[Withdrawn] Using the world leading NHS Health Check programme to prevent CVD
Published 24 January 2018
Summary
This edition of Health Matters explores how the NHS Health Check is playing an important role in the prevention and early detection of cardiovascular disease (CVD) in England. We will also examine options for increasing the coverage and uptake of evidenced based interventions following the NHS Health check to ensure that we are optimising the benefits of this world-leading prevention programme.
Scale of the problem
CVD is a family of diseases often caused by atherosclerosis – the furring or stiffening of artery walls. Atherosclerosis particularly results in coronary heart disease, stroke and peripheral arterial disease. CVD also covers other conditions such as vascular dementia, chronic kidney disease, cardiac arrhythmias, type 2 diabetes, sudden cardiac death and heart failure.
CVD morbidity and mortality and health inequalities
According to the WHO, CVD is the number 1 cause of death globally, with an estimated 17.7 million people having died from CVD conditions in 2015, representing 31% of all global deaths.
However, it is estimated that 50 to 80% of cases of CVD are caused by modifiable risk factors, such as smoking, obesity, high blood pressure, high cholesterol, excessive alcohol consumption and physical inactivity, so therefore could be prevented from occurring. In England, the NHS Health Check provides a cornerstone for the prevention of 7 of the top 8 risk factors for early death and disability identified in the Global Burden of Disease (GBD) study.
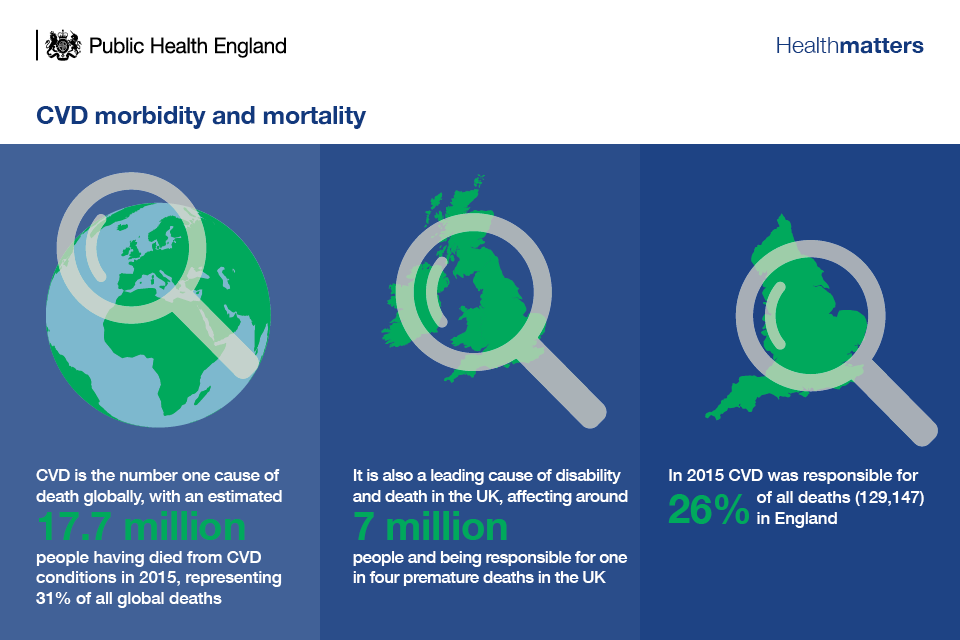
Infographic of CVD morbidity and mortality
CVD is one of the conditions most strongly associated with health inequalities. Risk factors such as smoking, physical inactivity and obesity are greater in lower socio-economic groups and the burden of morbidity and mortality is disproportionately shouldered by the most deprived.
Premature death rates from CVD in the most deprived 10% of the population are almost twice as high as rates in the least deprived 10%.
Risk factors of CVD
Whilst age, gender, family history and ethnicity are non-modifiable risk factors of CVD, these conditions often share common physiological and behavioural risk factors that can be modified.
