Making IT work: harnessing the power of health information technology to improve care in England
Published 7 September 2016
Executive summary
In order for the National Health Service (NHS) to continue to provide a high level of healthcare at an affordable cost, it simply must modernise and transform. This transformation will involve enormous changes in culture, structure, governance, workforce, and training.
But none of the changes are likely to be as sweeping, as important, or as challenging as creating a fully digitised NHS.
Impressively, the English GP sector began digitising in the 1980s, and by the mid-2000’s was nearly 100% digital. By contrast, an ambitious programme to digitise secondary care – the National Programme for Information Technology (NPfIT), launched in 2002 – was shut down in 2011 after having mostly failed to achieve its goals. Analyses of NPfIT criticised the programme for being too centralised, for not engaging with trusts and their healthcare professionals, and for trying to accomplish too much too quickly. A consensus has since emerged that the time has come to move forward, and, in 2016, the Treasury allocated £4.2 billion to support the digitisation of the NHS.
In late 2015, the National Advisory Group on Health Information Technology in England was formed to advise the Department of Health and NHS England on its efforts to digitise the secondary care system. Our recommendations fall into 2 broad categories: 10 overall findings and principles, followed by 10 implementation recommendations.
Overall findings and principles
1. Digitise for the correct reasons
The goal of digitisation of health systems is to promote what has become widely known as healthcare’s Triple Aim: better health, better healthcare, and lower cost. These aims are consistent with those of the NHS’s 2014 Five Year Forward View, which called for improvements in quality and service, as well as £22 billion in efficiencies. The Advisory Group believes that trying to achieve the aims of the Five Year Forward View without giving highest priority to digitisation would be a costly and painful mistake.
2. It is better to get digitisation right than to do it quickly
While there is urgency to digitise the NHS, there is also risk in going too quickly. The Advisory Group urges the NHS to digitise the secondary care sector in a staged fashion, in which trusts that are ready to digitise are prompted to do so, while those that are not ready should be encouraged and supported to build capacity, a process that will take several years.
3. ‘Return on investment’ from digitisation is not just financial
While it is natural to seek a short-term financial return on investment (ROI) from health IT, experience has shown that the short-term ROI is more likely to come in the form of improvements in safety and quality than in raw financial terms. In fact, cost savings may take 10 years or more to emerge (the so-called ‘productivity paradox’ of IT), since the keys to these gains are improvements in the technology, reconfiguration of the workforce, local adaptation to digital technologies, and a reimagining of the work.
4. When it comes to centralisation, the NHS should learn, but not over-learn, the lessons of NPfIT
While it is true that NPfIT erred partly through overcentralisation, it is also important to note that centralisation sometimes makes sense, particularly in the context of a national health system. A new digital strategy should seek an appropriate balance between local/regional control and engagement versus centralisation.
5. Interoperability should be built in from the start
Local and regional efforts to promote interoperability and data sharing, which are beginning to bear fruit, should be built upon. National standards for interoperability should be developed and enforced, with an expectation of widespread interoperability of core data elements by 2020. In addition, the Advisory Group endorses giving patients full access to their electronic data, including clinician notes.
6. While privacy is very important, so too is data sharing
Privacy is very important, but it is easy for privacy and confidentiality concerns to hinder data sharing that is desirable for patient care and research. It would be a mistake to lock down everyone’s healthcare data in the name of privacy. We endorse the recommendations of the National Data Guardian’s Review of Data Security, Consent, and Opt-Outs, which was commissioned to achieve this balance.
7. Health IT Systems must embrace user-centered design
IT systems must be designed with the input of end-users, employing basic principles of user-centered design. Poorly designed and implemented systems can create opportunities for errors, and can result in frustrated healthcare professionals and patients.
8. Going live with a health IT system is the beginning, not the end
The ‘go live’ period in a large hospital or trust is always difficult, but is nonetheless just the start. Health IT systems need to evolve and mature, and the workforce and leadership must be appropriate for this task. While patient safety is non-negotiable, regulators and commissioners need to have a degree of tolerance for short-term slow downs and unanticipated consequences in the period following electronic health record (EHR) implementation.
9. A successful digital strategy must be multifaceted, and requires workforce development
The NHS’s digital strategy should involve a thoughtful blend of funding and resources to help defray the costs of IT purchases and implementation, resources for infrastructure, support for leadership and informatics training, as well as support for education of leaders, front-line providers, trainees and clinician- and non-clinician informaticians. The Advisory Group was struck by the small number of leaders at most trusts who are trained in both clinical care and informatics, and their limited budgetary authority and organisational clout. This deficit, along with a general lack of workforce capacity amongst both clinician and non-clinician informatics professionals, needs to be remedied.
10. Health IT entails both technical and adaptive change
Many observers and stakeholders mistakenly believed that implementing health IT would be a simple matter of technical change – a straightforward process of following a recipe or a checklist. In fact, implementing health IT is one of the most complex adaptive changes in the history of healthcare, and perhaps of any industry. Adaptive change involves substantial and long-lasting engagement between the leaders implementing the changes and the individuals on the front lines who are tasked with making them work. Successful implementation of health IT across the NHS will require the sustained engagement of front-line users of the technology.
Recommendations
1. Carry out a thoughtful long-term national engagement strategy
The Advisory Group believes that a long-term engagement strategy is needed to promote the case for healthcare IT, identify the likely challenges during implementation, educate stakeholders about the opportunities afforded by a digital NHS, and set the stage for long-term engagement of end users and co-creation of systems and strategies. The campaign needs to emphasise that the goal is not digitisation for digitisation’s sake, but rather to improve the way care is delivered in the NHS, in part by using digital tools.
2. Appoint and give appropriate authority to a national chief clinical information officer
A national chief clinical information officer (CCIO), with a background in clinical care, informatics, and leadership, should be appointed to oversee and coordinate NHS clinical digitisation efforts. This individual and his or her team must be given appropriate organisational and budgetary authority. Because health IT crosses the domains and budgets of so many NHS organisations, this individual and team will assume a crucial coordinating function.
3. Develop a workforce of trained clinician-informaticists at the trusts, and give them appropriate resources and authority
There must be a major effort to place well-qualified clinicians with advanced informatics training in every trust. The Advisory Group estimates that an average-sized trust needs at least 5 such individuals on staff. Their leader, the CCIO, should be a well trained and credentialed clinician-informatician, and should report directly to the board or CEO. In considering whether to offer government money to subsidise digital implementation in a trust, close attention should be paid to the adequacy of the trust’s plan to hire and support this clinical-IT workforce.
4. Strengthen and grow the CCIO field, others trained in clinical care and informatics, and health IT professionals more generally
The dearth of professional, well-supported CCIOs with appropriate authority and resources is an enormous obstacle to successful deployment and benefits realisation of health IT at the trust level. To rectify this gap, not only will there need to be satisfying, sustainable positions available to CCIOs in trusts, but the CCIO field itself must also be strengthened and grown. This will involve a major effort by existing professional bodies to create and certify training programmes for clinician-informaticians. It will also require support for the development of vibrant professional societies. Moreover, the workforce of clinician and non-clinician informaticians, informatics researchers, programme evaluators, and system optimisers needs to be increased and nurtured. We favour a significant allocation of central resources – £42 million, or 1% of the £4.2 billion allocated for digitisation – to support this crucial workforce development.
5. Allocate the new national funding to help trusts go digital and achieve maximum benefit from digitisation
The £4.2 billion the Treasury made available in 2016 to promote digitisation, while welcome, is not enough to enable digital implementation and optimisation at all NHS trusts. Therefore, we suggest a phased approach. During phase 1 (2016 to 2019), national funding should be combined with local resources to support implementation in trusts that are prepared to digitise, and to support those that are already digitised and ready to reach even higher levels of digital maturity. Another tranche of government funding (not yet allocated) will likely be needed to support a second stage (phase 2, 2020 to 2023) of the strategy, as described under recommendation 6: While some trusts may need time to prepare to go digital, all trusts should be largely digitised by 2023.
6. While some trusts may need time to prepare to go digital, all trusts should be largely digitised by 2023
It would be reasonable to expect all trusts to have achieved a high degree of digital maturity by 2023. After that year, we recommend that no more government subsidies be made available, and that regulators should begin to deem trusts that have not reached a high level of digital maturity to be out of compliance on quality and safety grounds.
7. Link national funding to a viable local implementation/improvement plan
The availability of central money to support digitisation should be linked to a parallel investment from each trust (based in part on ability to pay), NHS approval of a plan that demonstrates that the trust is adequately prepared to succeed in both digitisation and in promoting regional interoperability, evaluation of progress, and ongoing accountability that the money was well spent.
8. Organise local/regional learning networks to support implementation and improvement
To support purchasing, implementation, and ongoing improvements by trusts, digital learning networks should be created or supported. Such networks may vary, with some helping in the early stages (choice of EHR system, contracting, implementation) and others at later stages (optimisation, decision support, analytics). The latter category may include IT supplier-specific networks.
9. Ensure interoperability as a core characteristic of the NHS digital ecosystem – to promote clinical care, innovation, and research
The new effort to digitise the NHS should guarantee widespread interoperability. The goals of interoperability are to enable seamless care delivery across traditional organisational boundaries, and to ensure that patients can access all parts of their clinical record and, over time, import information into it. Widespread interoperability will require the development and enforcement of standards, along with penalties for suppliers, trusts, GPs, and others who stand in the way of appropriate data sharing. The system, standards, and interfaces should enable a mixed ecosystem of IT system providers to flourish, with the goal of promoting innovation and avoiding having any one vendor dominate the market. Plans for interoperability should be harmonised with other ongoing efforts to join up elements of the health and social care systems, such as those represented by the sustainability and transformation plans (STPs).
10. A robust independent evaluation of the programme should be supported and acted upon
In light of the likelihood of unanticipated consequences, the high cost of digitisation, and the chequered history of past efforts to digitise the secondary care sector, the NHS should commission and help fund independent evaluations of the new IT strategy. Such evaluations should be formative (conducted and reported as the strategy is progressing) and summative (reporting at the end of each of the 2 phases of deployment). In assessing the benefits and costs of health IT, evaluations should consider the impact of digitsation on the satisfaction of healthcare professionals.
Conclusion
We believe that the NHS is poised to launch a successful national strategy to digitise the secondary care sector, and to create a digital and interoperable healthcare system. By using national incentives strategically, balancing limited centralisation with an emphasis on local and regional control, building and empowering the appropriate workforce, creating a timeline that stages implementation based on organisational readiness, and learning from past successes and failures as well as from real-time experience, this effort will create the infrastructure and culture to allow the NHS to provide high quality, safe, satisfying, accessible, and affordable healthcare.
The experience of industry after industry has demonstrated that just installing computers without altering the work and workforce does not allow the system and its people to reach this potential; in fact, technology can sometimes get in the way. Getting it right requires a new approach, one that may appear paradoxical yet is ultimately obvious: digitising effectively is not simply about the technology, it is mostly about the people.
To those who wonder whether the NHS can afford an ambitious effort to digitise in today’s environment of austerity and a myriad of ongoing challenges, we believe the answer is clear: the one thing that NHS cannot afford to do is to remain a largely non-digital system. It is time to get on with IT.
1. Introduction
The English people are proud of their National Health Service (NHS)[footnote 3] – and for good reason. The NHS cares for one million patients every 36 hours, delivers 700,000 babies annually, and handles 22 million annual visits to accident and emergency (A&E) departments. It provides every citizen with remarkably easy access to primary care, and achieves healthcare quality commensurate with, and often exceeding, that of countries that spend far more of their national wealth on healthcare (1). On certain measures, such as cancer and cardiovascular outcomes, the NHS has enjoyed substantial improvements in the past 15 to 20 years.
Yet the NHS cannot continue on its current path. Faced with growing demands from an ageing population, over the past 2 decades the NHS has attempted to improve service and efficiency through a series of reorganisations, cost-cutting manoeuvers, and changes in incentives and targets. While some of the changes have been effective, a steady drumbeat of patient safety problems, dissatisfaction amongst clinical staff, and deterioration in certain outcomes all point to a system under serious, perhaps unprecedented, stress (2, 3). (It is worth pointing out that health systems worldwide are grappling with similar challenges.) In order for the NHS to continue to provide a high level of healthcare at an affordable cost, it simply must modernise and transform.
Transformation of service provision and care delivery can take many forms, including changes in culture and workforce, as well as shifts in approaches to improvement and training. However, healthcare is mostly about information. It is about the A&E doctor having an accurate medication list when she evaluates a delirious patient, the oncologist having access to the results of a new clinical trial, and the ward nurse being alerted quickly that a patient’s changing vital signs may represent early sepsis. An information-rich healthcare system is also about ensuring that all of the relevant carers have the information they need to transfer the care of a frail patient from hospital to home care or to hospice. Moreover, the increasing importance of genomics in healthcare, patient access to new information via the Internet and social media, and our deepening understanding of the potential from big data analytics all place a growing premium on information. The NHS will simply not be able to provide high levels of service at an affordable cost without digitisation and appropriate use of digital data at every level.
The Five Year Forward View, released in 2014, outlines an ambitious set of goals for the NHS, including improvements in quality and service and £22 billion in efficiencies (4). If there were a way to achieve these goals – to provide high quality, safe, accessible, patient-centred care at an affordable cost – without digitisation, that would be fine. After all, transforming the NHS from one whose information backbone (in the secondary care sector) consists of thick paper files and fax machines to one with a modern digital infrastructure is undoubtedly going to require new investment. And it will surely be disruptive.
But, in the end, trying to achieve the aims articulated in the Five Year Forward View in a non-digital NHS will be far costlier, far more disruptive, and far riskier. Simply put, the NHS will be unable to achieve its goals without digitising effectively.
Computerisation and the NHS
Of course, computerisation is not new to the NHS and its associated primary care practices. In fact the GP sector is nearly 100% digitised, and both patients and healthcare professionals experience its benefits tens of thousands of times each day. NHS Choices, a comprehensive health information site, receives more than 40 million patient visits each month. Moreover, the UK has established some internationally renowned research programmes, such as the UK Biobank and the 100,000 Genomes Project, whose potential to improve care is tightly linked to their integration with clinical information systems, both for data collection and to support clinical decision making at the point of care.
In contrast to the successes in the GP sector, the digitisation of hospitals has been far from smooth, and the patchy computerisation of this sector stands as a considerable impediment to transforming care. The ambitious National Programme for Information Technology (NPfIT), designed to digitise hospitals and trusts, was launched in 2002, only to be shut down 9 years later (5). NPfIT did enjoy some successes, including the development of a national infrastructure to provide core services (the Spine); a single national patient identifier (the NHS number); and national electronic prescription and radiology programmes. But, against its primary goal of digitising the secondary care sector, NPfIT failed to deliver – largely because it was too centralised, failed to engage properly with trusts and their healthcare professionals, and tried to accomplish too much too quickly.
Since the demise of NPfIT, the NHS has, understandably, shied away from renewed ambitious efforts to digitise secondary care. But over the past few years, a consensus has emerged that the time has come to move forward. This consensus was articulated in a 2014 framework created by the National Information Board and bolstered by the allocation, in 2016, of £4.2 billion to support this work (6).
In late 2015, the Secretary of State for Health and the leadership of NHS England asked for the creation of a broadly representative external body: The National Advisory Group on Health Information Technology in England, to advise the Department of Health (DH) and the NHS on its efforts to digitise the secondary care system. The Group was asked to reflect on the experience not only of NPfIT but of other international efforts to digitise the health system, particularly that of the United States, and to make recommendations to help guide the DH and the NHS to the best possible outcomes. The Advisory Group’s Terms of Reference are shown in Appendix A and you can see the list of members. The Group’s process is described in section 3: The National Advisory Group’s methods.This document represents the findings and recommendations of this Advisory Group.
This report begins by covering the relevant background, particularly in 5 areas:
- General policy/practical issues that relate to health IT
- A brief history of NPfIT
- A brief history of health IT in England’s GP sector
- A brief history of the US experience with digitising its healthcare system, with some possible lessons for the NHS
- The recent consensus on digitising secondary care in England, reflected in the work of the National Information Board, the Five Year Forward View report, and the allocation of £4.2 billion to support digitisation
After exploring this background, we will outline our methods, and then describe 10 overall findings and principles drawn from our interviews, site visits, and deliberations. Finally, we list 10 implementation recommendations and their rationales.
2: Background
General issues relating to health IT in the context of our review
In 1993, Massachusetts Institute of Technology (MIT) researcher Eric Brynjolfsson coined the term ‘productivity paradox’ to describe a phenomenon witnessed in a cross-section of industries – financial services, retail, entertainment, and others – as they computerised (1). Logically, everyone predicted that computerisation would transform the industry, improving quality, reliability, and efficiency. In fact, such predictions were often what drove industry leaders to take the expensive and painful step of going digital.
In came the computers and then… nothing happened. That is, nothing except disrupted workflows, unhappy front-line staff, and a confused finance department. The experience was captured nicely in this quote from economist Robert Solow, who in 1987 (2) said,
You can see the computer age everywhere but in the productivity statistics
Sometimes, large-scale computer implementations not only failed to meet their lofty – and, in retrospect unrealistic – expectations (that is, the productivity paradox), they failed entirely. The US has seen massive failures following efforts to digitise the Federal Bureau of Investigation (FBI), the Air Traffic Control system, the Internal Revenue Service, and, most famously, the Healthcare.gov website established to implement the Affordable Care Act. In the UK, similar problems bedeviled a BBC digital video archiving project and a government effort to create a universal credit system.
While each of these failures – the outright disasters as well as subtler but equally vexing examples of the productivity paradox – has its own particulars, all share certain overarching characteristics:
- failure to appreciate the complexity of large-scale computerisation
- failure to gain the buy-in of end users of the new systems
- failure to achieve ongoing engagement of end users of the new systems
- failure to change the skill mix of the end users of the new systems, or to enlist new individuals with the appropriate skills to manage the change
- failure to appreciate that digitisation completely changes the work – the nature of the work, the tasks to be done, and who does them
- underbudgeting – either in toto, or by budgeting adequately for the purchase/building of the system but failing to account for the need for implementation, ongoing training, and modifications/innovations
- failure to stage the implementation and/or going more quickly than conditions allow
While several themes emerge from this list of contributing factors, a key one relates to the notion of ‘adaptive’ versus ‘technical’ change, a duality popularised by Harvard professor Ronald Heifetz (3). Technical changes are straightforward: follow a series of steps and things go well. Following a recipe is a technical change; so is downloading and then using most apps for your smartphone. Technical change is when you already know the answer to the problem – and know how to get there.
Heifetz contrasts technical changes with adaptive changes, which require that people themselves change. Adaptive changes are those in which managers don’t already know the answers, and therefore require changes in the behavior of front-line workers and their active engagement with the problem (Table 1: Technical versus adaptive problems (4)). They often require changes in the system as well. One of the challenges of computerisation is that it seems – on the surface – to be technical change: after all, it is a technology that promises to simplify and streamline the work and the workflow.
Table 1: Technical versus adaptive problems
| What’s the Work? | Who Does the Work? | |
|---|---|---|
| Technical Problems | Apply current know-how | The ‘authorities’ |
| Adaptive Change | Learn new ways | The people with the problem |
But digitising large, complex organisations – particularly those, like healthcare, that do not involve repetitive, assembly line-type work but rather work with substantial complexity, nuance, and decision making under uncertainty – is adaptive change of the highest order.
Failure to appreciate this leads to many of the other problems: underestimation of the cost, complexity, and time needed for implementation; failure to ensure the engagement and involvement of front-line workers; and inadequate skill mix. It is thus not surprising that many health IT implementations fail, not only in England but around the world.
Since efforts to computerise a single organisation (a hospital, for instance) often fail, it is unsurprising that NPfIT – an attempt to digitise an entire sector of a massive healthcare system, operating in a resource-constrained and politicised environment – proved far more difficult than anticipated. As we try again to digitise the secondary care sector of the NHS, the question is how to learn from the lessons of NPfIT, as well as those of other countries that have traversed this path, particularly the US. Finally, there is a success story to point to: the digitisation of England’s GP sector.
In the sections that follow, we will briefly review these 3 stories: NPfIT, health IT in the GP sector, and the US experience with digitisation. Before we do, however, it is worth ending this section on an optimistic note. Research from other industries demonstrates that the productivity paradox ultimately resolves, usually after about a decade (5). Like the opening of a safety deposit box, there seem to be 2 keys.
The first: the technology needs to get better, and it eventually does. New companies emerge to solve specific problems, user feedback is integrated into product design, and the underlying technologies mature. We start with Version 1.0 and end with Version 37.6, and each version gets progressively better.
The second key is more interesting, more challenging, and ultimately more important: people begin to reinvent the work. They ask,
Why are we doing this thing this way?
And they become progressively dissatisfied with the answer:
Oh, we did it this way when we used paper, and then we just digitised it.
Over time – particularly if they have the right resources, skills, and culture – they begin to develop new ways of achieving the goals, ways that take full advantage of digital tools and thinking. That is when the major improvements in quality, safety, customer engagement, and efficiency begin to emerge. That is when the productivity paradox resolves, when the technology leads to the creation of real value.
The question, really, is how best to promote the digitisation of the NHS in a way that learns past lessons correctly; appreciates that health IT is both technical and adaptive change; and minimises the time required to resolve the productivity paradox without falling into the trap of destructive impatience. Our recommendations are framed around addressing this question, and we are optimistic that – with the right choices – it can be done successfully.
The National Programme for Information Technology
The National Programme for Information Technology (NPfIT) was an ambitious £12.4 billion investment designed to reform how the NHS in England used information to improve service and patient care. The Programme was launched in 2002 under Prime Minister Tony Blair’s leadership. Its aim was to move England’s NHS toward a single, centrally-mandated electronic care record for patients, to connect 30,000 general practitioners to 300 hospitals, and to provide secure and audited access to these records by authorised health professionals.
NHS Connecting for Health (NHS CfH), the Department of Health’s (DH) arm’s length delivery vehicle for implementing and managing the central components of NPfIT, was formed in 2005. After a turbulent history, NHS CfH ceased to exist in 2013.
An impressive literature has been produced regarding the history of and lessons learnt from NPfIT (6, 7, 8). We summarise the key points below.
Background of NPfIT
The decision to pursue a new, more centralised health IT strategy was taken at a Downing Street seminar in February 2002 (9). The seminar itself was the result of a meeting between the Prime Minister and then CEO of Microsoft, Bill Gates, after which the Prime Minister is said to have become ‘hooked’ on the technological possibilities for improvement in the NHS. The goal of NPfIT was to use modern information technologies to enhance the way the NHS delivered services, improving the quality of patient care in the process.
