NIHR: The effectiveness of PPE in reducing the transmission of COVID-19 in health and social care settings: December 2021 update, 12 December 2021
Published 23 December 2021
This paper presents independent research funded by the National Institute for Health Research. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care or its partners.
Effectiveness of PPE in protection against COVID-19 transmission
In September 2020, we performed a rapid literature search to investigate the effectiveness of PPE in reducing the transmission of COVID-19 initially for unpaid carers. [footnote 1] In May 2021 we updated this to consider people working in health and social care settings as part of a fuller paper on mitigations for residential care in the post vaccination risk landscape. [footnote 2] Here we update that paper to bring it up to date for December 2021 in the light of the identification of the Omicron variant. It should be noted that all literature reported below predates identification of this variant of concern. Whilst our previous searches found no direct evidence regarding the use of PPE directly related to residential social care in our most recent search we did find reviews related to IPC measure in residential care setting. Nonetheless because of the focus, and quality, of that work we still depend primarily on literature about the effectiveness of PPE when used by healthcare workers. Our updated rapid literature search (Appendix A) reveals that studies reporting on PPE in health care workers are predominantly based in hospital settings with a focus on nurses and physicians. We have now also identified research on mask use in the general population and have drawn on the UK Health Security Agency (UKHSA) October 2021 review of the effectiveness of face coverings in reducing community transmission of COVID-19. [footnote 3] In addition the living review on coronavirus infection epidemiology and risk factors in health care workers based on cross-sectional, cohort, and case series studies and first published in 2020 [footnote 4] has been updated twice since we used update 8 (118 studies) in our May 2021 version of this briefing. Update 9 [footnote 5] adds 21 new studies and update 10 [footnote 6] has 20 new studies. Data from these 2 updates are thus included herein. [footnote 7] To date no meta-analysis of results has been undertaken because of heterogeneity of outcomes and continued methodological differences and limitations in the included studies. Update 10 presents a summary evidence table of risk factors and mitigations for COVID-19 infection amongst healthcare workers reproduced in Appendix B.
PPE use in healthcare workers
Up-to-date evidence on the effectiveness of PPE in healthcare workers is available in the living rapid review. [footnote 4] [footnote 5] [footnote 6] We have searched each update for results in relation to:
(a) mask use
(b) full use of PPE compared to partial use
(c) frequency and consistency of PPE use
(d) infection control training and education
The review provides a narrative summary of findings in relation to coronavirus exposure and PPE use and results are consistent across all updates. A notable finding from update 10 is that 7 studies consistently found that exposure to COVID-19 in a household or private setting is associated with increased risk of infection in HCWs (adjusted odds ratios [ORs] range from 2.55 to 8.98 and in most studies, household or private setting exposure is a stronger risk factor than work exposure).
Masks [footnote 8]
The living review continues to report consistent and robust evidence for the association between mask use and decreased infection risk from SARS-CoV-2 in healthcare workers (ORs from 0.002 to 0.71 for significant studies, or 1.7 including non-significant studies [footnote 9] ). While the initial review in 2020 extrapolated from results of studies on non-SARS-CoV-2 specific data, the more recent updates have focused on data from studies of SARS-CoV-2 infection only. Results are thus likely to be relevant to the current situation. However, all results relate to variants earlier than Omicron. Studies also suggest that N95 (FFP2) respirators are associated with decreased risk compared with surgical masks (ORs in the region of 0.75 in most cases). These studies are confounded by factors such as N95 being used in higher risk areas or during higher risk procedures (for example AGPs). No meta-analysis was conducted, but summary tables can be found in the update supplementary materials. The evidence remains clear for consistency of use of masks, with consistent use providing better protection than inconsistent use.
