Newborn blood spot sampling guidelines: quick reference guide
Updated 15 December 2021
1. Introduction
Newborn blood spot (NBS) screening identifies babies who may have rare but serious conditions.
These guidelines are written for the screening programme in England. Healthcare workers in Northern Ireland, Scotland and Wales must be aware of variation in practice and conditions screened for when referring to these guidelines.
The full, referenced version of the guidelines is also available.
1.1 Blood spot quality matters
Good quality blood spots are those where the circle is filled and evenly saturated by a single drop of blood that soaks through to the back of the blood spot card. They are vital to ensure that babies with rare but serious conditions are identified and treated early.
Poor quality blood spots could lead to false negative or false positive screening results. This means that babies with a condition might be missed or babies without a condition might be referred for further tests unnecessarily.
1.2 Avoidable repeats
If poor quality blood spots are received or the fields on the blood spot card are not completed fully and accurately, the screening laboratory will request an ‘avoidable repeat’ sample.
Avoidable repeat samples can cause anxiety for parents, distress to babies and delays in the screening process. This could lead to delayed identification and treatment of an affected baby. They are also a waste of healthcare resources.
Newborn screening laboratories in England are following a national, evidence-based consensus on blood spot quality, with standardised acceptance and rejection criteria. To ensure that an avoidable repeat sample is not requested, sample takers are advised to obtain 4 good quality blood spots and complete all fields on the card accurately.
To take a newborn blood spot sample you will need:
- baby’s NHS number (use of a bar-coded label is recommended)
- blood spot card and glassine envelope
- personal child health record (PCHR) and maternity/professional record
- water for cleansing
- non-sterile protective gloves
- age-appropriate, automated incision device
- sharps box
- cotton wool or gauze
- hypoallergenic spot plaster (if required)
- prepaid/stamped addressed envelope (first class) (if not using a courier)
2. Prepare for taking the blood spot sample
It is important to offer parents an informed choice about screening for their baby, to gain consent and to prepare them for the blood sampling procedure. Eligible movers in should be offered screening as soon as possible.
2.1 Antenatal period
At or prior to antenatal booking, women are encouraged to read the Screening tests for you and your baby leaflet. Translated versions are available. Parents should be asked if they have a family history of any of the inherited metabolic diseases (IMDs) so that early screening can be offered if appropriate.
2.2 Postnatal period
Ensure parents still have access to the pre-screening booklet at least 24 hours before taking the sample. A healthcare professional should offer screening and record the parents’ decision. They should explain the procedure to parents and record in the maternity/professional record that screening has been discussed and recommended, the booklet given and verbal consent sought.
Parents should be asked if they wish to be contacted about research linked to the screening programme. If a parent does not wish to be contacted about future research on their baby’s sample, ‘No research contact’ should be recorded clearly on the blood spot card.
Ensure parents are aware that patient identifiable information may be stored by the NHS Sickle Cell and Thalassaemia Screening Programme on the newborn outcomes system.
2.3 Parents who consent to screening
Record the parents’ screening decision as ‘consent’ and their decision about future research contact in the PCHR and maternity/professional record. If the baby is in hospital, the parents’ consent decision should also be recorded in the baby’s hospital records.
The blood spot sample should be taken on day 5 for all babies. For the purpose of screening, day of birth is day 0.
In exceptional circumstances the sample can be taken between day 5 and day 8.
