[Withdrawn] Assessors' guide: 2023 awards round
Updated 11 May 2023
Applies to England and Wales
About this guide
This guide is to inform scorers of national Clinical Impact Award (CIA) applications of the workings of the scheme and the scoring process. It covers the 2023 competition in England and Wales and tells you:
- how the award scheme works
- who is eligible to apply
- how the new application and assessment processes work
- how to score an individual application
Read this guide before you start scoring your allocated applications. New assessors may also find it useful to read the applicants’ and nominators’ guides.
If you’re based in Wales, you’ll find anything extra you need to know in the boxes throughout this guide.
All applications need to be submitted by 5pm on 5 May 2023. Any applications received after this will not be considered. Initial scoring will take place between May and June 2023, with a second round of scoring for N3 level awards taking place between July and September. Scoring for National Reserve (NRES) will occur thereafter between late September and early November 2023 – we will let you know the exact dates and the date of your regional subcommittee meeting in due course.
You should find everything you need to help you on the ACCIA homepage – if you have any questions that are not covered, contact us at accia@dhsc.gov.uk.
Part 1: introduction
About ACCIA and the Clinical Impact Awards scheme
ACCIA runs the national Clinical Impact Awards scheme for the Department of Health and Social Care (DHSC) in England.
The advisory committee also provides governance for the awards for the Welsh government.
Health ministers have agreed a limited number (up to 600) of new awards each year in England, so the selection process is very competitive. Three levels of award are available in England, from lowest to highest: National 1 (N1), National 2 (N2) and National 3 (N3).
In Wales a lower level (National 0) also exists.
The awards last for 5 years and have an annual, non-pensionable value of £10,000 (N0), £20,000 (N1), £30,000 (N2), £40,000 (N3).
A consultant can apply for a new award at any time after completing a full year in an eligible role. If a consultant already holds a national Clinical Excellence Award, transitional arrangements apply in England between the old and new schemes. To be considered, the applicant will need to show that what has been delivered has had an impact at a national level, and over and above the expectations defined in their job plan in developing and delivering a high quality service.
There will also be a need to demonstrate a commitment to, and nationally relevant impact on improving the NHS through:
- leadership
- education
- training
- people development
- innovation and research
There is also an opportunity to provide evidence of national impact in areas that are not captured in the first 4 domains, particularly if it relates to published NHS or other relevant health objectives. In all of the domains, applicants should provide evidence of national impact relating to equality, diversity and inclusion.
There is one online application form for all awards, so every applicant can highlight their contributions in the same way.
Based on the strength of applications and the ranking once scored, our regional sub-committees, N3 committee and our main committee will recommend applicants for national awards to health ministers for them to approve.
How national awards relate to local awards
The NCIA scheme aims to allow local and national awards to be held concurrently, but due to the costs of transitional pay protection arrangements this is not possible straightaway. In 2023, they will not be held at the same time – this will be reviewed on an ongoing basis. More information about local awards can be viewed on the NHS Employers website.
In Wales, employers give commitment awards. You can find more information about these in the amended National Consultant Contract in Wales 2003.
What the national scheme rewards
The national awards are granted by ministers to recognise and retain consultants or academic GPs who deliver national impact above the expectations of their job role or other paid work. Applicants need to give evidence of impact across the following 5 domains:
- Delivering and developing a high-quality service
- Leadership
- Education, training and people development
- Innovation and research
- Other areas of national impact, with specific reference to NHS priorities where relevant
These 5 domains are explained below in part 4 and part 5 of this guide.
We do not give awards for standalone overseas work.
Work in other countries is not directly relevant for an award, so is not considered on its own. Overseas work that has demonstrably helped the NHS and the health of the public directly or has had a direct reputational benefit for the NHS overseas may be supported if the evidence clearly describes this.
How we assess applications
We run the scheme fairly and openly offering every applicant an equal opportunity, and we consider all applications on merit. We include our analysis of each year’s competition in our annual report.
We assess all applications against the same criteria which you can find below in part 4 of this guide.
Our sub-committees are regional groups that assess applications for national awards for most applicants in their area. Based on application workload, and to provide balance and a degree of external scrutiny across these committees, we reallocate some sub-committee members to score in other regions (see part 4 for more information).
There are 13 regional ACCIA sub-committees in England:
- Cheshire and Mersey
- East of England
- East Midlands
- London North East
- London North West
- London South
- North East
- North West
- South
- South East
- South West
- West Midlands
- Yorkshire and Humber
There are separate sub-committees for:
- DHSC and arm’s length bodies (ALBs)
- assessing the highest-scoring regional applicants for N3 awards – N3 Committee
- rescoring applicants whose regional scores are tied at the lower cut-off ranking point for N1 and N2 award levels and any applicants where questions arise through governance review – NRES
Wales has its own sub-committees.
The sub-committees consider all applications in their area except for those from public health consultants and academic GPs contracted by the UK Health Security Agency and NHS England. These are assessed by the DHSC or arm’s length body (ALB) sub-committee where they can be benchmarked more easily. Each regional sub-committee is allocated an indicative number of awards at each level. This is based on the number of national awards available proportionately distributed based on the number of applications received that year in each region. This means there is an equal chance of achieving an NCIA in any region.
Sub-committee members come from a range of backgrounds with experience and expertise in many different areas. They assess and score applications independently based only on the information on the form. They must not assess any evidence from external urls or weblinks. All the individual scores for an application are averaged and then ranked against the other applications in that region. The top scoring applications in each region are provisionally allocated an NCIA. To ensure the highest-level awards are granted to those making the greatest national impact, a separate N3 sub-committee will rescore all those from each region falling within the N3 indicative allocation, plus the same number of applicants scoring highest in the N2 allocation. This rescoring provides a national benchmarking for determining who receives an N3 award.
Each sub-committee is typically made up of:
- medical and dental professionals – 50%
- non-medical professionals and lay members – 25%
- employers – 25%
Each sub-committee may be divided into scoring groups to manage the workload depending on the number of applications received. We ensure there is balanced diversity of scorers across these groups. These groups score a randomly selected group of applications to minimise any unconscious bias affecting the scoring. A normalisation process is used to ensure scores between any groups within a region are directly comparable. Scores across regions are not comparable.
Each group scores applications consistently against the guidance. There will be up to 600 new NCIAs available each year in England – subject to ministerial agreement and funding impacts during the transitional period. Our ambition is to award 330 N1, 200 N2 and 70 N3 awards each year.
When an application for an award is successful, the NCIA will last 5 years backdated to 1 April 2023. For NCEA holders under transitional arrangements, awards will last 5 years from 1 April 2024.
In Wales, the process for assessing applicants is different. For more details contact Chantelle Herbert at the Wales Secretariat at HSSWorkforceOD@gov.wales.
After regional sub-committee scoring has closed and the ranked list has been produced, our national chair and medical director review all the provisionally successful N1 and N2 applications that are not being considered for an N3 award. After their review, applications where questions arise or clarification may be helpful are discussed at the regional sub-committee meetings as part of our quality and governance review.
Applications that are tied at the cut-off point for N1 or between N1 and N2 awards are automatically referred for rescoring by NRES.
Applications where questions have not been resolved to the satisfaction of the national chair and medical director are also referred to NRES for rescoring. NRES is made up of the chairs and medical vice-chairs of the regional sub-committees and other experienced scorers from the regions. As a panel of our most experienced scorers, NRES acts as a quality assurance mechanism. Our chair and medical director recommend applications for awards to our main committee based on the sub-committee and NRES scores.
Following scrutiny from our main committee, English recommendations go to DHSC ministers.
Recommendations from the Wales sub-committee go to Welsh ministers for final approval, after scrutiny from the main committee.
If an award is approved, we will let the applicant and their employer know. Unsuccessful applicants will be informed at the same time.
Local awards and commitment awards
ACCIA does not have any say in local awards in England or commitment awards in Wales.
