Work, health and disability green paper: improving lives
Updated 30 November 2017
Ministerial foreword
From Damian Green, Secretary of State for Work and Pensions and Jeremy Hunt, Secretary of State for Health
This government is determined to build a country that works for everyone. A disability or health condition should not dictate the path a person is able to take in life – or in the workplace. What should count is a person’s talents and their determination and aspiration to succeed.
However, at the moment, for many people, a period of ill health, or a condition that gets worse, can cause huge difficulties. For those in work, but who are just managing, it can lead to them losing their job and then struggling to get back into work. Unable to support themselves and their family, and without the positive psychological and social support that comes from being in work, their wellbeing can decline and their health can worsen. The impact of this downward spiral is felt not just by each person affected and their families, but also by employers who lose valuable skills and health services that bear additional costs. There is a lack of practical support to help people stay connected to work and get back to work. This has to change.
We know that the right type of work is good for our physical and mental health and good health and support helps us in the workplace. We know that we must protect those with the most needs in society. We need a health and welfare system that recognises that – one that offers work for all those who can, help for those who could and care for those who can’t.
The UK has a strong track record on disability rights and the NHS provides unparalleled support to people with poor health. We have put mental and physical health on the same footing. We have seen hundreds of thousands more disabled people in work in recent years. However, despite that progress, we are not yet a country where all disabled people and people with health conditions are given the opportunity to reach their potential. That’s why we are committed to halving the disability employment gap and share this commitment with many others in society.
We are bold in our ambition and we must also be bold in action. We must highlight, confront and challenge the attitudes, prejudices and misunderstandings that, after many years, have become engrained in many of the policies and minds of employers, within the welfare state, across the health service and in wider society. Change will come, not by tinkering at the margins, but through real, innovative action. This Green Paper marks the start of that action and a far-reaching national debate, asking: ‘What will it take to transform the employment prospects of disabled people and people with long-term health conditions?’
This government is committed to acting but we can’t do it alone. Please get involved. Let’s ensure everyone has the opportunity to go as far as their talents will take them – for a healthier, working nation.
Work, health and disability: facts and figures
Evidence shows that appropriate work is good for our health. Good work leads to good health, and good health allows for good work. Also, worklessness leads to poor health, and poor health often leads to worklessness.
Reducing long term sickness absence is a priority 1.8 million employees on average have a long-term sickness absence of 4 weeks or more in a year.
Access to timely treatment varies across areas. Average waiting times for mental health treatment can differ by as much as 12 weeks across England and some evidence suggests treatment for musculoskeletal conditions can differ by as much as 23 weeks.
Ill-health among working age people costs the economy £100 billion and sickness absence costs employers £9 billion a year
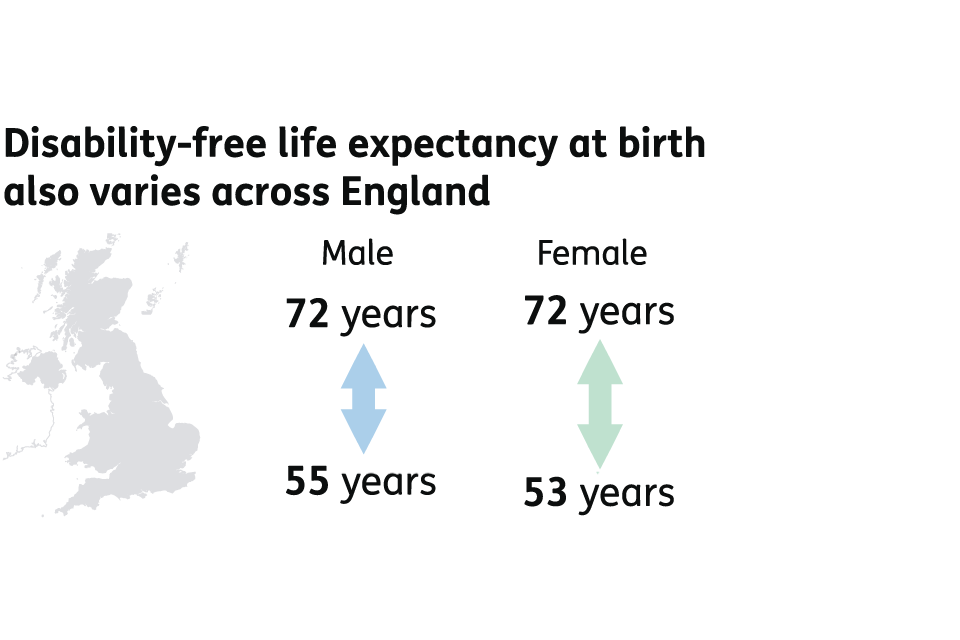
Disability-free life expectancy at birth also varies across England. For men, disability-free life expectancy can range from 55 to 72 years. For women, disability-free life expectancy can range from 53 to 72 years.
Only around 3 in 100 of all Employment and Support Allowance claimants leave the benefit each month.
Disability has been rising over 400,000 increase in the number of working age disabled people in the UK since 2013 taking the total to more than 7 million.
Compared to non-disabled people, disabled people are less likely to enter employment, so preventing them from leaving work is important. Between two quarters of a year, as many as 150,000 disabled people leave employment.
8% of employers report they have recruited a person with a disability or long term health condition over a year.
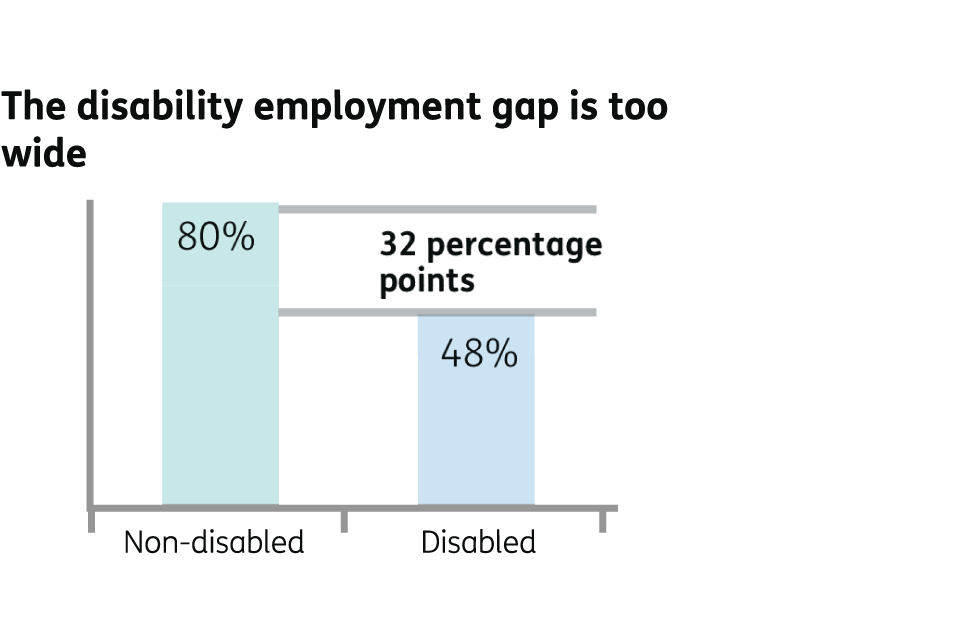
The disability employment gap is too wide. 80 per cent of non-disabled people are in employment, compared to 48 per cent of disabled people. That is a difference of 32 percentage points.
Executive summary
1) Employment rates amongst disabled people reveal one of the most significant inequalities in the UK today: less than half (48%) of disabled people are in employment compared to 80% of the non disabled population. [footnote 1] [footnote 2] Despite a record-breaking labour market, 4.6 million disabled people and people with long-term health conditions are out of work [footnote 3] leaving individuals, and some large parts of communities, disconnected from the benefits that work brings. People who are unemployed have higher rates of mortality [footnote 4] and a lower quality of life. [footnote 5] This is an injustice that we must address.
2) This green paper sets out the nature of the problem and why change is needed by employers, the welfare system, health and care providers, and all of us. We consider the relationship between health, work and disability. We recognise that health is important for all of us, that it can be a subjective issue and not everyone with a long-term health condition will see themselves as disabled. [footnote 6] We set out some proposed solutions and ask for your views on whether we are doing the right things to ensure that we are allowing everyone the opportunity to fulfil their potential.
The nature of the problem
3) Making progress on the government’s manifesto ambition to halve the disability employment gap is central to our social reform agenda by building a country and economy that works for everyone, whether or not they have a long-term health condition or disability. It is fundamental to creating a society based on fairness: people living in more disadvantaged areas have poorer health and a higher risk of disability. It will also support our health and economic policy objectives by contributing to the government’s full employment ambitions, enabling employers to access a wider pool of talent and skills, and improving health.
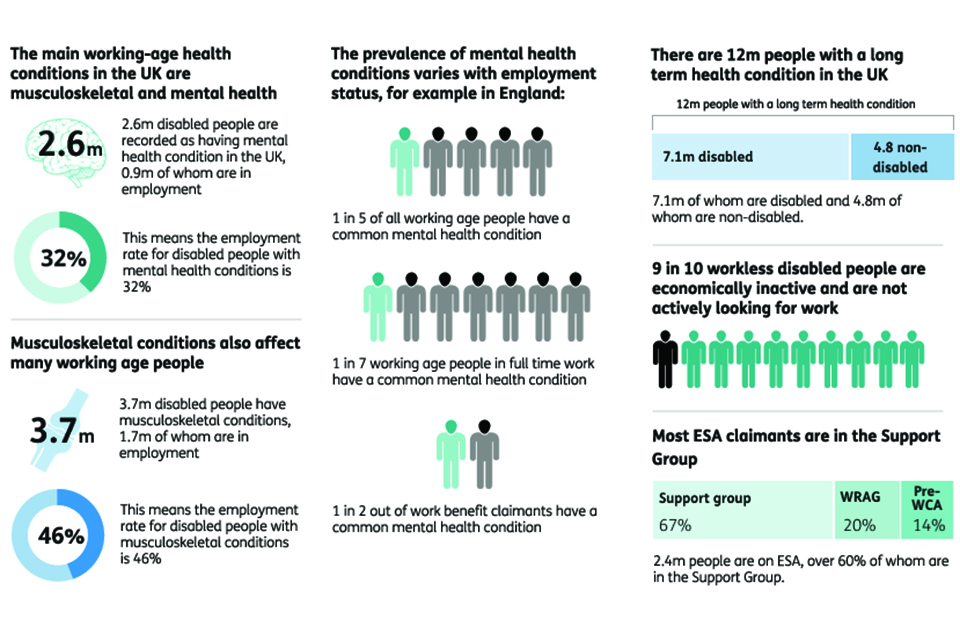
4) Almost 1 in 3 working-age people in the UK have a long-term health condition which puts their participation in work at risk. [footnote 7] Around 1 in 5 of the working-age population has a mental health condition. [footnote 8] As many as 150,000 disabled people who are in work one quarter are out of work the next. [footnote 9] Over half (54%) of all disabled people who are out of work experience mental health and/or musculoskeletal conditions as their main health condition. [footnote 10] It is evident that our health and welfare systems are struggling to provide meaningful support, and, put simply, the system provides too little too late. Too many people are falling into a downward spiral of declining health and being out of work, denying them the benefits that employment can bring, creating pressures on the NHS and sustaining a major injustice in our society.
5) Over 3.3 million disabled people are now in work. [footnote 11] Yet many disabled people experience expectations that are too low, employers who can be reluctant to give them a chance, limited access to services and a welfare system that does not provide enough personalised and tailored support to help people into work and to stay in work. Too many people experience a fragmented and disjointed system which does little to support their ambitions of employment, and indeed can erode those ambitions.
6) The evidence that appropriate work can bring health and wellbeing benefits is widely recognised. [footnote 12] Employment can help our physical and mental health and promote recovery. But the importance of employment for health is not fully reflected in commissioning decisions and clinical practice within health services, and opportunities to support people in their employment aspirations are regularly lost. Once people are on benefits, their chances of returning to work steadily worsen. There are systemic issues with the original design of Employment and Support Allowance with 1.5 million people now in the Support Group [footnote 13] who are treated in a one-size-fits-all way and get little by way of practical support from Jobcentres to help them into work. This consultation seeks to address these issues, exploring new ways to help people, but does not seek any further welfare savings beyond those already legislated for.
Areas for action
7) These challenges are complex and pressing. Our vision is to create a society in which everyone has a chance to fulfil their potential, where all that matters is the talent someone has and how hard they are prepared to work. We are determined to remove the long-standing injustices and barriers that stop disabled people and people with health conditions from getting into work and getting on, preventing them from being whatever they want to be. We are also determined to bring a new focus to efforts to prevent health conditions from developing and worsening, helping more people to remain in work for longer.
We want to:
- ensure that disabled people and people with long-term health conditions have equal access to labour market opportunities and are given the support they need to prevent them from falling out of work and to progress in workplaces which embed effective health and wellbeing practices
- help employers take action to create a workforce that reflects society as a whole and where employers are equipped to take a long-term view on the skills and capability of their workforce, managing an ageing workforce and increased chronic conditions to keep people in work, rather than reacting only when they lose employees
- ensure people are able to access the right employment and health services, at the right time and in a way which is personalised to their circumstances and integrated around their needs
- more effectively integrate the health and social care and welfare systems to help disabled people and people with long-term health conditions move into and remain in sustainable employment
- put mental and physical health on an equal footing, to ensure people get the right care and prevent mental illness in the first place
- invest in innovation to gain a better understanding of what works, for whom, why and at what cost so we can scale promising approaches quickly
- change cultures and mind-sets across all of society: employers, health services, the welfare system and among individuals themselves, so that we focus on the strengths of disabled people and what they can do
8) Taken together, this will mean the ambitions of disabled people and people with health conditions, their aspirations and their needs, are supported by more active, integrated and individualised support that wraps around them. This will help improve health and wellbeing, benefit our economy and enable more people to reach their potential.
9) To make early progress we are:
- working jointly across the whole of government: this green paper is jointly prepared by the Department of Health and the Department for Work and Pensions, working closely with the Department for Communities and Local Government, the Department for Business, Energy and Industrial Strategy, NHS England, Public Health England, local government, and other partners
- significantly improving our employment support: for example, expanding the number of employment advisers in talking therapies and introducing a new Personal Support Package offering tailored employment support which Jobcentre Plus work coaches will help disabled people or people with health conditions to access
- working with health partners such as NHS England, Public Health England, the National Institute for Health and Care Excellence, Health Education England, the Royal Colleges and regulators to embed evidence into clinical practice and support training and education across the NHS workforce
- investing £115 million of funding to develop new models of support to help people into work when they are managing a long-term health condition or disability. We will identify and rapidly scale those which can make a difference, while weeding out less promising approaches
10) We will not be satisfied with this, and further action needs to be sustained across all sectors. In this green paper we ask:
- how big a role can we expect employers to play in ensuring access to opportunities for disabled people, and how can the ‘business case’ for inclusive practices be strengthened? What is the best way to influence employers to support health and wellbeing in the workplace, both to ensure the effectiveness of their workforce and avoid employment practices which can negatively impact health? How can we prevent sickness absence resulting in detachment from the labour market?
- how can work coaches play a more active role for disabled people and people with health conditions? How can we build their skills and capabilities to support a diverse group with complex needs, build their mental health awareness, and develop a role in personalising support and helping individuals navigate a complex system?
- how can we improve a welfare system that leaves 1.5 million people – over 60% of people claiming Employment and Support Allowance [footnote 14] – with the impression they cannot work and without any regular access to employment support, even when many others with the same conditions are flourishing in the labour market? How can we build a system where the financial support received does not negatively impact access to support to find a job? How can we offer a better user experience, improve system efficiency in sharing data, and achieve closer alignment of assessments?
- how can we promote mental and physical health and ensure that people have timely access to the health and employment support that they need rather than struggling to access services (particularly musculoskeletal and mental health services)? How do we make sure that health and employment service providers provide a tailored and integrated service, and that the important role of employment is recognised?
- how can we develop better occupational health support right across the health and work journey?
- what will it take to reinforce work as a health outcome in commissioning decisions and clinical practice? How can we ensure good quality conversations about health and work, and improve how fit notes work?
- how can we best encourage, harness and spread innovation to ensure that commissioners know what works best in enabling disabled people and people with health conditions to work?
- perhaps most crucially, how can we build a culture of high hopes and expectations for what disabled people and people with long-term health conditions can achieve, and mobilise support across society?
11) This challenge is not one that will be solved quickly, but we know that to build a country that works for everyone, we must address issues with a long-term return. This is why we have a 10-year vision for reform, the foundations of which we have set out at the end of this consultation. Where we are certain of our ground we will act quickly, making the changes we know are needed. But we will also look to the long term, investing in innovation to understand what is most effective and reshaping services where they are needed.
Your views
12) The consultation on the proposals in this green paper is an important part of building a shared vision and achieving a real change in culture. We want to launch a discussion around how we can best support disabled people and people with long-term health conditions to get into, and to stay in, work. We want to bring together wide-ranging expertise, opinions and experiences. Over the coming months we will talk to disabled people and people with long-term conditions, their families and carers, health and social care professionals, their representative bodies, local and national organisations, employers, charities and anyone who, like us, wants change.
13) We recognise that the devolution administrations are important partners, particularly because of their responsibilities for health as a devolved matter and other related areas. The government is committed to working with the devolved administrations to improve the support accessible to disabled people and people with health conditions across the country at a national, local and community level.
14) Please let us know what we need to improve so that we can build a plan that will bring real and lasting change. You can:
Respond to this consultation online
Email us at workandhealth@dwp.gsi.gov.uk
Write to us at:
The Work, Health and Disability consultation,
Ground Floor,
Caxton House,
6-12 Tothill Street,
London,
SW1H 9NA
The consultation will run until Friday 17 February 2017.
15) We are committed to tackling the injustice of disability employment, so that all can share in the opportunities for health, wealth and wellbeing that the UK has to offer and where everyone has the chance to go as far as their talents will take them.
Definition of disability and long-term health conditions used in this paper:
- The Equality Act 2010 [footnote 15] defines a disabled person as someone who has a physical or mental impairment which has a substantial and long-term adverse effect on their ability to carry out normal day-to-day activities. ‘Long-term’ is defined as lasting or expecting to last for at least 12 months
- health can be a subjective issue – we know that the way people think about their health is diverse and that not everyone that meets the Equality Act definition would consider themselves to be disabled. But we follow the Equality Act definitions in this paper, so:
- an individual is considered in this paper as having a long-term health condition if they have a physical or mental health condition(s) or illness(es) that lasts, or is expected to last, 12 months or more.
- if a person with these condition(s) or illness(es) also reports it reduces their ability to carry out day-to-day activities as well, then they are also considered to be disabled
- this means some people who may have a long-term health condition will be grouped together with those people who do not have any long-term health condition and be considered as non disabled. We recognise that long-term health conditions can fluctuate and the effects of a condition on an individual’s day-to-day activities may change over time
- incapacity Benefits refers to Employment and Support Allowance and its predecessors Incapacity Benefit, Income Support on grounds of disability and Severe Disablement Allowance
1: Tackling a significant inequality – the case for action
Chapter summary
In this chapter we set out the injustice of the disability employment gap. We explore how:
- being in work can help an individual’s health and wellbeing
- systemic issues hold back too many disabled people and people with health conditions
- we need to learn from what works and develop innovative approaches
- we need to work beyond artificial boundaries and work with everyone to achieve our shared vision
Being in work can help an individual’s health and their overall wellbeing
16) This government is committed to helping everyone, whoever they are, enjoy the independence, security and good health that being in work can bring, giving them the chance to be all they want to be.
17) The evidence is clear that work and health are linked. Appropriate work is good for an individual’s physical and mental health. Being out of work is associated with a range of poor health outcomes. [footnote 16] Academics and organisations such as the WHO, [footnote 17] the ILO, [footnote 18] the OECD, [footnote 19] RAND Europe, [footnote 20] the Royal College of Psychiatrists [footnote 21] and NICE [footnote 22] all recognise that work influences health and health influences work. The workplace can either support health and wellbeing and the health system can actively support people into work in a virtuous circle or the workplace can be unsupportive and health and work systems can work against each other.
18) We know that the longer a person is out of work the more their health and wellbeing is likely to deteriorate. [footnote 23] So, every day matters. For every week, every month, every year someone remains outside the world of work, it is increasingly more difficult for them to return and their health and wellbeing may worsen as a result. We must address this downward spiral.
19) Of course, work can also bring a range of other benefits which support mental and physical health and wellbeing. [footnote 24] It is the best route to raising the living standards of disabled people and people with a long-term health condition and moving them out of poverty. [footnote 25] But a good standard of living is about more than just income. [footnote 26] Work can help someone to be independent in the widest sense: having purpose, self-esteem, and the opportunity to build relationships. Being in the right job can be positively life changing.
20) But, whilst work is good for health in most circumstances, the type of work matters. Many factors such as autonomy, an appropriate workload and supportive management are important for promoting health at work. [footnote 27] These factors can be very personal.
21) As many stakeholder organisations like Scope have highlighted, many disabled people and people with long-term health conditions already work and many more want to access all the benefits that work can bring. [footnote 28] We want to understand how to improve the current system of support to make this aspiration a reality. We also recognise that some disabled people and people with health conditions might not be able to work due to their condition, whether in the short or long term. This government is committed to ensuring that they are fully supported by the financial safety net that the welfare system provides and so this consultation does not seek any further welfare savings beyond those in current legislation.
…and there’s quite significant benefits associated with work over and above the financial benefit of working, the social aspects of it, things to do with people’s self-esteem, so trying to keep people plugged into that is very important for their overall health.” [footnote 29] - General Practitioner
I don’t have to work financially, but I want to… self-confidence, self-worth….” [footnote 30] - Individual
Closing the disability employment gap to tackle injustice and build our economy
See appendix for full description of this image: Population characteristics
22) This government is committed to building a country and an economy that work for everyone. The UK employment rate is the highest it has been since records began. Over 31 million people (nearly 75% of the working age population) are in employment. [footnote 31] However, while there has been an increase of almost half a million disabled people in employment over the last 3 years, there are still fewer than 5 in 10 disabled people in employment compared with 8 in 10 non-disabled people. [footnote 32] This disability employment rate gap, the difference between the employment rates of disabled and non-disabled people, has not changed significantly in recent years and now stands at 32 percentage points. [footnote 33] [footnote 34]
23) So 3.8 million disabled people are out of work despite a record breaking labour market. [footnote 35] People with particular health conditions can be disadvantaged, for example only 32% of people with mental health conditions are in employment. This leaves people, and in some places entire communities, disconnected from the benefits that work can bring. This is one of the most significant inequalities in the UK today and the government cannot stand aside when it sees social injustice and unfairness. That is why we have set ourselves the ambition to halve the disability employment gap.
24) This ambition is not only about tackling an unacceptable injustice for individuals. The disability employment gap also represents a waste of talent and potential which we cannot afford as a country: poor health and unemployment results in substantial costs to the economy.
25) The cost of working age ill health among working age people is around £100 billion a year. [footnote 36] The majority of this cost arises from lost output among working age people with health conditions not being in paid work. Economic inactivity costs government around £50 billion a year, including £19 billion of welfare benefit payments and lower tax revenues and national insurance contributions. The NHS also bears £7 billion of additional costs for treating people with conditions that keep them out of work. [footnote 37] And there is also a cost to employers: sickness absence is estimated to cost £9 billion per year. [footnote 38] And, of course, there is a cost to people and their families.
Action is needed now to prevent this situation getting worse
26) We have seen that the costs, to the individual and the economy, of the disability employment gap are already unacceptably high. Trends in demography and population health mean that we need to take action now to prevent these costs rising further.
27) Older people will make up a greater proportion of the workforce in the future. Between 2014 and 2024 the UK will have 200,000 fewer people aged 16 to 49 but 3.2 million more people aged 50 to State Pension age. [footnote 39] Older workers can bring great benefit to businesses and drawing on their knowledge, skills and experience may help businesses to remain competitive and to avoid skills and labour shortages.
28) We also know that while life expectancy at birth has been increasing year on year, changes in healthy life expectancy have not consistently been keeping pace: we are living longer lives but some more years in ill health. [footnote 40] There is a known correlation between an ageing population and an increasing prevalence of long-term chronic conditions and multiple health issues.
29) We know that the world of work is changing. For example, new information and communication technologies have changed the nature of work tasks. This change may bring benefits, for example enabling more flexible working to help people with health conditions stay in work, but can also have less positive effects like work intensification that may affect people’s ability to cope or adapt in work with a health condition. [footnote 41]
30) The impact of poor health on work is not inevitable for people at any age. For example, advances in technology can assist people to remain in work where they might have been previously unable to do so. Lifelong learning can also offer the opportunity for people to gain new skills to change roles if they develop a health condition or disability, or an existing one worsens. [footnote 42] And while many conditions are not preventable, the evidence is clear that the way we live our lives can influence health outcomes. Currently, 6 out of 10 adults are overweight or obese, [footnote 43] nearly 1 in 5 adults still smoke, [footnote 44] and more than 10 million adults drink alcohol at levels that pose a risk to their health. [footnote 45] Public health interventions form a vital part of the health and work agenda to help reduce the prevalence of conditions that can lead to people leaving the labour market due to ill health.
