HPR volume 11 issue 35: news (6 October)
Updated 15 December 2017
HIV in the UK: decline in new diagnoses in gay and bisexual men in London
There was an 18% year-on-year decrease in newly-diagnosed HIV in the UK between 2015 and 2016 – from 6,286 to 5,164 cases – according to PHE’s latest annual HIV data release [1,2], summarised in this issue of HPR [3].
The decline in new diagnoses – concentrated in gay and bisexual men and particularly marked in London – has been driven by both increased testing and more effective treatment: there have been significantly increased levels of HIV testing among gay and bisexual men attending sexual health clinics in recent years (up from 37,224 in 2007 to 143,560 in 2016) and increased uptake of anti-retroviral therapy (ART) following HIV diagnosis.
Whereas between 2007 and 2015 new diagnoses in gay and bisexual men rose steadily – from 2,850 to 3,570 – between 2015 and 2016 they decreased 21% year-on-year. The UK is one of the first countries in Europe to witness such a substantive decline in HIV diagnoses in gay and bisexual men.
The decline in diagnoses in gay and bisexual men was particularly marked in London, where diagnoses decreased by 29% – from 1,554 in 2015 to 1,096 in 2016 (see figure). Elsewhere in England HIV diagnoses in gay and bisexual men decreased by only 11% year-on-year.
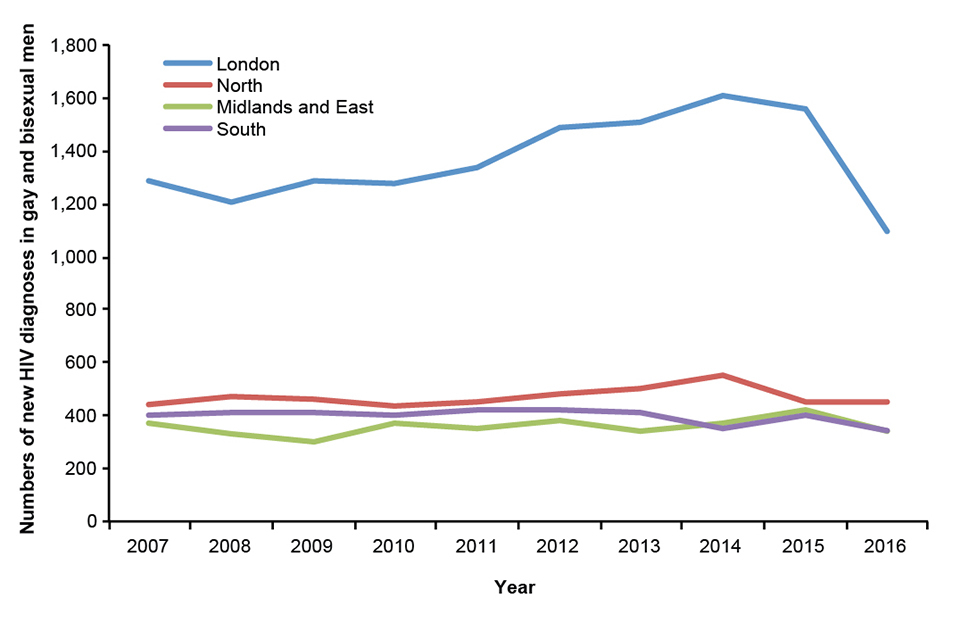
New HIV diagnoses in gay and bisexual men, by region of residence, 2007-2016, England
The largest declines were observed in parts of London with the highest testing rates and where access to treatment was fastest. That the decline in new diagnoses was due to reduced transmission was confirmed by data showing the high numbers and proportion of diagnoses that were made at a late stage of HIV infection: between 2007 and 2016, the median CD4 count at diagnosis among gay and bisexual men rose from 396 cells per cubic millimetre to 501 cpcm in London.
References
- PHE (3 October 2017). HIV: annual data tables
- PHE (4 October 2017). New PHE figures show decline in HIV diagnosis rates, PHE press release, 4 October.
- PHE (3 October 2017). HIV in the UK: decline in new HIV diagnoses in gay and bisexual men in London, 2017 report. HPR 11(35).
Cyclospora outbreak related to travel to Mexico (2017): final report
An outbreak of cyclosporiasis in UK travellers to Mexico, first reported in the HPR in July this year [1], has been declared over.
As of 27 September, 132 cases of cyclosporiasis have been reported in the UK in 2017; of these, 44 have been confirmed by a reference laboratory and 88 remain as probable cases (local laboratory diagnosis only). Cases have been reported in England, Scotland, Wales, Isle of Man and Jersey.
Although six cases were reported earlier in 2017 (two in January, one in March, three in May) cases began to increase from the beginning of June (week 22), with the majority of cases reported in June and July – a total of 92 – between weeks 22 and 30 (see figure), compared to 203 cases reported in the same period in 2016 (55% decrease).
