Travel-associated infections in England, Wales and Northern Ireland: 2022
Updated 14 August 2025
Applies to England, Northern Ireland and Wales
Background
This report, produced by the Travel Health and International Health Regulations (IHR) team in the Clinical and Emerging Infections Directorate, UK Health Security Agency (UKHSA), summarises case numbers of selected travel-associated infections reported in England, Wales and Northern Ireland between 2015 and 2022. Case numbers were previously reported through ECDC between 2015 and 2019 for chikungunya, cholera (Vibrio cholerae serogroup O1 or O139), dengue, yellow fever and Zika. The data presented in this report supersedes any other case numbers previously reported.
Detailed information is included on the trends of chikungunya, cholera, dengue, rickettsial infections and Zika in 2022. An infection summary and key findings are provided for Japanese encephalitis and yellow fever. Data presented here is derived from a variety of sources and may be subject to limitations in completeness due to various factors, including underreporting.
Detailed annual reports are available elsewhere for imported malaria cases in the UK and travel-associated enteric fever cases in EWNI.
Data sources
Data for cases of chikungunya, dengue, Japanese encephalitis, rickettsial infections, yellow fever and Zika was obtained from the Rare and Imported Pathogens Laboratory (RIPL), UKHSA Porton. Case definitions used for these infections are as follows:
- confirmed: molecular detection (PCR, other molecular amplification test or sequencing) and/or positive virus isolation and/or seroconversion between acute and convalescent samples and/or 4-fold rise in antibody titre
- probable: IgM and IgG positive and compatible clinical syndrome
Data for confirmed cholera cases was obtained from the UKHSA Gastrointestinal Bacteria Reference Unit (GBRU). A confirmed case is a person with Vibrio cholerae serogroup O1 or O139 confirmed by the GBRU.
For all cases, specimen collection date was used where available to conduct analysis. In cases where this information was not available, laboratory receipt date was used. Case numbers presented in this report include both confirmed and probable cases, gathered from multiple sources, including confirmed cases from GBRU and both confirmed and probable cases from RIPL.
Data for UK residents and UK overseas visitors was obtained using the International Passenger Survey (IPS) data provided to the Travel Health team by the Office of National Statistics (ONS). Further information and analysis for travel trends seen in 2022 were obtained from the ONS website (1).
World regions of travel were assigned based on the United Nations world region classifications (2).
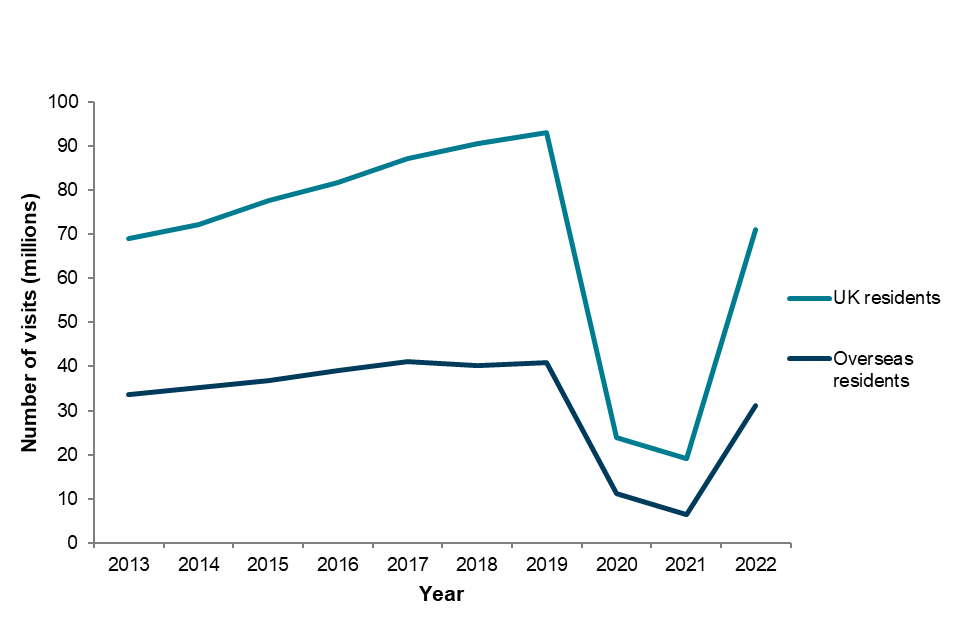
Changes in travel to and from the UK in 2022
Data on travel to and from the UK was obtained from the Office of National Statistics International Passenger Survey. In 2022, UK residents made 71.0 million visits abroad, a 4-fold increase compared to 2021 (19.1 million). There were 31.2 million visits made by overseas residents to the UK, a 5-fold increase compared to 2021 (6.4 million). These increases can be attributed to the easing of COVID-19 travel restrictions at the end of 2021. However, travel to and from the UK in 2022 remained below pre-COVID-19 pandemic levels in 2019 (Figure 1) (3).
For both UK visits abroad and overseas visits to the UK in 2022, seasonal travel trends returned to pre-COVID-19 travel patterns, with most travel in occurring during the summer and a peak in August. The most popular reasons for travel for UK residents in 2022 were holidays, with 45.6 million visits, followed by visiting friends and relatives (19.0 million) and business travel (4.8 million). The top 5 most visited countries were Spain, France, Italy, Greece and Portugal. Holiday travel was also the most popular reason for overseas residents visiting the UK in 2022, followed by visiting friends and relatives and business travel. This is a change compared to 2021 when visiting friends and relatives was the most popular reason for travel to the UK. Residents of the USA, France, Republic of Ireland, Germany and Spain represented the highest numbers of overseas residents visiting the UK (1).
