Investigation into monkeypox outbreak in England: technical briefing 3
Updated 19 December 2024
Applies to England
The UK Health Security Agency (UKHSA) is working with the NHS and the public health agencies of the 4 nations to investigate the monkeypox outbreak in recent weeks. This briefing is produced to share data useful to other public health investigators and academic partners undertaking related work. It includes early evidence and preliminary analyses which may be subject to change.
Data reported in the technical briefing are as of 6 July 2022 (or as specified in the text) to allow time for analysis.
Potential levels of the outbreak in England
The outbreak can be considered to fall into 1 of 4 potential levels of transmission.
Level 1
Incursions from rest of the world – small numbers of imported cases with limited onward transmission.
Level 2
Transmission within a defined sub-population.
Level 3
Transmission within multiple sub-populations or larger sub-population.
Level 4
Wider significant community transmission – with potential for endemic and local epi-zoonotic disease.
These may be refined with better understanding of modes of transmission.
At present, England is judged to be in Level 2 and is being closely monitored for any evidence of Level 3.
Part 1. Risk assessment
Monkeypox Technical Group – data and analysis as of 6 July 2022.
UK trajectory
Nowcast and growth
Incidence continues to grow.
The UKHSA monkeypox nowcasting model implies positive growth between 3.8% to 6.7% per day, corresponding to a doubling time of 15 days (90% CI: 10 days, 18 days). This is consistent with modelling from academic partners, which is not included in this report.
Assessment (confidence): the outbreak in the UK is growing (high).
Geographic spread
The proportion of cases in London is relatively stable at 74% of cases in England.
Assessment (confidence): cases are concentrated in London (moderate).
Ascertainment
Whilst testing is freely available and a mixed population group is being tested, it is likely that there is under ascertainment. Atypical symptoms, including single or scarce lesions, are reported and there are international reports of subclinical infection. A high proportion of cases (79%) for which there is information have no known contact with a confirmed case although this data is primarily available from earlier in the outbreak.
Assessment (confidence): insufficient information.
UK transmission
Outbreak level
There is considerable data lag. Of cases with information, 97% (681 out of 699) are in gay, bisexual and men who have sex with men (GBMSM). Trends in key epidemiological indicators from case questionnaires are stable, indicating transmission remains within the known high risk GBMSM group, although coverage of questionnaire data is now just 31%.
Where known, more than half had history of STI in the last year (54%, 233 out of 445); 30% (123) were living with HIV; 16% (67 out of 445) had one or no sexual partners, and 31% (134) had 10 or more sexual partners in the last 3 months. There have been 4 female cases and one child (under 16) in 2022 in England. Indications that transmission has moved outside the current network would be multiple cases in women or children. Despite potential uncertainty around ascertainment, there is no evidence of this in the UK at present.
Assessment (confidence): level 2 (moderate).
Route of transmission
Whilst the primary reported route is through close or sexual contact, monkeypox virus has been detected in air and environmental samples in the hospital room of infected patients. There are no confirmed instances of airborne transmission. Limited household transmission has been described in the UK.
Assessment (confidence): transmitting primarily through close or sexual contact (moderate).
Severity
Observed clinical severity
Approximately 10% of cases receive hospital care but this includes some cases admitted as unable to isolate at home. Antiviral therapy is an unreliable indicator at present. There are no reported deaths in the UK. In the 2022 global outbreak, 3 deaths have been reported from 6,027 cases. There is significant morbidity in the majority of people who are admitted to hospital for clinical care reasons, including complications due to secondary bacterial infection.
Assessment (confidence): in current population group, low mortality but significant morbidity (moderate). In wider population, insufficient data.
Virological characterisation
Outbreak cases are current in a distinct clade which has mutations of unknown significance. There is evidence suggestive of previous human transmission but not clear-cut evidence of adaptation for improved human transmission. There are no phenotypic data available for this clade to date.
Assessment (confidence): insufficient data.
International trajectory
Global growth
The number of cases reported internationally and the number of countries with cases continues to increase steeply and is most compatible with growth. However, the data are also likely to be affected by rapid changes in ascertainment.
Assessment (confidence): the global outbreak is growing (moderate).
International transmission
Routes of transmission reported by other countries
Cases in previously non-endemic countries are reported as primarily in GBMSM. Outside the UK, 3 confirmed cases in children have recently been reported in Europe and this signal requires close monitoring. In countries with a longer history of monkeypox, apparent wider population transmission is reported with unclear routes.Phylogenetic data suggests that human transmission has been occurring for a number of years in some areas prior to the appearance of the outbreak clade and there is at present no reason to assume that the epidemic as a whole will naturally reduce without interventions globally.
Assessment (confidence): transmitting primarily by close or sexual contact in non-endemic countries (low), with unknown transmission routes in endemic countries.
Part 2. Research and evidence gaps prioritisation
UKHSA has carried out a research and evidence gaps analysis relating to the monkeypox outbreak in the UK. We are working collaboratively with academic partners, including National Institute for Health and Care Research (NIHR) Health Protection Research Units and national research funders, to develop and implement rapid studies to address these.
Groups of questions were initially identified under the themes of:
- surveillance
- transmission dynamics
- biological characteristics and virology
- clinical characterisation
- vaccine response and immunology
- therapeutics
- diagnostics
- behavioural, social science and inequalities considerations
- evaluation of interventions
- other
The questions were tested and discussed with a range stakeholders and collaborators, then assigned as immediate, high and longer-term priority to aid UKHSA’s response to the outbreak.
