Physical activity for general health benefits in disabled children and disabled young people: rapid evidence review
Updated 12 April 2022
Acknowledgements
We would like to thank the numerous disabled children and disabled young people, parents and guardians, sport and disability organisations, and health and social care professionals who gave valuable advice throughout the work and were key in the co-production of the infographic. This includes:
- Abbot’s Lea School (Liverpool)
- Bishop Barrington Academy (Bishop Auckland)
- British Blind Sport
- Cerebral Palsy Sport
- Clare Mount Specialist Sports College (Wirral)
- Durham Trinity School (Durham)
- Get Ahead, Disability Rights UK
- LimbPower
- Mill Water School (East Devon)
- North East Autism Society
- UK Deaf Sport
- SPARC
- Sport England
- Sport for Confidence
- St Vincent’s School: A Specialist School for Sensory Impairment and Other Needs (Liverpool)
- Thornhill Park School (Sunderland)
- Youth Sport Trust
We would like to thank Sophie Phillips (Durham University) for her input into search string development, and Dr Lindsay McNaughton (Durham University) for her advice on interpreting the findings.
We would also like to thank the members of our Children and Young People’s Physical Activity and Disability Expert Group that reviewed the report:
- Professor Kelly Arbour-Nicitopoulos, University of Toronto, Canada
- Dr Ben Browning, GP and parent, UK
- Dr Sam Browning, GP, Leeds CCG Clinical Lead for Learning Disability and parent, UK
- Dr Catherine Carty, The United Nations Educational, Scientific and Cultural Organisation (UNESCO) Chair: ‘Transforming the Lives of People with Disabilities, their Families and Communities, Through Physical Education, Sport, Recreation and Fitness’
- Professor Florentina Hettinga, Northumbria University, UK
- Dr Jennifer McAnuff, Northumbria University, UK
- Professor Samantha Ross, West Virginia University, USA
- Victoria Wells, National Lead, Youth Sport Trust, UK
- Jon White, Clare Mount Specialist Sports College, UK
- Professor Craig Williams, University of Exeter, UK
- Chloë Williamson, University of Edinburgh, UK
- Chris Wright, Head of Health and Wellbeing, Youth Sport Trust, UK
- Amanda Vernalls, Head of Research and Insight, Youth Sport Trust, UK
Citation
To cite this report please use: Smith B, Rigby B, Netherway J, Wang W, Dodd-Reynolds C, Oliver E, Bone L and Foster C. Physical activity for general health in disabled children and disabled young people: summary of a rapid evidence review for the UK Chief Medical Officers’ update of the physical activity guidelines. Department of Health and Social Care: London, UK. 2022.
Foreword by the UK Chief Medical Officers
The 2019 UK Chief Medical Officers’ physical activity guidelines set out the evidence for why moving more is beneficial to physical and mental health and wellbeing at all stages of the life course. In collaboration with academics from across the UK, the 2019 report updated the physical activity guidelines for different age groups and provided additional guidance for being active during pregnancy, for after giving birth, and for disabled adults.
However, there remained a clear gap in the evidence relating to the benefits and risks of physical activity for disabled children and disabled young people and an absence of specific guidelines.
With many thanks to colleagues at Durham University, University of Bristol and Disability Rights UK for their work, we present this report to address this important issue. It details the findings of a rapid evidence review into the health benefits and potential risks of physical activity for children and young people (aged 5 to 17) who have disabilities. The scientific evidence is clear that disabled children and disabled young people can benefit from being physically active in their everyday lives. The report makes recommendations for the amount, frequency and intensity of physical activity that is beneficial for health, although it is clear that even small bouts of activity can provide benefits.
This report is accompanied by an infographic that has been co-produced with disabled children, disabled young people, parents, carers, health and educational professionals, and several disability and sport organisations. The infographic communicates the evidence-based recommendations in an engaging and accessible way and incorporates the lived experiences of disabled children and disabled young people on why they participate in physical activity. Their key message is that they are more likely to engage in physical activity when it is inclusive, fun and enjoyable.
Together, this report and infographic are an important step forward in addressing the gap in physical activity guidance for disabled children and disabled young people and for tackling some of the misconceptions that exist around risks and safety. However, there remains much more to do to enable disabled children and disabled young people to get more physically active, and more generally for us to create more active communities.
We therefore encourage schools, parents, carers, health and social care professionals, and the sport and physical activity sector to communicate these guidelines across your professional wider networks; and to enable appropriate physical activity opportunities for disabled children and disabled young people in your communities.
Sir Frank Atherton, Chief Medical Officer for Wales
Professor Sir Michael McBride, Chief Medical Officer for Northern Ireland
Professor Sir Gregor Smith, Chief Medical Officer for Scotland
Professor Sir Chris Whitty, Chief Medical Officer for England
Executive summary
Disabled children and disabled young people are at increased risk of being typically inactive, particularly as they become older. These issues have been exacerbated by the COVID-19 pandemic.
This public health-focused report provides a review of the scientific evidence of the health benefits from physical activity, specifically for disabled children and disabled young people in non-clinical settings (aged 2 to 17 years). The research responds to a gap identified in the review of evidence for the 2019 UK Chief Medical Officers’ (CMOs’) physical activity guidelines. This important adjunct report enhances the comprehensiveness of the UK’s physical activity guidelines provision. It also provides future research recommendations. Furthermore, the report will also inform the first evidence-based infographic co-produced with disabled children and disabled young people, their parents and carers, health and social care professionals, and key disability and sport organisations to communicate meaningful messages about these physical activity recommendations, especially in relation to the frequency and duration of activity.
There is evidence that shows a likely relationship between engaging in physical activity and positive health outcomes for disabled children and disabled young people. This report also provides suggestions about the amount (that is, frequency, duration and intensity) of physical activity that is likely to be important for disabled children and disabled young people to undertake to benefit their health. Some physical activity is better than nothing, as small amounts can bring health benefits. For likely substantial health gains, it is important for disabled children and disabled young people to do 120 to 180 minutes of mostly aerobic physical activity per week, at a moderate-to-vigorous intensity. The evidence suggests that this may be achieved in different ways (for example, 20 minutes per day or 40 minutes 3 times per week). It is also important for disabled children and disabled young people to do challenging strength and balance-focused activities on average 3 times per week. No evidence was found to show that physical activity is unsafe for disabled children and disabled young people when it is performed at an appropriate level for their current levels of physical development, fitness, physical and mental functioning (accounting for disability classification and severity), health and physical activity.
This report provides evidence that aligns in part with the 2019 UK Chief Medical Officers’ physical activity guidelines for non-disabled children and disabled young people, as well as the 2020 guidelines published by the World Health Organization (WHO) for disabled children and disabled young people. However, there are also important differences in terms of recommended frequency and time. These are made based on the available evidence to provide recommendations specific to disabled children and disabled young people. The report also aids the communication and implementation of the guidelines by providing an evidence-base for disability groups, health and social care professionals, and sport and physical activity organisations to encourage physical activity to disabled children and disabled young people.
The guidelines are the first to have included a review of evidence solely focused on disabled children and disabled young people’s physical activity, and thus represent the most comprehensive guidance globally.
Introduction
With a public health focus, this report is about physical activity for health benefits among disabled children and disabled young people (aged 2 to 17 years). It offers the first UK CMOs’ physical activity guidelines developed specifically for and with disabled children and disabled young people, using only research that includes disability.
Numerous definitions of disability and ways of identifying as disabled exist in the UK. Some people and organisations prefer to use the term ‘disabled people’, while others prefer ‘people living with disabilities’ or ‘people with an impairment’. Respecting difference in terminology used across the UK and around the world, following the social model of disability the term ‘disabled people’ is used here. Disability is part of the human condition. It refers to people who have long-term physical (for example, cerebral palsy), sensory (for example, visual impairment), cognitive (for example, learning difficulties), or mental impairments (for example, depression) that, in interaction with various barriers, may hinder their full and effective participation in society on an equal basis with others.
Physical activity participation for all children and young people is an important public health concern. Regarding non-disabled children and non-disabled young people, regular physical activity is associated with better physiological, psychological and psychosocial health. For this population regular physical activity can improve health, strengthen muscles and bones, maintain healthy weight, improve sleep, build confidence and social skills, and improve mental health, concentration and learning. There is also some evidence to suggest that physical activity levels track from childhood into adulthood (Kwon, S; Tammelin, R). That is important because the benefits gained from physical activity in childhood are likely to carry forward into adulthood. In this way, physical activity can also provide cost savings by reducing or preventing non-communicable diseases that commonly occur in adulthood and destabilise the health and social care services. For adults, regular physical activity is associated with improved mental health and reduced risk of diabetes, obesity, and osteoporosis and certain cancers (for example, colon and breast cancers). Adults who have a physically active lifestyle also have a lower risk of cardiovascular disease, coronary heart disease and stroke compared to those who are inactive. As such, ensuring that all children are as active as possible throughout childhood is important for current and future public health.
However, increasing physical activity at a population level is complex, as there are many interdependent factors that shape children and young people’s experiences, or lack thereof, of physical activity. Despite the varied and substantial benefits of physical activity, many children and young people are insufficiently active (Breda, J; Guthold, R). This includes disabled children and young people (Activity Alliance (PDF, 2MB); Sport England). While some data suggests there is little difference in physical activity prevalence rates between non-disabled and disabled children and young people (PDF, 2.8MB), other data suggests that disabled children are less active than non-disabled children. It has also been reported that the gap in activity widens as disabled children get older. Furthermore, similar to disabled adults, data suggests the discrepancy in physical activity levels between disabled and non-disabled children and young people has increased during the SARS-CoV-2 pandemic. Significant health inequalities now exist and need addressing.
There has been an increasing focus on the importance of national policy to address population levels of physical inactivity and reduce health inequalities. One of the cornerstones of policy is national guidelines on physical activity (DHSC 2019; Chalkley, A). These represent statements based on a review of the evidence, stakeholder engagement, scientific meetings, and wider consultation on the amount and type of physical activity needed to benefit health. Physical activity guidelines are a central component of a coherent and comprehensive policy framework for public health action. They constitute an important information resource, guide national goal setting, and inform policy development to help support the public to be physically active and improve health, including work tackling wider structural and social determinants. Guidelines also serve as primary benchmarks for physical activity monitoring and surveillance initiatives (DHSC 2019; Chalkley, A).
