this strategy has meant we now have enough PPE for the winter period, and we will have a 4-month stockpile available to cope with any future surge in place by November.
I’d like to thank Lord Deighton, for stepping forward to lead this national effort, and delivering once again for his country.
I’d also like to pay tribute to all the businesses that have generously come forward with offers to turn over their production lines as part of this national effort.
You have all played your part at this nation’s time of need, to put us in the best possible position, for this winter and beyond.
The Rt Hon Matt Hancock MP
Foreword from Lord Deighton
COVID-19 has presented many challenges and none more critical than ensuring the right PPE equipment is available at the right time to protect frontline health and social care staff.
In April 2020, I was asked to lead the national effort to produce PPE, known as ‘UK Make’. Then, in May 2020, to lead a PPE Taskforce with responsibility for buying sufficient supply of PPE from abroad, and for ensuring an efficient and effective PPE distribution system to all relevant settings across the UK.
We faced a number of complex challenges.
Prior to COVID-19 PPE had been in plentiful supply, mainly procuring from The People’s Republic of China, but that situation changed rapidly in March 2020. As the pandemic unfolded across the world, supply chains and transportation links were disrupted, and demand increased to unprecedented levels across the globe.
In the UK, as the number of COVID-19 cases increased, we were facing escalating demand for PPE and with a rapidly depleting stockpile and limited PPE domestic supply, there was a need to respond at speed. By this stage it was clear that established modes of sourcing PPE in the UK were no longer practical and that the influenza stockpile was insufficient to meet the COVID pandemic demand. In addition, offers were flooding in at pace from British businesses to assist in sourcing and supplying PPE.
The early period of the COVID-19 pandemic was largely one of emergency response; trying to make sure we were getting all the kit out to those who needed it.
Continuously learning from experience, we have brought together a team that consolidates our procurement expertise; we have better data on PPE demand and created a new PPE distribution network almost from scratch. UK manufacturing is now in place in all but one product category (gloves). On average, UK-based supply is anticipated to meet 70% of forecasted demand in December for all categories of PPE excluding gloves.
We have stabilised the UK PPE supply chain; we have over 32 billion PPE items on order and we will be rebuilding the stockpile during the autumn equivalent to approximately 4 months PPE usage at current COVID-19 usage levels.
It has been an extraordinary effort by so many to get to this point and my thanks and gratitude is extended to all involved.
We will not lose our focus; the PPE Strategy describes how we are building further resilience in order to be ready for any second spike of COVID-19 in the autumn, winter or beyond.
Lord Deighton
1. Executive summary
1.1 The UK government and devolved administrations are committed to the effective supply and distribution of PPE to those on the frontline responding to COVID-19. At every step of the way the UK government and devolved administrations have worked side by side. Each of the nations has its own supply chain operation for PPE and is responsible for ensuring distribution within Northern Ireland, Wales, Scotland and England. Each nation will have its own strategy; this strategy covers England.
1.2 A resilient supply chain system is capable of withstanding, adapting to, and recovering from disruption so that it can continue to meet supply needs. In the case of a pandemic, a resilient system can raise production to meet increased demand.
1.3 Detailed analysis of DHSC’s supply options for each category of medical-grade PPE has been conducted with the primary objective of resilient security of supply. Given the significant differences in the nature of the market for each category, DHSC is taking a detailed category-by-category approach to achieve optimal resilience.
1.4 UK manufacturing capability plays an important role in a more resilient supply chain. The UK manufacturing response to the crisis has been a significant achievement with, on average, UK-based supply anticipated to meet 70% of forecasted demand in England in December for all categories of PPE excluding gloves. It also has wider benefits, including the potential to create jobs and for the UK to become a centre for innovative products that meet user needs.
1.5 To ensure we can respond rapidly to demand surges in the future, DHSC is building a strategic stockpile. This will be equivalent to approximately 4 months’ stock of each product category and will be in place and stored in our warehouses by November 2020. Alongside a COVID-19 stockpile, we want to consider stockpile requirements for other types of pandemic threat. We are therefore beginning a review and commissioning new advice from experts such as the New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG) and other scientific advisers to determine the nature, composition and volume of a future pandemic stockpile.
1.6 As the people who helped us manage the procurement and distribution of PPE during the late winter and spring return to their normal roles, we have ensured that we are prepared to respond to any future need. We have developed a robust plan to stand procurement and distribution back up at pace to provide an effective and timely response.
1.7 Building resilience in the PPE supply chain cannot be separated from government’s wider efforts to support economic recovery through a New Deal. Our improved PPE supply chain can support and align with our goals for UK industry, levelling up jobs and skills across the country, and doing so in a way that is ethically responsible, supporting our ambition to eradicate modern slavery, and greener, helping us realise our net-zero ambition. Government will therefore also consider how its tendering principles and criteria can ensure high environmental standards and ethical labour practices.
1.8 DHSC is committed to understanding the needs of individuals using PPE and improving their user experience. We are listening to the reported practical difficulties with the use of some PPE experienced by women and Black, Asian and Minority Ethnic (BAME) individuals, among others, and are taking action to make sure user needs are adequately addressed in future provisions of PPE.
| Pre COVID-19 | Emergency response | Stabilise and build resilience September 2020 to March 2021 | |
|---|---|---|---|
| Supply | NHS supply chain Wholesalers Pandemic Influenza Preparedness Programme stockpile in place for pandemic influenza |
Demand model established 175 new global suppliers identified and contracted with Stockpile depleted In April, the National Supply Disruption Response hotline received on average 592 calls a day |
Demand model refined National Supply Disruption Response hotline receives on average less than 50 calls a day 4-month stockpile in place for all products by November Commission advice on new stockpile |
| Distribution | Distributed to 226 NHS trusts | Distributed to 58,000 different settings Local resilience forums Mobilised surge capacity across the public and private sector |
PPE portal A blue-print for rapid mobilisation for other pandemic responses |
| UK manufacturing | Less than 1% of PPE manufactured in the UK | Signed contracts with UK manufacturers Disposable PPE by default |
Reviewing future requirements to sustain this high level of UK PPE manufacture Reusable by design PPE where possible UK-based supply is anticipated to meet on average 70% of forecasted demand in December for all categories of PPE excluding gloves |
| User needs | Difficulties with PPE fit reported and compatibility with working practices | FFP3 fit-testing pilot Reflecting user need and preferences in PPE provision UK manufacturing uniquely placed to engage directly with users Shift towards more innovative and sustainable PPE |
2. Scope
2.1 Without any specific threat of COVID-19 or similar, the winter always presents a challenging time and places significant pressure on the NHS and social care. This strategy sets out how government is preparing for a potential second wave of COVID-19 or concurrent pandemic in England alongside these seasonal pressures. DHSC is confident that we have secured enough supply for this winter period and that we have the processes and logistics in place to distribute PPE to where it is needed.
