Extending free PPE to the health and care sector: government response to public consultation
Updated 13 January 2022
Executive summary
What we proposed
In response to COVID-19, the Department of Health and Social Care (DHSC) has provided free access to centrally procured personal protective equipment (PPE) to NHS trusts, adult social care providers, as well as primary care and some other healthcare providers. DHSC has previously committed to providing this central, free provision of COVID-19 PPE (subsequently referred to as ‘PPE’) until 31 March 2022.
Throughout October 2021, we conducted a public consultation on whether to extend the central, free provision of all items of PPE provided to the health and care sector for a further year.
The overarching principles we have considered when developing this policy and analysing responses are:
-
the trajectory of the pandemic
-
the need to protect front-line health and care staff
-
the impact on the businesses who operate in the PPE market
What we heard
We received 5,267 consultation responses:
- 65% on behalf of organisations
- 35% from individuals
The main sectors responding to the consultation were:
- social care (37% of responses)
- primary care (36%)
- community health care (8%)
Overall, the consultation responses showed that the overwhelming majority of health and care providers are strongly in favour of the option to extend the provision of free PPE.
The main themes that we identified among those responses in favour of the continuation of free PPE are that the scheme has and will continue to:
-
protect staff and patients in a broad range of settings, allowing them to continue delivering their services safely
-
relieve them of the financial burden associated with higher PPE requirements, and the rising costs of PPE
-
alleviate the burden of undertaking procurement thus allowing health and care providers to focus on their patients and residents
-
enable access to quality PPE of a reliable standard from a trustworthy source, which is particularly important while case numbers are still high, as face-to-face appointments are increased and to mitigate against any risk associated with waning immunity
Although the proportion of respondents not in favour of extending free PPE was meaningfully smaller (4%), 87% of wholesalers and suppliers indicated that they were not in favour of free PPE being extended.
The main reasons for not supporting the continuation of free PPE for a further year beyond 31 March 2022 were:
-
(in the case of wholesalers) they have already lost revenue and customers, and think DHSC should not continue to interfere with the market and should come up with alternative solutions instead
-
the supply issues from the early days of the pandemic have been resolved and we should go back to pre-pandemic arrangements
Our response and plan for the future
The government is grateful to those who took the time to provide their views as part of the consultation and has considered all their views carefully. In response to the consultation, and in order to help protect health and care staff while COVID-19 case levels are still high and high PPE usage is still required by infection prevention and control (IPC) guidance, the government has decided to extend the provision of free PPE to the health and care sector to 31 March 2023 or until such time as the UK IPC guidance is withdrawn or significantly amended, whichever is sooner.
DHSC has recruited users to test a new platform that will replace the current PPE Portal. This is a representative group of existing portal users from across all sectors, experience levels and users’ needs. User research began in January.
Introduction
In response to COVID-19, DHSC centralised the procurement of PPE across much of the health and care sector to ensure much needed PPE was delivered to the frontline. As part of the department’s PPE COVID-19 response, it has provided free access to central PPE stocks to NHS trusts, adult social care providers, as well as primary care and some other healthcare providers. DHSC has previously committed to providing this central, free provision of COVID-19 PPE until 31 March 2022.
The global COVID-19 pandemic is far from over. The Chief Medical Officer has advised that it is expected that COVID-19 will circulate widely around the world with significant and damaging surges in some geographical areas for at least the next 18 months and, depending on vaccination and variants, probably longer.
COVID-19 PPE usage in healthcare settings is driven by the requirements set out in the IPC guidance. Given current case levels and the recent emergence of the Omicron variant of concern, we do not expect to see a significant change in guidance on requirements for PPE use. We anticipate that PPE usage will remain at COVID-19 levels beyond March 2022 putting significant upward pressure on health and care costs in the next financial year.
Supporting our front-line health and care staff is our priority. However, the department recognises that continuing to intervene in the PPE market in the UK could have a negative impact on the businesses who operate in this market. In light of this, throughout October 2021, DHSC conducted a public consultation on whether to extend the central, free provision of all items of PPE provided to the health and care sector after 31 March 2022.
Our consultation
The department sought views from a wide range of stakeholders via this consultation in order to ensure a well-balanced and evidence-based decision.