NPfIT was not a single project but a programme of initiatives with interdependencies, different timescales, and varied contributions to benefits delivery. Its underpinning was to be an IT infrastructure with sufficient capacity to support the national applications and local systems (10). These national applications were:
- an integrated electronic health records system
- an electronic prescription system
- an electronic appointment booking system
Central to the Programme was the creation of a fully integrated electronic records system designed to reduce reliance on paper files, make accurate patient records available at all times, and enable the rapid transmission of information between different parts of the NHS. The key components of NPfIT are listed in Table 2: Key components of NPfIT (10).
Table 2: Key components of NPfIT
| System | Description |
|---|---|
| National infrastructure | |
| National network for the NHS | A broadband network connecting all sites providing NHS care |
| NHSmail | A secure email, text and fax service, transferring patient data, appointment alerts and confidential information |
| NHS Spine | A group of 8 applications designed to underpin the NHS Care Records Service. Its intent was to: Support the NHS in the exchange of information across national and local systems, host demographic information for 60 million citizens and connect clinicians, patients and local service providers throughout England to a number of essential national services, including the Electronic Prescription Service, Summary Care Record, e-Referral Service and Demographics |
| National applications | |
| Choose and Book | An electronic referral and booking service (now known as e-referrals) giving patients a choice of time and place for their first outpatient appointment |
| Electronic Prescription Service | Enables prescribers, such as GPs and practice nurses, to send prescriptions electronically to a dispenser, such as a pharmacy, of the patient’s choice |
| Summary Care Record | Part of the NHS Care Records Service, containing key medical information from a patient’s record that is important in supporting urgent or unscheduled care |
| GP record transfer | Enables patient records to be transferred electronically between GP practices, replacing the existing manual transfer process |
| Local services | |
| Detailed care records systems | Part of the NHS Care Records Service, containing full details of a patient’s medical history and treatment, accessible to a patient’s GP and local community and hospital settings |
| Picture Archiving and Communications System (PACS) | Enables images such as X-rays and other medical scans to be stored electronically and viewed on screens |
NPfIT was managed by NHS CfH. The Chief Executive of the NHS was the senior responsible owner for the Programme, while the DH was responsible for procuring and managing NPfIT’s central contracts, including those with the Local Service Providers (LSPs).
NPfIT originally divided England into 5 areas known as ‘clusters’ (11):
- Southern
- London
- East and East Midlands
- North West and West Midlands
- North East
For each cluster, a different LSP was contracted to deliver services at a local level (Figure 1: Regional clusters for Local Service Providers (12)). This structure was intended to avoid the risk of committing to a single supplier and to create competition. The responsibility for delivery was split between the LSPs and NHS trusts, with trusts generally responsible for business change, delivery plans, staff training, and attesting that systems had met their requirements.

Map of local service providers for the 5 regional clusters in England
In 2003 to 2004, NPfIT’s Director General negotiated contracts with several large commercial IT suppliers, who served as the LSPs. Each LSP was contracted to be the sole provider of the main hardware and software products for secondary care across a large region of England (7). The LSPs invested heavily in development of new products for the NHS and were tied into contracts with NHS CfH, which included steep financial penalties for non-delivery.
By 2008, relationships between NHS CfH and the LSPs had deteriorated; technical solutions were sometimes delayed and there was anxiety in some quarters about financial risk and uncertainty of outcome (11). Whilst the LSPs potentially stood to gain financially from their NHS contracts, many observers felt that they had underestimated the technical, social, and institutional challenges of developing a workable, networked EHR system for the NHS.
Although the negotiation of LSP contracts centrally is said to have saved an estimated £4.5 billion for the NHS, it came at a heavy price in intangibles, especially the goodwill that had previously characterised the relationship between IT suppliers and the NHS.
Funding
NPfIT entailed £12.4 billion of national investment. In 2003 to 2004, the DH awarded 5 10-year contracts totaling some £5 billion to the 4 suppliers for the delivery of local care records systems (13). The aim was for detailed care records systems to be delivered to all NHS trusts and GP practices by the end of 2007, with increased functionality and integration added until full implementation was complete in 2010.
By 2011, the Programme’s expenditures totalled some £6.4 billion (7). These costs included central expenditure for managing the Programme, delivering national systems, procuring systems for local NHS organisations, and local implementation costs to support the creation of detailed care records.
Leadership
Richard Granger was appointed the Director General of NHS IT, responsible for overseeing both the procurement and implementation of NPfIT. Granger had previously managed public sector IT projects, including the London congestion charge scheme, but had little experience in health care. Granger shifted the procurement approach away from local implementation to one that emphasised national standards. While the NPfIT timeline was not realistically achievable, under Granger’s leadership the procurement process was completed with remarkable speed for an enormous, complex public sector programme.
However, problems arose quickly. For one, NPfIT saw a near-constant rotation of senior management and leadership. This led to a loss of corporate knowledge and leadership, and a diffusion of accountability and responsibility. On top of that, delivery and implementation problems became commonplace, with missed deadlines, unreliable software, and a lack of engagement with end-users, particularly health professionals (6-8).
There were success stories: the electronic prescription service (EPS) and a new national IT network (N3) were both rolled out in early 2007, ahead of schedule. The electronic radiology system (PACS) was also delivered smoothly and on time. The Choose and Book system had a mixed history: by mid-2006, while it had been deployed to more than 7,600 locations, it was underutilised, accounting for only 20% of GP referrals, hindered by local implementation problems in clinics and out-of-date patient administration systems in many hospitals.
Components of NPfIT that still remain include:
- the Spine
- N3 Network
- NHSmail
- choose and book
- secondary uses service
- electronic prescription service
- PACS
- Summary Care Record
These components represented approximately one third of the £6.4 billion total programme expenditure through 31 March 2011. The Spine is used throughout the NHS and supported 24 hours a day, 365 days a year (13). Today, the Spine:
- connects more than 28,000 healthcare IT systems in 21,000 organisations
- handles 6 billion messages every year
- has 1.1 million registered Smartcard users
- typically has 250,000 users accessing the service at any one time
- holds more than 500 million records and documents
- in peak periods, handles 1,500 messages per second
The overall failure of NPfIT
Despite these successes, the Programme’s central deliverable – the creation of functioning electronic health record (EHR) systems in all NHS trusts, connected to other key systems (particularly GP EHRs), and producing information leading to better patient care and efficiency – was not met. In 2011, NPfIT was discontinued, and analyses in the popular press were unkind, dubbing the Programme ‘a fiasco’ and worse. While there has been no definitive analysis of the failings of the Programme, consensus opinion supports the following conclusions (6, 7, 8, 9):
From the outset, the Programme lacked clinical engagement.
The focus was placed upon technology and not service change, and minimal attention was given to the adaptive elements of massive IT installations. There was no comprehensive strategy to engage clinicians[footnote 4] or NHS executives to ensure they understood the reasons that NPfIT was being developed or implemented.
System suppliers and NPfIT leadership underestimated the power of the clinical community and the complexity of the NHS.
The Programme employed a controlled, top-down approach – a centrally-driven strategy to implement standardised IT systems. Some have likened it to a military procurement program, which, of course, involves far fewer adaptive change elements and far less need for local and professional buy-in.
The Programme was felt to have a politically driven agenda. While NHS clinicians and staff were supportive of digitisation, many viewed the Programme’s deployment schedule as rushed and built around political priorities. The initial allocation of Treasury funds was based on unrealistic promises, which led to unrealistic expectations. The Programme also suffered from scope creep – the tyranny of adding on ‘just one more thing’ until a project loses focus and is crushed under the weight of additional work.
Despite what appeared to many to be a generous allocation of funds, local trusts found there was insufficient support available to help them implement the nationally purchased systems.
Procurement and contracting arrangements were problematic. NPfIT’s procurement model called for nearly impossible delivery timelines, with contracts offered on a ‘take-it-or-leave-it’ basis. While procuring contracts centrally resulted in vigorous supplier competition and saved billions of pounds, the speed meant that the NHS had not prepared key policy areas (for example, information governance), standards (for example, for messaging and clinical coding), and information system architecture. Moreover, the scope of many contracts was unclear and much work needed to be done after the contract award to agree on key parameters such as scope and deliverables.
The Programme suffered from continuous leadership changes and a shortage of individuals with relevant skills. Specifically, NPfIT was hampered by a workforce that lacked experience in large-scale IT implementation and familiarity with health services. Additionally, the frequent senior leadership turnover plagued the programme. NHS organisations, particularly the trusts, also had limited informatics experience and expertise.
In January 2009, the government’s Public Accounts Committee criticised NPfIT, noting that costs were escalating without evidence of benefits. The Committee suggested that it might be time to start looking beyond the NPfIT framework. There were few supporters of the programme at that stage and, in 2011, NPfIT was essentially aborted[footnote 5].
Conclusion and lessons
NPfIT’s problems have some important consequences today. First, any new health IT programme will need to win back the hearts and minds of skeptical stakeholder groups, including political leaders, health system leaders, front-line clinicians, and the public. Second, the health IT workforce (both clinician-informatics experts and non-clinician health technology experts), which was never very robust to begin with, has been dangerously thinned. After the demise of NPfIT, those who were enthusiastic about working in England’s health IT sector have found other things to do. Third, any new effort to digitise UK trusts that seems too centralised will likely be rejected.
Technology has advanced considerably over the 15 years since NPfIT was launched. During this period, demands on health systems, including the NHS, have grown. The NHS finds itself at a critical point, with a mandate to improve both the quality and efficiency of care. Achieving these goals will require the modernisation of NHS’s digital infrastructure, taking advantage of prior successes and learning from past mistakes.
Health IT in UK general practice
General practitioners (GPs) in England conduct more than 300 million consultations per year, write more than one billion prescriptions, and perform the overwhelming majority of the nation’s healthcare interactions (14, 15). They provide community-based acute, preventive, and chronic disease care to a registered population and fulfill gate-keeping and coordinating functions by managing patient referrals into secondary care. Most GPs are independent contractors who run their own businesses, often in partnership with other GPs. Their practices vary in size and employ other clinical and non-clinical support staff accordingly.
In contrast to the problems in implementing health IT systems in English hospitals, efforts to digitise GP practices have been strikingly successful. For well over a decade, almost every general practice in England has employed a comprehensive EHR at the point of care.
The history of GP computerisation
The early computerisation of English general practice parallels computerisation in the rest of the economy. As new and affordable hardware and software became available, enthusiastic GPs – ‘early adopters’ – embraced it (16). This was sometimes funded by the practice itself (at times aided by the support of local hospitals) or through government research grants.
As early as 1975, a practice in Exeter reported designing and implementing a computer record keeping system that was, in essence, a full EHR (17). More often in the early years, practices implemented systems with more modest functionality. As private businesses, computer-generated efficiencies contributed to the profitability of the GP practice, and so the focus was on processes that could be easily automated, such as patient registration, repeat prescribing, recall and screening.
The profession recognised the implications of computerisation early on and, in 1980, the Royal College of General Practitioners–British Medical Association Joint Computer Group (RCGP-BMA JCG) was established to present a united negotiating voice to government (18). Adoption was limited to enthusiasts until direct government support was introduced with the ‘Micros for GPs’ programme in 1982, which offered to subsidise half the capital cost of a new system. This subsidy, funded by the Department of Industry, attracted 150 practices.
This early period of EHR adoption was followed, in the late 1980s, by private programmes offering free computers in return for data about morbidity, drug prescribing, and drug side effects. In 1989, the DH introduced a scheme for direct reimbursement of hardware and software costs associated with the implementation of accredited systems in GP practices, which further increased adoption (18). In 2004, the scheme changed from reimbursement to direct payments from the DH to suppliers. This arrangement – which amounted to 100% subsidy of the costs of purchase – and the accreditation of systems is currently managed by NHS Digital[footnote 6] , through the GP Systems of Choice (GPSoC) contractual framework (19). It has resulted in near-complete implementation of EHRs in English GP practices.
A consequence (and likely a motivator for some policymakers) of government subsidies of EHRs in GP practices was the ability to measure and influence practice. In 1990, the contract by which GPs were paid for services provided to the NHS became more data-driven, aimed at more directly linking remuneration and performance (20). The information requirement increased further with the enactment of the Quality Outcomes Framework (QOF) in 2004, a pay-for-performance scheme that now accounts for a significant proportion of practice income. GP performance is currently assessed through 81 indicators linked to clinical guideline recommendations. These indicators are reviewed annually and are mostly extracted from GP EHRs (21). It is not considered practically possible to qualify for QOF payments without an EHR. An example of a QOF indicator is:
The percentage of patients with coronary heart disease whose last measured total cholesterol (measured in the preceding 12 months) is 5mmol/l or less.
The process of purchasing patient care from providers is known as commissioning. Following a series of reforms in 2012, the purchasing function now rests with local organisations called Clinical Commissioning Groups (CCGs). CCGs are led by GPs and now control most of the budget for buying hospital services for patients. Effective commissioning requires a lot of information about patients and referral patterns, which has been facilitated by computerisation (and held back by the patchy digitisation of the secondary care sector).
There have been other advantages to widespread computerisation of GP practices. Patient information, collected through GP EHRs, has been used in public-private collaborations for research, epidemiological surveillance and quality improvement. As one example, the Clinical Practice Research Datalink (CPRD) extracts anonymised records from more than 600 practices for use in research studies and clinical trials. Specific cohorts of patients (that is, those with kidney disease or with diabetes) can be created and examined for treatment patterns or clinical outcomes (22). Another project linked anonymised GP data on more than 2 million patients to national mortality data to create a well-validated cardiovascular risk algorithm (QRisk2). In other words, the potential to undertake such innovative work at a national scale and at minimal cost is already being realised for ambulatory practices, and would increase significantly once hospital records are also digitised (23).
EHR systems have even supported a major pan-European Learning Health System project, but national efforts to anonymise and share patient information for research, through the care.data programme, have been hampered by public and professional concerns over privacy and information governance[footnote 7]. In any data sharing exercise, GPs are conscious of their legal position as Data Controllers, making them responsible for the security of data that they collect (24, 25). They are also mindful of the trust invested in the doctor-patient relationship and the professional duty of confidentiality. GPs appear to be increasingly willing to share data from their EHRs, and the major GP IT systems support such sharing.
The systems
Government intervention boosted the market for GP computer systems, through subsidy and, eventually, central purchasing. However, it has also curtailed diversity within the market, largely due to the strict accreditation criteria. From the late-1970s to the mid-1990s, many EHR systems designed for GPs were developed in the UK. At one point, there were between 30 and 50 competing systems, many used by only a handful of practices. As the market matured, the number of vendors offering GPSoC-accredited EHRs fell to 4 (EMIS, TPP, In Practice Systems, and Microtest), with EMIS and TPP dominating the market. There have been no new entrants to this market since 1997.
The accreditation criteria – while viewed as helpful in ensuring that systems are fit for purpose, secure, and robust – have also been criticised for imposing a large burden on EHR suppliers. In addition to making it difficult for smaller suppliers to keep up, the requirements may have sapped the capacity for innovations and improvements.
Although systems are purchased and funded centrally, GPs have the right to choose which accredited system they use. It should be noted that typical arguments for regional EHR uniformity – namely, interoperability and ease of information exchange – are not terribly salient, since relatively few GP practices share patients with one another and there is now a robust system for transferring patient records between GP practices with different IT systems. On the other hand, the ability of GP systems to share data with systems in trusts (including both hospitals and specialists’ practices) is extremely limited, even when the secondary care system is computerised (more on this later).
Although virtually all GPs now use a computer during patient encounters and operate paper-light practices, much correspondence, particularly that received from secondary care (from both hospitals and consultants), remains paper-based and has to be scanned.
GP EHRs represent a lifelong longitudinal record containing high-quality clinical data that is often not available from any other source.
The Summary Care Record (SCR) system allows emergency and out-of-hours clinicians to view basic clinical information from the GP EHR (26). As of this writing, there are approximately 55 million SCRs in NHS, with more than 70,000 accessed each week. In some regions, there is now widespread sharing of SCRs, leading to improved care and coordination. Since 2015, GPSoC-accredited systems have been required to allow patients to view their electronic records, although some practices have not actively promoted this feature (27).
Lab investigations conducted by other providers are readily accessible by GPs. However, the limited digitisation of the secondary care system means that GPs often rely on paper correspondence or electronic discharge summaries to find out about the care of their patients in other settings. Some community providers and nursing homes have implemented EHRs based on those used in general practice, but interoperability is very limited. As mentioned above, the transfer of patients between GP practices (for example, when patients move to a new area) is relatively advanced. The GP2GP service enables the transfer of entire electronic records between practices, even when they are using different EHRs.
Strengths and weaknesses of GP computer systems
Many of the strengths and weaknesses of current GP computer systems have their origins in decisions that were taken decades ago. All but one of the current systems accredited by GPSoC were originally developed by or in close collaboration with enthusiastic GPs in the UK. Throughout their development, these systems have been steered by strong user groups. This has resulted in an intimate understanding of GP requirements and has produced systems that do what GPs need them to do.
This history has also meant that systems have evolved over long periods, utilising technologies that may no longer be state of the art. The limited success of UK suppliers in international markets may be in part related to difficulties in making major adaptations to their systems.
International studies on the impact of primary care EHRs on quality and cost have produced mixed results (28).
However, the limited studies of GP EHR use in the UK have shown that systems are generally valued by the GPs that employ them. Commonly cited benefits include (29):
- improved financial rewards through meeting QOF payment requirements
- improved quality of care as demonstrated by progress against the QOF, reduced errors, reduced variability, and the ability to benchmark performance between clinicians and practices
- improved prevention and health promotion (by identifying patients who require intervention)
- improved efficiency (reduced duplication and greater availability of information; systems have not changed the length of office visits)
- reduction in space required to store paper notes
- helpful and customised decision support with local control over adoption that reduces alert fatigue
- improved documentation: notes shorter but more legible and complete thanks to the use of codes, the problem-orientated nature of the EHRs, and the link to payment
Importantly, unlike US primary care doctors, UK GPs are not required to perform massive amounts of documentation to justify billing levels, thus easing the amount of data entry and likely contributing to a warmer relationship with their EHRs (30). Overall, only 8% of Scottish GPs reported a negative opinion of their EHR, a far lower fraction than that seen in US studies (31).
While EHRs are generally popular among GPs, a number of drawbacks have been reported. (Most, it should be noted, are not specific to UK GP systems.) They include:
- user interfaces are sometimes cumbersome and inflexible
- system failures, although infrequent, are very disruptive
- data overload (management reports) and alert overload (during consultations)
- lack of training prevents clinicians from realising the full potential of systems
- data input is a problem for those who can not touch-type
- implementing new systems, and changing systems, is disruptive and impacts productivity. This can be exacerbated by long transitions and extended dual running of paper and electronic systems
Government
The government remains highly supportive of GP digitisation. The granular information produced by these systems has given NHS organisations a previously unimaginable view of quality and performance in every practice. It has also given government the ability to measure practices against central targets. There has been vigorous debate about whether such a target-driven approach improves holistic outcomes, but – given the targets – all sides appreciate the role of IT systems in reducing the administrative burden of data collection.
Patients
It has long been recognised that the use of computers during consultations can adversely affect GP-patient communications, but there has also been evidence that UK patients accept the role of computers and do not feel that they lead to loss of ‘the personal touch’ (32). Training (in areas like computer use, ergonomics, and doctor-patient communication) may play an important role, but its provision is not centrally funded and therefore varies.
One example of patient and media reaction altering the course of IT-related innovation is the recent outcry over the care.data programme (24). It seems likely that this experience will result in a larger role for patients in future discussions regarding health IT.
Conclusions and lessons
GP computer systems have evolved greatly over the last 40 years. Early systems, installed by enthusiasts, were simple enough that many were homegrown. Those systems were built by GPs, for GPs, and solved crucial business problems. Moreover, as such systems were being built, the profession established a united negotiating committee that clearly articulated policy requirements to government.
Over the past few decades, government funding has allowed for near-universal adoption of EHRs in GP practices, which has yielded major benefits in quality and efficiency. Universal adoption has come only through government subsidy, which was accompanied by a robust accreditation and regulatory framework. This, some believe, has stifled innovation in the market and led to a worrisome degree of consolidation in the supplier community. Despite these critiques, most stakeholders (GPs, government, patients) view the EHR experience in the GP market largely as a success.
In 2016, the establishment of an entirely digital infrastructure in England’s GP community is a massive advantage, one that is not yet shared by the rest of the NHS. Leveraging this advantage to enable greater patient engagement, more robust data sharing, better value, and a more innovative environment may require different choices than those that led to the current state. It will be important to learn from this experience in designing the future state of GP practices, as well as in designing systems and policies for the rest of the NHS.
The US experience with health IT, with possible lessons for the NHS
The US government’s decision to promote health IT began when President George W. Bush first learned of Tony Blair’s national IT initiative in 2003[footnote 8]. Reportedly seeking a domestic issue with broad bipartisan support in the run-up to his reelection campaign, President Bush instructed his advisers to create a framework for government to promote the adoption of health IT (33). The result was the Office of the National Coordinator for Health Information Technology (ONC). In 2004, David Brailer, a physician, economist, and entrepreneur, was appointed the first national coordinator (the ‘Health IT Czar’).
In its first 4 years, the ONC, working with a modest budget ($42 million [£32 million] at the start), focused on developing standards, promoting health IT, and engaging stakeholders. Things progressed in a measured way in these early years. In 2008, when the US economy collapsed, everything changed. In the final days of the Bush administration, Congress passed a $700 billion (£533 billion) stimulus package (the ‘American Reinvestment and Recovery Act,’ ARRA). Although ARRA was designed to spend money on infrastructure projects to promote job creation, health policy advisors to both the outgoing Bush and incoming Obama administrations saw a unique opportunity to garner significant government resources to promote the adoption of EHRs.
Their efforts resulted in the allocation of $30 billion (£23 billion) to a new programme, the Health Information Technology for Economic and Clinical Health Act (HITECH), to subsidise the purchase of computer systems by hospitals and doctors’ offices (34). The programme, which began distributing payments in 2010, was accompanied by a mandate for the government to create standards (‘Meaningful Use’) to determine whether health IT systems and doctors/hospitals qualified for the federal subsidies[footnote 9]. (Ironically, at about the time that HITECH and Meaningful Use were getting off the ground, NPfIT – which had inspired the US initiative – was terminated.)
Six years later, it is fair to say that Meaningful Use is the most controversial health IT programme in the US, often criticised as an example of federal regulatory overreach, and for failing to ensure usability and interoperability. Defenders of the policy point to the urgency to spend the money (which, after all, was designed to stimulate the economy), and to a desire to avoid creating barriers to implementation, such as insisting on robust usability testing or on interoperability. As David Blumenthal, ONC director at the time of HITECH’s launch (33) said,
I had the basic feeling that you had to operate before you could interoperate
The impact of HITECH and Meaningful Use
Measured against its primary goal – digitising the US healthcare system – there are few who dispute that HITECH succeeded.
