Closer monitoring and treatment of diabetic retinopathy
Updated 23 June 2025
Applies to England
1. Overview
This information is for people who have been referred from diabetic eye screening because they need:
- closer monitoring in a surveillance clinic
- referral for further investigation or treatment
Diabetic retinopathy progresses with time. If you want more information on how it can progress:
- visit NHS.UK
- see the separate leaflet Your guide to diabetic retinopathy
You may want to discuss this information with your health care team.
2. Closer monitoring in a surveillance clinic
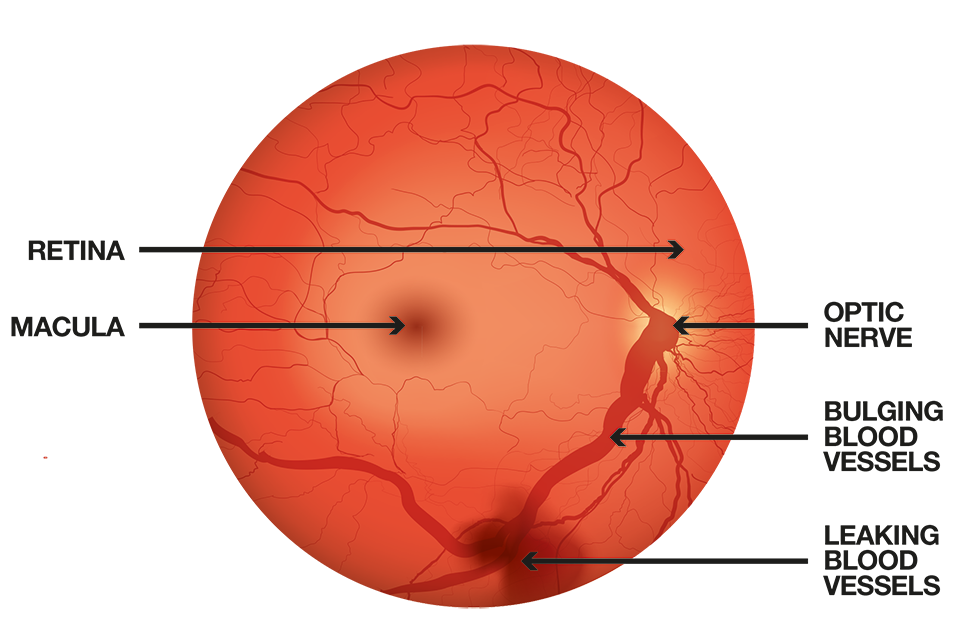
A digital photograph of a retina showing signs of damage from diabetic retinopathy
Diabetic retinopathy occurs when high blood sugar levels damage the back of the eye. It can cause the blood vessels in the retina to leak or become blocked.
Diabetic maculopathy is when retinopathy occurs on a part of the eye called the macula. The macula is the small central part of the retina that you use to see things clearly.
Untreated diabetic retinopathy can cause sight loss. If it is found early enough, treatment can reduce or prevent damage to your sight.
You may need closer eye monitoring in a surveillance clinic if you:
-
have signs of diabetic retinopathy that has progressed but does not need treatment yet (pre-proliferative retinopathy)
-
have signs of diabetic maculopathy but it does not need treatment yet
-
have been treated for diabetic retinopathy in the past
-
are pregnant – pregnancy can mean that diabetic retinopathy develops more quickly
Closer monitoring in a surveillance clinic can be offered every 3, 6, 9 or 12 months depending on how your eyes are changing. In a surveillance clinic you are still under the care of the screening programme.
During a surveillance clinic appointment, you may need to have an additional scan called Optical Coherence Tomography (OCT).
An OCT scan allows a detailed view of the eye’s internal structure, helping to detect the presence of diabetic maculopathy.
OCT scans are being introduced into the NHS Diabetic Eye Screening Programme from April 2025. This may mean you are invited to a clinic you may not have been to before.
It is important that you go to your appointment for closer monitoring because your diabetic retinopathy has got worse and needs to be checked more regularly with an OCT scan. This means you can be referred to the eye hospital at the right time for further tests or treatment.
If your retina scans show signs of improvement, you may go back to routine screening every 1 – 2 years.
If you have any questions about OCT or clinic locations, please contact your screening programme. You can find their contact details on your appointment letter.
3. Referral and treatment
If the scans of your retina show that the diabetic retinopathy has got worse, you may be sent to a hospital eye service clinic (ophthalmology) for further investigation or treatment. This means you may be at risk of long-term problems with your sight because your diabetes is affecting the small blood vessels in your retina.
An eye doctor (called an ophthalmologist) will examine your eyes. They will explain any possible treatments that could help you.
Once the ophthalmologist has finished their investigations and treatment you will be offered screening again.
4. Preparing for surveillance or hospital appointment
You should:
- bring your current glasses (spectacles) with you
- bring a list of any medication you are taking
- not drive for up to 4 to 6 hours after your appointment as you may be given eye drops that can blur vision
- bring sunglasses with you to wear home, as your eyes may be sensitive to bright light after your appointment
5. How you can help
You should:
- continue to attend your appointments
- keep your blood sugar (HbA1c) at the levels agreed with your health care team
- see your health care team regularly to check that your blood pressure is not raised
- keep your blood fats (cholesterol) at the levels agreed with your health care team
- get professional advice if you notice any new problems with your sight
- eat a healthy, balanced diet
- lose excess weight if you are overweight
- take your medication as prescribed
- exercise regularly
- cut down or stop smoking if you are a smoker
Remember, you should continue to visit an optician regularly for a normal eye examination as well as attending your diabetic eye screening appointment.
6. More information
You can find more information at:
The NHS screening programmes use personal information from your NHS records to invite you for screening at the right time. NHS England also uses your information to ensure you receive high quality care and to improve the screening programmes. Find out more about how your information is used and protected, and your options.
Find out how to opt out of screening.
