SPI-B, SPI-M and EMG: Considerations for potential impact of Plan B measures, 13 October 2021
Updated 13 May 2022
This paper considers the potential impact of several measures described by government as Plan B: reintroduction of working from home guidance, legally mandating face coverings in some settings, and vaccine-only certification in some limited settings. This paper should be read in conjunction with SPI-B: ‘Behavioural considerations for maintaining or reintroducing behavioural interventions and introducing new measures in Autumn 2021’, which also considers increasing communication of risk, and EMG-NERVTAG: ‘Update on transmission and environmental and behavioural mitigation strategies including in the context of Delta.’
Executive summary
-
The Plan B interventions are likely to be most effective in combination [High confidence]. Measures are not likely to be simply additive but may have complementary interactions that result in a greater cumulative impact on transmission [High confidence].
-
Reintroduction of working from home guidance, for those who can, may have the largest impact on transmission out of the potential Plan B measures. The impact of reintroducing working from home guidance would likely largely depend on what proportion of workers are attending their workplaces at that time and the behavioural response – that is, adherence by employers and employees [Medium confidence]. There are, however, associated harms and unequal impacts that should be considered prior to implementation [High confidence].
-
The version of certification proposed in Plan B differs significantly from versions implemented in most other countries (both in being vaccine only and the relatively narrow range of settings in which it would apply). This absence of comparators means there is little direct evidence for the likely impact [High confidence].
-
Vaccine-only certification as proposed may only have a very small direct impact on transmission [Medium confidence] but has potential to improve vaccine uptake in certain groups, particularly young adults [High confidence]. However, there are potential harms and inequalities that should be considered prior to implementation [High confidence].
-
Increasing the range of applicable settings, time-limiting certificates based on last vaccination date, and including a requirement for proof of a negative test, could all be considered to increase the potential impact on transmission and vaccine uptake. Clear and consistent communications (with sufficient notice and positive framing) are also likely to influence outcomes.
-
The view of the impact on transmission of face coverings remains consistent with previous SAGE advice: face coverings are likely to reduce transmission through all routes by partially reducing emission of and or exposure to the full range of aerosol and droplets that carry the virus, including those that remain airborne and those that deposit on surfaces [High confidence]. Face coverings are likely to be more effective when they are manufactured from high quality materials and fit well on the face, covering the nose and the mouth [High confidence]
-
Face coverings are only effective if they are worn (and worn correctly). Mandating the use of face coverings in appropriate situations is likely to increase usage, which has declined significantly in England since July 2021 when it ceased to be a legal requirement [High confidence].
-
Whether Plan B will be required will depend on a range of factors, in particular vaccine and booster uptake. Increasing vaccine uptake (including boosters) continues to be the most important measure to mitigate the health impacts of the SARS-CoV-2 epidemic in the UK.
-
Other measures are available which, if introduced, could also make Plan B (or more stringent measures) less likely (and could potentially offer better efficiency or effectiveness) for example encouraging wider use of rapid antigen testing in workplaces and the community, and ensuring self-isolation of those who test positive by providing sufficient support [High confidence].
Introduction
1. The UK government has recently set out its plan for autumn to winter 2021 which included the possibility of reintroduction of several non-pharmaceutical interventions (NPIs) as part of a Plan B - if data suggests the NHS is likely to come under unsustainable pressure [Reference 1]. Potential NPIs included a limited period of asking people to work from home where able, vaccine-only certification, legally mandating use of face coverings in certain settings and increasing communication of risk.
2. SAGE has previously advised on the potential and estimated impacts of NPIs on transmission, including working from home, use of face coverings, and certification [Reference 2] [Reference 3]. However, in recent months the context in the UK has changed with the emergence of the more transmissible Delta variant, more of the adult population being vaccinated and infected, emerging evidence of waning vaccine-induced immunity, relaxation of other NPIs (including increased international travel), and currently consistently high prevalence of infection in the community.
3. This note discusses the available evidence for the potential impact on transmission of introduction of Plan B measures this autumn and winter, including working from home guidance, vaccine-only certification, and use of face coverings – setting out important factors and considerations that are expected to influence potential impact.
4. Estimating the potential impact of different measures is challenging and there are some important caveats to consider.
-
The impact of different measures is highly dependent on a complex network of physical, biological, and behavioural factors influenced by:
- the epidemiological context in which measures are introduced (for example community infection rates)
- how measures are implemented
- the capability of, motivation to, and opportunities for individuals to adhere to NPIs [Reference 4]
- the interactions between different measures
-
Evidence for the effectiveness of individual interventions is underpinned by a degree of uncertainty and challenging to collect as there are often multiple interventions in place at one time and adherence may be heterogenous, poorly understood, and difficult to measure [Reference 2]. As set out in previous advice, different measures do not generally have a simple additive effect but will interact in a non-linear fashion [Reference 3].
5. Although the primary purpose of this paper is to consider the Plan B package, it should be noted that increasing vaccine uptake (including boosters) continues to be the most important measure to mitigating the health impacts of the SARS-CoV-2 epidemic in the UK. Coverage is high in older ages, but decreases with age, and unvaccinated are clustered within areas and communities.
6. In addition, encouraging and supporting uptake and adherence to existing symptomatic isolation and testing policies, as well as workplaces undertaking regular rapid testing, could help to mitigate against the need to adopt additional measures over the winter, and might be more efficient or effective than the interventions proposed. Reducing ‘presenteeism’ and encouraging working from home where possible among individuals experiencing symptoms of any infectious illness would not only widen the net around SARS-CoV-2 cases whose onwards transmission could be reduced but would also reduce the healthcare burden of other infections of concern over the winter (such as influenza, other respiratory infections). Preventing the transmission of infections within workplaces could also reduce the numbers of staff overall who are absent due to illness.
7. This paper should be read in conjunction with SPI-B: ‘Behavioural considerations for maintaining or reintroducing behavioural interventions and introducing new measures in Autumn 2021’ [Reference 5] and EMG-NERVTAG: ‘Update on transmission and environmental and behavioural mitigation strategies including in the context of Delta’ [Reference 6].
Working from home
8. SAGE has previously advised with high confidence that working from home can reduce transmission significantly [Reference 7]. Working from home reduces the risk of infection primarily by reducing the average number of contacts an individual has. The risk of infection from attending the workplace is a combination of infection risk at the workplace (which is also a combination of different risks affected by, for example, the ability to socially distance at the workplace and ventilation measures in place), risk from travelling to or from the workplace, and the risk from additional activities that would not otherwise be engaged in if working from home such as socialising with colleagues outside of the workplace.
9. Working from home also provides a benefit to those unable to work from home by reducing their average number of contacts and risk of exposure through reducing occupancy of settings such as public transport.
10. The likelihood of an individual becoming infected in a given environment will also depend on their level of immunity, whether from infection or vaccination. Factors outside of the workplace such as socioeconomic inequalities, household size, and barriers to self-isolation may also contribute to increased risk of infection for those unable to work from home.
11. While working from home can reduce transmission at the individual and population level, the impact of working from home guidance will depend on behaviour - the adherence to the guidance by employers and employees – which is difficult to estimate (see accompanying SPI-B paper).
12. Estimates vary for the increased risk of infection associated with not working from home. Study findings will be affected by the state of the epidemic at the time as well as the other NPIs in place, which could have affected work attendance, crowding and contact rates (for example: school closures; the availability of support; hospitality sector shut preventing socialising; social distancing measures). Many studies are from periods of low occupancy of many workplaces and public transport when significant NPIs were in place, and vaccination rates were also lower.
