Workplace health: applying All Our Health
Updated 10 March 2022
The Public Health England team leading this policy transitioned into the Office for Health Improvement and Disparities (OHID) on 1 October 2021.
Introduction
This guide is part of All Our Health, a resource which helps health professionals prevent ill health and promote health and wellbeing as part of their everyday practice. The information will help front-line health and care staff use their trusted relationships with patients, families and communities to promote the benefits of achieving and maintaining a healthy weight.
We also recommend important actions that managers and staff holding strategic roles can take.
Access the workplace health e-learning session
An interactive e-learning version of this topic is now available to use. OHID and Health Education England’s ‘e-Learning for Healthcare’ have developed this content to increase the confidence and skills of health and care professionals, to embed prevention in their day-to-day practice.
Why you should promote workplace health in your professional practice
Employment is an important factor for health, directly and indirectly making an impact on the individual, their families and communities.[footnote 1] Unemployment is associated with an increased risk of mortality and morbidity, including limiting illness, cardiovascular disease, poor mental health, suicide and health-damaging behaviours.[footnote 2] Individuals unemployed for more than 6 months have lower wellbeing than those unemployed for less time.[footnote 3] Health-related worklessness can be defined as individuals not in employment for a health reason.[footnote 4]
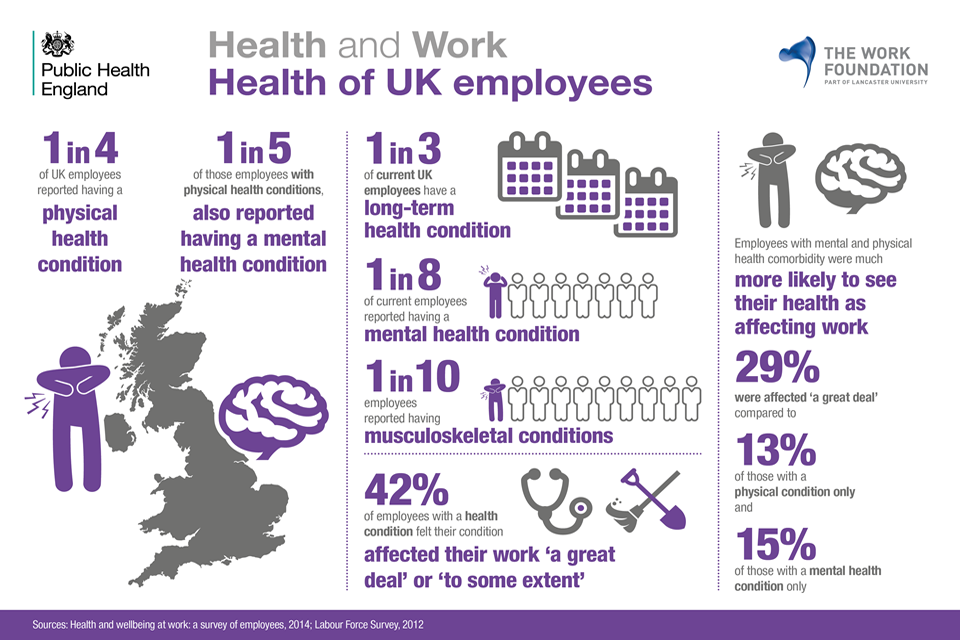
Health of UK
There are substantial variations in employment rates across groups and health conditions. In particular, people with histories of substance misuse and those affected by mental ill health often face barriers in securing employment.[footnote 5]
Workplace health is promoting and managing the health and wellbeing of staff and includes managing sickness absence and presenteeism (a person physically at work, but unproductive). Workplace health interventions include activities undertaken within the workplace by an employer or others to address these issues, and action to address health and safety risks.[footnote 6]
Labour market statistics show that 75.5%[footnote 7] of adults are in employment, on average spending a third of their waking hours in the workplace. Evidence shows that good work is good for health and that a bad working environment, characterised by low levels of job control and organisational fairness, and a high effort-reward imbalance, may contribute to poor health.
Facts about workplace health
Working for a healthier tomorrow found that the annual economic costs of sickness absence and worklessness is estimated to be over £100 billion.[footnote 8]
Health and Safety Executive statistics show:
- annual cost to society due to workplace injuries and ill health (excluding cancer) was £15 billion from 2016 to 2017
Office for National Statistics[footnote 11] reported that in 2017:
- 131 million days[footnote 3] were lost to sickness absence
- minor illnesses (such as coughs and colds) were the most common reason for sickness absence, accounting for approximately 34.3 million days lost (26.1% of the total days lost)
- musculoskeletal conditions (including back pain, neck and upper limb problems) cause 28.2 million days lost (21% of sickness absences)
- mental health issues (including stress, depression, anxiety and serious conditions) resulted in 15 million days lost (11.54% of sickness absences)
- lower sickness absence rates in the private sector (1.7%) but the gap with the public sector (2.6%) has narrowed over past 20 years
- of the larger public sector organisations, sickness rates are highest for those working in the health sector
- self-employed people are less likely than employees to have a spell of sickness
- the largest workforces report highest sickness levels
- sickness absence is lowest for managers, directors and senior officials
The 2019 Healthcare Professionals’ Consensus Statement on Health and Work
The 2019 Healthcare Professionals’ Consensus Statement on Health and Work (PDF, 520KB) (agreed by the Academy of Medical Royal Colleges, the Royal College of Nursing and the Allied Health Professions Federation) marks the collective commitment of health and care professionals to the Health and Work agenda.
