Health matters: tobacco standard packs
Published 15 September 2016
Summary
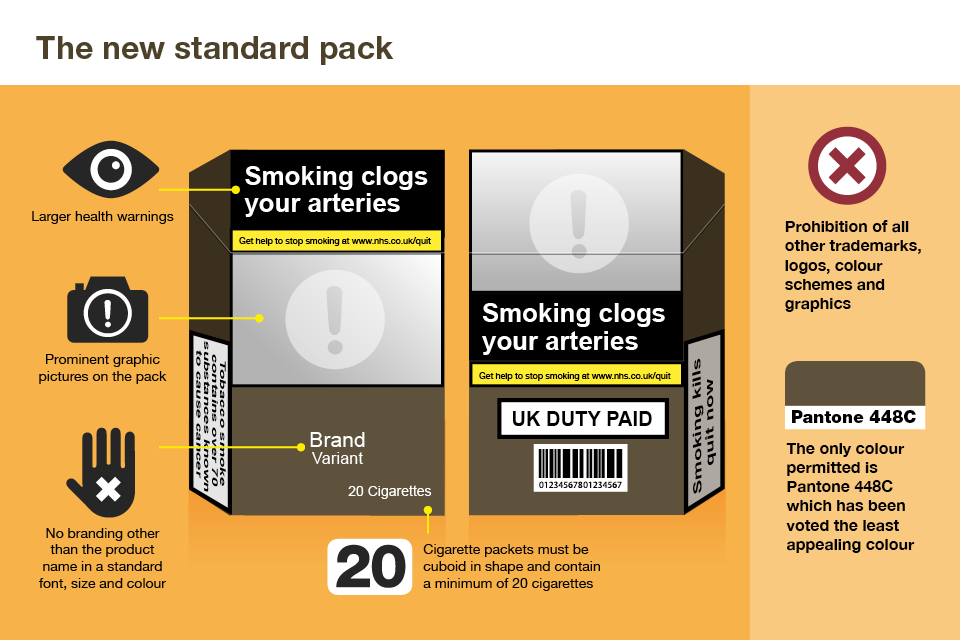
In May 2016, the UK became the second nation in the world after Australia to introduce standardised packaging of tobacco products. Standard packs are designed to prevent the next generation of smokers but they can also have a positive impact on quit rates. The roll out of standard packs in England presents a unique window of opportunity to support smokers to quit.
Standardised packaging
Standard packs are beginning to appear in the UK, with the first packs reported in August 2016.
All cigarettes and rolling tobacco sold in the UK will appear in standard packs with prominent health warnings by May 2017. Colourful, glamorous and stylish packs are no longer allowed.
Australia became the first country in the world to require cigarettes to be sold in standard packs in December 2012.

Cigarette packs are the last form of advertising
Tobacco companies now have fewer and fewer ways to tell people about their brand. In the UK, tobacco companies cannot advertise on television, on billboards, or in printed publications.
Cigarette packs are the last advertising medium for tobacco companies to sell the ‘personality’ of their brand to consumers. Smokers tend to retain the cigarette pack until all the cigarettes are used, unlike the packaging of many other products that gets thrown away.
Cigarette packs are constantly taken out and opened, as well as being left on public display during use. In this way, cigarette packaging acts as an advertisement.
Cigarettes enjoy enormous brand loyalty. Teenagers are more heavily swayed by brands than adults, according to Plain tobacco packaging research by University of Sterling. They choose a brand when they first start smoking, and research shows that only 10% of smokers switch brands in any year.
Brand loyalty comes despite the fact that many smokers cannot actually identify their brand just from smoking the cigarettes.
Tobacco companies design packs to appeal specifically to female smokers. Cigarettes for women are often packaged in slim, long packs, often with pastel or toned down colours, to appear feminine and sophisticated.
Preventing the next generation of smokers
There is very strong evidence that exposure to tobacco advertising and promotion increases the likelihood of children and young people taking up smoking.