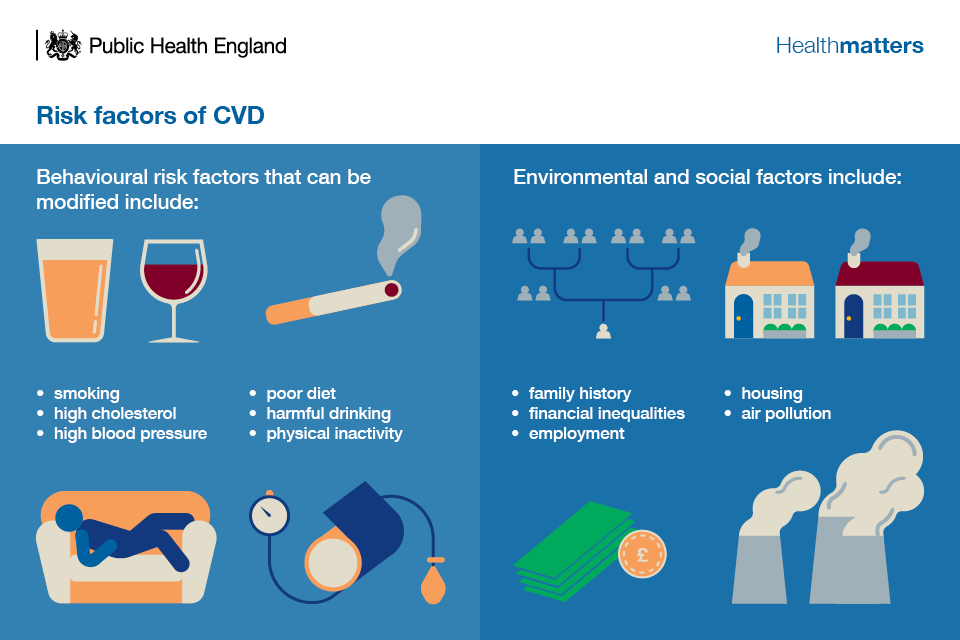
Infographic showing risk factors for CVD
We also know there are wider factors such as having a mental health diagnosis or being diagnosed with diabetes that can increase the risk of CVD.
The diagnosis and treatment gap
CVD and the burden it has on individuals, communities and the NHS are highly preventable through support for individual behaviour change, population measures such as tobacco control and salt and sugar reduction, and individual level interventions such as clinical management of high risk conditions such as high blood pressure, atrial fibrillation (AF) and high cholesterol.
However, in England, CVD prevention is being limited by the diagnosis and treatment gap for major CVD risk conditions including high blood pressure and AF, which cause heart attack and stroke (CVD events).
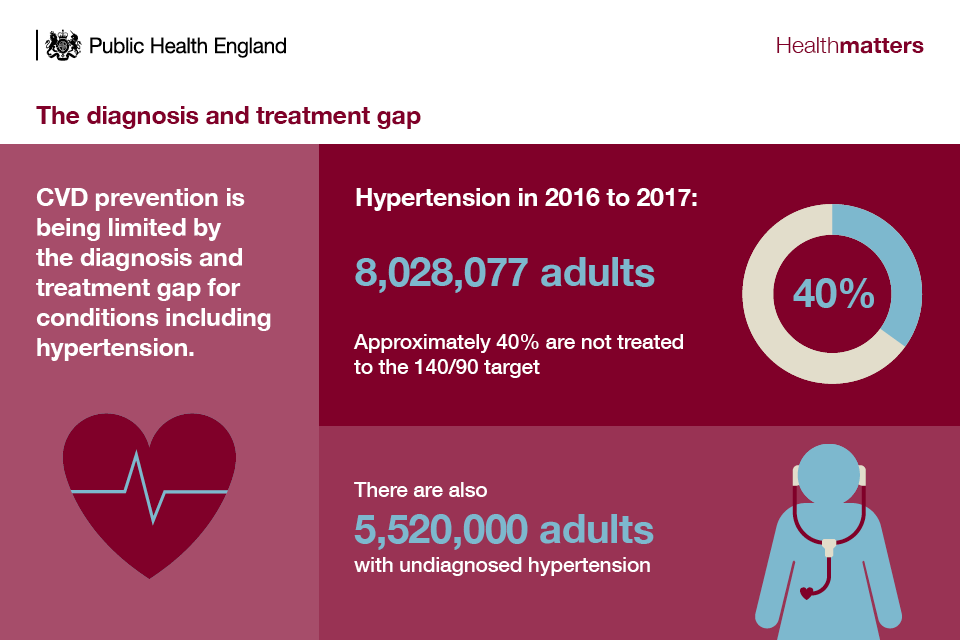
Infographic describing the CVD diagnosis and treatment gap
Atrial fibrillation in 2016 to 2017:
- GP registered population with AF: 1,065,569
- estimated GP registered population with undiagnosed AF: 340,000
- GP registered high risk AF patients not anticoagulated: 165,355
The diagnosis and treatment gap is also an issue for other CVD risk conditions such as non-diabetic hyperglycaemia (NDH, ‘pre-diabetes’), type 1 and 2 diabetes, high CVD risk and familial hypercholesterolaemia, and chronic kidney disease:
- 5 million people with NDH are undiagnosed and most do not receive intervention
- 940,000 people with type 1 and 2 diabetes are undiagnosed
- of those diagnosed with diabetes half do not receive all 8 care processes (46% of people with type 2, 63% of people with type 1)
- 3,960,000 people aged 30 to 85 years have a 10 year CVD risk over 20% and an estimated 49% are treated with statins
- 85% of familial hypercholesterolaemia cases are undiagnosed
- 1.1 million people with chronic kidney disease are undiagnosed and many have poor blood pressure and proteinuria control
In the high risk conditions such as hypertension and AF, preventive treatment is very effective, with evidence showing that:
- reducing blood pressure in all adults with diagnosed and undiagnosed hypertension by 5 mmHg reduces risk of heart attack, stroke and premature death by 10%
- statin therapy to reduce cholesterol by 1 mmol in people with a 10 year risk of CVD risk greater than 10% reduces risk of CVD events by 20 to 24%
- anti-coagulation of high risk AF patients averts one stroke in every 25 treated