Parents can decline screening for sickle cell disease (SCD), cystic fibrosis (CF) and congenital hypothyroidism (CHT) individually but the 6 IMDs can only be declined as a group.
2.4 Parents who decline screening
The healthcare professional responsible for ensuring that screening has been offered should:
- record each condition declined and reason (if stated) in the PCHR and maternity/professional record (and baby’s hospital records if applicable)
- if screening is declined for all conditions, complete the details on the blood spot card (add the reason for the decline if stated) and send marked ‘Decline – all conditions’ to the laboratory
- if screening is declined for only one or some of the conditions, arrange for the blood spot sample to be taken (the blood spot card should be completed and marked ‘Decline – XX’ where XX is the condition(s) declined – add the reason if stated)
- send a notification letter to the child health records department (CHRD), GP and health visitor and a separate letter to the parents (letter templates are available to adapt for local use)
- inform the NBS lead midwife/manager
- inform the parents who to contact if they change their mind or would like further information and record this information in the PCHR
3. Enter the details on the blood spot card
Check the card’s expiry date and place on a clean surface. Complete the details at the time of sampling.
The baby’s NHS number on the blood spot card is mandatory – use of a bar-coded label is recommended. Do not delay screening movers in if not registered with a GP – the CHRD can generate an NHS number. Newborn blood spot failsafe solution (NBSFS) users can print barcode labels in the demographic details section.
If using a bar-coded label, check that the information is accurate and complete all other fields on the card using block capital letters. If a label is not available, ensure all fields are completed using block capital letters.
For all cards you should:
- complete all the fields on the card
- check the completed blood spot card with the parents and make any necessary changes
4. Collect the blood spot sample
Sample takers should check that consent for screening has been obtained and recorded.
Recommend comfort measures for the baby. Ensure the baby is cuddled and in a secure position. Suggest that the baby is breast feeding.
Clean the heel by washing thoroughly with plain water using cotton wool/gauze. The water should not be heated and the baby’s foot should not be immersed. Do not use alcohol or alcohol wipes. Allow the heel to dry completely.
Wash hands and apply gloves.
Ensure the baby is warm and comfortable. Warming of the foot is not required.
Obtain the sample using an age-appropriate automated incision device (manual lancets must not be used). An arched-shaped incision device is recommended. See Figures 1 and 2 for preferred puncture sites. Avoid posterior curvature of the heel. Allow the heel to hang down to assist blood flow. Before activation, place the automated incision device against the heel in accordance with the manufacturer’s instruction.
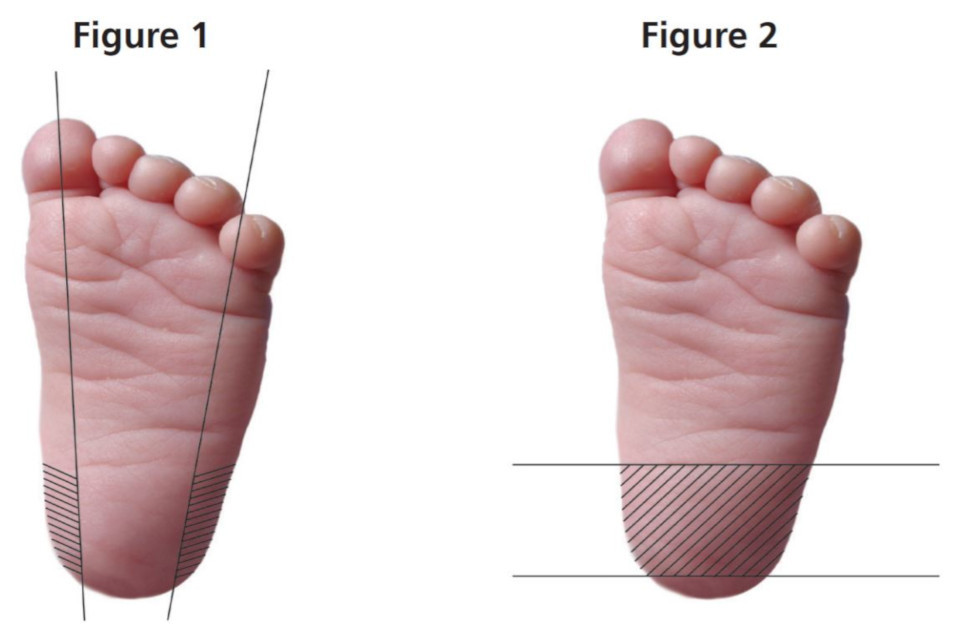
Figure 1. For full-term and preterm infants. Skin puncture must be no deeper than 2mm. Figure 2. For infants who have had repeated heel punctures. An automated incision device with a penetrative depth of no more than 1mm is recommended. These sites are also suitable for infants up to a year of age.
Good quality blood spots are vital to ensure that babies with rare but serious conditions are identified and treated early. The aim is to fill each circle on the blood spot card, using a single drop of blood for each circle.
Puncture the heel – wait for the blood to flow and a hanging drop to form. Allow one spot of blood to drop on to each of the circles on the blood spot card. There is no need to discard the first drop.
Make sure you:
- do not allow the heel to make contact with the card
- do not squeeze the foot in an attempt to increase blood flow
- allow the blood to fill the circle completely by natural flow, and seep through from front to back
- do not compress or apply pressure to the blood spots
4.1 Correct

