HPR volume 12 issue 35: news (28 September)
Updated 21 December 2018
Tuberculosis in England: 2018 report
PHE has published its annual tuberculosis (TB) report for England which contains data to the end of 2017 [1]. In addition, the report presents data on the UK pre-entry screening programme, latent TB infection (LTBI) testing and treatment, and BCG vaccination coverage estimates.
The information contained in the report, and accompanying monitoring data displayed on Fingertips (due to be released on 2 October 2018) [2], can be used to support action to achieve the aims for TB control set out in the Collaborative Tuberculosis Strategy for England 2015 to 2020 [3].
Epidemiology
In 2017, there were 5,102 people notified with TB, down from 5,616 in 2016. This decline marks a return to the annual declines of 10% achieved between 2012 and 2015. 2017 saw the lowest number of notifications since 1990, and a 38% decline since the peak in 2011. The incidence rate in 2017 was 9.2 per 100,000 (CI 8.9-9.4), compared with 10.2 per 100,000 (CI 9.9-10.4) in 2016, and is the lowest rate of TB in England since the start of enhanced TB surveillance in 2000 (see figure).
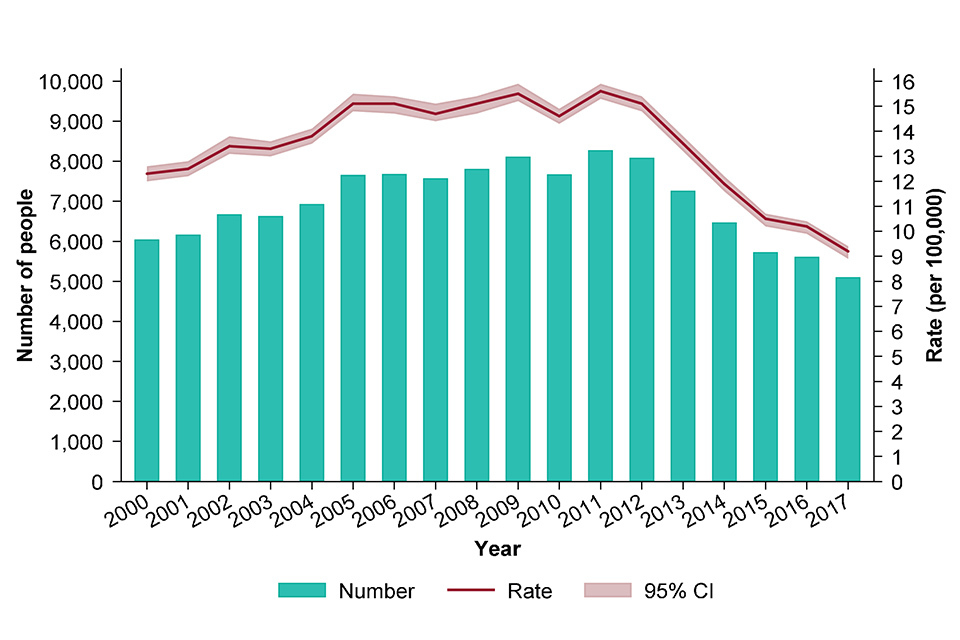
TB case notifications and rates, England, 2000-2017
The majority (71%) of TB cases notified in England are born outside the UK. Large decreases in the number of notifications and incidence rate were seen among this group; 3,556 in 2017 (41.1 per 100,000, CI 39.7-42.4) compared to 4,093 in 2016 (49.4 per 100,000, CI 47.9-50.9). However, there was no decline in either the number of notifications among people born in the UK or the incidence rate which remained at 3.1 per 100,000 (CI 3.0-3.3), between 2016 and 2017.
Outcomes in drug sensitive TB cases
The proportion of drug-sensitive TB cases notified in 2016 who completed treatment within 12 months increased to 84.4%, up from 83.7% for people notified in 2015. There was a small decrease in the proportion of people with drug-sensitive TB who died, from 6.1% for those notified in 2015, to 5.5% for those notified in 2016; most (64%) of these deaths occurred in those aged 65 and older.
Antimicrobial resistance
The number and proportion of cases in the drug-resistant cohort – confirmed or treated as multi-drug resistant/rifampicin resistant TB (MDR/RR-TB) – has remained relatively stable over the last three years, with 61 people notified in 2017. The number with initial confirmed MDR/RR-TB decreased slightly from 2016 (60 vs 55), although the proportion remained similar (1.7% vs 1.8%). Three people with XDR-TB were notified in 2017, fewer than in 2016.
Delay between symptom onset and start of treatment
A high proportion of cases continue to experience delays between symptom onset and the start of treatment. In 2017, 31% of those with pulmonary TB experienced a delay of more than four months, the same proportion as in 2016. Treatment delays of more than four months continue to be more common among people born in the UK (37%), compared with people born outside the UK (28%).
Social risk factors
There was an increase in the proportion of TB cases who had at least one social risk factor (homelessness, drug or alcohol misuse or imprisonment) from 11.0% in 2016 to 12.6% in 2017. Those notified in 2017 who had at least one social risk factor were more likely to have pulmonary TB (76.6%), drug resistance (2.7%) and worse outcomes, being more likely to have died (6.3%) or to have been lost to follow-up (6.5%) by 12 months compared to those without a risk factor.
Conclusions and recommendations
2017 saw the lowest number of TB notifications in England since 1990, and a return to the steep annual decline in notifications seen between 2012 and 2015. The rate of 9.2 per 100,000 is the lowest ever recorded rate of TB for England and for the first time falls below the 10 per 100,000 threshold which defines a low incidence country.
To continue to achieve year-on-year reductions in TB incidence and to meet the needs of the under-served populations, effort needs to be maintained to deliver all 10 key areas for action in the national strategy and to strengthen TB control. Recommendations to achieve this are outlined at the end of the annual report. Specifically, it will be important to focus on:
- reducing active TB in recent new migrants through the UK TB pre-entry screening programme
- preventing reactivation of TB among migrants through LTBI testing and treatment
- continuing efforts to reduce diagnostic delay through awareness raising in communities affected by TB and among health professionals
- maintaining the quality of TB diagnostic, treatment and care services to ensure high rates of culture confirmation and treatment completion
- maintaining a focus on the social factors associated with TB and ensuring an integrated approach to the specific needs of under-served populations.
UN General Assembly high level meeting on tuberculosis
Publication of the PHE report for England coincided with the first ever United Nations high-level meeting on tuberculosis at which a Political Declaration on TB was endorsed by Heads of State, that will strengthen action and investments to end TB, saving millions of lives [4].
The results of a study demonstrating the ability of whole genome sequencing to predict the susceptibility of infecting strains of TB to first-line drugs were announced at the UN meeting [5]. An editorial related to the publication called for universal drug-susceptibility testing to be included as a requirement for meeting the WHO’s End TB targets [6].
References
- PHE (September 2018). Tuberculosis in England: 2018 report (presenting data to end of 2017).
- PHE website. TB Strategy Monitoring Indicators.
- PHE (January 2015). Collaborative tuberculosis strategy for England 2015 to 2020.
- “World leaders commit to bold targets and urgent action to end TB”, WHO press release, 26 September 2018.
- The CRyPTIC Consortium and the 100,000 genomes Project (2018). ‘Prediction of susceptibility to first-line tuberculosis drugs by DNA sequencing’, NEJM online.
- Cox H and Mizrahi V (2018). ‘The coming of age of drug-susceptibility testing for tuberculosis’, NEJM editorial.
Infection and vaccine coverage reports in this issue of HPR
The following reports are published in this issue of HPR.