Figure 1. Visits to and from the UK from 2013 to 2022
Travel-associated infections 2015 to 2022
Table 1. Travel-associated infections in England, Wales and Northern Ireland (EWNI): 2015 to 2022
| Disease (Organism)* | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|---|---|---|
| Chikungunya | 101 | 155 | 90 | 59 | 100 | 33 | 17 | 31 |
| Cholera (Vibrio cholerae serogroup O1 or O139) | 15 | 16 | 14 | 17 | 15 | 2 | 2 | 20 |
| Dengue | 424 | 464 | 441 | 416 | 790 | 91 | 97 | 448 |
| Japanese encephalitis | 1 | 1 | 1 | – | – | – | – | – |
| Rickettsial infections | 51 | 33 | 42 | 39 | 39 | 12 | 4 | 31 |
| Yellow fever | – | – | – | 1 | – | – | – | – |
| Zika | 4 | 275 | 21 | 4 | 6 | 1 | 1 | 8 |
*Only includes confirmed and probable cases
Table 1 presents reported travel-associated infections in England, Wales, and Northern Ireland from 2015 to 2022. Dengue remains the most frequently reported infection, with the highest number of cases (790 cases) reported in 2019. While most of these infections have returned to pre-COVID-19 pandemic levels, case numbers for cholera have exceeded these. The reasons for these trends are not always clear and could reflect changes in ascertainment, testing patterns as well as the burden of disease.
Chikungunya
Chikungunya is a mosquito-borne infection transmitted by the bite of an infected female Aedes mosquito and is caused by a virus from the Flaviviridae family. It is characterised by a sudden onset of fever usually accompanied by joint pain (arthralgia); however, symptoms vary in severity. Serious complications are uncommon, but, rarely, in older people the disease can contribute to the cause of death, particularly if there is other underlying illness. Chikungunya mainly occurs in Africa, Asia and specifically in Southern Asia, although there have been cases reported in parts of Europe and North America (4).
