Diphtheria: cases among asylum seekers in England, health protection report (data to 25 November 2022)
Updated 9 January 2026
Applies to England
Main points
The main points are:
- increase in cases of toxigenic Corynebacterium diphtheriae reported among asylum seekers arriving into the UK
- from 1 January to 25 November 2022, toxigenic C. diphtheriae was isolated from 50 asylum seekers with recent arrival in England
- there have been 2 cases of severe respiratory diphtheria requiring hospitalisation and treatment with diphtheria anti-toxin and antibiotics
- there has been one fatality in an individual from whom the detection of DNA from Corynebacterium diphtheriae and the diphtheria toxin gene has been confirmed by polymerase chain reaction (PCR) test from a throat swab; cause of death awaited pending post mortem
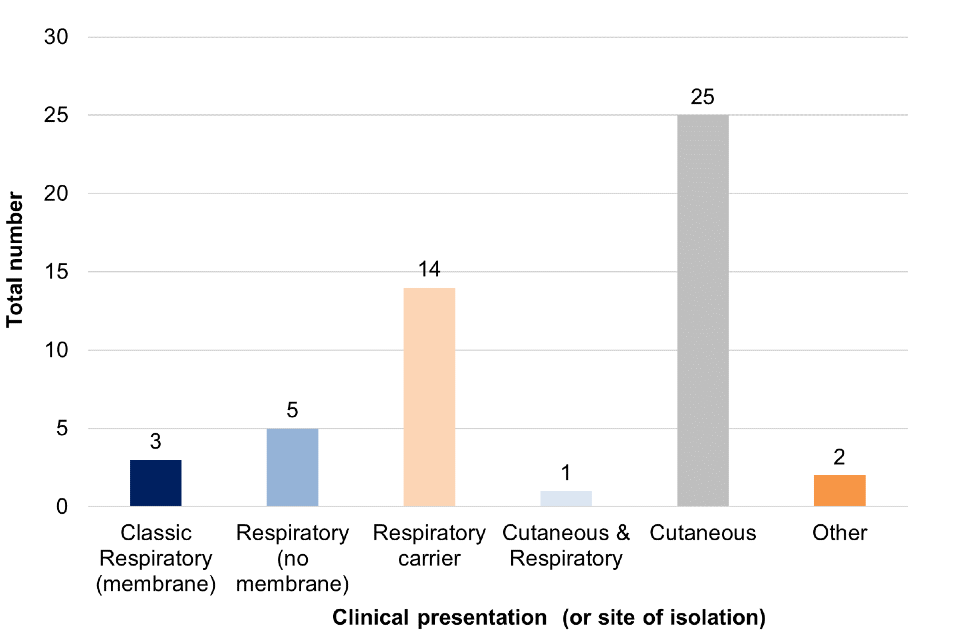
- there have been 25 cases with cutaneous diphtheria or colonisation of toxigenic C. diphtheriae in wounds
- there have been 5 cases of respiratory diphtheria and 14 cases with respiratory carriage with no (or unknown) respiratory symptoms
- there has been one case with both cutaneous and respiratory diphtheria, and 2 cases with other presentations
- whilst many cases originate from diphtheria endemic countries it is likely that they have acquired their infection either in their country of origin or on their extended journeys to the UK through Europe
- published resources available on GOV.UK (see further information)
Background
Diphtheria is a very rare infection in England due to the success of the routine immunisation programme that was introduced in 1942, a time when the average annual number of cases was about 60,000 per year, with 4,000 deaths (1).
Over the past decade, the number of diphtheria cases in England has increased from an average of 2 to 11 cases per year (with the exception of 2020). In 2021, there were 10 cases of diphtheria in the UK, 3 of of which were toxigenic Corynebacterim diphtheriae.
