Evaluation of the 2022 Fit Note Reforms
Published 3 April 2025
DWP research report no.1092
A report of research carried out by Woodnewton on behalf of the Joint Work and Health Directorate (Department for Work and Pensions and Department of Health and Social Care).
Crown copyright 2025.
You may re-use this information (not including logos) free of charge in any format or medium, under the terms of the Open Government Licence. To view this licence, visit http://www.nationalarchives.gov.uk/doc/open-government-licence/
or write to:
The Information Policy Team
The National Archives
Kew
London
TW9 4DU
or email:
This document/publication is also available on our website at:
If you would like to know more about DWP research, email socialresearch@dwp.gov.uk
First published April 2025.
ISBN: 978-1-78659-830-1
Views expressed in this report are not necessarily those of the Department for Work and Pensions or any other government department.
Executive summary
Woodnewton was commissioned by the Joint Work and Health Directorate, a joint unit between Department for Work and Pensions (DWP) and Department of Health and Social Care (DHSC), to evaluate 2 legislative changes to the fit note system made in 2022. In April 2022, regulation changes saw the introduction of digital certification, removing the requirement for fit notes to be signed by the healthcare professional (HCP) in ink. A further legislative change was made in July 2022 which extended the right to certify fit notes to 4 additional healthcare professions: registered nurses, occupational therapists, physiotherapists, and pharmacists (working in GP surgeries, hospitals or similar care settings but not in retail or community pharmacies). In addition to exploring views and experiences of the implementation of these reforms, the evaluation also examined wider attitudes to the fit note system and changes within NHS to place the reforms in context. The research was carried out between January and July 2023 in 2 waves. It involved focus groups and one-to-one interviews with 84 HCPs, 43 patients and 28 employers from across Great Britain. Public attitudes to the reforms were also measured using a nationally representative survey with 2,023 participants.
Attitudes to the 2022 reforms
There is broad agreement across HCPs, employers and patients that extending certification to other HCPs is fundamentally a good idea, but this should be in situations where the HCP has a meaningful interaction with the patient, and with safeguards including training, monitoring, and the option to refer complex cases to a doctor. The extension to include nurses was the change which participants understood fastest and approved of the most, while the extension to pharmacists raised some initial concerns. This may have been because the role of clinical pharmacists in GP surgeries is still relatively unfamiliar, but even for pharmacists, many participants interviewed approved of the extension once they understood which pharmacists were able to issue fit notes and that it did not include those working in retail or community pharmacies.
The research identified several drivers and barriers relevant to extended certification. Some HCPs were still unaware of the reforms, while a small minority of decision-makers (usually GP partners) were unconvinced that the changes are justified or will bring sufficient benefits to outweigh the costs. A larger minority were also positive about the changes but have prioritised other changes to working practices. The main drivers of uptake among HCPs are expectations that this will improve patient care by making it less stressful and time-consuming for patients to get a fit note and having more appropriate discussions about the potential to return to work; enhanced job satisfaction and career development for other HCPs; and reduced workload, particularly for administrative staff.
There was also widespread support for digital certification of fit notes within the wider use of telehealth, as this helped overcome problems some patients have in accessing primary care. It enabled the healthcare system to provide fit notes in digital formats, which was more convenient for patients. Employers also generally preferred digital fit notes as their HR records are now kept electronically.
Attitudes to the fit note system
The drivers and barriers to uptake of these reforms were influenced by attitudes to the fit note system as a whole, where there was broad agreement amongst HCPs, patients and employers.
-
A fit note system was needed. It was viewed particularly positively by employers as well as employees, when it provided advice on helping people back to work.
-
Although there was a widely held perception across respondent groups that patients can often obtain fit notes ‘on demand’, most participants felt the balance between access and scrutiny was about right. They believed it was important that those in genuine need of a fit note can obtain this easily.
-
There was widespread agreement that more people were suffering from anxiety, stress and mental ill-health which affected their ability to work, and it was important the fit note system should continue to ensure that those who needed help and support got it.
-
Many HCPs felt it was not their job to police the system, and patients and employers have some sympathy with this. However, there is also general view amongst patients and employers that signing people off is not always in their best long-term interest, particularly for their mental health. Some thought that HCPs should be monitored to help ensure the system is less open to misuse.
-
There was a prevailing expectation amongst the participants interviewed that where a patient presented with a new condition, there should be some form of substantial consultation or examination – even if online – before a fit note is issued; and where a fit note is being regularly renewed for a long-term condition, there is a process for periodic review.
There was also a widespread view among participants that the problems they had identified with the system – including difficulty accessing GPs to obtain a fit note, lack of detailed advice in fit notes on ways of returning to work, and potential misuse – are made worse largely by capacity, staffing and other challenges within the NHS.
Conclusions
Overall, the 2022 reforms have been well-received and seen to be making a positive contribution to patient care in 2 main ways. Firstly, patients faced fewer delays or additional hurdles when obtaining a fit note. Secondly, other HCPs could use their specialist knowledge to have better work and health discussions and tailor fit notes more to the needs of their patients, including facilitating a phased or partial return to work. This was complemented by the likelihood that other HCPs may be able to spend longer with the patient in the initial consultation and might also provide a series of treatment sessions. The research also indicated HCPs felt there had been some modest reductions in workload for HCPs and administrative staff. Neither change had undermined confidence in the fit note system.
The take-up of extended certification is limited at present but likely to diffuse further through the system, for example as HCPs who have issued fit notes in one care setting move to another. This process could potentially be accelerated through additional communications within the HCP professions, which could be based on the drivers and barriers to uptake identified in the report.
Acknowledgements
We would like to express our thanks to analytical and policy staff within the DWP and DHSC Joint Work and Health Directorate for their invaluable advice and feedback; to our colleagues Stephen Rooney and Zaaki Ahmad for their contribution to the fieldwork and logistics; to Roots Research and YouGov for their specialist support; and to the many healthcare professionals, employers, patients and members of the public who gave up their time to contribute to our research.
Authors Details
James Humphreys is a director of Woodnewton and is a specialist in behavioural change and policy development. He works extensively in the health sector in areas such as prescribing, patient involvement and medicine safety. He was formerly a senior civil servant and a visiting Professor of Government at City University London.
Mark Gill is a director at Woodnewton and has led many research projects to inform policy and service design, including in health, social care and education. He was formerly head of political and public sector employee research at Ipsos MORI and is a board member of the World Association for Public Opinion Research.
Glossary
| Term | Definition |
|---|---|
| Care setting | The physical space or organisational unit through which care is provided to patients, which might include a hospital, a GP surgery, a specialist clinic or even care provided in a patient’s home. |
| Integrated Care Boards (ICBs) | NHS organisations responsible for planning health services for their local population. There are 42 ICBs in England. |
| Fit note | The name commonly given to the Statement of Fitness for Work issued by a healthcare professional following a health and work assessment. It provides advice about the impact of a health condition on someone’s fitness for work and may enable access to health-related benefits or evidence of eligibility for Statutory Sick Pay (SSP). |
| Healthcare professional (HCP) | Is a qualified and professionally regulated medical person who can provide medical advice and treatment to patients. |
| MED3 | Statement of fitness for work form or fit note. |
| National Health Service (NHS) | Unless otherwise specified, when reference is made to the NHS within this report it applies to NHS England, NHS Scotland, and NHS Wales. |
| Occupational Health | Advisory and support services that help to maintain and promote employee health and wellbeing. They provide direct support and advice to employees and employers. |
| Occupational Therapist | Healthcare professional who helps people who have difficulties completing tasks or activities at home, school or in workplace because of disability, illness, trauma, age, or other long-term conditions. |
| Personal Independence Payment | Is a non-means-tested benefit to help with extra costs arising from health condition or disability. |
| Pharmacist | Healthcare professional qualified to advise, prepare and dispense medicine. |
| Physiotherapist | Healthcare professional who helps restore movement and function in those affected by injury, illness, or disability. |
| Primary care | GP surgeries and other health services providing initial assessment or treatment and referring on to secondary or specialist services as required. |
| Secondary care | Hospitals and other services providing specialist care which are in general accessed through referral from primary care provider. |
| Self-certification | If employee is off work for 7 days or less, they are not required to provide medical evidence to their employer that they have been ill and can just confirm to their employer they have been ill. This is known as ‘self-certification.’ |
| Statutory Sick Pay (SSP) | The basic statutory payment eligible employees may be entitled to if they are unable to work because of illness. It is paid by employers from fourth day of sickness and for up to 28 weeks. |
| Telehealth | This is used to cover the use of digital, IT and communications to provide healthcare remotely, and includes consultations by phone and video links and online systems for booking appointments |
| Universal credit | A monthly benefit payment for those of working age, including those who have health conditions or disabilities, to help with their daily living costs. A person may get Universal Credit if they are out of work or in-work and have low earnings. |
Abbreviations
| Term | Definition | |
|---|---|---|
| DHSC | Department of Health and Social Care | |
| DWP | Department for Work and Pensions | |
| ELFH | E-Learning for Healthcare | |
| FN | Fit note | |
| GP | General Practitioner | |
| HCP | Health Care Professional | |
| HR | Human Resources | |
| OT | Occupational Therapist | |
| HiEB | Health is Everyone’s Business |
1. Introduction
Woodnewton was commissioned by Joint Work and Health Directorate, a joint unit for the Department for Work and Pensions (DWP) and Department of Health and Social Care (DHSC), to evaluate 2 legislative changes to the ’Statement of fitness for work form’ (MED3), commonly known as the ‘fit note’. In 2022, regulations were amended to allow digital certification of fit notes and to enable 4 additional groups of healthcare professionals (HCPs) to assess patients’ fitness for work and issue fit notes.
When someone is not well enough to work, the state may provide a range of protection and support. This includes, for example, ensuring that they have a minimum level of income until they are able to return to work. An individual can declare to their employer that they are unable to work for a period of up to 7 days (through ‘self-certification’). After the first 7 days, an employee can be required by their employer to provide medical evidence, which can be in the form of a fit note from an eligible Healthcare Professional (HCP). Other types of evidence can also be accepted by an employer. The issuing of a fit note involves the HCP undertaking an assessment of how the person’s health has impacted their fitness for work. The assessment is used to determine if the person is ‘not fit for any work’ or ‘may be fit for work’ if certain workplace adjustments are put in place, such as amended duties or altered hours.
Before 2010, this kind of certificate was generally known as a sick note and was limited to confirming that a patient had a condition that prevented them from working. The changes in 2010 gave doctors the option to set out ways in which the patient could return to work, for example if their employer reduced their hours or gave them different duties. This emphasis on the potential ability of patients to work was reflected in the new name: fit note. Although not directly the subject of this evaluation, the 2010 reforms provide important context.
1.1 The 2022 reforms
Fit notes are the primary form of medical evidence used to support payments of Statutory Sick Pay (SSP) and certain DWP benefits. Two legislative changes were made to improve the fit note in 2022. Prior to this, only registered medical practitioners (usually GPs but also hospital doctors) were authorised to issue fit notes, and regulations required that the fit note was signed in ink by the issuer. In recognition of the move towards multi-disciplinary teams in primary care settings, the potential to reduce pressure on doctors and potential to improve quality of health and work conversations with those seeking a fit note, regulations were amended in July 2022 to expand the range of HCPs who could issue a fit note. The professions included in the new regulations are registered nurses, occupational therapists (OTs), physiotherapists, and pharmacists (working in GP surgeries or similar care settings but not in retail or community pharmacies). Regulation changes in April 2022 also enabled the fit note to be authorised and issued through secure digital means by removing the requirement to be signed in ink, removing a barrier to fully digital completion highlighted during the COVID-19 pandemic. These legalisation changes in 2022 applied across England, Scotland and Wales and were mirrored in Northern Ireland.
GP IT systems were updated to support the regulatory changes and a project is under way in secondary care to embed the fit note in IT systems which will remove the need for handwritten forms. Certifying HCPs, including doctors within GP practices, can continue to print a system-generated fit note at a patient’s request. HCPs who can now legally issue fit notes are not obliged to do so, and their employers (for example, within a GP surgery) are not obliged to let them. They should consider their scope of practice and ensure they have relevant skills and experience. The expectation behind the 2022 reforms was that they would be taken up first where they provided the greatest benefit either in reducing workloads on GPs, or improving patient outcomes, or both. Settings where the reforms might give rise to practical difficulties could choose not to implement them.
1.2 Research aims
The research explored the experiences and perspectives of HCPs, patients and employers to the 2022 fit note reforms. The aims of this research study were to:
-
evaluate whether these reforms are working as intended to meet commitments outlined in the Government’s response to ‘Health is Everyone’s Business’ (HiEB, 2021) to “enhance work and health conversations and the support provided to both individuals and employers”
-
identify barriers to, and enablers of, successful implementation of these changes at both the individual and practice level
-
describe and understand the impact of reforms on GPs and practice managers in relation to administrative burden
-
describe and understand the range of experiences of fit notes from HCPs, patients, and employers through themes emerging from the qualitative data
This report covers research conducted in 2 waves. The first wave focused on the knowledge, attitudes and behaviours towards the 2022 reforms of doctors and ‘in-scope’ HCPs (that is, those in the 4 groups of HCPs who can now issue fit notes following the legislative change). This wave covered digital certification and extending certification to additional groups of HCPs. The second wave explored in more depth the views of GPs and newly in-scope HCPs who can now issue fit notes, particularly towards the extension of certification, and expanded the research’s scope to also capture the views of patients and employers.
1.3 Methodology
NHS England[footnote 1] publishes quarterly data derived from fit notes issued electronically by GP practices in England. Since September 2023 this has also included data on the issuing of electronic fit notes by professional group (for example, GP or nurse). This kind of quantitative data is invaluable in showing what is happening, but it cannot give insights into why it is happening, that is, the reasons individual HCPs or organisations such as GP practices might decide to adopt these reforms, or not, and the impact on their wider roles, patient care, health outcomes, workload or job satisfaction. It also does not capture the perspectives of patients or employers towards the reforms.
A predominantly qualitative approach was adopted as the primary method for both waves of this study, as it allowed the research team to interview a broad range of relevant participants and develop a clearer understanding of their experiences, perspectives and preferences through in-depth interviews and focus groups. Quantitative research was also carried out with members of the public, using a survey to help establish the extent to which the views of the patients interviewed were representative of the wider public.
The qualitative approach also allowed us to set the views of those who took part in the interviews and focus groups participants in context, for example, how HCPs attitude towards the 2022 reforms might be influenced by their wider experience of changes and reforms within healthcare, or how their decision whether or not to adopt the reforms might depend on their personal priorities for career development. It also helped to build up a picture of the sources or channels of information which participants drew on in learning about the reforms and coming to decisions about participation. These included briefings from management, professional journals and informal conversations with colleagues.