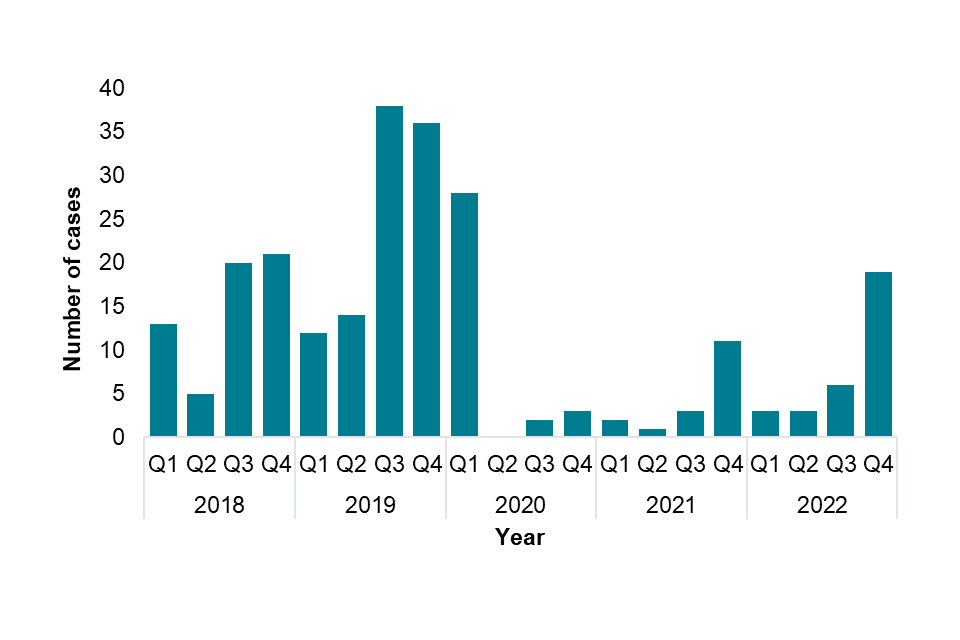
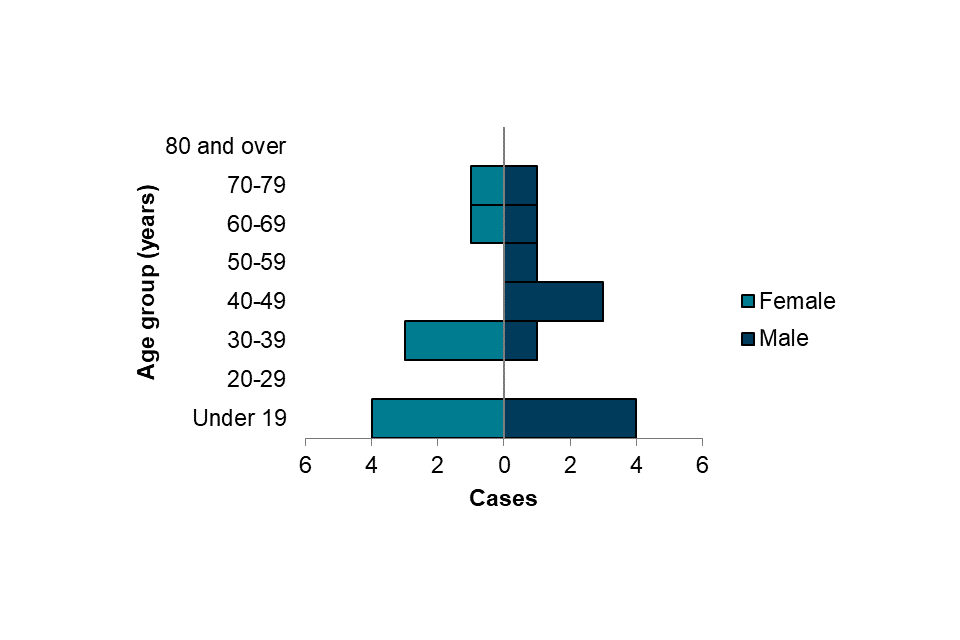
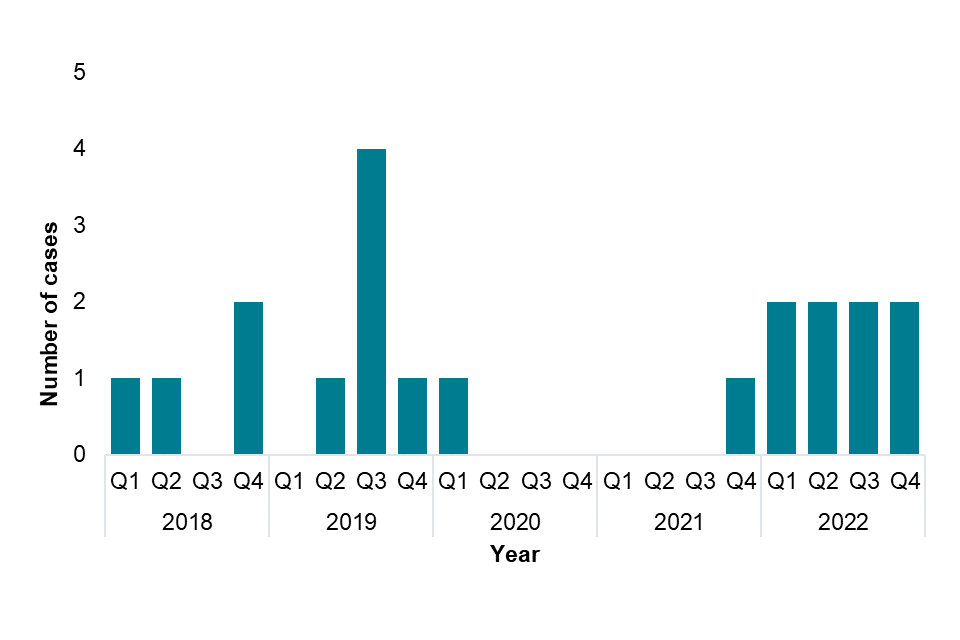
In EWNI there were 31 chikungunya cases reported in 2022, all of these from England. Of these, 11 (35%) were confirmed cases and 20 (65%) were probable cases. This represents an 82% increase compared to 2021 (n=17) but remains lower than the pre-COVID-19 pandemic average of 101 cases reported per year between 2015 and 2019. Case numbers were low in the first three quarters of 2022 (n=3, n=3, n=6) and the majority of cases (n=19) were diagnosed in the fourth quarter (Figure 2).
Figure 2. Cases of chikungunya by quarter, Q1 2018 to Q4 2022
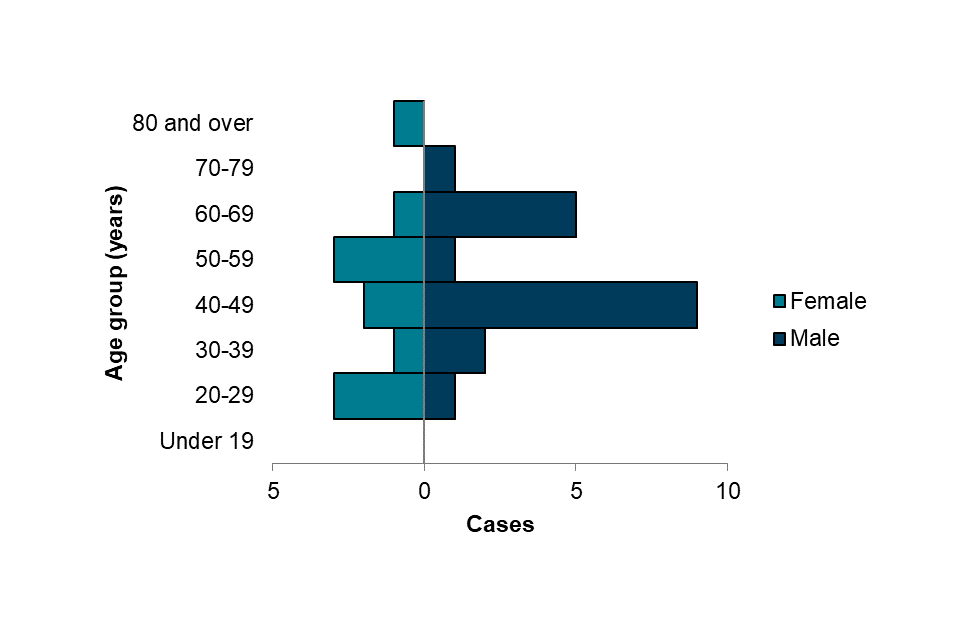
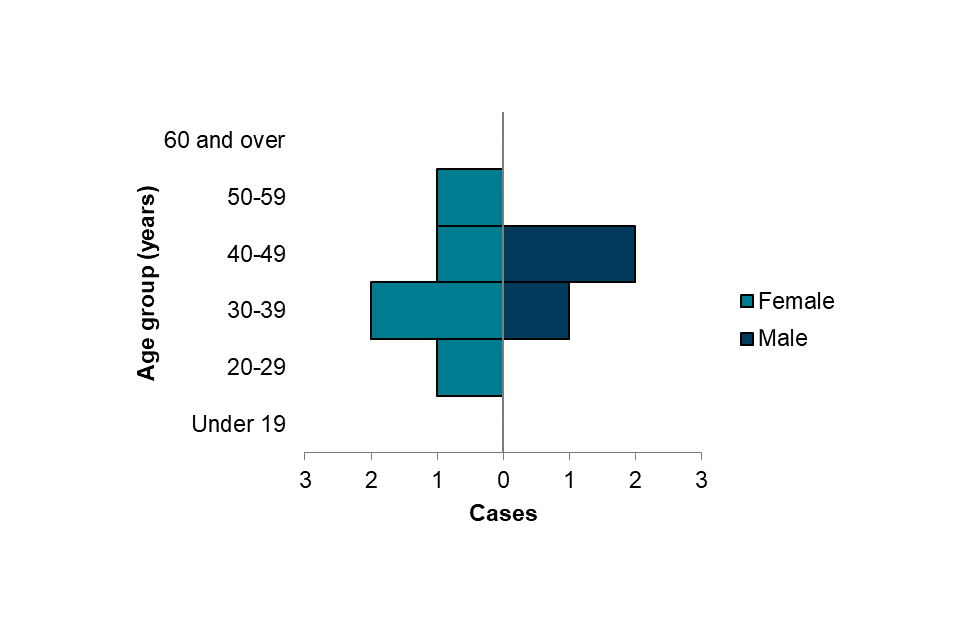
In 2022, 11 cases (36%) were female (aged 25 to 82 years, median=44) and 19 (61%) were male (aged 26 to 70, median=49) (Figure 3). Sex was not recorded for 1 case.
Figure 3. Cases of chikungunya by age group and sex, 2022 (n=30)
In 2022, travel history was known for 30 out of 31 cases, with the majority of these reporting travel to Southern Asia (15, 50%) and Western Africa (8 cases, 27%), similar to 2021 (Table 2). The most frequently reported countries of travel were:
- India (15)
- Ghana (3)
- Nigeria (3)
Cases who travelled to India reported travelling to a number of regions including Punjab, Uttar Pradesh, Delhi and West Bengal. India reported a 20% increase in chikungunya cases (confirmed and suspected) in 2022 compared to 2021 (5), including in Punjab, Uttar Pradesh and West Bengal where EWNI cases reported travelling to.
