Lead Exposure in Children Surveillance System (LEICSS) annual report, 2023
Updated 22 December 2025
Applies to England
Executive summary
This report summarises the surveillance of cases of lead exposure in children in England from 1 January to 31 December 2022. It outlines 2022 case data and gives an update of the surveillance activities.
Following a review of the evidence of the harm of lead exposure in children (1, 2), a UKHSA task and finish group recommended the lowering of the blood lead public health intervention level for England. Since 5 July 2021, the case definition for surveillance changed to half the original concentration, from 0.48 μmol/L (equivalent to ≥10μg/dl) to 0.24μmol/L (equivalent to ≥5μg/dl). As expected, this led to a steep increase in the number of cases being reported to LEICSS.
Since 5 July 2021, a case is defined as a child:
- with a blood lead concentration ≥0.24 micromoles per litre (μmol/L), equivalent to ≥5 micrograms per decilitre (μg/dL), as detected in a UK Accreditation Service (UKAS) accredited biochemistry or toxicology laboratory
- reported to UKHSA for public health intervention
- aged under 16 years at the time of first elevated blood lead concentration
- resident in England
Main results
Main findings of this report are that:
-
a total 191 cases of lead exposure in children that met the case definition were notified to UKHSA in 2022; most cases (160, 84%) were directly notified to LEICSS by participating laboratories, and 31 (16%) were notified by other routes, similar to other years. There were 58% more cases compared to the previous year, which had 121 cases
-
as a result of the case definition change, 119 (62%) cases were identified in the blood lead concentration (BLC) range of 5 to 10 μg/dL, almost double the number of cases (72, 38%) with a BLC ≥10 μg/dL
-
the median delay between the date of specimen collection and the date cases were entered onto HPZone was 17 (IQR 10 to 32) days; which is more than in 2021 when this was 11 days (IQR 8 to 15). The surveillance system experienced some resource issues in 2022 partly due to the demands of a number of national health protection incidents
-
cases were typically 1 to 4 years of age, male and resident in more deprived areas. The median blood lead concentration of cases was 0.37μmol/L (7.67 µg/dL) in 2022, which is similar to 2021 (0.38μmol/L (7.87 µg/dL)), both are almost half the median blood lead concentration in 2020, 0.71 μmol/L (14.69 µg/dL), due to the lower BLC reporting threshold
-
according to statistics from an international population survey, the number of cases reported to UKHSA was significantly lower than the estimated incidence of lead exposure (3, 4, 5).
-
the average detection rate for England between 2015 and 2022 was 6 cases per million children aged 0 to 15 years, although there were large regional variations, with Yorkshire and the Humber having the highest and the South East of England having the lowest
Main messages and recommendations
Lead is a persistent environmental contaminant that can have toxic effect even at low blood lead concentrations (BLC). There is no known safe threshold for lead exposure. Children exhibiting pica (see note 1) or hand to mouth behaviour in environments with lead hazards are likely to be at the highest risk of exposure.
Clinicians should be aware of the risk of lead exposure for children, the main sources of lead exposure, children most at risk, presenting symptoms and signs of exposure. For more information on resources for public health professionals and clinicians, see the Resources section of this report.
UKHSA lowered the public health intervention concentration for lead from ≥10μg/dL (≥0.48μmol/L) to ≥5μg/dL (≥0.24μmol/L) for children under 16 years and for pregnant women, with effect from 5 July 2021. This is the first full year with surveillance on the lowered intervention level which is why case numbers are higher than previous years.
Cases who fit the latest case definition, with a blood lead concentration above 5µg/dL (0.24µmol/L), should be notified to UKHSA health protection teams for public health case management. Details of other requirements for notification are outlined under Case reporting to LEICSS section of this report below.
Background
Around 1 in 3 children (up to 800 million globally) have blood lead concentrations (BLC) at or above 5µg/dL, the concentration at which clinical and public health action is advised in many countries (5). There are no recent comprehensive survey data estimating how many children in England are exposed to lead above this level.
International population survey data may be used for estimates; a survey conducted in France in 2008 to 2009 (see note 2) (3), estimated 1.5% of 1 to 6 year-olds had a BLC ≥0.24µmol/L (≥5µg/dL). Whereas in the USA (6), 2.6% of 1 to 6 year-olds had an estimated BLC ≥0.24µmol/L (≥5µg/dL). Applying the US estimate to the UK population of 1 to 4 year olds in England and Wales in 2021 (taken from ONS 2021 Census data) (6) suggests that as many as 83,200 children in the UK have BLCs above the intervention concentration.
However, recent estimations by the Institute of Health Metrics (7), using the Global Burden of Disease tools, suggest that for the UK in 2019 there were 213,702 (95% CI 186,000 to 281,500) children aged 0 to 19 years with a BLC of ≥0.24µmol/L (≥5µg/dL), and 29,036 (95% CI 25,000 to 42,500) children with BLC ≥0.48µmol/L (≥10µg/dL). Comparison with historic data suggests a substantial fall in average BLCs over time (8). Moreover, population lead exposure is strongly influenced by setting, so these findings give only a broad indication of the potential situation in England. In 2021, the US Centers for Disease Control and Prevention (CDC) reduced the blood lead intervention level from ≥0.24µmol/L (≥5µg/dL) to ≥0.17µmol/L (≥3.5µg/dL) (9).
Exposure to lead can result in severe multi-system toxicity (1). How this toxicity manifests depends on both the blood lead concentration (BLC) and how rapidly BLC rises. Overt manifestations of toxicity (that is, lead poisoning), such as anaemia or abdominal pain, accompany higher lead concentrations, for example, BLC>1.93μmol/L (>30µg/dL) (see note 3) (2, 10). Lead exposures resulting in a lower BLC may not cause such apparent symptoms, but still cause harm, particularly to the central nervous system. There is no known safe blood lead concentration; even BLC as low as 3.5 µg/dL may be associated with decreased intelligence in children, behavioural difficulties and learning problems (11). Timely removal or abatement of the exposure source is the mainstay of case management, but symptomatic children, and children with BLC greater than 2.4μmol/L may also require chelation therapy (10).
Primary prevention efforts – targeted at reducing the use of lead in paints and fuels, regulation of lead concentrations in drinking water, water supply pipes, remediation of lead in soil and control of industrial emissions – have been successful in reducing lead in the environment and exposures to lead, thus lowering BLC in children, as has been demonstrated in the USA (4). However, lead is a persistent contaminant, therefore children can still be exposed to lead present in the environment as a result of historical usage. Since the removal of lead from petrol, ingestion rather than inhalation has been the most common route of exposure in high income countries, particularly from dusts and flakes of leaded paint (10). Leaded paint had wide domestic use in the UK before gradual withdrawal from the 1960s onwards (12) and was eventually banned for sale in 1992. A recent study (13) found houses built pre-1970’s, and terraced housing, as key risk factors for increased BLC for children in England.
