Adult social care monthly statistics, England: July 2021
Updated 27 August 2021
Applies to England
Main points
Vaccination in social care settings
As of 22 June 2021, the proportions who had received both doses of the COVID-19 vaccine were:
-
92.2% of residents and 72.8% of staff of older adult care homes
-
86.1% of residents of younger adult care homes
-
70.1% of staff of younger adult care homes, 57.8% of domiciliary care staff and 29.1% of staff employed in other social care settings
Infection control measures in social care settings
In the week ending 22 June 2021:
- 93.0% of care homes in England were able to accommodate residents receiving visitors within care homes, compared to 40.3% at the beginning of March 2021
- 83.8% of care homes who had staff required to self-isolate paid those staff their full wages while self-isolating. This proportion has remained consistent since mid-December
- 76.1% of care homes had no staff members working in another health or social care setting, this proportion has remained largely consistent since mid-December
Personal protective equipment (PPE) availability in care homes
In the week ending 22 June 2021:
- 0.2% of care homes and 0.8% of domiciliary care providers in England had either no supply or were expecting to experience a shortage in the next 48 hours of at least one item of PPE. For care homes, this has been gradually decreasing since late September when 1.1% of care homes were experiencing a shortage
COVID-19 testing in care homes
ln the week ending 22 June 2021:
-
there were 409,743 PCR tests and 473,292 LFD tests taken by care home staff. There were 767 positive results returned from PCR tests and 444 returned from LFD tests. Between mid-May and the end of June, there has been a gradual increase in the number of positive PCR and LFD tests returned from care home staff, but this is still substantially fewer compared to mid-January
-
there were 83,621 PCR tests and 12,030 LFD tests taken by care home residents. There were 110 positive results returned from PCR tests and 12 returned from LFD tests. Between mid-May and the end of June, the number of positive PCR and LFD tests returned from care home residents has been broadly stable and remains substantially lower than mid-January levels.
Introduction
This is a monthly publication by the Department of Health and Social Care (DHSC) of statistics on adult social care in England. This statistical bulletin provides an overview on a range of information on social care settings, with a focus on the impact of COVID-19.
This report provides newly published information on:
-
selected infection prevention control (IPC) measures in care homes at national, regional and local authority (LA) level
-
staffing levels in care homes at national, regional and LA level
-
personal protective equipment (PPE) availability in care homes and domiciliary care at national, regional and LA level
-
testing for COVID-19 in care homes at national, regional and LA level
This report also includes previously published statistics on first and second dose uptake of COVID-19 vaccinations in adult social care settings.
For more information and links to other published sources of adult social care data please see the About this data section below.
Publication updates
This report for July 2021 now includes data on the following areas for the first time:
- personal protective equipment (PPE) availability for domiciliary care staff at national, regional and LA level
This report contains an update to the methodology for the COVID-19 testing in care homes data. The time series in this report has been backdated with the new methodology. For more details on the change see the COVID-19 testing in adult care homes section.
The next publication will be published on 12 August 2021. Dates for future publications will be pre-announced on the GOV.UK publication release calendar.
COVID-19 vaccination in adult social care settings
The NHS started administering vaccinations for COVID-19 in England on 8 December 2020. Social care staff and residents of care homes were prioritised for the vaccine according to the Joint Committee on Vaccination and Immunisation (JCVI) recommendation. For more information see guidance on priority groups for coronavirus (COVID-19) vaccination: advice from the JCVI.
Adult social care groups covered in this publication by JCVI priority group
This is a summary of the priority groups for different social care staff and residents.
JCVI priority group 1
-
residents in older adult care homes
-
staff directly employed by older adult care homes
-
agency staff working in older adult care homes
JCVI priority group 2
-
staff directly employed by younger adult care homes
-
agency staff working in younger adult care homes
-
domiciliary care staff registered to independent CQC providers
-
social care staff working in other settings (including non-registered providers and local authority employed)
Not in a specific JCVI priority group
- residents of younger adult care homes
How the data can be used
This data can be used for:
-
comparing vaccination rates across local authorities and regions in England as self-reported by care providers
-
monitoring vaccination rates over time
This data cannot be used for:
- estimating the number of social care staff or residents who have not been vaccinated
- comparing with vaccination rates in other countries of the UK
- directly comparing vaccination take up rates between different types of care home staff (directly employed and agency staff)
- estimating the number of vaccinations delivered each day
The total number of staff and residents for each social care setting as well as the number vaccinated are self-reported by the care provider and local authorities (LAs). Some care providers have reported the total number of staff or residents but not the numbers vaccinated and as a result of this, vaccination rates are affected by response rates. This is particularly prominent for second dose vaccination rates which have a lower response rate and as a result second dose vaccination rates may be underestimated. Full details on the response rates can be found in the accompanying methodology note.
COVID-19 vaccinations in JCVI priority group 1
First COVID-19 vaccine dose
95.5% of residents and 84.9% of older adult care home staff have received their first dose as of 22 June 2021. The proportion rapidly increased between January and February 2021 and has since continued to increase but at a slower pace as more of the population receive the first dose of the vaccine.
Among older adult care home staff, there is a substantial difference in reported vaccination rates between staff directly employed by care homes and staff employed by agencies operating within care homes. As of 22 June 2021, 85.9% of staff directly employed by care homes received their first dose, compared to only 60.0% of agency staff. This could be due to a different uptake of the vaccine but differing rates of unknown vaccination status across the staffing groups may also be a factor.
Therefore, directly comparing the vaccination rate of directly employed staff to agency staff should be done with caution as the 2 groups are likely to have different percentages of staff whose vaccination status is unknown. Care homes are less likely to know the vaccination status of their agency staff due to the nature of their employment. For more information, please refer to the accompanying background quality and methodology note.
First dose vaccination rates are similar across all regions for residents in older adult care homes. For staff in older adult care homes, first dose vaccination rates are also similar across regions with the exception of the North East which has a higher rate of 89.1% and London with a lower rate of 79.2%.