Table 2. Cases of chikungunya by region of travel, 2022
| Region of travel | Number of cases |
|---|---|
| Southern Asia | 15 |
| Western Africa | 8 |
| South-Eastern Asia | 4 |
| Eastern Africa | 2 |
| Middle Africa | 1 |
| Not stated | 1 |
| Total* | 31 |
*Some cases travelled to more than one region; all regions are included here so the total may be higher than the actual number of cases.
Cholera (Vibrio cholerae serogroup O1 or O139)
Cholera is caused by infection of one of 2 serogroups of the Vibrio cholerae bacteria, serogroups O1 and O139.
Cholera is an acute diarrhoeal disease caused by ingestion of contaminated food or water. A vaccine is available but is only recommended for some travellers. Cases of cholera may be asymptomatic or have mild symptoms, including acute, profuse watery diarrhoea (‘rice water stools’) and vomiting, leading to dehydration. Some infections may progress to severe disease, and in extreme cases may result in death if untreated (6). Cholera cases were reported in 35 countries in 2021 and the disease occurs mainly in Africa and Asia, but sporadic cases have also been reported in other regions (7).
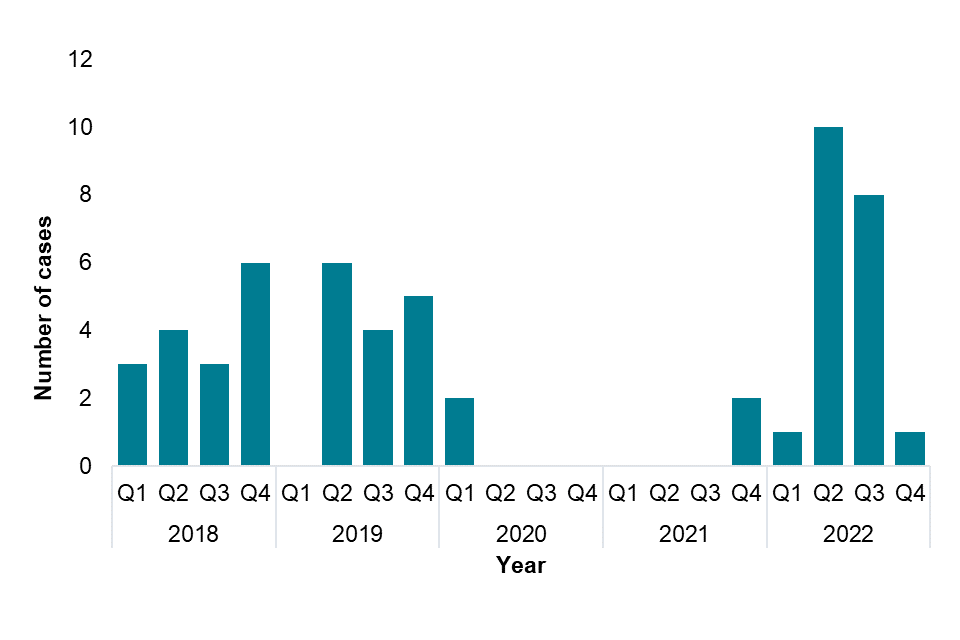
Between 2015 and 2019 there were an average of 15 cases each year in EWNI, with a peak of 17 cases in 2018. There were 20 cholera cases reported in 2022, all of which were reported in England. This was a large increase compared to 2021 where 2 cases were reported. Case numbers were highest in the second and third quarters (n=10 and n=8) (Figure 4).