A single, evenly saturated drop of blood that fills the circle completely and soaks through to the back of the blood spot card. Good quality blood spots are essential to obtain accurate screening results.
4.2 Incorrect

Insufficient sample: small volume spots. Risk of false negative result.

Insufficient sample: blood not soaked through to back of blood spot card. Risk of false negative result.

Inappropriate application of blood: multispotted. Risk of false negative result.

Compressed sample. Significant risk of false negative result.

Inappropriate application of blood: layered sample (for example, one spot of blood is layered directly on top of another) or blood applied to the front and the back of the blood spot card. Risk of false positive result.

Contaminated sample. Risk of inaccurate result.
Images courtesy of Wyn Griffiths, South East Thames Screening Laboratory and Roanna George, Wales Newborn Screening Laboratory.
4.3 Blood flow
If the blood flow ceases, the congealed blood should be wiped away firmly with cotton wool or gauze. Gently ‘massage’ the foot, avoid squeezing, and drop the blood on to the blood spot card.
If the baby is not bleeding, perform a second puncture on a different part of the same foot or on the other foot (see figures 1 and 2).
When sample collection is complete, wipe excess blood from the heel and apply gentle pressure to the wound with cotton wool or gauze. Apply a hypoallergenic spot plaster if required – remind parents to remove the plaster in a few hours.
5. After taking the blood spot sample
Allow blood spots to air-dry away from direct sunlight or heat before placing in the glassine envelope – take care to avoid contamination.
Dispatch the blood spot card in the prepaid/stamped addressed envelope (first class) on the same day (if not using a courier). If not possible, dispatch within 24 hours. Dispatch should not be delayed in order to batch blood spot cards together for postage. If a post box is used, ensure it is one that is emptied daily (Monday to Saturday).
Before sending the sample to the laboratory there should be no additional checking that would cause delay. Record that the sample has been taken in the PCHR and maternity/professional record, complying with local protocols. If the baby is in hospital, record and notify the baby’s screening status on discharge/ transfer notifications.
Inform parents that they will receive the results within 6 weeks (sooner if the baby screens positive for a condition). Ensure that parents know to contact their health visitor if results are not received within 6 weeks.
6. Babies born preterm or cared for in specialist units
Babies admitted to neonatal units are likely to have multiple blood samples taken. Blood spot screening should be coordinated with other tests when possible. On admission/prior to blood transfusion, babies less than 5 days of age should have a single circle blood spot sample taken for routine SCD screening. This should be on a separate blood spot card marked ‘Pre-transfusion’.
The pre-transfusion sample should be dispatched to the newborn screening laboratory together with the routine day 5 sample if the baby has received a blood transfusion in the interim. The pre-transfusion sample can be discarded appropriately if the baby has not received a blood transfusion. If the baby is transferred to another unit before the day 5 sample has been taken, ensure the pre-transfusion sample accompanies the infant.
The routine blood spot sample (4 spots) should be taken on day 5 for all babies. For the purpose of screening, day of birth is day 0.
In exceptional circumstances the sample can be taken between day 5 and day 8.
When a baby has had a blood transfusion, either intrauterine or in the newborn period, an interval of at least 3 clear days is required between the transfusion and the routine blood spot sample for CF, CHT and the IMDs.
However, in the event of multiple blood transfusions, or if a baby is on extra corporeal membrane oxygenation (ECMO), a routine blood spot sample should be taken by day 8 at the latest, even if it has not been 3 clear days since the last transfusion.
In this scenario, a repeat sample will be needed at least 3 clear days after the last transfusion or the end of ECMO. The date of the last blood transfusion or end of ECMO must be recorded on the blood spot card and on discharge/transfer notifications.
Inform parents of any outstanding screening tests, and record this in the PCHR and maternity/professional record.
6.1 CHT screening for preterm infants
Babies born at less than 32 weeks (less than or equal to 31 weeks + 6 days) require a second blood spot sample (2 spots) to be taken, in addition to the day 5 sample, at 28 days of age (counting day of birth as day 0) or day of discharge home, whichever is the sooner. Mark the card ‘CHT preterm’. Write the gestational age on the card.
If the baby is being discharged home before 28 days of age, write ‘discharged home’ on the repeat sample.
Record all blood spot samples taken in baby’s hospital records, on transfer documentation, PCHR and on an auditable IT system.
7. Ensuring completeness of coverage of newborn screening
7.1 Older babies
Babies under a year of age who become the responsibility of the provider organisation should be offered screening by a healthcare professional for all nine conditions if there are no documented results (or declines) for SCD, CF, CHT, phenylketonuria (PKU) and medium-chain acyl-CoA dehydrogenase (MCADD) (or all conditions except CF if the baby is over 56 days of age).
If there are documented results for these 9 conditions no further offer of screening is required. Only results documented in English should be accepted.
If the conclusive results cannot be found, parents should be given information and offered screening. Inform the GP if the baby is too old to be screened for CF.
7.2 Parents who consent to screening
Take a sample using the blood spot card and send to the screening laboratory. Either a capillary or venous sample can be spotted onto the blood spot card. If an automated incision device is used, ensure it is age-appropriate.
Inform parents that they will receive the results within 6 weeks (sooner if the baby screens positive for a condition).
7.3 Parents who decline screening
See earlier section for details.
7.4 Repeat samples
Repeat samples may be required from a few babies for a variety of reasons. These samples should be taken as soon as possible or at the age directed by the screening laboratory. Informed consent must be taken and parents should be informed of the reason for the repeat. Tick the ‘repeat sample’ box on the blood spot card.
A one-week interval between samples is recommended for borderline thyroid-stimulating hormone (TSH) results. Take a 4 spot sample and mark the card ‘CHT borderline’.
7.5 Failsafe processes
Provider organisations should implement failsafe measures that ensure:
- all babies that are transferred have their screening status notified
- all eligible babies are identified and offered screening
- all babies whose parents accept screening are tested
- all samples arrive at the laboratory in a timely manner
- all positive babies receive timely treatment within national standards
- parents receive their results within 6 weeks
Provider organisations should also perform daily checks of the newborn blood spot failsafe solution to identify babies that might have missed NBS screening.