Therefore, addressing the diagnosis and treatment gap of these high risk conditions is crucial for reducing the occurrence of CVD.
Why invest in prevention of CVD?
As well as being a life-changing problem for individuals and families, CVD places a considerable strain on the NHS and wider society. It accounts for an estimated £8.96 billion a year in NHS healthcare costs alone. Costs of informal care and productivity losses due to CVD came to £10.39 billion in 2015, excluding the direct costs incurred by social care.
With tighter budgets across the NHS and local government, it is imperative that investment goes towards the most cost-effective interventions for CVD prevention. Being able to calculate the return on investment (ROI) is important for this, as it will allow decision makers to make the best options for improving and protecting health.
Through optimising treatment in AF and hypertension, the potential CVD events averted and savings over 3 years were calculated by PHE and NHS England. Optimal anti-hypertensive treatment of diagnosed hypertensives averts within 3 years:
- 9,710 heart attacks, saving up to £72.5 million
- 14,500 strokes, saving up to £201.7 million
Furthermore, optimally treating high risk AF patents averts 14,220 strokes within 3 years, saving up to £241.6 million.
Although some useful resources already exist, there are still gaps in the economic evidence for prevention and the pressure on public sector spend fosters the need to regularly review costs and the use of funds. PHE is developing an overarching ROI tool and accompanying report for CVD prevention which will be available for use locally later this year. This will have the effect of moving away from individual risk condition modelling and aspiring towards modelling the cumulative effect of holistic action on CVD.
Sustainability Transformation Partnerships (STPs) and Accountable Care Systems (ACSs) offer a real opportunity for broad place-based partnerships to drive improvement in the prevention, detection and management of CVD. This opportunity is highlighted in the STP aide-mémoires on prevention and primary care.
NHS Health Check
By promoting healthy ageing and tackling the top 7 risk factors for early death and disability, the NHS Health Check provides a cornerstone for the prevention of other diseases that share common risk factors such as dementia, respiratory disease and some types of cancer, extending its benefits across the health and social care system.
