Appendices: assessing fitness to drive
Appendix to the assessing fitness to drive guide for medical professionals.
Appendix A: The legal basis for the medical standards
The Secretary of State for Transport, acting through DVLA, has the responsibility of ensuring all licence holders are fit to drive.
The legal basis of fitness to drive in the UK lies in the following legislation:
- The Road Traffic Act 1988
- The Motor Vehicles (Driving Licences) Regulations 1999 (as amended)
According to Section 92 of the Road Traffic Act 1988:
- A relevant disability is any condition which is either prescribed in regulations or any other disability where driving is likely to be a source of danger to the public. A driver who is suffering from a relevant disability must not be licensed, but there are some prescribed disabilities where licensing is permitted provided certain conditions are met.
- Prospective disabilities are any medical conditions that, because of their progressive or intermittent nature, may develop into relevant disabilities in time. Examples are Parkinson’s disease and early dementia. A driver with a prospective disability may be granted a driving licence for up to 5 years, after which renewal requires further medical review.
Sections 92 and 94 of the Road Traffic Act 1988 also cover drivers with physical disabilities who require adaptations to their vehicles to ensure safe control. These adaptations must be coded and shown on the licence. See Appendix G, disabilities and vehicle adaptations and Appendix H, Mobility Centres and Driving Assessment Centres.
‘Serious neurological disorders’
The law requires that driving licences shall not be issued to, nor renewed for, applicants with serious neurological disorders, unless supported by the applicant’s doctor.
A serious neurological disorder is defined for the purposes of driver licensing as any condition of the central or peripheral nervous system that has led, or may lead, to functional deficiency (sensory, including special senses, motor, and/or cognitive deficiency), and that could affect ability to drive.
When DVLA evaluates the licensing of these applicants, it will consider the functional status and risk of progression. A short-term licence for renewal after medical review is generally issued whenever there is a risk of progression.
Further information relating to specific functional criteria is found in the following sections:
- neurological disorders
- psychiatric disorders
- visual disorders
- miscellaneous conditions – excessive sleepiness
Appendix B: Epilepsy and seizure rules and further guidance
The legislation governing drivers who experience a seizure
The following 2 boxes extract the paragraphs from regulations 72 and 73 of the Motor Vehicle (Driving Licences) Regulations 1999 (as amended) that govern the way in which epilepsy is ‘prescribed’ as a ‘relevant’ disability for Group 1 or Group 2 drivers (also see Appendix A, the legal basis for the medical standards).
Group 1 car and motorcycle
Regulation 72
(2) Epilepsy is prescribed for the purposes of section 92(2) of the Traffic Act 1988 as a relevant disability in relation to an applicant for, or a holder of, a Group 1 licence who has had 2 or more epileptic seizures during the previous 5 year period.
(2A) Epilepsy is prescribed for the purposes of section 92(4)(b) of the Traffic Act 1988 in relation to an applicant for a Group 1 licence who satisfies the conditions set out in paragraph (2F) below and who has either:
(a) been free from any unprovoked seizure during the period of one year immediately preceding the date when the licence is granted
or
(b) during that one year period has suffered no unprovoked seizure other than a permitted seizure.
(2B) A permitted seizure for the purposes of paragraph (2A)(b) is:
(a) a seizure – which can include a medication-adjustment seizure – falling within only one of the permitted patterns of seizure, or
(b) a medication-adjustment seizure, where:
(i) that medication-adjustment seizure does not fall within a permitted pattern of seizure
(ii) previously effective medication has been reinstated for at least 6 months immediately preceding the date when the licence is granted
(iii) that seizure occurred more than 6 months before the date when the licence is granted, and
(iv) there have been no other unprovoked seizures since that seizure
or
(c) a seizure occurring before a medication-adjustment seizure permitted under sub-paragraph (b) where:
(i) that earlier seizure has, to that point, formed part of only one permitted pattern of seizure and had occurred prior to any medication-adjustment seizure not falling within the same permitted pattern
or
(ii) it is a medication-adjustment seizure, which was not followed by any other type of unprovoked seizure, except for another medication-adjustment seizure.
(2C) A permitted pattern of seizure for the purposes of paragraph (2B) is a pattern of seizures:
(a) occurring during sleep, where:
(i) there has been a seizure while asleep more than one year before the date when the licence is granted
(ii) there have been seizures only while asleep between the date of that seizure while asleep and the date the licence is granted
and
(iii) there has never been an unprovoked seizure while awake
or
(b) occurring during sleep, where:
(i) there has been a seizure while asleep more than 3 years before the date when the licence is granted
(ii) there have been seizures only while asleep between the date of that seizure while asleep and the date the licence is granted
and
(iii) there is also a history of unprovoked seizure while awake, the last of which occurred more than 3 years before the date when the licence is granted
or
(c) without influence on consciousness or the ability to act, where:
(i) such a seizure has occurred more than one year before the date when the licence is granted
(ii) there have only been such seizures between the date of that seizure and the date when the licence is granted
and
(iii) there has never been any other type of unprovoked seizure.