We received responses from a range of people and organisations including:
- primary and social care providers
- community health care services
- PPE wholesalers and suppliers
We have analysed the responses and noted specific concerns about whether or not to extend the provision of free PPE to health and care sectors beyond March 2022. This document summarises the responses received and the main points raised.
Scope
The consultation was open to anyone to respond to but was focused on the supply of free PPE to health and care settings. There are non-health and care settings who currently receive the free, central provision PPE but these settings are out of scope of this consultation. Annex A below sets out which user groups were in scope.
Methodology
The consultation, Extending free PPE to the health and care sector, comprised of closed-ended (quantitative) and open-ended (qualitative or free text) questions (see annex B below).
For the close-ended questions we analysed the number and percentage of respondents answering each question, and also broke down responses by type of respondent (for example, member of the public, social care provider, representative organisation or body).
Responses to the consultation are not representative of the groups referenced, but only of those who chose to respond to the consultation. Where particular groups are referred to or compared, this refers only to those responding to the consultation and cannot be taken to represent the views of the public more generally. Differences between responding groups have been highlighted using judgement. We have assumed in analysis that respondents submitted responses in good faith which, if given, accurately represent their characteristics and their view. For example, we take at face value those selecting ‘individual – social care’ are indeed from this group, as verification was not sought.
See annex C (below) for further details on the methods used to analyse the responses.
Analysis
Who responded
A total of 5,267 responses were received.
There were 5,238 completed responses to the consultation received through the GOV.UK page and 29 unique responses received via email.
65% of responses were on behalf of organisations; 35% were from individuals.
Of those who responded on behalf of organisations, these were split into:
- social care (43%)
- primary care, including general practice (14%)
- dentistry (10%)
- community health service (9%)
- other primary care services (9%)
- optometry (1%)
- pharmacy (0.3%).
Wholesalers and suppliers made up 2% of organisational level respondents. Other categories made up the remaining 22%.
Of those who responded as an individual, these were split into:
- social care (25%)
- general practice (20%)
- dentistry (13%)
- other primary care service (12%)
- optometry (0.5%)
- pharmacy (0.5%).
Wholesalers and suppliers made up 2% of individual respondents. Other categories made up the remaining 27%.
For all responses from individuals and organisations combined, social care (37%) and primary care (36%) were the largest groups of respondents, followed by community health care services (8%).
Figure 1: organisation and individual responses combined

Question 1: to what extent do you agree that free PPE should be extended beyond 31 March 2022 for 12 months?
Consultation feedback
95% of respondents were in favour of extending the supply of free PPE for a year to health and care settings beyond March 2022. 4% of respondents disagreed.
Figure 2: all respondents
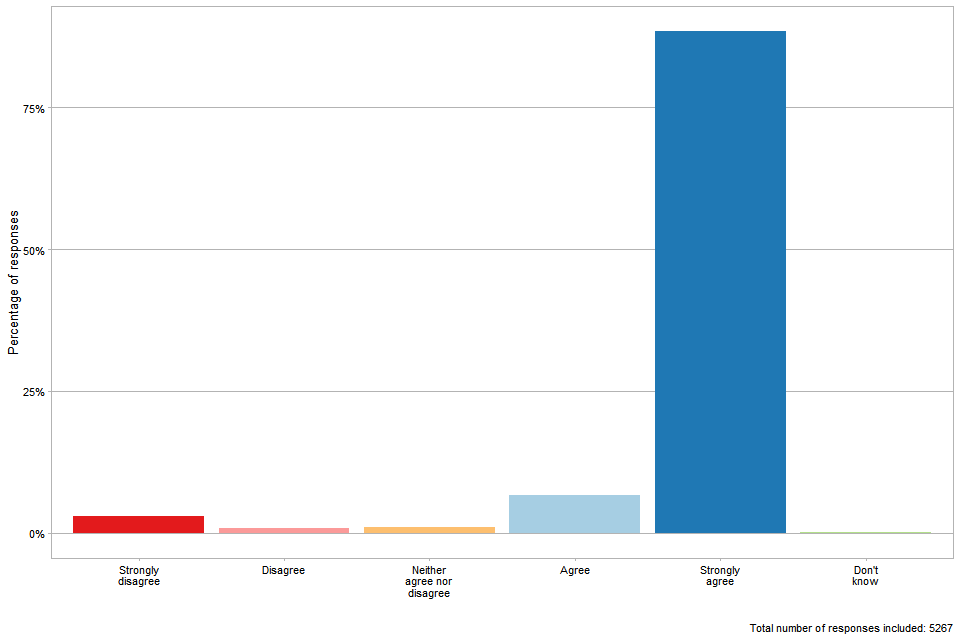
The vast majority (88%) of the responses to this question were from respondents from the health and care sector who have been in receipt of free PPE. Of these respondents, nearly all (96%) agreed or strongly agreed that free PPE should be extended.