This edition of Health Matters focuses specifically on the role of the NHS Health Check in relation to preventing and treating CVD.
The programme is world-leading and is arguably one of the largest prevention programmes of its type in the world, with almost 1.5 million people having the NHS Health Check every year.
Underpinned by NICE evidence-based recommendations, it continues to provide a significant opportunity to reduce early death, disability and health inequalities. A recent Expert Scientific and Clinical Advisory Panel (ESCAP) report outlines the evidence for the NHS Health Check programme.
As well as helping individuals to recognise and tackle their behavioural risk factors, it also provides a systematic approach to identifying people with previously undiagnosed high risk conditions.

Infographic describing the NHS Health Check
Although the greatest burden of death and disability from CVD occurs among people over the age of 50, we have known for some time that CVD is not an inevitable part of the ageing process.
Up to 80% of events could be avoided through better prevention of risk factors. The NHS Health Check offers an opportunity for people in midlife to assess their risk of CVD and make lifestyle changes that can prevent and delay the onset of CVD.
Uptake of NHS Health Checks
Between April 2013 and March 2018, 15,503,796 people in England were eligible for a NHS Health Check.
Since April 2013, more than 12.7 million people have been offered a NHS Health Check, which means that in the past 4 and a half years, 82.5 % of the expected eligible population (from 2013 to 2018) have been offered a check.
Over the same period, 6.1 million people have received a check.
Take up of the NHS Health Check has remained stable since 2013 with the national rate currently at 48.4%.
This means that just over half of all people invited for the NHS Health Check do not take up the offer, and there is huge variation in uptake across the country.
PHE’s latest NHS Health Check stocktake and action plan published in January 2018 has more details on how PHE is working with partners to support improvement in the programme over the coming 5 years.
Use PHE’s fingertips data to see uptake figures for your local area.
Who is having a NHS Health Check
Two large-scale national evaluations of the programme have shown that there is not a social gradient in the coverage of this prevention programme. This is hugely important as most universal healthcare interventions are commonly assessed by our more affluent communities. This shows that the programme is achieving its objective of tackling health inequalities and addresses early concerns that the NHS Health Check would be a programme for the ‘worried well’.
However, we know that more could be done to ensure that we improve coverage to younger populations and see more men taking up the offer of the NHS Health Check.
An evidence synthesis which looked at 68 papers, undertaken by members of the Primary Care Unit, University of Cambridge and supported by RAND Europe found that coverage is consistently higher among:
- older people
- individuals from the poorest communities
- people with a family history of coronary heart disease
Additionally, the national studies also show greater coverage among Bangladeshi, Caribbean and Indian ethnic groups than among white individuals and lower coverage among Chinese groups.
This demonstrates that NHS Health Checks are reaching people with the greatest risk of CVD.
All eligible people should be offered an NHS Health Check every 5 years but local teams should be targeting their resources towards those who are high risk and those from disadvantaged communities, who will most benefit from the check and subsequent risk reduction interventions. This is a concept known as proportionate universalism. Proportionate universalism aims to improve the health of the whole population, across the social gradient, while simultaneously improving the health of the most disadvantaged fastest.
How to increase uptake of NHS Health Check
In order to increase uptake it is important to understand the reasons why some people do not take up the offer of an NHS Health Check. The findings from the evidence synthesis highlight 6 major reasons:
- lack of awareness or knowledge: they do not know what it is, whether it is free or its relevance
- competing priorities: not having the time to go
- misunderstanding the purpose: a lack of recognition that the programme is preventative combined with the view that they do not want to burden the NHS when they feel healthy and well
- aversion to preventative medicine: some people are not interested, actively do not want to know or are afraid they might receive bad health news; others do not want to be told off or given lifestyle advice
- convenience: not being able to get an appointment at a time or on a day that suits them at their GP practice, particularly among people working office hours
- quality: concerns regarding the competence, privacy and confidentiality of checks that are delivered in pharmacies
These findings highlight the need for further action to address the lack of awareness and knowledge about the programme as well as addressing underlying aversion to preventative medicine. Improving convenience of access and reassuring people of the high quality of checks delivered by pharmacists may also help dispel the fears that stop people from attending.