(2D) An isolated seizure is prescribed for the purposes of section 92(2) of the Traffic Act 1988 as a relevant disability in relation to an applicant for, or a holder of, a Group 1 licence.
(a) in a case where there is an underlying causative factor that may increase future risk, where such a seizure has occurred during the previous one year period
and
(b) in any other case, where such a seizure has occurred during the previous 6 month period.
(2E) An isolated seizure is prescribed for the purposes of section 92(4)(b) of the Traffic Act 1988 in relation to an applicant for a Group 1 licence, who:
(a)
(i) in a case where there is an underlying causative factor that may increase future risk, has had such a seizure more than one year immediately before the date when the licence is granted
and
(ii) in any other case, has had such a seizure more than 6 months immediately before the date when the licence is granted
(b) has had no other unprovoked seizure since that seizure
and
(c) satisfies the condition set out in paragraph (2F).
(2F) The conditions are that:
(a) so far as is predictable, the applicant complies with the directions regarding treatment for epilepsy or isolated seizure, including directions as to regular medical check-ups made as part of that treatment, which may from time to time be given by a registered medical practitioner or one of the clinical team working under the supervision of that registered medical practitioner
(b) if required to do so by the Secretary of State, the applicant has provided a signed declaration agreeing to observe the condition in sub-paragraph (a)
(c) if required by the Secretary of State, there has been an appropriate medical assessment by a registered medical practitioner
and
(d) the Secretary of State is satisfied that the driving of a vehicle by the applicant in accordance with the licence is not likely to be a source of danger to the public.
Group 2 bus and lorry
Regulation 73
(8) Epilepsy is prescribed for the purposes of section 92(2) of the Traffic Act as a relevant disability in relation to an applicant for, or a holder of, a Group 2 licence, where two or more epileptic seizures have occurred, or that person has been prescribed medication to treat epilepsy, during the previous ten year period.
(8A) Epilepsy is prescribed for the purposes of section 92(4)(b) of the Traffic Act 1988 in relation to an applicant for a group 2 licence who:
(a) in the case of a person whose last epileptic seizure was an isolated seizure satisfies the conditions in paragraph (8C) and (8D)
or
(b) in any other case, satisfies the conditions set out in paragraph (8D) and who, for a period of at least 10 years immediately preceding the date when the licence is granted has:
(i) been free from any epileptic seizure
and
(ii) has not been prescribed any medication to treat epilepsy.
(8B) An isolated seizure is prescribed for the purposes of section 92(2) of the Traffic Act 1988 as a relevant disability, in relation to an applicant for, or a holder of, a Group 2 licence, where during the previous 5 year period, such a seizure has occurred, or that person has been prescribed medication to treat epilepsy or a seizure.
(8C) An isolated seizure is prescribed for the purposes of section 92(4)(b) of the Traffic Act 1988 in relation to an applicant for a Group 2 licence who satisfies the conditions set out in paragraph (8D) and who, for a period of at least 5 years immediately preceding the date when the licence is granted:
(a) has been free from any unprovoked seizure
and
(b) has not been prescribed medication to treat epilepsy or a seizure.
(8D) The conditions are that:
(a) if required by the Secretary of State, there has been an appropriate medical assessment by a neurologist
and
(b) the Secretary of State is satisfied that the driving of a vehicle by the applicant, in accordance with the licence, is not likely to be a source of danger to the public.
Withdrawal of epilepsy medication
This guidance relates only to epilepsy treatment.
During epilepsy medication being withdrawn or changed on the advice of a healthcare professional, the risk of further epileptic seizures should be considered relating to the recommendations from DVLA, and regarding insurance implications, the driver should be advised to inform their insurance company.
If an epileptic seizure does occur, the patient will need to meet the medical standards before resuming driving and will need to be counselled accordingly. If the change is under medical supervision a reduced period of 6 months may apply.
It is clearly recognised that withdrawal of epilepsy medication is associated with a risk of seizure recurrence. A number of studies have shown this, including a randomised study of withdrawal in patients in remission conducted by the Medical Research Council’s study group on epilepsy drug withdrawal. This study showed a 40% increased risk of seizure associated with the first year of withdrawal compared with continued treatment.
The Secretary of State for Transport’s Honorary Medical Advisory Panel on Driving and Disorders of the Nervous System states that patients should be warned of the risk they run, both of losing their driving licence and of having a seizure that could result in a road traffic accident.
