Health matters: preventing drug misuse deaths
Updated 15 September 2017
Summary
This professional resource outlines how providers and commissioners can prevent deaths from drug abuse.
Scale of the problem
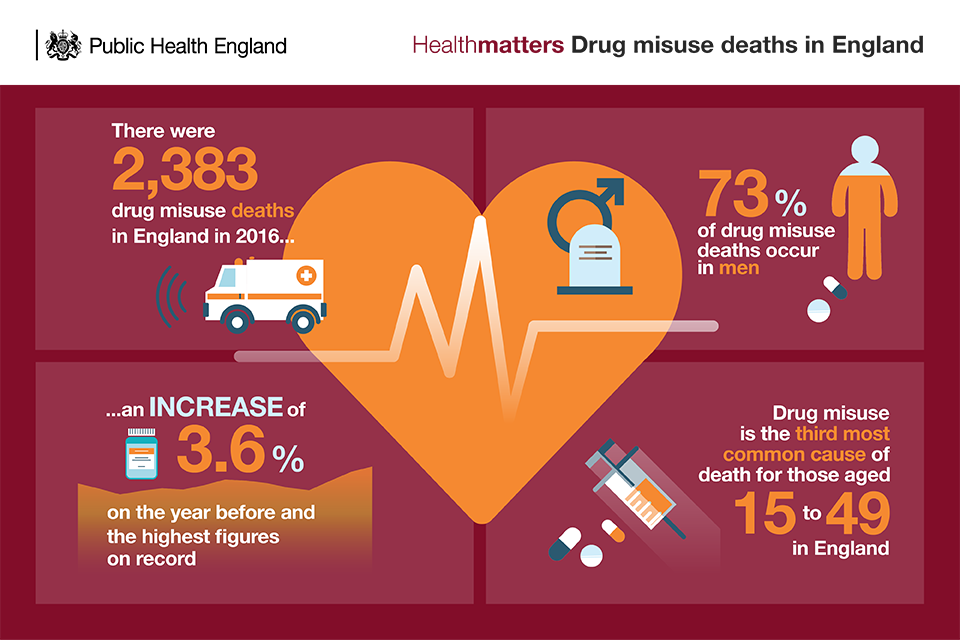
There were 2,383 drug misuse deaths registered in England in 2016. This represents an increase of 3.6% on the year before and the highest figure on record.
A drug misuse death is defined as a death where:
- the underlying cause is drug abuse or drug dependence
- the underlying cause is drug poisoning and where any of the substances controlled under the Misuse of Drugs Act 1971 are involved
The Office for National Statistics (ONS) publishes data on deaths from drug poisonings in England and Wales and is broken down by cause of death, sex, age and substances involved in the death.
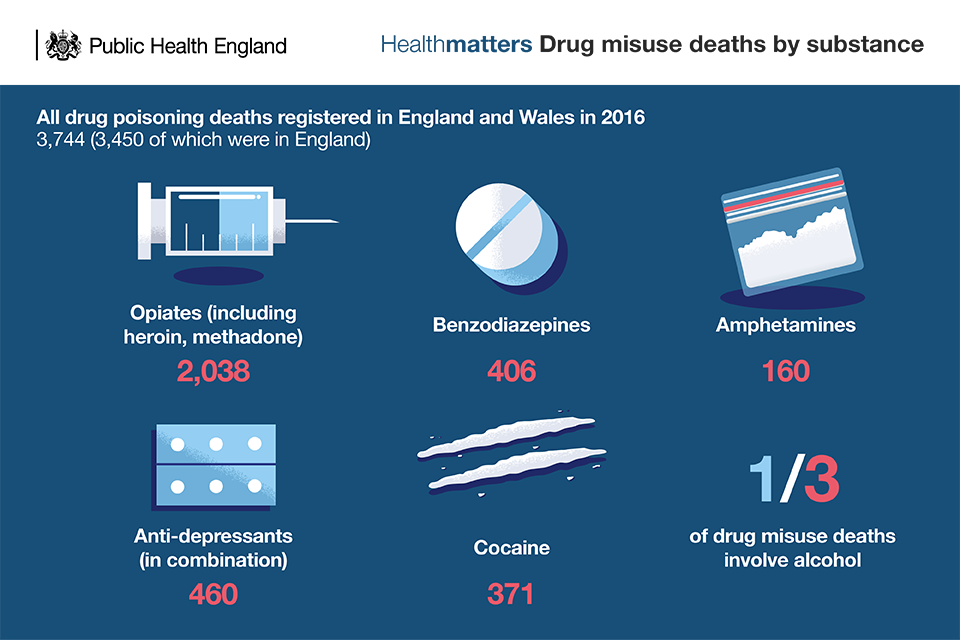
Deaths involving opioids (such as heroin) account for the majority of drug poisoning deaths. Heroin related deaths in England and Wales have more than doubled since 2012 to the highest number since records began 20 years ago.