Running an open, transparent scheme
More information about ACCIA and the NCIA scheme can be found on the ACCIA home page, including:
- a list of all national award holders
- personal statements from people who have received a new award
- the members of our main committee and our sub-committees
- a guide for applicants – with a supporting ‘quick guide’
- a guide for assessors on how to assess and score applications
- annual reports about each awards round
- summaries of the minutes for the main committee’s meetings
Disability
In line with the Equality Act 2010, employers must consider making reasonable adjustments for employees with disabilities. These are changes to things such as equipment or processes to make sure people with disabilities can do their job.
If an applicant has a disability, where relevant, any reasonable adjustments they have agreed with their employer should be explained in the job plan section of the application form. Employers may add explanations about any disabilities or other relevant aspects in their comments.
We treat all applications equally and use the same scoring criteria for everyone.
Extenuating circumstances
If there are extenuating circumstances that an applicant feels may affect their ability to submit a successful application, we would like them to let us know as soon as possible before the application closing date, so we can provide support and make sure the application is considered fairly. We cannot take any extenuating circumstances into account after the application form has been submitted and once scoring has started.
Each case is treated on its own merits, and the outcomes from each are based on the rules relating to the current scheme. If a consultant applies for an award and believes there are extenuating circumstances, these can be described in the job plan, personal statement and/or the relevant domains of the application form.
Pay careful attention to applications where a consultant’s circumstances and job plan have changed during the course of the 5 year assessment period. Applicants are strongly encouraged to be precise about the timing of any such changes in working pattern, and to provide dates for the achievements that they are presenting for assessment. For example, an applicant may describe periods of absence perhaps due to maternity leave, or ill-health during the relevant 5 year period. In such cases, it is reasonable to take into account work done over a more prolonged time period when assessing the application.
We understand that it can be difficult for applicants to share personal information. As assessors we expect you to treat any such information with respect and in confidence.
Transitional arrangements for people with existing national Clinical Excellence Awards
Following the introduction of a new NCIA scheme from 2022, existing national CEA holders are subject to prior CEA rules for their awards and tenure. There is a transitional period based on previously agreed schedule 30 arrangements for CEA holders applying for a first new award.
Rules that apply to existing national CEA holders:
-
if an application is made for a first new award before an existing national CEA would have been due for renewal under the old scheme and are unsuccessful, the individual keeps their existing CEA until its expiry – they may apply for an NCIA again up to the year before the CEA’s expiry
-
if a CEA would have been due for renewal and the application is unsuccessful, the reversion arrangements to receive a legacy, pensionable local CEA will continue to apply. The level of the local award depends on the score obtained in the new NCIA application
-
if a consultant applies in the year their national CEA expires, this CEA will lapse before the annual NCIA award round is completed and the applicant will not be eligible for the transitional arrangements
-
if an applicant applies in the year their NCEA would have been due for renewal and they successfully gain a new NCIA, their new award will start when their NCEA expires – the value of legacy CEAs and its pensionable benefits are protected for the duration of their first new award at an equivalent level
-
if an applicant applies at any other time before their NCEA expires and they successfully gain a new NCIA, the new award will start on 1 April following their application
-
if an NCIA is gained at an equivalent or higher level to their national CEA, the payment received will be no less than the value of their existing national CEA
-
if an NCIA is gained at a lower equivalent level, the applicant will receive no less than the legacy national CEA payment at that level – there will be an obligation in this case to accept the new NCIA and give up any unexpired CEA; local awards cannot be held simultaneously with NCIA awards that benefit from schedule 30 protection
The equivalent levels are:
- N1 NCIA – equivalent to silver CEA
- N2 NCIA – equivalent to gold CEA
- N3 NCIA – equivalent to platinum CEA
Any CEA award holders who enter the transitional arrangements will not currently be eligible for local CEA payments.
Initially, due to the cost of the transitional arrangements, NCIA holders are not eligible for local awards in England at the same time whether or not they held a prior national CEA. This will be reviewed during and after the transition period to see when national and local awards can be held concurrently. You can read more information about this in the consultation response.
Anyone awarded an NCIA, whether affected by schedule 30 transition or not, is considered to be successful in gaining an award and is obliged to accept it. Holders of existing NCIAs must give up any unexpired NCIA, even if the new award is at a lower level.
Part 2: eligibility for NCIAs
Who can apply for an award
To apply for an NCIA, a doctor or dentist needs to be a fully registered medical or dental practitioner on the General Dental Council (GDC) special list, General Medical Council (GMC) specialist list or GP register.
The applicant must be:
- fully registered with a licence to practise
- a permanent NHS consultant or academic GP in a permanent clinical academic role in higher education at the same level as a senior lecturer or above, for at least one year on 1 April in the award year – the year does not include time spent as a locum, but applicants can give evidence from their achievements as a locum in the same role
For consultants in a locum role for more than one year, we may consider them eligible for an NCIA if their employer confirms that they are employed on terms consistent with a permanent consultant contract.
In all cases, an applicant must be on an NHS consultant contract expressed in programmed activities (PAs), or on an academic contract expressed in an equivalent pay scale.
Consultants working in Wales must be on an NHS consultant contract expressed in sessions, or on an academic contract expressed in an equivalent pay scale.
If employees are unsure about whether they are eligible, they should contact the ACCIA Secretariat at accia@dhsc.gov.uk.
Qualifying criteria
A consultant will qualify if they are:
- employed by an NHS organisation (in England or Wales), DHSC or its arm’s length bodies, a university, medical or dental school, or local authority. Applications from employees of other organisations may be eligible, including those on consultant contracts providing contracted out NHS services. Those individuals are encouraged to contact us at accia@dhsc.gov.uk before applying if any clarification is required
In Wales, an applicant will also qualify if they are employed by similar Welsh government-associated organisations.
-
an academic GP if their responsibilities are the same as consultant clinical academic staff and they are fully registered with a licence to practise. An academic GP can apply for an award if they:
- work at least half their hours as an academic GP
- are a practising clinician providing some direct NHS services
- are contracted for at least 5 PAs or equivalent sessions that help the NHS – including teaching and clinical research if full time. Part-time consultants must be contracted for at least 3 PAs that are considered to be clinically relevant as assessed by ACCIA’s national medical director
-
a consultant or a dental practitioner with an honorary NHS contract who is fully registered with a licence to practise. Whether they qualify for an award does not only depend on their contribution to the NHS in the provision of direct patient care. A full-time academic consultant will also qualify for an award if they carry out at least 5 programmed clinical activities or equivalent clinically relevant sessions that help the NHS. This includes teaching, training and clinical research. An applicant who works less than full time (LTFT) and does fewer than 3 programmed clinically relevant activities (PAs) is not eligible to apply for an award
-
a fully registered public health consultant on the GMC specialist register or on the GDC specialist list with a licence to practise
-
a postgraduate dean, fully registered with the GMC or GDC with a licence to practise, who competed for the role against GPs and consultants and is responsible for postgraduate trainees across all specialties
-
a consultant or academic GP later employed as a dean or head of school in medicine or dentistry, fully registered with the GMC or GDC with a licence to practise. They can apply for an award based on their work in this post
-
a consultant fully registered with the GMC or GDC with a licence to practise working as an NHS organisation clinical or medical director, or a similar level medical manager post. We would anticipate consultants working in this capacity clarifying their eligibility with ACCIA prior to application – with particular reference to their contractual contribution over-and-above the expected duties in the role, as well as their contractual status. If the majority of the work is in a management role, an applicant can still qualify if they have an active consultant contract with a specific clinical or clinical leadership role, and maintains their licence to practise. If a consultant moves into general management and/or has a management contract outside the consultant pay scale, they are not eligible to apply for an award
As an NHS consultant, it does not make a difference if they have agreed to the national terms and conditions of service, or other terms with an individual organisation.