In 2019 the UK CMOs’ physical activity guidelines were updated. These new guidelines provided physical activity recommendations for non-disabled and disabled adults, older adults aged 65 years and over, women during pregnancy and during postpartum, the under-5s age group, and non-disabled children and young people. However, physical activity evidence pertaining to disabled children and disabled young people was not reviewed in the 2019 UK guidelines. It was recommended that specific public health guidelines need to be developed for this group. Infographics were also recommended to support the communication of physical activity guidelines and enable schools as well as health and social care professionals to encourage physical activity behaviour change.
To address these omissions, and recognising the serious impact of such exclusion, the Department of Health and Social Care (DHSC) commissioned a review of the available evidence and, if sufficient, subsequently provide evidence-based recommendations in the form of a co-produced infographic. The review would thus offer the necessary scientific base to compare with evidence and recommendations outlined in the 2019 UK CMOs’ physical activity guidelines. It would also offer the vital scientific base to compare with recommendations outlined in the 2020 WHO global physical activity and sedentary behaviour guidelines for people living with disability (Carty, C; WHO 2020). The evidence-base for these WHO guidelines consisted almost entirely of studies that did not include disabled people.
The review also builds on and extends the 2011 Everybody Active, Every Day report and the Public Health Outcomes Framework 2019 to 2020 by Public Health England, as well as other major reports. These include:
- the 2011 World Report on Disability by the WHO
- the UK government strategy, Sporting Future: A New Strategy for an Active Nation
- the United States of America 2018 Physical Activity Guidelines Advisory Committee Scientific Report
- Sport England’s strategy for 2021 to 2031
This review and the infographic being developed will support the United Nations Sustainable Development Goal of reducing inequalities and a vision of no one left behind, along with ensuring healthy lives and promoting well-being for all. The work also supports the Convention on the Rights of Persons with Disabilities which ensures that disability and disabled people are included in guideline development. Disabled children and disabled young people had a significant role in co-producing the accompanying infographic. This is important because we know little about how to most effectively develop physical activity-related messages for disabled children and disabled young people.
This report presents the findings from a rapid evidence review conducted to meet the following objectives to:
- collate the evidence across different impairment groups on physical activity for health benefits in disabled children and disabled young people in a single resource that can be used across the sector. That includes for future public health messaging and by health and social care professionals, disabled people, families, schools, disability organisations, sport organisations, and other relevant groups to tailor recommendations
- compare the evidence with the recommendations for physical activity outlined in the 2019 UK CMOs’ guidelines for those aged under 5 years, and children and young people aged 5 to 18 years
- produce evidence-based public health recommendations with disabled children and disabled young people and their parents and guardians, and schools, sport and disability organisations, and health and social care professionals
- produce an evidence base to underpin and inform the co-production of an infographic for disabled children and disabled young people and their families, guardians and carers, health and social care practitioners, schools, disabled organisations, and sporting and physical activity organisations with the view to enable communication and implementation of the CMOs’ physical activity guidelines and inform guideline updates in the future
- identify gaps in the current evidence-base and make recommendations for research
This research addresses these objectives. It extends the reach of 2019 UK CMOs’ physical activity guidelines by using and providing evidence from available research that focuses on a population absent in these guidelines – that is, disabled children and disabled young people. It is the first to work with disabled children and disabled young people, their parents and guardians, health and social care professionals, schools, sport organisations, and disability organisations to provide evidence-based physical activity recommendations for good health for a range of experiences of disability.
The primary purpose of this report is to present overall physical activity recommendations for all disabled children and disabled young people. However, by also considering the evidence for a range of impairments rather than focusing on just one impairment, the review also supports efforts to tailor recommendations to the needs and realities of different impairment groups. The review can be used in the future in updates of national and global guidelines.
It is not the purpose of this review to establish clinical or impairment-specific guidelines. Neither is it the purpose to present a ‘how to’ guide for promoting physical activity. It is a public health-focused review that provides recommendations about ‘what is needed’ to improve health. The review underpinned and informed the development of appropriate messages for the infographic focused on physical activity for disabled children and disabled young people.
Further research activity will be required to build on and consolidate the evidence and findings from this review. Future research recommendations presented herein are based on gaps in research evidence, and were identified by disabled children and disabled young people and their families and guardians as relevant and meaningful to them.
Methods
This review is reported with reference to the Preferred Reporting Items for Systematic Reviews and Meta-analyses. Endnote software (Clarivate Analytics, UK) was used to facilitate management of the review process.
A rapid evidence review methodology was used to provide a systematic, yet feasible, search strategy to assess available evidence sources. Research shows that while rapid reviews have fewer stages and may be less rigorous than systematic reviews, both approaches produce similar conclusions (Abou-Setta, AM; Featherstone, RM; O’Leary, DF). In light of this research supporting the use and effectiveness of rapid reviews to produce compressive results, this approach was adopted.
Protocol
The protocol established by Public Health England’s review of physical activity for general health benefits in disabled adults (PDF, 94KB) provided the template for the current rapid review. Furthermore, the protocol was informed by the Preferred Reporting Items for Systematic Reviews and Meta-analyses protocols (PRISMA-P).
Research questions
The team produced the research questions based on the previous disabled adults’ physical activity review (PDF, 94KB) and in response to calls for such research made by disabled children and disabled young people, their parents and guardians, health and social care professionals, sport organisations, and leading disability charities. Questions were refined to maximise the potential for public health impact, as distinct to clinical implications, and uptake in evidence-informed policy and programmes.
Research questions were designed according the following frameworks: Feasible, Interesting, Novel, Ethical, and Relevant (FINER); and Population, Intervention/Domain, Comparison/Control Group, Outcome and Time (PICOT).
The finalised research questions were:
- what is the association between physical activity and health-related outcomes for disabled children and disabled young people?
- what is the evidence that physical activity improves or maintains the health of disabled children and disabled young people?
- what is known about the physical activity components of frequency, intensity, time and type (FITT) for disabled children and disabled young people?
- is there any evidence that physical activity is unsafe for disabled children and disabled young people?
Eligibility criteria
Inclusion and exclusion criteria were based on those established for the disabled adults’ physical activity review (PDF, 94KB), which were guided by the PICOT framework. Adaptations were made by the team based on the current research questions and critical reflection on the previously used criteria. The criteria covered the following dimensions:
- study type (for example, published primary research)
- population (for example, disabled children and disabled young people only)
- intervention/domain studied (for example, physical activity)
- relevance/outcome measures (for example, cardiorespiratory fitness)
- report characteristics (for example, publication date 01/01/07 to 09/04/21)
Full eligibility criteria and justifications are provided in Appendix 1.
Information sources and search strategy
Formal bibliographic database searches were the primary method of identifying evidence sources. The following databases were searched as they provided comprehensive repositories of citations, abstracts and full-text articles in fields relevant to the research questions: Web of Science, MEDLINE, SPORTDiscus. It was not possible to search the Cinahl database, as per the previous disabled adults’ physical activity review (PDF, 94KB), due to institution access restrictions.
Based on the strategy adopted in the disabled adults’ physical activity review (PDF, 94KB), the team produced a PICOT-informed research strategy in consultation with subject experts. In contrast to the disabled adults’ physical activity review, mental impairments and additional mental health outcomes were included in the search strings. Search strings used free-text terms (including phrase-searching), search-field descriptors, truncation operators, Boolean operators and database search limits. The strings were tested and refined through discussion and consensus. The full search strategy is presented in Appendix 2.
Database searches were run by Ben Rigby between 26 March and 9 April 2021.
A hand-search for work on disability and physical activity in children and young people was also conducted by Ben Rigby. Reference lists of review articles included after title and abstract screening (n = 84) and relevant reviews cited in the WHO’s physical activity guidelines that could be retrieved (n = 9) were searched for potentially relevant records.
Hand searching took place between 5 May and 13 May 2021.
Given the review’s rapid nature, the scope of database- and hand-searching was limited to research published and indexed between 1 January 2007 and 9 April 2021.
Selection process (screening)
Stage 1
All records identified in the database searches were independently screened by Ben Rigby and Jake Netherway on the basis of title and abstract to assess their eligibility. Following recommendations for rapid reviews (Abou-Setta, AM; Featherstone, RM; O’Leary, DF), a random 10% sample of records were screened by a panel consisting of Brett Smith, Emily Oliver and Caroline Dodd-Reynolds. Disagreements were resolved by discussion and consensus. Uncertainty did not preclude inclusion at this stage.
Stage 2
The full-text of relevant articles identified in the database searches were retrieved and reviewed to identify those meeting the inclusion criteria. Any records not retrieved in full-text by 18 May 2021, despite extensive efforts, were excluded. Initially, a 10% sample of records was independently screened by Ben Rigby and Jake Netherway. Discrepancies were resolved by discussion. Thereafter the remaining full-texts were divided equally (50% per reviewer) and screened independently by Ben Rigby and Jake Netherway from A to Z and Z to A by publication author, respectively. Uncertainty and discrepancies were resolved by discussion or by a third reviewer (Brett Smith), if needed. Identified review articles were hand-searched and excluded at this stage.
Stage 3
All records identified through hand-searching were independently screened by title and abstract at the point of searching by Ben Rigby. Full-texts of potentially relevant records were retrieved. Ben Rigby and Jake Netherway each screened 50% of these texts independently as above. Uncertainty and discrepancies were resolved by discussion or by a third reviewer (Brett Smith), if needed.
Data collection (extraction)
Data were collected by Ben Rigby and Jake Netherway using a pre-determined extraction sheet. To minimise bias and ensure accuracy, extraction was initially performed by both reviewers on a random 10% sample of included records. Both reviewers checked the concordance of extraction. Any discrepancies were resolved through discussion. Thereafter Ben Rigby screened 75% and Jake Netherway screened 25% of the remaining records independently. Originally, Ben Rigby and Jake Netherway were to screen 50% each, however alterations to the protocol were made due to IT issues and thus for pragmatic reasons. As a quality-assurance measure, the reviewers extracted in the inverse order to stage 2 screening (Ben Rigby extracted from Z to A and Jake Netherway from A to Z by author). Further uncertainties were resolved through discussion.
Additionally, data on core outcome improvements was extracted from systematic reviews identified in the search process, as well as those included in the WHO physical activity guidelines. Extraction from these reviews was performed by Ben Rigby, while assessment of their methodological quality was performed independently by both Ben Rigby and Charlie Foster, and any discrepancies resolved through discussion. The core positive outcomes are presented in Appendix 3.