Other important potential routes of exposure to lead in children are ingestion of lead-contaminated water, contaminated soil or dust, herbal medicine preparations, contaminated food and spices, consumer products not meeting regulatory standards (for example, paint on toys, make-up, lead crystal glassware); also secondary exposure from parental hobbies or occupations (for example, resulting in children being exposed to lead dust on work-clothing) (10).
Children with learning and developmental disorders are at higher risk of exposure to lead due to increased mouthing (or ‘pica’) behaviour (14), which puts them at risk for ingestion of lead from non food items (paint flakes, lead in soil, and so on). Additionally children already exposed to lead, even at very low concentrations, have been shown to have reduced learning capacity and increased prevalence of developmental disorders (11, 15). Iron deficiency may further increase susceptibility to lead toxicity and can also cause pica. An audit of the lead exposure in children surveillance data from 2014 to 2022 found paint and soil to be the most reported sources of exposure for children in England (16).
Cases of lead exposure are identified by means of a blood test to measure the blood lead concentration. As signs and symptoms of lead exposure are non-specific, it is easily missed and misdiagnosed in clinical settings. An evidence review of the need for population screening was carried out by the UK National Screening Committee in 2018. A systematic population screening programme was not recommended (17), because of concerns about testing and treatment and the lack of up to date population prevalence data (alongside evidence of a steady decline in lead exposure over time).
Case detection therefore depends on clinicians having a high level of clinical suspicion; for example, taking account of a child’s home circumstances potentially increasing the risk of lead exposure, and subsequently ordering a blood test. Surveillance of cases identified by clinicians offers a means of gathering intelligence to guide public health action to prevent further cases of exposure.
The Lead Exposure in Children Surveillance System (LEICSS)
UKHSA coordinates LEICSS, a national surveillance system for children residing in England. Formal surveillance of lead exposure in children in England was initiated in 2010 by the Surveillance of elevated blood Lead in Children (SLiC) study, a joint research project between the British Paediatric Surveillance Unit and the Health Protection Agency (the forebear to PHE, now UKHSA). The SLiC study authors recommended implementation of a laboratory-based surveillance system in order to facilitate timely public health management of cases of lead poisoning in children (18). A pilot system, the Lead Poisoning in Children (LPIC) surveillance system, was therefore instigated in 2014. LPIC was then permanently implemented in 2016 following successful evaluation of the pilot, and its name changed to LEICSS to recognise broader aims of prevention of lead exposure in children, in addition to the rapid recognition of cases of lead poisoning.
The UKHSA LEPHIS (Lead Exposure Public Health Intervention and Survillence) working group and a steering group with additional representatives from participating laboratories, academia, NHS clinical toxicology and patient representative groups (eg Lead Exposure and Poisoning Prevention (LEAPP) Alliance oversee system aims and development (see Steering and Working Group Members below). The data collected from LEICSS feeds into the Environmental Public Health Surveillance System (EPHSS) for England operated by UKHSA as part of the Environmental Public Health Tracking programme and the steering group and working group report to the UKHSA Environmental Public Health Tracking Board.
LEICSS aims are:
- to facilitate timely public health action for individual cases, as the mainstay of treatment for cases of lead exposure is rapid removal of the putative source of exposure
- to meet population level surveillance objectives, to inform public health action that reduces the incidence of lead exposure in children in England, such as identification of risk geographic areas or populations, and identification of current and emerging sources of exposure.
Case reporting to LEICSS
LEICSS is a passive surveillance system that integrates reports of incident (newly detected) cases of lead exposure in children from 2 sources:
- Cases reported to UKHSA directly from a UK Accreditation Service (UKAS) accredited testing biochemistry or toxicology laboratory, or
- Searching HPZone (see note 4) for cases first reported from a non-UKHSA source (for example, the managing clinician or an environmental health officer) to a local UKHSA Health Protection Team (HPT) (see note 5), and cases first reported from other UKHSA Directorates (for example, the Radiation, Chemicals and Environmental Hazards Directorate) but not reported to LEICSS by laboratories participating in surveillance.
Case notification to UKHSA is voluntary but encouraged for case management and surveillance purposes.
Case reports from biochemistry and toxicology laboratories
Reports of cases meeting the following case definition are referred to as ‘laboratory-detected’ cases. Since 5 July 2021, a case is defined as a child:
- with a blood lead concentration ≥0.24μmol/L (equivalent to ≥5μg/dl), as detected in a UK Accreditation Service (UKAS) accredited biochemistry or toxicology laboratory
- reported to UKHSA for public health intervention
- aged under 16 years at the time of first elevated blood lead concentration
- resident in England
LEICSS surveillance staff enter case details onto the HPZone case management system following notification. The relevant local HPT is then alerted to investigate and manage the case. This route of notification to the investigating HPT has been found to be timelier than waiting for notification from other sources involved in treating the case, for example, the managing clinician (19).
‘HPZone-detected’ cases
HPZone-detected cases are those that are or were:
- notified directly to a health protection team in England for public health management and classified on HPZone as ‘toxic exposure to lead’
- aged under 16 years at the time of notification to the health protection team
- resident in England
- not initially notified to LEICSS by a participating biochemistry/toxicology laboratory
Blood lead concentration data is not routinely recorded on HPZone in a way that makes it available for analyses by LEICSS for these cases. Thus a HPZone detected case may have a BLC <5µg/dL (0.24 µmols/L) or be missing data on BLC.
The Supra-regional Assay Service (SAS) Trace Elements laboratories network, and other reporting laboratories
A group of highly specialised diagnostic laboratories, the SAS Trace Element network, provide a referral network for specialised laboratory investigations in the UK. Blood lead concentration is measured in 6 SAS Trace Elements laboratories in England, and it is estimated they perform the vast majority of such tests nationally. All 6 SAS laboratories participate in LEICSS, and a partnership between the SAS-associate laboratory in Wales (Cardiff Toxicology Laboratory) has been developed to alert LEICSS of England residents whose blood lead concentration may be determined in Cardiff. Other, non-SAS but UKAS accredited laboratories have also agreed to report cases to LEICSS; these are typically located in larger NHS Trusts or are private laboratories. All contributing laboratories are named in the Acknowledgements section of this report.