-
Virus Watch: Analysis of a subset (N = 10,808) of a community cohort study during the second wave of the epidemic in England and Wales estimated those leaving for work or education during this period had a 15% risk of being infected, compared to 9% for those who did not (OR 1.70, CI 1.50 to 1.92) [Reference 8]. Controlling for the impact of travelling to work on public transport reduced this increased risk of infection, although it remained significantly higher than for those not leaving the house for work or education.
-
JBC: Modelling considering available mobility, contact, and behavioural data suggests an approximate 10 percentage point increase in workplace mobility alone could lead to an approximate 0.1 increase in Rt[footnote 1], although this may underestimate the total effect if there are concurrent increases in transport use and out of work contacts (which is expected) [Reference 9].
-
REACT-1: Interim analysis of rounds 5 to 10 of REACT-1 (survey of more than 150,000 individuals in England each month)[footnote 2] suggests those working outside of the home have consistently been more likely to test positive, indicating a reduced risk of infection for those not working outside the home (OR 0.73, CI 0.68 to 0.79) [Reference 10].
-
ONS CIS: Multiple analyses of data from the ONS Coronavirus Infection Survey have indicated an increased risk of infection for those not working from home.
-
Interim analysis from ONS of the CIS suggests working outside of the home remains a predictor of positivity, although this increased risk (compared to those working from home) is currently not as pronounced compared to the period October 2020 to March 2021 [Reference 11]. For example, in the fortnight from 14 March to 27 March 2021 people working outside of the home were 1.61 times more likely to test positive than those working from home, while in the fortnight 29 August to 11 September, they were 1.26 times more likely.
-
Further ONS analysis of swab positivity rates of individuals (16 to 74 years old) between September 2020 and May 2021 suggests those in patient facing roles in healthcare were more likely to test positive than those in non-patient facing roles over this period [Reference 12]. However, this analysis did not differentiate by age or vaccination status and the comparatively low number of patient-facing roles means there is a larger degree of uncertainty for this group. More recent analysis from late June to early September 2021 found no statistical evidence of a difference for test positivity in those in patient facing roles and all other adults (including those not working).
-
Independent analysis of CIS data from May 2020 to February 2021 (N = 409,000 in 72,866 households) found that the highest infection rates were in those under the age of 25, living in larger households, and those who were unable to work from home and had to use public transport [Reference 13].
13. Risk at the workplace is highly variable across sectors and across job types, although it is extremely difficult to determine how much transmission takes place within the workplace, and how much is associated with related activities [Reference 14]. Mitigation measures implemented across similar workplaces are also highly variable. Smaller work teams and asynchronous work patterns have been suggested to reduce the infection risk [Reference 15] and there is literature to suggest reductions in risk can be achieved through staggering shifts and bubbling of staff [Reference 16].
14. Analysis of workplace outbreaks and modelling of factors which influence transmission in the workplaces is ongoing as part of the PROTECT National Core Study[footnote 3]. Outbreak studies suggests that workplace interactions can be complex and that settings such as break rooms, locker rooms, canteens, and shared vehicles, particularly where they are less supervised, could be as or more important than the main office or factory workspaces for exposure. Modelling suggests that reducing the number of employees in a workplace is likely to be the most successful strategy to minimise the size of an outbreak associated with a workplace.
15. Current average contact levels remain significantly below pre-pandemic levels and those going into the workplace have on average had fewer contacts in the workplace than before the pandemic – which is likely to change if work from home levels continue to decrease. Prior to the pandemic most daily contacts made by adults were in the workplace.
- CoMix: The CoMix social contact survey has consistently reported low average contacts for employed adults who are able to work from home (approximately 2.5 contacts per day compared to 7.5 per day for those attending their workplace) [Reference 17], although those attending their workplace are currently reporting far fewer contacts than in Autumn 2020 (7.5 compared to 11). The proportion of employees attending work if their workplace is open is comparable to Autumn 2020. The difference in reported contacts may be in part due to changes in those attending workplaces (for example more white-collar or office-based, increased hybrid working patterns) although this is unlikely to fully explain this effect.
16. Continued use of occupancy limits in some workplaces and mixed working patterns may lower risk at and travelling to or from the workplace, and subsequently the potential impact of reintroduction of a form of working from home guidance. It is very difficult to quantify the potential for reduction in transmission from reintroduction of working from home guidance without understanding what proportion of the workforce that can work from home have returned to their workplace, and in what working pattern. However, current behaviours and contact patterns remain significantly different to pre-pandemic and there remains potential for a rapid worsening of the epidemiological situation if contact levels increase significantly.
17. Similarly, vaccine effectiveness estimates are highly contextual and are currently derived from periods with contact rates below pre-pandemic norms. As contact rates increase (and particularly while prevalence remains high), vaccinated individuals are likely to be challenged more regularly and at higher doses through exposure to infectious individuals.
18. The relationship between average contacts and risk of infection resulting from attending a workplace is not likely to be linear. It is likely that as workplace and public transport occupancy increases along with overall contact levels and changes in behavioural norms, the risk of infection from leaving the house for work will increase more so.
19. Working from home is not an option for around half of the UK population (only around 47% are estimated to have been able to do so during the first lockdown in April 2020 [Reference 18] and the impact of reintroducing a form of working from home guidance would likely largely depend on what proportion of workers are attending their workplace at that time and subsequently are able to not continue to do so.
20. Even when able to work from home there is evidence that not all have done so. The impact of reintroducing guidance for some to work from home where possible is highly likely to be heterogenous across age, socioeconomic groups, employment sector or job type (for example, in April 2020 occupations requiring higher qualifications or experience were much more likely to be working from home [Reference 3], and regions.
21. Recent increases in workplace attendance have varied from region to region, with higher levels of attendance in areas with increased tourism and manufacturing sectors. London and the South East of England, where working from home rates have been reportedly higher than other regions [Reference 2] [Reference 19], has seen the slowest rate of return. In Scotland and Wales, the guidance on working from home has not yet been withdrawn.
22. Regions of persistent high prevalence in 2020 have been associated with several risk factors – including the reduced ability of individuals to work from home, as well as various factors that may influence the risk of attending work such as an increased proportion of the workforce attending settings associated with higher outbreak occurrence rates, mobility trends such as increased car sharing, and an increased proportion of low paid and insecure employment that may indicate a barrier to self-isolation [Reference 20]. Modelling has suggested that a higher number of people in routine occupations unable to work from home likely contributed towards persistent transmission in some LTLAs [Reference 21].
23. The impact of increasing rates of working from home on transmission is likely to increase over time, and the immediate impact may be small. This is likely to depend on multiple factors such as:
- rates of working from home at the time of implementation and wider behavioural norms that affect the average number of close contacts an individual has
- employee expectations and behaviours in response to the perception of a worsening epidemic situation (noting that the ability to work from home is usually not within control of individual employees and even if able to according to employer policy, lower socioeconomic groups have lower adoption due to factors such as housing)
- employer preference, and employer interpretation of the situation and guidance
- prevalence and effectiveness of workplace mitigations such as regular testing or ventilation that reduce the risk of infection at the workplace.
Considerations for implementation
24. Working from home is not necessarily a binary option, with many reporting a desire to work in a hybrid way with some days in the office and some at home [Reference 19]. All options with some home working will have the benefit of reducing the risk of infection for both those able to work from home and those unable to do so. The scale of benefits and harms of the different options should be considered.