2.2 The strategy covers the 6 specific categories of medical-grade PPE products required to protect against transmission of COVID-19:
-
films (aprons, body bags and clinical waste bags)
-
eye protection (goggles and visors, reusable and single use)
-
face masks (IIR, FFP3, FFP2 and PAPR respirator)
-
gloves
-
gowns (reusable and single use)
-
chemicals (hand hygiene, general purpose detergent)
2.3 DHSC will provide PPE to meet the requirements of all health and social care providers in England to support their COVID-19 needs, as well as other public sector organisations such as prisons and the police force. Our centralised procurement approach ensures that value for money (VfM) is secured through sound and legally compliant procurement processes. We will provide COVID-19 related PPE in full until March 2021 at the earliest. A decision on the future procurement model will be made next year.
2.4 Face coverings, as opposed to face masks, are out of scope of this PPE strategy. However, DHSC has played a key role in supporting Public Health England (PHE) to define guidance and ensuring distinction between the requirements for medical-grade PPE and face coverings so that medical-grade PPE can be prioritised for those settings where it is needed.
2.5 Co-operation across and between all 4 nations has been a key part of ensuring PPE gets to where it is needed. This is a UK-wide approach underpinned by a protocol being agreed between the 4 nations. Scotland, Wales and Northern Ireland will receive a Barnett formula allocation for purchase of PPE.
2.6 We are also continuing to work closely with colleagues in the Crown Dependencies and overseas territories to understand their needs and have throughout the COVID-19 response made significant stock available to them.
3. Context
3.1 The COVID-19 pandemic created an unprecedented PPE supply and distribution challenge for the health and social care sectors. The safety of staff working in health and social care was always the priority and the emergency response was shaped and designed to meet the emerging evidence of where there was need and where PPE would enable the ongoing delivery of safe and effective care that saved lives.
3.2 Our PPE plan, published in April 2020, set out our goal to ensure that health and social care staff get the PPE they need. The plan had 3 strands: guidance, distribution and future supply.
Guidance
3.3 Clear, concise, up-to-date guidance is essential to ensure those who should use PPE understand what is appropriate for them and their job and how to use PPE correctly and safely. To support this, government created a central hub of guidance on gov.uk. This guidance was updated on an ongoing basis as we learned more about how COVID-19 is transmitted and the risk to workers, especially health and social care staff. Understanding the pace and pressure under which health and social care staff are working, we produced easy to understand tables which show simply and at a glance what PPE is required in different settings.
Distribution
3.4 Prior to the current crisis, business-as-usual procurement of PPE was decentralised across health and social care settings. NHS trusts in England could procure their own PPE independently or via the NHS supply chain. Other health and social care organisations, including primary care organisations, were responsible for sourcing their own PPE through wholesalers or directly from suppliers.
3.5 Alongside this, PHE maintained the Pandemic Influenza Preparedness Programme (PIPP) stockpiles, including PPE stocks, on behalf of DHSC. This stockpile was built up over time and focused on the requirements for a response to a possible influenza pandemic. The devolved administrations held stockpiles separately for each of their nations.
3.6 However, different distribution plans were required to respond to the crisis. While the NHS supply chain and the PIPP stockpile were an important source of PPE, they were not designed to meet the operational need for the product types, volume and pace of distribution required for COVID-19. For instance, COVID-19 is a form of coronavirus, not an influenza virus, and therefore has different PPE requirements. To ensure that PPE reached where it needed to go, DHSC has significantly scaled up its distribution network and pace of delivery.
3.7 The existing NHS supply chain for PPE in England was designed to accommodate delivery to 226 NHS trusts. DHSC is now providing emergency PPE supplies to 58,000 different settings, including care homes, hospices, primary care providers such as GPs, community care organisations, coastguards and prisons. Many of these settings have never had need for certain items of medical-grade PPE before. This has been an unprecedented shift in scale in order to ensure that the right type and quantity of PPE was able to be obtained by all settings during a period with a volatile supply chain and global demand outstripping supply.
3.8 In general, adult social care sourced their own PPE through their usual or dedicated wholesaler routes. However, where providers were unable to access PPE as a result of global supply chain volatility, DHSC made emergency channels available. We established new emergency distribution channels through direct drops to local resilience forums (LRFs) to help them to respond to urgent local spikes in need across the adult social care system and other frontline services.
3.9 We took a targeted approach which considered the particular needs of providers. For example, in partnership with the e-commerce industry, we designed a new online portal to help primary care and small social care providers who were under-represented in terms of access to wholesalers. We have now invited around 52,000 primary and social care providers in England to register and order through the online PPE Portal, delivering over 100 million items of emergency PPE so far to support their COVID-19 needs.
3.10 Finally, a National Supply Disruption Response (NSDR) helpline was set up to supply a small amount of emergency stock to any service with an immediate and critical need that could not be met through other channels. This helpline was available to support requests from all 4 nations and the Crown Dependencies.
Supply
3.11 PPE had historically been in plentiful supply with over 80% being manufactured in China but that situation changed rapidly as the COVID-19 pandemic unfolded across the world. Disruptions in Chinese manufacturing fractured global supply chains, creating shortages in the face of soaring demand. Market competition increased, trade restrictions were implemented, and commercial flights were grounded. Securing supplies of critical PPE for all health and social care settings required expansion of suppliers of PPE from overseas and increased domestic manufacturing capability.
