Shiga toxin-producing Escherichia coli (STEC) data: 2020
Updated 30 July 2025
Main points
A total of 402 confirmed cases of Shiga toxin-producing Escherichia coli (STEC) O157 were reported in England and Wales in 2020.
The lowest incidence of STEC O157 was in the London region (0.29 per 100,000 population) and the highest in the South West region (1.04 per 100,000 population).
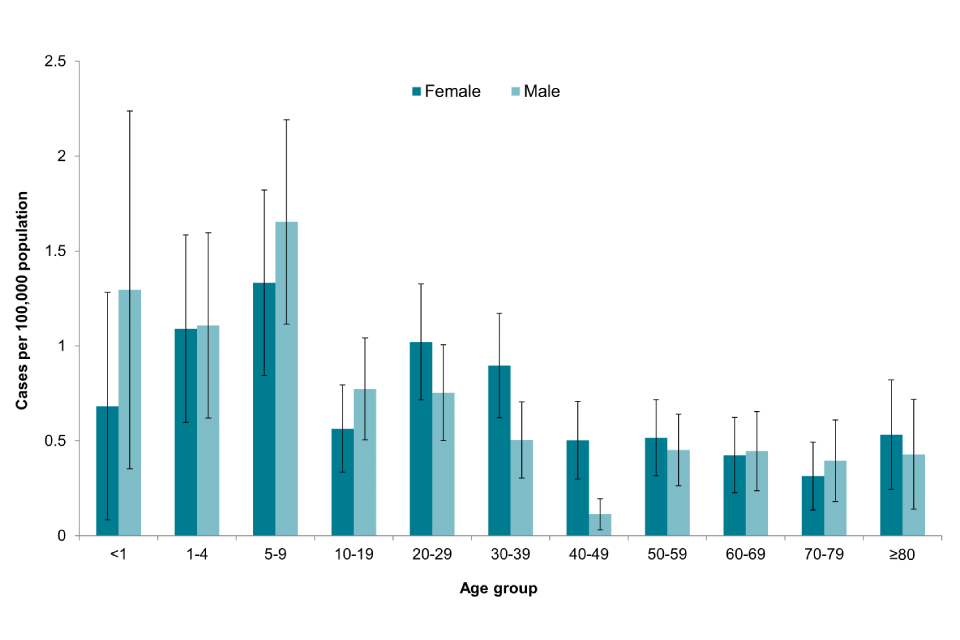
Children aged 5 to 9 years had the highest incidence of STEC O157 infection (1.50 per 100,000 population, 95% confidence interval (CI) 1.12 to 1.96).
One-third of confirmed STEC O157 cases in England were hospitalised and 3% were reported to have developed Haemolytic Uraemic Syndrome (HUS).
A further 286 specimens in England and 41 in Wales were positive for Shiga toxins (Stx) genes on polymerase chain reaction (PCR) at the Gastrointestinal Bacteria Reference Unit (GBRU) but an organism was not cultured.
The most commonly isolated non-O157 STEC serogroup was STEC O26 (England: n=103 out of 553, 19%; and Wales: n=26 out of 268, 15%).
Three outbreaks of STEC involving 63 cases in England were investigated in 2020.
Background
STEC, also known as Vero cytotoxin-producing Escherichia coli (VTEC), are bacteria that can cause gastroenteritis. Symptoms vary from mild to bloody diarrhoea and, in severe cases, can cause HUS, a serious and life-threatening condition predominantly affecting the kidneys. A small proportion of patients, mainly children, develop HUS (1).
The main reservoir for STEC is cattle although it is also carried by other ruminants such as sheep, goats and deer. Transmission can occur through direct or indirect contact with animals or their environments, consumption of contaminated food or water, and person to person spread.
STEC infections can present as sporadic cases or as outbreaks. Large national and multinational outbreaks have been associated with foodborne transmission (2 to 4).
The most common serogroup of STEC causing illness in England is O157 (5). Other serogroups (termed non-O157) can also cause illness and have been implicated in outbreaks in England, and elsewhere.
Frontline laboratories in England use culture methods to detect STEC O157 by its inability to ferment sorbitol on selective media (MacConkey agar). However, non-O157 STEC ferment sorbitol and there is no culture method to differentiate non-O157 STEC from non-pathogenic E.coli in frontline laboratories. Therefore, detection of non-O157 STEC relies on PCR.
The implementation and roll-out of a gastrointestinal (GI) PCR at frontline hospital laboratories began in December 2013, and by December 2019 around 20% of frontline laboratories had adopted this approach, although all frontline hospital laboratories in Wales now use PCR. As a consequence, there has been a substantial increase in the detection of non-O157 STEC cases. However, PCR is not universally used for detection of non-O157 STEC, and the true incidence in England remains unknown.