The Advisory Panel states that drivers should usually be advised not to drive from the start of the withdrawal period and for 6 months after treatment cessation – it considers that a person remains as much at risk of seizure during the withdrawal as during the following 6 months.
This advice may not be appropriate in every case, however. One specific example is withdrawal of anticonvulsant medication when there is a well-established history of seizures only while asleep.
In such cases, any restriction on driving is best determined by the healthcare professional concerned, after considering the history. It is the patient’s legal duty to comply with medical advice on driving.
It is important to remember that the driver licensing rules remain relevant in cases of medication being omitted as opposed to withdrawn, such as on admission to hospital.
For changes of medication, for example due to side effect profiles, the following general advice is applicable.
- When changing from one medication to another and both would be reasonably expected to be equally efficacious, then no period of time off driving is recommended.
- When the new medication is felt to be less efficacious than the previous medication, the 6 months off driving period is recommended. This time period would start from the end of the change over period.
Any restriction on driving is best determined by the healthcare professional concerned in light of the specific circumstances of the case and the patient’s history. Clinicians may want to consider whether restricting driving is appropriate where medication is being changed during or after pregnancy due to the effects of the pregnancy on drug metabolism.
Provoked seizures
To be considered a provoked seizure, the seizure must be attributable solely to a recognisable provoking cause and that causative factor must be reliably avoidable. It should be clear that the seizure has been provoked by a stimulus which is unlikely to be repeated. Driving will usually need to cease for 6 months (group 1) (in the absence of previous unprovoked seizures or existing cerebral pathology) or up to 5 years (group 2) following a provoked seizure.
Doctors may wish to advise patients that the likely total period of time they will be required by DVLA not to drive will be extended if there is a previous history of unprovoked seizure or evidence of pre-existing cerebral pathology (e.g. longstanding cerebral lesion, epileptic activity on EEG or evidence of fixed neurological deficit), that increases the risk of further seizures.
The following seizures may be treated as provoked:
- true seizures associated with cardiovascular syncope (convulsive syncope is not considered to be a seizure and the relevant syncope standard must be met)
- seizure in the first week following a head injury
- seizure in the first week following a stroke, TIA or spontaneous acute subdural haematoma
- seizure during, or in the first week following, intracranial surgery
- seizure associated with severe electrolyte or biochemical disturbance (including hypoglycaemia) documented within 24 hours of specific biochemical or haematologic abnormalities
- seizure associated with drug or alcohol intoxication or withdrawal, or exposure to well-defined epileptogenic drugs
The following provoked seizures are excepted and do not require driving to cease, although the relevant medical standards for the underlying condition will have to be met:
- seizures occurring at the very moment of impact of a head injury
- eclamptic seizures
- seizures provoked by electroconvulsive therapy
- seizures occurring within 5 minutes of cessation of repetitive trans-cranial magnetic stimulation (rTMS)
When a Group 2 driver who has had a previous provoked seizure ceases to take anti-seizure medication then Group 2 driving will need to stop and the driver inform DVLA.
Appendix C: Cardiovascular considerations
Group 2 bus and lorry entitlement only
Licence duration
A bus or lorry (Group 2) licence issued after cardiac assessment for established cardiovascular disease will usually be short-term, for a maximum licence duration of 3 years, and licence renewal will require satisfactory medical reports.
Exercise tolerance testing
The preferred functional test to assess fitness to drive is an exercise tolerance test.
The requirements for exercise evaluation to assess fitness for Group 2 licensing are:
- Discontinuation of anti-anginal medication (i.e., nitrates, beta blockers, calcium channel blockers, nicorandil, ivabradine, and ranolazine) prior to exercise tolerance testing is not required.
- The default test should be a treadmill exercise test with the Bruce protocol.
- Bicycle ergometry is a suitable alternative when the individual cannot use the treadmill.
- The customer should be able to safely complete 3 stages (9 minutes) of the standard Bruce protocol (or cycle for 10 minutes with 20 W per minute increments, to a total of 200 W) without signs of cardiovascular dysfunction, such as:
- angina pectoris
- syncope
- fall in systolic blood pressure of 20mmHg or more
- arrhythmia that requires intervention or premature termination of the exercise test
- There must be no electrocardiographic ST segment deviation that is interpreted by a cardiologist to be indicative of inducible myocardial ischaemia (usually defined as at least 2 mm horizontal or down-sloping ST-segment depression or 2mm ST-segment elevation), either during exercise or the recovery period.
- When exercise testing is undertaken as part of medical enquiries regarding aortic stenosis, hypertrophic cardiomyopathy or cardiac transplantation, pre-existing ST segment abnormality may confound interpretation of any exercise-induced ST-segment deviation. In such cases, the test is undertaken to assess the haemodynamic response to exercise and as a marker of exercise capacity.
