[Withdrawn] Factsheet: Patient Safety Commissioner
Updated 18 July 2024
For more information about the Patient Safety Commissioner, see the Patient Safety Commissioner website.
Top lines
The government amendment delivers on the second recommendation of the Independent Medicines and Medical Devices Safety Review, to establish a Patient Safety Commissioner (PSC) for England.
The PSC will be a champion for patients. The commissioner’s core role will be to promote the safety of patients and the importance of the views of patients in relation to medicines and medical devices.
The government has done a huge amount of work to improve patient safety, it continues to remain a key priority. We recognise that more can be done, and the new role will ensure the voices of patients are heard.
What the bill changes
The amendment establishes a PSC with statutory powers.
The PSC will be an independent statutory office holder, funded by the Department of Health and Social Care (DHSC) and appointed by the Secretary of State.
The PSC’s statutory functions include the power to make reports or recommendations and the power to request and share information with relevant persons.
The PSC will be provider neutral, and able to exercise these powers in relation to both the NHS and independent sector.
Policy background
Patient safety is of central importance to the government’s vision for the NHS.
Measures to reduce the possibility of harmful events are in place, for example establishing the Healthcare Safety Investigations Branch to examine serious patient safety incidents.
The NHS Patient Safety Strategy builds on this progress and aims to improve patient safety across the whole system.
The PSC will enhance this work, by focusing on the voice of patients and improvements to patient safety for medicines and medical devices.
The PSC will be under an obligation to publish a set of principles to govern the way in which they carry out their core duties. The PSC must take steps to consult patients and to ensure that patients are aware of their role.
The everyday workings of the PSC are to be finalised. Regulations will be made setting out further details about the appointment and operation of the commissioner, for example the terms of office.
How independence will be safeguarded
We expect the Secretary of State to work with the PSC to agree how their independence will be safeguarded.
It is common for commissioners to be sponsored by the government departments with relevant policy responsibility while maintaining their independence.
Process diagram
See the process of the patient journey at the end of annex A.
Annex A: PSC proposal – further detail
Establishment
The Patient Safety Commissioner for England will be an independent statutory office holder, funded by DHSC and appointed by the Secretary of State.
Independence
To be effective, it is fundamental that the commissioner has the freedom to act independently.
It is common practice for commissioners to be sponsored by the government department with relevant policy responsibility. The Children’s Commissioner does an exemplary job whilst being sponsored by the Department for Education. The Victims’ Commissioner does the same and is sponsored by the Ministry of Justice.
A relationship with DHSC would allow the commissioner a powerful place within the system. A commissioner which is entirely removed from the policy department can be more easily overlooked by government. It is crucial that the right person is appointed into the role, someone who is confident and knowledgeable of the sector to bring weight and intelligence to the commissioner position.
Independence will necessarily be exercised in the carrying out of the commissioner’s functions. For example, the commissioner will have the power to make recommendations or reports to the Secretary of State, who will then be under a duty to consider and respond, ensuring that the department is kept accountable. We will expect that the commissioner makes any such reports or recommendations independently, without recourse to or clearance from the Secretary of State or DHSC.
Reporting to Parliament
Regulations will be made setting out further details about the appointment and operation of the commissioner, which will be consulted on.
Regulations may require the commissioner to lay documents before Parliament and prepare reports. In combination this means that the regulations could for example, require the commissioner to lay an annual report before Parliament and specify what that report should cover.
Working within the system
It is integral that the commissioner is complementary to and enhances the work of the many existing healthcare services and regulatory bodies already operating in our health service in England.
Regulatory and safety bodies such as the Medicines and Healthcare products Regulatory Agency, NHS England and NHS Improvement, and the Care Quality Commission (CQC) have established areas of work and responsibility to do with patient safety.
The commissioner will be ‘provider neutral’. They will be able to exercise their powers in both the NHS and independent sector.
The commissioner’s functions will allow them to proactively interreact with other providers and public bodies and so complement and enhance the existing system. For example, the commissioner will have the power to make reports or recommendations to relevant public authorities and independent healthcare providers. It will also have the power to request and share information with these bodies which the relevant persons must cooperate with and respond to within such period as the commissioner may reasonably require.
The commissioner will have the power to react to non-compliance from independent providers. For example, if a provider fails to respond to requests for information or fails to respond to reports and recommendations, the commissioner could share information with or make a report to the CQC as the regulator of such bodies.
Existing patient safety initiatives
Following the tragedy of Mid-Staffordshire, and some other very concerning cases, the government has overhauled the infrastructure underpinning safety and quality in the past decade and put in place a comprehensive set of measures to reduce the possibility of harmful events. A culture which listens and responds to concerns in the first place is crucial if the right lessons are to be learned and errors are to be minimised. Measures include establishing:
-
the Healthcare Safety Investigations Branch to examine the most serious patient safety incidents and promote system-wide learning
-
medical examiners to provide much needed support for bereaved families and improve patient safety
-
a duty of candour so that hospitals tell patients if their safety has been compromised and apologise
-
protections for whistle blowers and Freedom to Speak Up Guardians across all trusts, supported by a National Guardian
The NHS Patient Safety Strategy published in July 2019 builds on this progress and aims to improve patient safety across the whole system. The strategy sets out the safety priorities for the NHS and the programmes planned and underway to deliver on them.