Average monthly number of PPE items distributed for use by health and social care services
The graphic below shows that the average monthly number of PPE items distributed for use by health and social care services increased during COVID-19:
- distribution of aprons increased by approximately 550% from 10 to 15 million units per month pre COVID-19 to 70 to 80 million units per month during COVID-19
- distribution of clinical waste bags increased by approximately 170% from 4 to 5 million units per month pre COVID-19 to 7 to 8 million units per month during COVID-19
- distribution of body bags increased by approximately 450% from 6 to 8 thousand units per month pre COVID-19 to 30 to 35 thousand units per month during COVID-19
- distribution of eye protection increased by approximately 17,000% from 40 to 45 thousand units per month pre COVID-19 to 7 to 8 million units per month during COVID-19
- distribution of masks increased by approximately 4,700% from 1 to 2 million units per month pre COVID-19 to 85 to 90 million units per month during COVID-19
- distribution of gloves increased by approximately 200% from 145 to 150 million units per month pre COVID-19 to 310 to 320 million units per month during COVID-19
- distribution of gowns increased by approximately 1,600% from 60 to 65 thousand units per month pre COVID-19 to 1 to 2 million units per month during COVID-19
- distribution of hand hygiene increased by approximately 950% from 170 to 175 thousand units per month pre COVID-19 to 1 to 2 million units per month during COVID-19
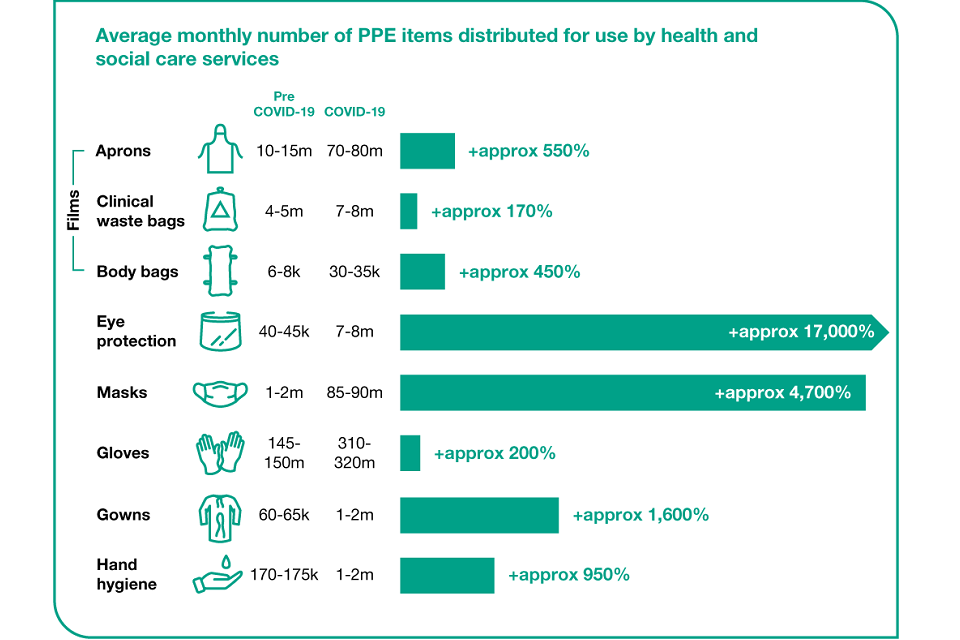
Graphic showing how the average monthly number of PPE items distributed for use by health and social care services increased during COVID-19
3.12 A cross-government PPE sourcing unit, staffed by over 400 people, was established to secure new supply lines from across the world. Government contracted with over 175 new global suppliers through a bespoke online tool that enabled any potential and interested supplier to express their interest in supplying PPE for the emergency response. This was an operation of unprecedented scale and complexity, involving the Foreign and Commonwealth Office (FCO), Department for International Trade (DIT), Ministry of Defence (MOD), DHSC and Cabinet Office, as well as direct NHS procurement. It resulted in DHSC raising purchase orders for over 32 billion items of PPE direct from new relationships in source countries, as well as through our trusted UK suppliers to the NHS. Of the 32 billion items purchased, over 16 billion items (50%) have already been delivered or are in transit.
3.13 In the UK, the end-to-end process of design through to manufacture, including procurement processes and governance approvals, was streamlined to ensure new domestic PPE supplies were rapidly procured and approved in a robust and legally compliant way. The PPE which was procured through this end-to-end process was then quickly delivered to where it was needed. Hundreds of UK manufacturers responded to the call to arms and DHSC have now signed contracts with UK-based manufacturers across all PPE categories except gloves.
3.14 Crucial to our procurement process was to understand the level of demand for PPE. At the start of the crisis, there was no PPE demand model. DHSC developed one at pace using several assumptions based on PHE guidance which were tested with clinical colleagues and end users. While these assumptions have proved more conservative than the actual usage data, these assumptions provided an agreed and sense-checked basis for procurement until we could collate additional data and information.
3.15 The emergency response phase introduced system improvements and changes that we will want to maintain as we stabilise and build resilience. For example, the pace at which the response was mobilised required a strong focus on data and information systems. Where urgency was such that direct contract awards needed to be made under permitted procurement law exemptions, we ensured that VfM was obtained through robust negotiation and benchmarking.
3.16 Disparate data sources, information and systems have been brought together and have been further refined to develop a clear picture of the end-to-end supply chain. We are now moving away from a system of disparate data with manual entry to one that is increasingly automated and enables a ‘single version of the truth’ that can give a dynamic picture from demand through to delivery. This national end-to-end view offers real potential for the system going forward.
3.17 DHSC has secured enough PPE for the winter period and we are building a 4-month stockpile available to cope with a future surge which will be in place by November 2020. We are now prioritising:
-
securing resilience of supply and the stability of longer-term deals by procuring diverse and resilient frameworks to ensure supply availability, continuity and VfM
-
continuing to support the increased UK manufacturing capability
-
incorporating user feedback in our future provision of PPE
4. Building resilience and overcoming supply challenges
We have built resilience and overcome supply challenges to make sure we are prepared for what’s next, including winter pressures.
A clear picture of demand for medical-grade PPE
4.1 Fundamental to the effectiveness of our strategy will be the accuracy with which DHSC can understand the level of demand for PPE in different settings and scenarios. This is not just about how much PPE we need, but what combinations of equipment, and in what type and sizes. Section 6 of this strategy details the steps that we are taking to meet different user needs.
4.2 During the COVID-19 emergency response a PPE demand model was established. The model assumptions were developed from PHE’s guidance and tested with clinical colleagues and end-users. Over 100 senior managers and clinicians provided input and modelled outputs were ‘sense-checked’ against what was seen in hospitals via chief executive officers, chief nursing officers and chief medical officers reviewing local data.
4.3 Once established, we continued to collate additional information to improve the data and assumptions in the model and triangulated the model with real data on usage. For example, at the start of the emergency response we did not have enough information about how social care settings were securing or using PPE. We completed a number of surveys and through commissioning several information requests, we collected data on different settings in adult social care and now have a rich source of information about how social care settings responded to the crisis and the role wholesalers played in supplying PPE to this sector. We have also carried out a PPE usage survey of GP practices and a similar survey for dental practices will soon be underway. As in-person, non-urgent primary care services have restarted, the model has been updated to reflect this increased usage and operational changes that have been made to keep patients and staff safe.