There are also a small but rising number of deaths involving:
- new psychoactive substances
- prescription and over-the-counter medicines, including pregabalin and tramadol
Further analysis by PHE found that alcohol is mentioned in around a third of drug misuse deaths annually in England, and that heroin related deaths increasingly also involve other substances.
The majority of drug misuse deaths, 80% in 2016 in England and Wales, are accidental poisonings. The number of suicides among drug misuse deaths is small but steadily rising. PHE’s analysis suggested that suicide was more common in particular groups. Specifically, 38% of drug misuse deaths occurring in 2012 among those aged 45 or over were classed as suicides, as were 34% of deaths among women.
Gender
The majority of drug misuse deaths (73% in 2016) occur in men. However, drug misuse deaths among women are on a long-term increasing trend.
Age
The highest rates of drug misuse deaths in England and Wales currently are among people in their 30s and 40s, with large increases in the death rates in these age groups since 2012 (30 to 39: 44% increase; 40 to 49: 73% increase).
In 2016, the drug misuse death rate among those aged 40 to 49 exceeded that among those aged 30 to 39 for the first time since records began in 1993. The rate among those aged 40 to 49 exceeded 100 per million population.
PHE’s further analysis found that the median age of drug misuse death increased by 9 years in a 13-year period. This pattern is consistent with other indications of an ageing drug-using population.
Drug use is the third most common cause of death for those aged 15 to 49 in England.
Drug misuse accounted for nearly 1 in 8 deaths among people in their 20s and 30s registered in 2015.
Geography
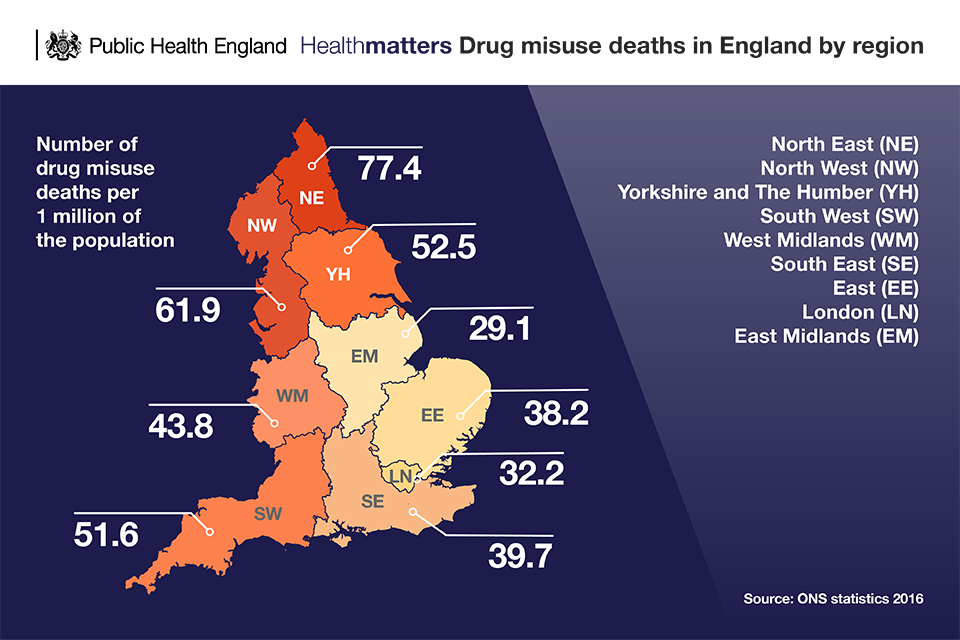
There is also considerable geographical variation in the drug misuse deaths figures, with the highest rates in the 2 northernmost regions of England (North East and North West). The lowest rate is in the East Midlands.