As knowledge and information emerges, we continue to share updates and developing protocols with our stakeholders and collaborators, including national research funders.
Part 3. Epidemiology update
3.1 Current epidemiological situation
Cases of monkeypox infection were confirmed in England from 6 May 2022. The outbreak has mainly been affecting people without documented history of travel to endemic countries. Up to 6 July 2022 there were 1,517 laboratory confirmed cases in the UK, of which 6 were female. Of the confirmed cases 41 were in Scotland, 11 in Northern Ireland, 18 in Wales and 1,447 were in England. The median age of confirmed cases in the UK was 36 years old (interquartile range 31 to 43).
Table 1. Number of laboratory confirmed cases by devolved administrations, 6 May 2022 to 6 July 2022 (n=1,517)
| Devolved administrations | Confirmed cases |
|---|---|
| England | 1,447 |
| Northern Ireland | 11 |
| Scotland | 41 |
| Wales | 18 |
| Total | 1,517 |
In England, a high proportion of cases were known to be London residents (74%, 890 out of 1,196 with reported home address), see Table 2.
Table 2. Number of laboratory confirmed monkeypox cases by region of residence, England, March to 6 July 2022
| Region of residence | Total confirmed |
|---|---|
| East of England | 50 |
| East Midlands | 14 |
| London | 890 |
| North East | 17 |
| North West | 71 |
| South East | 91 |
| South West | 21 |
| West Midlands | 22 |
| Yorkshire and Humber | 20 |
| Unknown* | 251 |
| Total | 1,447 |
*Address not yet confirmed
Figure 1 demonstrates symptom onset dates of confirmed cases in England, where known. The median reporting delay, calculated here as the time between symptom onset date and date first included in UKHSA surveillance data, was 10 days for cases newly reported in the week starting 27 June 2022. The reporting delay has improved since early in the incident, from 12 days for cases reported in the week starting 16 May 2022.
Figure 2 shows the number of cases by the day of the laboratory result. Where gender information was available, 1,400 out of 1,406 (99.7%) confirmed cases were male, with 4 confirmed female cases in England. Of these 4 cases in females, one was associated with travel to an endemic area of the world, and the other 3 had known links to confirmed monkeypox cases in England.
Recent foreign travel, within 21 days prior to symptom onset, was reported by 226 cases in England (16%), with 176 of these reporting travel within Europe (Figure 4).
Figure 1. Confirmed monkeypox cases by symptom onset date in England as of 6 July 2022. Dotted line represents reporting delay (between symptom onset and reporting date) of 16 days, based on 90% of cases between 26 June 2022 and 3 July 2022
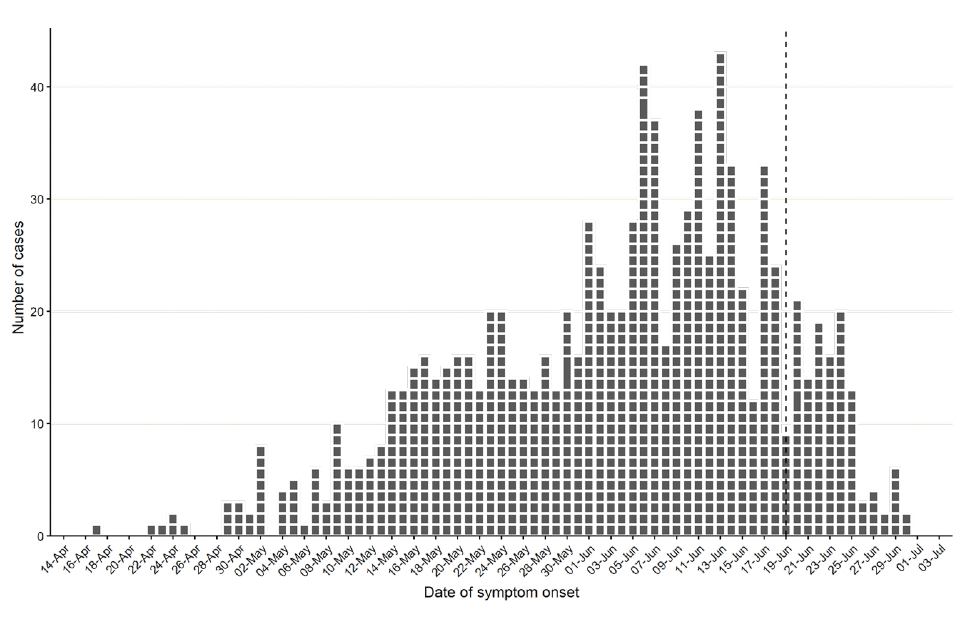
The data used in this graph can be found in the accompanying spreadsheet.