Approximately 78,000 people die prematurely from smoking-related diseases every year in England according to Statistics on Smoking in England in 2015. Tobacco companies therefore need to recruit new smokers to maintain their profits.
Most smokers start as teenagers: two-thirds before the age of 18. The reasons they start are complex, ranging from peer pressure, and behavioural problems to depictions of smoking in film and on television. Children are more likely to take up smoking if they live with people who smoke.

Evidence for standardised packaging
There have been a large number of experimental studies which have tested the possible effect of standardised packaging using a variety of methods including consumer perceptions, eye-tracking technology, neuroimaging, measures of consumer demand, and behavioural tasks.
A systematic review of these studies known as the Stirling Review concluded that:
- standardised packaging is less appealing than branded packaging
- graphic and text health warnings are more credible and memorable on standardised packaging than when juxtaposed with attractive branding
- whereas colours and descriptors on branded packaging confuse smokers into falsely perceiving some products as lighter and therefore healthier, products in standardised packages are more likely to be perceived as harmful
An independent review of Standardised packaging of tobacco undertaken by Sir Cyril Chantler on behalf of the UK government also concluded that it is highly likely that standardised packaging would serve to reduce the rate of children taking up smoking.
There is also real world data on Tobacco plain packaging to call upon from Australia since the introduction of standard packs in December 2012.

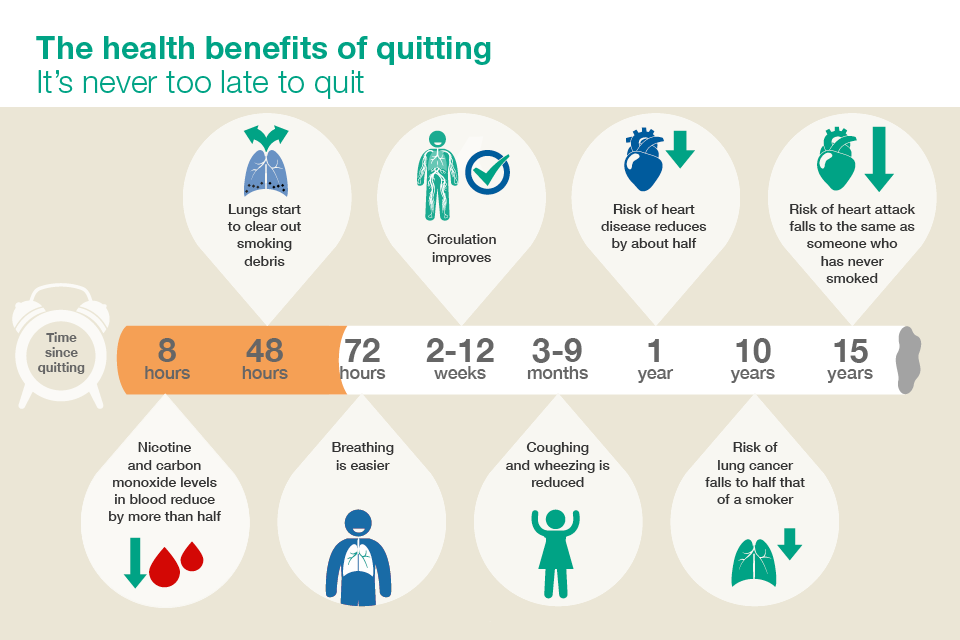
Seize the moment: encourage smokers to quit
Introduction effects of the Australian plain packaging policy on adult smokers: a cross-sectional study found, compared with smokers smoking from branded packs, smokers who were smoking from standard packs were more likely to perceive their tobacco as being lower in quality, tended to be lower in satisfaction, and were more likely to think about and prioritise quitting.
This has been borne out by the introduction of standard packs in Australia, which was associated with a 78% increase in calls to the smoking cessation Quitline in New South Wales, according to Association between tobacco plain packaging and Quitline calls: a population-based, interrupted time-series analysis. This peak occurred 4 weeks after the initial appearance of standard packs and the effect has been prolonged.