Across both waves of research, 84 healthcare participants who work within the NHS were recruited from across Great Britain and took part in the qualitative discussions through a mixture of in-depth interviews and focus groups. The healthcare participants included general practitioners (GPs), GP practice managers, hospital doctors, and HCPs now able to issue fit notes following the legislative change (registered nurses, occupational therapists, physiotherapists and pharmacists based within a GP surgery). In addition, in-depth interviews and focus group discussions were held with 43 patients (who had received at least one fit note in the last 12 months) and with 28 employers who deal with fit notes in their workplace, either as managers or human resources (HR) specialists. Participants were recruited mainly from a database of over 500,000 UK adults who had preregistered to take part in research.[footnote 2] Participants were paid an incentive to take part in this research to ensure that no group was disadvantaged by, or excluded from, taking part. Payment of the incentives was not tied to completion of the interview or focus group, and participants could withdraw from the research at any time, if they wished to do so, without suffering any loss.
The profile of those taking part in the qualitative research is shown in Table 1.1.
Table 1.1: Sample breakdown by participant group for the qualitative research
| Respondent Group | Completed Interviews |
|---|---|
| GPs | 34 |
| Hospital Doctors | 5 |
| Nurses | 18 |
| Occupational Therapists | 8 |
| Pharmacists (based in a GP surgery) | 6 |
| Physiotherapists | 10 |
| GP Practice Managers[footnote 3] | 3 |
| Patients who have received at least one fit note in last 12 months | 43 |
| Employers | 28 |
| Total | 155 |
Most of the healthcare participants (74 out of 84) interviewed, worked in primary care settings such as GP surgeries. The remainder worked within hospitals (which are known as secondary care settings). Of the 42 HCPs who are now eligible to issue fit notes following the 2022 policy changes (nurses, pharmacists, physiotherapists and occupational therapists), the majority interviewed had started to issue fit notes. However, some eligible HCPs who had not made use of these new powers were interviewed to provide additional insights into the barriers to uptake.
The patient and employer participants were adults of working age and included a balance by age, sex/gender and place of residence within Great Britain. The purpose of this was not to design a representative sample, but to ensure a good spectrum of perspectives and experiences towards fit notes and taking account of participant demographics. In addition, participants were recruited from different types of businesses, both in terms of organisation size and industry sector, to allow for a more inclusive analysis.
The interviews were conducted either by telephone or virtually (using either Zoom or Microsoft Teams) depending on the preference of the participant and lasted between 30 and 40 minutes. The focus groups conducted with patients also included a mix of in-person meetings and virtual discussions, typically lasting around 90 minutes. All interviews were conducted using semi-structured topic guides tailored to each audience group. Discussions were audio recorded (with the permission of participants) for analysis and quality control, but these were not shared with the client to maintain confidentiality.
Consent was also sought to having a selection of their comments included in this report to illustrate the findings. Where verbatim quotes have been used, they have been anonymised with just the participant’s occupation included to ensure participants could not be individually identified. The extent to which they represent the views of participants as a whole is made clear by the context. They are intended to provide a sense of how participants thought, and expressed themselves, about the issues raised.
The interviews and focus groups took place between January and February 2023 (Wave 1) and between May and July 2023 (Wave 2). All participants were resident in England, Wales or Scotland.
To support the qualitative evaluation, the public’s attitude towards the fit note process and the reforms was established through an online survey. This was designed and interpreted by Woodnewton and used YouGov’s ‘GB Omnibus’ for the fieldwork. The fieldwork took place between 16 and 19 June 2023 among 2,023 adults to provide a representative sample of members of the public in Great Britain. The additional data and insights generated from this survey have been integrated into the report’s analysis.
The research set out to evaluate the fit note reforms by gathering, analysing and presenting the experiences and perceptions of patients, HCPs, employers and members of the public. It is not a technical description of how the 2022 reforms are working, or of the wider operation of the fit note system.
1.4 COVID-19
These reforms were introduced relatively soon after the COVID-19 pandemic, which had a significant impact on every aspect of the health service. There are some clear relationships between COVID-19 and the reforms, particularly the greater use of remote consultations and other forms of telehealth during and after the pandemic. These are discussed in the relevant sections of the report.
There is also the wider question of whether the evidence in this report represents a temporary state, and attitudes and behaviours might move back towards their original position prior to the pandemic; or whether this is the ‘new normal’. The evidence from this research and supported by findings in other post-COVID healthcare research, strongly indicates that the picture in this report is essentially the ‘new normal’.
1.5 Structure of report
The report is structured into following chapters:
-
Chapter 2 examines participants’ perceptions and experiences of the introduction of digital certification of fit notes, including the drivers or barriers that might encourage or discourage uptake.
-
Chapter 3 examines participants’ perceptions and experiences of the extension of certification to 4 new groups of HCPs, covering drivers and barriers, as well as exploring themes such the relevance of HCP scope of practice and the role of training and support.
-
Chapter 4 presents wider perceptions of the fit note system to help provide some context to the views of patients, employers, HCPs and members of the public towards the 2 reforms.
-
Chapter 5 examines how the attitudes of HCPs towards the 2 reforms might be distinguished from wider expectations of how change is managed within the National Health Service.
-
Chapter 6 presents conclusions on the impact of the 2022 fit note reforms including an overall assessment of their impact so far and their likely dissemination in the future.
2. Digital certification
The focus of the evaluation was the impact of 2 legislative changes introduced in 2022: digital certification of fit notes and extending certification. This chapter explores participants’ experiences and perceptions of digital certification, which is defined as the removal of the requirement for fit notes to be signed in ink (‘wet signature’) and the move to digital authorisation within General Practice (GP) IT systems. This regulation was introduced on 6 April 2022.
2.1 Awareness
Almost all healthcare professionals (HCPs) in primary care who were issuing fit notes did so using an electronic signature. There was also high awareness of the change, in the sense that HCPs knew that a ‘wet’ signature was not necessary, but few participants recalled exactly when or why this change was made and there was low awareness of it as a specific reform. Many assumed the change was related to COVID-19 (that is, reducing the number of patients physically coming to a surgery) and general improvements in IT infrastructure. As some GPs had already begun issuing fit notes in electronic form prior to the legislative change, even though they did not have a legally valid wet signature, and this was accelerated by the COVID-19 pandemic.
I only realised that the admin stopped asking me to sign them. Previously we saved it to the record and the patient would come to collect it and the admin team would print it off and bring it in to be signed.
(GP)
In secondary care, awareness and uptake of this change was much less wide-spread and most participants said they continued to use paper forms. This was mainly because the IT systems they were using at the time of the fieldwork did not support digital fit notes, though some HCPs also expressed a preference for paper forms, for example because they were moving from ward to ward and would not want to have to find a workstation or a functioning printer on each ward.
There was low awareness of the change amongst patients, even when it became clear in discussions that they had themselves been issued with a digital fit note. All patients who expressed a view on this issue thought of the digital signature as an unimportant technical change to enable digital fit notes, and it was the latter that they had views about – mainly positive. In turn, digital fit notes were seen as another aspect of the wider move towards digital in healthcare, expedited by COVID-19. Amongst employers, awareness was higher: some Human Resources (HR) participants had, for example, been informed of the change and amended their internal company procedures accordingly before they started to receive digitally certified fit notes.
2.2 Drivers of implementation
Digital certification was seen as a positive and natural evolution of improved IT and better patient service. Very few participants across all groups felt it was a negative or controversial decision and they saw parallels with other changes in healthcare delivery, such as the ability to send electronic prescriptions directly to a pharmacy.
Healthcare Professionals
In general, HCPs were very positive about digital certification. They saw the change as part of making the entire fit note process digital, and so more efficient. Overall, it meant:
- it was quicker, easier and more convenient for HCPs to complete the form, particularly as the fit note process was now integrated into the patient’s electronic records
It’s quick and easy to do. I don’t have to deal with the printer, NHS printers never work. It’s not bothering the patient to have to come back to collect it. There are efficiencies to it, and there’s a digital record of it.
(Physiotherapist)
- there was a reduced burden on administrative or reception staff allowing them to focus on other tasks. Overall, this reduction appeared to be quite modest, but some participants felt it was significant in their particular care setting
It makes a massive difference being able to send them out electronically, more convenient for the patient, more environmentally friendly, less admin time for us.
(GP)
-
it was more convenient for patients to receive the digital fit note as, for example, they do not have to go to the GP surgery physically to collect their fit note
-
it was now easier for the HCP or patient to forward the fit note to the employer digitally rather than sending by post or having to take a physical fit note into work. Participants gave examples of submitting fit notes by email, text (SMS) and social media platforms such as WhatsApp
Now you can email it to the employer, or if they need it for Universal Credit. It used to be time consuming to issue fit notes but now it’s easy to issue and the admin team can issue additional copies easily from your original one.
(Nurse)
- it was viewed by some as potentially more secure, although there were mixed views on this, as some participants thought it might be easier to alter than a paper-based form
More secure, efficient less chance of things going astray, quicker and cleaner too.
(GP)
Very few HCPs saw any disadvantages to the introduction of digitally certified fit notes, in part because it was still possible to issue a printed fit note if circumstances required this.
When asked, almost all HCPs said they did not recall employers rejecting or questioning fit notes because they have been signed electronically rather than physically. One isolated example of an issue with an employer suggests that these are likely to be the ‘odd cases’ inevitable within any system:
I had one patient who came back to me saying their employer had questioned why their fit note was not signed. The patient was living in the UK, but employer was based in Italy and the Italians questioned why there was no signature.
(GP)
Employers
Most employers had received digitally certified fit notes and were happy to do so. In general, they were not aware that there had been a change to the law to enable this but had accepted it as part of a wider move to telehealth, driven largely by the COVID-19 pandemic. In most cases, employers already used electronic systems for employee records so would either scan the paper fit note themselves or receive a scan from their employee by email (or in some cases a picture taken on a smart phone by text message). In this sense, a digital fit note was more convenient and was particularly helpful where employees were working from home.
It makes absolute sense to do this digitally – if someone’s been assessed, why not certify that online?
(Employer)
As well as the benefits for the business, employers also commented on how digital fit notes were much more convenient for their employees, and they saw benefits for healthcare staff and the NHS.
Some employers had reservations about digital fit notes, largely because they believed there was potential for employees to amend the PDF (for example, extending the time the fit note covered, or changing the name of the person it was issued to). However, they also had reservations about scans of paper fit notes, which they felt could be manipulated in similar ways. In the discussion on security, it was apparent that some employers were not aware that the digital and printed fit notes include a QR code they could scan to check it was authentic. Overall, they tended to feel that the change to digital fit notes was inevitable, and that the benefits outweighed any potential there was for possible misuse by employees.
Patients
Amongst patients interviewed, the move to digital certification was generally seen as sensible or inevitable, with several participants saying it was what they would expect ‘in this day and age’. In many cases, patients had hardly noticed the change, and this appeared to be due to the wider switch to telehealth during the COVID-19 pandemic. They did not report any problems with employers accepting digital fit notes, who were in general using electronic employee records anyway, with many believing that a digital fit note was easier and faster for their employers to process. There were also some examples given of where a digital fit note was preferred by the patient beyond simple convenience as illustrated in the following quote:
I was issued with a paper copy that the GP printed off and signed, and I had to hand it to my employer. I was suffering from depression, and I wasn’t comfortable with going into work. I had to get a friend to take it. So, the digital format is perfect.
(Patient)
2.3 Barriers to implementation
A small number of HCP participants did not use digital certification. The reasons offered were:
-
Attitude of HCPs: one GP refused to use digitally certified fit notes because he was concerned about people requesting a fit note fraudulently. Therefore, he insisted on seeing patients in-person and physically signing the form. Some other HCPs felt that patients could potentially change a digitally certified fit note.
-
Demographics of patients: a couple of participants felt that digital fit notes were not suitable for some of their patients because of lack of access to or confidence with computers or smartphones. In such cases patients themselves preferred physical notes, and the current fit note regulations allow HCPs the option of providing patients with either a digital or a printed fit note.
We don’t use digital signature because we have demographic that tends to be older and not always comfortable with email. Also, it’s just more secure if they come in and give name, date of birth etc.
(Practice Manager)
- Inadequate IT systems: a small number of HCP participants in both primary and secondary care also reported that either their IT system was not capable of generating electronic fit notes / digital certification or that the system was too unreliable.
We do issue digital fit notes. We switched over systems post-Covid but it goes down every week or so and there’s always a queue for the IT helpdesk. So, I prefer to use paper.
(Physiotherapist)
3. Extending certification
This chapter explored participants’ views and experiences of the other fit note reform implemented in 2022, which was extending the ability to certify fit notes to 4 additional healthcare professions: registered nurses, occupational therapists (OTs), physiotherapists and pharmacists (based in a GP setting). Prior to this only doctors were able to legally certify fit notes. This legislative change came into force on 1 July 2022.
3.1 Awareness
There was a high level of awareness of this reform across the healthcare professional (HCP) participants. This may to some extent be due to the research recruitment process, as participants were informed of the broad topic area (that is, a discussion about fit notes) when being recruited to take part in the qualitative discussions. Significantly, many healthcare participants felt that this policy change had not been well communicated to them. Although many heard about it through formal means – such as an email from the practice manager or during a weekly team meeting – a number also commented that they had found out “by chance” through informal means such as social media. Some HCPs did admit that they did not have the time or inclination to keep as informed of developments in their profession as they would like.
I found out by reading a newspaper incidentally one day – this was something about my profession and not the way I should have found out.
(Occupational Therapist)
When probed, most healthcare participants did not feel many patients or members of the public were aware that some HCPs, who are not doctors, are now able to issue fit notes. This was felt to partly be due to relatively few fit notes were being issued by these HCPs who are now eligible to issue fit notes. They also did not recall any marketing campaign to inform the members of the public of this change.
I didn’t know the extension before this interview and I’ve not seen anything advertised. Maybe publicity would be useful and that might encourage patients to seek advice from healthcare professionals other than GPs.
(GP)
Findings from the online survey of the public’s knowledge of and attitudes to fit notes showed that the survey participants had low levels of awareness of this reform. It found that the majority of adults surveyed (84%) believed that GPs were able to issue fit notes. Two-thirds (65%) also believed that a hospital doctor or consultant would be able to issue a fit note. However, considerably smaller proportions of those surveyed thought other HCPs now legally able to certify fit notes, could do so (Table 3.1).
Table 3.1: Proportion of survey participants who correctly identified the HCPs who could issue fit notes
| GP % | Hospital Doctor % | Nurse % | Physiotherapist % | Occupational Therapist % | Pharmacist in GP Surgery % | |
|---|---|---|---|---|---|---|
| All | 84 | 65 | 18 | 14 | 18 | 9 |
| Men | 78 | 58 | 18 | 15 | 18 | 10 |
| Women | 89 | 71 | 18 | 13 | 18 | 8 |
| Age 18 to 24 | 66 | 51 | 24 | 23 | 24 | 16 |
| Age 25 to 34 | 88 | 65 | 26 | 19 | 24 | 10 |
| Age 35 to 54 | 82 | 60 | 20 | 14 | 20 | 8 |
| Age 45 to 54 | 86 | 65 | 20 | 15 | 21 | 9 |
| Age 55+ | 87 | 70 | 12 | 10 | 12 | 7 |
Base: 2,023 GB adults.
