Listeriosis in England and Wales: summary for 2020
Updated 8 May 2025
Main points for 2020
This report summarises the number, demographics and clinical outcomes of confirmed cases of listeriosis in England and Wales in 2020:
A total 124 cases of listeriosis were reported in England and Wales.
Incidence rates of listeriosis were highest in people aged 80 years and over.
Overall, the crude incidence of listeriosis was lower in men than women, but reported cases among men aged 60 to 69 were 4 times higher than in women aged 60 to 69.
Pregnancy associated infections accounted for a fifth of all reported cases and, a 34.8% of pregnancy-associated cases resulted in stillbirth or miscarriage.
Among non-pregnancy associated cases of listeriosis, death was reported for 29 cases (29.3%), of whom 17 (17.2%) were known to have listeriosis recorded as a cause of death on the death certificate.
Incidence of listeriosis varied geographically, with the lowest incidence in the North West (0.15 per 100,000 population) and the highest in the East Midlands (0.27 per 100,0000 population).
There were 2 listeriosis outbreaks investigated in England, including a national outbreak associated with smoked salmon.
Background
Listeriosis is a foodborne disease caused by the bacterium Listeria monocytogenes. These bacteria are widely distributed in the environment and infection usually occurs after consumption of contaminated raw, chilled, or ready-to-eat foods, and can cause sporadic infection and outbreaks of disease. People with listeriosis have been reported to develop symptoms between 1 to 70 days after consuming food contaminated with Listeria monocytogenes.
Compared to other foodborne pathogens, infections in humans are relatively rare, with 2,621 confirmed cases of listeriosis reported across 28 EU member states in 2019, and a median of 160 cases in England and Wales each year (2010 to 2019). However, listeriosis can cause severe clinical outcomes in vulnerable groups, including those aged over 60 years, pregnant women and their unborn or newborn babies, and people with impaired immunity. In these groups, listeriosis can present as infection of the bloodstream or brain. Due to the severity of infection and high case fatality rate, listeriosis is an important public health concern.
National surveillance of listeriosis in England and Wales has been undertaken since 1992. This report summarises the number, demographics and clinical outcomes of confirmed cases of listeriosis in England and Wales reported in 2020.
Methods
National surveillance of listeriosis in England and Wales is coordinated by the Gastrointestinal Infections and Food Safety (One Health) Division (GIFSOH) at UK Health Security Agency (UKHSA) and involves the collation of routinely collected epidemiological, clinical and microbiological data for cases of listeriosis.
New cases are reported to the surveillance system by local clinical laboratories, health protection teams and by the referral of L. monocytogenes isolates to the Gastrointestinal Bacteria Reference Unit (GBRU) for whole genome sequencing (WGS).
Demographic and food history data are collected via a standardised questionnaire (trawling questionnaire) administered to the case or a proxy via health protection teams or the local authority. Clinical data are collected from clinical microbiologists at the frontline diagnostic laboratories via a second separate questionnaire (clinical questionnaire).
The WGS derived analysis, combined with clinical and epidemiological data from standardised food and clinical questionnaires, are used to detect clusters of genomically and epidemiologically linked cases and inform outbreak investigations.
Case definitions
For reporting, a confirmed case of listeriosis is defined as:
- a person with a clinically compatible illness
and
- isolation of Listeria monocytogenes (or detection of nucleic acid) from a normally sterile site
or
- isolation of Listeria monocytogenes (or detection of nucleic acid) from a normally non-sterile site from a foetus, stillborn, newborn, placenta, foetal tissue or from the mother following birth
Clinical criteria
In adults, invasive disease caused by Listeria monocytogenes (listeriosis) manifests most commonly as meningoencephalitis or septicaemia.
Invasive listeriosis principally affects high risk groups including:
- people aged over 60 years
- people with malignancies (especially of the blood)
- kidney disease
- liver disease
- diabetes
- alcoholism
- patients on immunocompromising treatment
- pregnant women and their unborn or newborn infants
Symptoms are related to sepsis and include fever, confusion and collapse. Infection during pregnancy may result in foetal loss through miscarriage or stillbirth, neonatal meningitis or bacteraemia. Neonatal infection can range from mild illness to neonatal death, usually within 10 days of delivery.
Cases are further sub-classified as pregnancy-associated or non-pregnancy cases.