There are 3 Corynebacterium species that can potentially produce toxin:
- C. diphtheriae (associated with epidemic person-to-person spread via respiratory droplets and close contact)
- C. ulcerans and C. pseudotuberculosis (both less common globally and traditionally associated with farm animal contact and dairy products and more recently, for C. ulcerans, with companion animals) (2)
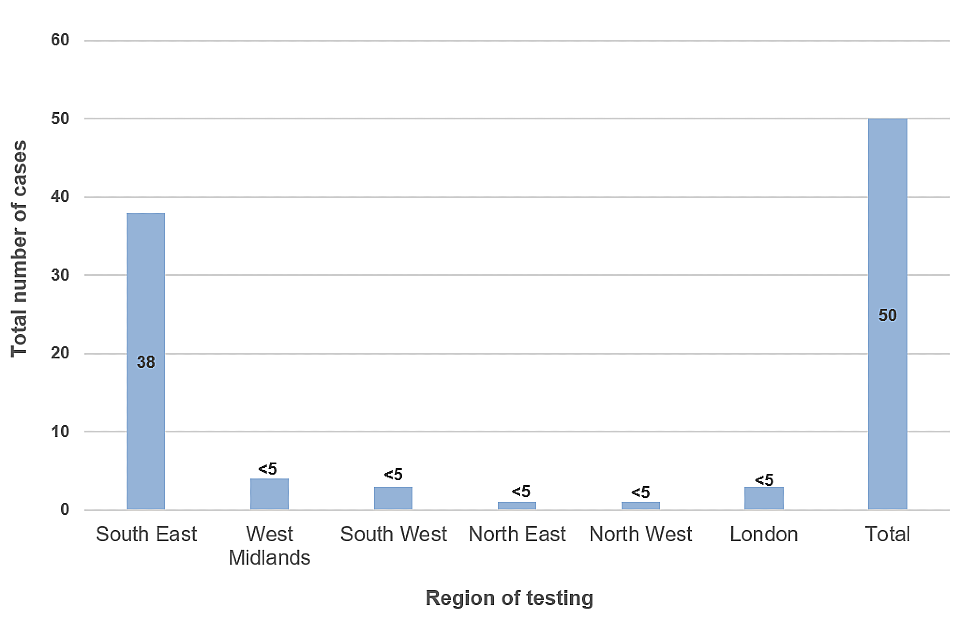
Since 1 June 2022, there has been an increase in cases of diphtheria due to toxigenic C. diphtheriae reported among asylum seekers in Europe (3). A similar increase in cases has been reported in the UK with the first confirmed case identified in February in the South East region and a further 49 confirmed cases reported as of 25 November 2022. These include 18 cases in October and 27 cases in November (see Figure 1). Cases have mostly been identified in the South East region of England shortly after arrival to the UK (see Figure 2).
Figure 1: Total number of toxigenic C. diphtheriae cases in asylum seekers by month of reporting, February to 25 November 2022
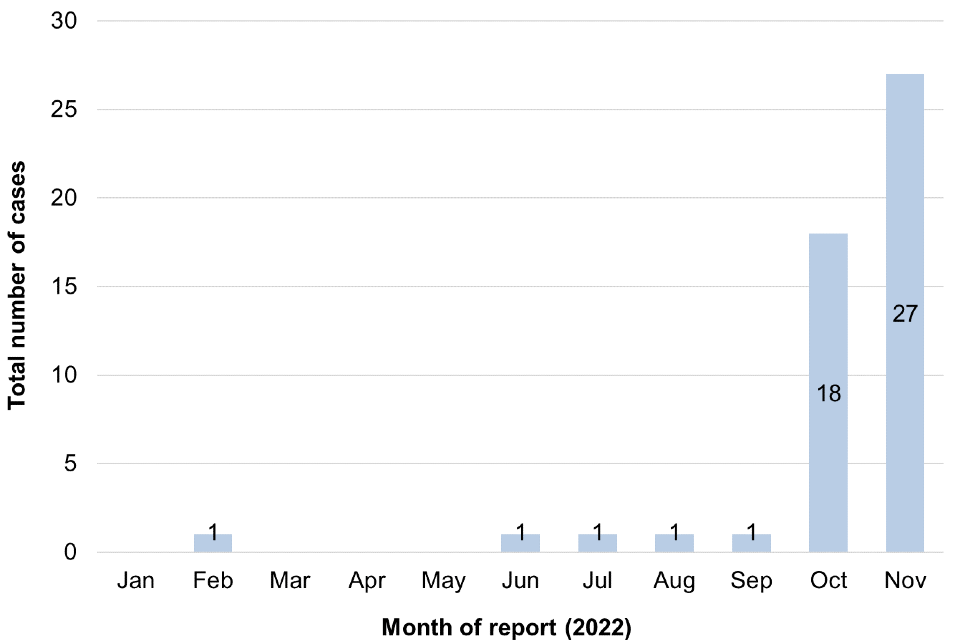
Figure 2: Total number of toxigenic C. diphtheriae cases in asylum seekers by region at point of testing, February to 25 November 2022
Diphtheria can present with a range of clinical presentations. Classical respiratory diphtheria is characterised by a swollen ‘bull neck’ and strongly adherent pseudomembrane which obstructs the airways. A milder respiratory form of the disease where patients present with sore throat or pharyngitis can occur in immunised or partially immunised individuals (2).
