Sero-surveillance of COVID-19
Updated 29 July 2021
Control of COVID-19 requires the ability to detect asymptomatic and mild infections, that would not present to healthcare and would otherwise remain undetected through existing surveillance systems. This is important to determine the true number of infections within the general population to understand transmission, to inform control measures such as social distancing and school closures and to provide a denominator for the estimation of severity measures such as infection fatality and infection hospitalisation ratios.
A number of serological collections have been established by PHE to provide an age-stratified geographically representative sample across England over time. These include samples from healthy adult blood donors, supplied by the NHS Blood and Transplant (NHS BT). Donor samples from different geographic regions (approximately 1000 samples per region) in England are tested each week. The results presented here are based on testing using the Euroimmun assay. Figure 1 shows the overall prevalence in each region over time which has been adjusted for the accuracy of the Euroimmun assay (sensitivity and specificity).
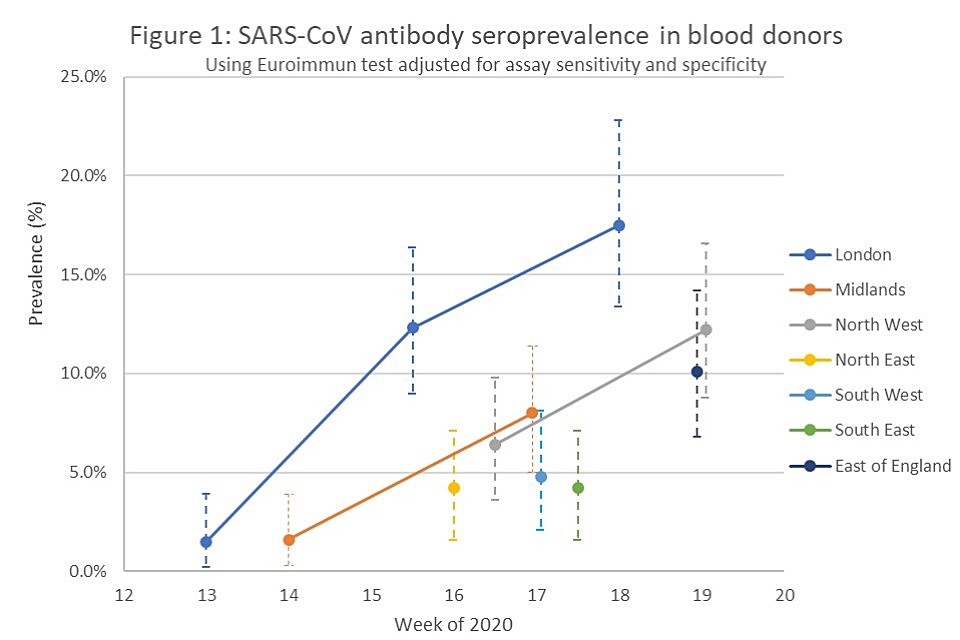
Graph showing sars-cov antibody seroprevalence in blood donors
After making adjustments for the accuracy of the assay and the age and gender distribution of the population, the overall adjusted prevalence in London increased from 1.5% in week 13 to 12.3% in weeks 15 to 16 and 17.5% in week 18.
The estimates among adults show a continued increase in prevalence within London, however the increase seen between weeks 16 and 18 is relatively smaller than the increase observed between weeks 13 and 16. Given that the antibody response takes at least two weeks to become detectable, those displaying a positive result in week 18 are likely to have become infected before mid-April. As the incidence in this period may only have just begun to slow following the impact of lockdown measures, this may explain the slight increase over that period.
The lower prevalence in the samples from other regions including the Midlands, North East, South East and South West regions is consistent with data from other surveillance systems. The adjusted prevalence in the Midlands in week 14 was similar to that in London in weeks 13 to 14 but lower in week 17 compared with later sampling in London. The adjusted prevalence in North East and North West regions in weeks 16 is well above baseline (4.2% and 6.4% respectively), higher than in London and the Midlands in week 14, but not as high as seen in London in week 16, which is consistent with the surveillance trends reported for England.
The highest adjusted prevalence in all regions is found among adolescents and young adults in the 17 to 29 year old age group (varying from 6.3% in the South East to 20.5% in the North West regions). However, in the most recent data from London, the increase is more marked in older age groups suggesting that this population have been affected later. These patterns may reflect differences in behaviour and mixing patterns in the different age groups.
Latest version of this information is available in the week 22 report