- Should atrial fibrillation develop de novo during exercise testing, the supervising clinician should determine whether it is appropriate to complete the test. If the test is completed and the DVLA exercise tolerance test criteria above are met, licensing will be subject to echocardiographic confirmation that left ventricular ejection fraction is at least 40% and the licensing requirements for individuals with pre-existing atrial fibrillation (see Arrhythmias section in ‘Assessing fitness to drive: guide for medical professionals’).
- If there is established coronary heart disease, DVLA will require exercise or other functional evaluation at regular intervals not to exceed 3 years.
Stress myocardial perfusion scan or stress echocardiography
A functional imaging test (radionuclide stress myocardial perfusion imaging, stress echocardiography, or stress cardiac MRI) can be considered as an alternative to exercise testing for customers with:
- left bundle branch block (LBBB)
- right bundle branch block with QRS exceeding 120 ms
- paced rhythm
- musculoskeletal or other disability that prevents exercise on a treadmill or cycle ergometer
If the exercise standard cannot be met because of lack of fitness or other non-cardiac reasons, a report may be requested from the supervising clinician before a functional imaging test is commissioned.
The licensing standards for functional imaging tests are:
- no more than 10% of the left ventricular myocardium is affected by reversible ischaemic change on myocardial perfusion imaging
or
- no more than one segment is affected by reversible ischaemic change on stress echocardiography
Left ventricular ejection fraction
Group 2 licencing requires a resting left ventricular ejection fraction of at least 40%. The preferred methods for assessment of left ventricular function are echocardiography or cardiac magnetic resonance imaging.
Full DVLA protocol requirements for these tests are available on request (see contact details).
Coronary angiography
For licensing purposes in individuals with coronary artery disease, DVLA considers non-invasive functional assessment to be more important than angiographic assessment of coronary artery disease severity.
For this reason, coronary angiography is not commissioned by DVLA. Exercise tolerance testing and, where necessary, myocardial perfusion imaging or stress echocardiography are the investigations of relevance (outlined above) with the standards as indicated to be applied.
If there is a conflict between the results of a non-invasive functional test and recent (within 6 months) coronary angiography, the case will be considered individually. This assessment will take account of angiographic evidence of obstructive and non-obstructive coronary artery disease, and any evidence of functional coronary artery abnormality.
Marfan syndrome: aortic root surgery
Group 2 licencing after aortic surgery for Marfan syndrome will require individual assessment.
A bus or lorry licence for annual review may be issued after elective aortic root replacement surgery provided:
- surgery is successful without complications
- there is satisfactory regular specialist follow-up
- there is no evidence of suture-line aneurysm postoperatively and on 2-yearly MRI or CT surveillance
Group 2 licensing following elective external aortic support procedures will require individual consideration. Continued licensing thereafter will require regular clinical review, including MRI imaging one year after surgery and every 3 years thereafter.
Aortic stenosis (to include sub-aortic and supravalvular stenosis)
Aortic stenosis severity should be assessed from clinical, echocardiographic and biomarker parameters, in line with recommendations in 2021 ESC/EACTS guidelines for the management of valvular heart disease.
ESC Hypertrophic Cardiomyopathy Risk-SCD Calculator
This calculator is recommended by the European Society of Cardiology to assess sudden cardiac death (SCD) risk in individuals with hypertrophic cardiomyopathy. The calculator assigns individuals with hypertrophic cardiomyopathy to low risk (5-year risk of SCD less than 4%), intermediate risk (5-year risk of SCD 4 to 6%), or high risk (5-year risk of SCD equal to or greater than 6%) categories.
An online version of the calculator is available.
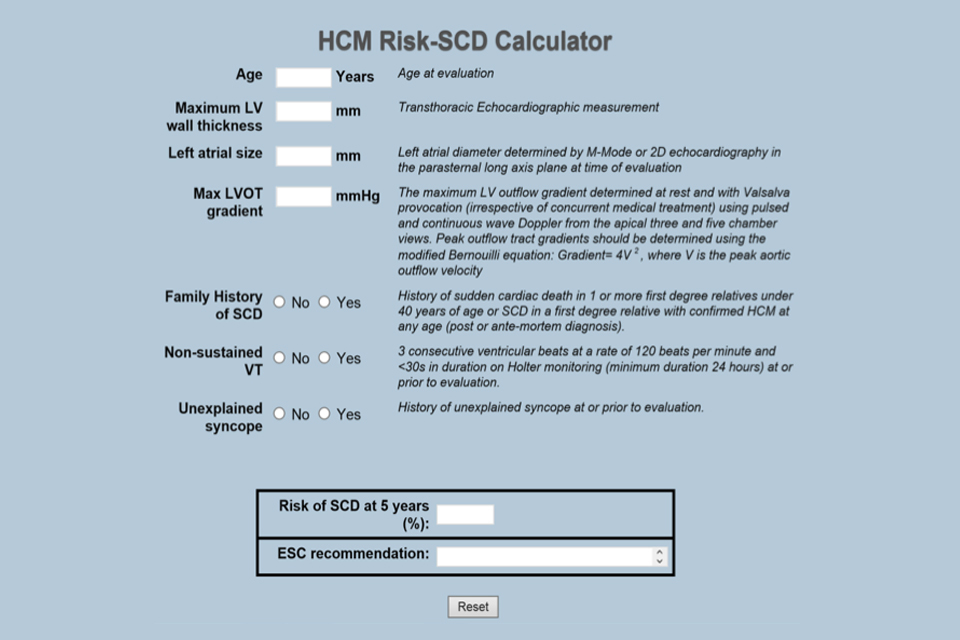
Image showing screenshot of risk calculator
Congenital heart disease
Complexity of congenital heart disease can be classified as mild, moderate or severe. Refer to table 4 in the 2020 European Society of Cardiology guidelines for the management of adult congenital heart disease.