While non-O157 STEC can cause serious illness, variation exists among non-O157 STEC serogroups in their associations with severe disease, likely explained by differences in the virulence factors produced by different strains. STEC can produce 2 Shiga toxins, Stx1 (of which there are 4 subtypes, 1a to 1d) and/or Stx2 (of which there are 7 subtypes, Stx2a to 2g).
Stx2, specifically subtype Stx2a, is more likely to cause HUS in cases infected with STEC (1, 6). The increasing numbers of non-O157 STEC has led to the need to prioritise the public health actions due to insufficient resources to follow up all cases. Risk assessment, based on clinical symptoms and risk group of the patient and potential pathogenicity of the strain of STEC infecting the patient, is challenging. In response, the Public Health Operational Guidance for Shiga toxin producing Escherichia coli for the public health management of O157 and non-O157 STEC cases (including an algorithm to assist in follow-up decision-making) was updated and published in January 2023.
National enhanced surveillance of STEC in England and Wales has been undertaken since 2009. This report summarises the epidemiological data on confirmed cases of STEC O157 and non-O157 STEC cases in England in 2020 and compares it to previous years.
COVID-19 pandemic
During 2020 it is likely that the emergence of SARS-CoV-2 (COVID-19) and subsequent non-pharmaceutical interventions (NPIs) implemented to control COVID-19 transmission affected notifications of STEC infections to national surveillance in a number of ways. These include, but are not limited to, changes which may have impacted ascertainment (for example healthcare seeking behaviour, access to health care, availability or capacity of testing and so on) as well as changes which likely impacted incidence (for example closures of educational settings, limited foreign travel, closure of hospitality and attractions such as petting farms and so on) which will have also varied over time.
Therefore, trends presented in this report should be interpreted with caution. Additional in-depth analyses examining the impact of the COVID-19 pandemic are underway which will be published separately.
Methods
The National Enhanced Surveillance System for STEC (NESSS) infection in England began in January 2009 in order to supplement our understanding of the epidemiology of STEC infection. The system collects a standard data set of clinical, epidemiological and microbiological data for all STEC cases, in order to improve outbreak recognition and facilitate public health investigations. The data is collected from enhanced surveillance questionnaires (ESQs) and reconciled with laboratory reports associated with cases.
STEC is notifiable under the Public Health (Control of Diseases) Act 1984 and the Health Protection (Notification) Regulations 2010. In England, local diagnostic laboratories report presumptive cases of STEC to UKHSA Health Protection Teams (HPTs) and then refer samples to the GBRU for confirmation and further testing.
Depending on the virulence profile of the STEC strain and the outlined healthcare management process under the Operational Guidance algorithm, each HPT arranges for ESQ to be completed to obtain a detailed history of exposures 7 days prior to onset of illness.
The ESQ collects:
- demographic details
- risk status
- clinical conditions
- exposures including travel, food and water consumption
- environmental exposures
- outbreak status
Completed ESQs are submitted to the national Gastrointestinal Infections team at UKHSA to be included in NESSS.
For cases resident in England, data included in this report were validated and extracted from NESSS and cases meeting the case definitions below were included in analyses.
Welsh STEC cases are defined as a resident of Wales for whom a sample was referred to the GBRU. Laboratory data for cases in Wales was extracted and validated from the UKHSA Gastro Data Warehouse (GDW). Welsh data is included in Figure 1 as only laboratory data was available and is excluded from other sections of the report other than the outbreak section.
Data from the 2020 Office for National Statistics (ONS) mid-year population estimates was used to provide denominators for the calculation of incidence rates. All dates for the figures are based on the receipt date of a sample specimen at the GBRU.
Both microbiological and epidemiological case definitions are described in Tables 1 and 2 below.
Table 1: Microbiological case definitions
| Classification | Definition |
|---|---|
| Confirmed | Positive STEC culture or PCR positive for stx genes confirmed by GBRU |
| Probable | Suspect case with serum antibodies to lipopolysaccharide of E. coli O157 or other STEC, detected at the GBRU (up until March 2020 after which this method was discontinued) |
Table 2: Epidemiological case definitions
| Classification | Definition |
|---|---|
| Primary | A symptomatic case with no history of close contact with a confirmed case in the 7 days prior to onset of illness |
| Secondary | Case with a date of onset more than 4 days after the primary case or where transmission is believed to be through exposure to a primary case |
| Unsure | It is not possible to determine whether the case is primary or secondary with the information available. This may be because the patient was lost to follow-up, is asymptomatic or in an outbreak where it is not possible to identify the primary cases |
| Travel-associated | Case who has reported any travel outside of the UK in the 7 days prior to their date of onset of illness |
| Asymptomatic | A person from whom STEC was identified through contact screening procedures but who is asymptomatic |
Data
Cases of STEC in England and Wales in 2020
In 2020, 1,419 confirmed cases of STEC were reported in England and Wales; these comprised 402 culture-confirmed cases of STEC serogroup O157 (365 cases in England and 37 in Wales) and 690 cases (557 in England; 133 in Wales) where a serogroup other than O157 was isolated (non-O157). For a further 329 cases, samples were confirmed as STEC by testing positive by PCR for stx genes, but STEC was not cultured (288 in England; 41 in Wales).