UK Health Security Agency (UKHSA) updated the review of the effectiveness of face coverings in reducing community transmission of COVID-19 in October 2021 [footnote 3] , drawing on evidence reviews up until 14 September 2021. The review includes 25 studies (23 observational studies, 2 RCTs). The report suggests that face coverings reduce the spread of COVID-19 in the community, through source control, wearer protection, and universal masking, but draws no conclusions as to face coverings are more effective as source control or wearer protection. RCT evidence (medium quality) from one RCT provides direct evidence that face coverings (surgical and cloth face coverings) are effective when used as universal masking, particularly for surgical masks and for older people, and that the interventions to increase face covering use also increased social distancing. The other RCT was inconclusive, reporting a non-significant reduction in COVID-19 infections from wearer protection using surgical masks. Relatively few participants in this study developed COVID-19 and thus the study lacked precision. Contact tracing studies (n=8) that analysed face covering use suggest that contacts of primary cases were less likely to develop COVID-19 if either or both wore a face covering. Further, (mostly low quality) observational studies (n=15) had mixed results for the effectiveness of face coverings. For all these observational studies confounding factors such as differences between wearers and non-wearers of masks, and mitigation measures such as hand washing and social distancing could have impacted on the results.
UKHSA conclude that the results are broadly in line with the previous review; but that addition of RCTs and substantially more individual-level observational studies increase the certainty of the results and strengthens the evidence for the effectiveness of face coverings in reducing transmission in community settings. The authors of the large cluster RCT estimated that an increase from 0% to 100% of people wearing face coverings over the nose and mouth would be associated with 32% decrease in symptomatic COVID-19 seroprevalence.
A narrative systematic review [footnote 10] identified by our updated search (Appendix A) focuses on aerosol particle size, transmission in the air and filtering and barrier properties of masks and reports that factors determining mask effectiveness are filter efficiency, facemask fit and proper use. Cloth masks provide marginal protection and surgical offer 30% to 50% against particles meeting aerosol definition. N95 masks provide better protection but effectiveness is still dependent on fit and proper use. Perhaps uncontroversially they conclude mask wearing “should only be considered a measure of protection rather than a complete control method”. A modelling study suggests that differences in variations in mask efficacy can be explained by differences in virus abundance in the environment. [footnote 11] Most environments and contacts are in conditions of low viral abundance, and surgical masks are effective, but virus rich environments require masks with greater filtering and barrier properties and overall masks are particularly effective in combination with other preventive measures.
Nonetheless, findings are overall consistent with research reported to SAGE on 10 September 2020 [footnote 12] that N95 or FFP2 [footnote 13] mask (penetration by contaminants < 0.01%) is better than medical mask (penetration 44%) which is better than general cloth mask (penetration 97%). The latter thus may offer the wearer reassurance, but little or no real protection. A rapid review by PHE (1 October 2020) of factors associated with COVID-19 in care homes and interventions to prevent ingress and transmission identified only weak observational evidence for universal mask wearing in residential care as part of fuller package of interventions and identifies the need for further research on all interventions including PPE and mask use in residential care settings.
Other PPE – gloves, gowns, eye protection
The living review also reports associations between use of gloves, gowns, eye protection, shoe covers, and decreased risk of transmission (29 studies included in update 10). Studies are reasonably consistent in that full PPE use (gloves, mask, gown, and eye protection) was associated with decreased risk of infection compared to partial or no PPE use (ORs from 0.03 to 0.68). Some studies however find association between PPE use (including glove use) and increased risks. These findings likely relate to PPE use being a marker of exposure risk, inadequate training and inconsistent use (for example findings of staff not wearing PPE in staff rooms during breaks), and methodological issues in the studies.
The Cochrane review (version 15 May 2020 as reported in September 2020) on PPE use [footnote 14] with infectious diseases included 24 studies, (22 simulation studies, 14 randomised). The review evaluates which types of full-body PPE, and which donning and doffing methods, have the least risk of contamination, and which training methods increase compliance. Overall, the authors found low- to very low-certainty evidence that covering larger areas of the body results in better protection. Gowns may provide better protection against contamination than aprons. PPE made of breathable material, which is associated with greater user satisfaction, was not demonstrated to be worse than water repellent material. The evidence is limited, based on small sample simulation studies. The review also highlights low-certainty evidence from one SARS-related study and 2 simulation studies that more active training (video and computer simulation or face-to-face training) in PPE use decreases noncompliance with donning and doffing guidelines to a greater extent than passive training (lectures only). At December 2021 there has been no update on this review since May 2020.
The HSE report [footnote 15] on aprons, gowns and eye protection draws on the Cochrane review as providing core evidence and concludes that aprons and gowns are suitable, but points to pros and cons during donning, use and doffing. HSE also point out the lack of evidence on the effectiveness of goggles or face shields. No evidence is identified that directly relates to residential social care settings.