Appendix D: Transient loss of consciousness (blackouts) and lost or altered awareness
Including blackout with seizure markers and cough syncope
Driving standards for non-traumatic transient loss of consciousness.
Transient loss of consciousness (TLoC) or ‘blackout’ unrelated to trauma is very common and affects up to half the population in the UK at some point in their lives.
TLoC is a state of real or apparent loss if consciousness which is associated with loss of awareness, amnesia for the period of unconsciousness, abnormal motor control, and loss of responsiveness. The condition is of short duration.
Following an episode of transient loss of consciousness, Group 1 and Group 2 drivers should be assessed as soon as possible by a healthcare professional to advise regarding driving implications as set out in this guidance.
If a healthcare professional can attribute a diagnosis to the episode(s) of TLoC then the relevant medical standard for that diagnosis will be applied from the appropriate section of this guide (neurological disorders, cardiovascular disorders or diabetes mellitus).
If a diagnosis cannot be attributed, or until a diagnosis is established, the standard for “unexplained loss of consciousness” will apply.
Causes of transient loss of consciousness relevant to driving include:
- syncope - see relevant section of this guidance
- epilepsy and seizures - see relevant section of the Neurological disorders guidance
- hypoglycaemia - see relevant section of the Diabetes mellitus guidance
- unexplained - see relevant section of this guidance
Other diagnosed causes of loss of consciousness will only require notification to DVLA and subsequent enquiry if medical opinion considers that they are relevant to driving. This will include episodes clinically attributed to Postural Orthostatic Tachycardia Syndrome (POTS) and orthostatic hypotension.
Syncope
Syncope is defined as transient loss of consciousness due to cerebral hypoperfusion, characterised by a rapid onset, short duration, and spontaneous complete recovery.
The term presyncope describes symptoms and signs of cerebral hypoperfusion that occur before complete loss of consciousness. For licensing decisions, an episode of presyncope without progression to TLoC is relevant if medical opinion considers that the presyncope has caused an individual to be unable to safely control or stop a vehicle. In such cases, the standards for syncope will apply.
Causes of syncope relevant to driving include:
- reflex syncope (vasovagal/neurocardiogenic syncope and situational syncope)
- cardiac causes of syncope including arrhythmia and structural heart disease (including valve disease, pulmonary arterial hypertension, cardiomyopathy, and Brugada Syndrome)
Reflex syncope
The application of medical standards for reflex syncope requires a positive diagnosis based on clinical assessment and investigations. The diagnosis of reflex syncope is made on the balance of probability and if a clinician cannot attribute a cause of syncope, the standard for unexplained transient loss of consciousness will apply.
Reflex syncope can be associated with either or both:
- prodrome, such as sweating or feeling warm/hot before loss of consciousness
- provocation, such as pain, emotional stress or a medical procedure
Some episodes of reflex syncope are related to micturition, defecation, or swallowing (‘situational’ syncope).
A ‘reliable prodrome’ occurs predictably before syncope, is recognised by the driver as a warning of impending loss of consciousness and should be of sufficient duration to allow the driver to safely stop the vehicle.
An ‘avoidable provocation’ includes factors that may provoke syncope, but which can be avoided and are not expected to occur while driving, such as exposure to a medical procedure, or syncope after a prolonged period of standing (for example, soldier on parade).