Second COVID-19 vaccine dose
As of 22 June 2021, 92.2% of residents and 72.8% of older adult care home staff have also received their second dose. The difference between staff directly employed by care homes and agency staff is also substantial for the second dose with 73.9% compared to 42.6% of staff receiving the second dose, respectively.
The London region has a slightly lower second dose vaccination rate for older care residents than other regions, with 89.9% having received their second dose by 22 June 2021.
There is little variation across regions in second dose vaccination for staff in older care homes, with the exception of the North East region where 78.6% have received their second dose, and the London region where only 65.8% have received it.
Some care providers have reported the total number of staff or residents but not the numbers vaccinated and as a result of this, vaccination rates are affected by response rates. As of 22 June 2021, second dose vaccination has been reported at least once by 98.0% of older adult care homes.
Figure 1: cumulative proportion of JCVI priority group 1 staff and residents who have received the first and second doses, England
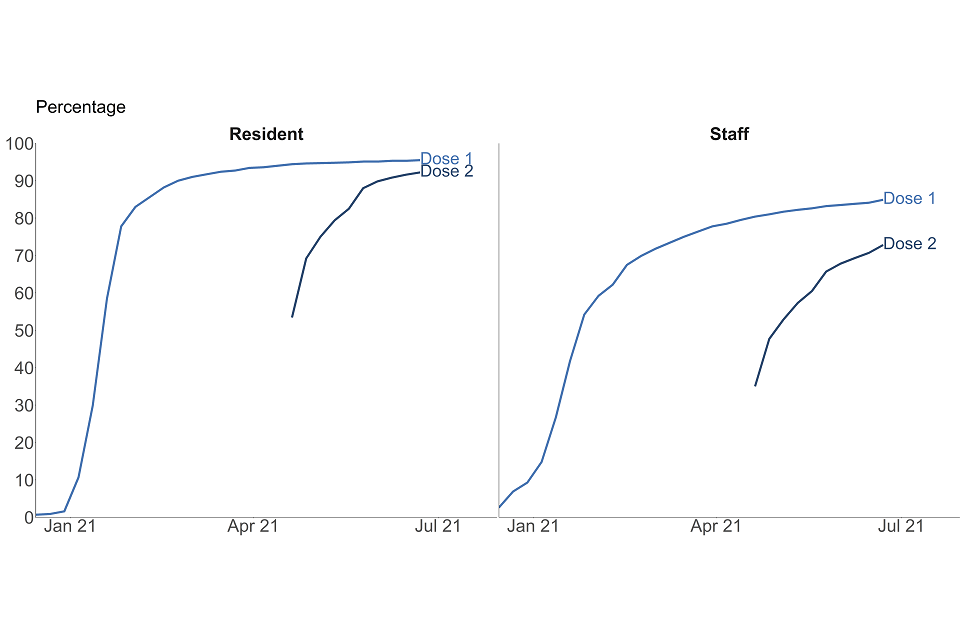
This data can be found in tables 1 and 2 of the accompanying ‘COVID-vaccination’ tables in addition to data by region and local authority. Data for the second COVID-19 vaccine dose became available on 20 April 2021.
COVID-19 vaccinations in JCVI priority group 2
First COVID-19 vaccine dose
81.9% of staff of younger adult care homes have received their first dose as of 22 June 2021. The proportion rapidly increased between January and March 2021 and has since continued to increase but at a slower pace as more of the population receive the vaccine.
Among staff of younger adult care homes, 83.3% of staff directly employed by younger adult care homes received their first dose compared to 59.3% of agency staff.
77.7% of domiciliary care staff and 75.7% of staff working in other settings have received their first dose as of 22 June 2021.
Second COVID-19 vaccine dose
70.1% of younger adult care home staff have received their second dose as 22 June 2021. There is a substantial difference between staff directly employed by care homes and agency staff with 71.8% and 41.1% of staff received the second dose, respectively.
57.8% of domiciliary care staff and 29.1% of staff working in other settings have received their second dose as of 22 June 2021.
Some care providers have reported the total number of staff or residents but not the numbers vaccinated and, as a result of this, vaccination rates are affected by response rates. As of 22 June 2021 second dose vaccination has been reported at least once by 97% of younger adult care homes, 92% of independent CQC-registered domiciliary care providers and 92 of 151 local authorities have reported data for staff working in other settings.
Figure 2: cumulative proportion of JCVI priority group 2 staff who have received the first and second doses, England
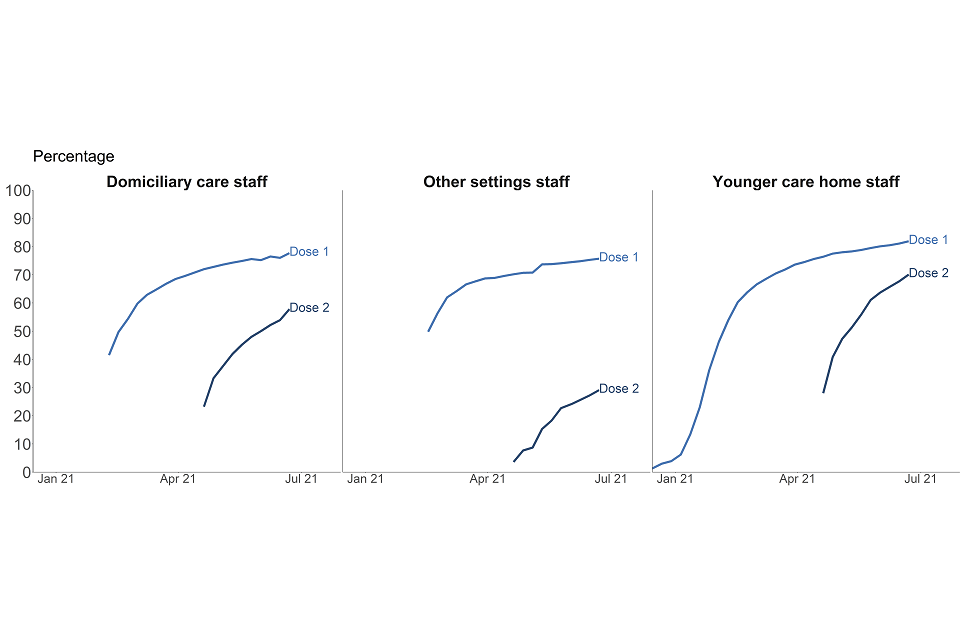
This data can be found in tables 6, 9 and 10 of the accompanying ‘COVID-vaccination’ tables in addition to data by region and local authority. Data collection for the second dose began on 20 April 2021.