PHE has published guidance on ways to increase the uptake of the NHS Health Check, which includes advice on:
- using the template invitation letter
- text message primers and reminders
- computer prompts to clinical staff
- behaviourally informed messaging
- targeted telephone outreach
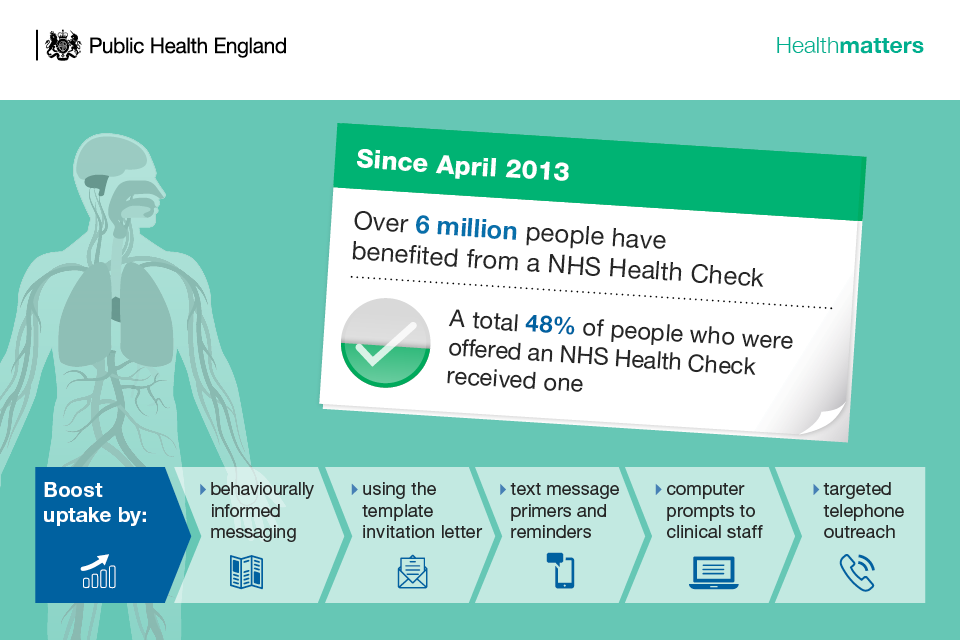
Infographic showing over 6 million people have had an NHS Health Check
NHS Health Check Outcomes
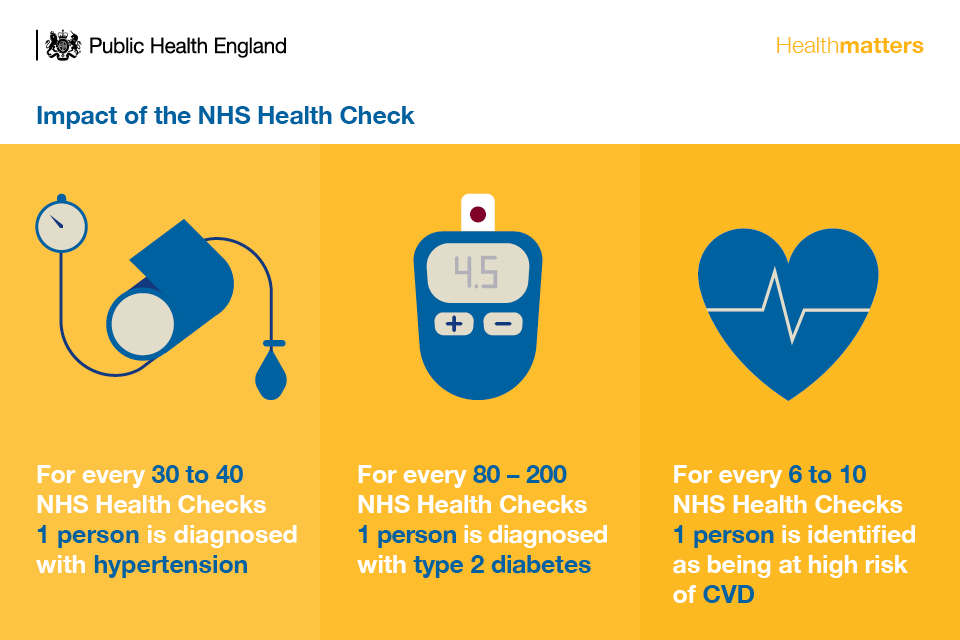
Infographic describing the impact of the NHS Health Check
National evaluations show that treating blood pressure and cholesterol alone could prevent somewhere between 251 and 505 major CVD events each year. With improvements to clinical management this could be even greater.