Source: YouGov GB Omnibus Survey, 16 to 19 June 2023
Survey participants were twice as likely to correctly believe a pharmacist in a GP surgery could issue a fit note rather than one based in the community or high street (9% vs. 4%), but the 9% figure still represents slightly less than 1 in 10 people realising that a pharmacist in a GP surgery could legally certify fit notes. Twice this proportion believed nurses and occupational therapists (both 18%) were able to legally issue fit notes, while 14% believed physiotherapists could issue fit notes. Overall, just over a third of respondents to the survey (36%), correctly identified at least one of the 4 groups of HCPs as now being able to issue a fit note.
There was no significant difference between men and women on this question. Younger adults were more likely to identify the HCPs covered by extended certification correctly. For example, twice as many 18 to 24-year-olds (23%) assumed physiotherapists could issue fit notes compared to those aged 55 years or older (10%). However, this was not necessarily a reflection of younger adults having better understanding or being better informed about issuing of fit notes, as more 18 to 24-year-olds also wrongly assumed that other HCPs could issue fit notes, for example 22% felt dentists could (vs. 12% of over 55s who said this). The 18 to 24-year-old group were also significantly less likely to say GPs (66%) or hospital doctors /consultants (51%).
Very few of the employers interviewed were aware of the extension of certification to other HCPs. No patterns in levels of awareness among employers were identified (for example, larger compared to smaller employers, or by sector) though this may simply reflect the relatively small sample size.
3.2 Drivers of implementation
In contrast to the widespread adoption of digital certification, it is likely that relatively few newly eligible HCPs were issuing fit notes when this research took place. Although this cannot be determined precisely through qualitative methods, the research suggests relatively low numbers based on (a) the difficulty in tracing HCPs now eligible to issue fit notes, who are actively issuing fit notes, during recruitment of participants for the research, (b) those that are issuing fit notes tend to be more experienced and senior, and (c) feedback from those participants interviewed, who suggest that uptake is currently fairly low.
Amongst HCP participants, the main perceived benefits were that it:
-
provided better patient care and improved the patient journey
-
reduced the workload for GPs
-
allowed GPs to focus on different patients / other consultations
-
formalised existing informal practice
-
other HCPs are as well placed as, if not better placed than, a GP to issue fit notes
-
recognised the skills, expertise and status of relevant HCPs
Of these, better patient care and improved patient journey was the benefit which HCPs raised most often, particularly those providing extended treatment to patients (such as a course of physiotherapy). Extension of certification allowed them to provide a more ‘joined-up’ service and saved their patients the trouble of having to make a separate GP appointment, potentially at a different location, and likely to involve some delay in securing their fit note. It also allowed them to discuss their patient’s work within the context of their condition, enabling them to provide more detailed guidance to an employer about ways in which the patient could re-engage with work which were likely to be more realistic and more effective.
Nearly all HCPs participants – both GPs and other HCPs – agreed that in many cases GPs’ time was better spent dealing with other issues instead of issuing fit notes and these reforms would help to reduce GPs’ workload (or at least free up their time to deal with other or more complex cases). There were some differences in views about the time savings for GPs. Some thought these were significant, because patients would not need to make a separate appointment to see a GP for a fit note, after having also seen another HCP. Some GPs, though, said that fit note appointments were usually very brief and (in the context of having a long list of patients to see and usually only around 10 minutes allocated to each), a short appointment could help GPs catch up when other consultations over-ran. Routine appointments for fit notes were welcomed for this reason by some GPs. Overall, though, the extension changes were perceived positively.
The more other professionals can do this, the easier the workload for GPs - it’s a great help.
(GP)
These are positive changes. Fit notes were a bit of a bottleneck, particularly for the ‘barn door’ ones, for example where the hospital hasn’t issued one after surgery. For more complex cases you still need a GP.
(GP)
In primary care practices, in most cases, the decision to allow other HCPs to sign fit notes was made by the senior GPs (GP partners) and their attitude largely determined whether their practice implemented the reforms. Some participants also stated that they had received guidance from their Integrated Care Board (ICB), which encouraged their practice to allow newly eligible HCPs to issue fit notes. Although there were also examples of these HCPs taking the initiative in adopting extended certification, usually by raising it with the management of their care setting (for example, at a weekly team meeting). In such cases, the reasons given for this were that it provided better care to the patient, contributed to the working of the care setting and extended the professional practice of the HCP.
The senior partner made that decision, so we’re not burdened with just doing sick notes. You don’t need a ten-minute consultation just for a fit note. It frees up our time to deal with chronic illness and other things.
(GP)
I made the decision myself. I thought it would be really helpful and make my practice more effective.
(Physiotherapist)
Some HCPs also reported that the legislative changes enabled them to formalise existing practices. Before the policy changes, some GP surgeries were effectively allowing ineligible HCPs to issue fit notes: the HCP would complete the form following their assessment of the patient and the GP would act as a “rubber stamp” in signing the note. This reflects the common view among HCPs that issuing a fit note for most patients is relatively straightforward, particularly when the medical need is clear, and does not rely on skills that only GPs have. Issuing fit notes is also seen as low risk – if a fit note is issued incorrectly there is little or no risk of harm (in contrast, for example, to using incorrect medication).
Many participants also noted that often those HCPs now eligible to issue fit notes can be better placed than doctors to issue fit notes or it is more appropriate for them to do so. The reasons given were that they were able to spend longer with a patient and so could carry out a more thorough work and health assessment or would have more experience in dealing with the condition and so were able to give better workplace advice. In these cases, allowing these HCPs to issue fit notes made better clinical sense.
GPs don’t have the training in occupational health and can’t be expected to make decisions on adjustments they’re not qualified to make. For example, occupational health departments coming back for additional comments or the patient comes back to us asking ‘this is what occupational health have said and my company wants to know if you think that’s ok’.
(GP)
It made sense, especially as I was seeing, assessing, diagnosing, requesting treatments etc – and if I would get to the point of saying someone was not fit for work, I would have needed to get a GP, take up their time, on something I’m more than capable to do.
(Nurse)
Among these newly eligible HCPs, some issued fit notes because it fitted in with their existing ways of working and helped them to provide more seamless and holistic care to patients. For others, undertaking the specific training and being qualified to administer fit notes was part of their career progression and professional status. For some of these HCPs, it was a combination of both reasons.
I know my patients as I get the opportunity to spend time with patients – my appointments are an hour long. I do a holistic assessment rather than just medical. I’ve got years of experience doing vocational rehab. GP might just write “phased return to work” which is very vague.
(Occupational Therapist)
It gives me more feeling of responsibility and autonomy which I wanted to have. It enables more efficiency so I’m not creating duplicate appointments with reception and admin staff and bothering the GPs. It enables me to be a little bit more respected by patients as well because I’m not restricted as much in what I can and can’t do.
(Physiotherapist)
No instances were reported within this research of these HCPs feeling pressured into taking on the role of issuing fit notes.
3.3 Barriers to implementation
The research revealed 5 core barriers to extending certification. These are:
-
lack of awareness of the reforms
-
senior GP reluctance to allowing other HCPs to issue fit notes
-
lack of relevance of fit notes to the work of some of the newly in-scope HCPs
-
skills and attitudes of the newly in-scope HCPs to taking on new responsibilities
-
existing workload
The research indicated that a lack of awareness of extending certification to other HCPs may not necessarily just be lack of knowledge of extended certification itself. It may also reveal a lack of understanding of the practical implications of the change, such as who precisely would benefit from being able to issue fit notes, what support or training is required, and what level of monitoring or accountability is involved. In many cases, relevant HCPs and their senior GP colleagues reported that they would want to see evidence and examples of the practical benefits of the change and an understanding of how any risks can be mitigated. For example, if a patient booked an appointment to secure a fit note, a GP might spot an unconnected underlying health condition, while a physiotherapist or occupational therapist might not have the skills or experience to do this. Others also highlighted that changes in working practices can take a long time to be accepted and implemented and that extended certification was still a recent innovation.
It’s difficult to change people’s mindset and we are talking about less than a year since the change took place.
(GP)
Some GPs – and based on findings from this research this is likely to be a minority and probably focused among those nearer retirement – are more resistant to allowing other HCPs to take on the role of issuing fit notes. The points these GPs made in the interviews included:
- assessing fit notes is a medical responsibility for which GPs are best suited, as it was felt newly eligible HCPs will face more pressure from patients to issue fit notes where they are not warranted because these HCPs might not be seen to have the same status or authority as doctors
Patients may not hold other professions in as high regard as they should. So, I’d worry it’s open to abuse.
(GP)
-
it is the responsibility of the GP to plan a patient’s care. This reflects the more traditional doctor-led model of care, which has generally been superseded by a multi-disciplinary approach in which a range of HCPs work collaboratively
-
introducing the reform in their care setting would take up management time and incur training and other costs but might not deliver much improvement in care outcomes. It might also divert management and other resources away from other potential improvements in the services they provided, which they felt might offer a better ‘return’ on that investment
-
the benefits of extending certification are modest as they felt fit notes do not take long to issue
Why have they extended it? It’s an empty gesture. During a consultation, I’m doing the work for a fit note in the background. It maybe adds 30 seconds.
(GP)
The research also explored more widely HCPs’ views on whether those HCPs now able to issue fit notes would be more likely to be pressured by patients to issue a fit note than a doctor. The more widely held view was that the personality of the individual HCP is a more important factor in how ‘easily’ that they would provide a fit note. Several HCPs (including some GPs) went further, saying that that the newly eligible HCPs would be less likely than doctors to give a fit note inappropriately because they were newer to this role and therefore more likely to be cautious; and tended to be stricter in following guidance than a typical GP.
I don’t think it differs other than when GPs need to get a patient out the room, so they say yes to requests. Some patients think nurses will give them notes quicker than a GP, but I tend to question more and go into reasons they are wanting a sick note.
(Nurse)
GPs are just as easy to persuade as nurses. I declined someone, but a GP issued it. Whenever I issue a fit note, I want to make sure there is a plan to follow… we can be more ruthless than GPs. We want to make sure we are doing it the way we have been told to do it. Less blasé than doctors.
(Nurse)
In addition to lack of awareness and any resistance from senior GPs, a further barrier to uptake is whether a HCP now eligible to issue fit notes, sees the right types of patients to warrant doing the training to allow them to issue fit notes.
Our nurse practitioner mainly sees patients with coughs, colds, ears etc., which reflects her skills set rather than joints/pains, which are more common issues where a fit note might be issued.
(GP)
I struggle to see how a pharmacist would be useful to issue them. I can see other healthcare professions, like a physio, it would be useful for them to be able to.
(Pharmacist)
The skills and attitudes of the HCPs now able to certify fit notes were also identified as significant barriers to uptake. More junior HCPs are unlikely to be asked to take on these responsibilities, for example, uptake among nurses tends to be with advanced nurse practitioners or nurses with prescribing powers. Several participants provided feedback that lack of confidence or people’s worry about taking on any additional legal responsibilities would put them off.
It’s a legal thing at the end of the day – it becomes your responsibility and you can be held accountable.
(Occupational Therapist)
I think that the nurses are just not feeling confident enough to do it. Because it’s new and they need to do new training for it, they’re not really wanting to do it. Anything that’s new always takes a long time to come into place.
(GP)
Furthermore, there was a perception among some HCPs that some of the most experienced HCPs who are now eligible to issue fit notes may not wish to take on the additional responsibility, as they are at the stage of their career where they do not want further career development or perceived stress. Some of these experienced HCPs also stated that they did not want this added responsibility.
A lot of my colleagues, especially older staff, would never give someone a fit note… they just tell the patient to go to the GP. They just don’t want the stress and they are used to working in a certain way.
(Physiotherapist)
Some of our eligible HCPs are coming up to retirement and they don’t want to do more training so they are not interested in issuing fit notes.
(Nurse)
Finally, even where there was awareness of the policy change and acceptance by the GP partners and relevant HCPs that patients would benefit from the change, some participants explained these had not yet been implemented due to staff shortages or current working pressures. In addition, some smaller GP surgeries mentioned that they did not have any of the relevant HCPs working for them, so there is not anyone other than the GP available to issue fit notes.
We are one nurse down and have been for a year, so the existing nurse doesn’t have capacity to take this on. So, it didn’t make sense to ask her to.
(Practice Manager)
Everyone is really busy, so trying to get people to take on different roles is always tricky. You need to do an e-learning course – you have to be a bit motivated in order to want to do it and have the extra responsibility.
(GP)
3.4 Scope of practice
In almost every case, the decision whether to enable the newly eligible HCPs to issue fit notes within a care setting was taken by doctors, and usually by the partners in GP surgeries. In general, doctors were receptive to the reform extending certification to a wider range of HCPs, so long as these HCPs are acting within their scope of practice, that is, they have the skills, training and competence to carry out the task properly. For example, several GPs commented that physiotherapists would be well-placed to issue fit notes for conditions they were qualified to treat such as musculoskeletal conditions, but not more widely.
It might be a good idea to limit to requests that are in line with their work – if it’s an MSK issue then a physio should be able to issue a fit note. But obviously they are not trained to assess other medical problems.
(GP)
This applied across all 4 groups of HCPs who could now issue fit notes, though as with employers and the members of the public (see Section 3.5), GPs were more cautious about pharmacists.
Tricky one. Certainly, there’s some role they can play, but how many are dealing with patients that need a condition for more than 7 days off work? They should be seeing a GP rather than just a pharmacist. Perhaps for certain medications, like chemo, that could be appropriate.
(Hospital doctor)
In a small minority of cases, GPs questioned whether other HCPs should ever issue fit notes, even when provided with training and support, suggesting they did not have sufficient general medical training or experience, or the confidence to make independent judgements and not just follow a defined procedure, or the self-confidence to deal with difficult patients. They also expressed concerns that GPs would end up being drawn into greater supervision of these HCPs because they felt they would retain ultimate responsibility for ensuring patients received proper care. It should be noted that these reservations appeared not to be restricted to this fit note reform: some of the GPs who held these views were also critical of other innovations which could be perceived to impinge on the traditional role of the GP.
The need to link fit notes to scope of practice was a view also shared by many of the HCPs now able to issue fit notes. They thought it was vital that in-scope HCPs only issued fit notes when they had the appropriate skills and training, both in general and for the specific patient and condition. Where other HCPs in a care setting did not have the relevant skills and experience, or where a patient had a complex set of conditions, the GP might be better placed to issue the fit note.
I wouldn’t expect a physiotherapist to be handing out fit notes for anything unless it was in their field and part of their consultation.
(Nurse)
I rarely do extensions myself, because I think if someone is off for a protracted period, they should have a GP have a look at their case. For most illnesses, unless there’s something seriously wrong with you, you should be better within a week, and most people self-certify for that time, so I don’t give out fit notes very easily.