This increase is similar to that observed following the introduction in Australia of graphic health warnings on packs in 2006, but the impact from standardised packaging has been more sustained.
A review of Standardised packaging of tobacco products carried out by the Irish Department of Health concluded that standardised packing could encourage, motivate and support current smokers to quit.
Currently, 2 out of 3 adult smokers say they want to quit. That proportion is set to increase over the coming months and local healthcare systems need to be ready to make the most of this opportunity to boost quitting rates in their populations.
Health professionals have an important role to play in encouraging smokers to quit. Prompts from health professionals are the second most common reason for a quit attempt.
All health professionals should identify and refer smokers using the method known as Very Brief Advice (VBA) which has 3 components: Ask, Advise and Act. National Centre for Smoking Cessation and Training guidance is to:
- ASK and record smoking status; is the patient a smoker, ex-smoker, or non-smoker?
- ADVISE on the best way of quitting; the best way of stopping smoking is with a combination of medication and specialist support
- ACT on patient response; build confidence, give information, refer, and prescribe
Local stop smoking services offer the best chance of success. A combination of behavioural and pharmacological support is up to 4 times more effective than no help or over the counter nicotine replacement therapy (NRT). However, many smokers still use the quitting methods with the least evidence of effectiveness. E-cigarettes are the most common quitting aid used in England, according to latest survey data from the Smoking Toolkit Study.
The 5 most common quitting aids used in England in 2016 are:
- E-cigarettes.
- NRT over the counter.
- NRT on prescription.
- Varenicline (Champix).
- Behavioural support.
In 2015, just over a million smokers (1,027,000) used an e-cigarette in a quit attempt while around 700,000 used a licensed NRT product.
Identify those who need support
Smoking is concentrated in disadvantaged communities and groups. Disadvantaged smokers are equally likely to try to quit, but less likely to succeed. Disadvantaged smokers significantly improve their chances of success where they access local stop smoking services. Support for quitting smoking should be targeted to reach disadvantaged and high prevalence groups.
Socio-economic status
Large regional variations in smoking prevalence reflect health inequalities between the richest and poorest in England. Ill-health caused by smoking is much more common amongst the poorest and most disadvantaged in society.
PHE health profiles data shows that smoking prevalence is higher than the England average for 2015 (16.9%) in the:
- East Midlands (18%)
- North East (18.7%)
- North West (18.6%)
- Yorkshire and the Humber (18.6%)
The ONS Adult smoking habits in Great Britain report states that half of all smokers in England work in routine and manual occupations. Workers in routine and manual jobs are twice as likely to smoke as those in managerial and professional roles, and unemployed people are twice as likely to smoke as those in employment.
People with long-term conditions
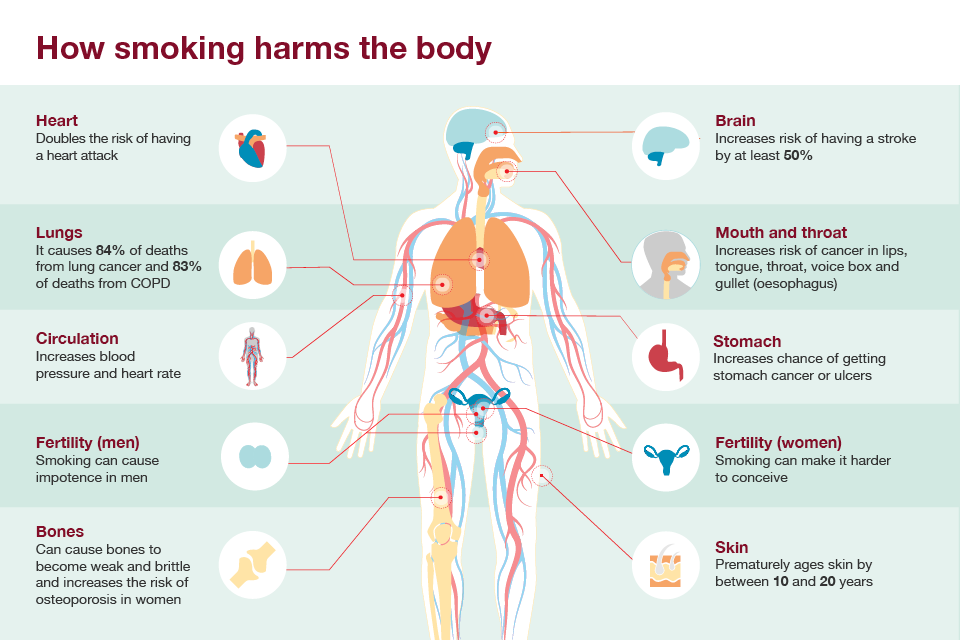
Smoking both causes and exacerbates long-term conditions.
