Health matters: cold weather and COVID-19
Published 11 November 2020
Summary
As we approach the first winter with coronavirus (COVID-19) circulating, it’s essential that action is taken across the health and social care sector to enable people to stay safe and well and to ensure that the NHS is not overwhelmed.
This edition of Health Matters will cover the impact of cold weather on health, how COVID-19 amplifies cold-related risks, and actions that can be taken to prevent harm, particularly to those most vulnerable.

Cover image for Health Matters edition on cold and COVID-19 showing people reacting to cold weather
Cold weather – a public health challenge
Cold-related deaths represent the biggest weather-related source of mortality in England, and on average, there are approximately 35,000 excess winter deaths each year in England and Wales. The reasons more people die in winter relative to other times of the year are complex and interlinked and include:
-
poor quality housing, particularly cold homes
-
circulating infectious diseases, particularly flu and norovirus
-
physical hazards such as snow and ice
-
health inequalities
As well as the significant rise in deaths, the winter period also sees a substantial increase in illnesses.
Despite there being several contributing factors, in many cases simple preventative actions could avoid many of the deaths, illnesses and injuries associated with the cold. Many of these measures need to be planned and undertaken in advance of cold weather.
This will be the first winter that SARS-CoV-2 (the virus that causes COVID-19 disease) will be circulating. It’s critical that plans are in place to address the risks that may arise from the concurrence of cold and COVID-19 this winter.
Vulnerable groups
Some groups are particularly vulnerable to cold weather, including:
-
older people, especially those over 65 years old
-
older people who are frail and/or socially isolated
-
people with pre-existing chronic medical conditions such as cardiovascular and respiratory conditions, in particular chronic obstructive pulmonary disease (COPD) and asthma, and diabetes
-
children
-
people with cognitive impairment, mental health conditions or learning difficulties
-
people assessed as being at risk of or having had recurrent falls – over 65s are more at risk of falls and home hazards increase this risk, which may be exacerbated by being indoors for long periods
-
people who are housebound or otherwise have low mobility
-
people living on a low income or in deprived circumstances
-
people who are living in households experiencing fuel poverty
-
people experiencing homelessness or rough sleeping
-
pregnant women
Many of these groups are also at greater risk of severe illness from COVID-19, as well as other winter illnesses such as flu. Therefore, it is more important than ever that those most vulnerable are supported this year.

An infographic showing the groups of people more at risk of harm from cold weather, such as over sixty-fives and children.
Health impacts of exposure to cold weather
The risk of death increases as temperatures fall, so periods of extremely low temperatures can cause significant harm. However, adverse impacts on health occur at outdoor temperatures that might be considered relatively mild (4 to 8°C).
The human body responds in several different ways to exposure to cold weather. Exposure to cold temperatures has a range of physiological effects, including increased blood pressure and risk of clotting, suppression of the immune system, diminished capacity of the lungs to fight off infection and narrowing of airways.
Cold temperatures and winter weather can have direct and indirect effects on our health.
Direct effects include:
-
heart attack
-
stroke
-
respiratory disease
-
influenza
-
falls and injuries
-
hypothermia
Indirect effects include:
-
poor mental health – this can be due to the impacts of living in a cold home, reduced contact with loved ones, staying at home to keep warm, getting into debt due to fuel bills and/or becoming socially isolated
-
reduced education and employment success, as a cold home affects a child’s ability to study or do homework
-
carbon monoxide poisoning, which can result from a faulty heating system and poorly ventilated home
-
poor hygiene, from a lack of hot water for showers and washing
-
poor diet and nutrition, from a lack of energy for home cooking and/or financial pressure due to higher energy bills

The infographic highlights the direct effects of cold weather such as flu, and indirect effects such as fuel poverty.
Excess winter deaths
Excess winter deaths (EWDs) – the difference between average daily deaths in winter months (December to March) versus other months – occur throughout England. Large fluctuations in EWDs between years are common. Across the winter of 2017 to 2018, there was a large peak with just over 50,000 EWDs England and Wales, and in 2018 to 2019, there were an estimated 23,200 EWDs.