(Nurse)
3.5 Patient and employer attitudes
Patients and employers were asked about their attitudes towards extending the right to issue fit notes to the 4 groups of HCPs. The main reasons given in support of the extension were:
- it helped address the problem of access to GPs, which was a concern expressed strongly by many participants
To even get through to see a GP these days is equivalent to winning the lottery.
(Employer)
- it freed up resources within the healthcare system as it enabled GPs to concentrate on other aspects of their responsibilities
It allows GPs to focus on other more complex things and is a more efficient use of resources in the system.
(Employer)
- it was felt these 4 groups of HCPs would have a good knowledge of the patient, because they were treating them, not arranging treatment for them (as a GP might)
Nurses have a really good understanding of what is going on… there are so many qualified professionals who can do this.
(Employer)
- these HCPs had specialist knowledge – for example, physiotherapists had expertise on assessing and treating back pain – which was directly relevant to assessing fitness to work or advising on adjustments in the workplace
There were some reservations expressed by patients and employers about the extension. These were mainly about ensuring that HCPs only issued fit notes within their scope of practice and that proper safeguards would be in place.
There definitely has to be training – including a basic list of questions they should ask – and questions or guidance depending on the conditions or symptoms.
(Employer)
A physio is not going to sign you off if you have a stomach bug, I hope!
(Employer)
3.6 Impact
Most HCPs were positive about the impact of the extension of certification, with little negative feedback. None of the participants reported that they had introduced the extension and then reversed that decision. From the perspective of many GP participants, the main impact was sharing the fit note workload, which meant GPs had more time to commit to other responsibilities, though they were not specific about how they would use this extra time. The GPs interviewed found it hard to say with confidence the extent to which implementation of the changes has reduced their workload. In part, this was because they said these reforms have been introduced against the background of increased demand from people with long-term health conditions. Most typically, GPs felt it has helped to some degree, but was not a transformational change, usually because among the HCPs now able to certify fit notes, only the more senior staff within a care setting would issue fit notes.
It hasn’t made a massive difference as only our nurse practitioner was affected.
(GP)
For HCPs now able to issue fit notes, the impact has clearly been significant and positive. There was a strong sense from these HCPs that the reform allows them to provide more holistic care, reduces waiting times for patients and avoids duplication of healthcare resources. They explained this led to more team working, better job satisfaction and improved status and morale from being able to make greater use of their professional skills and experience.
Being able to officially and legally sign sick notes has been a big change. For 20 years I’ve been filling them in and giving them to a GP to sign. It was ridiculous that after going through a whole episode of care with a patient, I wasn’t able to do that – even though the GP was signing it without actually seeing the patient, just on my recommendation.
(Nurse)
In particular, they said it allowed for a more thorough and supportive discussion about the scope for patients to return to work in some form, because these HCPs usually have longer consultation slots and may also see the same patient for a course of treatment.
The fit note legislation has been fantastic. It makes total sense and streamlines what I do. I often have occupational health discussions with my patients about how their issues impact their work.
(Physiotherapist)
The reform was seen by HCPs who can now issue fit notes as positive, both for patients and the HCPs themselves. In addition, there was a shared view that while these changes may take some time to become more widespread, the direction of travel is clear and reflects how primary care is changing and making more use of multidisciplinary teams.
It’s another service that I can provide that’s relevant to our patients and saves the GPs and other people the task of just doing that as well – and I feel quite well placed to make those sorts of decisions with my background.
(Physiotherapist)
At a GP surgery level, HCPs explained this can also positively impact the wider patient-customer journey.
Workflow in the surgery is much easier. It allows me to fully care for my patient group and I still have the GP behind me if I am not sure.
(Nurse)
It’s positive. We don’t have that many patients waiting for appointments because we have good nurse practitioners who can see them and now, they don’t need a separate appointment for a GP to get a fit note.
(Nurse)
The reform also benefitted staff and patients where the latter had been referred by their GP to a specialist service, such as a pain clinic, on a different site as it avoided the patient having to make a separate visit or call back to their GP surgery to get a fit note. This helped the specialist provider offer the commissioning body a more complete service.
I don’t need to send them back to the GP. The GPs like that as well. They see it as an addition to the service we offer them when they refer to us.
(Physiotherapist)
None of the HCPs in primary care reported that employers had questioned or refused to accept a fit note that was signed by one of the newly in-scope HCPs.
Feedback from HCPs working in secondary care was fairly consistent with those in primary care. The main impact of allowing other HCPs to issue fit notes has been improved patient journeys, most notably in cutting waiting times for discharge. As with primary care, usually only more senior nurses or other HCPs will issue a fit note. In contrast to primary care, the decision to issue a fit note is often a team decision as part of the discharge procedures for a patient. Given most of these fit notes are still paper forms, several participants also reported that fit note paper pads are now kept in a more secure place in the hospital department / ward, as more members of staff now have access to them, given it is no longer just doctors who can issue fit notes.
The way HCP participants thought about the impact of extending certification was also influenced by the stage of implementation they had reached. Where the changes had only just been introduced, or where they were being implemented gradually within their care setting, the impact was less, or less easy to evaluate. Although, in those cases participants were still positive about the beneficial impact they expected to see in the future.
About 15-20% of fit notes are going to HCPs but that’s likely to rise as everyone becomes more confident.
(GP)
3.7 Types of conversations
All HCPs were asked if patients, who receive a fit note from one of the HCPs who can now issue fit notes, would have a different conversation than they would with a doctor. Some reported that the conversation would be very similar, based on the assumption that doctors would ask similar questions of their patients.
It’s exactly the same conversation. It’s all about discussing the time they need to get well and back to work; working with the employer and occupational health to maximise function based on the clinical care pathway; and making sure the patient understands their clinical pathway as well so they can alert their employer and understand their outlook for the future.
(Nurse)
More commonly, the feedback (especially from HCPs now eligible to issue fit notes) was that those patients seeking a fit note from one of the newly eligible HCPs may be more likely to have an enhanced conversation than they would often have with a doctor. Firstly, these HCPs issue fit notes within their area of expertise and may therefore have a better understanding of the cause of the illness and adaptions at work that can help.
As OTs we understand the person more than a doctor, particularly around their abilities to work including grading to work. We might also be in a good position to identify other services to enhance recovery or support returning to work.
(Occupational Therapist)
If I’m seeing the patient, I’ll know more about their MSK conditions than the GP, so I can give the right timeframe for the fit note… …and it helps me plan their care.
(Physiotherapist)
Secondly, HCPs felt these HCPs who can now issue fit notes usually have more time with a patient than a GP does, so will therefore be able to have more in-depth discussions.
I have had patients say that when they come to see me or other ACPs [Advanced Clinical Practitioner] that we tend to understand them more - but in terms of care, I think it’s the same with the GP and ourselves.
(Nurse)
There are patients I see for an hour every week, so obviously I know them really well. They can feel like they are actually being listened to…we have a lot more time to sit and discuss why they’re off work, why they want the time…and it can be easier to make more specialist recommendations.
(Occupational Therapist)
Thirdly, these HCPs are new to issuing fit notes, so they felt they would be more conscientious in how they do so. Similarly, some of the HCPs who can now issue fit notes commented that the culture of their professions tended to place a strong emphasis on following defined processes and would therefore be more likely to fulfil requirements, such as taking the opportunity to have a substantial work-focused conversation.
Because it’s new to nurse practitioners, we would be more strict and have more questions versus someone who’s done it for a long time, it’s more mundane.
(Nurse)
I find that our assessments are more in-depth and we document everything compared with a GP. We look at other options as well to get them back to work.
(Nurse)
Several HCPs who can now issue fit notes thought that they were providing a greater level of detail in the fit notes to employers than doctors would tend to, because they potentially had more time and a better understanding of workplace adaptations that can help.
Employers are also sometimes getting a lot more detailed info from us than they would from a GP.
(Physiotherapist)
We frequently have conversations with patients who are on the mend but not confident about returning to work. We talk about lighter duties or part-time work, When I write to them, I’m really writing to their employers.
(Physiotherapist)
A number of participants also mentioned that if they had any doubts, or felt over-pressured to issue a fit note, they could refer the patient to someone more senior or a doctor.
3.8 Patient Experiences
A small number of the patient participants in the research recalled being issued a fit note in the last 12 months from one of the 4 HCPs’ professions now able to issue fit notes. Some of these were surprised that other HCPs could issue a fit note, and some reported they had encountered a few teething problems. There was no clear pattern to these problems, but the quote that follows gives one example:
I got one from a nurse practitioner. I wasn’t getting any better, so I went down there, they gave me antibiotics and I asked for a fit note because I needed more time. The nurse said it was only her second time doing one, so she wasn’t really sure about how to do it. She didn’t really discuss me being fit to work; she was more worried about getting it off the computer right.
(Patient)
Overall, patients reported positive experiences with newly in-scope HCPs issuing them with fit notes. In part this was because they got what they needed, but several did also comment on the wider benefits of this approach. These benefits were similar to those highlighted by HCPs: that these HCPs had extra specialist knowledge or insight; they could spend more time with patients than GPs; they were easier to contact; they were more approachable and more supportive. They said this all led to better and more relevant discussions about the potential to return to work.
I was seeing an OT regularly and at each of these appointments discussed if I was ready to go back to work or not and issued a fit note accordingly. I found it really helpful, it felt like a lot more based around how to get myself on track to be returning to work, things like goal setting and things like that.
(Patient)
Got an appointment with a nurse at the local GP practice because of the migraines I was suffering. I felt a lot more heard with her than with a GP. I could always ask more questions and make suggestions about things I could do and asked about my work. It felt like a more rounded approach and more detailed about what I could do at work. So, I was able to return to work with some less pressure.
(Patient)
3.9 Training, support and monitoring
Guidance which provides advice to newly eligible HCPs and their employers on certifying fit notes following the reforms to the fit note system,[footnote 4] states HCPs starting to take on the task of issuing fit notes should complete the e-learning for healthcare (elfh) training modules which supports HCPs in preparing to certify fit notes and they should also have a ‘period of structured mentorship and support’. The length of this support may vary depending on HCP’s level of capability, experience and confidence.
The majority of the HCPs who were now eligible to issue fit notes said they had received specific training. Some recalled undertaking the e-learning designed by the Department for Work and Pensions (DWP), but not all participants did, with others saying they took part in training provided by their employer.
I know there is guidance, but my company consolidates the info and I go by what they say.
(Pharmacist)
Overall, most of those who took part in the e-learning were positive about the course, particularly the emphasis on fitness for work and the inclusion of supporting statistics to help the newly eligible HCPs understand how fit notes are or could be used to support patient’s work and health needs.
We did the training through e-learning for health. Gave quite a lot of information and was helpful – facts and figures useful and I use them with patients (such as likelihood to return to work after 6 months). A lot of emphasis on “maybe fit for work” – which is good.
(Nurse)
I’ve done the online modules, and it was fairly useful. It made me think more about whether I was the right person to sign people off and to think about the bigger picture more. The statistics on how likely people were to return to work after being signed off for extended periods were really useful and led you to think more about recommending what amendments can be made to duties before a full sign off.
(Physiotherapist)
Some of these HCPs thought it might act as a useful, long-term resource.
E-learning was really good and informative. Once done it you don’t need to do again, but I said to myself I’ll do it at least every 12 months. Plus, we had in-house training – I have 2 mentors, GP partners, so had some internal training and when I started issuing notes, they would review them.
(Nurse)
The main reservation was over its length which was felt to be too long. This was raised by a significant proportion of HCPs who had taken the course.
Only did the NHS e-learning for health. About 7 hours. Long - one of the longest courses I’ve done. Some of it was useful, but too long.
(Nurse)
However, not all HCPs now eligible to issue fit notes had taken the e-learning course and some were not aware of it.
We didn’t have any training. We weren’t aware of it. I and my colleagues got together and worked out how to do it. But we were informally advising patients about how to get back to work already.
(Physiotherapist)
There was no need for training. I felt I could do it.
(Nurse)
Those HCPs who have not started to issue fit notes said they would expect to receive specific training before they felt confident to do so, and often their first preference is a ‘live’ course rather than e-learning, so that they could ask questions of the course leader or other participants.
I wouldn’t feel comfortable just reading some information with no opportunity to ask questions, so I prefer a format with someone leading the sessions for questions and clarification.
(Pharmacist)
In addition to the formal training provided to HCPs, a further common theme to emerge from the research was the ongoing support that the newly in scope HCPs can access from their GP colleagues if they require it. Typically, these HCPs described how they would seek advice from a GP or would be encouraged to do so, if they were considering issuing a fit note but had some concerns or questions, or if a case were too complex or outside their professional scope of practice.
Sometimes patients can be really, really demanding, screaming at you down the phone… in those cases I don’t give in, I refer them to someone more senior so they can be assessed.
(Pharmacist)
Protocols are in place – we can only go to a certain extent. If a person hasn’t been seen for a period of time, then a review is needed with a GP. They developed a flow chart protocol for us to follow - the practice did this for themselves.
(Nurse)
Several HCPs interviewed also agreed that there should be enhanced monitoring of fit notes issued by the newly in-scope HCPs, particularly where a fit note is renewed for an extended length of time, so that patient cases are periodically reviewed. It was not possible to determine from this research how embedded this type of monitoring is.
If non-GPs are allowed to give recurrent fit notes, they might be missing major medical issues. There should be clear guidelines for that.
(GP)
If we get recurrent patients, perhaps a GP should see them occasionally to just check as they are responsible for the practice as a whole.
(Nurse)
Most of the doctors who participated in the research only had a vague recollection of how fit notes were covered in their original training, and some thought that they may not have received any training. However, they were generally of the view that they had sufficient knowledge to follow the process effectively, drawing on their wider formal training and subsequent professional experience.
3.10 Attitudes by professional group
All participant groups – HCPs, patients and employers – were asked about potential benefits and any concerns in allowing the 4 groups of HCPs to issue fit notes. The order in which the 4 professions were put to participants was randomised to avoid ‘order bias’.
Across all the participant groups, the feedback was very consistent, with the majority agreeing that the extension to these 4 groups of HCPs was a positive development. For nurses, participants tended to offer a positive view at once; for physiotherapists and occupational therapists, they sometimes took a little longer; and they had more reservations overall about pharmacists being able to issue fit notes.
Nurses
Across all the groups, participants were generally positive about extending certification to nurses, except for the few who were against extension of certification altogether. There was very little discussion of either benefits or risks, though some suggested that nurses had wider training and experience which made them able to deal with a wider range of reasons or conditions for patients to be issued with a fit note.
Nurses have a really good understanding of what is going on… there are so many qualified professionals who can do this.
(Employer)
Physiotherapists
In general, participants were supportive of the extension of certification rights to physiotherapists. They cited the specialist skills in conditions such as back pain which were directly related to people’s ability to work, and the ongoing nature of the physiotherapist-patient relationship, which tended to have extended consultation and treatment sessions often extending over weeks.