Case study – Susannah
Susannah was diagnosed with osteoarthritis and rheumatoid arthritis in 2010, she had lived with symptoms for more than 6 months before getting a formal diagnosis. She has lived a very active life and was working on a farm in France at the time of diagnosis. Following diagnosis, Susannah returned to the UK and now works as the personal assistant at a country house and estate.
Upon receiving her diagnosis, her employer was quite understanding of the impact rheumatoid arthritis was having on her. Her manager spoke with the HR team who provided her with reasonable adjustments to her workplace. Fatigue is also major issue for Susannah, as with many others with rheumatoid arthritis, she feels very tired after a day at work and this limits her from socialising in the evenings or at weekends. Nevertheless, she admits she does have some difficulties with her workload but she does not feel comfortable asking her employer for further adjustments to it.
In light of her current difficulties she is planning to retire early, having originally planned to retire at 66. She says she has accumulated enough earnings to have a reasonable retirement. When asked if anything could accommodate her to remain in work and thus not retire, she says working 3 days rather than 4 would probably be sufficient, however, she says this would amount to a job share which would be impractical for her employer and something she is not prepared to ask for.
Retiring early isn’t ideal and I would like to keep on working but I just can’t perform all of the roles of the job anymore and my work-life balance has suffered due to my tiredness and pain at the end of each day. I don’t see my friends much anymore and it’s something I really miss. If I could work a 3-day week I could probably carry on, but I don’t feel that is something which could be accommodated. Before my diagnosis I never contemplated having to retire early but now I see it as almost inevitable.
– Provided by National Rheumatoid Arthritis Society
Underlying factors play an important role
31) To reduce the disability employment gap, we need to understand the reasons why disabled people might be unable to enter or stay in work, and to recognise the wide variety of conditions and circumstances they face. The disability employment gap is affected by a number of factors, for example people frequently move in or out of disability and employment over time. It is therefore important to look at a wider group of work and health indicators to allow us to better understand the wider picture. The Work, Health and Disability Green Paper Data Pack accompanying this publication includes more statistics about the disability employment gap.
32) Almost 12 million working age people in the UK have a long-term health condition, and of these 7 million are disabled. [footnote 46] A health condition does not, in itself, necessarily prevent someone from working. Indeed people with a long-term health condition who are not reported as being disabled have a very similar employment rate to people without any type of health condition – around 80%. [footnote 47] However, employment rates are much lower among disabled people with only 48% in work. [footnote 48]
33) This suggests that it is important to try to prevent long-term health conditions developing or worsening to the extent that they are disabling. We know that a person’s health is affected by the conditions and environments in which they live. Fair Society, Healthy Lives [footnote 49] provided evidence that the conditions in which people are born, live, work and age, are the fundamental drivers of health and health inequalities. Where people live can have a big impact on both health and employment outcomes. In England, men born in the most deprived areas can expect 9.2 fewer years of life, and 19.0 fewer years of life lived in good health than people in the least deprived areas. For women the equivalent figures are 7.0 and 20.2 years. [footnote 50]
34) We also know that disabled people from more disadvantaged backgrounds are more likely to be out of work. For example, while employment rates can be as low as 16% for people with mental health conditions who live in social housing, for disabled people who live in a mortgaged house and who have 1 or 2 health conditions, the employment rate is as high as 80%. [footnote 51] This is similar to the overall employment rate for non-disabled people. [footnote 52]
35) In addition to the strong links between socio-economic disadvantage and poorer work and health outcomes, other factors can also be significant. Attitudes in society can have a significant impact: for example, people may have lower expectations of disabled people and people with health conditions, which may impact on whether an individual feels able to work. There may also be physical barriers to employment for some disabled people and people with long-term health conditions, such as difficulties accessing transport and buildings.
36) We also need to recognise that some disabled people or people with long-term health conditions may face other disadvantages associated with worklessness. They may need a wide range of support, through different agencies working in partnership, to address all of the connected and overlapping problems they face. These might include drug or alcohol addiction, a criminal record, homelessness or caring responsibilities for young children. We recognise that these are complex problems, requiring a focused look at the factors that stand in the way of employment for these groups, which is why the government has asked Dame Carol Black to conduct an independent review into the impact on employment outcomes of alcohol or drug addiction, and obesity.
37) Although factors unrelated to an individual’s health condition or disability have a significant impact on their ability to work, there do appear to be some patterns in employment rates for people with certain conditions, or for those who have multiple conditions. For example, disabled people with mental health conditions have an employment rate of just 32%, which is significantly below the overall employment rate for disabled people at 48%. [footnote 53] People who have more than one condition are also more likely to be out of work – disabled people with one long-term health condition have an employment rate of 61%, but the 1.2 million disabled people who have 5 or more long-term health conditions have an employment rate of just 23%. [footnote 54]
38) Of course not all health conditions are static. Many, such as some mental health conditions, fluctuate over time, and affect people differently at different times. What is clear, though, is that once someone is out of work due to a health condition and claims Employment and Support Allowance their chance of finding work is slim. Only around 3 in 100 of all people receiving Employment and Support Allowance stop receiving the benefit each month, and not all of these people return to work. [footnote 55] While the government recognises that some people will not be able to work and rightly need to receive financial support, for others this starts a journey away from work which can make their health problems worse and, in turn, negatively impact upon their employment prospects.
39) It is impossible to address this complex picture with a simple, one-size-fits-all solution. We need to change our attitudes and behaviours towards disabled people and people with health conditions, working with everyone from employers to schools, health professionals to community groups. We need to develop a more personalised and integrated system that puts individuals at the centre, and gives all individuals the chance to prosper and play their part in a country and an economy that works for everyone.
Tackling the systemic issues
40) The disability employment gap has persisted over many years and its causes are long-term, systemic and cultural. Efforts to help disabled people and those with long-term health conditions have been hindered by a lack of vision and by systems which fail to join up and take people’s needs properly into account.
41) A number of systemic issues hold back too many disabled people and people with health conditions:
- employees are not being supported to stay healthy when in work, and to manage their health condition to stop them falling out of work: in one report, mental ill health at work was estimated to cost businesses £26 billion annually through lost productivity and sickness absence [footnote 57]
- too many disabled people and people with long-term health conditions are being parked on financial support alone: over 60% of people on Employment and Support Allowance do not have access to integrated and personalised employment and health support which focuses on what they can and want to do
- individuals are not getting access to the right support and treatment: for example, some evidence suggests that waiting times for musculoskeletal services can vary from between 4 to 27 weeks [footnote 58]
- the health and welfare systems do not always work well together to join up around an individual’s needs and offer personalised and integrated support to help them manage their condition.
42) Our strategy is to provide support centred on the disabled person or person with a health condition. Disabled people and people with health conditions are the best judges of what integrated support they need to secure work or stay and flourish in work. To do this, we want to align systems better so that we can make a real difference to people’s health and work prospects. In this green paper we explore how we can encourage employers, the welfare system and health services to take a more joined-up approach to health and work:
- how we can encourage employers to be confident and willing to recruit disabled people, to put in place approaches to prevent people from falling out of work, and to support effectively those employees on a period of sickness absence to encourage their return to work
- how we can create a welfare system that provides employment support in a more personalised and tailored way, with a simpler and more streamlined process for those with the most severe health conditions
- how we can create a health system where work is seen as a health outcome and where all health professionals are sufficiently trained and confident to have work-related conversations with individuals to increase their chances of maintaining or returning to employment
- how we can better integrate occupational health type support with other services to ensure more holistic patient care
43) We also need to look beyond ‘systems’ to look at the important role played by individuals, carers and the voluntary and community sectors.
The role of individuals
44) Disabled people, people with long-term health conditions and those who may develop them are at the heart of our strategy. We want to deliver services which enable people to have more information about their care and support, be better able to manage any health conditions, and have more say in the health and employment support they may need. The patients’ organisation National Voices puts it clearly: personalised care will only happen when services recognise that patients’ own life goals are what count; that services need to support families, carers and communities; that promoting wellbeing and independence need to be the key outcomes of care; and that patients, their families and carers are often ‘experts by experience’. [footnote 59]
45) Individuals can also support employers to make workplaces more inclusive by working in partnership with them to deliver changes in recruitment and retention practices and promoting a healthy work culture.
The role of carers
46) This government recognises that carers can play a fundamental role in enabling disabled people and people with long-term health conditions to be all they want to be. The support of carers can be crucial in supporting disabled people and people with a long-term health condition to return to or remain in work. According to a report from 2009, [footnote 60] as many as 3 million people combine paid work with providing informal care to family and friends who might have a range of physical or learning disabilities, or who may have long-term health conditions related to ageing.
47) Carers UK recently found that carers in England are ‘struggling to get the support they need to care well, maintain their own health, balance work and care, and have a life of their own outside of caring.’ The challenges of balancing paid work with a caring role can mean that carers have to reduce their working hours, pass up career opportunities, or leave employment altogether: an estimated 2 million people have given up paid work to care. [footnote 62] Of these, there are currently 315,000 working age adults who, having left work to care, remain unemployed after their caring role has ended. These impacts are felt disproportionately by older workers, with around 1 in every 6 economically inactive people aged between 50 and State Pension age citing caring responsibilities as the reason for inactivity. [footnote 63]
48) Many of the challenges faced by carers in balancing their work and caring roles stem from the same issues faced by workers who are themselves disabled or have a long-term health condition, for example a risk-averse attitude among employers to recruiting disabled people and caring responsibilities, and a lack of flexible working arrangements in many organisations. Changing attitudes and behaviours towards disabled people and people with long-term health conditions should also have a positive impact on carers, but there is more to be done.
49) The government is committed to supporting carers. A key objective of our future work will be to support carers of all ages to enter, remain in and re-enter work. The government’s Fuller Working Lives programme focuses on the challenges for older workers to remaining in or returning to work due to caring responsibilities, ill health or disability. As part of the programme a series of Carers in Employment pilots was launched in April 2015, to help support carers to stay in work or return to paid work alongside their caring responsibilities. Early next year the government will publish a new, cross-government and employer-led national strategy, which will set out the future direction of this Fuller Working Lives agenda.
The role of the voluntary and community sectors, local authorities and other local partners
50) We recognise that the voluntary and community sectors play a crucial role in helping more people to lead healthy and fulfilling lives, and that there are many organisations from these sectors, with broad reach and diversity, working to support and involve disabled people and people with long term health conditions. These voluntary and community organisations embody a spirit of citizenship upon which our country is built, and we want to better harness their expertise and capacity in order to achieve the best outcomes for disabled people and people with long-term health conditions.
51) As a government, we are already working to invest in, and partner with, the voluntary and community sectors, including:
- the Department of Health, NHS England and Public Health England, working closely with the sectors, have published a co-produced review of investment and partnerships in the sector. The review contains a range of recommendations for the department, the wider health and care system and the sectors. From this review, work is underway to progress recommendations and to promote more integrated working between the statutory and voluntary sectors to improve health and wellbeing outcomes
- the Office for Civil Society is providing £20 million of funding through its Local Sustainability Fund, to help voluntary, community and social enterprise organisations review and transform their operating models to develop more sustainable ways of working
- the National Citizen’s Service is a programme open to all 16 and 17-year-olds in England, giving them the opportunity to develop the skills and attitudes needed to engage with their local communities and become active and responsible citizens
52) When it comes to unlocking the potential of disabled people and people with long-term health conditions, we want to build on these strong foundations, as well as on the many successful programmes and initiatives led by the voluntary and community sectors themselves, to deliver real change.
53) By being close to their users, charities have ‘a unique perspective on their needs and how to improve services’. [footnote 64] As advocates and providers of services, the voluntary and community sectors form an essential part of achieving lasting change and bringing about a new approach to work and health support. The voluntary and community sectors can help drive change by speaking out for people and their needs, both to the public sector and wider society. The sectors also have an important role in service delivery and have already demonstrated successful programmes such as peer support programmes and mentoring networks, which help people understand and manage their disabilities and health conditions, and explore ways to get into and remain in work. We want to build on these strong foundations to deliver real change.
54) Part of the reason the voluntary and community sectors are so important is because of their links with and reach within their local communities. Evidence shows that employment outcomes for disabled people and people with long-term health conditions vary across different regions in the country. [footnote 65] There are significant opportunities to advance this agenda through a ‘place-based’ approach, unlocking the political capital and resources needed to drive innovation and deliver the system-wide response needed to improve outcomes and local growth. It is also important that employment support for those furthest from the labour market plays an active role in helping people get back to work and unlocking productivity in places. Approaches to integrating work and health provision should draw on the strategic intelligence of Local Enterprise Partnerships and building on the existing strengths of local employers. Better outcomes for disabled people and people with long-term health conditions will require a concerted partnership between communities, central government departments, local authorities, Local Enterprise Partnerships, local providers, and devolution partners.
55) Ultimately, stronger engagement, partnership and co-production with the voluntary and community sectors forms a central part of our work if we are to reach disabled people and people with long term health conditions within their local communities, better understand their experiences with services, listen fully to what they as individuals want to achieve, and offer them support that is rounded, tailored and easily accessible.
The role of the devolved administrations
56) We recognise that services and support for disabled people and people with long-term health conditions needs to join up more effectively and holistically around the needs of the individual. Devolution, with the ability it brings to make decisions and formulate policy at a localised level, plays a key part in this ambition. The devolved administrations are important partners in developing appropriate local solutions, particularly because of their responsibilities for health as a devolved matter. The government is committed to working with the devolved administrations and devolution deal areas to improve the support accessible to disabled people and people with health conditions across the country at a regional, local and community level.
Case study: Working with deaf children
I lost my hearing progressively from early childhood and as it deteriorated it became harder to participate and I felt increasingly isolated and dependent. I became acutely aware that people had different expectations of me because I was deaf. However, I didn’t see myself, or my capabilities, as any different from my hearing friends. “I struggled in the workplace as I was increasingly unable to use the phone and found meetings challenging. I was fortunate to have excellent support from colleagues that I worked with in the civil service and from speech to text reporters, made possible by the government’s Access to Work scheme. In 2006, I had cochlear implant surgery and thanks to the technology and the habilitation support that I received afterwards, I was able to ‘re-enter’ the hearing world, grow my confidence at work and in social situations. This enabled me to have a successful career in the senior civil service.
The speech and language therapists at St Thomas’ Hospital in London provided me with the support to make sense of the new sounds that I was able to access through my hearing technology. Without such support, I would not benefit from the investment that the NHS makes in these wonderful devices. Habilitation is key.
I am now Chief Executive of a charity that works with deaf children and their families to provide critical support in the early years of their lives. This includes enabling them to develop the listening and spoken language skills that gives them an equal start at school and enables them to access the same opportunities in life as their hearing peers. Auditory verbal therapy is a parent coaching programme delivered by highly specialist speech and language therapists who have undergone an additional 3 years of training in auditory verbal practice. Our oldest graduates of the programme are now entering the world of university and work – equipped with the skills to succeed.
– Anita Grover, Chief Executive, Auditory Verbal UK. Provided by the Royal College of Speech and Language Therapists
Achieving lasting change: investing in innovation
57) Change on this scale will take time to achieve and not everything we try will work. Success demands we take an innovative, experimental approach to test a wide range of approaches in different environments and learn quickly, shifting focus early from any failures and moving rapidly to scale up successful approaches. It means working with a wide range of people to identify where we should focus our efforts. And we should look to capture the impacts across the whole of government, where possible, to build the case for future investment and help us influence a wider range of actors. Having a clear idea of what works in what context will enable us to:
- focus our resources on services and commissioning models which have the most impact
- influence commissioners of services to make the right decisions to invest in different support to meet local population needs
- provide employers with information about successful approaches and spread best practice
58) We want to take early action to build our evidence base on what works in the areas that we already know are important. We start with a solid understanding of some of key principles based on evidence from past delivery. For instance, evidence suggests that when a person faces both health and employment barriers, both should be addressed simultaneously, since there is no evidence that treating either problem in isolation is effective. [footnote 66] As an example, Individual Placement and Support, an integrated health and employment model, has demonstrated improved employment outcomes for those with severe and enduring mental health condition. A UK evaluation found that chances of finding employment doubles for those who received this service. [footnote 67]
59) We also know that evidence gaps exist, in particular:
- how best to support those in work and at risk of falling out of work, including the part employers can play
- understanding how best to help those people in the Employment and Support Allowance Support Group who could and want to work (discussed further in chapter 2)
- the settings that are most effective to engage people in employment and health support
- how musculoskeletal treatment and occupational health interventions improve employment outcomes
60) We have a range of activity underway that is focused on the evidence gaps we have identified, including access to services and levels of support we should offer. This will help us to develop new models of support to help people into work when they are managing a long-term health condition or disability.
61) As part of this our £70 million Work and Health Innovation Fund, jointly managed by the Work and Health Unit and NHS England, will support promising local initiatives to drive integration across the health, care and employment systems. The first areas we will work with are West Midlands Combined Authority and Sheffield City Region. Seed funding will be provided to support the design trials to test new approaches at scale and understand if they can improve employment and health outcomes. Following this design phase, we plan to review these proposals and decide if they are viable for implementation, with access to further funding and national support available to enable full implementation from spring 2017.
62) By bringing local Clinical Commissioning Groups, Jobcentre Plus and local authorities into new partnerships these trials will create new support pathways for people with common physical and mental health conditions to help them stay in or return to work.
63) Alongside this, we are testing a range of approaches to improve outcomes for people with common mental health conditions, who make up 49% of those on Employment and Support Allowance. [footnote 68] We want to rapidly scale up those which show they can make a real impact. Trials include testing interventions that offer faster access to treatment and support services, co-locating employment support in a health setting and building on the evidence for Individual Placement and Support to understand if this is a model which can work successfully for people with common mental health conditions.
64) Examples of this approach include the Mental Health Trailblazers. These combine a specific type of employment support, Individual Placement and Support, with psychological support provided through the NHS talking therapy services in 3 areas: Blackpool, West London and the North East.
65) As set out in the 2015 Spending Review, there are opportunities to make use of Social Impact Bonds to help people with mental health problems. Social investment offers an exciting new opportunity to draw on both private capital and voluntary and community sector innovation to test and scale new forms of support. We are reviewing how Social Impact Bonds can be best used across our range of innovation activity and will invest up to £20 million on work and health outcomes. The Government Inclusive Economy Unit will explore the possible role of existing or new public service mutuals, which already operate to good effect in the health and care sectors
66) We recently launched our Small Business Challenge Fund to encourage small businesses in developing small-scale innovative models for supporting small and medium-sized enterprises with sickness absence. This approach will allow us to use a small amount of funding to identify promising interventions and prototypes to take forward to more robust testing.
67) We aim to build on this Challenge Fund approach to develop small-scale innovative approaches to quickly understand which may work and fail fast on those which do not. Such an approach is likely to be most useful where there is limited evidence, such as supporting small and medium-sized employers with sickness absence, or where there is already a market of innovators, such on digital health technologies. We are particularly interested to use the consultation process to identify key areas where such an approach may be appropriate.
68) Finally, it is important we share information on what works widely to support local delivery. To do this, we will work with Public Health England to develop a set of work and health indicators and identify how we can best bring together and share the existing evidence for local commissioners and delivery partners. We will continue to draw on a range of internal and external evidence, including trials and research, the academic literature and relevant third sector organisations to improve policy making and delivery nationally and locally.
Your views
69) We are committed to building a pipeline of innovation to rapidly improve support for individuals. As part of this we will be developing a structured evidence base so that we know what works, and we recognise that there will be rich sources that have already been developed or are being drawn together by others. We want to hear from you about areas you are already exploring or have learnt from:
- what innovative and evidence-based support are you already delivering to improve health and employment outcomes for people in your community which you think could be replicated at scale? What evidence sources did you draw on when making your investment decision?
- what evidence gaps have you identified in your local area in relation to supporting disabled people or people with long-term health conditions? Are there particular gaps that a Challenge Fund approach could most successfully respond to?
- how should we develop, structure and communicate the evidence base to influence commissioning decisions?
Respond to this consultation online
Building a shared vision
70) This green paper sets out the pressing case for action, and the systemic challenges we face. Achieving our vision will require us to work beyond artificial system boundaries and work with those in our local communities. We will also need to be innovative and test new ways of doing things.
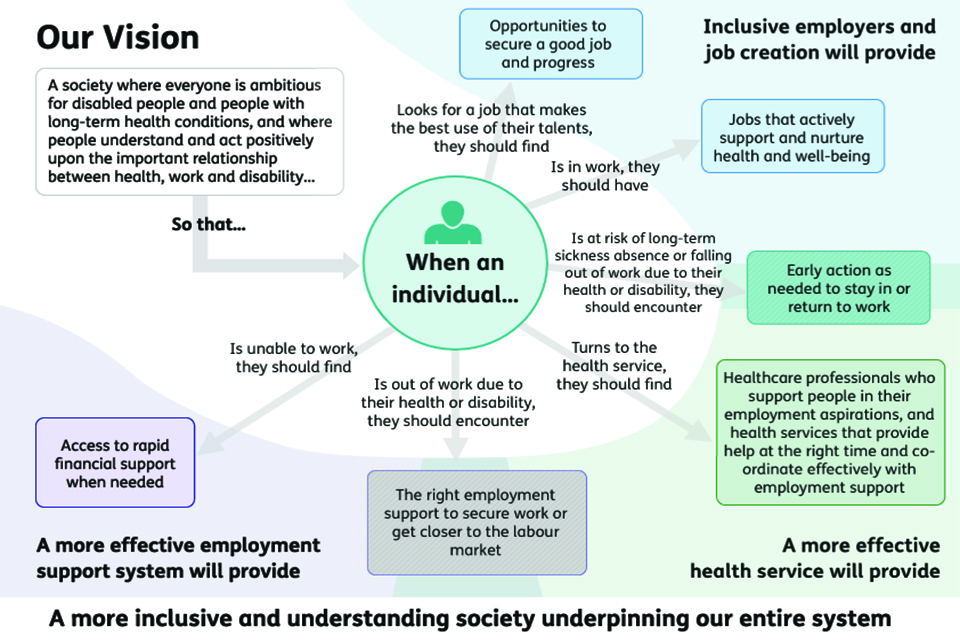
See appendix for full description of this image: Our vision
71) This green paper discusses a number of areas where we want to see change to make systems work better for people. It considers:
- supporting more people into work (chapter 2)
- assessments for benefits for people with health conditions (chapter 3)
- supporting employers to recruit with confidence and embed a healthy working culture in the workplace (chapter 4)
- supporting employment through health and high quality care for all (chapter 5)
72) Chapter 6 discusses the vital role all of us can play in delivering the changes we want to see, and sets out how you can respond to this consultation. The involvement of employers, local government, practitioners, providers, advocacy groups, carers, disabled people, and people with long-term health conditions is vital. Please let us know what we need to improve so that we can build a plan that will bring real and lasting change.
Summary of consultation questions
We are committed to building a structured evidence base so that we know what works and recognise that there will be rich sources that have already been developed or are being drawn together by others. We want to hear from you about areas you are already exploring or have learnt from:
- what innovative and evidence-based support are you already delivering to improve health and employment outcomes for people in your community which you think could be replicated at scale? What evidence sources did you draw on when making your investment decision?
- what evidence gaps have you identified in your local area in relation to supporting disabled people or people with long-term health conditions? Are there particular gaps that a Challenge Fund approach could most successfully respond to?
- how should we develop, structure and communicate the evidence base to influence commissioning decisions?
Respond to this consultation online
2: Supporting people into work
Chapter summary
In this chapter we focus on how we can best provide employment support to disabled people and people with health conditions. It explores:
- our vision for how people can access an integrated network of health and employment support delivered from a range of sectors, supported by a dedicated Jobcentre Plus work coach who can work closely with someone to build a relationship and offer personalised support that is tailored to their needs
- how we are investing in the skills and capabilities of Jobcentre Plus work coaches to enable them to better support people with a wide range of health conditions, including mental health conditions, bringing in external expertise
- our new Personal Support Package, including an enhanced menu of employment support for work coaches to draw on
- how we can better engage with people placed in the Employment and Support Allowance Support Group or the Universal Credit Limited Capability for Work and Work-Related Activity Group (LCWRA). We will undertake research and a trial to better understand how we can support individuals to move closer to the labour market and into employment, where appropriate
Introduction
73) We want everyone to have the opportunity to benefit from the positive impacts that work can have, including on their health and wellbeing. Where people want to work, and have the potential to do so immediately or in the future, we should do everything we can to support them towards their goal. We want people to be able to access appropriate, personalised and integrated support at the earliest opportunity, which focuses on what they can do, builds on their talents and addresses their individual needs.
74) Where someone is out of work as a result of a health condition or a disability, the employment and health support they receive should be tailored to their personal needs and circumstances. This support might be delivered by a range of partners in their local area, such as by Jobcentre Plus, contracted provision, local authorities or third sector providers. Increasingly, our work coaches across Jobcentre Plus will assess an individual’s needs and ensure that they access the right help. Work coaches will be supported by new Community Partners and Disability Employment Advisers, who will be able to use their networks and expertise to work with local organisations, to support disabled people and people with health conditions to achieve their potential.