Public health management of cases
Following a review of the evidence of the harm of lead exposure in children (2), a UKHSA task and finish group recommended the lowering of the blood lead public health intervention concentration. Since 5 July 2021 the case definition for surveillance changed to half the original concentration, from 0.48 μmol/L (equivalent to ≥10μg/dL) to 0.24μmol/L (equivalent to ≥5μg/dL). A BLC of ≥0.24μmol/L (or ≥5μg/dL) is the current threshold (‘public health intervention concentration’) for public health case management in England for children and pregnant women as it indicates a specific source is present. HPTs will take steps to systematically identify and remove the potential source(s) of lead exposure in cases, following guidance in a HPT Standard Operating Procedure (SOP) (20). This involves liaison and involvement with other UKHSA stakeholders, such as the Environmental Hazards and Emergencies department, and non-UKHSA stakeholders, such as the responsible clinician and local authority where the case resides. General information on lead and incident management can be found on UKHSA’s incident management webpages.
Purpose of this report
This report provides a summary of data extracted from the national LEICSS data set for cases of child lead exposure in residents of England reported to HPTs during 1 January to 31 December 2022. As the case definition changed in 2021, we expected more cases than previous years due to the lowering on the intervention (and hence reporting) threshold. In this report the 2022 metrics were compared to the previous 2015 to 2021 data 7-year average, where relevant, using data from cases reported between 1 January to 31 December for each of these years.
Figures are correct at the time of publication and may be subject to change as new information about cases becomes available.
This report, previous years’ annual reports and other surveillance reports are available at Lead exposure in children: surveillance reports, for reports from 2021 and Lead Exposure in Children Surveillance System: Surveillance Reports published before 2021 for reports previous to 2021.
Surveillance data indicators
Number of unique cases
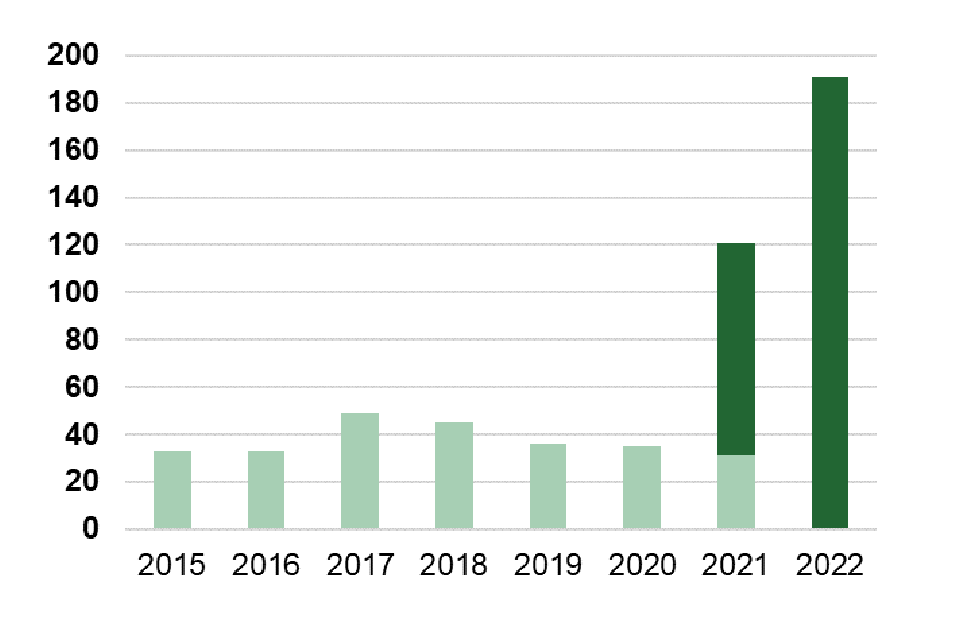
A total of 212 reports of elevated BLC in children were reported to LEICSS in 2022. Of these, 191 met the case definition (reports of BLC <0.24μmol/L were not included). Eighty-four per cent of cases were direct laboratory reports to LEICSS, with 16% from other reporting routes (direct to HPTs, etc) (Table 1). Figure 1 shows the number of cases by reporting route in 2022, and in 2015 to 2021, in England.
Table 1. Count and percentage of LEICSS cases, by reporting route to LEICSS, England 2022, and 2015 to 2021
| Route of detection by LEICSS | Count of cases 2022 (% of total) | Count of cases 2015 to 2021 (% of total) |
|---|---|---|
| Direct laboratory reports | 160 (84) | 280 (77) |
| Other Routes (HPZone search) | 31 (16) | 86 (23) |
| Total | 191 | 366 |
Figure 1. Count of LEICSS cases per year, England 2015 to 2022
Note: The darker green bar in 2021 and 2022 denotes the number of cases, post-case definition change
Timeliness of reporting of lab-detected cases to LEICSS and notification to Health Protection Teams
For the laboratory reported cases, the median delay between the date of specimen collection and the date the case was entered onto HPZone (as a proxy for the date of report to HPTs) was 17 days, with a wide interquartile range (IQR) of 10 to 32 days, which is higher than the average for 2015 to 2021 (median of 10 days; IQR: 7 to 14) (Table 2). The surveillance system experienced some resource issues in 2022 partly due to the demands of a number of national health protection incidents, which may have contributed to this delay.
Table 2. Time between specimen collection and entry of case onto HPZone for case management for lab-detected LEICSS cases, England 2022, and 2015 to 2021
| Year | Cases | Cases with valid data* | Median days delay | IQR** |
|---|---|---|---|---|
| 2022 | 160 | 159 | 17 | 10 to 32 |
| 2015 to 2021 | 280 | 255 | 10 | 7 to 14 |
*Cases where both a valid specimen date and a valid date of entry onto to HPZone were extracted from HPZone.
**IQR = Inter quartile range.
Occurrence and trends of cases of lead exposure in children
Count and detection rate (by LEICSS) of cases by regions and year
A larger number of cases were detected in 2022 compared with previous years due to the lowering of the public health intervention concentration (see Figure 2 and Table 3). The percentage increase in cases from 2021 to 2022 was on average 58% for England.
Figure 2. Graph showing detection rate of LEICSS cases per regional population of 0 to 15 year olds, per million, 2015 to 2022, England

*Centres where an SAS laboratory that participates in the surveillance system is situated; 2021 population data was used as the denominator for 2022 cases.