Figure 2. Incidence of confirmed monkeypox cases by laboratory result date in England as of 6 July 2022
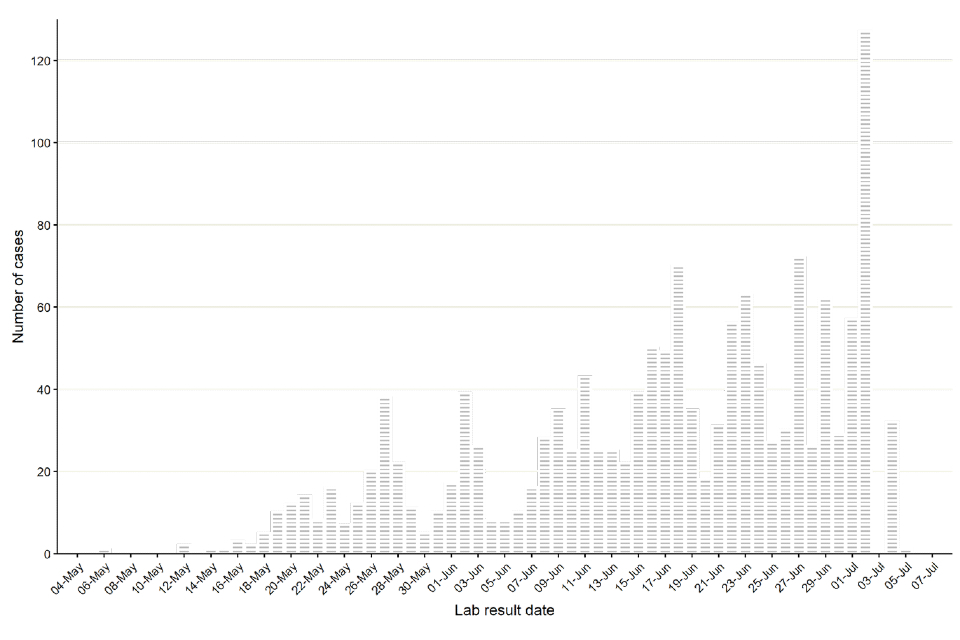
The data used in this graph can be found in the accompanying spreadsheet.
Figure 3. Age and sex distribution of confirmed Monkeypox cases by laboratory result date in England as of 6 July 2022
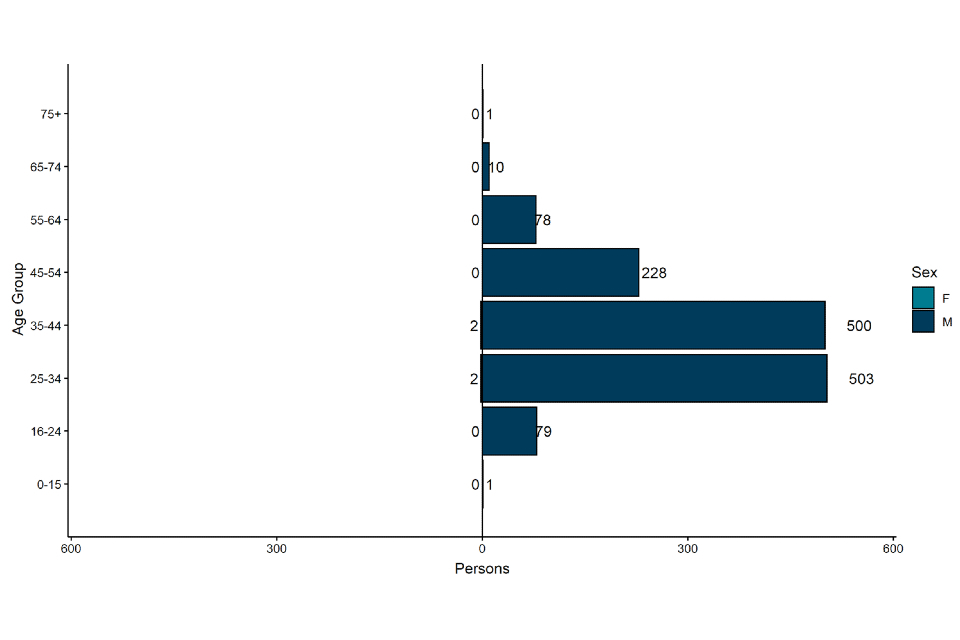
The data used in this graph can be found in the accompanying spreadsheet.
Figure 4. Cases with reported foreign travel within the 21 days prior to symptom onset as of 5 July
Travel data obtained from enhanced surveillance questionnaires and Public Health records (HPZone)
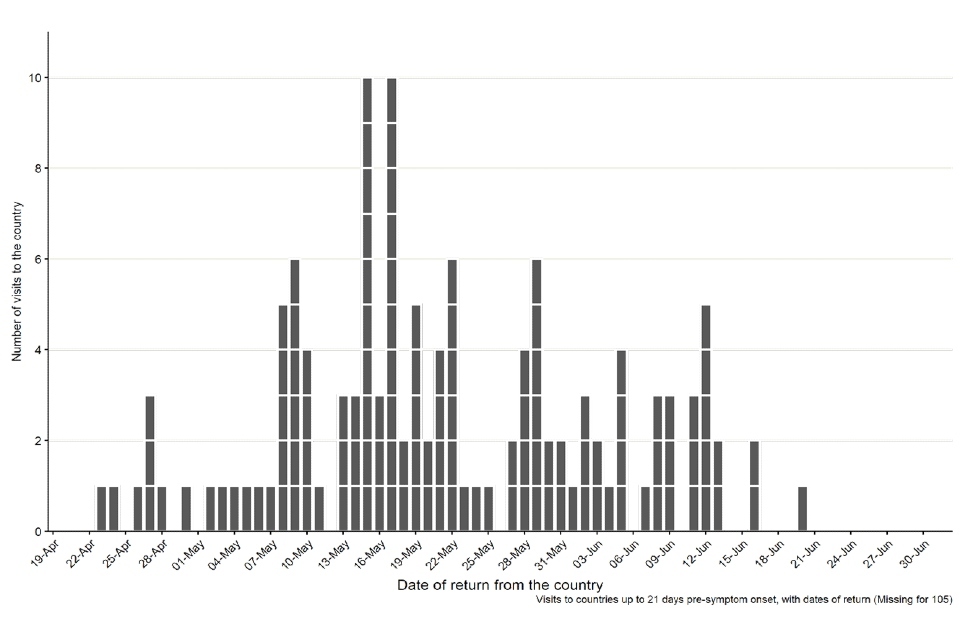
The data used in this graph can be found in the accompanying spreadsheet.