Seven confirmed cases were infected with multiple serogroups:
- O145 and O157
- O26 and O157
- O125ac and O145
- O145 and O146
- O26 and O168
- O91 and O146
- O87 and O113
Between January and March 2020, there were 2 probable cases with serological evidence of STEC infection, with antibodies detected to O157 lipopolysaccharides in both cases (England: 2; Wales:0). After March 2020 this method was discontinued.
The crude incidence rate of confirmed STEC O157 in England and Wales was 0.68 per 100,000 cases (95% CI 0.61 to 0.75), continuing the downward trend observed since 2015 (Figure 1). It is the lowest rate reported annually since 1996, when testing began in England for STEC O157 on all faecal specimens from patients with suspected gastrointestinal infection (7). However, it is likely that the COVID-19 pandemic contributed to the drop in 2020 so this trend should be interpreted with caution.
Figure 1: Incidence of STEC O157 culture-confirmed cases by year, England and Wales, 2006 to 2020

Cases of STEC in 2020 in England
Figure 2: Incidence of STEC O157 in England by region, 2020 only
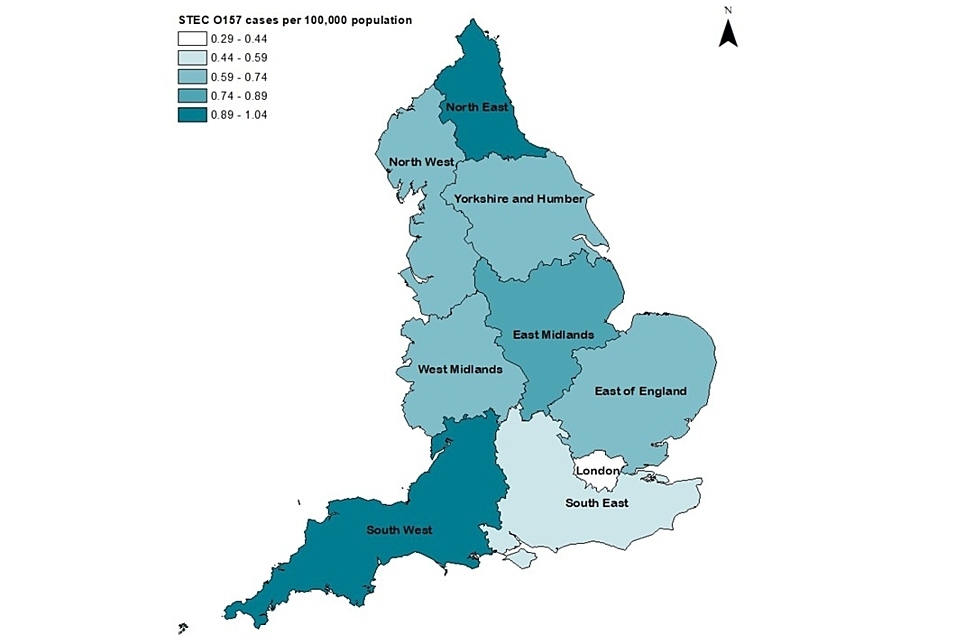
Coordinate System: British National Grid
Projection: Transverse Mercator
Contains Ordinance Survey data © copyright and database right 2019
Contains National Statistics data © copyright and database right 2019
The highest incidence of STEC O157 was in South West (1.04 cases per 100,000 population, 95% CI 0.79 to 1.34) and the lowest was in the London (0.29 cases per 100,000 population, 95% CI 0.19 to 0.42) (Figure 2).
Age, gender and seasonality of STEC O157 cases
Of 365 confirmed STEC O157 cases in England, 195 (53%) were female. In 2020, children aged 5 to 9 years had the highest incidence of infection (1.50 per 100,000 population, CI 1.21 to 1.96), unlike in previous years where the highest incidence was in children aged 1 to 4 years.
In all age groups aged under 19 years, males had the highest incidence in 2020; females had a higher incidence in all age groups aged over 20 years except those groups aged 60 to 69 years, and aged 70 to 79 years (Figure 3). This differs to previous years where incidence was generally higher for females in the 3 age groups of those aged 9 years and under.