Approximately 10% of doctors’ offices and hospitals had EHRs in 2009. Today, the number is estimated to be over 75% in doctors’ offices and over 90% in hospitals (35). Driven mostly by these government subsidies, in just the past 5 years the US healthcare system has gone from being primarily analog to being primarily digital.
Not only did the $30 billion catalyse the adoption of enterprise EHRs, it also stimulated Silicon Valley to enter the health IT arena. In essence, the consumer-facing IT world (big companies like Google and Apple, as well as start-ups, accelerators, and venture capitalists) had been waiting on the sidelines when it came to healthcare, despite the fact that healthcare accounts for 18% of US gross domestic product. Although none of the HITECH money went directly to these companies, the entire Silicon Valley ‘ecosystem’ was waiting for a signal that healthcare was now a digital business. When that signal became unmistakable, massive amounts of venture capital flowed in to digital health (approximately $4.5 billion in 2015), along with hundreds of startups involved in activities ranging from peer-to-peer communities, to sensor-laden ‘wearables’, to patient-facing apps.
In contrast to the largely decentralised, free-for-all environment on the consumer-facing side of health IT, the enterprise side has consolidated around a handful of large national suppliers. This consolidation (which mirrors the consolidation in the UK’s GP sector described earlier) occurred partly because smaller companies and homegrown systems were hard-pressed to meet the Meaningful Use requirements. Even many of the large healthcare systems that prided themselves on their homegrown IT systems (such as Partners Healthcare, which owns Harvard’s main teaching hospitals) ultimately switched to commercial systems.
Despite Meaningful Use (which included some provisions aimed at promoting information exchange), neither it, nor the business case for data portability, were sufficiently compelling to result in widespread interoperability. Even today in the US, it remains difficult to share electronic data between hospitals and clinics using EHRs built by different vendors. Interoperability between healthcare delivery organisations and pharmacies/laboratories is reasonably good, although not uniform. And there is relatively little data-sharing between the growing number of consumer-facing apps and sensors (for example, Fitbit) and the EHRs in doctors’ offices and hospitals.
Patient portals/connecting patient-facing and enterprise health IT systems
About a decade ago, some of America’s IT giants, including Google and Microsoft, tried to build consumer-facing patient portals. Despite large investments, these efforts mostly failed, in part because they were unable to solve the interoperability and ease-of-use issues.
Today, many of the enterprise EHRs come bundled with patient-facing portals, allowing patients to read their laboratory and radiology results, make appointments, and email their doctors. About 10 million patients in the US have full access to their clinician notes (‘OpenNotes’). Although this development was feared by many clinicians, research to date has shown high levels of acceptance by both patients and clinicians (36). But the larger issues of how the increasingly dynamic world of patient-facing health data and the more corporate world of enterprise health IT can fuse into one stream, and how this vast data stream will be managed and protected, remain largely unresolved.
Other issues surrounding Meaningful Use
Table 3 shows the 3 stages of Meaningful Use (37). The early stages, designed to ensure that people and organisations that accepted HITECH subsidies were actually using their EHRs in ‘meaningful’ ways, were popular and widely accepted.
However, later stages of Meaningful Use involved marked increases in regulation, creating a major burden on both suppliers and delivery systems, stifling innovation, and contributing to the consolidation in the supplier marketplace.
Table 3: The 3 stages of Meaningful Use (37)
| Stage 1 | Stage 2 | Stage 3 | |
|---|---|---|---|
| 2011 to 2012 | 2014 | 2016 | |
| Data capture and sharing | Advance clinical processes | Improved outcomes | |
| Meaningful Use criteria focus | Electronically capturing health information in a standardised format. Using that information to track key clinical conditions. Communicating that information for care coordination processes. Initiating the reporting of clinical quality measures and public health information. Using information to engage patients and their families in their care. | More rigorous health information exchange (HIE). Increased requirements for e-prescribing and incorporating lab results. Electronic transmission of patient care summaries across multiple settings. More patient controlled data. | Improving quality, safety and efficiency, leading to improved health outcomes. Decision support for national high-priority conditions. Patient access to self management tools. Access to comprehensive data through patient-centered HIE. Improving population health |
Many analysts believe the government has a key role in creating standards (perhaps even mandates) for interoperability and in helping to ensure privacy and security. But the fact that many US clinicians and IT professionals now refer to Meaningful Use as ‘meaningless abuse’ illustrates the level of discontent (33). In 2016, Medicare[footnote 10] acting administrator Andy Slavitt announced that Meaningful Use would soon end, to be replaced by a more streamlined programme, ‘Advancing Care Information’(38). Slavitt said,
We have to get the hearts and minds of physicians back. I think we’ve lost them.
In analysing the impact of Meaningful Use and HITECH, it is important to place these programmes in the context of larger changes in the US healthcare delivery system. As the US system pushes clinicians and delivery organisations to shift their focus from ‘volume to value’ (via the Affordable Care Act and other initiatives[footnote 11]), the hope is that they will seek and buy IT tools that help them meet those goals. This, the theory goes, will drive these organisations to innovate and improve their IT systems, obviating the need for the aggressive regulations found in the later stages of Meaningful Use.
The pressure for interoperability has grown tremendously in the past few years. The media and the US Congress have criticised EHR suppliers and some healthcare systems for willful ‘information blocking’; there is even talk of prosecution of individuals or organisations that participate in such alleged blocking (39). While some of this is political hyperbole, it is clear that the pressure on healthcare delivery organisations (the US equivalent of trusts) and suppliers to share information will grow, likely leading to far greater interoperability within the next 5 years.
A primary vehicle to promote interoperability has been the development of regional health information exchanges (HIEs). These are central hubs (usually non-profit organisations created for this purpose, sometimes run by an existing entity such as a hospital association) that mostly depend on fees from users, though there has also been federal and foundation support for HIEs. They are designed to collect and then distribute EHR data to different systems in a region. Unfortunately, the track record of HIEs is uninspiring. A few have been successful. And new ones are cropping up, in response to the growth of Accountable Care Organizations and bundling (see footnote), which creates a need for healthcare systems to follow patients within geographic regions. Still, billions of dollars have been invested by governments and foundations in the creation of HIEs, and most have failed, due largely to the absence of a strong business case for information exchange (40).
One key obstacle to information exchange and interoperability in the US: a regulation dating back to the 1990s that makes it illegal for the government to create a universal patient identifier. This action, taken after intense lobbying from privacy advocates, means that vast resources in the world of HIEs are spent on trying to confirm the identity of a given patient. In this regard, the presence of a single NHS number as a national patient identifier is an enormous advantage.
Other observations about the state of US health IT in 2016
Sites covered, and not covered, by HITECH
When HITECH’s $30 billion was being allocated, the decision was made to concentrate solely on office practices and hospitals. Post-acute care settings, including nursing homes, skilled nursing facilities, and hospices, were excluded, and most still lack EHRs. As in the UK, the social care sector remains mostly paper-based.
EHR design
Another widely held criticism of today’s EHRs is their relative inattention to basic principles of user-centered design, particularly when judged against the electronic tools we have grown used to in the rest of our lives. There are several reasons for this. One is that EHRs were designed to address billing/financial functions at least as much as, if not more than, the clinical needs of doctors, nurses, and patients (33). Another is that suppliers have not put in the resources to perform adequate testing with actual users. While there are myriad examples of error-prone functions and interfaces (confusing lab displays, the same keystrokes leading to very different results on different systems), perhaps the poster child for the lack of user-centered design is the problem of alert/alarm fatigue (41). In one month at UCSF Medical Center, for example, the electronic monitors for the 70 ICU beds threw off 2.5 million (!) alerts and alarms (42). In The Digital Doctor, a case is described in which the lack of user-centered design, along with alert fatigue and overreliance on technology, resulted in a 39-fold overdose of a common antibiotic (33).
EHRs and the health professional workforce
Rates of physician burnout in the US now exceed 50%, a 9% increase over the past 3 years (43). A 2013 RAND Corporation study commissioned by the American Medical Association found that many doctors cited EHRs as a major source of burnout (44). The problem lies partly in poor design, and partly in the fact that EHRs have become enablers for third parties who wish to ask doctors and nurses to document additional pieces of information (for billing, quality measurement, etc.), turning clinicians into ‘expensive data entry clerks’. One sign of this documentation burden is the meteoric growth in the number of ‘scribes’, individuals hired to provide real-time EHR documentation, allowing physicians to concentrate on (and make eye contact with) their patients.
EHRs and ‘Big Data’
While there is great enthusiasm for using ‘big data’ to develop personalised approaches for individual patients (‘precision medicine’), provide customised decision support to both clinicians and patients, and create ‘learning healthcare systems’, today all these goals are more promise than reality. Realising the potential will depend on significant changes through the entire system: changing incentives, far better interoperability, more meaningful data, the availability of analysts with skills in genomics, IT, clinical medicine, and more.
Lessons drawn from the US implementation of health IT
While this point can be debated, many observers believe that HITECH was a wise intervention, in that US healthcare represented an IT business failure (that is, typical business incentives did not drive healthcare delivery systems to implement IT, as happens in most other industries), and the programme created a tipping point for digitisation of the health care sector (33). The major downside of HITECH is that it opened the door to the overregulation of Meaningful Use Stages 2 and 3[footnote 12].
In terms of its impact on clinical care, the US experience with health IT has been disappointing. While the literature points to modest improvements in safety and quality, the promised efficiency gains[footnote 13] have not yet materialised (45, 46). And, as noted, unhappiness among health professionals is a dominant theme of the current era. While there are many reasons for this, there is little question that health IT has, to a surprising degree, added to the woes.
Why have things gone relatively poorly? Here, we return to the concept of the productivity paradox: the experience of many industries in which the promised improvements in quality and efficiency from IT failed to materialise in the first few years after digitisation (1, 5).
But the lessons of the productivity paradox offer room for optimism. By most measures, American healthcare is still in its first 5 years of widespread digitisation. The US is beginning to see improvements in the technology, a heightened pace of innovation, and early efforts to rethink the work, staffing, and workflow at hospitals with more mature IT systems (1, 5, 47). While the pace of change is slower than anyone would like, the system appears to be on the cusp of major improvements.
Which lessons from the US experience might be relevant to England? We offer the following thoughts:
Great attention needs to be paid to issues of adaptive change from the start. In particular, the predicament of clinicians, especially doctors and nurses, must be deeply appreciated. The tendency simply to digitise ineffective and inefficient analog processes needs to be resisted. Digitisation offers an opportunity to rethink the work and workflow.
If computers make the lives of clinicians substantially harder, if user-centered design is lacking, if the work is not reimagined for a digital environment, clinicians will become obstacles rather than supporters.
This will be difficult to overcome; every effort should be made to win the ‘hearts and minds’ of clinicians from the start, and to keep them engaged in optimising systems and rethinking ineffective work processes.
The US was well served by several decades of research into information technology and a strong cadre of clinician-leaders in IT, many of whom became chief medical/nursing/pharmacy information officers (the equivalent of UK CCIOs and CNIOs). These individuals serve as crucial bridges between the technology and front-line clinicians. The UK lacks a large cadre of such individuals; early efforts to build such a workforce will need to be supported and expanded.
Great thought needs to be given to several key tensions, including the benefits of central vs. decentralised implementation and the question of whether to rely on general business incentives (perhaps altered for the purpose of promoting implementation) versus regulation.
IT implementation is expensive. In the US, large hospitals often spend more than $100 million (£76 million) implementing an advanced, full-featured EHR. While few trusts will be able to afford such systems[footnote 14], it will be important to allocate appropriate resources for purchase, upkeep, and workforce training, and to provide the funds needed to support innovation and the integration of IT into improvement work.
The risk of ‘vendor lock’ is real[footnote 15]. For example, in the US, it will be very difficult to displace Epic from its near-monopoly position in large healthcare systems (48). However, it seems unrealistic to believe that homegrown systems or those built by small companies can meet the needs of large trusts (although they may be able to deliver some key components of systems). There is a risk of overlearning the lessons from NPfIT or incorrectly generalising from the positive experience with health IT in GP offices in the UK. In the short- to medium-term, digitisation of England’s hospital sector is likely to be accomplished with commercial systems, many built by non-UK companies.
Patience is required. The history of the productivity paradox points to a lag of 10 years or more before the full benefits of health IT are realised. An effective communication strategy should aim to balance enthusiasm for digitisation with appropriate expectations amongst various stakeholder groups.
The lack of digitisation in the US outside acute care settings now presents a significant problem. For example, although hospitals and outpatient practices are largely digital, most nursing homes and mental health facilities are not. An effort should be made to wire the entire UK system, leaving no sector – including mental health and social care – behind.
It is important to think broadly about interoperability, and to do so from the start. Interoperability is not just about how supplier-built EHRs can exchange information with EHRs built by other suppliers, as important as this is. It is also about the ease of ‘bolting on’ third-party systems to enterprise EHR systems, and integrating information from patient-facing apps, sensors, and other tools into these EHR systems. These latter connections set the stage for higher levels of innovation and flexibility. Data from interconnected systems also enables new types of research that can improve patient care, increase the quality and efficiency of health systems, and create enormous business opportunities.
Although not the subject of this review, privacy and security issues need to be addressed. While the idea of a fully wired, integrated, cloud-based system in which a patient’s complete information is stored in one place is tremendously attractive, it also means that an intruder could gain access to all the information about a single patient, or millions of patients, with a single breach. Getting this balance right is challenging, and crucial.
Recent advances in digitising the NHS’s secondary care sector: The National Information Board, the Five Year Forward View, and the £4.2 billion allocation
The demise of NPfIT in 2011 effectively halted any momentum toward a fully digital and interoperable NHS. The government made provisions to support functioning services such as the Spine and the Electronic Prescription Service, and responsibility for technology and informatics was spread across a number of government agencies (11). But NPfIT contracts between service providers and trusts were terminated and few people were bold enough to begin advocating for another ambitious health IT strategy.
However, policymakers soon realised that, while NPfIT had been unsuccessful, its goals remained crucial to the future of the NHS. The need for a new strategic plan for digitisation was clear. In 2012, the National Information Board (NIB) was established to create such a plan by bringing together organisations from across the NHS, public health, clinical science, social care, local governments, and the public. The membership of the board includes 37 organisations spanning the health and social care system.
The NIB report and the allocation of £4.2 billion
The NIB worked to craft an overarching framework for digitising the secondary care sector and achieving widespread intereoperability. In part informed by its analysis of the US experience with HITECH, NIB leaders chose to emphasise interoperability, rather than just adoption, of health IT. In light of the experience with NPfIT, they recognised that a highly centralised strategy was both politically impossible and undesirable. Their solution: divided the NHS into regions that would be asked to plan their digital strategies, including plans for regional interoperability.
In 2014, the NIB issued its major report, Personalised Health and Care 2020, which laid out the broad strategy (50). In essence, it called for:
- dividing the NHS in England into local ‘footprints’ – geographic areas composed of providers, commissioners, and other elements of the healthcare and social care sectors. The mandate is for footprints to organise themselves to conduct local transformation. A total of 73 footprints have now been established, each led by one or more Clinical Commissioning Groups (CCGs). This work is being aligned with a parallel effort to establish ‘Sustainability and Transformation Plans’ (STPs)[footnote 16].
- a ‘digital maturity assessment’, which seeks to identify (via a self-assessment questionnaire completed by each of England’s 154 acute trusts) the baseline digital state of local health economies. This assessment will be repeated over time to track progress across the country against national goals for digitisation (see Appendix E).
- allocating resources to support these footprints in achieving the goals described in their submitted and approved plans.
At the time of the 2014 NIB report, these resources had not yet been identified. But in February 2016, Secretary of State for Health Jeremy Hunt announced that the Treasury had allocated £4.2 billion over the next several years in support of the NIB framework (51). The monies were designed to support various component of NHS digitisation, as follows:
- £1.8 billion for a ‘paper-free NHS’
- £1.0 billion for infrastructure, including networks
- £750 million for ‘transforming care’
- £400 million as an enabler for NHS digitisation, including a new NHS.uk website and free wifi
- £250 million for data to support audit, planning and research
In April 2016, NHS published the results of the first round of digital maturity assessments (52). The results illustrate substantial variations in self-reported digital maturity – reflecting both the level of digitisation and interoperability – across England.
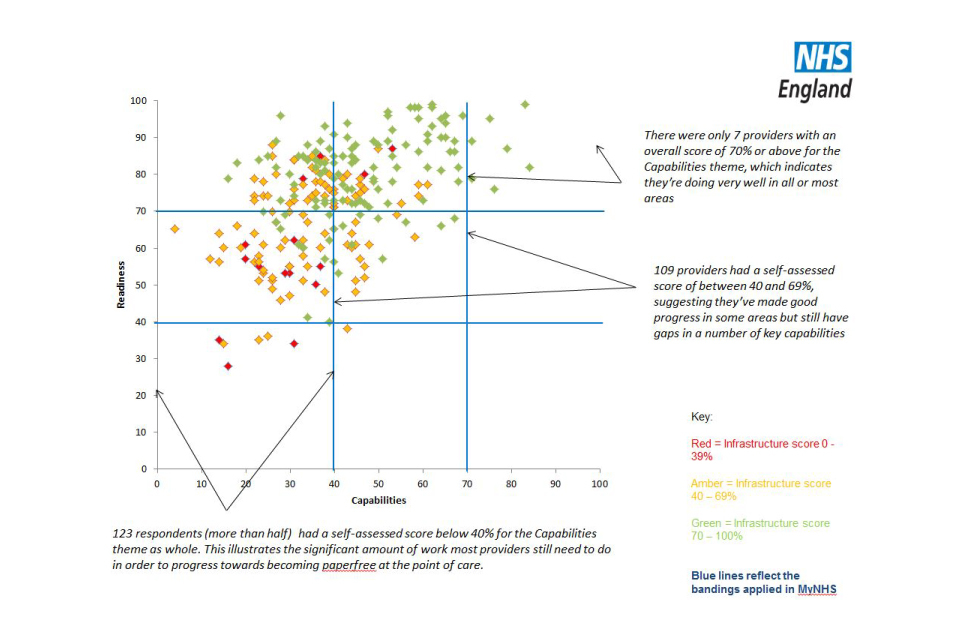
How respondents scored against readiness and capabilities. More than half of respondents scored below 40% for digital capabilities as a whole
The 2014 NIB report acknowledges that simply having a plan for implementation and interoperability is not enough to ensure a successful digital deployment. The report describes several key determinants of success, including ‘building and sustaining public trust’ and ‘supporting care professionals to make the best use of data and technology’. For our purposes, we highlight the latter category, which includes a description of the importance and current inadequacy of the clinician-informatics workforce[footnote 17].
While the Digital Maturity Assessment and the creation of the footprints emphasise interoperability over adoption, the NIB appreciated that effective implementation is challenging, and a fundamental precondition for interoperability. Our Advisory Group was charged, in part, because the leaders of the NIB, DH, and the NHS acknowledged the challenges in adoption and clinician engagement, areas that were underemphasised in the NIB report.
The Five Year Forward View and digitisation
We have already made reference to the Five Year Forward View, published by the NHS in October 2014, and designed to serve as an overall strategic view for the Service over the subsequent 5 years (53). The Forward View identified 3 widening gaps that needed to be addressed to create a sustainable NHS: a health and wellbeing gap, a care and quality gap, and a financial gap. In response to these challenges, the Forward View calls for:
- Transformation of care delivery through new care models, most notably the development of multispecialty community providers and primary and acute care systems, similar to the Accountable Care Organisation (ACO) model in the US.
- A radical upgrade in prevention and public health
- Greater investment in the health and well being of employees
- Exploitation of the information revolution, including greater transparency of data and acceleration of health innovation
Regarding this final point, the Forward View calls for ubiquitous EHRs, advanced interoperability, electronic prescribing, and the use of digital data to support continuous quality improvement in the NHS.
Conclusions
Following the failure of NPfIT, the NHS went through a period of stagnation with regards to digitisation.
Impressively, the past few years have seen the emergence of a new consensus that, while NPfIT had been unsuccessful, its goals were, and remain, essential.
In short, it will be impossible for the NHS to become a modern, effective, and efficient healthcare system without complete digitisation.
The overarching strategy established by the Five Year Forward View, the more digitally-focused goals and framework created by the NIB, and the allocation of significant resources to support digitisation by the Treasury all set the stage for the current effort, and for this report.
3: The National Advisory Group’s methods
In November 2015, Professor Robert Wachter of the University of California, San Francisco (UCSF) was asked by the UK Secretary of State for Health, Jeremy Hunt, to organise a group to advise NHS England on digital implementation in the secondary care sector. The committee’s Terms of Reference are shown in Appendix A. After extensive consultations, an interdisciplinary group of experts – including in informatics, policy, interoperability, usability, clinical practice, workforce, and the patient perspective – was convened. Seven are based in the UK (6 in England, 1 in Scotland), 7 are from the US, and one each is from Australia and Denmark (page 3).
The Advisory Group held 9 2-hour meetings by teleconference, as well as a two-day meeting in London in April 2016. During the April meeting, the Group heard presentations from about a dozen diverse experts and stakeholders. Dr. Wachter also held individual or group meetings with approximately 100 people, met with several stakeholder groups, and received written input from many other individuals and organisations. He conducted on-site visits at the Barts, Salford, and Imperial Trusts; he and several members of the Advisory Group also visited Addenbrooke’s Hospital during the April meeting in England. Appendix B lists all the meetings, visits, and interviews.
This report was drafted in sections by the relevant experts on the committee, and written mostly by Prof. Wachter with editorial assistance from Katie Hafner, a journalist with extensive experience in healthcare and technology. In addition, the Group received essential staff support from Harpreet Sood. We also benefited from the assistance of Tom Foley and Peter Thomson. The Group commissioned reports on the history of NPfIT (an edited version, The National Programme for information technology is in the background section, written primarily by Dr. Sood), the experience digitising the UK’s GP sector (The history of GP computerisation, written primarily by Dr. Foley), the American experience with health IT (The US experience with health IT, with possible lessons for the NHS, written primarily by Dr. Wachter), and another on the structure of the NHS and its entities that relate to digitisation (written primarily by Dr. Thomson; its findings are woven throughout this report). Ms. Hafner and other staff members were compensated for their work. Drs. Wachter, Thomson, and Foley, and the Advisory Group members received no remuneration other than payment for travel.
The findings and recommendations that follow have been endorsed by the members of the National Advisory Group. While they have been reviewed by relevant officials and senior leaders in the NHS and DH, as well as by selected outside experts (with feedback considered carefully and, where appropriate, accepted), the conclusions and recommendations represent the independent work of the Advisory Group and do not necessarily represent the views of any other parties, including the NHS and the Department of Health.