25. With heterogenous and potentially unequal impacts, if reintroducing guidance to increase rates of working from home, consideration should be given to other measures to support and protect those unable to work from home (particularly those most affected such as deprived and ethnic minority populations). This could include wider provision of regular rapid antigen testing at workplaces for those unable to work from home, as discussed in more detail below.
Mitigating workplace risk
26. Policies that are effective in identifying and preventing the presence of infectious individuals at the workplace will mitigate against the need to take stronger measures. Current policies include:
- isolation upon onset of core COVID-19 symptoms and PCR testing (with isolation for 10 days if positive)
- availability of asymptomatic testing using rapid antigen tests, with 10-day isolation on positive test with availability of a confirmatory PCR test
27. However, there is evidence that adherence to isolation has reduced over time [Reference 22] and that there are significant barriers to isolation, such as poor symptom recognition and awareness of the requirement to take a test if symptomatic [Reference 5]. Surveys have reported various reasons for non-uptake of isolation including the need to attend workplaces and lack of income support [Reference 5]. Broadening the symptom criteria for taking a test could include a greater proportion of cases, potentially improving detection of infected and infectious individuals, potentially reducing the probability of infectious individuals attending a workplace.
28. Continuing to attend a workplace while ill with a respiratory illness was common prior to the SARS-CoV-2 pandemic. Only 34% of working adult participants (40% overall) in the Flu Watch study (2006 to 2011) took time off work or education for their illness with PCR-confirmed influenza A infection, although symptoms lasted 9.6 days on average (in whole cohort[footnote 4]).[Reference 23].
29. Encouraging individuals with a wider set of symptoms of respiratory illness to work from home if possible would likely isolate additional cases of COVID-19 (not identified by the core symptomatic isolation and testing criteria) but also have a wider benefit of reducing transmission of non-SARS-CoV-2 infections in the workplace (with potential to reduce population transmission and resultant hospitalisations from other infections). This may also result in fewer employees being infected at their workplace with other respiratory illnesses and reduced work absences [Reference 23] [Reference 24].
30. The current testing policy is highly unlikely to eliminate the presence of all COVID-19 infections in the workplace. With 100% adherence (and no delays between symptom onset and isolation) it is estimated that the current symptomatic testing policy would prevent only 71% (95% UI: 35, 88%) of an individual’s infectivity, due to pre-symptomatic and asymptomatic transmission [Reference 25].
31. Regular asymptomatic rapid antigen testing at workplaces could be an effective measure alongside other mitigations to reduce the infection risk in workplaces, for example ventilation and social distancing. Similarly, ensuring sufficient support (financial and otherwise) for effective self-isolation of those testing positive may reduce attendance of infectious individuals at their workplace – reducing the risk to those unable to work from home. It is important to ensure that there is also sufficient awareness of the availability of support, in advance of it being required.
32. Effectiveness of regular testing for those attending their workplace is dependent on frequency of testing, communication of good testing procedures and result comprehension, provision of tests and the ability for individuals to take up and adhere to the policy over time (and the extent to which this is correlated with vaccination and household transmission risks) [Reference 26] [Reference 27]. In the UK, rapid antigen testing has been found to be acceptable and feasible in the context of daily contact testing [Reference 28] including among staff and students at secondary schools [Reference 29] [Reference 30]. However, studies of mass asymptomatic testing in Liverpool have shown that uptake varies by sociodemographic characteristics including neighbourhood deprivation level, ethnicity, and gender [Reference 31] [Reference 32].
33. Rapid antigen testing is highly complementary to physical interventions such as masks, ventilation, and distancing. Rapid antigen test sensitivity is correlated to viral load at time of testing (expected to correlate in part to infectiousness[footnote 5]). As such, rapid antigen testing and subsequent isolation is likely to be effective at removing high viral load infections from a setting, while physical interventions are most effective with lower viral load infections.
Vaccine-only certification
Potential impact on transmission
34. Certification requiring a negative test decreases the probability that an individual entering an applicable setting is infectious [Reference 3]. Proof of vaccination may reduce the likelihood that an individual entering a setting is infected, as well as the likelihood of those present becoming infected if exposed and suffering severe symptoms if infected. There are only a few examples in comparator countries of certification policy that required proof of vaccination status that did not also allow certification with proof of COVID-19 recovery or a negative test result [Reference 33] [Reference 34]. These have been introduced very recently and as such there is very limited comparative evidence to estimate the potential impact of a vaccination-only policy on transmission.
35. Countries that have implemented certification policies have generally done so in a wide range of settings (such as indoor hospitality, leisure facilities, events, gyms) [Reference 33] [Reference 34]. Even under these circumstances, there is limited evidence for the direct impact of certification on population level rates of infection and or severe disease. Pilot studies from earlier in the pandemic produced mixed results and often included use of additional measures such as face coverings.
36. Several important considerations may affect the impact of vaccine-only certification on transmission including vaccine effectiveness, timing of vaccine-induced protection (including time to develop immunity and waning), vaccine uptake, the range of applicable settings, implementation and enforcement (including the use of fake certificates), and the prevalence of infection in the community (when prevalence is high, it is more likely that vaccinated individuals entering a setting will be infected [Reference 35]).
-
Vaccine effectiveness. The impact of vaccine-only certification on transmission within a setting will be reduced if vaccine effectiveness against infection or onward transmission is lower. Although there is evidence that vaccination reduces onward transmission of the Delta variant, this may be less than for the Alpha variant [Reference 36] [Reference 37]. Future variants may also have an impact on vaccine effectiveness against infection and onward transmission.
-
Waning immunity. Waning of vaccine-derived immunity, reducing effectiveness against infection and symptomatic disease, is apparent 10 weeks after the second dose, particularly in elderly and vulnerable groups [Reference 38]. Time limiting the validity of vaccine-only certificates according to the date of last vaccination could be considered.
Potential impact on vaccine uptake
37. Evidence from other countries of the impact of certification policies on vaccine uptake is mixed but suggests that there is potential for a positive impact, particularly in younger age groups.
- Analysis of 7 comparator countries found that in the majority there was little or no increase in vaccine uptake following announcement of certification. Israel was the exception, who observed a marked increase over the 10 days post-announcement [Reference 33]. Although this may have largely resulted from vaccine eligibility changes and increased communications [Reference 34].
- Analyses looking at vaccine uptake in younger age groups (most likely to be affected by the policy and to be unvaccinated) in France (where passports were required in wide range of settings), demonstrated an increase immediately after the announcement [Reference 39] [Reference 9].
- Analysis of 6 countries that introduced mandatory COVID-19 certification between May and August 2021 (with a control group of 20) found increased vaccine uptake prior to and after implementation. This was dependent on prior levels of vaccine uptake, with those countries with lower uptake prior to implementation exhibiting greater uptake afterwards but no significant effect seen in those countries that already had high uptake. Analysis by age showed the impact on uptake was highest in those younger than 20 and between 20 to 29 years old. Specific access restrictions to settings such as nightclubs were associated with higher uptake in younger age groups, and when extended to broader settings, higher age groups [Reference 34].
38. The impact vaccine-only certification may have on vaccine uptake is likely to depend upon the current state of vaccine rollout (and uptake across age groups), ease of access to vaccination, degree of vaccine hesitancy or complacency (with uptake only likely to be affected among the least hesitant or most complacent [Reference 5]), which groups are likely to be most affected, the scope of the proposed policy (such as settings and activities affected), and how the policy introduction is communicated to those likely to be affected.