We may assume that hypothermia is the primary cause of cold-related death, however respiratory and circulatory (lung and heart) conditions, as well as dementia and Alzheimer’s are the leading causes of the observed EWDs. Whilst the greatest impact is among older age groups, EWDs occur across all ages.
EWDs also represent a significant health inequality, with people experiencing greater socioeconomic deprivation being more likely to be affected.
There are a number of complex and interlinked factors that contribute to EWDs, including:
-
seasonal factors such as weather and circulating infectious diseases (particularly flu and norovirus)
-
individual vulnerability to health effects of cold
-
attitudes to cold and associated behaviours
-
housing and economic factors including inadequate heating, poorly insulated homes, household income, cost of fuel and energy efficiency of the home

The graphic highlights factors contributing to excess winter deaths in England and Wales, such as seasonal factors like norovirus.
The Cold Weather Plan for England
The Cold Weather Plan for England (CWP) aims to prevent the major avoidable effects on health during periods of cold weather by raising both professional and public awareness. It’s an important part of emergency planning and longer term strategic planning and provides advice for professionals, organisations and individuals to enable them to plan for and respond to cold temperatures.
The CWP is underpinned by the Cold Weather Alert Service, which runs annually from 1 November to 31 March. It comprises 5 levels (Levels 0 to 4), from year-round planning for cold weather, through winter and severe cold weather action, to a major national emergency. Extraordinary alerts may be issued outside of alerting periods if trigger criteria are met. Each alert level triggers a series of actions within the NHS, local government and public health system, which are detailed in the CWP, as well as communication of risks to the public.
The core elements of the CWP
The CWP depends on having well-coordinated arrangements for dealing with cold weather in place before winter starts. The essential elements of effective cold weather planning include:
-
coordinated multi-agency long-term planning and commissioning for cold weather
-
a national alert system (advance warning and advice over the winter)
-
winter preparedness and action, including severe cold weather
-
raising awareness and engaging with the community to ensure they know what to do to prepare for and respond to cold weather
-
monitoring and evaluation – near real-time surveillance will be undertaken by PHE, and ongoing evaluation undertaken by PHE and other partners
Engaging the community is fundamental and may offer significant assistance in identifying and supporting particularly vulnerable or marginalised individuals, such as isolated older people and those with a serious illness or disability. For example, checking that they are able to keep their home warm, or that they have everything they need if a cold spell has been forecast.
This support can come from the voluntary and community sector, faith groups, families, emergency services that carry out Safe and Well home visits, and others.
Supporting resources
The CWP is complemented by National Institute for Health and Care Excellence (NICE) guidance on EWDs and illness and the health risks associated with cold homes.
Along with the CWP, the NICE guideline offers strategic and practical recommendations to reduce the risks to health from cold weather for:
-
the NHS, local authorities, social care and other public agencies
-
professionals working with people at risk
-
individuals, local communities and voluntary groups
The recommendations are in place to support vulnerable people who have health, housing or economic circumstances that increase their risk of harm. PHE’s Public Health Outcomes Framework (PHOF) help us understand how well public health is being improved and protected. There are 2 PHOF indicators that are directly linked to the CWP – EWDs and fuel poverty. However, many more framework indicators connected to the wider determinants of health, such as poverty, educational achievement and social isolation, can also be linked to long-term planning for cold weather and action to reduce the harm from cold.
The PHOF EWD indicator allows comparison between local authorities and examination of trends over time. It’s based on Office for National Statistics (ONS) estimates of EWDs published annually in November of each year, which is not timely enough to guide urgent public health action but is important for longer-term monitoring, commissioning and advocacy.