Data items
Outcomes
Data were sought for the following variables, including all information on outcome measures, measurement time points and results at each point:
- cardiorespiratory fitness outcomes (for example, aerobic capacity, walking speed, heart rate, energy use)
- muscular outcomes (for example, strength, endurance, power, hypertrophy, speed, motor-skills, agility)
- disease risk and prevention outcomes (for example, step count, MVPA, body composition, blood pressure, blood lipids, sedentary behaviour, immune function, bone health, vascular health)
- psychological outcomes (for example, stress, anxiety, depression, happiness, mood, esteem, body satisfaction)
- functional skills outcomes (for example, gait patterns, falls prevention, balance, mobility, flexibility, activities of daily living)
- (psycho)social, community, and wellbeing outcomes (for example, wellbeing, pain, social development, quality of life, community development, fatigue, perceived health)
- cognitive outcomes (for example, attention, memory, executive functions)
- behavioural outcomes (for example, classroom behaviour, hyperactivity)
Other variables
The following additional data items were collected: bibliometric data, country of origin, study design, population and participant characteristics, disability category, intervention components (frequency, intensity, time, type; FITT), behavioural components, safety/adverse effects information, and additional notes including key limitations.
Furthermore, implementation factors were extracted from qualitative papers only (for example, barriers and facilitators to implementing physical activity for disabled children and disabled young people). Qualitative research had previously been identified as highly valued by disabled people (PDF, 94KB).
Where information about any data collection item was missing, no assumptions were made by the reviewers, with the exception of likely country of origin based on available information (for example, author affiliations), which was recorded against a statement of ‘not reported’ in relevant studies.
Reporting of outcomes
The review identified multiple outcomes that were likely to be associated with physical activity in the literature. To ensure consistency with the literature, data were extracted to reflect what the authors of studies identified as potentially important outcomes. We used the same terminology for outcomes as reported by the research authors.
Study risk of bias assessment
Level of evidence was recorded for all identified quantitative studies. A random 10% sample was initially graded by both Ben Rigby and Jake Netherway. Discrepancies were resolved by discussion and consensus. Thereafter, the 2 reviewers independently graded the remaining studies alongside data extraction 75% and 25%, respectively).
The criteria for each level of evidence were as follows.
Level 1 (high):
- a control group was used
- a pre-/post- or repeated-measures design was used
- groups were randomised
- example: randomised controlled trial
Level 2 (moderate):
- pre-/post- and/or repeated measures design was used
- a control or comparison group may have been used, but was not required
- groups were not required to be randomised
- a retrospective design may be used
- examples: cohort, case-control, time series studies
Level 3 (low):
- post-test only or cross-sectional design was used
- case studies (individual or very small cohort)
- uncontrolled study
- a retrospective design may be used
- example: cross-sectional study
Methodological quality of included studies was assessed using the Quality Assessment Tool for Studies with Diverse Designs (QATSDD). Included papers were rated against QATSDD quality criteria on a 4-point scale from ‘not at all’ (0) to ‘complete’ (3). Percentage scores were calculated using the actual score and the maximum total score of 42 for quantitative studies and 39 for qualitative studies. Inter-rater reliability for qualitative research (item-14) was excluded from the assessment, as recommended, due to being a flawed and ineffective measure (Levitt, HM (PDF, 165KB); Smith, B). Papers scoring over 74.9% were rated as being of ‘high’ quality, those between 50% and 74.9% as ‘good’ quality, 25% to 49.9% as ‘moderate’ and below 25% as ‘poor’. This scoring is consistent with other disability-focused evidence reviews across various disciplines, including health-related studies (Augestad, LB; Harrison, RA; Klingenberg, OG).
A random 10% sample of studies was assessed independently by Ben Rigby and Wei Wang. Discrepancies were resolved through discussion and consensus. The remaining studies were assessed by Wei Wang, and any further queries were discussed and resolved through discussion with Ben Rigby.
To further enhance the quality of this review, the team also compared all results with core findings extracted from review studies and key physical activity reports, including the WHO physical activity guidelines, UK physical activity guidelines and the USA physical activity guidelines.
Synthesis methods
The team synthesised the results to develop concluding statements for each research question. Data was synthesised in tabular form to provide a breakdown of:
- evidence for each major health outcome group for different impairment groups
- evidence of the FITT principles associated with major health outcome groups for different impairment groups
- any information related to safety of physical activity for disabled children and disabled young people
No statistical synthesis was conducted.
Throughout this review, studies were categorised in each of the 4 major impairment groups (physical, intellectual and learning, sensory, and mental) as recognised by the UK government. It is acknowledged that different definitions and categorisations exist, both nationally and globally. For example, attention deficit hyperactivity disorder (ADHD) is sometimes considered a learning disability, at other times a learning difficulty. In the context of this review, intellectual and learning disabilities combined are defined as a significantly reduced ability to understand new or complex information (impaired intelligence), with a reduced ability to cope independently (impaired social functioning), that started before adulthood. The majority of papers reviewed did not differentiate between intellectual and learning disabilities. An additional mixed category was also used to capture studies that presented data from samples across different impairment groups. Where sufficient data permitted, additional analyses were conducted according to sub-types within impairment groups.
Development of a narrative summary
A narrative summary of the synthesis was developed and research recommendations related to the questions were produced.
Table 1: matrix showing level and quality of evidence coding
| Quality assessment | Evidence level 1 | Evidence level 2 | Evidence level 3 |
|---|---|---|---|
| High | Strong evidence | Strong evidence | Moderately strong evidence |
| Good | Strong evidence | Moderately strong evidence | Moderately weak evidence |
| Moderate | Moderately strong evidence | Moderately weak evidence | Weak evidence |
| Poor | Moderately weak evidence | Weak evidence | Weak evidence |
The types of studies that provided strong evidence included randomised controlled trials (RCTs) of good quality. Moderately strong evidence comprised of moderate RCTs or good quality quasi-experimental, case control and similar-type studies. Moderately weak evidence was typically provided by moderate quality quasi-experimental, case control or similar-type studies. Weak evidence typically comprised case study, post-intervention or cross-sectional design studies. The outcomes of this assessment informed the recommendations within the results section.
Qualitative studies of high or good quality provided contextual evidence about physical activity, such as the barriers and facilitators to being active, necessary for implementation purposes.
Sense-checking
The narrative summary was sense-checked by a panel of people with lived experience and expert stakeholders in the fields of disabled children and disabled young people, physical activity for health, and physical activity guidelines development and communication. This panel included representation from parents of disabled children and disabled young people, healthcare professionals, charities and academia. The panel’s comments were discussed by the team and incorporated into the final report as appropriate.
See acknowledgements above for a list of expert group members.
Results
Study selection
Flow of studies
Database searches yielded 3,309 records after duplicates were removed. Following title and abstract screening (stage 1), 354 full-text records were retrieved and assessed for eligibility. Hand-searching of review articles and screening of identified records yielded an additional 73 records for full-text assessment. In total, 176 reports were eligible for inclusion in the current review, which included 9 qualitative studies.
See Appendix 4 for the PRISMA flow diagram.
Excluded studies
251 reports were excluded during full-text screening for the following reasons:
- wrong study type, including review articles (n = 90)
- no (disaggregated) data on populations of interest (n = 88)
- incorrect intervention or domain, including clinical treatment and therapy studies (n = 54)
- no data on health outcomes as a result of physical activity (n = 18)
- not published in English (n = 1)
See Appendix 5 for a list of excluded studies and justifications.
Study characteristics
Among the 176 included records were:
- 71 randomised controlled studies
- 77 uncontrolled studies; 31 studies with follow-up periods (4 to 36 weeks)
- 9 studies that presented post-intervention data only
This review examined the health outcomes from physical activity for disabled children and disabled young people with physical disabilities (79 studies), intellectual and learning disabilities (79 studies), sensory impairments (9 studies) and mixed disabilities (9 studies). Studies in this latter category presented data across impairment groups that could not be disaggregated, rather than data about individuals with multiple disabilities. Searches yielded no studies explicitly about children and young people with mental impairments. Table 2 provides a breakdown of impairment sub-types in studies for each major impairment group.
Due to the rapid nature of this review, studies with multiple publications reporting on the same cohort have not been identified and combined. Therefore, grand mean sample statistics could not be generated. Nevertheless, sample sizes were typically modest. Fifty-six studies had a sample ≥30 of which 18 had a sample ≥50. Twenty-six studies had a sample <10, of which 7 had a single participant. Participants in included studies were aged 2 to 17. There were considerably more male than female participants across the studies.
The number of studies by impairment type can be broken down into the following:
Table 2: breakdown of impairment sub-types
| Physical disability | Number of studies |
|---|---|
| Cerebral palsy | 65 |
| Developmental coordination disorder | 7 |
| Mixed | 2 |
| Muscular dystrophy | 1 |
| Spinal cord dysfunction | 2 |
| Sub-type not reported | 2 |
| Intellectual and learning disabilities | Number of studies |
|---|---|
| AD/HD | 33 |
| Autistic spectrum disorder | 11 |
| Behavioural health disorder | 1 |
| Down syndrome | 8 |
| Mixed | 2 |
| Unspecified learning disability | 3 |
| Sub-type not reported | 21 |
| Sensory impairment | Number of studies |
|---|---|
| Hearing impairment | 1 |
| Mixed (hearing impairment or visual impairment) | 2 |
| Visual impairment | 6 |
| Mixed disabilities | Number of studies |
|---|---|
| Cerebral palsy or intellectual disability | 1 |
| Cerebral palsy or severe traumatic brain injury | 1 |
| Sub-types not reported | 7 |
Where reported, research was conducted with subpopulations from 32 countries. The USA was the most commonly reported research setting (25 studies) and was the only country from which participants were drawn from each major impairment group. Forty-one studies did not report the country in which study populations were based. Assessment of authorship of these studies suggested that no countries in addition to those reported were likely to have been included as research settings. The reported global distribution of included studies is shown in Figure 1.
See Appendix 6 for a reference list of included papers that informed the review, and Appendix 7 for summary characteristics of individual studies, including country of origin.