The Ministry of Defence runs its own award scheme, but we also recognise eligible NHS employee contributions over-and-above the expected standards to military medical and dental services.
If a consultant works LTFT, they can apply for an award if they undertake a minimum of 3 clinically relevant contractual PAs. If an applicant is eligible based on this minimum PA requirement and is successful, we will pay the full award. However, if a consultant is working LTFT and in a transition provision from a national CEA based on schedule 30 legacy award values, they will receive a pro-rated award. Their working arrangement should be described in the job plan and the domains assessed against the LTFT expectations.
Retirement and pensions arrangements
If a consultant retires during an awards round before we announce the results, we take this to mean that the application has been withdrawn.
If a national CEA would have been due for renewal in 2023 and a consultant expects to retire up to 6 months after the award is due to expire in March 2024, we may consider extending the award without the need to apply for a new NCIA.
National CEAs are consolidated with the pension, which means it is taken into account when the pension is calculated. These awards stop when a consultant retires and leaves the NHS permanently. If they return to work on a permanent NHS consultant contract retaining or regaining full registration with a licence to practise, they can apply for a new NCIA.
NCIAs are not consolidated with pensions. If a consultant retires with an NCIA and does not return to eligible employment either on a partial or full-time basis, the award will end. Further details are available in the applicants’ guide on the application guidance page.
If a retired consultant applies for an NCIA when they come back to work following a break in their employment, assessors and employers should only consider and reflect upon the consultant’s achievements since their new contract started. They should not consider evidence used to apply for the last award, evidence from before the new contract date, or evidence that is not clearly dated.
A consultant who did not have a national award when they retired can still apply for an NCIA.
Flexible retirement or partial drawdown of pension benefits
As of 1 April 2023, if a consultant begins receiving pension benefits, up to 100% of their allowance, but continues in eligible employment their award will continue until its scheduled expiry date, provided they continue to meet the standard eligibility criteria.
Holders of NCEAs, or NCIA holders subject to transition arrangements, who reduce their contracted PAs with their employer will have their award paid pro rata in the same way as any award holder working LTFT.
For example:
- if a consultant draws down pension benefits and makes a small reduction in their contracted PAs, we may pro rate their award accordingly
- if a consultant draws down pension benefits and makes a significant reduction in their contracted PAs and job plan, we may shorten the duration of their award and ask them to re-apply early
- if a consultant draws down pension benefits and makes a significant reduction in their contracted PAs which takes them below the minimum eligibility requirements, we will cease their award
Consultants that may not be eligible for an award
A consultant is not eligible to apply for an award if they are:
- not on the consultant pay scale as expressed in PA or an equivalent
- a locum consultant – though if an applicant then becomes a permanent consultant, they can potentially use evidence from the locum role in their application if it is relevant
- a consultant who primarily works in general management, such as a chief executive, general manager, chief operating officer, or a senior university office-holder without a specific clinical role
- not fully registered with a licence to practise
Investigations into a consultant’s work and disciplinary or legal action against an individual can affect their award or application. This includes interim, temporary or final court orders or penalties relating to professional or personal conduct that may reflect badly on their judgement, or the expected standards of the profession.
Consultants must let us know about any investigations or sanctions by an employer or professional regulator (GMC or GDC) and their progression, interim and final decisions and any sanctions. We will look at each case individually, but we may remove an award if there are adverse outcomes following investigations or disciplinary measures, or if we believe a doctor has failed to notify us appropriately or in a timely manner. If this happens, any over payments will need to be repaid. If employers become aware of such matters, they are also expected to notify ACCIA.
We also ask about an organisation’s latest inspection outcome. If an organisation is in special measures, we expect a consultant to comment on any relevance of this to their role. We will also ask their employer to check that you are happy with any response when you sign off the application. If a consultant is on the board of an organisation in special measures and is recommended for an award, we will inform our main committee.
Part 3: the application process
Filling in the application
A consultant must fill in their own application form – nobody else can do it for them.
Applications can only be made online at the ACCIA application portal. Detailed advice on how to make an application is available in the applicants’ guide on the application guidance page.
On application, a consultant must first select the NHS or arm’s length body that holds their substantive or honorary contract and their specialty, so that the right sub-committee considers the application. The employer is selectable via a ‘search’ in the new online application form. If an individual is employed by more than one body, they are asked to state all of their employers and roles – being clear which is the main employer based on who pays their salary.
Support for applications
We cannot accept applications without sign-off from the employer(s). They will need to complete a short form to verify the application; this requires joint sign-off from all employers if there is more than one. Further details are available in the employers’ guide.
If a consultant works for a university (clinical academic), the chief executive of the organisation where they hold an honorary contract, or their nominated deputy, should complete this section. It is ACCIA’s expectation that both the relevant NHS organisation and the university or medical school will be involved in the approval process and the preparation of any supporting citation, and that an up-to-date job plan has been agreed by both parties. See part 5 below on how to interpret citations.
Many membership and specialty organisations can provide assistance and general guidance with applications using tools made available to them by ACCIA. Organisations must not proofread, review or directly critique any part of an application. Applicants can indicate on their form if they have sought advice from any such organisations.
Timetable for 2023 national awards
Consultants must submit their online national Clinical Impact Award application to ACCIA by 5pm on 5 May 2023. Applications will not be valid after this – regardless of the reason that the deadline was missed.
The indicative timetable for the 2023 awards round is set out below. This may change based on the impact of the coronavirus (COVID-19) pandemic and other operational factors – we will review it regularly:
- 10 March to 5 May 2023 – applications open
- 9 May to 29 June 2023 – first round scoring
- 3 July to 4 September 2023 – N3 scoring
- 3 July to 6 November 2023 – governance review
- 5 September to 6 November 2023 – NRES scoring
- end November 2023 – main committee finalisation of recommendations
- December 2023 – recommendations to and sign-off by ministers
- mid-January 2024 – notifications sent to successful applicants and finance processes initiated to back pay awards
- mid-January to mid-February 2024 – appeals window open
General advice for applicants
Applicants are advised to start their application early enough to allow time to get sign-off from their employer and engage with any relevant membership or other organisation, or university pre-selection processes.
When a consultant fills in their application form, they are advised to follow the steps indicated in the applicants’ guide. Knowing what advice has been provided to applicants should help assessors apply their scoring criteria fairly, what to look for in a good application, and where problems and inconsistencies may arise – see part 5 for further information.
In the applicants’ guide, it is advised that candidates applying for an NCIA are expected to:
-
give clear dates for their achievements – if the dates are not clear, you should not score this highly
-
concentrate on evidence of national impact (not activity) from the last 5 years, make it clear what has been achieved since any prior award and how a consultant’s work has progressed since then
-
confirm if their last award was less than 5 years ago, give evidence since this last award and be clear about what has been achieved since then
-
if their last award was more than 5 years ago, concentrate on evidence from the last 5 years
-
not repeat information from old applications – assessors will compare new and previous applications and will check for repeated information
-
write society and group names in full – avoid acronyms because sub-committee members reading the application may not be familiar with them. The same applies to other medical abbreviations, such as those used for diseases, operative procedures, or diagnostic techniques
-
give measurable information such as outcome data wherever they can and quote the dates, source and relevant benchmarks
-
explain the impact of their work – simply holding a position such as an officer in a college or specialist society will not in itself justify an award (the national impact needs to be clear, otherwise you should not give a high score)
-
use a new line for each entry, consider using bullet points to make the information clearer and easier to read
-
stay within the character limit for each domain and not include any website addresses or other external links to additional information
-
be prepared for scrutiny by ACCIA if anything is unclear in their application
We make it clear that if there are special circumstances that could affect an application such as ill health, we are keen to know as soon as possible before the deadline as we may consider extending an award.
Part 4: the assessment process
While we have moved to a non-stratified system of scoring with no renewals, the fundamental principles and processes of the assessment scheme have not changed. As explained above, an online application form will be submitted for competitive scoring in the first instance to one of the 13 regional sub-committees or to the ALB committee, with separate arrangements in place for applicants in Wales and for the armed services.