Cutaneous presentations, characterised by ‘rolled edge’ ulcers, are also common, particularly in tropical regions (4) and cutaneous lesions or wounds have been the most prominent presentation reported among migrant cases to date (5).
Treatment involves prompt administration of diphtheria anti-toxin (DAT) for severe cases and clearance with appropriate antibiotics.
Public health management of clinical cases of diphtheria in England is provided by local health protection teams, including identification, assessment and prophylaxis of close contacts (4).
Supplementary guidance (6) has been developed to support management of cases in asylum seeker accommodation settings in England as part of an Enhanced National Incident response.
In addition, mass antibiotic prophylaxis and vaccination have been recommended for those resident in, or previously resident in, initial reception centres where significant barriers to individual targeted case and contact management have been identified (such as challenges with contact tracing, testing and prophylaxis) (6).
Laboratory confirmation of diphtheria is usually made by isolation of toxigenic strains of C. diphtheriae, C. ulcerans or C. pseudotuberculosis from the patient. In England, all putative isolates of the 3 toxigenic species are submitted to UK Health Security Agency’s (UKHSA) Vaccine Preventable Bacteria section (VPBS), Respiratory and Vaccine Preventable Bacteria Reference Unit (RVPBRU), which is the National Reference Laboratory (NRL) for diphtheria.
Since 1 April 2014, a real-time PCR for confirmation of species identity and presence of the tox gene has been used as the front-line test for putative toxigenic corynebacteria to inform public health action. If the tox gene is detected, expression of diphtheria toxin is confirmed using the modified Elek test (7). Public health action is initiated on the basis of detection of the toxin gene by PCR testing.
Corynebacterium diphtheriae among asylum seekers in England, 2022
Toxigenic C. diphtheriae strains from 50 asylum seekers were identified between February and 25 November 2022. Cases were predominantly among young males aged 14 to 25 years old (with an age range of 2 to 41 years and median age of 16.5 years).
The majority of cases have presented with cutaneous skin lesions or wounds acquired during extensive travel en route to the UK thus prompting clinical assessment and screening for corynebacteria. There have been 25 cases of toxigenic C. diphtheriae isolated from wound swabs. Not all cases presenting with wounds have had subsequent isolation of C. diphtheriae, with other organisms (such as Group A Streptococcus and Staphylococcus aureus) also commonly isolated from these sites.
There have been 2 severe cases of respiratory diphtheria. Both cases had classical diphtheria, presenting with sore throat, membrane and fever, and requiring hospitalisation and treatment with DAT. Contact tracing from one of the cases identified a further 2 cases with toxigenic C. diphtheriae isolated from throat swabs.
There has been one fatality in an individual from whom the detection of DNA from C. diphtheriae and the diphtheria toxin gene has been confirmed by PCR from a throat swab. However, the cause of death is yet to be confirmed pending post mortem.
There have been 19 confirmed cases with toxigenic C. diphtheriae isolated from nose and/or throat samples. Of these cases, 5 have reported respiratory symptoms (including sore throat, cough and/or swollen glands) and 14 cases reported no (or unknown) associated respiratory symptoms. Of note, 10 cases with respiratory carriage reported skin lesions or wounds, but C. diphtheriae was not isolated from these sites.