Figure 3: Age-specific incidence rate of STEC O157 cases in England, 2020 only
As per previous years, STEC O157 infections displayed a distinct seasonality with the peak of infection in the summer months, usually July or August. However, in 2020 infections peaked later, with the highest number of cases reported in September and following low levels of reporting which coincided with the emergence of COVID-19 and the implementation of control measures from March 2020 onwards (Figure 4).
Figure 4: Seasonal trend of laboratory confirmed cases of STEC O157 in England, 2015 to 2020

Severity of illness
Of the 365 confirmed STEC O157 cases in England in 2020, ESQs were received for 359 (87%). Of those, symptoms were reported for 347 (97%) cases; the majority of which reported diarrhoea (93%, n=333) as well as bloody stools (64%, n=230).
Other symptoms included abdominal pain (291, 81%), nausea (172, 48%), vomiting (173, 48%), and fever (187, 52%). Hospitalisation occurred in 34% (n=121) of cases; duration of hospitalisation ranged from 1 to 14 days with median stay of 3 days.
During 2020, HUS occurred in 10 confirmed (3%) and neither of the 2 probable STEC O157 cases. One fifth of HUS cases were under 5 years of age (n=2, 20%) with a median age of 13 (range 1 to 93 years old). The incidence of STEC O157 HUS in children under 5 in 2020 was 0.06 per 100,000 cases per population (CI 0.01 to 0.22). Two deaths were reported among confirmed STEC O157 cases.
Transmission routes
In England, of the 359 confirmed cases for whom ESQs were received during 2020, there were 335 primary or co-primary cases, 12 secondary cases, and 11 asymptomatic contacts. A notable drop in travel related cases was observed with only 30 cases (8%) reporting travel abroad during their incubation period (7 days prior to onset), compared to 28% and 31% in 2018 and 2019 respectively. Of those 30, 5 spent their entire incubation period abroad. The most frequently reported travel destinations included Turkey, Spain, and Malta.
Frequently reported subtypes of STEC O157
As with previous years, phage type (PT) 8 and 21 out of 28 were the most commonly reported STEC O157 phage types in 2020 (Figure 5), with a combined proportion of 64%. These were followed by PT 54 (8%), PT 32 (6%) and PT 14 (5%). The peak in PT34 in 2016 was due to a large outbreak linked to mixed-salad leaves, where 165 cases were reported between 31 May and 29 July 2016 (4).
Figure 5: Number of STEC O157 cases by the 10 of the most common phage types, 2013 to 2020

Among 365 isolates from confirmed STEC O157 cases in England in 2020, most (n=182, 50%) had Stx1+2, 48% (n=176) had Stx2 only, and 2% (n=7) had Stx1 only. Of those isolates with Stx2 or Stx1+2, 41% (n=151) had stx2a; the subtype most likely to cause HUS. Of the 365 isolates, 364 had the eae gene.
Non-O157 STEC cases in England and Wales
Historically, cases of non-O157 STEC have been under ascertained, with 89 cases of STEC non-O157 reported between 2009 and 2013, prior to PCR being implemented.
Following the increase in recent years in frontline laboratories using PCR, there has been a significant increase in the detection of non-O157 STEC in England. It is not possible to estimate a denominator for incidence calculations for non-O157 STEC because details of contract arrangements for referral of samples from primary care and catchment areas of each diagnostic laboratory using PCR are not known.
In 2020, of 4,095 human faecal samples received at GBRU (excluding non-human samples and quality assessment samples) for STEC testing, 843 non-O157 STEC cases were confirmed in England. Of the 837 non-O157 cases, 557 culture positive cases of 95 different serogroups were confirmed. For 13 isolates, a serotype could not be identified as the genes encoding the somatic O antigen did not match any known sequence in the database. Specimens for a further 289 cases in England were positive for stx genes on PCR at GBRU but an organism was not cultured (PCR positive-culture negative).
In Wales, 132 non-O157 cases of 53 different serotypes were confirmed and a further 41 were PCR positive-culture negative. The most common non-O157 serogroups isolated in 2020 were O26 (n=27, 20%), O146 (n=14, 11%), O91 (n=14, 11%), O128ab (n=10, 8%) and O145 (n=9, 7%).
Non-O157 STEC cases in England
In England, the 5 most common non-O157 serogroups isolated from the 557 non-O157 cases in 2020 were O26 (n=103, 18%) followed by O146 (n=80, 14%), O91 (n=51, 9%), O128ab (n=37, 7%) and O145 (n=24, 4%) (Table 3). All except O145 were in the top 4 non-O157 serogroups were also most frequently detected in 2019 (see the 2019 report).