3.2 Findings from enhanced surveillance questionnaires
Of the 1,447 cases identified in England up to 6 July 2022, a total of 445 (30.8%) had enhanced surveillance questionnaires. This includes data collected via rapid sexual health questionnaires administered during the initial weeks of the outbreak (used from 27 to 31 May 2022), questionnaires completed by health protection teams during telephone interviews (used from 1 to 24 June 2022), and self-completed questionnaires sent electronically to cases (used from 25 June 2022 onwards).
As reported in technical briefing 1 and technical briefing 2, monkeypox is predominantly being transmitted in interconnected sexual networks of GBMSM (Table 3).
Table 3. Selected epidemiological metrics from enhanced surveillance questionnaires in confirmed monkeypox cases in England as of 6 July 2022
N=445, some metrics have slightly smaller denominators due to missing values
| Metric | N (%) |
|---|---|
| Gay, bisexual, or men who have sex with men | 427 (96.2%) |
| Travel abroad prior to symptom onset (21 days) | 136 (30.6%) |
| Age under 30 years | 86 (21.5%) |
| History of STI in the last year | 233 (53.7%) |
| One or no sexual partners in last 3 months | 67 (15.7%) |
| 10+ sexual partners in last 3 months | 134 (31.3%) |
| Living with HIV | 123 (29.5%) |
| On HIV treatment (among living with HIV) | 121 (99.2%) |
| Ever used PrEP (among HIV negative) | 222 (79.3%) |
Figure 5 shows trends of selected epidemiological metrics in a subset of 425 cases with completed questionnaires who had symptom onset dates between epidemiological weeks 18 to 25 (from 1 May to 25 June 2022). Cases with onset dates before or after these dates were excluded from these analyses due to small numbers.
Questionnaire data shows that, between epidemiological weeks 18 to 25, sustained transmission of monkeypox virus in England occurred in defined sexual networks of GBMSM, without significant week-by-week changes in these metrics.
Figure 5. Trends of selected epidemiological metrics in confirmed monkeypox cases by week of symptom onset in England, epidemiological weeks 18 to 25 (1 May 2022 to 25 June 2022)
N=425 with completed questionnaires in this time period
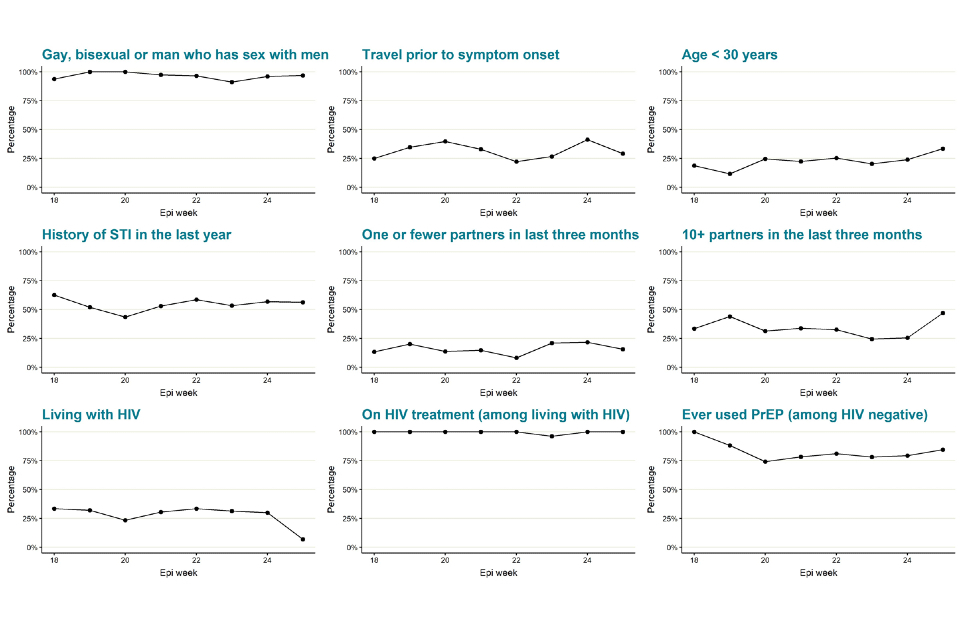
Supplementary data is not available for this figure. Due to delays between symptom onset and questionnaire completion, data for epidemiological week 25 is likely to change and should be interpreted with caution.
3.3 Common exposure settings
People with confirmed monkeypox were asked about attendance at venues and events during the time period when they may have acquired the infection, and also attendance when they may have been infectious. Information was collated from enhanced and rapid sexual health questionnaires, and from HPZone records (more recently introduced self-reported questionnaires are not yet included).
In total, 572 events were reported by 239 individuals: the majority of these, 546, were people who reported attending during the period when they may have acquired the infection. Note that attendance is not evidence that transmission occurred at that venue or event, and individuals may have attended multiple events.