There is notable regional variation for all staff groups in priority group 2.
Table 1: percentage of staff in JCVI priority group 2 who have received the first and second doses up to 25 May 2021 by region, England
| Region | Younger adult care homes: dose 1 | Younger adult care homes: dose 2 | Domiciliary care staff : dose 1 | Domiciliary care staff : dose 2 | Staff employed in other social care settings: dose 1 | Staff employed in other social care settings: dose 2 |
|---|---|---|---|---|---|---|
| East Midlands | 79.4 | 68.3 | 78.4 | 59.4 | 77.6 | 37.3 |
| East of England | 82.1 | 69.4 | 79.7 | 62.3 | 75.2 | 40.6 |
| London | 77.5 | 65.3 | 66.5 | 33.3 | 65.4 | 25.1 |
| North East | 89.7 | 80.8 | 86.4 | 69.3 | 87.6 | 13.6 |
| North West | 80.7 | 69.8 | 77.5 | 59.5 | 71.3 | 27.6 |
| South East | 82.1 | 69.6 | 79.7 | 62.2 | 78.8 | 25.7 |
| South West | 84.8 | 74.1 | 81.2 | 66.0 | 85.2 | 30.4 |
| West Midlands | 80.5 | 66.6 | 76.6 | 55.0 | 69.1 | 22.3 |
| Yorkshire and the Humber | 83.2 | 71.6 | 81.4 | 65.7 | 77.1 | 35.9 |
COVID-19 vaccinations for residents of younger adult care homes
Residents of younger adult care homes are not part of a single priority group. However, the conditions for which they reside in care homes are likely to make them more vulnerable to COVID-19 and they are therefore likely to be part of priority groups 3 to 9.
As of 22 June 2021, 92.1% of residents in younger care homes have received their first COVID-19 vaccine dose and 86.1% received their second dose.
Infection prevention control measures
How the data can be used
This data can be used for:
- estimating the number and proportion of care homes that indicate they:
- are accommodating COVID-safe visits within the care homes
- are paying full wages to their self-isolating staff
- restrict staff movement across settings
- monitoring trends over time
- comparisons across local authorities and regions in England
This data cannot be used for:
- estimating the number of visitors in care homes and their infection/vaccination status
- identifying the reasons for care home staff shortages and absences
- linking staff shortages and the number of positive cases among care home staff
- comparing with other countries of the UK
- linking staff movement across settings to positivity rates
The Adult Social Care Infection Control Fund provides funding from local authorities to ensure that infection prevention control (IPC) measures are in place to curb the spread of COVID-19. This publication provides data on how providers are implementing the following measures:
-
limitation of staff movement across different social care settings
-
accommodating COVID-19 safe visitation in care homes
-
payment of full wages when care home staff are isolating due to COVID-19
More details on the data collection, coverage and quality of this data can be found in the About this data section below.
Accommodating COVID-safe visitation in care homes
The guidance on allowing care home residents to have visitors has changed since December 2020 which is summarised in the table below.
Table 2: visiting guidance since December 2020
| Date | Guidance |
|---|---|
| 17 May 2021 to present | Residents are permitted to have 5 named visitors for regular visits with testing in place |
| 12 April 2021 to 16 May 2021 | Residents are permitted to have 2 named visitors for regular visits with testing in place |
| 8 March to 11 April 2021 | Residents are permitted to have 1 named visitor for indoor visits with testing in place |
| 6 January to 7 March 2021 | No indoor visits permitted due to the national lockdown |
| 1 January 2020 to 5 January 2021 | Indoor visits permitted with testing in place (from 19 December 2020 – no indoor visits permitted in Tier 4 areas) |
More information can be found in the guidance on care home visiting.
In the week ending 22 June 2021, 93.0 % of care homes in England were able to accommodate residents receiving visitors within care homes in all circumstances compared to 40.3% in the week ending 2 March 2021.
The number of providers accommodating visiting in all circumstances has been gradually increasing since early March in line with visitation guidance introduced on 8 March 2021 which allows residents to have designated regular visitors. A further 3.0% were able to accommodate visits in exceptional circumstances in the week ending 22 June 2021. Exceptional circumstances are individually defined by each care home but are generally thought to be considered when residents are palliative.
Between late December and early January 2021, the proportion of care homes accommodating visiting steadily declined in line with the change in guidance introduced, as well as the national lockdown.
There is substantial regional variation with 96.3% of care homes accommodating visitors in Yorkshire and The Humber in comparison to 87.1% in London in the week ending 22 June 2021.