Cold weather-related risks and COVID-19
How COVID-19 can exacerbate cold weather-related risks
A number of important risk factors are shared across cold weather and COVID-19, which may amplify an individual’s risk to both hazards. The potential interactions between cold weather and COVID-19 include:
-
shared risk factors amongst population sub-groups affected by both cold temperatures and COVID-19
-
clinical impacts arising due to concurrence of cold weather and COVID-19
-
increased exposure to cold temperatures due to change in patterns of energy use at home, fuel poverty and reduced access to warm public spaces
-
reduced access to social and community networks and resources
-
change in patterns of health and social care use, access and delivery and health seeking behaviour
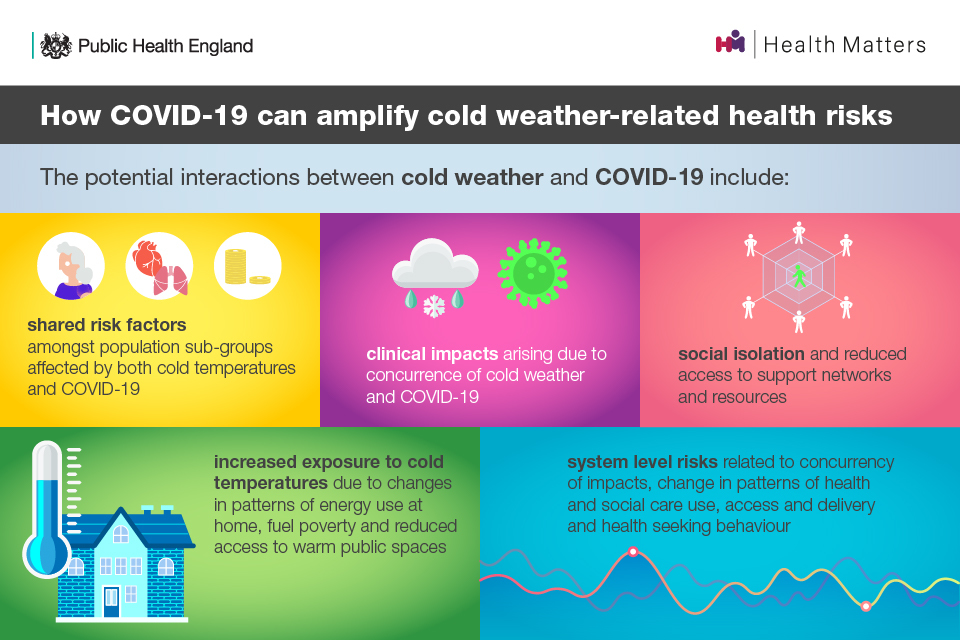
This graphic shows the effects of cold weather during COVID-19, such as clinical impacts, and social isolation.
Shared risk factors
Clinical risk factors that have been linked with severe illness from COVID-19 that are also risks for cold-related harms include:
-
older age, risks for both cold and COVID-19 increase with age
-
underlying health conditions, particularly chronic respiratory and cardiovascular disease
-
diabetes
-
pregnancy
Factors that impact on people’s ability to adapt to cold temperatures may also impact their ability to reduce exposure to COVID-19, for example through reduced ability to maintain good respiratory and hand hygiene. Other factors include:
-
severe mental illness
-
dementia and other causes of cognitive impairment
-
disabilities
-
being bed-bound
-
being very young
-
drug and alcohol dependencies
-
reduced access to strength and balance exercise and other physical activity that may help older people to stay warm and reduce risk of falls
Other groups with increased risk across the 2 hazards include people living in deprived circumstances, people experiencing homelessness or rough sleeping, and other marginalised or socially isolated individuals or groups.
Clinical impacts of COVID-19 and other winter risks
We still have much to learn about how COVID-19 infection affects the body, however it is possible that clinical outcomes may be more severe where exposure to cold and COVID-19 co-occurs for a given individual, for example through increased stress on the cardiovascular and respiratory systems. Longer-term complications of COVID-19 over the months prior to a significant cold weather event may also increase the number of people with vulnerability to low temperatures.
Winter is linked to a rise in respiratory infections, due to an increase in transmission and susceptibility to infection in cold weather. The impact of protective or harmful interactions between COVID-19 and other infections, including the common cold, rhinovirus and bacterial pathogens, is not yet know.
However, there is emerging evidence of poorer outcomes in those who are co-infected with COVID-19 and flu. PHE has recently published new research on the interactions between SARS-CoV-2 (the virus that causes COVID-19) and flu, and the impact of co-infection on disease severity. A total of 19,256 individuals were tested for both flu and COVID-19 between 20 January 2020 and 25 April 2020. In terms of mortality rates:
-
43.1% of those with co-infection died
-
26.9% of those who tested positive for only COVID-19 died
-
4.8% of those who tested positive for only flu died
This year, there may also be the challenge of overlapping symptoms and potential for mis-diagnosis or late diagnosis in community settings.