Figure 1: The global distribution of studies included in the rapid review by disability group
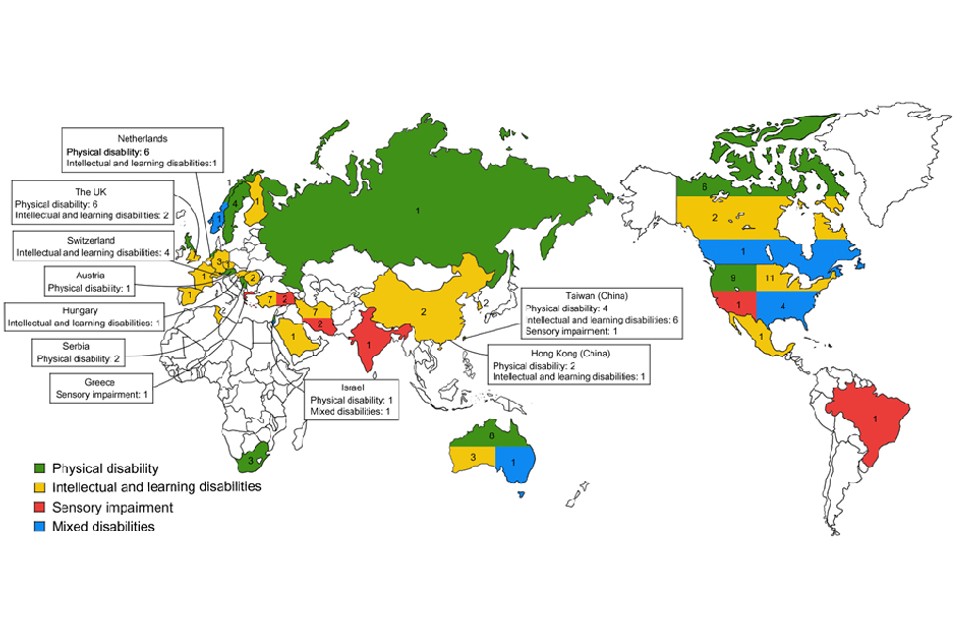
Table 3: text alternative to global distribution of studies map
| Country | Number of physical disability studies | Number of intellectual and learning disabilities studies | Number of sensory impairment studies | Number of mixed disabilities studies |
|---|---|---|---|---|
| Australia | 8 | 3 | 0 | 1 |
| Austria | 1 | 0 | 0 | 0 |
| Brazil | 0 | 4 | 0 | 0 |
| Canada | 6 | 2 | 0 | 1 |
| China | 0 | 2 | 0 | 0 |
| Czech Republic | 0 | 1 | 0 | 0 |
| Finland | 0 | 1 | 0 | 0 |
| France | 0 | 1 | 0 | 0 |
| Germany | 0 | 3 | 0 | 0 |
| Greece | 0 | 0 | 1 | 0 |
| Hong Kong | 2 | 1 | 0 | 0 |
| Hungary | 0 | 1 | 0 | 0 |
| India | 0 | 0 | 1 | 0 |
| Iran | 0 | 7 | 2 | 0 |
| Israel | 1 | 0 | 0 | 1 |
| Mexico | 0 | 1 | 0 | 0 |
| Netherlands | 6 | 1 | 0 | 0 |
| Norway | 1 | 0 | 0 | 1 |
| Romania | 0 | 2 | 0 | 0 |
| Russia | 1 | 0 | 0 | 0 |
| Saudi Arabia | 0 | 1 | 0 | 0 |
| Serbia | 2 | 0 | 0 | 0 |
| South Africa | 3 | 0 | 0 | 0 |
| South Korea | 0 | 2 | 0 | 0 |
| Spain | 1 | 0 | 0 | 0 |
| Sweden | 4 | 0 | 0 | 0 |
| Switzerland | 0 | 4 | 0 | 0 |
| Taiwan | 4 | 6 | 1 | 0 |
| Tunisia | 0 | 2 | 0 | 0 |
| Turkey | 0 | 7 | 2 | 0 |
| United Kingdom | 6 | 2 | 0 | 0 |
| USA | 9 | 11 | 1 | 4 |
Risk of bias in studies
Level of evidence
The total number of quantitative studies at each level of evidence were as follows: level 1 = 70, level 2 = 70 and level 3 = 27.
Quality assessment
The totals for each quality grade across all studies, as assessed using the QATSDD tool, were as follows: high = 1; good = 28; moderate = 136; and poor = 11. Regarding the subset of qualitative studies, these were graded as follows: high = 1; good = 2; and moderate = 6.
Table 4: number of included quantitative studies in each level-by-quality category.
| Quality assessment | Evidence level 1 | Evidence level 2 | Evidence level 3 |
|---|---|---|---|
| High | n = 0 | n = 0 | n = 0 |
| Good | n = 12 | n = 11 | n = 3 |
| Moderate | n = 52 | n = 54 | n = 24 |
| Poor | n = 6 | n = 5 | n = 0 |
Table 4 displays the level-by-quality of evidence matrix for all included quantitative studies. In total, there were 12 strong studies, 63 moderately strong studies, 63 moderately weak studies, and 29 weak studies.
See Appendix 7 for a breakdown of level and quality of evidence for each individual study.
Results of syntheses
The evidence used in this report is summarised in Appendix 7. This includes results from individual studies.
Question 1a: what is the association between physical activity and health-related outcomes for disabled children and disabled young people?
In most cases, there was insufficient strength of evidence to conclusively demonstrate a formal association between physical activity and positive health-related outcomes for disabled children and disabled young people in general.
Crucially, however, there was no evidence of a lack of association between physical activity and health. Nevertheless, there was sufficient strength of evidence relating to a limited number of outcomes in specific impairment groups.
Question 1b: what is the evidence that physical activity improves or maintains the health of disabled children and disabled young people?
Despite the issues of methodological strength, both the quantitative and qualitative evidence reviewed presented consistently positive trends in outcome data, which when viewed in the context of previous research reviews and public health guidance, indicated that physical activity likely contributes to the improvement, or at least maintenance, of the health of disabled children and disabled young people.
General overview across impairment groups
Considering all impairment groups collectively, there is insufficient evidence to conclusively demonstrate a formal association between physical activity and positive health-related outcomes for disabled children and disabled young people.
Overall, there is moderately weak evidence that across impairment categories, physical activity may be associated with improved cardiorespiratory fitness, muscular outcomes and functional skills, as well as improvements in some aspects of disease risk and prevention, psychosocial wellbeing and community health, cognition and behaviour. A moderately strong evidence-base was found for 8 outcomes in the available data. There was a weak evidence-base for the quality of life outcome.
In several cases, there was a lack of research from which to draw safe conclusions. This was particularly evident in relation to psychological outcomes, for which there was insufficient data across all outcomes, despite positive findings in previous systematic reviews (see Appendix 3). Furthermore, it is worth noting that research elsewhere has consistently indicated positive associations between physical activity and psychological outcomes (for example, depression symptoms or self-concept), including among children in general (Biddle, SJ; Kapsal, NJ; Rodriquez-Ayllon, M) and disabled people (Smith, B (PDF, 1.6MB); Subramaniapillai, M). Among the outcomes cited as having insufficient data, there were still positive trends in the available studies for the following outcomes: muscle architecture/hypertrophy; happiness; confidence; cholesterol; sleep; independence; and perceived psychosocial health.
Figure 2: breakdown of evidence for each outcome for all impairment groups collectively
Cardiorespiratory fitness:
- moderately strong: walking/running/cycling speed
- moderately weak:
- aerobic capacity and cardiovascular fitness
- exercising and resting heart rate
- energy expenditure
Muscular outcomes:
- moderately strong: motor skills (function and proficiency)
- moderately weak:
- muscular strength
- agility
- power
- muscular endurance
- insufficient data available:
- muscle architecture (hypertrophy)
- spasticity
Disease risk and prevention:
- moderately weak:
- body composition
- BMI
- insufficient data available:
- bone density
- cholesterol
- sleep quality
Cognitive outcomes:
- moderately strong:
- attention
- executive functions
- insufficient data available:
- reaction time
- metacognition
Phycological outcomes:
- insufficient data available:
- depression
- happiness
- confidence
- anxiety
- stress
- self-concept
Functional skills:
- moderately strong:
- balance
- coordination
- moderately weak:
- mobility
- flexibility
- insufficient data available:
- gait patterns
- activities of daily living
Psychosocial community and wellbeing:
- moderately strong: social development
- moderately weak: achievement and aspiration
- weak: quality of life
Insufficient data available:
- perceived psychosocial health
- fatigue and energy levels
- pain
- independence
Behavioural outcomes:
- moderately strong: problem behaviours
- moderately week:
- hyperactivity
- non-specific behavioural improvements
Insufficient data available: classroom behaviours
An analysis of outcomes by type of evidence presented similar findings. Level 1 studies (that is, typically RCTs) often presented mixed results, with a few notable exceptions for those outcomes for which moderately strong evidence was identified or where only a few studies were identified. The lack of consistent outcomes presented in high-quality RCTs is a significant factor in the overall findings of this review.
Issues of methodological strength, however, should not detract from the finding that overall, the quantitative evidence reviewed presented consistently positive trends in outcome data: 66 of 70 level 1 studies, 68 of 70 level 2 studies and 24 of 27 level 3 studies reported improvements in at least one health outcome. Likewise, improvements in health outcomes were reported in 8 of 9 qualitative studies, particularly in relation to psychosocial factors. These consistencies emphasise the likely contribution of physical activity to improved health.
Detrimental outcomes were reported against 8 outcome measures in 6 of 176 included studies.
Evidence by impairment category
The evidence for a range of impairments is identified to support efforts to tailor recommendations to the needs and realities of different impairment groups.
In addition to the overall trends presented above, there was sufficient strength of evidence relating to a limited number of outcomes in specific impairment groups. It should be noted that these findings may result from the focus of identified studies. Research may have collected data on outcomes likely to have beneficial effects for target subpopulations, but may be replicable in other groups where research currently lacks.
Regarding physical disabilities, there was moderately strong evidence that physical activity is associated with social development, motor skills, muscular strength, walking/cycling/running speed, and mobility. The evidence for these latter 2 outcomes is most relevant to children and young people with cerebral palsy. While there was insufficient evidence related to physical disabilities alone, there were also positive trends in attention, and muscular architecture/hypertrophy. However, caution is noted regarding balance outcomes, where the evidence is more mixed, particularly among children and young people with cerebral palsy.