Figure 4. Cases of cholera by quarter, Q1 2018 to Q4 2022
In 2022, 9 cases (45%) were female (aged 1 to 78 years, median=34) and 11 (55%) were male (aged 1 to 72 years, median=43) (Figure 5).
Figure 5. Cases of cholera by age group and sex, 2022 (n=20)
In 2022, travel history was known for all cases, with the majority of these reporting travel to Southern Asia (17, 85%) (Table 3).
The most frequently reported countries of travel were:
- Pakistan (10)
- Bangladesh (4)
- India (2)
- Iraq (2)
The high number of cases reporting travel to Pakistan reflects ongoing floods and heavy rain reported in Pakistan in 2022 during the rainy season, which has led to increased cholera cases reported in flood affected regions (8). One case each reported travel to Iran and the Philippines, making this the first report of travel to these countries in data available since 2004 for cholera cases in EWNI. Both countries reported cholera outbreaks in 2022 (9). Since 2022, 30 countries across Africa, Asia and the Caribbean have reported cholera cases or outbreaks, with many countries reporting higher cholera case numbers and case fatality ratios (9).
Table 3. Cases of cholera by region of travel, 2022
| Region of travel | Number of cases |
|---|---|
| Southern Asia | 17 |
| Western Asia | 2 |
| South-Eastern Asia | 1 |
| Total | 20 |
Dengue
Dengue is a mosquito-borne infection transmitted by the bite of an infected female Aedes mosquito. It is caused by a virus from the Flaviviridae family and has 4 main serotypes: DEN-1, 2, 3 and 4.
Illness is characterised by an abrupt onset of fever often accompanied by severe headache and pain behind the eyes, muscle pain, joint pains, nausea, vomiting, abdominal pain and loss of appetite; however, symptoms can range from mild or non-existent to severe.
Severe dengue is rare in travellers. Dengue is endemic in over 100 countries across Africa, the Americas, the Eastern Mediterranean, South-East Asia and the Western Pacific, with sporadic cases occurring in some other countries in Europe (10).
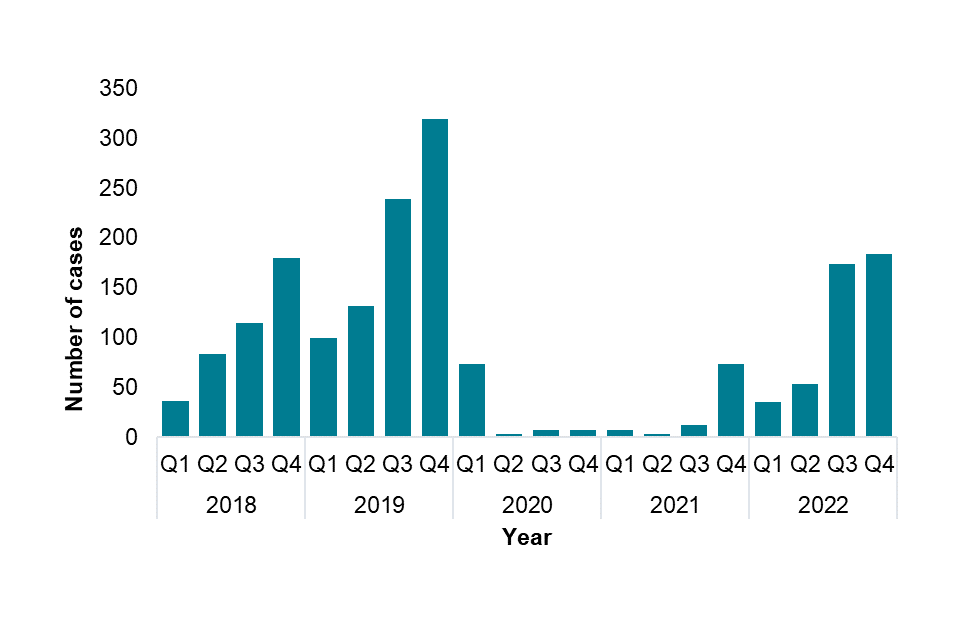
In EWNI there were 448 dengue cases reported in 2022 (427 in England, 16 in Wales and 5 in Northern Ireland), of which 410 (92%) were confirmed cases and 38 (8%) were probable cases. This was a significant increase compared to the 97 cases reported in 2021, though it remains lower than the pre-COVID-19 pandemic average of 507 cases reported per year between 2015 and 2019. Case numbers were low in the first 2 quarters of 2022 (n=36, n=54) and the majority of cases were diagnosed in quarters 3 and 4 with 174 and 184 cases respectively (Figure 6).