Figure 3: proportion of care homes accommodating or limiting visits for residents, England
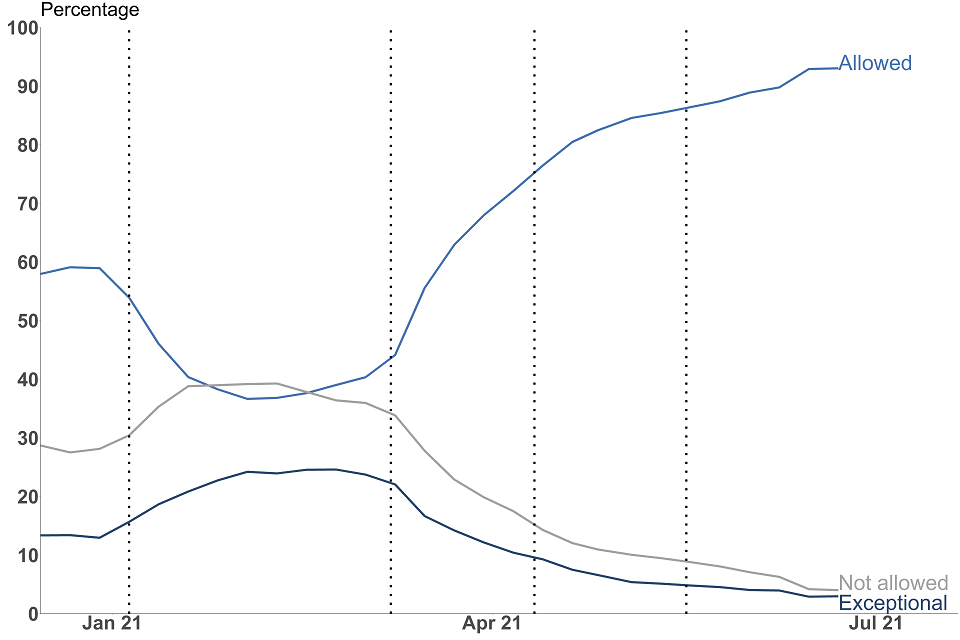
This data can be found in table 1 of the accompanying ‘Infection control’ tables in addition to data by region and local authority.
Payment of care home staff whilst self-isolating due to COVID-19
The infection control funds can be used to ensure staff who are self-isolating along with government guidance are paid their full wages. This includes:
-
staff isolating while waiting for a test
-
isolating after having tested positive or after a positive test in their household
-
staff required to quarantine prior to receiving certain NHS procedures
For more information see stay at home: guidance for households with possible or confirmed coronavirus (COVID-19) infection.
Employers who do not pay their staff their full wages whilst self-isolating must pay their staff at least Statutory Sick Pay (SSP) when the employee meets the following criteria:
-
is classed as an employee and has done some work for their employer
-
earns an average of at least £120 per week
-
has been ill or is self-isolating for at least 4 days in a row (including non-working days)
Care home staff who do not meet the criteria may not be eligible and as a result not paid to self-isolate. For more information, please see guidance on Statutory Sick Pay.
In the week ending 22 June 2021, 83.8% of care homes who had staff needing to self-isolate paid staff their full wages. This proportion has remained consistent since mid-December.
There is notable regional variation with 89.7% of providers in the North East paying their staff full wages compared to 76.4% in the West Midlands in the week ending 22 June 2021.
Figure 4: proportion of care homes by wages paid to staff during self-isolation in the week ending 25 May 2021, England
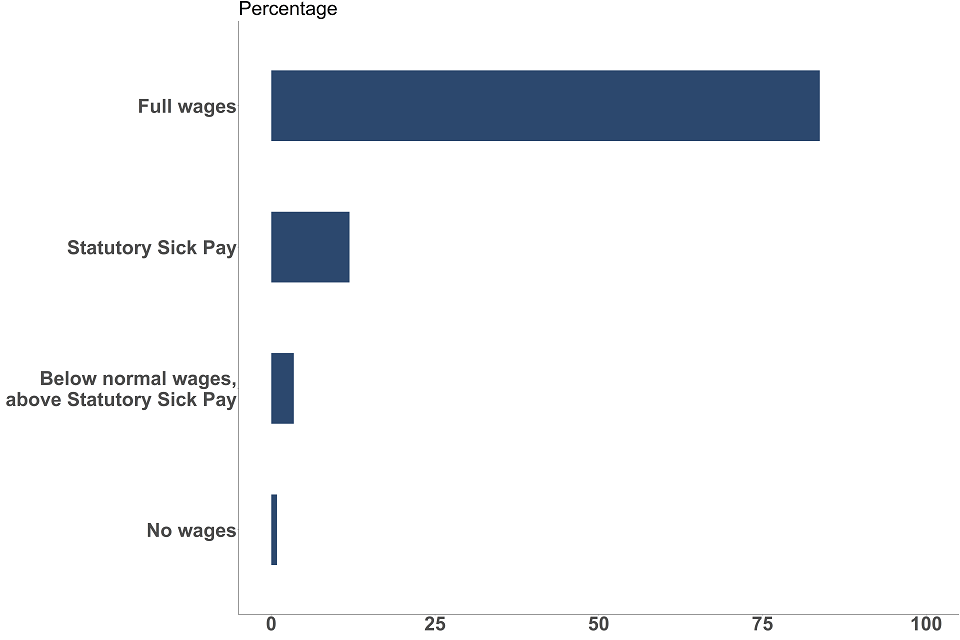
This data can be found in table 2 of the accompanying ‘Infection control’ tables in addition to data by region and local authority.
Limiting staff movement between care settings
Infection control funding can be used to reduce the need for staff movement between social care settings to limit the spread of infection, for example they can be used to recruit additional staff to enable staff to only work across one care home.
In the week ending 22 June 2021 76.1% of care homes had no staff members working in another social care setting, this proportion has remained largely consistent since mid-December 2020. 7.1% of care homes had some staff additionally working in another health or social care setting whilst a further 16.8% of care homes had some staff additionally working in another health or social care setting due to exceptional circumstances. Exceptional circumstances are defined as the care home having exhausted all other reasonable steps to ensure there are sufficient staffing levels.