Table 1: Sub-classification of confirmed listeriosis cases
| Pregnancy associated case | Non-pregnancy case |
|---|---|
| Listeria illness in a pregnant patient and neonatal patients aged 28 days or less. | Listeria illness in a patient aged over 28 days. |
| A mother-baby pair is considered a single case. |
Counts and rates
Data presented relate to confirmed cases reported to the national enhanced surveillance system for Listeria monocytogenes during the period 2011 to 2020.
Population and deaths data were sourced from the Office for National Statistics (ONS). Mid-year 2020 population estimates for England and Wales were used to provide denominators for the calculation of incidence rates. All rates are calculated as per 100,000 population.
National surveillance data for listeriosis
Annual cases of listeriosis
In 2020, 124 cases of listeriosis were reported in England and Wales (Figure 1), representing an 22.0% decline in reported cases compared to the previous 5 year median (n=159, 2015 to 2019). The crude incidence of listeriosis in 2020 was 0.21 cases per 100,000 population (95% CI: 0.17 to 0.25), compared to a crude incidence of 0.24 cases per 100,000 in the previous year (95% CI: 0.20 to 0.29).
Figure 1: Annual cases and crude incidence rate of listeriosis reported in England and Wales (2011 to 2020)
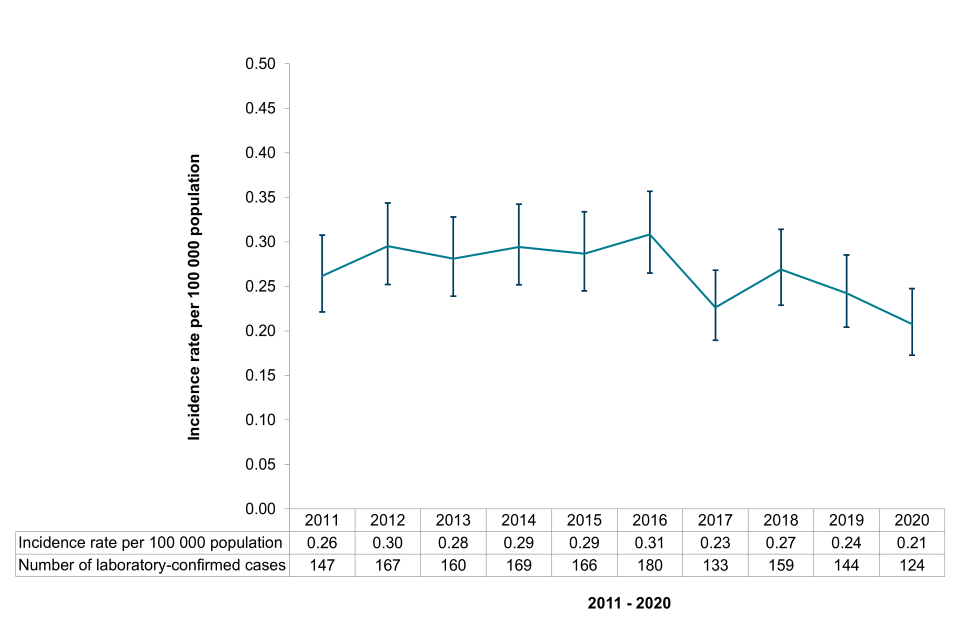
Figure 1. Annual cases and crude incidence rate of listeriosis reported in England and Wales, 2011 – 2020
Text alternative for figure 1
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Incidence rate per 100,000 population | 0.26 | 0.30 | 0.28 | 0.29 | 0.29 | 0.31 | 0.23 | 0.27 | 0.24 | 0.21 |
| Number of laboratory-confirmed cases | 147 | 167 | 160 | 169 | 166 | 180 | 133 | 159 | 144 | 124 |
Age and sex distribution of cases
Incidence of listeriosis varied by age group and sex, with age-specific incidence rates highest in people aged 80 years and over (Figure 2). Overall, the crude incidence of listeriosis was lower in males than females (Table 2, IRR: 0.79, 95% CI: 0.54 to 1.14), but higher in males aged 60 to 69 compared to females aged 60 to 69 (Figure 2, IRR: 4.21, 95% CI: 1.14 to 23.23). Of the 21 cases in the 10 to 19, 20 to 29 and 30 to 39 age groups, 19 were female, of which 16 cases were associated with pregnancy (range: aged 19 to 39 years).