Figure 6. Cases of dengue by quarter, Q1 2018 to Q4 2022
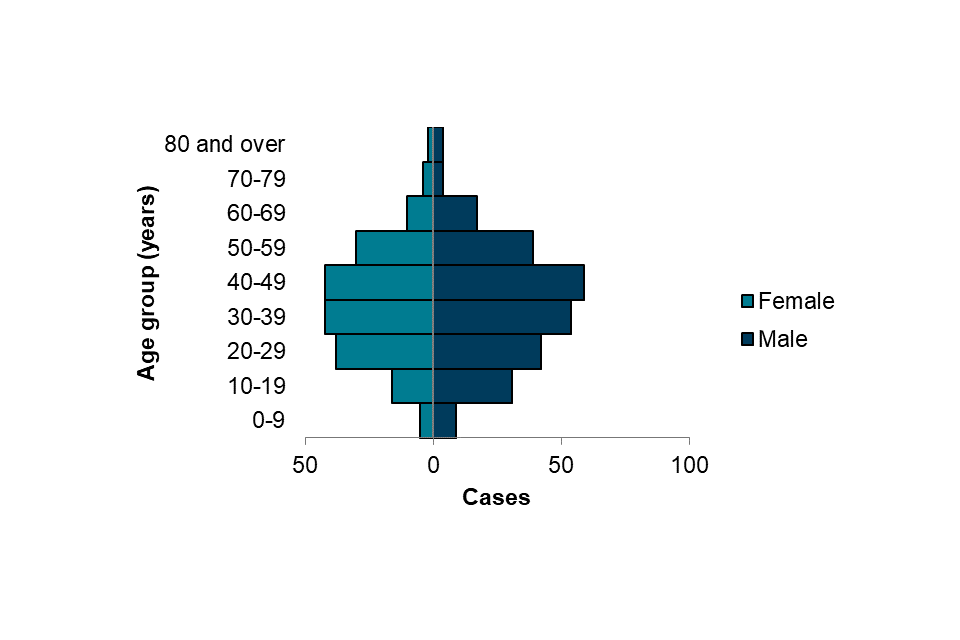
In 2022, 189 cases (42%) were female (aged 2 to 85 years, median=37) and 259 (58%) were male (aged 3 to 90, median=37) (Figure 7).
Figure 7. Cases of dengue by age group and sex, 2022 (n=448)
In 2022, travel history was known for 388 out of 448 cases (87%), with the majority of cases reporting travel to Southern Asia (248, 64%) and South-Eastern Asia (52, 13%) (Table 4). The most frequently reported countries of travel in Southern Asia were:
- India (n=106)
- Pakistan (n=57)
- Nepal (n=47)
Many Southern Asian countries have reported a surge in dengue cases in 2022 compared to 2021, including India which reported its highest case numbers since 2017, with 233,251 reported dengue cases (11). Nepal and Pakistan have also reported increased case numbers, due to unprecedented heavy rains and flooding that coincided with monsoon seasons (12, 13). Notably, one EWNI case reported travel to Southern France. Autochthonous dengue has been sporadically reported in Europe, including in France 2022 (14). Current global reports on dengue cases indicate a rising trend, due to factors including climate change, rising temperatures and flooding (15).
Table 4. Cases of dengue by region of travel, 2022
| Region of travel | Number of cases |
|---|---|
| Southern Asia | 248 |
| South-Eastern Asia | 52 |
| Caribbean | 24 |
| Eastern Africa | 23 |
| South America | 20 |
| Central America | 15 |
| Western Asia | 8 |
| Western Africa | 3 |
| Middle Africa | 2 |
| Western Europe | 1 |
| Northern America | 1 |
| Not stated | 60 |
| Total* | 457 |
*Some cases travelled to more than one region; all regions are included here so the total may be higher than the actual number of cases.
Rickettsial infections
Rickettsial infections are a group of bacterial infections of the genera Orientia and Rickettsia, which are transmitted by different arthropod vectors, including ticks, mites, lice and fleas, to animals such as humans, dogs, cats and cattle. In general, the incubation period is between 6 to 14 days post infection and symptoms vary but may include fever, myalgia, headache, dry cough and rash (16, 17, 18).
Human rickettsial infections are classified into 3 main groups: spotted fever group, typhus group and scrub typhus group. Spotted fever group infections are caused by over 30 Rickettsia species such as Rickettsia africae, Rickettsia conorii sp., and Rickettsia rickettsii. They are transmitted by ticks and have a wide geographical distribution. Typhus group infections are caused by Rickettsia typhi and R. prowazekii and are transmitted to humans through louse and flea faeces mostly in Asia, Africa and the Western Pacific. Scrub typhus infections are mainly caused by Orientia tsutsugamushi and transmitted through the bite of infected mite larvae. They are endemic across Asia, the Western Pacific, South America and Africa and causes an estimated 1 million cases per year (17, 18).