Table 4. Event attendance among confirmed monkeypox cases in England as of 7 July 2022
| Event Type | % of total (n) |
|---|---|
| Festival** | 40% (226) |
| Sex-on-premise venue | 17% (98) |
| Bar | 12% (68) |
| Nightclub | 9% (50) |
| Sauna | 8% (45) |
| Gym/ swimming pools | 6% (33) |
| Private sex party | 4% (23) |
| Event | 3% (18) |
| Other | 2% (11) |
| Total | 100% (572)* |
*572 event or venue attendances reported by 239 unique cases.
**Some cases have attended the same festival or event over multiple dates; each date has been reported separately.
Only events or venues with at least 2 cases in attendance on a given date are included.
Common exposures were defined as instances where 2 or more people with confirmed monkeypox reported attending the same event or venue on the same day. As of 5 July 2022, there were 25 common exposures in London. Only one common exposure was reported elsewhere in England (in the North West region).
Figure 6. Timeline of self-reported attendance at London venues among confirmed cases during their incubation and/or infectious period
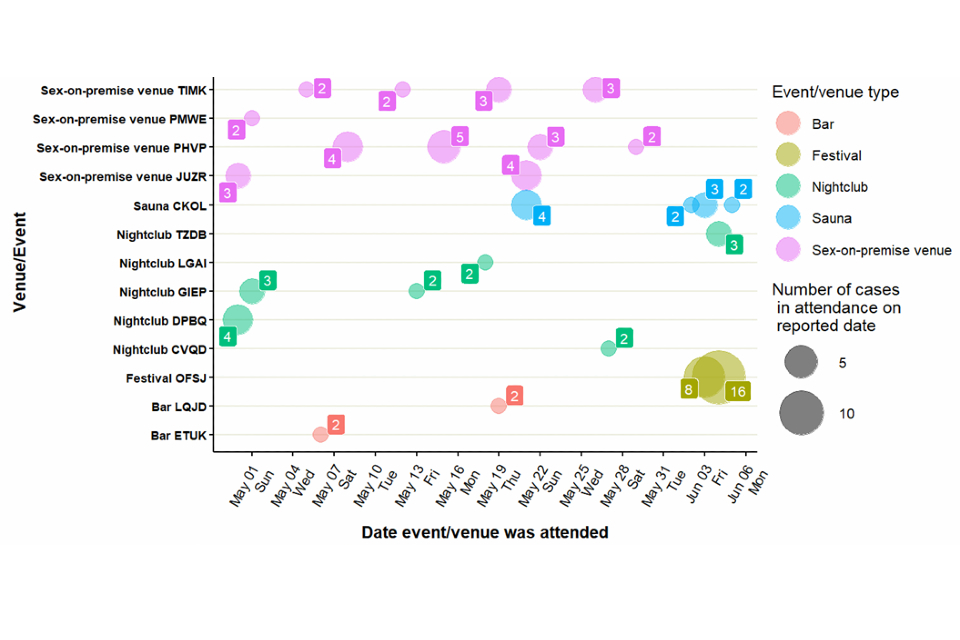
Source: event activity reported in enhanced case and rapid sexual health questionnaires, or manually extracted from case notes on HPZone. Data may be subject to reporting bias.
Only events with at least 2 cases in attendance on a given date are included.
A total of 275 attendances at London venues or events were reported by 170 unique cases.
A total of 27 attendances were excluded as no date provided.
Two-hundred-and-fifty-eight attendances at events or venues outside of the UK were also reported by 61 unique cases. These included festivals and venues in Spain (including Gran Canaria), Belgium and Israel.
Figure 7. Timeline of self-reported attendance at venues or events outside the United Kingdom, among confirmed cases during their incubation and/or infectious period
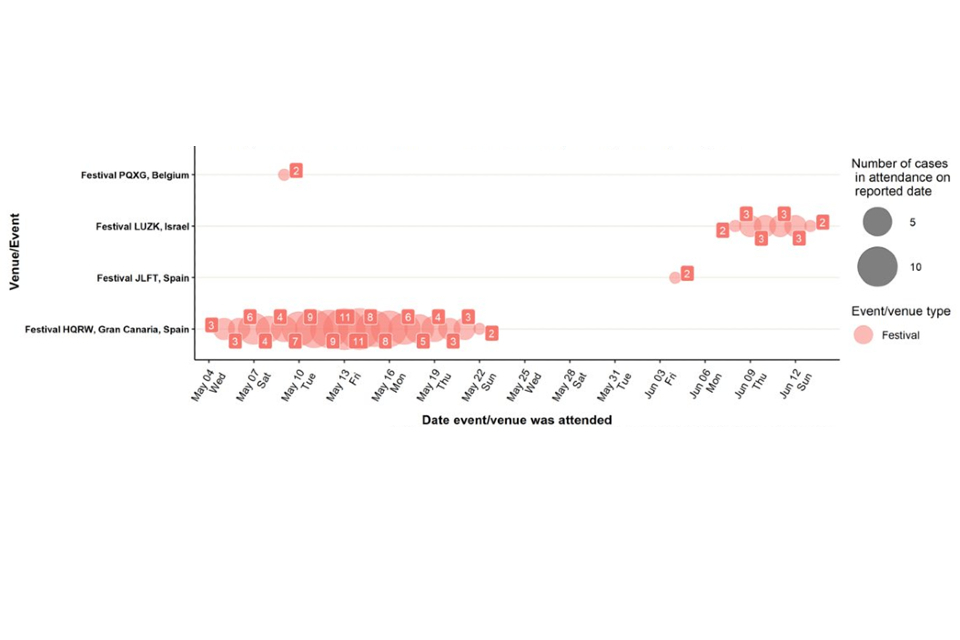
Source: event activity reported in enhanced case and rapid sexual health questionnaires, or manually extracted from case notes on HPZone. Data may be subject to reporting bias.