Reflex syncope (often referred to as vasovagal syncope) with a reliable prodrome
| Group 1 Car and motorcycle |
Group 2 Bus and lorry |
|
|---|---|---|
| Single episode | ✓- If syncope has not occurred while driving, may drive and need not notify DVLA. ✘- If syncope has occurred while driving, then must not drive and need not notify DVLA. Driving may resume one month following the episode of syncope. Should a further episode occur within 24 months the guidance for multiple episodes will apply. |
! - Must notify DVLA. Should a further episode occur within 24 months the guidance for multiple episodes will apply. ✓- If syncope was associated with an avoidable provocation and did not occur while driving, may resume driving after recovery from the episode of syncope. ✘- If syncope was not associated with an avoidable provocation, or syncope occurred while driving, must not drive. Driving may resume 3 months following the syncopal episode subject to an appropriate specialist report.*** |
| Multiple episodes* (2 or more episodes in preceding 24 months) | ✓- If syncope has not occurred while driving, may drive and need not notify DVLA. ✘- If syncope has occurred while driving, must not drive and must notify DVLA. Driving may resume 3 months following the most recent episode of syncope. |
✘- Must notify DVLA and must not drive. ✓- If syncope is associated with an avoidable provocation and has not occurred while driving, may resume driving after recovery from the most recent episode of syncope. If syncope is not associated with an avoidable provocation or has occurred while driving, must not drive. Driving may resume 6 months following the most recent episode of syncope subject to an appropriate specialist report.*** |
Reflex syncope without a reliable prodrome
| Group 1 Car and motorcycle |
Group 2 Bus and lorry |
|
|---|---|---|
| Single episode | ✘- Must not drive and must notify DVLA. ✓- If syncope was associated with an avoidable provocation and syncope did not occur while driving, driving may resume after the recovery from the episode of syncope. If syncope was not associated with an avoidable provocation or has occurred while driving, driving may resume 3 months following the episode of syncope. |
✘- Must not drive and must notify DVLA. ! - If syncope was associated with an avoidable provocation and did not occur while driving, driving may resume 3 months following the syncope subject to an appropriate specialist report.*** ! - If syncope was not associated with avoidable provocation or has occurred while driving, driving may resume 12 months following the syncope subject to an appropriate specialist report.*** |
| Multiple episodes* (2 or more episodes in preceding 24 months) | ✘- Must not drive and must notify DVLA. If syncope is associated with an avoidable provocation and has not occurred while driving, driving may resume 3 months following the most recent episode of syncope. If syncope is not associated with an avoidable provocation or has occurred while driving, driving may resume 6 months following the most recent episode of syncope. |
✘- Must not drive and must notify DVLA. Relicensing may be considered 12 months following the most recent episode, subject to an appropriate specialist report.*** |
*this standard should apply when any of the multiple episodes occurs without a reliable prodrome.
Unexplained loss of consciousness
Unexplained loss of consciousness (without seizure markers)
| Group 1 Car and motorcycle |
Group 2 Bus and lorry |
|
|---|---|---|
| Single episode | ✘- Must not drive and must notify DVLA. May resume driving 6 months after the episode of unexplained loss of consciousness. If the cause of loss of consciousness is established the relevant standard should be applied from the appropriate section of this guide. |
✘- Must not drive and must notify DVLA. Licence will be revoked for 12 months. If the cause of loss of consciousness is established the relevant standard should be applied. |
| Multiple episodes** (2 or more episodes within a 24 month period unless the most recent episode of that cluster has occurred more than 5 years ago) | ✘- Must not drive and must notify DVLA. Licence will be revoked for 12 months after most recent episode of unexplained loss of consciousness. If the cause of loss of consciousness is established the relevant standard should be applied from the appropriate section of this guide. |
✘- Must not drive and must notify DVLA. Licence will be revoked for 5 years after most recent episode of unexplained loss of consciousness. If the cause of loss of consciousness is established the relevant standard should be applied. |
** for multiple episodes of mixed presentation/aetiology the relevant standard applies to each episode of loss of consciousness.
Note
***An “appropriate specialist” is a clinician (doctor or other healthcare provider) whose work regularly results in exposure to this medical condition. Examples would include clinicians who undertake independent decision making in neurology clinic, cardiology clinics, syncope clinics, and so on.
The content of a specialist report should include:
- the level if confidence in any diagnosis of reflex syncope
- confirmation as to whether syncope has ever occurred whilst driving
- confirmation as to the presence or absence of reliable prodrome
- discussion of any provocation
- opinion (balance of probability) of the risk of further episodes with regard to the 20% per year threshold for Group 1 licensing and the equivalent 2% per year threshold for Group 2 licensing
Blackouts with seizure markers
This category is for those where on the balance of probability there is clinical suspicion of a seizure but no definite evidence. Individuals will require assessment by an appropriate specialist and investigation, for example EEG and brain scan, where indicated.