Costs to society
Drug misuse and dependency can lead to a range of harms for the user including:
- poor physical and mental health and ultimately death
- unemployment
- homelessness
- family breakdown
- criminal activity
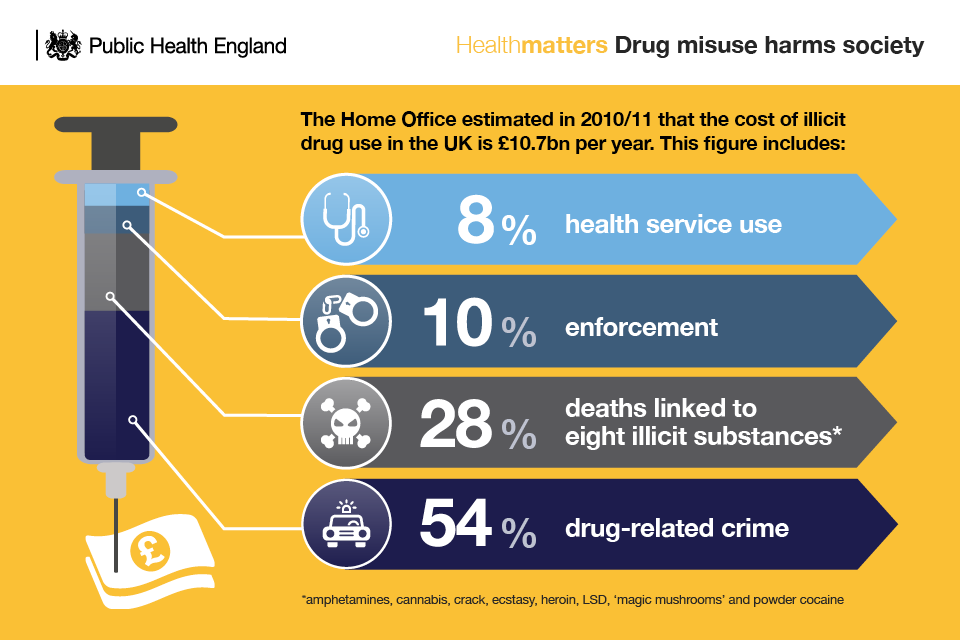
But drug misuse also impacts on all those around the user and the wider society. The Home Office estimated in 2010 to 2011 that the cost of illicit drug use in the UK was £10.7 billion per year.
The UK Drug Policy Commission (UKDPC) estimated the annual cost to the family members and carers of heroin or crack cocaine users to be £2 billion.
Why invest
Investing in treatment services to reduce drug misuse and dependency will not only help to save lives but will also substantially reduce the economic and social costs of drug-related harm.