Table 3. Count (and % of total) of LEICSS cases, percentage change from 2021 to 2022, and average detection rate† of cases (per million 0 to 15-year-old children) by Region and year of notification, England 2015 to 2022
| Region | Cases 2015 (%) | Cases 2016 (%) | Cases 2017 (%) | Cases 2018 (%) | Cases 2019 (%) | Cases 2020 (%) | Cases 2021 (%) | Cases 2022 (%) | Cases 2105 to 2022 (%) | % change in cases from 2021 to 2022 | Average detection rate‡ of cases (per million per year) 2015 to 2022 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| South East* | 6 (18) | 0 (0) | 4 (8) | 3 (7) | 1 (3) | 0 (0) | 7 (6) | 10 (5) | 31 (6) | 43% | 2.05 |
| London* | 5 (15) | 7 (21) | 10 (20) | 12 (27) | 11 (31) | 4 (11) | 20 (17) | 24 (12) | 93 (17) | 20% | 5.83 |
| South West | 2 (6) | 0 (0) | 2 (4) | 4 (9) | 2 (6) | 3 (9) | 9 (7) | 9 (5) | 31 (6) | 0% | 3.55 |
| West Midlands* | 2 (6) | 3 (9) | 3 (6) | 4 (9) | 0 (0) | 2 (6) | 11 (9) | 38 (20) | 63 (11) | 245% | 6.14 |
| East Midlands | 1 (3) | 0 (0) | 0 (0) | 3 (7) | 1 (3) | 3 (9) | 0 (0) | 10 (5) | 18 (3) | 1000% | 2.28 |
| North West | 4 (12) | 6 (18) | 11 (22) | 3 (7) | 4 (11) | 5 (14) | 11 (9) | 26 (14) | 70 (13) | 136% | 5.66 |
| North East | 1 (3) | 0 (0) | 1 (2) | 0(0) | 0 (0) | 2 (6) | 5 (4) | 3(2) | 12 (2) | - 40% | 2.85 |
| Yorkshire and the Humber* | 9 (27) | 12 (36) | 16 (33) | 12 (27) | 14 (38) | 12 (34) | 54 (45) | 65 (34) | 194 (36) | 20% | 21.01 |
| East of England | 3 (9) | 5 (15) | 2 (4) | 4 (9) | 3 (8) | 4 (11) | 4 (3) | 6 (3) | 31 (6) | 50% | 2.80 |
| England | 33 | 33 | 49 | 45 | 36 | 35 | 121 | 191 | 543 | 58% | 5.52 |
†Should not be interpreted as an estimate of incidence – see ‘The case detection rate and ascertainment’ section of this report.
‡The numerator for this indicator is incident cases from 2015 to 2022, and the denominator is the ONS mid-year estimate of the 0 to 15 year-old population from 2015 to 2022 (in 2022, we used the 2021 mid-year estimate). Cases allocated to UKHSA Centre according to postcode of residence.
*Centres where participating SAS laboratories are situated.
Figure 3. Average detection rate† of LEICSS cases (per million 0 to 15 year-old children) by Region, England 2015 to 2022

† Should not be interpreted as an estimate of incidence – see ‘The case detection rate and ascertainment’ section below.
The case detection rate and ascertainment
Due to the lack of specific symptoms at blood lead concentrations below 1.93μmol/L (>30µg/dL), surveillance of clinically reported cases is likely to underestimate the number of affected children. International population surveys, which provide a more precise estimate of the number of children exposed to lead, indicate that there should be more cases of paediatric lead exposure than were identified by LEICSS (3, 4, 5, 8).The figures above should not therefore be considered representative of the incidence of child lead exposure in England.
The variance seen between regions in LEICSS data is likely to result from bias in case ascertainment rather than reflecting variation in incidence/prevalence. For instance, UKHSA is aware of a system set up by the Leeds SAS laboratory (located in Yorkshire and Humber) to actively encourage clinicians to think about testing for lead exposure in children whose blood is being tested for possible iron deficiency and when the child is also known to have pica (21). This laboratory actively involves local clinicians as well. The 90% increase in testing and case reporting in this region after the implementation of this system shows that variations in clinician awareness and testing frequency have a significant impact on case detection by the surveillance system (possibly more so than regional variations in the frequency of lead hazards in the environment). Although it is expected that SAS labs conduct the majority of BLC tests in children in England, testing in laboratories that do not submit cases to LEICSS may also contribute to the regional difference in case ascertainment.
Count and detection rate of cases by gender and age
The majority of cases in 2022 were male (68%), similar to the 2015 to 2021 proportion (63%) (Table 4). Across all age groups the notification rate was higher in males than females (Figure 4). This gender disparity is reflected in the literature (8, 9, 13, 16,17) and may indicate a pre-disposition for males to behaviours or comorbidities that result in lead exposure, such as autism (22), itself associated with pica (23).
Table 4. Count and percentage of LEICSS cases by sex, England, 2022, and 2015 to 2021
| Sex | Count of cases 2022 (%) | Count of cases 2015 to 2021 (%) |
|---|---|---|
| Female | 62 (32) | 124 (35) |
| Male | 129 (68) | 221 (63) |
| Unknown | 0 (0) | 7 (2) |
| Total | 191 | 352 |
The highest case detection rate was in children aged 1 to 4 years, for both males and females (Figure 4). 72% of cases identified in 2022 were from this category, slightly higher than the 2015 to 2021 period average (64%) (Table 5). Fewer cases were aged between 5 to 11 years (22%) and (4%) <1 years old, while 2% were in the oldest age group.
Since lead exposure in children is most likely to occur through ingestion of lead-containing substances (especially from deteriorating paint), the high percentage of cases in pre-school age children may indicate a greater vulnerability to lead exposure due to mouthing behaviours (4). Additionally, developmental delay may become more evident at this age group, and autism symptoms may also become more apparent, which could result in more investigations for these children.
Table 5. Count and percentage of LEICSS cases by age group*, England, 2022, and 2015 to 2021
| Age group* | Count of cases 2022 (%) | Count of cases 2015 to 2021 (%) |
|---|---|---|
| Under 1 year | 8 (4) | 14 (4) |
| 1 to 4 years | 138 (72) | 225 (64) |
| 5 to 11 years | 41 (22) | 97 (28) |
| 12 to 15 years | 4 (2) | 16 (4) |
| Total | 191 | 352 |
*Age of child at date of entry onto HPZone
Figure 4. Average case age* and gender-specific detection rate† per million 0 to 15 year old children per year, England 2015 to 2022 (n=534 cases with gender and age data)
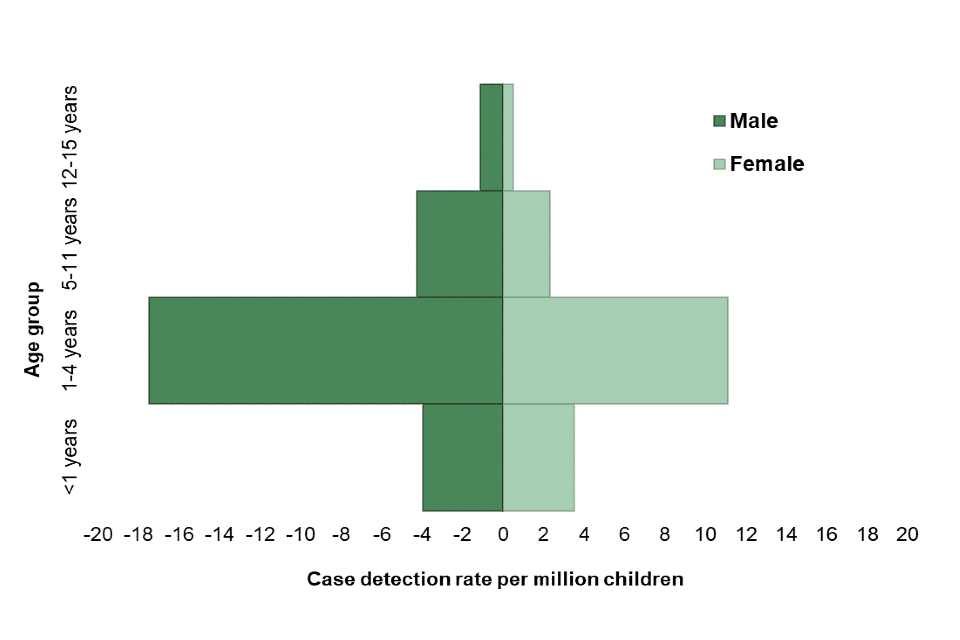
*Age of child at date of entry onto HPZone;
† The numerator for this indicator is the count of age-gender specific incident cases in 2015 to 2022, and the denominator is the mid-year estimate of the age-gender specific 0 to 15 year old population from 2015 to 2022 (for 2022, we used 2021 MYE population data).