Regarding intellectual and learning disabilities, there was moderately strong evidence that physical activity is associated with social development, motor skills, muscular endurance, coordination, balance, attention and executive functions (although planning and working memory data is mixed). There was moderately weak evidence related to power and agility. Insufficient data but positive trends related to problem behaviours and reaction time.
Moderately strong associations between physical activity and health outcomes for disabled children and disabled young people with physical or intellectual and learning disabilities are visualised in Table 5.
Table 5: moderately strong evidence for health outcomes for physical and intellectual disabilities
| Physical disabilities | Intellectual and learning disabilities | |
|---|---|---|
| Walk, cycle or run speed | Yes | No |
| Mobility | Yes | No |
| Muscular strength | Yes | No |
| Social development | Yes | Yes |
| Motor skills | Yes | Yes |
| Muscular endurance | No | Yes |
| Coordination | No | Yes |
| Balance | No | Yes |
| Attention | No | Yes |
| Executive function | No | Yes |
While there is some evidence for physical activity improving health of children and young people with sensory impairments (9 studies), there are few high level studies that have examined physical activity and health benefits for this group (see Appendix 7). Furthermore, much of the available evidence combines hearing and visual impairments. Previous qualitative research has identified perceived benefits to this group, and positive trends were identified here in relation to balance, coordination and sleep outcomes.
Where studies had assessed outcomes across mixed disability groups, the findings were consistent with the overall evidence assessment above. Small but positive trends were identified for this group of studies in relation to independence, social development, flexibility, muscle endurance and body composition.
This review identified no studies that examined the effect of physical activity on health outcomes for children and young people classified in a study as having mental impairments. However, one systematic review that was selected to inform the wider findings of this project included 3 studies (one each of strong, moderate and weak quality) relevant to this impairment category, but which fell outside our inclusion criteria. Two of the 3 studies showed null findings on feelings and depression outcomes from aerobic activities. Nevertheless, there is emerging evidence elsewhere that children and young people within this impairment group (for example, bipolar disorder) may benefit comparably to non-disabled peers.
Conclusions
Physical activity likely contributes to the improvement, or at least maintenance, of the health of disabled children and disabled young people.
Currently there is insufficient strength of evidence to conclusively demonstrate a formal association between physical activity and positive health-related outcomes for disabled children and disabled young people in general. This conclusion is influenced significantly by a lack of high-quality RCT studies with consistent positive results. Crucially, however, there was no evidence of a lack of association between physical activity and health. There was, however, sufficient strength of evidence relating to a limited number of outcomes in specific impairment groups.
Nevertheless, the ratings and conclusions pertaining to quality, level and agreement of evidence of the sub-components of outcomes are consistent with those reported in previous systematic reviews (see Appendix 3) and evidence reviewed by WHO. Naturally, there is variation in the results of individual studies included in each review. Discrepancies, may in part be methodologically driven. In relation to the current study, this may be a function of the assessment tool used to accommodate diverse study designs, or differences in eligibility criteria.
Despite the issues of methodological strength, both the quantitative and qualitative evidence reviewed presented consistently positive trends in outcome data. When viewed in the context of the aforementioned previous research reviews, this indicated that physical activity likely contributes to the improvement, or at least maintenance, of the health of disabled children and disabled young people. This conclusion, reached with moderate certainty, about the likely health benefits of physical activity is consistent with those drawn in relation to disabled populations in existing public health guidance globally. (WHO guidelines; Smith, B (PDF, 94KB); USDHHS)
Question 2: what is known about the physical activity components of FITT (frequency, intensity, time and type) for disabled children and disabled young people?
Findings related to FITT should be considered in the context of the moderately weak methodological strength of included studies.
Nevertheless, the available evidence indicates that for likely improved health outcomes it is important for disabled children and disabled young people to participate in 120 to 180 minutes of aerobic physical activity per week at a moderate-to-vigorous intensity. The evidence suggests that this may be achieved in different ways (for example, 20 minutes per day or 40 minutes 3 times per week), and how to translate this evidence on frequency and duration into the most appropriate message will be examined by the infographic co-producers (that is, disabled children and disabled young people).
Irrespective of messaging preferences, there was little evidence to support the WHO recommendations that disabled children and disabled young people engage in at least a weekly average of 60 minutes per day of moderate-to-vigorous intensity physical activity.
There is some evidence that children and young people may accrue certain health benefits when they engage in physical activity at a lower frequency, intensity or duration. Thus, some physical activity is good, but more is better if appropriately based on an individual’s health, functioning and fitness status.
It is also important for disabled children and disabled young people to do challenging but manageable strength and balance-focused activities on average 3 times per week to accrue health benefits.
Progression toward achieving these physical activity levels should account for individuals’ current levels of physical development, fitness, physical and mental functioning (including disability classification and severity), health and physical activity.
There was also some evidence to suggest health benefits from lower amounts of physical activity, therefore some activity is better than nothing.
The table below offers a breakdown of the evidence found for different health outcomes across the specified range of impairment groups.
Table 6: a breakdown of the evidence for FITT by impairment group
| Physical disabilities | Intellectual and learning disabilities | Sensory impairments | Mental impairments | Mixed disabilities | |
|---|---|---|---|---|---|
| Cardiorespiratory fitness | Moderately weak evidence | Moderately weak evidence | Insufficient evidence | No evidence | Insufficient evidence |
| Muscular outcomes | Moderately strong evidence | Moderately strong evidence | Insufficient evidence | No evidence | Moderately weak evidence |
| Disease risk and prevention | Moderately weak evidence | Moderately strong evidence | Insufficient evidence | No evidence | Insufficient evidence |
| Psychological outcomes | Insufficient evidence | Moderately weak evidence | Insufficient evidence | No evidence | Insufficient evidence |
| Functional skills | Moderately weak evidence | Moderately weak evidence | Moderately strong evidence | No evidence | Insufficient evidence |
| Psychosocial, community and wellbeing | Moderately strong evidence | Moderately strong evidence | Insufficient evidence | No evidence | Moderately weak evidence |
| Cognitive outcomes | Moderately weak evidence | Moderately strong evidence | No evidence | No evidence | No evidence |
| Behavioural outcomes | Insufficient evidence | Moderately strong evidence | No evidence | No evidence | No evidence |
Cardiorespiratory fitness
The total number of records reviewed for this outcome category was 49. Thirty-one of these studies were graded ‘moderately weak’ or ‘weak’. There is thus moderately weak evidence that physical activity is likely to be effective at improving cardiorespiratory fitness outcomes across impairment groups among disabled children and disabled young people. Taken separately, there was insufficient evidence from cohorts with sensory impairments or studies that included mixed disabilities.
Available evidence suggests that 30 to 60 minutes of moderate-to-vigorous (50 to 80% HRmax) mostly aerobic physical activity 2 to 4 times per week, may be effective for cardiorespiratory fitness benefits. There is also evidence, albeit typically weaker, that suggests benefits may be accrued from fewer weekly bouts of activity (for example, 1 to 2), or less cumulative duration (for example, 60 to 75 minutes per week). This may present an important consideration for initiating physical activity among typically inactive and sedentary disabled children and disabled young people.
Muscular outcomes
The total number of records reviewed for this outcome category was 91. Forty-nine of these studies were graded ‘moderately weak’ or ‘weak’, and null findings were presented in approximately half of stronger studies. There is thus moderately weak evidence that physical activity is likely to be effective at improving muscular outcomes (for example, motor skills, and muscular strength and endurance). Taken separately, there was insufficient evidence from cohorts with sensory impairments.
Available evidence suggests improved muscular outcomes may result from 3 sets of 10 to 12 reps of strength and balance-focused activities. It is important that this activity is carried out 2 to 4 times per week, at a manageable but challenging tailored load. There is some weaker evidence that suggests that similar benefits may be accrued from an increased number of sets (4 to 6) and reps (15 to 20) at lighter loads (40% of max), or fewer reps (6 to 8) at higher loads (75 to 100% of max). The available evidence also indicates that improved muscular outcomes may be gained from participating in mostly aerobic physical activities, as set out above (see cardiorespiratory fitness).
It is particularly important to consider disabled children and disabled young people’s current levels of physical development and functioning (accounting for disability classification and severity), when performing strength and balance-focused activities.
Disease risk and prevention
The total number of records reviewed for this outcome category was 21. Twelve of these studies were graded ‘moderately weak’ or ‘weak’, although findings were moderately strong for intellectual and learning disabilities. Overall, however, there is moderately weak evidence that physical activity is likely to be effective at improving disease risk and prevention outcomes. Taken separately, there was insufficient evidence from cohorts with sensory impairments or studies that included mixed disabilities.
However, due to a lack of reported physical activity intensity data in the included studies, it is not possible to determine the FITT components likely associated with these outcomes. Positive outcomes were typically evidenced following mostly aerobic or sports-based activities. Their frequency and duration were comparable to those outlined above (see cardiorespiratory fitness).
Psychological outcomes
The total number of records reviewed for this outcome category was 15. Seven of these were graded ‘moderately weak’ or ‘weak’, and 3 were qualitative and therefore did not contribute to the assessment of FITT. Overall, there is thus moderately weak evidence that physical activity is likely to be effective at improving psychological outcomes. Taken separately, there was insufficient evidence from cohorts with physical or sensory impairments, or studies that included mixed disabilities.
Due to a lack of reported physical activity intensity data in the included studies, it is not possible to determine the FITT components likely associated with these outcomes. However, positive outcomes were typically evidenced following mostly aerobic or sports-based activities of lower frequency (1 to 2 times per week). The mechanisms for these outcomes are unclear. Nevertheless, it may be likely that disabled children and disabled young people may experience improved psychological outcomes if participating in physical activity as set out against other outcomes above.
Functional skills
The total number of records reviewed for this outcome category was 81. Forty-six of these studies were graded ‘moderately weak’ or ‘weak’, although evidence among sensory impairment studies was moderately strong. Overall, however, the evidence base is moderately weak. Taken separately, there was insufficient evidence from studies that included mixed disabilities.
Available evidence suggests that improved functional skills may be gained from 45 to 60 minutes of mostly aerobic physical activity 2 to 3 times per week. Evidence related to intensity is typically from weaker studies, but this best available evidence indicates that it may be important for activity to be of moderate-to-vigorous intensity (60 to 80% of HRmax). Improved functional skills may also be gained by participating in resistance-based activities as set out above (see muscular outcomes). Weaker evidence suggests that certain functional skills improvements (for example, balance) may be gained by participating in low-to-moderate intensity physical activities (for example, Pilates and Tai Chi).