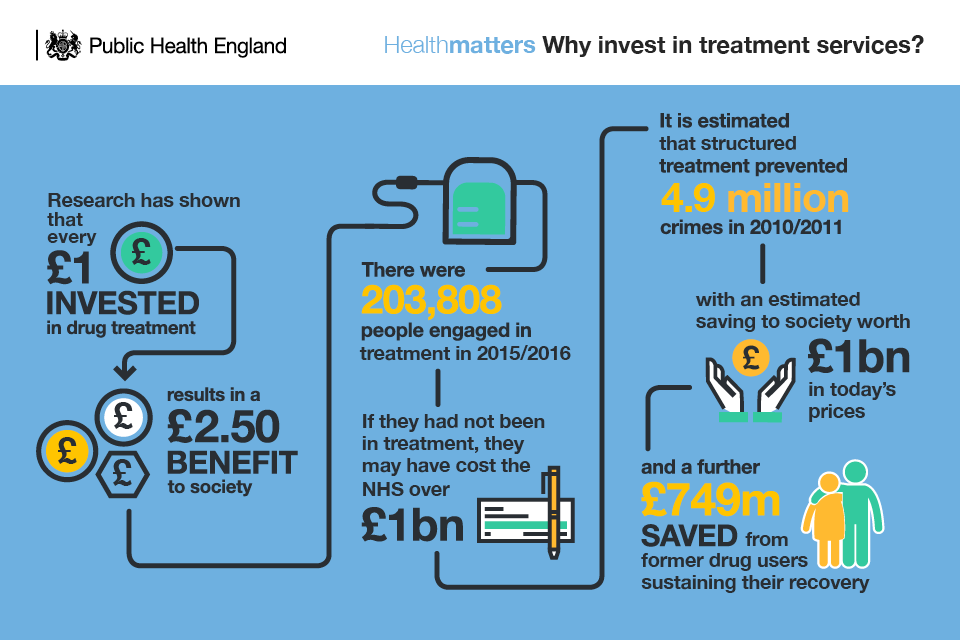
Research has shown that every £1 invested in drug treatment results in a £2.50 benefit to society. For many drug users, engaging in treatment can be the catalyst for getting the medical help they need to address their physical and mental health problems.
The public values drug treatment because it makes their communities safer and reduces crime; 82% said that the greatest benefit of treatment was improved community safety.
Factors causing the rise in drug misuse deaths
PHE, with the Local Government Association, convened a national inquiry to better understand the causes of the rises. Two important factors were identified that may be responsible for the increase in drug-related deaths.
1. Increase in availability and purity of heroin
The apparent sudden increase in drug-related deaths in 2013, 2014, 2015 and 2016 was likely to have been caused, at least in part, by an increase in the availability of heroin, following a fall in deaths during a period when heroin purity and availability was significantly reduced.
2. Ageing heroin users
The proportion of older heroin users, aged 40 and over, in treatment with poor health has been increasing in recent years and is likely to continue to rise.
An ageing cohort of 1980s and 1990s heroin users is now experiencing cumulative physical and mental health conditions. Older heroin users also seem to be more susceptible to overdose because of long-term smoking and other risk factors.
PHE has linked opioid misuse deaths with treatment data and found that as of 2012, more than half of those who died were not known to have been in contact with treatment for at least 5 years. Engaging in drug treatment has a protective effect.
The inquiry identified other factors that contribute smaller numbers to the rise. They include:
- increasing suicides by drug poisoning generally and among drug users specifically; still far fewer in number than accidental poisoning but steadily rising
- increasing deaths among women; far fewer in number than among men but steadily rising even during the period of reduced heroin availability
- a potential increase in people using multiple drugs and alcohol concurrently; there are certainly more people reported as dying with multiple drugs in their systems but the link between the increases and the prevalence of polydrug use is unproven
- an increase in the prescription of medicines; there is a correlation here as the frequency with which some prescribed medicines are found in drug misuse deaths has risen significantly but there is no evidence of causation
- variations in coroner identification and reporting of drug deaths; this seems likely but is as yet unproven
Established risk factors for drug misuse

Risk factors are all negatively associated with health status and there is a complex and reciprocal association between social factors and illicit drug use.