Figure 5: proportion of care homes with no staff working in another health or social care setting in the week ending 25 May 2021, England
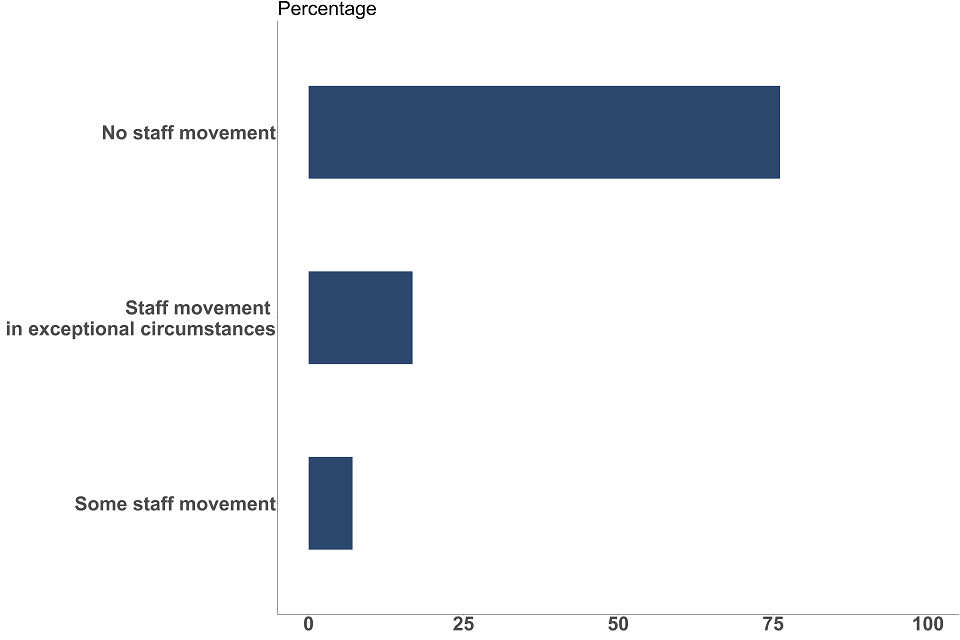
This data can be found in table 3 of the accompanying ‘Infection control’ tables in addition to data by region and local authority.
There is notable regional variation with 85.1% of providers in the North East having no staff working in another health or social care setting in the week ending 22 June 2021, in comparison to 68.1% in London.
Care home staffing levels
To enable providers to meet workforce challenges, such as maintaining safe staffing-levels over the winter period, on 16 January 2021 the government announced an extra £120 million Workforce Capacity Fund to support local authorities to manage workforce pressures.
In order to measure the workforce pressures on providers during the pandemic, each provider is asked to assess their workforce pressures based on their agreed staffing ratios.
In the week ending 22 June 2021, 0.2% of providers flagged that their agreed staffing ratios had been breached, 2.4% flagged that they were operating within the agreed staffing ratios but there is a significant risk of escalation in the coming days and 97.4% were operating within their agreed staffing ratios. This has remained consistent since mid-December 2020. If a care home’s staffing ratio has been breached, then business continuity measures may be put in place.
Figure 6: proportion of care homes where the agreed staffing ratios have been breached in the week ending 25 May 2021, England

This data can be found in table 4 of the accompanying ‘Infection control’ tables in addition to data by region and local authority.
PPE availability in care settings
How the data can be used
This data can be used for:
-
estimating the number and proportion of care homes and domiciliary care providers who are experiencing PPE shortages in the next 48 hours, and comparing across local authorities and regions in England
-
monitoring trends over time
This data cannot be used for:
- predicting PPE shortages in the coming weeks
- comparing with other countries of the UK
- linking PPE shortage to positivity rates
All care homes and domiciliary care providers are responsible for ensuring safe systems of work and have duties concerning the provision and use of PPE in the workplace.
This publication covers the availability of the following 5 items of PPE:
-
aprons
-
eye protection
-
gloves
-
hand sanitiser
-
face masks
In care homes
Guidance on what PPE should be used in various circumstances is available from Personal protective equipment (PPE): resource for care workers working in care homes during sustained COVID-19 transmission in England.
In the week ending 22 June 2021, 0.2% of care homes in England had either no supply or were expecting to experience a shortage in the next 48 hours of at least one item of PPE. This has been gradually decreasing since late September when 1.1% of care homes were experiencing a shortage.
In domiciliary care settings
Guidance on what PPE should be used in various circumstances is available from COVID-19: how to work safely in domiciliary care in England.
In the week ending 22 June 2021, 0.8% of domiciliary care providers in England reported having no supply or were expecting to experience a shortage in the next 48 hours of at least one item of PPE. This proportion has remained consistent since mid-December.
COVID-19 testing in adult care homes
How the data can be used
This data can be used for:
-
estimating the number of PCR and LFD tests taken and positive results returned in care homes, and comparing across local authorities and regions in England
-
estimating trends in prevalence and positivity rates for COVID-19 in care homes based on trends in positive tests
This data cannot be used for:
- calculating positivity rates for COVID-19 in care homes due to routine and repeat testing of individuals
- linking positivity rates in care homes to lower vaccination rates in care homes
- estimating the number of people tested and positive cases in care homes as people can take more than one test
The rollout of the testing programme in care homes is summarised in the About this data section. See the terminology section for more details on testing kits used.
This report contains an update to the methodology to the testing for COVID-19 in care homes data. Previously reports included tests where someone had identified their occupation as any of:
- care worker or home carer
- residential, day or domiciliary care manager or proprietor
- senior care worker
From the July report onwards, tests where someone has identified their occupation as one of the above and the test is associated with testing kits sent to domiciliary care providers have been removed from the counts.
The time series in this report has been revised and backdated with the new methodology and has resulted in the removal of a substantial number of staff tests compared to previous reports. The revisions have occurred in the period relating to 2 September 2020 to 25 May 2021 with around 1,500,000 PCR and 200,000 LFD tests being removed. As a result, some weeks’ counts have been revised down by up to 16% for PCR tests and 6% for LFD tests. Negative, positive and void tests have all been revised by similar proportions.
Data on testing in domiciliary care providers will be included in future reports.
Number of PCR and LFD tests conducted in adult care homes
Care home staff
The number of PCR tests conducted among care home staff in the weeks ending 13 April 2021 and 22 June 2021 were 418,109 and 409,743, respectively. Over this period, the number of PCR tests has remained broadly stable, with an average of 408,566 tests having been conducted.