Percentage of cases by quintile of index of multiple deprivation (IMD) status
IMD provides a measure of deprivation, evaluated across 7 domains (see note 6), summarised at the area-level. Seventy-two per cent of cases in 2022 lived in areas in the 2 most deprived quintiles of IMD, similar to the previous 6-year average (71%) (Figure 5). Just over 50% of 2022 cases lived in the most deprived areas (Q5). This proportion is still higher than expected (40%). These findings are consistent with patterns of lead exposure by socioeconomic status in US national survey data (11). Possible explanations include increased exposure to lead-containing hazards, such as older housing (9, 13), a greater frequency of co-morbid conditions (such as iron deficiency anaemia), or an increased tendency for clinician testing of children from deprived regions. Children of ethnic minority origin may be disproportionately affected as they are more likely to experience deprivation; however, this cannot be evaluated in the LEICSS dataset because of insufficient ethnicity data (16, 24).
Figure 5. Percentage of LEICSS cases in each quintile of index of multiple deprivation ¥, England 2022 and 2015 to 2021
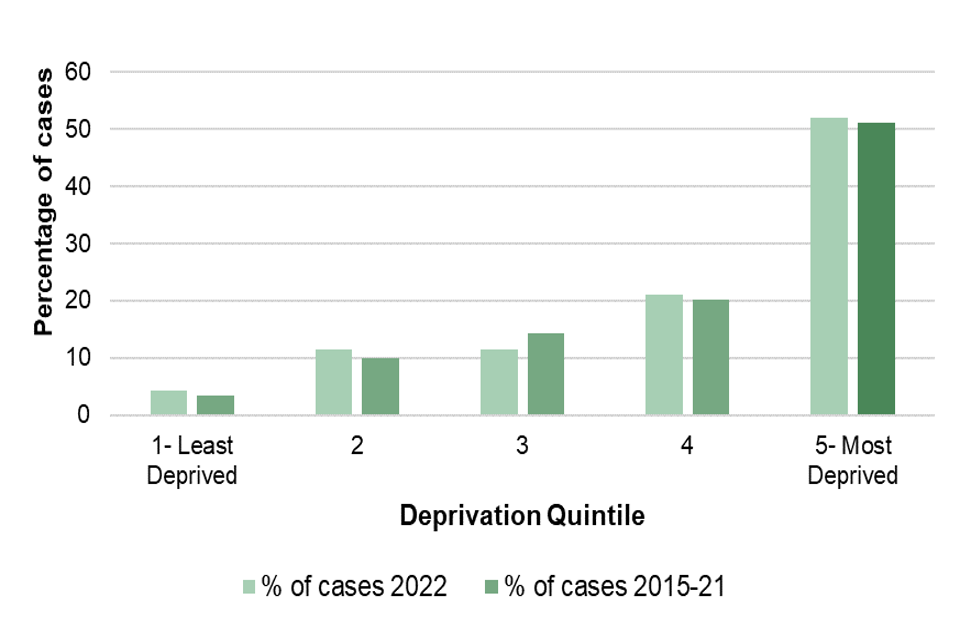
¥ Index of multiple deprivation (IMD) assigned to the Lower-level Super Output Area of the cases’s postcode, using IMD scores from 2019.
Blood lead concentrations of laboratory-detected cases
The median blood lead concentration (BLC) in 2022 was 0.37 μmol/L (7.6 µg/dL), much lower than the 2015 to 2020 median of 0.61 μmol/L (12.6 µg/dL) (Table 6). This was expected following the lowering of the public health intervention BLC and consequent change in case definition. However, although the majority of cases notified in 2022 were in the BLC 5 to <10 µg/dL range, the number of children notified with BLC ≥10 µg/dL (N=72) is still considerably higher than in previous years (average number of notifications with BLC ≥10 µg/dL 2015 to 2021 = 34 per year), suggesting that the increase is not solely due to the lowering of the public health intervention concentration but may reflect improved clinician awareness. 72% (data not shown) of blood lead concentrations were below 1.45μmol/L (<30µg/dL) in 2015 to 2022, a concentration below which children would most likely be asymptomatic, or present with non-specific neuro-behavioural clinical manifestations (10), indicating these children were detected based on a high index of clinical suspicion. Table 7 shows the distribution of BLC recorded for the cases in 2022 and 2015 to 2021.
Table 6. Blood lead concentration (μmol/L) of laboratory detected LEICSS cases, England, 2022, compared to 2015 to 2021.
| Year | Lab detected cases (total cases) | Minimum | Maximum | Median | Lower Quartile | Upper Quartile | Mean |
|---|---|---|---|---|---|---|---|
| 2022* | 160 (191) | 0.24 | 4.03 | 0.37 | 0.29 | 0.66 | 0.61 |
| 2015 to 2021 | 266 (352) | 0.1 | 17.59 | 0.61 | 0.48 | 0.93 | 0.85 |
*Only children with a with a BLC≥0.24μmol/L were eligible for notification to LEICSS
Table 7. Blood lead concentration (μmol/L) of laboratory detected LEICSS cases, England, 2022, compared to 2015 to 2021.
| Year | BLC<5µg/dL (%) | BLC 5 to <10µg/dL(%) | BLC ≥10µg/dL(%) |
|---|---|---|---|
| 2022* | 0 (– ) | 119 (62) | 72 (38) |
| 2015 to 2021 | 18 (6)** | 60 (19) | 240 (75) |
*Only children with a with a BLC ≥5μg/dL (equivalent to ≥0.24μmol/L) **There are often reports of children with BLC below the reporting threshold from labs and other sources.