Psychosocial, community and wellbeing
The total number of records reviewed for this outcome category was 35. Thirteen of these studies were graded strong or moderately strong evidence. Qualitative studies aside (n = 7), this thus means the evidence-base is moderately strong. Taken separately, there was insufficient evidence from cohorts with sensory impairments.
Available evidence suggests that 40 to 90 minutes of mostly aerobic or sports-based physical activities 2 to 3 times per week is likely to be effective for improving psychosocial, wellbeing and community outcomes. Evidence related to intensity is typically from weaker studies and suggests it may be important for activity to be of moderate-to-vigorous intensity (50 to 80% HRmax). It is worth noting that such outcomes (for example, social development) may be associated as much with the physical activity environment, as they are with the FITT components of said physical activity. An assessment of this relationship is beyond the scope of the current review.
Cognitive outcomes
The total number of records reviewed for this outcome category was 42. Thirteen of these studies were graded strong or moderately strong evidence. Once qualitative studies are disregarded (n = 7), this thus means the evidence-base is moderately strong overall and from cohorts with intellectual and learning disabilities (32 of 37 ADHD). No evidence was found relating to FITT among cohorts with sensory impairments or from studies that included mixed disabilities.
Available evidence suggests that improved cognitive outcomes may be gained from 30 to 60 minutes of moderate-to-vigorous (50 to 70% HRmax) mostly aerobic physical activity 2 to 3 times per week. While there is insufficient intensity data, some strong studies also demonstrated positive cognitive outcomes from strength and balance-focused activities. There is some limited but strong evidence that acute bouts of physical activity may lead to immediate executive function improvements.
Behavioural outcomes
The total number of records reviewed for this outcome category was 17 (including 14 from cohorts with intellectual and learning disabilities, 10 of which focused on ADHD). Twelve of these studies were graded ’strong’ or ‘moderately strong’. Thus, there is moderately strong evidence that physical activity is effective at improving behavioural outcomes. Taken separately, there was insufficient evidence from cohorts with physical or sensory impairments. No evidence was found relating to FITT from studies that included mixed disabilities.
Due to a lack of reported physical activity intensity data in the included studies, it is not possible to determine the FITT components likely associated with these outcomes. However, positive outcomes were typically evidenced following mostly aerobic activities of 40 to 60 minutes, 2 to 3 times per week. There is some moderately weak evidence that shorter bouts (10 to 20 minutes) may be effective in educational settings.
Comparison to existing public health guidance
To our knowledge, this is the first comprehensive review of physical activity FITT components associated with broad-ranging health outcomes among solely disabled children and disabled young people. Therefore, the guidance and associated evidence detailed above improvements that which was included in recent physical activity guidelines for disabled children and disabled young people from the USA and WHO (2020).
It is worth noting that WHO guidance was based, in part, on a narrow selection of reviews with limited research that included disabled children and disabled young people. That may have precluded the development of more specific guidance from WHO for particular health outcomes. However, the findings from these reviews were similar in outcomes and methodological quality and confidence as presented here (see Appendix 3). The US guidelines did not present a consideration of FITT principles.
The WHO recommends that, for health benefits, children and adolescents living with disability participate in strengthening exercises 3 times per week, as well as a weekly average of 60 minutes per day of mostly aerobic physical activity. The UK guidelines for non-disabled children and young people include the same advice about aerobic physical activity, albeit do not include an explicit FITT statement about strengthening activities.
The findings of the current review align with WHO’s recommendations for strengthening activities (that is, 3 times per week), but also differ in terms of aerobic physical activity. The available evidence from studies that include disabled children and disabled young people suggests 120 to 180 minutes per week of aerobic physical activity for health benefits, which, as highlighted above, may be translated into alternative messages by the infographic co-producers (for example, 20 minutes per day or 40 minutes 3 times per week). The frequency and duration derived solely from the available evidence differs to the recommendation of a weekly average of 60 minutes per day made by WHO. We found little evidence to support this WHO recommendation.
It should be stressed that this lack of evidence does not mean the WHO recommendations are invalid or that these UK guidelines are superior. It simply needs recognising that the 2 are methodologically different. The set of guidelines reported here is based on the available evidence from studies that included disabled children and disabled young people. This focus was deemed important by those children and young people with lived experience of disability, along with their parents, during pre-review workshops. Evidence for possible physiological differences between disabled and non-disabled children and young people, within certain impairment groups, also highlighted the importance of reviewing studies that included disabled children and disabled young people. It is hoped that the differences between guidelines outlined in this report may stimulate both debate and research attention toward a common global goal of improving the health and lives of disabled children and disabled young people through physical activity.
The evidence available for disabled children and disabled young people is, however, comparable in several ways to that set out in the guidelines for disabled adults. Several reasons for this may exist, which we consider here. First, there may be different physiological responses to physical activity for certain impairment groups, such as children with cerebral palsy, samples of whom featured heavily in the current review and thus markedly influence the overall findings.
The threshold for likely substantial health benefits in our review was identified as being between 120 to 180 minutes of mostly aerobic physical activity. Approximately, this equates to a daily amount that typically would not need to exceed an average of 30 minutes per day, and is therefore at least 50% fewer minutes of daily activity than the UK CMOs’ current guideline of an average amount of at least 60 minutes per day across the week for non-disabled children and young people.
Evidence from both physiological and observational studies (Bingham, DD; Unnithan, VB) could provide an explanation for this observation. Mechanistic physiological studies consistently show greater energy costs, typically 40 to 80% for different physical activities and exercises for disabled children and disabled young people compared to non-disabled control groups. This greater energy cost would mean that everyday activities would exert a greater impact on the aerobic system, due to increased workload. Alongside this, various disabled children and disabled young people, especially those with certain physical impairments, have different physiological functional abilities which would also contribute to greater work capacity needed for typical physical activities, like ‘low walking economy’. These 2 issues may also be reflected in observational studies on the physical activity levels of disabled children and disabled young people. For example, one study observed 50% lower levels of daily physical activity compared to non-disabled groups, using device-derived indices of physical activity.
It is important to note that studies in this review have typically assessed a dose of physical activity or exercise, performed by volunteers, on health outcomes. These studies are laboratory-based rather than naturalistic. They show some dose-response relationships between physical activity and exercise on outcomes. These are efficacy studies, and represent ‘effects upon outcomes’, rather than choice-based changes by increasing leisure-time physical activity on outcomes. One recent study has examined this relationship and reported that overall physical activity was not significantly related to V̇O2 peak, suggesting that maximal aerobic power in itself does not have an independent role in an individual’s overall physical activity. The potential to be more active may not be limited by V̇O2 but rather other behavioural, social or environmental determinants. However, as V̇O2 is much reduced, training effects of being active would be achieved by shorter total volumes of physical activity. It is known that disabled children and disabled young people are at increased risk of being typically inactive and sedentary. This observation may reflect the recruitment of participants who were:
- initially unable to participate in increased amounts of physical activity
- able to realise the benefits of physical activity sooner and from less intense activities
There is also the potential for methodological differences in how previous guideline reviews were conducted, which may have contributed to the observed findings here. For example, the evidence-base that underpinned the WHO guidelines consisted almost entirely of studies that did not include disabled people. Furthermore, the current review only included primary research studies. Within such studies, there remains a lack of standardised research protocols for physical activity for disabled children and disabled young people, and it is possible that studies may have based their programmes on research from disabled adult cohorts.
While there is little evidence to determine the mostly likely reason behind the observed differences and therefore in physical activity recommendations for disabled children and disabled young people, this highlights the importance of including only disabled children and disabled young people, as we have done here. We are confident that based on the evidence carefully reviewed the recommendation of 120 to 180 minutes of physical activity, is effective and supported by a small set of physiological and behavioural studies, with the caveat that more research is needed. If deemed a better and more effective message among infographic co-producers (i.e. disabled children and disabled young people), this recommendation may, for example, be translated to an average 20 minutes per day threshold, or alternatively 40 minutes 3 times per week.
Important considerations: physical activity intensity
The conclusions of this review were impacted by a lack of detailed reporting on physical activity intensity. Intensity was reported in just 76 of 167 included quantitative studies. This may be due to the lack of practical, valid and reliable measures of intensity for cohorts of disabled children and disabled young people (Corry, I; Kārkliņa, B)
Nevertheless, it may be likely that disabled children and disabled young people who attempt to meet the recommended level and intensity of physical activity for cardiorespiratory fitness and muscular outcomes will also see improvements in outcomes for which there is insufficient FITT-related evidence. Here again safe progression toward such activity levels must be considered, particularly in relation to developmental readiness for increased demands, and for those with lower starting functional-levels and movement economies. Furthermore, it is especially important for those disabled children and disabled young people who are typically inactive and/or sedentary.
Although the safest methods of progressing physical activity have not been established for disabled children and disabled young people, research from other populations offers important insight. For typically inactive individuals, adding an additional 5 to 10 minutes of light-to-moderate activity (for example, walking or wheeling) 2 to 3 times per week, has a low risk of musculoskeletal injury and no known risk of adverse cardiac events. As recommended elsewhere (Smith, B (PDF, 94KB); USDHHS), frequency and duration should be increased before raising activity intensity. This message is particularly important for typically inactive disabled children and disabled young people who have pre-existing health conditions, use medication, or are susceptible to secondary health conditions. It reinforces the message that some physical activity is better than nothing, especially for those who are inactive or starting to get active.
When determining and increasing intensity, care is required. Evidence from disabled adult subpopulations suggests that objective measures of intensity like metabolic equivalents (METs), or measures of relative intensity such as rate of perceived exertion (RPE) or talk tests, are inaccurate. However, RPE in particular is popular among healthcare professionals and researchers and this method, along with METs, should not be avoided if they offer the most effective or trusted means for ensuring activity is not too intense for the participating group (PDF, 94KB). It is possible that a range of methods including talk tests, RPE and objective measures (for example, device-based) may be used in combination to better contextualise intensity in disabled children and disabled young people’s physical activity. We feel it is vital to develop an intensity scale that has utility, but is also relative for each disabled child or young person.
Type of physical activity
Examples of physical activity types included in the reviewed studies were adapted sports (cycling, gymnastics, ice skating, tap dancing), aerobic exercises (walking, running, cycling), aquatic exercise, balance training, cycle ergometry, dancing, functional power and strength training, gross motor skill exercises, high-intensity circuit training, indoor wall climbing, locomotor training, martial arts, modified sports (basketball, cricket, netball, soccer, tee-ball), progressive resistance training, rope jumping, proprioceptive activities, surfing, Special Olympics, VR/exergaming, wheelchair sports, and yoga.
