Cervical screening: having a colposcopy
Updated 23 July 2024
Applies to England
Why you need a colposcopy
We have invited you to have a colposcopy because of the result of your cervical screening test (previously called a ‘smear test’). This is usually for one of 4 reasons, which are:
- we found some abnormal cells in your cervix and an infection with human papillomavirus (HPV)
- you have an HPV infection which hasn’t gone away
- you have had several screening tests where we were unable to give you a result (it is likely there is nothing wrong, but a colposcopy can find out for sure)
- the nurse or doctor who carried out your screening test thought your cervix did not look as healthy as it should
Most people who have a colposcopy do not have cervical cancer.
The colposcopy examination
A colposcopy is an examination to check whether there are abnormal cells on your cervix, and if so, how serious they are. This is a follow-up to your cervical screening test. Colposcopy usually takes place in an outpatient hospital clinic.
A specialist will take a close look at your cervix using a magnifying lens with a light (a colposcope). They may take a small tissue sample (a biopsy) to check any areas of your cervix which look unusual. If the colposcopy confirms there are abnormal cells on your cervix, you may need to have them removed to help prevent cervical cancer.
Having a colposcopy
Before your appointment
If you would like a female nurse or doctor to carry out your colposcopy, please call the clinic to request this when you receive your appointment.
If you think you might have your period on the day of your appointment, you may want to call the clinic to arrange a different appointment. But you can come for your appointment during your period if you want to.
To make it easier to look at your cervix during your colposcopy, please do not have sex or use vaginal medications, lubricants, or creams for at least 24 hours beforehand.
You should take a panty liner to your appointment as you may have a small amount of vaginal discharge after your colposcopy. If you have a small tissue sample taken (a biopsy), you may have some bleeding too.
You can bring a friend, partner or member of your family with you if you want.
At your appointment
You will need to undress from your waist down and lie down on a bed with your knees bent. You will be asked to place your legs onto some padded supports. You will have a paper sheet or towel to cover your stomach and hips. The examination takes about 10 to 20 minutes.
Just like at your screening test, the nurse or doctor will put a speculum into your vagina and open it gently. They will then use a colposcope to take a close look at your cervix. The colposcope does not go inside you, or even touch your skin. It stays about 30cm (12 inches) outside your vagina. The image of your cervix from the colposcope will sometimes be on a screen. This helps the nurse or doctor see your cervix more clearly.
They will dab different liquids onto your cervix. The liquids make any abnormal cells a different colour so that they can be seen more easily. If the nurse or doctor finds anything unusual they may take away a small tissue sample, a few millimetres across (a biopsy). The biopsy will then be checked in the laboratory.
The examination can feel uncomfortable and some people may feel some pain. If it feels painful, tell the nurse or doctor and they will try to make it more comfortable for you.
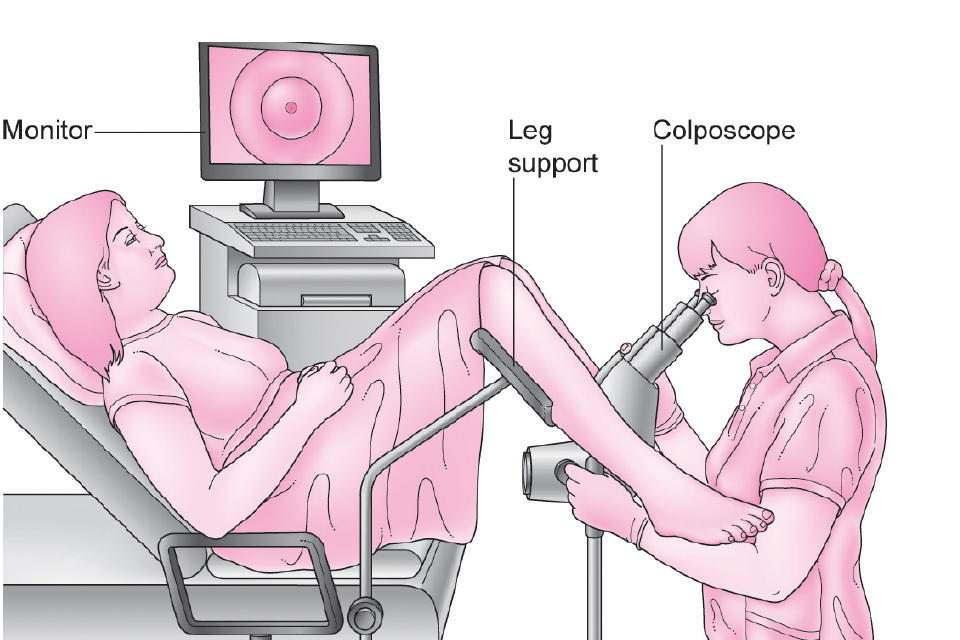
Illustration of a woman having a colposcopy. She is lying on a couch with her legs in supports. The colposcopist sits between her legs, looking at her cervix with a colposcope.
After your appointment
Most people feel well enough to go about their day-to-day activities straight away, but some may need to go home and rest for a while. You may have some brownish discharge from your vagina from the liquids that were used during your colposcopy.
