HPR volume 12 issue 20: news (8 June)
Updated 21 December 2018
PHE publishes full annual STIs data for 2017
Public Health England (PHE) has released its annual data on sexually transmitted infections and screening for chlamydia in England comprising 2 main reports:
- a review report: Sexually Transmitted Infections and Screening for Chlamydia in England, 2017 [1]
- Monitoring Rates of Chlamydia Re-testing within the English National Screening Programme, January 2013 to June 2017 [2]
The review report provides an overview of trends for the STIs of most concern in England: gonorrhoea, syphilis, chlamydia, genital herpes and genital warts [1].
The latest data show that although the overall number of new STI diagnoses decreased by 0.3% in 2017, compared with 2016 (from 423,352 to 422,147), there were marked year-on-year increases in syphilis and gonorrhoea diagnoses (up 20% and 22%, respectively, compared with 2016). These increases were particularly concentrated in gay, bisexual and other men who have sex with men (MSM), among whom gonorrhoea diagnoses increased 21% and syphilis diagnoses increased 17% between 2016 and 2017 (see figure). The increase in gonorrhoea is of particular concern given the recent emergence of extensively drug resistant Neisseria gonorrhoeae [3].
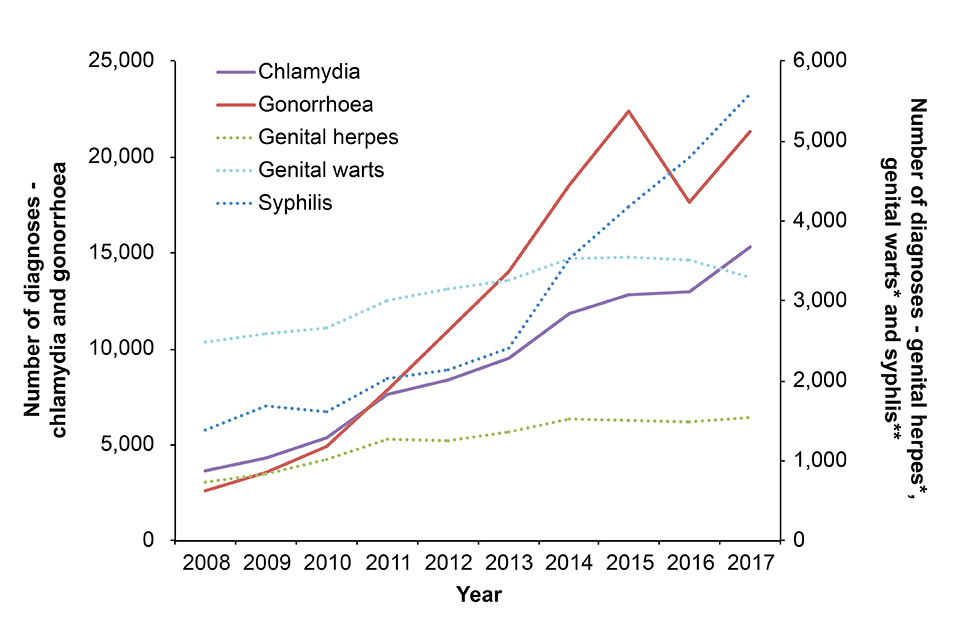
Number of new diagnoses of selected sexually transmitted infections in gay, bisexual and other men who have sex with men attending sexual health services, 2008–2017 (England). [Data from routine specialist and non-specialist SHS returns to the GUMCAD STI Surveillance System.]
However, there were continued falls in genital warts diagnoses, especially among young women. In 2017, there were 441 diagnoses of first-episode genital warts in 15 to 17 year old girls, a 90% decrease relative to 2009. This decrease is largely due to the high coverage National HPV Immunisation Programme in school-aged girls.
Chlamydia was the most commonly diagnosed STI in 2017, accounting for 48% (203,116 cases) of all diagnoses. The main STI review report includes data, from the National Chlamydia Screening Programme (NCSP), on chlamydia testing among residents in England. In 2017, over 1.3 million chlamydia tests were carried out and over 126,000 chlamydia diagnoses were made among England residents aged 15 to 24 years – the target age group for the NCSP. Overall, there were 2,361 fewer chlamydia diagnoses made among 15 to 24 year olds in 2017 than in 2016, a reduction of 2%. There was an 8% decline in the number of chlamydia tests in 2017 compared to 2016. Most of this decrease in testing took place in sexual and reproductive health services, where chlamydia testing has fallen by 61% since 2015, reflecting a reduction in service provision in this setting, the report suggests.
The separate report on re-testing following a positive diagnosis – Monitoring Rates of Chlamydia Re-testing within the English National Screening Programme from January 2013 to June 2017 [2] – presents quarterly re-testing rates for England and PHE Centre areas. Since 2013, quarterly re-testing rates for England ranged between 10.9% and 14.2% for non-specialist sexual health services (SHSs) and between 11.5% and 14.0% in specialist SHSs. Re-testing rates in specialist SHSs have increased from 11.7% in Q1 2013 to 13.1% in Q2 2017. Positivity at re-test was consistently higher in specialist SHSs (15.8% to 18.7%) than in non-specialist SHSs (11.2% to 14.3%). These findings support the inclusion of offer of re-test at around 3 months within the NCSP case management guidance.