Only events with at least 2 cases in attendance on a given date are included.
A total of 258 attendances at venues or events outside the UK were reported by 61 unique cases.
A total of 9 attendances were excluded as no date provided.
3.4 Contact data
Information on named contacts is collected by UKHSA. This is not expected to be a complete dataset, as not all contacts may have been disclosed, or may not have been known or able to be named by the case (this is likely to affect sexual contacts in particular). A total 1,920 contacts were named to UKHSA by cases reported from 9 May 2022 to 5 July 2022. These contacts were named by a case without consideration of date of exposure or onset and may represent exposures during incubation or infectious periods. Among all named contacts, 349 (18%) were listed as sexual contacts. Being named as a contact is not evidence of where transmission, or even exposure may have occurred.
Of those 1,920 people named as contacts, 66 were also confirmed as cases by UKHSA. Where risk category of the contact was recorded, 11 had a category 3 exposure, and 1 had a category 2 exposure to a confirmed case: however, this person also reported other sexual contacts in their incubation period.
In addition, the setting for contact was reported as sexual for 39 of the 66 cases. Review of additional anecdotal information on the remainder suggests that intimate and/or sexual contact with the linked case or other (unlinked individuals) had occurred during the incubation period of the case and was likely to be the main transmission risk. Significant uncertainties, remain around the information collected, but there is currently a lack of evidence of transmission outside of close intimate or sexual contact.
3.5 Testing data
Analysis of orthopox screening and monkeypox testing carried out at UKHSA for this outbreak up to 5 July 2022 indicated that more adult men were screened for orthopox virus (2,672, 79% of all tests) compared to adult woman (356, 11% of all tests) and children (136, 4%). This analysis excludes the 3 first confirmed cases in England, reported in early May 2022, as these are considered separate incidents.
Monkeypox positivity rate was considerably higher in adult men, 51%, compared to less than 1% in adult woman and 0% in children.
Table 5. Monkeypox positivity rate by group, as of 5 July 2022
| Group | Result | Total | Positivity rate |
|---|---|---|---|
| Adult men [1] | Negative | 1,302 | N/A |
| Adult men [1] | Positive | 1,367 | 51.22 |
| Adult unknown [2] | Negative | 136 | N/A |
| Adult unknown [2] | Positive | 73 | 34.93 |
| Adult women [3] | Negative | 354 | N/A |
| Adult women [3] | Positive | 2 | 0.56 |
| Children [4] | Negative | 135 | N/A |
| Children [4] | Positive | 0 | 0 |
| Sex and age unknown [5] | Negative | 4 | N/A |
| Sex and age unknown [5] | Positive | 2 | 33.33 |
[1] Any person categorised as M and over 15 years old
[2] Any person that provided no information on sex and over 15 years old
[3] Any person categorised as F and over 15 years old
[4] Any person (of either sex) aged between 0 and 15 years old
[5] Any person with no information on sex or age
Part 4. Transmission dynamics
There is little evidence that transmission dynamics have changed substantially since technical briefing 2. Nowcasting, the specimen date, suggests that growth in the incidence of monkeypox has continued and this is consistent with cases by report date.
4.1 Nowcasting by specimen date
As the epidemic has grown, the availability of data with recorded symptom onset date has declined. This biases the epidemic curve by symptom onset date, since the proportion of cases being recorded will decay over time, even when adjusting for reporting delays. Therefore, here we model the epidemic using specimen date, that is the date the sample is collected from a patient. This reflects an epidemic curve lagged by the delay between infection and seeking healthcare.
Visualising the epidemic curve by specimen date is affected by the delay from specimen date to the case being reported to UKHSA. To correct for this delay, nowcasting methods adjust the observed data by the distribution of reporting delays to create predictions of the actual frequency. We use a generalised additive model to nowcast current cases and apply this to non-travel associated cases in England. The nowcasting suggests that the epidemic is still growing (Figure 8), with doubling time estimated to be around 15 days (90% Confidence Interval (CI): 10 days, 18 days), which is consistent with the data on cases by date of report.
Figure 8. Estimates of nowcast growth rate of monkeypox cases in England (A) and incidence (B)
The charts exclude cases associated with travel. The shaded area is the 90% Credible Interval (CrI), the dark shaded area is the 50% CrI and the lighter area is the 90% CrI.