There has been one case with both respiratory and cutaneous presentation and 2 cases with other presentations (toxigenic C. diphtheriae was isolated from a urethral swab and a penile skin swab, but with no lesions or significant wounds noted).
Figure 3: Clinical presentation of toxigenic C. diphtheriae cases in asylum seekers, England, February to 25 November 2022
Contact tracing efforts have been made to screen and prophylax close contacts of cases. In initial reception centres where there are challenges to individual case management and contact tracing. Mass antibiotic and vaccination of residents have been recommended and information resources in key languages made available to support implementation. The Home Office is working with the NHS and other partners to operationalise this.
Most cases have had onset of symptoms prior to arrival into the UK suggesting infection has occurred along the extended travel route through Europe or at country of origin.
Further information
Advice on immunisation against diphtheria, provision of vaccine and provision of DAT for therapeutic use is available from the UKHSA Colindale Immunisation and Vaccine Preventable Diseases Division and in the revised guidance for public health control and management of diphtheria (4) and Supplementary guidance for cases and outbreaks in asylum seeker accommodation settings (6).
Further resources are available online including:
- Diphtheria anti-toxin: clinical guidance (8)
- Diphtheria anti-toxin (DAT): information for healthcare professionals (9)
- Diphtheria: vaccination resources (10)
- Warn and Inform letter (including diphtheria factsheet translated into 13 key languages) (11)
- Diphtheria disease and azithromycin: PGD template (12)
- Diphtheria training slide set for healthcare professionals (13)
Microbiological laboratories are requested to promptly submit all suspect isolates of C. diphtheriae, C. ulcerans and C. pseudotuberculosis for confirmation and toxigencity testing to the NRL at UKHSA, RVPBRU, Colindale, London using the laboratory request form R3 (14).
The NRL also provides advice on all aspects of laboratory testing for diphtheria and related infections.
References
1. UKHSA. ‘Diphtheria: the green book, chapter 15: Public Health England; 2013’
2. Wagner KS, White JM, Crowcroft NS, De Martin S, Mann G, Efstratiou A. ‘Diphtheria in the United Kingdom, 1986 to 2008: the increasing role of Corynebacterium ulcerans’. Epidemiology and Infection 2010: volume 138, issue 11, pages 1,519 to 1,530
3. European Centre for Disease Prevention and Control. ‘Increase of reported diphtheria cases among migrants in Europe due to Corynebacterium diphtheriae, 2022’
4. UKHSA. ‘Public health control and management of diphtheria in England: 2022 guidelines: UK Health Security Agency’
5. European Centre for Disease Prevention and Control. ‘Weekly Communicable Disease Threats Report, 13 to 19 November 2022, week 46’
6. UKHSA (2022). ‘Supplementary guidance for cases and outbreaks in asylum seeker accommodation settings’
7. De Zoysa A, Efstratiou A, Mann G, Harrison TG, Fry NK. ‘Development, validation and implementation of a quadruplex real-time PCR assay for identification of potentially toxigenic corynebacteria’. Journal of Medical Microbiology 2016: volume 65, issue 12, pages 1,521 to 1,527
8. UKHSA. ‘Diphtheria anti-toxin: clinical guidance’
9. UKHSA. ‘Diphtheria anti-toxin (DAT): information for healthcare professionals’
10. UKHSA. ‘Diphtheria: vaccination resources’
11. UKHSA. ‘Warn and Inform letter (including diphtheria factsheet)’
12. UKHSA. ‘Diphtheria disease and azithromycin: PGD template’
13. UKHSA. ‘Diphtheria training slide set for healthcare professionals’
14. UKHSA. ‘R3: vaccine preventable bacteria section request form’
Prepared by
Shennae O’Boyle, Gayatri Amirthalingam, Rebecca Cordery, Norman Fry, David Litt, Josh D’Aeth and Emma O’Brien.
For queries relating to this document, please contact: immunisation.lead@ukhsa.gov.uk