These studies demonstrated that various physical activity types may likely improve health benefits across different outcome categories. Therefore, it is important for disabled children and disabled young people to choose types of activities that meet their needs and interests. Table 7 presents examples of the types of activities that were associated with different outcome categories in the included studies.
Table 7: examples of physical activity types by outcome category for a sample of studies
| Cardiorespiratory fitness | Muscular outcomes | Functional skills | Psychosocial outcomes | Cognitive outcomes | Behavioural outcomes | |
|---|---|---|---|---|---|---|
| Adapted sports | No | Yes | Yes | Yes | No | Yes |
| Aerobic exercise | Yes | No | No | No | Yes | No |
| Balance training | No | No | No | No | No | No |
| Dance | No | No | No | No | Yes | No |
| Exergaming | Yes | No | Yes | No | No | No |
| Functional power and strength training | No | Yes | No | No | No | No |
| Gross motor skills training | No | No | No | No | Yes | No |
| High-intensity circuit training | No | Yes | No | No | Yes | No |
| Indoor climbing | No | No | No | Yes | No | No |
| Martial arts | Yes | No | Yes | No | Yes | No |
| Resistance exercise | No | Yes | Yes | No | No | No |
| Special Olympics | No | No | No | No | No | Yes |
| Surfing | Yes | Yes | Yes | Yes | No | No |
| Wheelchair sports | No | Yes | No | Yes | No | No |
| Yoga | No | No | No | No | Yes | No |
Promoting physical activity among disabled children and disabled young people
Crucially, evidence from qualitative research identifies some notable facilitators and barriers that could affect disabled children and disabled young people’s physical activity participation.
Facilitators determined by provisions of choice, equipment and environment suggest an increase in physical activity behaviours. This includes access to programmes and services that:
- have a variety of activities with the choice to opt-out
- are graded for inclusion
- are without time pressures
- provide predictability and opportunities to establish routines
- enable access to nature and the outdoors
In addition, adaptive equipment and assisted devices that are well matched for disabled children and disabled young people may lead to increased physical activity behaviours.
Evidence also suggests the social environment to be another key facilitator of being physically active, including the availability of social support. Encouragement from, and competence of, others who are not parents, namely specialised health professionals, coaches, physiotherapists, and teachers, is likely to encourage participation. Disabled coaches also act as role models for disabled children and disabled young people. Furthermore, the opportunity to experience valued social roles, social modelling and making friends are key factors in increasing physical activity behaviour.
Moreover, having fun and experiencing expert autonomy through physical activity participation can lead to self-concept enhancement. Activities that make individuals feel good are likely to be more effective in getting inactive people active and creating long-term physical activity engagement. Such affective dimensions have commonly been overlooked, but there is strong quantitative and qualitative evidence that highlights the importance of fun and pleasure for initiating and maintaining physical activity (Decker, ES; Ekkekais, P; Phoenix, C; Williams, TL; Zenko, Z). Recent research also suggests that emphasising acute positive aspects of participation (PDF, 1.3MB) like these should be a priority for physical activity messaging efforts.
Conversely, lack of provision of choice, equipment and environment may also pose barriers to physical activity participation if not appropriately considered. The evidence suggests the availability of equipment and the time required to set it up, long travel times to activities, inadequate support in schools, the competing demands across families, and the lack of participation partners are all examples of environmental barriers to disabled children and disabled young people’s physical activity engagement.
Lack of support from others also poses further limitations to participation, with evidence of disabled children and disabled young people being dependent on others, and some deliverers having a lack of condition-specific knowledge to appropriately support participants. There is also evidence of further self-concept and interpersonal barriers to participation, including a feeling that something is wrong with their body, fatigue, pain or injury resulting from participation, and a lack of perceived confidence from others. Evidence from qualitative studies identify disabled children and disabled young people perceive their non-disabled peers to have an advantage in physical activity contexts due to rates of development, an unfairness in competitive situations, and examples of being bullied while being physically active.
Numerous physical activity programmes reviewed in this report included behavioural components, and instances of these were collated during data extraction. However, it is important to note that it was the effectiveness of physical activity on health outcomes, and not the effectiveness of the behavioural components, that was being examined. Common features of effective programmes constitute 4 categories:
- instruction on how to perform particular tasks and physical activities
- monitoring and feedback (for example, praise and encouragement, training diaries and parent logbooks)
- motivators (for example, stickers, pizza parties, reward charts) and
- goal-setting
Conclusions
Based on the available evidence, our conclusions are as follows.
It is important for disabled children and disabled young people to do challenging but manageable strength and balance-focused activities on average 3 times per week. This conclusion is in agreement with WHO guidelines.
It is also important for disabled children and disabled young people to engage in 120 to 180 minutes of mostly aerobic physical activity each week, at a moderate-to-vigorous intensity. This conclusion differs from the WHO guidelines for disabled children and disabled young people and some of the existing UK guidelines for non-disabled children and young people, but is aligned with the UK guidelines for disabled adults.
The quality of physical activity participation is important to begin and maintain an active lifestyle. It is also important that physical activity participation be progressive, fostering a disabled child or disabled young person’s opportunities for personal development. Examples of this include increasing load in resistance exercises, increasing the speed of or total ambulation distance, or increasing social contacts. Underpinning this development should be an emphasis on affective benefits of participation and the involvement and support of credible others (for example, care workers or teachers). This should be accompanied by messaging such as ‘physical activity is cool and fun’ or ‘move in a way that feels good’.
While the consequences of messaging in relation to sedentary behaviour have necessarily been noted above, it was beyond the scope of the current review to produce specific sedentary behaviour guidelines. The reader is directed to the most recent evidence in this regard, pertaining to disabled children and disabled young people, which indicates that they ‘should limit the amount of time being sedentary, particularly the amount of recreational screen time’.
In the future, it is also concluded that it may be beneficial to emphasise the dose-response relationship of physical activity and benefits to health. It is suggested that the health benefits of engaging in less than 120 to 180 minutes of mostly aerobic physical activity is communicated in guidelines and messages. This is particularly important for disabled children and disabled young people who are at an increased risk of being typically inactive. This recommendation is based on the evidence reviewed, which suggests there may be, for example, some health benefits of engaging in physical activity for 45 to 60 minutes per week. This emphasis on the dose-response relationship, including the acceptability and effectiveness of associated messaging, has previously been noted by disabled people and health care professionals as part of the guidelines review process for physical activity and disabled adults (PDF, 94KB). If applied appropriately for disabled children and disabled young people, this approach may lead to greater public health benefit. An example is provided in Figure 3.
Figure 3. An example multi-faceted dose-response curve of physical activity
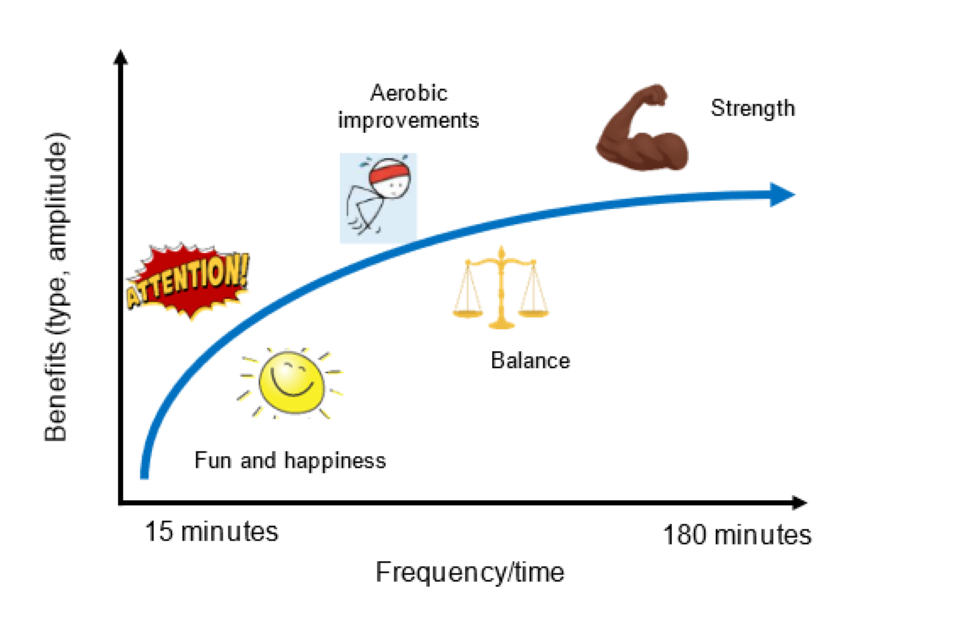
This diagram denotes likely dose-outcome responses for some of the outcomes in the available data. Individuals may accrue comparable benefits from higher or lower doses than depicted.
Question 3: Is there any evidence that physical activity is unsafe for disabled children and disabled young people?
No evidence was found that suggests physical activity presents an adverse risk to disabled children and disabled young people, if appropriately supervised and tailored in terms of FITT to the needs of groups or individuals.
In total, 33 of 176 included studies reported on safety and adverse effects from physical activity interventions. Of these, 13 studies recorded no adverse events. No data was found relating to sensory impairments.
While only a small number of studies reported data applicable to this research question, these indicated that it is unlikely that there is any good evidence to suggest that appropriate physical activity is unsafe for disabled children and disabled young people.
Nevertheless, physical activity is not without risk in all subpopulations, and it is important to note that certain impairment groups may be susceptible to some risks more than others (for example, visual impairment and falls). Where adverse effects were reported, 15 studies related to physical disabilities, 3 to intellectual and learning disabilities and 2 to mixed disabilities. However, there were no reported instances of children withdrawing from physical activity as a result of said events.
Fourteen of the 15 identified physical disability-related studies were about children with cerebral palsy. While one of these identified a possible increase in spasticity and another reported 2 instances of trips, the most commonly reported complaints among children with physical disabilities were of general discomfort or fatigue, which may in most cases be associated with expected adaptations to training among inactive populations, but additional or heightened symptoms among children with cerebral palsy in particular cannot be discounted. Where reported, injuries were minor (for example, blisters or bruising). Adverse effects of pain, fatigue and trips were reported in children with cerebral palsy from high-intensity walking, power training, shuttle running and plyometric training, with most discomfort reported in intervention intensities above 80% of participants’ baseline measures. One moderate study reported the effects of acute exercise are of greater concern in children with cerebral palsy as a result of muscle fatigue.