Table 2: Sex-specific incidence rates of listeriosis reported in England and Wales, 2020
| Gender | Reported cases | Incidence rate | 95% Confidence Interval |
|---|---|---|---|
| Male | 54 | 0.18 | 0.14 to 0.24 |
| Female | 70 | 0.23 | 0.18 to 0.29 |
Figure 2: Age-specific incidence of listeriosis in England and Wales grouped by sex (2020)
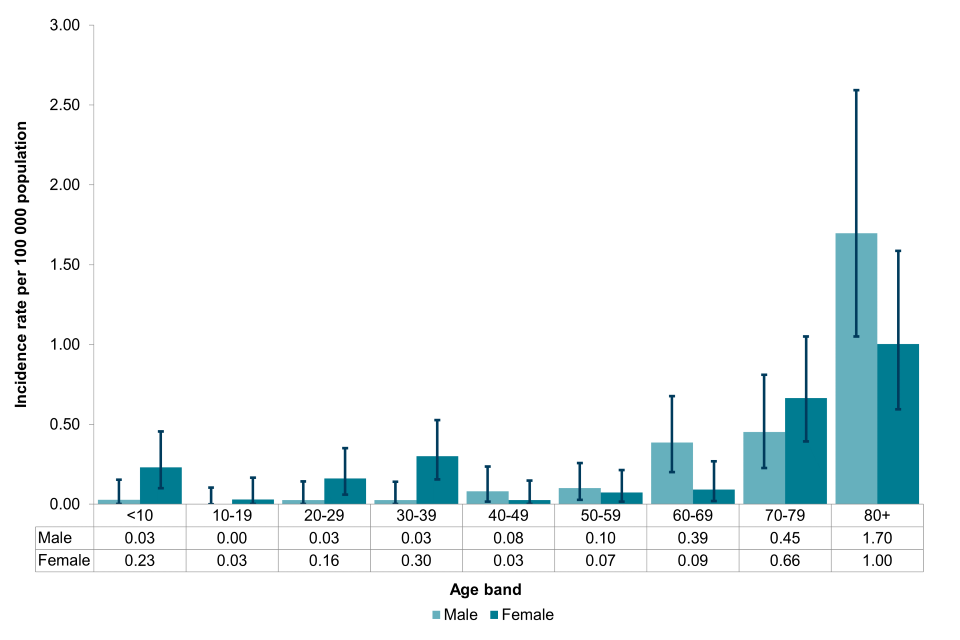
A bar chart depicting the incidence rate of listeriosis per 100,000 population, by age and sex.
Text alternative for figure 2
| <10 | 10 to 19 | 20 to 29 | 30 to 39 | 40 to 49 | 50 to 59 | 60 to 69 | 70 to 79 | 80 and over | |
|---|---|---|---|---|---|---|---|---|---|
| Male | 0.03 | 0.00 | 0.03 | 0.03 | 0.08 | 0.10 | 0.39 | 0.45 | 1.70 |
| Female | 0.23 | 0.03 | 0.16 | 0.30 | 0.03 | 0.07 | 0.09 | 0.66 | 1.00 |
Pregnancy associated cases
In 2020, a fifth of cases were associated with pregnancy (n=25, 20.2%), which was higher than previous years (10.1% to 19.5%, 2010 to 2019).
Amongst pregnancy associated cases, where known, 65.2% of pregnancies resulted in live births and 34.8% resulted in stillbirth or miscarriage (Figure 3).