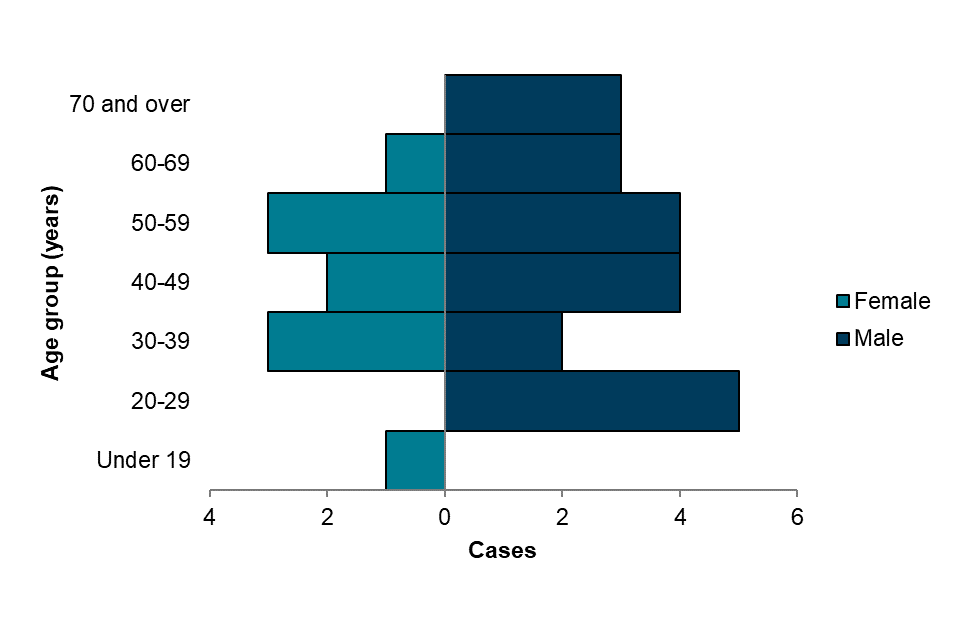
In 2022 there were 31 cases of rickettsial infections reported in EWNI (30 in England and 1 in Wales), Of these, 17 (55%) were confirmed cases and 14 (45%) were probable cases. This represents a large increase compared to 4 cases reported in 2021, and slightly lower than the pre-COVID-19 pandemic average of 41 cases reported per year between 2015 and 2019. Case numbers in 2022 were the highest in quarters 2 and 3 (n=10 and n=9) (Figure 10). Of reported cases there were 20 cases (65%) in the spotted fever group, 6 cases (19%) in the scrub typhus group and 5 cases (16%) in the typhus group.
Figure 10. Cases of rickettsial infections by quarter, Q1 2018 to Q4 2022

In 2022, 10 cases (32%) were female (aged 17 to 68 years, median=45) and 21 (68%) were male (aged 21 to 76 years, median=48) (Figure 11).
Figure 11. Cases of rickettsial infections by age group and sex, 2022 (n=31)
In 2022, travel history was known for 29 out of 31 cases. Of these, the majority of spotted fever cases reported travel to Southern Africa (13, 57%) and Eastern Africa (4, 17%). All scrub typhus cases reported travelling to Southern Asia (6) and half of typhus group cases reported travel to Middle Africa (3, 50%) (Table 5).
For all cases of rickettsial infection, the most frequently reported country of travel was South Africa (13), followed by India (3) and Cameroon, Mozambique, Eswatini and Sri Lanka, with 2 cases reporting travel to each.
Table 5. Cases of rickettsial infection by region of travel and rickettsial group, 2022
| Region of travel | Scrub typhus | Spotted fever | Typhus group | Total number of cases |
|---|---|---|---|---|
| Southern Africa | – | 13 | – | 13 |
| Southern Asia | 6 | – | – | 6 |
| Eastern Africa | – | 4 | – | 4 |
| Middle Africa | – | – | 3 | 3 |
| Western Asia | – | – | 2 | 2 |
| Caribbean | – | 1 | – | 1 |
| Central America | – | 1 | – | 1 |
| Northern America | – | 1 | – | 1 |
| South-Eastern Asia | – | – | 1 | 1 |
| Southern Europe | – | 1 | – | 1 |
| Not stated | – | 2 | – | 2 |
| Total* | 6 | 23 | 6 | 35 |
*Some cases travelled to more than one region; all regions are included here so the total may be higher than the actual number of cases.
Zika
Zika is a mosquito-borne infection transmitted by the bite of an infected female Aedes mosquito. It is caused by a virus from the Flaviviridae family. Less commonly, transmission can occur through sexual contact, congenitally from a pregnant woman to her foetus and though blood transfusion (19).
The majority of people with Zika infection do not develop symptoms. Those that do often have mild symptoms which can include fever, headache, malaise, joint and muscle pain, a rash, itching, conjunctivitis and swollen joints (20).
Serious complications are uncommon, however an infection with Zika is a cause of congenital Zika Syndrome (characterised by microcephaly and other congenital anomalies) and neurological complications such as Guillain-Barré Syndrome.
During 2015 to 2016, there was a large outbreak of Zika virus infection in the Americas and the Caribbean, leading to the first imported Zika cases in the UK. As of 2022, 89 countries across Africa, Europe, the Americas, South-East Asia and the Western Pacific have reported autochthonous Zika cases (21).
In 2022, there were 8 Zika cases reported, all of these from England. Of cases reported in 2022, 7 (88%) were confirmed cases and 1 (13%) was classified as a probable case. Case numbers were consistent across all 4 quarters of 2022 (Figure 16). This represents a large increase compared to 2021, when only 1 case was reported. However, this remains lower than the pre-COVID-19 pandemic average of 25 cases reported per year between 2015 and 2019.
Figure 16. Cases of Zika by quarter, Q1 2018 to Q4 2022
In 2022, 5 cases (63%) were female (aged 26 to 52 years, median=33) and 3 (37%) were male (aged 33 to 45, median=44) (Figure 17).