Each region is pre-allocated an indicative number of awards at each level (N1, N2 and N3) to retain the equity of regional opportunity for success. This continues to be based on the number of awards available nationally and the number of applications received. A 2-stage scoring system then operates.
In the initial scoring round, all applications will be assessed on merit, scoring each domain a 0, 2, 6, or 10 (see part 5), and a ranked list generated on the basis of mean scores for the applicants as normalised between any regional scoring groups. This leads to a provisional allocation of a certain number of awards at N1, N2 and N3 level on this basis. For example, in the event of there being 2,000 applications this year, and a planned final total award number of 600, this gives a 30% success rate. A large region may have an indicative number of say as many as 400 applications. With a fixed proportion of N1, N2 and N3 awards – 55%, 33% and 12%, this would mean that in the initial scoring round, the region sub-committee would recommend 66 awards at N1 level, 40 awards at N2 level and 14 awards at N3 level. The cut-off score is dictated by the indicative numbers and the distribution of the average scores within a region.
To determine the final allocation of N3 (platinum equivalent) and N2 awards in this region, the 14 presumptive N3s and 14 top-ranked N2 awards are then referred for rescoring by the national N3 committee, comprising chairs and medical vice-chairs drawn from the English regions, and selected other experienced scorers. This virtual committee will rescore the 28 applications together with all other similarly placed applications from all other regional subcommittees. At a national level, the aim will be to allocate 70 applications at N3 level. These will be those ranked in the top 50% after review by the N3 committee, while the bottom 50% will be recommended for an N2 award.
The N2 awardees nationally will therefore comprise 70 applicants drawn from the lower ranked 50% from the national N3 committee and 130 individuals chosen through stage 1 scoring – making a total of 200 awards subject to governance and any financial constraints related to transitional pay protection costs.
Governance review
N3 awards will be subject to governance review by the ACCIA chair, medical director and the main ACCIA committee, as were platinum awards previously. Chair and medical director scrutiny will also be applied to all N1 awards and the lower N2 cohort with referral to NRES, as was previously the case. Detailed NRES processes will be advised at a later date and will depend on the numbers of applicants referred.
See Annex A for a diagram of the scoring process. The final number of awards may be limited by the financial envelope available, and is ultimately subject to ministerial approval.
Regional sub-committees
A regional sub-committee (RSC) has a lay chair, medical vice-chair (MVC) and typically between 15 and 30 members. These roles are voluntary and regularly refreshed. Applications are vetted and approved by the ACCIA chair and medical director. Regional chairs and MVCs are refreshed each year as tenures expire. We continue to keep this under review.
It is the RSC members who have responsibility for stage 1 scoring. All applicants for an award will be typically randomised to 2 groups – or in a region with very large numbers of applicants, 3 groups. As an RSC member, you will be allocated to one of these groups and score typically between 30 and 70 applications. In some cases, scorers will be allocated to a different region, something we introduced in 2021 to balance diversity and workload, and deal with conflicts of interest – for example, if a professional RSC member is also applying for an award. A small number of experienced assessors may also be asked to join the national reserve committee. ACCIA will inform all scorers of their obligations at the end of the application round, when all the applications have been submitted and we have a clear idea of the number of applications which need to be assessed.
RSC meetings will typically be online using Microsoft Teams, or in some cases hybrid depending on circumstances. They will be organised and attended by one or more members of the ACCIA secretariat. These will take place in late spring or early summer, with dates to be advised 4 to 6 months in advance. Prior to each meeting, all provisionally successful allocations will be reviewed by the ACCIA chair or medical director. All discussions regarding NCIAs are confidential and no aspects must be disclosed or discussed outside of the meeting.
Any application where we have governance concerns (typically 5% to 10% of successful applications) will be flagged in advance to the RSC scorers for discussion at that meeting. The purpose of the meeting is to discuss the relevant issues and decide on the need for referral to NRES (see part 4). There is no rescoring regionally or changing of marks or ranking, and your role at the regional committee meeting is to provide corroboration and triangulation of information on the form where possible. No specific additional information known to committee members but absent from the written application can be considered at this point, nor is it your role as an RSC member to lobby for any particular individual. Applications below the derived cut-off scores are not discussed, though applications will be referred to NRES in the event of a tie of these scores.
RSC meetings will be chaired by the ACCIA chair, with support from the local chair and MVC. There is the option for the RSC chair or MVC to organise a pre meeting on the same day or on another occasion to discuss those applications flagged by the governance review, or other local issues, but this is no longer compulsory. The same rules apply, and scores cannot be modified in any way.
All new RSC members are required to attend the scorer training ACCIA are offering in the spring of 2023. This will be delivered in an interactive way using the Microsoft Teams platform. Each session lasts between approximately 2 to 3 hours. Experienced scorers are not only welcome but encouraged to attend for refresher training.
Part 5: how to score an application
Your role as an assessor – principles and priorities
Your role as an assessor is to assess clinical impact. This about providing high quality services to patients that go beyond a consultant’s immediate remit, that improve clinical outcomes for as many patients as possible, use resources efficiently and make national services more productive.
Applicants also need to show you evidence of how they worked to make services more efficient and productive at a national level and improved quality at the same time, as well as demonstrating their role as an enabler and leader of health provision, prevention and policy development and implementation. There will also be an opportunity to demonstrate a commitment to, and nationally relevant impact on improving the NHS through leadership, education, training, people development, and innovation and research. Applicants do not need to show they have achieved over-and-above expected standards in all these areas – a lot will depend on the type and nature of their post.
You are expected to:
-
assess evidence on the application form in the 5 domains against expectations in the job plan provided, considering any extenuating circumstances as necessary
-
base the assessment only on written information presented in the form – not hearsay or reputation, or prior personal knowledge
-
not assess any information from website addresses or other external links applicants may include to provide additional information
-
ensure applicants do not seek to gain an advantage by linking to additional external evidence and you must not access or score evidence that is not on the application form itself
-
review the employer sign-off and citations to triangulate the evidence; citations, personal statements and other components of the application form are not scored
-
score independently without discussion or consultation
-
be consistent and fair in your scoring, remaining constantly aware of the possibility of conscious and unconscious bias
-
identify any major conflicts of interest, and if necessary omit to score one or more applications, informing ACCIA of why you elected to take this course of action. A candidate will not be disadvantaged by this as the aggregate scores from the other scorers are still averaged in the same way
-
declare any conflicts of interest to the secretariat as soon as they are known. To ensure the probity of the awards process, sub-committee members should not participate in the scoring or discussion of applications from close personal friends, family members or those with whom they have a managerial or subordinate reporting relationship
-
sub-committee members applying for an award should take no part in the scoring of any applications or the associated discussions within their region or if relevant within any national committee
-
seek advice as necessary – from ACCIA, a MVC or a chair
-
keep all aspects of the applications, ranking and RSC discussions strictly confidential
Professional members should not score or discuss any applications in a particular region if they are applying in that region, and may be asked not to score in NRES or N3 scoring.
Professional, lay and employer representatives are there to score and assess individual applications – not to represent any speciality or organisation, race or gender.
Confidentiality is paramount and applies equally in these contexts:
- assessing and scoring applications
- discussions at Regional Subcommittee or other meetings
- discussion of applications at training sessions
- informal mentoring and discussions with applicants
- discussion or casual conversations outside of committee meetings
You should only confer with other sub-committee members (who are not themselves applying) once you all have scored the applications and scoring has closed. If you have any concerns about an application or the scoring process, you should raise them with your committee’s chair, MVC and with central ACCIA. Under no circumstances should you discuss the process with any of the applicants or any other party.