4: Overall findings and principles
Below, we describe 10 findings and principles that our Advisory Group came to agreement on and which guided our implementation recommends (they follow in section 5 ). For each one, we present the core findings and principles (in italics) and then offer some additional background and rationale, as well as links to appropriate references.
1. Digitise for the correct reasons
The goal of digitisation of health systems is to promote what has become widely known as healthcare’s Triple Aim: better health, better healthcare, and lower cost. These goals are consistent with those of the NHS’s 2014 Five Year Forward View.
Reasonably strong evidence supports the premise that, if appropriately deployed and used, digital health care is safer and of higher quality than care delivered through paper-based systems. Digitisation should also be an enabler of better health, by creating new methods to follow populations of patients, to engage them in their own care and wellness, and to promote preventive services and public health interventions. Efficiency gains, however, take time to emerge, since organisations need to restructure to take advantage of new digital capabilities (the so-called ‘Productivity Paradox’ of information technology).
In 2008, Don Berwick, then head of the Institute for Healthcare Improvement (IHI), and colleagues described the so-called ‘Triple Aim’ for healthcare systems: better health, better healthcare, and lower cost (1,2) When Berwick became director of the Centers for Medicare & Medicaid Services (CMS) in 2010, this became the organisation’s guidepost. (Interestingly, in light of growing rates of burnout among healthcare professionals, there is a new movement to add a fourth aim: professional satisfaction, a point we’ll return to later (3)).
The Triple Aim, of course, is consistent with the goals of the Five Year Forward View, which highlights the need for service transformation and integrated models of care – all of which require effective sharing of information and the creation of a learning healthcare system (4).
Why is it important to focus on clinical aims when it comes to digitisation? First, it makes clear that digitisation is not the end-goal – it is a means to an end. Therefore, metrics for success should be framed more in terms of the ultimate goals (Did patients live longer? Were they more engaged in their care? Were there fewer readmissions?) than the IT-related goals (Does the hospital have computerised order entry? Is there a Summary Care Record?). This is a nuanced issue: it is often important to measure the building blocks, but the ultimate goals should relate to patients, patient care, and population health.
The second reason this is important is that the ultimate benefits take time to accrue. This is one of the greatest challenges in health IT policymaking: leaders need to generate enthusiasm for spending public money to implement digital systems, and yet the ultimate benefits may take years to emerge. In the US, there is mounting evidence that digitisation has led to improvements in quality and safety, mostly by preventing medication errors through ePrescribing, and by guiding doctors to provide evidence-based treatments (5). Yet, despite a 2005 RAND study that projected $81 billion (£62 billion) in annual savings from digitisation, a more recent study found no clear evidence of efficiency gains, largely because of the extra time that healthcare professionals were spending on documentation (5,6).
Is this an argument against digitisation? Absolutely not. But it is an argument for keeping sight of the ultimate goals of improved health, better healthcare, and lower costs; for being prepared for unexpected consequences; for creating a system that is nimble and able to adapt over time; and for retaining a relatively long-time horizon.
2. It is better to get digitisation right than to do it quickly
While there is urgency to digitise the NHS, there is also risk in going too quickly. The Advisory Group urges the NHS to digitise the secondary care sector in a staged fashion, in which trusts[footnote 18] that are ready to digitise are catalysed to do so, while those that are not ready should be encouraged and supported to build capacity, a process that can take several years. Digitisation of health systems is a long journey, and rushing the latter group into computerisation is likely to lead to poor morale and costly failures.
This is a crucial point. It should not be assumed that a new national strategy to digitise the secondary care sector is without risk simply because it differs from NPfIT in leadership or structure. We worry that, in light of the current austerity conditions, the uncertainties introduced by Brexit, and the somewhat demoralised NHS workforce, a push to digitise the secondary care sector rapidly carries a high risk of failure.
Now that national money has been allocated to digitise the secondary care sector, it would be natural to want to ’just get on with it’. We believe that a strong push to comprehensively digitise every trust over the next few years would be an error. We say this for several reasons.
First, while the Treasury’s allocation of £4.2 billion is generous in light of today’s austerity conditions, we do not believe it is enough to complete the entire job (recall that only £1.8 billion is targeted at implementing systems to achieve the goal of a ‘paper-free NHS’). Although a detailed economic analysis is beyond the scope of our review, a rough calculation may suffice here. Let’s assume that it would cost the average acute trust a minimum of £40 million to digitise (including the costs of purchasing or licensing the software, consultants, staff training, and new staff hires). Let’s further assume that half of this £40 million – £20 million – would need to come from the central government allocation. With 154 acute trusts, the total amount required from the government would be slightly more than £3 billion, or nearly twice the amount allocated.
In addition to the practical reality of a funding shortfall, our assessment is that some trusts are currently too financially strapped, and/or lacking the staff, the training, and the culture to digitise effectively. We believe it would be an error to rush these organisations into implementing clinical information systems. Rather, we think it would be better to spend a few years helping these organisations prepare for successful implementations.
Both of these factors – the insufficient resources to digitise every trust and the fact that some organisations need time to get ready – lead us to recommend a staged approach to implementation. Staging may also address the political reality that, given the problems with NPfIT, politicians and the public seem ready to pounce on failed implementations as evidence of a poorly conceived and executed plan.
Case study: Cambridge University Hospitals
In April 2013, Cambridge University Hospitals NHS Foundation Trust (CUH), a world-renowned teaching hospital in Cambridge with some 1,200 beds and 575,000 outpatients per year, signed a ten-year, £200 million contract for implementing a trust-wide electronic health record (EHR) system. Eighteen months later, the trust installed the Epic EHR system at both Addenbrooke’s Hospital and The Rosie, its maternity hospital.
To put the CUH’s achievement in perspective, it is worth noting that prior to 2013, the trust had been given a rating of Stage 1 (‘minimal digital adoption’) on the Electronic Medical Record Adoption Model (EMRAM), whose stages range from 0 to 7.
CUH’s digital transformation programme, dubbed eHospital, entailed the training of some 12,000 staff over a nine-week period, as well as the installation of some 6,750 personal computers and 500 laptops, 395 workstations on wheels, and 420 hand-held ‘Rover’ (iPod Touch) devices.
Today, CUH benefits from the integration of all patient-related administrative and clinical information. Every patient wears a barcoded wristband linked to the EHR, which has improved patient safety. Moreover, the trust saves roughly £460,000 annually in staff time for eliminating the need to retrieve paper notes, as well as £655,000 each quarter in charting, thanks to device integration. The fracture clinic now reviews notes and x-rays virtually, freeing up some 4,500 clinic appointments.
CUH’s was a classic, by-the-book, Epic implementation. That is, the trust opted to ‘go live’ all at once rather than phase the system in. The strategy behind a so-called ‘Big Bang’ implementation is to feel the pain all at once and work through it, as opposed to continuous pain over an extended period. (Think of a double hip replacement, and throw in 2 new knees at the same time, and you’ll get the picture.)
It was not surprising to the Advisory Group that for CUH – and, we should add, for most healthcare systems that undergo a completely digital transformation - the road to digitisation was anything but smooth. In the immediate period following the Epic installation, CUH experienced a number of service disruptions: disruption to pathology services caused by problems with specimen label printers; disruption to the delivery of results of pathology investigations to primary care and other external consultants; a 4-hour period of unplanned downtime necessitating an ambulance diversion plan and a several-day period of instability of one of the transfusion system interfaces; and disruptions in the consistency of clinical care including venous thromboembolism assessment, nursing care plans and community referrals, completion of discharge summaries and complex inpatient prescribing. Further, there was a substantial decrease in productivity, principally in outpatient clinics, in particular in hard-pressed services such as dermatology, cardiology, ophthalmology and ENT.
In April 2015, just 6 months after the Epic implementation, the Care Quality Commission (CQC) carried out an inspection of the trust, and in its report, published in September, the CQC identified 8 areas across the Trust that required focus for improvement, including Epic and IT support. CUH’s problems also caught the attention of the national press (‘The NHS’s chaotic IT systems show no sign of recovery,’ wrote the Guardian in December 2014).
Following a visit in April 2016 to CUH, the Advisory Group concluded that the problems caused by the Epic installation have largely been ironed out. The system appeared to be functioning well, and managers and healthcare professionals were taking advantage of its functions to improve care quality and efficiency. In May 2016, Professor Sir Mike Richards, CQC’s Chief Inspector of Hospitals, said the CQC was pleased to see improvements, while concluding that ‘further work needed to ensure the standards of care meet those which people should be able to expect’.
Currently at Stage 6 in EMRAM ratings – among the nation’s highest – CUH is now aiming for Stage 7 status. In April 2016, the trust installed Epic’s MyChart patient portal, and has plans to implement the NHS interoperability toolkit to link its Epic system to GP practices, and Epic’s ‘Care Everywhere’ for exchanging specific parts of patients medical records with other digitised hospitals. Although the Advisory Group took away important lessons from CUH’s early experience with implementation, in the eyes of the Group, the trust’s current digital maturity was the highest of any of the trusts visited.
This provides yet additional rationale to ensure that early implementations succeed. We believe that these early successes will lay the groundwork for a powerful argument for additional resources to be made available to get the rest of the job done in a second phase. As one national IT leader told our group, ’Never give money out faster than it can be absorbed.’
Importantly, although the new effort is vastly different from NPfIT (with extreme care being taken to avoid calling it a ‘national programme’ and to minimise centralisation), this does not guarantee success.
Our Advisory Group was very concerned that an aggressive push to digitise the entire secondary care sector by 2020 was more likely to fail than succeed.
3. ‘Return on investment’ from digitisation is not just financial
While it is natural to seek a short-term financial return on investment from health IT, experience has shown that the short-term ROI is more likely to come in the form of improvements in safety and quality than in raw financial terms: pounds saved versus pounds invested. In other countries that have implemented health IT, including the US, cost savings have not materialised in the first few years after implementation. Instead, the history of organisational digitisation teaches us that cost savings may take 10 years or more to emerge, since the keys to these gains are improvements in the technology, reconfiguration of the workforce, local adaptation to digital technologies, and a reimagining of the work. In fact, the first year or so after implementation is more likely to see efficiency losses than gains. In health IT, patience is a virtue.
It follows from the prior discussion that measuring digitisation in pure ‘return on investment’ terms is a mistake – both because the ROI is unlikely to be immediate, and because the ‘returns’ should be framed in overall benefit, not simply financial benefit. It concerned us that many of the discussions we heard from national IT and health policy leaders regarding health IT referenced financial returns, perhaps because the arguments for public monies need to be framed this way, and because public resources are currently so scarce (in 2012 only a handful of English hospitals ran deficits; in 2016 the vast majority do) (7). While we understand the political realities, it is important to appreciate that the returns on investment are more likely to be clinical than financial in the short term, and that financial returns require transformation of care and redesign of the work, with IT providing the scaffolding (8).
That said, it is reasonable to consider the financial benefits of digitisation, which may go beyond efficiency gains. In such an accounting, it will be important to think broadly, and across sectors. For example, the US experience has shown that the $30 billion spent under HITECH led to enormous economic benefits in job creation, including parallel investments by consumer- and business-facing technology companies like Google, Apple, and IBM (9). There are also tremendous efficiencies from digitally facilitated research. For example, a nationally used cardiac risk algorithm was developed in the UK using clinical EHR-derived data at a fraction of the cost of primary data collection (10).
4. When it comes to centralisation, the NHS should learn, but not over-learn, the lessons of NPfIT
Most analyses of the failure of NPfIT emphasise that its structure and approach were overly centralised and top-down. In England, there is considerable variation between regions – in both the care delivery system and the needs of the population. This, along with the well-known hazards of centralisation, argues for a more regional approach. As the NHS pursues a new effort to digitise secondary care, NPfIT’s lesson is clear: while national funding is essential to promoting digitisation, too much centralisation would be a mistake.
Still, it is important not to overlearn the lessons of NPfIT. Centralisation sometimes makes sense. In the case of a new national health IT initiative, areas that would benefit from some degree of centralisation include: establishing a framework to support local/regional implementations, supporting efforts to improve the usability of systems, supporting the development of business cases and contracting, supporting relevant research activities (including developing a national data repository), guaranteeing interoperability, ensuring privacy and security, and leveraging national structures such as the Spine and the NHS number.
Moreover, we favour forging national ‘framework’ contracts with leading EHR suppliers to give small trusts the option of using a pre-negotiated contract, instead of having to negotiate individual EHR contracts themselves. The point of such framework contracts would simply be to facilitate the trusts’ choices and to ease the process of contracting; the NHS should not dictate which clinical information system a trust should purchase.
The balance between regional and centralised approaches represents a core tension within the NHS. Of course, there is no one right answer – the correct approach needs to consider the problem being addressed and many other factors. In general, centralisation should be applied when its benefits outweigh its harms: when centralising creates economies of scale, when there are market failures that can be remedied only by centralising, or when there is insufficient capacity at the local level.
The analyses conducted after the demise of NPfIT typically emphasised overcentralisation as a major explanation for the programme’s woes (11,12). We agree. However, part of the challenge in constructing a new policy approach to digitisation is that NPfIT’s history creates a sizable, and perhaps unfair, bias against centralised approaches. While the overall policy thrust of the new effort should emphasise local and regional solutions (particularly when it comes to which EHR to purchase, the need to achieve local buy-in and engagement, and the locus of support for this work), we believe it would be a mistake to avoid centralisation in certain areas where it just makes sense. We have listed these areas above.
One important area relates to contracts with suppliers. In NPfIT, all contracts were negotiated centrally, as were all decisions about which EHR product would be implemented in a given region. While well intentioned (the leaders of NPfIT believed that this approach offered major economies of scale, created tremendous negotiating leverage, and ensured regional interoperability since everyone in a region would be on the same system), the flaws in this approach are now obvious.
While our approach emphasises local control of purchasing decisions, we do believe that small trusts may be at a disadvantage as they try to negotiate complex contracts with large international IT suppliers. Because of this, we favour central negotiation of so-called framework contracts with several of the leading suppliers[footnote 19]. That way, local trusts can take advantage of any cost reductions from the negotiation, as well as the central expertise that they may not have regarding the legal and contractual nuances. Importantly, use of these framework contracts would be entirely optional; trusts would have complete choice of products. Maintaining the sense of local ownership of the process by trusts and their clinicians is crucial – particularly on the heels of NPfIT, a failed programme of externally imposed contracts (13). For trusts that do not want to avail themselves of a central framework contract, another option may be shared purchases by multiple trusts, particularly those in the same local footprint (14).
5. Interoperability should be built in from the start
Local and regional efforts to promote interoperability and data sharing, which are beginning to bear fruit, should be built upon. Not only is interoperability important for individual patients who need their data shared for their own care, but it also promotes life-saving research and innovation – the latter by giving small companies a chance to solve specific problems with apps and other software that can bolt onto larger ‘enterprise’ IT systems. National standards for interoperability should be developed and enforced, with an expectation of widespread interoperability of core data elements by 2020.
In addition to data sharing for health professionals, we endorse giving patients full access to their electronic data, including clinician notes (‘OpenNotes’). We also favour creating easy ways for patients to download such data (in a computable format) for their own use, and to upload patient-generated data (via surveys, sensors, wearables, patient-reported outcome measures, and data from other apps) into their electronic record. Such methods need to be built using principles of user-centered design, with careful attention paid to the implications for clinical workflow and workforce.
We applaud the NIB’s emphasis on interoperability as a core attribute of any new programme to digitise the secondary care sector (15). The fact that, in 2016, many GP practices – virtually completely digital – still receive faxed versions of printed consultations from hospital-based specialists (and sometimes don’t receive them!) is an illustration of how important it is to build in interoperability from the start. On the other hand, over 70% of acute trusts now share discharges electronically, progress that can be built upon.
Interoperability is deceptively difficult. It is important to take a holistic approach to it – just having the right standards and interfaces is not enough if, for example, a GP worries about liability after sharing data. All of these issues – technical, economic, legal, political – need to be addressed in order to create a functioning interoperable system.
While complete interoperability (all digital information, available everywhere) is the ultimate goal, in the short- to medium-term, it would be best to focus on the most salient parts of the care record, and on regional, rather than national, exchange.
The development of the Summary Care Record (SCR) was an effort under NPfIT to address the former problem, and it has had mixed success and limited uptake. While the SCR may serve as a starting point for sharing core information nationally, we encourage more experimentation and evaluation to determine the optimal content to be exchanged (16). (One problem with the SCR is that its content is completely controlled by the GP, whereas a truly interoperable clinical exchange needs to be modifiable by different clinicians in different clinical settings.) The SCR should be seen as complementing the development of local shared records and providing a core information set (such as lists of medications, allergies, and chronic diseases) when such information is not available locally. These decisions about interoperability require significant involvement of stakeholders, including clinicians, managers, patients, and IT suppliers, with government serving as a convener and enabler rather than the final arbiter – particularly until standards mature.
In terms of geography, we would emphasise interoperability within a region, and the footprints (see The NIB report and the allocation of £4.2 billion) seem like a reasonable way of thinking about the shape of the region for this purpose, although this may evolve as the STPs mature. As success stories emerge from regions that have achieved robust interoperability, the NHS should become more ambitious, turning its attention to linking several footprints together, on the path to an ultimate goal of a nationally interoperable system.
Elsewhere in our recommendations (finding 7: Health IT Systems must embrace user-centered design), we emphasise the importance of user-centered design and a deep appreciation of the impact of digitisation on the workforce when it comes to EHRs. This sensibility is also important as we bring patients in as active partners in seeing and contributing to their digital data. It is one thing to say, ‘patients will have access to their electronic data from their GP and their hospital’. It is quite another to ensure that the data come in a usable, actionable form.
Moreover, while ultimately giving patients access to electronic tools is likely to decrease the burden on the healthcare system (as patients are able to perform higher degrees of self-management), in the short term the opposite is often true. The patient who looks up her problem on the Internet, or emails her doctor, or whose data from sensors or wearables is transmitted to the doctor or hospital may well create additional work for a healthcare system whose resources are already stretched. This workflow needs to be anticipated and addressed.
6. While privacy is very important, so too is data sharing
Privacy is very important, but it is easy for privacy and confidentiality concerns to hinder data sharing that is desirable for patient care and research. Striking the right balance is critical. The problems with the implementation of the care.data programme – which lacked a comprehensive communication strategy to engage with the public and a clear protocol regarding who could access the data – illustrate how sensitive these issues are.
Nevertheless, it would be a mistake to lock down everyone’s healthcare data in the name of privacy. It is critical to ensure that the appropriate technical safeguards are in place. It is equally critical to design and implement a system of regulation and governance that reassures patients that their rights and interests are fully respected, that provides clear guidance to professionals and managers, that effectively monitors for problems, and that takes actions where needed. The key is proportionate governance: balancing individual rights while recognising the enormous opportunities for patient benefit through the systematic secondary uses of NHS’s unique national data assets. We endorse the recommendations of the National Data Guardian’s 2016 Review of Data Security, Consent, and Opt-Outs, which was commissioned to achieve this balance.
The problems with privacy and security are obvious and tangible, and there is a vocal group of advocates defending the need for strong steps to protect data from misuse. The benefits of data liquidity are less obvious, more diffuse, and may accrue to individuals in the form of health benefits in the future.
It would be a shame if the NHS moved to a more interoperable system, yet the potential benefits – for individual patients and the entire system – were to become unavailable because data were so tightly locked down.
We know the National Data Guardian review grappled with these issues and we support her committee’s recently reported findings and recommendations.
Issues of design are relevant here as well. Poorly designed systems to ensure privacy and security may encourage – in some cases nearly require – workarounds by healthcare professionals. As one example, as part of NPfIT every doctor and nurse was issued a security card to sign into their EHRs. The idea was that every clinician would sign in with his or her own card, thus ensuring that patient data would be accessed only by authorised individuals (‘role-based access’). The problem: in one A&E department the sign-in process took several minutes, far too long for busy doctors and nurses to wait while seeing large numbers of acutely ill patients. The solution: one healthcare worker signed in early in each shift and simply left his or her card in the machine, thus thwarting the very purpose of the security system. We learned that this kind of workaround is common practice.
7. Health IT systems must embrace user-centered design
IT systems must be designed with the input of end-users, employing basic principles of user-centered design. Without user-centered design, such systems are unlikely to meet their full potential and have been shown to create opportunities for new types of errors and risks for patient harm. Poorly designed and implemented systems also result in frustrated healthcare professionals, by adding to their already substantial workloads and diverting them from meaningful work. While the NHS does not possess the skills to judge usability, it should support academic or other partners to conduct such reviews using validated assessment methodologies. Such reviews could then factor into decisions by trusts regarding IT systems. The NHS and England’s funders should also support research in this area.
The usability of technology is one of the major drivers of its widespread adoption and use in everyday life. Usability also affects the quality of the data collected, and is thus a major determinant of the power of analytics. In high-risk industries like healthcare, usability is inextricably tied to safety. Poorly designed or implemented EHRs that do not support the way clinicians work also result in increased frustration, increased workload, and workarounds. While there may be short-term gains from education of end-users, in general education and training cannot compensate for poor usability. Consideration should also be given to the patient, who will interact with these new systems and their own EHRs. A negative user experience for the patient may well have consequences for both the individual and the healthcare system.
The usability of any device or system can be broken down into 2 major categories: basic interface design (‘bin 1’) and cognitive support of the user (whether clinician or patient) (‘bin 2’) (17). The basic interface design should follow well-established principles (such as choices of font size and color) that ensure information is clear and readable, while also providing adequate contrast between the text and the background. Good bin 2 design entails much more detailed – and deeper – understanding of the cognitive work of the typical user’s information needs (including when and how information is displayed, as well as decision support and functional needs). In healthcare, while there are a number of best practices for designing user interfaces, there are also enormous opportunities to improve Bin 2 design, and this work, in particular, has been underemphasised to date (18,19).
For example, a well designed bin 1 electronic order screen may have clearly labeled medications in a readable font and size, with an intuitive search function that minimises the potential for user error by separating and graphically distinguishing similar sounding medications. A bin 2-savvy display would provide the functionality a provider needs to accomplish tasks with a reduced cognitive load. Ethnographic work (that is, direct observation) is often necessary to guide these designs; while focus groups can provide some information, end-users themselves are not always able to articulate their needs.
To improve bin 1 and bin 2 usability, there are specific policy and non-policy based levers that England should consider. These include involving clinical users and patients in design, measuring the usability of systems using standard methodologies, providing usability information to trusts to aid in their purchase and implementation decisions, and creating mechanisms to allow users to share information regarding usability problems in their EHRs. Given the concerns about centralisation and limited NHS budgets, we do not favour an ambitious central regulatory apparatus to certify EHRs on usability. Rather, we would emphasise making usability information – perhaps collected by third parties – available to trusts to guide their purchasing decisions.
