Enteric fever (typhoid and paratyphoid) England, Wales and Northern Ireland: 2020
Updated 22 August 2024
Applies to England, Northern Ireland and Wales
Enteric fever (also known as typhoid and paratyphoid) is an illness caused by the bacteria Salmonella enterica subspecies enterica serovar Typhi (typhoid) or serovars Paratyphi A, B or C (paratyphoid). Typhoid fever is a serious disease and can be life-threatening unless treated promptly with antibiotics. The disease may last several weeks and convalescence takes some time. In the literature, paratyphoid is considered to be typically milder than typhoid and of shorter duration (1, 2).
The bacteria that cause typhoid and paratyphoid only occur in humans. Humans acquire infection through eating food or drinking water that has been contaminated with infected faeces or through direct faecal-oral transmission. Transmission occurs following the ingestion of food or water that has been heavily contaminated (10 or more organisms may be required to cause illness) by the bacterium S. Typhi or S. Paratyphi. In the UK, most cases of typhoid and paratyphoid are acquired abroad in countries and regions of the world where hygiene or sanitation is poor.
This report summarises the epidemiology of laboratory-confirmed cases of S. Typhi and S. Paratyphi reported in England, Wales and Northern Ireland (EWNI) in 2020. It includes both reference laboratory and enhanced enteric fever surveillance data.
Data sources
Confirmed symptomatic cases of S. Typhi and S. Paratyphi in England, Wales and Northern Ireland are diagnosed by the UK Health Security Agency (UKHSA) Salmonella Reference Service (SRS), within the Gastrointestinal Bacteria Reference Unit (GBRU)[footnote 1]. Data for laboratory-confirmed cases from 2007 onwards was extracted from the reference laboratory database using ‘date received by the laboratory’.
All S. Typhi and S. Paratyphi isolates referred to the SRS undergo identification using whole genome sequencing (WGS) and single nucleotide polymorphism (SNP) typing (3, 4). Epidemiological information was obtained from enhanced enteric fever surveillance (5).
Cases are occasionally tested multiple times for confirmation and to check the infection has cleared, therefore data has been deduplicated so that only one laboratory report for each case is counted.
Confirmed asymptomatic, probable and possible cases are analysed separately at the end of this report.
All data was analysed using Excel for Office 365 (Version 2002, Microsoft).
General trend
Since the beginning of the coronavirus (COVID-19) pandemic in early 2020 there has been a significant decrease in international travel worldwide as many countries, including the UK, imposed restrictions on both arriving and departing travellers (6). Data on travel to and from the UK was obtained from the Office of National Statistics (ONS) International Passenger Survey (7).
In 2020, UK residents made 23.8 million visits abroad, a 74% decrease from 2019, and there were 11.1 million visits made by overseas residents to the UK, a 73% decrease compared to 2019 (8). In line with falling numbers of travellers arriving in the UK, there was a significant decrease in cases of enteric fever (typhoid and paratyphoid) diagnosed in EWNI in 2020 compared to previous years.
In 2020, 190 laboratory-confirmed symptomatic cases of S. Typhi and S. Paratyphi infection were reported by the UKHSA SRS in EWNI, which is a decrease of 63% when compared to the 507 cases reported in 2019 (see table 1 and figure 1).
This is the largest annual decrease observed since 2000. The annual change in total case numbers of S. Typhi and S. Paratyphi varied considerably between 2016 and 2020, with a range of -63% to +46%. The largest increases occurred in 2018 and 2019 immediately prior to the start of the COVID-19 pandemic. In 2020, 67% of cases were caused by S. Typhi and 33% by S. Paratyphi A and B (see table 1). There were no cases of S. Paratyphi C reported in 2020.
Table 1. Laboratory-confirmed symptomatic cases of enteric fever, England, Wales and Northern Ireland by organism: 2011 to 2020
| Year | S. Typhi | S. Paratyphi A | S. Paratyphi B | S. Paratyphi C | Mixed infection | Total | % S. Typhi |
|---|---|---|---|---|---|---|---|
| 2011 | 253 | 219 | 7 | 0 | 1 | 480 | 53% |
| 2012 | 177 | 162 | 12 | 2 | 1 | 354 | 50% |
| 2013 | 185 | 121 | 6 | 0 | 0 | 312 | 59% |
| 2014 | 185 | 114 | 10 | 1 | 1 | 311 | 59% |
| 2015 | 168 | 107 | 26 | 0 | 0 | 301 | 56% |
| 2016 | 172 | 133 | 8 | 0 | 0 | 313 | 55% |
| 2017 | 187 | 103 | 15 | 0 | 0 | 305 | 61% |
| 2018 | 203 | 126 | 19 | 0 | 0 | 348 | 58% |
| 2019 | 321 | 166 | 19 | 1 | 0 | 507 | 63% |
| 2020 | 127 | 57 | 6 | 0 | 0 | 190 | 67% |
Figure 1. Laboratory confirmed cases of S. Typhi and S. Paratyphi, with % change year to year, England, Wales and Northern Ireland: 2011 to 2020

Age and sex
In 2020, age and sex were known for all 190 confirmed symptomatic cases: 36% were adults aged between 20 and 39 years (see figure 2); and the median age was 24 years (range 0 to 90 years). Those under 15 years accounted for 35% of cases, with 4% (7 cases) of the total in children under 2 years (and thus not routinely eligible for vaccination). Overall, there were slightly more male (53%) than female cases.
