Your guide to NHS bowel cancer screening
Updated 23 June 2025
Applies to England
You can choose if you take part in bowel cancer screening. This leaflet aims to help you decide.
Why the NHS offers bowel cancer screening
We offer screening to try and find signs of bowel cancer at an early stage when there are no symptoms. This is when treatment can be more effective.
Sometimes cells in the bowel grow too quickly and form a clump known as a bowel polyp. Polyps are not cancers but can develop into cancers over time. Finding polyps means they can be removed.
Regular screening reduces your risk of getting and dying from bowel cancer.
Who we invite for bowel cancer screening
We invite people aged 50 to 74 years for bowel cancer screening every 2 years. We send a bowel cancer screening home test kit.
You must be registered with a GP and live in England to be invited. Your GP surgery gives us your contact information. Please make sure they have the correct details, including your:
- name
- date of birth
- address
- phone number
- email address.
If you are 75 or over, you can still take part in bowel cancer screening every 2 years, but you will not be invited. Phone our free helpline on 0800 707 60 60.
Bowel cancer
The bowel is part of your digestive system. It takes nutrients and water from food and turns what’s left into poo. As illustrated below, the colon and rectum make up the large bowel.
Bowel cancer is cancer that’s found anywhere in the large bowel. This includes the colon and rectum.
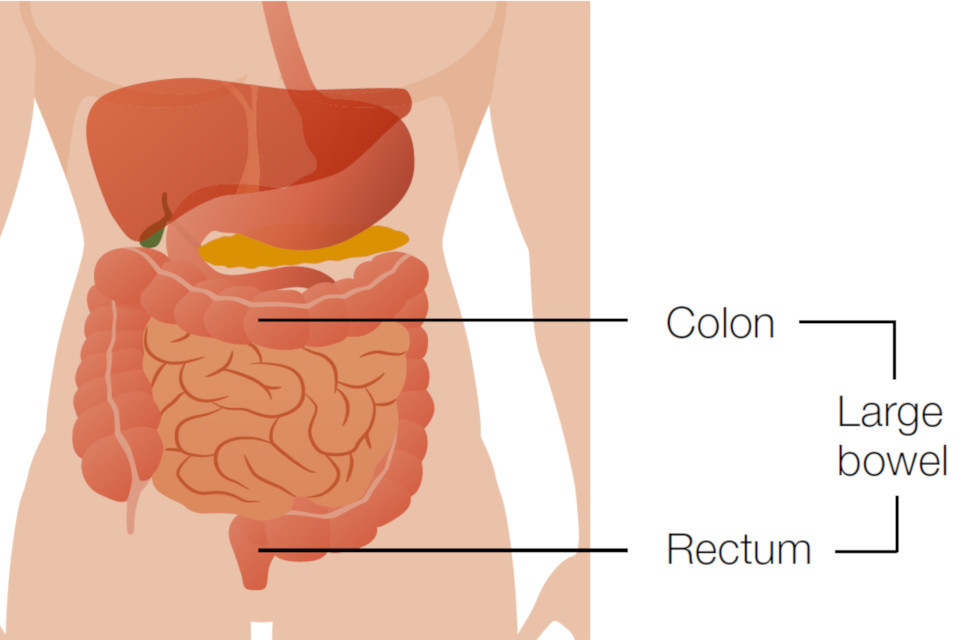
The colon and rectum make up the large bowel and are part of the digestive system.
How bowel cancer screening works
Your invitation will give you information about bowel cancer screening.
We’ll send you a home test kit, called a faecal immunochemical test (FIT). You use this kit to collect a small sample of poo and send it to a lab. The lab checks the sample for tiny amounts of blood. This is because polyps and bowel cancers sometimes bleed. After this, most people will not need any further tests.
If we find blood in your poo sample, you may need further tests to help us find what is causing the blood. We’ll offer you an appointment to talk about having a colonoscopy. A colonoscopy looks at the inside of your bowel.

For most people, no further tests are needed. We offer people who do need further tests an appointment to discuss colonoscopy.
Using the home test kit
To do the screening test, you need to collect a small amount of your poo using the kit. Please use a clean disposable container to collect your sample. You then send this sample in the post for testing. The kit includes prepaid packaging and full instructions.
Once we’ve checked your sample, we record the result and destroy the test kit and contents.
If you have any questions, please call our free helpline on 0800 707 60 60. This includes if you:
- need help to do the test
- are unsure if you should use it, for example, if you’ve had surgery
- have a stoma bag (colostomy or ileostomy) and need advice.
It’s best to collect your sample when you’re not having a period. Avoid the 2 days before or after you bleed.

This is an image of the home test kit. Instructions for using the kit are inside the packaging.
Bowel cancer screening results
You should get your results within 2 weeks of sending in your sample. There are 2 possible results:
- No further tests needed at this time
- Further tests needed.
No further tests needed at this time
Most people (around 97 to 98 in 100) have this result.
It means that we did not find any blood in your sample, or only a tiny amount which is less than the screening level.