Duration of case investigation
Of the cases where the investigation had been concluded by the time of data extraction for this report (86%, January 2023), the median duration of the investigation was 7 weeks in 2022, lower than 2021 (12 weeks), and lower than the median for 2015 to 2021 of 12 weeks (Table 8).
Table 8. Duration, in weeks, of the public health investigation of LEICSS cases* reported to the surveillance system, England, 2022, and 2015 to 2021
| Year | Closed cases/total cases (%) | Median duration (weeks)*(LQ-UQ) |
|---|---|---|
| 2022 | 165/191 (86) | 7 (2 to 16) |
| 2015 to 2021 | 324/352 (92) | 12 (3 to 25) |
*Period between date entered onto HPZone and date case closed on HPZone; cases must have been closed at date of data extraction from HPZone in January 2023; LQ – Lower Quartile; UQ – Upper Quartile.
Children whose death was attributed to lead exposure
One child’s death occurred in 2015; a case report demonstrating the death of the 2-year-old child, with pica and iron deficiency, who had ingested lead-containing paint and had acute lead toxicity has been published (17). The delay in diagnosis and subsequent death of the child were attributed to clinicians’ ignorance of the link between lead exposure and pica (21). Historical data has shown deaths from lead exposure in children to be very infrequent in England (22, 25).
System developments
Progress on developing surveillance of lead cases has continued in 2022 to 2023. The COVID-19 global pandemic was the focus of the majority of UKHSA’s health protection operations in the years 2020 to 2022. As resources begin the recover from the pandemic response, we have continued to respond to cases reported to UKHSA and have continued to develop the surveillance system.
To reflect the multi-disciplinary nature of managing lead exposures, sources, interventions and clinical management, the governance of the UKHSA working group has been updated. The new Lead Exposure Public Health Interventions and Surveillance (LEPHIS) Working Group now meets regularly to oversee co-ordination of surveillance, intervention work and raising awareness of lead hazards.
Invitation of further laboratories to participate in surveillance
We continue to invite laboratories in the UK National External Quality Assessment Scheme for Trace Elements (which includes measurement of blood lead concentration) to participate in case reporting to LEICSS. Presentations to the Association of Clinical Biochemists (ACB) on the surveillance raises awareness of reporting by laboratories and has resulted in the recruitment of more laboratories participating in surveillance. Contact ephss@ukhsa.gov.uk for more information
Alerts for testing for blood lead
Introduction of an alert on the electronic test request system by Leeds SAS laboratory to encourage clinicians to consider testing for blood lead (for those children suspected of pica/iron deficiency) increased test requests by 90% in 2017. We supported laboratories to explore the feasibility of implementation of a similar model across the SAS laboratory network but unfortunately due to the diversity of information systems being used, a standardised alerting system is not feasible to implement at this time. However, discussion with laboratories is underway to amend the text on blood lead reporting to include better information on expected BLC in line with Leeds SAS laboratory reporting.
Exposure assessment
Information on exposures in children with elevated BLC was in the past captured through a questionnaire completed by HPTs on paper or as an electronic document which was uploaded to HPZone. This questionnaire has been converted into an online survey format to help HPTs explore and scope exposure information and collect relevant information for initial case management and surveillance purposes. The new online questionnaire went live at the same time as the public health intervention concentration was lowered in 2021. This information will enable us to better scrutinise exposure sources for surveillance purposes (19). Analysis of this data from 2014 to 2022 has been completed recently and the findings submitted for publication (16).
UKHSA’s Environmental Public Health Surveillance System
The Environmental Public Health Surveillance System (EPHSS) collates and integrates data from selected databases on environmental hazards, exposures and health outcome data; further details are provided on GOV.UK. A lead exposure in children module incorporated into EPHSS allows for anonymous aggregated LEICSS data to be interrogated and analysed, producing user defined outputs for surveillance reporting purposes. Currently, the EPHSS platform is only available to UKHSA staff, but the intention is to make it accessible to external users. 2021 case data has been uploaded into EPHSS so users can pull reports on data from 2014 to 2021 inclusive. We are in the process of uploading 2022 and 2023 data to EPHSS.
To gain access to LEICSS outputs via EPHSS, email to: ephss@ukhsa.gov.uk
Current and future activities
-
In April 2023, the LEPHIS group in collaboration with national HPTs hosted a workshop to raise awareness of lead exposure in UKHSA regional teams and to gain feedback on how to support HPTs in case management of LEICSS cases and processing. Feedback from this workshop has helped update the exposure survey questionnaire, SOPs and guidance information.
-
The LEPHIS Steering Group were surveyed to identify the priorities for lead exposure research and practice in 2020. Topics identified included: prevalence study of lead levels in population; exposure assessment for lead exposure cases; survey of blood lead concentrations in samples; interventions impact review; developing case management advice; awareness raising activities; prioritising lead research and surveillance; lead surveillance resourcing; supporting labs with development of lead testing and awareness; long-term prevention strategies.
-
Coupled with the lead workshop, a programme of work has been defined. A sub-group of the LEPHIS Steering Group are planning a prevalence study of blood lead concentrations in children in England. This proposed Elevated Childhood Lead Prevalence Study (ECLIPS) is working on defining a protocol for taking blood from a representative sample of children, piloting the methods to be used, and are currently seeking funding to conduct the study.
-
The Environmental Hazards & Emergencies Department of UKHSA worked with the HPTs to produce a suite of documents and standardised letters available to practitioners to support their BLC work as part of the duty doctors’ pack. A publication is available summarising this guidance (26).
-
The Environmental Epidemiology Group at UKHSA are working to explore exposure source data including hazard maps for risk factors such as soil lead concentrations, housing age and index of multiple deprivation to aid development of a lead exposure model. The first research output from this project was a paper on housing characteristics of cases [(13) that identified vulnerable populations to target for information campaigns.
-
UKHSA was approached by the UK National Screening Committee in 2022 to comment on the preparations for an evidence review to support their review of the need for a screening programme for lead in children. Comments on the proposal were provided by members of the LEICSS Steering and Working groups. It was noted that prevalence studies such as ECLIPS would provide up to date data on the prevalence of elevated lead in children in England and hence be of value for the NSC review. The NSC review is due for renewal.
-
A collaboration with academics from University of Oxford and University of Warwick is ongoing, working on mapping disparities in lead exposure in children. UKHSA is supporting the research by sharing risk factor information on cases captured through surveillance.
-
UKHSA was approached by the Ministry of Justice to discuss the issue of environmental lead exposure and its association with crime, as identified in a number of research studies (27 to 31). UKHSA recognises the importance of these findings and hope to discuss the possibility of furthering this work with stakeholders.