75) Universal Credit is already making improvements which put people at the heart of the welfare system, giving more personalised and integrated support from a dedicated work coach in Jobcentre Plus to help claimants with a health condition move closer to the labour market and get into work. It will also, for the first time, help those claimants with health conditions who are already in work to progress in the labour market supporting them to earn more. Evaluation has found people receiving Universal Credit are more likely to move into employment and move into work quicker than similar individuals receiving Jobseeker’s Allowance. [footnote 69] To ensure that disabled people and people with health conditions receive the best possible support, we will introduce a new Personal Support Package for people with health conditions in Jobcentre Plus, with a range of new interventions and initiatives designed to provide more tailored support.
76) However, further action is needed to build on the principles Universal Credit has introduced. We cannot make significant progress towards halving the disability employment gap with a system that treats 1.5 million people [footnote 70] – the current size of the Support Group in Employment and Support Allowance – in a one-size-fits-all way. The current approach does not do enough to treat people as individuals: more must be done to ensure that people do not miss out on accessing the wealth of local, integrated support available through Jobcentre Plus. We will achieve this by identifying evidence gaps, building on insights from trials and drawing on the knowledge of both service users and providers.
77) In this chapter we will discuss 2 key themes:
- Universal Credit is moving in the right direction, but there is still more to do to improve how work coaches systematically engage with disabled people and people with health conditions. We want to identify the most effective support based on a person’s circumstances and the capabilities required in Jobcentre Plus to deliver these interventions. Work coaches will also be able to offer an array of targeted support as part of the Personal Support Package summarised below
- the current one-size-fits-all approach to employment support is not appropriate. This is because people in the Employment and Support Allowance Support Group, and those with ‘Limited Capability for Work and Work Related Activity’ (LCWRA) in Universal Credit, do not routinely have any contact with a Jobcentre Plus work coach. We are committed to protecting those with the most needs, but want to test how we might offer a more personalised approach to employment support, which reflects the wide variety of conditions and needs within this group and is in keeping with Universal Credit principles.
We are introducing the new Personal Support Package for people with health conditions. This is a range of new measures and interventions designed to offer a package of support which can be tailored to people’s individual needs.
The offer, set out in more detail in this chapter, includes the following new forms of support for all Employment and Support Allowance claimants (and Universal Credit equivalents):
- personal support from disability trained, accredited work coaches. A particular focus of training will be mental health. Work coaches will also be better supported by an extra 300 Disability Employment Advisers and around 200 new Community Partners, with disability expertise and local knowledge. This will lead to better signposting to other local voluntary and public sector services
- a Health and Work Conversation for everyone claiming Employment and Support Allowance, as appropriate
For new claimants in the Employment and Support Allowance Work-Related Activity Group (ESA WRAG), and the equivalent Universal Credit Limited Capability for Work Group (UC LCW), an enhanced offer of support will also include:
- a place on either the new Work and Health Programme or Work Choice, for all eligible and suitable claimants who wish to volunteer
- additional places on the Specialist Employability Support programme
- Job Clubs delivered via peer support networks
- work experience places, with wrap-around support, for young people
- increased funding for the Access to Work Mental Health Support Service
- Jobcentres reaching out to employers, particularly small employers, to identify opportunities and help match people to jobs in a new Small Employer Offer
We will continue to develop the offer by:
- trialling the use of specialist medical advice to further support work coaches
- working with local authorities to pilot an approach to invest in Local Supported Employment for disabled people known to social care, notably those with learning disabilities and autism, and secondary mental health service users
- testing a Jobcentre-led alternative to Specialist Employability Support
- trialling additional work coach interventions
Action already taken
78) There is a significant amount of work already underway to strengthen and improve the employment support offer available to disabled people and people with health conditions. These activities are explored in more detail within the chapter, and include:
- Universal Credit – replacing 6 benefits with 1, the introduction of Universal Credit will make a significant difference in improving the level and quality of support offered to individuals with health conditions
- expansion of the Disability Employment Adviser role – we are recruiting an additional 300 Disability Employment Advisers, taking the total to 500
- permitted work – from April 2017, we will remove the 52-week limit on how long Employment and Support Allowance claimants placed in the Work-Related Activity Group (WRAG) are able to work for. This will improve work incentives for this group
- the Work and Health Programme – following the end of the Work Programme, this provision will be available to disabled people receiving Employment and Support Allowance or Universal Credit on a voluntary basis from October 2017
Universal Credit and the financial benefits of work
79) It is essential to ensure that people are better off in work. Under Universal Credit, people can more clearly see the financial benefits of moving into work, allowing them to take small steps into the labour market and to work flexibly in line with their needs.
80) In Universal Credit, for people who have ‘limited capability for work’ (LCW) or ‘limited capability for work and work related activity’ (LCWRA), there is a work allowance for earned income. This means that someone assessed as having LCW or LCWRA, with housing costs, can earn up to £192 a month, and a similar person, without housing costs, can earn up to £397 a month, in both cases without affecting their Universal Credit payment. For any earnings above these allowances, the Universal Credit 65% taper applies, which means that only 65% of the extra earnings above those allowances are deducted from the claimant’s Universal Credit entitlement - a steady and predictable rate as people gradually increase their hours and earn more, rather than the cliff-edge approach of Employment and Support Allowance. This is particularly well suited for people whose disability or health condition means they can only work some of the time.
81) Individuals on Employment and Support Allowance are allowed to work up to 16 hours and earn up to £115.50 a week and keep all of their benefit. If earnings exceed this amount, Employment and Support Allowance stops altogether. The permitted work rules allow people claiming Employment and Support Allowance to undertake some part-time work without it impacting on their benefit, to encourage them to gradually build their employment skills and return to work. However for those in the Work-Related Activity Group this is limited to 52 weeks. We will remove this limit from April 2017 to bring the Employment and Support Allowance rules more into line with Universal Credit and improve the incentive to work.
Early engagement
82) Being better off in work is not enough on its own if disabled people and people with health conditions are not being enabled to find work in the first place. Universal Credit ensures that people with health conditions still have an opportunity to engage with a work coach prior to their Work Capability Assessment, where appropriate. This approach builds on evidence that early intervention can play an important role in improving the chances of disabled people and people with a health condition returning to work. [footnote 71]
83) This is a significant improvement on the current process in Employment and Support Allowance, where people are not routinely having a face-to-face conversation with a work coach about practical support to help them back to work until after their Work Capability Assessment is complete – and this can be many months after their initial claim. Over 60% of the 2.4 million people receiving Employment and Support Allowance – those currently in the Support Group [footnote 72] – do not get this opportunity and often have no contact at all with a work coach and therefore do not access tailored support when they need it. We are missing a significant opportunity to provide help to people when they could benefit most.
84) This earlier engagement between an individual and a work coach in Universal Credit will also serve as a gateway to a wider, integrated system of support offered by the Department for Work and Pensions and other agencies, such as the NHS and local authorities. If a work coach identifies that someone has particularly complex barriers to work or complex health conditions, they will be able to advise individuals about other types of support in their local area – whether health services, skills courses or support with budgeting.
85) This builds on the approach of Universal Support, which helps people make and maintain their Universal Credit claim, and will assist people with their financial and digital capability throughout the life of their claim. This is delivered in partnership between the Department for Work and Pensions and local authorities, and with other local partners such as Citizens Advice and Credit Unions. Through Universal Support we are transforming the way Jobcentres work as part of their local communities to ensure they more effectively tackle the complex needs some people have and support them into sustainable employment. The Troubled Families programme offers another example of an integrated approach, with local authorities coordinating wider support services for complex families, including those with health conditions, and in doing so, driving public service reform around the needs of families. The Department for Work and Pensions provides work coaches acting as Troubled Family Employment Advisers, based within local authorities, where they play an important role in integrating employment support with the wider services.
###Building work coach capability
86) The relationship between a person and their work coach should be at the heart of each individual’s journey in the welfare system. To ensure that people with complex and fluctuating health conditions receive the most appropriate support, we will continue to build and develop the capability of our work coaches. We have introduced an accredited learning journey for work coaches, which includes additional mandatory training in supporting those with physical and mental health conditions. From 2017, we will introduce an enhanced training offer which better enables work coaches to support people with mental health conditions and more confidently engage with employers on the issue of mental health.
87) Work coaches will be supported by specialist Disability Employment Advisers. We are currently recruiting up to 300 more Disability Employment Advisers, taking the total to over 500. These advisers will work alongside work coaches to provide additional professional expertise and local knowledge on health issues, particularly around mental health conditions. The role will have a much stronger focus on coaching work coaches to help build their confidence and expertise in supporting individuals with a health condition or disability.
88) We also recognise the value of bringing external expertise into Jobcentres and of working more effectively with the voluntary sector in our design and delivery of support. We know that voluntary organisations have unique insight and expertise about the people they work with and their conditions, and we want to harness this. So, we will recruit around 200 Community Partners across Jobcentre Plus. These will be people with personal and professional experience of disability and many will be seconded from a Disabled People’s User-Led Organisation or disability charity. From next year, Community Partners will be working with Jobcentre Plus staff, to build their capability and provide valuable first-hand insight into the issues individuals with a health condition or disability face in securing and sustaining employment. Drawing on their local knowledge, they will identify more tailored local provision to ensure individuals with health conditions can benefit from the full range of support and expertise available. Community Partners will also engage with local employers to help improve the recruitment and retention of disabled people and people with health conditions.
89) Our Community Partners will map local services available in each of our Jobcentre Plus districts. This will include understanding where there are peer support and patient groups which engage with disabled people and people with long-term health conditions who might otherwise find it hard to re engage with employment, helping develop confidence and motivation. Where there are gaps in provision our districts may be able to make local decisions to fund any priority areas, using the Flexible Support Fund. We will be providing an extra £15 million a year in 2017/18 and 2018/19 for our Flexible Support Fund so that local managers can buy services including mentoring and better engage the third sector in their community. We will introduce a new Dynamic Purchasing System across the country by December 2016 which will allow third sector and other organisations to develop employment-related service proposals that Jobcentres can quickly contract for. Our goal is to extend the reach of Jobcentre Plus into third sector support groups which are already well established.
90) Often, the best advocates of the positive impact of being in work are people who themselves have had the experience of managing a serious health condition, or overcoming an employer’s prejudice about disability. We have already tested Journey to Employment peer support job clubs on a small scale, offering personalised support in a group environment delivered by people who have personal experience of disability, drawing on research by Disability Rights UK and the Work Foundation. These clubs often take place outside a Jobcentre as this provides an alternative setting which may be more effective for some individuals with health conditions. We are extending our Journey to Employment job clubs to 71 Jobcentre Plus areas with the highest number of people receiving Employment and Support Allowance, to further test the effectiveness of peer support job clubs at supporting those with health conditions.
Case study – Journey to Employment (J2E) Job Club
Jayne was employed, but life events affected her health and changed everything. Jayne joined the J2E Project in 2015 and she started her journey to recovery.
Describing her time before the Job Club, she said:
I shut down to protect myself and drew inward trying to block things in work. I didn’t feel I was functioning on ‘all cylinders’, my confidence was shot, I was checking up on what I was doing constantly and this spiralled out of control.
I felt I was in limbo I didn’t really know what I wanted to do, I could not afford not to work so felt confused about where go and who to seek help from. I was suffering with anxiety and terrible panic attacks, I was also depressed and can recognise now through help I have received and my own research that it was all due to the environment I was in.
I suffer mainly with anxiety and this escalated due to having to make the decision to leave my job to protect my mental health. Life was still awful, leaving work meant my fear increased and I was really down and family noticed the change in me. I wasn’t getting up in the mornings and I was confining myself to my room.
I had a good supportive GP and work coach called Janis. I needed support to attend the appointment with Janis and felt that Janis really listened, had empathy and was so supportive. I felt she was on my side, she indicated different choices and J2E sounded ideal to give me structure and at last it felt good to know where I was going.
I felt nervous going to see Louise my Community Employment Specialist, but once I met her and had a chat I knew that attending the J2E training course would be beneficial for me.
Attending the course gave me insight into my options, it helped me to manage myself better. Being amongst others that understood what I was going through, having balance and hearing about other people’s lives gave me a perspective on my situation. By that I mean that, it made me see that some people were struggling with a great deal more than I was.
All my concerns, talking about my situation with other people were eased, because I felt the others in the group understood. I also completed a mindfulness course via my GP which lasted for 6 to 8 weeks, this also helped me self-manage.
91) We want to make sure work coaches can access the right specialist advice and support, so they can understand how a complex health condition might affect an individual’s ability to work, and access advice on how someone can better manage a health condition to be able to work. We therefore intend to trial access to specialist advice through a 3-way conversation between a work coach, healthcare professional and a person who has been placed in the Work-Related Activity Group, following a Work Capability Assessment. The trial will begin in 2017, with a view to rolling out provision on a wider scale in future years, depending upon results.
Early intervention in Employment and Support Allowance
92) These improvements will place the relationship with the work coach and access to a network of integrated support at the heart of each individual’s journey. We also want those receiving Employment and Support Allowance to benefit from the support that disabled people and people with health conditions who receive Universal Credit can already access as part of their Claimant Commitment discussion. To that end, we have developed a new Health and Work Conversation between an individual and their work coach. In the Health and Work Conversation, work coaches will use specially designed techniques to help individuals with health conditions to identify their health and work goals, draw out their strengths, make realistic plans, and build resilience and motivation. People will be required to attend the Health and Work Conversation, where appropriate, but the actions they subsequently agree to within the conversation will be entirely voluntary in the period before the Work Capability Assessment, and will be captured in a new Employment and Support Allowance Claimant Commitment.
93) The Health and Work Conversation will focus on what individuals can do to move closer to work while managing or treating their health condition, rather than on what they are unable to do. This new conversation was co-designed with disabled people’s organisations and occupational health professionals and practitioners and the Behavioural Insights Team. As a person and their work coach works together, the Claimant Commitment can be updated over time as the individual moves closer to being able to work. This approach will mean that a person will have an established relationship with their work coach and be able to explore the implications of their Work Capability Assessment with them after it takes place. They will also be able to review the Claimant Commitment actions they have jointly developed up until that point. We are exploring how we could integrate this approach into Universal Credit as well.
Your views
94) Work coaches play a crucial role in ensuring that disabled people and people with a long-term health condition can access the right support, at the right time, and in an integrated manner at a local level. We also recognise that there is more that can be done to improve how work coaches engage with these individuals.
- how do we ensure that Jobcentres can support the provision of the right personal support at the right time for individuals?
- what specialist tools or support should we provide to work coaches to help them work with disabled people and people with health conditions?
Respond to this consultation online
Employment support for disabled people and people with health conditions
95) Work coaches will increasingly be able to offer a wide menu of interventions tailored to people’s needs. Building on what we have learnt from the Work Programme and Work Choice, the Work and Health Programme will offer a more personalised, local approach to supporting disabled people to overcome barriers to employment. The Work and Health Programme will be targeted at people who are likely to be able to find work within 12 months, with more specialist support. Disabled people can volunteer for the programme at any time. Providers will be expected to support people based on the needs, strengths and aspirations of the individual; deliver effective services which are integrated with local services; and connect individuals with local employers and place and support them in sustainable employment. From 2017 we plan to be able to offer a place on either Work Choice or the Work and Health Programme to all eligible and suitable new Employment and Support Allowance (Work-Related Activity Group) and Universal Credit (Limited Capability for Work) claimants who are assessed as being within 12 months of being able to start work, and who wish to volunteer. This commitment will not include a small number of claimants who will be placed into the control group of the Randomised Control Trial used to evaluate the performance of the Work & Health Programme.
Localism and devolution
We are already funding work with Greater Manchester, London and in Glasgow and the Clyde Valley to deliver locally designed employment support to help those residents who claim Employment and Support Allowance who have left the Work Programme without finding work.
In parallel, through the Devolution Deal process, we have agreed to co-design the new Work and Health Programme with the Tees Valley, East Anglia, Sheffield City Region, the West of England, West Midlands, Liverpool City Region and Cardiff Capital Region. This will ensure there is a more personalised approach in those areas and one which fully supports local plans to integrate services to provide a more co-ordinated service for residents to avoid duplication and people getting lost in the system. We are also working with London and Greater Manchester to not only co-design the programme with them but also ensure that they can jointly shape every element of the commissioning process, from strategy to service design, managing provider relationships and reviewing service provision. We are keen to understand what works locally to inform future strategy for supporting local delivery and supporting areas ambitions for integrating health and work provision.
96) The Work and Health Programme will not be suitable for everyone, as some people have additional and more complex needs. We currently offer additional help through the Specialist Employability Support programme. This provision focuses on helping those furthest away from the employment market and for whom other provision is unsuitable due to the complexities of their barriers to employment. Specialist Employability Support offers an individually tailored combination of advice, guidance, training, work placements and work experience. We are currently considering how we should continue this support in the future, including how to provide more places to individuals in the Employment and Support Allowance Work-Related Activity Group or assessed as having limited capability for work in Universal Credit from April 2017.
97) We will continue to support disabled people and people with health conditions who wish to start their own business. The New Enterprise Allowance scheme provides access to business mentoring and offers financial support to those in receipt of an eligible benefit, including those on Employment and Support Allowance and Universal Credit. The New Enterprise Allowance has so far supported around 90,000 people into self employment, where 21% of these businesses have been established by individuals who have declared a disability. [footnote 73]
98) We will also ensure we make better use of local support mechanisms. For those with a learning disability or autism who are known to adult social care, or those in contact with secondary mental health services, we will pilot an approach working with local authorities to deliver Supported Employment on an outcome-payment basis. Supported Employment uses a ‘place then train’ approach, aimed at moving people into paid employment. This will help us to test the effectiveness of locally-driven solutions to best support people with the most challenging conditions, and build on our learning of what works for them.
99) We also want to support local areas to design new, integrated approaches to improving health and work outcomes at scale. We are using the Innovation Fund to develop large-scale health-led trials creating partnerships between local health service commissioners and providers, Jobcentres, and councils. These partnerships will test if health-led support services are effective at supporting disabled people and people with health conditions into work, how effectively they support people to stay in work and how to get a region to work collaboratively on the health and employment agenda, through the introduction and integration of services.
Supporting people with mental health conditions
100) Improving our offer of support for people with mental health conditions will be integral to our approach. The Five Year Forward View for Mental Health and NHS England’s Implementation Plan sets out a series of actions to prevent mental ill health, improve services and reduce stigma. Around half of Employment and Support Allowance claimants in the Support Group report a mental or behavioural disorder as their primary health condition – the most prevalent of these being depression, stress and anxiety. [footnote 74] The government will invest in trials, proofs of concept and feasibility studies over the next 3 years to test ways to provide specialist support for people with common mental health conditions and ensure that we are providing access to the most effective health support when it is needed. As discussed in chapter 5, we are also increasing the number of employment support advisers co-located in talking therapy services. We are supportive of co locating services where it can improve support and will consider whether there is wider learning on co-location we can draw from this work.
101) The new support we will test to establish what works best for people with mental health conditions who are out of work includes:
- Group Work – to test whether the JOBS II model, a form of group work, improves employment prospects and wellbeing
- supported computerised Cognitive Behavioural Therapy (cCBT) testing whether early access to supported cCBT can support employment outcomes alongside recovery
Case study – a community employment specialist
I am a Community Employment Specialist and really enjoy making a difference and changing attitudes, I have worked in a variety of roles and in various sectors, including small community development projects supporting people with multiple barriers to the workplace and managing a large branch of Waterstones booksellers. For most of my early life I struggled with a mental health condition and ended up claiming Employment and Support Allowance as I was not prepared to acknowledge or seek proper treatment for my condition. My mental health reached a crisis point and I ended up homeless and living in my car, at that point I did seek help.
After 9 months of this situation, I managed to secure a council flat and slowly began a recovery journey. I joined the Fed Centre for Independent Living because I wanted to work in a role where my experience and situation could actually help others instead of feeling like something I was always trying to hide.
I was thrilled at the opportunity of delivering a Journey to Employment (J2E) job club and support others. Working directly in Jobcentre Plus has enabled me to support work coaches, build relationships and provide advice to people with health conditions.
I also deliver J2E training which I deliver in a very flexible, person-centred way building the course content around each group of participants. I have support in the job club from a colleague who also has lived experience of managing a health condition, and exploring development of different coping mechanisms. This allows us to provide insight into the recovery journey, provide support wellbeing, resilience and respond to the changing needs of the people we work with so that we can support them on their journey back into employment.
Supporting young people
102) Gaining employment after leaving education should be a core part of the journey into adulthood for disabled young people and young people with health conditions yet successful outcomes are far too low. Young people who are out of work and begin to claim Employment and Support Allowance or Universal Credit early in their lives can face scarring effects of long-term unemployment if they do not move into work. To explore how to better support this group we will test a voluntary, supported Work Experience programme for young people with limited capability for work. This will enable young people to benefit from time in the workplace with a mainstream employer to build their confidence and skills, enhance their CV and demonstrate their ability to perform a job role.
103) There are over 250,000 children and young people in education in England with a Statement of Special Educational Needs or an Education Health and Care (EHC) plan.[footnote 75] Most have a learning disability or autism and many do not get the support they need to move into work. These young people who have an EHC plan at age 15 are more than twice as likely not to be in education, employment or training at 18. Just 5.8% of adults with a learning disability known to local authorities are in a job. [footnote 76] This must be addressed. We will work with organisations to listen to the views of people with a learning disability and their families to look at what we can do to improve employment opportunities for this group.
104) We will open up apprenticeships to young people with a learning disability. For this group, we will make adjustments to English and maths requirements and draw on the £2.5 billion the government will make available for apprenticeships each year by the end of this Parliament. We will also work with social enterprises and disabled entrepreneurs to set up apprenticeships specifically for young disabled people. Jobcentre Plus will increase support in schools for young disabled people, by bringing in Supported Employment providers, business mentors and young disabled people who are in work to inspire young people to see employment as an achievable goal. This could include 2 weeks supported work experience.
105) A further way that young people with a health condition or disability can be helped while still in full time education is through supported internships. These give 16 to 25 year-olds with an EHC plan (or equivalent) an unpaid work placement of at least 6 months, personal support from a job coach and a personalised study programme. The results can be impressive: evaluation found 36% of participants in the trial secured paid work. [footnote 77]
106) It is our ambition that all young people with an EHC plan should be able to do a supported internship [footnote 78] but to achieve this we need many more employers to offer these opportunities. We suspect too few employers know where to go for information about how to offer a supported internship and do not understand the benefits, which can include: the flexibility to create opportunities that meet their needs; free support; and the chance to grow their employees of the future. We therefore want to help employers to link up with schools and colleges to increase the number of supported internships.
Supporting people in work
107) Universal Credit will also support disabled people and people with health conditions to not only get into work, but to progress in work as well. It is payable to those on a low income and aims to support those individuals to increase their earnings, progress in work and reach their full potential. This is the first time any country has attempted this approach. Therefore, it is crucial that we build the evidence base to understand what works. We have developed a substantial programme of trials as part of the wider test and learn strategy in Universal Credit. Evidence from these trials will be central to the development of our future in-work support service, and will provide a foundation for further development of support for disabled people and people with health conditions.
108) Whatever a person’s needs, this new package of support offered through Jobcentre Plus will ensure more personalised, integrated and targeted approaches for disabled people or people with a long term health condition. The work coach is the key gateway to this support within the Jobcentre Plus network and across local provision – transforming the way we engage with individuals with health conditions from the very start of their claim and testing direct referral into health services. We need to provide work coaches with additional tools to ensure that they are referring people to the right forms of support. We are therefore keen to hear from stakeholders about how best to support individuals, to inform our evidence base.
Your views
- what support should we offer to help those ‘in work’ stay in work and progress?
- what does the evidence tell us about the right type of employment support for people with mental health conditions?
- if you are an employer who has considered providing a supported internship placement but have not done so, please let us know what the barriers were. If you are interested in offering a supported internship, please provide your contact details so we can help to match you to a local school or college.
Respond to this consultation online
Improving access to employment support
109) The new Personal Support Package, along with the earlier intervention and changes that Universal Credit introduces, marks a step change in the approach to helping people move towards and into sustainable employment. In practice however, over the last 12 months we have seen on average 50% of Employment and Support Allowance claimants being placed in the Support Group following their Work Capability Assessment, [footnote 79] meaning they will not access this support and risk facing long periods of time on benefits.
110) We recognise the challenges of helping those with the most complex health conditions move closer to work, particularly when there is limited evidence of what works best. Our aim is not to reduce the amount of benefit those in the Support Group (or the Limited Capability for Work and Work-Related Activity Group in Universal Credit) receive or to change the conditions of entitlement, but we do want to ensure people are treated as individuals. We want people to be able to access a personalised, tailored, practical employment support service that recognises that someone might not currently be able to engage with employment support but that they may be able to access and make good use of that support in the future.
111) While we do offer employment support to individuals in the Support Group, this has historically received a very low take up, with very few people volunteering for this help. We need to do more to understand how we can best help this group and offer appropriate support.
112) We will undertake comprehensive research to better understand how best to engage with people in the Support Group and those found to have limited capability for work and work related activity in Universal Credit, and what interventions are needed to support them effectively. We will also develop a large-scale trial to test and learn from different approaches of offering employment and health support, and ways to increase the numbers of people taking up offers of voluntary support. We will explore how we can improve the nature of engagement with someone placed in the Support Group, and consider alternative ways of working with people which could include engagement outside a Jobcentre environment or through other local partners.