For the next few days, you may have some light bleeding from your vagina, especially if you have had a biopsy. This is normal and usually stops after 3 to 5 days. It’s best to avoid sex, using tampons, and any vaginal medications, lubricants or creams until the bleeding stops.
Results
The nurse or doctor may be able to tell you what they have found straight away. If you have had a biopsy taken, it will need to be checked in the laboratory. If this happens, you will get your results by post about 4 weeks later.
A normal result
About 4 in 10 people who have a colposcopy will have a normal result. If you have a normal colposcopy result, this means that your cervix looks healthy and you have low risk of developing cervical cancer before your next screening test.
You can have a normal colposcopy result even if you had an abnormal result in your cervical screening test.
Abnormal cells confirmed
About 6 in 10 people will have abnormal cells found at colposcopy. The medical term for abnormal cells is CIN (‘cervical intraepithelial neoplasia’). CIN is not cancer, but it can sometimes go on to develop into cancer.
Your colposcopy and biopsy results will show if you need to have the abnormal cells removed or whether they can be left alone for now. This will depend on whether your CIN is ‘low grade’ or ‘high grade’ (see below).
CIN 1 (‘low grade’)
You are unlikely to develop cervical cancer. Often the abnormal cells will go away on their own when your immune system gets rid of the HPV. This happens in most cases. We will normally invite you for another cervical screening test in 12 months to check whether you still have HPV.
CIN 2 or CIN 3 (‘high grade’)
You have a higher chance of developing cervical cancer than someone with ‘low grade’ CIN. We will normally offer you treatment to remove the abnormal cells as this will lower your risk of developing cervical cancer.
Cervical cancer
Rarely, someone having a colposcopy will be found to have cervical cancer. If this happens to you, we will refer you for care and treatment from a team of specialists. Cancers diagnosed through screening are usually found at an earlier stage. People who have early stage cancers are more likely to survive than people with later stage cancers.
Treatment to remove abnormal cells on the cervix
The usual treatment for high grade abnormal cells is to remove them, taking care not to damage the healthy parts of the cervix. The treatment most often used to remove abnormal cells is LLETZ (‘large loop excision of the transformation zone’). You can find more information about this by searching for ‘colposcopy treatment’ on the NHS.UK website.
People sometimes need to come back for another colposcopy to have treatment, but often it is possible to remove the abnormal cells during your first colposcopy.
If you need to come back for treatment this will also be in an outpatient clinic. We usually use a local anaesthetic for the treatment, so you will be awake but won’t feel any pain.
After treatment we will invite you to have a cervical screening test sooner than usual to check that the treatment was successful.
If you are pregnant, we will be able to remove the abnormal cells after you give birth. You should talk to the nurse or doctor about when it is best for you to have this done.
Risks of treatment
Although it is an effective way of preventing cervical cancer, treatment has some risks.
There is a risk of infection from having abnormal cells removed. Signs of infection that you need to see your GP about are:
- heavy bleeding
- bleeding that does not go away
- vaginal discharge that smells
- pain in your tummy that doesn’t go away
Having abnormal cells removed may affect any future pregnancies you have. Women who get pregnant after having abnormal cells removed are not at increased risk of having their baby early if they undergo standard treatment. However if more cervical tissue needs to be removed, women are slightly more likely to have their baby 1 to 2 months early. This may affect around 16% of women (16 in 100) who have had this more extensive treatment and then have a baby [footnote 1].
Not everyone who has abnormal cells removed would have gone on to develop cervical cancer. We offer treatment to everyone with serious abnormal cells because it is not possible to tell who will and who will not develop cervical cancer.
Symptoms of cervical cancer
Cancer can start to develop between your regular screening tests. It is important to look out for anything that is unusual for you, especially:
- bleeding between your periods, during or after sex, or after the menopause
- a change to vaginal discharge
If you have any of these changes, please see your GP as soon as possible.
Usually these symptoms will not mean you have cancer. But if you are found to have cancer, getting it diagnosed and treated early can mean you are more likely to survive.
What happens to tissue samples after colposcopy
Your tissue samples will be kept by the laboratory for at least 10 years. Your colposcopy results may be seen by staff who work elsewhere in the health service, so that they can make sure the service is as good as possible and to improve the skills of specialist staff.
More information and support
For more information, you can:
- speak with your GP or practice nurse
- visit the NHS.UK website
- visit the GOV.UK website and search for ‘cervical screening’
The NHS screening programmes use personal information from your NHS records to invite you for screening at the right time. NHS England also uses your information to ensure you receive high quality care and to improve the screening programmes. Find out more about how your information is used and protected, and your options.
About this leaflet
You may re-use this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence v3.0. Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
The following images in this document are used under licence. Contact the copyright holder/s to obtain permission for any further use.
Illustration of colposcopy examination: Jo’s Cervical Cancer Trust (this charity has disbanded)
-
Castanon, A and others (2014). Risk of preterm delivery with increasing depth of excision for cervical intraepithelial neoplasia in England: nested case-control study. British Medical Journal; 349: g6223 ↩
