SPI-M-O: Statement on their concerns for next few months, 14 July 2021
Updated 26 October 2021
SPI-M-O: Statement on their concerns for next few months
Date: 14 July 2021
All probability statements are in line with the framework given in the Annex.
1. As the final step of easing restrictions of the Roadmap is taken, it is expected there will be further waves of infections, hospitalisations, and deaths, as discussed in SPI-M-O’s latest modelling of the potential impact of Step 4[footnote 1]. One key concern for SPI-M-O is that any epidemic trajectory that could lead to unsustainable pressure on the NHS or other adverse outcomes would need to be identified and a contingency enacted within days.
High incidence and prevalence of infection
2. In a world of high incidence, doubling of large numbers of infections could lead to an unsustainably high prevalence quickly and associated increases in hospitalisations and deaths in the following weeks. The momentum and delays built into the system often means that a doubling in, for example, hospitalisations is likely to happen, even if any action to prevent new infections is taken.
3. If growth in incidence does not show signs of starting to plateau at expected levels, or significantly exceeding estimates from Roadmap modelling, then stringent measures may be required to reverse growth. Delaying introduction of measures increases the risk that they will have to be more stringent if applied.
4. With very high numbers of cases, testing capacity could be overwhelmed, hampering surveillance and leading to difficulties monitoring the progress of the epidemic, and sequencing capacity could delay detection of novel variants. Further issues with surveillance are also possible if other data streams become saturated or unexpected patterns emerge, for example due to interactions with other infections.
5. It is possible that testing behaviour in the general population will change; this alone will make the data more difficult to interpret. The closure of schools for summer holidays is likely to reduce transmission overall but will also reduce an important surveillance data stream from lateral flow testing.
6. If incidence reaches very high levels, such as greater than 1 million infections per week, there could be implications for workforces and critical infrastructure due to both acute disease and longer sequelae, and the required self-isolation due to contact with cases.
7. High community prevalence will be a particular challenge for hospitals and care homes, which are known to be more risky settings. Immunocompromised and more vulnerable people are more likely to come into contact with the health and care system.
Impact on vaccine effectiveness and coverage
8. As the force of infection increases with increasing incidence, it is possible that vaccines could be less effective than is currently estimated[footnote 2]. Vaccine effectiveness to date has been measured in a relatively low prevalence world with infrequent exposures. As infections increase, so will the number and strength of challenges from SARS-CoV-2 that vaccinated individuals will face. If vaccines protect against a given percentage of challenges, rather than a percentage of individuals, the effectiveness estimated to date may be overly optimistic.
9. As previously discussed[footnote 1], the number of people who are not vaccinated is not precisely known, so estimates of vaccine uptake remain uncertain. There may also be other populations, such as those not registered with the health system, where SARS-CoV-2 infections are spreading but not identified; these may propagate and continue increases in the wider population. If those who remain unvaccinated are focused in higher risk groups, such as Black, Asian, and minority ethnic individuals or those living in urban or higher transmission settings, it is possible that there will be more and more serious health outcomes, amplifying the inequalities already present. Continued effort to vaccinate all age groups is required, noting that increased coverage from, say, 85 percent to 90 percent reduces the proportion unvaccinated by one third.
Reliance on population immunity
10. How high the peak will be or when it might occur are unknown. Population immunity, either through natural infection or vaccination, will eventually lead to decreases in growth of SARS-CoV-2, however, there may be a range of dynamic effects at work and the peak may be drawn out over many weeks. Clear signals at local levels, such as upper or lower tier local authorities, are currently very limited, which emphasises the need for continued surveillance. It is possible that there will be chronic pressure on healthcare services over a period of high prevalence, whilst capacity is not exceeded.
11. With spatial heterogeneity in population immunity, it is possible that some areas may have significant further growth in cases and hospitalisations, even after others have peaked and incidence is clearly decreasing. These effects on healthcare may be exacerbated by differential provision in different locations, for example, some places may have more cases and smaller hospitals.
12. Waning of vaccination and infection-acquired immunity and reduced cross-protection to novel variants are a significant concern, given that control measures are likely to rely on population immunity effects. This, however, is unlikely to be important until later in the year, and into 2022.
Autumn and Winter 2021 to 2022
13. SPI-M-O is concerned that September and October 2021 will be a particularly risky point in the trajectory of the epidemic. It is likely behaviours will take time to return to more normal levels and, if this coincides with the return of schools and universities in the autumn, significant pressures on healthcare could be seen. This could be exacerbated by other normally seasonal infectious diseases increasing in prevalence.