Respiratory conditions
Smoking is the most important risk factor for chronic obstructive pulmonary disease (COPD) and around half of smokers will develop the disease. COPD causes 24,000 deaths in England every year and smoking accounts for as many as 85% of COPD related deaths, according to Health and Social Care Information Centre figures.
Stopping smoking is the only intervention in COPD that can reduce coughing, wheezing, breathlessness and chest pain, as well as slowing the decline in lung function and reducing COPD readmissions and mortality.
NICE recommendations for Managing stable COPD are that all COPD patents who smoke are offered smoking cessation, regardless of age, at every opportunity.
People suffering from asthma who smoke experience higher rates of hospitalisation, worse symptoms and more rapid decline in lung function than those with asthma who do not smoke, according to the British Thoracic Society.
Cardiovascular disease and diabetes
Smoking significantly increases the risk of heart disease and stroke. Smokers are 2 to 4 times more likely to have a stroke, according to Smoking and stroke: the more you smoke the more you stroke.
Smoking as a modifiable risk factor for type 2 diabetes in middle-aged men estimates that 12% of all type 2 diabetes in the US may be attributable to smoking. If the same proportion is applied to the UK, smoking may account for as many as 350,000 cases of diabetes.
Smokers with diabetes have increased risks of macrovascular and microvascular complications and premature death. Research on The impact of smoking and quitting smoking on patients with diabetes has shown that smoking is linked to worsening diabetes control and insulin resistance and may even induce diabetes.
People living with mental health conditions
In England, 33% of people with a mental health condition smoke. A PHE and NHS England survey found that smoking prevalence among service users in mental health units is even higher at 64%. High smoking rates among people with mental health conditions are the single largest contributor to their 10 to 20-year reduced life expectancy.
PHE and NHS England published Smoking cessation in secondary care guidance to help medium and low secure mental health units best implement the National Institute for Health and Care Excellence (NICE) guidelines PH48 that all NHS funded sites should provide access to on-site stop smoking services and deliver care in an environment free of smoke.
Lesbian, gay, bisexual and trans (LGBT) community
Action on smoking and health found that people from LGBT communities are more likely to experience health inequalities and have higher rates of smoking. Data from the ONS Integrated Household Survey 2014 shows that smoking prevalence among adults who identified themselves as gay, lesbian or bisexual was 25.3% compared to 18.4% among those who identified themselves as heterosexual or straight, almost 40% higher.
LGBT people are more likely to suffer from a number of social disadvantages, such as homelessness and mental ill health, which make them more vulnerable to smoking.
LGBT people often report limited access to health services so good communication between health professionals and LGBT people can help to encourage them to be involved in their own healthcare and promotes better health outcomes.
It is important that local stop smoking services actively seek to engage with LGBT communities and are accessible in a range of settings that are appropriate for LGBT communities.