Homelessness, for example, is a complex problem that occurs for many different reasons. Some individuals may later turn to addiction as a means to cope with their lack of a fixed home. However, it can be difficult to determine how much substance abuse leads to homelessness compared with the frequency by which homelessness leads to substance abuse.
Drug misuse can cause social disadvantage, and socioeconomic disadvantage may lead to drug use and dependence.
In addition, risk factors associated with drug misuse often lead to other adverse outcomes such as poor physical or mental health, offending or risky sexual behaviour.
Watch a panel of opinion leaders discuss preventing deaths from drug misuse
Preventing deaths from drug misuse
Preventing drug misuse deaths
Identifying drug users in the community
Treatment can help people control and, eventually, overcome their addiction but services need to be easily accessible and attractive to encourage drug users to make contact.
Improving people’s access to services and getting them to stay can be improved through:
- outreach programmes
- needle and syringe programmes
- accessible locations and flexible opening times
- open sessions and sessions restricted to particular groups and issues
- individualised and welcoming communications, and reminding patients of appointments and checking how they are doing after they leave treatment
- providing transport and childcare
- key workers skilled in building a therapeutic alliance and in motivational techniques, knowing when to take the lead and when to take a back seat
- ensuring effective and supported pathways to treatment from prison
Local authorities are responsible for commissioning drug interventions and services.
The drugs joint strategic needs assessment (JSNA) support pack – updated annually – will help local areas to develop JSNAs and local joint health and wellbeing strategies, which effectively address drug use.
There are 2 documents:
-
A series of good practice evidence-based prompts to help local areas assess need, plan and commission effective services and interventions
Needle and syringe programmes
People who inject drugs are particularly vulnerable to contracting and spreading blood-borne viruses (such as hepatitis B, hepatitis C and HIV) and other infections.
Needle and syringe programmes help to reduce the spread of these viruses caused by sharing injecting equipment. They have been a huge success story in the UK, and are credited with helping HIV rates among people who inject drugs to be as low as 1%. This is one of the lowest rates in the world and compares very favourably to many countries, including the US at 11% and Spain at 33%.
They can also act as a gateway for drug users to more structured treatment and recovery. The National Institute for Health and Care Excellence (NICE) has published guidance on providing needle and syringe programmes.
Drug treatment services
It is important to get drug users into treatment. The majority of drug misuse deaths occur among people who are not in treatment. Evidence shows that being in treatment is protective against the risk of mortality.
Modelling shows that the English public treatment system for opioid use disorder prevented an average of 880 deaths each year from opioid-related poisoning.
England has a well-established network of locally commissioned services that provide drug treatment.
A report by the independent Advisory Council on the Misuse of Drugs has recommended to government that the capacity and quality of these drug treatment services must be maintained in order to prevent further increases in drug misuse deaths, particularly those caused by opioids like heroin.
A recent evidence review into treatment outcomes in England, conducted by PHE, was positive and found that:
- 60% of heroin users are in treatment
- 97% receive access to treatment within 3 weeks
- the rate of drop out from treatment before 3 and 6 months (18% and 34%,respectively) is comparable to the literature (28% on average)
- the rate of stopping injecting (52% after 3 months; 58% after 6 months; 61% after 1 year) is comparable with, or better than, the scientific literature
- treatment in England is associated with a marked reduction in convictions (47% among those retained in treatment for 2 years or successfully completed treatment)
- successful completion of treatment rates for non-opiate drug users, who only receive psychosocial interventions, have increased from 14% in 2005 to 2006 to 37% in 2014 to 2015 for non-opiate drug and alcohol users, and from 13% in 2005 to 2006 to 42% in 2014 to 2015 for users of non-opiate drugs alone
However, the drug-related death rate in England (39 per million in 2013 to 2015) is considerably higher than elsewhere in Europe, although substantially lower than in the USA.
PHE estimates that the proportion of people in treatment with entrenched dependence and complex needs will increase and the proportion who successfully complete treatment will therefore continue to fall.