You can read more about flu and COVID-19 in the Health Matters edition on delivering the flu immunisation programme during the COVID-19 pandemic.
Older age
NHS England and Improvement data on factors associated with COVID-19 related death found that there was a strong association with age, with over 90% of the COVID-19 related deaths in the UK having been in people aged over 60.
After full adjustment for other factors that might increase someone’s risk of death from COVID-19, such as obesity and chronic respiratory disease, compared with people aged 50 to 59 years, people aged:
-
80 years and over were 20 times more likely to die from COVID-19
-
70 to 79 years were over 6 times more likely to die from COVID-19
-
60 to 69 years were almost 2.5 times more likely to die from COVID-19
It’s important to note the wide variation in risk of death between the 60 to 69 age group and the 80 and over age group.
In the same analysis, people aged under 50 years old were considerably less likely to die from COVID-19, with death rates among 18 to 39 year olds almost 16 times lower than in 50 to 59 year olds.
Older age is also recognised as a risk factor for more severe outcomes from COVID-19.
Older people, particularly those over 65 years, are at increased risk of harm from cold weather. This is partly because there is an increased likelihood of suffering from pre-existing chronic illness as we age which can be made worse by the cold, and partly because as we get older we experience a reduction in muscle and fat, which are important in retaining body heat.
Older people tend to spend a large proportion of their time at home. Whilst any household can be affected by fuel poverty, older people are at greater risk of harm if they are living in a cold home.
Living in low temperatures can also hamper mobility and increase the likelihood of falls and nonintentional injuries. This can be for number of reasons, including:
-
symptoms of arthritis worsen in cold, damp homes
-
strength and dexterity decrease as temperatures drop, increasing the risk of non-intentional injuries
-
snowy and icy conditions increase the risk of trips and falls outdoors
Snow and ice may cause significant disruption to the delivery of healthcare and other services, which will have an indirect impact on health and wellbeing.
Mental health
Poor mental health can impact on a person’s ability to undertake adaptive behaviours. People with existing mental health problems may be more vulnerable to harm from cold temperatures and winter weather. Social interactions are likely to reduce over the winter months, particularly this winter with COVID-19 restrictions in place. This may exacerbate feelings of loneliness and social isolation.
The occurrence of common mental health problems, such as depression and anxiety, is increased for those living in damp and cold housing. A questionnaire linking proxies for fuel poverty to common mental disorders (CMD) – including depression and anxiety – showed that 10% of those with CMD reported not being able to keep their home warm enough in winter, compared with just 3% without CMD. Of those with CMD, 15% said they had mould in their home, compared with 8% with no CMD.
Being unable to heat the home, in particular common living spaces, is associated with an increased risk of common mental health disorders, social isolation and increased stigma. Self-reported wellbeing has also been shown to be affected by living in low temperatures, with a number of studies demonstrating that improving indoor temperatures through heating and energy efficiency interventions are associated with improved self-reported wellbeing.
Housing and fuel poverty
With more than 90% of our time being spent indoors, the home environment is an important factor in both physical and mental health.
Fuel poverty is one of the major causes of cold homes. When the home is also damp with poor ventilation, mould is likely to occur, and cold, damp and mould all cause a range of health impacts. Fuel poverty is determined by the interaction of 3 main drivers:
-
energy efficiency of the household
-
energy prices
-
income
During the COVID-19 pandemic, increased numbers of people are spending more time at home than usual, which may lead to a higher demand for energy and an increase in associated costs of heating bills. This winter, new groups of people and households may also be drawn into fuel poverty for the first time and be unaware of the funds and resources available to help with keeping warm.