Our updated search identified one new review of direct relevance since June 2021. This review [footnote 16] assesses the utility of face shields as protection from coronavirus transmission for healthcare workers, with 7 studies fulfilling their inclusion criteria. The use of a face shield alone as protection against COVID-19 is insufficient. They conclude face shields should not be used for respiratory protection, much less replace it, and should be used simultaneously with other forms of protection including masks, other PPE and IPC measures. N95 should be used when there is risk of aerosol. They highlight that there are no industry standards for face shields, with numerous different models on the market, requiring rigorous evaluation of both their protective and usability properties.
PPE in social care settings
A review by Khunti et al. [footnote 17] (August 2020) highlights that most of the guidance surrounding PPE use focuses on emergency or inpatient care settings and it is often assumed that primary or community care settings (which may include social care) are at low risk in comparison. The reality is likely much more nuanced, as community care may often expose healthcare workers and those they care for to a high degree of risk through close prolonged contact (see below, [footnote 18] ) . The Khunti et al review found little direct evidence for the effectiveness of PPE in primary or community care. However, indirect evidence from single-centre experimental studies supports the appropriate use of PPE in community and social care settings according to PHE [footnote 18] and WHO [footnote 19]guidelines in order to protect against COVID-19. The reviews discussed above on community use of masks strongly reinforces this view.
One study, new to the living review update 10, reports on PPE use in nursing homes in the USA finding increased risk related to PPE use (OR =2.18 (1.26 to 3.80)). The authors of that study [footnote 20] were at pains to point out the higher rates of infection in nursing home personnel in their study compared to hospital personnel (13.1%, (11.5% to 14.9%) compared to 3.1%, (2.7% to 3.5%)). They point to the use of PPE in nursing homes as being a marker of the infection risk related of where staff were working (such as on a COVID-19 unit), potentially exacerbated by staffing shortages, poor training, and artefacts related to staff workplace allocations and seropositivity from earlier infection.
Training [footnote 21]
The living review reports a consistent association across studies between infection control training and decreased infection risk, with not being trained being associated with higher risk. However only one study reports a significant relationship. The evidence is limited as risk factor studies are retrospective, with the possibility of recall bias regarding use of PPE. None of the studies used an RCT design, some studies did not control for confounders, and those that did were limited in their ability to control for exposure. PHE and NHS launched an IPC toolkit in July 2021 for NHS organisations. [footnote 22] It follows a conventional booklet format available online, but has not been formally evaluated.
Behaviour
Behavioural measures to support proper doffing and donning and general infection control measures should be promoted in tandem with PPE use. [footnote 23] Research from healthcare settings emphasises the importance of training staff in correct donning and doffing procedures and safe disposal of PPE after use. However, none of the associations in the living review between infection and donning/doffing procedures or with training in donning/doffing are significant.
Hand hygiene
Handwashing is also considered in the living rapid review with 4 studies reporting on association with risk of SARS-CoV-1 infection, generally with poor practice being associated with increased risk. However only one study reports significant results with poor handwashing practice having OR =2.64 (1.04 to 6.71). As a key intervention of known effectiveness, handwashing recommendations should be applied across the board for all healthcare workers. Hand hygiene guidelines are generally informed by the WHO’s ‘five moments for hand hygiene’ [footnote 24] which recommend that healthcare workers clean their hands:
- before touching a patient
- before clean and aseptic procedures
- after body fluid exposure or risk
- after touching a patient
- after touching patient surroundings
Hand hygiene is a behaviour very amenable to behavioural intervention and use of behaviour change techniques, and more effort is needed in this regard. [footnote 25]
Use of PPE
It is highly likely that correct and comprehensive use of masks, gloves, gowns, eye protection, and so on, together with behavioural infection control measures, such as hand washing and physical distancing, will result in a decreased risk of coronavirus transmission. Handwashing is an intervention available in all healthcare settings. However, a major caveat relating to PPE is that these procedures must be properly instigated (including donning and doffing) and consistently followed if they are to be effective. Standard precautions should be taken where risk is low (such as handwashing and use of masks). Contact and droplet precautions should be taken for suspected or confirmed cases of COVID-19 (such as handwashing, mask, gown, googles, and gloves). To date the literature related to SARS-COV-2 and training in use of PPE suggests that far more needs to be done to ensure social care staff are properly trained.