Figure 8A
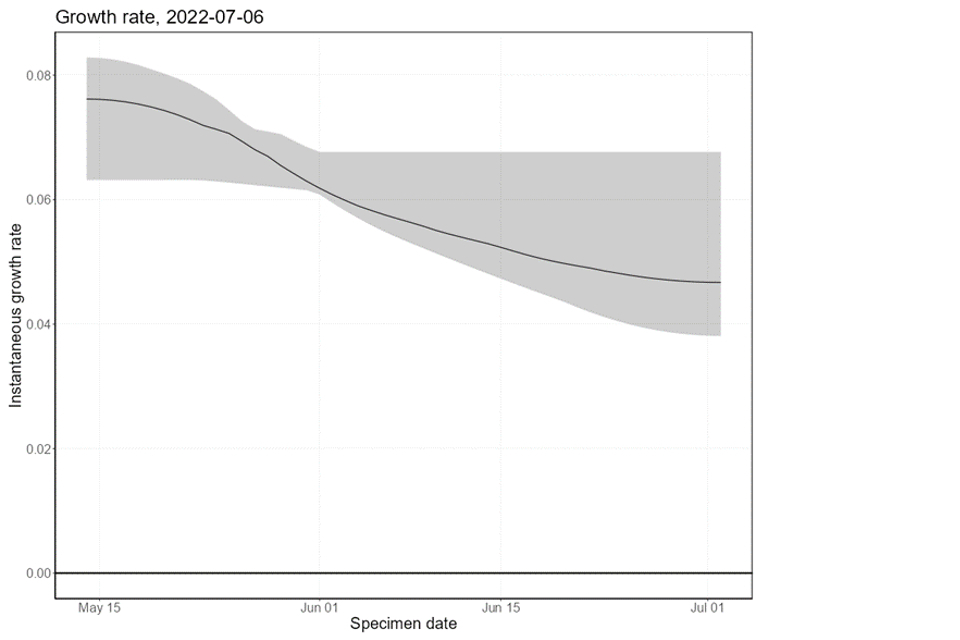
Figure 8B
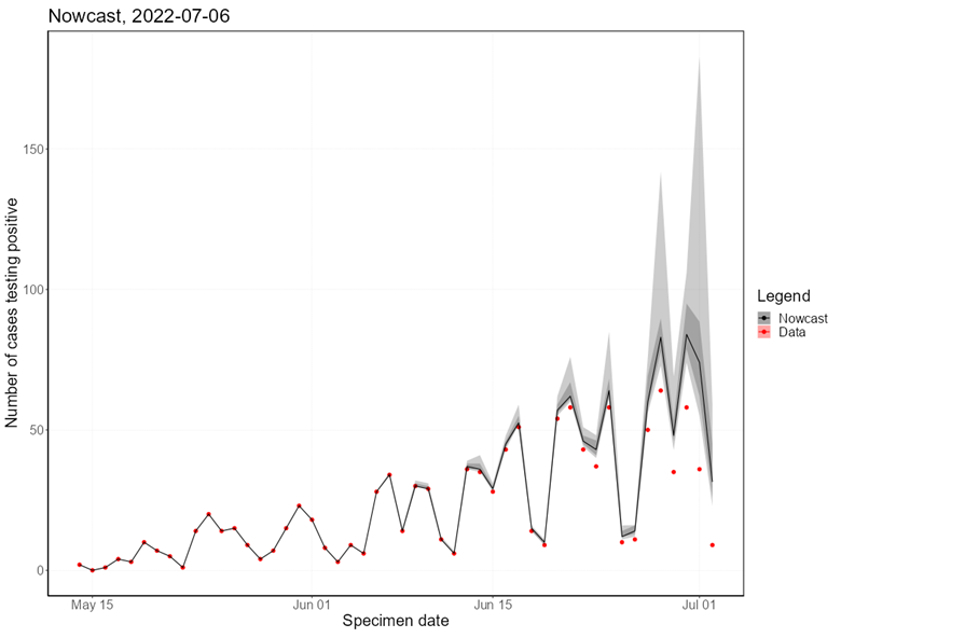
Supplementary data is not available for these figures.
4.2 B.1 and prior circulation in humans
The University of Edinburgh reported to the Technical Group that when originally described and the first genomes were sequenced in May, the 2022 epidemic lineage B.1 (Happi and others, 2022) was reconstructed to have emerged from lineage A.1 represented by genomes sequenced from cases in 2018 from Nigeria, UK, Israel and Singapore (cases in the last 3 of these countries had travel history in Nigeria).
Originally 46 mutations were described differentiating the B.1 lineage from the closest match in lineage A.1 (Isidro and others, 2022). However, a sequenced genome from a 2021 Monkeypox virus (MPXV) case in Maryland, USA, with travel history to Nigeria lies on the branch leading to B.1. This means that much of this diversity likely arose amongst circulating viruses in Nigeria.
A further 3 genomes from USA (from Texas and Virginia in 2021 with travel history to Nigeria, and Florida in 2022 without travel information) also lie outside the diversity of B.1. This shows that the 2022 multi-national epidemic is part of, and emerged from, a greater but largely under-sampled epidemic.
Although MPXV has generally been considered a zoonotic virus with limited human transmission following exposure to a non-human animal reservoir, there may have been sustained human to human transmission since 2017 (O’Toole and Rambaut, 2022).
The presence of the following 11 mutations (relative to the 2018 reference genome, NCBI accession number NC_063383) will indicate membership of the epidemic lineage B.1: G3111A, C39139T, G73239A, G74205A, G77383A, C84587T, C150469T, A151461C, G155795A, G170262A and C183519T.
Part 5. Clinical experience
Increasing clinical experience in the NHS enables us to better describe the clinical syndrome associated with the current outbreak of monkeypox including eliciting previously unknown signs and symptoms. This data will allow us to refine case definitions and improve clinical management of patients with early recognition of developing complications by patients and clinicians.