We’ll offer you bowel cancer screening again in 2 years if you are under the age of 75.
This result does not guarantee that you do not have bowel cancer. Bowel cancer could still develop in the future. See a GP if you have or get symptoms of bowel cancer.
Further tests needed
Around 2 to 3 in 100 people have this result.
It means we found an amount of blood in your poo at or above the screening level. This is also known as a threshold.
Several things can cause blood in poo. We will offer you an appointment to discuss having a colonoscopy to check the cause of the blood.
A colonoscopy is a test to check inside your bowels. Find more information on colonoscopy on NHS.UK.
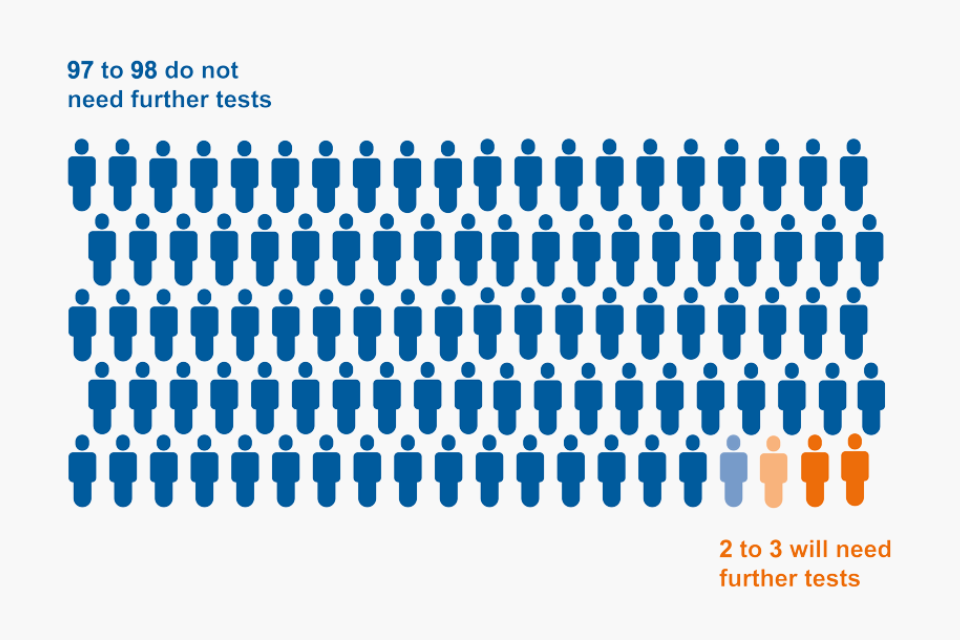
For every 100 people getting their home test kit results, 97 to 98 do not need further tests and 2 to 3 will need further tests.
Possible risks of bowel cancer screening
No screening test is 100% reliable.
Bowel cancer screening could miss a polyp or cancer. This could happen if the polyp or cancer was not bleeding when you used the home test kit.
Most people will not need further tests. If you do, there’s a small risk that having a colonoscopy could damage your bowel, but this is rare. You’ll get more information to help you decide when you have an appointment to discuss a colonoscopy.
Bowel cancer symptoms
Symptoms of bowel cancer may include:
- changes in your poo, such as having softer poo, diarrhoea or constipation that is not usual for you
- needing to poo more or less often than usual for you
- blood in your poo, which may look red or black
- bleeding from your bottom
- often feeling like you need to poo, even if you’ve just been to the toilet
- tummy (abdominal) pain
- a lump in your tummy (abdomen)
- bloating
- losing weight without trying
- feeling very tired, for example because of a lower than normal level of red blood cells (anaemia).
These symptoms do not necessarily mean that you have bowel cancer. If you have any of these symptoms for 3 weeks or more, please speak with your GP. It’s important to do this even if you have recently had bowel cancer screening.
Who is more likely to get bowel cancer
You may be more likely to get bowel cancer if:
- you’re over 50
- you smoke
- you’re overweight
- a close relative has had bowel cancer
- you have inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis
- you have small growths in your bowel called bowel polyps
- you have Lynch Syndrome or familial adenomatous polyposis.
Find more information on how to lower your risk of bowel cancer on NHS.UK.
More information and support
For advice on bowel cancer screening, you can phone our free helpline on 0800 707 60 60.
If you have hearing or speech difficulties, you can use the Relay UK service to contact us. Dial 18001 then 0800 707 60 60 from your textphone or use the Relay UK app.
This information is available in alternative formats, including easy read and other languages. To request another format, you can phone 0300 311 22 33 or email england.contactus@nhs.net.
You can also:
- find more information on bowel cancer screening on NHS.UK
- read our leaflet on having a colonoscopy, if you need further tests
- read information for transgender and non-binary people about NHS screening programmes.
We use personal information from your NHS records to invite you for screening at the right time. NHS England also uses your information to ensure you receive high quality care and to improve the screening programmes. Read more about how we use and protect your information.
Find out how to opt out of screening.