The number of PCR tests conducted steeply increased from 257,113 tests in the week ending 8 September 2020 to 484,067 in the week ending 22 December 2020. A decrease in the number of tests was seen in the period between late December and early January due to the Christmas and New Year period. Between January 2021 and early April 2021, the number of PCR tests conducted gradually declined.
The number of LFD tests conducted among care home staff in the weeks ending 13 April 2021 and 22 June 2021 were 459,566 and 473,292, respectively. Over this period, the number of LFD tests has remained broadly stable, with an average of 462,167 tests having been conducted.
The number of LFD tests conducted among care home staff increased sharply from 46,019 tests in the week ending 29 December 2020[footnote 1], when LFD testing guidance was introduced, to 551,317 in the week ending 9 February 2021. Between early February 2021 and early April 2021, the number of LFD tests conducted then gradually declined.
Given that anyone who tests positive with a PCR test is exempt from regular testing for 90 days, the number of tests conducted with both PCR and LFD kits can fluctuate slightly in relation to COVID-19 prevalence.
Care home residents
The number of PCR tests conducted among care home residents increased from 76,134 tests in the week ending 8 September 2020 to 117,272 in the week ending 12 January 2021. Thereafter the number of tests begun to decline until mid-March and has since remained broadly consistent up to the end of June with 83,621 tests conducted in the week ending 22 June 2021.
The number of LFD tests conducted among care home residents gradually increased from late December 2020, reaching 14,115 in the week ending 2 March 2021. Thereafter the number of tests begun to decline with 5,711 tests conducted in the week ending 6 April 2021. This has since begun to gradually increase again with 12,030 tests conducted in the week ending 22 June 2021.
The testing regime for staff is more frequent than for residents (see the About this data section). As a result, the total number of staff tests is higher than the total number of resident tests.
Figure 7: number of PCR and LFD tests conducted in care homes, England
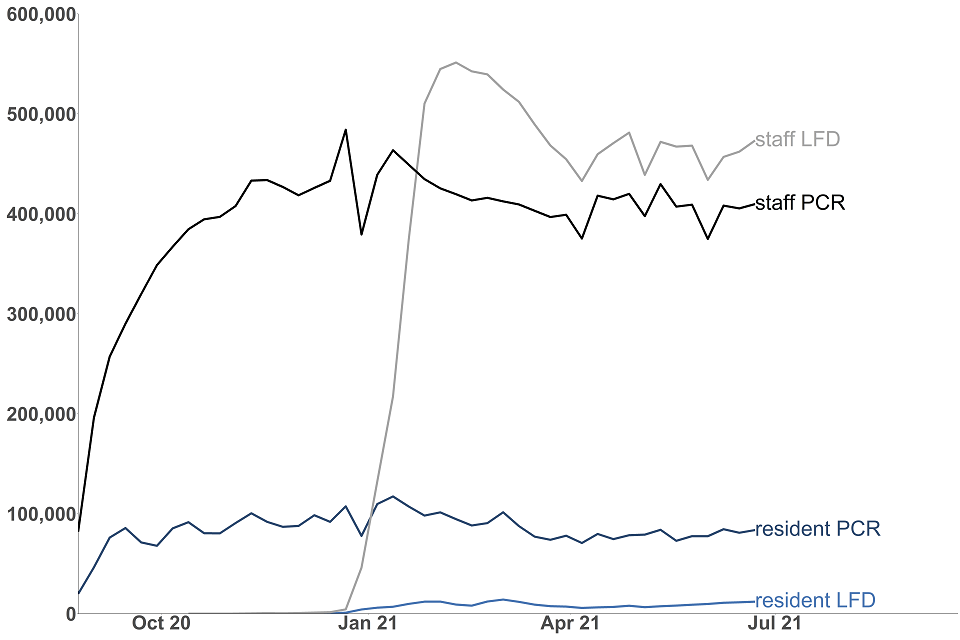
This data can be found in tables 1 and 2 of the accompanying ‘Testing’ tables in addition to data by region and local authority.
Visitors
Following the change in guidance for residents receiving visitors on 8 March 2021, there was a sharp increase of LFD tests conducted among visitors to residents of care homes, from 12,008 tests in the week ending 2 March 2021 to 44,854 tests in the week ending 16 March 2021. The number of tests conducted among visitors has been gradually increasing since with 97,330 tests in the week ending 22 June 2021.
Positive test results returned in adult care homes
Care home staff
The number of positive tests in care home staff has gradually increased between the end of May and the end of June. There were 278 positive LFD tests in the week ending 25 May 2021 compared to 444 positive tests in the week ending 22 June 2021. For PCR tests, there were 169 positive tests week ending 18 May 2021 compared to 767 in the week ending 22 June 2021.
The number of positive tests in the week ending 22 June 2021 is still substantially fewer than the levels seen in mid-January. The number of positive test results returned from PCR kits in care home staff steeply increased from 2,202 tests in the week ending 8 September 2020 to 18,295 in the week ending 12 January 2021. There were 3,137 positive test results returned from LFD kits in the week ending 12 January 2021.
Care home residents
The number of positive tests for care home residents at the end of June are broadly similar to mid-May. For the week ending 11 May 2021, there were 5 positive LFD tests and 100 positive PCR tests. Comparing with the week ending 22 June 2021, there were 12 positive LFD tests and 110 positive PCR tests.
The number of positive tests in care home residents at the end of June is still substantially fewer than the numbers seen in mid-January. The number of positive test results returned from PCR kits in care home staff steeply increased from 846 tests in the week ending 8 September 2020 to 9,414 in the week ending 12 January 2021. Thereafter the number of positive test results from PCR kits has overall begun to sharply decline. There were 1,047 positive test results returned from LFD kits in the week ending 12 January 2021.