The following factors indicate a likely seizure:
- loss of consciousness for more than 5 minutes
- amnesia longer than 5 minutes
- injury
- tongue biting
- incontinence
- post ictal confusion
- headache post attack
| Group 1 Car and motorcycle |
Group 2 Bus and lorry |
|
|---|---|---|
| Isolated episode | ✘- Must stop driving and notify DVLA. 6 months off driving from the date of the episode. If there are factors that may lead to an increased risk of recurrence, 12 months off driving would be required. |
✘ - Must stop driving and notify DVLA. 5 years off driving from the date of the episode. |
| Recurrent episodes | ✘- Must stop driving and notify DVLA. Depending on previous medical history, the standards for isolated seizure or epilepsy will apply. |
✘- Must stop driving and notify DVLA. Depending on previous medical history, the standards for isolated seizure or epilepsy will apply. |
Cough syncope
Having experienced an episode or episodes of cough syncope, a person has identified themselves as being in a higher risk group that is predisposed to cough syncope. Therefore, even if the cough syncope episode occurred during a short-lived period of increased cough (such as an episode of acute respiratory infection), this would not alter the fact that the person is then at a higher risk of experiencing an episode of cough syncope whenever they cough, regardless of the cause.
Treatment, management or resolution of the condition which caused the cough does not reduce the risk of syncope with further episodes of cough.
| Group 1 Car and motorcycle |
Group 2 Bus and lorry |
|---|---|
| ✘- Must not drive and must notify DVLA. Must not drive for 6 months following a single episode and for 12 months following multiple episodes over 5 years. If more than one episode of cough syncope occurs within a 24 hour period, this will be counted as a single event. However, if the episodes of cough syncope are more than 24 hours apart, these are considered as multiple episodes. |
✘- Must not drive and must notify DVLA. Must not drive for 12 months following a single episode and 5 years following multiple episodes over 5 years. If more than one episode of cough syncope occurs within a 24 hour period, this will be counted as a single event. However, if the episodes of cough syncope are more than 24 hours apart, these are considered as multiple episodes. |
Appendix E: INF188/2 leaflet
Information for drivers with diabetes, including the INF294 leaflet.
Appendix F: Important notes concerning psychiatric disorders
All mental health symptoms must be considered
Any psychiatric condition that does not fit neatly into the classifications of the Psychiatric disorders section will need to be reported to DVLA if it is causing or is considered likely to cause symptoms that would affect driving.
Such symptoms include, for example:
- any impairment of consciousness or awareness
- any increased liability to distraction
- or any other symptoms affecting the safe operation of the vehicle
The patient should be advised to declare both the condition and the symptoms of concern.
It is the relationship of symptoms to driving that is of importance.
The law sets out the minimum medical standards of fitness to drive and the requirements for mental health in broad terms state that:
- there is a clear distinction between the standards for Group 1 car and motorcycle, and Group 2 bus and lorry licensing. The standards for the latter are more stringent because of the size of the vehicles and the greater amounts of time spent at the wheel by occupational drivers
- severe mental disorder is a prescribed disability for the purposes of section 92 of the Road Traffic Act 1988. Regulations define “severe mental disorder” as including mental illness, arrested or incomplete development of the mind, psychopathic disorder, and severe impairment of intelligence or social functioning
- the standards of fitness to drive must reflect, not only the need for an improvement in the mental state, but also a period of stability, such that the risk of relapse can be assessed should the patient fail to recognise any deterioration
- misuse of or dependence on alcohol or drugs are cases that require consideration of the standards, in addition to those for psychiatric disorders
Medications
Section 4 of the Road Traffic Act 1988 does not differentiate between illicit and prescribed drugs.
Any person driving or attempting to drive on a public highway or other public place while unfit due to any drug is liable for prosecution.
- All drugs with an action on the central nervous system can impair alertness, concentration and driving performance.
- This is of particular relevance at the initiation of treatment, or soon after, and also when dosage is being increased. Anyone who is adversely affected must not drive.
- It should be taken into account when planning the treatment of a patient who is a professional driver that the older tricyclic antidepressants can have pronounced anticholinergic and antihistaminic effects, which may impair driving, whereas the more recently developed antidepressants may have fewer such effects.
- Antipsychotic drugs, including depot preparations, can cause motor or extrapyramidal effects as well as sedation or poor concentration. These effects, either alone or in combination, may be sufficient to impair driving, and careful clinical assessment is required.
- The epileptogenic potential of psychotropic medication should be given particular consideration in patients who are professional drivers.
- Benzodiazepines are the psychotropic medications most likely to impair driving performance – the long-acting compounds in particular – and alcohol will potentiate effects.
- Doctors have a duty of care to advise their patients of the potential dangers of adverse effects from medications and their interactions with other substances, especially alcohol.
Electroconvulsive therapy
The likely severity of the underlying condition requiring electroconvulsive therapy (ECT) means the driver should be advised that they must notify DVLA.