One concern was whether HCPs in private practice might have a financial incentive to issue fit notes, as this would extend the treatment programme and so earn them more money. However, this may be based on a misconception among non-HCP participants about the role of private HCPs in issuing fit notes.[footnote 5]
Occupational Therapists
Overall, participants expressed similar views as for physiotherapists, which was that they offered relevant specialist skills and potentially a close relationship with the patient, which were both very valuable. These views were a little more tentative among employers and patients, perhaps because non-HCP participants in the research had less experience of occupational therapy or less clarity about what occupational therapists did. Nonetheless, some employers were particularly positive about the extension to occupational therapists because of their expertise in workplace adjustments, which they felt might make the fit notes they issued more helpful.
Pharmacists
Initially, most non-HCP participants (and some HCP participants) in the research were surprised by the inclusion of pharmacists. The doubts initially raised included: pharmacists not having the same on-going relationship with patients; that they were not co-located with doctors, who could provide advice or supervision; they were more commercially minded; and they might not have the same medical training. Other participants thought that pharmacists should be included because they did have relevant skills and professional training and several noted that pharmacists were being asked to take on more roles within the NHS, and this was a natural extension.
I wasn’t sure about the qualifications of pharmacists to issue fit notes. I’ve got a little bit of a pharmacist down the road, and it almost seems like a corner shop and when you have lots of these little shops up and down the country, you worry about their qualifications.
(Employer)
However, it was clear that many participants were initially thinking of ‘pharmacists’ in terms of community or retail pharmacies. Following clarification that the extension only covers pharmacists working within GP surgeries or equivalent care settings and does not include ‘High Street; or ‘local’ pharmacies, many participants changed their mind and thought that it would make sense to include pharmacists. Some spontaneously linked this to their own experiences (or had heard about) of pharmacists in GP surgeries performing medication reviews or similar roles. Although some participants still had reservations, support for including pharmacists was much closer to that for the other professions following this clarification.
Wider Public Views
These views are reflected to a certain extent in the findings from the online survey of the public’s attitudes to fit notes and the reforms. In the survey, respondents were presented with a list of HCPs and were firstly asked whether they thought each group was able to issue fit notes and were then asked whether they should be able to issue them (Table 3.2). As highlighted earlier in this chapter (Section 3.1), the findings revealed very low awareness of the extension of certification among the survey respondents. For example, less than 1 in 5 of those surveyed knew that nurses (18%) or occupational therapists (18%) can issue fit notes. More positively, there was clear support for increasing the range of HCPs to those who could now issue fit notes. For example, while 18% of people thought nurses could issue fit notes, 40% thought they should be able to. As Table 3.2 shows, there were similar differences for all groups of HCPs (except GPs), showing that a significant proportion of the members of the public believe the extension of certification is a positive step.
The survey also highlighted attitudes towards pharmacists being allowed to issue fit notes. Support for extending certification to ‘High Street’ pharmacists was 19% compared to 30% for pharmacists based in a GP surgery. Even with this clarification, it may be that some participants in the focus groups and those surveyed still had in mind a community or retail pharmacist, dispensing medicines in a retail setting, rather than a pharmacist directly employed by a GP surgery as part of the clinical team. As many GP surgeries have co-located retail pharmacies it could be that some participants may have considered this to cover pharmacists ‘based in’ a GP surgery.
The survey also revealed that support for the 4 groups of HCPs was lower than that for GPs (82%) or hospital doctors (76%). This reflects to some extent the doubts and reservations which were initially expressed by some participants in the focus groups and interviews about the extension. In those cases, once the participants had the chance to reflect on the extensions and (within the focus groups) exchange views with others, they became more positive.
Table 3.2: Public perceptions on which types of healthcare professionals can issue fit notes and should be able to issue fit notes
| Profession | Are able to issue fit notes % | Should be able to issue fit notes % | Difference % |
|---|---|---|---|
| GP | 84 | 82 | -2 |
| Hospital doctor / consultant | 65 | 76 | +11 |
| Nurse | 18 | 40 | +22 |
| Occupational therapist | 18 | 35 | +17 |
| Dentist | 15 | 38 | +23 |
| Physiotherapist | 14 | 36 | +22 |
| Pharmacist based in GP surgery | 9 | 30 | +21 |
| Optician | 8 | 23 | +15 |
| Paramedic | 4 | 20 | +16 |
| Pharmacists in a community / high street pharmacy | 4 | 19 | +15 |
| Dietitian | 4 | 10 | +6 |
| Other | 1 | 1 | - |
| Don’t know | 11 | 8 | -3 |
Base: 2,023 GB adults,
Source: YouGov GB Omnibus Survey, 16 to 19 June 2023
Other Professions
All the participants interviewed, or who took part in focus groups, were also asked to name any additional professions they thought could currently issue fit notes, or professions who ought to be allowed to do so. The groups most frequently cited were:
-
Dentists
-
Opticians
-
Dieticians
-
Counsellors or others providing talking therapies (in general, participants were not specific about roles or titles within this group)
Overall, participants tended to think in terms of 2 categories: those like opticians and dentists, who had the right medical training but where the need to issue a fit note would be rare; and those – particularly mental health therapists – who might be in a position to issue fit notes regularly but might not have the right training or professional standing.
Some participants felt that allowing additional mental health professions to issue fit notes would be positive. The reasons given included the close connection between a mental health professional and their patient or client, and the link for example between a change in medication and the need for time away from work. However, others were concerned that some mental health professionals would be “too close” to the patient and might issue fit notes too easily, or in the case of therapists or counsellors would not have sufficient medical training. Views from participants were not at all polarised and indicate that the majority would support the extension to a wider range of mental health professionals if the right safeguards were in place. A key theme to emerge with the widening of the groups that can issue fit notes, was an expectation that there are systems in place to monitor that assessments are done properly and that the process is credible.
4. Attitudes to fit notes
Attitudes to the 2022 reforms amongst healthcare professionals (HCPs), patients and employers will be influenced by their wider views about fit notes and the relationship between health, sickness and employment. Participants were therefore asked to share their views about the fit note system, before exploring their understanding of the 2022 policy changes.
4.1 Positive attitudes
Healthcare Professionals
Overall, the GPs and other HCPs taking part in this research were positive about fit notes. They felt that fit notes are an important element in how people are supported when they are sick, either through access to health-related state benefits or by ensuring that employers fulfil their obligations to staff, including through payment of Statutory Sick Pay. In particular, there was widespread approval of the reforms implemented in 2010 (see Chapter 1 for more details) which moved the emphasis towards people’s potential to work, with the fit note providing doctors with the option to assess a person as ‘may be fit for work’.
The move to fit notes from sick notes was very positive. I like that you can write about altered hours, and phased return. It can be quite powerful in relieving patient stress either because you state they aren’t fit or that they can do certain things which can help with their employer.
(GP)
I think the fact that it gives you the opportunity to show if people can work with amended duties or amended hours, I think that’s probably the biggest positive impact.
(GP)
However, most GPs described issuing fit notes as a low priority task. Some actively do not like having to do them and many treat issuing fit notes as an administrative task more than a medical one.
Dealing with fit notes is one of the things I push right to the bottom of my list, as I know it’s not an urgent thing.
(GP)
It’s an easy task; they don’t take up much headspace or thinking. Only occasionally you feel like you need an extended discussion with a patient… I treat them as an admin task.
(GP)
The process of issuing a fit note was seen as straightforward, which has been further improved by digitisation, which HCPs were positive about.
It’s a straightforward form. There are lots of ridiculous forms in the NHS, but this one is simple and easy to complete.
(Hospital doctor)
HCPs also highlighted that fit notes can cover many different types of problems and in some cases, the medical need is clear, for example, post-operative rest for a knee operation. In other cases, it can be more complicated, such as for mental health issues, where more reliance may need to be placed on the patient’s description and presentation of their illness. However, within the typical ten-minute consultation slot, GPs have a limited ability to deal with the more complex cases and this can mean they do not assess the patient as fully as they would like. For HCPs who spend more time with their patients – either because their appointment slots are longer, or because they see them repeatedly during a course of treatment – the complexity of a case is less of an issue, as they have time to build a better understanding of the condition and the context.
Patients and the public
These positive views from HCPs were shared by patients and members of the public. Among patients who have received at least one fit note in the past 12 months, the system was seen as an important tool to support people when they need it, for example by providing a medical validation for their condition, which employers accept without question. Above all, it was described as something that “protects employees” (Patient).
Findings from the online survey of the public’s views on fit notes revealed that just under half of the survey respondents (46%) felt that ‘the fit note/sick note system works well so people who are ill get the support they need in the workplace’. A quarter (26%) of them disagreed with this statement and the remainder (28%) said that they did not know. Drawing on the findings from the qualitative interviews with patients, it is likely that the relatively high proportion of ‘don’t know’ responses stem from the proportion of the public with no direct or recent experience of fit notes. Among those who have received a fit note in the last 12 months, so had recent experience, the proportion who agreed with the statement (56%) was higher; while 30% disagreed and 14% did not know.
The patients who were interviewed saw the value of the fit note system in general as providing an official record so their employer would accept their absence, supporting people to continue to be paid while off sick (or claim Statutory Sick Pay) and helping the employer understand how to support the employee. There was broad recognition amongst the patients interviewed that fit notes are intended not just to confirm someone is not fit for work but also should support them back into their workplace or to help them adjust to their work.
Generally, they satisfy your employer and take the stress and pressure off you to justify why you’re not in work. My employer finds it easier if I have seen a doctor and they explain why I’m off.
(Patient)
It was good. It allowed me to work part-time.
(Patient)
Employers
In general, employers understood and supported the fit note system and felt it was helpful to have an expert confirm that an employee was unable to work on medical grounds. They too were very positive about the move away from the idea of a ‘sick note’ to the fit note, with its greater emphasis on people’s potential to work. However, the change in name may also have caused some confusion among some employers. A very small number of employer participants thought that ‘fit notes’ were issued to confirm a patient was fit to work again after a period of absence covered by a ‘sick note’.
Changes in working arrangements, with greater acceptability of being able to work from home in recent years, has made work adjustments more practical for many employers. Some expressed frustration with fit notes that lacked the level of detail – for example, adjustments they might make – which would have helped them manage their employee’s situation more effectively. They felt this was a missed opportunity.
4.2 Concerns about the fit note system
In general, HCPs did express some concerns with the fit note system. Their main frustration was with patients who felt they were entitled to a fit note, even when there was no medical justification for it, as this could take up time and cause tension in the patient-HCP relationship. Another frustration was where patients might be playing the system, because this was also wasting their time and taking resources from the state that could be better used elsewhere. However, these concerns were not considered a high priority: HCPs felt they had other more pressing concerns in their working lives.
Among patients who expressed concerns with the fit note system, 2 main concerns were mentioned. One was that it was sometimes hard for them to get a fit note because of pressures on the primary healthcare system, particularly the difficulty of getting an appointment with a GP to obtain the fit note. The other concern was a perception that it was at the same time too easy for others to get a fit note, when they believed there was no justification for issuing one. Patients also commented that the system was very inconsistent between care settings and even between individual HCPs in the same care setting.
Employers also tended to believe that anyone who deliberately set out to obtain an inappropriate fit note would be able to do so. However, most employers saw inappropriate fit notes as part of a wider problem, which was high levels of unjustified absences, which included self-certified absences.
4.2.1 Access
Patients and employers reported that it could be difficult for patients to get a GP appointment to obtain a fit note, and this can cause additional stress for the employee. This could create tensions in that relationship, for example where a line manager might sympathise with an employee about the difficulty of obtaining a fit note but were themselves under a duty to follow defined company procedures.
This was one of the main complaints about the fit note system from both patient and employer participants. For example, several patients said that their GP surgery would not issue a fit note even though the 7-day self-certification period was about to expire. This meant they could not plan ahead and would have to try and secure a GP appointment within a short window to comply with the requirements of their employers.
When you actually get in contact with the staff, they’re all lovely, and they’re all working really hard, but it’s just really difficult to get in contact with them, and when I was off, I’m extremely clinically vulnerable.
(Patient)
Employers expect to get a fit note by the end of the first day off. But it can take 4-5 days to get a fit note from my medical centre. From previous bad experiences I always want to stick to the rules, though my current employer has been very understanding.
(Patient)
In many areas, patients can request a fit note in a number of ways including online via an e-consult form. Findings from the online survey showed that of those respondents who said they had received a fit note in the last 12 months[footnote 6] almost as many recalled that the last fit note they received was following a telephone conversation as it was following an in-person consultation (37% and 41% respectively). One in 8 (13%) said it was all done online and 6% via a virtual consultation.
Generally, it appears that GP surgeries will issue a fit note without a consultation if the patient’s written records suggest it is warranted but there appears to be a lack of consistency in the approach taken.
Some patients who request a fit note are not seen by a GP – it’s done through e-consult to the GP surgery and will be dealt with by the duty doctor. It depends on the patient whether to see or talk to them – for example, if we know the patient has an episodic chronic illness it will not be necessary to see them; if not, I would call them at least.
(GP)
We ask people to fill in a form online rather than see us physically. We triage the form and if what they’ve written sounds reasonable, we sign it off without seeing them, unless there’s any warning signals, such as chest pain, and then we have a conversation
(Practice manager)
In most cases, HCPs appear to be making decisions whether to see a patient or not, or have a consultation or not, based on the patient’s clinical need, and the previous medical records of the patient.
People can submit an e-consult to request a fit note if it’s an extension and often we wouldn’t speak to the patient. If it’s for the first time, we have to have an actual conversation.
(GP)
We’re pushing a lot through e-consultation. If it’s something they have seen a GP about then maybe I’m happy to do without a consultation. If they’ve not touched based for a while, then I’d assess them in person.
(GP)
However, some GPs said that they might issue fit notes without significant checks or without having a complete understanding of the patient’s needs. They were cautious in discussing this as it could be seen as a departure from their professional responsibilities, but the reasons most often mentioned by GPs were a lack of time to understand the patient’s situation; the difficulty of diagnosing conditions such as back pain and depression; and the risks in challenging the patient’s assessment of their condition and circumstances. The latter itself being driven by an unwillingness to undermine the patient-clinician relationship by suggesting the patient was being untruthful. This is explored further in Section 4.3.
The culture in my practice is you don’t ask and you just do it. And you have 72 hours to grant it… We don’t want conflict or patients complaining about us and giving us bad ratings.
(GP)
Post-Covid, a lot of fit note consultations are taking place over the phone, so there’s no real examination or assessment of the patient sometimes, and you’re also not necessarily an expert in the issue or illness that they’re complaining of, that’s preventing them from working. So, for example, when it’s back pain or musculoskeletal pain – I’m not a physiotherapist, GPs generally aren’t – we’re just relying on what the patient is saying and relaying that to the employer via a sick note.
(GP)
4.2.2 Consistency
The research demonstrated that there is little consistency in how GP surgeries (or HCPs within the same GP surgery) deal with fit notes, despite the availability of fit note training and guidance. This largely reflects the way in which individual GP surgeries differ from each other in many aspects of their approach to care provision, reflecting their status as independent contractors who are encouraged to innovate and reflect local needs and circumstances. Individual surgeries also differ in their capacity for, and interest in, taking up innovations or reforms. The consequence is that, at least at this stage of the dissemination of the 2022 fit note reforms, both patients and HCPs experience considerable differences in approach to dealing with fit notes.