-
A national audit of lead cases was conducted to explore sources of lead explore and treatment outcomes (13). The findings of this audit will be presented to stakeholders and summary findings will be included in the next annual report.
-
An evaluation of the LEICSS was conducted in 2023 by a UKHSA Field Epidemiology Training Programme Fellow. The findings were reported to the LEICSS surveillance team and the implications will be discussed with the LEPHIS working and steering groups.
-
UKHSA is working with the Georgian National Centre for Disease Control on a research project to identify sources of lead exposure in children. Lead isotope analysis is being used to match blood lead and environmental lead isotopes in spices, food, milk, water, soil, dust and toys as part of a national prevalence study. The study has so far identified spices to be a significant source of lead ingestion and a significant decline in BLC occurred in children after intervention (32 to 34). Further work is in progress.
-
Papers and reports (as detailed below) on the issues of BLC in children and surveillance have been published and reached a wide clinician base. However, LEICSS data has shown the disparity between areas where clinicians are reminded by laboratories to take blood lead samples and those that are not. We are therefore producing letters and guidance materials to send to the Royal Colleges for onward distribution to their members.
Notes
Note 1. Pica is the persistent ingestion of non-nutritive substances at an age where this is developmentally inappropriate.
Note 2. France banned white lead-based interior paint in 1909 (earlier than England); thus exposures from this source would be expected to be lower than in the UK.
Note 3. Both µmol/L and µg/dL units are commonly used internationally to express blood lead concentrations, where 1 µg/dl = 0.0483µmol/L. Divide the concentration in µg/dl by 20.7 to obtain the concentration in µmol/L.
Note 4. HPZone is the public health case management system used in England by UKHSA Health Protection Teams when investigating and managing public health threats to their local populations.
Note 5. HPTs are frontline units responsible for investigating and managing public health threats to their populations.
References
1. Public Health England (2017). Lead: toxicological overview
2. Public Health England (2021). Evaluation of whether to lower the public health intervention concentration for lead exposure in children
3. Etchevers A, and others (2014). Blood lead levels and risk factors in young children in France, 2008 to 2009. International Journal of Hygiene and Environmental Health: volume 217, pages 528 to 537
4. American Academy of Pediatrics Committee on Environmental Health (2005). Lead exposure in children: prevention, detection, and management. Pediatrics: volume 116 number 4, pages 1036 to 1046
5. Rees N and Fuller R (2020). The Toxic Truth: Children’s exposure to lead pollution undermines a generation of future potential. Unicef and Pure Earth.
6. US Centers for Disease Control and Prevention (2021). Blood lead levels (µg/dL) among U.S. children under 72 months of age, by state, year, and blood lead level.
7. Vos T, and others (2020). Global burden of 369 diseases and injuries in 204 countries and territories: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet: volume 396, number 10258, pages 1204 to 1222
8. Tsoi MF, and others (2016).Continual decrease in blood lead level in Americans: United States National Health Nutrition and Examination Survey 1999 to 2014. American Journal of Medicine: volume 129, number 11, pages 1213 to 1218
9. Ruckart PZ, and others (2021). Update of the Blood Lead Reference Value: United States, 2021. Morbidity and Mortality Weekly Report: volume 70 number 43, pages 1509 to 1512
10. WHO (2010). Childhood lead poisoning: pages 1 to 72
11. US Centers for Disease Control and Prevention (2021). CDC updates blood lead reference value for children Press release, 28 October
12. Johnson L, Barlow PJ and Barratt RS (1984). Lead in paint: brushed aside? Journal of the Royal Society of Health: volume 104 number 2, pages 64 to 67
13. Crabbe H, and others (2022). As safe as houses; the risk of childhood lead exposure from housing in England and implications for public health. BMC Public Health volume 22 number 1, page 2052
14. US Centers for Disease Control and Prevention (1991). Preventing lead poisoning in young children
15. Lewendon G, and others (2001). Should children with developmental and behavioural problems be routinely screened for lead? Archives of Disease in Childhood volume 85 number 4, pages 286 to 288
16. Dave M, and others (2023). Lead exposure sources and public health investigations for children with elevated blood lead in England, 2014 to 2022. In press
17. Bazian Ltd (2018). Screening for elevated blood lead levels in asymptomatic children aged 1 to 5 years. In: External review against programme appraisal criteria for the UK National Screening Committee.
18. Public Health England (2018). Surveillance of elevated blood lead in children (SLiC): a British Paediatric Surveillance Unit analysis
19. Crabbe H, and others (2016). Lead poisoning in children: evaluation of a pilot surveillance system in England, 2014 to 2015. In: International Society of Environmental Epidemiology: Environmental Health Perspectives
20. Public Health England (2016). Lead action card: chronic exposures guidance for duty doctors
21. Talbot A, Lippiatt C and Tantry A (2018). Lead in a case of encephalopathy. BMJ Case Reports
22. Loomes R, Hull L and Mandy WPL (2017). What is the male-tofemale ratio in autism spectrum disorder? A systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry: volume 56 number 6, pages 466 to 474
23. Matson JL, and others (2011). Pica in persons with developmental disabilities: Characteristics, diagnosis, and assessment. Research in Autism Spectrum Disorders volume 5 number 4, pages 1459 to 1464.
24. Perry MJ, and others (2021). Pervasive structural racism in environmental epidemiology. Environmental Health: volume 20 number 1, page 119
25. Elliott P, and others (1999). Clinical lead poisoning in England: an analysis of routine sources of data. Occupational and Environmental Medicine: volume 56 number 12, pages 820 to 824
26. Roberts DJ, and others (2022). Lead exposure in children. British Medical Journal: volume 377
27. Boutwell BB, and others (2016). The intersection of aggregate-level lead exposure and crime. Environmental Research: volume 148, pages 79 to 85
28. Naicker N, and others (2018). Is there a relationship between lead exposure and aggressive behavior in shooters? International Journal of Environmental Research and Public Health: volume 15 number 7.