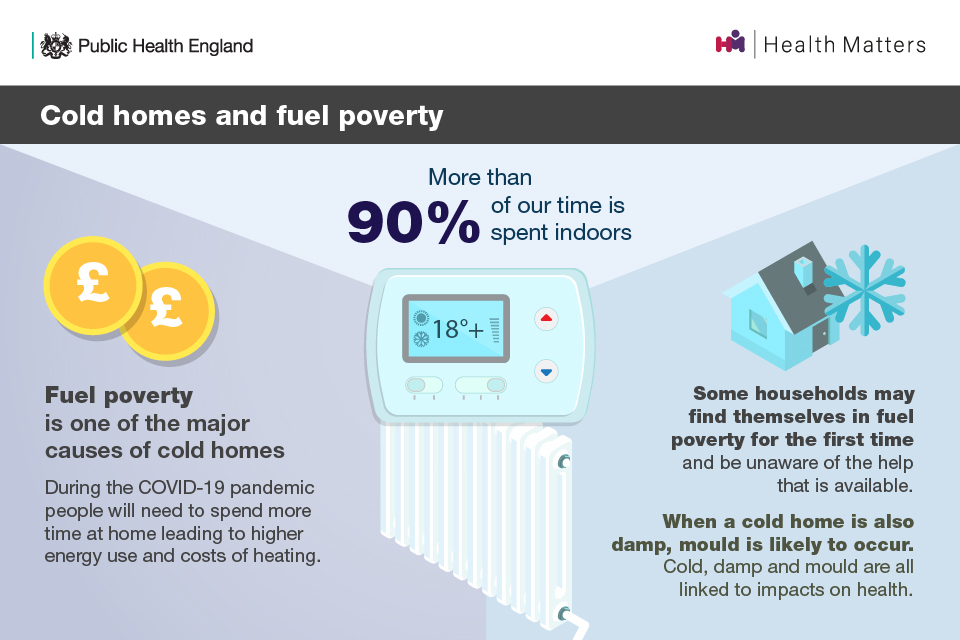
This infographic highlights the impact of cold weather and fuel poverty, and the likelihood that during COVID-19 people will be at home more often.
Another health harm related to cold weather and housing is transmission of viruses. People spend significantly more time indoors during the winter, and risk of transmission can increase due to housing factors such as:
-
overcrowding, including multiple occupancy and intergenerational households
-
poor ventilation, which increases the density of virus particles accumulating in a room
Barriers to ventilation include fuel poverty and living in an area with noise, pollution and security concerns.
Homelessness and rough sleeping
People experiencing homelessness, whether sleeping rough or in temporary accommodation, are at increased risk from cold weather. As well as being more exposed to cold weather, they are also more likely to have pre-existing health conditions and may be more likely to experience social isolation, cognitive impairment, living alone and/or experiencing fuel poverty.
This year, due to COVID-19 measures, there may be reduced access to shelters and other public warm spaces, which increases risk of exposure to cold for this vulnerable group. They may also be at increased risk of exposure to COVID-19 due to overcrowding and barriers to practising regular hand and respiratory hygiene, as well as facing a high burden of pre-existing problems such as smoking and chronic obstructive pulmonary disease (COPD).
The extent of interacting risks from cold and COVID-19 faced by this vulnerable group will be influenced by decisions about future arrangements, such as the safe provision of shelters, alternative accommodation and the activation of local Severe Weather Emergency Protocols (SWEP).
A Cold Weather Package was recently launched by the government to keep people experiencing rough sleeping safe during winter. In addition to further funding for local authorities and the faith and voluntary sector, the Ministry of Housing, Communities and Local Government (MHCLG) has published night shelter operating principles, with advice and input from PHE, and in consultation with Homeless Link, Housing Justice, councils and representatives from the shelter sector.
System level risks
Change in patterns of health service use and reorganisation of health and social care systems to address COVID-19 has impacted the ability of the NHS to deal with non-COVID-19 work.
Perceptions of risk from COVID-19 may also negatively impact attitudes to accessing healthcare during the pandemic. Polling found that 76% of UK people surveyed in May were anxious about the risk of exposure to COVID-19 and 47% were uncomfortable accessing a hospital. In July, confidence was returning and 77% felt comfortable to access a hospital.
The Health Foundation’s COVID-19 Survey found that among people from Black, Asian and Minority Ethnic (BAME) backgrounds surveyed, concerns were more likely to impact behaviours, with 9% having considered using a health service but decided not to, compared to 5% overall. In the same survey, 28% of people from BAME backgrounds and 34% of people with a disability said they would feel uncomfortable about using their local hospital, compared to 22% overall. Concerns about COVID-19 risks have also influenced older peoples’ decisions to access care. During the first wave, 14% of older people living with long-term conditions who needed community health and social care services did not try to access them.