Figure 2. Laboratory confirmed cases of enteric fever, England, Wales and Northern Ireland by age and sex: 2020 (total 190 cases)

Geographical distribution
Geographical areas were assigned based on patient postcode; in a small number of cases patient postcode was missing and the sending laboratory postcode was used. The largest proportion of English cases of S. Typhi and S. Paratyphi in 2020 were reported in London (29%), a decrease on the previous year (32% in 2019) (see table 2). The largest relative decrease in cases reported in 2020 compared to 2019 was seen in Wales (from 11 to 1 case) followed by the North East region (87% decrease). No regions saw an increase in cases compared to the previous year.
Table 2. Laboratory confirmed cases of S. Typhi and S. Paratyphi, England, Wales and Northern Ireland by geographical distribution: 2019 and 2020
| Geographical area (UKHSA centre) | 2020 | 2019 | % change |
|---|---|---|---|
| London | 55 | 164 | -66% |
| North West | 35 | 83 | -58% |
| South East | 30 | 56 | -46% |
| West Midlands | 20 | 62 | -68% |
| Yorkshire and the Humber | 15 | 36 | -58% |
| East of England | 14 | 38 | -63% |
| East Midlands | 9 | 23 | -61% |
| South West | 8 | 17 | -53% |
| North East | 2 | 15 | -87% |
| England total | 188 | 494 | -62% |
| Wales | 1 | 11 | -91% |
| Northern Ireland | 1 | 2 | -50% |
| EWNI total | 190 | 507 | -63% |
Disease presentation and outcomes
In 2020, symptom information was known for 181 out of 190 cases. The most common symptom for all cases combined was fever (89%); followed by diarrhoea (67%); abdominal pain (50%); vomiting (48%); and headaches (44%). A higher proportion of S. Typhi cases experienced fever (88%) compared to S. Paratyphi cases (82%), but cases of S. Paratyphi reported more abdominal pain (53%) than that of S. Typhi (45%). Reporting for the remaining symptoms were similar for both S. Typhi and S. Paratyphi with the difference being 5% or less for each symptom.
Where the data was available (143 out of 186 cases), more S. Typhi cases reported absence from work (69%) as a result of their illness than S. Paratyphi (61%). Where data was available for length of absence (52 out of 143 cases), cases of S. Typhi reported on average missing at least 10 days, while S. Paratyphi cases reported missing at least 12 days of work as a consequence of their illness.
Where the data was available (184 out of 186 cases) more S. Typhi cases were admitted to hospital as a result of their illness (84%) than S. Paratyphi cases (72%). Where data for length of stay (LOS) was available (40 out of 184 cases), on average both S. Typhi and S. Paratyphi cases reported a LOS of at least 6 days.
Travel history
In 2020, 98% (187 out of 190) of symptomatic laboratory-confirmed cases of S. Typhi and S. Paratyphi had travel history information recorded (that is, whether they had travelled abroad or not) (see figure 3). In 2020, 93% (173 out of 187) of confirmed symptomatic cases with recorded travel history reported onset of illness within 28 days of travel to an endemic region of the world (and therefore were presumed to have acquired the infection abroad). This represents a decrease from 97% (490 out of 506) in 2019. Of cases in 2020, 165 out of 173 (95%) were UK residents and had travelled abroad from EWNI, while the remainder were new entrants to EWNI (8 cases). For 14 (7%) cases no foreign travel in the 28 days prior to becoming symptomatic was reported, compared to 16 (3%) in 2019.