Figure 3: Pregnancy associated cases of listeriosis in England and Wales (2020)
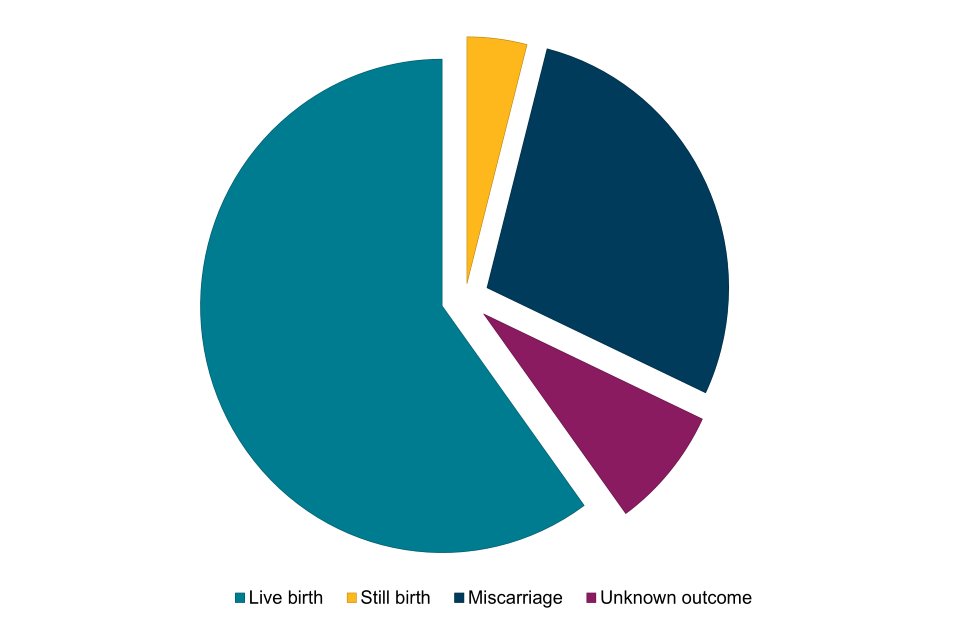
A pie chart depicting the outcomes of pregnancy associated cases of listeriosis.
Mortality rate
In 2020, there were 29 deaths among 99 non-pregnancy cases reported to surveillance (29.3%), compared to the previous five-year median (n=45, 26.0% to 45.4%, 2015 to 2019).
Of the 29 deaths, 17 were known to have a clinical manifestation of invasive L. monocytogenes infection recorded as a cause of death. This represented a case fatality rate of 17.2%, compared to 12.8% in the previous year.
Regional distribution of cases
The incidence rate of listeriosis varied geographically (Table 3; Figure 4). In England, East Midlands had the highest incidence rate of 0.27 cases per 100,000 population whilst the North West had the lowest incidence rate of 0.15 cases per 100,000 population. In Wales, the incidence rate was 0.25 cases per 100,000 population.
Table 3: Regional incidence of listeriosis reported in England and Wales, 2020
| Region | Cases | Incidence rate | 95% Confidence Interval |
|---|---|---|---|
| East Midlands | 13 | 0.27 | 0.14 to 0.46 |
| East of England | 11 | 0.18 | 0.09 to 0.31 |
| London | 21 | 0.23 | 0.14 to 0.36 |
| North East | 6 | 0.22 | 0.08 to 0.49 |
| North West | 11 | 0.15 | 0.07 to 0.27 |
| South East | 19 | 0.21 | 0.12 to 0.32 |
| South West | 14 | 0.25 | 0.14 to 0.42 |
| West Midlands | 9 | 0.15 | 0.07 to 0.29 |
| Yorkshire and The Humber | 12 | 0.22 | 0.11 to 0.38 |
| Wales | 8 | 0.25 | 0.11 to 0.50 |
Figure 4: Incidence rates of reported listeriosis cases in England and Wales, by region (2020)
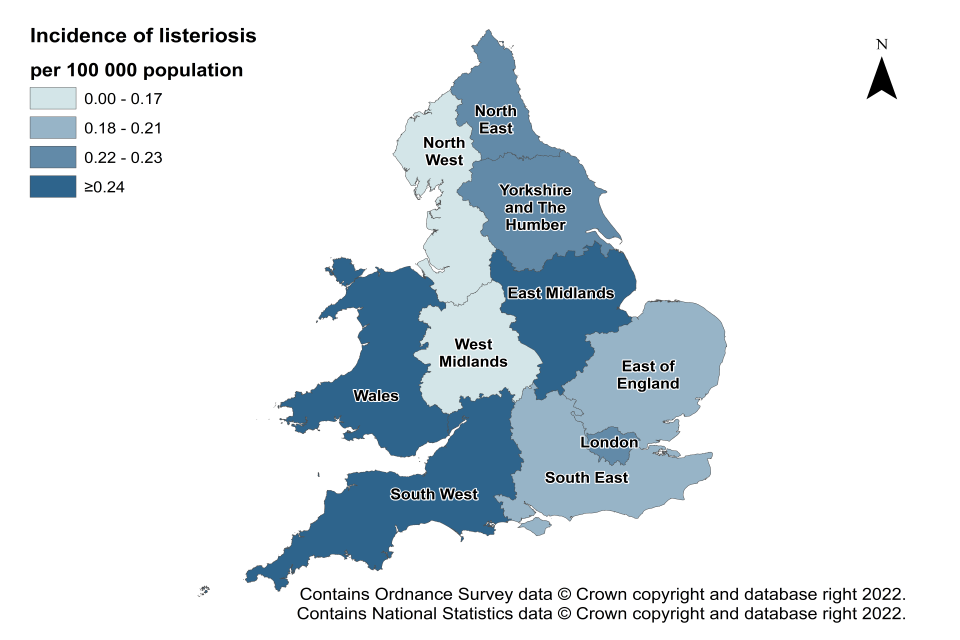
A map depicting the 9 UKHSA regions of England, and Wales, shaded according to the incidence of listeriosis per 100,000 population.