Considerations for implementation
39. SAGE have previously noted certification has the potential for harms as well as benefits, noting the potential for adverse behavioural responses and unequal impacts [Reference 40].
40. There are difficult practical and ethical issues to be considered to minimise disproportionate impacts (ensuring equity and accessibility of certification and vaccination) and allow for effective implementation – which is highly likely to affect the overall impact on vaccine uptake and transmission. Examples of relatively robust certification policies (such as QR passes in Netherlands) have been hampered by loopholes, use of counterfeit certificates, and likely heterogenous enforcement across venues. This is thought to have contributed to chains of transmission linked directly to venues using and enforcing this certification approach [Reference 33]. Implementation and approach to enforcement is highly likely to influence the potential impact on reducing transmission within an affected setting [Reference 5].
41. Effective implementation is likely to require public support, particularly in those groups most likely to be affected. Public support for certification is generally high for large-scale events but declines for retail settings and workplaces [Reference 5] [Reference 33]. Certification may also reduce trust in some communities and entrench negative views about vaccination (in some instances certification has been associated with decreased self-reported willingness to be vaccinated in the most hesitant populations [Reference 5] [Reference 33]. Public support may be increased by ensuring clear communication that set out positively the potential for an impact of increased vaccine uptake and enabling activities, rather than restricting them.
42. Care should also be paid to consistency of messaging around certification and unintended impacts on other aspects of vaccination policy, such as uptake of booster doses. Specifically requiring two doses for certification could inadvertently confuse messaging around the need for boosters and disincentivise uptake. Similarly, consideration should be given to emerging evidence on waning of vaccine-induced protection and to time limiting certificate validity from date of last dose.
43. Overall, vaccine-only certification may only have a very small direct impact on transmission but has potential to improve vaccine uptake in certain groups, particularly young adults. However, there are potential associated harms and inequalities that should be considered prior to implementation. Increasing the range of applicable settings, time-limiting certificates based on last vaccination date, and including a requirement for proof of a negative test, could all be considered to increase the potential impact on transmission and vaccine uptake. Clear and consistent communications (with sufficient notice and positive framing) are also likely to influence outcomes.
Face coverings
44. The prevailing SAGE view on face coverings remains consistent with previous advice [Reference 7], that face coverings are likely to reduce transmission through all routes by partially reducing emission of and or exposure to the full range of aerosol and droplets that carry the virus [Reference 41] [Reference 42] [Reference 43], including those that remain airborne and those that deposit on surfaces [high confidence]. The full consensus statement from EMG on face coverings is included in Annex 1.
45. Face coverings are effective at reducing spread of virus from an infected individual and, to a lesser extent, providing protection to the wearer [Reference 44] [Reference 45] [Reference 46] [Reference 47] [Reference 48] [Reference 49] [high confidence]. The effectiveness of a face covering in protecting a susceptible individual from infection is dependent on the material from which the face covering is made, the extent to which it excludes infected particles, closeness of fit on the face and whether they cover both the nose and mouth [Reference 7] [Reference 50] [high confidence]. Plastic face shields are not a suitable alternative to a fabric face covering and are unlikely to provide much benefit in reducing emission of the virus or exposure to the virus when worn without a face covering [high confidence] [Reference 7]. Efficacy of face coverings in reducing transmission is dependent on the proportion and frequency of face covering wearing within the population, as well as material quality and fit [Reference 7]. The wider and more frequent the use, the more likely it is that an infected person will be wearing a face covering when they are sharing an environment with others [high confidence].
46. Face coverings can reduce the risk of transmission when people are in close proximity or small spaces even for short durations of time [Reference 7] [medium confidence]. They cannot compensate for poor ventilation but may further reduce risks of longer-range airborne transmission when people are in shared air for longer periods of time, and this effect may be more important in poorly ventilated spaces [low confidence].
47. Face coverings are likely to have benefits for the reduction of the transmission of other respiratory viruses including influenza [Reference 51] [Reference 52] [Reference 53] [Reference 54] [high confidence].
48. Effective use of face coverings is very significantly determined by human behaviour [high confidence]. Successful application of face coverings as a population scale measure requires, at minimum, clear and consistent messaging around where and why they should be worn, as well as how to choose and wear a face covering or mask [Reference 5].
49. Mandating the use of face coverings in appropriate situations is likely to increase usage [high confidence]. Usage has declined significantly in England since July 2021 when it ceased to be a legal requirement [Reference 17]. Increasing accessibility to face coverings has also been reported to increase uptake in different studies [Reference 46].
Interactions and hierarchy of measures
50. The epidemiological situation is still dynamic, and we have not yet reached a steady state. The effectiveness of measures is highly dependent upon the context in which they are introduced, and measures will often interact and have complementary effects that should be considered. Packages of measures are highly likely to be more effective than individual measures.
51. Reintroduction of measures is likely to present additional challenges and consideration should be given to minimising harms and disruption if this is necessary. SAGE have previously advised on the importance of positively framing the introduction of measures, ensuring equity, co-production, and providing adequate support for those affected [Reference 2].
52. Reintroduction of working from home guidance, for those who can, may have the largest impact on transmission out of the potential Plan B measures, however there are associated harms and unequal impacts that should be considered upon implementation. It is difficult to estimate the effectiveness of individual measures and they should not be viewed in isolation.
53. There are other measures that could be introduced to mitigate the need for Plan B or more stringent interventions, in addition to increasing vaccine and booster rollout and uptake. This could include encouraging wider use of rapid antigen testing in workplaces, the community, and ensuring people receive sufficient support (and are aware, in advance, that they can access support) to self-isolate when infected.
References
1. COVID-19 Response: Autumn and Winter Plan 2021. September 2021.
2. SAGE. Summary of the effectiveness and harms of different non-pharmaceutical interventions.. September 2020.
3. EMG, SPI-M, and SPI-B. Considerations in implementing long-term ‘baseline’ NPIs. April 2021.
4. SPI-B. Sustaining behaviours to reduce SARS-CoV-2 transmission. April 2021.
5. SPI-B. Behavioural considerations for maintaining or reintroducing behavioural interventions and introducing new measures in Autumn 2021 . October 2021, unpublished.
6. EMG and NERVTAG. Update on Transmission and Environmental and Behavioural Mitigation Strategies, including in the context of Delta, October 2021, unpublished.
7. EMG. Application of physical distancing and fabric face coverings in mitigating the B117 variant SARS-CoV-2 virus in public, workplace and community. January 2021.
8. Hayward, A and Hoskins, S. The relative importance of attending work, public transport, retail and other non-household activities on risk of adults acquiring COVID-19 outside the household during the second wave of COVID-19 infection in England and Wales. September 2021, unpublished.
9. JBC. Unpublished Analysis. 2021.
10. Wang, H., et al. Community prevalence and risk factors for SARS-CoV-2 infection in England during Winter 2020 to 2021 (REACT-1). Draft analysis, unpublished.
11. ONS. Analysis of populations in the UK by risk of testing positive for COVID-19, September 2021. 27 September 2021.
12. ONS. Coronavirus (COVID-19) Infection Survey: characteristics of people testing positive for COVID-19 in countries of the UK. 22 September 2021.