Assessing the domains
Applicants need to make it clear that their achievements are relevant. As an assessor, you need to know when they occurred or if an applicant is still doing these activities. It is essential that they make the dates of their achievements clear, as without dates they cannot be scored. You should differentiate between achievements (results and output) and activity (input) and score achievements that are national more highly. Activity alone should not generate high scores.
Expectations of applicants:
- an applicant could get a national award based on an excellent local or regional contribution if it has been disseminated and had a demonstrable impact on the wider NHS
- they should highlight the most important examples of their work focusing on its national and sometimes international impacts
- they should describe the national impact they have had in any roles listed, including acknowledging the contribution of colleagues and other members of the multi-professional team
- applicants should make it clear when their roles started and ended, or if they are ongoing
To determine if a consultant is performing over and above, it is helpful if they list their achievements against the original aims in their job plan or personal development plan.
An applicant should not include evidence given for an earlier award unless it shows how they have actively built on or consolidated previous achievements in the last 5 years or since their prior award if less than 5 years ago.
Quantified data is particularly useful, including outcome measures, that:
- show what has been achieved since a previous award, and specifically over the last 5 years
- include relevant dates, sources, and appropriate benchmarks
If work is subject to national audit processes, it may be helpful if applicants include this information too – be advised that it is much easier to quantify clinical quality and performance in some clinical areas than others.
The ‘Job Plan’ section of the application form forms an important benchmark for expectations of the applicant’s paid roles. It should list clearly and separately each direct clinical care, supporting and other PA the applicant is paid for, including (if relevant) a detailed breakdown of any academic PAs (research, teaching, and university management responsibilities). It should state clearly which activities the NHS pays for directly and which, if any, are paid for by others such as a university, research council, the National Institute for Health Research (NIHR), another research funder or deanery.
Applicants should also describe any other paid roles that are relevant to the evidence provided in the application – how many PAs they represent and for what activities. We do not need to know the amount paid.
If they receive any income outside their job plan from wider roles that may be relevant to the evidence provided in their application such as editorial payments, consultancy or lecture fees, or roles or shareholdings in private companies (such as non-executive roles or senior positions in spin-off companies between academia or NHS organisations and the private sector), these should be outlined in this section.
We do not need to know the amount paid and there is no requirement to list private or wider income if it is not relevant to the evidence set out in the application.
If the job plan is not clear it can be difficult to assess the evidence in the domains and you may allocate lower scores as a result. Work that is paid as part of the job plan is considered in role. Other work that is paid from elsewhere should also not be scored highly unless it is made clear how its impact is above the expectations of its remuneration.
Committee members should score the domain sections as follows:
- 10 = the application is excellent with clear and sustained national and or international impact
- 6 = the work is over-and-above the applicant’s contract terms and should have national or at least demonstrable regional impact
- 2 = an applicant has met the terms of their contract or may have contributed more but mainly within their locality
- 0 = a consultant has not met the terms of their contract or there is not enough information to make a judgement
What to look for in each domain
There are 5 domains, achievements should be described in line with each one avoiding repetition across domains unless the evidence shows different aspects of work that is relevant to the domain. In all cases, dates must be included. Any evidence that is repeated can only be scored in one domain.
We recognise the extraordinary requirements of the COVID-19 pandemic and the work that many consultants, academic GPs and multiple other healthcare workers have contributed. Applicants may choose to include evidence related to this as part of their evidence-base over prior years. If this is the case, look for evidence of impact of contributions over-and-above an applicant’s expected role, where it has had an impact outside of their immediate local remit.
We recognise how important redeployment and extended hours and remits have been in COVID-19, and that these are broadly universal across the NHS. Some recognition may be given for efforts made to maintain or restart other key clinical services, research activities, and teaching and training during the pandemic period. While local work related to COVID-19 was essential, it should be scored higher where there is clear evidence demonstrating how it has had broad and ideally national impact.
Domain 1: delivering and developing a high-quality service
In this section, applicants should give clearly dated evidence of what has been achieved in relation to:
-
providing and developing a safe service with measurable, effective clinical outcomes based on delivery of high technical and clinical standards of service that provides a good experience for patients, and how they have cascaded this more widely to colleagues who have implemented improvements based on this experience. Relevant publications may provide corroboration
-
consistently looking for and introducing ways that have improved their service – sharing the learning and seeing evidence of its embedding in practice elsewhere
Applicants should explain which activities relate to clinical services where they are paid by the NHS, and to other aspects of their work as a consultant.
Applicants should include quantified measures like outcome data. These need to reflect the whole service the multi-professional team provide and how they have collectively disseminated their experience. Applicants should use validated indicators for quality improvement or quality standards and other reference data sources in England or the healthcare standards for Wales – ideally providing performance data against benchmark or national indicators for their specialty, showing local and wider improvements as a result of their work.
For good patient experience, applicants should show how they have ensured patients are cared for with compassion, integrity and dignity and how they have demonstrated commitment to patient safety and wellbeing.
Evidence could show:
- excellent standards for dealing with patients, relatives, and staff. Surveys or collated 360-degree feedback to validate evidence of patients’ quality care, especially when this practice has been further shared and used to improve services elsewhere
- excellent work in preventative medicine and public health, for example, in alcohol abuse, vaccination programmes, stopping smoking and preventing injury and where this work has been further developed outside their immediate remit
- how wider NHS resources are used effectively and their efficiencies improved
Look for evidence of the quality and breadth of a service from audits or assessments by patients, peers, the employer or external bodies. It should not impact negatively on your scoring if there is less readily quantifiable evidence available in a particular specialty.
Evaluate the source of the information given and whether all relevant dates have been included.
Here are some examples:
I have further developed efficiency and quality of the X heart magnetic resonance imaging (MRI) service and disseminated achievements beyond my job-planned activities.
Since 2018 I have grown the service by 25% to 3,000 per year (largest in X of England).
In 2019 I introduced patient-centred governance (including annual 360 patient feedback, audit cycles, safety and quality reviews). The service was rewarded with European Association of Cardiovascular Imaging accreditation in 2022.
Through close university partnership I improve NHS service efficiency (in 2021 academics delivered NHS service with NHS staff reassigned to COVID care) and quality (rapid research-clinical translation).
While most other NHS wait times increased, I kept heart MRI wait below national pre-COVID benchmark throughout the pandemic – 2019 to 2021.
In 2020 introduced a faster heart MRI protocol with equivalent quality to previous methods. This improved local service efficiency by 25% (more scans at same cost) and patient experience (shorter scan). Method published in a sector-leading X journal and disseminated in internationally in 2022.
Pioneered new MRI methods for non-invasive, radiation-free diagnosis of heart disease in newborns in 2021 and in the foetus in 2022. Published the method (reference) and first clinical experience (in press 2022) to cascade beyond local service.
In 2018 proposed an automated quantitative method in collaboration with UK and US scientists that allows more objective diagnosis of heart disease and can replace expensive radiation-based nuclear imaging. From 2019 the method was available to NHS patients in X and London and is now embedded in more than 10 NHS hospitals.
In 2018 set up heart screening for patients at high cardiac risk (for example, diabetes, rheumatoid arthritis), implementing the national NHS strategy.
I have set up a short stay programme which has the lowest length of stay for hip replacements in England – 2.7 days as against the England average of 6.1 days … 67% of patients are home after 2 nights … 98.5% patient satisfaction service … readmission rate of 5.1% as compared to the regional average of 7%. This has been communicated in X forums and adopted as best practice standards by X body.
National or regional benchmark comparisons are useful, if available. For example, standard mortality ratios, peri-operative complication rates, MRSA, C. difficile rates, venous thromboembolism (VTE) prevention, or length of stay data.
A strong applicant may show how they have significantly improved the clinical effectiveness of their local services and either improved services elsewhere, or used their experience to enable others to do so. Similarly, this experience may be translatable to other clinical services in the wider NHS in other areas. This includes making services better, safer and more cost effective more widely, particularly in addressing differences in outcomes between different geographic regions, or diverse patient groups. Relevant publications authored by the applicant may be informative.