Figure 3: healthcare respondents
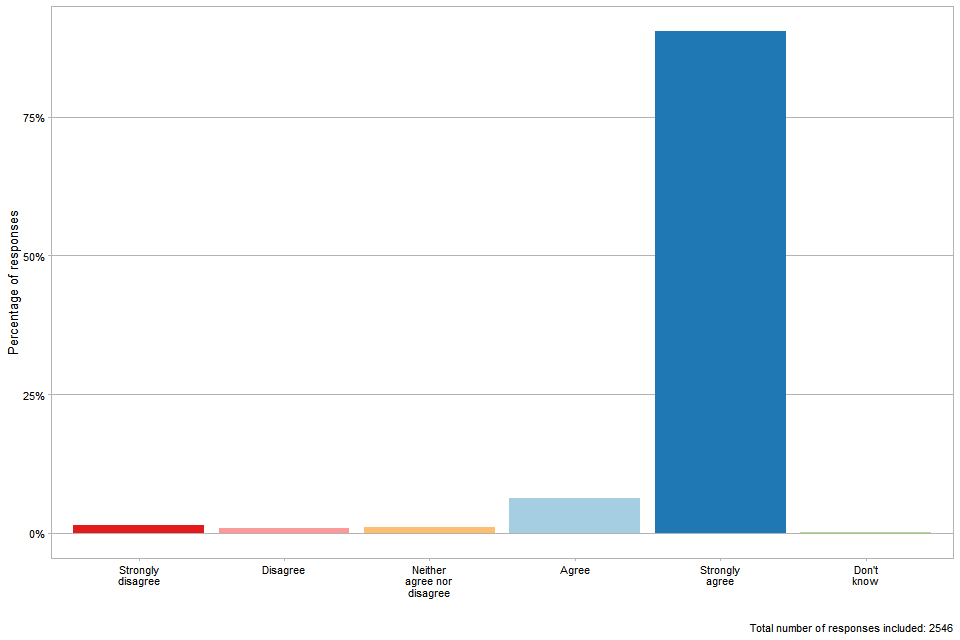
Figure 4: social care respondents
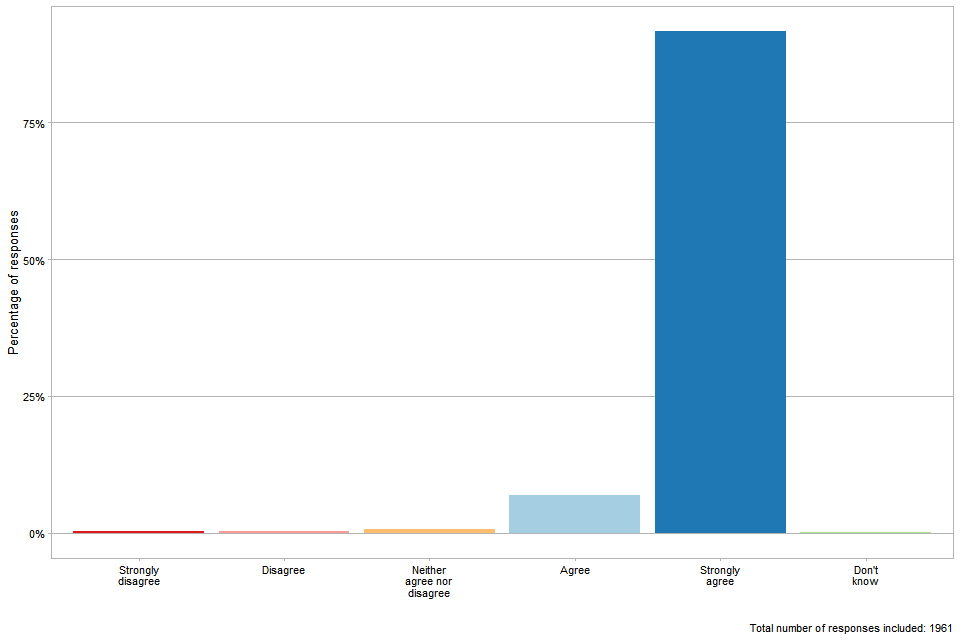
In addition, there were 86 responses from hospices. They all either agreed or strongly agreed with the extension of free PPE.