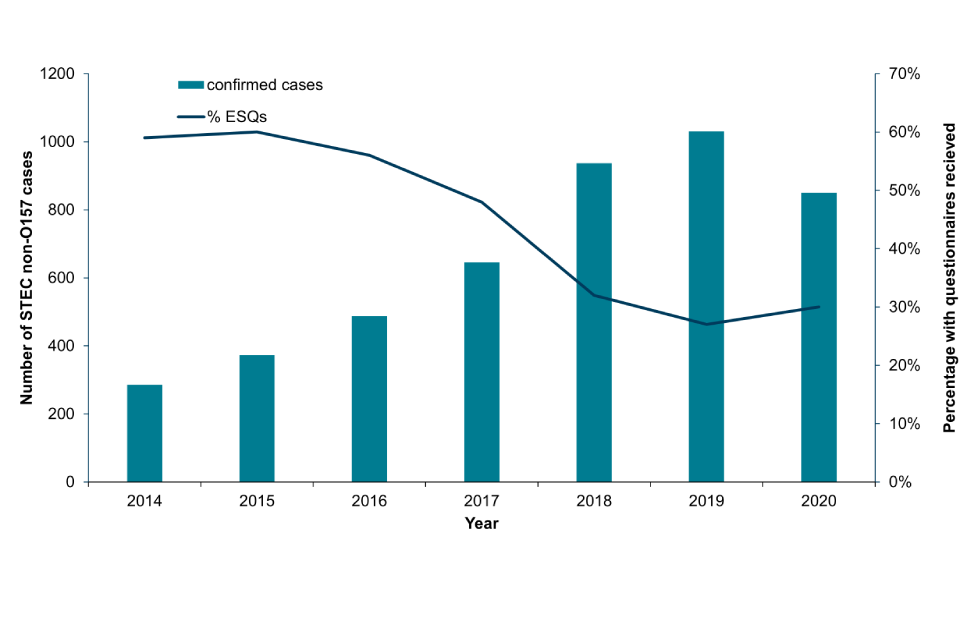
In 2020, ESQs were received for 30% (n=253 out of 843) of STEC non-O157 cases, of which 85% (n=215 out of 253) were for culture positive non-O157 STEC cases, and 15% of STEC cases confirmed only by PCR.
Since 2017, there has been decline in the number of ESQs received for STEC non-O157 cases, with a 35% reduction in the number of ESQs received from 2017 to 2020 (46% in 2017, 33% in 2018, 27% in 2019 and 30% in 2020), which may be associated with increasing numbers necessitating prioritisation and the implementation of algorithms in the 2018 guidance, which was subsequently updated in 2023.
Of the 253 ESQs received for confirmed cases, 243 (96%) were symptomatic. Among the symptomatic cases, 84% (n=205) reported diarrhoea, including bloody stools in 43% (n=104) cases. This was accompanied by abdominal pain (n=178, 73%), nausea (n=85, 35%), vomiting (n=73, 30%), and fever (n=63, 26%). In total 85 cases (35%) were hospitalised.
Figure 6: The number of confirmed STEC non-O157 cases and enhanced surveillance questionnaires received in England, 2020
HUS occurred in 28 confirmed STEC non-O157 cases. From the 28 cases of STEC non-O157 HUS, the most frequently isolated serogroups where O26 (36%, n=10) and O145 (14%, n=4). Stx genes were detected in faecal samples for 5 cases, but no organism was isolated.
Ten percent of confirmed STEC O26 cases developed HUS as compared to 3% in confirmed STEC O157 cases. HUS cases ranged from 10 months to 6 years of age and 70% (n=10) were between 1 and 4 years of age. There were 3 deaths reported among cases of non-O157 STEC.
ESQs were received for 73% (n=75) of all 103 confirmed STEC O26 cases. Of the 68 (91%) cases that were symptomatic, 87% (n=59) cases had diarrhoea, 69% (n=47) reported abdominal pain, 56% (n=38) reported vomiting, 41% (n=28) reported bloody stools and 28% (n=19) reported nausea. Overall, in 2020 a higher proportion of STEC O26 cases (40%, n=27) reported hospitalisation compared to STEC O157 cases (34%, n=121).
Of 103 STEC O26 cases in England, 56 (54%) were female. Children aged 1 to 4 years of age comprised 34% (n=35) of cases.
Figure 7: Age-sex distribution of STEC O26 cases in England, 2020

Among all 557 isolates from confirmed cases of non-O157 STEC in England in 2020, 34% (n=283) possessed the Stx1 toxin alone, 34% (n=283) possessed Stx1 and Stx2 and 33% (n=277) possessed Stx2 toxin alone.
The most common stx subtypes detected through sequencing of the 557 isolates were stx1a only in 19% (n=107), stx1c only in 18% (n=99), stx1c stx2b in 15% (n=83), stx2a only in 15% (n=81), stx2b only in 11% (n=62), stx1a stx2b in 6% (n=35), stx1a stx2a in 5% (n=29), stx1c stx2d stx2b in 3% (n=14), stx2c only in 2% (n=9), stx2d only in 2% (n=9), stx2e only in 1% (n=5), stx2b stx2d in 1% (n=4), stx2a stx2e in 1% (n=3) and stx2g only in 1% (n=3) (Table 3).