It outlines 4 principles for all health and care professionals as follows.
We will work together, as individual organisations and collaboratively, to enable every health and care professional to:
- Understand the health benefits of good work, and the long term effects of avoidable health related worklessness
- Have the skill to incorporate discussions about working in the context of a health outcome with patients in their care, as appropriate to the health or disability of that individual
- Feel supported to understand and interact with the wider health and work system employers, occupational health services and other bodies that have a role in assisting individuals who are not working for health-related reasons
- Recognise their own role to support healthy and safe working environments, looking after their own health and wellbeing and those of their colleagues.
Core principles for healthcare professionals
Frontline health and care professionals
Health and care professionals can have an impact on an individual level by:
- supporting the co-location of employment services and individual placement support in healthcare settings
- promoting work as a health outcome
- issuing ‘fit notes’ which help people on long term sick leave back into work by changing perceptions of work capability
- using the ‘health first’ approach, emphasising management of health conditions of people on health-related welfare benefits before addressing employability
- promoting active workforces and active workplaces
- making it easy for people to stay active and connected to people around them
- undertake and encourage colleagues to complete HEE’s Work and Health eLearning suite[footnote 10]
- GPs should consider engaging with OHID GP health and work champions in regions where these exist, (currently London, East Midlands and North East)
- occupational therapists should consider becoming a RCOT Health and Work Champion and deliver a standardised training package to their colleagues, (see more information on the scheme below)
Royal College of Occupational Therapist (RCOT) Health and Work Champions
RCOT Health and Work Champions deliver training in their NHS organisations to enable colleagues to routinely ask about employment and provide brief advice when delivering care to working age adults.
Advantages of becoming a Health and Work Champion
The advantages of becoming a Health and Work Champion are:
- a chance to take a key leadership role in health and work
- the prospect of leading culture change in healthcare
- an opportunity for you to share your expertise
- the option to develop your career and continuing professional development
- the chance to be part of a fast growing wave of change
As a Health and Work Champion, you will deliver free training to colleagues in your employing organisation and beyond. This is a standard package that lasts for an hour.
Team leaders and managers
Community health professionals and providers of specialist services can have an impact by:
- supporting local authority (LA) and national employment programmes
- promoting training of line managers in business, starting with LA staff
- working in partnership with LA public health teams to ensure that activity on workplace health is reaching the maximum amount of businesses
- encouraging people to stay active, connected, eat well and reduce alcohol consumption
- using national data profiles or tools to understand the health needs of the local community
- using the OHID wider determinants tool to understand the impact the wider determinants have on the health needs of the local community
- encourage colleagues to complete HEE’s Work and Health eLearning[footnote 10]
- allow your staff to become a RCOT Health and Work Champion
Senior and strategic leaders
Healthcare professionals working within commissioning, management or policy and partnership roles should be aware of the interventions that may be available to promote health through the workplace at population level, which include:
- promoting work as a health outcome
- embedding the ‘health first’ approach emphasising management of health conditions of people on health-related welfare benefits before addressing employability in all programmes and initiatives
- being aware of the potential for the workplace to be a source of ill-health, such as through accidents, stress, exposure to potential harms
- senior buy-in for the RCOT Health and Work Champion pilot, by allowing staff to deliver this training during the working hours
- promoting health interventions to workplaces of all types within their area, enabling individual health behaviours to be addressed at scale (including groups not easily reached through traditional services)
- promoting comprehensive methods of managing health within an integrated workplace programme which combines occupation health and HR: for example an evidence-based local accreditation scheme or OHID Employer toolkits
- leading by example by recommending and encouraging each NHS organisation to promote health internally
- encouraging local health risk reduction and promotion programmes (such as NHS Health Checks, One You campaign, NHS Stop Smoking Services) to partner with employers within or linked to workplaces
- encouraging people to stay active, connected, eat well and reduce alcohol consumption
- promoting and increasing awareness of national programmes, guidance and legislation on employment to those with disabilities, long term or fluctuating health conditions
- as commissioners, ensuring that promotion of workplace health and the use of workplaces as a delivery setting is prominent within commissioned healthcare services
- encouraging Health and Wellbeing Boards to include workplace health in their Joint Strategic Needs Assessment (JSNA) and commissioning of services to address the needs of the population
- ensuring that staff are involved in the development and leadership of any population level interventions on health in workplace settings
- integrating multidisciplinary occupational health advice in care pathways
Understanding local needs
Public Health Outcomes Framework (PHOF)
There are 7 PHOF indicators that relate to employment:
- 1.05: 16 to 17 year olds not in education, employment or training (NEET) or whose activity is not known
- 1.08i: Gap in the employment rate between those with a long-term health condition and the overall employment rate
- 1.08ii: Gap in the employment rate between those with a learning disability and the overall employment rate
- 1.08iii: Gap in the employment rate for those in contact with secondary mental health services and the overall employment rate
- 1.08iv: Percentage of people aged 16 to 64 in employment
- 1.09i: Sickness absence – the percentage of employees who had at least one day off in the previous week
- 1.09ii: Sickness absence – the percentage of working days lost due to sickness absence
Commissioning for Quality and Innovation (CQUIN)
The 2017 to 2019 CQUIN outlined where NHS England would like to improve the health of their staff. The goal is to improve the support available to NHS staff to help promote their health and wellbeing in order for them to remain healthy and well.