The main STI report [1,4] concludes by highlighting PHE’s initiatives to address the higher rates of STIs in MSM, black ethnic minority populations and young people.
The full range of data and commentary published this week is provided on PHE’s annual STI and NCSP data pages in the form of data tables and slide sets. An infographic is also available.
References
- PHE (5 June 2018). Sexually transmitted infections and screening for chlamydia in England, 2017. HPR 12(20) Advance Access report.
- PHE (5 June 2018). Monitoring rates of chlamydia re-testing within the English National Screening Programme, January 2013 to June 2017). HPR 12(20) Advance Access report.
- PHE website. Multi-drug resistant gonorrhoea in England: 2018.
- ‘New data reveal 420,000 cases of STIs in 2017’, PHE website news story, 5 June 2018.
Increased parvovirus activity in England (2018)
Parvovirus B19 causes the common childhood illness, erythema infectiosum – or fifth disease [1] – widely known as ‘slapped cheek’ due to the typical presentation of erythematous cheeks which, together with rash and fever, are characteristic of the disease. Accurate diagnosis on a clinical basis can be challenging, however, and parvovirus B19 infection can be difficult to differentiate from other infections such as rubella.
In temperate countries, there is increased parvovirus B19 activity every 4 to 5 years, often with 2 to 3 years increased activity and then lower activity in the intervening years. Reported cases of parvovirus B19 were relatively high in 2017, although activity did not reach the levels seen in 2013, the previous peak year [2] (see figure). This year has also seen reports of increased parvovirus B19 activity, with the expectation that numbers will exceed those recorded in 2013 (see figure). Parvovirus B19 is not a notifiable disease and testing practice is likely to vary around the country: with the exception of women presenting with a rash illness in pregnancy, there is no recommendation for routine testing for parvovirus B19.
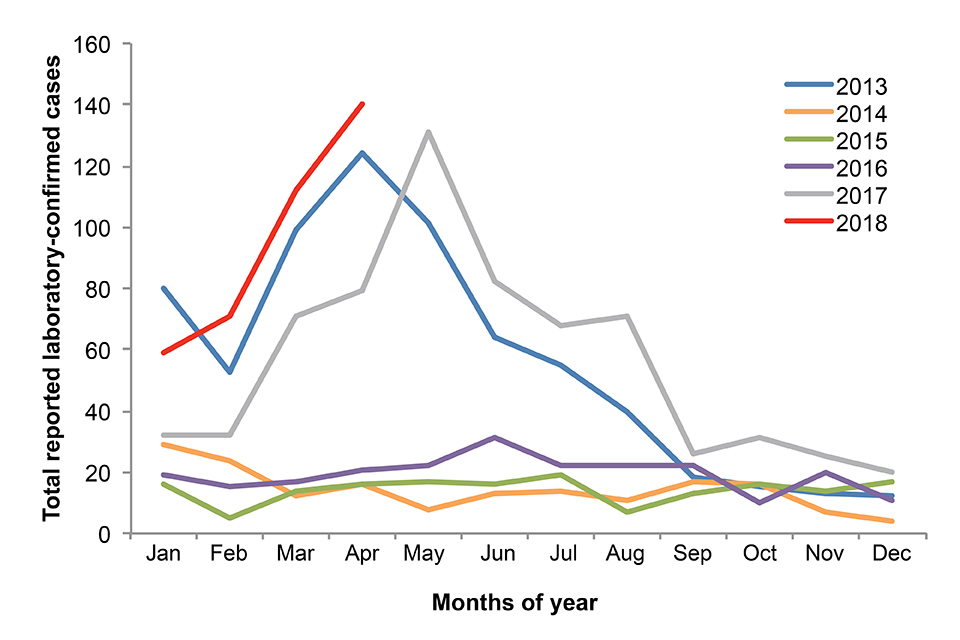
Monthly laboratory confirmed reports of Parvovirus B19 infection in women aged 15-44 years, 2013 to end-April 2018 (England only)
Infection in the first 20 weeks of pregnancy is associated with increased risk of intra-uterine death and hydrops fetalis. Infection usually presents as a mild febrile illness but in patients with increased red blood cell turnover (for example underlying haemolytic haemoglobulinopathies such as sickle cell disease) infection can lead to transient aplastic crisis, and in patients who are immunocompromised infection may lead to pure red cell aplasia and chronic anaemia. Both these groups of patients have high level viraemia and should be considered infectious. Clinicians should be aware that there are NICE Clinical Knowledge Summaries [3] and national guidelines for managing the infection in healthcare settings and the community [4], and in pregnant women [5].
References
- Brown KE (2007). Parvovirus B19 infection in the fetus and child. In: David TJ (ed.). Recent advances in paediatrics, RSM Press, 209 to 222.
- PHE (2017). Raised levels of parvovirus B19 activity in England and Wales, HPR 11(19), May 2017.
- NICE (February 2017). Clinical Knowledge Summaries: Parvovirus B19 infection.
- Crowcroft NS, Roth CE, Cohen BJ, Miller E. (1999). Guidance for control of Parvovirus B19 infection in healthcare settings and the community. J Public Health 21(4): 439 to 446.
- PE website. Parvovirus B19: guidance, data and analysis.
Infection reports in this issue of HPR
The following infection reports are published in this issue of HPR.