4.4 We developed the model over the course of the pandemic. The experiences from 16 different care sectors, covering over 275 factors, are now fed into the requirement model. This has included adapting the model to:
-
determine COVID-19 versus non-COVID-19 demand, including consideration of increasing demand as more NHS services reopen and come onstream
-
improve assumptions on the social care sectors’ use of PPE
-
improve the balance of PPE items used by GP practices
-
include assumptions on other sectors’ use of medical-grade PPE
-
consider the impact of seasonal flu in winter 2020 to 2021, including the PPE required to run an expanded flu vaccination programme
4.5 At the peak of the pandemic, the priority was to supply medical-grade PPE to health and care settings where providers could not obtain PPE from business-as-usual suppliers. Many other public sector settings were scaled back and, where they required PPE, most drew on their own reserves and contracts, with DHSC supplying to a small number of key sectors. Over the summer, with a stronger supply chain in place, DHSC has collated requirement data from across government and has built this into the demand model. DHSC will be supplying medical-grade PPE to wider sectors until March 2021 based on this demand modelling. The demand model will continue to be adjusted to reflect new information, increased activity, changes in policy and requirements for medical-grade PPE.
A product category approach
We are ensuring resilience to future demand surges through detailed category analysis
4.6 A resilient supply chain system is capable of withstanding, adapting to, and recovering from disruption so that it can continue to meet supply needs, and, in the case of a pandemic, can raise production to meet increased demand.
4.7 There are significant differences in the nature of the market for each category of medical-grade PPE and in order to achieve optimal resilience in DHSC’s supply chains, a detailed category by category approach is necessary. The approach to securing increased resilience will look different for each category of PPE, and will include a combination of stockpiling, strengthened relationships with strategic suppliers, broadening the diversity of our supply base nationally and internationally, and potentially contracting with suppliers to hold extra manufacturing capability for use in the event of a crisis.
4.8 DHSC PPE category leads have conducted a detailed analysis of DHSC’s supply options for their category with the primary objective of a resilient security of supply and 4 months’ additional stockpile. Factors for consideration include an assessment of DHSC’s confidence levels that stock will arrive to time and quality, expediency of access, and the extent to which supply options are vulnerable to risks relating to scarcity of raw materials required for production. These factors will form part of future tender evaluation processes for PPE products. Recognising that increased UK manufacturing is an important part of a more resilient supply chain but involves varying levels of time and investment to set up depending on PPE category, category leads have suggested the optimal mix of UK manufacturing and purchasing from overseas.
Raw materials
4.9 Through the PPE category approach, the category leads have developed a greater understanding of the supply chain and the necessary elements that support the manufacture of the 6 specific categories of medical-grade PPE products required to protect against transmission of COVID-19. The category leads strategies’ development did not just identify and appraise the supplier base, but also looked at the risk of raw materials for internal and UK manufacture. We were able to identify and look to mitigate raw materials risks by seeking to diversify the supply, exploring the capabilities of new entrants into the market, reducing reliance on some of the raw materials (reuse) and improving the diversity of similar raw materials.
4.10 The category leads have examined the future demands and engaged with international and UK manufacturers to ensure resilience in raw materials. Additionally, the available sources of raw materials have increased as demand has increased globally. Any raw material demand will form part of future tender evaluation process for PPE products and we have reviewed the bulk purchasing of raw material into the UK.
4.11 In each individual product category, we now have a supply mix that secures continuous supply for the coming months and are building a 4-month stockpile. This includes understanding how the mix will alter as demand rises.
Improved relationships with overseas suppliers
We are further strengthening our resilience by focusing on long-term deals with a more diverse range of overseas suppliers
4.12 COVID-19 has reinforced the importance of understanding the UK’s relationship with global supply chains, with most of the world’s PPE supply made in China. The UK government therefore continues to pursue diversification of supply through trade in overseas markets. As part of a combined cross-government effort, we have screened and approved global manufacturers and have developed a pre-market supply chain engagement plan that, within the public procurement rules, enables suppliers to better support DHSC’s needs. We will use the data we gathered in this pre-market engagement to inform tender specifications in order to create diverse and resilient frameworks to ensure long-term supply security. For each category we have considered options that secure medium to long term capacity through setting up Original Equipment Manufacturers (OEM) contracts, as well as purchasing on spot markets.
Strengthening relationships with overseas markets
The (COVID-19) International Partnerships Initiative led by the Foreign, Commonwealth and Development Office (FCDO) is working to deepen the UK’s PPE resilience through international co-operation and mutual support. They are in discussion with other countries about potential areas for international co-operation and reuse.
These potential areas for co-operation include agreements on mutual exchange of PPE in the event of a further crisis, commercial co-operation, information sharing to improve readiness for new demand surges, collaboration on demand reduction technologies on cleaning and reuse of PPE, and open markets to liberalise trade and eliminate export restrictions.
Enhanced distribution networks
Striving to ensure PPE arrives to time and is of the right quality
4.13 During the emergency response, a logistics and distribution team was rapidly established with resources from the NHS, military, business and volunteers. The focus was to get PPE rapidly and reliably to the end user. As the system stabilises, DHSC is now able to move to an enhanced model, benefiting from our experience of some of the collaborations and processes that emerged in the emergency and have served us well.
4.14 Regarding the distribution to the various customers, a range of logistics solutions are being secured. At the moment smaller volumes are being ordered through the PPE portal through a ‘pull’ system (customers order what they need), and other larger quantities (pallets) are being distributed through a ‘push’ system (an agreed quantity and mix is sent out on a regular basis, monthly or weekly). Some customers require a tailored solution which we are defining with each stakeholder, understanding their specific needs in terms of quantities, storage capacity, and frequency of orders.
4.15 The warehouse follows a quality assurance process to ensure products sent to customers are of the expected standards. This includes sampling and sending through documentation and photographs to regulators for approval.
4.16 The PPE portal can be used by all adult social care residential care homes, domiciliary care providers, children’s social care settings, GPs, community pharmacies, dentists and optometrists in England. The PPE portal is intended to meet all COVID-19 needs supplied for free to these NHS contractors, supplementing the PPE supply for business-as-usual needs that these settings should continue accessing via their normal supply routes. The PPE portal product range has been expanded and now includes aprons, gloves, type IIR masks, hand hygiene and visors. Additional items, such as respirator masks and gowns will also be made available to eligible service providers via the PPE portal by October. Weekly order limits are based on provider size, and these will be increased to higher levels using modelled demand of COVID-19 PPE needs.
4.17 We have provided every LRF with a PPE stockpile that local services can access in case of a severe local spike of COVID-19 or in the unlikely event of a temporary failure of other PPE distribution methods. Each LRF will have up to a week’s supply of FFP3 masks and a month’s supply of other PPE items for meeting the demand from local services in their area.