13. Ding, X, Brazel, D and Mills, M. Factors affecting adherence to non-pharmaceutical interventions for COVID-19 infections in the first year of the pandemic in the UK: Analysis of the repeated household Covid Infection Survey (CIS). BMJ Open. 2021.
14. EMG. COVID-19 risk by occupation and workplace. February 2021.
15. Hill, E M, et al. A network modelling approach to assess non-pharmaceutical disease controls in a worker population: An application to SARS-CoV-2. PLOS Computational Biology. 2021.
16. Block, P, et al. Social network-based distancing strategies to flatten the COVID-19 curve in a post-lockdown world. Nature Human Behaviour. 2020.
17. Jarvis, C, Gimma, A and Wong, K. Social contacts in the UK from the CoMix social contact survey. Report for survey week 77. 21 September 2021.
18. ONS. Coronavirus and homeworking in the UK: April 2020. July 2020.
19. ONS. Business and individual attitudes towards the future of homeworking, UK: April to May 2021. 14 June 2021.
21. Finnie, T., et al. Identifying factors contributing to persistent transmission using interpretable machine learning. Preparing for publication.
22. ONS. Coronavirus and self-isolation after testing positive in England: 5 July to 10 July 2021. 29 July 2021.
23. Fragaszy, E., et al. Effects of seasonal and pandemic influenza on health-related quality of life, work and school absence in England: Results from the Flu Watch cohort study. 2018.
24. Daniels, S, Wei, H and Han, Y. Risk factors associated with respiratory infectious disease-related presenteeism: a rapid review. 2021.
25. Quilty, B., et al. Effectiveness of symptomatic self-isolation in reducing onwards transmission of SARS-CoV-2. 28 April 2021.
26. SPI-M-O: Statement on daily contact testing. March 2021.
27. Modelling alternative options for care home asymptomatic staff testing to current PCR and LFD dual testing protocol in response to PCR testing capacity issues in July 2021 anticipated to continue for several weeks. SPI-M paper. 28 July 2021, unpublished.
28. Love, N K, Ready, D and Turner, C. The acceptability of testing contacts of confirmed COVID-19 cases using serial, self-administered lateral flow devices as an alternative to self-isolation. 26 March 2021.
29. Young, B C, Eyre, D W and Kendrick, S._ A cluster randomised trial of the impact of a policy of daily testing for contacts of COVID-19 cases on attendance and COVID-19 transmission in English secondary schools and colleges. 25 July 2021.
30. Denford, S, Towler, L and Ali, B. Feasibility and acceptability of daily testing at school as an alternative to self-isolation following close contact with a confirmed case of COVID-19: A qualitative analysis. 7 October 2021.
31. Liverpool Covid-SMART Community Testing Pilot. 17 June 2021.
32. Green, M A, García-Fiñana, M and Barr, B. Evaluating social and spatial inequalities of large scale rapid lateral flow SARS-CoV-2 antigen testing in COVID-19 management: An observational study of Liverpool, UK (November 2020 to January 2021). July 2021.
33. ICJU Unpublished Analysis. 2021.
34. Mills, M C and Rüttenauer, T. The impact of mandatory COVID-19 certificates on vaccine uptake: Synthetic Control Modelling of Six Countries. 2021.
35. NERVTAG. Immunity certification update. February 2021.
36. UKHSA. COVID-19 vaccine surveillance report; Week 40. 7 October 2021.
37. Eyre, D W, et al. The impact of SARS-CoV-2 vaccination on Alpha and Delta variant transmission. 29 September 2021.
38. PHE. Duration of protection of COVID-19 vaccines against clinical disease. 9 September 2021.
39. The Economist. How France tackled vaccine hesitancy. 18 September 2021.
40. SPI-B. Health status certification in relation to COVID-19, behavioural and social considerations. 9 December 2020.
41. Coleman, K K, et al. Viral Load of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Respiratory Aerosols Emitted by Patients With Coronavirus Disease 2019 (COVID-19) While Breathing, Talking, and Singing. Clinical Infectious Diseases. 6 August 2021.
42. Adenaiye, O O, et al. Infectious SARS-CoV-2 in Exhaled Aerosols and Efficacy of Masks During Early Mild Infection. Clinical Infectious Diseases. 14 September 2021.
43. Aydin, O, et al. Performance of fabrics for home-made masks against the spread of COVID-19 through droplets: A quantitative mechanistic study. Extreme Mechanics Letters. October 2020.
44. UKHSA. The role of face coverings in mitigating the transmission of SARS-CoV-2 virus: statement from the Respiratory Evidence Panel. 2021.
45. Sharma, S, Pinto, R and Saha, A. On secondary atomization and blockage of surrogate cough droplets in single-and multilayer face masks. Science advances. 5 March 2021.
46. Abaluck, J, et al. The Impact of Community Masking on COVID-19: A Cluster Randomized Trial in Bangladesh. Clinical Trials. 2 September 2021.
47. SAGE 94 minutes. 22 July 2021.
48. Lessler, J, et al. Household COVID-19 risk and in-person schooling. Science. 29 April 2021.
49. Gettings, J, et al. Mask use and ventilation improvements to reduce COVID-19 incidence in elementary schools—Georgia, November 16 to December 11, 2020. Morbidity and Mortality Weekly Report. 28 May 2021.
50. Sharma, A, Omidvarborna, H and Kumar, P. Efficacy of facemasks in mitigating respiratory exposure to submicron aerosols. Journal of hazardous materials. 15 January 2022.
51. Wang, C C, Prather, K A and Sznitman, J. Airborne transmission of respiratory viruses. Science. 27 August 2021.
52. Leung, N H, Chu, D K and Shiu, E Y. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature medicine. 3 April 2020.
53. Chiu, N C, et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: Retrospective national epidemiological surveillance study. Journal of Medical Internet Research. 20 August 2020.
54. Wong, S C, et al. Absence of nosocomial influenza and respiratory syncytial virus infection in the coronavirus disease 2019 (COVID-19) era: implication of universal masking in hospitals. Infection Control and Hospital Epidemiology. 17 August 2021.
Annex 1 – EMG Consensus statement on face coverings, 28 September 2021
This paper provides a short summary of the current knowledge around the effectiveness of face coverings and the characteristics of settings where face coverings are most likely to have the greatest impact. We have not been able to undertake a comprehensive review due to the tight timescales involved, so this paper draws on previous work alongside more recent studies. Face coverings and their effectiveness were covered in some detail in the EMG paper from 13th Jan [Annex reference 1], hence this paper summarises key points from the previous paper together with new evidence where available.
It is important to recognise that mitigation measures for COVID-19 must consider all modes of transmission and should be applied in combination. Transmission can potentially happen in any setting where people interact, and while some settings carry higher risks than others; simply applying a single measure in a setting will have a limited effect on transmission. Although this paper predominantly focuses on face coverings it is important to remember that their effectiveness will depend on the setting, other mitigations in place, the nature of interactions, and other factors.
The paper only considers face coverings for community settings that are designed to closely cover the nose and mouth (cloth face coverings, surgical masks and higher filtration masks (N95/FFP2) for sale to the public). It does not consider workplace PPE or medical grade masks for healthcare use. It also does not consider plastic face shields which are discussed in an earlier paper [Annex reference 1] and are recognised to have a limited impact on mitigating transmission.
Executive summary
The consensus is broadly in line with that presented before in previous EMG papers:
-
Face coverings are likely to reduce transmission through all routes by partially reducing emission of and/or exposure to the full range of aerosol and droplets that carry the virus, including those that deposit on surfaces (high confidence).