Figure 8: number of positive test results returned in care homes, England
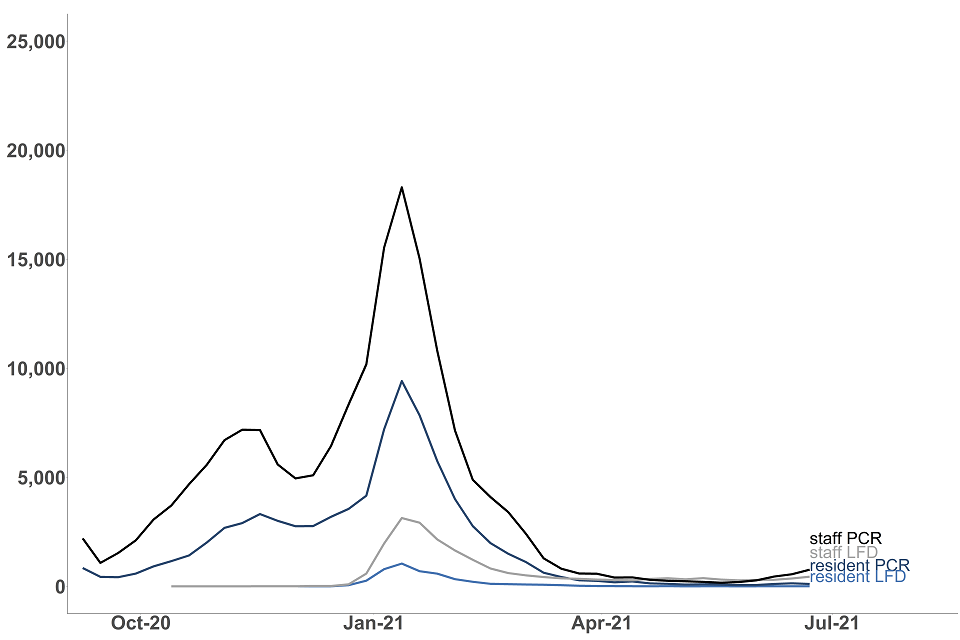
This data can be found in tables 1 and 2 of the accompanying ‘Testing’ tables in addition to data by region and local authority.
Staff and residents have different testing regimes as outlined in the About this data section. As a result, the number of positive test results returned expected to be of a different scale between staff and residents.
Visitors
There have been very few positive tests returned in visitors to residents of care homes or visiting professionals.
Terminology
Care home: facilities providing residential care. The data in this bulletin refers to Care Quality Commission (CQC) registered care homes.
Older adult care homes: care homes serving any older people (aged 65 and over) as identified from the latest Care Quality Commission (CQC) data on care homes in the ‘older people service’ user band. A small number of residents within care homes serving older people may be aged under 65.
Younger adult care homes: care homes not serving any older people (aged 65 and over) as identified from the latest CQC data on care homes in the ‘older people service’ user band.
Domiciliary care: services providing personal care for people living in their own homes. The data in this bulletin refers to domiciliary staff employed by independent CQC registered providers.
Staff: unless specified, staff can refer to staff directly employed by a provider and/or through an agency.
Staff employed by other settings: this includes non-registered providers and local authority employed: all other eligible frontline social care staff working in close and personal contact with people clinically vulnerable to COVID-19 (as defined by the Joint Committee on Vaccination and Immunisation (JCVI) priority groups) who need care and support irrespective of where they work or who they are employed by, for example, local government, NHS, private sector or third sector.
Agreed staffing ratios: the agreed number of residents for any given member of staff. This is determined by individual providers to ensure there is safe levels of staffing for care to be delivered. This can be subject to inspection by the CQC. See Regulation of staffing for more information.
PCR (polymerase chain reaction) tests: PCR tests check for the genetic material of the coronavirus in the sample, which is taken using a swab and is processed in a lab via a polymerase chain reaction (PCR). These are predominantly used in care homes for people who experience symptoms, and for routine asymptomatic testing for staff and residents.
LFD (lateral flow device): often referred to as ‘rapid tests’, these test for the presence of proteins called ‘antigens’ which are produced by the virus. They are swab tests that give results in 30 minutes or less, without the need for processing in a laboratory. These tests are primarily used in care homes for routine asymptomatic testing for staff, residents and visitors.
PPE (personal protective equipment): equipment worn by staff, visitors or essential care-givers in care homes to reduce transmission of COVID-19. This publication refers to supplies of aprons, eye protection, gloves, hand sanitiser and face masks in care homes.
About this data
These statistics are being published as a part of a wider landscape of statistics on adult social care. The Government Statistical Service (GSS) compiles a UK adult social care database of official statistics on adult social care across the 4 nations of the UK. This is updated on a monthly basis.
The UK Statistics Authority (UKSA) conducted a review of adult social care statistics in England which called for:
-
better leadership and collaboration across different organisations publishing official statistics. This publication has been produced in collaboration with other statistics providers of COVID-19 adult social care data and DHSC will endeavour to work with various stakeholders as more data is published through this publication
-
addressing of gaps in available data, particularly in privately funded care. This bulletin aims to plug some of that gap by including data on residents privately funding their care in addition to those funded by local authorities
-
improving existing official statistics. These statistics are being badged as experimental statistics and more data will be added iteratively based on user needs
Other sources of adult social care COVID-19 data
COVID-19 vaccination
NHS England and Improvement (NHSEI) also publish data on vaccinations in adult social care settings as part of their broader statistical release on COVID-19 vaccination, using the same methodology and the same data source as this publication but there are differences in the:
-
reporting period; data in this publication reports data collected up to 11:59pm on a Tuesday whereas NHSEI use data collected up to 11:59pm on a Sunday
-
a small amount of data may be collected after the respective reporting periods
-
regional breakdowns; data in this publication uses the administrative regions of England and NHSEI use NHS regions
COVID-19 testing
DHSC also publishes care home testing data in the weekly NHS Test and Trace statistics (England) at national level. This publication uses the same data source but has a different methodology for presenting testing in care homes and differences in the figures will occur due to the following reasons:
-
differences in which tests from different routes are included. Both methodologies include the number of tests registered from kits sent directly to care homes, but this publication additionally includes care home staff or residents tested via other routes such as regional or local test sites. As a result, figures in this report will be substantially higher for PCR tests conducted in care home staff due to the current guidance recommending staff with symptoms to be tested outside of the care home (see coronavirus (COVID-19) testing in adult care homes for more information)
-
different reporting periods. This publication uses the start time of the test in comparison to the Test and Trace statistics which use the date on which the test result was received by the individual taking the test
-
different times of extracting the data
For more details on the NHS Test and Trace programme and the statistics please see the NHS Test and Trace methodology document.