4.18 We are setting up bespoke PPE distribution arrangements for those LRFs and local authorities that would like to assume a role for regular PPE distribution to services that cannot be supplied via the PPE portal. We are exploring alternative distribution routes in those areas where LRFs are not assuming a role.
4.19 During the crisis, many departments across government secured PPE to meet the needs of their public services. DHSC contributed PPE to support some sectors, for example prison healthcare. During the emergency, government always ensured that the PPE was secured in a legally compliant way consistent with public procurement law and state aid law. DHSC has a robust end-to-end procurement system in place, with confidence in the volumes that will be available. The majority of PPE provision to the public sector required to reduce COVID-19 transmission will now be supplied by DHSC until the threat of COVID-19 has passed.
How PPE is now distributed to the UK health and care systems
The diagram below shows how PPE is now distributed to the health and social care sector.
DHSC Buy, UK Make and NHS Supply Chain are responsible for buying PPE.
Once PPE is procured and has been received, it is stored in warehouses in Daventry. Some PPE is also stored in overflow storage and container storage. It takes 48 hours for requested stock to be available to pick from the Daventry warehouse. Deliveries are made from the Daventry warehouse 7 days per week.
PPE is distributed from the warehouse direct to NHS trusts and other government departments. It is distributed to non-acute healthcare and social care via the PPE portal (e-Portal), LRFs, wholesalers and the NSDR helpline. PPE is also distributed to the devolved administrations and Crown Dependencies by request.
Allocations are made to: NHS trusts, other government departments, the NSDR, the PPE Portal (e-Portal), LRFs, wholesalers, devolved administrations and Crown Dependencies (by request), and other providers.
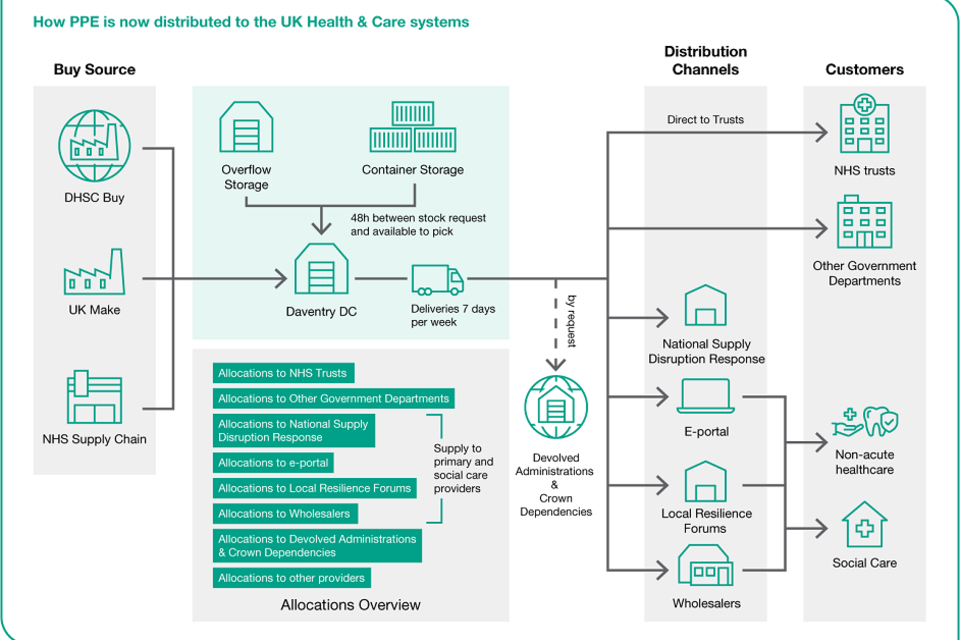
Graphic showing how PPE is currently distributed
Stockpile
Learning from experience, we have ensured our stockpile is ready for winter and any second wave of COVID-19. We are also assessing the stockpile requirements for other types of pandemic threat and commissioning new expert advice to inform this.
4.20 To ensure the UK remains able to respond rapidly to demand surges in the future, DHSC is building a strategic stockpile. This will be equivalent to 4 months’ (120 days) stock of each product category and will be in place and stored in our warehouses by November 2020.
4.21 In some product categories, for example aprons, where we have increased UK manufacturing capability, we have contracted with UK suppliers to retain some manufacturing capacity which could be switched on at short notice to meet additional demand. For these products, the stockpile will bridge the gap between a demand surge and UK capacity ramping up. Given this improved supply, PHE withdrew its Acute Shortages Guidance on 9 September 2020.
Days stock at COVID-19 usage levels on 1 November
The graphic below shows that on 1 November, we will have the following days stock at COVID-19 usage levels:
- 144 days stock of aprons
- 132 days stock of eye protectors
- 144 days stock of FFP3 face masks
- more than 180 days of type IIR face masks
- 139 days stock of gloves
- more than 180 days stock of gowns
A 4-month stockpile is equivalent to 120 days of stock.

Graphic showing the stock levels for different types of PPE that will be held by 1 November
4.22 Our storage network consists of over 25 locations across the country. All stock is visible through a single system that keeps similar products together and that we can easily access in the event of a demand surge. Stock can be distributed to customers within 48 hours of the order being placed.
4.23 To enhance future preparedness, as well as COVID-19 stockpile, we want to consider stockpile requirements for other types of pandemic threat. We are therefore beginning a review and commissioning new advice from experts such as NERVTAG and other scientific advisers to provide clinical input and leadership to determine the nature, composition and volume of a future pandemic stockpile.
A ‘blueprint’ for rapid mobilisation
We are confident we have a robust plan to stand up rapidly, if necessary
4.24 Throughout the emergency response there have been remarkable contributions from across the public and private sector, both of which have stepped up and worked effectively together in response to the pandemic.
4.25 As the people who helped us manage the procurement and distribution of PPE during the late winter and spring return to their normal roles, we have ensured that we are prepared to respond to any future need. We have developed a robust plan to stand procurement and distribution systems back up at pace to provide a timely response which provides maximum effectiveness. The plan includes a clear understanding of the triggers for when any emergency resource should be stood up, identifying the number of people and types of skills needed in advance, and a system in place to provide a single source for data and a full line of sight of the supply and distribution process.
4.26 The model developed to respond to this pandemic could become the blueprint for creating a highly effective supply organisation for health and social care settings in other pandemic responses. Learning, tools and resources from this response are being recorded and archived to make them available for any future large-scale response. A plan for how these will be picked up in a future response will be developed to ensure that they are of use when the need arises.