In addition, we believe that the NHS should help create systems that foster the rapid collection of data regarding safety hazards of health IT systems. Such systems should make it easy to upload to a suitable repository a screenshot of an unsafe interface, the user’s context (for example, doctor or nurse, clinical unit, and type of EHR system), and a brief description of the problem it created. Instead of creating a new agency to receive and analyse these reports, we favour adding them to the reports already collected by the National Reporting and Learning System (NRLS), now being managed by NHS Improvement (20). NRLS would be tasked with turning these reports into meaningful insights, and disseminating the lessons to users and suppliers, as appropriate (21). Based on the US experience (where some EHR vendors have forced purchasers to sign non-disclosure agreements that block clinicians from sharing screenshots, even those depicting unsafe conditions), the NHS should require EHR suppliers to allow this kind of transparency (22).
It is worth connecting this discussion of usability to 2 additional issues: the clinician-informatician workforce and the importance of anglicisation.
Regarding the workforce, while crucial usability work must be performed by EHR developers, every product needs to be customised by the hospital or practice that implements it. In fact, much of the bin 2 work can only be done by those with a deep appreciation of how work is done in that organisation. This is yet another reason that the NHS needs a far larger, more professional, and better supported network of individuals embedded in trusts who understand both the clinical work and the technology (recommendation 3: Develop a workforce of trained clinician-informaticians at the trusts, and give them appropriate resources and authority). Among other skills, such individuals must possess a strong understanding of user-centered design principles (23).
In addition, since many, perhaps most, trust EHR installations will be of systems built in other countries, considerable attention needs to be paid to issues of anglicisation. User interfaces, workflows, and legal requirements that might make perfect sense in, say, the US or France, might not transfer seamlessly to the NHS. Fortunately, most major hospital suppliers have already implemented in the UK and addressed these issues, at least in part.
8. Going live with a health IT system is the beginning, not the end
Turning on a new information system in a large hospital or trust (so-called ‘Go-Live’) is always a difficult period, but is nonetheless just the start. (Actually, the start must occur years earlier, as the organisation prepares for a successful implementation by assessing and improving its workforce, its processes, and its overall digital readiness – a point we highlight later.) Health IT systems need to evolve and mature, and the workforce and leadership must be appropriate for this task.
Even with perfect preparation, many trusts (along with hospitals in other countries) have experienced challenges, including increased waiting times or budget overruns, during the Go Live period. Such initial turbulence occurs frequently, and generally resolves over 6 to 18 months.
While maintaining patient safety is non-negotiable, regulators and commissioners need to have a degree of tolerance for short-term slow downs and unanticipated consequences in the period following EHR implementation – they are the norm, not the exception.
We learned of several Go-Lives in England in which there were problems; perhaps the most famous is the Epic installation at Addenbrooke’s Hospital in Cambridge. In such cases, the threat of penalties or press coverage that make the problems appear scandalous can lead organisations that are considering digitisation to think again. One of the memorable lines we heard in our research was this: ‘If you consider all the things that can get a trust CEO fired, not implementing health IT is not on the list’.
Our recommendations are designed to change that dynamic, because such attitudes harm the NHS and its ultimate ability to meet the vision of the Five Year Forward View (4). However, even if the national subsidies are sufficient, knowing that, say, a short-term increase in waiting times or a budget overrun will lead to tremendous unpleasantness for the organisation and its leader creates an unhelpful atmosphere of fear and risk aversion. There must be some slack built into the system for the very difficult process of switching from analog to digital work. This doesn’t mean that leaders should be unaccountable for poorly planned and executed implementations, or that patient safety should be compromised. But it does mean that we want the average trust CEO to approach implementation realistically and enthusiastically, and to transmit this message to the clinical and non-clinical staff.
9. A successful digital strategy must be multifaceted, and requires workforce development
The new digital strategy for the NHS should involve a thoughtful blend of funding to help defray the costs of IT purchases and implementation, resources for infrastructure (hardware such as monitors and keyboards, network modernisation, wifi), support for leadership and informatics training, as well as support for education of leaders, front-line providers, trainees and, as above, chief clinical information officers (CCIOs) and other clinician- and non-clinician informaticians. It also needs to include support for real-time evaluations and mid-course corrections. The odds of failure will be increased by focusing only on buying and installing IT systems without attending to issues like hardware, network stability and speed, workforce training and development, programme evaluation, and iterative improvements.
The Advisory Group was struck by the small number of leaders at most trusts who are trained in both clinical care and informatics, and their limited budgetary authority and organisational clout. This deficit, along with a general lack of workforce capacity amongst both clinician and non-clinician informatics professionals, needs to be remedied if trusts are to succeed in implementing and optimising health IT systems. Let’s begin with the nuts and bolts. In order for a clinical information system to be successfully implemented, there needs to be a robust and reliable network, ubiquitous wifi, plentiful and functioning computer terminals, and brisk sign-on. Buying an EHR without them would be akin to buying a modern car but leaving the roads unpaved.
As we’ve emphasised, we worry most about the relative absence of a well-trained, professional informatics workforce. Some of today’s informatician shortfall reflects an exodus of workers from the healthcare marketplace in the wake of NPfIT. But the problem also reflects a lack of understanding regarding the adaption and optimisation process. Since Go-Live is just the beginning of an organisation’s digital journey, there simply must be adequate and well trained staff to continue (not complete, since that never happens) the journey.
Of particular concern is the need for a cadre of CCIOs and others with both clinical and informatics training. We visited several NHS trusts that had one or, at most, 2 individuals with such backgrounds – and their aggregate time allocated was less than one whole-time equivalent. That is not nearly enough to get this difficult job done well.
Moreover, such individuals are needed to provide support for system improvements – ranging from basic fixes to true innovations. At one trust we visited, a simple problem (the results of point-of-care blood tests could not be entered into the EHR) had gone unaddressed for 18 months, and the doctors and nurses had given up on asking the trust to fix it. These kinds of responses – workarounds and learned helplessness – are predictable if IT systems are created without a deep understanding of the nature of the work, an appreciation of and empathy for the predicament of the workers, and trained staff who can listen to clinicians’ concerns and fix faults in a system.
10. Health IT entails both technical and adaptive change
Harvard political scientist Ronald Heifetz has popularised the paradigm of technical versus adaptive change. Technical change is straightforward: simply follow a recipe or a checklist and the problem will be solved. Adaptive change involves substantial and long-lasting engagement between those implementing the changes and the individuals tasked with making them work. Partly because technology adoption in the rest of our lives has become so easy (think about downloading an app on your smartphone), most observers and stakeholders mistakenly believed that implementing health IT would also be a simple matter of technical change.
In fact, it is one of the most complex adaptive changes in the history of healthcare, and perhaps of any industry.
This means that successful implementation of health IT requires the initial and sustained engagement of front-line users of the technology, whether it is healthcare professionals or patients. It also means that trusts need a robust, well trained, and well supported cadre of experts (CCIOs and others) who understand clinical practice, technology, and change management. These individuals are crucial in promoting the adaptive changes that are needed when an organisation switches from one way of doing work to another.
We have made this point earlier and reemphasise it here because it is our overarching message, the message that weaves together all the threads (24). Even after NPfIT, we do not believe the lessons of adaptive change have been fully learnt, and this may well be the greatest threat to the current efforts to digitise the NHS.
5: Recommendations
Based on our review of the history and current state, and in keeping with our findings and principles articulated above, we offer the following 10 recommendations, followed by our rationale for each of them and, where appropriate, recommended deliverables and an associated timeline (a summary of these deliverables/timeline is in Appendix C:
1. Carry out a thoughtful long-term national engagement strategy
A new national effort to computerise the secondary care sector is likely to generate scepticism from the public, the media, and legislators. Here are 2 predictable questions/concerns:
- Will this be another version of NPfIT?
- Given today’s austerity, how can the NHS afford to computerise?
These concerns must be tackled head on. At the outset, a long-term engagement strategy should be enacted to promote the need for healthcare information technology, identify the likely challenges during implementation, educate stakeholders about the opportunities afforded by a digital NHS, and set the stage for long-term engagement of end users and co-creation of systems and strategies.
The campaign needs to emphasise that the goal is not to ‘go digital’, ‘go paperless’, or even ‘save money’. Instead, digitisation is an essential tool for meeting the needs of patients, their families, healthcare professionals, and the entire nation – in short, to improve the way care is delivered in the NHS.
The campaign should steer clear of slogans and unrealistic promises – authenticity, engagement, and co-creation are essential.
We understand that NPfIT included plans for a similar ‘campaign’, but it failed, largely because such a campaign cannot be imposed from the centre. As Professor Trish Greenhalgh told our group, ‘“Clinical engagement” is more about being listened to than being written to’. Getting this right will require buy-in from trust leaders, engagement of front-line workers, the presence of CCIOs and others who can make the case for IT in clinical (not financial) terms, and a deep appreciation for the adaptive aspects of this new digital strategy.
We are concerned by the absence of a name for this new initiative. We understand the reluctance to attach a label to another ‘national programme’, but even in this report we have found it difficult to describe this new phase in which the NHS is making another effort to digitise the secondary care sector and forge an interoperable system. We recommend that a suitable name be developed to provide some clarity and focus around engagement efforts.
It will be important to generate enthusiasm for the new initiative, yet this should be done with realistic promises and timelines. As one example, we believe that the target of ‘paperless by 2020’ should be discarded as unrealistic. The goal is not paperless – it is improvement, facilitated by having information where it’s needed, when it’s needed. Regarding timing, we have set 2023 as a reasonable goal to have robust clinical information systems[footnote 20] implemented in all NHS trusts, along with a high degree of interoperability. We believe this is ambitious but – with additional funding for our proposed Phase 2 – achievable.
Deliverables and timeline for recommendation 1:
By January 2017:
- create and publicise a name and appropriate branding for the new effort to digitise the NHS
By July 2017:
- create and begin to enact a national campaign to engage clinicians and trust leaders in the new effort to digitise the NHS
2. Appoint and give appropriate authority to a national CCIO
In reviewing today’s NHS organisational chart and meeting with NHS leaders, we were unable to identify any high-level health IT policymakers who have both clinical training/experience and experience/training in health IT. We believe that such a person – a national CCIO – should be identified to oversee and coordinate NHS clinical digitisation efforts. This will signal that the NHS understands the adaptive nature of this effort to change, that it is serious about clinician engagement when it comes to health IT, and that it is putting a premium on clinical, not simply financial, outcomes. Such a person – who will need to have a background in clinical care, informatics, and leadership – should be given appropriate organisational and budgetary authority. Because health IT crosses the domains and budgets of so many NHS organisations, such an individual will assume an important coordinating function, not unlike the National Coordinator for Health IT in the United States.
While a single individual and his/her office can do only so much, we found it both practically and symbolically meaningful that we could not identify any individuals who have ever cared for patients among those who have overall strategic authority for health IT in the NHS. We believe this needs to be remedied[footnote 21].
While it will be important that the individual has a suitable staff, budget and authority, much of the role will be as coordinator and an influencer, and it should be structured accordingly. In the US, the role of the National Coordinator for Health IT was created in 2004; the person in this role reports directly to the cabinet secretary (Secretary of Health and Human Services). In England, we believe that this national CCIO should report directly to the Secretary of State for Health or the NHS England CEO, and serve as chair or co-chair of the multi-stakeholder National Information Board (NIB). He or she needs to be optimally positioned to leverage the informatics capabilities and resources in, amongst others, DH, NHS England, NHS Improvement, NHS Digital, and the Care Quality Commission (CQC). To maximise the return on investment to the UK, it will also be important to work cross-sectorally with the Office for Life Sciences, the Department of Business Innovations and Skills, and other key departments.
Deliverables and timeline for recommendation 2:
Already completed:
- create a job description for, and then hire, a prominent physician-executive with broad experience in information technology, leadership, and change management to become the NHS’s Chief Clinical Information Officer (CCIO)
By January 2017:
- clarify and publicise the national CCIO’s role in leading the digitisation of the NHS, in terms of his or her relationship with NHS England, NHS Digital, NHS Improvement, the National Information Board, and other relevant bodies
3. Develop a workforce of trained clinician-informaticians at the trusts, and give them appropriate resources and authority
There must be a major effort to place well-qualified clinicians with advanced informatics training in every trust. For a large trust, there must be a senior clinician-informatician (chief clinical information officer, or CCIO), reporting at the level of the board or the CEO, whose primary job (>75% time) is to lead and manage the purchase, implementation, and evolution of the clinical information system. Reporting to this person must be a cadre of clinician-informaticians (whose clinical background may be medicine, nursing, or pharmacy, depending on the needs of the unit). To implement and optimise an EHR effectively, trusts must make such individuals available to major clinical areas ( including medicine wards, A&E, surgery and perioperative) and service areas (such as nursing and pharmacy). The Advisory Group estimates that an average-sized trust needs at least 5 such individuals on staff. In considering whether to offer government money to a trust to subsidise digital implementation, close attention should be paid to the adequacy of its plan to hire and support this workforce.
As one experienced CCIO told us about implementing an EHR,
You can’t just do a dump and run… It is transformation, it is a journey.
CCIOs and other informatics and improvement staff are key to this transformation. At one very large trust we visited, there was one part-time CCIO (about 50% time as CCIO) and 4 deputies, each of whom had a half-day per week allocated for their informatics work. In contrast, at UCSF Medical Center, a health system in San Francisco similar in size to the aforementioned trust, there are 15 such individuals, who have a total of 7 whole-time equivalents devoted to their IT work. Even adjusting for the differences in health expenditures between the US and the UK, we find the UK situation to represent a massive underinvestment in individuals with the appropriate skill mix.
Deliverables and timeline for recommendation 3:
By January 2017:
- trusts seeking Phase 1 (2016-2019) national funding for digital implementation/improvement (Groups A and B; defined under recommendation 7: Link national funding to a viable local implementation/improvement plan) must prepare and defend their workforce plans; plans must include a demonstration that the clinician-IT workforce is sufficiently robust to lead successful digitisation within the trust
By 2019:
-
trusts that have received national funding for Phase 1 digital implementation/improvement (Groups A and B) must have in place a CCIO, devoting at least 75% of his or her time to this task, who reports to the board or CEO (for largest trusts, may be to the chief medical officer or equivalent), with sufficient support staff, budget, and authority to lead successful digitisation and benefits realization within the trust
-
average-sized trusts should have approximately 5 individuals on staff with skills in clinical practice (from any discipline, including medicine, nursing, and pharmacy) and information technology; larger and smaller trusts should adjust these numbers proportionally. These individuals should have at least 25% of their time allocated to their IT and related work
4. Strengthen and grow the CCIO field, others trained in clinical care and informatics, and health IT professionals more generally
We see the absence of professional, well-supported CCIOs with appropriate authority and resources as an enormous obstacle to successful deployment and benefits realisation of health IT at the trust level.
Moreover, we believe that the adaptive-change aspects of health IT cannot be managed effectively without such individuals embedded within trusts. To rectify the gap in the availability of such individuals, not only will there need to be satisfying, sustainable positions available to CCIOs in trusts (recommendation 3: Develop a workforce of trained clinician-informaticians at the trusts, and give them appropriate resources and authority), but the CCIO field must also be strengthened and grown. This will involve a major effort by existing professional bodies such as the Royal Colleges, the General Medical Council, and the British Computer Society to create and certify training programmes for clinician-informaticians. It will also require support for the development of vibrant professional societies.
In addition to the CCIOs, the workforce of both clinician and non-clinician informaticians, researchers with expertise in clinical informatics, programme evaluators, and system optimisers (data processers, analysts, quality and safety leads) needs to be increased and nurtured. Without the right people and skills, digitisation will fail, or at least not achieve its full potential.
Given the importance of the workforce to the success of the overall strategy, we recommend an investment in workforce development of £42 million, one percent of the £4.2 billion currently allocated for health IT. Again, some of this is described elsewhere in the report. Moreover, the National Information Board report highlighted, in a general way, the need for a more robust CCIO workforce, and some of this effort has already begun under the NIB’s Domain G (1)[footnote 22]. Finally, we acknowledge a proposal for the creation of a Faculty of Clinical Informatics, which may help address the issues of certification and professionalisation (2).
To inform our group’s work, the CCIO Network undertook a survey of its members in early 2016. One hundred members completed the survey, 64% from acute care trusts. While nearly two-thirds had been clinicians for more than 20 years, less than 20% had been in their CCIO roles for more than 5 years.
Confirming our impressions, about half of the respondents spend one day per week or less on their CCIO role, and most organisations have only 1 or 2 clinician-informatics experts with dedicated time for this role. 76% of respondents disagreed or strongly disagreed with the statement, ‘We have enough trained clinicians in health IT and informatics to maximise the potential of our systems’ (Table 4). Three comments from the CCIO survey help illustrate the problems:
My authority comes from my clinical and technical expertise rather than directly as a consequence of the title and position in trust hierarchy. Not holding any budget or having anyone report to me leaves me somewhat as an advisor rather than leader.
Yes – [need] some training to bring all CCIOs up to a level. Yes, needs national recognition that this is really important for an NHS to be fit for 21st Century. My organisation feels a CCIO is a ‘nice to have’, not a mandatory role that requires time, resource and investment.
Huge opportunities and risks. As full time clinician NHS is not releasing me enough to maximise my contribution to this. Difficult job to do ‘winging it’. Too important. But clinical credibility is key too, the balance needs to be better though.
CCIOs were presented with these statements and were asked to rate their agreement with them on a 5-point scale.
Table 4: Responses from the 2016 CCIO Network survey
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |
|---|---|---|---|---|---|
| We have enough trained clinicians in health IT and Informatics to maximise the potential of our systems (configuration/ workflow/ setup) | 3 | 5 | 9 | 35 | 19 |
| Clinicians are given dedicated time to support implementation | 4 | 7 | 15 | 27 | 13 |
| We have (or have access to) high calibre technical staff to support implementation decisions | 6 | 29 | 16 | 14 | 2 |
| There is a good working relationship between clinical staff and IT staff | 7 | 34 | 17 | 7 | 2 |
| The non-clinical members of the team have a good understanding of clinical workflow | 2 | 21 | 22 | 17 | 5 |
| We have enough project management support | 6 | 16 | 18 | 23 | 7 |
| We have well developed change management skills and techniques | 1 | 19 | 24 | 16 | 8 |
| We have well developed clinical engagement methodologies | 3 | 21 | 25 | 13 | 7 |
| We are well resourced to ensure successful and time deployment of our IT implementations | 1 | 9 | 17 | 24 | 18 |
We emphasise the interdependence of Recommendations 3 and 4: without the availability of high level CCIO jobs in trusts (reporting at the board or CEO level, significant budget and staff, highly respected in the organisation) and a sustainable career track, few talented individuals will choose to leave the full-time practice of clinical medicine, nursing or pharmacy to obtain additional training and certification in informatics, and few students will choose this hybrid path as a career choice. And even those who do choose to pursue careers in health IT will find more attractive positions in the private sector.
But even if appropriate roles for CCIOs and other clinician-IT experts became available in many trusts, there are not enough individuals with such training in the UK to fill these roles. Both of these issues – supply and demand – need to be addressed simultaneously. There must also be other well-trained workers, with a wide array of IT-related skills, to round out the team.
In particular, the data processing, analytics, and informatics research workforce must not be forgotten, particularly since the UK has an enormous opportunity to bring the promise of big data to life. Working through ambitious entities such as the Farr Institute, the UK could be the first nation to take data science to scale and build a truly national learning health system (3, 4, 5). The combination of a cradle-to-grave patient record (mostly digitised) collected for clinical (not billing) purposes, the NHS number, and a secure NHS network (the Spine) is unique and should be much better exploited for patient, population, and societal gains.
Two other points about the workforce are worth making. First, all healthcare professionals will be practicing in a digital environment for the rest of their careers. Therefore, all of them should receive foundational training in informatics, and – probably more importantly – in the integration of digital tools into their practices (6). Such training should begin relatively early in professional education.
Second, the NHS needs to train national leaders in informatics – and not just CCIOs. We have been impressed with the results of the NHS’s National Medical Directors Clinical Fellow Scheme, which embeds junior doctors in large policy-relevant organisations (such as NHS England or the National Institute for Health and Care Excellence [NICE]) for year-long apprenticeships (7). We believe that the creation of several slots each year for individuals with an interest in clinical informatics – embedded in trusts, in national IT-related organisations, or even with commercial IT suppliers) would be an excellent investment.
Developing this workforce will require a significant investment. In the US, under the 2009 HITECH Act, $118 million was allocated to workforce development (8). Adjusting for inflation, the relative size of the US and English health systems, the private investment available in the US to augment the government allocation, and the fact that the UK’s IT-related workforce is less developed than America’s was in 2009, we believe that an allocation of £42 million – representing one percent of the £4.2 billion current investment in health IT – for workforce development is needed.
Deliverables and timeline for recommendation 4:
By January 2017:
- confirm allocation of approximately £42 million (1% of the £4.2 billion to be spent on digitising the NHS) to support workforce development and deployment.
By December 2017:
- establish and launch a programme designed to rapidly train CCIOs, CIOs, and other healthcare informaticians in executive leadership and informatics. The first few “classes” in this intensive 6-12 month training program should focus on training individual who will work at the trusts in Groups A and B.
- the Faculty of Clinical Informatics, working closely with the British Computer Society and the Royal Colleges, should launch an accreditation and professionalisation agenda designed, ultimately, to certify and professionalise the CCIO workforce.
- NHS England and other UK bodies should establish a partnership with relevant international partners (including leading international training programmes and informatics certifying organisations) to help inform UK workforce development efforts
- NHS England should complete and begin to implement a workforce plan designed to grow other segments of IT-related workforce, including clinician and non-clinician informaticians, researchers with expertise in clinical informatics, programme evaluators, and system optimisers (such as data processers, analysts, quality and safety leads)
- Health Education England, in collaboration with the Royal Colleges and other relevant bodies, should develop and begin to implement a plan to raise the level of digital education in all health professional educational settings, including medical, nursing and pharmacy schools, and in continuing education settings for practicing healthcare professionals.
By 2019:
The Faculty of Clinical Informatics, working closely with the British Computer Society and the Royal Colleges, should complete the training and certification of at least 100 new graduates of CCIO training programmes in the UK. At least 80% of these professionals should take positions in trusts or other NHS healthcare delivery organisations.
5. Allocate the new national funding to help trusts go digital and achieve maximum benefit from digitisation
Given the upfront costs of switching from analog to digital (tens of millions of pounds for a mid-sized trust, still more for a large one), new investments are required to promote digitisation across the secondary care sector. We applaud the DH and the Treasury for making available £4.2 billion (approximately one-third of which is for IT system purchases and implementation support) to promote digitisation. Given the challenging financial state of many trusts, secondary care digitisation would have been impossible without new central resources.