PHE estimates that there will be an increase, over the next 4 years, in the proportion of people in treatment for opiate dependence who are likely to die from long-term health conditions and overdose.
What makes an effective treatment service
Drug treatment is supported by a well-established body of evidence-based guidelines, which should guide both clinical practice and the commissioning of services.
NICE has produced a pathway for drug misuse management which brings together a number of clinical guidelines alongside a quality standard. This includes guidance on opioid detoxification and the management of opioid dependence.
There is also a UK guideline on clinical management of drug misuse and dependence, commonly called the ‘orange book’. The 2007 edition has been updated and will be published shortly.
PHE’s evidence review makes clear that drug treatment systems should continue to address a broad range of outcomes including:
- harm reduction
- reduced drug use
- social integration and recovery
The assessment of drug treatment outcomes should be expanded beyond the current successful completions indicator to better reflect the breadth of the benefits of drug misuse interventions. Social factors, including housing, employment and deprivation, are associated with substance misuse and these social factors moderate drug treatment outcomes.
Factors that can increase the likelihood of opiate users successfully completing treatment include:
- being in education or employment
- being in good physical health
- not drinking alcohol everyday
Factors that can decrease the likelihood of opiate users successfully completing treatment include:
- using opiates everyday on top of any prescription medication
- having housing problems
- living in an area of higher deprivation
- previously dropping out of treatment
Commissioners and providers should use the new Public Health Outcomes Framework (PHOF) indicator (2.15iv) measuring drug-related deaths in local areas to benchmark performance and encourage improvement.
Widening availability of naloxone
Naloxone is the emergency antidote for overdoses caused by heroin and other opiates/opioids (such as methadone and morphine).
The main life-threatening effect of heroin and other opiates is to slow down and stop breathing. Naloxone blocks this effect and reverses the breathing difficulties.
Naloxone can be supplied to those:
- currently using illicit opiates, such as heroin
- receiving opioid substitution therapy
- leaving prison with a history of opioid use
- who had previously used opiate drugs (to protect in the event of relapse)
On 1 October 2015, new regulations came into force, which allow for widening of the availability of naloxone.
This means that a range of drug treatment services can order naloxone from a wholesaler so that people engaged or employed in their services can, as part of their role, make a supply of the naloxone available to others without a prescription.
With the agreement of the individual at risk, it could also be prescribed to family members, friends and peers.
Read PHE’s guidance on naloxone use for commissioners and providers.
Call to action
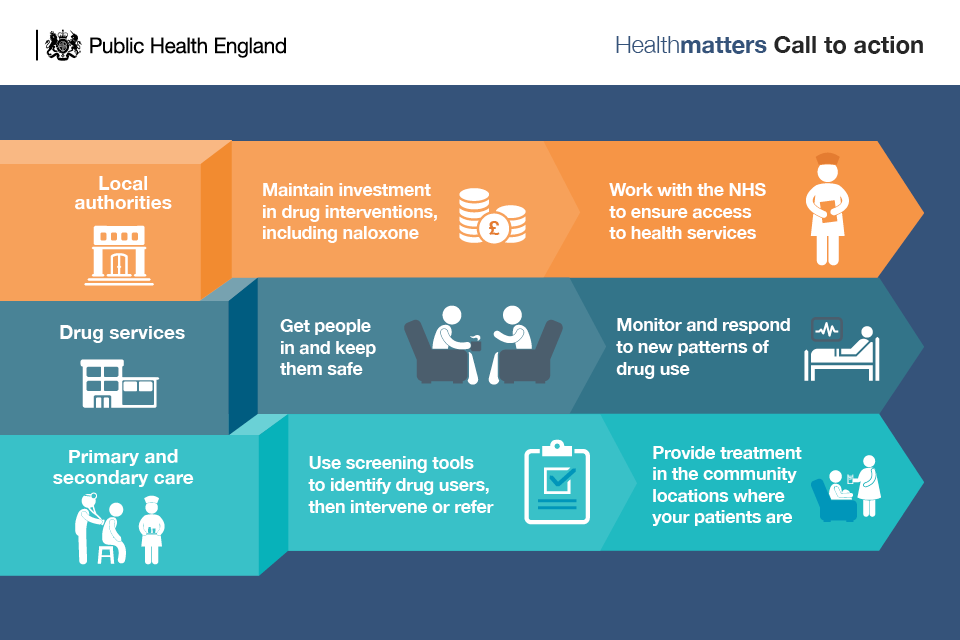
Local authorities and the NHS
Local authorities need to invest adequately in the services that can prevent drug misuse deaths. These include:
- drug prevention
- low threshold, harm reducing services, like needle and syringe programmes
- structured drug treatment
Naloxone and overdose training also need to be provided for drug service users, drug users not in treatment, family and friends, hostel residents and others.