Our updated search (Appendix A) identified a further review of training in use of PPE focussing on donning and doffing. [footnote 26] Although PPE skills can be mastered in a controlled learning environment, maintaining the integrity of the procedure during critical situations is challenging. The review highlights the opportunities for e-learning and other technology solutions to provide training and education under pandemic conditions but that much more work is required, especially in terms of clinical benefits to patients. We also identified a review and meta-analysis of IPC measures in general workplace settings. [footnote 27]Meta-analyses revealed lower COVID-19 positivity estimates in workplace settings that implemented combined measures compared with settings that applied single measures. Combinations of PPE, timely and thorough outbreak investigation (contact tracing and isolation), syndromic surveillance and testing, and staff zoning emerge as important considerations. They also highlight that these measures should be paired with improved building ventilation and indoor air quality.
Two reviews identified by our updated search identify adverse effects to PPE use amongst healthcare workers, including dermatological reactions to PPE use [footnote 28] and headaches related to PPE use. [footnote 29] Perhaps not surprisingly mask use is associated with adverse skin reactions around the mouth, cheeks and nose (mask wearing median 57% adverse reactions). Duration of wearing is associated with occurrence and severity. The evidence on type of mask is unclear but N95 masks appear to be associated with more problems. Many reactions are relatively minor, if uncomfortable, and wearers benefit from prophylactic use of hydrocolloid dressing on pressure areas. There is widespread self-report of headache related to mask or goggle use (26% to 91%). Type of mask (surgical compared to N95) and how long the mask is worn during a shift are important variables for headache generation.
Another potential factor to consider in relation to frail or older people is the risk of falls from long gowns or other ill-fitting PPE, although currently there is no literature reporting on PPE trip hazards. Providing care for people with communication issues relating to deafness or cognitive impairment can provide additional challenges when it comes to PPE use. For people with hearing loss, mask use results in reduced acoustic transmission and prevents lip reading, and may also be uncomfortable for those wearing hearing devices. [footnote 30] Furthermore, mask use is not suitable for those with severely compromised respiratory systems [footnote 31] or those who cannot remove or adjust their own masks. [footnote 32] Many residents will fall into these categories and hence mask use is more often observed amongst staff and visitors rather than residents themselves.
Apps
In May 2020, an app was launched by the NHS to support social care workers during the COVID-19 pandemic. [footnote 33] The app provided care workers in England with guidance and learning resources on crucial areas such as infection control, as well as wellbeing toolkits to support staff through the pandemic. The app was closed down on 31 March 2021. The Social Care Institute for Excellence (SCIE) has set up online hygiene training in response to the COVID-19 pandemic for care providers. This course covers the basics of infection control (how infections spread and how to prevent spread, hand hygiene, managing the care environment, laundry safely, use of PPE, and waste disposal) and is reported as taking about 30 minutes to complete online. As far as we know, the effectiveness of the course has not been evaluated. An existing evidence-based digital intervention was adapted for the COVID-19 pandemic with recent evidence for change in intentions to improve infection control behaviours. [footnote 34] Whilst Germ Defence was designed for the public it is relevant to social care workers, both in their home lives and their work lives and should be promoted. NIHR have recently funded an initial study to modify Germ Defence for residential care settings.
Conclusion
The evidence reviewed in this briefing is all based on studies undertaken before the identification of the Omicron variant, and indeed in populations that did not have the levels of vaccination currently observed in UK social care staff, residents or the UK general public. That said there is no obvious reason to reject the evidence presented herein. Overall there is likely to be an intersection between high risk, high exposure and low resource, which needs to be addressed when considering how best to reduce transmission across different health and social care settings. It is highly likely that the use of masks, gloves, gowns and other PPE together with behavioural infection control measures, such as hand washing, will result in a decreased risk of coronavirus transmission in social care. However the major caveat here is that these procedures must be properly instigated (including donning, doffing, and disposal of used PPE) and consistently followed if they are to be effective. There is little direct evidence for the effectiveness of PPE in social care, but we recommend that infection control measures are implemented based on the WHO risk classification. Standard precautions should be taken where risk is low (such as handwashing and use of masks). Contact and droplet precautions should be taken for suspected or confirmed cases of COVID-19 (such as handwashing, mask, gown, googles, and gloves). Situations in which there is likely to be aerosol generation require further measures.