-
Face coverings are effective as a source control (reducing spread of virus from an infected individual) and to a lesser extent to provide protection to the wearer (high confidence).
-
The effectiveness of a face covering in protecting a susceptible individual from infection increases with the effectiveness of the material from which the face covering is made, the extent to which it excludes infected particles and the and closeness of the fit on the face. This is particularly important for reducing the exposure risks associated with the smallest aerosol particles. Face coverings provide greater protection when they cover both the nose and mouth (high confidence).
-
Face coverings worn as source control can reduce transmission at population level when worn by enough people. Their effectiveness as a source control depends on material quality and fit (including covering the nose and mouth), the proportion of people wearing face coverings and the frequency with which they wear them. The wider the use, the more likely it is that an infected person will be wearing a face covering (high confidence).
-
When used correctly, face coverings can reduce the risk of transmission when people are in close proximity or small spaces even for short durations of time (medium confidence)
-
Face coverings cannot compensate for poor ventilation but may further reduce risks of longer-range airborne transmission when people are in shared air for longer periods of time, and this effect may be more important in poorly ventilated spaces (low confidence).
-
Face coverings are likely to have benefits for the reduction of the transmission of other respiratory viruses (high confidence).
-
Effective use of face coverings is very significantly determined by human behaviour (high confidence). Successful application of face coverings as a population scale measure requires, at minimum, clear and consistent messaging around where and why they should be worn, as well as how to choose and wear a face covering or mask.
-
Mandating the use of face coverings in appropriate situations is likely to increase usage (high confidence).
Evidence summary
Does the latest scientific evidence (since the position set out for the SDR review) change the relative importance / impact of mitigations such as for face coverings, social distancing/work from home.
Recent evidence concerning transmission of the delta variant largely confirms previous information with regard to both transmission and mitigation measures; there is no evidence of any substantial changes in modes of transmission. However, the delta variant is more transmissible, which means infections by all modes of transmission may increase. The scientific consensus is that the risk of exposure to virus is greatest at close-range, but the relative contributions of close-range, long range airborne transmission, and fomites are likely to vary depending on the setting and behaviours and may be influenced by variants. Data to evidence this directly is very limited. There is a small amount of additional evidence from direct measurements of exhaled breath from COVID-19 patients to suggest that: viral emissions may be more likely to be in smaller aerosols than previously thought; there are higher viral emissions from people with the alpha variant compared to earlier variants (no data for delta); and that surgical masks and cloth face coverings do reduce virus containing emissions from people who are infected [Annex reference 2],[Annex reference 3]. Data showed that surgical face masks or cloth face coverings worn by participants reduced fine aerosol <5-micron diameter by 48% (95% confidence interval [CI], 3 to 72%) and coarse >5 micron by 77% (95% CI, 51 to 89%) [Annex reference 3]. Previous studies have also shown high effectiveness >98% for large droplets (>100 micron) for surgical masks and multilayer cloth masks [Annex reference 4]. There is a greater confidence that face coverings reduce emission and inhalation of large droplets than fine aerosols.
A recent UKHSA respiratory evidence review (May 2021, papers published prior to the delta variant) [Annex reference 5] suggests with high confidence that: all types of face coverings are to some extent effective at reducing transmission; good quality cloth face coverings can have a similar filtration efficiency to surgical masks; face coverings should be well fitting and over the nose and mouth to be effective. The report indicates that fitted respiratory protective equipment (N95 [footnote 6]) may be more effective than surgical masks at reducing risk of infection to the mask wearer in healthcare settings, but that evidence is limited. The need to provide improved public health messaging around face coverings and training where they are used as personal protective equipment is highlighted by the report.
Does the advice on relative importance / impact of different measures change in light of the potential to control flu / other respiratory illnesses in addition to Covid considerations.
We have not been able to carry out a detailed review of measures to control other respiratory illnesses given the tight deadline, however a recent review indicates that a number of respiratory viruses including influenza, rhinovirus, RSV and seasonal coronaviruses are also likely to be transmitted through respiratory aerosols and droplets in a similar way to COVID-19 [Annex reference 6] and a number of studies show the potential impact of face coverings on mitigating transmission [Annex reference 7] - [Annex reference 10] (UKHSA surveillance suggests that influenza cases are currently very low but some other respiratory infections have risen over the summer, and there is an increase in rhinovirus in school age and younger children. It is not clear how these infections will behave over the next few months, but it is a reasonable assumption that as people are mixing more, cases of other respiratory viruses are likely to increase. Public messaging to highlight that the measures to control COVID-19 are also likely to control other infections is likely to be a beneficial public message, and if it leads to positive changes in behaviour could reduce some of the expected pressure from respiratory infections on the NHS during the winter months.
Are face coverings likely to have greater importance without social distancing measures in place - as people mix more closely.
Exposure to the SARS-CoV-2 virus is likely to be greatest when people are close to an infected person. As previously detailed, aerosols and droplets in exhaled breath are more concentrated in the immediate respiratory plume close to a source and are more readily inhaled or can deposit on mucous membranes as larger particles will not have had time to deposit [Annex reference 1]. While surfaces are considered a lower risk for transmission than aerosols or droplets, surfaces in close proximity to an infected person are more likely to be contaminated than those further away. Mitigation measures that can impact on close range exposure are distancing, face coverings, face shields and screens. Screens may have an effect on large droplet exposure when people are face to face, but there are many environments where people are in close proximity and it is not practical to install a screen, and there are studies that show screens do not block smaller airborne particles which may be suspended for some time and move more freely in the space [Annex reference 11]. Face shields may also have an impact on protecting against large droplet exposure, including to the eyes, but have limited effect at protecting against aerosols or as a source control. With the removal of social distancing measures, face coverings are likely to be the only practical measure that can be used flexibly to mitigate close range exposure in many settings, and hence have become more important.
How effective can we expect face coverings to be in a poorly ventilated environment - how much can they compensate for poor ventilation.
The interplay/relative contribution of close-range transmission risk, which may be mitigated through face coverings, and the risk associated with long range transmission, which may be mitigated by ventilation (to increase air change) and face coverings (to reduce the volume of airborne particles containing virus) is uncertain. In spaces with people in close proximity, face coverings remain an important mitigation.
Face coverings do not compensate for poor ventilation and should not be a reason to not ventilate a space, but may be beneficial for further reducing airborne transmission risks (when people are >2m apart). The relative impact of both face coverings and ventilation will depend on multiple factors including the duration of time spent in a space, the number of people present in the time period of interest, the volume of the space, the activities carried out in the space and the infectiousness of the source. In large spaces over a short period of time, the long-range airborne risk may be low even if the ventilation is poor. However, in small spaces (e.g. lifts, toilets, vehicles) even a short duration exposure could be high risk even at >2m distancing as the small volume of the space results in a higher concentration of virus in air for the same emission rate.