Research using national data and comparing NHS Health Check attendees with matched non-attendees, reports favourable changes among people having a check on:
- blood pressure
- body mass index
- modelled CVD risk
Referrals for lifestyle management
Everyone having an NHS Health Check should benefit from tailored lifestyle advice and access to local services, such as:
- stop smoking services
- weight management services
- physical activity services
- alcohol reduction services
- national diabetes prevention programme
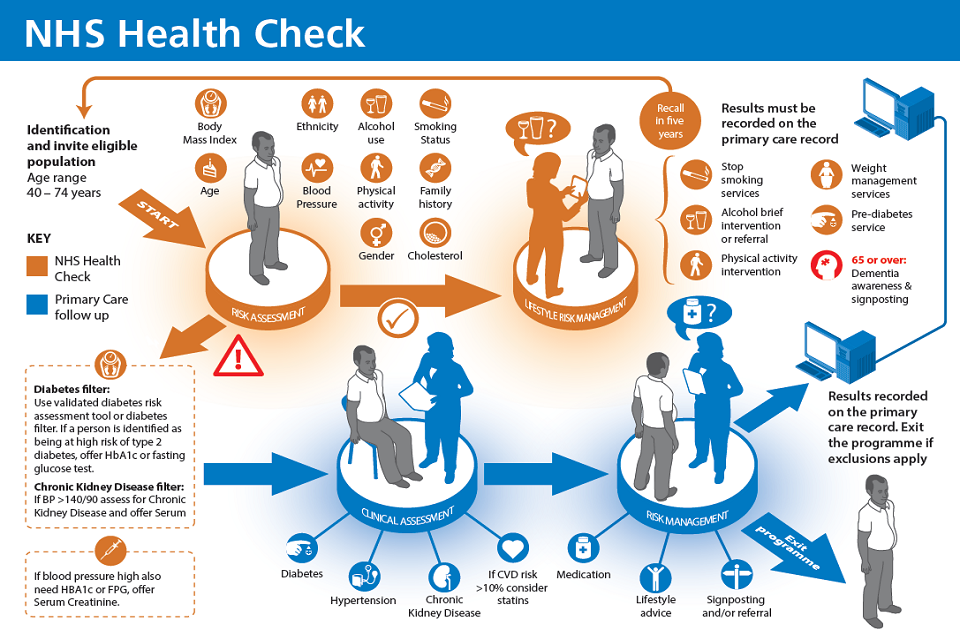
Infographic showing the NHS Health Check process flow
[Research published in the BMJ] has shown that people who attend an NHS Health Check are more likely to be referred to lifestyle management services than those who do not attend.

Infographic illustrating referrals for lifestyle management
PHE’s One You campaign, aimed at people aged 40 to 60, can help to motivate people to take steps to improve their health, through action on the main risk factors such as smoking, inactivity, obesity, alcohol consumption.
Prescribing after the NHS Health Check
Statins and antihypertensives should be prescribed to patients in line with NICE guidance, and general practice should be incentivised to prescribe them in addition to lifestyle advice where appropriate.
However, only 1 in 5 NHS Health Check attendees at high risk of CVD have been prescribed a statin and only 1 in 12 NHS Health Check attendees at high risk of CVD have been prescribed an antihypertensive.