With my previous practice it was so easy for patients to get a fit note, they only had to ask, and it was there for them. This practice that I’m in, it’s a lot harder to get a sick note.
(Nurse)
It depends on who you’re speaking to. Sometimes I’ve been able to get one quite easily, other times you meet someone who’s actually doing the right thing and being really thorough in terms of their questioning.
(Patient)
Similarly, HCP participants based in hospitals also mentioned how the way fit notes are issued can vary significantly between wards / departments within a hospital as well as between different Trusts. Some staff or departments will have a policy of not asking patients if they need a fit note, while others will ask patients proactively, for example those attending for surgery. Those working in acute departments (such as A&E) will be more likely to only give a short-term fit note, as they will tend to deal with short-term health issues. The expectation is that the patient will then need to follow-up with their GP. Other times, no fit notes are produced as the patient will receive discharge notes from the hospital, which is usually sufficient proof to show to employers about the reasons for not being at work for certain length of time.
4.2.3 Secondary Care
Some doctors and other HCPs expressed frustrations with hospitals not issuing fit notes following a hospital visit or stay to those who could not return to work. This led to patients seeking GP appointments to request a fit note. This in turn led to disjointed patient care and extra burdens on GP surgeries.
If in hospitals more OTs and nurses were trained and made aware of this then potentially it will ease traffic to GPs after hospital discharge, for routine things like operations when the patient needs a set period of time off. It would also speed up discharge, which is really important.
(GP)
Sometimes people are desperate for a fit note before leaving hospital, but it was a challenge to track down the doctor – it’s less of a priority for them. Sharing the load of work is really useful. Also, patients might forget and it’s very difficult to contact an acute hospital when you’re not a patient there anymore. Nurses on wards do a lot of work getting patients out so they would be well placed to deal with the fit note.
(Occupational Therapist)
4.2.4 Self-certification
If employee is off sick for 7 days or less then their employer should not ask for medical evidence that they are ill, and the employee can just confirm that they have been ill (‘self-certification’). However, a small number of HCPs did raise concerns that some patients – usually at the request of their employer – still made appointments for a fit note within the 7-day self-certification period, which was seen to be a waste of NHS resources. This could also potentially cause considerable stress for patients, where firms insist on a fit note before the 7-day period expires and a GP surgery would not issue one, resulting in a common theme of patients feeling potentially caught in the middle between their GP surgery and their employer.
A lot of patients don’t understand about 7 days self-certification. It wastes a lot of time and appointments.
(Nurse)
My company policy is 5 days self-certify, not 7.
(Patient)
In the online survey of the public’s knowledge and attitudes on fit notes, while 61% of those surveyed[footnote 7] said they knew that they needed to self-certify for 7 days before being able to request a fit note, 39% said they either did not know or disagreed that this was the case, which demonstrates a significant proportion of the survey respondents are not aware of correct rules around self-certification. The findings found that slightly more women than men were aware of this rule (64% compared to 59%), but more significantly only 35% of 18 to 24-year-olds were aware compared to 59% of those aged 25 to 34-year-olds). Furthermore, even amongst those who had recent experience of fit note process there was confusion around the rules, with 35% of those who had received a fit note in the last 12 months[footnote 8], reporting they did not know or did not think they needed to self-certify for 7 days.
Several patients were also frustrated that GP surgeries would not issue a fit note during the period of self-certification. There was also misunderstanding among some participants around backdating of fit notes, with some believing it was not permitted when in fact the fit note guidance states that HCPs are allowed to backdate fit notes when this is justified by circumstances.
They cannot be backdated. My experience was that I had difficulty securing a GP appointment when I most needed it and I explained to them they were understanding and issued a fit note, but I found that they couldn’t account for the delay.
(Patient)
I had gall stones and was waiting for an operation and in terrible pain. I struggled in to see the nurse and she wouldn’t issue a fit note as I still had one day to run of my self-certification. This was in the evening so there was only 4 hours to go. So, I had to apply online the next morning and of course I had to wait 4 or 5 days for it.
(Patient)
A further concern, raised by both patients and employers, was where employees who had received a fit note saying they were not fit for work were not being allowed to return to work either until their fit note duration had been completed or without a medical note stating they were fit to return to work, even if employee felt they were fit for work.
I’ve had a problem where I’ve given it to work, and then when I found myself in a position where I wanted to return to work early, my employer wouldn’t allow me to do that because of the wording on my fit note.
(Patient)
Again, this issue may be arising due to misunderstanding of the fit note system as anyone in receipt of a fit note is free to return to work before the end date if they feel well enough and their employer agrees.
4.3 Inappropriate fit notes
An ‘inappropriate’ fit note is where a healthcare professional (HCP) has issued a valid fit note for a non-medical reason, such as bereavement[footnote 9] or childcare, or where they do not believe someone is unfit for work, but they do not want to refuse, perhaps to avoid jeopardising the clinician-patient relationship. This contrasts with a fraudulent fit note, which might involve misrepresentation, forgery or other forms of deliberate misuse. Participants were asked about their views on inappropriate fit notes and across the whole sample of participants there was a very consistent perception that it was easy for someone to obtain a fit note inappropriately. Although the discussion that follows sets out the views of HCPs, patients and members of the public, and employers in turn, there was considerable alignment in their views.
Healthcare Professionals
Almost all HCPs thought that fit notes could be issued where it is not necessarily appropriate in some cases, though they differed on how prevalent this was, and on the extent to which they or their colleagues did, could or should police the rules. The latter was driven by several factors; above all, the lack of time that clinicians could spend with patients. It was felt a typical ten-minute appointment might not be adequate to establish if the patient genuinely needed a fit note.
It takes 2 minutes to sign a sick note, and 20 minutes to explain to someone why they shouldn’t have a sick note, so you can see why they’re easily disseminated to patients.
(Nurse)
It’s difficult to regulate or check whether people use fit notes appropriately. It’s down to the GP to determine if someone is fit to work or not, and often this can’t be done in 10 minutes as it is more complicated than that.
(GP)
The second most commonly-cited factor was that HCPs do not see it as their role to question or doubt their patients, but to respond to what they were being told – even if they could not be certain it is true.
Because there is no way for us to say the patient is lying, we tend to veer on what they want… if they want it [fit note], we just give it to them
(GP)
Other factors mentioned by HCPs included:
- unwilling to have an argument with or ‘second guess’ a patient who claims they are unfit to work about not giving them one
Is it worth my time challenging a patient? I have bigger fires to fight… after 3 months they’ll get a DWP assessment, I believe.
(GP)
- time more worthwhile spent with patients with other conditions
GPs can be in a situation where they have to choose between arguing with the patient or just trade that time to attend to another patient.
(GP)
- fear of reprisal or receiving a formal complaint if refuse to issue fit note
Within medicine now there is a big culture of not wanting to get complaints, because complaint letters take ages to deal with and generate hours and hours of work. And I think a lot of GPs don’t want to get complaints for saying no to fit note requests.
(GP)
- concern that refusing to issue a fit note may undermine the patient-GP relationship
It can be tricky because if you challenge the patient, it can damage the relationship.
(GP)
- taking a cautious approach, in which time off work is seen as a low-risk option compared to other interventions such as anti-depressants, which might also be a more expensive option or have long waiting times
Not much harm in giving them… sometimes I can see they are not necessarily needed… but people are complex, there could be other reasons that they are fully justified in getting them. It’s very different to prescribing medication which could be harmful if prescribed inappropriately.
(GP)
I’m not under that time pressure as much so I tend to get to the reason behind the demand. However, it’s not really much of an issue, the worst that could happen is someone gets some time off work.
(Physiotherapist)
These factors were generally presented as natural responses to the provision of healthcare in a busy service with resource constraints. Although some participants were open about times when either they or colleagues were issuing fit notes in circumstances which were harder to justify.
Some colleagues use fit notes just to get people out of the door.
(GP)
Some HCPs thought that mental health conditions were the most likely to potentially lead to inappropriate fit notes, as it is hard for a clinician to diagnose and determine the best approach quickly (particularly for HCPs without specialist mental health training or experience). They were therefore more reliant on trusting what the patient says as they do not have time to explore in more depth with patients. The alternative options such as talking therapies or medication were also perceived as less likely to be available or carried higher risks.
If somebody comes and they say that they’re, you know, very, very stressed, or low in mood and depressed, and they want some time off work, I don’t really question that, I will give them a sick note for that.
(GP)
The HCPs based in secondary care felt it was difficult to issue a fit note inappropriately from a hospital. They said this was primarily due to most patients in a hospital setting being more likely to have a physical illness or injury, which was easier to diagnose than a mental health concern.
Patients and the public
Among patients there was also a belief that fit notes are open to potential misuse and people can ‘hide behind them’ to get time off work. When asked if it was easy or hard to get a fit note issued inappropriately, virtually all felt it was easy. Some also said they either knew individuals (family members or colleagues) who had obtained a fit note inappropriately, which suggests perceptions are not only based on rumour or media coverage, but also on direct experience.
There are people who are cheating the system when it comes to fit notes, and this is costing taxpayers a large amount of money that could be invested in healthcare.
(Patient)
It’s a good system if you need it, but it’s open to abuse. I know people who’ll take advantage of it.
(Patient)
There was also a belief among a significant proportion of the online survey respondents that it was easy to obtain a fit note when it is not needed (Table 4.1). Nearly 4 in 10 (38%) agreed with the statement “it is easy for someone to get a fit note / sick note when they do not really need one” compared to 34% who disagreed, while 28% said they did not know. Among those who have received a fit note in the last 12 months, a similar proportion agreed it was easy to get fit note when not really needed (39%), although slightly higher proportion disagreed (42%).
Across the survey respondents, more men than women agreed with the statement that it is easy to obtain a fit note when it is not needed (41% and 35%, respectively). Similarly, middle class respondents (ABC1 social grades) were somewhat more likely to agree with the statement than working class respondents (C2DE social grades) – 39% and 36%, respectively. In contrast, agreement was lowest among 18 to 34-year-olds (30%) and highest among those aged 55 or over (41%).
Patients interviewed identified the time pressures on GPs as one of the key drivers for inappropriate notes, as well as potentially a lack of motivation to challenge a patient about the need for a fit note. Interestingly, these participants tended not to blame the GPs for this but considered it a reflection of the pressures on the NHS. Often, participants suggested that obtaining repeat or follow-on fit notes can be even easier as it may not necessarily involve speaking to a GP or other HCP.
Although members of the public were very critical of the potential for inappropriate fit notes and often felt angry it happens, there was also some resignation that any process that is intended to support genuinely sick people will potentially be open to misuse. Some also talked about feeling guilty for getting a fit note because they themselves did not want to be perceived as ‘work shy’ or ‘playing the system’. Further, almost all participants – even those who felt strongly that there were people misusing the system – thought that it was right that employers and HCPs were cautious in challenging requests. They might wish HCPs, in particular, to be more assertive but they understood that these were difficult judgements to make.
Overall, despite the concerns with the current system, there was not a strong or widespread feeling that it needed to be made significantly more difficult to obtain a fit note. Patients did, though, expect there to be effective monitoring of when and why fit notes were issued.
Table 4.1: Public views on inappropriate fit notes
“It is easy for someone to get a fit note / sick note when they do not really need one”
| Agree % | Disagree % | Don’t know % | |
|---|---|---|---|
| All | 38 | 34 | 28 |
| Men | 41 | 32 | 28 |
| Women | 35 | 36 | 29 |
| ABC1 (social grade) | 39 | 33 | 27 |
| C2DE (social grade) | 36 | 35 | 29 |
| Age 18 to 24 | 31 | 42 | 27 |
| Age 25 to 34 | 35 | 42 | 22 |
| Age 35 to 54 | 40 | 35 | 25 |
| Age 45 to 54 | 33 | 34 | 33 |
| Age 55+ | 42 | 28 | 30 |
Base: 2,023 GB adults,
Source: YouGov GB Omnibus Survey, 16 to 19 June 2023
Employers
Reflecting the views of HCPs and patients, almost all employers thought that it would be easy for someone to obtain an inappropriate fit note. The main reason they gave was the ease with which they believed employees could pretend to have symptoms, whether it was a ‘bad back’ or ‘stress’.
Most employers had developed a sympathetic understanding of the position of HCPs and why they might issue inappropriate fit notes. Employers understood that it would be difficult for HCPs to prove the patient wrong, and that for a range of reasons (such as time pressures or protecting the patient relationship), HCPs were going to issue them based on trust. These views align strongly with HCPs’ reasons for why inappropriate fit notes are issued, as explored earlier in this chapter.
GPs are not incentivised to police the system.
(Employer)
To ask a GP to not give a fit note when they have to disagree with their patient or to ask the patient to do something they are not keen on is very difficult for GPs. But I am not sure what the alternative will be.
(Employer)
Some employers expressed frustration that there was no mechanism for feeding back to HCPs when they received a fit note which they thought had been issued inappropriately. For some, this frustration was linked to the impact on their business or a sense of injustice that people were playing the system; others thought it wasn’t good for those signed off, as it could lead to isolation and potentially make stress and anxiety worse.
Sickness statistics have gone up – it’s good to give these notes, but you want a nation coming back to work – this doesn’t cure the issue just to sign people off.
(Employer)
Most employers saw inappropriate fit notes as a secondary issue within the wider problem of sickness within the workforce, particularly relating to mental health. They recognised that many, perhaps most, of those taking time off for stress and anxiety were genuine, but that there were also times when they believed that some employees may deliberately play the system. Some employers suggested that this had always been a problem, others believed that it was much worse than in the past, although not necessarily because more people were using claims of stress or anxiety to secure an inappropriate fit note – employers also thought that the ‘real’ incidence of these conditions had risen in society. Several employers commented that self-certification was much more of a problem than fit notes, because employees could use it to take odd days off to suit their lifestyle, which could be more disruptive than a single, extended period of illness.
Employer participants were also asked to reflect on the balance between making it easy for those who needed one to get a fit note, and preventing fit notes being issued that were inappropriate or fraudulent. In almost every case, employers felt the balance was about right.
Any system would be open to abuse; it comes down to the attention that is paid by the employer. If you desperately need one and they make it harder to get one, that puts pressure on the NHS and on an individual who is potentially very poorly, so maybe the balance is right.
(Employer)
Mental Health
Many employers and patients, and some HCPs, thought that it was comparatively easy to gain an inappropriate fit notes through presenting with mental health conditions.
You could just sit there and say, ‘I am stressed’, and who’s the doctor to argue how that person is feeling?
(Patient)
I know a young man, a friend of my daughter, who’s self-diagnosed with anxiety. He’s not on medication, he’s never ‘seen’ a doctor, but he’s been signed off for 8 weeks full pay. He’s laughing his head off. The managers know but they’re too scared to say anything. They’re worried about a charge of bullying.