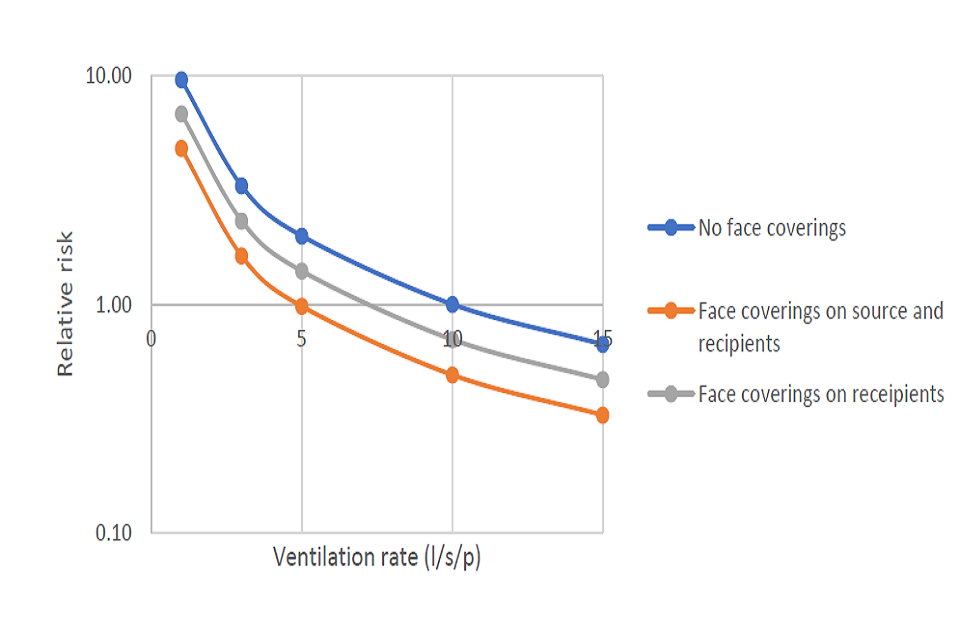
To compare the relative impact of face coverings and ventilation in a space with a consistent longer occupancy duration (e.g. office, classroom), the figure below uses the Wells-Riley risk model to compare relative risks over a 4 hour period in a 160m3 space with 30 people, assuming steady state conditions. It is assumed that the face coverings reduce both source viral emissions and susceptible inhalation by 30% which is a realistic but relatively conservative estimate. With a high proportion of wearing that covers both source and recipients, the risk with ventilation of 5 l/s/p is comparable to that at 10 l/s/p with no face coverings. It is important to remember that this is an idealised model that doesn’t consider the variability that happens in real spaces, however it gives an indication of the potential risk reduction but only for long range airborne transmission. Higher performing face coverings and greater numbers of wearers would reduce the risk further. They would also be likely to impact on the close range and fomite transmission routes as discussed above depending on the type of interactions in the space.
Should face coverings be required to conform to certain standards to help ensure effectiveness.
There is good evidence that high quality face covering material (N95 standard, surgical face mask material, three layer tight weave fabric) is much more effective at blocking aerosols and droplets than single layer fabric or material with a looser weave [Annex reference 1]. A study of multilayer masks also points to the benefits in reducing fragmentation of larger droplets into smaller ones, suggesting three layers of fabric are best [Annex reference 12]. There is also good evidence that a face mask or face covering that fits closely and tightly to the face improves effectiveness by reducing leakage around the sides of the mask that can enable ingress or egress of virus particles. As previously highlighted there may be a benefit in a minimum standard for commercially available face coverings [Annex reference 1]. However performance in practice depends very heavily on individual behaviour; even a well-designed face covering is ineffective if it does not cover the nose and mouth or is only worn for a brief portion of the period of exposure. As highlighted previously it is recommended to change face coverings every 4 hours for hygiene and comfort [Annex reference 1]. A recent study considered the trade-off between particle capture and breathability of different types of face covering materials indicated that the maximum duration of wearing for optimal effectiveness and comfort is likely to be 3.2–9.5 h (N95/FFP2), 2.6–7.3 h (surgical style masks) and 4.0–8.8 h (cloth face coverings) [Annex reference 13]. In terms of both source control and personal protection a face covering manufactured to N95/FFP2 material standards will provide the greatest benefit relative to other kinds of face covering material providing it is worn to cover the nose and mouth and fits closely to the face.; those with valves may provide less benefit as a source control because of the risk that unfiltered air is emitted by the wearer. Recent evidence from an RCT in Bangladesh suggests that surgical masks are usually more effective than cloth face coverings, although laboratory data indicates that the fit and design of both types mean that there may not be a substantial difference in practice [Annex reference 14]. Data from the human challenge study suggests virus can be shed from the nose and hence covering the nose and mouth is important for face coverings to be effective [Annex reference 15].
Can any quantification be given to the effectiveness of face coverings overall as a control measure.
The population level benefits from face coverings will depend on the proportion of people wearing them and the frequency with and extent to which they are worn, among other factors. There is a double benefit to face coverings due to them providing both source control and personal protection for the wearer. However, this is only fully realised when infected people wear face coverings, which provides protection for everyone in the space, not just those wearing face coverings for personal protection. The more people who wear face coverings, the lower the likelihood that an infected person, who may be asymptomatic, will pass the virus on to others. The more settings they are worn in, the greater the chance that this benefit will be multiplied across different spaces.
A small number of studies have attempted to quantify effectiveness through population scale data on infection rates and mask mandates; this ranges from 6-15%, and possibly up to 45% as stated previously [Annex reference 1]. A recent RCT in Bangladesh [Annex reference 14] suggested that strategies to promote effective wearing of cloth face coverings and surgical masks increased the proper use of face coverings from 13.3% to 43.3%, which resulted in a reduction in symptomatic infection of 9.3%. Settings where face covering wearing was observed in the study included inside mosques and at high footfall outdoor settings, but it is not known in how many other indoor spaces face coverings were worn. Two earlier studies from the USA considering large scale data suggest that requiring staff and/or pupils to wear face coverings in schools was associated with lower incidence of COVID-19 [Annex reference 16], [Annex reference 17]. Two further CDC MMWR reports published in Sept 2021 also suggest that face covering requirements were associated with a lower likelihood of an outbreak [Annex reference 18] and lower rates of infection [Annex reference 19]. Modelling studies can give some insight into the effectiveness of face coverings, although it is important to note that these will be influenced by the assumptions made about the modelling. Unpublished data from modelling of exposure to virus on public transport suggests that increased wearing of face coverings can reduce both the median exposure to virus in the air and the low frequency but high dose exposures that may occur when people are in close proximity.
The population scale benefits of face coverings can only be realised if they are worn correctly and by sufficient people in a setting, and this depends very significantly on human behaviour. Evidence suggests that wearing of face coverings in public spaces is influenced significantly both by national level requirements and public messaging. YouGov and ONS data indicate that much higher numbers of people reported wearing face coverings during periods when they were legally mandated. Since July 2021 when face coverings were encouraged but not mandated there has been a steady decline in both reported and observed wearing. Self-reported data often shows a much higher usage than observed data and should be treated with caution; for example data from August 2021 shows 79 % self-report wearing a face covering while travelling, whereas evidence based on CCTV footage of weekend journeys showed that only 39 % of people did in fact wear a covering while travelling [Annex reference 20]. Unpublished data from the Events Research Programme across 21 events, based on CCTV footage, showed wearing of face coverings was on average 58% when mandated and 14% when not mandated. Data from national rail surveys suggest average wearing has fallen from around 90% in June to around 60% at 22nd Sept, with variability across different routes. There is evidence that provision of free face coverings can increase wearing [Annex reference 15], [Annex reference 21]. The effectiveness of messaging from policy makers may be diminished if those policy makers do not themselves model the behaviour being advised, such as wearing face coverings in crowded spaces [Annex reference 22].