Figure 17. Cases of Zika by age group and sex, 2022 (n=8)
In 2022, travel history was known for the majority of cases, with most reporting travel to South-Eastern Asia (6, 75%) (Table 8). The most frequently reported country of travel was Thailand (n=5). Other reported countries included Cambodia (n=1), the Philippines (n=1), Singapore (n=1) and Vietnam (n=1). Of the remaining two cases, one case travelled to Sri Lanka (Southern Asia), while for the other case, travel country/region was not known.
Table 8. Cases of Zika by region of travel, 2022
| Region of travel | Number of cases |
|---|---|
| South-Eastern Asia | 6 |
| Southern Asia | 1 |
| Not stated | 1 |
| Total* | 8 |
*Some cases travelled to more than one region; all regions are included here so the total may be higher than the actual number of cases.
Other travel-associated infections
Japanese encephalitis
Japanese encephalitis (JE) is a vaccine preventable mosquito-borne infection transmitted by the bite of Culex species mosquitoes. It is a flavivirus from the Flaviviridae family and is transmitted via mosquitoes to humans from pigs and water birds. Japanese encephalitis is found in 24 countries in South-Eastern Asia and the Pacific, mainly in settings where humans live in close proximity to pigs and water birds. A vaccine is available; however this is only advised for travellers at increased risk of infection. Most people with JE do not develop symptoms but for those who do symptoms may include fever and headache or vomiting in children. Less than 1% of people develop severe disease, which is characterised by encephalitic symptoms such as disorientation, seizures, coma and paralysis and approximately 30% of these cases are fatal. For cases who survive, approximately 30% suffer long term cognitive, behavioural or neurological complications (22, 23).
There were no cases of Japanese encephalitis reported in EWNI in 2022. The most recently reported case in EWNI was in 2017 in a traveller who had visited Thailand.
Yellow fever
Yellow fever is a vaccine preventable mosquito-borne infection transmitted by the bite of multiple species of infected mosquitoes, including Aedes and Haemogogus species. Yellow fever virus is a flavivirus from the Flaviviridae family. Yellow fever is endemic in all or parts of 47 countries in Africa and Central and South America. The virus incubates in the body for 3 to 6 days post infection. Many people do not develop symptoms but for those who do, these may include fever, headache, nausea or vomiting, muscle pain (often with backache), and loss of appetite. Most people will make a full recovery after 3 to 4 days, however a small number (approximately 15%) will progress to a second phase of the infection and go on to develop jaundice, abdominal pain, renal failure and haemorrhage (bleeding). Up to half of infections in cases who develop severe symptoms may result in death. Yellow fever is rare in international travellers as there is a safe and effective vaccine available. Although the vaccine is safe, there have been reports of rate adverse events associated with its use (24).
Data for cases of Yellow fever was obtained from RIPL, UKHSA Porton.
In EWNI there were no cases of yellow fever reported in 2022. The most recently reported case in EWNI was in 2018 in a traveller who had visited Brazil.
References
1. ONS. ‘Travel trends: 2022’
2. UNSD. ‘Methodology’
3. ONS. ‘Travel trends estimates: overseas residents in the UK and UK residents abroad’
4. WHO. ‘Chikungunya’ (updated 8 December 2022)
5. NCVBDC. ‘Chikungunya Situation in India’
6. WHO (2017). ‘Cholera vaccines: WHO position paper’
7. WHO (2021). ‘Cholera Annual Report 2021’. Weekly Epidemiological Record: volume 97 (37), pages 453 to 464
8. WHO. ‘Pakistan Floods Situation Report’
9. WHO. ‘Cholera – Global situation’ (updated 11 February 2023)
10. WHO. ‘Dengue and severe dengue’ (updated 17 March 2023)
11. NCVBDC. ‘Dengue Situation in India’
12. WHO. ‘Dengue – Nepal’ (updated 10 October 2023)
13. WHO. ‘Dengue – Pakistan’ (updated 13 October 2023)
14. ECDC. ‘Autochthonous vectorial transmission of dengue virus in mainland EU/EEA, 2010-present’ (updated 20 September 2023)
15. Mondal N (2023). ‘The resurgence of dengue epidemic and climate change in India’. The Lancet: volume 401, issue 10378
16. Premaratna R (2022). ‘Rickettsial illnesses, a leading cause of acute febrile illness’. Clinical Medicine Journal: volume 22, issue 1
17. Blanton LS (2019). ‘The Rickettsioses: A Practical Update’. Infectious Disease Clinics of North America: volume 33, issue 1
18. Warrell CE, Osborne J, Nabarro L, Gibney B, Carter DP, Warner J, Houlihan CF, Brooks TJG, Rampling T (2023) ‘Imported rickettsial infections to the United Kingdom, 2015–2020’. Journal of Infection: volume 86, issue 5
19.WHO. ‘Zika virus factsheet’ (updated 8 December 2022)
20. PHE. ‘Zika virus: symptoms and complications guidance’ (updated 2 August 2017)
21. WHO. ‘Zika epidemiology update - February 2022)’
22. WHO. ‘Japanese encephalitis’ (updated 9 May 2019)
23. Yun SI, Lee YM (2013). ‘Japanese encephalitis: the virus and vaccines’. Human Vaccines & Immunotherapuetics: volume 10, issue 2
24. WHO. ‘Yellow fever’ (updated 31 May 2023)