5. Increased UK manufacturing capability
Increased UK manufacturing capability has been a significant achievement. This puts us in a stronger supply position and offers opportunities for innovation.
5.1 UK manufacturing is now in place in all but one product category (gloves as raw materials are not available in the UK). On average, UK-based supply is anticipated to meet 70% of forecasted demand in December for all categories of PPE excluding gloves. This is an extraordinary leap. For example, there was no production of aprons in the UK prior to the COVID crisis and there are now 4 manufacturers (Elite, Polystar, PFF, Lincoln) who have repurposed their factories from producing plastic bags to producing plastic aprons to respond to the crisis. This ‘can do’ attitude is indicative of the response by UK industry to this crisis and its support for frontline staff.
5.2 Government received over 24,000 offers of support from more than 15,000 suppliers, to assist with the crisis and provide PPE to frontline staff. Many companies and individuals have worked with local hospitals and care providers to supply additional PPE. In central government, we prioritised deals with companies that could provide large volumes at pace. We have signed contracts with UK manufacturers across all PPE categories except gloves.
5.3 This strong domestic supply base transforms our ability to respond to a future crisis and provides greater resilience for any second wave. It also has wider benefits including the potential to create jobs and for the UK to become a centre for innovative products that meet user needs. Throughout this transformation of UK PPE manufacturing capability, government ensured that the specific COVID-19 response guidance provided by the European Commission to the whole of Europe was followed, to ensure that suppliers were dealt with fairly, transparently and that subsequent contracts agreed were legally compliant.
Honeywell masks
Honeywell has been contracted to produce at a site in Motherwell and will have the capability to produce more than 65 million FFP2 and FFP3 respirators masks per year. These face masks protect wearers from up to 99% of external particles, such as dust, pathogens and mould.
The workforce has used their expertise and technical capability to repurpose product lines so that these types of masks can be manufactured on the site for the very first time. The production has started and will run until the end of 2021 and will create around 450 jobs.
Survitec gowns
Survitec was selected by DHSC to produce sterilised surgical isolation gowns in order to supply the NHS with much needed PPE.
Survitec’s Birkenhead factory, which has continued to operate during the COVID-19 crisis supporting the UK’s aerospace and defence industries, has been expanded to include a dedicated area for the production of the sterilised surgical isolation gowns. The company has hired over 100 additional workers from the local area to support this critical work.
Survitec already produces safety-related products for strictly regulated environments such as aerospace and has worked closely with the government in order to move quickly through the regulatory and procurement process thereby enabling it to begin production upon receipt of the specialised raw material and to ramp up production of the gowns for the health and social care sectors.
PFF Packaging Group aprons
PFF, an independently owned, entrepreneurial UK manufacturing company, was selected by DHSC to manufacture disposable aprons to supply the NHS with essential PPE.
PFF continued to operate during the COVID-19 crisis, supporting the UK’s food retail sector through the production and supply of food packaging and additionally standing up new capability and capacity to manufacture aprons. At one of the company’s sites, based in Washington, in the North East of England, PFF has reorganised the shop floor and created a dedicated area to produce the aprons 365 days a year, 24 hours a day, 7 days a week.
The business has invested over £1 million to manufacture this new product line of aprons. Specialist machines have been purchased and commissioned to produce the required output volumes of the aprons onto a roll format during the 24-hour production and packing process. Over 100 additional workers have been hired for the duration of the contract to deliver this critical work. PFF is proud to be helping the NHS and simultaneously creating job opportunities for the North East region.
5.4 We are now reviewing future requirements and considering the best way to re-procure a resilient supply which can incentivise and sustain this high level of UK PPE manufacture.
5.5 We will consider how our tendering principles and criteria will need to adapt to deliver our overall approach to resilience, ensuring that the experience and learning gained from the crisis procurement processes are applied in the future, for example short lead times for delivery.
5.6 Building resilience in the PPE supply chain cannot be separated from government’s wider efforts to support economic recovery through a New Deal. Our PPE supply chain can support and align with our goals for UK industry, levelling up jobs and skills across the country, and doing so in a way that is ethically responsible, supporting our ambition to eradicate modern slavery, and greener, helping us realise our net-zero ambition. We are therefore also considering how our tendering principles and criteria can ensure high environmental standards and ethical labour practices.
5.7 The government published the world’s first Government Modern Slavery Statement in March 2020, setting out how we are tackling modern slavery in government supply chains. Moving forward, where it is relevant and proportionate, contractual clauses will be included to prevent instances of modern slavery. Additional contractual provisions could allow for further auditing, supplier remediation, and/or adherence to international labour standards, to give just a few examples. We will work in partnership with our suppliers to make tangible improvements to worker conditions if any issues are identified and take remedial action where documented abuses have not been adequately addressed.
5.8 We will also look at whether our regulatory approach to PPE and testing need to change to speed access to market for new manufacturers and innovators, especially where this supports wider government strategies.
Explore and increase reuse and innovation opportunities for medical-grade PPE
We are keen to build on and explore opportunities for innovation, particularly in UK manufacturing, while ensuring staff have the assurances they need that reuse is safe
5.9 Given shortfalls in global supply and further potential periods of instability in the PPE market around the world, some countries have adopted substitute and reuse strategies to manage short-term stock shortages. DHSC and the NHS are keen to pursue similar reuse and innovation strategies to improve resilience to future scarcities and VfM, but also because we remain committed to a greener NHS. The NHS Long Term Plan committed to reviewing and reducing the NHS’s environmental footprint and we want to ensure that our use of PPE aligns with this wider goal.
5.10 In April, we began UK-wide work across government and with regulators such as the Medicines and Health Products Regulation Authority (MHRA), Health and Safety Executive (HSE) and the Office for Product Safety and Standards (OPSS), to rapidly identify and assess the potential of different reuse opportunities.
Safe repurposing of single-use PPE in emergency circumstances
5.11 We want to ensure that in the event of an emergency response, we have options for safe, effective decontamination of single-use PPE where other options for securing supplies have been exhausted. Our current focus is on FFP3 respirators. This is the most challenging item in terms of global availability and costs have escalated considerably compared with historical pricing. To ensure resilience and provide emergency provision of respirators in this challenging circumstance, countries are exploring whether it is possible to decontaminate single-use FFP3s so they can be reused. We are conducting testing using Moist Heat Treatment (MHT) on a range of masks. MHT describes the technique by which decontamination of single-use FFP3s for repurposing is achieved, by using steam sterilisers on defined time/temperature cycles. Early trials indicate certain make and models of FFP3s are suitable for MHT decontamination and further analysis is being undertaken.