Are there specific settings for which wearing face coverings would be highly recommended (beyond general guidance on enclosed, crowded and close-contact settings).
There are a number of factors which influence where face coverings are likely to have a significant impact on transmission. This can be used to enable the identification of specific settings and occasions where they can be recommended. The more of these factors are present, the more likely that face coverings will have even more benefit. The key factors include:
-
Prevalence of virus – face coverings are more likely to be beneficial during times when prevalence of virus in the community is high, as there is a greater chance that an infected person will be present in any particular situation
-
Proximity of people to others – face coverings are likely to one of the most effective means of mitigating close proximity contact including unintended proximity (e.g. public transport, queuing, crowded buildings) as well as deliberate proximity (e.g provision of personal care or health care). Where people are in close proximity for extended periods of time higher quality and better fitting face coverings are likely to provide greater mitigation, especially if there is a high chance that the person may be interacting with a positive individual
-
Small spaces – face coverings are likely to be more beneficial in locations where there is a small air volume, even if people are able to maintain physical distance, as virus in the air may be more concentrated. This includes spaces such as lifts, toilets, changing rooms and vehicles.
-
When people have respiratory symptoms – even if they have tested negative for SARS-CoV-2, wearing of face coverings could significantly limit the dispersal of pathogens into the environment, including other viruses
-
Indoor spaces with high numbers of people or high throughput, which increase the probability that there will be interaction with an infected person, especially during times of high prevalence
-
Poorly ventilated indoor spaces – in shared indoor spaces where people are together for longer periods of time, face coverings can reduce the overall virus concentration in air (source control) and the exposure to any virus. This will have a greater impact where people are close together and spaces are small-medium sized; there is likely to be less effect in very large spaces
-
Spaces where there are likely to be higher respiratory emissions – where singing, continuous talking and high aerobic activity take place the risk of exposure increases. The greatest risk is where infected individuals are doing these activities, and the greatest benefit will be achieved where it is feasible for those people to wear face coverings. Published evidence suggests that these people are most likely to be super shedders. However, if this is impractical, then face coverings worn by those observing the activities may reduce exposure, particularly if people are close together and/or in a poorly ventilated space.
-
Spaces where there are multiple commonly touched surfaces – wearing of face coverings by infected people can reduce the likelihood of contamination of the environment.
References
2. Kristen K Coleman, et al Viral Load of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Respiratory Aerosols Emitted by Patients With Coronavirus Disease 2019 (COVID-19) While Breathing, Talking, and Singing, Clinical Infectious Diseases, 2021;, ciab691, https://doi.org/10.1093/cid/ciab691
3. Oluwasanmi O Adenaiye, et al Infectious SARS-CoV-2 in Exhaled Aerosols and Efficacy of Masks During Early Mild Infection, Clinical Infectious Diseases, 2021;, ciab797, https://doi.org/10.1093/cid/ciab797
4. Onur Aydin et al Performance of fabrics for home-made masks against the spread of COVID-19 through droplets: A quantitative mechanistic study, Extreme Mechanics Letters, 40: 100924, 2020 https://doi.org/10.1016/j.eml.2020.100924
5. UKHSA The role of face coverings in mitigating the transmission of SARS-CoV-2 virus: statement from the Respiratory Evidence Panel, July 2021
6. Chia C Wang et al. Airborne transmission of respiratory viruses, Science, 373: 6558, 2021, DOI: 10.1126/science.abd9149
7. Nancy H.L. Leung et al. Respiratory virus shedding in exhaled breath and efficacy of face masks, Nature Medicine: 26: 276-680, 2020 doi.org/10.1038/s41591-020-0843-2
8. Chiu N et al. Impact of Wearing Masks, Hand Hygiene, and Social Distancing on Influenza, Enterovirus, and All-Cause Pneumonia During the Coronavirus Pandemic: Retrospective National Epidemiological Surveillance Study. J Med Internet Res 2020;22(8):e21257doi: 10.2196/21257
9. Wong, S et al (2021). Absence of nosocomial influenza and respiratory syncytial virus infection in the coronavirus disease 2019 (COVID-19) era: Implication of universal masking in hospitals. Infection Control & Hospital Epidemiology, 42(2), 218-221. doi:10.1017/ice.2020.425
10. Long, Y, Hu, T, Liu, L, et al. Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis. J Evid Based Med. 2020; 13: 93– 101. https://doi.org/10.1111/jebm.12381
11. EMG: Role of screens and barriers in mitigating COVID-19 transmission, 1 July 2021. https://doi.org/10.1126/sciadv.abf0452
12. Sharma S et al. On secondary atomization and blockage of surrogate cough droplets in single- and multilayer face masks, Science Advances: 7 (10): 2021 DOI: 10.1126/sciadv.abf0452
13. Sharma A. et al Efficacy of facemasks in mitigating respiratory exposure to submicron aerosols, J. Hazard. Mat. 422: 126783: 2022 doi.org/10.1016/j.jhazmat.2021.126783
14. Abaluck J. et al The Impact of Community Masking on COVID-19: A Cluster-Randomized Trial in Bangladesh
15. Nervtag update on human challenge
16. Lessler J. Et al Household COVID-19 risk and in-person schooling, Science: 372: 6546, 2021 DOI: 10.1126/science.abh2939
17. Gettings J, Czarnik M, Morris E, et al. Mask Use and Ventilation Improvements to Reduce COVID-19 Incidence in Elementary Schools — Georgia, November 16–December 11, 2020. MMWR Morb Mortal Wkly Rep 2021;70:779–784. DOI: http://dx.doi.org/10.15585/mmwr.mm7021e1
18. Jehn M, et al. Association Between K–12 School Mask Policies and School-Associated COVID-19 Outbreaks — Maricopa and Pima Counties, Arizona, July–August 2021. MMWR Morb Mortal Wkly Rep. ePub: 24 Sept 2021. DOI: http://dx.doi.org/10.15585/mmwr.mm7039e1
19. Budzyn SE, Panaggio MJ, Parks SE, et al. Pediatric COVID-19 Cases in Counties With and Without School Mask Requirements — United States, July 1–September 4, 2021. MMWR Morb Mortal Wkly Rep. ePub: 24 September 2021. DOI: http://dx.doi.org/10.15585/mmwr.mm7039e3
20. Behavioural Sitrep 23.09.21 Cabinet Office
21. Fretheim, A et al. The Effectiveness of Free Face Mask Distribution on Use of Face Masks. A Cluster Randomised Trial in Stovner District of Oslo, Norway. Int. J. Environ. Res. Public Health 2021, 18, 8971. https://doi.org/10.3390/ijerph18178971
22. Fancourt D, Steptoe A, Wright L. The Cummings effect: politics, trust, and behaviours during the COVID-19 pandemic. The Lancet. 2020 Aug 15;396(10249):464-5.
Footnotes
-
Rt = Effective reproduction number – the average number of secondary cases per infectious case in a population of susceptible and non-susceptible individuals. ↩
-
Real-time Assessment of Community Transmission (REACT) Study ↩
-
The PROTECT COVID-19 National Core Study on transmission and environment ↩
-
Flu Watch cohort included cases that neither consulted for care nor met the symptom definition of an influenza-like illness. ↩
-
Infectiousness among working age adults varies across individuals and by viral load at time of testing, vaccination status, time since vaccination, and symptom status. ↩
-
Available evidence largely comes from previous studies in countries which use N95 masks, which are equivalent to FFP2 in the UK. ↩