29. Stretesky PB and MJ Lynch (2004). The relationship between lead and crime. Journal of Health and Social Behaviour: volume 45 number 2, pages 214 to 229
30. Taylor MP, and others (2016). The relationship between atmospheric lead emissions and aggressive crime: an ecological study. Environmental Health: volume 15, page 23
31. Wright JP, and others (2021). Developmental lead exposure and adult criminal behavior: A 30-year prospective birth cohort study. Neurotoxicology and Teratology: volume 85
32. Ericson B, and others (2020). Elevated Levels of Lead (Pb) Identified in Georgian Spices. Annals of Global Health: volume 86 number 1, page 124
33. Ruadze E, and others (2021). Reduction in blood lead concentration in children across the Republic of Georgia following interventions to address widespread exceedance of reference value in 2019. International Journal of Environmental Research and Public Health: volume 18 number 22
34. Laycock A, and others (2022). The Use of Pb isotope ratios to determine environmental sources of high blood Pb concentrations in children: a feasibility study in Georgia. International Journal of Environmental Research and Public Health: volume 19 number 22
Resources
The UKHSA launched a free online training course, ‘Tackling lead poisoning in public health’, in July 2021, designed for professionals involved in responding to lead incidents to develop their understanding of lead poisoning and public health policy. A webinar on the importance of lead exposure was held by the Royal College of Paediatrics and Child Health (RCPCH) for training of physicans and paediatrics, which is available on YouTube: ‘Lead Toxicity in Children: a continuing problem’
UKHSA’s Environmental Public Health Surveillance System
The Environmental Public Health Surveillance System (EPHSS) collates and integrates data from selected databases on environmental hazard, exposures and health outcome data. Further details are provided on the EPHSS webpages. A lead exposure in children module incorporated into EPHSS allows for anonymous aggregated LEICSS data to be interrogated and analysed, producing user defined outputs for surveillance reporting purposes. 2021 case data has been added to EPHSS, and 2022 and 2023 will be shortly uploaded. Currently, the EPHSS platform is available to UKHSA staff, but will soon become accessible to external users.
To stay updated with the work of UKHSA’s Environmental Public Health Tracking (EPHT) group and EPHSS, email epht@ukhsa.gov.uk
To find out more about gaining access to LEICSS outputs via EPHSS, email ephss@ukhsa.gov.uk
The LEPHIS Steering group, with The British Paediatric Surveillance Unit (BPSU) and Royal College of Paediatrics and Child Health presented a webinar on lead as part of their series on rare diseases (to raise awareness of LEICSS amongst clinicians). The details of this are listed in the presentations section above.
Further UKHSA resources for the public health management of cases of lead exposure
Lead pages in the UKHSA chemicals compendium
Lead Exposure in Children Surveillance System: Surveillance Reports from 2021
Lead Exposure in Children Surveillance System: Surveillance Reports published before 2021
Duty Doctors Pack- containing Lead Action Card, SOPs and standardised letters and advice (available to UKHSA staff only at present, updated resources following lowering of intervention level)
Health and Safety Executive report on Exposure to lead in Great Britain, 2022. Medical surveillance of blood-lead levels in British workers, 2021/22: Exposure to lead in Great Britain, 2022 (hse.gov.uk)
Resources for clinicians
Clinicians with clinical lead exposure queries should consult TOXBASE or contact the National Poisons Information Service.
Procedures for reporting of lead cases to UKHSA
For adult cases with a BLC of ≥0.48μmol/L (equivalent to ≥10μg/dl): contact the local HPT of the case. HP details can be found on GOV.UK, by entering the cases postcode.
For pregnant women with a BLC of ≥0.24μmol/L (equivalent to ≥5μg/dl): contact the local HPT of the case. HP details can be found on GOV.UK, by entering the cases postcode.
For children aged under 16 years old at the time of first elevated BLC: please report cases to the LEICSS, using lpic@nhs.net
Sources and presentations of lead exposure in children
Important sources of lead exposure in children are as follows:
- deteriorating leaded paint (particularly houses built prior to early 1970s)
- herbal medicinal preparations
- consumer products (if unregulated): medicines, food, spices, ceramic cookware, toys, make-up
- parental hobbies or occupations (including dust on clothing)
- lead water pipes, and lead from drinking water pipe fittings (namely, solder) (particularly houses built prior to early 1970s)
- contaminated soil or land
Children at most risk of lead exposure are as follows:
- children with pica or increased hand to mouth behaviour (for example, children with autism or global developmental delay), particularly with iron deficiency
- children who have recently migrated from countries with less regulation to prevent lead exposure
- children living in older homes and attending older schools containing leaded paint
- children living in more urban or industrial environments
Presentations of lead exposure in children is as follows:
- acute exposure resulting in high BLC: anorexia, abdominal pain, constipation, irritability and reduced concentration, encephalopathy
- chronic exposure
- lower BLCs: mild cognitive and behavioural impairments, may contribute to global developmental delay, decreased academic achievement, IQ, and specific cognitive measures (S); increased incidence of attention-related behaviours and problem behaviours (S), and delayed puberty and decreased kidney function in children ≥12 years of age (L)
- higher BLCs: reduced appetite, abdominal pain, constipation, anaemia, delayed puberty, reduced postnatal growth, decreased IQ, and decreased hearing (S); and increased hypersensitivity or allergy by skin prick test to allergens and increased IgE (L)
Where (S) = sufficient evidence and (L) = limited evidence
Contacts
To notify cases (participating laboratories only), contact: UKHSA.leicss@nhs.net
For general enquiries, contact: epht@ukhsa.gov.uk
For lead surveillance module in UKHSA’s Environmental Public Health Surveillance System, contact: ephss@ukhsa.gov.uk
To notify cases directly to a Health Protection Team in England, identify the relevant HPT by entering the residential postcode of the case into GOV.UK.
Steering and working group members (UKHSA unless otherwise indicated)
LEICSS surveillance team: Araceli Busby (surveillance lead and Chair); Geraldine White; Giovanni Leonardi; Helen Crabbe; Neelam Iqbal; Rebecca Close; Neena George; Priya Mondal; Emma Benham.
LEPHIS Working Group (as above plus the following members): Sarah Dack; Alec Dobney; Lorraine Stewart; Kerry Foxall; Ovnair Sepai; Richard Dunn; Lee Grayson; Tim Marczylo; John Astbury (NIEH); Darren Bagheri; Bernd Eggen.
LEPHIS Steering group (includes the above working group plus the following members): Alan Emond (University of Bristol/British Paediatric Surveillance Unit); Louise Ander (British Geological Survey); Sally Bradberry (National Poisons Information Service, City Hospital, Birmingham); Kishor Raja / Carys Lippiatt (Supra-regional Assay Service Trace Elements laboratories); Andrew Kibble (RCE Wales); Tim Pye (Lead Safe World UK); Rahul Gupta; Jack Gordon-Brown; Geoffrey Mullings.
Acknowledgement to laboratories
NHS Supra-regional Assay Services Trace Elements laboratories: Birmingham; Leeds; Southampton; Guildford; London Charing Cross; London Kings College.
Other laboratories notifying cases included in this report: The Doctors’ Laboratory, London; Cardiff Toxicology Laboratories; Southmead Hospital, Bristol; Alder Hey Children’s Hospital, Liverpool; Royal Liverpool University Hospital; Northern General Hospital, Sheffield; Birmingham Heartlands Hospital; Nottingham University NHS Trust Hospital.