There was a significant reduction in presentations to emergency care for both minor and urgent conditions between March to May. There is also evidence suggesting the pandemic resulted in an inflation in acute cardiovascular deaths, nearly half of which occurred in the community and most did not relate to COVID-19. This suggests there were delays to seeking help or that the deaths were likely the result of undiagnosed COVID-19.
Such changes in patterns of health seeking behaviour may impact on cold-related health harms such as heart attacks and strokes.
Preventing cold-related harm
Main recommendations for all
This winter, fear of COVID-19 should not prevent action to tackle the risks from cold temperatures and winter weather. It is critical that these preventative actions continue, including identifying and supporting vulnerable people at risk, with necessary adaptations in line with COVID-19 guidance to keep everyone safe.
In light of the guidance and good practice recommendations made in the CWP, and current COVID-19 risks, there are 3 main messages:
1. All local authorities, NHS commissioners and their partner organisations, including health and social care providers, should consider the CWP and make sure the suggested actions and Cold Weather Alert Service are understood across their locality and any additional need has been considered in local planning.
2. People at risk from cold weather may also be vulnerable to COVID-19 infection and vice versa. This can be due to concurrence of both clinical and environmental or socioeconomic factors. Identify those at greatest risk this winter, taking into account intersecting risks. Ask about living in a cold home and support vulnerable individuals to access existing resources to keep warm.
3. Cold weather actions and decision should also take into account risks from COVID-19 and related policies, such as shielding and self-isolation advice.
The following short film discusses key issues related to cold weather and COVID-19. It includes contributions from colleagues within PHE, the NHS and Age UK and covers EWDs, housing, older people, key messages from the Cold Weather Plan and more.
The CWP sets out guidance and good practice recommendations (see Figures 3.1 to 3.7) for:
-
commissioners of health and social care (all settings) and local authorities
-
provider organisations – health and social care (community services, hospitals, care homes, prisons)
-
frontline staff – health and social care, voluntary and community sector (including care homes)
-
GPs and practice staff
-
voluntary and community sector
-
national level: NHS England and Improvement, PHE, DHSC, Met Office, other government departments
-
individuals
These should continue to be followed with some additional considerations to mitigate concurrent COVID-19 risks.
Several important calls to action are summarised here. You can see additional recommendations in the CWP, NICE guidelines NG6 and Cold Weather and COVID-19 slide-set.
Health and social care commissioners and local authority Directors of Public Health
In addition to the actions set out in the CWP (page 36), health and social care commissioners and local authority Directors of Public Health should:
-
ensure there is a single point of contact to provide tailored advice for people living in cold homes to help them access advice and support
-
ensure that professionals from all disciplines and backgrounds making home visits are adequately trained to identify individuals most at risk, and know what actions to take to support them (an e-learning module is available to support this)
-
use existing structures across the local area, such as primary care networks, and work with relevant community and voluntary sector organisations to identify those most at risk, paying particular attention to those who may be socially isolated
-
consider potential measures which could be implemented to reduce the cold-related risks faced by individuals who are clinically vulnerable, clinically extremely vulnerable or self-isolating at risk of a cold home
-