Data sources
COVID-19 vaccination, infection prevention control (IPC), PPE availability and staffing levels
Data in this publication is taken from self-reported data submitted by care providers in England through a data collection and insight tool called Capacity Tracker.
Care providers are expected to submit data on IPC compliance on a weekly basis whilst data on vaccinations, PPE availability and staffing levels is expected to be updated on a daily basis.
Infection control data for each reporting week refers to data up to 2pm on the date stated as the ‘week ending’ and the 7 days prior. For PPE and staffing-levels data relates up to 11:59pm on the date stated as the ‘week ending’. The reporting week usually ends on a Tuesday but occasionally no data is available for this date, in these situations the ‘week ending’ date will be the nearest available date.
This bulletin presents the proportion of staff and residents vaccinated out of the total number of staff and residents as self-reported by care providers. Only individuals who have not tested positive for COVID-19 in the last 28 days are eligible to receive the vaccine. Data on the number of staff and residents of older adult care homes eligible for the vaccination over time can be found in the accompanying COVID-19 vaccination tables.
For more information, please see the ‘Data Sources’ section of the accompanying methodology note.
COVID-19 testing data
Testing data is collected from management information generated during the operation of the NHS Test and Trace service.
For more information, please see the ‘Data Sources’ section of the accompanying Background quality and methodology note.
Data coverage and quality
All data in this publication refers to adult social care settings in England only.
Data submitted by providers reflects the current priorities to monitor the COVID-19 pandemic in social care settings. Data collection could be subject to change based on changes to the priorities and therefore the reporting in this publication will be adapted accordingly.
IPC, PPE availability and staffing levels
Providers are expected to submit data on IPC measures on a weekly basis while staffing levels and PPE availability data are expected to be submitted on a daily basis. Any providers who have not submitted data within the last 7 days are excluded from the relevant analysis for the associated time period where no response was received. The full response rates for all data points are available in the accompanying tables.
COVID-19 vaccinations
Data on total number of staff and residents as well as those vaccinated is self-reported by care providers and local authorities (LAs). Providers are expected to update their vaccination data on a daily basis. There may be a time lag between individuals receiving the vaccine and the week they are reported in the statistics depending on when providers have updated their vaccination data.
COVID-19 testing
This report includes the number of tests conducted on care homes residents, staff and visitors who were tested by:
-
PCR and LFD kits sent directly to the care home for regular testing, which were registered through the National Testing Programme digital infrastructure
-
PCR and LFD kits conducted at another testing site such as a regional or local test site or a mobile testing unit or tests that were registered
The figures in this report are only deduplicated to report on the number of individual tests taken, not the number of people tested. Because people can have more than one test, the data should not be compared with prevalence rates or case positivity rates.
This report does not contain data on those tested through pillar 1.
Data for each reporting period relates to the day an individual took their test.
The rollout of the testing program in care homes is summarised in the table 3 below:
Table 3: testing guidance in care homes
| Dates | Frequency | Test Kit | |
|---|---|---|---|
| Care home residents | 7 June 2020 to present | Monthly In the event of an outbreak: day 1 and between days 4 to 7 |
PCR |
| Care home residents | 22 February 2021 to present | In the event of an outbreak: day 1 and between days 4 to 7 at health protection team discretion | LFD |
| Care home staff | 7 June 2020 to present | Weekly In the event of an outbreak: day 1 and between days 4 to 7 |
PCR |
| Care home staff | 23 December 2020 to present | Twice a week In the event of a positive case: daily until 5 days without a positive | LFD |
| Care home indoor visitors | 8 March 2021 to present | Weekly – essential care givers | PCR |
| Care home indoor visitors | 8 March 2021 to present | Twice weekly – essential care givers | LFD |
| Care home indoor visitors | 2 December 2020 to present* | On visit | LFD |
| Care home visiting professionals – CQC inspectors | 14 December 2020 to present | Weekly | PCR |
| Care home visiting professionals – CQC inspectors | 22 December 2020 to present | Before visit | LFD |
| Care home visiting professionals – all other professionals | 14 December 2020 to present | On arrival, unless part of a regular testing regime and can provide proof of a negative result within 72 hours | LFD |
*Close contact visits with LFD testing began on 2 December 2020 but ceased on 6 January 2021 because of the national lockdown. Throughout the period of national restrictions, visits were limited to outdoors, in visiting pods, or with a substantial screen; as well as those in exceptional circumstances such as end of life.
The figures in this report are only de-duplicated to report on the number of individual tests taken, not the number of people tested. Because people can have more than one test, the data should not be compared with prevalence rates or case positivity rates.
Revisions
Any revisions to past publications will be in line with DHSC’s revision policy and highlighted in future publications accordingly.
Future developments
We plan to add new statistics to this publication to support user needs. Over the coming months, we will explore the feasibility of publishing the following statistics:
- staffing levels and PPE testing in domiciliary care settings
- other non-COVID-19 related adult social care data
Feedback
For feedback and any further questions, please contact asc.statistics@dhsc.gov.uk.
-
Due to the change in guidance issued on 23 December 2020 to increase testing in care home staff, the requirement for care home staff to register negative LFD test results was suspended between 31 December 2020 and 15 January 2021 inclusive. As a result, a proportion of LFD tests conducted on care home staff will not be included for these dates. ↩