An additional 10 stx subtype combinations were detected in the samples of 12 cases.
Table 3: Prevalence of Stx subtype combination reported amongst the top 9 non-O157 STEC serogroups in England, 2020
| Serogroup | Stx subtype | n | % |
|---|---|---|---|
| O26 | stx2a | 47 | 46 |
| stx1a | 34 | 33 | |
| stx1a stx2a | 21 | 21 | |
| O146 | stx1c | 37 | 41 |
| stx1c stx2b | 20 | 22 | |
| stx2b | 20 | 22 | |
| stx1c stx2d stx2b | 7 | 8 | |
| stx2b stx2d | 5 | 5 | |
| stx1a stx1c | 1 | 1 | |
| stx1a stx2b | 1 | 1 | |
| O91 | stx1a stx2b | 31 | 62 |
| stx2b | 11 | 22 | |
| stx1a | 6 | 12 | |
| stx2d | 1 | 2 | |
| stx1a stx2b stx2d | 1 | 2 | |
| O128ab | stx1c stx2b | 22 | 61 |
| stx2b | 9 | 25 | |
| stx1c | 4 | 11 | |
| stx1c stx2b | 1 | 3 | |
| O145 | stx2a | 22 | 88 |
| stx1a | 1 | 4 | |
| stx2c | 1 | 4 | |
| stx2f | 1 | 4 | |
| O117 | stx1a | 15 | 88 |
| stx1a stx2b | 1 | 6 | |
| stx1c | 1 | 6 | |
| O103 | stx1a | 12 | 92 |
| stx1a stx2a | 1 | 8 | |
| O113 | stx1c stx2b | 10 | 56 |
| stx1c stx2d stx2b | 3 | 17 | |
| stx2d | 2 | 11 | |
| stx2b | 2 | 11 | |
| stx2b stx2c stx2d | 1 | 6 | |
| O76 | stx1c | 10 | 91 |
| stx1c stx2b | 1 | 9 |
Outbreaks
STEC outbreaks investigated in England during 2020
Three STEC outbreaks affecting 63 people in England were investigated in 2020 (typically, an exceedance is investigated when 5 or more cases fall within the same 5 SNP single linkage cluster for clinically severe serotypes, or an outbreak may be declared if a number of cases are linked to a setting. However, an investigation may be undertaken after considering a number of factors, including the number of persons affected, temporal and geographic distribution, clinical severity, and the microbiological characteristics of the STEC strain).
All 3 outbreaks were caused by STEC serogroup O157, and thus 42% of confirmed STEC O157 cases were attributed to these 3 outbreaks (Table 4). It was only possible to determine the vehicle and/or source for 1 of the 3 outbreaks, despite epidemiological investigations for all.
Despite epidemiological investigations, it was not possible to determine the vehicle and/or source of infection for all outbreaks. There were no HUS cases associated with outbreaks in 2020, and no deaths.
Table 4: STEC O157 and non-O157 outbreaks in England, 2020
| Agent | Total number affected | Total laboratory confirmed | Hospitalised | Source | Region |
|---|---|---|---|---|---|
| STEC O157 PT8 Stx1a Stx2c | 15* | 15 | 4 | Foodborne (suspected) | National |
| STEC O157 PT8 Stx1a Stx2c | 27† | 27 | 9 | Foodborne, cucumbers | National |
| STEC O157 PT8 Stx1a Stx2c | 18 | 18 | 3 | Undetermined | South West |
*15 confirmed cases in England, 4 in Wales and 1 in Scotland
† 27 confirmed cases in England and 9 in Wales
‡ Non-O157 (O26) serotype
In August 2020, UKHSA investigated 3 STEC outbreaks. UKHSA with Public Health Scotland (PHS) and Public Health Wales (PHW) investigated an outbreak of STEC O157 stx1a stx2c eae positive. There were 20 confirmed cases, of which 15 were resident in England, 4 in Wales and one in Scotland. The median age was 42 years. Questionnaires were available for 18 cases. Overall, 95% of cases reported diarrhoea, (n=15), 8 cases reported blood in stools (50%), 5 were hospitalised (31%) but none developed HUS. No deaths were reported.
UKHSA and PHW investigated a second outbreak of STEC O157 stx1a stx2c eae positive, which identified the vehicle of infection as imported cucumbers consumed as part of a fast-food product (8). There were 36 confirmed cases of which 27 cases resided in England and 9 in Wales. Questionnaires were received for 33 (92%) cases, of which 13 (40%) reported hospitalisation for their symptoms, however there were no reports of HUS or deaths. Thirty-two (97%) cases reported diarrhoea, with 25 (76%) cases reported having bloody diarrhoea.