Pregnant women
Smoking is the single most important modifiable risk factor in pregnancy. Statistics on women’s smoking status at time of delivery, England 2015 to 2016 found that 10.6% of mothers were recorded as smokers at the time of delivery which is lower than 2014 to 2015 (11.4%). However, considerable variations remain prevalent across NHS England Regions, from 16.0% in Cumbria and North East to 4.9% in London.
Smoking, and exposure to tobacco smoke, is associated with a range of poor pregnancy outcomes including miscarriage, stillbirth and sudden infant death syndrome. Babies born to mothers who smoke are more likely to have a low birth weight and are at increased risk of developing respiratory conditions, learning difficulties, problems of the ear, nose and throat, obesity and diabetes.
It is therefore vital to encourage pregnant women to stop smoking, and ideally remain smoke-free following the birth. This offers health benefits for both the mother and unborn baby, along with reducing exposure to secondhand smoke for the infant.
It is important that pregnant women who smoke are identified and referred for specialist support at the earliest opportunity. Unfortunately, there has been an 8% fall in the number of pregnant women who have set a quit date with local stop smoking services according to Statistics on NHS stop smoking services. 17,433 pregnant women set a quit date in 2014 to 2015 compared to 18,887 in 2013 to 2014.
Smoking: stopping in pregnancy and after childbirth guidance from NICE outlines interventions to support stopping smoking in pregnancy and after childbirth.
Invest in tobacco control
The total cost of smoking to society in England is approximately £13.9 billion per year according to ASH. This includes costs to:
- the NHS
- social care
- businesses
- local government
- fire services
Businesses and the local economy bear the brunt of the costs so reducing smoking will help revitalise local economies.
ASH Tobacco economics estimates that smoking costs the NHS in England approximately £2 billion a year for treating diseases caused by smoking.
Every £1 spent on smoking cessation saves £10 in future health care costs and health gains according to the NICE return on investment tool.
Smoking is the biggest cause of preventable illness and tackling it provides the biggest opportunity for making services across the entire health and care system more sustainable.
A unique window of opportunity to support smokers to quit
PHE believes that standardised packaging will make an invaluable contribution to achieving a tobacco free generation by 2025. As a powerful addition to the existing levers available, standardised packaging could be the game changer in helping to prevent future generations from taking up smoking.
As the evidence from Australia shows, the introduction of standard packs also offers a crucial window of opportunity to engage with smokers and encourage more people to quit. The majority of smokers want to give up and now is the time for concerted and collaborative action.
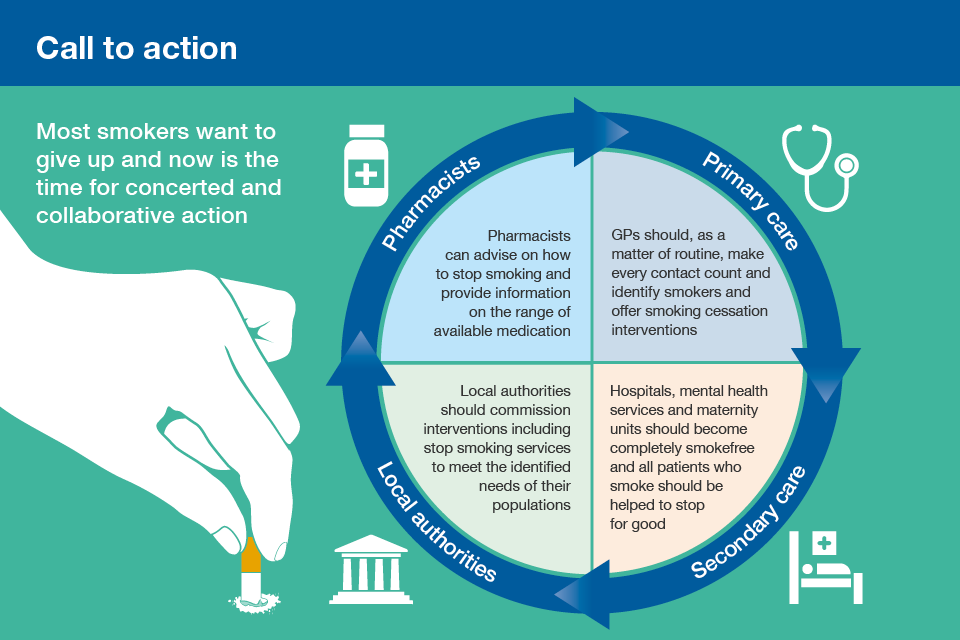
Pharmacists and their teams
Pharmacy teams have an important contribution to make to help people to stop smoking. They have many opportunities to do so including when:
- people buy nicotine replacement therapies products
- people buy other over-the-counter medicines such as cough medicines repeatedly
- dispensing medicines for smokers with conditions such as high blood pressure
They are ideally placed to provide information on the range of available medicines and provide advice about the use of these medicines. Some community pharmacies also provide behavioural support for smokers who want to stop. Many pharmacies engage both in PHE’s Stoptober and January Health Harms campaigns. Both these campaigns provide ideal times when pharmacy teams can encourage smokers to stop smoking.