A review of 133 cases managed at a single centre between 6 May 2022 and 24 June 2022 underlines that most cases of monkeypox are safely self-managed in the community however approximately 10 to 15% of individuals requiring either further support as outpatients or admission to hospital for symptom control or management of complications.
Novel manifestations of monkeypox are clearly linked to the location of mucocutaneous monkeypox lesions. Nearly all patients reporting peri-anal or rectal lesions reported pain and hospital admission has been required for patients with severe rectal pain with some having radiologically evident proctitis.
Oropharyngeal symptoms (for example, tonsillitis, peritonsillar cellulitis or peritonsillar abscess or neck lymphadenopathy) have developed in some individuals causing pain or difficulty swallowing. Monkeypox lesions on external genitalia have caused severe swelling and pain and, in some cases, led to the development of paraphimoses. Cutaneous lesions have resulted in secondary bacterial infections of skin and soft tissues (cellulitis).
Systemic symptoms including fever, lymphadenopathy and myalgia are common but in contrast to current understanding do not always precede mucocutaneous manifestations of monkeypox and approximately 10% of patients did not exhibit any systemic symptoms. Furthermore, 15 individuals (11.3%) have presented with a solitary cutaneous lesion with no subsequent skin lesions. These findings taken together indicate a need for further data collection to refine the case definition.
Part 6. Air and environmental findings
The NIHR and UKHSA are conducting environmental sampling investigations in hospitals caring for people who need to be admitted for management of complications of monkeypox. Initial findings show widespread shedding of viable (infectious) MPXV onto multiple surfaces within the negative pressure isolation rooms where patients stay.
Additionally, some air samples obtained within the patient rooms, during and following the changing of bed linen, contain MPXV DNA and, in one case, viable MPXV isolated by virus culture. Sampling and analysis of results continues, but the initial findings support the need for appropriate infection prevention and control measures for inpatient settings, to prevent people from being exposed to infectious virus.
Sources and acknowledgments
Data sources
Monkeypox virus PCR results are submitted to UKHSA daily by the Rare and Imported Pathogens Laboratory (RIPL), Porton. Data on people testing positive since 6 May 2022 is enhanced with demographic, symptom, epidemiological, and exposure information extracted from the UKHSA Health Protection team case management system (HPZone), or collected in enhanced surveillance questionnaires.
Enhanced surveillance questionnaires include data collected via rapid sexual health questionnaires administered during the initial weeks of the outbreak (used from 27 to 31 May 2022), questionnaires completed by health protection teams during telephone interviews (used from 1 to 24 June 2022), and self-completed questionnaires sent electronically to cases (used from 25 June 2022 onwards).
Authors of this report
Zahidul Abedin, Charlotte Anderson, Carolina Arevalo, Sooria Balasegaram, Jessica Bridgen, Chloe Byers, Meera Chand, Rachel Christie, Fergus Cumming, Jake Dunning, Paula Blomquist, Katie Wrenn, Ashley Goddard, Irene Gonsalvez, Diane Hatziioanou, Susan Hopkins, Tim Laurence, Geraldine O’Hara, Christopher Overton, Karthik Paranthaman, Mateo Prochazka, Cian Ryan, Roberto Vivancos, Thomas Ward, William Welfare, JinMin Yuan, Andrew Rambaut.
Contributors
UKHSA:
- Data, Epidemiology and Analytics Cell
- Research and Science Cell
- Modelling Cell
- Genomics Public Health Analysis
- Sexual Health Liaison Group
- Monkeypox Incident Management Team
Monkeypox Technical Group
The Monkeypox Technical Group includes members with expertise in clinical infectious diseases, clinical research, epidemiology, genomics, modelling and virology.
| Person | Institution |
|---|---|
| Meera Chand (Chair) | UKHSA |
| Andre Charlett | UKHSA |
| Allan Bennett | UKHSA |
| Calum Semple | University of Liverpool |
| Christophe Fraser | University of Oxford |
| Claire Dewsnap | British Association for Sexual Health and HIV |
| Claire Gordon | UKHSA |
| Erik Volz | Imperial College London |
| Emma Thomson | Medical Research Council-University of Glasgow Centre for Virus Research |
| Fergus Cumming | UKHSA |
| Giri Shankar | Public Health Wales |
| Geoffrey L. Smith | University of Cambridge |
| Geraldine O’Hara | High Consequence Infectious Diseases Network |
| Helen Fifer | UKHSA |
| Isabel Oliver | UKHSA |
| Jake Dunning | University of Oxford / Royal Free Hospital |
| Jason Mercer | University of Birmingham |
| Public Health Scotland | |
| Matt Keeling | Warwick University |
| Matt Phillips | British Association for Sexual Health and HIV |
| Neil Ferguson | Imperial College London |
| Obaghe Edeghere | UKHSA |
| Philip Veal | Health and Social Care Northern Ireland |
| Richard Myers | UKHSA |
| Steven Riley | UKHSA |
| Susan Hopkins | UKHSA |
| Tommy Rampling | UKHSA |
| Andrew Rambaut | University of Edinburgh |
Acknowledgements
The authors are grateful to those teams and groups providing data for these analyses including:
- British HIV Association (BHIVA)
- British Association for Sexual Health and HIV (BASHH)
- Sexual Health Services
- NHS England and Improvement
- High Consequence Infectious Diseases Network
- Public Health Scotland
- Public Health Wales
- Public Health Agency, Northern Ireland