While welcome, this level of funding is likely not enough to enable digital implementation and optimisation in all NHS trusts. Therefore, we suggest a phased approach. During Phase 1 (2016-2019), national funding should be combined with local resources to support implementation in trusts that are prepared to digitise, and to support those that are already digitised and are ready to take the next step. We believe that another tranche of government funding (not yet allocated) will likely be needed to support a second stage (Phase 2, 2020-2023) of the strategy, as described under recommendation 6: While some trusts may need time to prepare to go digital, all trusts should be largely digitised by 2023.
We have described our rationale for this under finding 2: It is better to get digitisation right than to do it quickly. For deliverables and timeline, see under recommendation 7: Link national funding to a viable local implementation/improvement plan.
6. While some trusts may need time to prepare to go digital, all trusts should be largely digitised by 2023
It would be reasonable to expect all trusts to have achieved a high degree of digital maturity by 2023. National subsidies should be offered in 2 phases, giving trusts that are already digitally advanced the chance to become even better, trusts that are ready to digitise the chance to do so, and trusts that need time to prepare for their digital journey the opportunity to do so before starting. We also recommend that this staged approach be bundled with an independent evaluation plan to ensure that lessons learnt at each stage help inform subsequent stages.
This staged approach must not be an invitation for the leaders of trusts in the third (Group C, ‘not ready’) category to procrastinate. We favour 2023 as the year after which no more government subsidies will be available, and after which regulators will begin to deem trusts that have not reached a high level of digital maturity to be out of compliance on quality and safety grounds, or simply unable to meet heightened clinical performance standards linked to payments. This combination of subsidy payments available in stages over the next few years, an explicit end date for the availability of such funds, and regulatory or financial penalties for failure to digitise by 2023 will promote the movement towards a digital NHS at a pace that is fast enough, but not too fast.
We have described the rationale for this approach earlier. We understand that there are no current plans for the second tranche of resources.
But (depending on the state of the NHS and the overall economy), we believe that it is better to have a successful first phase and petition for the needed resources than to have a failed strategy because the limited resources were stretched too thin over too little time.
NPfIT led to a significant loss of trust – trust that digitisation of the NHS was wise, trust that the NHS could pull it off, trust that the money would not be wasted (9). Phase 1 of the new IT strategy must be designed to reestablish that trust.
The issue of regulatory requirements for digitisation merits some discussion. The Care Quality Commission (CQC) is charged with ensuring that health and social care organisations meet fundamental standards of quality and safety. While the CQC might choose to require a high level of digital maturity as a quality standard, we favour standards that link back to purpose; namely, to provide better, safer, less expensive care (see finding 1: Digitise for the Correct Reasons). In other words, we encourage the CQC to create care standards that are clinically meaningful and are progressively easier to achieve with good digital systems and processes. Importantly, this strategy mirrors what happened in the GP sector: rather than requiring that all GPs use EHRs, GPs found it impossible to run their practices and meet the reporting requirements of the Quality Outcomes Framework if they were still using paper records (further described in the background section) (10).
For deliverables and timeline, see under recommendation 7: Link national funding to a viable local implementation/improvement plan).
7. Link national funding to a viable local implementation/improvement plan
The availability of public money to support digitisation should be linked to:
- a parallel investment from each trust, based in part on ability to pay (that is, buying and installing a new clinical information system should be a shared investment between trusts and NHS England[footnote 23])
- the approval by the NHS of a plan that demonstrates that the trust is adequately prepared to succeed in both digitisation and in promoting regional interoperability
- a description of the return on investment expected (framed in terms of clinical outcomes, service delivery, and financial outcomes)
- ongoing accountability that the money was well spent (such as through penalties for failure to deliver under reasonable timescales or a threat of loss of further funding)
- evaluation of progress made
Recognising that levels of digital maturity (and, for those trusts that have not yet gone digital, digital readiness) vary widely across England’s acute trusts, we recommend that Phase 1 funding targeted at implementation be allocated to trusts via 3 major categories:
Group A
Funding to trusts that have already achieved moderate or high levels of digital maturity. These trusts are likely to develop important innovations, to inspire other trusts to digitise, and to help anchor local health IT learning networks (recommendation 8: Organise digital learning networks to support implementation and improvement). Trusts in this category that receive funding will also be required to ‘pay it forward’, helping the next generation of trusts digitise by sharing learning and expertise and, where appropriate, computer code, decision-support tools, and apps. We estimate that approximately 12 to 15 trusts will fall into Group A. To promote shared learning, we favour the creation of a consortium – a learning network – of these trusts, with the aspiration that they become digitally superb. It would be worth thinking about partnering this network with a US or other non-UK organisation that has a world-class health IT system and strong culture of education and collaboration.
Group B
Funding to trusts that are currently digitally immature but are able to demonstrate sufficient readiness to begin implementing clinical information systems. This funding should not only support the purchasing of software licenses, hardware, and infrastructure improvements, but should also support workforce development, training, and participation in regional health IT learning networks. We estimate that approximately one in 3 NHS trusts will fall into Group B.
Group C
Smaller amounts of funding to trusts that are not yet prepared to digitise. This funding should not be for the implementation of robust clinical information systems in 2016 to 2019. Instead, it should be designed to help these trusts build capacity before they are mandated to implement clinical information systems in 2020-2023. (Some may choose to implement focused IT systems, such as ePrescribing, with their limited Phase 1 funding). The regional learning networks should help these trusts in their preparations and should, where appropriate, temporarily send relevant staff to more advanced organisations so they can shadow and learn. The proposed Phase 2 national funding will be needed to support this group’s digitisation in 2020 to 2023. We estimate that approximately half of the acute trusts will fall into this category.
Group D
Trusts that are reasonably far along but are not ready to advance. These trusts should receive no or minimal new funding during Phase 1. We anticipate that relatively few trusts will be in this category.
Our approach is summarised in Table 5.
Table 5: Categorising trusts’ readiness to advance and current state of digitisation
| Ready to advance | Not ready to advance | |
|---|---|---|
| Digital Now | Early Adopter (Group A) provide moderate funding to achieve even higher state, serve as role model, and teach others. Consider creation of a consortium of members of this group to promote shared learning. | Stable (Group D) provide no or minimal funding to help advance to next stage. Expect higher level of digital maturity over next 3 to 6 years |
| Not Yet Digital | Ready to Launch (Group B) provide substantial funding to buy system, train, Go-Live and support early enhancement. Expect reasonable digital maturity by 2020 | Not Ready (Group C) provide modest funding to improve readiness, with hope of digital launch (with additional funding) around 2020; expect high level of digital maturity by 2023 |
This may be one of the more challenging recommendations to meet, but we see it as one of the most important. The information gathered through the digital maturity index surveys (Figure 2 and Appendix E) is helpful in this regard, but does not fully deliver what we believe is needed – both because it is gleaned through self-report (and thus subject to gaming) and because it doesn’t fully explicate whether an organisation is truly ready to digitise successfully. Rather, it looks at how far along the organisation is – a related, but not identical, concept. It will be important to develop new tools to determine which of these categories each trust falls into, being thoughtful about which NHS organisation should undertake this important sorting task. Whatever is determined regarding the latter point, the new NHS CCIO (recommendation 2: Appoint and give appropriate authority to a national CCIO) should take a leading role in this process.
This sorting of trusts is important because it determines how much central funding they should receive and what the funding should be used for. Just as it would be a mistake to give precious implementation funding to a Group C (not ready) trust, it would be a mistake to give that trust no support since some funds will be needed to prepare it for digitisation. And the Group A cohort – the early adopters – need very specific support, earmarked both to make them better and to engage them in helping others. They may even benefit from a competition for resources – based on proposals that illustrate innovative new uses of their IT capacity.
It is worth noting that, while there are examples of trusts that have reasonably high levels of digital maturity, on an international stage, none would be considered digitally superb currently, in terms of their levels of IT use, innovation, integration, education, and research. However, given the unique assets of the NHS, there is no reason that members of this group cannot become world class, and we favour a significant investment that might allow them to become exemplars. The investment would need to include workforce development, support for analytics, and more. We also favour the creation of a consortium of these trusts, and perhaps linking them to a highly advanced (from an IT perspective) international health system that can serve as a partner and mentor. A similar relationship in the areas of quality, patient safety and innovation was forged in 2015 between 5 NHS trusts and a leading US hospital, and is reportedly working well (11).
However the groups are chosen, all of this must begin with an accurate determination of current status, a body of work that will require significant investment and analysis. Similar to the situation with procurement contracts (When it Comes to Centralisation, the NHS Should Learn, but not Over-Learn, the Lessons of NPfIT ), the NHS Tech Fund allocated its funds based on a tool designed to assess organisational readiness and clinical engagement (12). This experience should be reviewed to help inform the process of selecting trusts to receive national funds for EHR adoption. The NHS should work hard to make this process as streamlined as possible for trusts, limiting the amount of information to be submitted to only that which is necessary for the determination of eligibility and readiness.
Deliverables and timeline for recommendations 5 to 7:
By December 2016:
-
NHS England should announce a detailed plan for how it will allocate the £4.2 billion devoted to digitisation, with specific attention to how much will go to trusts to support purchase of software and IT implementation, how much will be allocated to infrastructure improvement, how much will support workforce development, and so on. The plans should include the relative distribution of resources to the 3 categories of trusts (Groups A, B, and C) described under recommendation 7: Link national funding to a viable local implementation/improvement plan)
-
the national CCIO should develop and then disseminate the methods by which trusts will be sorted into groups A, B and C
By January 2017:
- NHS England should approve plans and distribute resources to enable digitisation in Group A, including the expectation of shared funding (central funding combined with funding from the trusts themselves) - we applaud early plans to designate up to12 leading trusts as NHS Centres of Global Digital Excellence
- NHS England should finalise plans for these Centres, including timelines and deliverables
- NHS England should approve a plan for an international partnership to work closely with the NHS Centres of Global Digital Excellence, to help the Centres reach the goals of being world-class leaders in healthcare digitisation and exemplars for the rest of the NHS
By April 2017:
- NHS England should approve plans and distribute resources to enable digitisation in Group B trusts, including the expectation of shared funding (central funding combined with funding from the trusts themselves)
- NHS England should finalise plans for these Centres, including timelines and deliverables
By December 2018:
-
all trusts receiving funding in Phase 1 (Groups A and B) should report on progress. Eligibility for additional funding should be approved by the NHS, based on the progress to date
- specifically, the Centres of Global Digital Excellence (Group A) should be assessed on the following deliverables:
- achieving high levels of staff engagement
- deployment of and support for appropriate workforce within the trust (including IT professionals)
- digitisation of all key processes of care and integration of all key clinical and administrative systems (both within the trust as well as with national systems such as PACS, eReferrals and Electronic Prescribing)
- Substantial use of the electronic patient record to improve care through decision support and practice redesign
- information sharing with patients via patient portals, ability of patients to download key data, and integration with third party apps (including patient-facing apps) through open APIs
- leading efforts to promote digitisation within region, including supporting other trusts
- leading efforts to achieve regional interoperability
- constructive engagement with international partner(s)
- implementation of robust privacy and security standards
By 2019:
- NHS England and the national CCIO should identify and announce plans for funding and supporting those trusts that did not participate in initial digitisation efforts (Group C), including plans for dealing with any trusts that still cannot demonstrate readiness to digitise
By 2020:
- launch of Phase 2, with concrete plans to digitise Group C, and to continue improvements in Group A and B (will likely require additional central resources)
By 2023:
- national funding for trust digitisation ends, accompanied by an expectation that the entire NHS is digitised
- The Care Quality Commission should implement a plan to assess the digital status of trusts (including digital maturity and use of digitisation to promote care improvement), and to deem those that are not sufficiently digitally mature as out of compliance on quality/safety grounds
8. Organise digital learning networks to support implementation and improvement
To support purchasing, implementation, and ongoing improvements by trusts, digital learning networks should be created or supported. Some regions already have such networks, sometimes anchored by a trust with a high level of digital maturity. While some support might take the form of offering help in choosing a supplier, once a trust chooses a given EHR product it may wish to take advantage of a supplier-specific user network, since many of the issues are specific to each product. Such networks should also be encouraged and nurtured. A national effort, led by the new national CCIO, would help ensure that lessons are spread, but the primary point of contact for a given trust should be its local or regional network.
The networks would link to the 3 categories of trusts (recommendation 7) in the following way:
- Organisations ready to begin digitising (Group B) would take advantage of the digital learning networks to guide their choice of EHR system, their contracting, and their early implementation work.
- Organisations already at an advanced stage of digitisation (Group A) would be expected to help lead these networks, while also learning from others regarding optimisation. In addition, we favour the creation of a consortium of some or all of the Group A trusts to accelerate their own progress (recommendation 7: Link national funding to a viable local implementation/improvement plan).
- Organisations deemed not ready to digitise today (Group C, the group slated to digitise in Phase 2, 2020 to 2023) would use the networks to help prepare themselves for successful digitisation.
Here, it seems worthwhile to point to some existing models, such as the one in Trafford and others in London, Salford, and a few other regions.
Case study: Trafford Clinical Commissioning Group
In keeping with the NHS’s Five Year Forward View, the Trafford Clinical Commissioning Group (CCG) has built an integrated system that illustrates patient-centered care at its most effective.
After 4 years of developing a plan for addressing the growing need for better communication and integration across different health sectors, in early 2015, Trafford signed a 15-million-pound contract with IT-services vendor CSC to build a ‘Patient Care Co-ordination Centre’. The Centre went fully live in January 2016.
‘The question was, “Can we use the technologies to really understand our patients and to really understand what coordination looks like?”’ said Gina Lawrence, chief operating officer of Trafford CCG.
Trafford is a largely urban area with a population of some 237,000 people. Lawrence said the goal from the start was to trim waste and maximise efficiency by wrapping clinical services around people, looking at trends and population data within care pathways to determine the true demands on the system.
At the outset, the biggest challenge facing the project was the wide range of IT systems and infrastructure used by providers in the Trafford area, as well as the need for cultural change among healthcare professionals. Lawrence said that a great deal of outside-the-box thinking had to happen in order to make it work. ‘CSC is a big firm, very different from the NHS. Even our language was different,’ she said. ‘So we had to do a lot of training, not just training to understand the system, but training to work together culturally’.
Lawrence said her CCG decided to create a single IT system in order to understand everything from a uniform perspective. All GPs were moved onto a single IT system, as were community services, matrons and the acute trusts. The system is also integrated with social care.
The design called for a clinical team to sit in the Centre – a group of about 8 nurses, and 15 administrators who work with on the ‘onboarding’ of patients, determine a patient’s needs, follow through on referrals, and order tests. Community matrons then pick up and manage the individual cases. The idea, Lawrence said, is to ensure that people are moving in the system in the right way at the right time to the right place.
One theoretical example, Lawrence said, would be an older woman who visits her GP, and is told to have a battery of tests. The Care Coordination Centre gets involved immediately. The Centre sees that she has carers going in, and they have access to the carers’ schedule. The patient is flagged in the system as she moves through it. The Centre make certain the patient gets to appointments on time, and can continue to profile her to see what else is happening. If she deteriorates and goes to the A&E department, the system is alerted and the level of intervention can be determined. The Centre can do everything from booking transportation to ordering equipment. Once she is home, the Centre calls to check in with her.
Unfortunately, there is as yet no sophisticated digital connection between hospitals and GP’s at Trafford. When a patient is admitted to a hospital, or has visited the A&E, the system is alerted. The clinical summary of the visit is then transmitted to the patient’s GP either by post or fax, then scanned into the system.
Approximately 10,000 people are currently in the system. Lawrence expects that eventually all 240,00 Trafford resident will be in it. The next project, Lawrence said, is a patient portal, to allow patients to see their entire medical record.
If Lawrence has any advice to dispense to other regions seeking to build a fully integrated system, it is this: Don’t rush. ‘You have to build it bit by bit,’ she said. ‘This is a huge system change, and it takes time’.
During the implementation of HITECH in the US, significant funding was given to help create a network of regional extension centers that provided support to practices that were implementing health IT systems (13). (It is worth noting that much of this help went to small office practices [the equivalent of GP surgeries], since HITECH aimed to digitise both offices and hospitals. In the current NHS effort, the centres would be orientated to helping trusts with their digitisation.) The development and operations of such regional networks may require some national funding.
Once a trust has chosen a supplier, in addition to general help with contracting, implementation and optimisation, it may need advice on how to work with that supplier and its product. While there may be regions with enough volume for a supplier to create product-specific regional networks, we suspect that these supplier-orientated networks are more likely to be national, or even international. For example, there is already an active Cerner network in the UK, and active Epic, Cerner, Athena, and other vendor-specific networks in the US.
In some cases, trusts may want support in working on certain problems, such as the management of sepsis or the discharge process. Here, while IT-specific networks may emerge, it is possible such needs may be better served through the network of CLAHRCs (Collaboration for Leadership in Applied Health Research and Care), or through one of the Academic Health Science Networks (AHSNs). The NHS may wish to establish a fund to allow various types of support networks to compete for resources; this would encourage different networks to form around clearly articulated needs of trusts.
Deliverables and timeline for recommendation 8:
By July 2017:
- NHS England and NHS Digital should approve plans to promote regional learning and improvement within every region in England. These plans should identify the role of the Centres of Global Digital Excellence in helping other trusts go digital, in building regional interoperability, and in linking the region’s IT strategy to its STP and Vanguards programmes.
9. Ensure interoperability as a core characteristic of NHS Digital ecosystem – to support clinical care and to promote innovation and research
The new effort to digitise the NHS should ensure widespread interoperability. The goals of interoperability are not merely to create the technical capability to exchange digital data. Rather, interoperability needs to enable integrated workflow, service redesign, and clinical decision support. It also needs to support seamless care delivery across traditional organisational boundaries, and ensure that patients can access all parts of their clinical record and, over time, contribute to it. Finally, the roadmap for interoperability must include plans to use connected health records to inform population health management and analytics.
The further development of a governance and regulatory framework for data sharing should be a key priority[footnote 24]. It should be guided by participatory principles, so that those affected – patients and their families, professionals, managers, and academics – have a voice in its design and implementation. This framework should bring together a mixture of system levers, incentives, and technical solutions in order to meet the key goals. This approach has already begun to bear fruit. For example, there are now penalties in place for failure to use the NHS number in general practice, and over 70% of acute trusts are now sharing most of their discharge summaries electronically.
Interoperability should, at the very least, allow for easy movement and use of clinical and operational data through all sectors of the healthcare delivery system (GPs, secondary care, social care). The process of standards development to enable interoperability should be prioritised by clinical need, built on widely accepted open international standards, and done in close collaboration with the supplier community. The system, standards, and interfaces should enable a mixed ecosystem of information system providers to flourish, with the goal of promoting innovation and avoiding ‘vendor-lock’. It is important to allow for the inclusion of large EHR suppliers, of course, but also of smaller firms with products orientated to solving more specific problems, including patient-facing ones.
We favour the Institute of Electrical and Electronics Engineers’ (IEEE) definition of interoperability: the ability of systems to exchange and use electronic health information from other systems without special effort on the part of the user (14). Interoperability is a rapidly evolving field. Technical standards are changing quickly, as are the political and business pressures that promote data sharing. In certain cases, the key to interoperability will be a technical requirement, such as a requirement that EHRs provide open APIs (application-programme interfaces) to allow suitable products from third parties to interface correctly. (NHS already requires the use of SNOMED-CT as a standard terminology.) In other cases, the solutions may lie more in business or organisational arrangements and incentives.
The goals, in the end, are crucial, and here we would encourage a stretch goal: interoperability of key data elements within regions by 2020. Rather than trying to do everything, it is worth focusing on regional (not national) interoperability of key data elements, and for specific use cases (such as hospital discharge to GP, or consultant-to-GP communication) (15). The Code 4 Health Interoperability Community has taken this approach (supported by the new INTEROPen supplier community), and seems to be making good progress. The Professional Record Standards Body (PRSB) also plays a key role here, by bringing together the Royal Colleges and suppliers to develop and endorse data standards. Even with a relatively decentralised approach to standards development, it will be important for the centre to monitor and guide this activity to prevent wheel reinvention.
Importantly, data sharing should also support research. For example, one can envision a single point of entry to NHS England’s data, which is made available to researchers and others working on problems deemed high priority by NHS and the Department of Health.
Deliverables and timeline for recommendation 9:
By July 2017:
- NHS England and NHS Digital should announce a multi-pronged plan to ensure regional interoperability (including GPs, trusts, and social care systems), to be implemented no later than 2020
By 2020:
- complete regional interoperability should be established, so the medical records freely flow with a region, with appropriate privacy and security safeguards
By 2022:
- complete national interoperability should be established, so that records can flow freely across entire NHS, with appropriate privacy and security safeguards
10. A robust independent evaluation of the programme should be supported and acted upon
We have argued that individual trusts need to build capacity to continuously learn as they attempt to implement and optimise their health IT systems. Underinvestment in the people and processes needed for such a learning system markedly increases the risk for failure.
The same is true at the national level in the context of launching a new strategy to digitise the secondary care sector and create interoperability. The case for independent programme evaluation was made in a 2014 paper by Sheikh and colleagues (16):
Lessons from evaluations of NPfIT demonstrate why it is essential that countries embarking on major healthcare information initiatives build an objective body of evidence to inform policy and practice on how best to successfully design and deliver… national HIT programmes. Such evaluations are also essential to provide clear accountability for investments that use scarce taxpayer resources.
In light of the likelihood of unanticipated consequences, the high cost of digitisation, and the chequered history of similar efforts in the past, we believe that the NHS should commission and help fund independent evaluations of the new strategy.
The evaluations should be both formative (conducted and reported as the strategy is progressing) and summative (reporting at the ends of both Phase 1, in 2019, and Phase 2, in 2023). The evaluations should be conducted by a broadly representative group and led by individuals with a strong track record in programme evaluation. They should utilise multiple modalities (data analysis, site visits, interviews, ethnographic methods), and be insulated from political influence and pressure. As Sheikh notes, such insulation is critical since ‘policymakers find that the results [of independent evaluations] often reveal inconvenient truths’.
In the US the adoption of health IT has resulted in growing rates of clinician (particularly physician) dissatisfaction and burnout, in part because of increasing administrative burdens and challenges to efficiency. Therefore, programme evaluations should also consider the impact of digitisation on the satisfaction of healthcare professionals. Moreover, such satisfaction should be added to the list of metrics that trust leaders are evaluated on. Finally, research on the link between digitisation and workforce satisfaction – including studies of human factors, workforce training, and IT usability – should be supported.
There simply must be a robust evaluation plan – one that is adequately resourced and insulated from political pressure, and whose results are fed back into the system to allow for iterative improvements and mid-course corrections. Even with all of the background wisdom born of prior experiences in the UK and elsewhere, the chances of getting it perfectly right at the start are low. On the other hand, the chances of having gotten it right at the end are high… if the system remains flexible and if people and organisations are open to learning from experience.