This paper presents independent research funded by the National Institute for Health Research. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care or its partners.
Appendix A – Search strategy
PPE and social care – Search strategy (update 1 December 2021)
Please note, identical search strategy until 14 May 2021 for previous update yielded 39 papers, only 2 of which were relevant.
Search for PPE effectiveness in health and social care:
a) Google Scholar keywords and terms:
- personal protective equipment
- PPE
- effectiveness
- health care professionals
- social care workers
- residential care
- community health services
- COVID-19
b) MEDLINE (Ovid) Search Strategy Flow Chart:
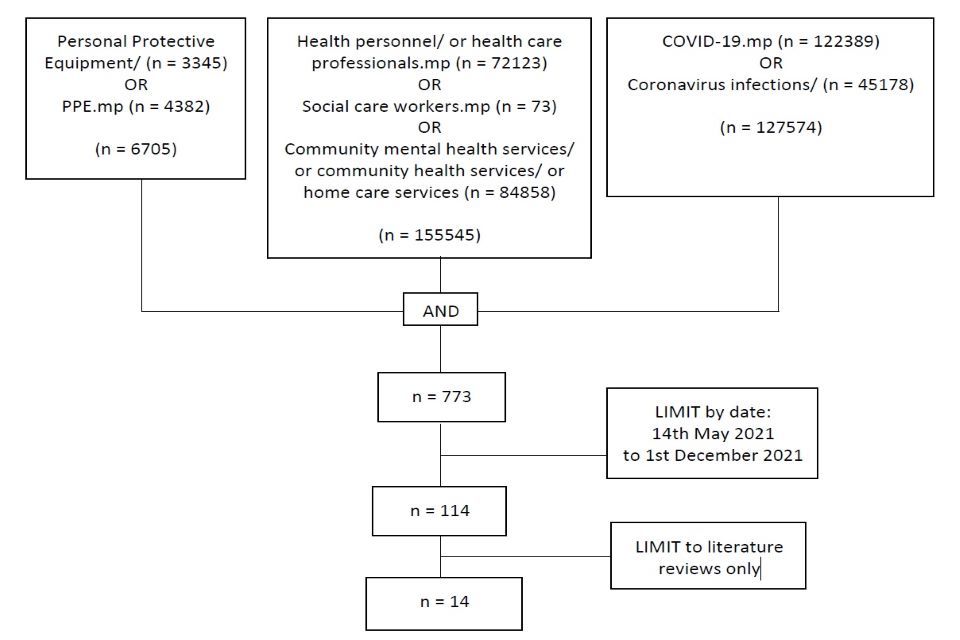
Flowchart search strategy looking at PPE, healthcare professionals, Social care workers, Community mental health services, community health services, homecare services, Coronavirus infections. Then date: 14 May to 1 December 2021 and literature reviews.
Title, abstract and full text review identified 7 of 14 papers total as not presenting data relevant to this review. The 7 remaining papers are referenced in this briefing.
Appendix B – Evidence map from Chou et al 2021
| Risk factor | Size of evidence | Strength of evidence and effect |
|---|---|---|
| Age | More than 50 studies with more than 200,000 health care workers | Moderate strength of evidence with no association on effect |
| Sex | More than 50 studies with more than 200,000 health care workers | Moderate strength of evidence with no association on effect |
| Race or ethnicity | 20 to 50 studies with more than 100,000 health care workers | Moderate strength of evidence with positive association on effect |
| Antibody status | Less than 10 studies with less than 20,000 health care workers | Low strength of evidence with negative association on effect |
| Health Care Worker role | More than 50 studies with more than 200,000 health care workers | Moderate strength of evidence with no association on effect |
| Directness or intensity of contact | More than 50 studies with more than 200,000 health care workers | Low strength of evidence with positive association on effect |
| Participation in high risk procedure | 20 to 50 studies with more than 100,000 health care workers | Low strength of evidence with positive association on effect |
| Education or training | Less than 10 studies with less than 20,000 health care workers | Low strength of evidence with negative association on effect |
| Mask use | 10 to 20 studies with more than 50,000 health care workers | Low strength of evidence with negative association on effect |
| PPE use | 20 to 50 studies with more than 100,000 health care workers | Moderate strength of evidence with negative association on effect |
Chou R, et al. Update alert 10: epidemiology of and risk factors for coronavirus infection in health care workers. Ann Intern Med. 16 November 2021. [Epub ahead of print]. doi:10.7326/M21-4294 Supplementary Tables.