The 5 percentage point improvement should be achieved over a period of 2 years, with the baseline survey being the 2016 staff survey.
Measuring impact
As a health and care professional, there are a range of reasons why it makes sense to measure your impact and demonstrate the value of your contribution. This could be about sharing what has worked well in order to benefit your colleagues and local people or help you with your professional development.
Further reading, resources and good practice
Health Education England
Work and Health e-learning programme
This e-learning course[footnote 10] is about the crucial relationship between work and health. It aims to improve healthcare practitioners’ confidence to support patients with long term or chronic health conditions, via brief conversations in routine consultations.
The resource focuses on the relationship between health professionals and patients and is made up of 8 sessions including:
- Introductory course to work and health
- Self-care for Healthcare Professionals
- Young people
- Working age adults
- Older people
- Mental health
- MSK
NICE guidelines
Promoting mental wellbeing at work (PH22) is guidance for those who have a direct or indirect role in, and responsibility for, promoting mental wellbeing at work.
Managing long term sickness and incapacity for work (PH19) is guidance for all those who manage long term (or recurring short or long term) sickness absence and incapacity, including employers and people working in the NHS.
Workplace interventions to promote smoking cessation (PH5) is guidance for all those involved in providing employees with help to stop smoking.
Promoting physical activity in the workplace (PH13) is guidance for employers and professionals in small, medium and large organisations, especially those working in human resources or occupational health.
Workplace health: policy and management practices (NG13) covers how to improve the health and wellbeing of employees, with a focus on organisational culture and the role of line managers.
Health and Safety Executive
Health and Safety Executive guidance
Public Health England
Movement into employment: return on investment tool is guidance to help local commissioners estimate the benefits of moving an individual from worklessness into employment.
Health and work: infographics are designed to help raise awareness and understanding of the relationship between health and work.
Work, worklessness and health: local infographic tool includes a slide set with regional and local level data relating to work, worklessness and health for each county or unitary authority in England.
Public Health England (PHE) and Business in the Community employer toolkits
PHE and Business in the Community developed a series of toolkits providing guidance to employers on:
- mental health
- sleep and recovery
- drugs
- alcohol and tobacco
- physical activity, healthy eating and healthy weight
- domestic violence
- musculoskeletal health
Good practice example
Talking Work, a guide for doctors discussing work and work modifications with patients. (PDF, 461KB)
-
JM.McGinnis, P.Williams-Russo, JR. Knickman, The case for more active policy attention to health promotion. Health Affairs. 2002;21(2):78 to 93. ↩
-
M.Marmot, J.Allen J, P.Goldblatt , T.Boyce, D.McNeish, M.Grady, and others. Fair society, healthy lives: strategic review of health inequalities in England post 2010. London: The Marmot Review; 2010. ↩
-
J. Chanfreau, C.Lloyd, C. Byron, C.Roberts, R.Craig, D.De Feo, S. McManus. Predictors of wellbeing (PDF, 1.02MB) ↩ ↩2
-
Health, work and health related worklessness: A guide for local authorities. (PDF, 471KB) ↩
-
L.Bauld, G.Hay, J.McKell and C.Carroll Problem drug users’ experiences of employment and the benefit system (PDF, 441KB) Royal College of Psychiatrists Mental Health and Work (PDF, 1.36MB) ↩
-
Health, work and health related worklessness: A guide for local authorities (PDF, 471KB) ↩
-
2018 July to September: Employment rate (age 16 to 64 seasonally adjusted. ↩
-
Dame Carol Black’s Review of the health of Britain’s working age population - Working for a healthier tomorrow (PDF, 3MB) ↩
-
E- Learning for Health, Health Education England, Public Health England, Department for Health and Social Care and Department for Work and Pensions - Work and Health Programme. ↩ ↩2 ↩3