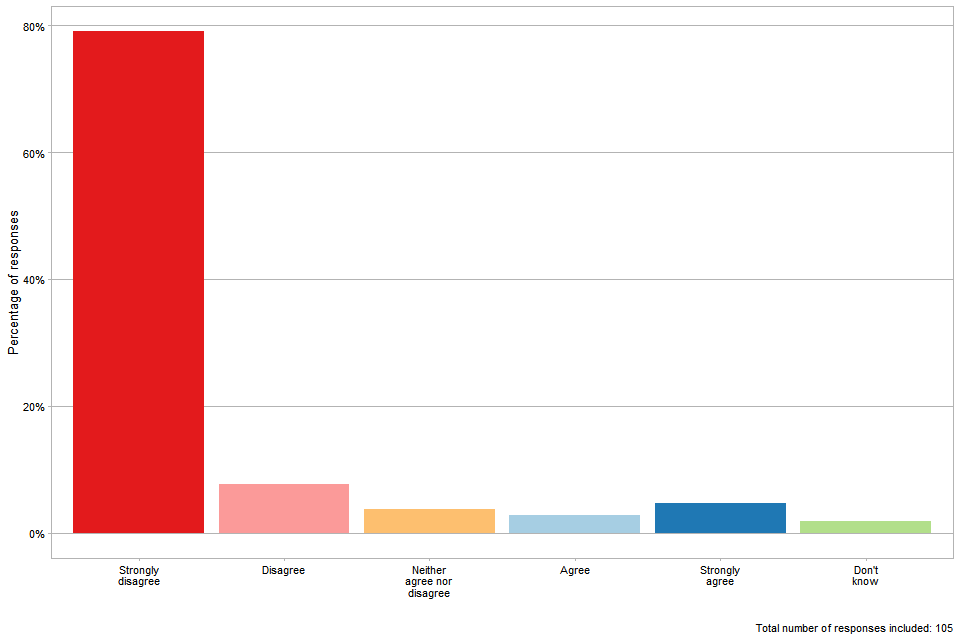
Of those who responded on behalf of wholesaler and supplier organisations, the large majority (87%) disagreed with extending free PPE.
Figure 5: supplier and wholesaler respondents
Key themes that occurred in the ‘agree’ and ‘strongly agree’ responses
Those in support of extending free PPE beyond March 2022 want this arrangement to continue because of the costs associated with COVID-19 PPE requirements and the burden this places on them. They reported that continuing free PPE will allow them to continue providing their services while protecting staff, patients and the public.
They also say that having free PPE has alleviated the stress involved in resourcing and procuring PPE, and that it provides stable access to quality PPE of a reliable standard from a trustworthy source.
Responses differed slightly by sector. For social care respondents, the top themes that emerged included:
-
the costs of PPE and the burden that this would place on providers
-
free PPE enables them to continue to protect the safety of staff and the public
-
a lack of their own funding for PPE
Top themes for primary care respondents included:
-
free PPE allows them to deliver face-to-face and close contact services or appointments while protecting themselves and service users
-
the financial burden of funding PPE themselves
-
the continuing need for PPE beyond March 2022
For community health care services, the top themes included:
-
free PPE allows them to ensure the safety of staff and the public
-
the financial burden of funding PPE themselves
-
centralised provision alleviates the stress and burden of PPE and gives assurance that they are using good quality PPE
To illustrate, a social care provider stated:
We simply could not afford the amount financially to buy the huge numbers needed. There is also a huge admin burden [having] to track down suppliers, order, check and pay.