References
-
Reported in Social Care Working Group update paper, 23 September 2020. Tabled at Scientific Advisory Group for Emergencies Meeting 59; 24 September 2020 (accessed 10 December 2021. ↩
-
What are the appropriate mitigations to deploy in care homes in the context of the post vaccination risk landscape? Social Care Working Group paper submitted to Scientific Advisory Group for Emergencies Meeting 90; 27 May 2021. Accessed 10 December 2021. ↩
-
UK Health Security Agency. The effectiveness of face coverings to reduce transmission of COVID-19 in community settings: A rapid review update 2 , 2021. Accessed 10 December 2021. ↩ ↩2
-
Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers: A Living Rapid Review. Ann Intern Med. 2020;173(2):120-136. doi:10.7326/M20-1632. ↩ ↩2
-
Chou R, et al. Update alert 9: epidemiology of and risk factors for coronavirus infection in health care workers. Ann Intern Med. 1 June 2021. [Epub ahead of print]. doi:10.7326/L21-0302. ↩ ↩2
-
Chou R, et al. Update alert 10: epidemiology of and risk factors for coronavirus infection in health care workers. Ann Intern Med. 16 November 2021. [Epub ahead of print]. doi:10.7326/M21-4294. ↩ ↩2
-
Chou et al initially updated the living review monthly, then changed to a bi-monthly schedule. As evidence shows little change month-on-month in June 2021 the review moved to a bi-annual update schedule. The initial review in 2020 extrapolated from results of studies on non-SARS-CoV-2 specific data. The more recent updates have focused on data from studies of SARS-CoV-2 infection. This, and slight changes to the search and inclusion criteria, has resulted in changes in the numbers of papers included over time. Thus numbers of paper reported here may not be completely consistent with numbers reported in the 2 previous versions of this briefing. ↩
-
Review updates 9 and 10 add 3 new studies, thus 11 studies are included in update 10. ↩
-
This OR of 1.70 is based on a study where only 2 of 478 persons total did not wear masks. ↩
-
Locke L, Dada O, Shedd JS. Aerosol Transmission of Infectious Disease and the Efficacy of Personal Protective Equipment (PPE): A Systematic Review. J Occup Environ Med. 01 November 2021;63(11):e783-e791. doi: 10.1097/JOM.0000000000002366. ↩
-
Cheng Y, Ma N, Witt C, Rapp S, Wild PS, Andreae MO, Pöschl U, Su H. Face masks effectively limit the probability of SARS-CoV-2 transmission. _Science._20 May 2021:eabg6296. doi: 10.1126/science.abg6296. Epub ahead of print. ↩
-
Processing Methods to Facilitate the Re-Use of Personal Protective Equipment (PPE). Paper presented to SAGE Meeting 56, 10 September 2020. ↩
-
HSE Rapid evidence review: Part 1 Equivalence of N95 and FFP2 masks, concludes there is no material difference between N95 and FFP2 masks and both would provide comparable protection against coronavirus as long as the wearer was face-fit tested. Since this review UK IPC guidance has been updated and requires FFP3 respirators to be worn where AGPs are being performed. Accessed 10 December 2021, webpage last updated 9 December 2021. ↩
-
Verbeek JH, Rajamaki B, Ijaz S, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2020;(5). doi:10.1002/14651858.CD011621.pub5. ↩
-
HSE Rapid evidence review: Part 2 Aprons, Gowns and eye protection., accessed 10 December 2021, webpage last updated 09 December 2021. ↩
-
de Oliveira E Silva AC, Nogueira WP, Gir E, de Almeida SA, de Lima Barroso BI, Freire MEM. Limiting factors of face shield use for health professionals during the COVID-19 pandemic. Work. 2021;70(2):355-363. doi: 10.3233/WOR-210542. PMID: 34633340. ↩
