Laboratory confirmed cases of measles, rubella and mumps in England: April to June 2022
Updated 28 February 2023
Applies to England
Measles, rubella and mumps are notifiable diseases and healthcare professionals are legally required to inform their local health protection team (HPT) of all suspected cases. National enhanced surveillance including oral fluid (OF) testing of all suspected cases is provided through the Virus Reference Department (VRD) at Colindale to support and monitor progress towards World Health Organization (WHO) measles and rubella elimination targets.
Two WHO indicators are of prime importance for measuring the performance of national measles and rubella surveillance systems. These are:
- The rate of laboratory investigations (at least 80% of suspected cases).
- The annual rate of discarded cases (at least 2 per 100,000 population).
In order to achieve these targets, the focus of the UK Health Security Agency (UKHSA) is on ensuring that all suspected cases are appropriately tested. IgM serology testing and oral fluid testing are the only tests considered adequate by WHO for confirming – and, importantly, discarding – suspected measles and rubella cases. Recent infection is confirmed by measuring the presence of IgM antibodies or detecting viral RNA (by PCR) in these samples.
Samples that have been confirmed positive for measles or rubella are further sequenced and entered on the WHO global Measles Nucleotide Surveillance (MeaNS) or the Rubella Nucleotide Surveillance (RubeNS) system, respectively, which are hosted at the National Reference Laboratory. Genotyping and further characterisation of measles and rubella is used to support investigation of transmission pathways and sources of infection.
Data presented here is for the second quarter of 2022 (April to June). Analyses are done by date of onset of rash or symptoms and regional breakdown figures relate to Government Office Regions.
Historical annual and quarterly measles, rubella and mumps epidemiological data is available from 2013 onwards:
Results from all samples tested at Colindale are reported on the MOLIS/LIMS system and reported back to the patient’s GP and local HPT.
Table 1. Total suspected cases of measles, rubella and mumps reported to health protection teams (HPTs) and proportion tested through different routes: weeks 14 to 26 of 2022
| Notified as | Number of suspected cases* | Number (%) tested by OF. [Target: 80% (measles and rubella only)] | Other samples received in Virus Reference Laboratory | Number of samples IgM positive or viral detection | Discard rate based on negative tests per 100,000 population (all samples)** |
|---|---|---|---|---|---|
| Measles | 351 | 188 (54%) | 28 | 23 | 0.34 |
| Rubella | 92 | 22 (24%) | 40 | 0 | 0.04 |
| Mumps | 1,422 | 665 (47%) | 51 | 7 | – |
| Rash fever surveillance¥ | 9,393 | – ¥¥ | – | – | – |
The cases are broken down by:
- proportion tested by OF
- other samples received from notified cases
- cases confirmed (all tests) nationally at the VRD, and at local NHS hospitals and private laboratories
- discard rate (measles and rubella only)
*This represents all cases reported to HPTs in England, that is, possible, probable, confirmed and discarded cases on HPZone.
**The rate of suspected measles or rubella cases investigated and discarded as non-measles or non-rubella using laboratory testing in a proficient laboratory. The annual discard rate target set by WHO is 2 cases per 100,000 population. We present quarterly rates here with an equivalent target of 0.5 per 100,000 population.
¥Includes samples received through the UKHSA rash fever surveillance.
¥¥This quarter some rash fever samples may have been received but not tested due to a laboratory supply chain issue.
Measles
In the period between April and June 2022, 23 laboratory confirmed case of measles were reported in England compared to 1 case reported in the previous quarter (Figure 1). All of these cases had an onset date from late May onwards with 4 imported cases who had recently travelled to Pakistan, United Arab Emirates and Somalia that led to at least 6 import-related cases. Over half of the detected cases were in London, with small clusters linked in a nursery, a school and some healthcare setting exposures.
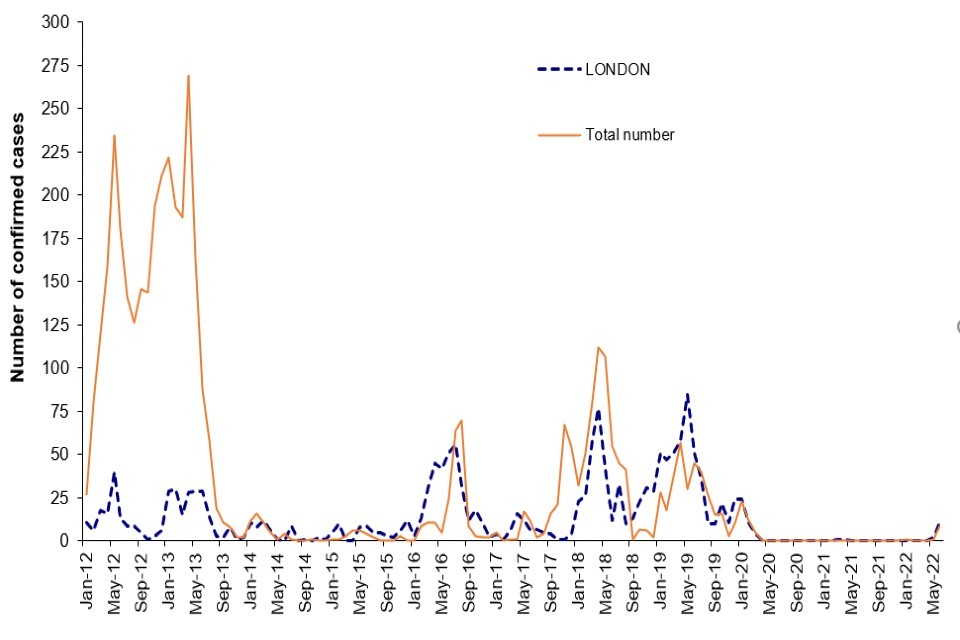
Figure 1. Laboratory confirmed cases of measles by month of onset of rash or symptoms reported, London and England: January 2012 to June 2022
Over 90% (21 out of 23) of the cases this quarter were in children under the age of 10. Of these:
- 6 cases (26%) were infants under the age of 1
- 7 cases (30%) were aged 1 to 4 years
- 7 cases (30%) were aged 5 to 9 years
- 1 case was 10 to 14 years old
All these cases were unvaccinated.
All suspected cases of measles and rubella should be reported promptly to HPTs, a risk assessment conducted, and an OF kit sent for confirmatory testing even if local diagnostic testing is underway. This quarter, an OF sample was returned for 54% of all suspected measles cases reported in England, well below the 80% WHO target (Table 1).
Mumps
In England, there were only 7 laboratory confirmed mumps infections in the period between April and June 2022 compared to 10 between January and March 2022. Most (6 out of 7) of the cases this quarter were in adults above the age of 18 years.

Figure 2. Laboratory confirmed cases of mumps by quarter, England: 2012 to 2022
Rubella
There have been no new laboratory confirmed cases of rubella reported in the UK since 2019.