5.12 As well as MHT, we are piloting a technique that aims to provide decontamination and repurposing of single use FFP3s, by using Hydrogen Peroxide Vapour (HPV) that is generated from hydrogen generators, currently used in acute settings to decontaminate rooms, wards and equipment. The testing is against agreed HSE and PHE protocols and will be undertaken with 2 UK suppliers, commencing in September 2020. Other countries already use this method of decontamination; however, we want to ensure it is safe and effective to do so in the UK and in line with regulations which currently only permit their use in situations of supply constraints. Initial results are expected in the autumn.
5.13 We will work with the Royal Colleges and unions to understand the assurances and information that staff will need to feel comfortable and confident in safely reusing PPE.
PPE designed for reuse
5.14 We want to move away from disposable by default and assess new types of PPE that are designed for reuse from the outset, particularly through UK manufacturing.
5.15 NHS England and Improvement are currently piloting the use of reusable gowns with 20 providers and 60 waiting to join the pilot, working alongside laundry suppliers to increase the proportion of reusable gowns in the system and reduce waste of single use gowns. Each reusable gown reduces the use of up to 75 single-use gowns for a modest cost increase.
5.16 We conducted a rapid review to understand the challenges and potential barriers to increased innovation and sustainability in PPE. We engaged with over 40 stakeholders to understand the actions government can take at the national level to realise the benefit of any high-impact PPE innovations. This included representatives from national teams, Academic Health Science Networks (AHSNs), HSE, providers and innovators.
5.17 The review identified a number of challenges for the development and uptake of PPE innovations. These included:
- a complicated stakeholder landscape
- a need for improved demand signalling and engagement between innovators and frontline staff
- difficulty navigating the regulatory process for new entrants
- financial and procurement frameworks that incentivise single-use PPE with low purchase prices but potentially higher overall life cycle costs
5.18 In response, we are prioritising further work to develop a framework and purchasing environment that enables a shift towards more innovative and sustainable PPE. We are also supporting engagement with all stakeholders along the innovation pathway by ensuring guidance on PPE standards and use is clear to industry and providers and working with partner organisations along the end-to-end PPE process to support the research, regulation, procurement and implementation of innovative products. This work will involve conversations with industry and across government.
| Product category | UK Make and innovation opportunities |
|---|---|
| Plastic films | UK Make capacity is now available for aprons. Pre COVID-19 this manufacturing capability did not exist in the UK. Key barriers are the availability and cost of the machines to produce aprons for different care settings. Investigating alternative materials to reduce unit costs and exploring environmentally sustainable materials. |
| Eye protection | Market research suggests the UK has the capability to both design and manufacture eye protection to meet normal and COVID-19 volumes. Eye protection lends itself to the development of a reusable product which could also be fully recyclable. |
| Masks | UK capacity is available for FFP3 masks with a large proportion of demand met by UK Make. International suppliers are also building factories in the UK. Challenges around global availability and escalation of costs. Exploring decontamination of single-use FFP3s to allow them to be reused. |
| Gloves | No existing manufacturers in the UK as raw materials are not available in the UK. DHSC continues to review the potential for buying gloves from UK-based suppliers. Looking to diversify international suppliers beyond China and Malaysia. High capital investment cost and environmental challenges are key barriers. Opportunities to re-engineer glove packaging to reduce wastage and to reduce glove usage where possible to avoid hand health issues. |
| Gowns | UK manufacturing and raw material is available from the UK textile industry by repurposing fashion or furnishings factories. Certification process for small UK manufactures presents a barrier to entry. We’re working with regulators to simplify the process. We want to increase reusable sterile and non-sterile gowns with a potential to develop gowns as a service, for example a comprehensive business model for the user including laundry. We’re working with UK textile industry and leading universities on raw materials innovation, for example graphene. |
| Chemicals | Strong UK capacity with potential to secure 100% of demand from UK-based supply in 2021. Currently there are limited innovation opportunities. |
6. Improving user experience
6.1 Our overall objective remains to supply PPE that offers protection from the transmission of COVID-19. Throughout the course of the pandemic DHSC has learnt more about user experience and our understanding of need is evolving.
6.2 PPE must be fit for purpose. In light of experience gained during the COVID-19 emergency response and incorporating user feedback on the type and quality of PPE, we assessed whether any modification to technical specifications is required. Products that are fit for purpose represent the right value to the end user and system, offering the correct protection, usability and VfM.
6.3 PPE must be fit for all. We now know more about how PPE is used on the frontline and the sort of issues that arise. As well as medical need, we need to consider the individual needs of the user. Women and BAME individuals, among others, have reported practical difficulties when using some PPE. We are committed to understanding user needs and following anecdotal feedback, NHS England and Improvement have launched a project led by the Deputy Chief Nursing Officer to gather the robust evidence and data we need to understand any problems and take action. The FFP3 fit-testing project collected data from 5,557 participants across 47 NHS trusts from a range of diverse backgrounds. Informed by this data, the NHS England and Improvement project will work with manufacturers to design FFP3 respirator masks to improve mask fit.
6.4 As part of DHSC’s efforts to collate PPE requirement data from across government (see paragraph 4.5), departments have been asked to provide information on:
- how potential inequalities have been considered
- the demographics of both their workforce and the public their workforce interact with which has proved significant in the use of PPE
- incompatibilities or difficulties observed between any of the PPE used by their workforce
This will ensure the demand model reflects the different combination and size of equipment required to meet different user needs in wider settings.
6.5 We also need to consider user comfort and any harm caused by wearing PPE, particularly for those individuals wearing PPE for prolonged periods. NHS England and Improvement are liaising with Southampton University who are undertaking research on PPE use and skin damage including critical thresholds for PPE use, the frequency of breaks required to relieve the skin and the specific regions of the face affected by different FFP3 mask designs.
6.6 Using gloves is one of the many measures health and social care staff can take to protect themselves and patients. However, there is a body of evidence demonstrating how the overuse of non-sterile gloves is associated with poor hand hygiene and the cross-contamination and transmission of healthcare associated infections, as well as contact dermatitis. To combat this, in 2018, Great Ormond Street Hospital launched an initiative aimed to improve hand hygiene practice and the appropriate use of gloves. During 2018 to 2019, this resulted in a reduction in the number of referrals to occupational health for contact dermatitis, whilst the use of plastic gloves reduced by 33%. The government is exploring whether a gloves awareness project, aimed at improving hand hygiene, may lead to improved hand health for staff.
6.7 There are also patient needs to consider and the impact of PPE on their interactions and experience. For example, those who need staff to wear alternative protective equipment in order to lip read.