Although prescribing rates are higher than those who attend for a NHS Health Check, overall prescribing rates vary, and improving this provides an opportunity to increase the effectiveness of the programme significantly.
PHE has collaborated with NHS England and others to develop the NHS RightCare CVD prevention pathway which should be used to optimise clinical management of CVD and improve prescribing rates of statins and antihypertensives.
The Size of the Prize resource presents opportunities for each STP to work differently to prevent many thousands of heart attacks and strokes, through evidence-based treatments for conditions such as high blood pressure, atrial fibrillation and high cholesterol.
Call to action
The Next Steps on the NHS Five Year Forward View outlines PHE’s ambition to reach over 2.8 million more people with an NHS Health Check.
This will identify around 280,000 people at high risk of CVD and facilitate follow up, preventative care for 70,000 patients with high blood pressure, 14,000 patients with type 2 diabetes and over 4,600 patients with chronic kidney disease who will be diagnosed earlier and treated by the NHS. For this to happen, everyone needs to play their part.
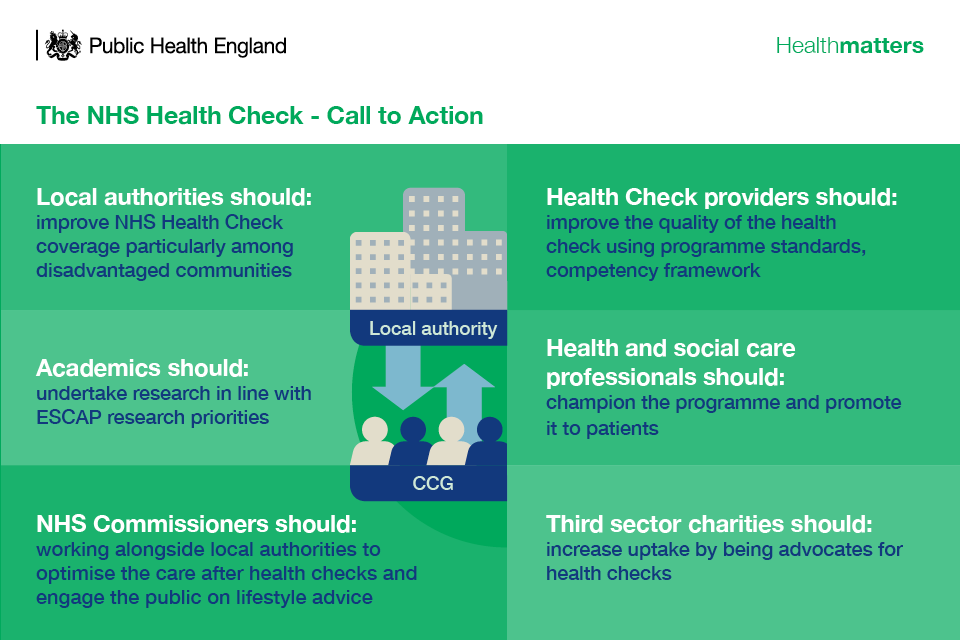
Infographic describing the call to action
Local authorities
Local authorities can increase the uptake of NHS Health Checks by expanding the range of providers beyond general practice to include other settings such as pharmacies, major retailers and the voluntary sector. This helps provide a flexible programme that meets the needs of their local communities and improves access for hard to reach groups.
NHS Commissioners
NHS commissioners should work alongside local authorities to increase uptake and identify those who could benefit from a NHS Health Check. Use PHE’s fingertips guidance to measure local uptake.
Commissioners have a key role to play in optimising the care following a NHS Health Check and ensuring that patients are offered lifestyle advice and, if necessary, medication such as statins.
NHS Health Check providers
Providers should maintain and improve the quality of the NHS Health Check using programme standards and the competency framework.
Health and social care professionals
Health and social care professionals should be champions of the programme and actively promote it to eligible members of the public.
Staff should be encouraged to take up the offer.
Third sector charities
The third sector has an important role in being an advocate of NHS Health Checks and can help to increase uptake and awareness among high risk groups.
Academics
Academics should continue to undertake research in line with ESCAP research priorities for the programme.