In all cases an applicant should make their personal contribution clear, not just their department’s contribution, stating what they have contributed as part of a wider team where relevant. Examples of any changes made after the results of an audit, or changes to which the applicant contributed as part of governance reviews. Look for evidence of how the applicant may have personally helped these activities contribute to wider change in the NHS.
Evidence could, for example, cover the impact of work on:
- developing and running audit cycles or plans for evidence-based practice to make the service measurably better
- national or local clinical audits and national confidential enquiries
- developing and using diagnostic and other tools and techniques to find barriers to clinical effectiveness, and ways to overcome them and implement new ways of working
- analysing and managing risk – details of specific improvements, or how risk was lowered and safety improved
- providing a better service, with proof of the effect it has had – for example, how a service has become more patient centred and accessible
- improving the service after speaking to patients or setting up and engaging with patient support groups
- redesigning a service to be more productive and efficient, with no decrease in the quality, particularly at a regional or national level
- developing new health or healthcare plans or policies
- large reviews, inquiries or investigations
- national policies to modernise health services, new ways of working or professional practice
Look for audit or published research to show where the consultant’s work has directly improved their service and disseminated this good practice more widely.
Domain 2: leadership
In this section, an applicant should show how they made a significant personal contribution to leading and developing a service, health policy or guidelines with national or international impact where it is outside the expectations of any paid leadership role they may have. Especially consider work that had delivered against objectives within the NHS Long Term Plan.
Applicants should describe the impact and outcomes generated in the specific roles they list and how it has been cascaded and implemented widely. Evidence can include, but is not limited to, proof of:
-
effective leadership techniques and processes – giving specific examples of how they improved the quality of care for patients and where they have directly or indirectly influenced other parts of the NHS to achieve these benefits
-
change management programmes or service innovations they have led – showing how they made the service more effective, productive or efficient for patients, public and staff, beyond their direct remit
-
excellent leadership in developing and providing preventative medicine, particularly working across organisational or professional boundaries with other agencies, such as local councils and the voluntary sector, demonstrating the outcomes or impacts that have been delivered – for example in delivering benefits where health inequalities exist
-
how applicants helped staff or teams more widely improve patient care – giving specific examples and their outcomes such as mentoring or coaching. Consultants who work in England may mention the guidance on talent and leadership planning
-
any ambassador or change champion roles, for example if they were involved in, or their job involved explaining complex issues and how this translated into changes in practice
-
how applicants developed a clear, shared vision and desire for change in others – for example, showing how they invested in new ways of working and handled resistant behaviour to deliver wider change outside of their remit, particularly where they did not have direct oversight responsibility
-
how applicants helped staff into senior leadership roles by removing barriers, encouraging diversity and achieving equality and inclusion outcomes
-
how applicants contributed to developing patient-focused services in their area and cascaded the experience and expertise to influence others to adopt new ways of working, particularly at a regional or national level
-
national impact through personal work and influence through any committee membership. Look for evidence of what was done personally, with a description of the impact of any output. Membership alone is not enough
-
the effects of team leadership where the applicant had full or joint responsibility or having taken turns with other leaders to lead specific areas of complementary work
-
where applicants took personal leadership for clinical governance, including developing and implementing policies, services or change programmes
Applicants are required to show specific evidence of contribution, the source of any data and relevant dates.
Here is an example.
“National and international:
-
As RCP special advisor on X since 2019 I lead the RCP’s X policy, interfacing with the Department of Health. I organised a meeting at Number 10 (2021). I respond to X consultations, reports and news items
-
As chair of the RCP advisory group on X (2019) and advisory group on health inequalities member (2020), I’ve worked across professional boundaries and with patient groups
-
I have developed and presented an X documentary ‘X, England’s most pressing healthcare challenge?’, highlighting the complexities of X, viewed more than 13,000 times since March 2022
-
I co-chair NHS England’s Clinical Advisory Group for Tier 3 and 4 services (from 2021) responsible for mapping and establishing services across England
-
I am a trustee and chair of the nationwide patient charity X Empowerment Network UK steering group from 2019 (see domains 3 and 5)
-
I am a trustee for the Association for the Study of X (ASX) since 2016 and organise annual national clinical network meetings to share best practice
-
I am currently a member NICE X Clinical Guideline Committee (since 2021) responsible for updating the guidelines. So far we have updated the following 3 guidelines…
-
I am a member of the working group that led to the establishment of the National X Audit (since 2020) which has delivered…”
Work in roles in education, such as chairperson of a training committee should not be cited in this domain. Applicants should include that information in domain 3.
Domain 3: education, training and people development
In this section, an applicant should give evidence to show their contribution to wider education and training across the professions and to patients outside their local or paid remit. It should be made clear if any training or lecturing is externally or separately remunerated.
Where relevant, applicants should give evidence of the impact of their work in supporting the NHS People Plan and if it falls into any of the following categories. We do not expect examples for all these categories and other categories can be included.
Teaching
This can be medical undergraduate or multidisciplinary team teaching, if it is outside the job plan. Undergraduate teaching, or local academic management activities (for example chairing an examination board) that are a core part of an individual’s job plan are not considered to be over and above their role.
Applicants are encouraged to give evidence of student feedback or other teacher quality assessments and especially focus on how their educational work has improved others’ performance and has had a positive impact on healthcare. As an assessor, you should look for evidence of a personal role in curriculum development and/or assessment and, if relevant, evidence of wider adoption of novel work in these areas in UK medical schools, or internationally.
Leadership and innovation in training
This should include evidence of the impact of these activities outside of an applicant’s own remit, preferably nationally or internationally. This might include:
- developing and introducing a new course, such as at masters level
- innovative assessment methods
- introducing new learning facilities
- writing successful textbooks or developing online teaching or training modules, or an app
- contributing to postgraduate education and life-long learning
- contributing to teaching and assessment in other UK centres or abroad
- developing other innovative training methods, such as simulation-based
Supporting information could be presentations, invitations to lecture, and publications on education – evidence should be included of the wider national impact of these activities.
Educating and informing patients and public
Examples could include how applicants:
- promote good health and disease prevention within the community which has delivered wider impacts
- facilitate the development of patient support groups at a regional or national level that can show improved patient engagement and outcomes, tangible improvements in preventing illness and injury, or improved patient and public involvement in research
College or university success in teaching audits
An applicant could explain if they helped a college or university succeed in regulatory body and quality assessment audits for teaching. This could include undergraduate or postgraduate exams, or supervising postgraduate students and trainees leading to a demonstrable impact on healthcare as a result.
Personal commitment to developing teaching skills
Evidence could be included of higher education academy membership or fellowship and any educationally focused courses completed, and how these new skills or qualifications have been implemented in practice to improve and modernise training and education.
Unexpected or non-mainstream contributions
This could be any other teaching or educational commitment that has had national impact and is outside the job plan, or other paid work, that is not recognised in standard ways.
Here is an example:
“My main leadership role as Royal College of X Medical Director for Education and Training is to ensure continued high quality workforce supply to support patient services in Xology to meet national objectives.
-
Provided Royal College data in 2020 into the X Review to support the need for 1,000 extra Xologists
-
Led nationally to support training programmes and trusts accommodating 150 new Xology training posts in England and extra senior posts in 2021 and 2022. This included support to make the local business case given the financial benefit of trainees and this has successfully unlocked previously unavailable training capacity in each region
-
Led the negotiation of changes to Xology trainee recruitment with the national recruitment team. This new process successfully enabled increased numbers of candidates to be assessed in 2021 and 2022 to fill capacity from training post expansion
-
Led a new process of recruiting trainees nationally at a more senior ST3 level to meet workforce need and training number targets. This involved development of a detailed certificate of training equivalence to demonstrate ST2 competencies achieved elsewhere and required agreement of national heads of training. Fifteen candidates were offered training posts in May 2022
-
Leading the development of virtual and technology enhanced training material and imaging platforms with the new imaging X academies in England in collaboration with academy leads. This has promoted a sharing ethos, with remote teaching sessions made available across Xology academies in 2021 to 2022 to support increasing training provision”
Domain 4: innovation and research
This section looks at innovation and its impact in any relevant setting and may include evidence of impactful work other than the activities that are traditionally considered as research.