Deliverables and timeline for recommendation 10:
By late 2017:
- National Institute for Health Research (NIHR) should commission a formative evaluation of the digitisation programme by a respected academic leader/centre - the report should be published by mid-2018 to allow for mid-course corrections
By 2020:
- final evaluation of Phase 1 efforts should be delivered by same academic leader/centre
By 2023:
- final evaluation of Phase 2 efforts should be delivered by same academic leader/centre
6: Conclusion
We believe that the NHS is ready to implement a successful national strategy to digitise the secondary care sector, and to create a digital and interoperable healthcare system. By using national incentives strategically, balancing limited centralisation with an emphasis on local and regional control, building and empowering the appropriate workforce, creating a timeline that stages implementation based on organisational readiness, and learning from past successes and failures as well as from real-time experience, this effort will create the infrastructure and culture to allow the NHS to provide healthcare that is of high quality, safe, satisfying, accessible, and affordable.
We cannot emphasise enough that the purpose here is not to computerise, nor to go paperless (though when the change is complete, there will be little paper). The purpose is to radically improve the chances that important information will be available when and where it is needed, because no health system or clinician can perform at the top of their potential if it is not. In light of this purpose, the question quickly becomes: how do we do that? The experience of industry after industry has demonstrated that just installing computers without altering the work does not allow the system and its people to reach this potential; in fact, technology can sometimes get in the way.
Getting it right requires a new approach, one that may appear paradoxical yet is ultimately obvious: digitising effectively is not simply about the technology, it is mostly about the people. We have emphasised that approach in this report.
To those who wonder whether the NHS can afford an ambitious effort to digitise in today’s environment of austerity and a myriad of ongoing challenges, we believe the answer is clear: the one thing that NHS cannot afford to do is to remain a largely non-digital system. It is time to get on with IT.
References
References are numbered and listed by each section. There are no references for section 3.
Introduction (section 1)
- Davis K, Stremikis K, Schoen C, Squires D. Mirror, Mirror on the Wall, 2014 Update: How the U.S. Health Care System Compares Internationally. The Commonwealth Fund, June 2014.
- Ham C. The Fourth Whitehall Lecture: What Needs to Be Done to Secure the Future of the NHS? 7 April 2016.
- Berwick D. Quality Improvement in the NHS. The King’s Fund, 23 Feb 2016.
- National Health Service. Five Year Forward View. October 2014.
- Campion-Awaad O et al, 2014. The National Programme for IT in the NHS – A Case History, University of Cambridge - accessed January 5th 2016
- National Information Board. Personalised Health and Care: A Framework for Action 2020. 2004
Background (section 2)
- Brynjolfsson E. The productivity paradox of information technology. Communications of the ACM 1993; 36:66–77.
- Solow RM, review of Manufacturing Matters: The Myth of the Post-Industrial Economy, by Cohen S and Zysman J. New York Times Book Review, July 12, 1987.
- Heifetz R, Laurie DL. The work of leadership. Harvard Business Review, December 2001.
- Linsky M, Heifetz R. Leadership on the Line: Staying Alive Through the Dangers of Leading. Cambridge, MA: Harvard Business Review Press, 2002.
- Brynjolfsson E, Hitt LM. Beyond the productivity paradox: computers are the catalyst for bigger changes. Communications of the ACM 1998; 41:49–55.
- Coiera E. Lessons from the NHS National Programme for IT. MJA 2007; 186(1): 3-4.
- Majors Project Authority. 2011. Programme assessment review of the National Programme for IT - accessed January 5th 2016
- Maughan A. 2010. Six reasons why the NHS National Programme for IT failed - accessed January 4th 2016.
- Campion-Awaad O et al, 2014. The National Programme for IT in the NHS – A Case History. University of Cambridge - accessed January 5th 2016
- National Audit Office, 2011. The National Programme for IT in the NHS: an update on the delivery of detailed care records systems - accessed January 4th 2016.
- House of Commons Committee of Public Accounts, 2013. The dismantled National Programme for IT in the NHS, Nineteenth Report of the Session 2013-14 - accessed January 4th 2016.
- Select Committee on Health, 2007. Sixth Report. House of Commons – accessed January 5th 2016.
- HSCIC – The Spine - accessed January 7th 2016.
- RCGP. The 2022 GP: A vision for general practice in the future NHS: Royal College of General Practitioners, 2013.
- HSCIC. More than 1 billion prescription items dispensed in a year - or 1,900 a minute. Secondary More than 1 billion prescription items dispensed in a year - or 1,900 a minute 2013.
- Bouamrane MM, Mair FS. A study of general practitioners’ perspectives on electronic medical records systems in NHSScotland. BMC Medical Informatics and decision making 2013;13:58.
- Bradshaw-Smith JH. A computer record-keeping system for general practice. British Medical Journal 1976; 1:1395-7.
- Benson T. Why general practitioners use computers and hospital doctors do not–Part 1: incentives. BMJ 2002;325:1086-9.
- HSCIC. GP Systems of Choice. Secondary GP Systems of Choice 2015.
- Silcock J, Ratcliffe J. The 1990 GP contract–meeting needs? Health Policy 1996;36(2):199-207.
- HSCIC. QOF 2014/15 Results. Secondary QOF 2014/15 Results 2015.
- The Clinical Practice Research Datalink
- Hippisley-Cox J, Coupland C, Brindle P. The performance of seven QPrediction risk scores in an independent external sample of patients from general practice: a validation study. BMJ Open 2014 Aug 28;4(8):e005809. doi:10.1136/bmjopen-2014-005809.
- Dunhill L. Care.data to restart this month. Secondary Care.data to restart this month 2015.
- Matthews-King A. GPs held responsible for patient complaints over NHS data-sharing project, says ICO. Pulse 2014.
- HSCIC. Summary Care Records. Secondary Summary Care Records 2015.
- Employers N, BMA, England N. 2015/16 General Medical Services (GMS) contract, 2015.
- Holroyd-Leduc JM, Lorenzetti D, Straus SE, et al. The impact of the electronic medical record on structure, process, and outcomes within primary care: a systematic review of the evidence. Journal of the American Medical Informatics Association : JAMIA 2011;18(6):732-7.
- Schade CP, Sullivan FM, de Lusignan S, et al. e-Prescribing, efficiency, quality: lessons from the computerization of UK family practice. Journal of the American Medical Informatics Association: JAMIA 2006;13(5):470-5.
- O’Malley AS, Grossman JM, Cohen GR, et al. Are electronic medical records helpful for care coordination? Experiences of physician practices. Journal of general internal medicine 2010;25(3):177-85.
- Friedberg MW, Chen PG, Pitchforth E, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. Santa Monica, CA: RAND Corporation, 2013.
- Ridsdale L, Hudd S. Computers in the consultation: the patient’s view. The British journal of general practice : the journal of the Royal College of General Practitioners 1994;44(385):367-9.
- Wachter RM. The Digital Doctor: Hope, Hype, and Harm at the Dawn of Medicine’s Computer Age. New York: McGraw-Hill, 2015.
- Blumenthal D. Launching HITECH. N Engl J Med 2015; 362:382–385.
- Adler-Milstein J, DesRoches CM, Kralovec P, et al. Electronic health record adoption In US hospitals: progress continues, but challenges persist. Health Aff (Millwood) 2015; 34:2174-80.
- Delbanco T, Walker J, Bell SK, et al. Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med 2012; 157:461-70.
- Meaningful Use Opens Up Its Deep End: With Some Providers Still Dipping Toes, CMS has Opened up its Health IT Program’s More Challenging Deep End with Stage 2
- CMS chief vows to replace meaningful use with better policy. AMA Wire 13 January, 2016.
- Report on Health Information Blocking. Report to Congress, April 2015. Prepared by the Office of the National Coordinator for Health IT.
- Miller RH, Miller BS. The Santa Barbara Country Care Data Exchange: what happened? Health Affairs 2007; 26:w568-580.
- Schiff GD, Amato MG, Eguale T, et al. Computerized physician order entry-related medication errors: analysis of reported errors and vulnerability testing of current systems. BMJ Qual & Safety 2015; 24: 264-71.
- Drew BJ, Harris P, Zègre-Hemsey JK, et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive intensive care unit patients. PLoS One 2014; 9:e110274.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015; 90:1600-13.
- Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Santa Monica, CA: RAND Corporation 2013.
- Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Affairs 2005; 24:1103–1117.
- Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: An updated systematic review with a focus on Meaningful Use. Ann Intern Med 2014; 160:48-54.
- Jones SS, Heaton PS, Rudin RS, Schneider EC. Unraveling the IT productivity paradox—lessons for health care. N Engl J Med 2012; 366:2243–2245.
- Koppel R, Lehmann CU. Implications of an emerging EHR monoculture for hospitals and healthcare systems. J Am Med Inform Assoc 2015; 22:465-71.
- Cresswell KM, Mozaffar H, Lee L, Williams R, Sheikh A. Safety risks associated with the lack of integration and interfacing of hospital health information systems. BMJ Qual Saf 2016 Apr 1 [Epub ahead of print].
- National Information Board. Personalised Health and Care: A Framework for Action 2020. 2004
- Press Association. £4.2 billion investment to bring the NHS into the digital age. Daily Mail, 7 February 2016.
- Digital maturity assessment
- National Health Service. Five Year Forward View. October 2014.
Overall findings and principles (section 4)
- Berwick DM, et al. The triple aim: care, health, and cost. Health Aff (Millwood) 2008 May-Jun;27(3):759-69. doi: 10.1377/hlthaff.27.3.759.
- Sheikh A et al. Leveraging health information technology to achieve the “triple aim” of healthcare reform. J Am Med Inform Assoc 2015 Jul;22(4):849-56. doi: 10.1093/jamia/ocv022. Epub 2015 Apr 15.
- Bodenheimer T, et al. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6. doi: 10.1370/afm.1713.
- National Health Service. Five Year Forward View. October 2014.
- Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: An updated systematic review with a focus on Meaningful Use. Ann Intern Med 2014; 160:48-54.
- Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Affairs 2005; 24:1103–1117.
- Triggle N. Virtually all hospitals now in deficit. BBC, 19 Feb 2016.
- Jones SS, Heaton PS, Rudin RS, Schneider EC. Unraveling the IT productivity paradox—lessons for health care. N Engl J Med 2012; 366:2243–2245.
- Farr C. Silicon Valley investors ponder the “next big thing” in health care. Venture Beat, 16 May 2013.
- Hippisley-Cox J, Coupland C, Brindle P. The performance of seven QPrediction risk scores in an independent external sample of patients from general practice: a validation study. BMJ Open 2014 Aug 28;4(8):e005809. doi:10.1136/bmjopen-2014-005809.
- Coiera E. Lessons from the NHS National Programme for IT. MJA 2007; 186(1): 3-4.
- Maughan A. 2010. Six reasons why the NHS National Programme for IT failed - accessed January 4th 2016.
- Cresswell KM, et al. Qualitative analysis of vendor discussions on the procurement of Computerised Physician Order Entry and Clinical Decision Support systems in hospitals. BMJ Open 2015 Oct 26;5(10):e008313.
- Lee L, et al. How does joint procurement affect the design, customisation and usability of a hospital ePrescribing system? Health Informatics J 2015 Aug 10.
- National Information Board. Personalised Health and Care: A Framework for Action 2020. 2004
- Greenhalgh T, Stramer K, Bratan T, et al. Adoption and non-adoption of a shared electronic summary care record in England: a mixed-method case study. BMJ 2010; 340:c3111.
- Ratwani RM, Fairbanks RJ, Hettinger AZ, Benda N. Electronic health record usability: analysis of the user centered design processes of eleven electronic health record vendors. J Am Med Informatics Assoc. 2015; 22:1179-82.
- Australian Commission on Safety and Quality in Health Care. National Guidelines for On-Screen Display of Clinical Medicines Information. 2016.
- Vicente KJ. Cognitive Work Analysis: Toward Safe, Productive, and Healthy Computer-Based Work. Lawrence Erlbaum Assoc Inc; 1999.
- Patient Safety: Practical information, tools and support to improve patient safety in the NHS
- Singh H, et al. Creating an oversight infrastructure for electronic health record-related patient safety hazards. J Patient Saf 2011 Dec;7(4):169-74 etc
- Koppel R, Kreda D. Health care information technology vendors’ “hold harmless” clause: implications for patients and clinicians. JAMA 2009; 301:1276-1278. doi:10.1001/jama.2009.398.
- Gardner RM, et al. Core content for the subspecialty of clinical informatics. J Am Med Inform Assoc 2009; 16:153-7.
- Heifetz R, Laurie DL. The work of leadership. Harvard Business Review, December 2001.
Recommendations (section 5)
- National Information Board. National Information Board’s Workstreams. 4 March 2015.
- Detmer DE, et al. Clinical informatics: prospects for a new medical subspecialty. JAMA. 2014 May;311(20):2067-8.
- Institute of Medicine of the National Academies. Continuous improvement and innovation in health and health care. Roundtable on value and science-driven health care. National Academies Press, 2011.
- Friedman CP, et al. Achieving a nationwide learning health system. Sci Transl Med 2010; 2:57cm29.
- Sheikh A et al. Leveraging health information technology to achieve the “triple aim” of healthcare reform. J Am Med Inform Assoc 2015; 22:849-56. doi: 10.1093/jamia/ocv022. Epub 2015 Apr 15.
- Shortliffe EH, Biomedical informatics in the education of physicians. JAMA 2010; 304:1227-8.
- Faculty of Medical Leadership and Management
- Hersh W. The health information technology workforce. Estimations of demand and a framework for requirements. App Clin Inform 2010; 1:197-212.
- Robertson A, et al. The rise and fall of England’s National Programme for IT. J R Soc Med 2011; 104:434-5.
- Benson T. Why general practitioners use computers and hospital doctors do not–Part 1: incentives. Bmj 2002;325:1086-9.
- Lydall R. ‘World’s safest hospital’ to mentor east London trusts under plan to improve care. Evening Standard. 16 July, 2015.
- NHS England Latest round of technology funding announced
- American Institutes for Research. REC Program Evaluation. Interim Report: Round 1 Case Studies. January 2014.
- The Institute of Electrical and Electronics Engineers, Standards Glossary
- Richesson RL, Chute CG. Health information technology data standards get down to business: maturation within domains and the emergence of interoperability. JAMIA 2015; 22:492-4.
- Sheikh A, Atun R, Bates DW. The need for independent evaluations of government-led health information technology initiatives. BMJ Qual Saf 2014; 23:611-3.
Members of the National Advisory Group
Members of the National Advisory Group on Health Information Technology in England [footnote 1].
| Robert Wachter, MD (Chair) | Professor and Interim Chairman, Department of Medicine, University of California, San Francisco |
| Julia Adler-Milstein, PhD | Associate Professor, Schools of Information and of Public Health, University of Michigan |
| David Brailer, MD, PhD | CEO, Health Evolution Partners; First US National Coordinator for Health IT (2004 to 2006) |
| Dave deBronkart | Patient Advocate, known as ‘e-Patient Dave’ |
| Mary Dixon-Woods, MSc, DPhil | RAND Professor of Health Services Research, University of Cambridge |
| Rollin (Terry) Fairbanks, MD, MS | Director, National Center for Human Factors in Healthcare; Emergency Physician, MedStar Health (US) |
| John Halamka, MD, MS | Chief Information Officer, Beth Israel Deaconess Medical Center; Professor, Harvard Medical School |
| Crispin Hebron | Learning Disability Consultant Nurse, NHS Gloucestershire |
| Tim Kelsey | Commercial Director, Telstra Health; National Director for Patients and Information, NHS England (2012 to 2015) |
| Richard Lilford, PhD, MB | Director, Centre for Applied Health Research and Delivery, University of Warwick, UK |
| Christian Nohr, MSc, PhD | Professor, Aalborg University, Denmark |
| Aziz Sheikh, MD, MSc | Professor of Primary Care Research and Development, University of Edinburgh |
| Christine Sinsky, MD | Vice-President of Professional Satisfaction, American Medical Association; Primary care internist, Dubuque, Iowa |
| Ann Slee, MSc, MRPharmS | ePrescribing Lead for Integrated Digital Care Record and Digital Medicines Strategy, NHS England |
| Lynda Thomas [footnote 2] | CEO, MacMillan Cancer Support, UK |
| Wai Keong Wong, MD, PhD | Consultant Haematologist, University College London Hospitals; Past chair, CCIO Leaders Network Advisory Panel |
| Harpreet Sood, MBBS, MPH | Senior Fellow to the Chair and CEO, NHS England and NHS Doctor (Staff to the Advisory Group) |
Acknowledgments
We are grateful to the members of the National Advisory Group on Health IT. In addition, we received strong staff support from Harpreet Sood, as well as Tom Foley, Peter Thomson, and Diana Paine. We also received excellent editorial assistance from Katie Hafner.
All of the interviewees and leaders of organisations that hosted our visits (listed in Appendix B) were exceptionally cooperative and welcoming, and we greatly appreciate their openness and hospitality.
Several individuals provided important input into specific chapters. The chapter on information technology in general practice benefited from input from Marcus Baw, Tim Benson, Brendan Delaney, John Lockley, and Geraint Lewis. Several members of the MedStar Health Human Factors Research Team (Natalie Benda, Raj Ratwani, Zach Hettinger, and Erica Savage) contributed to the section on usability.
We are grateful to the leadership of the Department of Health and the National Health Service, particularly Secretary of State for Health Jeremy Hunt and NHS England CEO Simon Stevens. They and their teams managed to provide us just the right amount of support without compromising our independence. Their commitment to ensuring the continued excellence of the NHS is impressive.
When Secretary Hunt commissioned our report, he asked that it be modeled on the impactful 2013 report that Don Berwick led on patient safety in the wake of the tragic problems at Mid Staffordshire Hospitals. Don was exceptionally generous with his time and insights, and we modeled much of our process on the one he used for the Berwick Report.
Appendix A: Terms of Reference (Department of Health, February 2016)
The review will inform the English health and care system’s approach to the further implementation of IT in healthcare, in particular the use of electronic health records and other digital systems in the acute sector, to achieve the ambition of a paper free health and care system by 2020. It will have a particular focus on issues around successful clinical engagement with implementation.
Professor Wachter and the advisory board will:
- Review and articulate the factors impacting the successful adoption of health information systems in secondary and tertiary care in England, drawing relevant comparisons with the US experience
- Provide a set of recommendations drawing on the key challenges, priorities and opportunities for the health and social care system in England. These recommendations will cover both the high levels features of mplementations and the best ways in which to engage clinicians in the adoption and use of such systems
In making recommendations, the board will consider the following points:
- the experiences of clinicians and Trust leadership teams in the planning, implementation and adoption of digital systems and standards
- the current capacity and capability of Trusts in understanding and commissioning of health IT systems and workflow/process changes
- the current experiences of a number of Trusts using different systems and at different points in the adoption lifecycle
- the impact and potential of digital systems on clinical workflows and on the relationship between patients and their clinicians and carers
Evidence will be gathered through a combination of available written evidence, meetings with senior figures in the health and care system, and site visits to Trusts with varied experience of implementing IT systems.
Professor Wachter will report his recommendations to the Secretary of State for Health and the National Information Board in June 2016[footnote 25].