One GP stated:
The challenge on primary care budgets is higher than it has been in some time. Costs are increasing from all suppliers due to increased fuel or supply costs and this is already eating into the primary care budget. Adding the costs of PPE to this will reduce the budget further adding extra pressure and could result in having to reduce staffing and hours to fund these increased costs.
Another GP said:
[…] we are seeing increasing numbers of patients in primary care and the IPC requirement has not been relaxed and neither should it be. We are using significantly more PPE than before COVID. For example, the cost to meet the requirement to provide a Type II face covering for each and every patient would be prohibitively expensive to general practice.
A respondent from the dentistry sector wrote:
This has helped us protect staff and patients without financial worries. Essentially we would have to limit the PPE usage if we had to purchase our own.
One community health care service responded:
As a private provider, our margins are very slim in order to remain competitive, so the cost of providing PPE on a daily basis is not viable financially.
Another primary care service stated:
It’s a cost that we cannot afford being a small business.
A social care provider said:
Given the other issues we are dealing with on a daily basis, especially recruitment and retention, to not have to worry about sourcing PPE is of huge benefit in many different ways. From stress and management time spent looking for PPE and getting the best price and the cost savings are also very helpful thanks, especially given cost pressures elsewhere in our sector – especially in staff cost.
An acute health service provider added:
Not having to source and raise orders for the increased volumes and variety of PPE has been a blessing during the pandemic and will continue to be so in the uncertain times ahead.
Respondents from the health and care sector did not provide any substantive quantitative evidence on the impact of free PPE to date or the potential impact if free PPE is not extended.
Key themes that occurred in the ‘disagree’ and ‘strongly disagree’ responses
Only 4% of respondents disagreed or strongly disagreed that the scheme should continue, but it is important to note that although they made up a much smaller proportion of respondents, the majority of wholesalers or suppliers of PPE (87%) disagreed or strongly disagreed with extending free PPE.
Their key concerns were:
-
the impact of the scheme on their businesses in terms of loss of revenue and job losses
-
the need to implement alternative or longer-term solutions, which involve central government working in partnership with commercial suppliers
-
the (perceived) lack of need for DHSC to provide the PPE now that supply issues have been resolved and prices have dropped
To illustrate, one wholesaler argued:
We fully understand and support the reasons why DHSC centralised procurement of PPE at the outset of the COVID-19 pandemic. Global demand outstripped supply and prices were increasing rapidly leading to unprecedented challenges in the PPE supply chain. This intervention was necessary to ensure health and care providers could access the volumes of PPE required to deliver services safely at an affordable price.
Despite the continued high demand for PPE by health and care providers, the unprecedented challenge on the PPE supply chain does not exist today. Global supply has now increased to meet this new demand and manufacturing price is almost back to pre-pandemic levels. Therefore, we no longer see the need for such intervention by DHSC.
Another wholesaler stated:
The decision to provide free PPE had a huge impact on us as a business as we had stocked up in good faith to support care homes only for the government to suddenly provide PPE FOC [free of charge] and left us with a considerable amount of excess stock that we are now unable to sell.
Similarly, a supplier stated:
We have millions of disposable aprons sitting in our warehouse because the government have continued with giving free PPE to all hospitals, nursing homes, GP and dental surgeries.
Other wholesalers stated similar things, for example:
We are an independent medical wholesaler supplying care homes with PPE and other products, since government intervention by supplying free PPE to care homes our turnover on PPE products mainly gloves and aprons gone down by 42% and this has put our company to a difficult position. We were hoping by the end of March 2022 (end of free PPE period) we can get back to some normality, if government extend the free PPE beyond March 2022 for 12 months that would make our position even worse and won’t be able to run our business.
Another PPE supplier said:
If DHSC continues to supply PPE free of charge to the adult social sector until March 2022 (and beyond) our business is at risk of going into administration or at the best laying off staff. We are concerned that the decision of DHSC to continue to intervene in the market for the supply of PPE will have a lasting and detrimental impact on an existing and future competitive market and our business. These decisions have resulted in significant financial losses to us.