UKHSA investigated a third outbreak of STEC O157 Stx1a Stx2c eae positive. There were 18 confirmed cases of which questionnaires were received for all cases. All 18 cases reported diarrhoea with 67% reporting bloody diarrhoea (n=12) and 89% reporting abdominal pain (n=16). Three cases reported hospitalisation (17%) and there were no reports of HUS or deaths.
These outbreaks continued to highlight the importance of stx1a in causing severe disease and is supported by increasing evidence in the literature that the presence of stx1a is also a risk factor for severe symptoms (5).
Conclusions
The number of STEC O157 cases in England continued to drop in 2020 as well as the number of outbreak investigations undertaken. While the reason for this decline in recent years is unclear it is likely that the impact of the COVID-19 pandemic contributed the 25% drop in cases observed in 2020 compared to 2019. The reasons for this decreased incidence are considered multifactorial but the concurrent drop in reported foreign travel by STEC O157 cases from approximately 30% in previous years to only 8% in 2020 indicates limited travel abroad is likely a key factor.
This report presents changes in epidemiology of STEC O157 infections in 2020, with a later peak in reporting than in most previous years as well as a change in the age-sex distribution. In 2020 there was a divergence from historical trends, with an overall higher incidence in males and the highest incidence in children aged 5 to 10 years rather than 1 to 4 years. While the percentage of STEC O157 cases who developed HUS remained the same at 3%, the percentage of cases hospitalised for their illness increased from 29% in 2019 to 34% in 2020, suggesting better ascertainment of more clinically severe cases during 2020 and which is supported by studies on the impact of COVID-19 on GI pathogen surveillance (9).
All 3 outbreaks investigated in 2020 were STEC O157 PT8 Stx1a Stx2c, with 50% to 76% of cases in each outbreak reporting bloody diarrhoea and 17% to 40% reporting hospitalisation, these outbreaks highlight the association of Stx1a Stx 2c with severe disease, as well as the importance of STEC O157 infection as a public health concern.
The detection of non-O157 STEC infections decreased compared to 2019. Though lower, the number detected still reflects the more widespread use of PCR in frontline laboratories to detect a broader range of serogroups. The most common non-O157 serogroup detected in 2020 was STEC O26 and cases infected with this serogroup had a higher proportion (10%) of HUS than O157 cases (3%).
Overall trends during 2020 should be interpreted with caution due to the wide ranging impacts of the COVID-19 pandemic. It is likely that the interventions implemented to control COVID-19 led to a reduction STEC, both O157 and non-O157, transmission. However, given the decreasing trend in STEC O157 notifications during pre-COVID-19 years, the reduction in STEC cases in 2020 cannot wholly be attributed to these control measures alone.
UKHSA STEC publications in 2020
- Byrne L, Adams N, Jenkins C. Association between Shiga toxin-producing Escherichia coli O157:H7 Stx gene subtype and disease severity, England, 2009 to 2019, Emerging Infectious Diseases October 2020: volume 26, issue 10, pages 2,394 to 2,400. doi: 10.3201/eid2610.200319
- Byrne L, Kaindama L, Bentley M, Jenkins C, Aird H, Oliver I, Paranthaman K, Incident Management Team. Investigation into a national outbreak of STEC O157:H7 associated with frozen beef burgers, UK, 2017, Epidemiology and Infection 16 July 2020: 148:e215. doi: 10.1017/S0950268820001582.PMID: 32669142
- Sharp A, Smout E, Byrne L, Greenwood R, Abdoollah R, Hutchinson C, Jenkins C, Arunachalam N, Padfield S, Hughes G, Gent M. An outbreak of Shiga toxin-producing Escherichia coli O157:H7 linked to a mud-based obstacle course, England, August 2018, Zoonoses Public Health August 2020: volume 67, issue 5, pages 467 to 473. doi: 10.1111/zph.12744. Epub 2020 Jun 21.PMID: 32564515
- Jenkins C, Byrne L, Vishram B, Sawyer C, Balasegaram S, Ahyow L, Johnson S. Shiga toxin-producing Escherichia coli haemolytic uraemic syndrome (STEC-HUS): diagnosis, surveillance and public-health management in England, Journal of Medical Microbiology July 2020: volume 69, issue 7, pages 1,034 to 1,036. doi: 10.1099/jmm.0.001215
- Gentle A, Day MR, Hopkins KL, Godbole G, Jenkins C. Antimicrobial resistance in Shiga toxin-producing Escherichia coli other than serotype O157 : H7 in England, 2014 to 2016, Journal of Medical Microbiology March 2020: volume 69, issue 3, pages 379 to 386. doi: 10.1099/jmm.0.001146