113) This will help us to better equip work coaches to support individuals to fulfil their potential and allow us to target future support in better ways. We want to explore how to work more closely with the voluntary sector and local partners, to see if such organisations are better placed to offer individuals the right help. We will ensure that any additional support is effective for individuals, as well as offering affordability and value for money for the taxpayer. These findings will build on the range of interventions being trialled through the Work and Health Unit’s Innovation Portfolio, which will help establish a stronger evidence base for what works and help inform how we might help disabled people and people with health conditions.
114) As there is currently no requirement for people in the Support Group to stay in touch with the Jobcentre, besides engaging with reassessments, we could consider implementing a ‘keep-in-touch’ discussion with work coaches. This could provide an opportunity for work coaches to offer appropriate support tailored to the individual’s current circumstances, reflecting any changes since their Work Capability Assessment. This light-touch intervention could be explored as a voluntary or mandatory requirement and we would consider our approach carefully, utilising digital and telephone channels in addition to face-to-face contact, depending on which was more appropriate for the individual and their circumstances.
Your views
- should we offer targeted health and employment support to individuals in the Support Group, and Universal Credit equivalent, where appropriate?
- what type of support might be most effective and who should provide this?
- how might the voluntary sector and local partners be able to help this group?
- how can we best maintain contact with people in the Support Group to ensure no-one is written off?
Respond to this consultation online
Conclusion
115) Where people want to work, and have the potential to do so immediately or in the future, receiving the health and employment support that is tailored to their personal needs and circumstances can help them to achieve their goals. This chapter has set out our new Personal Support Package, the ways we are supporting work coaches to better help people with health conditions, and the work we are undertaking to better understand the needs of the Support Group.
116) We want to work with disabled people, their families and their representatives to ensure we are delivering the services which best support disabled people and people with health conditions to reach their full potential. The next chapter outlines how we could go further, to reform the Work Capability Assessment itself and further break down the barriers to being able to offer personalised support to disabled people and people with health conditions.
Summary of consultation questions
Building work coach capability
- how do we ensure that Jobcentres can support the provision of the right personal support at the right time for individuals?
- what specialist tools or support should we provide to work coaches to help them work with disabled people and people with health conditions?
Supporting people into work
- what support should we offer to help those ‘in work’ stay in work and progress?
- what does the evidence tell us about the right type of employment support for people with mental health conditions?
- if you are an employer who has considered providing a supported internship placement but have not done so, please let us know what the barriers were. If you are interested in offering a supported internship, please provide your contact details so we can help to match you to a local school or college.
Improving access to employment support
- should we offer targeted health and employment support to individuals in the Support Group, and Universal Credit equivalent, where appropriate?
- what type of support might be most effective and who should provide this?
- how might the voluntary sector and local partners be able to help this group?
- how can we best maintain contact with people in the Support Group to ensure no-one is written off?
3: Assessments for benefits for people with health conditions
Chapter summary
In this chapter we consider how we can best provide disabled people and people with health conditions with financial support in a straightforward and timely way if they fall out of employment. It explores:
- whether breaking the link between cash entitlement and Jobcentre support would lead to a more personalised offer of support, rather than this being decided by the category an individual is placed in following their Work Capability Assessment, as is the case with the current system
- how this could work in practice, with eligibility for financial support still being decided by an assessment but allowing work coaches to determine the offer of employment support, making decisions on a case by case basis based on an individual’s needs and circumstances
- how we can share information more effectively across health and welfare systems, to create a more streamlined process for individuals with severe and lifelong conditions to secure financial support, building on our announcement to stop reassessments for this group
- how improved data-sharing between health assessments (Employment and Support Allowance and Personal Independence Payment) could ensure we are able to make timely, accurate decisions about an individual’s entitlement to financial support
Introduction
117) People who have recently developed a health condition or become disabled are likely to be facing a stressful and challenging period in their lives. Falling out of work because of their health is an added stress. We want people not only to be able to access tailored employment support available through Jobcentre Plus, but also to get the financial help they are entitled to in a simple, straightforward way – especially for people with the most severe lifelong health conditions or disabilities. Crucially, the financial support they receive should not affect their eligibility to accessing employment support.
118) Universal Credit is already transforming lives, ensuring that individuals are supported when they have the most needs: both by accessing the financial support they need, and getting practical help to take the necessary steps to move back to work through an integrated support offer. Universal Credit goes a long way to simplifying the system, replacing 6 benefits with one, so it is easier for individuals to get the financial help they need without making multiple applications to different benefits or switching between benefits when their circumstances change, and offering personalised and tailored support from a dedicated work coach. But there is more we could do to build on these foundations to ensure that we are maximising employment opportunities for people, whilst also ensuring access to the appropriate financial support.
119) The Work Capability Assessment process for Employment and Support Allowance and Universal Credit does not lead to the individualised employment and health support service that we would like. We currently have an assessment system that places people into fixed categories for the purposes of engagement with local Jobcentres and specialist support programmes, with over half of individuals not receiving any systematic support towards employment as a result.
120) As Jobcentre Plus moves towards offering a Personal Support Package focused on early intervention, we believe it is wrong for these individuals to miss out on the personalised support Jobcentre Plus and other agencies, including health and voluntary sector providers, can offer. This support could help them manage, or overcome, health or other issues preventing them working.
121) This consultation does not seek further welfare savings beyond those in current legislation. But there are ways that we can improve how the current functional assessment process for people with health conditions works, in particular in relation to employment and health support.
122) In this chapter we want to explore 2 areas:
- the first area is whether we can improve how we assess entitlement to benefits
- the second area is the need to be able to share information more effectively across welfare and health systems. There are challenges to achieving this, but also significant opportunities for government departments to work together to share the information already available, to take the stress out of assessment processes for securing financial support and ensure we make timely, accurate decisions about financial entitlement
123) These 2 areas of reform are important to delivering the type of personalised and effective services we know disabled people and people with health conditions, their families and stakeholders want to see. We want to hear your views about how we can best do this.
The role of assessments in determining employment and health-related support
124) Employment and Support Allowance was introduced in 2008 to deliver a more proactive approach to supporting individuals with health conditions into work, with an expectation that a significant proportion of those going through the Work Capability Assessment would be placed in the Work-Related Activity Group, where they would be offered practical support to prepare to return to work if and when they were ready. Those who were unable to engage with any type of employment-related support would be placed in the Support Group and those who were found to be ‘capable of work’ would claim Jobseeker’s Allowance instead.
125) We are already taking steps to improve the assessment process and have responded to a range of recommendations from 5 independent reviews of the Work Capability Assessment. Last year, the Centre for Health and Disability Assessments (CHDA) introduced a telephone support service to help individuals to complete their health questionnaire, known as the ESA50 or UC50. We are also sharing information from the Work Capability Assessment with Jobcentre Plus work coaches, to allow them to consider health conditions and barriers to work-related activity in order to better tailor support. Employment and Support Allowance and Universal Credit forms and letters are being reviewed with groups representing service users and CHDA to improve their clarity. We are revising the letter sent to GPs by decision makers when an individual is found to be capable of doing some work to encourage their collaboration and highlight the benefits of work. We are also launching an online Employment and Support Allowance claims process to give individuals and their representatives more flexibility in how and when they apply, while also improving the quality of evidence received.
126) However, it is clear that more needs to be done to improve assessments and ensure people are not being written off without support. At the time Employment and Support Allowance was implemented in 2008 it was assumed that less than 10% of those having a Work Capability Assessment would go into the Support Group and that, as a result of this additional support, there was an aspiration that 1 million fewer people would be on incapacity benefits (Employment and Support Allowance, Incapacity Benefit and Severe Disablement Allowance) by 2015. In practice, over the last 12 months we have seen on average 50% of people going into the Support Group, [footnote 80] as shown in Figure 1. While it is right that these people receive additional financial support, it was never intended that we apply a one size-fits-all approach on accessing employment support to such a large group of individuals with a wide variety of conditions and differing prognoses.
Figure 1 – Outcomes of initial Work Capability Assessment
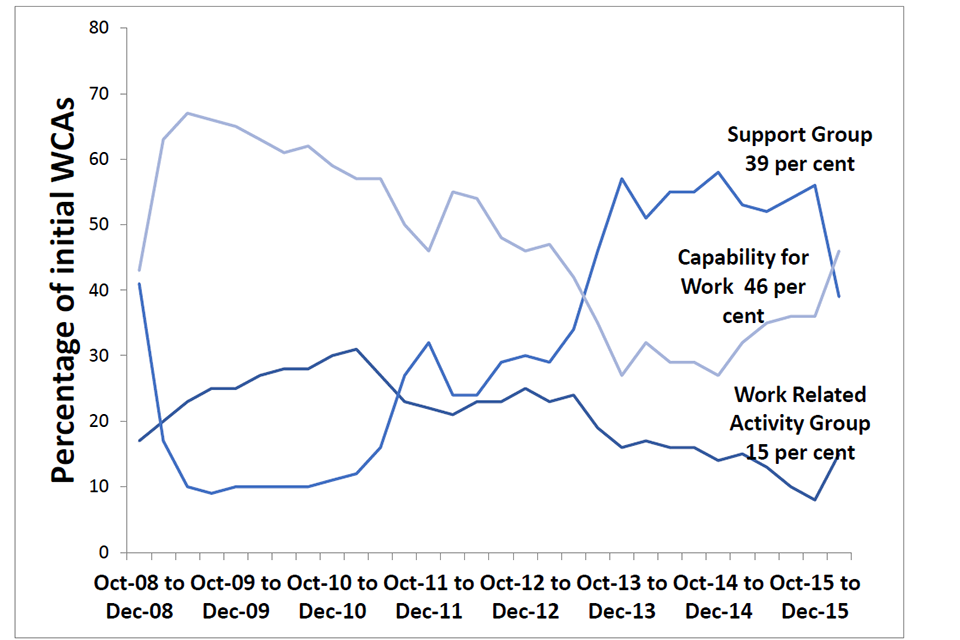
See appendix for full description of this image: Outcomes of initial Work Capability Assessment
127) As a result of these trends, over 1.5 million people have been given the perception they do not have any capability for work and are unlikely to think about when and how they might start to prepare for an eventual return to work as a result of the Work Capability Assessment. This label may then apply for years and results in them not receiving any systematic contact with a Jobcentre Plus work coach. 69% of those in the Support Group have been on the benefit for 2 years or more: [footnote 81] a high proportion not being engaged for a long period of time. And only 1 person in every 100 of those in each of the Work-Related Activity Group and Support Group leave Employment and Support Allowance each month. [footnote 82]
128) The one-size-fits-all approach is inappropriate considering the wide range of primary conditions and needs within Employment and Support Allowance and the Support Group. Conditions in the Support Group can range from having a mental health condition (50%) to diseases of the musculoskeletal system (12%) or nervous system (7%). [footnote 83] People might have fluctuating health conditions so they are able to engage with help one week but not the next. And survey data shows that 52% of people in the Support Group do want to work, [footnote 84] although their health condition may be a barrier to this.
129) Alongside their entitlement to additional financial support, these people deserve a personalised, tailored, practical support service as outlined in chapter 2. For instance, someone might be unable to engage with employment support at the point they undertake their Work Capability Assessment, but at a later point they could benefit from light-touch contact with a work coach who could provide advice on the health or employment services that might benefit them.
Reforming the assessment process
130) In order to realise our ambition to ensure individuals can access personalised support while still receiving the additional financial help they need, we need to consider whether the Work Capability Assessment is the right vehicle for deciding access to personalised employment support. This process initially included a Work-Focused Health-Related Assessment to explore with individuals their perceptions about work and to identify potential barriers to employment, but this was suspended in 2010 after we identified it was not as effective as had been hoped. This means we have a single functional assessment that tries to do 2 things: deciding both financial entitlement and also levels of systematic contact with Jobcentre Plus. We need to consider whether this is the right approach for the future.
131) Instead, it ought to be possible to build a more effective approach to assessing entitlement to financial and employment support. For instance, establishing entitlement to financial support could still be decided by an assessment, but that assessment could be used solely to determine whether an individual should get additional financial support. Decisions on whether someone should engage with Jobcentre Plus or specialist programmes could then be made through a separate process. This would avoid the current situation where someone’s entitlement to additional financial support can also result in them being given no employment support.
132) For instance, trained work coaches could have discretion to make case-by-case decisions about the type of employment support a person is able to engage with. To do this effectively, they would work closely with the person, building on information gathered at early discussions such as the Health and Work Conversation to ensure they are signposted to help that is appropriate to their needs. Work coaches will be able to draw on additional advice where needed, from Disability Employment Advisers and Community Partners, and could access specialist advice such as occupational health and Jobcentre Plus work psychologists where individuals have more complex health conditions.
133) That important relationship with a work coach would then continue beyond the assessment, ensuring those assessed as needing the most financial support can still access the holistic health and employment support and signposting offered by and through Jobcentre Plus. Work coaches could have full discretion to tailor any employment support to each individual claimant. This approach would be truly responsive, allowing the work coach to adjust requirements and goals dependent on changes in a person’s condition or circumstances. This is particularly important for people with fluctuating health conditions, as the support available would always be reflective of their needs.
134) This would mean that people are really offered a personalised service that takes appropriate account of their needs while still receiving the same financial support as under the current system – rather than having the offer of employment support determined by a fixed category. We would of course put safeguards in place to ensure that work coaches do not require someone to attend an appointment where this would not be reasonable.
135) There are a number of principles to how a new assessment approach could work which we would want to test. For instance, any assessment for financial support should draw as far as possible on existing information that has been gathered from the NHS, the adult social care system or through other benefit applications, such as from a Personal Independence Payment application, where this is appropriate and relevant. And it should still focus on the impact that an individual’s health condition has on them – recognising that those with the greatest level of disability have the biggest labour market disadvantage. [footnote 85]
136) An assessment which only considered financial support would also align to the principles of Universal Credit, meaning that an individual would continue to receive the ‘limited capability for work and work related activity’ rate of Universal Credit even if they moved into work, which would taper away as earnings increased.
137) This diagram illustrates a possible model for how this proposed approach could work in future – it does not describe the current system. We would like to hear views on whether this model would work, or whether there are alternative options we should explore.
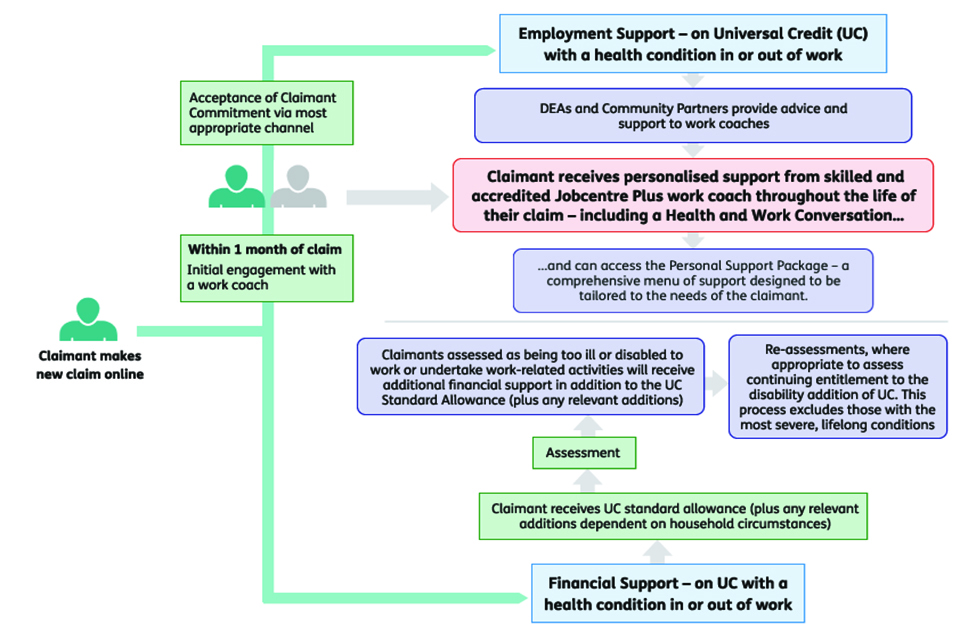
See appendix for full description of this image: A possible new model for assessments in Universal Credit
Your views
138) We recognise that stakeholders have repeatedly highlighted concerns about the effectiveness of the Work Capability Assessment. We want to hear your views on alternative ways that we could improve the process by which people are assessed for entitlement to financial support.
- Should the assessment for the financial support an individual receives from the system be separate from the discussion a claimant has about employment or health support?
- How can we ensure that each claimant is matched to a personalised and tailored employment-related support offer?
- What other alternatives could we explore to improve the system for assessing financial support?
Respond to this consultation online
Improving the data we use to assess financial support
139) People rightly expect public services to work together with each other, and to use the information they have provided to ensure the best possible service. This is even more important for services that provide essential financial support when someone is in need, such as when they have developed a health condition, or lost their job and their source of income.
140) For example, the Armed Forces Covenant helps ensure that service personnel, veterans and their families are supported and treated fairly, and recognises that special consideration is appropriate in some cases, especially for those who have given the most, such as those who have been injured. The Department for Work and Pensions uses Service Medical Board evidence where it can so a severely disabled person doesn’t have to undergo additional examinations for Employment and Support Allowance purposes.
141) However, there may be opportunities to use this evidence more widely in Employment and Support Allowance and Universal Credit assessments for all members of the armed forces which would result in speedier benefit awards and a less burdensome claiming process for the individuals.
142) If a person falls out of work as a result of a health condition or disability, they might already be accessing NHS services and potentially support from their local authority such as adult social care. They might also apply for financial assistance from a range of NHS schemes, such as the Healthcare Travel Costs Scheme. In addition, they might also claim a number of benefits, including Employment and Support Allowance or Universal Credit, and Disability Living Allowance or Personal Independence Payment.
143) In order to receive both Employment and Support Allowance or Universal Credit, and Personal Independence Payment, people will take part in 2 separate assessment processes. Around half of those who claim Employment and Support Allowance also receive Personal Independence Payment (or Disability Living Allowance), and 64% of those in the Employment and Support Allowance Support Group claim Personal Independence Payment or Disability Living Allowance. [footnote 86] This means that these individuals have to make 2 separate benefit applications where they often have to provide much of the same information, which might be in addition to applying to the NHS, local services or other bodies to receive specific support. For those who claim both Employment and Support Allowance and Personal Independence Payment, as at April 2016, around 70% applied for Employment and Support Allowance first. [footnote 87]
144) Different schemes provide financial support to meet different needs. For instance, Employment and Support Allowance and Universal Credit are paid to replace and supplement someone’s income while they are out of work or in low-paid work with a health condition. However Personal Independence Payment is designed to contribute to additional costs arising from a disability. It is sometimes appropriate that individuals might receive one and not the other, so to some extent it may be unavoidable that more than one application and assessment is required to determine eligibility for these different schemes.
145) However, where there are opportunities to share common information across processes and where information is up to date and relevant, we should reduce the burden on the individual of providing the same details over and over again should they claim both. This could also improve the accuracy of assessments to ensure individuals get the financial support they are entitled to, by making more effective use of data already held within the welfare system.
146) For example, subject to establishing that any data to be shared is up to date and relevant, we can consider sharing of data between the 2 assessments for Employment Support Allowance/Universal Credit and Personal Independence Payment. This could mean sending relevant sections of the Work Capability Assessment report to Personal Independence Payment assessors should an individual in receipt of Employment Support Allowance/Universal Credit, subsequently claim Personal Independence Payment. This could simplify the process so that once someone has provided information about their health condition to one part of the system, that information is used if they make a claim to a different benefit. This would ensure a person receives what they are entitled to without having to submit the same information again.
147) We will also explore how the assessment process could use data already gathered by the NHS or local authorities where appropriate, to ensure people do not have to repeatedly provide the same information. There are inevitably important sensitivities around how an individual’s data is used, and Dame Fiona Caldicott’s review of data security and consent opt outs has explored how we achieve the right balance between protecting an individual’s data, and using it to improve services. [footnote 88] However, if we can strike the right balance, there is a valuable opportunity to create a more seamless journey for people with the most needs, using data in a way that improves their access to services, and promotes more integrated services.
Those with the most severe lifelong conditions
148) Some people have been diagnosed with the most severe health conditions and disabilities from which they will never recover, and which require high levels of day-to-day care. People in these circumstances are likely to already have significant engagement with the NHS or social care services and in many cases they will already have had detailed and up-to-date NHS or local authority health or care assessments.
149) As these people’s conditions are extremely unlikely to improve, we have recently announced that they will no longer be required to take part in reassessments and are engaging with experts to design the criteria for deciding to whom this should apply. They are still currently expected to take part in an initial Work Capability Assessment to determine if they should have access to increased financial support and to decide their access to employment support.
150) We are therefore consulting on whether we should introduce a more appropriate process for people who have severe health conditions and disabilities, who represent a small proportion of those in the Employment and Support Allowance caseload. For instance, we could consider whether a simpler assessment process could be developed, that means that people do not need to provide as much information as required under the current system. It may be possible to achieve this, with an individual’s consent, by using data already held in the NHS to determine severity of condition and functional impact where this is appropriate.
151) In order to test the feasibility of this approach we will be conducting a case review exercise in our Assessment Centres to determine whether a healthcare professional could have completed a shortened assessment process using, for example, pre-existing NHS or local authority evidence such as care plans to make their recommendation. This would avoid placing any further burdens on the individual to fill in additional questionnaires or attend a face-to-face assessment to determine their eligibility. As part of this and the data-sharing work, we are also looking at wider opportunities to reduce bureaucracy and improve individuals’ experiences of assessment processes.
Your views
152) We want to hear from you about how we can make these processes work more effectively and seamlessly for individuals accessing financial support.
- How might we share evidence between assessments, including between Employment Support Allowance/Universal Credit and Personal Independence Payments to help the Department for Work and Pensions benefit decision makers and reduce burdens on claimants?
- What benefits and challenges would this bring?
- Building on our plans to exempt people with the most severe health conditions and disabilities from reassessment, how can we further improve the process for assessing financial support for this group?
- Is there scope to improve the way the Department for Work and Pensions uses the evidence from Service Medical Boards and other institutions, who may have assessed service personnel, which would enable awards of benefit to be made without the need for the claimant to send in the same information or attend a face-to-face assessment?
Respond to this consultation online
Conclusion
153) Disabled people and people with health conditions need a simple, effective route to the most appropriate financial support so that they can focus on managing their disability or health condition and accessing employment support where appropriate. This paper is seeking views on whether individuals could receive a better experience in accessing financial support – with improved used of data, and an assessment process that enables them to access financial support without this affecting their engagement employment support.
Summary of consultation questions
- Should the assessment for the financial support an individual receives from the system be separate from the discussion a claimant has about employment or health support?
- How can we ensure that each claimant is matched to a personalised and tailored employment-related support offer?
- What other alternatives could we explore to improve the system for assessing financial support?
- How might we share evidence between assessments, including between Employment and Support Allowance/Universal Credit and Personal Independence Payments to help the Department for Work and Pensions benefit decision makers and reduce burdens on claimants?
- What benefits and challenges would this bring?
- Building on our plans to exempt people with the most severe health conditions and disabilities from reassessment, how can we further improve the process for assessing financial support for this group?
- Is there scope to improve the way the Department for Work and Pensions uses the evidence from Service Medical Boards and other institutions, who may have assessed service personnel, which would enable awards of benefit to be made without the need for the claimant to send in the same information or attend a face-to-face assessment?
4: Supporting employers to recruit with confidence and create healthy workplaces
Chapter summary
In this chapter we consider the role of employers in supporting more disabled people and people with health conditions into work. We explore:
- why employers should take action, highlighting the benefits of investment and the risks of inaction
- how employers can be supported to establish good practices and supportive workplace cultures. We discuss the role of the public sector as a major employer in its own right and then look at how employers can be helped to address stigma and monitor workplace health, how they can access information, support and peer networks, how we can strengthen the evidence base for action and the possible role of incentives in driving the right behaviour and innovation
- how we can encourage employers to recruit disabled people and people with health conditions
- how employers can support more disabled people and people with health conditions to stay in or return to work. We explore the critical role of promoting health, practical preventative and rehabilitative support, how sickness absence management can be improved to support phased returns to work and the role of insurance schemes in supporting prevention activities and protecting incomes
Introduction
154) We want to create a country and an economy that works for everyone, in which disabled people and people with health conditions are given the chance to be all they want to be and employers can benefit from a large, valuable and under-used section of the labour market.
155) Employers are important partners in this enterprise. Many are already creating healthy, inclusive workplaces and our vision is for this to become normal practice for all employers. This chapter sets out an ambitious view of what employers can do. We first consider why it is in the interests of employers to act and then consider the foundation step of embedding good practices and healthy, inclusive cultures – which will underpin our efforts to help disabled people and people with health conditions to move into, stay in, progress in, or return to work.
156) We then focus on the tangible things we could do now to move towards an employment culture that recognises the contribution that disabled people and people with health conditions make to the workplace and where investment in health and wellbeing is the norm. We particularly want to know how to support, encourage and incentivise employers to adopt good practice, particularly among small and medium-sized businesses.