Qualitative responses to the consultation illustrate there has been an impact to wholesalers and suppliers. However, wholesalers and suppliers did not provide any substantive quantitative evidence of the impact of free PPE to their business – for example, job losses. The supply of free PPE by DHSC is for COVID-19 PPE only. Health and care providers are expected to purchase their business-as-usual PPE from other sources including wholesalers and suppliers.
Question 2: are there other options we should consider?
Consultation feedback
21% of respondents replied that yes, there were other options we should consider. Responses again varied by sector. Social care, primary care and community health service respondents commonly raised ideas around identifying other ways of meeting PPE costs – for example continuing to provide some items of PPE for free, or that PPE should be subsidised or discounted, or providers being given grants or allowances to cover costs. They also wanted to see more flexibility on the type and/or amounts of PPE available to them.
In addition, a number of social care respondents mentioned wanting to see wider reforms in social care such as increased funding and higher salaries.
Some respondents from primary care and community health services referred to the importance of maintaining a reliable supply of PPE in order to be able to respond to future demand shocks, including support for UK manufacturing, ensuring good supply chains and maintaining stock centrally. The latter group also talked about wanting free PPE to continue on a longer-term basis.
A number of wholesalers and suppliers referred to the excess stock that they hold and making better use of this.
Question 3 (for hospices only): to what extent do you agree that the regional hubs should be stood down and hospices onboarded on to the portal?
Consultation feedback
Besides the key consultation question about whether or not to extend free PPE to the health and care sectors beyond March 2022, there was a dedicated question for hospices regarding access to the PPE portal. Hospices currently receive free PPE via a series of regional hubs which are largely reliant on volunteers, rather than via the PPE portal or local authorities or local resilience forums (LRFs). We asked respondents representing hospices the extent to which they agreed that the regional hubs should be stood down and hospices onboarded to the portal.
49% of the respondents to this question either agreed or strongly agreed that hospices should be onboarded to the PPE portal. The reasons that are given are that they hope the portal allows them to order PPE that is clinically assured. Others feel that the portal would allow them to tailor their orders more efficiently, cut down on travel distances to collect from hubs, and that the portal might make the system less reliant on volunteers. On the former, it is worth pointing out that the PPE received through the regional hubs is of the same quality as the PPE that is distributed through the portal. The PPE programme has a standard process for assessing and assuring the PPE products that have been purchased and this determines whether or not products are suitable to be released to the frontline.
15% disagreed because they think that the hubs are efficient and useful, cut down on administrative tasks for smaller organisations, and are a proven method.
The remainder of respondents either did not know which option they preferred, or neither agreed nor disagreed. These respondents report they do not have a preference for either the hub system or the portal, as long as they continue to receive supply. Some hospices mentioned needing more information about the portal in order to ensure it meets their needs.
Figure 6: hospices respondents
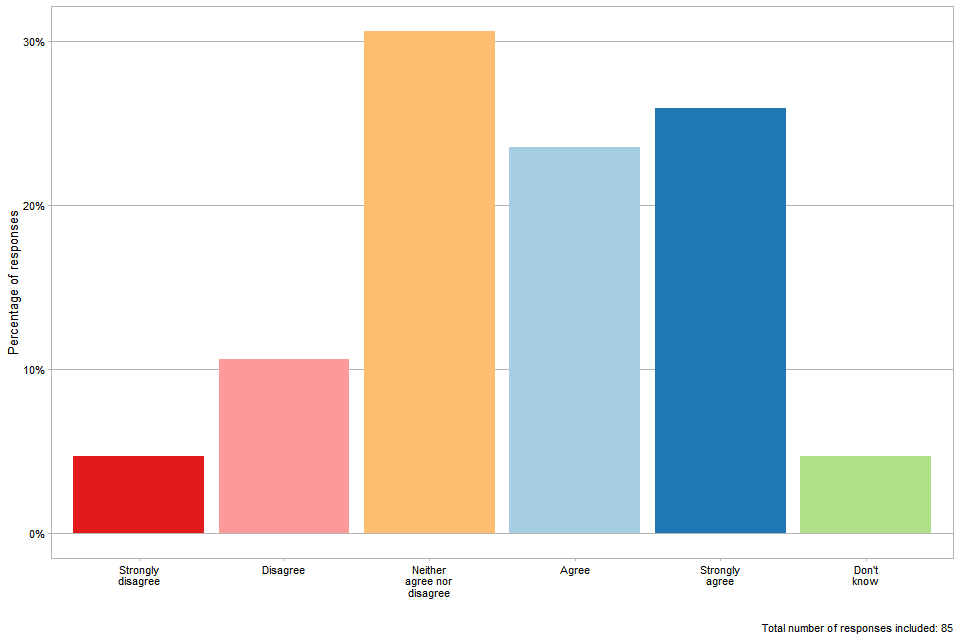
The consultation responses included some positive feedback about hospices moving onto the portal to acquire PPE. We will continue to work with delivery partners to consider how best to take forward this work. Any changes to current arrangements will be communicated in due course.