ensure establishments such as hospitals, care homes and schools are aware of and have access to the cold weather guidance
-
Local Health Resilience Partnerships may want to make sure that there is adequate review of plans for surge capacity across health and care systems in light of COVID-19
-
ensure adequate provision to scale up programmes such as those offering emergency shelter to people experiencing homelessness if needed
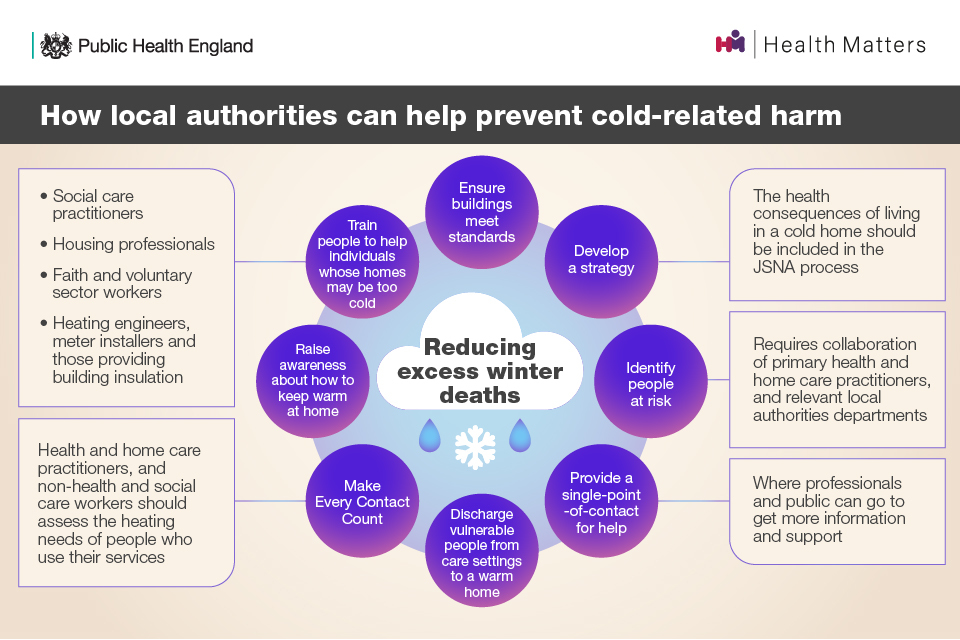
An infographic showing the actions Local Authorities can take to prevent harm from cold weather, such as raising awareness about how to heat your home
Providers – health and social care staff in all settings
In addition to the actions set out in the CWP (page 37 to 39), health and social care staff in all settings, including primary and community care, hospitals and care homes, should:
-
review who may be at high risk – identify those at greatest risk this winter, taking into account intersecting risks, and ask about living in a cold home
-
provide care and support during winter, which is particularly important in the context of additional risks and vulnerabilities related to COVID-19 and cold weather
-
review usual plans for surge capacity in cold weather in light of possible additional need and COVID-19-related staff absence
-
ensure a minimum temperature of 18C is kept and patients are comfortably warm whilst following COVID-19 guidance on ventilation
-
ensure safe discharge – for example, not discharging patients to cold homes
-
ensure regular post-discharge support and use of multi-disciplinary approaches such as hospital-at-home and reablement services
-
encourage physical activity for older people in the form of strength and balance exercise where possible
In terms of staff, providers should:
-
encourage them to sign up to cold weather alerts
-
communicate alerts to them
-
ensure they know what to do when the weather gets cold
-
encourage them to get their flu vaccinations
The NICE guidelines also provide specific recommendations for the NHS, including Health and Wellbeing Boards, Clinical Commissioning Groups, primary and secondary healthcare practitioners.
Community and voluntary sector and individuals
In addition to the actions set out in the CWP (page 40), community and voluntary sector and individuals should:
-
have plans in place to be able to check on others safely in advance of the cold weather
-
develop clear messaging to the public to encourage them to begin preparing for winter – for example, checking eligibility for assistance with heating costs, checking heating appliances and checking on vulnerable neighbours and relatives (information on eligibility, benefits and support is available.)
-
encourage those who may find it more difficult to cope in cold weather to request help, for example through volunteer networks or local cold homes services
-
advise those at risk that plans are in place to deliver services safely despite COVID-19, and so they should continue to seek medical help if they are feeling unwell
National level – PHE, NHS England and Improvement, DHSC and Met Office
In addition to the actions set out in the CWP (page 41), there are some actions that national level organisations can take.
NHS England and Improvement should:
-
consider the impact of cold weather on workforce capacity and wellbeing ahead of cold weather
-
ensure that alerts are cascaded widely and promptly, including to patient-facing and clinical staff
PHE Regions should:
-
be aware of the CWP and allied resources, including COVID-19 specific resources
-
provide support to Directors of Public Health and other local stakeholders as appropriate
PHE surveillance systems should:
- monitor and assess the impacts of cold weather
PHE Extreme Events and Health Protection team should:
-
provide early warning of potential health impacts of weather
-
evidence informed advice and guidance to support preparation, response and recovery to a cold weather event
PHE and the Met Office should:
- be hypervigilant within the cold weather alerting system to ensure the earliest possible issuing of cold weather alerts and the maximum possible warning time