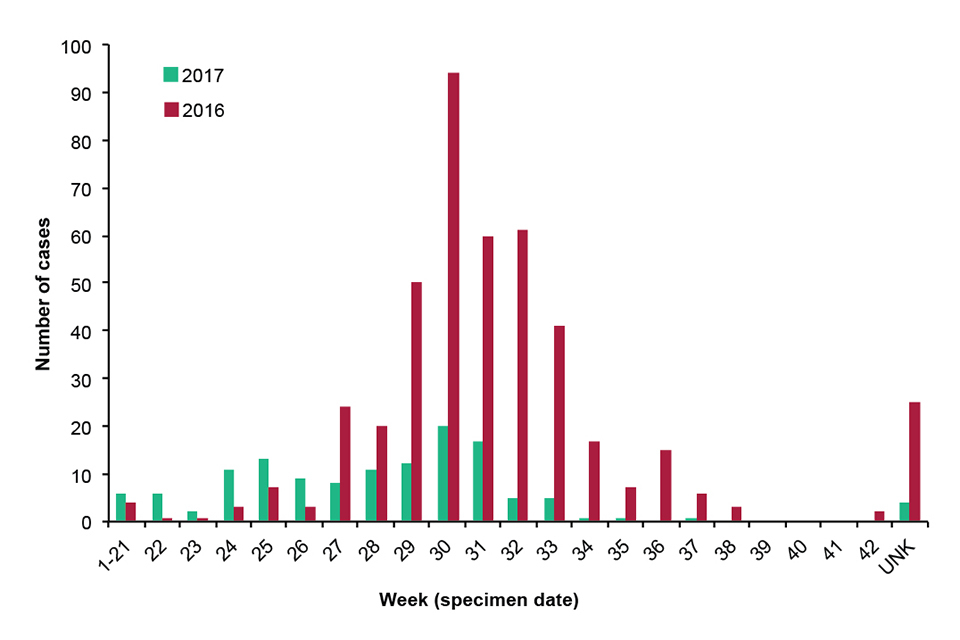
Epidemic curve of cyclosporiasis in the UK (by specimen date): 2017 and 2016
As in 2015 and 2016 [2,3], Mexico has featured as the most common country of acquisition for cases of cyclosporiasis in the UK. Of 132 cases reported in 2017, travel history information is currently known for 109 cases (83%). Of these, 84 (77%) reported travel to Mexico, 18 travelled to 14 other destinations (including three to Dominican Republic) and seven did not travel outside the UK in the 14 days prior to onset of symptoms. Of the 77 cases that travelled to Mexico with a known onset date, the earliest onset date was 19 May 2017 and the most recent onset date was 18 August 2017; 91% of cases had onset in June and July 2017. The median age for cases that travelled to Mexico was 42 years (range 16-77 years); 53% were female and 47% male.
Of the cases that travelled to Mexico, 74 had information about region within Mexico or the hotel they stayed at. Of these, all but one stayed in the Riviera Maya and Cancun region on the Caribbean coast of the Yucatán peninsula, north eastern Mexico.
Cases stayed at 27 different hotels, with 37 cases having stayed at one of three different hotels and 37 cases stayed at 24 other hotels.
Limited information on food and drink exposures was available for 50 cases that travelled to Mexico. More than two-thirds of cases consumed bottled water, mixed salad leaves, orange juice, tomatoes, mint in drinks, ice in drinks, lettuce and onions. A case-control study was not conducted; it was therefore not possible to identify the likely vehicle of infection. However, it is likely that that the vehicle of infection was a food or drink item that is seasonally distributed to hotels in Riviera Maya given that cases have occurred during the UK summer months in 2015, 2016 and 2017 and travel to Mexico from the UK occurs year round.
PHE will continue to monitor for reports of cyclosporiasis in travellers returning from Mexico throughout the year but particular vigilance should be applied during the run up to the summer holidays in 2018.
Advice on how to prevent cyclosporiasis is available on the NaTHNaC and PHE websites.
References
- PHE (2017). Cyclospora outbreak related to travel to Mexico (2017)”. HPR 11(26).
- Nichols GL, Freedman J, Pollock KG, Rumble C, Chalmers RM, Chiodini P, et al (2015). Cyclospora infection linked to travel to Mexico, June to September 2015. Euro Surveill 20(43).
- Marques DFP, Alexander CL, Chalmers RM, Chiodini P, Elson R, Freedman J, et al (2017). Cyclosporiasis in travellers returning to the United Kingdom from Mexico in summer 2017: lessons from the recent past to inform the future. Euro Surveill 22(32).
Legionnaires’ disease associated with travel to Dubai, 2016 to 2017
PHE has been supporting the ECDC response to an increased number of Legionnaires’ Disease cases in EU residents, associated with travel to Dubai, recorded over the past year in the EU agency’s ELDSnet surveillance system of travel-related LD cases in EU residents.
The UK has reported a large number of Dubai-associated LD cases among UK residents. In a recently-published rapid communication, there were 36 Dubai-associated cases among residents of the UK with onset dates between 1 October 2016 and 31 August 2017, as of 18 September 2017 [1]. As of 19 September 2017, ECDC had recorded a total of 75 Dubai-associated cases – reported from EU/EEA countries (including the UK) – since 1 October 2016 [2].
In a risk assessment for the UK [3], PHE notes that:
[T]he overall risk of LD to UK travellers to Dubai remains low [but] there may be an increased risk for those persons who are generally more likely to develop LD due to their older age (over 50 years), smoking or an underlying medical condition (such as immunosuppression or long term respiratory conditions). For travellers with clinical or radiological evidence of pneumonia and a travel history to Dubai in the 2-10 days preceding the onset of their symptoms, LD testing should be considered.
Travel health information about this situation has also been published on the TravelHealthPro website.
References
- Dabrera G, Brandsema P, Lofdahl M, Naik F, Cameron R, McMenamin J, et al (2017). “Increase in Legionnaires’ disease cases associated with travel to Dubai among travellers from the United Kingdom, Sweden and the Netherlands, October 2016 to end August 2017”, Euro Surveill 22(38) Rapid Communication.
- ECDC (21 September 2017). “Increase of Legionnaires’ disease in EU travellers returning from Dubai since October 2016”. Rapid Risk Assessment: first update.
- PHE/NaTHNaC (15 September 2017). Risk Assessment on Legionnaires’Disease Associated with Travel to Dubai.
Infection reports in this issue of HPR
The following reports are published in this issue of HPR.