Figure 3. Laboratory confirmed cases of enteric fever, England, Wales and Northern Ireland by travel history: 2011 to 2020
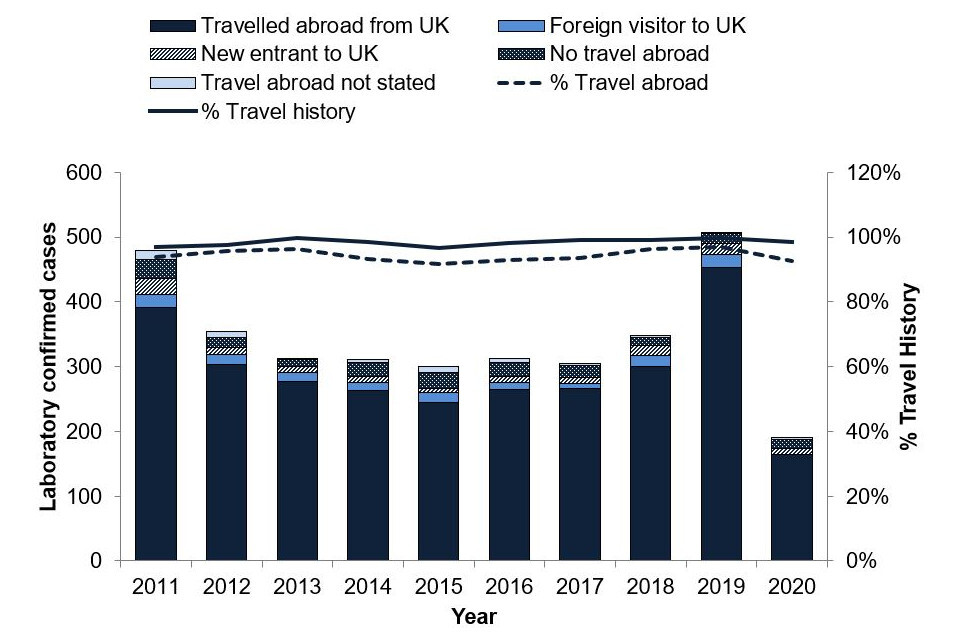
Figure 4. Reason for travel for laboratory confirmed cases of enteric fever that travelled abroad from England, Wales and Northern Ireland: 2020 (total 165 cases)

Where reason for travel was documented (157 cases), 89% (139 out of 157) of cases travelled abroad from EWNI to visit friends and relatives (VFR) (see figure 4). The majority travelled to countries in Southern Asia (see table 3) and acquired the infection while visiting friends or relatives abroad in Pakistan, India and Bangladesh.
Ethnicity was not known for 14 cases that travelled abroad to visit friends and relatives, these individuals travelled to Pakistan (7), India (5), Bangladesh (1) and a country in Africa (1). Of the 4 other or mixed ethnicity cases with travel to Pakistan, 3 reported their ethnicity as white or Asian Pakistani.
For those UK resident cases who did not visit friends and relatives (18 cases), where reason for travel was known the reasons given included holidays (13), business (2), and other, such as studying abroad (3). Cases that did not travel to visit friends and relatives travelled to a number of countries, including India (9), Pakistan (1), Bangladesh (1), other countries in Asia (6), and the Americas (7), with some travelling to more than one country. Of the 8 cases where reason for travel was not stated, 6 travelled to Pakistan.
Table 3. Countries of travel and ethnicity for laboratory confirmed cases of enteric fever that travelled abroad from England, Wales and Northern Ireland to visit friends and relatives: 2020 (total cases 139)
Note: some cases travelled to more than one country; all countries are included here so the totals will be higher than the actual number of cases.
| Presumed country of infection | Pakistani ethnicity | Indian ethnicity | Bangladeshi ethnicity | Asian other ethnicity | Black African ethnicity | Other or mixed ethnicity | Ethnicity not stated | Total |
|---|---|---|---|---|---|---|---|---|
| Pakistan | 74 | - | - | - | - | 4 | 7 | 85 |
| India | - | 32 | - | 1 | - | - | 5 | 38 |
| Bangladesh | 1 | - | 9 | - | - | - | 1 | 11 |
| Other Asia | 1 | 1 | - | 1 | - | - | - | 3 |
| Africa | - | - | - | - | 3 | - | 1 | 4 |
| Europe | - | - | - | - | - | 1 | - | 1 |
| Total | 76 | 33 | 9 | 2 | 3 | 5 | 14 | 142 |
Since November 2016, Pakistan has had an ongoing outbreak of extensively drug-resistant (XDR) strain of S. Typhi in the Sindh province, with resistance seen to most antibiotics used to treat enteric fever, including ampicillin, chloramphenicol, co-trimoxazole (which confers multidrug-resistant (MDR) S. Typhi), fluoroquinolones and third generation cephalosporins (bla CTX-M-15 extended spectrum beta-lactamase (ESBL) producers) (9, 10).
Since 2019, the XDR strain has been found circulating in other areas of Pakistan and is no longer restricted to the Sindh province (10, 11).
Prior to the COVID-19 pandemic there had been an increasing trend of imported XDR S. typhi cases from Pakistan, with 1 case reported in 2017, 6 cases from 2018 and 34 in 2019 (9, 12).