Primary care
GPs are normally the first point of contact for patients. As a matter of routine, they should make every contact count and identify smokers and offer smoking cessation interventions.
The NHS Health Check, for adults aged 40 to 74, presents an ideal opportunity to offer advice on quitting smoking. All smokers should be offered a referral to their local stop smoking service.
Secondary care
NICE Smoking: acute, maternity and mental health services guidance recommends that all hospitals, mental health services and maternity units become completely smoke-free to help all patients who smoke to stop smoking whilst they receive care, and preferably help them to stop for good.
Up to 70% of smokers attending hospital say that they would like to stop; stopping smoking is central to treatment and prognosis of almost every disease.
The guidance states that:
- everyone should be provided with verbal and written information about the hospital’s smoke-free policy before their appointment, procedure or hospital stay, including short and long-term benefits of stopping smoking and details of the support available to help them stop smoking before, during and after their stay or visit
- intensive support should be offered for smokers using secondary care services, including discussing past and current smoking behaviour and developing a personal stop smoking plan
- measurements of exhaled carbon monoxide (CO) should be offered for people using acute, maternity and mental health services, as part of the intensive stop smoking support provided, during each contact, to provide feedback on progress and increase their motivation to stop completely
- relatives, carers, friends and other visitors should be provided with information about the risks of smoking and secondhand smoke
In its The Case for Change report, the British Thoracic Society (BTS) explains how NHS trusts can benefit financially from investing in stop smoking services at a number of levels, including admission avoidance, reducing length of stay and reducing re-admissions.
Local authorities
Local authorities should take a comprehensive and evidence-based approach to identifying smoking prevalence in their areas and commission appropriate interventions including smoking cessation services.
Tackling tobacco use enables local authorities to:
- reduce health inequalities
- protect children from secondhand tobacco smoke
- drive improvement across key measures of population health
The Local Tobacco Control Profiles for England provide a snapshot of the extent of tobacco use, tobacco-related harm and measures being taken to reduce this harm at local level.
PHE’s CLeaR local tobacco control assessment is an evidence-based improvement model designed to help local authorities and health and wellbeing boards develop local action to tackle tobacco use in their areas.
PHE encourages all local authorities to show their commitment to tackling smoking by signing up to the Local Government Declaration on Tobacco Control. It is a statement of a council’s commitment to ensure tobacco control is part of mainstream public health work and commits councils to taking comprehensive action to address the harm from smoking. Over 80 councils have already signed up.
Exploit every opportunity to help smokers quit
PHE’s Stoptober campaign is back for a fifth year to encourage thousands of smokers to quit together this October.
Health professionals can signpost patients to the Stoptober website where they will find a range of free and proven support tools, including apps, email and social media support, as well as information on the different types of stop smoking aids and the expert support available from local stop smoking services.