The Patient Safety Commissioner proposal will enhance the existing work we have done to improve patient safety in England. The commissioner will help us learn more about what we can do to improve patient safety in relation to medicines and medical devices and put patients at the forefront of what we do.
Appointment
The government understands the urgency to establish the role of Patient Safety Commissioner, but there is a need to balance urgency to appoint the first commissioner with ensuring time is allowed for the required due process to recruit the right person with the skills and experience needed to be effective in the role.
Interaction with patients
The government amendment will put the Patient Safety Commissioner under a duty to involve patients in the discharge of their core duties and take reasonable steps to ensure patients are aware of the commissioner’s role, how they might communicate with the commissioner, and consult patients on the matters the commissioner proposes to consider.
The commissioner will have powers to receive information from patients or any other person they think appropriate for them to carry out their role. The commissioner may not exercise any of their functions to investigate an individual case, as this function is already the responsibility of a number of existing regulatory bodies. The commissioner can, however, consider individual cases and draw conclusions about them for the purpose of considering a wider, general issue.
Governance and regulations
The commissioner will be under an obligation to prepare and publish a set of principles to govern the way in which they carry out their core duties and the commissioner must carry out a public consultation in preparing or revising the principles.
This amendment would establish a Patient Safety Commissioner to be appointed by the Secretary of State, though we cannot give a precise timetable for that appointment. Regulations contain provisions for factors including:
- the commissioner’s terms of office
- financial or other assistance
- the appointment of a board to provide advice to the commissioner
The government is wholly committed to the establishment and implementation of this position.
Indemnity
We are continuing to work to determine the most appropriate way to indemnify the commissioner.
The commissioner will be listed under section 71(2) of the NHS Act 2006 so that, when established, the commissioner would be eligible to participate in certain indemnity schemes established under that section.
This does not mean however, that the commissioner will automatically be a member of any such scheme or will end up participating in any such scheme. What it does do is it ensures that future potential avenues for indemnity under this section will be open to the commissioner.
Process of the patient journey
Patient safety and patient voice
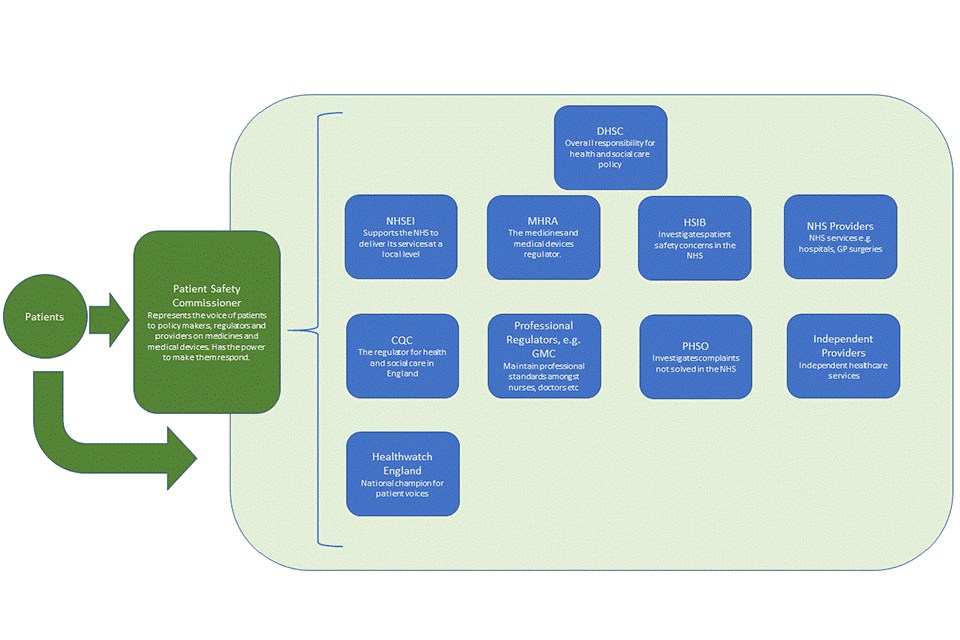
This diagram shows how the PSC represents the voices of patients to policy makers, regulators and providers of medicines and medical devices, which includes:
- DHSC, which has the overall responsibility for health and social care
- NHSEI, which supports the NHS to deliver its services at local level
- MHRA, which is the medicines and medical devices regulator
- HSIB, which investigates patient safety concern in the NHS
- NHS providers, which provide NHS services including GP surgeries, hospitals and so on
- CQC, which is the regulator for health and social care in England
- professional regulators, for example GMC, which maintain professional standards amongst nurses, doctors and so on
- PHSO, which investigates complaints not solved in the NHS
- independent providers, which provide independent health care services
- Healthwatch England, which is the national champion for patient voices
The PSC has the power to make them respond.