Question 4: do you have any other views related to this consultation that you would like to express?
Consultation feedback
We received 1,270 relevant responses to this question. Many social care respondents and respondents from community health services referred to the pressures on staff caused by the pandemic as well as the costs that would be associated with these providers needing to buy their own PPE. In addition, a common theme from social care respondents was to express gratitude for the free provision to date, signalling how much it had helped them.
Themes identified in the responses from primary care respondents included the fact that PPE makes staff feel safer in delivering their services.
The wholesalers and suppliers who chose to respond to this question reiterated concerns raised about the proposal to extend free PPE. This included:
- questioning the need for an extension of free PPE because of the present widespread availability of PPE
- stressing the impact this would have on their business
- reiterating the view that the government should not continue to interfere with the market
Our decision
The government is grateful to those that took the time to provide their views as part of the consultation and has considered these carefully.
Responses to the consultation demonstrate that high numbers of respondents are in favour of DHSC continuing free PPE provision over the next financial year, typically health and care providers. These respondents reported that the costs of COVID-19 PPE would place significant financial burdens on them which could have negative impacts on their services.
Some providers said that the costs would be unaffordable for them, and that this could result in staff going without PPE, making up for the extra costs by cutting back staff hours, or having to reduce their services. They also said that continuing free PPE would help them continue to provide their services while still protecting staff and patients.
However, the majority of wholesalers and suppliers disagreed with an extension of free PPE, expressing concern about the impact this would have on their businesses and questioning the need for an extension of free PPE.
PPE usage is driven by IPC guidance which sets out the requirements for PPE in the health sector. This is mirrored in the how to work safely in care homes guidance which applies to care workers in care homes. Although hospital cases and deaths are thankfully not as high as they were earlier in the pandemic, the NHS and other frontline services are under immense pressure as a result of COVID-19 and other demands on services.
The recent NHS report on priorities and operational planning guidance stresses that the typical seasonal pressure on the NHS seen over the winter period is likely to be “intensified by the ongoing impact of the COVID-19 pandemic”. In addition, the government’s Chief Medical Officer recently advised that it is expected that COVID-19 will circulate widely around the world with significant and damaging surges in some geographical areas for at least the next 18 months and, depending on vaccination and variants, probably longer. The pathway through the pandemic is even more uncertain now with the emergence of the Omicron variant of concern.
The IPC cell is currently meeting weekly to review evidence following the emergence of the Omicron variant. Based on ongoing engagement with the IPC cell, it seems clear that the IPC guidance on PPE usage is unlikely to step down significantly before spring, meaning PPE requirements are expected to continue at current levels for the time being. The last update to IPC guidance was published on 21 December 2021 to reflect the consensus opinion on Omicron. In the event of IPC guidance being withdrawn in 2022 to 2023, the department will issue a press release to inform stakeholders that the supply of free PPE will come to an end.
As set out above, asking providers to absorb PPE costs would have significant financial impacts on them, which could have negative impacts on their services, their staff and the people they care for. Maintaining free provision while we are still in the midst of the pandemic will help to ensure a stable and equitable supply of PPE to health and care sectors for the period April 2022 to March 2023, or until the point IPC guidance is withdrawn or amended significantly (whichever is sooner). This will enable all providers to comply with IPC guidance on PPE usage, allowing them to continue to deliver frontline services while also protecting frontline staff and the people they care for.