The case for employer action
157) Businesses drive our economy and are rightly focused on growth, productivity and delivering a return on their investments. Investing in workplace inclusivity, health and wellbeing is critical to these goals:
- employers will have access to a wider pool of talent and skills if they have inclusive and disability-friendly recruitment, retention and progression policies, [footnote 89] and may also be able to serve their customer base more effectively
- organisations that promote and value health and wellbeing benefit from improved engagement and retention of employees, with consequent gains for performance and productivity. Highly engaged employees are less likely to report workplace stress, take fewer days sick absence [footnote 90] and make the most productive and happiest employees [footnote 91]
- employers lose out when people go sick: 139 million sick days were taken in 2015 [footnote 92] and the direct cost to businesses of sickness absence has been estimated at £9 billion per year. One survey put the median cost at £622 for each absent employee [footnote 94]
- the challenge will become greater as the working age population gets older – the workforce is projected to increase by roughly a million in the coming decade, with the majority of this increase in the 50 to 64 year old age group. [footnote 95] With health conditions and disabilities more prevalent in this group, employers will increasingly need to support their employees to remain healthy and manage their conditions if they are to make the most of their skills and experience
- by helping someone who is having difficulty in work due to illness or disability or intervening early in a period of sickness absence, employers can retain skilled employees and avoid additional recruitment costs. One study found that the average costs of replacing a worker earning more than £25,000 ranged between £20,000 and £40,000 [footnote 96]
- in addition to being bad for employers and the economy in general, a prolonged period of sickness absence is bad for individuals – early intervention is important, [footnote 97] the longer someone is away from work, the harder it is for them to get back to work, and the greater the risk of them missing out on all the benefits that work can bring [footnote 98]
- beyond the workplace, there are benefits to employers from investing in health and disability: households including disabled people have a combined spending power of around £212 billion [footnote 99] and we know that there is scope for businesses to better serve disabled consumers and communities and therefore capitalise on this spending power
The benefits of work experience placements
What’s not to like about hiring exceptional candidates? We’ve quickly learned that there can be a fabulous overlap between candidates with learning difficulties and exceptional employees – and any employer that isn’t interested in that overlap is missing out in a big way
Partner at a global law firm which works with Mencap to offer work placements and has recruited disabled people
Action already taken
158) Employers already have to take certain actions to comply with health and safety and equality laws and the government has recently appointed Matthew Taylor to lead an independent review to look at how current regulations may need to change in order to keep pace with the growing number of people who are registered as self-employed, on zero hours contracts or in temporary work. The review will look at job security, pay and rights and it will also examine whether there are ways to increase opportunities for carers, disabled people and older people.
159) Employers can also access government support to recruit and retain disabled people and people with health conditions in several ways:
- Disability Confident is a campaign that challenges negative attitudes to disability and disability employment and aims to help disabled people achieve their potential. We want the Disability Confident badge to become a recognised symbol of a good employer and for the list to be published so disabled jobseekers can find supportive employers
- Access to Work supports the disability-related needs of individuals in the workplace where they go beyond reasonable adjustments required under the Equality Act 2010. Last year Access to Work invested around £100 million to support over 36,000 disabled people. Additional funding announced in 2015 will mean that we will be helping over 60,000 people per year by the end of the Parliament. It has also seen a new focus to respond to those with hidden impairments like mental health conditions and learning disabilities
- Fit for Work provides a free, expert, impartial work and health advice service for employers and a targeted occupational health assessment for employees who are off sick for 4 weeks or more
- a Small Employer Offer is being rolled out to support smaller employers to create more job opportunities for disabled people and people with health conditions. Advisers based in Jobcentre Plus will work with employers to create tailored in-work support for employees, and provide advice and support for employers on workplace adaptations. Small employers can apply for a payment of £500 where employment continues for 3 months
- the Small Business Research Initiative aims to solve challenges by harnessing creative ideas from business. A competition launched in October 2016 looks at innovative ways small and medium-sized businesses can manage sickness absences and support early returns to work. A decision on successful bids will be made in January 2017
Embedding good practices and supportive cultures
160) We know that the right organisational culture and practices can enable more disabled people and people with health conditions to get into and stay in work. Many employers already have a strong track record in this area and we want to learn from their success and support others who need to do more. In this section, we set out the steps we will take to encourage inclusive cultures which have supportive employment practices by focusing on:
- the public sector leading by example
- addressing stigma and encouraging disclosure
- providing guidance and helping employers to learn from each other
- incentivising action and encouraging innovation
The public sector as an employer
161) The public sector is a large employer, and we are committed to ensuring that it leads the way in developing employment practices that allow disabled people and people with health conditions to flourish. There are a number of activities already underway to support this ambition. For example:
- all central government departments provide support to help all employees to stay well and manage their health conditions at work. This support includes a variety of programmes like occupational health support, online cognitive behavioural therapy, counselling support and the Civil Service reasonable adjustments service
- departments also have a variety of employee networks focused on health and disability. These are supported by senior managers and allow employees to support and learn from each other
- work is also underway in other parts of the public sector. The NHS employs 1.4 million people and NHS England, through its Healthy Workforce Programme is providing healthy food options, NHS health checks and voluntary initiatives such as weight watching to NHS employees. It is also working to improve recruitment of people with learning disabilities
162) This investment has proved effective in bringing down civil service sickness rates: for example, sickness rates in the Department for Work and Pensions have fallen from 11.1 days per staff year in 2007 to 6.2 in 2016. [footnote 100] However, it is clear that more needs to be done. Sickness absence in the wider public sector stands at 8.7 average working days lost per person compared to 6.1 in the Civil Service and 5.8 in the private sector. [footnote 101] Just under 12% of those who work in the public sector report having a disability, compared to an overall disability prevalence rate of 17% within society overall. [footnote 102]
163) We are committed to the public sector leading by example and will take action to:
- ensure public sector employers monitor and review their recruitment, sickness absence and wellbeing activities and take action where issues are identified. The ambition is that inclusive recruitment, tailored wellbeing and ill-health prevention activity to support and sustain people in work is the norm
- ensure all government departments are signed up as being Disability Confident by the end of the year. In addition, we will extend this expectation across other public sector employers over the next 12 months
- explore whether the use of procurement, which has been simplified and streamlined since 2015, can deliver wider objectives as well as value for money. For example, whether the Department for Work and Pensions’ initiative that encourages suppliers to provide employment and other opportunities to disadvantaged groups, including disabled people, could be expanded to other government departments or employers who receive public funding
Addressing stigma and encouraging disclosure
164) Of course any employer, whether public, private or voluntary and community sector, can only help someone start or stay in work if they are aware of a health condition or disability. Many conditions can be hidden and a person’s decision to disclose a disability or health condition to an employer can hinge on a number of factors. These include the extent to which they feel able to have a conversation with their manager, whether they fear disclosure might result in stigma or discrimination and the level of support they feel their manager, employer or colleagues more generally might give them. Broaching the subject of disability and health may feel too sensitive or off-limits for many managers and employers who fear saying or doing the wrong thing.
165) Yet in many instances open and supportive conversations about disabilities and health conditions will help employees and employers work together to enable someone to fulfil their potential at work, and remain in work if a condition fluctuates or develops. It is also important for employers to understand the profile of their workforce both through individual conversations and by analysing data they hold (for example on sickness absence and from worker health surveys) to plan for, and address, issues it may present.
166) Currently UK employers are not required to know the details about disability or sickness in their workforce. [footnote 103] If we are to realise our ambition of a healthy UK workforce with fewer people dropping out of work because of ill health, then we need to see all employers creating environments where employees feel able to disclose health issues and where employers act on that information to improve employee health. We would like to hear how best employers can be supported to create environments that support disclosure and what it is reasonable to expect employers to do as regards monitoring and acting on the health needs of their workforce.
Creating a culture that encourages disclosure: Barclays Bank
Since 2013, Barclays has run a “This is Me” campaign to tackle the awareness and understanding of mental health in the workplace. The campaign is designed to address the hesitancy to speak out about the topic itself, is driven and designed by employees with personal experience of managing their own mental health and wellness, and fully supported by Barclays disability network, Reach.
The campaign was built on individual experiences and has a three-fold approach – authentic stories of colleagues talking about their lives including their own mental health and wellness, identifying and addressing areas for improvement, for example through manager training and policy reviews, and an external commitment to breaking the stigma related to mental health issues by signing the Time to Change pledge. From just 9 stories, the campaign grew and to date over 160 stories have been shared by colleagues and they have seen more than 60,000 visits to the website.
As a result of the response from other businesses, Barclays has partnered with the Lord Mayor of London to expand its campaign to “This is Me in the City”. This city-wide campaign has encourage over 70 London based organisations to launch a similar ‘This is Me’ style campaign within their own organisations.
Mark McLane, Global Head of Diversity and Inclusion at Barclays, said:
It is clear that authentic story-telling truly engages people and, when led by colleagues, it leads to real inclusion and builds a sense of trust. However daunting it may seem at the start, this approach encourages more people to speak out about their own experiences. Strong leadership and support from well informed charity partners has proved to be invaluable.
Providing and publicising guidance and supporting employers to work together
167) Employers may be prevented from creating a supportive culture by a lack of expertise, support or capacity. This can be a particular issue for smaller businesses, where they might be facing the issues for the first time. There is already a wealth of information about how employers can support disabled people and people with health conditions, but the extent to which it is known about, used or found useful is unknown. So we want to consider how we can bring this information together, make it accessible and support employers to work together.
As well as guidance, we want to provide more information on the business case for employers to be more inclusive for their employees and their customers. Although the evidential case for employer action on health and work is already compelling, we believe there is scope for it to be stronger still, and particularly so for smaller employers. We believe there is a case for research to build and illustrate the business case for employer action in a number of areas. These could include: the benefits of wellbeing, prevention and rehabilitation activities, including occupational health support for employers and others; the return on investment for employers who purchase income protection insurance; and effective recruitment methods across different disabilities and health conditions.
168) Many organisations have recommended consolidating some of the evidence on the business case for change, as well as practical information, into a one-stop shop for employers. This could include case studies, examples of reasonable adjustments as well as running awareness sessions. We agree that there could be benefits to this and so we will undertake research to find out what employers would find most useful in a one-stop shop on health and work. We also seek your views on this as part of the consultation.
169) Partners have also suggested that government should be more proactive in making businesses aware of the information and support that is available to them, rather than expecting them to find it themselves. We agree, and so we will work with partners to develop and run information campaigns on key topics around health and work to help employers access existing information and adopt good practices. We want to hear from employers about how best to do this, for example, who employers are influenced by and how to reach different sectors.
Realising potential
170) Seeing more disabled people and people with health conditions get into work is important but on its own it is not ambitious enough – we want to see these employees reaching their full potential, making their fullest contribution and going as far as their talent and drive can take them. Senior, executive and board positions should be within their reach.
171) Evidence suggests that seeing employers have success in hiring disabled people and people with health conditions can be a powerful way of motivating other employers to act. [footnote 104] Employer-employee networks and business-led initiatives therefore have a big role to play in influencing employers to recognise the talents of disabled employees and employees with health conditions and creating the momentum to support these employees excel.
172) Some organisations already support networks that stimulate the exchange of new ideas and good practices. The Business Disability Forum brings together business people, disabled opinion leaders and government while Purple Space focuses more specifically on employee networks, providing learning, networking and professional development opportunities.
173) Business-led initiatives can also have great influence. For example, from 2010 to 2015, the number of women on the boards of FTSE 350 companies more than doubled, following the business-led Lord Davies Review set up by Government into women on boards. The Davies Review worked with key stakeholders including businesses, investors and executive search firms, and we saw the target for 25% women on boards of the FTSE 100 by 2015 exceeded, and all-male boards in the FTSE 100 eliminated. Work continues under the new Hampton-Alexander Review, with the increased target for 33% women on FTSE 350 boards by 2020.
174) The Review created a culture change in business, with companies recognising that achieving a better gender balance at these levels will not only help to close the gender pay gap, but companies will also benefit from better decision making, accessing the widest talent pool and being more responsive to the market. Increasing the number of women at senior levels is about improving performance and productivity.
175) We believe there is much more we can do to achieve the same results for disabled people. Although representation of disabled people and people with health conditions in senior positions is unknown (noting employers are not required to collect data on this), it is reasonable to surmise that with a disability employment gap of 32 percentage points, representation at senior levels is also likely to be lacking. So we want to know what the role of employers and government should be in helping disabled people and people with long-term health conditions progress in work and secure senior roles.
176) We want to see businesses leading the way and creating the same sort of momentum as they have to increase the number of women on boards. To achieve this, we will establish a Disability Confident Business Leaders Group who will work alongside ministers and officials to increase employer engagement around disabled employment, starting with FTSE 250 companies.
177) In addition, we think there is scope to do more, especially among small and medium-sized employers, to establish supportive networks between employers, employees and charities around health and work, and would like your views on the best way of doing this.
Incentivising action and stimulating innovation
178) We want to know whether financial or other incentives would encourage employers to try new and creative things to support more disabled people and people with health conditions in work. The reality is that in order to halve the disability employment gap, all things being equal, we need to see around a million additional disabled people entering work and we want to explore how we can incentivise employers in creating new roles for disabled people and people with long-term health conditions. Several financial incentive schemes around health and work and stimulating employment more generally already exist:
- to encourage employers taking action to prevent employee ill health, employers can claim tax relief on up to £500 of the cost of treatment for an employee recommended by an occupational health practitioner and can claim corporation tax relief on their premiums when they purchase income protection insurance products for their employees
- to encourage job creation, particularly among young people, the Employment Allowance scheme allows businesses to employ 4 adults, or 10 18–20 year-olds, full-time on the National Minimum Wage without paying employer National Insurance contributions
- a small grant promoting the employment of disabled people and people with health conditions is being trialled through the “Small Employer Offer” mentioned at paragraph 159 above. Small and medium-sized enterprises who sustain such employees at work for 3 months will receive £500 to provide on-going mentoring and support for employees
179) We recognise that the evidence about the effectiveness of such initiatives in sustaining people in or supporting them into employment is mixed. However we believe that, given the scale of the challenge ahead of us, it is right to consider if they have a role to play.
180) Partners have suggested, for example, using financial incentives to encourage large employers to share their HR, occupational health or employee assistance services with smaller employers; or encouraging employers to provide occupational health support to their employees. Schemes like this may help build capacity among small and medium-sized employers.
181) More broadly, we know that employer indexes such as Stonewall’s Equality Index can support changes in employer behaviours. [footnote 105] The mental health charity Mind launched its Workplace Wellbeing Index earlier this year. [footnote 106] It may be helpful for the Disability Confident scheme to include an index of employers on how inclusive of disability they are. We would like your views on whether there is a role for these and other incentives in helping more disabled people and people with health conditions to move into or stay in work.
Your views
- What are the key barriers preventing employers of all sizes and sectors recruiting and retaining the talent of disabled people and people with health conditions?
- What expectation should there be on employers to recruit or retain disabled people and people with health conditions?
- Which measures would best support employers to recruit and retain the talent of disabled people and people with health conditions? Please consider:
- The information it would be reasonable for employers to be aware of to address the health needs of their employees?
- The barriers to employers using the support currently available
- The role a ‘one stop shop’ could play to overcome the barriers
- How government can support the development of effective networks between employers, employees and charities
- The role of information campaigns to highlight good practices and what they should cover
- The role for government in ensuring that disabled people and people with health conditions can progress in work, including securing senior roles
- The impact previous financial, or other, incentives have had and the type of incentive that would influence employer behaviour, particularly to create new jobs for disabled people?
- Any other measures you think would increase the recruitment and retention of disabled people and people with health conditions.
- Should there be a different approach for different sized organisations and different sectors?
- How can we best strengthen the business case for employer action?
Respond to this consultation online
Moving into work
182) A supportive inclusive culture is demonstrated in practice at 2 critical points – the recruitment of disabled people and people with health conditions, and how they are supported to stay and progress in work. In this section, we set out some existing good practice for inclusive recruitment and consider how we might improve existing government schemes to support employers to recruit disabled people and people with health conditions.
183) The Disability Charities Consortium has identified that employers who are good at recruiting disabled people consider the challenges such candidates may face and take innovative steps including offering ‘working interviews’ and providing supported internships and apprenticeships to help disabled people gain skills and experience. [footnote 107] Disability Confident suggests other ways of making recruitment practices more inclusive include making online recruitment more accessible and providing additional training for recruiting managers. We would like to establish what good practice employers are already taking and how government schemes can support this.
184) There are already a number of government schemes that support employers or employees to manage health conditions and disabilities at work, such as Disability Confident and Access to Work. Various organisations have suggested ways in which the remit and operation of some of these schemes could be changed to support employers to recruit more disabled people and people with health conditions. We would like to hear about the ways these schemes could be enhanced to help even more disabled people move into work.
Your views
- How can existing government support be reformed to better support the recruitment and retention of disabled people and people with health conditions?
Respond to this consultation online
Case study – Jamie
Jamie joined North One Television on a one year-internship leading up to the Rio Paralympics, where he then joined the Channel 4 production team in Brazil. The objective of the internship at North One was to give Jamie direct exposure to sports production, and to this end we placed Jamie within our MotoGP team, producing coverage for BT Sport of the world motorcycle racing championship.
Channel 4 has been leading the way in creating opportunities for people with disabilities in the media. But the main challenge (and one that we have whole-heartedly supported) is to accept that people with disabilities simply want to achieve what the rest of us have – a career with prospects that can provide an income to allow them to plan for and support their long-term future.
This requires a management and workforce to accept and share the challenges that a person with disabilities has, to feel able to speak openly about them to make the workplace as practical as possible, but then – crucially – to put the disability second and the ability first.
Jamie is a wheelchair user so a number of workplace adjustments took place (accessibility issues and so on). But that was dealt with. Jamie then got stuck in to his role on MotoGP and has proven himself to be an extremely capable Researcher/Assistant Producer, to the extent that he will be returning after the Paralympics to join our team beyond this internship.
There are no favours here, no preferential treatment or tokenism. Jamie has earnt this position because he is a good Researcher/ Assistant Producer. I think this is a fundamental issue, but it requires open and frank discussion about what a disability means in practical terms and then to focus on the job, as you would with any other employee.
But the process of making adjustments to the workplace and engaging employees in that process makes for a far more accepting and understanding wider workforce, shifting the general focus from disability to ability. Account from Robert Gough, North One Television.
Staying in or returning to work
185) A person who falls ill in work or who has an existing condition or disability that worsens may face a critical point where the right support from their employer can make all the difference between them remaining and flourishing in work or struggling to cope and falling out of work. An inclusive culture, where health is promoted and action taken to prevent or manage ill health supports the interests of both employer and employee. Yet some employers focus on compliance with health and safety legislation without necessarily considering wider health and wellbeing.
186) A true preventative approach requires a focus on both physical and mental health and support for those having difficulty in work due to illness or those who have gone off sick. In this section, we consider:
- how employers can proactively promote health and wellbeing and preventing ill health
- managing sickness absence and the role of Statutory Sick Pay in supporting phased returns to work
- how insurance products could better support employers to manage the potential costs of ill health
Promoting health and wellbeing and preventing ill health
187) Given the time most working people spend in the workplace it should be a key place to support health and wellbeing. Investing in the health and wellbeing of employees can bring business benefits by reducing sickness absence rates and improving productivity. To be effective, initiatives will need to be tailored to the organisation, although various organisations and studies have identified several core components which positively embed health and wellbeing in the workplace. These include:
- the right culture and leadership such as supportive company values and standards, the right working policies and practices, a commitment to health and wellbeing at all levels but particularly among senior leaders and effective communication and consultation with employees
- the right physical environment through safe and appropriate working conditions
- effective people management where managers have the confidence and capacity to deal with workplace health and wellbeing issues. Where in place this has been linked with improved performance and wellbeing; where it isn’t it creates pressure among those who continue to work despite illness [footnote 108] and has been linked with stress, burnout and depression [footnote 109]
188) These are not new concepts and build on the key elements of effective health and safety management. Advice and support for employers on how to embed these elements is readily available (although we are considering how we can ensure it is more effectively organised and made available) and there are many practical ways employers can support workforce wellbeing.
189) Interventions should be based on the specific health needs of each organisation’s workforce and employers may find it helpful to work with their local NHS and local government to identify needs and deliver interventions. These could include initiatives like healthy food, support with weight management, stop smoking schemes or mental health or physical opportunities like cycle-to-work schemes. Employee assistance providers can also help employees with wider life issues that can impact health such as bereavement, domestic violence, debt and relationships.
190) As part of creating healthy workplaces employers can do a great deal to help and encourage their staff to be physically active. The physical and mental health benefits of physical activity are well established, with Public Health England’s Everybody Active Every Day report from 2014 setting out the evidence and making a powerful case for creating an active society with active environments. The benefits of physical activity are most pronounced for those who are currently inactive. Disabled people and those with serious health conditions are much less likely to be physically active than others.
191) The government’s sport strategy, Sporting Future: a New Strategy for an Active Nation, which the Department for Culture Media and Sport published last December, set out the benefits for employers and staff of a physically active workforce, including greater levels of staff engagement and commitment to the organisation. Government will be working with others to establish an employers’ network to promote physical activity. In addition, as part of the public sector setting an example, we have established a Civil Service Physical Activity Workplace Challenge which is currently being piloted across a number of departments.
192) There are various assessment and accreditation schemes available to help employers identify suitable actions to take on workforce wellbeing and standards endorsed by Public Health England. Schemes include Liverpool City Council’s Workplace Wellbeing Charter, [footnote 110] London’s Healthy Workplace Charter [footnote 111] and the North East’s Better Health at Work Award. [^]112 The Health and Safety Executive’s Stress Management Standards also provide well-evidenced support with mental health issues. [footnote 113]
193) We want employers to do more to promote health and wellbeing and believe there is a place for a proactive good practice information campaign. To support this, we would like to know what good practices are already taking place and seek your views on what the campaign might cover below.
Case study: Hatstand Nelly
Hatstand Nelly is a hair and beauty salon in Aberdeen with 18 employees. In 2007, the business introduced an incentive scheme to encourage higher levels of attendance. The quarterly bonus of £75 for full attendance paid for itself. They also looked at the reasons for absence and helped staff to avoid back problems with a programme of talks and activities at work. A qualified physiotherapist, gave a talk about the long-term effects of poor posture which was followed up with a pilates lesson in the salon helping the team to learn practical skills to improve their fitness levels.
As a result of all this work, sickness absence at Hatstand Nelly reduced by around 60% and the Manager Lorraine Watson commented that the new culture of wellbeing showed in the atmosphere at the salon and that customers had picked up on it too. [footnote 114]
194) Occupational health services can help employers promote health and wellbeing and also support employees to manage a disability or health condition at work. Although our understanding of the effectiveness of different types of occupational health support in different settings is incomplete, there is some evidence that providing such support can lead to reduced sickness absence, boosted productivity and increased employee satisfaction. [footnote 115]
195) There is scope for employers to be doing significantly more to provide this support in the workplace. A 2014 survey found 72% of public sector employees had access to occupational health support compared to 52% in the voluntary sector and 39% in the private sectors. [footnote 116]
196) Of private sector employers, 80% of large employers provide occupational health provision, demonstrating their recognition of the role it can play. Yet even then awareness and usage appears inconsistent – only 65% of employees of large employers claimed to have occupational health access. In addition, only around a third who had been in work prior to claiming Employment Support Allowance reported having access to occupational health support at work. [footnote 117]
197) Chapter 5 discusses our vision for occupational health in more detail, but we would like your views on how we can encourage more employers to provide occupational health support.
Managing sickness absence and the role of Statutory Sick Pay in supporting phased returns to work
198) Supportive absence management processes are key to helping people stay in work or return to work after a period of sickness absence. Offering periods of flexible working in particular may help people to manage or recover from a health condition. This is in the interests of employers who benefit from keeping employees in work and avoiding the costs associated with lower productivity, disruption and replacing employees. However we know that too few people return from a period of sickness absence. 45% of Employment and Support Allowance claimants who had worked at some point in the 12 months before their claim had a period of sickness absence before they left work. [footnote 118]
199) We know that the longer someone remains out of work the less likely they are to return. So keeping up contact between employers and employees is critical in retaining a person in employment. Furthermore, evidence shows that phased returns to work from sickness absence can see employees return quicker and stay in employment longer. [footnote 119]
200) Some countries take the approach of mandating contact between employers and employees when the latter is off with ill health, requiring employer action to support employees back into work or ultimately to pay for sickness or benefit costs if this is not achieved. Such approaches would represent a shift to the current UK landscape with new requirements placed on employers where retention is unsuccessful, although success in sustaining these employees in work could bring gains from retained skills and experience and avoided replacement costs.
International approaches to preventing and addressing sickness absence [footnote 120]
Several countries take a different approach by mandating employer action to manage sickness absence. In Norway and the Netherlands within or by the first 8 weeks of absence an employer must draw up a return-to-work plan with the employee. In Norway, this must be submitted to the national insurance office on request. In the Netherlands, where employers may have to pay sickness benefits for up to 2 years, the plan must include evaluation criteria which is reviewed every 6 weeks and at the 12 month stage, including a forward look.
Denmark similarly requires employers to monitor and address issues in the work environment and its Working Environment Authority visits employers unannounced. If violations are not addressed within 6 months, fines can be imposed and the performance of employers is published as a further incentive to employers to address issues.
Several countries also either require or encourage employers to provide preventative or rehabilitative support, often in the form of occupational health support. Finland, the Netherlands and Sweden have all had varying approaches to this, some supported with government subsidies.