Electroconvulsive therapy is usually employed in the context of an acute intervention for a severe depressive illness or, less commonly, as longer-term maintenance therapy.
In both courses, it is the severity of the underlying mental health condition that is of prime importance to the determination of whether driving may be permitted.
A seizure induced by ECT is regarded as provoked for the purposes of fitness to drive and is not a bar to licensing and driving – under both Group 1 car and motorcycle, and Group 2 bus and lorry.
The concerns for driving are:
- severity of the underlying illness requiring ECT treatment
- potential cognitive or memory disturbances associated with both the underlying depression and the ECT therapy
Driving must stop during an acute course of treatment with ECT and is not permitted until the relevant medical standards and observation periods associated with underlying conditions have been met, as set out in the Psychiatric disorders section and with respect to any other mental health symptoms or psychiatric conditions that do not fit neatly into classifications.
Again, this guidance must stress that the underlying condition and response to treatment are what determine licensing and driving.
Where ECT is used as maintenance treatment with a single treatment sometimes given weeks apart there may be minimal or no symptoms. This would not affect driving or licensing providing there is no relapse of the underlying condition.
Driving must stop for 48 hours following the administration of an anaesthetic agent.
Appendix G: Disabilities and vehicle adaptations
Group 1 car and motorcycle
Driving often remains possible with certain adjustments for a disability, whether for a static and progressive disorder or a relapsing one. These vehicle modifications may be needed for:
- permanent limb and spinal disabilities – for example, amputation, hemiplegia, cerebral palsy, ankylosing spondylitis, or severe arthritis (especially with pain)
- chronic neurological disorders – for example, multiple sclerosis, Parkinson’s disease, motor neurone disease, or peripheral neuropathy
Vehicle adaptations range from simple automatic transmission for many disorders, to sophisticated modifications such as joysticks and infrared controls for people with severe disabilities.
DVLA will need to know about a disability and whether any controls require modification, and will ask the patient to complete a simple questionnaire.
The driving licence is coded to reflect any vehicle modifications.
Assessment centres offer people advice about driving with a disability (these are listed in Appendix H).
Note that a person in receipt of the mobility component of Personal Independence Payment (PIP) can hold a driving licence from 16 years of age. (A person can’t apply for PIP until their 16th birthday.)
Group 2 bus and lorry
Some disabilities, if mild and non-progressive, may be compatible with driving large vehicles. DVLA needs to be notified and will require an individual assessment.
Mobility scooters and powered wheelchairs
Users of Class 2 or 3 mobility vehicles – which are limited to 4 mph or 8 mph respectively – are not required to hold a driving licence, and they do not need to meet the medical standards for driving motor vehicles. DVLA recommends the following, however:
- individuals with a medical condition that may affect their ability to drive these mobility vehicles should consult their GP first
- users should be able to read a car number plate from a distance of 12.3 metres
For more information, see Mobility scooters and powered wheelchairs: the rules.
Appendix H: Mobility Centres and Driving Assessment Centres
Find a centre on the Driving Mobility website.
Updates to this page
-
Correction to the advice for Group 2 drivers with reflex syncope, regarding the occurrence of episodes.
-
Under the heading ‘Reflex syncope’, the table ‘Reflex syncope without a reliable prodrome’ has been updated for Group 1 drivers who have experienced multiple episodes of syncope.
-
Addition of a new appendix titled - 'Appendix D: Transient loss of consciousness (blackouts) and lost or altered awareness', removed from neurology chapter. References to new appendix are now included in both neurology and cardiovascular chapter.
-
Changes to the ‘Withdrawal of epilepsy medication’ section and the actions taken by healthcare professionals.’ Changes to ‘Provoked seizures’ to clarify the action a Group 2 driver should take when stopping anti-seizure medication.
-
Minor grammar changes to Appendix A. Clarification of the provoked seizure paragraphs in Appendix B. Significant changes to Appendix C for cardiovascular considerations, including exercise tolerance testing, stress myocardial perfusion scanning, coronary angiography, marfan syndrome, aortic stenosis and congenital heart disease. To note there have been no changes to the standards, the wording and testing requirements have been clarified.
-
Hypertrophic cardiomyopathy – interpretation of ECG changes during exercise testing (Appendix C). Congenital heart disease – referencing of classification of complexity of congenital heart disease (Appendix C).
-
Changes to the style of the text.
-
Clarification regarding provoked seizures, including confirmation that eclamptic seizures do not require time from driving.
-
Appendix G: list of mobility centres and driving assessment centres replaced with new search tool on the Driving Mobility website.
-
Panel updates.
-
Panel updates.
-
Appendix B - Rewritten section on provoked seizures. Appendix C - Inclusion of the European Society of Cardiology Risk of Sudden Cardiac Death calculator.
-
First published.