In 2020, 27 cases of XDR S. Typhi were diagnosed in the UK which were part of a 5-SNP cluster of cases imported from Pakistan. Of these, 26 cases travelled abroad from the UK to Pakistan representing 28% of all cases who travelled abroad from the UK to Pakistan. The remaining case did not travel and had contact with a family member or friend who had travelled to an endemic country. See clinical guidance for the management of these extensively drug-resistant cases.
Non-travel-associated cases
In 2020, there were 14 cases classified as non-travel-associated cases, these were confirmed cases of symptomatic enteric fever where the case reported that they had not travel in the 28 days prior to becoming symptomatic:
- 10 were caused by S. Typhi
- 3 were caused by S. Paratyphi A
- 1 was caused by S. Paratyphi B
Of the 14 non-travel-associated cases, 5 cases had contact with a family member or friend who had travelled to an endemic country and 2 cases were contacts other cases who had recently travelled abroad. Two additional cases had no recent travel history but had travelled to an endemic region in the previous 9 months. No potential source was identified for the remaining 5 cases.
Confirmed asymptomatic cases
In 2020, there were 4 confirmed cases of asymptomatic enteric fever caused by S. Typhi (2 cases), S. Paratyphi A (1 case), and S. Paratyphi B (1 case). Of these cases travel history was known for 3:
- 1 did not travel but had contact with a family member who had recently travelled to Pakistan
- 1 case was VFR in Pakistan
- the final case travelled to Mexico and Bolivia on holiday
Probable and possible cases
In 2020, there were 4 possible cases of enteric fever as defined in the public health operational guidelines for enteric fever (13). Of these, all had travelled abroad from the UK. Travel history information for the possible cases is detailed in table 4. Caution should be used when interpreting this data as it has not been confirmed by the UKHSA reference laboratory. There were no probable cases of enteric fever reported in 2020.
Table 4. Country of travel and reason for travel for probable and possible cases of enteric fever that travelled abroad from England, Wales and Northern Ireland: 2020 (total 4 cases)
| World region of travel | VFR | Business | Total |
|---|---|---|---|
| Gabon | 1 | - | 1 |
| Liberia | - | 1 | 1 |
| Pakistan | 1 | - | 1 |
| Uganda | 1 | - | 1 |
| Total | 3 | 1 | 4 |
Information resources
NaTHNaC typhoid and paratyphoid fact sheet
NaTHNaC food and water hygiene advice
UKHSA typhoid and paratyphoid page
Typhoid: health advice for travellers (Asian languages)
Travelling overseas to visit friends and relatives – health advice
Gastrointestinal bacteria reference unit – reference and diagnostic services
References
- Cook GC and Zumla A. ‘Manson’s tropical diseases’ Elsevier Health Sciences 2009.
- Heymann DL. ‘Control of communicable diseases manual’ American Public Health Association 2008.
- Chattaway MA and others. ‘The transformation of reference microbiology methods and surveillance for Salmonella with the use of whole genome sequencing in England and Wales’ Frontiers in Public Health 2019, volume 7, page 317.
- Dallman, TJ and others. ‘SnapperDB: a database solution for routine sequencing analysis of bacterial isolates’ bioRxiv 189118 (viewed 7 February 2023).
- UK Health Security Agency. ‘Typhoid and paratyphoid: guidance, data and analysis’ - health protection collection (online) (viewed 7 February 2023).
- Office for National Statistics. ‘Coronavirus and the impact on the UK travel and tourism industry’ (online) (viewed 9 February 2023).
- Office for National Statistics. ‘International Passenger Survey’ (online) (viewed 9 February 2023).
- Office for National Statistics. ‘Overseas travel and tourism: 2020’ (online) (viewed 9 February 2023).
- Nair S and others. ‘ESBL-producing strains isolated from imported cases of enteric fever in England and Wales reveal multiple chromosomal integrations of blaCTX-M-15 in XDR Salmonella Typhi’. Journal of Antimicrobial Chemotherapy 2021, volume 76, issue 6, pages 1459 to 1466.
- World Health Organization disease outbreak news item. ‘Typhoid fever - Islamic Republic of Pakistan’ (viewed 21 February 2023).
- Rasheed F and others. ‘Emergence of resistance to fluoroquinolones and third-generation cephalosporins in Salmonella Typhi in Lahore, Pakistan’ Microorganisms 2020, volume 8, page 1336 (viewed 21 February 2023).
- Chattaway MA and others. ‘Phylogenomics and antimicrobial resistance of Salmonella Typhi and Paratyphi A, B and C in England, 2016 to 2019’ Microbial Genomics 2021, volume 7, issue 8, 000633.
- Public Health England and the Chartered Institute of Environmental Health. ‘Public health operational guidelines for typhoid and paratyphoid (enteric fever)’ (viewed 7 February 2023).
-
As we only collect data from the UKHSA Salmonella Reference Service, local reports of cases of enteric fever may differ for Wales and Northern Ireland. ↩