201) Although it is likely that many employers are already having supportive contact with their employees who are off with illness, we also know that managers can shy away from such conversations because of a lack of confidence, lack of knowledge or a feeling that it is not their role. We also hear anecdotally that some employers feel unable to have such conversations during periods they are paying Statutory Sick Pay, or during the period specified on a fit note, because they perceive these as allowances of leave that people are allowed to exhaust.
202) We are clear that the systems around fit notes and Statutory Sick Pay should not discourage conversations between employers and employees, or the exercise of flexibilities, that support employees to remain in or return to work. We discuss the issues around fit notes in chapter 5 but believe that we should reform the Statutory Sick Pay system so that it better encourages supportive conversations and phased returns to work.
203) Currently, Statutory Sick Pay is paid by employers when a person does no work at all. [footnote 121] This means that people who are low paid may be deterred from returning to work on reduced hours because they would not qualify for Statutory Sick Pay and their earnings may prove to be less than the amount provided by Statutory Sick Pay. Or alternatively it may encourage them to return to their usual hours before they are ready, potentially leading to further absence or falling out of work altogether.
204) One approach to reforming Statutory Sick Pay to allow phased returns would be that where an employee would earn less than the Statutory Sick Pay rate of £88.45 per week in returning on reduced hours, the employer would be able to ‘top up’ their wages to the Statutory Sick Pay level (see example below).
205) This would mean that the maximum amount of Statutory Sick Pay and/or pay spent by employers and received by employees during a period of transition back from sickness remains constant. It would also allow for an earlier, albeit phased, return to work which could be good for the employee and employer. Of course this approach would not prevent an employer from paying Statutory Sick Pay on a pro-rata basis alongside wages. In this case a person’s income would reflect a proportion of Statutory Sick Pay for hours not worked, and paid wages for the period worked, potentially offering an income above the basic allowance, and a greater incentive for the individual to return to work as part of a phased return.
206) As regards contact during sickness absence, we would like to see regular conversations between employers and their employees who are off ill to agree steps that can be taken to support a return to work. We seek views on what it would be reasonable to expect of employers and employees in this regard.
Example
An employee works 25 hours a week for £7.20 per hour or £180 per week.
If they went on a period of sickness absence they will need to return to work for at least 13 hours in order to compensate for the loss of £88.45 in Statutory Sick Pay(13 hours x £7.20 = £93.60).
If the employer and employee came to an agreement for a partial return to work of 10 hours per week, the employer would ‘top up’ the salary to the Statutory Sick Pay level. For example, the employer would pay £72 in wages (£7.20 x 10 hours) plus £16.45 to ‘top up’ to the Statutory Sick Pay rate of £88.45.
Encourage better provision by the insurance industry, and take-up by employers, of income protection insurance
207) There are various insurance policies that employers and employees can take out to support them in addressing the risks and impacts of ill health: life insurance, private medical insurance, critical illness cover or personal accident or sickness insurance. This final element can be taken out by individuals, in the form of Individual Income Protection, or by employers on behalf of their employees as Group Income Protection.
208) Group Income Protection insurance generally provides 3 elements: a financial element which pays an income to employees who cannot work because they are ill or injured after an agreed period (usually 6 months); ill health prevention programmes; and specific support for employees and the employers for example physiotherapy, mental health support and HR support.
209) The benefits of Group Income Protection to employers and their staff may vary, but analysis by the Centre for Economics and Business Research indicates that employees who have access to early intervention and rehabilitation services and use them tend to have shorter duration long-term absences compared to those that do not. On average, the duration is shorter by 16.6%. [footnote 122]
210) Although Group Income Protection policies have the potential to support employers to retain disabled employees and employees with health conditions, uptake is low: only 7-8% of the working population is covered by such a policy. Coverage is particularly low among small and medium-sized employers. In part this might be because some insurance providers do not offer products to very small businesses, but cost and awareness of the products are also thought to be a factor (between £250–£450 per employee per year).
211) As this paper sets out, we want to see employers doing more to invest in their employees’ health and wellbeing and to thereby reap the benefits that such investment brings. We think group income protection insurance policies have a much greater role to play in supporting employers in taking this action and therefore want to explore why larger employers are not making better use of these products and what would encourage them to do so.
212) Smaller employers are also important: they represent the vast majority of UK businesses and employ around 36% of the UK workforce. We are working with the insurance industry to explore the viability of group income protection insurance products for smaller employers and, if there is sufficient interest, could look at how such employers could be supported to pool resources to purchase existing products as a collective.
213) We therefore want the insurance industry to develop group income protection products that are affordable for, and tailored to meet the needs of, smaller employers, including micro businesses, and for them to raise awareness and make access to such products easier.
Your views
- What good practice is already in place to support inclusive recruitment, promote health and wellbeing, prevent ill health and support people to return to work after periods of sickness absence?
- Should Statutory Sick Pay be reformed to encourage a phased return to work? If so, how?
- What role should the insurance sector play in supporting the recruitment and retention of disabled people and people with health conditions?
- What are the barriers and opportunities for employers of different sizes adopting insurance products for their staff?
Respond to this consultation online
Conclusion
214) This chapter has considered what can be done by or with employers to support our ambition of more disabled people and people with health conditions getting into and staying in work. We want to see more employers providing the right support at the right time, and taking a more proactive approach to the health and wellbeing of their workforce for the benefit of their employees and their business.
215) If someone does fall out of work because of their health or disability, they are likely to be facing a stressful and challenging period in their lives. It is essential that, at the appropriate time, they can access the integrated health and employment support they need to manage their health condition and move back towards work, as we discussed in chapter 2. This, and the role of health and high quality care, is discussed in the next chapter.
Summary of consultation questions
Embedding good practices and supportive cultures
- What are the key barriers preventing employers of all sizes and sectors recruiting and retaining the talent of disabled people and people with health conditions?
- What expectation should there be on employers to recruit or retain disabled people and people with health conditions?
- Which measures would best support employers to recruit and retain the talent of disabled people and people with health conditions? Please consider:
- The information it would be reasonable for employers to be aware of to address the health needs of their employees?
- The barriers to employers using the support currently available
- The role a ‘one stop shop’ could play to overcome the barriers
- How government can support the development of effective networks between employers, employees and charities
- The role of information campaigns to highlight good practices and what they should cover
- The role for government in ensuring that disabled people and people with health conditions can progress in work, including securing senior roles
- The impact previous financial, or other, incentives have had and the type of incentive that would influence employer behaviour, particularly to create new jobs for disabled people?
- Any other measures you think would increase the recruitment and retention of disabled people and people with health conditions.
- Should there be a different approach for different sized organisations and different sectors?
- How can we best strengthen the business case for employer action?
Moving into work
- How can existing government support be reformed to better support the recruitment and retention of disabled people and people with health conditions?
Staying in or returning to work
- What good practice is already in place to support inclusive recruitment, promote health and wellbeing, prevent ill health and support people to return to work after periods of sickness absence?
- Should Statutory Sick Pay be reformed to encourage a phased return to work? If so, how?
- What role should the insurance sector play in supporting the recruitment and retention of disabled people and people with health conditions?
- What are the barriers and opportunities for employers of different sizes adopting insurance products for their staff?
5: Supporting employment through health and high quality care for all
Chapter summary
In this chapter we look at how work can make a significant contribution to someone’s health. We explore:
- how we can promote health and prevent ill health
- how we can ensure an individual can access health services, which consider their employment needs, particularly for common conditions which affect an individual’s ability to work – especially musculoskeletal and mental health
- how we can strengthen the role of occupational health and related professions and services, so that people’s health and employment needs are considered together
- how we need to create the right conditions for joined-up support
- how we can reinforce the recognition across the health and care system that work can promote good health – that work is in itself a ‘health outcome’
Introduction
216) By now, we hope that the case is clear that appropriate of work can have a positive effect on an individual’s health and that having the right health support can have a positive effect on an individual’s ability to work and progress in their career. While many factors affect a person’s health and employment, in this chapter we concentrate on how people, whether in or out of work, can access the right health and social care support in the right place and at the right time to enable them to enjoy the benefits of work.
217) We know we still have a long way to go to ensure that people get the right health and employment support when they need it. Services do not always work well together. Decisions can be taken in isolation rather than recognising that we may have different needs at different times, and that work and health are importantly linked. [footnote 123] This is frustrating for people who are forced to navigate complex and fragmented systems and who may miss out on support.
218) We also know that the health service is facing significant challenges of preventable ill health and health inequalities and variable quality of services, as set out in the NHS Five Year Forward View which set out a vision for the future of the NHS. The Five Year Forward View highlighted how important it is that we get serious about prevention, deliver the right care in the right place, and build a more engaged relationship with patients, carers and citizens.
219) We want to look at health in the broadest sense and do more to encourage employers, Jobcentre Plus staff, and those working in the voluntary and community sectors to support health through promoting health, preventing ill health, early intervention and ensuring access to joined-up services. Individuals, as partners in their care, can also do more to look after their own health and manage their care. It is when these groups work together that we will see real benefits for individuals, for the health of the population, and for the economy.
220) In this chapter, we set out our plans to improve care and support so that it starts with the individual, and meets their health and employment needs. This isn’t something government can achieve on its own – those working in health services and employment support, especially commissioners, will play a critical role – so we also want to hear how we can support and encourage the changes we wish to see.
221) This chapter focuses on key opportunities when the right health and care support can make a difference to, and be considered alongside, an individual’s employment needs. These include:
- the importance of promoting health, and recognising that work can make a significant contribution to someone’s health
- ensuring an individual can access health services, which consider their employment needs, particularly for common conditions which affect an individual’s ability to work – especially musculoskeletal and mental health conditions
- strengthening the role of occupational health and related professions and services, so that people’s health and employment needs are considered together to help them get into, and stay in, work
222) For the right joined-up support to be available at each of these times, this chapter then explores how we need to create the right conditions, and reinforce the recognition across the health and care system that appropriate work can promote good health – that work is in itself a ‘health outcome’.
223) Throughout this chapter is the fundamental principle that individuals are partners in their care, and that innovative approaches, including digital ones, can help people look after their health and manage their own care.
Action already taken
224) The government has already taken steps to support work through measures to improve health. We have:
- put in place ill-health prevention measures including the diabetes prevention programme, national immunisation and screening programmes and public health campaigns such as the ‘One You’ campaign
- funded local authorities to commission a range of public health services to improve the health of their populations, including health checks, stop smoking services and drug and alcohol treatment services
- invested in early intervention for psychosis, and improved access to talking therapies
- set out plans to increase recurrent funding in primary care, including to support mental health in primary care, by an estimated £2.4 billion a year by 2020 to 2021 and a 5-year ‘turnaround’ package of £500 million
- encouraged health and care services to plan their Sustainability and Transformation Plans [footnote 124] on ‘footprints’ which bring together health and care leaders to support the delivery of improved health and care based on the needs of local populations
Promoting health
225) Health issues can prevent people from getting into work, and fulfilling their role at work, and can be a factor in people falling out of employment or taking early retirement. But this does not always have to be the case and there are several areas where we could do more to prevent ill health or disability becoming a barrier to people achieving their potential in work and in life in general.
226) There are primarily 2 types of health conditions that impact on an individual’s potential to participate in work and wider society:
- a long-term condition which may be fluctuating but once developed may last throughout an individual’s life such as diabetes, arthritis or some mental health conditions. Some conditions, may of course, be present from birth
- a sudden health event like a heart attack or a broken leg where the event happens and then there is a recovery phase to either full health or a new normal for the individual
227) Some conditions are preventable, or manageable, and promoting healthy lifestyles can prevent or delay conditions developing. The workplace can play an important role in promoting health, and minimising risks to health, for example through encouraging staff to take action on obesity and smoking, as set out in chapter 4. Where an individual experiences health issues, such as a sudden health event or a long-term condition, there is the potential for earlier action to support individuals better to remain active in society and participate in work to retain their financial independence and the health benefits of employment.
228) Preventing health-related worklessness means taking a proactive approach to engaging and supporting people to talk about their concerns about work and signposting and supporting them to access help or reasonable adjustments.
229) Clinicians, patient support groups and charities all have a role to play in supporting people with health conditions to achieve their potential. For example, simply asking about work in routine clinical consultations may open an opportunity to identify individuals who might be at risk of falling out of work due to ill health where this could be prevented. Indeed a fear of falling out of work may make a health condition worse.
230) Helping people achieve their potential is important for everyone. For young people with long-term conditions, mental health issues and physical and sensory impairments, there are opportunities to integrate careers advice, education support and clinical management to give this group of young people the best start in life and the best chance at gaining employment.
Improving discussions about fitness to work and sickness certification
231) When an individual first becomes ill, or an existing condition worsens, their first port of call is usually their general practitioner (GP). Discussions about work and health and an assessment of a patient’s fitness for work provide an opportunity for doctors to discuss ways in which a patient may be helped to stay in work by, for example, advising on workplace adjustments or a phased return to work. It may also lead to a referral to Fit for Work for patients who are off sick for 4 weeks or more.
232) The Statement of Fitness for Work, or ‘fit note’, was introduced in 2010 to encourage fuller discussions about work and health. Fit notes are used to support payment of Statutory Sick Pay by employers or as medical validation to make a claim to health-related benefits. The information they provide can be used by employers or work coaches within Jobcentre Plus to support a return to work.
233) The fit note has the potential to be a key tool to identify a person’s needs and help them to manage their condition and stay in or return to work whilst working with an employer or work coach. This could shorten periods of sickness absence and ultimately reduce the need for repeat fit notes, reducing pressures on GPs and potentially reducing costs over the longer term. It can also act as a prompt for the GP to consider a referral to Fit for Work if appropriate.
234) However, although over 60% of GPs agree or somewhat agree that the fit note has improved the quality of their return to work discussions with patients, and over 90% agreed that helping patients to stay in or return to work was an important part of their role, [footnote 125] the fit note is not fully achieving what it set out to do. Although the fit note includes the option for the doctor to use a ‘may be fit for work subject to the following advice’, this option is rarely used.
235) Decisions on whether a person is able, or not able, to work may be made without the recognition that many people can work with the appropriate support. This means that opportunities to influence someone’s understanding around what work is possible for them to do can be lost, from the first GP consultation onwards. This increases the risk that the individual falls out of work altogether or moves further away from securing employment.
236) Evidence from GPs suggests that they may, on occasion, find it difficult to refuse to issue a fit note. The value of the initial discussion between a healthcare professional, individual and employers about the work an individual can do would then largely be lost, with the fit note process seen as an administrative burden rather than an opportunity to provide work and health-focused support.
237) We want to ensure that individuals are better supported to understand their health condition, treatment needs and how this might impact on their ability to work, and employers need access to information which will enable them to support their staff. That means developing a system where:
- healthcare professionals have the right skills and knowledge to provide early advice about functional ability to work and the ability to provide, or easily access, the right support so that individuals, employers and work coaches have the necessary information at the earliest opportunity to expedite treatment and support
- we reinforce the beliefs of the primary and secondary care workforce that work is important for health and encourage them to take a leading role in changing behaviours – so that work becomes an integral part of an individual’s life, where appropriate
- healthcare professionals feel confident to use their skills and knowledge to issue fit notes only when appropriate and make full use of the “may be fit” option that is available to them
- healthcare professionals recognise the value of a referral to Fit for Work for occupational health advice and return to work support and make referrals routine for eligible patients when appropriate
- we continuously learn about people’s health and employment needs so that we can gather evidence and target future investment and support in the most effective way
238) The government intends to review the current operation of the fit note, and in line with the General Practice Forward View published in April, review whether fit note certification should be extended from doctors in primary care and other settings to other healthcare professionals. The review will look at the current system and whether it meets the needs of its users – doctors and other healthcare professionals, employers, patients/claimants and the benefits system.
Your views
239) We want to work across all sectors to fully review the current fit note certification process. We want to know your views on the following:
- How can we bring about better work-focussed conversations between an individual, healthcare professional, employer and Jobcentre Plus work coach, which focus on what work an individual can do, particularly during the early stages of an illness/developing condition?
- How can we ensure that all healthcare professionals recognise the value of work and consider work during consultations with working age patients? How can we encourage doctors in hospitals to consider fitness for work and, where appropriate, issue a fit note?
- Are doctors best placed to provide work and health information, make a judgement on fitness for work and provide sickness certification? If not, which other healthcare professionals do you think should play a role in this process to ensure that individuals who are sick understand the positive role that work can play in their recovery and that the right level of information is provided?
- Regarding the fit note certificate, what information should be captured to best help the individual, work coaches and employers better support a return to work or job retention?
- Is the current fit note the right vehicle to capture this information, or should we consider other ways to capture fitness for work and health information? Does the fit note meet the needs of employers, patients and healthcare professionals?
Respond to this consultation online
###Mental health and musculoskeletal services
240) Too many people with mental health or musculoskeletal conditions fall out of work each year, many end up on sickness benefits and few return to work. Individuals with such conditions represent 62% of people claiming Employment and Support Allowance, huge cost and unfulfilled potential. [footnote 126]
241) A key factor which could help address this problem is timely access to support. Evidence shows that offering early support to individuals, including people with a health condition or a disability, can improve their chances of getting back to work. [footnote 127] Yet too often services for people with common conditions are not available when an individual needs them.
Mental health services
242) Almost 1 in 5 working age people have a common mental health condition in England rising to almost 1 in 2 among people on out-of-work benefits. [footnote 128] There are around 1.8 million [footnote 129] out-of-work disabled people of working age with a mental health condition in the UK. Mental health conditions are the most commonly reported primary conditions among the total 2.4 million people who claim Employment and Support Allowance; around 1.2 million cite a mental health condition as their primary health condition but many of them may not be accessing the support that might help them. [footnote 131] Having a mental health condition is also associated with many physical health conditions. [footnote 130] The Work, Health and Disability Green Paper Data Pack which accompanies this paper provides more information about the population with mental health conditions. [footnote 132]
243) As the Five Year Forward View for Mental Health sets out, the evidence is clear that improving outcomes for people with mental health problems helps them to improve wellbeing and build resilience as well as reducing premature mortality, but service provision can be patchy and access difficult.
244) The increasing access to psychological therapies programme has been successful in increasing access to NICE-approved treatments for common mental health conditions. But there is variation across England in terms of access to these talking therapies.
245) The government will further increase access to psychological therapies and improve how these services join up with other services. By 2020/21, at least 25% of people (or 1.5 million) with common mental health conditions will access services each year. Alongside this we will consider how individuals at risk of job loss or recently unemployed can gain early access to talking therapies to prevent worsening health and drift away from the labour market.
246) We are more than doubling the number of employment advisers in talking therapies to help people in that service retain, return to and secure employment. This will be a significant boost to the talking therapies workforce and ensure many more services have a clear employment offering that can improve pathways between employment services and talking therapies services. We are evaluating the impact of this provision and the elements that bring greatest results. We also have a number of trials underway to identify new and innovative ways mental health and employment services could support people to return to work.
247) The talking therapies programme has demonstrated that we can collect and publish extensive data about outcomes. Such data is an important driver to improve outcomes. We would like to see this go further, with data on employment status routinely recorded and published as a matter of course across all mental health services.
Musculoskeletal services
248) Over 32 million of the 139 million working days lost to sickness absence in 2015 were due to some form of musculoskeletal condition, [footnote 133] and around 2.1 million of the 3.8 million working age disabled people out of work suffer from some form of musculoskeletal condition [footnote 134] which may be associated with other health conditions. 309,000 of the total 2.4 million people on Employment and Support Allowance report a musculoskeletal or a connective tissue condition as their main disabling condition. [footnote 135]
249) Despite the impact on individuals of musculoskeletal problems, some evidence suggests that waiting times for musculoskeletal services can vary from between 4 to 27 weeks [footnote 136] depending on where the person lives, and Arthritis UK highlighted in their 2014 report that only 12% of people with musculoskeletal conditions had a care plan. [footnote 137] This is unacceptable, when we know that earlier diagnosis and treatment of musculoskeletal conditions would, in many cases, prevent further deterioration in the condition and enable the individual to stay in work. [footnote 138]
250) We are supportive of new ways of providing musculoskeletal care, which are being developed in a number of local areas. These include physiotherapists working from general practice surgeries and self-referral to musculoskeletal services. These have benefits of affording patients wider access, lowering levels of work absence and empowering patients to self-manage their care.
251) A preventive approach and encouraging early self care and exercise is often appropriate to avoid over-medicalising some conditions for which the best treatment may be self-care and a return to normal activities, often including work, with workplace adaptations where needed.
Case study: Physiotherapy First
Physiotherapy First is a joint initiative between 2 NHS providers, Cheshire and Wirral Partnership NHS Foundation Trust and the Countess of Chester Hospital Foundation Trust.
36 GP surgeries in the West Cheshire area now provide their patients with the choice of seeing a physiotherapist when they first contact the practice with musculoskeletal symptoms. The service sees around 1000 patients per month – roughly a quarter of the GPs’ musculoskeletal caseload. Just under 3% are referred back to the GP for medication review or for non-musculoskeletal conditions, while over 6 in 10 patients are discharged after one appointment with the general practice physiotherapist.
The service has reduced referrals to physiotherapy services by 3% (after a year-on-year increase of 12% over the previous 5 years) and has high patient and GP satisfaction.
252) NHS musculoskeletal services need to link better to work and people’s needs for employment support. Initial assessment and access should include an integrated assessment of health and work needs. This may not always be best provided by a GP, who may not have the time to give the work related support needed, but they should be able to refer to other professionals or services which can help.
253) As well as encouraging the new types of provision already being developed, we wish to trial new kinds of approach for musculoskeletal services so that people’s health and employment needs are met in the best possible way, including the further development of community based pathways and developing better links between treatment and employment support. This will include exploring different referral routes, including how Jobcentre Plus staff can refer claimants into services.
254) There is also a lack of detailed information about what kinds of musculoskeletal services are currently commissioned, and the extent to which the services meet local need. The government will therefore work with NHS England to identify opportunities for regular collection of data about incidence, prevalence, clinical activity and outcomes of musculoskeletal patients and services in England.
Your views
- How should access to services, assessment, treatment and employment support change for people with mental health or musculoskeletal conditions so that their health and employment needs are met in the best possible way?
- How can we help individuals to easily find information about the mental health and musculoskeletal services they can access?
Respond to this consultation online
Tailored and integrated work and health services
Case study – Robert
Robert, a secondary school teacher had a very severe stroke in September 2012. This led to paralysis of the right side of his body and his speech and reading abilities were affected by aphasia. He was determined to return to work, but even if the school could accommodate his wheelchair, he could not resume teaching until his speech was at the level required in the classroom to be understood.
Subsequently, Robert received individual speech therapy and also joined the local aphasia group where he presented weekly topics to the group and received feedback on his intelligibility. After 18 months of therapy, Robert began a phased return to work. During the first academic year, this was based around sixth form supervision and the following academic year it included a return to some teaching of younger years pupils. Robert’s speech and language therapist completed the “Allied Health Professions Advisory Fitness to Work Report” to guide his employers on the level of support which was required for his return to work. For example, he needs extra time for written work so as not to compromise on accuracy.
Today, Robert works 4 short days per week and teaches whole classes of year 7 and 8 pupils. He also attends after school meetings and parents’ evenings as required.
To get to this point, Robert received community speech therapy for some 18 months. This sounds like a long time to invest resources in the rehabilitation of an individual. It is but as a direct result, not only has Robert’s life been transformed it has also saved him living on 20 years’ worth of sickness benefits.
An account from his treating speech and language therapist - Provided by Royal College of Speech and Language Therapists
255) Occupational health and vocational rehabilitation, consisting of physiotherapy and occupational therapy, and related professions and services, can play a pivotal role in supporting people to get into work, and preventing them from falling out of work due to health reasons or disabilities. Offering the right support at the right time can make a real difference to people’s ability to manage their condition and continue to play their part in society.
256) However, occupational health and related services are currently variable and fragmented. Provision can be inconsistent, not easily accessible for all, and not well tailored to the different needs of individuals.
257) Some employers, particularly larger organisations, do provide some occupational health support, but this is not universal. Survey data suggests only 51% of employees have access to occupational health through their employer which can vary depending on their size. [footnote 139] There is also no standardised approach to the support that is offered.
258) For people who cannot access occupational health services through an employer, provision is patchy. Elements of occupational health provision such as physiotherapy are provided by the NHS, but services are rarely commissioned specifically for work-related health. There is a great deal of variation in the types of services available, where they are offered, and how many people can access them.
259) There is also a shortage of health professionals with occupational health expertise. In 2016, The Council for Work and Health highlighted that the UK is short of over 40,000 of the full range of occupational health related specialist practitioners, and the situation will only get worse – “recruitment into specialist training is inadequate and will not replenish the existing workforce”. [footnote 140] Dame Carol Black’s 2008 review [footnote 141] raised concerns about a shrinking workforce, a lack of good quality data, and a detachment from mainstream healthcare.
260) The government established the Fit for Work service to support employees who are off sick for 4 weeks or more. We want to explore how we can promote referrals to occupational health services and advice.
Transforming the landscape of work and health support
261) This government is determined to transform the landscape of occupational health and related services. Provision needs to respond more closely across the spectrum of need, including the needs of those who are self-employed or out of work, as well as those who are currently off sick from work.