It can include new care pathways that have been developed and implemented, improved ways of working and process efficiencies that have been adopted widely, and have demonstrably made more cost effective use of NHS resources. It can also include benefits of digital technology or other activities from projects with external partners that have demonstrated a benefit to the wider NHS, or that support the GMC’s objectives of promoting research for doctors. Remunerated roles for implementing digital healthcare tools locally would not be expected to score highly unless clearly over and above the paid role or implemented outside their geographic remit.
Applicants should be clear what evidence is over-and-above any research, academic or other expectations of their role and give evidence of the wider impact of the research and/or innovation. This may include developing the evidence base for measuring how quality has improved.
In the section on references, applicants should show details of achievements such as published peer reviewed papers – not the names of referees or electronic links to papers or reviews. Any publications listed should be from the last 5 years. Evidence should include the relevance of these publications, where they have been published and explain the wider impact they have had. Providing the number of citations each paper has had or its academic score is not sufficient without further explanation of its impact.
As an assessor, you should look for linkage between this section and evidence provided in other parts of the form. For example, if in domain 1 or 2 an applicant has indicated that they have played a major role in the development of a clinical guideline, look for a relevant publication. The guideline itself may have been published in an official document (such as through a government agency) or in a relevant journal.
When assessing publications, you should be aware that it is easier for investigators in certain specialities to publish work in so-called high-impact journals such as The Lancet or the British Medical Journal (BMJ), than in other clinical areas. The short explanatory comments attached to a paper should help, and may for example confirm that a particular journal is the leading one in that area, something of which you may not be aware as an assessor.
On a separate line, applicants could explain what they have achieved in the last 5 years and how this innovation or research has quantifiably improved health outcomes. They must give supporting evidence. For example, they could give details of new evidence-based techniques, innovative systems or service models developed that others have adopted more widely.
Applicants could also explain how they have improved patient and public engagement in research and innovation both in the planning and delivery stages, or encouraged new ways of thinking informed by patient involvement when it comes to improving patient services, detailing the specific wider benefits this has brought.
Applicants should describe the effect of their research (including laboratory research) and any new techniques they have developed and the wider benefits delivered on:
- health service practice
- health service policy
- developing and improving health services and enhancing patient care
As an assessor, you should look for a clear explanation of how their research is currently relevant to the health of patients and the public, or how it may do so in the future.
Applicants could give details of the impacts delivered as a result of:
- large trials or evaluations (including systematic reviews) they led or coinvestigated, and published in the last 5 years. It may be helpful to look at the publication list to corroborate the applicant’s involvement in this work
- their contributions as a research leader, how they have helped and supervised other people’s research and mentored new investigators. For example, look at the publication list to see whether the applicant has published paper(s) with research students, or other members of the multi-professional research team
Applicants could include other examples of the personal impact they have made in their chosen research fields. For example, how their work on any review boards of national funding agencies, charities or learned societies has delivered quantifiable improvements over a defined time period.
Applicants could also:
-
list any grants they hold personally (specifying their role as chief or principal investigator where relevant) and explain how this funding is being used to deliver benefits. You should bear in mind that it may be some time (5 to 10 years) before a research grant produces tangible results. It is also the case that there is not always a direct relationship between the monetary value of a research grant and the resulting impact of the work funded. Important research findings and clinical innovations can result from relatively modest grants, and obtaining multimillion pound grants without evidence of quality outputs should not in itself earn a high score. Evaluating the publications section may be useful. You should, as an example, consider whether the grant funding resulted in one or more high quality papers or reports
-
describe peer-reviewed publications, chapters or books written or edited – defining their editorial activity for each one, for example senior editor, and any quantitative measures on how effective they have been in changing practice
-
give details if they played a major part in research studies in more than one centre, for example personally recruiting participants to large clinical trials
-
include evidence of outstanding research that has led to new ways of preventing illness and injury, or more rapid, cost-effective and reliable diagnosis that have been implemented in the NHS
-
show how they have engaged with a funding council, National Institute for Health Research (NIHR) or a major research charity, specifying their role (clinical director, senior reviewer, or research or fellowship programme lead). Applicants must give clear dates and evidence of their roles and impact
Here is an excerpt from a high-scoring 2022 example.
“Director, Musculoskeletal Research Group (MRG):
As a clinician scientist I am a clinician first. Our 36 researchers address questions from the clinic. Current programmes include:
-
understanding why rheumatoid arthritis (RA) flares
-
can RA be prevented in those at risk?
-
can patients in remission stop their treatment?
-
can established RA be cured?
-
why do RA patients lose muscle? Can it be reversed?
Success indicators:
-
active funding £6.5 million as principal investigator (PI), £1 million as co-investigator from 2018 to 2022
-
72 peer-reviewed papers published since 2018
-
prestigious EULAR Centre of Excellence status awarded in 2020 (for third time: 2010 to 2025)
International firsts:
-
designed and completed (2022) the first trial to target joint lining cells in RA, for patients refractory to standard therapy
-
developed our own cell therapy to switch off RA. Phase 2 trial starts 2022
Collaboration:
I led RA-MAP, an academic/industry consortium seeking biomarkers to inform clinical management and drug discovery. Such partnerships critically underpin the UK Industrial and Life Sciences strategies. Our MRC-funded work, published 2022, involved over 150 researchers and 267 patients with early RA.
Director of Research:
-
Our strategy endorses a mixed portfolio of commercial research, aligned with the UK’s Innovation Strategy and NHS Long Term Plan, and investigator-led research, equally critical for innovation within the NHS
-
Our Dragon’s Den in 2022 will encourage NHS staff to submit their best ideas for mentorship and seed funding
Deputy Director NIHR X Biomedical Research Centre (BRC):
BRCs support research that tests treatments and assays in patients for the first time, driving NHS innovation. As Deputy Director of our £15 million BRC since 2019 I oversee strategy across 6 themes. PPIE plays an essential role in strategy development, plus our strong emphasis on training, education and people development. I also lead our musculoskeletal theme”
Domain 5: additional national impact
This domain is an opportunity for applicants to provide evidence of wider beneficial impacts that have not been captured elsewhere in the information provided on the form in the other domains, and/or to demonstrate how their work has had a wider effect on areas that are national clinical priorities. This could relate to work within their job plan, but should demonstrate the national impact over and above the expectations of activity that they are paid to do. Any evidence that is repeated from prior domains should not be awarded any scoring points here.
Applicants may include any work for charitable organisations, and work which may have more of a patient or public focus, tackling health and workplace inequalities and fostering interprofessional team building or new ways of working. It can also include international work in training, research or recruitment that is of clear benefit to the NHS but in all cases the impact should be clear, with any national benefits scored most highly.
Other relevant activities are NHS priority disease areas such as cancer, its diagnosis, prevention, treatment and outcomes, communicable and non-communicable diseases or other areas where there is outstanding need or identified health inequalities or disparities. It may also cover public health and patient care pathways. For example, an applicant could seek to demonstrate how they prevented inappropriate emergency department attendance or generated other benefits, such as working with social care providers, Information Commissioner’s Offices (ICOs) or third parties in other ways and how this experience has been shared and implemented elsewhere.
Applicants could include work on delivering wider health policies or their impact related to the NHS Long Term Plan and/or the NHS People Plan, particularly in reference to collaborative working, demonstrating an inclusive culture and the health and wellbeing of NHS staff and their retention in the face of increasing pressures. In all cases, applicants should give details of how they are delivering wider change and the magnitude of any impacts over a defined time period. They may choose to inform us if they are actively involved in a leadership capacity at a regional or national level in the delivery of the COVID-19 backlog plan – clearly defining the impact of their personal contribution.