Clear face masks to address communication barriers
DHSC is currently piloting clear face masks with the NHS and social care. A new deal with US-based company ClearMask has seen a limited stock of 250,000 masks made available across the UK. Some deliveries have already been distributed to NHS regions. Social care providers have access to the masks through a new pilot system with LRFs. This applies across the whole of the UK and the government is working with the devolved administrations on allocations of the masks.
The masks are see-through and have an anti-fogging barrier to ensure the face and mouth are always visible to help doctors, nurses and carers communicate better with their patients. DHSC is gathering feedback from the NHS and social care providers on their experiences. Based on the feedback we receive from the health and social care sector, we will continue to work closely with suppliers on future orders based on demand.
With around 12 million people in the UK thought to have hearing loss, the masks will be invaluable for people who need to lip-read to communicate during the ongoing response to the COVID-19 pandemic and beyond. The masks will also help those who rely on facial expressions to support communication. For example, people with learning disabilities, autism or dementia, or foreign language speakers and their interpreters.
Disability charities have welcomed the introduction of clear masks for use in frontline health and social care services and have noted the benefits they will bring to disabled people who rely on lip-reading and facial expression to communicate and for whom PPE presents a barrier in terms of their communication.
6.8 Going forward, we will take appropriate action to incorporate user feedback in PPE provision. This will be underpinned by thorough equality assessments and practical solutions and adjustments to make sure that user needs are adequately addressed.
6.9 There is a role for training and support networks to ensure that people can feel confident with the fit-testing process. Phase 2 of the aforementioned FFP3 project led by NHS England and Improvement will focus on the quality of fit-testing in NHS trusts, including improving training. NHS trusts must also comply with PHE, HSE and other COVID-19 related infection prevention and control (IPC) guidance which requires staff to undergo training that is compliant with HSE legal requirements and a record of this training is maintained. A Board Assurance Framework has been developed to support all healthcare providers to effectively self-assess their compliance. Compliance will be monitored by NHS Trust Boards and submitted at the request of the Care Quality Commission. Regional IPC leads have also been asked to set up communities of practice to support organisations with the fundamentals of IPC practice, including the fit-testing process.
6.10 Increased UK manufacturing offers more opportunities for industry to hear directly from the user and involve them in the design and development of products. Some UK manufacturers are already actively ensuring that frontline user experience and preferences are incorporated into the design and development of products.
Engaging with the frontline
Medicom has been manufacturing masks internationally for nearly 4 decades. They are building a UK factory in Northampton with the capability to supply over 100 million FFP3 respirator masks and over 500 million Type IIR masks to the NHS.
Medicom recognised that the needs of frontline staff are paramount, so they visited 4 NHS trusts to better understand the specific needs, concerns and requirements of NHS FFP3 users. They received valuable feedback on all aspects of FFP3 use in the NHS and are tailoring the introduction of the new respirators, including information and materials, so that users can feel safe and confident in FFP3s that are easy to fit-test and easy to use.
6.11 We are moving from a system of quality control to quality assurance with the onus on quality assurance at source upstream in the supply chain. Building relationships with manufacturers allows for a ‘right first time’ approach, removing unnecessary process, complexity and delay within our current operating system whilst building capability within suppliers to produce the right product every day. This relationship and understanding are key to building user confidence around product quality and reliability in addition to driving a more efficient supply with lower waste and higher user acceptance. The programme will benchmark best practice across all industry sectors.
7. Enablers
7.1 Delivery of the PPE programme will require a well-led, resilient organisational structure, as well as a governance approach that clarifies roles and responsibilities and enables robust assurance and monitoring of progress and risks.
7.2 Governance structures, controls and assurance have evolved in line with the current model and recommendations and oversight made by external authorities. The following principles underpin the overall programme governance approach:
-
Strike the right balance: between responsiveness to strategic and operational imperatives and appropriate controls.
-
Provide transparency: defined roles and responsibilities, and clear lines of sight for decision-making and risk management.
-
Create headspace: through clear delineation of day to day operations delivery and broader organisational issues and overall performance.
-
Ensure alignment: with existing DHSC and NHS England and Improvement enterprise standards, processes and procedures for governance, controls and assurance.
7.3 Successful delivery of the PPE programme will also be dependent on the governance structures ensuring that good procurement practice is maintained. PPE will be purchased using fair and open procurement processes which are consistent with both Cabinet Office guidance and national and World Trade Organisation (WTO) legal frameworks. Good procurement practice is not only a legal requirement, it delivers VfM by using competitive tensions to ensure the best mix of quality and effectiveness of PPE products are purchased for the least possible financial outlay.
7.4 It is vital that we meet this challenge as 4 united nations. At every step of the way we have ensured that we have worked side by side with the devolved nations and we have set up a 4 nations PPE oversight board to manage demand and supply.
8. Going forward
8.1 Subject to winter pressures and any second wave of COVID-19, DSHC will assess the PPE programme against the criteria listed in the box below. To complete the stabilisation phase and move to the long-term future operating model, supply and delivery of PPE will need to have been achieved against metrics associated with each of these criteria.
PPE programme success criteria
-
Continuous supply of medical-grade PPE, of the right type and quality, against a clear picture of demand.
-
Controlled programme response to a second wave of COVID-19 and scalability of supply to meet additional demand for medical-grade PPE (in the event of planned scenarios).
-
Successful delivery of a resilient supply chain system and the identification of longer-term strategic benefits.
-
Demonstration of appropriate management of resourcing, funding and risk.
-
Comprehensive handover of supply chain operations to the accepting (future) organisation and programme closure.
8.2 Throughout the emergency response, securing supply was our primary consideration. Prices were volatile due to global demand and accordingly became a secondary factor. On average, the price of PPE products has increased significantly, with some categories seeing prices double if not treble when compared to pre-COVID-19 costs. As the situation stabilises, we will refocus on achieving VfM and efficiency.
8.3 Next year, DHSC wants to start transitioning to a future model that is both resilient (able to respond to any demand surges related to COVID-19 or another pandemic threat) and proportionate. Key considerations for the model beyond March 2021 include the following:
-
To what extent and for how long should a separate PPE supply chain exist?
-
How do we build on and best use the COVID-19 experience gained from this programme?
-
How to best distribute stock and ensure that different parts of the UK health and social care system are not competing with each other to secure supply?
-
How do we maintain our UK manufacturing base?
-
How can resilience be established for the long term in order to scale supply up and down to meet any future threats?
8.4 During 2020 we have seen monumental change in the way that PPE has been secured and supplied across the country. The supply chain is now resilient and supply needs will be met through the winter. We have learnt a great deal from this experience and are in a strong position for the future.