262) Our vision is of a whole person approach to occupational health and related services, which meets the differing needs of individuals. We want to cover:
- integrated, expert and impartial advice that meets the needs of the ‘whole person’, through an approach that covers work-related health and social issues to support the individual, employers, GPs, work coaches and other professionals, delivered in an equitable and accessible way (perhaps through local commissioning and provision)
- timely and appropriate access to support (such as occupational health and vocational rehabilitation) adjusted according to need, and whether someone is employed or not
263) We want to support: :
- health and social care professionals so that the benefits that can come from work are an ingrained part of their training
- work coaches and employability professionals to provide positive work and health support
- appropriate delivery models, including those that are locally driven
264) The government is therefore consulting on how we can develop a new approach to work and health support that will fulfill this vision. Whilst a transformation to occupational health will take time, we will explore options which could lead to early changes:
- to increase the access to occupational health assessments and advice, we will explore how we can make it the default position that everyone who would benefit from occupational health assessment and advice is referred to such services, except where it is inappropriate or unlawful to do so. We will test whether changes to GP computer systems would be successful in raising awareness and use of publically funded services. We will develop the detailed design and implementation of this by taking account of views in response to this green paper, and in further discussion with stakeholders
- we will explore models of integrating occupational health within NHS primary and secondary care services provision, re-orientating a part of the NHS occupational health workforce to provide patient services directly. This will enable a greater focus on work as part of an individual’s care pathway within mainstream healthcare. Potentially it may also be possible to expand availability of occupational health, at least for people with more complex needs who do not have occupational health provided by their employer, are self-employed, or are out of work
- we will develop a partnership with one or more NHS occupational health providers in England to test how we can integrate services within different clinical pathways.
Illustrative delivery models
An individual has a number of complex health and social issues that are preventing them from returning to or moving into work. A reformed system would be responsive to their needs by providing access to services that are appropriate and timely.
Example 1: National combined with Local Commissioning
Under a reformed system, there would be a mixture of national and local support so the individual with complex needs would access a nationally-commissioned triage system and have access to a more intensive, locally-commissioned service as appropriate, supported by a single case manager and would be referred to an external partner if ongoing support was required after 6 months.
Example 2: NHS led integrated service
The individual would be referred to a NHS service which would have established links between hospital-based occupational health teams, NHS nurses, primary care and wider professionals with occupational health and vocational rehabilitation-related skills who could assess the immediate needs of the individual and signpost to the appropriate level of support. The service would be available to NHS providers and small and medium-sized enterprises.
Example 3: Group Income Protection access to occupational health/vocational rehabilitation support
An organisation, whether private or public, would secure Group Income Protection which would act as a gateway into a spectrum of occupational health related provision.
Your views
265) We want to hear from you about how to change work and health provision, services and support so that they meet individuals’ needs, including:
- How can occupational health and related provision be organised so that it is accessible and tailored for all? Is this best delivered at work, through private provision, through the health system, or a combination?
- What has been your experience of the Fit for Work service, and how should this inform integrated provision for the future?
- What kind of service design would deliver a position in which everyone who needs occupational health assessment and advice is referred as matter of course?
Respond to this consultation online
Creating the right environment to join up work and health
Integrating local health and employment support
266) We want to support joined-up health and employment services that are locally designed and delivered. Reviews of the research evidence by the King’s Fund and the Nuffield Trust conclude that ‘significant benefits can arise from the integration of services where these are targeted at those client groups for whom care is currently poorly co-ordinated’. [footnote 142]
267) There are different ways of providing this joined-up support. It may involve providing a single service that covers both health and employment support, such as the ‘Individual Placement and Support’ model for people with severe and enduring mental health problems. Or it may involve linking up existing local services so that individuals get seamless support without creating a new single service, the approach taken by the Troubled Families programme.
268) At a national level, we can still have fragmented thinking which sees systems rather than people, and commissioning arrangements which, in some areas, get in the way of joined-up support. We want to build on existing examples of best practice to create the right environment for local commissioners to develop services that work differently and work together to achieve complementary outcomes.
Case study: A local approach to joining services: Tameside public service hub
Tameside’s public service hub, set up in 2014, is a ground-breaking response to the challenge of supporting people/families with complex needs (unemployment, physical/ mental health, domestic abuse, substance misuse, debt, housing, child protection) and in so doing helps meet the fiscal challenge to shift investment upstream to earlier intervention to reduce demand and costs.
Any service can refer to the hub, which brings together Jobcentre Plus, adult mental health, substance misuse, housing, children’s services, police, probation and the Working Well programme. Each service has access to their ‘home’ organisation’s system. Underpinning this information sharing process is a comprehensive Information Sharing Agreement which has the strategic support of a range of agencies as well as Information Governance leads.
The hub allocates a key worker to sequence and coordinate support for people with complex needs, which they are able to do effectively as they have a holistic picture of the individual and their family situation. This approach is beneficial as it brings services together, where all parties involved understand the full needs of the person (and family) they are supporting. It streamlines the support that people receive, and minimises unnecessary disruption. This has a secondary benefit of reducing the cost of duplicative interventions.
269) This will involve encouraging local leadership through Sustainability and Transformation Plans and other mechanisms (such as Joint Strategic Needs Assessments) which bring partners together around a shared vision, and sharing good practice. It will also involve the effective sharing of data. Not only can better sharing of data mean that individuals don’t have to repeat their story to different services, it also means that providers can more accurately oversee the commissioning and governance of services and support and track a range of complementary outcomes.
270) Innovation and local networks encourage the delivery of person-centred care across health, social care, employment and voluntary sector boundaries. The government is calling for evidence on good examples of co-ordinated services and of the factors which contribute to successful collaborations so that we can learn from them.
Increasing data transparency to improve outcomes
271) Increased data sharing can help improve both health and work outcomes for individuals. We will work with NHS Digital to create a new information standard for data on employment status in healthcare data sets, to enable useful data collection and analysis by employment status at both a national and local level in England. The proposed information standard will be subject to consultation.
272) If work is truly to be seen as a health outcome, we may need to support the recording of occupational status in all clinical settings, for example by:
- developing an agreed terminology, as an aid to communication and analysis
- encouraging and incentivising its use through software prompts and through regular clinical audit
273) There could be real benefits. Encouraging and enabling the reporting of employment as an outcome of clinical intervention should help normalise discussion of whether one treatment or another will help a patient to be well enough to return to work. We would be interested in further suggestions on how we could encourage the better use of data.
274) Where data are available, indicator sets or outcomes frameworks can help to increase transparency and accountability across services. In England work outcomes already feature in 2 indicators in the NHS Outcomes Framework and the Public Health Outcomes Framework and one indicator in the Adult Social Care Outcomes Framework.
275) We will also work with Public Health England to develop a basket of work and health indicators to support improved health and work outcomes in place-based systems and make them available through Public Health England’s open data access platform or ‘fingertips tool’. This tool will be part of Public Health England’s wider determinants of health profile, recognising that health and work are connected with other aspects of life and will be based on the use of aggregate data. The indicators could cover:
- labour market outcomes, for example, employment rate gaps between disabled and non disabled people, and information on health-related benefits recipients
- health outcomes related to working age people and health services generally, for example, disability-free life expectancy, and markers of quality, such as emergency admissions for acute conditions that should not usually require hospital admission; and the proportion of people feeling supported to manage their long-term condition
- wider issues related to the health of working age people – on which we would welcome suggestions and evidence
276) A wealth of evidence and knowledge exists from a variety of sources that can support improved outcomes, including evidence reviews on specific interventions, as well as evidence which support our understanding of population needs. Working with Public Health England, we will explore how to bring existing evidence and knowledge on health and work together in one place for commissioners and local delivery partners, for example by creating a single website.
Your views
277) We want to understand what more could be done to encourage local areas to bring health and employment systems together to better support people:
- How can we best encourage innovation through local networks, including promoting models of joint working such as co-location, to improve health and work outcomes?
- How can we encourage the recording of occupational status in all clinical settings and good use of these data?
- What should we include in a basket of health and work indicators covering both labour market and health outcomes at local level?
- How can government and local partners best encourage improved sharing of health and employment data?
- What is the best way to bring together and share existing evidence in one place for commissioners and delivery partners?
Respond to this consultation online
Reinforcing that work can promote good health
278) Underpinning all of the above actions is the conviction that work promotes health and should be seen as a health outcome. We cannot achieve change without positive attitudes towards work and health from a wide range of people, particularly health and care professionals and disabled people and people with health conditions.
279) Evidence shows that being in appropriate work is good for health and that being out of work can have a detrimental effect on health. [footnote 143] For health and care professionals, therefore, supporting an individual to be in work appropriate for them is central to delivering effective, personalised care and addressing a key social determinant of health.
280) For clinicians this could be described as considering work as part of an individual’s ‘health outcome’. For example, the Faculty of Occupational Medicine highlight the positive relationship between work and physical and mental health, noting ‘the importance of returning to work as a healthcare outcome’. [footnote 144] The National Institute for Health and Care Excellence (NICE) clinical guidelines recognise that a range of outcomes from interventions should be considered, including impact on functional ability and return to work. [footnote 145]
281) We are already taking action to promote the importance of work in the health system. By November 2016, Public Health England and the College of Occupational Therapists will have recruited and started evaluation of a pilot group of Health and Work Clinical Champions, with the aim of promoting work as a clinical health outcome within their health trust.
282) We want to make the benefits of work an ingrained part of the training and professional approach of the health and social care workforce. We will work with Health Education England, Public Health England, professional regulators, Royal Colleges and the Welsh and Scottish Governments, to address capability and capacity issues for the NHS workforce, including:
- building upon the educational curriculum for medical and nursing/allied health professional undergraduate training programmes
- training current healthcare professionals on the links between work and health and how to embed as part of care plans.
- exploring the option to encourage nurses and allied health professions who may have left clinical practice to return to utilise their expert skills within a different setting
283) NICE has already committed that it will, at the point of guidance update or new development, take into consideration any available employment outcomes across conditions which affect primarily the working age population. We are actively considering with NICE the development of guidelines to support improved employment outcomes among people out of work due to ill health.
284) To support local decision makers, in 2017 Public Health England will publish a report on worklessness, estimating the potential cost-savings for health and social care services, wider government savings, and benefits to the individual (and to the local economy) of moving a person into work.
Your views
285) Our ambition is that work is consistently recognised as a health outcome in the health and care systems:
- What is the best way to encourage clinicians, allied health professionals and commissioners of health and other services to promote work as a health outcome?
Respond to this consultation online
Patients as partners
286) We also need to do more to recognise that patients and those who use services should be partners in their care. The Kings Fund points to the ‘growing body of evidence which demonstrates that individuals who are empowered to manage their own condition are more likely to experience better health outcomes’. [footnote 146]
287) Individuals can be supported in different ways: through having better information about navigating the employment and healthcare systems, having the ability to self-refer to an increasing range of services, and being able to improve their health literacy with a particular focus on the link between work and health.
288) Innovative digital services will have a role here. We are relaunching NHS Choices as NHS.UK with a fuller range of online services including booking appointments and ordering and tracking of prescriptions. By autumn 2017 the Department of Health, NHS England and NHS Digital will have developed the tools to enable instant, downloadable access to personal health records, making it easier for patients to access their health information and share it with people concerned with their care. In addition to this, NHS England will approve a set of selected of apps by March 2017, offering support to patients, including those with long-term conditions, in managing their health.
289) We will also use innovation funding to look at new ways, including digital tools, of providing integrated health and employment support for disabled people and people with health conditions to stay in work or enter work.
Conclusion
290) Whenever an individual needs health and care support, that care needs to consider their needs in the round, including the important role work can play. So we are committed to ensuring that we promote health in its broadest sense, ensure access to the right types of support, and join up health and employment services in providing that support. This will require us to create the right conditions for change and see patients as true partners in their care.
Summary of consultation questions
Improving discussions about fitness to work and sickness certification
- How can we bring about better work-focussed conversations between an individual, healthcare professional, employer and Jobcentre Plus work coach, which focus on what work an individual can do, particularly during the early stages of an illness/developing condition?
- How can we ensure that all healthcare professionals recognise the value of work and consider work during consultations with working age patients? How can we encourage doctors in hospitals to consider fitness for work and, where appropriate, issue a fit note?
- Are doctors best placed to provide work and health information, make a judgement on fitness for work and provide sickness certification? If not, which other healthcare professionals do you think should play a role in this process to ensure that individuals who are sick understand the positive role that work can play in their recovery and that the right level of information is provided?
- Turning to the fit note certificate itself, what information should be captured to best help the individual, work coaches and employers better support a return to work or job retention?
- Is the current fit note the right vehicle to capture this information, or should we consider other ways to capture fitness for work and health information? Does the fit note meet the needs of employers, patients and healthcare professionals?
Mental health and musculoskeletal services
- How should access to services, assessment, treatment and employment support change for people with mental health or musculoskeletal conditions so that their health and employment needs are met in the best possible way?
- How can we help individuals to easily find information about the mental health and musculoskeletal services they can access?
Transforming the landscape of work and health support
- How can occupational health and related provision be organised so that it is accessible and tailored for all? Is this best delivered at work, through private provision, through the health system, or a combination?
- What has been your experience of the Fit for Work service, and how should this inform integrated provision for the future?
- What kind of service design would deliver a position in which everyone who needs occupational health assessment and advice is referred as matter of course?
Creating the right environment to join up work and health
- How can we best encourage innovation through local networks, including promoting models of joint working such as co-location, to improve health and work outcomes?
- How can we encourage the recording of occupational status in all clinical settings and good use of these data?
- What should we include in a basket of health and work indicators covering both labour market and health outcomes at local level?
- How can government and local partners best encourage improved sharing of health and employment data?
- What is the best way to bring together and share existing evidence in one place for commissioners and delivery partners?
- What is the best way to encourage clinicians, allied health professionals and commissioners of health and other services to promote work as a health outcome?
6: Building a movement for change: taking action together
Chapter summary
This chapter summarises our commitment to act. We set out our plans to:
- change perceptions and culture around health, work and disability
- launch a pro-active and wide-ranging conversation around the issues and proposals in this green paper
- set out our plans to take forward a programme of work in the short-term and over the next 10 years
Introduction
291) We are committed to halving the disability employment gap and enabling disabled people and people with long-term health conditions to access all the benefits that work can bring. But, as set out in chapter 1 and expanded upon within each of the chapters, this challenge is complex and cannot be approached from one angle alone.
292) Where we are confident of the positive results that action will bring, we will be quick to implement change. Yet while government action is important, it will not be sufficient to drive the required changes on its own. Action is required by many different partners on a number of fronts: everyone has a role to play, and we are asking others to engage and work with us, both now and in the future.
293) We want to create a movement for change across society, one that meets this challenge and ensures that we achieve our ambitions for disabled people and people with long-term health conditions. This chapter sets out 3 ways in which we intend to do this:
- real and lasting change will only come about if we can also address negative cultural and social attitudes about disabled people and people with long-term health conditions. We therefore want to work with others to change perceptions and transform the culture around disability, health and work, to ensure that real and long-lasting progress is made
- we want to launch a proactive, wide-ranging and challenging conversation around the issues and proposals set out in this green paper. The consultation questions posed, and the consultation process that we have designed, aim to do just this. Without this dialogue, we will not be able to develop or advance our proposals or the positive work that is already underway
- in recognition that our ambitions will not be achieved overnight, we will take forward a programme of work for the next 10 years, to ensure that sustained progress is made and change achieved in the immediate future, over the course of this Parliament, and beyond
Changing the culture around work and health
294) We know that currently the way individuals and groups of people think, talk and act about the relationship between work, health and disability can get in the way of the best employment and health outcomes for disabled people and people with long-term health conditions. For example:
- employers can be reluctant to employ disabled people or may create workplace environments where people do not feel comfortable discussing long-term health conditions or disabilities. For example, in 2013, 30% of disabled working age benefit claimants saw ‘attitudes of employers’ as a barrier to seeking work, finding work, or working more hours [footnote 147]
- healthcare professionals and work coaches can lack confidence dealing with health-related return-to-work issues. A study found that 4 in 10 GPs didn’t feel confident in dealing with patient issues around a return to work [footnote 148]
- parents, carers and service providers can have misconceptions about working with a disability or long-term health condition, which can result in them advising against a disabled person or someone with a long-term health condition trying work for fear of it damaging their health [footnote 149]
- disabled people and people with long-term health conditions may not be fully aware of the health benefits of work, or may not realise the range of employment options and support available. For example, in a survey of working age disabled benefit claimants, only 23% thought work would be beneficial to their health compared to almost two thirds who thought work would make them better off financially [footnote 150]
295) We want these perceptions to change, so that the actions taken forward by the government and others are met by the right behaviours and attitudes. This will need a range of actions across the board to develop our culture into one which always supports disabled people and people with long term health conditions to work.
296) The actions in this paper are designed to foster this shift in some of the key areas that we have identified. In chapter 2 we explored how we can equip work coaches with the right skills and capabilities to better engage with disabled people and people with health conditions from the very start of their journey, to offer them personalised support tailored to their individual needs. In chapter 3, we considered how we can best provide disabled people and people with health conditions with financial support in a straightforward and timely way if they fall out of employment. In chapter 4, we set out how employers are crucial partners in creating the right conditions for disabled people and people with health conditions to enter and flourish in work. In chapter 5 we discussed in detail the importance of healthcare professionals understanding the benefits of work, and of this understanding being fully translated into discussions about fitness to work and sickness certification. We also discussed the importance of empowering individuals to be active partners in their care and to build their belief in their own potential.
297) But changing attitudes is complex and will require sustained action over time, as well as a commitment from all of us to truly embed a new way of thinking. People who shape our thinking at local level, particularly in schools and community groups, play an important role in shifting our attitudes to disabilities and health conditions. The government has an important role in facilitating change, but everyone has their own part to play. We are asking for engagement and action from others:
- we want to see disabled people and people with long-term health conditions working with employers and involved in local service design
- we want families, friends, teachers and carers to feel confident that disabled people and people with long-term conditions will get the support that they need to fulfil their aspirations
- we want employers to recruit inclusively and with confidence, promote health and wellbeing in their workplaces, and fully support employees facing ill health or disability to remain productive and in work
- we want GPs and other healthcare professionals to have high work ambitions for their patients, in recognition that this is good for their health and wellbeing, and for work to be embedded as a health outcome in their discussions with patients who have a disability or long-term health condition
- we want local leaders and commissioners in health, social care, local authorities and more widely across communities to place work and health at the heart of their commissioning decisions and service design
- we want work coaches and other employment advisers to have the skills and capability needed to offer appropriate, tailored and timely support to disabled people and people with long-term health conditions who are out of work
- we want voluntary and community organisations to share effective practice and continue to be active partners with government in positively changing attitudes, and providing support and mentoring to disabled people and people with long-term health conditions, helping them to realise their full potential
Case study: the creative benefits of diversity
We’ve seen directly the creative benefits of diversity. Through our work, we’ve discovered some fantastic new on and off screen talent who bring new perspectives and ideas which make the stories we tell richer and more interesting. A great example of this is the Paralympics where more than 15% of the production team and two thirds of our presenters at the Rio 2016 Games were disabled, which added additional heart, depth and expertise to our coverage. Ratings for the coverage were higher than anticipated too, which is great for business. We’ve found this in our commercial partnerships too, from working with advertisers to independent production companies. We have also had extremely positive feedback from all the creative SMEs who have worked with Channel 4 trainees with disabilities, many of whom have already been offered ongoing employment following the scheme.
We know there is much more progress to be made, but at Channel 4 we are already seeing the benefits of proactively working to increase representation and employment of disabled people. As a broadcaster it’s vital that we both reflect and appeal to our diverse viewers and the best way of doing this is through having a diverse workforce.
Dan Brooke, Chief Marketing and Communications Officer and Channel 4 Board member responsible for diversity
298) Disabled people and people with health conditions will engage with different types of support and services depending on their individual needs, and no 2 people will have the same journey towards employment. It is vital that whatever the support received by an individual, the right attitude runs throughout our society and services, so that we make every contact count.
Your views
299) We have spoken about the shift in attitudes, behaviours and support towards disabled people and people with health conditions that we are setting out to achieve across various groups, systems and services. We recognise that this requires a change across society: schools, community groups, employers and others all have a role to play. In this chapter we emphasise once more that any action we take must go hand in hand with this change in culture. We want to hear from you:
- How can we bring about a shift in society’s wider attitudes to make progress and achieve long lasting change?
- What is the role of government in bringing about positive change to our attitudes to disabled people and people with health conditions?
Respond to this consultation online
The consultation process: launching the conversation
300) This consultation is crucial to building a shared plan for future action and achieving culture change. We want this consultation to bring together wide-ranging expertise, opinions and experiences and launch a rich and challenging discussion, one that can inform our programme of working going forward.
301) In developing the proposals in this green paper, we have already started a valuable process of engagement with a number of stakeholders:
- in May 2016 we established an Expert Advisory Group consisting of representatives from the health, research, disability charity, business and employer communities to consider themes and proposed areas for action in the green paper. This group will continue to meet on an ongoing basis to consider wider work and health issues
- we have also facilitated a number of roundtables and workshops, including with the Royal Colleges and other health organisations, which allowed us to test some of our thinking and to shape our consultation questions, as well as to consider how best to engage a broad audience
302) We recognise that different people will require or prefer different channels through which to respond to the consultation questions. As such, and using the feedback given by stakeholders to date, we have developed a number of avenues through which you can share your views:
- we have organised a series of face-to-face consultation events, hosted by partners from disability charities and employers, to collectively explore the green paper’s themes and questions. These have been designed in close collaboration with organisations including the Disability Benefits Consortium and the Disability Charities Consortium
- an online survey hosted on Citizen Space provides a simple and easily accessible way to respond to all consultation questions.
- a series of moderated online forums, supplemented by consultation materials
- you can email us at: workandhealth@dwp.gsi.gov.uk or write to us at The Work, Health and Disability consultation, Ground Floor, Caxton House, 6-12 Tothill Street, London, SW1H 9NA
303) Using one of these channels for responding, we now invite you to provide your views on the consultation questions set out within this paper. We welcome your suggestions, evidence, ideas and recommendations, although you should not feel restricted to these areas alone.
304) In order to satisfy our duty under the Equality Act 2010 to have due regard to the need to eliminate unlawful discrimination, advance equality of opportunity and foster good relations between different groups, we want to consider the potential impacts of the proposals in this green paper on protected groups under that Act. We therefore also ask you to consider equality impacts as part of your response to the consultative parts of this document and answer the following question. Please include any relevant evidence or data that supports your views:
- Could any of the proposals within the green paper potentially have an adverse effect on people with a protected characteristic? If so, which proposal, and which protected group/s are affected? And how might the group/s be affected?
305) The consultation will run until Friday 17 February 2017. This is a public consultation to which anyone with an interest may respond. A summary of all consultation questions can be found in the appendix.
Taking action together: developing a 10-year plan
306) We know that our ambition to halve the disability employment gap is challenging. It will not be easy and will take time to achieve. But it is necessary if we want to create a country that works for everyone. In this paper we have set out our vision and some early actions. We know that we cannot do this alone. Change will require concerted action over time from disabled people and people with long-term health conditions, employers, healthcare professionals, employment support providers, voluntary and community sector organisations and many others.
307) Where we are sure of the improvement and positive transformation that action can bring, we will continue to be quick in bringing about change and building upon existing support. Looking ahead, we will need to have clear goals for both the short and long term in order to deliver the ambition set out within this green paper and build upon activity already underway. We are committed to engaging and working with people in the areas that require change and to testing approaches as they evolve through the consultation period and beyond. We are committed to investing in innovation, learning what works and spreading the lessons and widely. The programme of work outlined below demonstrates our commitment to take action and work with others both in the immediate future, throughout the Parliament and beyond 2020.
Ten year programme of work
This outlines our programme of work across 3 key strands, taking place over the next 2 years, over this Parliament and beyond 2020.
Across all areas, your responses to our Green Paper consultation will shape the actions that we already have underway, the direction of future discussions with stakeholders and partners, and the development of our policy for this Parliament and beyond.
Our first strand of work is ‘Developing an improved system and transforming services’. We will work with others to ensure the right health and employment support offer for individuals.
Over the next 2 years we will:
- launch the Health and Work Conversation for ESA claimants in late 2016
- introduce measures to support people in the WRAG, including “Journey to Employment” Job Clubs and Community Partners from 2017
- expand IAPT and link employer advisers in around 40 per cent of IAPT services from January 2017
- launch the Work and Health Programme in autumn 2017
- explore improving Fit for Work referrals from primary care
- re-procure and scale Access to Work offer from 2017
- develop a set of work and health indicators with Public Health England, for use at a local level
- extend “Journey to Employment” Job Clubs in 2017
- stop reassessments for those with severe lifelong conditions from late 2017
- begin research and trials to help the Support Group from 2017
- re-procure and scale Access to Work offer from 2017
Over this Parliament we will:
- progress digital health initiatives, building upon initiatives such as NHS England’s set of selected health apps and the launch of NHS.UK
- explore improving data sharing across benefit assessments
- explore reform of the Work Capability Assessment
- consider how Fit for Work fits with future provision and ensure it remains fit for purpose
- develop capability and capacity of the NHS workforce to promote work as a health outcome
- work with others to design and test future policy delivery for musculoskeletal services
- scope and develop suitable approaches to a new occupational health landscape
By 2020 and beyond we want to achieve timely access to integrated and individualised health and employment support, which helps disabled people and people with long-term conditions to go as far as their talents will take them
Our second strand of work is ‘Investing in innovation’. We will work with others to implement and scale trials, and in partnership with specialist organisations, to promote products and digital health technologies.