Applicants may consider providing evidence of the impact on delivering improved joined-up care in line with its recommendations in optimal settings, by implementing new service models or specifically digital innovations or efficiencies across the wider health environments. This is particularly relevant if they have expanded these beyond their immediate area or remit. They may also offer evidence of involvement and leadership in activities and innovations that have been developed in partnership with external partners, which provided positive impacts to the NHS and are in line with the government’s life sciences strategy.
There is also scope for including impacts on outcomes improvement, particularly in areas identified with unmet need or where there is undue national or regional variation in outcomes across the NHS.
This domain could also be used to provide additional evidence that is related to evidence from a prior domain. Applicants should avoid repeating evidence however, as it can only be scored once. They should take the opportunity to demonstrate different aspects of their work that is over and above their job role and how these have had incremental impact.
As an assessor, your priority is to look for evidence of outputs that have had a real impact, rather than activity alone.
Here are examples of high-scoring domain 5 evidence from the 2022 round.
As a member of the NHS England X Clinical Reference Group (2016 to 2022) I develop innovative policies and service specifications to improve current and future care and efficiency in all NHS tertiary services. This includes my detailed work on the NICE COVID-19 rapid guideline for the immunocompromised (May 2020) and the NHS England Multidrug Resistance Policy (2019).
I have jointly overseen X regional clinical management for COVID-19 complications. Since April 2020 the team conducted around 170 emergency consultations across the region.
I have led joint work between UK Clinical Research Facility Directors, the Medicines and Healthcare products Regulatory Agency and the Health Research Authority to develop a national framework for the governance and safe conduct of highest risk phase 1 trials in Clinical Research Facilities and the NHS. This was rolled out during the pandemic for experienced sites to support those without existing phase 1 expertise, expanding NHS and national capability to support public and industry funded new drug and vaccine development.
“I ensure participant safety and effective trial delivery via my roles as:
-
independent chair of the Data Monitoring and Safety Committee (DMSC) for a UK healthy human immune challenge trial
-
independent chair of the COVID-19 vaccine trial steering committee
-
member of the South African COVID-19 booster trial DSMC.”
I developed high quality national guidelines via my membership of the NICE guideline committee for X (2020) and of the international X campaign working party (2018 to 2019). I was one of 3 royal college representatives to the Academy of Medical Royal Colleges’ X Position Statement Working Party (2020 to 2022).
Employer citations primarily serve to confirm that the applicant’s job plan has been agreed, and that they are meeting their contractual obligations as defined in that job plan. We expect confirmation that a consultant has engaged fully with local appraisal processes as required for revalidation by the GMC. We anticipate that all consultants will be supported by their employer. If an employer elects not to provide support, they should indicate why this is the case. A consultant can still apply for an NCIA. This information will be available to you as an assessor in the form and you will have to take a view as to its relevance in the context of the application as a whole.
The person (for example, a trust medical director or senior human resources (HR) manager) who is writing the employer citation may or may not be in a position to comment on the bulk of the nationally or regionally-focused work that an applicant will have included on the form. They may instead focus on local clinical or management activity. This makes employer citations of variable value. A citation that does not mention or endorse an applicant’s national work should not be viewed negatively.
Employers are asked to comment on any disciplinary matters. If these have not concluded we always presume innocence unless it has been proven otherwise. The presence of ongoing disciplinary matters without any sanctions should not affect any scores. ACCIA will determine any action required once the matter is completed.
Assessing applications from less than full time applicants
Consultants working LTFT were eligible to apply for ACCEA awards under that scheme. Many high quality applications were received with a high success rate, although the payment for these awards was pro-rated in proportion to the number of programmed activities worked. Under the ACCIA scheme, LTFT consultants are still eligible, however if successful, the award will be paid at the full level – N1, N2 or N3. To qualify, a consultant must have a contract that incorporates a minimum of 3 clinically-relevant PAs.
If a consultant is working LTFT and in a transition provision from a national CEA based on legacy award values, they will receive a pro-rated award (see part 1).
Consultants elect to work LTFT for a range of reasons, personal and professional. NCIA does not require an applicant to indicate why they have chosen to do so. However, where there are extenuating circumstances, for example ill-health, that have precipitated the need to work LTFT, an applicant may choose to inform NCIA directly, and/or mention these on their form in their job plan, personal statement or in a relevant domain (see part 1).
We advise you to look carefully at the job plan for all applicants – this is particularly important for LTFT applicants in order to help you decide if the contributions described in the domains on the form (clinical and/or academic) are over and above what might be expected.
You are also advised to pay careful attention to applications where a consultant’s circumstances and job plan have changed during the course of the 5 year assessment period, perhaps working part of the period LTFT, and part full-time. Applicants are strongly encouraged to be precise about the timing of such changes in working pattern and to provide dates for the achievements that they are presenting for assessment.
Annex A: ACCIA scoring process 2023
Diagram 1: scoring process 2023
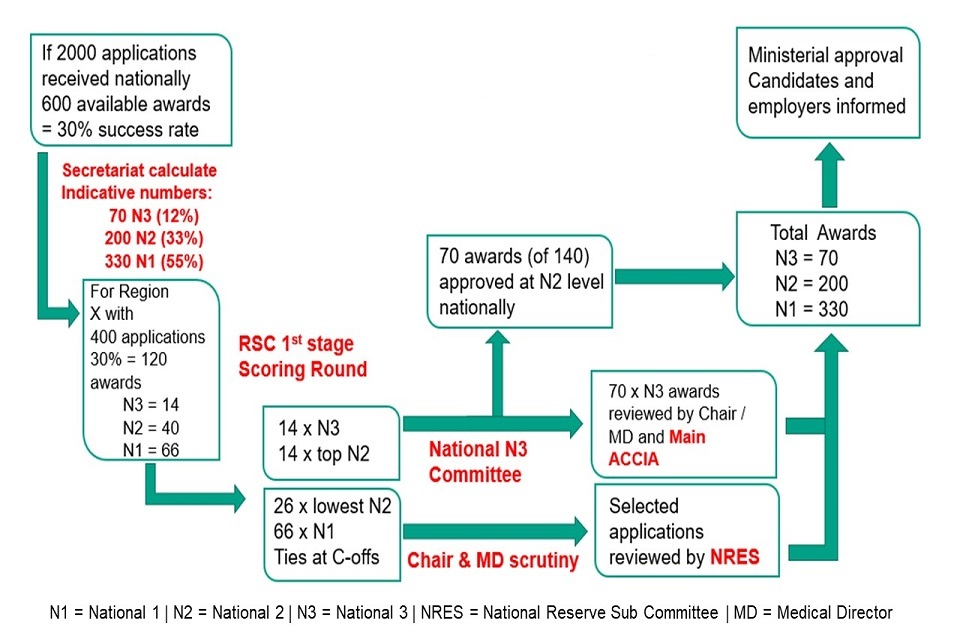
flow chart
The flow chart sets out an example of how the scoring process might look if there are 600 awards available.
First, the secretariat would calculate indicative numbers. These would then be split by region proportionate to the number of applications received. At this stage regional sub-committee scoring will take place.
Then all the available National 1 awards and the top proportion of National 2 awards will go to the National N3 Committee for scrutiny. Meanwhile the lowest National 2 awards and all National 1 awards will be sent for scrutiny by the chair and medical director.
Once the chair and medical director scrutiny and National 3 committee review has taken place, all National 1 and National 2 awards should be approved, bar a select few submitted to the National Reserve sub-committee.
The remaining National 3 awards will simultaneously be reviewed by the chair, medical director and ACCIA main committee. Once all these processes are complete the awards will be decided. The final list of successful applicants will be sent for ministerial approval.