Appendix B: Meetings held by Chair and/or Advisory Group
NHS Trusts Visited
- Addenbrooke’s Hospital, Cambridge University Hospitals Trust, 6 April, 2016
- Royal London, Barts Health NHS Trust, 4 February, 2016
- Salford Royal NHS Foundation Trust, 2 February, 2016
- St Mary’s Hospital, Imperial College Healthcare NHS Trust, 5 February, 2016
Group meetings/presentations
British Computer Society, 1 February 2016: attendees
| Helen Beck | Deputy COO, West Suffolk |
| Afzal Chaudhry | CCIO, Cambridge University Foundation Hospital |
| Hannah Coffey | Director of Operations, Guys & St Thomas’ |
| Fran Cousins | Associate Director, Deloitte |
| Tom Denwood | Board & Exec team member / Vice Chair Strategy & Policy, HSCIC / BCS |
| Rachel Duncsombe | CIO, Salford Royal |
| Ian Eaves | Executive Director, Hertfordshire Partnership University NHS Foundation Trust |
| Sanjay Gautama | CCIO, Imperial College Healthcare NHS Trust |
| Emma Goddard | Director of Service Development, Milton Keynes |
| Cathy Kelly | CCIO, UCLP Partners |
| David Kwo | CIO, UCLH Foundation Trust |
| Alex Price-Forbes | Lead for EPR Programme, University Hospitals Coventry and Warwickshire NHS Trust |
| Justin Whatling | Chair, BCS Health |
CCIO Network/HSCIC roundtable, 2 February 2016: attendees
| Adrian Bryne | Chair CIO LN, Director of IM&T at University Hospitals Southampton NHS Foundation Trust |
| Jon Hoeksma | Chief Executive Officer, Digital Health |
| Andy Kinnear | Director of Digital Transformation at NHS South, Central and West CSU |
| Geoff Lavelle | CCIO Tameside Acute Foundation Trust |
| Joe McDonald | Chair CCIO LN and Consultant Psychiatrist, Northumberland, Tyne and Wear NHS Foundation Trust |
| Masood Nazir | GP and NHS England Patient online lead |
| Paul Sherry | CCIO, Warrington and Halton Hospitals NHS Foundation Trusts |
| Caron Swinscoe | Chief Nursing Information Officer (CNIO), Nottingham University Hospitals NHS Trust |
King’s Fund, 3 February 2016: attendees
| Junaid Bajwa | Director of Healthcare Services, MSD |
| Paul Bate | Executive Director of Strategy & Intelligence, CQC |
| Julie Bretland | Development Director, DigitalHealth.London |
| Adrian Bull | Managing Director, Imperial College Health Partners |
| Diarmaid Crean | Deputy Director, Digital, Public Health England |
| Cosima Gretton | Academic Foundation Doctor, Guy’s & St Thomas’ NHS FT |
| Chris Ham | Chief Executive Officer, The King’s Fund |
| Matthew Honeyman | Researcher, The King’s Fund |
| Phil Koczan | GP, CCIO and Digital Clinical Champion for London |
| Charles Lowe | Managing Director, Digital Health & Care Alliance (DHACA) |
| Arvind Madan | Director of Primary Care, NHS England |
| Katie Mantell | Interim Director of Communications and Information, The King’s Fund |
| Kristen McLeod | Director of Strategy, Implementation and Planning, Department of Health |
| Mike Richards | Chief Inspector of Hospitals, CQC |
| Mike Short | Chief Executive Officer, Telefonica |
| David Sloman | Chief Executive Officer, Royal Free London NHS Foundation Trust |
| Rob Webster | Chief Executive Officer, NHS Confederation |
Nuffield Trust seminar, 3 February, 2016: attendees
| Maureen Baker | Chair of RCGP Council, RCGP |
| Derek Bell | Faculty of Medicine, Imperial College London |
| Gary Davies | Consultant Respiratory & Acute Medicine, Chelsea & Westminster Healthcare NHS FT |
| Tim Evans | National Director of Clinical Productivity, DH |
| Stephen Fowlie | Medical Director, Nottingham University Hospitals |
| Andrew Gibson | Medical Director’s Office, Sheffield Teaching Hospital NHS Foundation Trust |
| Toby Graves | Consultant Physician, Dorset County Hospital NHS Foundation Trust |
| Mark Holland | President of the Society for Acute Medicine, Society for Acute Medicine |
| Juliane Kause | Care Group Lead Emergency Care, Visiting Fellow at the University of Southampton |
| Kevin Kelleher | Clinical Director, Dartford & Gravesham |
| Amir Khan | Medical Director, Walsall Healthcare NHS Trust |
| Ajay Kumar | Consultant Physician & Nephrologist / Clinical Director for Medicine, St Helier, Jersey |
| Karl Mainprize | Medical Director, Airedale General Hospital |
| Ben Mearns | Consultant in Acute Medicine, Surrey & Sussex Healthcare NHS Trust |
| Shirlene Oh | Head of Industry, Imperial College Health Partners |
| Kevin Percival | Senior Nurse Clinical Change, Frimley Park Hospital |
| Adam Sewell-Jones | Executive Director of Provider Sustainability at Monitor |
| Mark Temple | Future Hospital Officer, RCP |
Tech UK breakfast roundtable, 7 April 2016: attendees
| Adrian Baker | Head of Health and Social Care, TechUK |
| Rob Blay | CEO, JAC Computer Services & Chair, techUk, Health and Social Care Council |
| Paul Cooper | Research Director, IMS Maxim & Vice-Chair, techUK Health and Social Care Council |
| Kathy Mason | Partner, THE IT Health Partnership & Vice-Chair, techUK Health and Social Care Council |
Individuals presenting before entire Advisory Group, London, April 2016
| Simon Ball | Associate Medical Director and consultant nephrologist, University Hospital Birmingham |
| Charlotte Buckley | Deputy Director for Local Insight and Resilience at Department of Health. Lead for social care information and technology at Department of Health |
| Terry Dafter | North West Care and Health Improvement Advisor (social care adviser) at Local Government Association |
| Roz Davies | Founder, We Love Life (WeLL) |
| Mark Golledge | Information and Technology lead (for social care) at Local Government Association |
| Trish Greenhalgh | Professor of Primary Care Health Science and practising GP |
| Charles Gutteridge | CCIO and consultant haematologist, Barts Health Trust |
| Sarah Jackson | Health and Social Care Information Centre |
| Dominic King | NIHR clinical lecturer in surgery, Imperial College, London, with particular interest in digital health |
| Mark Nicholas | Social Care Account Manager at the Health and Social Care Information Centre (now NHS Digital) |
| Robert Wah | Chief Medical Officer, CSC |
| Neil Watson | Clinical Director of Pharmacy and Medicines Optimisation, Newcastle upon Tyne NHS Foundation Trust |
Individuals interviewed by Professor Wachter
| Maureen Baker | Chair, RCGP Council |
| Paul Bate | Executive Director of Strategy & Intelligence, CQC |
| David Behan | Chief Executive Officer, CQC |
| Ann Blandford | Professor of Human-Computer Interaction & Director of UCL Institute of Digital Health |
| Beverley Bryant | Director of Digital Technology, NHS England |
| Fiona Caldicott | National Data Guardian, UK Government |
| Will Cavendish | Director General of Innovation, Growth and Technology, Department of Health |
| John Chisholm | Executive Chair, Genomics England |
| John Connolly | Chief Medical Officer, TPP |
| Ian Cumming | Chief Executive Officer, Health Education England |
| Ian Dodge | National Commissioning Director, NHS England |
| Tim Donohoe | Director of Informatics Delivery, Department of Health |
| Emma Doyle | Head of Data Policy, Patients and Information, NHS England |
| Nigel Edwards | CEO, Nuffield Trust |
| Tamara Finkelstein | Chief Operating Officer, Department of Health |
| George Freeman | Minister of Life Sciences |
| Harry Hemingway | Director of the Farr Institute of Health Informatics Research, London |
| Frank Hester | Chief Executive Officer, TPP |
| Jeremy Hunt | Secretary of State for Health, UK |
| Candace Imison | Director of Policy, Nuffield Trust |
| Samantha Jones | Director, New Care Models Programme, NHS England |
| Bruce Keogh | National Medical Director, NHS England |
| David Knight | Deputy Director, Information and Transparency Branch, Department of Health |
| Michael Macdonnell | Director of Commissioning Strategy, NHS England |
| Kingsley Manning | Chair, HSCIC (Now NHS Digital) |
| Alex Markham | Director of Research and Professor of Medicine, University of Leeds |
| Clare Marx | President, Royal College of Surgeons and Chair National Information Board, Strategic Clinical Reference Group |
| John Newton | Interim Chair, National Information Board |
| Shaun O’Hanlon | Chief Medical Officer, EMIS |
| Paul Rice | Head of Technology Strategy, Patients and Information, NHS England |
| Sally Davies | Chief Medical Officer, Department of Health (DH) |
| John Savill | CEO, Medical Research Council |
| Nick Seddon | Health Advisor to the Prime Minister |
| Peter Sinden | CIO, NHS Improvement |
| Indy Singh | Head of Enterprise Architecture, NHS England |
| David Stables | Chairman, Endeavour Trust |
| Simon Stevens | Chief Executive Officer, NHS England |
| Mustafa Suleyman | Co-founder, Google Deepmind |
| Matthew Swindells | National Director of Commissioning Operations, NHS England |
| Andy Williams | CEO, HSCIC (now NHS Digital) |
| Jeremy Wyatt | Professor of Digital Healthcare & Director, Wessex Institute of Health & Research, Faculty of Medicine, University of Southampton |
Appendix C: Summary of timetable for deliverables related to key recommendations
Recommendation 1: A robust engagement strategy
By January 2017:
- create and publicise a name and appropriate branding for the new effort to digitise the NHS.
By July 2017:
- create and begin to enact a national campaign to engage clinicians and trust leaders in the new effort to digitise the NHS
Recommendation 2: A National CCIO
Already completed:
- create a job description for, and then hire, a prominent physician-executive with broad experience in information technology, leadership, and change management to become the NHS’s Chief Clinical Information Officer (CCIO)
By January 2017:
- clarify and publicise the national CCIO’s role in leading the digitisation of the NHS, in terms of his or her relationship with NHS England, NHS Digital, NHS Improvement, the National Information Board, and other relevant bodies
Recommendation 3: Grow the workforce of trained clinician-informaticists at trust level
By January 2017:
- trusts seeking Phase 1 (2016-2019) national funding for digital implementation/improvement (Groups A and B; defined under recommendation 7: Link national funding to a viable local implementation/improvement plan) must prepare and defend their workforce plans; plans must include a demonstration that the clinician-IT workforce is sufficiently robust to lead successful digitisation within the trust
By 2019:
-
trusts that have received national funding for Phase 1 digital implementation/improvement (Groups A and B) must have in place a CCIO, devoting at least 75% of his or her time to this task, who reports to the board or CEO (for largest trusts, may be to the chief medical officer or equivalent), with sufficient support staff, budget, and authority to lead successful digitisation and benefits realization within the trust
-
average-sized trusts should have approximately 5 individuals on staff with skills in clinical practice (from any discipline, including medicine, nursing, and pharmacy) and information technology; larger and smaller trusts should adjust these numbers proportionally. These individuals should have at least 25% of their time allocated to their IT and related work
Recommendation 4: Strengthen and grow the CCIO field and the health IT workforce
By January 2017:
- confirm allocation of approximately £42 million (1% of the £4.2 billion to be spent on digitising the NHS) to support workforce development and deployment.
By December 2017:
- establish and launch a programme designed to rapidly train CCIOs, CIOs, and other healthcare informaticians in executive leadership and informatics. The first few “classes” in this intensive 6-12 month training program should focus on training individual who will work at the trusts in Groups A and B.
- the Faculty of Clinical Informatics, working closely with the British Computer Society and the Royal Colleges, should launch an accreditation and professionalisation agenda designed, ultimately, to certify and professionalise the CCIO workforce.
- NHS England and other UK bodies should establish a partnership with relevant international partners (including leading international training programmes and informatics certifying organisations) to help inform UK workforce development efforts
- NHS England should complete and begin to implement a workforce plan designed to grow other segments of IT-related workforce, including clinician and non-clinician informaticians, researchers with expertise in clinical informatics, programme evaluators, and system optimisers (such as data processers, analysts, quality and safety leads)
- Health Education England, in collaboration with the Royal Colleges and other relevant bodies, should develop and begin to implement a plan to raise the level of digital education in all health professional educational settings, including medical, nursing and pharmacy schools, and in continuing education settings for practicing healthcare professionals.
By 2019:
The Faculty of Clinical Informatics, working closely with the British Computer Society and the Royal Colleges, should complete the training and certification of at least 100 new graduates of CCIO training programmes in the UK. At least 80% of these professionals should take positions in trusts or other NHS healthcare delivery organisations.
Recommendations 5, 6, and 7: Develop and enact plan for phased digitisation
By December 2016:
-
NHS England should announce a detailed plan for how it will allocate the £4.2 billion devoted to digitisation, with specific attention to how much will go to trusts to support purchase of software and IT implementation, how much will be allocated to infrastructure improvement, how much will support workforce development, and so on. The plans should include the relative distribution of resources to the 3 categories of trusts (Groups A, B, and C) described under recommendation 7: Link national funding to a viable local implementation/improvement plan)
-
the national CCIO should develop and then disseminate the methods by which trusts will be sorted into groups A, B and C
By January 2017:
- NHS England should approve plans and distribute resources to enable digitisation in Group A, including the expectation of shared funding (central funding combined with funding from the trusts themselves) - we applaud early plans to designate up to12 leading trusts as NHS Centres of Global Digital Excellence
- NHS England should finalise plans for these Centres, including timelines and deliverables
- NHS England should approve a plan for an international partnership to work closely with the NHS Centres of Global Digital Excellence, to help the Centres reach the goals of being world-class leaders in healthcare digitisation and exemplars for the rest of the NHS
By April 2017:
- NHS England should approve plans and distribute resources to enable digitisation in Group B trusts, including the expectation of shared funding (central funding combined with funding from the trusts themselves)
- NHS England should finalise plans for these Centres, including timelines and deliverables
By December 2018:
-
all trusts receiving funding in Phase 1 (Groups A and B) should report on progress. Eligibility for additional funding should be approved by the NHS, based on the progress to date
- specifically, the Centres of Global Digital Excellence (Group A) should be assessed on the following deliverables:
- achieving high levels of staff engagement
- deployment of and support for appropriate workforce within the trust (including IT professionals)
- digitisation of all key processes of care and integration of all key clinical and administrative systems (both within the trust as well as with national systems such as PACS, eReferrals and Electronic Prescribing)
- Substantial use of the electronic patient record to improve care through decision support and practice redesign
- information sharing with patients via patient portals, ability of patients to download key data, and integration with third party apps (including patient-facing apps) through open APIs
- leading efforts to promote digitisation within region, including supporting other trusts
- leading efforts to achieve regional interoperability
- constructive engagement with international partner(s)
- implementation of robust privacy and security standards
By 2019:
- NHS England and the national CCIO should identify and announce plans for funding and supporting those trusts that did not participate in initial digitisation efforts (Group C), including plans for dealing with any trusts that still cannot demonstrate readiness to digitise
By 2020:
- launch of Phase 2, with concrete plans to digitise Group C, and to continue improvements in Group A and B (will likely require additional central resources)
By 2023:
- national funding for trust digitisation ends, accompanied by an expectation that the entire NHS is digitised
- The Care Quality Commission should implement a plan to assess the digital status of trusts (including digital maturity and use of digitisation to promote care improvement), and to deem those that are not sufficiently digitally mature as out of compliance on quality/safety grounds
Recommendation 8: Creation of learning networks
By July 2017:
- NHS England and NHS Digital should approve plans to promote regional learning and improvement within every region in England. These plans should identify the role of the Centres of Global Digital Excellence in helping other trusts go digital, in building regional interoperability, and in linking the region’s IT strategy to its STP and Vanguards programmes.
Recommendation 9: Ensure interoperability
By July 2017:
- NHS England and NHS Digital should announce a multi-pronged plan to ensure regional interoperability (including GPs, trusts, and social care systems), to be implemented no later than 2020
By 2020:
- complete regional interoperability should be established, so the medical records freely flow with a region, with appropriate privacy and security safeguards
By 2022:
- complete national interoperability should be established, so that records can flow freely across entire NHS, with appropriate privacy and security safeguards
Recommendation 10: independent programme evaluation
By late 2017:
- National Institute for Health Research (NIHR) should commission a formative evaluation of the digitisation programme by a respected academic leader/centre - the report should be published by mid-2018 to allow for mid-course corrections
By 2020:
- final evaluation of Phase 1 efforts should be delivered by same academic leader/centre
By 2023:
- final evaluation of Phase 2 efforts should be delivered by same academic leader/centre.
Appendix D: Milestones in digitising the NHS
Also includes relevant milestones in the US
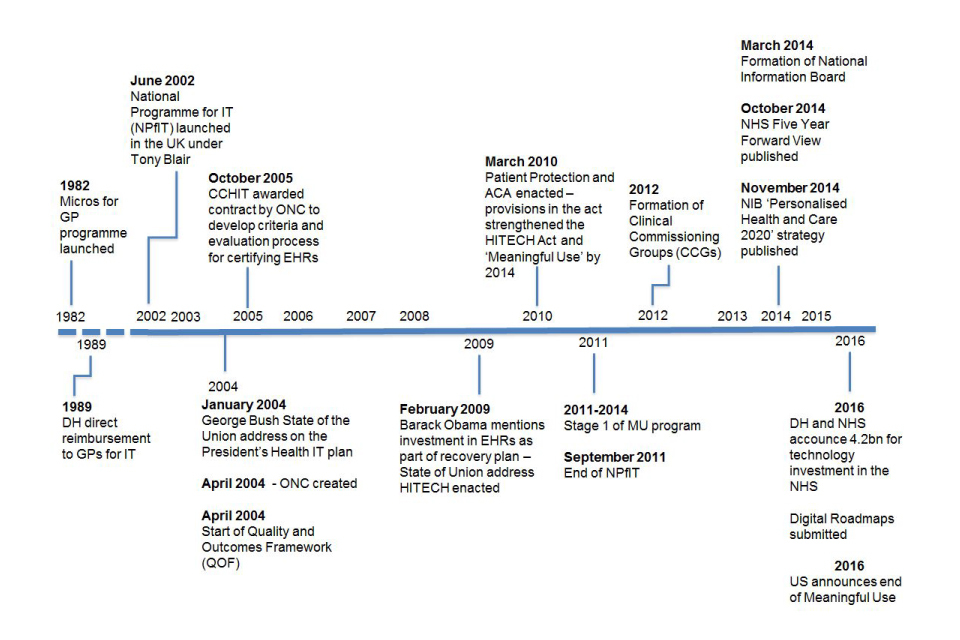
A timeline of events in the UK and US for digitising the NHS, from 1982 to 2016, including £4.2 billion investment in NHS technology in 2016
Abbreviations
| DH | Department of Health |
| NPfIT | National Programme for Information Technology |
| CCHIT | Certification Commission for Health Information Technology (US) |
| ONC | Office of the National Coordinator for Health Information Technology (US) |
| QOF | Quality and Outcomes Framework |
| ACA | Affordable Care Act (US) |
| MU | Meaningful Use (US) |
| NIB | National Information Board |
Appendix E: Digital maturity assessment
The digital maturity self-assessment took 3 main themes on board:
- readiness – strategic alignment, leadership, resourcing, governance and information governance
- capabilities – covering records, assessments and plans, transfers of care, orders and results management, medicines management and optimization, remote and assistive care and standards
- infrastructure – wifi, mobile devices, single sign-on and business continuity
From the Digital Maturity Assessment Guide
| Section | Sub-sections | Description |
|---|---|---|
| Readiness | Strategic alignment, leadership, resourcing, governance, information governance | An assessment of the organisation’s ability to plan, deliver and optimise the digital systems it needs to operate paper-free at the point of care |
| Capabilities | Records, assessments and plans, transfers of care, orders and results management, medicines management and optimisation, decision support, remote and assistive care, asset and resource optimisation, standards | An assessment of the digital capabilities available to that organisation and the extent to which those capabilities and available and being optimised across the organisation as a whole |
| Enabling infrastructure | An assessment of the extent to which the underpinning infrastructure is in place to support delivery of these capabilities |
-
Throughout the document, the term ‘NHS’ refers to the NHS in England. ↩
-
In this report, the terms ‘clinician’, ‘provider’, and ‘healthcare professional’ are used interchangeably. ↩
-
Some legacy components of NPfIT still remain; they are now run by other NHS entities. Approximately £500 million of the recent £4.2 billion allocation for health IT is earmarked for maintaining these systems. ↩
-
Formerly the Health and Social Care Information Centre, HSCIC. ↩
-
In July 2016, the care.data program was terminated. ↩
-
An interesting pattern that you may have discerned: Tony Blair was inspired to launch NPfIT after conversation with an American, Bill Gates. Upon learning of the British programme from Tony Blair, George W. Bush was similarly inspired to launch the US government’s effort to digitise its health system. ↩
-
A typical Meaningful Use standard: ‘Implement 5 clinical decision support interventions related to 4 or more clinical quality measures at a relevant point in patient care…’ ↩
-
Medicare is the US government’s insurance programme covering people age 65 and older, as well as younger people with disabilities. It accounts for about one-fourth of US healthcare spending. ↩
-
With few exceptions, the US system has traditionally been organised around ‘fee for service’. The managed care movement in the mid-1990s sought to shift the system toward capitation (fixed payments to cover a population of patients, putting the delivery system at risk for the cost of care). This movement failed, amid criticism for focusing primarily on cost reduction and corporate profits, not quality. Moreover, Americans were unwilling to accept the rationing and gate-keeping that are generally accepted in the UK. Over the past 5 years, driven by evidence of problems with quality, safety, access, and costs, the US system is once again shifting toward global budgets and delivery system-based accountability for outcomes and costs. Today’s terminology is ‘value-based purchasing’, and the primary vehicles are Accountable Care Organizations (ACOs, a new twist on the health maintenance organization) and bundled payments (fixed payments for an episode of care, such as a hip replacement or a heart failure exacerbation). Of course, the similarity of these initiatives to UK efforts to promote joined up care through the STPs, Vanguards, and other new care models is unmistakable. ↩
-
Meaningful Use Stage 1 is generally viewed as a success; it was designed to ensure that clinicians were actually using their EHRs, purchased in part with federal subsidies. Most criticisms have focused on the far more prescriptive and onerous requirements under Stages 2 and 3. ↩
-
In a 2005 analysis, the RAND Corporation projected that EHRs would result in $81 billion (£62 billion) in annual savings to the US healthcare system (45). A 2014 analysis found that no savings had yet occurred (46). ↩
-
Many trusts have chosen to implement standalone (that is, ePrescribing or electronic charting) systems rather than enterprise systems that cover many or all clinical and financial functions. While the former approach is generally less expensive, it creates the need to build or buy interface engines to weave together the component parts, and this kind of integration is often imperfect (49). ↩
-
In the US, IT suppliers are typically referred to as ‘vendors’. ↩
-
While efforts are being made to align the activities, today the structural elements of digitisation and transformation are more than a little confusing. The 154 acute trusts, along with their CCGs, have been divided into the 73 digital footprints. In addition, local health and care systems have been asked to come together to produce STP roadmaps. Although the 73 footprints have leadership and governance structures, as of July 2016 the groups that have produced the 44 STP roadmaps do not. Our focus in this report is on digitisation of the 154 trusts, but it is important to realise that the trusts operate in this changing framework, which is attempting to promote more integration between GPs, trusts, and other elements of the health and social care systems. While these integrated entities may ultimately promote a learning health system, efficiency, and interoperability (for example, in the future, it may be that a network represented by an STP would oversee regional digitisation), it is fair to say that they also add to the challenges faced by trust leaders. ↩
-
The NIB’s ‘Work Stream 6 Roadmap’, published in June 2015, focuses on this area. ↩
-
Under the National Information Board’s framework, regional ‘footprints’, sometimes composed of multiple trusts as well as other care delivery organisations, may be the entity that purchases and implements technology. For the purpose of this report, we will refer to ‘trusts’ as the unit of purchase/implementation, while recognizing that in some cases, the buyer will be the larger, more integrated organisation represented by the footprint. ↩
-
A similar programme has now been enacted for trusts using monies from the Tech Fund to purchase ePrescribing systems. At first there was no framework, and most trusts tried to tender contracts themselves. Many of them experienced failed procurements, with flawed contracts, unrealistic expectations, and specifications that were impossible to meet. The situation has improved with the development of a centralised procurement framework. The NHS Diabetes Prevention Programme also utilises a national framework procurement, which also appears to be functioning well. It will be important to learn from these and similar experiences in developing a centralised framework for EHR contracting. ↩
-
Some prefer the term ‘clinical information system’ to EHR, since its scope and functionality go beyond that of a simple record – including elements such as patient portals, communication tools, advanced decision support, and robust use of clinical and operational analytics. ↩
-
We were pleased to learn that, in response to our recommendations, on 7 July 2016 NHS England and NHS Improvement announced the appointment of Prof. Keith McNeil, a seasoned healthcare administrator and former transplant specialist, as the first NHS Chief Clinical Information Officer, supported by Will Smart in the role of NHS CIO. ↩
-
‘Paper-free at the Point of Care’ domain, previously NIB Workstream 6. ↩
-
We believe that some local investment is important; it puts trusts in a position of having some ‘skin in the game’. That said, the current financial status of trusts is precarious enough that, for some, a substantial investment may be impossible without dangerous cuts in services. This should be addressed on a case-by-case basis. ↩
-
Some important work in this area has already been done by NHS, which has divided England into 73 ‘local digital footprints’. Each footprint includes trusts, clinical commissioning groups, GPs, and other elements of the care system. The footprints are developing plans for digitisation, including the expectation of supporting regional interoperability. ↩
-
Sir David Dalton, CEO of Salford Royal NHS Foundation Trust, participated in early deliberations but left the committee in April 2016 due to other obligations. ↩
-
Declan Hunt, Executive Director of Technology for MacMillan Cancer Support, attended several meetings as an alternate to Ms. Thomas. ↩
-
The final report of the recommendations was delayed until September 2016 because of the period of purdah preceding the Brexit vote. ↩