With so many drug misuse deaths occurring among people who have not (at least recently) been in drug treatment, local authority commissioners should be working with their drug service providers to increase the proportion of the local drug misuser population who are accessing drug treatment. Outreach, needle and syringe programmes, and screening and referral from other services can all help get people through the treatment door.
Local authorities are also central to ensuring that people who use drugs get the broader support they need to recover from drug dependence and maintain their recovery, such as safe and secure housing, meaningful work or other occupation, peer support and mutual aid.
But local authorities can’t fix the problems of drug-related deaths on their own - they need to work closely with NHS commissioners to ensure that people who misuse drugs have the access they need to mental and physical health services.
This means developing pathways that facilitate people who use drugs being screened for health conditions and then treated when appropriate, for example, when leaving prison and for conditions such as:
- liver disease
- lung disease including COPD
- cardiovascular disease
- mental health problems including depression and anxiety
Drug services
Drug treatment services have to ensure that their services are attractive and accessible so that people come for treatment. They need outreach and low threshold services to make contact with people using drugs who don’t necessarily want treatment. And they need to provide the range of treatment options that people want (both abstinent and non-abstinent recovery, with peer support).
Services then need to ensure the quality and effectiveness of the treatment and recovery interventions they provide to individuals, so that they stay as long as needed and are then supported to leave when they are ready. Transition points in treatment are times of especially high risk for drug related deaths (DRDs) such as leaving treatment, leaving prison, leaving residential rehabilitation and detoxification. Drug users need services to support them to move between environments safely.
Drug services should support access for their service users through effective pathways to physical and mental healthcare. This means building links and pathways with, or even hosting, interventions like smoking cessation, lung health screening, and liver disease treatment.
Services should be developing systems, and ensuring their staff have the skills, to identify high-risk times and indicators for overdose and suicide. And, having identified people at risk, they need to intervene, broaching the difficult question of suicide, stepping up treatment, providing access to other services.
Much of this is for ‘traditional’ drugs and their users but services also need to be monitoring and responding to new patterns of drug use and new groups of users. They should ensure their staff are competent to work with a variety of populations in ways that are sensitive to different cultures and different needs.
Primary and secondary care
Other services that will be in contact with people who might be misusing drugs include:
- GPs
- pharmacists
- sexual health services
- emergency departments
These should all be using simple, locally-agreed screening tools to identify people who could benefit from help. Having identified them, these services can then provide brief interventions that might change a person’s behaviour or put them in touch with their local drug treatment services.
Across healthcare, people who use drugs, as for any patient, should be provided with health screening and interventions that are appropriate to their age and health status. But people who use drugs may also need earlier and additional screening and interventions specific to the heightened risk of the many conditions that drug use causes or exacerbates.
Secondary healthcare services, in particular, need to make it easier for drug users to access their help. Some need get out into the community locations (such as drug services) where their patients are. Here they can make contact with, screen and assess potential patients, and perhaps provide treatment on site and, ultimately, save lives.
Resources
Case study: Responding to drug related deaths in Newcastle
Case study: Working with accident and emergency units to distribute naloxone