In children with intellectual and learning disabilities, 3 studies reported issues relating to overstimulation, uncomfortable blood lactate build-up and an inability to learn independent (and therefore safe) physical activity skills, respectively. These adverse effects related to high-intensity shuttle running and active games. While evidence of further adverse effects including pain, fatigue and tiredness were reported, no evidence of serious injury was reported within these studies.
Of the 2 studies that included mixed disabilities, falls and a single minor injury were reported in an adaptive ice-skating programme. A second study about wheelchair basketball identified tiredness, aches and pains, which may have also led to frustration among participants due to the subsequent dependence on adults thereafter (for example, needing additional help from parents or carers).
Across all impairment groups (excluding sensory), the potential risks identified in this review, especially for those disabled children and disabled young people who are inactive, may be categorised as follows:
- pain and fatigue experienced during physical activity
- trips and falls
- adverse response to adapted protocols or equipment
- challenging behaviours that present during physical activity
Those who have concerns about these potential risks may wish to seek advice from trained professionals (for example, physical activity specialists or healthcare professionals). It is recommended that physical activities are:
- completed in safe and suitable environments
- supported by appropriate supervision
- tailored and progressed in terms of FITT to individual or group needs (see question 2 above)
- monitored carefully for signs of adverse effects
These mitigation strategies are particularly important considerations for those typically inactive disabled children and disabled young people. The potential risks, examples and preventative measures identified in the evidence review are illustrated in Table 8. Users of these guidelines should consider this information alongside their lived or professional experiences of disability among children and young people. However, it must be reiterated that the available evidence indicates that appropriately performed physical activity presents minimal risk to disabled children and disabled young people. They can be confident in initiating physical activity safely.
Table 8: The main safety concerns identified in included articles, examples and suggested prevention measures
| Safety concern | Example | Prevention measure |
|---|---|---|
| Pain and fatigue experienced during physical activity | Muscle pain (for example, delayed onset muscle soreness (DOMS)) or feeling tired after activity sessions | Monitoring of training dose frequency to allow for rest and recovery is advised |
| Trips and falls | Trips during organised sports and games; falls during adapted skating | Risk assessment, protective equipment and monitoring of disabled persons during activities |
| Adverse response to adapted protocol or equipment | Falls using skating equipment, blister development, pain from cycling posture | Monitoring of disabled persons during physical activity is advised |
| Challenging behaviours that present during physical activity | Drinking water from swimming pool, hyperstimulation from physical activity | Support disabled persons by providing suitable environment for participation |
Conclusions
Based on the available evidence, the risks associated with taking part in physical activity are low and continuing with an inactive or sedentary lifestyle presents greater health risks than gradually increasing physical activity levels. Engaging in physical activity that is appropriate to an individual’s current levels of physical development, fitness, physical and mental functioning (accounting for disability classification and severity), health and physical activity is considered safe and beneficial for disabled children and disabled young people without contraindications. These recommendations align with previous physical activity guidance, including that provided by the UK CMOs for non-disabled children and young people, and disabled adults.(DHSC 2019; WHO 2020; Smith, B (PDF, 1.6MB); USDHHS)
Research gaps
Historically, research about physical activity and disabled children and disabled young people has been not been prioritised in terms of research focus or funding. There are also well documented issues around researchers failing to include certain groups of people in research trials, especially from smaller subpopulations such as those included in this review.
Nevertheless, research about physical activity and disabled children and disabled young people is slowly accumulating. Yet important gaps in knowledge remain. Based on identified gaps in research and priorities identified by disabled people, 9 areas are highlighted where there are gaps, or where more research would help in drawing conclusions.
The identified gaps were in:
-
evidence about physical activity and health outcomes for children and young people with mental impairments and children and young people with long-term health conditions (for example, congenital heart disease or cystic fibrosis) that manifest as disabilities
-
evidence about the impact of physical activity on disease and risk prevention, and psychological health outcomes for disabled children and disabled young people, as well as those outcomes in impairment groups that have been identified as having positive trends but without sufficient information to make clear recommendations
-
evidence about different subpopulations of disabled children and disabled young people, in particular among girls and young women. This should be accompanied by a greater understanding of the influence of health inequalities on physical activity participation in these populations
-
evidence around the association between sedentary behaviour (that is, low energy-expending waking behaviour while seated or lying down) and multiple health outcomes in disabled children and disabled young people
-
evidence on how to translate, communicate and implement these guidelines, focusing on delivery preferences for different impairment groups. Building on the evidence compiled by the UK CMOs’ Expert Committee for Communication of Physical Activity Guidelines, this work will is in part fulfilled by development of the infographic
The recommendations around further research were to:
-
develop new, or adapt existing, measures of physical activity intensity for use with disabled children and disabled young people, that are effective and easy to use. A focus should be put on self-rating scales of physical activity, as well as improving metrices of validity and reliability
-
produce more high-quality and practically useful research. This should include the quantification of effectiveness in user-friendly terms and clinical significance
-
conduct evidence reviews of physical activity for the treatment and rehabilitation of specific impairments in clinical and/or care settings.
-
develop theoretically based and co-produced programmes to enhance disabled children and disabled young people’s quality and quantity of physical activity participation over the life course
Despite the expansion of evidence, and evidenced benefits of physical activity for health, more work is needed on physical activity, disability and health if we are to realise the potential of being active, more often for people with different impairments across the UK. Too often this is hampered by silo work. What is thus important is the need for public health bodies, university researchers, funding communities, disability communities, and relevant sport and disability organisations to all work closely together. This would avoid duplication of work, ensure best practice is shared, and enable the production of high quality, impactful research.
Disabled people are often oppressed and discriminated against. Individual behaviours, including physical activity behaviours, are determined not solely by individual choice but by disablism, ableism, health inequalities, and other social, cultural, economic, and environmental factors that restrict significantly what disabled people could do, can do, and may become. These factors also need to be foregrounded much more in research and implementation of evidence so that change can happen. They can provide the necessary foundation for public health agencies, health and social care professionals, schools, disability groups, and sport and physical activity organisations to encourage physical activity to, with, and for disabled people. Disabled children and disabled young people, as well as their parents and guardians, need to play an active role in all of this.
These are critical research needs and commitment is needed to advocate and prioritise these with UK research councils.
Summary and next steps
This rapid review provided a detailed overview of the existing evidence-base on health benefits from physical activity for disabled children and disabled young people (aged 2 to 17 years). There is evidence to suggest a likely positive relationship between physical activity and broad health outcomes.
Based on the available evidence, and aligned with the 2019 UK CMOs’ physical activity guidelines, it is recommended that for disabled children and disabled young people, some physical activity compared to none is good, but more is better.
For likely substantial health benefits, disabled children and disabled young people should engage in 120 to 180 minutes of mostly aerobic physical activity per week, at a moderate-to-vigorous intensity. This is to be accompanied by challenging but manageable strength and balance-focused activities on average 3 times per week.
These specific recommendations are aligned with some aspects of the 2019 UK physical activity guidelines for disabled adults and non-disabled children and young people as well as the 2020 WHO physical guidelines for children and adolescents living with disability. However, there is little available evidence from research that includes only disabled children and disabled young people to support the WHO guidelines that this population should do at least an average of 60 minutes per day of moderate-to-vigorous intensity, mostly aerobic, physical activity, across the week. The available evidence from that research suggests that disabled children and disabled young people engage in 120 to 180 minutes of mostly aerobic physical activity per week, at a moderate-to-vigorous intensity. With new evidence this recommendation may or may not change in the future.
With respect to safety, no evidence exists that suggests appropriate physical activity presents a risk to disabled children and disabled young people. Conscious effort to dispel false narratives about physical activity being inherently harmful for this group should be urgently addressed. Cautious progression of activities is advised to avoid adverse events, given disabled children and disabled young people are at heightened risk of typical inactivity, and can accrue benefits from lower doses of physical activity.
It would seem, therefore, that for disabled children and disabled young people there are analogous health benefits of engaging in physical activity as for the rest of the child population.
Irrespective of the nuances of different national or international guidelines, there is an unequivocal need to address the complexities of physical activity, reduce inequities, and uphold the human rights of disabled children and disabled young people, including full access to high-quality physical activity and sports (Arbour-Nicitopoulos, KP). This report and associated work contribute to this aim.
The main strengths of this report are that it is has focused on physical activity in a population not represented in previous UK guidelines, that is, disabled children and disabled young people. To our knowledge, these guidelines are the first to have included a review of evidence solely focused on disabled children and disabled young people’s physical activity, and thus represent the most comprehensive guidance globally. The guidelines were also developed with disabled children and associated stakeholders and organisations, which represents another first.
The review is also timely in that it complements the recent UK CMOs’ updated guidelines for disabled adults and non-disabled children and young people, published in 2019, as well as advancing findings from other recent public health guidance reviews.
Lastly, this review has enhanced the rapid synthesis methodology developed for the 2019 UK disabled adults’ physical activity review and thus provides an in depth framework for future reviews and evidence updates. This can support the planned interim review of the UK CMOs’ physical activity guidelines in 2024.
The development of a co-produced evidence-based infographic with disabled children and disabled young people will help to distil and communicate these guidelines appropriately for this target population. Co-produced infographics have been identified as a key strategy in creating more inclusive physical activity messages. The purpose of the infographic is to capture health benefits, dose-response physical activity relationships, fun and other relevant messages co-producers identify as meaningful and useful. In addition to disabled children and disabled young people, the infographic will also likely be useful to other audiences who, for example, may wish to use it to learn more about physical activity for disabled children and disabled young people. It will also be a resource for those wishing to communicate messages about physical activity, such as parents and carers, sport organisations, and education, health and social care professionals. It will support their conversations and help guide behaviour change, for example.
Other information
Support
This project was funded by the UK Department of Health and Social Care. Additional financial support for project delivery was provided by the Economic and Social Research Council (ESRC) Impact Acceleration Account (Durham University). Non-financial support was provided by Durham University Library, the Expert Group, and learned colleagues.
Competing interests
Lydia Bone works for Disability Rights UK.
Availability of data
All studies included in this review are published and available in the public domain.