14. During the past 18 months, diseases such as influenza, Respiratory Syncytial Virus (RSV), and norovirus, have been circulating much less in the population than previous years. Their transmission dynamics have changed due to the measures to control COVID-19 and, as a result, there may be a period of unpredictable epidemics of these diseases before their normal seasonal patterns return[footnote 3]. It is also possible there will be interactions between SARS-CoV-2 and other infections, both in combination and in competition. Any such effects are as yet unknown. Surveillance of COVID-19 may also be more difficult during peaks of other respiratory viruses.
Novel variants
15. Increasing numbers of infections combined with selection pressure from vaccination (either one or two doses) may create an environment for further viral evolution. This combination may lead to the virus evolving in a way that escapes immunity, however, it will be very difficult to predict any precise genetic changes. Excellent surveillance systems are needed to ensure any novel variants are identified. It is also possible that other strains of SARS-CoV-2, such as B.1.351 (beta) and P1 (gamma) [footnote 4], may also increase in prevalence as population mixing increases. Reducing the number of infections will reduce the risk of emergence or establishment of new variants, albeit not necessarily in a linear manner, and make it easier to detect any new threats.
16. If a novel variant emerges and successfully establishes itself, options for intervention may be even more limited. A novel variant would be of concern if it has:
i) a transmission advantage;
ii) escape from immunity (vaccine- or natural infection-induced) or
iii) leads to more severe health outcomes,
or any combination of these three.
17. Rapid identification of genetic variants remains crucial. Monitoring of the emergence and spread of the alpha and delta variants was possible due to the S-gene target failure signals. Further data streams from rapid typing are vital, and it is essential for these to be linked to epidemiological patterns to identify potential outbreaks and establishments of new or imported variants.
International
18. The international context of the pandemic will remain important as the UK epidemic is not happening in isolation. Global surveillance, particularly on the emergence and control of novel variants of concern, and vaccination is required to bring infections worldwide under control. Any increase in foreign travel over the summer and the return of international students to universities in the autumn is of particular concern.
Data availability
19. Data gaps continue to limit SPI-M-O’s view of the pandemic and could mean that important signals are missed, or their detection is delayed. In particular, SPI-M-O are missing timely and linked data on vaccination status and hospital admissions. There is no national database of infection control measures used across different hospital trusts.
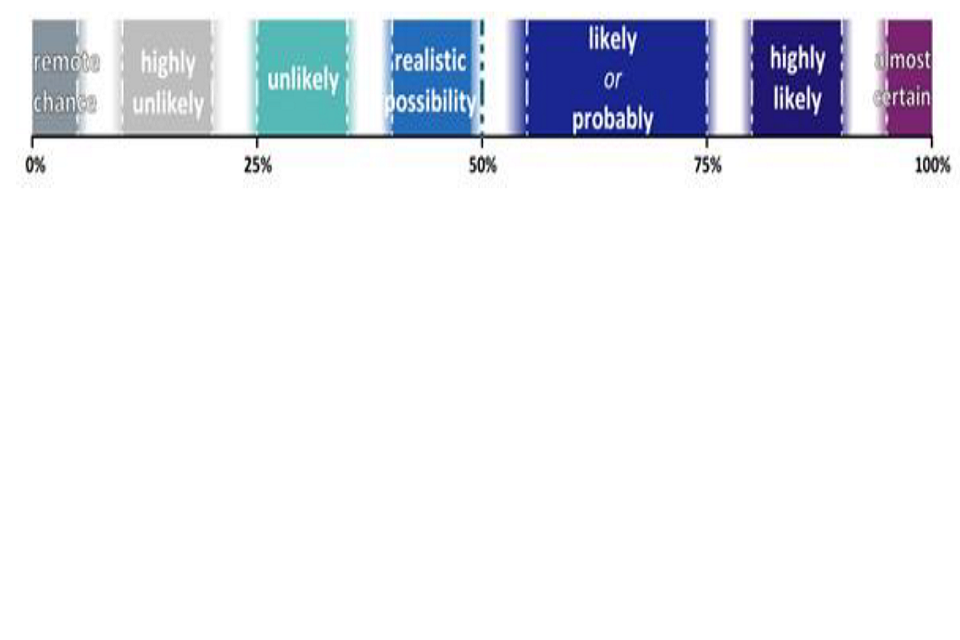
Annex: PHIA framework of language for discussing probabilities
-
SPI-M-O: Summary of further modelling of easing restrictions – Roadmap Step 4 on 19 July 2021; SAGE 93, 7 July ↩ ↩2
-
COVID-19 vaccine surveillance reports; Public Health England ↩
-
COVID-19: Preparing for the future. Looking ahead to winter 2021/22 Academy of Medical Sciences ↩
-
The World Health Organisation recommended using letters of the Greek alphabet when referring to SARS-CoV-2 variants. Current variants of concern labelling stands as B.1.1.7 as alpha, B.1.351 as beta, P.1 as gamma, and B.1.617.2 as delta. ↩