-
Khunti K, Adisesh A, Burton C, et al. The efficacy of PPE for COVID-19-type respiratory illnesses in primary and community care staff. Br J Gen Pract. 2020;70(697):413-416. doi:10.3399/bjgp20X710969. ↩
-
Public Health England. Coronavirus (COVID-19): personal protective equipment (PPE) hub. Updated July 2020. Accessed 18 May 2021. ↩ ↩2
-
World Health Organization. Prevention, identification and management of health worker infection in the context of COVID-19 . Updated October 2020. Accessed 18 May 2021. ↩
-
Akinbami LJ, Chan PA, Vuong N, et al. Severe Acute Respiratory Syndrome Coronavirus 2 Seropositivity among Healthcare Personnel in Hospitals and Nursing Homes, Rhode Island, USA, July to August 2020. Emerging Infectious Diseases. 2021;27(3):823-834. doi:10.3201/eid2703.204508. ↩
-
Two new studies were added at update 9 and none at update 10. ↩
-
NHSE and PHE Supporting excellence in infection prevention and control behaviours: Implementation Toolkit, accessed 16 December 2021. ↩
-
Greenhalgh T, Chan XHS, Khunti K, et al. What Is the Efficacy of Standard Face Masks Compared to Respirator Masks in Preventing COVID-Type Respiratory Illnesses in Primary Care Staff? Centre for Evidence-Based Medicine; 2020. Accessed 20 May 2021. ↩
-
Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67(1):9-21. doi:10.1016/j.jhin.2007.06.004. ↩
-
Price L, MacDonald J, Gozdzielewska L, Howe T, Flowers P, Shepherd L, Watt Y, Reilly J. Interventions to improve healthcare workers’ hand hygiene compliance: A systematic review of systematic reviews. Infect Control Hosp Epidemiol. December 2018;39(12):1449-1456. doi: 10.1017/ice.2018.262. PMID: 30526716. ↩
-
Nayahangan LJ, Konge L, Russell L, et al. Training and education of healthcare workers during viral epidemics: a systematic review. BMJ Open 2021;11:e044111. doi:10.1136/ bmjopen-2020-044111. ↩
-
Ingram, C.; Downey, V.; Roe, M.; Chen, Y.; Archibald, M.; Kallas, K.-A.; Kumar, J.; Naughton, P.; Uteh, C.O.; Rojas-Chaves, A.; et al. COVID-19 Prevention and Control Measures in Workplace Settings: A Rapid Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 7847. ↩
-
Montero-Vilchez T, Cuenca-Barrales C, Martinez-Lopez A, Molina-Leyva A, Arias-Santiago S. Skin adverse events related to personal protective equipment: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. October 2021;35(10):1994-2006. doi: 10.1111/jdv.17436. ↩
-
Ong JJY, Chan ACY, Bharatendu C, Teoh HL, Chan YC, Sharma VK. Headache Related to PPE Use during the COVID-19 Pandemic. Curr Pain Headache Rep., June 2021 15;25(8):53. doi: 10.1007/s11916-021-00968-x. ↩
-
Trecca EMC, Gelardi M, Cassano M. COVID-19 and hearing difficulties. Am J Otolaryngol. 2020;41(4):102496. doi:10.1016/j.amjoto.2020.102496. ↩
-
Kao T-W, Huang K-C, Huang Y-L, Tsai T-J, Hsieh B-S, Wu M-S. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc Taiwan Yi Zhi. 2004;103(8):624-628. ↩
-
Desai AN, Aronoff DM. Masks and Coronavirus Disease 2019 (COVID-19). JAMA. 2020;323(20):2103. doi:10.1001/jama.2020.6437. ↩
-
Department of Health and Social Care. Dedicated app for social care workers launched. Published May 2020. Accessed 18 May 2021. The app was closed on 31 March 2021. ↩
-
Ainsworth B, Miller S, Denison-Day J, Stuart B, Groot J, Rice C, Bostock J, Hu X, Morton K, Towler L, Moore M, Willcox M, Chadborn T, Gold N, Amlôt R, Little P, Yardley L. Infection Control Behavior at Home During the COVID-19 Pandemic: Observational Study of a Web-Based Behavioral Intervention (Germ Defence) J Med Internet Res 2021;23(2):e22197 doi:10.2196/22197. ↩