Over the next 2 years we will:
- launch Challenge Prize competitions to stimulate and incentivise innovation by spring 2017
- launch a series of mental health and employment trials in early 2017, including Individual Placement Support and computerised Cognitive Behavioural Therapy health treatments
- launch a series of health-led employment trials from spring 2017
- commission research by April 2017 to better understand how we can engage with those individuals in the Support Group
- Public Health England to publish an Economic Framework on worklessness in March 2017
Over this Parliament we will:
- develop a work and health indicator framework with Public Health England, for use at local level
- gather evidence on good practice amongst employers, and research on content for an employer ‘one-stop-shop’ on health and work
- build our knowledge of international evidence and best practice in relation to health, employment and disability
- draw early findings from trials – stopping where the approach is not working and scaling trials where evidence supports this
- during this Parliament and beyond we will continue to build a fuller evidence base and act on findings
- we want to achieve a clear picture of what support works for whom, and transformed models of support that can scale quickly, drawing upon innovation and a strong evidence base
Our third strand of work is ‘Engaging across society’. We will work across society to build consensus, understand how to facilitate engagement and action, and to develop and drive our programme of work.
Over the next 2 years we will:
- use webinars and other forums to engage with musculoskeletal conditions community from early 2017
- discuss medical verification and judgements on fitness for work with work coaches, employers and employee organisations
- establish Disability Confident Business Leaders Group
- NICE to include work considerations in future clinical guidelines
- establish supportive networks between employers, employees and charities
- engage with NHS and wider healthcare professionals on embedding work as a health outcome
- hold discussions with insurance industry to establish validity of developing Group Income Protection products for smaller employers
During this Parliament we will:
- bring together existing information and support for employers
- run information campaigns with partners on key health and work issues
- build the employer evidence base and business case on disability
- explore reform to Statutory Sick Pay to better encourage supportive conversations and phased returns to work
- create a new information standard with NHS Digital for the inclusion of employment status in healthcare data sets
We want to achieve a society where everyone is ambitious for disabled people, and where people understand and act positively upon the important relationship between health, work and disability.
Appendix: written description of images
Population characteristics
- The main working-age health conditions in the UK are musculoskeletal and mental health. 2.6 million disabled people are recorded as having mental health condition in the UK, 0.9 million of whom are in employment. This means the employment rate for disabled people with mental health conditions is 32 per cent.
- Musculoskeletal conditions also affect many working age people. 3.7 million disabled people have musculoskeletal conditions, 1.7 million of whom are in employment. This means the employment rate for disabled people with musculoskeletal conditions is 48 per cent.
- The prevalence of mental health conditions varies with employment status. For example in England, 1 in 5 of all working age people have a common mental health condition. 1 in 7 working age people in full-time work have a common mental health condition. 1 in 2 out-of-work benefit claimants have a common mental health condition.
- There are 12 million people with a long-term health condition in the UK, 7.1 million of these people are disabled and 4.8 million of these people are non-disabled.
- 9 in 10 workless disabled people are economically inactive and are not actively looking for work.
- Most Employment and Support Allowance claimants are in the Support Group. Of the 2.4 million people who are on Employment and Support Allowance, 67 per cent are in the Support Group. 20 per cent are in the Work Related Activity Group, and 14 per cent have yet to take their Work Capability Assessment.
Our vision
- Our vision is of a society where everyone is ambitious for disabled people, and where people understand and act positively upon the important relationship between health, work and disability, so that:
- When an individual looks for a job that makes the best use of their talents, they should find opportunities to secure a good job and progress, provided by inclusive employers and job creation
- When an individual is in work, they should have jobs that actively support and nurture health and well-being, provided by inclusive employers who understand the link between work, health and disability
- When an individual is at risk of long-term sickness absence or falling out of work due to their health or disability, they should encounter early action as needed to stay in or return to work, provided by both inclusive employers who understand the link between work, health and disability and a more effective health service
- When an individual turns to the health service, they should find healthcare professionals who support people in their employment aspirations, and health services that provide help at the right time and co-ordinate effectively with employment support
- When an individual is out of work due to their health or disability, they should encounter the right employment support to secure work or get closer to the labour market, provided by a more effective employment support system and a more effective health service
- When an individual is unable to work, they should find access to rapid financial support when needed, provided by a more effective employment support system
- A more inclusive and understanding society will underpin this entire system of more effective employment support, a more effective health service, and inclusive employers and job creation.
- For the individual to encounter this seamless, wrap-around system which responds appropriately to their needs, inclusive employers, a more effective the health service and a more effective employment support system will work together harmoniously.
Figure 1: outcomes of initial Work Capability Assessment
- This line graph shows the outcomes of initial Work Capability Assessments between October 2008 and March 2016.
- In March 2016, 39 per cent of people entered the Support Group following their initial Work Capability Assessment. Over the last 12 months we have seen on average 50 per cent of people going into the Support Group. This compares to the October 2008-March 2011 average of 17 per cent entering the Support Group.
- In March 2016, 46 per cent of people entered the Capability for Work category following their initial Work Capability Assessment. This compares to the October 2008-March 2011 average of 60 per cent entering the Capability for Work category.
- In March 2016, 15 per cent of people entered the Work Related Activity Group following their initial Work Capability Assessment. This compares to the October 2008-March 2011 average of 26 per cent entering the Work Related Activity Group.
A possible new model for assessments in Universal Credit
- This flow chart illustrates a possible model in Universal Credit for an assessment which would consider financial support and employment support separately.
- In terms of employment support, the claimant journey could be:
- A claimant makes a new claim online for Universal Credit. They have a health condition, and could be in or out of work.
- Within one month of their claim they have initial engagement with a work coach.
- The claimant will accept a Claimant Commitment via the most appropriate channel.
- Having made a Claimant Commitment, the claimant gains access to employment support.
- Disability Employment Advisers and Community Partners provide advice and support to work coaches.
- The claimant receives personalised support from a skilled and accredited Jobcentre Plus work coach throughout the life of their claim. This includes a Health and Work Conversation.
- The claimant can also access the Personal Support Package, a comprehensive menu of support designed to be tailored to the needs of the claimant.
- In terms of financial support, the claimant journey could be:
- A claimant makes a new claim online for Universal Credit. They have a health condition, and could be in or out of work.
- The claimant receives Universal Credit standard allowance, plus any relevant additions dependent on household circumstances
- They undergo an assessment for financial support
- Claimants assessed as being too ill or disabled to work or undertake work-related activities will receive additional financial support in addition to the Universal Credit Standard Allowance (plus any relevant additions).
- Re-assessments will be undertaken where appropriate to assess continuing entitlement to the disability element of Universal Credit. This process excludes those with the most severe, lifelong conditions.
-
References for preceding infographics: “Evidence shows that appropriate work is good for our health” Source: Waddell G, Burton AK. Is work good for your health and wellbeing; 2006. “Ill-health among working age people costs the economy £100bn a year in sickness absence and costs employers £9bn a year”. Sources: Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016 and Black C , Frost C. Health at work - an independent review of sickness absence; 2011. “Reducing long term sickness absence is a priority. 1.8 million employees on average have a long term sickness absence of four weeks or more in a year.” Source: Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. “Only around 3 in 100 of all Employment and Support Allowance claimants leave the benefit each month.” Source: Department for Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016 . “8% of employers report they have recruited a person with a disability or long term health condition over a year.” Source: Department for Work and Pensions. Employer Engagement and Experience Survey; 2013. “Access to timely treatment varies across areas. Average waiting times for mental health treatment can differ as much as 12 weeks across England and some evidence suggests treatment for musculoskeletal conditions can differ as much as 23 weeks.” Source: Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016 and Chartered Society of Physiotherapy. Stretched to the limit; 2012. “Disability free life expectancy at birth also varies across England. Disability free life expectancy at birth in upper tier local authorities in England range from 55 to 72 years for Males and 53 to 72 years for Females in 2012-2014.” Source: Office for National Statistics. Disability-Free Life Expectancy (DFLE) and Life Expectancy (LE) at birth by Upper Tier Local Authority, England, 2012 to 2014; 2014. “Disability has been rising - over 400,000 increase in the number of working age disabled people in the UK since 2013, taking the total to more than 7 million.” Source: Office for National Statistics. Labour Force Survey, Q2 2016; 2016. “Compared to non-disabled people, disabled people are less likely to enter employment so preventing them from leaving work is important. Between two quarters as many as 150,000 disabled people leave employment.” Source: Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. “The disability employment gap is too wide. 80% of non-disabled working age people are in employment compared to 48% of disabled people. This leads to a disability employment gap of 32 percentage points.” Source: Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Roelfs D J, Shor E, Davidson KW, Schwartz, JE. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Social Science & Medicine 2011;72(6): 840–854. ↩
-
Analysis of the Annual Population Survey (APS) Wellbeing Data, Apr-Oct 2011 Cabinet Office report (accessed October 2016). ↩
-
For the definitions used in this paper, see the box on p9 ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
McManus S, Bebbington P, Jenkins R, Brugha T. (eds.). Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Waddell G, Burton AK. Is work good for your health and wellbeing; 2006 ↩
-
Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016 ↩
-
Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016 ↩
-
Equality Act 2010 (accessed October 2016) ↩
-
Waddell G, Burton AK. Is work good for your health and wellbeing; 2006; Rueda, S., Chambers, L., WIlson, M., Mustard, et al. Association of returning to work with better health in working-aged adults: a systematic review. American Journal of Public Health, 2012;102, 541–56.; Paul KI, Moser K. Unemployment impairs mental health: Meta-analyses. Journal of Vocational Behavior, 2009;74, 264–282.; Roelfs DJ, Shor E, Davidson KW, Schwartz JE. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Social Science & Medicine, 2011;72(6), 840–854. ↩
-
Benach J, Muntaner C, Santana V. Employment Conditions and Health Inequalities. Final Report to the WHO Commission on Social Determinants of Health (CSDH) Employment Conditions Knowledge Network. 2007. (accessed October 2016). ↩
-
ILO & Finnish Ministry of Social Affairs. The Economics of Health, Safety and Well-being. Barefoot Economics: Assessing the economic value of developing a healthy work environment; (accessed October 2016). ↩
-
Ministerial Statement: Building More Resilient and Inclusive Labour Markets. OECD Labour and Employment Ministerial Meeting. January 2016 ↩
-
van Stolk C, Hofman H, Hafner M, Janta, B. Psychological Wellbeing and Work: Improving Service Provision and Outcomes January 2014.A report by RAND Europe (accessed October 2016). ↩
-
Royal College of Psychiatrists. Mental Health and Work (accessed October 2016). ↩
-
NICE. Workplace health. Local government briefing (LGB2) (accessed October 2016). ↩
-
Maier R, Egger A, Barth A, Winker R, Osterode W, Kundi M, Wolf C, Ruediger H. Effects of short- and long-term unemployment on physical work capacity and on serum cortisol. International Archives of Occupational and Environmental Health. 2006;79(3): 193–8.; Hämäläinen J, Poikolainen K, Isometsä E, Kaprio J, Heikkinen M, Lindeman S and Aro H. Major depressive episode related to long unemployment and frequent alcohol intoxication. Nordic Journal of Psychiatry. 2005;59 (6): 486–491.; Voss M, Nylén L, Floderus B, Diderichsen F, Terry P D (2004) Unemployment and Early Cause-; Royal College of Psychiatrists: Mental Health and Work (accessed October 2016). ↩
-
Bivand, P. and Simmonds. The benefits of tackling worklessness and low pay. (October 2016). ↩
-
Scope. A million futures: halving the disability employment gap. (accessed October 2016). ↩
-
Scope. Better Living Higher Standards: Improving the lives of disabled people by 2020. (accessed October 2016). ↩
-
Institute of Health Equity. Local action on health inequalities: Increasing employment opportunities and improving workplace health. Health Equity Evidence Review; 2014. ↩
-
Scope. A million futures: halving the disability employment gap. (accessed October 2016) ↩
-
Fylan F, Gwyn B, Caveney L. GP’s perception of potential services to help employees on sick leave return to work. Department for Work and Pensions. 820; 2012. ↩
-
Work and Health Unit run in-depth interviews in Bedfordshire, December 2015. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
References for preceeding infographics: “The main working-age health conditions in the UK are musculoskeletal and mental health. 2.6m disabled people recorded as having mental health condition in the UK, 0.9m of whom are in employment. This means employment rate for disabled people with mental health conditions is 32%.” Source: Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack, Supplementary Tables; 2016. “Musculoskeletal conditions also affect many working age people. 3.7m disabled people have musculoskeletal conditions, 1.7m of whom are in employment. This means the employment rate for disabled people with musculoskeletal conditions is 46%.” Source: Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack, Supplementary Tables; 2016 “The prevalence of health problems varies with employment status, for example in England: 1 in 5 of all working age people have a common mental health condition, 1 in 7 working age people in full time work have a common mental health condition and 1 in 2 out of work benefit claimants have a common mental health condition.” Sources: McManus S, Bebbington P, Jenkins R, Brugha T. (eds.). Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey; 2016. “There are 12m people with a long term health condition in the UK, 7.1m of whom are disabled and 4.8m of whom are non-disabled”. Source: Office for National Statistics. Labour Force Survey, Q2 2016; 2016.; “9 in 10 workless disabled people are economically inactive and are not actively looking for work.” Source: Office for National Statistics. Labour Force Survey, Q2 2016; 2016.; “Most ESA claimants are in the Support Group. 67% of ESA claimants are in the Support Group, 20% of claimants are in the Work Related Activity Group and 14% are pre-Work Capability Assessment. 2.4m people are on ESA, over 60% of whom are in the Support Group. Source: Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Black C, Frost D. Health at work – an independent review of sickness absence; 2011 ↩
-
Department for Work and Pensions. Fuller working lives reference data. (accessed October 2016). ↩
-
Healthy life expectancy at birth is only 63.4 for males and 64 for females. Source: Office for National Statistics. Disability-Free Life Expectancy (DFLE) and Life Expectancy (LE) at birth by Upper Tier Local Authority, England, 2012 to 2014; 2014. ↩
-
Green, F. Why Has Work Effort Become More Intense? Industrial Relations: A Journal of Economy and Society 2004;43: 709-741. ↩
-
Institute of Health Equity. Local action on health inequalities: Adult Learning Services. Health Equity Evidence Review; 2014 ↩
-
Office National Statistics. Statistics on obesity, physical activity and diet. (accessed October 2016). ↩
-
Office for National Statistics. Statistics on smoking. (accessed October 2016) ↩
-
Department for Work and Pensions. Health matters. (accessed October 2016). ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Marmot, M. Fair society, healthy lives: the Marmot Review: strategic review of health inequalities in England post-2010; 2010 ↩
-
Public Health England; Public Health Outcomes Framework. Figures for 2012-14; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Office for National Statistics. Labour Force Survey, Q2 2016; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Source: Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016. ↩
-
Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016. ↩
-
Chartered Society of Physiotherapy. Stretched to the Limit. (accessed October 2016) ↩
-
National Health Service. NHS Five Year Forward View. (accessed October 2016). ↩
-
The European Commission. The 2009 Ageing Report: Dealing with the impact of an ageing population in the EU;2009. ↩
-
Carers UK and YouGov. Caring & Family Finances Inquiry UK report Carers UK; 2014. ↩
-
Department for Work and Pensions. Fuller working lives reference data. ↩
-
National Council for Voluntary Organisations. The charity sector and public services. (accessed October 2016). ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. Resolution Foundation. Retention Deficit: A new approach to boosting employment for people with health problems and disabilities. (accessed October 2016). ↩
-
Psychological Wellbeing and Work: Improving Service Provision and Outcomes. (accessed )ctober 2016). ↩
-
Heslin L, Howard M, Leese P, McCrone P. Rice C. Randomized controlled trial of supported employment in England: 2 year follow-up of the Supported Work and Needs (SWAN) study, World Psychiatry, 2011;10, 132–137. ↩
-
Department for Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016, Primary health condition ↩
-
Department for Work and Pensions. Estimating the Early Labour Market Impacts of Universal Credit. DWP Report number: 28; 2015. ↩
-
Department for Work and Pensions Longitudinal Study, DWP Tabulation Tool. (accessed 10 February 2016). ↩
-
Coleman, N., Sykes, W. and Groom, C. What works for whom in helping disabled people into work? Department for Work and Pensions.Working paper: 120, 2013. ↩
-
Department for Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016. ↩
-
Department for Work and Pensions. New Enterprise Allowance Statistics: April 2011 – June 2016. (accessed October 2016). ↩
-
Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016. ↩
-
Department for Education. Special Educational Needs in England: January 2016. ↩
-
NHS Digital. Adult Social Care Statistics; 2016. ↩
-
Department for Education. ↩
-
Department for Education and Department for Business Innovation and Skills. Post-16 Skills Plan. 2016. ↩
-
Department for Work and Pensions. DWP Employment and Support Allowance: Work Capability Assessments, Mandatory Reconsiderations and Appeals. ESA-WCA outcomes to March 2016 (MRs to July 2016); 2016. ↩
-
Department for Work and Pensions. Employment and Support Allowance: Work Capability Assessments, Mandatory Reconsiderations and Appeals. ESA-WCA outcomes to March 2016 (MRs to July 2016); 2016. ↩
-
Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016. ↩
-
Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016. ↩
-
Department for Work and Pensions. Work and Pensions Longitudinal Study, DWP Tabulation Tool February 2016. ↩
-
Department for Work and Pensions. DWP A Survey of Disabled Working Age Benefit Claimants; 2013. ↩
-
Rigg J. Labour Market Disadvantage amongst Disabled People: A longitudinal perspective. CASE paper No. 103. Centre for Analysis of Social Exclusion, London School of Economics; 2005. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
National Data Guardian. Review of Data Security, Consent and Opt-Outs; 2016. ↩
-
Gulliford J. Enabling work: disabled people, employment and the UK economy; 2015. ↩
-
Clark N. Enhancing performance through employee engagement – the MacLeod Review; 2010 ↩
-
Clark N. Enhancing performance through employee engagement – the MacLeod Review; 2010 ↩
-
Office for National Statistics.ONS Sickness Absence in the Labour Market: February 2014. 2014 ↩
-
Confederation of British Industry. CBIFit for purpose: Absence and workplace health survey 2013; 2013 ↩
-
Office for National Statistics.ONS. Principal Population Projections; 2015. ↩
-
Oxford Economics. The cost of the brain drain: understanding the financial impact of staff turnover; 2014. ↩
-
Gabbay M, Taylor L, Sheppard L, Hillage J, Bambra C, Ford F, et al. NICE guidance on long-term sickness and incapacity. British Journal of General Practice.Brit J Gen Pract. 2011;61(584):206-7. ↩
-
Black C, Frost D. Health at work – an independent review of sickness absence: 2011. ↩
-
Department for Work and Pensions. Annual net income of households containing a disabled person 2012 to 2013; 2014. ↩
-
The Civil Service measures average working days lost (AWDL) per staff year, based on hours actually worked by employees. This produces a more accurate but generally higher absence figure than the AWDL per person figure used for external comparisons. Source: Department for Work and Pensions. Sick Leave: Written question – 29117. (accessed October 2016). ↩
-
Chartered Institute of Personnel and Development. Absence measurement and management fact sheet. (accessed October 2016). CIPD October 2015 ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Although public sector bodies are required to publish employment data concerning protected characteristics under the Public Sector Equality Duty under the Equality Act 2010. ↩
-
Organisation for Economic Co-operation and Development. OECD’sSickness, Disability and Work, Breaking the Barriers; 2010. ↩
-
Workplace Equality Index. (accessed October 2016). ↩
-
Workplace Wellbeing Index. (accessed October 2016). ↩
-
The Disability Charities Consortium is made up of eight of the largest disability charities in the UK: Action on Hearing Loss, Disability Rights UK, Leonard Cheshire Disability, Mencap, Mind, National Autistic Society, RNIB, and Scope. ↩
-
Poor health but not absent: Prevalence, predictors and outcomes of presenteeism. Journal of Occupational and Environmental Medicine 2012 54: 1344–9. ↩
-
Tait et al. Impact of Organizational Leadership on Physician Burnout and Satisfaction. Mayo Clinic Proceedings 2015: 90, (4); 432–440. ↩
-
Healthy Workplace Charter Greater London Authority. ↩
-
Health and Safety Executive. What are the Management Standards ↩
-
NHS Scotland. Healthy Working Lives Case Study. ↩
-
Building the case for wellness; 2008 PricewaterhouseCoopers LLP. ↩
-
Health and Wellbeing at work: a survey of Employees. 2014. DWP Research Report 901; 2015. Read Karen Steadman’s blog. ↩
-
Routes onto Employment and Support Allowance DWP Research Report 774; 2011. ↩
-
Adam L, Oldfield K, Riley C, Duncan B, Downing C. Understanding the journeys from work to Employment and Support Allowance (ESA). DWPs Research Report No. 902; 2015. ↩
-
Sickness, Disability and Work: Breaking the Barriers. A synthesis of findings across OECD countries; 2010 ↩
-
Statutory Sick Pay is paid from the 4th consecutive day of absence at £88.45 per week for up to 28 weeks. Employers may also decide to pay employees their own occupational sick pay too. ↩
-
Centre for Economics and Business Research. The benefits of early intervention and rehabilitation; Supporting employees when they need it the most. London; 2015. Section 3.2 ↩
-
An Independent Review of the Work Capability Assessment – year four; 2013: Dr Paul Litchfield ↩
-
NHS Operational Planning and Contracting Guidance 2017-2019 ↩
-
General Practitioners’ attitudes towards patients’ health and work, 2010-12. DWP Research Report 835; 2013 ↩
-
Department for Work and Pensions Tabulation Tool : Employment and Support Allowance ↩
-
What works for whom in helping disabled people into work? Working paper 120. Department for Work and Pensions; 2013. ↩
-
McManus S, Bebbington P, Jenkins R, Brugha T. (eds.) Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey 2014. Leeds: NHS Digital; 2016. ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016 ↩
-
For instance, in 2015/16 43,000 people who finished a course of IAPT stated they were claiming ESA or a predecessor benefit: NHS Digital. Psychological Therapies: Annual Report on the use of IAPT services – England, 2015-16; 2016 ↩
-
Department for Work and Pensions Longitudinal Study, DWP Tabulation Tool; February 162016 ↩
-
McManus S, Bebbington P, Jenkins R, Brugha T. (eds.) (2016) Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey 2014. Leeds: NHS Digital. ↩
-
ONS Sickness Absence Report 2014 ↩
-
Department for Work and Pensions and Department of Health. Work, Health and Disability Green Paper Data Pack; 2016. ↩
-
Department for Work and Pensions Longitudinal Study, DWP Tabulation Tool; February 162016 ↩
-
Chartered Society of Physiotherapy. Stretched to the Limit; 2012 ↩
-
Care planning and musculoskeletal health; 2014 Arthritis Research UK. ↩
-
Fit For Work? Musculoskeletal Disorders in the European Workforce The Work Foundation; 2009 ↩
-
Health and Wellbeing at work: a survey of Employees 2014. DWP Research Report 901; 2015. Also read blog by Karen Steadman: Working for better mental health - results from a survey of employees ↩
-
The 41,708 figure is derived by subtracting total figures for ‘current registered numbers’ from total figures for ‘Number required to deliver a quality service to the current UK workforce’ in Figure 5. The Council for Work and Health. Planning the future: Implications for occupational health; delivery and training; 2016. ↩
-
Working for a Healthier Tomorrow Dame Carol Black’s Review of the health of Britain’s working age population; 2008. ↩
-
Integrated care for patients and populations: Improving outcomes by working together. A report to the Department of Health and the NHS Future Forum; 2012. ↩
-
Is Work Good for Your Health and Wellbeing? Report by Gordon Waddell and Kim Burton ↩
-
Faculty of Occupational Medicine. Press Release Work is a health outcome and improves mental health: we can’t afford to ignore this ↩
-
NICE guidance Low back pain and sciatica: management of non-specific low back pain and sciatica, (Draft); 2016 ↩
-
Delivering better services for people with long term condition The King’s Fund; 2013. ↩
-
A survey of disabled working age benefit claimants. In House Research Report No 16. Department for Work and Pensions; 2013. ↩
-
General Practitioners’ attitudes towards patients’ health and work, 2010–12 ↩
-
McCluskey S. et al. The Influence of ‘significant others’ on persistent back pain and work participation: A qualitative exploration of illness perceptions. BMC Musculoskeletal Disorders 2011;12:236. McCluskey, S. et al. Are the treatment expectations of ‘significant others’ psychosocial obstacles to work participation for those with persistent low back pain? Work 2014),;48:391-398. S. McCluskey et al. ‘I think positivity breeds positivity’: a qualitative exploration of the role of family members in supporting those with chronic musculoskeletal pain to stay at work. BMC Family Practice 2015;16:85. ↩
-
A survey of disabled working age benefit claimants. In House Research Report No 16. Department for Work and Pensions; 2013. ↩