(Patient)
However, across all the participant groups there was a clear view that the incidence of mental health conditions had risen within society, and that there was also much greater recognition of or understanding of mental health and so easier to report a mental health condition which might have gone unrecognised in the past. Overall, participants thought that the majority of those presenting with mental health conditions would be ‘genuine’ and thought it was a positive trend in society that mental health was less stigmatised and people were more ready to acknowledge that they were facing difficulties. Even those who thought that misuse of the system was widespread were not suggesting that fit notes for mental health conditions should be limited. In general, patients and employers (and to some extent HCPs) thought the ‘answer’ to misuse of the system was for HCPs to be more ready to challenge those who might be seeking to misuse the system, for example by looking at long-term patterns of behaviour.
Also in this context, there was widespread agreement that some patients with mental health conditions would benefit from remaining engaged with the workplace, even if this was challenging for them; and that the alternative of being signed off work for an extended period could have a negative effect on people’s mental health (including if their initial condition was a physical one). Again, there was a general acceptance that these were fine judgements to make, and that in many cases time away from work would be appropriate, but that there would also be cases when ‘signing someone off’ in the sense of them having no ongoing connection with work would not be beneficial for their health.
4.4 Fraudulent fit notes
Participants were asked for their views on fraudulent fit notes and were given the following examples of what might constitute a fraudulent fit note: “someone has made one up at home; altered someone else’s; organised gangs making claims when not entitled; changed 2 weeks to 2 months, etc.”
Across HCPs, patients and employers there was some surprise at the idea of fraudulent fit notes and consequently very few cases of participants identifying instances of when this has happened.
I’ve never heard of this happening!
(Patient)
Sometimes we’ve had companies checking with us about a fit note and we’ve discovered the holder is not actually our patient. Or sometimes we’ve had it where the patient has altered the fit note PDF from 5 days to 2 weeks.
(Practice Manager)
Healthcare professionals
Initially, most HCPs participants took the view that digitally certified fit notes would be more secure than paper notes.
I think it’s difficult now that it’s done electronically. The handwritten ones you were more likely to get people trying to change them and I don’t see that anymore.
(GP)
On reflection, and in discussion in the focus groups, a consensus emerged that if an individual was determined to alter a note and had the necessary IT skills, then it would probably be fairly easy for them to attempt to do so. Overall, though the change from paper to electronic notes (or from wet to digital signatures) made little difference to participants’ views on fraudulent fit notes as outright fraud of this kind was not seen as a significant issue.
I haven’t really given thought to whether that would be open to fraud to be honest. I imagine if someone really wanted to be fraudulent, they could find a way around that - but I haven’t really considered it.
(Physiotherapist)
Employers
Most of the employer participants had either never encountered a fraudulent fit note, or had done so only rarely, so that they might recall a specific example from many years ago.
We have a lot of apprentices and one young lad came in with a fit note and it was funny really how badly he’d done it. We took him to one side and explained he could get himself in a lot of trouble trying this kind of thing and he got the message.
(Employer)
They recognised that there might be fraudulent fit notes which they did not recognise as being fraudulent, but they did not see this as a serious problem. This was largely due to employers feeling the risks of detection outweighed the benefits. Some employers also made the point that as valid fit notes were easy to obtain, there would be little point going to the trouble of forging one.
I don’t think people would take this risk to do this.
(Employer)
Some employers said that, even if they did have concerns about a fit note, it would be difficult to act on these concerns as they would be reluctant to approach the HCP who was supposed to have issued the fit note. They were concerned this might look like they were trying to victimise the employee, which could have consequences ranging from undermining the employee-employer relationship to the threat of a formal complaint or even litigation; and they assumed in any case that the HCP would be prevented from responding by patient confidentiality. A few employers said that they had contacted an employee’s HCP to check validity of fit note, but that this was not routine.
We work on trust and never really doubt the veracity of a note. It’s very difficult to check them because if a GP has issued it then it is not for us to question it.
(Employer)
Litigation is the biggest fear. No-one wants to end up in an employment tribunal.
(Employer)
Several employers noted that the QR code on the digital fit notes gave them the opportunity to check the validity of the fit note, and they welcomed this. Although most were unaware either of the QR code or were uncertain of how to check it or what the process would be.
Some employers said they assumed that there would be checks somewhere in the system to match issued fit notes against patient records. This may help explain why they generally had a positive view about the integrity of the system in relation to fraud.
Overall, employers did not have significant concerns about fraudulent fit notes. Nor did they have strong views about whether the move from paper to digital fit notes would make fraud more likely. Although few understood the use of the QR code on digital fit notes to check authenticity, those that did approved of this as it might give them more confidence that they could check a fit note without compromising patient confidentiality.
4.5 Monitoring and assistance
Many GPs seem to accept that the fit note system is open to, and is, misused by some patients. Some GPs and HCPs do challenge patients, but others do not worry much about it, or do not see it as part of their responsibilities.
Ultimately, it’s someone else’s job to make sure they are not abusing the system – we can’t know everything about the patient or their work.
(GP)
Others are frustrated that there is little, or no monitoring of how fit notes are issued, and no external scrutiny.
Quite often a patient will request a new one, and it’s just an admin task on a very long list and it’s often just signed off on the assumption that someone else will track that this person has been on a fit note for a long time and look into it.
(GP)
Some GPs would like the option of referring patients to a specialist service to support their return to work, and this would also empower GPs to have more difficult conversations with patients. Although outside the scope of this research, the evidence from HCP participants points to a widespread feeling, particularly amongst GPs, that fitness for work conversations often require time to establish the context and discuss options with patients, and it often requires specialist skills. This implies most GPs would see a case for having the option to refer complex cases to a specialist service which could support patients’ return to work.
I feel it shouldn’t be my responsibility if I have a patient on long term sick … there needs to be a third party looking at them.
(GP)
Some of the sharpest criticisms of the management of fit notes came from other HCPs who are observing the system in action from close quarters. Several HCP participants gave examples of where their colleagues were either not sticking to the rules on fit notes or they felt were not providing effective support to those who had been issued with fit notes to support their return to work.
The system is often abused – we should be reviewing them more regularly asking, for example, why is your diabetes not allowing you to work?
(Occupational Therapist)
I question whether people are actually getting the fit-to-work consultation. There are people getting recurrent fit notes and no-one’s sitting down to discuss whether they still need to be off - and we know that the longer people are off work, the harder it is for them to get back.
(Nurse)
There was no set pattern to these concerns. In effect, the more that staff care about the job they do, the more likely they are to feel that some of their colleagues are not ‘doing their bit’ and are either creating more work for them or undermining patient care, thus giving rise to considerable frustration.
4.6 Guidance from Department for Work and Pensions
Most GP participants said they are aware of Department for Work and Pensions (DWP) guidance on fit notes, but they were not very familiar with it or did not use it day-to-day. The general attitude seemed to be that this is guidance only and GPs can use their medical expertise to interpret “the rules” quite widely. In addition, many GP participants interviewed reflected that they had not properly looked at this guidance in some time.
Yes, I’m aware of it and probably looked at it when I did the training. I know it’s there but generally it’s not really used all the time.
(GP)
Most other HCPs were largely aware of the DWP guidance but did not appear to see it as a significant part of how they administered the fit note system. They believed they understood the general principles, and their application would depend on the individual patient.
Some HCPs (including a few GPs) felt that more guidance would be helpful, particularly on understanding the wider care and benefits system and how their decisions might, for example, affect the eligibility of their patients for benefits such as Universal Credit or Personal Independence Payments. Although, some HCPs were almost hostile to the idea of being guided by DWP, as they felt it was their responsibility to make informed judgements about their patients’ needs.
No. I don’t care about it. It doesn’t impact my delivery of care at the point of time. I don’t know what the guidance says, so I don’t know how important it is.
(GP)
Bereavement
One significant finding regarding awareness of the guidance on fit notes relates to whether it is appropriate to issue a fit note ‘for’ bereavement. A significant number of HCPs thought this was not permitted or were unsure if it was, but they took the view that if bereavement is causing a person distress, then it would be appropriate to issue a fit note, whatever the formal guidance might state.
For bereavement, if someone were unfit to work due to emotional distress or instability then that’s not inappropriate at all.
(Nurse)
I have given notes for bereavement because it does affect your mental health, I wouldn’t classify that as inappropriate. It’s quite subjective really.
(GP)
In fact, the DWP guidance for HCPs[footnote 10] does not say this is inappropriate, as it states “…if someone has suffered a bereavement and you assess that they are too distressed to work, it may be appropriate to write ‘distress due to bereavement’. This should only be the case if your clinical judgement is that their fitness for work has been affected. You cannot however write bereavement as a diagnosis on a fit note”. This is because a bereavement is not considered a clinical condition, and a fit note should carry a clinical diagnosis.
This misconception also illustrates how many HCPs feel that their prime duty is to prioritise the needs of their patients, not ‘police’ the fit note system. The discussions on this issue suggested that while HCPs thought there should be guidance and rules on issuing of fit note, it was important there was flexibility for them to make the judgement in individual circumstances.
Similarly, several patients also said that bereavement ought to be explicitly covered by the fit note system, as the qualification that the fit note could be issued for the effects of bereavement, but not bereavement itself, was not widely understood. This could discourage those who needed help from seeking it.
For my case it was more about bereavement reactions, I was suffering with migraines, anxiety, insomnia and flashbacks - so in terms of bereavement I think it’s proper to issue them depending on the case. I explained my symptoms and then the clinician probed into more detail and then issued a fit note. So, I wouldn’t consider it inappropriate.
(Patient)
5. Change in the NHS
The attitudes of healthcare professionals (HCPs) towards any specific reform are likely to be significantly influenced by their prior experience of how change in general is handled in the health service and how change might affect their working lives, for example, in terms of career progression or providing the best possible care for their patients. These perceptions and experiences were explored as part of the qualitative discussions with HCPs. This provides context for the evaluation of the 2022 fit note reforms, including identifying potential barriers to or drivers of implementation.
5.1 Attitudes towards change in the NHS
Healthcare participants were asked to rate how change is managed in the NHS on a scale from 1 to 10 with 1 meaning ‘very negative’ and 10 meaning ‘very positive’. This was mainly done to initiate a conversation about change with HCP interview participants, and to provide some understanding of the extent to which views of the 2022 fit note reforms were coloured by overall attitudes towards change.
The overall rating from HCP participants was 4.5, compared to a rating of 6.1 when asked to rate the NHS as an institution. These scores do need to be interpreted with some caution, for example, some participants explained that they had given a low score because there was not enough change in the NHS, not too much. However, they do validate to some extent a sense from this research around the recent fit note reforms that system changes of any kind in the NHS are perceived to be particularly problematic. Frequently, the HCP participants talked about their weariness and suspicion of change and how they felt change can make their working lives more difficult, especially where policymakers have insufficient understanding of how change impacts negatively on practitioners’ ability to provide quality patient care. Often, they felt change was done to them, rather than to support them.
Change is almost forced upon you. Rather than give us an incentive to do something, it is designed to take things away if we don’t comply. Sometimes feel like we are set up to fail.
(GP)
Some participants linked problems with change to a lack of support or additional resources. For example, in the context of the 2022 fit note reforms, an HCP now eligible to issue fit notes might end up completing the fit note training in their own time because they would not be able or willing to make time during working hours, because of workloads. Moving to digital certification depended on reliable IT (and more training on it) and even, as many HCPs pointed out with feeling, on functioning printers if a patient asked for a printed copy.
Others cited problems with communications, including the detail of the changes and the expected benefits. This could even apply to major structural changes in service delivery, as well as changes in practice or process such as the fit note reforms.
The main response from HCPs was not that any proposed change was wrong, but rather that HCPs could only cope with a certain amount of change due to time and resources, and some worthy initiatives had to be delayed or set aside because of this constraint. Some HCPs who participated in the research placed the 2022 fit note reforms in this category.
Nevertheless, few HCPs were against change. They offered examples of recent positive developments, including greater use of technology (partly driven by the COVID-19 pandemic) and greater use of multidisciplinary teams, which links back to the extension of certification in the 2022 reforms. Often, they were frustrated by the lack of change.
I don’t agree with conventional wisdom that the NHS is bad at change. Lots of young people in the workforce are generally up for change and very adaptable and flexible. The main problem is that nothing is standardised. Even between wards in the same hospital.
(GP)
GP participants, especially more senior ones, placed a high value on having maximum autonomy in how they organise their practice, including their working hours and services offered. Change or policies that they felt impinged on this autonomy might therefore potentially be ignored or resisted. Other HCPs who were not in management or decision-making positions sometimes felt the opposite – that they are currently given too little autonomy and face too much micromanagement, and change offers the chance for greater responsibility and career development. For them, the problem might be local management blocking change or failing to take up the opportunities for improvements.
Older clinicians are set in their ways. Management come and go; they think they can make change and it can be impossible to do clinically.
(Occupational Therapist)
So much hesitancy [to change] especially in GP practices with longstanding partners who are very reluctant to make big changes.
(GP)
These views are directly relevant to some attitudes towards the extension of the groups of HCPs who can authorise fit notes. As the research found, one of the barriers to implementation of the 2022 fit note reforms is GP-partner resistance in some GP surgeries, whereas one of the drivers is the chance for newly in-scope HCPs to take on (or sometimes formalise) new responsibilities.
Overall, the picture provided by participants is of a health service where most staff are committed to their roles but face many frustrations which reduce their job satisfaction, particularly in providing the level of patient care they would like, and above all in spending more time with patients. They also felt patients are in general becoming more demanding and harder to satisfy. Lower job satisfaction is, in turn, likely to reduce the appetite for change. Against this backdrop, change is welcomed in principle, but in practice many participants felt it is not communicated effectively, may not be realistic and does not take account of pressures on time and other resources. This has implications for how the 2022 reforms might be communicated in future, which is discussed further in Chapter 6.
5.2 Motivation and Engagement
The research also explored the drivers of job satisfaction amongst HCPs, which include both transactional elements such as pay and conditions and more emotional or psychological elements such as personal and professional development and team working (sometimes known collectively as the ‘psychological contract’). The simple matrix in Figure 5.1 helps draw these drivers out.