The market for PPE has increased exponentially as a consequence of the COVID-19 pandemic. The supply of free PPE by DHSC is for COVID-19 PPE only. Health and care providers are expected to purchase their business-as-usual PPE from other sources including wholesalers and suppliers. However, we recognise the concerns that wholesalers and suppliers have raised in the consultation about the impact on their businesses and the people they employ. Our impact assessment, which we expect to publish shortly, illustrates that the policy represents the effective use of public money to support health and social care services in delivering care in a way that protects the safety of the workforce and service users.
We will mitigate some of these concerns by continuing to emphasise that we are supplying PPE only for COVID-19 requirements, with providers still needing to purchase their business-as-usual PPE from wholesalers and other suppliers. The order limits on the PPE portal are set with this in mind, with limits based on:
- the latest available public health guidance
- COVID-19 trends
- PPE requirements modelling
- analysis
- provider feedback
We regularly review these order limits to check they are proportionate. In particular we will be pushing to ensure there is appropriate usage of nitrile gloves and that these are only used for COVID-19 purposes.
In conclusion, government has decided to extend free PPE to health and care sectors by up to one year to the end of March 2023 or until the IPC guidance on PPE usage for COVID-19 is either withdrawn or significantly amended (whichever is sooner).
Annex A: groups in scope of the consultation on the extension of free PPE
| User group | In scope? |
|---|---|
| NHS trusts or foundation trusts (acute trusts, ambulance trusts, community trusts and mental health trusts) | Yes |
| Community health and care | Yes |
| Dentists and orthodontists | Yes |
| General practice | Yes |
| Pharmacists | Yes |
| Optometrists | Yes |
| Mental health services | Yes |
| Palliative and end of life care, including hospices | Yes |
| Adult social care (residential care, domiciliary care, shared lives services, supported living, extra care, day services, personal assistants and unpaid carers) | Yes |
| Independent sector providers delivering NHS care | Yes |
| Other government departments | No |
| Non-health and care local authority services (for example, domestic violence shelters, rough sleeping shelters) | No |
| Children’s social care | No |
Annex B: consultation questions
Question 1: to what extent do you agree that free PPE should be extended beyond 31 March 2022 for 12 months?
-
strongly agree
-
agree
-
neither agree nor disagree
-
disagree
-
strongly disagree
-
don’t know
If you wish, please explain your position and provide any supporting evidence (preferably no more than 500 words).
Question 2: are there other options you think we should consider?
-
yes
-
no
If ‘yes’, please describe alternative options and why these might be helpful and provide any supporting evidence (preferably no more than 750 words).
Question 3 (for hospices only)
Hospices currently receive free PPE via a series of regional hubs which are largely reliant on volunteers, rather than via the PPE portal or local authorities or LRFs. Instead, hospices could use the PPE portal to access their COVID-19 PPE needs from 1 April 2022. To what extent do you agree that the regional hubs should be stood down and hospices onboarded to the portal?
-
strongly agree
-
agree
-
neither agree nor disagree
-
disagree
-
strongly disagree
-
don’t know
If you wish, please explain your position and provide any supporting evidence (preferably no more than 500 words).
Question 4: do you have any other views related to this consultation that you would like to express?
-
yes
-
no
If ‘yes’, please explain (preferably no more than 500 words).
Annex C: methodology
For the analysis of the open-ended questions, we identified key themes across all responses, and counted the number of times each theme was referred to per respondent type, using a recognised data science technique.
More specifically, we used an ‘unsupervised clustering’ data science technique to label each response with topics. This technique looks for clusters of words that appear frequently with each other in responses. We manually label these word clusters to give them a ‘human meaning’. For example, if the words ‘cost’, ‘financial’, ‘pressure’ and ‘funding’ appear in a cluster, we infer that this cluster is relating to financial pressures. Each cluster of words is known as a ‘topic’.
The process then maps these topics onto each open-ended consultation response, giving a probability that a given topic is being discussed in each response. We set a cut-off probability value, taking only the top, most likely topics per response. From this we have labelled each consultation response with discrete, common topics. We then analysed the results to see which topics were most frequently discussed by each respondent type, which respondent types were raising common themes, identifying key themes in the responses.
More information on text mining with R and the topic modelling approach used in this analysis