- Yara DA, Greig DR, Gally DL, Dallman TJ, Jenkins C. Comparison of Shiga toxin-encoding bacteriophages in highly pathogenic strains of Shiga toxin-producing Escherichia coli O157:H7 in the UK, Microbial Genomics March 2020: volume 6, issue 3. doi: 10.1099/mgen.0.000334. Epub 2020 February 24
- Elson R, Davies TM, Jenkins C, Vivancos R, O’Brien SJ, Lake IR. Application of kernel smoothing to estimate the spatio-temporal variation in risk of STEC O157 in England, Spatial and Spatio-Temporal Epidemiology February 2020: volume 32:100305. doi: 10.1016/j.sste.2019.100305. Epub 2019 October 24
- Jenkins C, Perry NT, Godbole G, Gharbia S. Evaluation of chromogenic selective agar (CHROMagar STEC) for the direct detection of Shiga toxin-producing Escherichia coli from faecal specimens, Journal of Medical Microbiology 2020: volume 69, issue 3, pages 487 to 491. doi: 10.1099/jmm.0.001136
- Greig DR, Jenkins C, Dallman TJ. A Shiga toxin-encoding prophage recombination event confounds the phylogenetic relationship between two isolates of Escherichia coli O157:H7 from the same patient, Frontiers in Microbiology 23 October 2020: volume 11, 588769. doi: 10.3389/fmicb.2020.588769
- Greig DR, Mikhail AFW, Dallman TJ, Jenkins C. Analysis Shiga toxin-encoding bacteriophage in a rare strain of Shiga toxin-producing Escherichia coli O157:H7 stx2a/stx2c, Frontiers in Microbiology 21 October 2020: volume 11, 577658. doi: 10.3389/fmicb.2020.577658
Acknowledgements
We are grateful to:
- the microbiologists, local authorities and local health protection and environmental health specialists who contribute data and reports to NESSS
- the epidemiologists and information officers who have worked on NESSS
- staff in GBRU for providing the Reference Laboratory Services and laboratory surveillance functions and expertise
- UKHSA Regional and Collaborating Public Health Laboratories and Food Water and Environmental Microbiology Services for providing a surveillance function for GI pathogens and testing of food and environmental samples during outbreak investigations
References
1. Launders N and others. Disease severity of Shiga toxin-producing E. coli O157 and factors influencing the development of typical haemolytic uraemic syndrome: a retrospective cohort study, 2009 to 2012. British Medical Journal Open 2016: volume 6, issue 1, page e009933
2. Dodd CC and Cooper MJ. Multidisciplinary response to the Escherichia coli 0104 outbreak in Europe. Military Medicine 2012: volume 177, issue 11, pages 1,406 to 1,410
3. Launders N and others. Outbreak of Shiga toxin-producing E. coli O157 associated with consumption of watercress, United Kingdom, August to September 2013. Eurosurveillance 2013: volume 18, issue 44
4. Gobin M and others. National outbreak of Shiga toxin-producing Escherichia coli O157:H7 linked to mixed salad leaves, United Kingdom, 2016. Eurosurveillance 2018: volume 23, issue 18, page 17-00197
5. Byrne L, Adams N and Jenkins C. Association between Shiga Toxin-Producing Escherichia coli O157:H7 stx Gene Subtype and Disease Severity, England, 2009-2019. Emerging Infectious Diseases 2020: volume 26, issue 10, pages 2,394 to 2,400
6. Brandal LT and others. Shiga toxin-producing escherichia coli infections in Norway, 1992-2012: characterization of isolates and identification of risk factors for haemolytic uremic syndrome. BioMed Central Infectious Diseases 2015: volume 15, page 324
7. Adams NL and others. Shiga Toxin-Producing Escherichia coli O157, England and Wales, 1983-2012. Emerging Infectious Diseases 2016: volume 22, issue 4, pages 590 to 597
8. Mulchandani R and others. Outbreak of Shiga toxin-producing Escherichia coli O157 linked with consumption of a fast-food product containing imported cucumbers, UK, August 2020. International Journal of Infectious Diseases October 2021: volume 110 supplement 1:S62-S68. doi: 10.1016/j.ijid.2021.04.001
9. Love NK and others. ‘Impact of the COVID-19 pandemic on gastrointestinal infection trends in England, February to July 2020’ British Medical Journal Open 21 March 2022: volume 12, issue 3, page e050469. doi: 10.1136/bmjopen-2021-050469. PMID: 35314468; PMCID: PMC8968111
Preparation of this report
This report was prepared by the Gastrointestinal Infections and Food Safety (One Health) Division, UKHSA and Public Health Wales. For queries relating to this document, please contact: VTEC@ukhsa.gov.uk