Figure 5.1: Drivers of job satisfaction amongst healthcare professionals
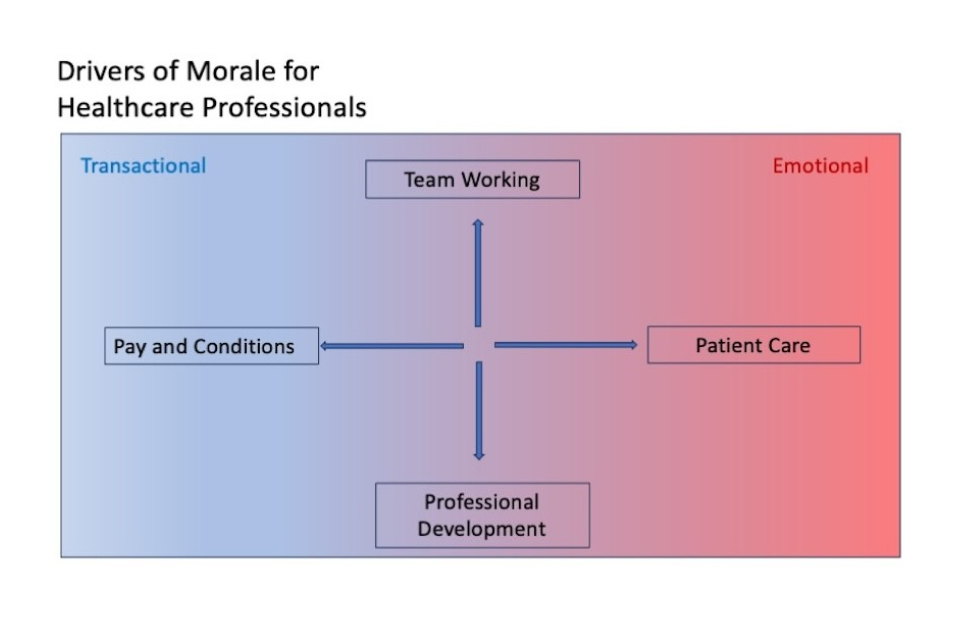
One of the key findings from this evaluation, as shown in Chapter 3, is the clear benefits for patients from extension of certification. Yet the net effect for GPs is that they will see less of their patients because they will be seen by other HCPs who can now issue fit notes, so they will have little direct experience of those benefits. For them, this reform is more managerial or transactional; and as the research has shown transactional gains are relatively modest, many GPs are likely to have relatively weak motivation for implementing it.
In contrast, for the 4 new groups of HCPs who can issue fit notes, the gains for patients are much clearer and experienced more directly, and therefore more motivating. These groups also gain significantly from professional development, which has a transactional element in terms of career progression but also may include status and the satisfaction from acquiring and using skills. There is also a more modest gain from feeling more ‘part of the team’ which comes from easing the burdens on GP colleagues and being more involved in clinical decision-making. This is why these groups are more likely to be strongly motivated to adopt the reform when they can do so.
This may have implications for how the reforms could best be communicated. The research has shown that GP partners are the main decision-making group. For them, the most powerful arguments are not likely to be about benefits for their own workload or for their patients, but from the way implementing these reforms will increase the job satisfaction of their colleagues by allowing them to provide their patients with better care and gaining from professional development and enhanced team working. This should combine a realistic transactional case with some psychological motivation arising from GP-managers feeling they are developing their staff and acting as effective leaders and innovators.
Finally, the ‘patient care’ axis was seen in different ways by different HCP participants. The majority who talked about the benefits for patients emphasised how the reforms made the system more convenient. A smaller number stressed the opportunities the reforms created for more meaningful conversations with patients about how they might return to or remain in work, with adjustments or support, and how the alternative of signing patients off work for an extended period could be harmful to their health. The more that the extension of certification is seen in terms of providing patients with better care and better health outcomes, and the more this is recognised by GP-partners as well as other HCPs, the stronger the motivation for implementation.
6. Conclusions
There is widespread support amongst healthcare professionals (HCPs), employers, patients and members of the public for the 2 reforms to fit notes introduced in 2022, although the nature of that support varies considerably between the 2 reforms.
6.1 Digital certification
In one sense, this reform has hardly been noticed, even by HCPs. Some GPs were already completing fit notes electronically, and although in theory they had to be printed and signed in ink before the reform, some fit notes were being issued and accepted by employers in electronic form without a legally valid ink signature. This may have predated the COVID-19 pandemic, but the rapid uptake of digital correspondence and restrictions on patients visiting GP surgeries during the pandemic appears to have accelerated this practice.[footnote 11] Digital certification was generally seen by HCPs as being part of the wider move towards digital-based healthcare in areas such as online booking of appointments and electronic prescriptions. Almost all HCPs are strongly supportive of it, seeing it as much more efficient, more convenient for patients and requiring less administration.
In general, patients find them more convenient, particularly if it avoids them having to travel to the GP surgery to collect it. Many employers were already accepting scans or photographs of fit notes, and this research found no evidence that employers were challenging the validity of digitally certified fit notes. Most participants do not think that digital certification will make fraud more likely, and some believe that it will make the system more secure.
The main barrier to uptake of digital certification is the current capability and availability of IT systems within care settings, particularly in secondary care. There is also some inertia, with a small number of HCPs issuing fit notes on paper because the perceived benefits of switching are modest and the perceived drawbacks of learning a new system (such as training or redrafting internal processes) are greater.
One key finding was that there will continue to be circumstances in which a paper fit note is more convenient for HCPs who do not have access to IT systems with the right functionality or it is more appropriate for patients, such as those with high levels of anxiety centred on technology. There might be considerable pushback if printed fit notes were to be discontinued, although the facility for a fit note to be printed at patient request was retained in the legislative change.
Overall, the conclusion from this research is that digital certification of fit notes is meeting its objectives.
6.2 Extended certification
There is low awareness of the extension of certification amongst employers and the public. Levels of awareness are higher among HCPs, but by no means universal. Those with direct experience of the reform are largely supportive. Amongst those who are presented with the idea for the first time, most either accept it at once or do so after some reflection. However, there was an expectation that the extension comes with safeguards such as training, monitoring and that these HCPs have the relevant skills and experience to take on this role. As a result, the majority of participants had a positive view.
Where employers and patients still had reservations about extension, these were largely based on their perceptions of the skills and experience of the HCPs now able to issue fit notes. Some thought they might either be more likely to issue an inappropriate fit note or to issue a fit note outside their scope of practice.
Some employers or patients who did not have direct experience of extended certification speculated that newly eligible HCPs might be more vulnerable to being pressured into issuing an inappropriate fit note than GPs. However, HCPs and those patients and employers who did have direct experience did not see this as a major concern, while some HCPs might be less self-assured, others would have plenty of experience and confidence to draw upon. They thought that some HCPs might even be more ‘resistant’ to pressure than GPs, particularly where they had specialist relevant experience in fields such as musculoskeletal disorders.
6.2.1 Costs and benefits
Almost all participants thought that extending certification would bring significant benefits with minimal costs, but these benefits, and the associated costs, were not seen to fall equally between doctors, other HCPs, patients and employers.
Doctors
Although extending certification might on the surface appear to reduce burdens on GPs, most GPs did not think it would make much difference to their own workload. Instead, the main benefits were improved patient experience and more substantial discussions between HCPs and patients on the potential for them to return to work. This was true even for those GPs who did think there would be a significant reduction in administration.
A number of doctors were unconvinced that the perceived transitional costs – management time in planning and introducing the changes, and staff time on training – would be justified by the long-term gains. They were also sensitive to the opportunity costs of devoting management time to bringing in extended certification which could have been used for other changes to improve the services they provide. A few GPs thought the reform would bring additional on-going costs through their having to supervise other HCPs and that these would outweigh any benefits. This could potentially help to partially explain why, although GPs and other HCPs were largely in favour of extended certification, the rate of uptake was relatively slow.
It was also clear that many of the fit notes that would be diverted away from GPs to other HCPs would not be taking up much GP time in the first place. Furthermore, straightforward fit note cases which might be dealt with quickly were seen as a positive by many GPs, as they could help them regain a few precious minutes in dealing with a demanding list of consultations.
Overall, most GPs were in favour of the reform, but the cost-benefit trade-off for them as individuals was less clear-cut than for other groups.
Newly eligible HCPs
The main benefit for the HCPs, who were now able to issue fit notes, was an improvement in patient care, both in terms of the quality of treatment or support (such as more tailored advice about returning to work) and in the ‘experience’ of seeking care (patients not having to make separate appointments to see a GP to obtain a fit note). They were also able to develop their professional skills, take on additional responsibility and, through providing better patient care, experience enhanced job satisfaction. Those who were aware of the reforms but had not yet taken part were similarly positive. Very few anticipated they would be required to take on issuing fit notes, and so those who might have felt the training was a significant burden, or did not anticipate the same benefits, had either opted out, or assumed they could do so. Therefore, the corresponding costs were low.
Patients
Overall, patients saw the extension of certification as providing clear benefits, notably in helping them to secure a fit note more quickly and conveniently, and potentially with more time to explore with the HCP the causes of their condition and opportunities to speed their return to work, including the specialist knowledge of HCPs in areas such as musculoskeletal disorders. Some also thought other HCPs would be more sympathetic or approachable. They saw few, if any, costs.
Employers
As with patients, employers saw significant benefits and few costs. The reform would mean their employees could obtain a fit note more rapidly as it helped overcome the difficulty of accessing a GP to obtain a fit note, and it would potentially support an earlier return to work, by providing more detailed and relevant advice within fit notes on potential adjustments.
When patient and employer participants were asked why they thought the extension of certification had been introduced, in most cases the assumption was that it was to reduce the burdens on GPs. Few of those who had not had direct experience of receiving a fit note from another HCP mentioned ease of access for patients, or a possibility of a more in-depth discussion on return to work, although this was mentioned by those who had direct experience. This may have implications for how the reform is communicated in the future, with more emphasis on a better patient / employer experience, and in facilitating return to work, and less on tackling GP workload. In contrast, GPs and other HCPs thought that, while the main reason for the introduction of the reforms was to reduce GP workload, the main benefits were enhanced conversations with patients and a smoother process for obtaining a fit note.
6.2.2 Variation in views on extending certification
The evidence from this research was characterised more by the overlap of views across the different participant groups to extending certification than by variation, but some notable differences did emerge.
GPs and other HCPs with reservations about the reforms tended to be further on in their careers and appeared to be less enthusiastic about change of any kind within the healthcare system, not just the 2022 fit note reforms. Also, more doctors expressed reservations about the extension of certification than other HCPs who could now issue fit notes, though those with reservations were still a minority.
6.2.3 Work and health conversations
There was a general view across all 3 participant groups that the extension of certification would improve the overall quality of work-related conversations. It was felt that the HCPs now eligible to issue fit notes would have additional relevant skills and experience, would usually have longer with patients, and might see them repeatedly over a course of treatment. It was not that doctors could not or did not already have effective work and health conversations, but that as more of the newly in-scope HCPs took up extended certification, the proportion of effective work-related conversations would rise.
6.3 Equality, diversity and inclusion
The evidence does not suggest that the introduction of digital certification has had any discernible impact on equality, diversity or inclusion, either positively or negatively. The wider moves to remote consultation and digital communications in healthcare does have notable equality, diversity and inclusion implications, and digitally certified fit notes may play a small part in this, but the evidence from this research does not allow us to draw any firm conclusions.
The extension of certification does have some equality, diversity and inclusion implications. Several participants commented that patients (by implication from vulnerable or marginal groups) might be more comfortable dealing with HCPs from the extended groups who can now issue fit notes, largely because they would feel less of a difference in social class compared to a doctor. Extension also brought with it opportunities for personal and career development for HCPs, and this in turn would potentially improve inclusion in the workplace, particularly by ethnicity and social class. There was no evidence from this research of any actual or potential negative effects.
6.4 Implications for future uptake
The evidence from this research suggests that the uptake of extended certification will continue to grow, driven by: wider knowledge (including the entrance of new graduates to the workforce who have been trained in issuing fit notes); greater familiarity and confidence; the movement of the HCPs who have issued fit notes to new care settings; and more awareness amongst patients leading to more demand. Findings from this research indicate that the speed of uptake has been affected by competing priorities and also by the effects of COVID-19 but, it is likely that almost all care settings will in time adopt the extension of certification, and that most HCPs will issue fit notes when it is appropriate for them to do so, given their scope of practice and responsibilities. This process could be accelerated through additional communications within the HCP professions, which could be based around the drivers and barriers to uptake identified in this report.
The communication of the changes to members of the public appears straightforward, except for the need to clarify that only pharmacists working in GP surgeries or community and hospital settings will be issuing fit notes to NHS patients, not those working in retail settings. The same might apply to physiotherapists and occupational therapists, clarifying that only those working in NHS care settings are included, not those in private practice.
6.5 Wider implications
Although the core objective of this project was to evaluate the 2022 fit note reforms, the process of establishing the wider context, including views on the fit note system as a whole, has generated some interesting insights which are reported in detail in Chapter 4. However, 2 findings stand out in their potential implications for the fit note system.
Monitoring
There was a widespread assumption amongst patients and employers that there should be a system in place to monitor how fit notes were issued. This would either detect patients who were repeatedly securing inappropriate fit notes or identify HCPs who were issuing a significant proportion of inappropriate fit notes, or both.
Some participants had noted that the digital fit notes had a QR code that would allow the validity of the fit note to be checked by the employer, and they thought this was a positive innovation. Again, they assumed that this meant there was a process to monitor the certification practice of individual HCPs.
The medical role of fit notes
A significant number of HCPs see fit notes as an administrative task rather than providing a form of medical care. There was wide agreement amongst patients, employers and most HCPs that it was often in the patient’s best interest – including for their health – to remain connected to their workplace whenever this was possible, and there were corresponding risks if patients could not return to work for extended periods. However, several HCPs reported that they or their colleagues saw signing a patient off work as being the ‘safer’ option, or having little or no cost, or a way to cope with overly demanding patients.
Similarly, many patients and employers saw value in fit notes providing advice on how a patient could return to work in some form. Again, treating the fit note as an administrative task and not having a discussion with the patient about the scope to return to work, or providing advice to the employer about how to facilitate this, was seen by many participants as not in the patient’s best interest.
It is clearly for clinicians to make judgements about the needs of their individual patients and how to assign their very limited time. However, the evidence from this research and findings from wider healthcare research suggests that the more HCPs are helped to appreciate the role of fit notes in helping patients to remain engaged in the workplace, and the medical and wellbeing benefits of this, the more they will try to make time for thorough and probing discussions about how their patients can remain engaged with their workplace, which should lead to better patient outcomes.
-
A few participants were recruited separately for pre-testing of the research materials. ↩
-
In this research the terms ‘healthcare professional’ and ‘HCP’ also includes GP practice managers. ↩
-
Who can issue fit notes: guidance for healthcare professionals and their employers - GOV.UK ↩
-
HCPs working privately can issue fit notes for delivering NHS services to NHS patients. They cannot issue a fit note to a private patient. Where patients pay for their own treatment rather than receiving care through the NHS, the HCP would issue a private medical certificate on their fitness for work. ↩
-
312 survey respondents. ↩
-
2,023 survey respondents were asked this self-certification question. ↩
-
301 survey respondents had received a fit note in last 12 months. ↩
-
In some circumstances it might be fully appropriate to issue a fit note to someone who has experienced bereavement when it has had an impact on an individual’s health and wellbeing. ↩
-
Getting the most out of the fit note: guidance for healthcare professionals - GOV.UK ↩
-
Prior to the reform fit notes could be produced electronically but would need to be printed out as they required a wet signature. ↩