Seasonality
October was the peak month for listeriosis reporting in 2020, with no outbreak activity influencing the peak. In 2018, case numbers peaked in July and in 2019 case numbers peaked in May, with one outbreak influencing the peak. Comparison with the seasonal trend in 2020 should be made with caution, as the low number of reported listeriosis cases in 2020 complicates the interpretation of the trend and any other potential influences during this period.
Figure 5: Seasonal trend of reported listeriosis cases in England and Wales (2018 to 2020)

A line graph depicting the seasonal trend of listeriosis reports to national surveillance.
Incidents of listeriosis
There were 2 outbreaks (comprising 2 or more linked cases) of listeriosis investigated in England in 2020 (Table 4). The source of the outbreaks were prepacked sandwiches served in hospitals and smoked salmon, both considered to be high-risk foods for listeriosis in vulnerable groups.
Additionally, 1 incident was investigated involving a sporadic case reported in 2020 that was microbiologically linked to food or a food environment by the detection of the same strain (≤5 SNPs) of L. monocytogenes by whole genome sequencing.
Table 4: Outbreaks of listeriosis in England investigated in 2020
| Outbreak | Clinical cases | Time-frame | Region | Source of contamination |
|---|---|---|---|---|
| 1 | 2 | 2018 to 2020 | England | Prepacked sandwiches served in hospitals |
| 2 | 4 | 2020 | England | Smoked salmon |
Time-frame indicates the years from which clinical cases associated with each cluster were reported.
National outbreak of listeriosis in England associated with smoked salmon, 2020
Between January and October 2020, an outbreak of listeriosis was detected in England after 4 people were infected with the same strain of L. monocytogenes, 2 of whom died. All 4 cases had underlying comorbidities and risk factors for listeriosis, including 1 pregnancy-related case. One of the outbreak cases reported consuming salmon trimmings and smoked salmon slices purchased from a UK supermarket chain.
Following international inquiry through the European surveillance portal (EPIS, now known as EpiPulse), whole genome sequencing (WGS) analysis of food isolates sampled from smoked salmon in an EU country identified the outbreak strain. The samples were traced back to a salmon supplier in the UK that distributed salmon products to the supermarket chain reported by one of the cases.
Conclusions
Listeriosis remains a rarely reported disease in England and Wales, with 0.21 cases per 100,000 population. The outcome of listeriosis in pregnancy remains severe with over a third resulting in miscarriage or stillbirth. Mortality amongst non-pregnancy cases remains high, with a case fatality rate of 17.2%. Two national outbreaks were traced back to high-risk foods for listeriosis, supported by the linkage of cases to contaminated food through the analysis of strain relatedness using whole genome sequencing data.
As a predominantly foodborne infection, awareness of high-risk foods for vulnerable groups is vital. The low number of reported cases complicates the interpretation of the trend and any comparisons with previous years. It remains imperative that sporadic cases of illness and clusters of disease continue to be monitored and investigated to inform the continued risk assessment of the food chain.
Data sources
National Enhanced Surveillance System for Listeria monocytogenes infection in England and Wales
Second Generation Surveillance System (SGSS)
Acknowledgements
We are grateful to the microbiologists, health protection and environmental health specialists who have contributed data and reports to the national surveillance system.
We also thank our colleagues in the:
- Gastrointestinal Bacteria Reference Unit (GBRU) for providing the Reference Laboratory Services and laboratory surveillance functions and expertise
- UKHSA Local Public Health Laboratories and Food, Water and Environmental Microbiology Services for providing a surveillance function for GI pathogens and testing of food and environmental samples routinely and during outbreak investigation
- UKHSA Health Protection and Field Service teams for their contributions to incident investigations
